Abstract
Introduction
Occiput posterior (OP) position rates at birth are 5%–8% in studies mainly comprising white European women. The anthropoid pelvis is common in black African women. This pelvic shape has a narrow anterior segment and an ample room posteriorly. The fetal head is wider posteriorly, and the OP position may be favorable in women with an anthropoid pelvic shape. We aimed to examine the fetal rotation with ultrasound longitudinally during the active phase of labor in a sub‐Saharan population. We also aimed to examine associations between fetal position, delivery mode, and duration of labor.
Material and Methods
The study was conducted at Kilimanjaro Christian Medical Centre in Moshi, Tanzania from the 19th of November 2023 to 13th of April 2024. Women with a single fetus in cephalic presentation, gestational age >37 weeks, without previous or pre‐labor cesarean section were eligible. Fetal position was classified as occiput anterior (OA) from 10 to 2 o'clock, occiput transverse (OT) at 3 or 9 o'clock, and OP position from 4 to 8 o'clock.
Results
The study participants comprised 215 women. Fetal positions at admission, in the first and second stage of labor and at birth are presented in the graphical figure. In all, 65/215 (30.2%) fetuses were in OP position at admission, 59/204 (28.9%) in the first stage, 38/210 (18.1%) in the second stage and 35/215 (16.3%) were delivered in OP position. The OP rates at birth were 25/92 (27.2%) in nulliparous and 10/123 (8.1%) in parous women. The operative delivery rate was 10/157 (6.4%) in women with ultrasound assessed fetal position as OA in the second stage (six cesarean section and four vacuum extractions), and 28/48 (58.3%) in the non‐OA group (27 cesarean section and one vacuum extraction) (p < 0.01). The hazard ratio for delivery in the second stage was 0.26 (95% CI 0.13–0.52) for the non‐OA vs the OA group in nulliparous women and 0.25 (95% CI 0.12–0.52) in parous women.
Conclusions
The persistent OP position rate at birth was higher than previously reported, and the operative intervention rate was nine time higher in women with the fetus in non‐OA vs OA position in the second stage.
Keywords: birth, cesarean, maternity care, obstetrics, ultrasound
The persistent OP position rate at birth was higher than usually reported, and the operative intervention rate was very high in women with OP positions in the second stage of labor. Fetal position (entire population) at admission (n = 215), active first stage (n = 204; 11 admitted in the second stage), second stage (n = 210; 5 delivered by cesarean in active first stage), and at delivery (n = 215). Occiput anterior position (light blue), occiput transverse position (red), occiput posterior position (green), missing information (dark blue).

Abbreviations
- HR
hazard ratio
- OA
occiput anterior
- OASIS
obstetric anal sphincter injuries
- OP
occiput posterior
- OT
occiput transverse
Key message.
Fewer fetuses rotated from occiput posterior to occiput anterior position than usually reported, leading to a high rate of persistent occiput posterior position at birth, especially in nulliparous women. Occiput posterior and occiput transverse position in the second stage of labor were associated with a very high cesarean section rate.
1. INTRODUCTION
Fetal occiput posterior (OP) position at admission or in early labor occurs in more than 30% of women,1, 2, 3, 4 but most fetuses rotate to the occiput anterior (OA) position during labor.1, 5, 6 Persistent OP position may be defined as OP position persisting in the second stage of labor, 7 or as OP position persisting until delivery. 8 The OP position rates based on ultrasound examinations after full cervical dilatation have been found to range from 14% to 27%.3, 9, 10 and another study found the OP position rate based on clinical examinations in nulliparous women to be 13%. 11 The overall OP position rate at delivery in studies mainly comprising white European women has been reported to be 5%–8%.12, 13, 14, 15, 16, 17 Higher rates are found in nulliparous women than in parous women,16, 17 and in women with epidural analgesia. 18 Persistent OP position is associated with longer duration of labor, increased rates of cesarean section, instrumental vaginal delivery, obstetrical anal sphincter injury (OASIS), postpartum hemorrhage, and adverse neonatal outcomes.5, 14, 15, 16, 18, 19, 20 Most previous studies have reported labor outcomes associated with the position of the newborn at birth rather than the position of the fetus during labor, which limits the clinical implications.12, 13, 14, 15
Fetal position can be determined with ultrasound,1, 2, 3, 21, 22 which is a more precise method than clinical assessments,23, 24, 25, 26, 27 and some studies have investigated fetal rotation longitudinally with ultrasound.3, 9, 10, 18, 28
The human birth canal varies among ethnic groups, and the shape of the birth canal influences the possibility of fetal rotation.29, 30 The normal labor and birth presented in obstetrical literature is modeled from white European women, 31 but disparities in obstetrical outcome and care exist among ethnicities. 32 The anthropoid pelvis is more common in black African women. 33 A study from 1938 reported the frequencies of anthropoid pelvis being around 40% in black women and around 25% in white women. 34 A previous study demonstrated persistent OP position to be more common in black African‐American women. 17 In this study, we aimed to examine the fetal rotation with ultrasound longitudinally during the active phase of labor in a sub‐Saharan population. We also aimed to examine associations between fetal position, delivery mode and duration of labor.
2. MATERIAL AND METHODS
We conducted a longitudinal cohort study at Kilimanjaro Christian Medical Centre (KCMC), a public‐private partnership zonal consultant hospital in Moshi municipal in the Kilimanjaro region, Tanzania The study was conducted from the 19th of November 2023 to the 13th of April 2024. Women were informed about the study at admission to the labor ward and gave consent before inclusion.
Women with a single fetus in cephalic presentation, gestational age >37 weeks, without a previous or a pre‐labor cesarean section were eligible for the study. Other prerequisites for inclusion included a live fetus, without known anomalies, normal cardiotocography at admission, no suspicion of chorioamnionitis (temperature at admission <38°), or other conditions requiring immediate delivery. Women with a cesarean section in the latent phase were excluded. The inclusion was nonconsecutive depending on a competent ultrasound examiner available. Gestational age was calculated from the first day of the last menstrual period and by ultrasound in the first trimester in women with uncertain last periods.
