Abstract
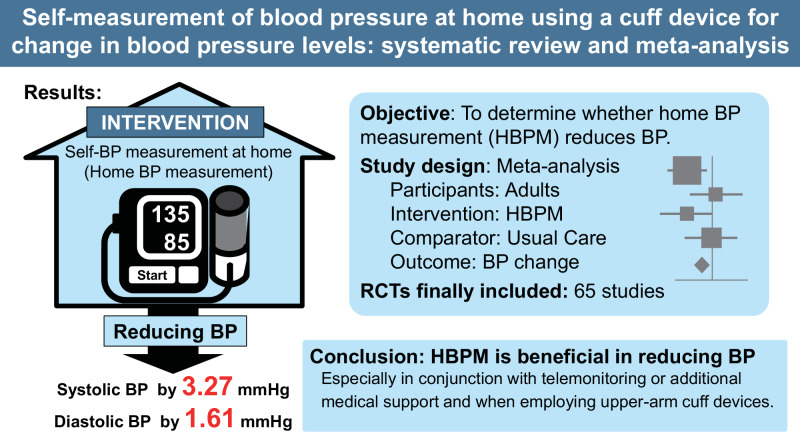
The effect of self-measurement of blood pressure (BP) at home (home BP measurement, HBPM) has been evaluated over the past decade. This meta-analysis included the latest studies to determine whether HBPM reduced BP (PROSPERO ID: CRD42023442225). PubMed, Cochrane Library Database, and IchuShi-Web were searched for randomized controlled trials after the year 2000 which demonstrated the effect of HBPM on BP change compared with usual care (UC). Overall, 65 articles (n = 21,053; 63 based on patients with hypertension) were included. The systolic/diastolic BP reduction was significantly greater in the HBPM than in the UC group by 3.27/1.61 mmHg (95% confidence intervals: 2.40–4.15/1.14–2.07) at the end of the intervention, and I2 values ≥ 46.7% suggested moderate-to-high heterogeneity. The funnel plots exhibited no notable publication bias (Egger’s test p ≥ 0.16). HBPM with co-interventions (such as telemonitoring) showed a stronger BP-lowering effect than without co-interventions while the effect of HBPM on BP change remained significant in the absence of co-interventions. HBPM was not associated with systolic BP changes when we combined the four studies that used a wrist cuff device for HBPM. The number of antihypertensive medications increased by 0.17 medications in the HBPM group compared with that in the UC group. There were no significant differences in body mass index changes or risk of severe adverse outcomes between the groups. Our results demonstrated a beneficial effect of HBPM in reducing BP, particularly when used in conjunction with telemonitoring or additional medical support and when employing upper-arm cuff devices.
Keywords: Blood pressure monitoring, Ambulatory, Systematic review, Meta-analysis, Telemedicine, Randomized controlled trial
Introduction
High blood pressure (BP) is a known risk factor for cardiovascular diseases [1–4]. Self-measured BP at home (i.e., home BP) has been shown to predict cardiovascular risks more accurately than conventional BP measured in a medical setting. The Japanese Hypertension Guidelines state that “when there is a discrepancy in diagnosis between office BP and home BP, a home BP-based diagnosis should have priority” [1]. Furthermore, home BP measurement (HBPM) is useful for follow-up of hypertensive patients and recording long-term BP variations (such as seasonal BP). In this context, various home BP monitors have been developed and are currently available. Further development of digital personal health record devices may accelerate the adoption of HBPM as a common healthcare tool.
Previous meta-analyses have revealed that HBPM can lower BP [5–8]. The results of the meta-analyses imply that HBPM alone does not have a large effect [5, 6] and that additional co-interventions (such as telemonitoring) are preferable to achieving an adequate BP-lowering effect [5, 7, 8]. However, several other studies have been published on the effect of self-monitoring of BP since the above-mentioned meta-analyses. Including these recent reports in a meta-analysis allows more accurate estimates to be calculated.
Digital technologies related to human health are developing rapidly and these technologies can sometimes be combined with HBPM, for example, to improve the accuracy of recordings or to make devices wearable. The objective of this meta-analysis was to determine the amplitude of BP reduction after HBPM by including the results of recent reports. Evaluating the magnitude of BP reduction from HBPM can reveal how HBPM contributes to BP management.
Methods
Search strategy
This systematic review examined the BP-lowering effects of HBPM compared to usual care (UC). This systematic review was registered in the International Prospective Register of Systematic Reviews known as PROSPERO (ID: CRD42023442225). This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. This study has used existing, de-identified data from previously published manuscripts or reported on websites, and therefore, was exempted from Institutional Review Board approval. This work is the systematic review for the Task Force “Guideline for BP control using digital technologies” of the Japanese Society of Hypertension.
Studies published in PubMed, Cochrane Library Database, and IchuShi-Web databases were used in this analysis. Studies were included if (1) were reported after the year 2000, (2) were published in English or Japanese, (3) provided the information necessary to calculate estimates and distributions, (4) were randomized controlled trials, or (5) used a cuff device for HBPM. Studies were excluded if (i) were conference abstracts, review articles, case series, qualitative studies, or editorials without any available data, (ii) participants were required to self-measure variables other than BP (e.g., blood glucose) as part of the interventions, (iii) were on pregnant women, (iv) were conducted immediately after a cardiovascular event, and (v) primarily designed to observe the effect of education or other interventions and treated HBPM only as a co-intervention. For studies with overlapping participants, we selected the most recent study with a larger sample size.
The search terms used were combinations of terms related to “self-measured blood pressure” and “randomized controlled trial” as indicated in Supplementary Tables 1–3. The search was performed on August 1, 2023.
Intervention and comparator
The targeted intervention was self-BP measurement using a cuff device, i.e., HBPM. This included HBPM combined with support from physicians, co-medical professionals, or those using telemonitoring and new technologies (e.g., smartphone applications). The comparator was set as UC without HBPM; however, education or setting the target BP as additional care was allowed if it was considered not to critically affect the present purpose.
Outcomes
The outcomes were changes in BP, prevention of hypertension, and tapering off BP-lowering medications. However, the latter two outcomes were not often reported in the previous studies. Instead of collecting data on the tapering of BP-lowering medications, we collected data on a change in the number of antihypertensive medications to collect adequate study data. Additional outcomes were adverse events and changes in body mass index (BMI) as a risk factor for cardiovascular diseases. For the outcome of the BP change, we referred to an office or ambulatory BP change because few studies have assessed home BP changes in the UC group.
Data extraction, selection process, and assessment of bias risk
Data from the included studies were extracted into a standardized form detailing the first author, year of publication, country, study period, population characteristics, study design, intervention, outcomes, sample size, and reported estimates and distributions. When studies reported more than one outcome point, data from the longest intervention period were used for the main analysis. One reviewer extracted the information, and another reviewer confirmed its accuracy.
