Abstract
To date, the use of the most suitable first-pass technique for Mechanical Thrombectomy is still debated. In last years, several observational studies have suggested noninferiority or superiority of A Direct Aspiration first-Pass Technique (ADAPT) technique to achieve better reperfusion in comparison to stent retriever. While ASA/AHA 2018 guidelines recommend that patients with AIS should receive Mechanical Thrombectomy with a stent retriever, last European Stroke Organization guidelines report no evidence that stent retriever compared with contact aspiration could improve reperfusion rate. ADAPT is based on aspiration alone as the primary mechanism of thrombectomy and, if initially unsuccessful, then incorporating adjunctive alternatives. ADAPT improvement is also related to last generation of aspiration catheters. The purpose of this review is to report ADAPT principles, technique, efficacy, and safety as first-line treatment for acute ischemic stroke with the latest generation of reperfusion devices.
Keywords: Stroke, interventional, thrombectomy, thromboaspiration, technique
Introduction
Early treatment of acute ischemic stroke (AIS) represents a key point in the management of cerebrovascular patients, being a main factor involved in modifying mortality and long-term clinical outcome.
Treatment of AIS has evolved remarkably in the past decade. Several randomized stroke clinical trials1–5 demonstrated the superiority of mechanical thrombectomy (MT) from large vessel occlusion when compared with the standard intravenous thrombolysis alone in patients with AIS. Most patients in these RCTs were treated with self-expandable stent retriever (SR), which has led many to believe that they represent the gold standard of thrombectomy devices. Nevertheless, clinical experience has reported situations that are resistant to SR recanalization attempts. The technical evolution of stroke devices and techniques during this time period played a significant role, as safer, faster, and more effective treatments could be performed. 6 Some operators, in conjunction with SR, utilized balloon guide catheters (BGCs) to achieve proximal flow arrest to mitigate the likelihood of distal emboli, while others placed a large-bore aspiration catheter immediately adjacent to the deployed SR (“Combined technique”) and removed the SR into the catheter under aspiration to minimize the chance of fragmentation. The growing acceptance of aspiration approach arises questions regarding the safety and efficacy of aspiration thrombectomy techniques as a first-line therapy: compared with other endovascular approaches, the technique of A Direct Aspiration first-Pass Technique (ADAPT) has obtained growing acceptance as it is thought to facilitate a high rate of recanalization, and potentially at lower costs when used alone, and promising clinical results, especially when used in intracranial large vessel occlusions (LVO).6–10
While international guidelines and best level evidence are at least 5-year old, contact aspiration devices are constantly evolving.
The purpose of this review is to report ADAPT principles, technique, efficacy, and safety as first-line treatment for AIS with the latest generation of large-bore reperfusion devices.
Main text
Thromboaspiration—State of the art
To date, the use of the most suitable first-pass technique for MT is still debated.
The aspiration technique has been an early hallmark in the history of MT; since 2009, its use has been demonstrated in a large number of trials and clinical experiences. 7
Randomized clinical trials
Starting from 2016, several observational studies have suggested noninferiority or superiority of the ADAPT technique to achieve better reperfusion rates in comparison to SR.8–11 The Contact Aspiration vs Stent Retriever for Successful Revascularization (ASTER) trial was the first open-label randomized clinical trial to compare efficacy and adverse events using the contact aspiration technique versus the standard stent retriever technique as a first-line endovascular treatment among patients with AIS and large vessel occlusion: successful revascularization defined as a modified Thrombolysis in Cerebral Infarction (mTICI) score of 2b or 3 outcome was not significantly different in the two groups, with no significant difference in the total number of revascularization attempts. Unfortunately, the ASTER trial failed to meet its primary endpoint (defined as the percentage of patients with successful revascularization—mTICI score of 2b or 3 at the end of angiography after all endovascular treatments) of angiographic superiority for aspiration thrombectomy as first-pass: the primary efficacy outcome was not significantly different in the contact aspiration versus stent retriever groups (85.4% [n = 164] vs 83.1% [n = 157]; OR, 1.20; 95% CI, 0.68–2.10; p = .53). As a result, it remained unclear whether the benefit of MT was unique to a single approach-stent retriever as first-line or whether alternate approaches to thrombectomy would have also conferred a clinical benefit. The COMPASS study, 12 published in 2019, was a prospective, multicenter randomized trial assessing the non-inferiority of aspiration thrombectomy as first-pass versus stent retriever for large vessel occlusion. Results of this trail demonstrated that of patients presenting within 6 h of onset for anterior circulation acute large vessel occlusion and an ASPECT greater than 6, those who were treated with a direct aspiration as first-pass thrombectomy had non-inferior functional