The first ultrasound examination was done during admission. Women admitted in the latent phase had a second scan when diagnosed to be in the active phase of labor. In this project, the active stage of labor was defined when contractions were regular, and the cervix dilated five centimeters. The third ultrasound examination was done when the cervix was fully dilated. Fetal position, cervical dilatation, effacement, and fetal station were examined clinically by the midwife at the same time as the ultrasound examinations were done. Fetal station was classified from −5 to +5. Three medical doctors did the ultrasound examinations. They had previous experience in fetal sonography during pregnancy, and the last author spent one week training them in transabdominal intrapartum ultrasound before the start of the study. The training followed the guidelines from the international society of ultrasound in obstetrics and gynecology (ISUOG). 35 The ultrasound examiners were not informed about the clinical findings and not involved in clinical decisions. The clinicians did not observe the ultrasound examinations and were not informed about the ultrasound findings. Clinical follow‐up was based on the clinical assessments and the established guidelines in the department. Prolonged first stage of labor was defined when cervical dilatation crossed the action line displaced 4 h from the alert line in accordance with previous recommendations from the World Health Organization, 36 and duration of the second stage of labor should not exceed 2 h in nulliparous women and 1 h in parous women. Vacuum extraction is only occasionally used in this labor ward. The women must consent before the procedure, and they often refuse. The staff has limited experience in vacuum extractions. Manual rotation is not used.
A Voluson S8 (Zipf, Austria) with a 3D transabdominal multifrequency transducer (2–8 MHz) was used at the reception for examinations of women admitted in the latent phase, and a Mindray DP‐30 (Shenzhen, China) with a 2D transabdominal multifrequency transducer (2–6 mHz) was used in the labor ward.
Fetal head position was classified like a clock phase with hourly divisions; and categorized into eight sectors: 11–1 o'clock as OA, 2 o'clock as left occiput anterior; 3 o'clock as left occiput transverse, 4 o'clock as left occiput posterior, 5–7 o'clock as OP, 8 o'clock as right occiput posterior, 9 o'clock as right occiput transverse and 10 o'clock as right occiput anterior position. For a simpler presentation of results, we merged groups and classified them into three groups, OA from 10 to 2 o'clock, occiput transverse (OT) at 3 or 9 o'clock and OP position from 4 to 8 o'clock. 35 The orbits, intracranial structures, the head midline, the fetal spine, and the choroid plexus were used to determine the head position with ultrasound. Head circumference and abdominal circumference were measured by ultrasound at admission and fetal weight was estimated using Hadlock's formula. The amniotic fluid index was calculated in women admitted in the latent phase.
The main outcome measures were fetal rotation, delivery mode, time spent in active labor in the hospital, and duration of the second stage of labor. Secondary outcomes were perineal tears, Apgar score, and admission to the newborn intensive care unit.
Currently, women must pay 40 US dollars for a vaginal delivery at the hospital, and 140 US dollars for a cesarean section. Epidural analgesia is not offered during childbirth.
2.1. Sample size calculation
The sample size calculation was based on the operative delivery rate in the persistent OP position in the second stage of labor. In another study that assessed the impact of OP position in the second stage of labor, the operative delivery rates were 69% vs. 41% in OP and OA positions, respectively. 11 The study included mainly white European nulliparous women with epidural analgesia and a high rate of operative vaginal deliveries, very different from our population. We were not able to find any relevant publication from a black African population without epidural analgesia and decided to use these numbers in the sample size calculation. We assumed an allocation ratio of 70:20:10 between OA:OP:OT in the second stage of labor. Using a power of 80% and alfa 0.05, 207 women should be included. We supposed that some women would be delivered by cesarean section during the first stage of labor and decided to include 215 women in the study.
2.2. Statistical analyses
Fetal rotation is presented as a change in fetal position during labor. Categorical variables were analyzed with a chi‐square test. The time spent in active labor in OA, OT, and OP groups was first compared using one‐way ANOVA and thereafter estimated with Kaplan–Meier survival analyses and compared with log‐rank test. Women were categorized into OA (10–2 o'clock) or non‐OA (3–9 o'clock) position in the second stage of labor due to few women with the fetus in OT position in the second stage. The probability of delivery is illustrated with 1‐survival plots, and cesarean sections and vacuum deliveries were interval censored. The duration of the second stage ≥120 min was right censored in second‐stage analyses. Two hours was the upper limit for the second stage duration in accordance with local guidelines. The hazard ratio (HR) as an estimate of the relative risk of delivery in the second stage of labor was calculated using Cox regression analyses, with OA position as reference. Maternal age, gestational age, body mass index, and estimated birthweight >3500 g were considered as possible confounders and included in multivariable regression analyses. Oxytocin augmentation was considered as a mediator and not as a possible confounder. The assumptions of proportional hazards for the Cox regression analyses were checked using log minus log plots. p‐value <0.05 was considered significant and data were analyzed with the Statistical Package for Social Science (SPSS) version 25.0.
3. RESULTS
3.1. Study population
In all, 889 women delivered at the hospital during the study period. The study population comprised 215 women; 92 nulliparous women, 53 women were para 1, 42 were para 2, 18 were para 3, nine women were para 4 and one woman was para 6. A flow chart of the study population is presented in Figure 1. The ethnicity was black African in all women included in the study. Four (1.9%) women had no formal education, 29 (13.5%) were educated in primary school, 64 (29.8%) in secondary school and 118 (54.9%) at a college or university. The labor was induced in 32/215 (14.9%) women. Eighty‐eight women were admitted in the latent phase, 116 in the active first stage of labor, and 11 in the second stage of labor. Maternal characteristics, labor characteristics, and interventions during labor are presented in Table 1.