At each stage, two members of the team independently reviewed the studies. Titles and abstracts were screened during the first screening process. Full texts of relevant articles were sourced in the second screening process, which involved a thorough review of the full texts to ensure the eligibility criteria were met and check for possible repetition of patient data. In cases of disagreement that could not be resolved by consensus, a third reviewer of the review team adjudicated. Two reviewers assessed the potential risk of bias and indirectness of each selected report according to the Minds Manual for Guidelines [9].
Statistical analysis
The estimates of group differences and 95% confidence intervals (CIs) in BP change at the end of intervention were obtained by fitting random-effects models using restricted maximum likelihood. The 95% CIs were estimated from the standard error (SE) values. When the standard deviation (SD) instead of SE was reported, we computed it as SD/(n0.5). When the SEs of the differences in BP were not available, we first estimated the SE of the BP difference as [SEa2 + SEb2]0.5. For example, when we calculated the SE of the BP difference between baseline and follow-up, SEa indicated the SE of the BP at baseline and SEb indicated the SE of the BP at follow-up. If either SEa or SEb were unavailable, the missing data were interpolated based on a regression equation derived from the available data for SEa and SEb. Studies without any information on BP distribution were excluded from the analysis. The value obtained at the end of the intervention period was used as BP at follow-up. The present study did not consider changes in BP during observation period after the end of the intervention.
Heterogeneity among the studies was tested using Q-statistics and quantified using I2 statistics [10]. We considered I2 < 30% to indicate low heterogeneity between studies, 30%–60% to indicate moderate heterogeneity, and >60% to indicate substantial heterogeneity. Furthermore, the leave-one-out method was used to observe the influence of individual studies on the overall heterogeneity. Funnel plot asymmetry was used to detect publication bias. Egger’s and Begg’s tests were used to examine statistical significance.
Subgroup or meta-regression analyses were used to identify associations between the effect of the intervention on BP change and relevant characteristics including the duration of follow-up, BP measurement methods (office or ambulatory BP), type of device used for the HBPM intervention (wrist or upper arm cuff), co-intervention (present or absent), and change in the number of antihypertensive medications as possible factors of heterogeneity. Co-intervention was defined as the use of telemonitoring, co-medical staff support, or other methods including reminders via telephone or text messages. In meta-regression analyses, when multiple outcome points were found in one study, all data were used after considering the individual studies as random effects. We collected data on office and ambulatory BP as outcomes if the study contained both types of information. When the study had both office and ambulatory BP data, office BP was preferentially considered the main outcome because it was the most common outcome measure.
Analysis was performed using R version 4.4.1 (R Foundation for Statistical Computing, Vienna, Austria) and the R package of “metafor”. Two-sided p values of <0.05 were regarded to indicate nominal statistical significance.
Results
Study overview
Our search strategy yielded 4378 reports, of which 73 were eligible for a full-text review. Finally, 65 articles were included in the analysis (Supplementary Fig. 1) [11–75]. The characteristics of the included studies are shown in Tables 1 and 2. The study participants were patients with hypertension in 63 of the 65 studies. In one study [14], the previously treated group with SBP/DBP <150/<90 mmHg (n = 19 of 40) was not included because of the impracticality of the intervention; in that subgroup, the first attempt was to reduce the number or dosage of antihypertensive medications, resulting in an increase in SBP of ~10 mmHg.
Table 1.
Summary of basic characteristics
| Authors | Year | Country | Hypertension status | Antihypertensive treatment at baseline | Trial name (ID) | Age | Men | N of interventiona | N of controla |
|---|---|---|---|---|---|---|---|---|---|
| Vetter et al. [11] | 2000 | Switzerland | Hypertension | With monotherapy of losartan | SVATCH Study | 57.9 | 49.2% | 296 | 326 |
| Mehos et al. [12] | 2000 | USA | Hypertension | With antihypertensive medication | – | 58.8 | 30.6% | 18 | 18 |
| Rogers et al. [13] | 2001 | USA | Hypertension | With or without antihypertensive treatment | – | 61.4 | 49.6% | 60 | 61 |
| Broege et al. [14] | 2001 | USA | Hypertension | BP > 150/90 mmHg without antihypertensive treatment, age ≥ 65 (the treated group was not considered due to inappropriate protocol) | – | 73 | 32.5% | 9 | 10 |
| Rudd et al. [15] | 2004 | USA | Hypertension | BP ≥ 150/95 mmHg, with or without antihypertensive treatment | – | 59.5 | 47.0% | 74 | 76 |
| Halme et al. [16] | 2005 | Finland | Hypertension | With or without antihypertensive treatment | HOMER - | 57.2 | 32.8% | 113 | 119 |
| Zillich et al. [17] | 2005 | USA | Hypertension | With antihypertensive treatment | HOME - | 65.0 | 39.2% | 64 | 61 |
| Marquez-Contreras et al. [18] | 2006 | Spain | Hypertension | With or without antihypertensive treatment | EAPACUM–HTA | 59.1 | 51.0% | 100 | 100 |
| Verberk et al. [19] | 2007 | Netherlands | Hypertension | With or without antihypertensive treatment | HOMERUS | 55 | 55% | 214 | 216 |
| Kauric-Klein and Artinian [20] | 2007 | USA | Hypertension | With or without antihypertensive treatment, hemodialysis | – | 48.7 | 32% | 17 | 17 |
| Artinian et al. [21] | 2007 | USA | Hypertension | With or without antihypertensive treatment | – | 59.6 | 36% | 194 | 193 |
| Tobe et al. [22] | 2008 | Canada | Hypertension | With antihypertensive treatment | IMPPACT | 62.9 | 49% | 173 | 97 |