outcome (modified Rankin Scale 0–2 at 90 days) compared with those treated with a stent retriever as first-line approach: 52% (95% CI 43·8–60.3) in the aspiration group and 50% (41.6–57.4) in the stent retriever group (p non-inferiority = 0.0014), showing that aspiration as first pass was non-inferior to the stent retriever first line approach. Additionally, the final angiographic recanalization categories of TICI 2b or greater, 2c or greater, and 3 were similar for both the cohorts; also, clinical results (NIH Stroke Scale, Stroke Impact Scale, and mortality) were similar. These findings might be partly explained by the ASTER study, which used previous generation of aspiration devices with smaller distal inner diameter (the Penumbra ACE 64), whereas in the COMPASS the Penumbra ACE 68 was mainly used (the largest catheter approved at that time). Notably, thromboaspiration has also been used in combination with SR. Several techniques using the combination of SR and aspiration have been described: Solumbra (which refers to Solitaire (Medtronic Neurovascular, Irvine, CA) and Penumbra combination), 13 ARTS (Aspiration (catheter)-(stent) Retriever Technique for Stroke) 14 and SAVE (Stent retriever Assisted Vacuum-locked Extraction) are some examples. 15 Again, although several observational studies have reported promising results with such a combined approach, no clear superiority over DA has been shown in a RCT. Published studies and RCT suffer from significant heterogeneity in thrombectomy technique. It is important to underline that many SR patients were not in fact SR-only patients but rather patients treated with a combined approach.
International guidelines
The ASA/AHA 2018 guidelines 16 recommend that patients with AIS should receive MT with a SR (Class of Recommendation—COR I Level of evidence-LOE A), that SR represents the first choice (COR IIb LOE B-R) and that a large-bore distal-access catheter, in conjunction with SR may be beneficial (COR IIa LOE C-LD). These guidelines come from trials based on the use of SR as first choice in all cases; in fact, it also reported that more studies should examine which systems provide the highest recanalization rates with the lowest risk for nontarget embolization.1,3,5,17
Conversely, the last European Stroke Organization (ESO) 2019 guidelines report no evidence that SR compared with contact aspiration could improve reperfusion rate, but the majority of experts believe that ADAPT may be used as standard first-line treatment, followed by SR thrombectomy as rescue therapy if needed. These results might be partly due to a cost-effective analysis, as COMPASS trial and other previous non-randomized data 18 demonstrated that total device cost are significantly less with the aspiration first-pass approach, supporting the concept of a cost advantage for contact aspiration.
Thromboaspiration procedure
A Direct Aspiration first-Pass Technique (ADAPT) is based on using aspiration alone as the primary mechanism of thrombectomy and, if initially unsuccessful, then incorporating adjunctive alternatives such as SR to achieve revascularization.
General anesthesia or conscious sedation
Mechanical thrombectomy may be performed either under general anesthesia with intubation or under conscious sedation. Some stroke interventionists prefer general anesthesia with intubation, assuming it may be associated with less pain, anxiety, agitation, movement, and lower risk for aspiration, whereas others favor conscious sedation to save time, evoke less hemodynamic instability, and risk fewer ventilation-associated complications. Up to now, the results of some nonrandomized and a few RCTs showed contradictory results about which method is superior.19,20 Thus, the absence of conclusive evidence, whether general anesthesia or conscious sedation is superior, suggests that the stroke team should choose the preferred method based on their experience. 21
Arterial access
Access to the cerebral vasculature needs at least an 8Fr arterial introducer. The transfemoral approach encompassed different techniques. As a rule, a short 8 or 9 Fr sheath is inserted and a guide catheter or a balloon guide catheter are navigated into the craniocervical vessels over a long 5 Fr angled guide catheter. Groin characteristics such as severe atherosclerotic disease in iliofemoral arteries and prominent groin fat deposits may lead to significant difficulties in safe and effective sheath placement. 22 Abnormalities in the aorta such as dissections and aneurysms, unfolding or unfavorable aortic arch. (e.g., type III arch.), tortuous craniocervical vessel origin and course may also contribute to extreme difficulties to cerebral artery catheterization and may lead to extensive delays in clot engagement during interventional management of AIS. 23 In these conditions, trans-radial approach could improve patient safety and treatment efficacy, as already demonstrated by numerous single-center studies and large randomized trials.24–26 Also trans-ulnar artery access is under investigation for use in patients who cannot undergo trans-radial approach. 27 It is important to appreciate that trans-radial access has a significant learning curve and is said to require commitment prior to obtaining its rewards 28 : cerebral thrombectomy normally requires a relatively high catheter/sheath placement and therefore TRA has been considered not ideal because of its relatively small size, but access with new sheathless guide-catheters could solve this problem and prevent access site complications.