FIGURE 1.
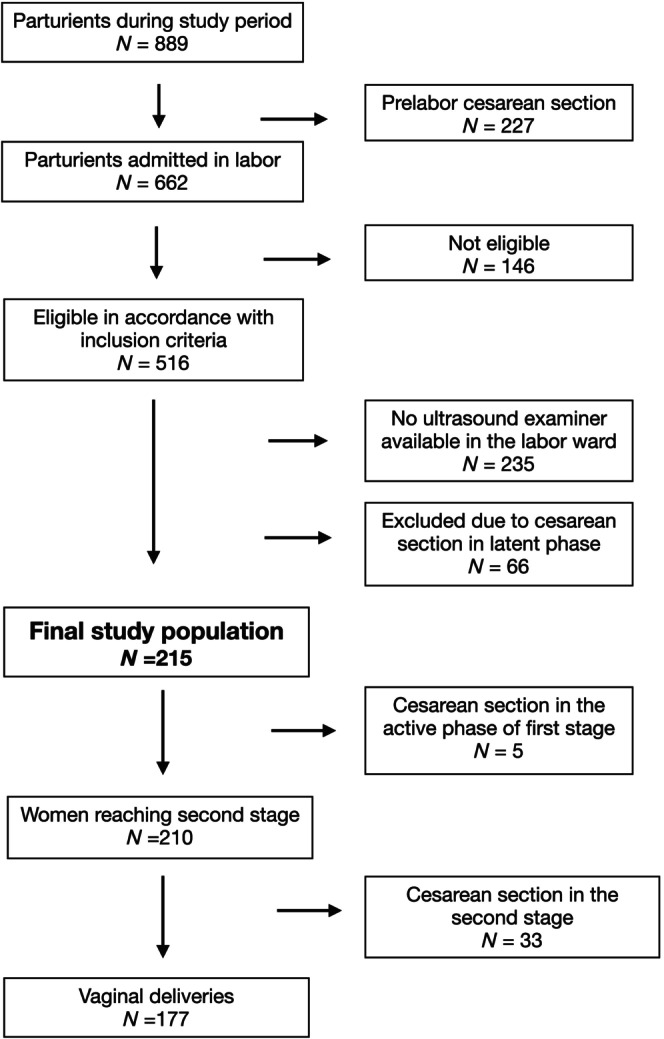
Flow chart of the study population.
TABLE 1.
Maternal and labor characteristics differentiated into fetal position at admission.
| OA | OT | OP | |
|---|---|---|---|
| mean (SD) or n (%) | |||
| n = 92 | n = 58 | n = 65 | |
| Maternal characteristics | |||
| Maternal age (year) | 30 (5.5) | 28 (5.6) | 29 (5.5) |
| Gestational age (days) | 275 (8.9) | 274 (8.8) | 276 (7.4) |
| BMI at admission (kg/m2) | 30.5 (4.7) | 28.5 (4.4) | 29.8 (4.5) |
| Induced labor | 12 (13.0) | 10 (17.2) | 10 (15.4) |
| Admitted in active labor phase | 59 (64.1) | 32 (55.2) | 36 (55.4) |
| Ruptured membranes (latent phase) | 2 (2.2) | 1 (1.7) | 3 (4.6) |
| Clinical findings at admission | |||
| Cervical dilatation (cm) | 5.7 (2.4) | 5.1 (2.3) | 5.1 (2.5) |
| Cervical effacement (%) | 72 (20) | 68 (21) | 66 (25) |
| Station | −0.7 (1.2) | −1.0 (0.8) | −1.2 (1.0) |
| Ultrasound findings at admission | |||
| Amniotic fluid index (latent phase) | 11.2 (3.5) | 11.8 (3.0) | 11.2 (3.7) |
| Estimated fetal weight (g) | 3215 (616) | 3078 (718) | 3439 (445) |
| Interventions during labor | |||
| Oxytocin augmentation | 61 (66.3) | 46 (79.3) | 54 (83.1) |
| Episotomy | 6 (6.5) | 4 (6.9) | 11 (16.9) |
3.2. Fetal rotation
Ultrasound examinations of fetal positions at admission, in the active first stage of labor, and in the second stage of labor differentiated into eight sectors, are presented in Table 2. Fetal positions at the ultrasound examinations and at birth differentiated into OA, OT, or OP positions, are presented in Figure 2. In all, 65/215 (30.2%) fetuses were in OP position at admission, 59/204 (28.9%) in the first stage, 38/210 (18.1%) were in OP position in the second stage and 35/215 (16.3%) were born in OP position. Corresponding OP position rates in nulliparous women were 39/92 (42.4%), 34/87 (39.1%), 26/89 (29.2%), and 25/92 (27.2%), and in parous women 26/123 (21.1%), 25/117 (21.4%), 12/121 (9.9%), and 10/123 (8.1%), respectively. Fetal position could be determined with ultrasound in all cases at admission and in the first stage of labor, but failed in five women in the second stage, leading to missing information in these women in the second stage.
TABLE 2.
Fetal positions differentiated into eight sectors.
| Admission n = 215 | Active first stage n = 204 | Second stage n = 210 | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Occiput anterior | 21 (9.8) | 14 (6.9) | 85 (40.5) |
| Left occiput anterior | 25 (11.6) | 26 (12.7) | 23 (11.0) |
| Left occiput transverse | 28 (13.0) | 21 (10.3) | 4 (1.9) |
| Left occiput posterior | 19 (8.8) | 20 (9.8) | 8 (3.8) |
| Occiput posterior | 24 (11.2) | 16 (7.8) | 22 (10.5) |
| Right occiput posterior | 22 (10.2) | 23 (11.3) | 8 (3.8) |
| Right occiput transverse | 30 (14.0) | 32 (15.7) | 6 (2.9) |
| Right occiput anterior | 46 (21.4) | 52 (25.5) | 49 (23.3) |
| Not determined | 0 | 0 | 5 (2.4) |
FIGURE 2.