| Madsen et al. [23] | 2008 | Denmark | Hypertension | With or without antihypertensive treatment | (NCT00282334) | 55.9 | 50% | 113 | 123 |
| Green et al. [24] | 2008 | USA | Hypertension | With antihypertensive treatment | e-BP (NCT00158639) | 59.1 | 48% |
(1) 259 (2) 261 |
258 |
| Parati et al. [25] | 2009 | Italy | Hypertension | With or without antihypertensive treatment | TeleBPCare - | 57.5 | 54% | 187 | 111 |
| da Silva et al. [26] | 2009 | Brazil | Hypertension | With or without antihypertensive treatment, hemodialysis | ([CRG060800146]) | 51.6 | 66.2% | 34 | 31 |
| Dejesus et al. [27] | 2009 | USA | Hypertension | Type 2 diabetes (antihypertensive treatment status is uncertain) | – | >60, 76% | 48% | 19 | 17 |
| Bosworth et al. [28] | 2009 | USA | Hypertension | With or without antihypertensive treatment | TCYB (NCT00123058) | 61 | 34% | 158 | 159 |
| Rinfret et al. [29] | 2009 | Canada | Hypertension | With or without antihypertensive treatment | (NCT00374829; ISRCTN75436659) | 56 | 54% | 111 | 112 |
| Godwin et al. [30] | 2010 | Canada | Hypertension | With antihypertensive medications and not at target BP | – | 68 | 49% | 285 | 267 |
| McManus et al. [31] | 2010 | UK | Hypertension | With antihypertensive treatment | TASMINH2 (ISRCTN17585681) | 66 | 47% | 234 | 246 |
| Varis and Kantola [32] | 2010 | Finland | Hypertension | Without antihypertensive treatment | – | N/A | 39% | 104 | 85 |
| Bosworth et al. [33] | 2011 | USA | Hypertension | With antihypertensive treatment | HINTS (NCT00237692) | 64 | 16% | 149 | 147 |
| Magid et al. [34] | 2011 | USA | Hypertension | With antihypertensive treatment | (NCT00520988) | 65.9 | 65% | 138 | 145 |
| Hebert et al. [35] | 2012 | USA | Hypertension | with antihypertensive treatment self-described black or Hispanic adults | – | 61 | 34% |
(1)120 (2)120 |
(1)129 (2)118 |
| Fuchs et al. [36] | 2012 | Brazil | Hypertension | With antihypertensive treatment | MONITOR (NCT00921791) | 59 | 40% | 62 | 59 |
| Piette et al. [37] | 2012 | USA and Mexico | Hypertension | With or without antihypertensive treatment | (NCT01484782) | 57.6 | 33% | 89 | 92 |
| Williams et al. [38] | 2012 | Australia | Hypertension | With antihypertensive treatment, diabetes, and chronic kidney disease | MESMI (ACTRN12607000044426) | 67.0 | 56% | 39 | 41 |
| Kerry et al. [39] | 2013 | UK | Hypertension |
With or without antihypertensive treatment, Stroke or transient ischemic attack within the 9 months before enrollment and hypertension. |
(NCT00514800) | 72 | 57% | 187 | 194 |
| Magid et al. [40] | 2013 | USA | Hypertension | With or without antihypertensive treatment | (NCT01162759) | 60 | 60% | 175 | 173 |
| McKinstry et al. [41] | 2013 | UK | Hypertension | With or without antihypertensive treatment | HITS (ISRCTN72614272) | 61 | 59% | 218 | 225 |
| Margolis et al. [42] | 2013 | USA | Hypertension | With or without antihypertensive treatment | (NCT00781365) | 61.1 | 55% | 228 | 222 |
| Ogedegbe et al. [43] | 2014 | USA | Hypertension | With antihypertensive treatment | CAATCH (NCT00233220) | 56.5 | 28% | 529 | 510 |
| Stewart et al. [44] | 2014 | Australia | Hypertension | With antihypertensive treatment (at least one hypertensive medication) | HAPPy - | 66.7 | 51% | 207 | 188 |
| McManus et al. [45] | 2014 | UK | Hypertension | With high-risk conditions (cardiovascular disease, diabetes, stage 3 chronic kidney disease, or coronary heart disease) | TASMIN-SR - | 69.5 | 60% | 276 | 276 |
| Hosseininasab et al. [46] | 2014 | Iran | Hypertension | With or without antihypertensive treatment | (NCT01525108) | 58.7 | 38.7% | 97 | 97 |
| Kim et al. [47] | 2014 | USA | Hypertension | With or without antihypertensive treatment (Korean American aged ≥60 years) | Self-Help Intervention Program on the Control of home BP (NCT00406614) | 70.9 | 30% | 184 | 185 |
| Yi et al. [48] | 2015 | USA | Hypertension | With antihypertensive treatment | (NCT01123577) | 61.3 | 32% | 409 | 419 |
| Hanley et al. [49] | 2015 | UK | Hypertension | With antihypertensive treatment (Stroke/TIA survivors with uncontrolled BP) | (ISRCTN61528726) | 70.9 | 60% | 40 | 15 |
| Aekplakorn et al. [50] | 2016 | Thailand | Hypertension | With antihypertensive treatment | – | 59.4 | 35% | 111 | 113 |
| Kim et al. [51] | 2016 | USA | Hypertension | With antihypertensive treatment | (NCT01975428) | 57.6 | 32% | 52 | 43 |
| Tzourio et al. [52] | 2017 | France | Hypertension | With or without antihypertensive treatment, age ≥ 65 | (ISRCTN97164929) | 79.1 | 43.0 | 526 | 517 |
| Klarskov et al. [53] | 2018 | Denmark | Hypertension | With or without antihypertensive treatment | BRIDGE | 61.8 | 48.1% | 533 | 515 |
| Martinez et al. [54] | 2018 | Spain | Hypertension | With antihypertensive treatment | RECAVA | 66 | 64% | 64 | 52 |
| McManus et al. [55] | 2018 | UK | Hypertension | With antihypertensive treatment | TASMINH4 | 66.9 | 53.6% |
(1) 391 (2) 389 |
393 |
| Pan et al. [56] | 2018 | China | Hypertension | With or without antihypertensive treatment | – | 57.2 | 46.8% | 52 | 55 |
| Skolarus et al. [57] | 2018 | USA | Hypertension | With or without antihypertensive treatment | Reach Out ED (NCT02664610) | 58 | 21% | 48 | 46 |
| Cuffee et al. [58] | 2019 | USA | Hypertension | With antihypertensive treatment | ([NCT01035554]) | 58.7 | 59.2% | 106 | 107 |
| Gu et al. [59] | 2020 | China | Hypertension | With antihypertensive treatment, diabetes, aged ≥ 60 | (UMIN000021613) | 71.1 | 36.7% | 45 | 45 |
| Ojji et al. [60] | 2020 | Nigeria | Hypertension | With or without antihypertensive treatment | – | 44 | 40% | 20 | 20 |
| Zha et al. [61] | 2020 | USA | Hypertension | With antihypertensive treatment | (NCT02632838) | 52.3 | 12% | 12 | 13 |
| Ionov et al. [62] | 2021 | Russia | Hypertension | With antihypertensive treatment | – | 47 | 60% | 160 | 80 |
| McManus et al. [63] | 2021 | UK | Hypertension | With antihypertensive treatment | HOME BP (ISRCTN13790648) | 66 | 54% | 305 | 317 |
| Zhang et al. [64] | 2021 | China | Hypertension | With or without antihypertensive treatment | (NCT00670566) | 55.1 | 47% | 96 | 405 |