ADAPT technique
The ADAPT consists of a large guide catheter advanced as distally as possible to reach the cervical or proximal petrous segment of the ICA; a balloon guide catheter (BGC) could also be navigated as a guiding catheter into the target proximal cervical vessel (carotid or vertebral artery) for proximal flow arrest. The aspiration catheter of caliber to fit in the vessel is selected for each case (distal ICA or proximal middle cerebral artery); for posterior circulation AIS, an intracranial access system is navigated into the largest-caliber vertebral artery and positioned into the distal V2 vertebral artery segment. The largest-caliber aspiration catheter that the occluded vessel can accommodate is selected for each case.
Under road map guidance (if the patient is under general anesthesia), the reperfusion catheter is advanced in front of the thrombus, coaxially over a microwire and a microcatheter the operator chooses, without crossing the clot. Then, microcatheter and wire are removed and aspiration is applied either manually with a 60 mL syringe or preferable through an aspiration pump system. Aspiration is left for approximately 60/90 s (there is no consensus regarding the optimal duration after suction activation from which the catheter should be removed). Inability to draw back on aspiration confirms optimal position of the aspiration catheter abutting the thrombus. At this point, the catheter is slightly advanced to ensure firm engagement with the thrombus. The aspiration catheter is then slowly withdrawn while maintaining aspiration. Simultaneous manual aspiration/second pump aspiration system is also applied to the sideport of the guide-catheter to prevent dislodging the thrombus from the aspiration catheter’s aperture as it is withdrawn into the sheath. If aspiration fails, the aspiration catheter can be rapidly advanced to the thrombus, at which point a repeat aspiration can be attempted. In smaller-caliber vessels, the technique can similarly be employed with either a smaller inner diameter reperfusion catheter.
ADAPT avoids going beyond the thrombus with microwire/microguide, reducing risk for vessel perforation, dissection (also due to the soft and flexible catheter shaft design) and stripping SAH after SR retrival; moreover, total device cost has been demonstrated to be significantly less with the aspiration first pass approach in comparison with SR first pass.
When aspiration alone does not result in successful revascularization, an SR could be added through the large-bore catheter.
There are several technical variations that deserve mention:
- The choice of aspiration catheter and number of attempts is up to the primary operator; the larger catheter tip lumen fitting the vessel diameter is usually chosen from the available 29 ;
- To speed up the procedure, in some favorable anatomical configurations, last generation of soft-tipped, flexible, braided single lumen aspiration catheters could also be navigated intracranially without a microcatheter (with a .035 wire or even with no device at all), as first reported in the so called SNAKE Technique. 30
- Before suction, the microcatheter should be removed, as it has been shown to influence aspiration force. 31 To avoid fragmentation, microcatheter and microwire should not cross the clot, especially in proximal occlusions (Figure 1); exception could be made if anatomical tortuosities avoid intracranial access for the aspiration catheter: in these cases, distal microcatheter anchorage could be useful for aspiration catheter to reach the clot (Figure 2).
- BGC might improve the final and first-pass recanalization rates 32 : one explanation could be that inflation of the BGC might reduce the systolic blood pressure acting on the proximal clot face, thus enhancing the effect of aspiration. In our experience, the standardized technique based on the use of a proximal large-bore guide-catheter, (Neuron Max 088, Penumbra Inc., CA, USA), could provide both intracranial support for navigation (also in sever tortuosity) and proximal anterograde flow control/arrest due to catheter-induced ICA mechanical vasospasm. It is, however, important to note that the largest aspiration catheters (JET 7, Vecta and React 071 and Sofia Plus) are not compatible with current BGCs.
- As thromboaspiration technology continues to evolve, preliminary experience of intracranial navigation with a 0.088″ large-bore catheter in MT has been recently reported 33 appearing technically feasible and safe.
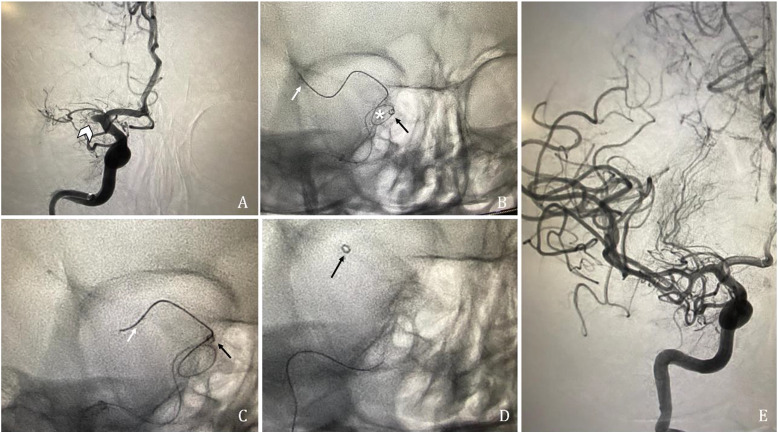
Figure 1.