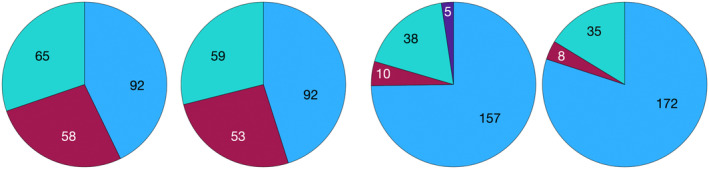
Fetal position (entire population) at admission (n = 215), active first stage (n = 204; 11 admitted in the second stage), second stage (n = 210; 5 delivered by cesarean in first stage), and at delivery (n = 215). Occiput anterior position (light blue), occiput transverse position (red), occiput posterior position (green), missing information (dark blue).
At admission, 92 fetuses were in the OA position, 87/92 (94.6%) remained in the OA position in the second stage, 2/92 (2.2%) rotated to OT, and 2/92 (2.2%) rotated to the OP position. Fifty‐eight fetuses were in OT position at admission; 8/58 (13.8%) remained in OT position in the second stage, 38/58 (66.5%) rotated to OA, and 8/58 (13.8%) rotated to OP position. Sixty‐five fetuses were in OP position at admission, 28/65 (38.5%) remained in OP, and 32/65 (49.2) rotated to OA position. The mean fetal station assessed clinically at admission was −0.7 (SD 1.2) in the OA group, −1.0 (SD 0.8) in the OT group, and −1.2 (SD 1.0) in the OP group.
Five fetuses were delivered by cesarean section in the first stage of labor, one in OT position and four in OP position. All 157 fetuses in OA position in the second stage were delivered in OA position. The five fetuses with missing information in the second stage were all delivered in OA position. Ten fetuses were in OT position in the second stage, 3/10 (30.0%) rotated to OA and 7/10 (70.0%) remained in OT position at delivery. All the fetuses in OT position at delivery were delivered by cesarean section. Thirty‐eight fetuses were in OP position in the second stage of labor, of whom 7/38 (18.4%) rotated to OA and 31/38 (81.6%) were delivered in OP position. All together 35/215 (16.3%) fetuses were in OP position at delivery. The mean fetal station assessed clinically in the beginning of the second stage was +1.1 (SD 0.8) in OA group, +0.7 (SD 0.8) in the OT group and +0.6 (0.8) in the OP group.
3.3. Delivery mode
In all, 38/215 (17.7%) were delivered by cesarean section during the active labor phase, five (2.3%) in the first stage of labor, and 33 (15.3%) in the second stage of labor. The intrapartum cesarean delivery rate was 8.7%, 17.2%, and 30.8% in the OA, OT, and OP groups at admission, respectively (p < 0.01). Labor outcomes are presented in Table 3.
TABLE 3.
Labor outcomes differentiated into fetuses presenting in OA, OT or OP position at admission.
| OA | OT | OP | p‐value | |
|---|---|---|---|---|
| mean (SD or 95% CI) or n (%) | ||||
| n = 92 | n = 58 | n = 65 | ||
| Delivery mode | ||||
| Cesarean (all) | 8/92 (8.7) | 10/58 (17.2) | 20/65 (30.8) | <0.01 |
| Cesarean nulliparous (n = 92) | 6/24 (25.0) | 8/29 (27.6) | 14/39 (35.9) | 0.61 |
| Cesarean parous (n = 123) | 2/68 (2.9) | 2/29 (6.9) | 6/26 (23.1) | <0.01 |
| Vacuum extractions (all) | 2 (2.2) | 0 | 3 (4.6) | N/A |
| Vacuum extractions nulliparous | 0 | 0 | 3/39 (7.7) | |
| Vacuum extractions parous | 2/68 (2.9) | 0 | 0 | |
| Actual time in active labor (minutes) | ||||
| All women | 195 (163–227) | 246 (203–289) | 288 (242–333) | <0.01 |
| Nulliparous | 255 (196–315) | 260 (191–329) | 307 (256–358) | 0.35 |
| Parous | 174 (136–212) | 231 (176–287) | 258 (170–347) | 0.06 |
| Estimated time in active labor using survival methods (minutes) | ||||
| All women | 217 (172–262) | 271 (220–322) | 374 (304–444) | <0.01 |
| Nulliparous | 287 (215–359) | 303 (221–385) | 405 (327–482) | 0.16 |
| Parous | 187 (141–233) | 242 (183–301) | 304 (197–412) | 0.04 |
| Perineal tears | ||||
| Grade 1–2 | 44 (47.8) | 31 (53.4) | 23 (35.4) | 0.11 |
| Grade 3–4 | 1 | 0 | 0 | N/A |
| Fetal outcomes | ||||
| Birthweight | 3295 (400) | 3254 (406) | 3482 (411) | <0.01 |
| 5‐min Apgar score <7 | 0 | 1 (1.7) | 1 (1.5) | N/A |
| Referral to NICU | 3 (3.3) | 2 (3.4) | 8 (12.3) | 0.04 |
Abbreviations: CI, confidence interval; NICU, neontal intensive care unit; OA, occiput anterior; OP occiput posterior; OT occiput transverse; SD, standard deviation.
The operative delivery rate was 10/157 (6.4%) in women with the fetus in the OA position in the second stage of labor (six cesarean sections and four vacuum extractions), and 28/48 (58.3%) in the non‐OA group (27 cesarean section and one vacuum extraction) (p < 0.01). The position was unknown in five cases.
The cesarean section rate in the second stage of labor was 25/89 (28.1%) in nulliparous women and 8/121 (6.6%) in parous women (p < 0.01). Vacuum extraction was done in three nulliparous and two parous women.