| Akl et al. [65] | 2021 | Lebanon | Hypertension | With antihypertensive treatment (uncertain if the study included patients without antihypertensive treatment) | (ISRCTN16450193) | 60.2 | 51% | 39 | 40 |
| Margolis et al. [66] | 2022 | USA | Hypertension | With or without antihypertensive treatment | Hyperlink 3 (NCT02996565) | 60.2 | 47% | 1648 | 1423 |
| Okoro et al. [67] | 2022 | Nigeria | No restriction | CKD Stage1-4 with antihypertensive treatment | – | 52.2 | 38% | 73 | 74 |
| Muijsers et al. [68] | 2022 | Netherlands and Germany | No restriction | Women with a history of preeclampsia and/or HELLP syndrome but without antihypertensive treatment | BP-PRESELF (NCT03228082) | 45.4 | 0% | 96 | 95 |
| Calderón-Anyosa et al. [69] | 2023 | Peru | Hypertension | With antihypertensive treatment | (NCT03524456) | 68.1 | 32% | 20 | 20 |
| Doogue et al. [70] | 2023 | UK | Hypertension | Stroke or TIA patients with antihypertensive treatment | TASMIN5S IRL (ISRCTN57946500) | 70 | 80% | 10 | 5 |
| Hoppe et al. [71] | 2023 | USA | Hypertension | With antihypertensive treatment, age of 18–39 years | the MyHEART randomized clinical trial (NCT03158051) | 35 | 53% | 157 | 159 |
| Leupold et al. [72] | 2023 | Germany | Hypertension | With antihypertensive treatment | PIA (DRKS00012680) | 58 | 53% | 331 | 305 |
| Martínez-Ibáñez et al. [73] | 2023 | Spain | Hypertension | With antihypertensive treatment | ADAMPA (NCT03242785) | 64.4 | 47% | 156 | 156 |
| Nejamis et al. [74] | 2023 | Argentina | Hypertension | With or without antihypertensive treatment | – | 58.6 | 49% | 144 | 148 |
| Ramos-Zavala et al. [75] | 2023 | México | Hypertension | With antihypertensive treatment | – | 58.1 | 45.5% | 94 | 84 |
aThe number of participants at baseline, including the participants that were excluded from the main analysis. BP blood pressure
Table 2.
Summary of methods for intervention and control
| Authors | Year | HBPM method: type/method (device) | Outcome BP | Co-intervention 1 | Co-intervention 2 | Co-intervention 3 | Control |
|---|---|---|---|---|---|---|---|
| Vetter et al. [11] | 2000 | Wrist/oscillometric (Omron HEM-605) | OBP | None | – | – | Usual care |
| Mehos et al. [12] | 2000 | Upper arm/oscillometric (A&D UA-702) | OBP | Education/change in medication | Telephone calls including checking BP on a phone | Pharmacist support | Usual care |
| Rogers et al. [13] | 2001 | Upper arm/oscillometric (Welch Allyn 52500) | 24 h-ABP | None | Telemonitoring (telecommunication) | – | Usual care |
| Broege et al. [14] | 2001 | Upper arm/oscillometric (Omron HEM-702) | OBP, day/night ABP | Setting target BP | Telephone calls including checking BP on a phone | – | Setting target BP |
| Rudd et al. [15] | 2004 | Upper arm/oscillometric (A&D UA-751) | OBP | Change in medication | Telephone calls including checking BP on a phone | Nurse support | Usual care |
| Halme et al. [16] | 2005 | Upper arm/oscillometric (Omron M4) | OBP/HBP | Setting target BP | – | – | Setting target BP |
| Zillich et al. [17] | 2005 | Upper arm/oscillometric (Omron HEM-737A) | OBP | Change in medication | – | Pharmacist support | Usual care |
| Marquez-Contreras et al. [18] | 2006 | Upper arm/oscillometric (Omron M4) | OBP | None | – | – | Usual care |
| Verberk et al. [19] | 2007 | Upper arm/oscillometric (Omron HEM-705-CP) | OBP, 24 h-/day/night ABP, HBP | Change in medication | – | – | Usual care |
| Kauric-Klein and Artinian [20] | 2007 | Upper arm/oscillometric (Omron 1C) | OBP | Other (hemodialysis) | – | – | Education |
| Artinian et al. [21] | 2007 | Upper arm/oscillometric (A&D UA-767) | OBP | Education | Telemonitoring | Nurse support | Usual care |
| Tobe et al. [22] | 2008 | Upper arm/oscillometric (A&D UA-767P) | OBP | Change in medication | – | – | Usual care |
| Madsen et al. [23] | 2008 | Upper arm/semi-automatic oscillometric (Omron 705IT) | Day/night ABP | None | Telemonitoring | – | Usual care |
| Green et al. [24] | 2008 | Upper arm/oscillometric (Omron HEM-705-CP) | OBP | Education |
(1) Web-site use (2) Web-site use |
(1) None (2) Pharmacist support |
Usual care |
| Parati et al. [25] | 2009 | Upper arm/oscillometric (Tensioday, Tensiomed) | OBP, day ABP | None | Telemonitoring | – | Setting target BP |
| da Silva et al. [26] | 2009 | Upper arm/oscillometric (Omron HEM-705-CP) | 24 h-ABP/HBP | Change in medication | – | – | Usual care |
| Dejesus et al. [27] | 2009 | Upper arm/oscillometric (Life Source UA-767 Plus) | OBP | Education | – | (A class focusing on hypertension in diabetes) | Education (data based on no intervention group was not considered) |
| Bosworth et al. [28] | 2009 | Upper arm/oscillometric (Omron HEM 773AC) or wrist/oscillometric (Omron HEM 637) | OBP | None | Mailing BP logs to the center | – | Usual care |
| Rinfret et al. [29] | 2009 | Upper arm/digital (Omron HEM-711AC) | 24 h-ABP | Education/change in medication | Telemonitoring | – | Usual care |
| Godwin et al. [30] | 2010 | Upper arm/oscillometric (A&D UA-767) | 24 h-ABP | None | – | – | Usual care |
| McManus et al. [31] | 2010 | Upper arm/automated sphygmomanometer (Omron 705IT) | OBP | Change in medication | Telemonitoring | – | Usual care |
| Varis and Kantola [32] | 2010 | Upper arm/oscillometric (Omron 1C) | OBP | None | Mailing BP logs to the center | – | Usual care |
| Bosworth et al. [33] | 2011 | Upper arm/oscillometric (A&D UA-767PC) | OBP | Change in medication | Telemedicine (Behavioral Management Intervention group was not considered) | Nurse support | Usual care |
| Magid et al. [34] | 2011 | Upper arm/oscillometric (A&D UA-767) | OBP | Education | Telemonitoring | Pharmacist support | Usual care |
| Hebert et al. [35] | 2012 | Upper arm/oscillometric (Omron HEM-712C) | OBP |
(1) None (2) Education |
(1) None (2) Telephone calls including checking BP on a phone |
(1) None (2) Nurse support |
Usual care |
| Fuchs et al. [36] | 2012 | Upper arm/oscillometric (Omron HEM-705-CP) | OBP, 24 h-/day/night ABP | Half of them received pharmacist care | – | – | Usual care (but half of them received pharmacist care) |