(A) Acute ischemic stroke with right M1 cerebral artery occlusion (arrowhead). (B, C) Under road map guidance, microwire and a microcatheter (white arrows) are advanced in front of the thrombus, without crossing the clot as the aspiration catheter (black arrows) could be pushed over the co-axial system to reach the thrombus, with no obstacles. (D) Complete reperfusion (mTICI 3) is obtained after a single aspiration pass.
Figure 2.
(A) Same right M1 occlusion as the Figure 1 (arrowhead). (B, C, D) In this case, because of a right carotid siphon coiling (asterix), microcatheter and microwire (white arrows) overcome the clot to stabilize the co-axial system, to allow the aspiration catheter (black arrows) to be navigated over the coiling in front of the thrombus. (E) Complete recanalization is obtained at the first aspiration attempt (mTICI 3).
Emerging thromboaspiration devices
Aspiration force and tip diameter
The concept of ADAPT is to engage the clot, clog the catheter tip, and retrieve the catheter and clot together under negative pressure. The size and composition of the clot on the one hand and suction force at the catheter tip on the other are supposedly the most crucial factors for successful MT with ADAPT. 34 While the length and composition of a clot cannot be influenced, the force at the catheter tip is the product of applied pressure and cross-sectional area of the catheter. Consequently, the catheter with the largest tip diameter will apply the greatest force. Instinctively, one would think it would be best to follow the principle of “the bigger the better” using the largest available catheter, but smaller catheters leave more spare lumen in the access catheter for proximal aspiration and have the advantage of better maneuverability and therefore allow easier and less traumatic access to the occlusion site, even if in distal site. Hence, the ideal catheter is as small as possible and as large as necessary. However, the force needed to engage a given clot is unknown. 35 It is still not clear what are the optimal levels of suction pressure that should be applied to remove thrombi of different sizes, different stiffness, and in different cerebral vessels; what is the exact relation between the suction force produced on the thrombus and them suction distance (i.e., the distance from the suction catheter tip to the thrombus). About the latter, a fluid dynamics study 36 analyzed the suction-force-suction distance relation during aspiration thrombectomy for ischemic stroke and showed the interesting phenomenon that the suction force developed when the catheter tip is 0.1 mm away from the thrombus surface is larger than that when the catheter tip is in full contact with the thrombus surface, under the flow system simulated. This information is important as it will directly influence the operational protocols of the aspiration thrombectomy procedures. From an in vivo animal experiment, Nikoubashman et al. 35 have developed the hypothesis that there is a minimal catheter size required for ADAPT but that larger catheters do not necessarily result in successful recanalization: they calculated that catheters with an inner diameter of 0.040 and 0.064 inch, respectively, are needed to be effective in a MCA occlusion with a diameter of 2.5 mm or in the terminal segment of the internal carotid artery occlusion with a diameter of 4 mm. Because the cross-sectional area increases by the square of the radius, small changes of distal inner diameter result in a large change of force. For instance, a 27% increase of the inner diameter of a 6F catheter compared with a 5F catheter (0.07 vs 0.055 inch) results in a 62% increase of force. A recent study of Yaeger et al. 37 compared various vacuum pumps and examine the aspiration forces they generate as well as the force of catheter tip detachment from an artificial thrombus: the Penumbra Jet Engine pump system generated a higher aspiration pressure than the older-generation Penumbra Max pump, other pump systems (Stryker and Microvention), and manual aspiration with a 60 cc syringe. Using this high vacuum pressure system with various thrombectomy catheters, they confirmed the observation that tip force depends proportionally on tip diameter. The development of aspiration pumps with cyclic or ramp-shaped pressure profiles may allow for improved removal through deformation and rearrangement of the thrombus, possibly resulting in fewer maneuvers and less distal fragmentation.
Last generation of large-bore catheters
The importance for the larger tip inner diameter (ID) for ADAPT efficacy is well-established by the increasing production of new large-bore aspiration catheters in the last few years:
- AXS Vecta (Stryker Neurovascular, Fremont, CA) – 0.074 and 0.071 inch ID;
- JET 7 Reperfusion catheter with Standard Tip (Penumbra, Alameda, CA) – 0.072 inch ID;
- RED 72 (Penumbra, Alameda, CA) – 0.072 inch ID;
- pHLO AC (Phenox GmbH, Bochum, Germany) 0.072 inch ID;
- React 71 (Medtronic Neurovascular, Irvine, CAA) – 0.071 inch ID;
- SOFIA PLUS (Microvention, Terumo, California, USA) – 0.070 inch ID.