3.4. Duration of labor
The duration of the active labor phase was significantly longer in women with the fetus in OP position vs. OA position at admission, but the difference was not significant in analyses stratified into parity. The actual mean duration and the estimated mean duration using survival methods stratified in nulliparous and parous women are presented in Table 3. The probability of delivery differentiated into OA, OT, and OP positions at admission (entire population) is presented as a 1‐minus survival plot in Figure 3.
FIGURE 3.
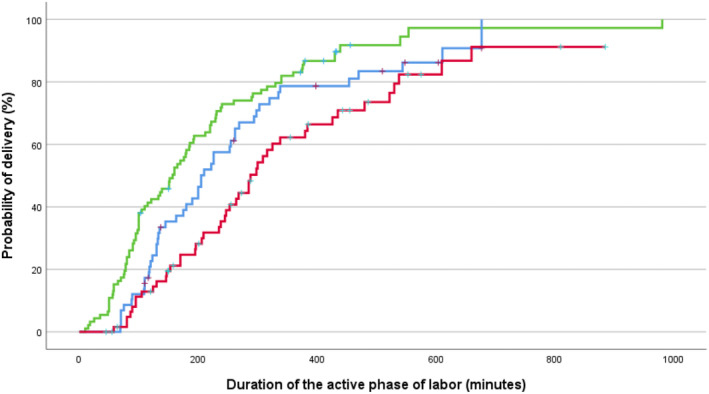
One‐minus survival plot (entire population) showing the probability of delivery as a function of time for fetuses in occiput anterior (green), occiput transverse (blue) and occiput posterior (red) position during the active phase of labor. Operative interventions were censored.
The estimated mean duration of the second stage of labor was 55 min (95% CI 48–61) in nulliparous women in the OA group and 91 min (95% CI 78–103) in the non‐OA group, respectively. Corresponding values in parous women were 34 min (95% CI 30–37) and 69 min (95% CI 50–88), respectively. The probability of delivery stratified in nulliparous and parous women is presented as 1‐minus survival plots in Figure 4, and the HR for delivery was examined using multivariable Cox‐regression analyses (Table 4). Hazard ratio <1 represents longer duration than the reference, and the adjusted HR for a vaginal delivery in the non‐OA group, using the OA group as reference, was 0.26 (95% CI 0.13–0.52) in nulliparous women and 0.25 (95% CI 0.12–0.52) in parous women.
FIGURE 4.
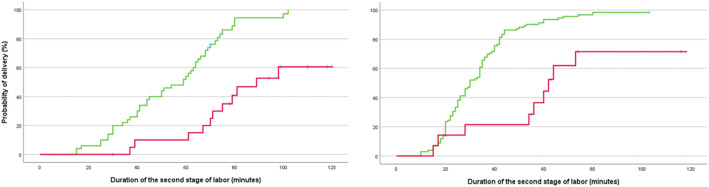
One‐minus survival plots showing the probability of delivery for fetuses in occiput anterior (green) and non‐occiput anterior (red) during the second stage of labor as a function of time. Nulliparous women in the left figure and parous women in the right figure. Operative interventions and duration of the second stage ≥120 min were censored.
TABLE 4.
Cox regression analysis for predicting duration of the second stage of labor.
| Unadjusted HR | Adjusted HR | |
|---|---|---|
| Nulliparous women | ||
| OA | 1.0 | |
| Non‐OA | 0.22 (0.11–0.44) | 0.26 (0.13–0.52) |
| Maternal age | 1.05 (0.98–1.13) | 1.04 (0.96–1.11) |
| Gestation age | 0.98 (0.95–1.01) | 0.97 (0.94–1.01) |
| BMI | 0.95 (0.89–1.02) | 0.96 (0.89–1.04) |
| EFW ≤3500 | 1.0 | |
| EFW >3500 | 0.50 (0.27–0.93) | 0.85 (0.42–1.71) |
| Parous women | ||
| OA | 1.0 | |
| Non‐OA | 0.27 (0.13–0.54) | 0.25 (0.12–0.52) |
| Maternal age | 1.01 (0.97–1.04) | 1.03 (0.99–1.07) |
| Gestational age | 1.01 (0.99–1.03) | 1.01 (0.99–1.03) |
| BMI | 0.98 (0.94–1.02) | 0.98 (0.94–1.02) |
| EFW ≤3500 | 1.0 | |
| EFW >3500 | 0.96 (0.62–1.47) | 1.09 (0.69–1.72) |
Abbreviations: BMI, body mass index; EFW, esitmated fetal weight; HR, hazard ratio; OA, occiput anterior.
4. DISCUSSION
The overall persistent OP position rate at birth was 16.3%; 27.2% in nulliparous women and 8.1% in parous women, which are higher rates of persistent OP position at delivery than reported in other populations. The duration of the second stage of labor was longer, and the operative delivery rate was nine times higher in women with the fetus in a non‐OA position compared with an OA position in the second stage of labor.
The four classical shapes of the maternal pelvis are the gynecoid, the android, the anthropoid, and the platypelloid 30 ; however, mixed variations exist.30, 34 The anthropoid pelvis has a narrow anterior segment and an ample room posteriorly. The fetal head is wider posteriorly, and the OP position may be favorable in women with an anthropoid pelvic shape. The anthropoid pelvis is more common in black African women, 33 and a study from South Africa found that black females presented with a smaller pelvic cavity anteriorly than white females. 37
Five previous studies examined fetal rotation longitudinally with ultrasound. Souka et al. examined 148 white European women and found that malrotation from initial OA position was highly unlikely, and that persistent OP position was a consequence of failure to rotate. The duration of labor was associated with fetal position. 10 Hjartardottir et al. examined a population comprising 99 white European women and found that 77% of the fetuses in OP position at admission rotated to OA position during labor, but the rotation often occurred late in labor. 3 Lieberman et al. examined a population of whom 75% were white women, and found that the final fetal position was established late in labor, and that epidural analgesia was associated with higher rates of OP position at delivery; 12.9% vs 3.3%, respectively. 18 Blasi et al. included 84 women from Italy and Germany with diverse ethnicity, and found 27% in OP position in the second stage of labor, but only 7% were delivered in OP position. 9 Adam et al. did not report ethnicity but found that 89.2% of fetuses starting in OP or OT position delivered vaginally in OA position. We found that 65/215 (30.2%) fetuses were in OP position at admission, 38/210 (18.1%) were in OP position in the second stage and 35/215 (16.3%) were in OP position at delivery, which are higher rates of persistent OP position at delivery than reported in the other studies.3, 9, 10, 18, 28 The persistent OP position rate at delivery was more than three times higher in nulliparous than in parous women; 27.2% vs 8.1%, respectively. None of the women in our study had epidural analgesia.