| Piette et al. [37] | 2012 | Unknown device (in-home cuffs for measurement of BP [on Web page of protocol]) | OBP | Education | Automated telephone call | – | Usual care |
| Williams et al. [38] | 2012 | Upper arm/oscillometric (A&D UA-787) | OBP | Education | – | Nurse support | Usual care |
| Kerry et al. [39] | 2013 | Upper arm/oscillometric (Omron M6) | OBP | Education | Telephone calls including checking BP on a phone | Nurse support | Usual care |
| Magid et al. [40] | 2013 | Upper arm/oscillometric (Omron HEM-790IT) | OBP | Education/change in medication | Telemonitoring | Pharmacist support | Usual care |
| McKinstry et al. [41] | 2013 | Upper arm/oscillometric (Stabil-O-Graph mobil) | Day ABP | None | Telemonitoring | – | Usual care |
| Margolis et al. [42] | 2013 | Upper arm/oscillometric (A&D 767PC) | OBP | Education/change in medication | Telemonitoring | Pharmacist support | Education |
| Ogedegbe et al. [43] | 2014 | Upper arm/oscillometric (Microlife BP 3AC1-1) | OBP | Education | – | – | Education |
| Stewart et al. [44] | 2014 | Upper arm/oscillometric (Omron T9IT) | OBP |
Education Change in medication |
– | Pharmacist support | Usual care |
| McManus et al. [45] | 2014 | Upper arm/oscillometric (Microlife Watch BP Home) | OBP | Change in medication | – | – | Usual care |
| Hosseininasab et al. [46] | 2014 | Wrist/oscillometric (Samsung C&T SHB-200w) | OBP | None | – | – | Usual care |
| Kim et al. [47] | 2014 | Upper arm/oscillometric (A&D UA-767) | OBP | Education | Telemonitoring | Nurses and nutritionists support | Usual care |
| Yi et al. [48] | 2015 | Unknown device but considered to be cuff-type | OBP | Education | Telemonitoring | — | Usual care |
| Hanley et al. [49] | 2015 | Upper arm/oscillometric (IEM Stabil-O-graph) | Day ABP | None | Telemonitoring | Nurse support | Usual care |
| Aekplakorn et al. [50] | 2016 | Upper arm/oscillometric (Omron HEM-7117) | OBP | None | – | – | Usual care |
| Kim et al. [51] | 2016 | Upper arm/oscillometric (Withings BP Monitor) | OBP | Education | Reminder by an App | – | Usual care |
| Tzourio et al. [52] | 2017 | Upper arm/oscillometric (Omron M6) | OBP, HBP | None | – | – | Usual care |
| Klarskov et al. [53] | 2018 | Upper arm/oscillometric (Microlife BP 3AC1) | OBP, day/night ABP | None | – | – | Usual care |
| Martinez et al. [54] | 2018 | Upper arm/oscillometric (Microlife WatchHome) | 24 h-/day/night ABP | None | – | – | Usual care |
| McManus et al. [55] | 2018 | Upper arm/oscillometric (Omron M10-IT) | OBP | Change in medication |
(1) None (2) Telemonitoring |
– | Usual care |
| Pan et al. [56] | 2018 | Upper arm/oscillometric (“maibobo” RBP3900 and RBP9000) | OBP | Education | Telemonitoring | A technology including an App | Usual care |
| Skolarus et al. [57] | 2018 | Upper arm/oscillometric (Omron BP760) | OBP | Education | SMS message to remind BP measurements | – | Usual care |
| Cuffee et al. [58] | 2019 | [Upper arm/oscillometric (Carrera Upper Arm BP Monitor)] | 24 h-ABP | None | – | – |
Usual care Education |
| Gu et al. [59] | 2020 | Upper arm/oscillometric (KD598, Andon) | OBP | Other (Pedometer group was not considered) | Telephone calls | – | Education |
| Ojji et al. [60] | 2020 | Upper arm/oscillometric (Omron M3 HEM-7131-E) | OBP | None | – | – | Usual care |
| Zha et al. [61] | 2020 | Wrist/oscillometric (iHealth BP7 Wireless BP Monitor, iHealth Lab Inc.) | OBP | Education | Telemonitoring | Nurse support | Usual care |
| Ionov et al. [62] | 2021 | Unknown but the device had to be listed in the “STRIDE BP” database. | OBP, 24 h-ABP | Change in medication | Telemonitoring | – | Usual care |
| McManus et al. [63] | 2021 | Upper arm/oscillometric (Omron M3 monitor) | OBP | Education | Telemonitoring | A technology including an App | Usual care |
| Zhang et al. [64] | 2021 | Upper arm/oscillometric (HEM-7051, Omron Healthcare) | OBP | Setting target BP | – | – | Usual care (setting target BP) |
| Akl et al. [65] | 2021 | Upper arm/oscillometric (Omron MIT Elite Plus arm monitor) | OBP | Education | – | – | Usual care |
| Margolis et al. [66] | 2022 | Upper arm/oscillometric (A&D Medical 767PC) | OBP | Education | Telemonitoring | Pharmacist support | Usual care |
| Okoro et al. [67] | 2022 | Upper arm/oscillometric (Chidalex, Joytech Healthcare Co. Ltd) | OBP | Education | Telephone calls including checking BP on a phone | Pharmacist support | Usual care |
| Muijsers et al. [68] | 2022 | Upper arm/oscillometric (Withings BP Monitor) | OBP | Education | Telemonitoring | – | Usual care |
| Calderón-Anyosa et al. [69] | 2023 | Upper arm/oscillometric (Omron Series 10) | OBP | Change in medication | Telemonitoring | – | Usual care |
| Doogue et al. [70] | 2023 | Upper arm/oscillometric (Omron M10-IT) | OBP | Change in medication | Telemonitoring | – | Usual care |
| Hoppe et al. [71] | 2023 | Upper arm/oscillometric (Omron, 7 Series) | OBP, 24 h-ABP | Education | Telephone calls including checking BP on a phone | Health coaching | Usual care |
| Leupold et al. [72] | 2023 | Upper arm/oscillometric (BOSO® Medicus Family 4) | OBP | Change in medication | Telemonitoring | A technology including an App | Usual care |
| Martínez-Ibáñez et al. [73] | 2023 | Upper arm/oscillometric (Omron M3 HEM-7131-E) | OBP | Change in medication | – | – | Usual care |
| Nejamis et al. [74] | 2023 | Upper arm/oscillometric (automatic home BP monitor, model unspecified) | OBP | None (peer mentoring arm was excluded) | – | – | Usual care |
| Ramos-Zavala et al. [75] | 2023 | Upper arm/oscillometric (Omron HEM-9200T) | OBP | Education | Telemonitoring | – | Usual care |
BP blood pressure, OBP office blood pressure, ABP ambulatory blood pressure, HBP home blood pressure
The assessment of bias risk and indirectness is presented in Supplementary Table 4. Participants were not blinded in all studies because of the nature of the intervention, which increased performance bias. Twenty-four studies were assessed as having a high bias risk because at least one of the risks was high.