In comparing these newest large bore aspiration catheters, similar angiographic efficacy is achieved 38 : all had similar angiographic results after the first (TICI score 2b/3 in 45% of cases) and final pass (TICI score 2b/3 in 92% of cases) with comparable procedural times (mean 28 minutes), procedural complications, and early clinical results. Of potential clinical value, however, React 71 and Vecta 71 were found to be tracked more reliably to the clot over a microcatheter as compared with Jet 7. Intention to treat, final clinical results, and even procedural time for cases treated with Jet 7 were comparable to the other 2 groups. In the majority of cases with Jet 7, a stentriever or alternative catheter was needed to gain access to the clot: this result need to be compared with larger-number of cases as a recent preliminary experience on Jet 7 in T-ICA occlusion 39 demonstrated a low rate of rescue therapy with a SR (5%, n = 1/19 patients) compared to smaller Sofia Plus and ACE68 (0.068 inch ID - Penumbra, Alameda, CA, USA) catheters. Although this new generation of large-bore aspiration catheters appears to be efficient and safe based on recent non-controlled observation studies40,41 navigability and trackability are influenced by their size, especially around the ophthalmic artery in tortuous vessels: in these cases, use of a SR is usually required (“grappling hook technique”) to deliver the aspiration catheter up to the clot level. Further studies are needed to better investigate the efficiency and safety of this new generation of aspiration catheters. No studies are available about RED 72 efficacy; more studies need to be published as only preliminary experiences are available in literature.39,42
Intermediate-bore catheters
Occlusion of smaller arteries, such as the M2 or M3 segments of the middle cerebral artery, pericallosal artery, or the posterior cerebral artery, sometimes causes ischemic strokes with pronounced clinical impact on the patient despite a smaller core infarct volume. The current American Heart Association guidelines recommend treating occlusions of the distal M2-M3 segment with MT in carefully selected patients within 6 h of symptom onset (Class of recommendation 2b). 16 With iterative further advances in catheter technology, distal and medium vessel occlusions (DMVOs) are now emerging as a promising next potential EVT frontier. 43 There are only sporadic studies describing ADAPT as frontline therapy in the distal intracranial vasculature and most of them used intermediate-bore catheters, similar but smaller in size than those catheters routinely applied in large caliber arteries like distal internal carotid artery and M1 segment.44–46 Penumbra 0.041in (4MAX) and 0.054in (5MAX) catheters, 47 Sofia 0.055in (Microvention) 48 and Catalyst 0.058in and 0.060in (respectively, AXS Catalyst 5 and Catalyst 6)44–46 could be considered as “intermediate” aspiration catheters reporting good technical and clinical outcomes for medium/distal vessel occlusions.
In literature, only one retrospective study has directly compared contact aspiration and stent retriever as first-line approach in patients with DMVOs. 49 In this study, the use of a 3 mm stent retriever (Trevo, Stryker Neurovascular, Fremont, CA) compared to 3MAX device (Penumbra, Alameda, CA) resulted in higher rates of first-pass mTICI 2b–3 reperfusion and lower utilization of adjuvant therapy. The ADAPT technique in distal occlusions do not differs from proximal LVOs, despite the microwire need more often to be pushed over the thrombus.
Correlation with clot composition
It has been demonstrated that thrombi retrieved from patients with AIS are highly heterogeneous. The histopathological composition of thrombi contributes to the difficulty in removing clot during MT. 50 Studies indicate that fibrin-rich thrombi (“white thrombi”) are associated with an increased number of recanalization attempts during thrombectomy procedure and increased resistance to thrombolysis compared to red blood cell-rich thrombus (“red thrombi”).51,52 The enhanced efficacy of recanalizing RBC-rich thrombi may be attributed to its physical characteristics, which exhibit decreased stiffness and increased deformability compared to white clots. 53 The increasing presence of fibrin within the white thrombus makes the clot stiffer and less elastic, thus reducing the likelihood of successful engagement and interaction with thrombectomy devices. That’s why in cases of inelastic, organized, fibrin-rich thrombi, aspiration should be considered the first choice (cohesive clot: lower risk of clot stripping during aspiration), while for SR could be harder to incorporate the clot. On the other hand, in cases of fresh, elastic, soft RBC-rich clot, aspiration should be obtained with the larger aspiration catheter to avoid clot fragmentation/stripping, or a combined technique should be preferred. 54
Conclusion
Mechanical thrombectomy using ADAPT could be considered a valid approach for AIS, as reported by last RCTs and International Guidelines. In spite of the recent increasing popularity of ADAPT, the data supporting this technique is not yet as mature as that available on stent retrievers. Last generation of large aspiration catheters may be more effective in removing clot but have yet to be evaluated in RCTs.