It has been discussed whether OP position at birth is a consequence of persistent OP position during labor or caused by malrotation from an initial OA or OT position.1, 2, 4, 10 One study showed that malrotation did not occur at low stations. 38 We found that most OP positions at delivery were a consequence of failure to rotate, but that malrotation to OP position from initial OA or OT at admission occurred in 10/215 fetuses (4.7%).
Many studies have reported higher cesarean section rates in women with the fetus delivered in OP position.1, 15, 38, 39 We observed a higher overall cesarean section rate also in women with the fetus in OP position at admission, but the difference was not significant in nulliparous women in a stratified analysis (Table 2), and similar results have been found in other studies comprising nulliparous women.4, 5 Most fetuses rotated during the active labor phase and the clinical importance of fetal position at admission is therefore limited. However, women with the fetus in non‐OA position in the second stage of labor had a much higher operative delivery rate compared with the OA group (58.3% vs. 6.4%, respectively).
A recent publication using survival analyses found a huge difference in duration of the active phase of labor in women with the fetus delivered in OP position compared with fetuses delivered in OA position. However, this was an historical cohort study using fetal position at delivery and not fetal position during labor. 14 We present both actual mean time in active phase of labor and the estimated mean duration of labor using Kaplan–Meier analysis (Table 3). The estimated duration was only slightly longer than the actual time because most interventions were done in the second stage of labor. The HR for delivery in the second stage of labor was four time lower in women with the fetus in non‐OA position using OA position as reference (Table 4). Many studies have reported longer duration of the second stage in non‐OP positions,6, 11, 22, 40 but the magnitude of the difference was huge in our population.
Most fetuses presenting with OT or OP positions at admission rotated to OA during labor, and unnecessary interventions in the first stage of labor should be avoided. Malposition was associated with slow progress, and exact knowledge about fetal position is essential in women with slow progress. These women need thorough surveillance, especially in the second stage of labor. The persistent OP position rate at delivery was high in our study, which may reflect restricted possibility for internal rotation. Vacuum extractions were rarely used in this labor ward. The fetus may rotate also during a vacuum extraction, 41 and the OP rate at delivery would probably have been lower if more fetuses were delivered by vacuum extraction. Allowing longer duration of the second stage of labor might also increase the possibility of spontaneous rotation.
An important clinical implication for labor wards with high cesarean section rates may be to emphasize the favorable outcomes related to OA position. All fetuses presenting in OA position in the seconds stage of labor were delivered in OA position, and the intrapartum cesarean section rate was low in these women. Vacuum extraction has low risk of failure in a fetus in OA position, 42 and for labor wards not using instrumental deliveries, exact knowledge of fetal position may be helpful in re‐introducing this procedure.
The longitudinal design, inclusion of only one ethnicity, and the use of survival methods are strengths of our study. The birth attendants and the ultrasound examiners were blinded to each other findings.
The study population comprised both nulliparous and parous women, which complicate the interpretations, however, we have stratified most analyses in accordance with parity. Our study population represent a selected population with high educational level. However, it is unlikely that the pelvic shape and the fetal rotation should be influenced by socioeconomic level. The high intrapartum cesarean section rate and the low rate of vacuum extractions both in nulliparous and parous women are limitations which may reduce the external validity. However, a similar trend is seen in many low‐ and mid‐resource countries with high cesarean section rates and an underuse of assisted vaginal deliveries.43, 44 Our study population comprised women able to pay for the delivery, but the same low rate of vacuum extraction is also seen in the public hospital in Moshi (Mawenzi Regional Referral Hospital) as well as in the largest referral hospital in Tanzania. 45 We could not estimate the duration of the active phase of labor, only the time spent in active labor in the hospital, because many women were admitted during the active phase. The estimated duration of the second stage illustrates the large difference between fetuses in OA or non‐OA position. We do not have detailed information about fetal position in the fetuses delivered with cesarean section during the latent phase. These women were excluded because the fetus has limited chance for spontaneous rotation during the latent phase of labor.
5. CONCLUSION
The persistent OP position rate at delivery was higher than usually reported, and the operative intervention rate was very high in women with OP position in the second stage of labor.
AUTHOR CONTRIBUTIONS
Kenneth Bagandanshwa planned the study, did the ultrasound examinations, did the statistical analyses and drafted the manuscript. Bariki Mchome planned the study, supervised Kenneth Bagandanshwa in this project, and drafted the manuscript. Signe Egenberg planned the study. Raziya Gaffur planned the study and supervised Kenneth Bagandanshwa in this project. Pendo Mlay and Gileard Masengaand planned the study. Torbjørn Moe Eggebø: planned the study, did the statistical analyses, drafted the manuscript. Ibrahim Salum and Upendo Kibona did ultrasound examinations. Adelaida Kavishe and Cecilia Mushi did clinical examinations and recorded data. All authors reviewed and accepted the manuscript before submission.
FUNDING INFORMATION
This study was funded by Laerdal Foundation, Stavanger, Norway. General Electric supported the study with a second‐hand Voluson 8 device.
CONFLICT OF INTEREST STATEMENT
The authors report no conflict of interest.