The effect of the intervention on BP
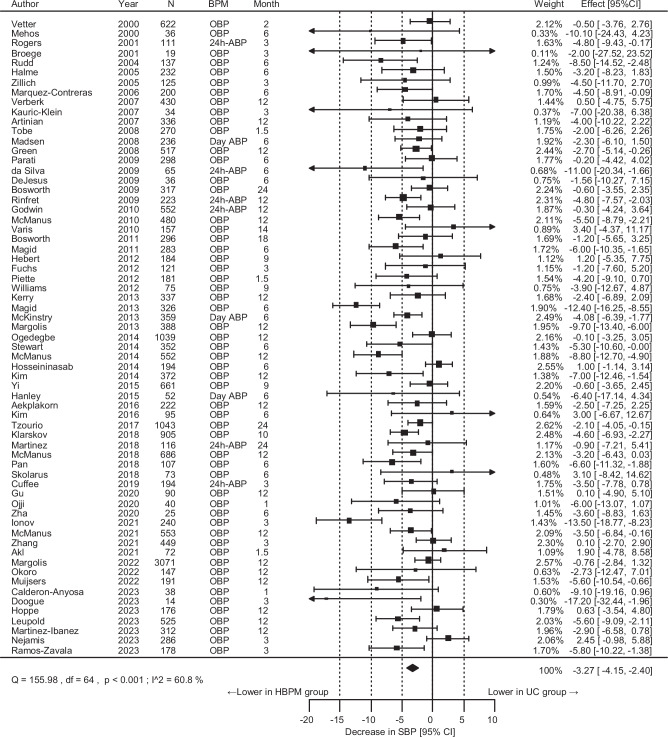
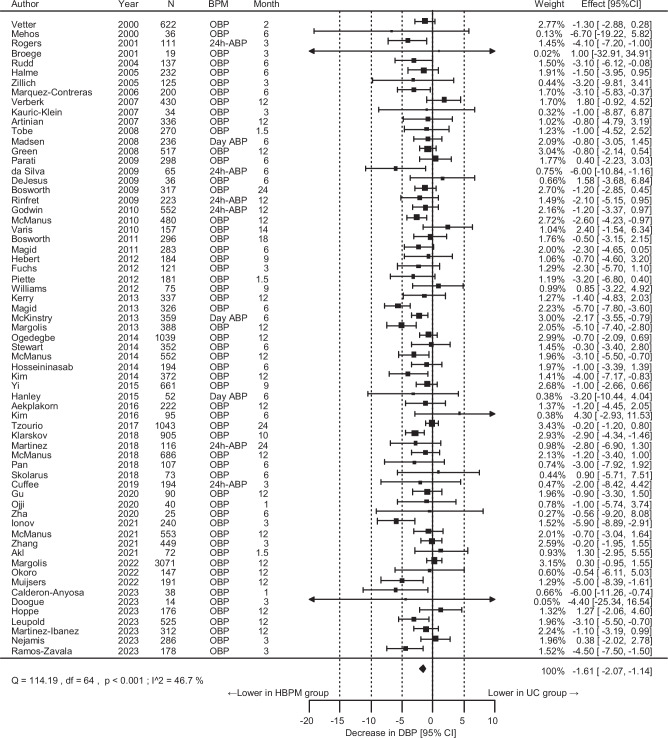
Of the 65 unique randomized controlled trials, 21,053 participants were included to assess SBP change outcomes. The SBP reduction was significantly greater by 3.27 mmHg at the end of the intervention in the HBPM than in the UC group, although the I2 value showed high heterogeneity (Fig. 1). Leave-one-out analysis did not identify any specific study to contribute to the high heterogeneity (I2 value: 53.7–61.6%). The DBP reduction was greater by 1.61 mmHg in the HBPM than in the UC group (Fig. 2, I2 value: 46.7%). Funnel plots did not exhibit notable publication bias or evidence of publication bias based on Egger’s test (p = 0.16 for SBP, p = 0.63 for DBP) (Supplementary Fig. 2).
Fig. 1.
Overall results for the differences in the systolic blood pressure (SBP) change. N indicates the final number of participants used for analysis in each study. CI confidence interval, BPM blood pressure measurement method to obtain the outcome value, OBP office blood pressure, ABP ambulatory blood pressure, HBPM home blood pressure measurement, UC usual care
Fig. 2.
Overall results for the difference in the diastolic blood pressure (DBP) change. N indicates the final number of participants used for analysis in each study. CI confidence interval, BPM blood pressure measurement method to obtain the outcome value, OBP office blood pressure, ABP ambulatory blood pressure, HBPM home blood pressure measurement, UC usual care
The proportion of participants with controlled BP at the follow-up examination was significantly higher in the HBPM group than in the UC group (proportion rate [95%CI]: 1.24 [1.15–1.34], proportion difference [95%CI]: 0.11% [0.07–0.15], Supplementary Fig. 3) when the sub-analysis was performed in the 30 studies with available data.
Sensitivity analysis regarding the BP outcome
HBPM intervention was similarly associated with a lower BP change regardless of the type of outcome measure (office or ambulatory BP) (Supplementary Fig. 4 for SBP change and Supplementary Fig. 5 for DBP change). After excluding the 23 studies with a high risk of bias, the result was similar and there was no change in heterogeneity The systolic/diastolic BP change was greater in the HBPM group by 3.47 (95% CI: 2.37–4.56) mmHg (I2 = 60.9%)/1.72 (95% CI: 1.15–2.28) (I2 = 43.3%) than the UC group.