Appendix.
Abbreviations
- ADAPT
A direct aspiration first-pass technique
- AIS
Acute ischemic stroke
- SR
Stent retriever
- MT
Mechanical thrombectomy
- GBCs
Balloon guide catheters
- LVO
Large vessel occlusions
- mTICI
Modified thrombolysis in cerebral infarction
- ESO
European stroke organization
- TRA
Trans-radial approach
- ID
Inner diameter
- DMVOs
Distal and medium vessel occlusions
Footnotes
Author contributions: Made substantial contributions to conception and design of the study and performed data analysis and interpretation: F.G.; performed data acquisition, F.G., F.D, D.G.R.; provided administrative, technical, and material support: F.G., R.D.G., R.S.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Giulia Frauenfelder https://orcid.org/0000-0001-5912-3345
Francesco Diana https://orcid.org/0000-0002-3245-917X
References
- 1.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. [DOI] [PubMed] [Google Scholar]
- 3.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 5.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 6.Spiotta AM, Kyle M, Fargen KM, et al. ADAPT: a direct aspiration first pass technique. Endovascular Today 2016; 15(2): 68–70. [Google Scholar]
- 7.Grunwald IQ, Walter S, Papanagiotou P, et al. Revascularization in acute ischaemic stroke using the penumbra system: the first single center experience. Eur J Neurol 2009; 16: 1210–1216. DOI: 10.1111/j.1468-1331.2009.02750.x. [DOI] [PubMed] [Google Scholar]
- 8.Lapergue B, Blanc R, Guedin P, et al. A direct aspiration, first pass technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. AJNR Am J Neuroradiol 2016; 37: 1860–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stapleton CJ, Torok CM, Patel AB. 110 noninferiority of a direct aspiration first-pass technique vs stent retriever thrombectomy in emergent large-vessel intracranial occlusions. Neurosurgery 2016; 63(suppl 1): 146–147. [DOI] [PubMed] [Google Scholar]
- 10.Romano DG, Frauenfelder G, Casseri T, et al. Efficacy of ADAPT with large-bore reperfusion catheter in anterior circulation acute ischemic stroke: a multicentric Italian experience. Radiol Med 2020; 125(1): 57–65. DOI: 10.1007/s11547-019-01069-x. [DOI] [PubMed] [Google Scholar]
- 11.Turk AS, Turner R, Spiotta A, et al. Comparison of endovascular treatment approaches for acute ischemic stroke: cost effectiveness, technical success, and clinical outcomes. J Neurointerventional Surg 2015; 7(9): 666–670. [DOI] [PubMed] [Google Scholar]
- 12.Turk AS, 3rd, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet 2019; 393(10175): 998–1008. DOI: 10.1016/S0140-6736(19)30297-1. [DOI] [PubMed] [Google Scholar]
- 13.Humphries W, Hoit D, Doss VT, et al. Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerventional Surg 2015; 7: 90–94. [DOI] [PubMed] [Google Scholar]
- 14.Massari F, Henninger N, Lozano JD, et al. ARTS (aspiration-retriever technique for stroke): initial clinical experi ence. Intervent Neuroradiol 2016; 22: 325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maus V, Behme D, Kabbasch C, et al. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol 2018; 28: 327–338. [DOI] [PubMed] [Google Scholar]
- 16.Powers WJ, Rabinstein AA, Ackerson T, et al. American Heart Association Stroke Council. guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 2018; 49(3): e46–e110. DOI: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 17.Zaidat O, Castonguay AC, Nogueira RG, et al. TREVO stent-retriever mechanical thrombectomy for acute ischemic stroke secondary to large vessel occlusion registry. J Neurointerventional Surg 2018; 10(6): 516–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Comai A, Haglmuller T, Ferro F, et al. Sequential endovascular thrombectomy approach (SETA) to acute ischemic stroke: preliminary single-centre results and cost analysis. Radiol Med 2015; 120: 655–661. [DOI] [PubMed] [Google Scholar]
- 19.Berkhemer OA, van den Berg LA, Fransen PS, et al. The effect of anesthetic management during intra-arterial therapy for acute stroke in MR CLEAN. Neurology 2016; 87: 656–664. DOI: 10.1212/WNL.0000000000002976. [DOI] [PubMed] [Google Scholar]