ETHICS STATEMENT
This study was approved by the Kilimanjaro Christian Medical University College and Research Committee (PG 27/2023) on August 15, 2023.
ACKNOWLEDGEMENTS
We would like to thank Ester Ngowi, Deonista Lyimo, Selemani Kateko, and Happines Lauwo for data collection.
Bagandanshwa K, Mchome B, Kibona U, et al. Fetal rotation examined with ultrasound in a sub‐Saharan population: A longitudinal cohort study. Acta Obstet Gynecol Scand. 2025;104:225‐234. doi: 10.1111/aogs.15013
REFERENCES
- 1. Akmal S, Tsoi E, Howard R, Osei E, Nicolaides KH. Investigation of occiput posterior delivery by intrapartum sonography. Ultrasound Obstet Gynecol. 2004;24:425‐428. [DOI] [PubMed] [Google Scholar]
- 2. Gardberg M, Laakkonen E, Salevaara M. Intrapartum sonography and persistent occiput posterior position: a study of 408 deliveries. Obstet Gynecol. 1998;91:746‐749. [DOI] [PubMed] [Google Scholar]
- 3. Hjartardottir H, Lund SH, Benediktsdottir S, Geirsson RT, Eggebo TM. When does fetal head rotation occur in spontaneous labor at term: results of an ultrasound‐based longitudinal study in nulliparous women. Am J Obstet Gynecol. 2021;224(514):514.e1‐514.e9. [DOI] [PubMed] [Google Scholar]
- 4. Torkildsen EA, Salvesen KA, Vonb P, Eggebo TM. Predictive value of ultrasound assessed fetal head position in primiparous women with prolonged first stage of labor. Acta Obstet Gynecol Scand. 2012;91:1300‐1305. [DOI] [PubMed] [Google Scholar]
- 5. Hjartardottir H, Lund SH, Benediktsdottir S, Geirsson RT, Eggebo TM. Can ultrasound on admission in active labor predict labor duration and a spontaneous delivery? Am J Obstet Gynecol MFM. 2021;3:100383. [DOI] [PubMed] [Google Scholar]
- 6. Calkins LA. Occiput posterior: incidence, significance and management. Am J Obstet Gynecol. 1939;38:993‐1001. [Google Scholar]
- 7. Parsy T, Bettiol C, Vidal F, Allouche M, Loussert‐Chambre L, Guerby P. Persistent occiput posterior position: predictive factors of spontaneous rotation of the fetal head. J Matern Fetal Neonatal Med. 2023;36:2192854. [DOI] [PubMed] [Google Scholar]
- 8. Barth WH Jr. Persistent occiput posterior. Obstet Gynecol. 2015;125:695‐709. [DOI] [PubMed] [Google Scholar]
- 9. Blasi I, D'Amico R, Fenu V, et al. Sonographic assessment of fetal spine and head position during the first and second stages of labor for the diagnosis of persistent occiput posterior position: a pilot study. Ultrasound Obstet Gynecol. 2010;35:210‐215. [DOI] [PubMed] [Google Scholar]
- 10. Souka AP, Haritos T, Basayiannis K, Noikokyri N, Antsaklis A. Intrapartum ultrasound for the examination of the fetal head position in normal and obstructed labor. J Matern Fetal Neonatal Med. 2003;13:59‐63. [DOI] [PubMed] [Google Scholar]
- 11. Senecal J, Xiong X, Fraser WD. Pushing early or pushing late with epidural study g. effect of fetal position on second‐stage duration and labor outcome. Obstet Gynecol. 2005;105:763‐772. [DOI] [PubMed] [Google Scholar]
- 12. Dahlqvist K, Jonsson M. Neonatal outcomes of deliveries in occiput posterior position when delayed pushing is practiced: a cohort study. BMC Pregnancy Childbirth. 2017;17:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Simkin P. The fetal occiput posterior position: state of the science and a new perspective. Birth. 2010;37:61‐71. [DOI] [PubMed] [Google Scholar]
- 14. Eide B, Sande RK, Von Brandis P, Kessler J, Tappert C, Eggebo TM. Associations between fetal position at delivery and duration of active phase of labor: a historical cohort study. Acta Obstet Gynecol Scand. 2024;103:1888‐1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fitzpatrick M, McQuillan K, O'Herlihy C. Influence of persistent occiput posterior position on delivery outcome. Obstet Gynecol. 2001;98:1027‐1031. [DOI] [PubMed] [Google Scholar]
- 16. Ponkey SE, Cohen AP, Heffner LJ, Lieberman E. Persistent fetal occiput posterior position: obstetric outcomes. Obstet Gynecol. 2003;101:915‐920. [DOI] [PubMed] [Google Scholar]
- 17. Cheng YW, Shaffer BL, Caughey AB. Associated factors and outcomes of persistent occiput posterior position: a retrospective cohort study from 1976 to 2001. J Matern Fetal Neonatal Med. 2006;19:563‐568. [DOI] [PubMed] [Google Scholar]
- 18. Lieberman E, Davidson K, Lee‐Parritz A, Shearer E. Changes in fetal position during labor and their association with epidural analgesia. Obstet Gynecol. 2005;105:974‐982. [DOI] [PubMed] [Google Scholar]
- 19. Akmal S, Kametas N, Tsoi E, Howard R, Nicolaides KH. Ultrasonographic occiput position in early labour in the prediction of caesarean section. BJOG. 2004;111:532‐536. [DOI] [PubMed] [Google Scholar]
- 20. Eggebo TM, Rygh AB, von Brandis P, Skjeldestad FE. Prevention of obstetric anal sphincter injuries with perineal support and lateral episiotomy: a historical cohort study. Acta Obstet Gynecol Scand. 2024;103:488‐497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Eggebo TM, Hassan WA, Salvesen KA, Torkildsen EA, Ostborg TB, Lees CC. Prediction of delivery mode by ultrasound‐assessed fetal position in nulliparous women with prolonged first stage of labor. Ultrasound Obstet Gynecol. 2015;46:606‐610. [DOI] [PubMed] [Google Scholar]