To ensure the effect of the follow-up period, a meta-regression analysis was performed based on 97 points of estimates from 65 studies. There was a J-shaped association between follow-up periods and differences in BP changes (Supplementary Fig. 6). The upper limit of the 95% CI became >0 at 20.5 months for the differences in SBP change and 19.5 months for the DBP change, although only three studies indicated the effect of HBPM intervention after 20 months. In an analysis based on the five studies with a follow-up period >12 months, the SBP and DBP changes between groups were lower than the main analysis and became non-significant levels (HBPM minus UC: −1.38 [95% CI: −2.84 to 0.08] mmHg for SBP change and −0.44 [95% CI: −1.23 to 0.34] mmHg for DBP change).
A wrist cuff device was used for the HBPM intervention in four studies (Supplementary Figs. 7 and 8). HBPM intervention was not associated with SBP change when the results from the four studies were combined (−0.06 [95%CI: −1.53 to 1.40] mmHg Supplementary Fig. 7).
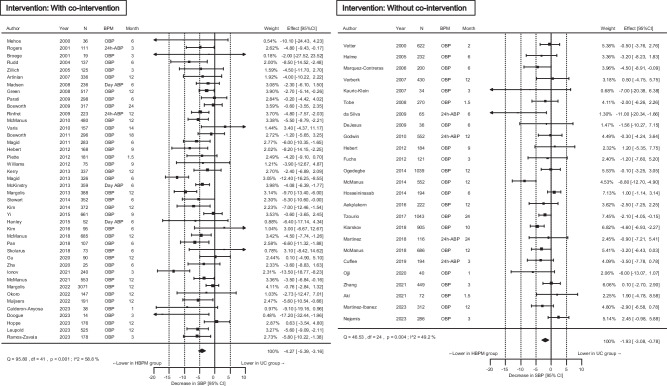
HBPM analysis with a co-intervention (such as telemonitoring) showed a stronger BP-lowering effect than without co-intervention. The effect of HBPM on BP change remained significant without a co-intervention (Figs. 3 and 4). After further stratification by the type of co-intervention, BP reduction by HBPM was greater in the intervention with telemonitoring or co-medical staff support than in those with other methods including those with only text messages or telephone calls (Supplementary Fig. 9).
Fig. 3.
Differences in the systolic blood pressure (SBP) change stratified by co-interventions. Co-intervention indicates support through telemonitoring, co-medical staff, or other methods including reminders via telephone or text message. CI confidence interval, BPM blood pressure measurement method to obtain the outcome value, OBP office blood pressure, ABP ambulatory blood pressure, HBPM home blood pressure measurement, UC usual care
Fig. 4.
Differences in the diastolic blood pressure (DBP) change stratified by co-interventions. Co-intervention indicates support through telemonitoring, co-medical staff, or other methods including reminders via telephone or text message. CI confidence interval, BPM blood pressure measurement method to obtain the outcome value, OBP office blood pressure, ABP ambulatory blood pressure, HBPM home blood pressure measurement, UC usual care
Antihypertensive drug change
Of the 65 studies, 11 reported a change in the number of antihypertensive medications. The number of antihypertensive medications increased by 0.17 medications in the HBPM than in the UC group (Supplementary Fig. 10). The BP-lowering effect of HBPM was more pronounced as the number of antihypertensive medications increased while the meta-regression analysis showed the intercept of the regression slope was −1.72/−1.40 mmHg for SBP/DBP change (p = 0.0085/0.012) (Supplementary Fig. 11).
Other outcomes
We collected information on changes in BMI as a representative index of cardiovascular disease risk factors. No significant difference in BMI change was found when the results of four studies were combined (HBPM minus UC: 0.17 [95%CI: −0.18 to 0.52] kg/m2, Supplementary Fig. 12).
Death and cardiovascular disease outcomes were reported as severe adverse events in three studies and five studies, respectively. The analyses based on these studies showed that the risk ratios of HBPM vs UC as a reference for death and cardiovascular diseases were 1.03 (95% CI: 0.63–1.70) and 1.20 (95% CI: 0.68–2.11), respectively, and there were no significant differences between the groups (Supplementary Fig. 13).
Discussion
The present study demonstrated that HBPM was significantly associated with a larger BP reduction when compared with the UC. A larger BP reduction favoring HBPM was observed when the intervention period was within 20 months, when HBPM was combined with co-interventions such as telemonitoring or co-medical staff support, or when HBPM was performed using an upper-arm cuff device. The meta-analysis had a high heterogeneity but no significant publication bias was observed.
The present meta-analysis revealed that the HBPM can lower SBP/DBP by 3.27/1.61 mmHg more than the UC. HBPM has been recommended for monitoring BP in patients with hypertension because home BP is a stronger predictor of cardiovascular diseases, provides more precise and accurate BP information, and captures longer-term BP or pulse rate variations than office BP [1]. In the previous meta-analyses, HBPM intervention was reported to lower SBP/DBP by 2.63–3.82/1.45–1.68 mmHg compared with UC [5–7]. The values presented in the previous meta-analyses are similar to the present study findings, but the present study estimates the values more accurately by including the latest studies.
A favorable association between HBPM and BP changes appeared to be weakened or enhanced under certain conditions. First, the effect of HBPM may have weakened 20 months after the initiation of the intervention. However, this point should be re-evaluated in the future, as there were only three trials with interventions lasting more than 20 months. Second, the combination of telemonitoring and co-medical staff support can enhance the BP-lowering effect of HBPM, which has been supported by previous meta-analyses [5–7]. The latest individual participant data meta-analysis (IPD) suggested that HBPM alone was not associated with lower BP in the absence of co-interventions [5]. This IPD meta-analysis did not include studies with small sample sizes (n < 200). Meanwhile, the present meta-analysis, which evaluated a whole study, suggested that a small but significant favorable BP change could be caused by HBPM, even in the absence of co-interventions. Third, HBPM using a wrist cuff device may not improve the patient’s BP, although the number of reports based on a wrist cuff device was limited. Increasing the sample size may not change this outcome because the effect size of wrist cuff device-based HBPM on systolic BP is almost negligible. Therefore, a thorough review of the protocol may be required to detect the beneficial effects of HBPM using a wrist cuff device. For instance, the use of newly developed wrist cuff devices designed for accurate BP measurement or the implementation of strict patient education may be necessary. An upper arm cuff device has been recommended to obtain accurate BP [1]. The present findings suggest that accurate measurement of BP with an upper arm cuff is critical to obtain the benefits of HBPM at this time.