- 20.Schönenberger S, Uhlmann L, Hacke W, et al. Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA 2016; 316: 1986–1996. DOI: 10.1001/jama.2016.16623. [DOI] [PubMed] [Google Scholar]
- 21.Papanagiotou P, Ntaios G. Endovascular thrombectomy in acute ischemic stroke. Circ Cardiovasc Interv 2018; 11(1): e005362. DOI: 10.1161/CIRCINTERVENTIONS.117.005362. [DOI] [PubMed] [Google Scholar]
- 22.Haussen DC, Nogueira RG, DeSousa KG, et al. Transradial access in acute ischemic stroke intervention. J Neurointerventional Surg 2016; 8(3): 247–250. DOI: 10.1136/neurintsurg-2014-011519. [DOI] [PubMed] [Google Scholar]
- 23.Ribo M, Flores A, Rubiera M, et al. Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J Neurointerventional Surg 2013; 5(Suppl 1): i70–i73. [DOI] [PubMed] [Google Scholar]
- 24.Liu Y, Wen X, Bai J, et al. A single-center, randomized, controlled comparison of the transradial vs transfemoral approach for cerebral angiography: a learning curve analysis. J Endovasc Ther 2019; 26(5): 717–724. [DOI] [PubMed] [Google Scholar]
- 25.Romano DG, Frauenfelder G, Tartaglione S, et al. Trans-radial approach: technical and clinical outcomes in neurovascular procedures. CVIR Endovasc 2020; 3(1): 58. DOI: 10.1186/s42155-020-00152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fischman AM, Swinburne NC, Patel RS. A technical guide describing the use of transradial access technique for endovascular interventions. Tech Vasc Intervent Radiol 2015; 18(2): 58–65. DOI: 10.1053/j.tvir.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 27.Barros G, Bass DI, Osbun JW, et al. Left transradial access for cerebral angiography. J Neurointerventional Surg 2020; 12(4): 427–430. [DOI] [PubMed] [Google Scholar]
- 28.Mendiz OA, Sampaolesi AH, Londero HF, et al. Initial experience with transradial access for carotid artery stenting. Vasc Endovasc Surg 2011; 45: 499–503. [DOI] [PubMed] [Google Scholar]
- 29.Pampana E, Fabiano S, De Rubeis G, et al. Tailored vessel-catheter diameter ratio in a direct aspiration first-pass technique: is it a matter of caliber? AJNR Am J Neuroradiol 2021; 42(3): 546–550. DOI: 10.3174/ajnr.A6987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heit JJ, Wong JH, Mofaff AM, et al. Sofia intermediate catheter and the SNAKE technique: safety and efficacy of the Sofia catheter without guidewire or microcatheter construct. J Neurointerventional Surg 2018; 10(4): 401–406. DOI: 10.1136/neurintsurg-2017-013256. [DOI] [PubMed] [Google Scholar]
- 31.Nikoubashman O, Alt JP, Nikoubashman A, et al. Optimizing endovascular stroke treatment: removing the microcatheter before clot retrieval with stent-retrievers increases aspiration flow. J Neurointerventional Surg 2017; 9: 459–462. [DOI] [PubMed] [Google Scholar]
- 32.Kang D-H, Kim BM, Heo JH, et al. Effect of balloon guide catheter utilization on contact aspiration thrombectomy. J Neurosurg 2018; 131: 1–7. [DOI] [PubMed] [Google Scholar]
- 33.Nogueira RG, Mohammaden MH, Al-Bayati AR, et al. Preliminary experience with 088 large bore intracranial catheters during stroke thrombectomy. Intervent Neuroradiol 2020; 22: 1591019920982219. DOI: 10.1177/1591019920982219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turk AS, Spiotta A, Frei D, et al. Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerventional Surg 2014; 6: 231–237. [DOI] [PubMed] [Google Scholar]
- 35.Nikoubashman O, Nikoubashman A, Busen M, et al. Necessary catheter diameters for mechanical thrombectomy with ADAPT. AJNR 2017; 38: 2277–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi Y, Cheshire D, Lally F, et al. Suction force-suction distance relation during aspiration thrombectomy for ischemic stroke: a computational fluid dynamics study. Physics in Medicine 2017; 3: 1–8. DOI: 10.1016/j.phmed.2016.11.001. [DOI] [Google Scholar]
- 37.Yaeger K, Iserson A, Singh P, et al. A technical comparison of thrombectomy vacuum aspiration systems. J Neurointerventional Surg 2020; 12(1): 72–76. DOI: 10.1136/neurintsurg-2019-014929. [DOI] [PubMed] [Google Scholar]