- 22. Ghi T, Maroni E, Youssef A, et al. Sonographic pattern of fetal head descent: relationship with duration of active second stage of labor and occiput position at delivery. Ultrasound Obstet Gynecol. 2014;44:82‐89. [DOI] [PubMed] [Google Scholar]
- 23. Akmal S, Kametas N, Tsoi E, Hargreaves C, Nicolaides KH. Comparison of transvaginal digital examination with intrapartum sonography to determine fetal head position before instrumental delivery. Ultrasound Obstet Gynecol. 2003;21:437‐440. [DOI] [PubMed] [Google Scholar]
- 24. Dupuis O, Ruimark S, Corinne D, Simone T, Andre D, Rene‐Charles R. Fetal head position during the second stage of labor: comparison of digital vaginal examination and transabdominal ultrasonographic examination. Eur J Obstet Gynecol Reprod Biol. 2005;123:193‐197. [DOI] [PubMed] [Google Scholar]
- 25. Ramphul M, Ooi PV, Burke G, et al. Instrumental delivery and ultrasound: a multicentre randomised controlled trial of ultrasound assessment of the fetal head position versus standard care as an approach to prevent morbidity at instrumental delivery. BJOG. 2014;121:1029‐1038. [DOI] [PubMed] [Google Scholar]
- 26. Wiafe YA, Whitehead B, Venables H, Dassah ET. Comparing intrapartum ultrasound and clinical examination in the assessment of fetal head position in African women. J Ultrason. 2019;19:249‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chou MR, Kreiser D, Taslimi MM, Druzin ML, El‐Sayed YY. Vaginal versus ultrasound examination of fetal occiput position during the second stage of labor. Am J Obstet Gynecol. 2004;191:521‐524. [DOI] [PubMed] [Google Scholar]
- 28. Adam G, Sirbu O, Voicu C, Dominic D, Tudorache S, Cernea N. Intrapartum ultrasound assessment of fetal head position, tip the scale: natural or instrumental delivery? Curr Health Sci J. 2014;40:18‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ghi T, Youssef A, Martelli F, et al. Narrow subpubic arch angle is associated with higher risk of persistent occiput posterior position at delivery. Ultrasound Obstet Gynecol. 2016;48:511‐515. [DOI] [PubMed] [Google Scholar]
- 30. Caldwell WE, Moloy HC. Anatomical variations in the female pelvis: their classification and obstetrical significance: (section of obstetrics and Gynaecology). Proc R Soc Med. 1938;32:1‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Betti L. Shaping birth: variation in the birth canal and the importance of inclusive obstetric care. Philos Trans R Soc Lond Ser B Biol Sci. 2021;376:20200024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. Am J Obstet Gynecol. 2010;202:335‐343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Handa VL, Lockhart ME, Fielding JR, et al. Racial differences in pelvic anatomy by magnetic resonance imaging. Obstet Gynecol. 2008;111:914‐920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hunter JO. The anthropoid pelvis. In Southern Medicine & Surgery. Vol 100. Charlotte; 1938. [Google Scholar]
- 35. Ghi T, Eggebo T, Lees C, et al. ISUOG practice guidelines: intrapartum ultrasound. Ultrasound Obstet Gynecol. 2018;52:128‐139. [DOI] [PubMed] [Google Scholar]
- 36. World Health Organization . WHO Recommendations: Intrapartum Care for a Positive Childbirth Experience. WHO; 2018. [PubMed] [Google Scholar]
- 37. Jagesur S, Wiid A, Pretorius S, Bosman MC, Oettle AC. Assessment of the variability in the dimensions of the intact pelvic canal in south Africans: a pilot study. Homo. 2017;68:30‐37. [DOI] [PubMed] [Google Scholar]
- 38. Vitner D, Paltieli Y, Haberman S, Gonen R, Ville Y, Nizard J. Prospective multicenter study of ultrasound‐based measurements of fetal head station and position throughout labor. Ultrasound Obstet Gynecol. 2015;46:611‐615. [DOI] [PubMed] [Google Scholar]
- 39. Cheng YW, Hubbard A, Caughey AB, Tager IB. The association between persistent fetal occiput posterior position and perinatal outcomes: an example of propensity score and covariate distance matching. Am J Epidemiol. 2010;171:656‐663. [DOI] [PubMed] [Google Scholar]
- 40. Walling AD. Persistent fetal occiput posterior position. Am Fam Physician. 2004;69:191‐192. [Google Scholar]
- 41. Kahrs BH, Usman S, Ghi T, et al. Fetal rotation during vacuum extractions for prolonged labor: a prospective cohort study. Acta Obstet Gynecol Scand. 2018;97:998‐1005. [DOI] [PubMed] [Google Scholar]
- 42. Kahrs BH, Usman S, Ghi T, et al. Sonographic prediction of outcome of vacuum deliveries: a multicenter, prospective cohort study. Am J Obstet Gynecol. 2017;217(69):e61. [DOI] [PubMed] [Google Scholar]
- 43. Merriam AA, Ananth CV, Wright JD, Siddiq Z, D'Alton ME, Friedman AM. Trends in operative vaginal delivery, 2005‐2013: a population‐based study. BJOG. 2017;124:1365‐1372. [DOI] [PubMed] [Google Scholar]
- 44. Ameh CA, Weeks AD. The role of instrumental vaginal delivery in low resource settings. BJOG. 2009;116(Suppl 1):22‐25. [DOI] [PubMed] [Google Scholar]
- 45. Makokha‐Sandell H, Mgaya A, Belachew J, Litorp H, Hussein K, Essen B. Low use of vacuum extraction: health care professionals' perspective in a university hospital, Dar es Salaam. Sex Reprod Healthc. 2020;25:100533. [DOI] [PubMed] [Google Scholar]