- 38.Gross BA, Jadhav AP, Jovin TG, et al. Clinical comparison of new generation 0.071-inch and 0.072-inch aspiration catheters. World Neurosurg 2019; 130: e463–e466. DOI: 10.1016/j.wneu.2019.06.120. [DOI] [PubMed] [Google Scholar]
- 39.Romano DG, Frauenfelder G, Diana F, et al. JET 7 catheter for direct aspiration in carotid T occlusions: preliminary experience and literature review. Radiol Med 2022; 127: 330–340. DOI: 10.1007/s11547-022-01451-2. [DOI] [PubMed] [Google Scholar]
- 40.Hassan A, Fifi J, Zaidat O. Efficacy and safety of mechanical thrombectomy using larger bore jet 7 aspiration catheters for intracranial large vessel occlusion. J NeuroIntervent Surg 2019; 11: A126. [Google Scholar]
- 41.Satti S, Sivapatham T, Almallouhi E, et al. Vecta 071 and 074 large bore aspiration catheter: initial multi-center experience. J NeuroIntervent Surg 2019; 11: A114–A115. [Google Scholar]
- 42.Almallouhi E, Anadani M, Al Kasab S, et al. Initial experience in direct aspiration thrombectomy using a novel 0.071-inch aspiration catheter. World Neurosurg 2019; 126: 272–275. DOI: 10.1016/j.wneu.2019.03.055. [DOI] [PubMed] [Google Scholar]
- 43.Saver JL, Chapot R, Agid R, et al. Distal thrombectomy summit group*†. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke 2020; 51(9): 2872–2884. DOI: 10.1161/STROKEAHA.120.028956. [DOI] [PubMed] [Google Scholar]
- 44.Grieb D, Schlunz-Hendann M, Brinjikji W, et al. Mechanical thrombectomy of M2 occlusions with distal access catheters using ADAPT. J Neuroradiol 2019; 46(4): 231–237. [DOI] [PubMed] [Google Scholar]
- 45.Chartrain AG, Kellner CP, Morey JR, et al. Aspiration thrombectomy with off-label distal access catheters in the distal intracranial vasculature. J Clin Neurosci 2017; 45: 140–145. [DOI] [PubMed] [Google Scholar]
- 46.Romano DG, Frauenfelder G, Caragliano A, et al. Multicentric experience with an intermediate aspiration catheter for distal M2 ischemic stroke. J Stroke Cerebrovasc Dis 2020; 29(12): 105389. DOI: 10.1016/j.jstrokecerebrovasdis.2020.105389. [DOI] [PubMed] [Google Scholar]
- 47.Vargas J, Spiotta AM, Fargen K, et al. Experience with a direct aspiration first pass technique (ADAPT) for thrombectomy in distal cerebral artery occlusions causing acute ischemic stroke. World Neurosurg 2017; 99: 31–36. [DOI] [PubMed] [Google Scholar]
- 48.Stampfl S, Kabbasch C, Muller M, et al. Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: clinical safety and efficacy. J Neurointerventional Surg 2016; 8: 714–718. [DOI] [PubMed] [Google Scholar]
- 49.Haussen DC, Eby B, Al-Bayati AR, et al. A comparative analysis of 3MAX aspiration versus 3 MM trevo retriever for distal occlusion thrombectomy in acute stroke. J Neurointerventional Surg 2020; 12: 279–282. [DOI] [PubMed] [Google Scholar]
- 50.Yuki I, Kan I, Vinters HV, et al. The impact of thromboemboli histology on the performance of a mechanical thrombectomy device. AJNR Am J Neuroradiol 2012; 33: 643–648. DOI: 10.3174/ajnr.A2842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sporns PB, Hanning U, Schwindt W, et al. Ischemic stroke: histological thrombus composition and pre-interventional CT attenuation are associated with intervention time and rate of secondary embolism. Cerebrovasc Dis 2017; 44: 344–350. DOI: 10.1159/000481578. [DOI] [PubMed] [Google Scholar]
- 52.Nam HS, Lee KY, Kim YD, et al. Failure of complete recanalization is associated with poor outcome after cardioembolic stroke. Eur J Neurol 2011; 18: 1171–1178. DOI: 10.1111/j.1468-1331.2011.03360. [DOI] [PubMed] [Google Scholar]
- 53.Jolugbo P, Ariëns RAS. Thrombus composition and efficacy of thrombolysis and thrombectomy in acute ischemic stroke. Stroke 2021; 52(3): 1131–1142. DOI: 10.1161/STROKEAHA.120.032810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mehta BP, Nogueira RG. Should clot composition affect choice of endovascular therapy? Neurology 2012; 79(13 Suppl 1): S63–S67. [DOI] [PubMed] [Google Scholar]