Our sensitivity analysis suggested that intensifying the antihypertensive treatment might have caused the BP-lowering effect of HBPM. The previous IPD meta-analysis also indicated a correlation between increased number of medication changes and reduced BP, which is similar to the present study results [5]. Home BP-based treatment is superior to office BP-based treatment in achieving the BP target [76]. These findings suggest that HBPM can help identify masked or white-coat uncontrolled hypertension and appropriately adjust for antihypertensive medications. Meanwhile, the meta-regression analysis showed that the intercept of the regression equation between the group difference in the change of antihypertensive medication and the group difference in the BP-lowering effect of HBPM was significantly negative. This intercept reflects the effect of HBPM when the antihypertensive medications were adjusted equally between HBPM and UC groups. Therefore, HBPM per se presumably has a BP-lowering effect even when antihypertensive medications are not changed. Two studies reported that systolic BP tended to decrease more in the HBPM group than in the UC group, despite almost no difference in the change of antihypertensive medication between the groups [39, 58]. Although the effect of HBPM on systolic BP change in each study was not statistically significant [39, 58], the present meta-analysis demonstrated a possible effect of HBPM independent of antihypertensive medication changes by combining the results from these studies. Based on previous studies [77, 78], improved medication adherence or personalized antihypertensive treatment could have contributed to HBPM’s effectiveness. Another potential pathway for HBPM’s effect could be lifestyle improvement through self-feedback of BP levels although our meta-analysis did not reveal significant difference in BMI changes between HBPM and UC groups.
We found no significant differences in the risk of death or cardiovascular diseases as severe outcomes between the HBPM and UC groups. To capture the risks of these outcomes, a long-term follow-up period and more accurate outcome measurements are required. A previous study based on patients treated with antihypertensive medications estimated that reducing systolic BP by 5 mmHg led to a 9% risk reduction of cardiovascular diseases [79]. Based on this evidence [79], a reduction in systolic BP of 3.27 mmHg with HBPM might reduce cardiovascular risks by 6.0%, if our results can be applied to the management of hypertensive patients.
Our study has several limitations. First, heterogeneity was high in most analyses. This may be due to variations in the inclusion criteria, HBPM intervention methods, outcome measures, and follow-up period. If HBPM method is introduced in clinical practice, we should refer to an individual study with a similar intervention method. Second, we could not evaluate the long-term effects of HBPM beyond 1.5 years because of the limited number of trials. Third, owing to the nature of the intervention, the results may be biased based on the Hawthorne effect. However, HBPM intervention is expected to contain the effect by encouraging participants to improve their health behaviors in the first place. It is difficult to distinguish biases such as Hawthorne effect from the effects of HBPM. Fourth, we could not conduct analyses for health behavioral changes to lower BP, adherence to HBPM, and change in the quality of life because of the inconsistent outcomes or missing values among the reports although these were set as additional outcomes in our protocol. One meta-analysis that investigated the effect of HBPM on medication adherence suggested that HBPM intervention may contribute to improved medication adherence [77]. Finally, most studies were based on participants under antihypertensive treatment or populations mixed with treated and untreated individuals. Antihypertensive treatment may have been initiated in participants without prior treatment. Therefore, future studies in non-hypertensive patients who do not require pharmacological therapy may be necessary to assess the impact of HBPM that is not mediated by antihypertensive medications.
Conclusion
Our results demonstrated a beneficial effect of HBPM in lowering BP, particularly when used in conjunction with telemonitoring or additional medical support, and when measurements are taken with an upper-arm cuff device. Although further research is required to elucidate the long-term effects of HBPM and its impact on severe health outcomes, HBPM is a valuable tool for the treatment of hypertension, potentially enhancing medication adherence and facilitating more personalized and effective management of BP. The development and dissemination of digital technologies for HBPM and support systems can aid in BP management.
Supplementary information
Acknowledgements
This research was supported by the Japan Agency for Medical Research and Development (AMED) (Grant Number 22rea522002h0001). This manuscript’s writing was assisted by ChatGPT, Grammarly, and Claude for language support.
Author contributions
M Satoh: conceptualization, data curation, formal analysis, investigation, resources, methodology, validation, visualization, supervision, and writing of the original draft. Y Tatsumi and S Nakayama: conceptualization, data curation, formal analysis, investigation, resources, methodology, validation, and visualization. Y Shinohara, M Kawazoe, Y Nozato, A Kunimura, T Murakami, M Toyama, T Muroya, T Yagihashi: conceptualization, data curation, investigation, resources, methodology, and validation. A Sakima, M Abe, H Arima, T Ohkubo: conceptualization, investigation, methodology, project administration, and supervision. All coauthors were involved in writing, reviewing, and editing the manuscript.
Data availability
The authors declare that all supporting data are available in the article and online Supplementary files.
Compliance with ethical standards
Conflict of interest
TO received honoraria (lecture fee) and a joint research grant from Omron Healthcare Co., Ltd.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41440-024-01981-4.
References
- 1.Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 3.Satoh M, Asayama K, Kikuya M, Inoue R, Metoki H, Hosaka M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension. 2016;67:48–55. [DOI] [PubMed] [Google Scholar]
- 4.Mancia G, Kreutz R, Brunstrom M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41:1874–2071. [DOI] [PubMed] [Google Scholar]
- 5.Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14:e1002389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bray EP, Holder R, Mant J, McManus RJ. Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann Med. 2010;42:371–86. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38. [DOI] [PubMed] [Google Scholar]
- 8.Uhlig K, Patel K, Ip S, Kitsios GD, Balk EM. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–94. [DOI] [PubMed] [Google Scholar]
- 9.Medical Information Network Distribution Service (Minds). Minds Manual for Guideline Development 2020 ver. 3.0. (in Japanese). 2021. https://minds.jcqhc.or.jp/s/manual_2020_3_0. Accessed 29 Jan 2024.
- 10.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vetter W, Hess L, Brignoli R. Influence of self-measurement of blood pressure on the responder rate in hypertensive patients treated with losartan: results of the SVATCH Study. Standard vs automatic treatment control of COSAAR in hypertension. J Hum Hypertens. 2000;14:235–41. [DOI] [PubMed] [Google Scholar]
- 12.Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy. 2000;20:1384–9. [DOI] [PubMed] [Google Scholar]
- 13.Rogers MA, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension: a randomized, controlled trial. Ann Intern Med. 2001;134:1024–32. [DOI] [PubMed] [Google Scholar]
- 14.Broege PA, James GD, Pickering TG. Management of hypertension in the elderly using home blood pressures. Blood Press Monit. 2001;6:139–44. [DOI] [PubMed] [Google Scholar]
- 15.Rudd P, Miller NH, Kaufman J, Kraemer HC, Bandura A, Greenwald G, et al. Nurse management for hypertension: a systems approach. Am J Hypertens. 2004;17:921–7. [DOI] [PubMed] [Google Scholar]
- 16.Halme L, Vesalainen R, Kaaja M, Kantola I, group HOMobps. Self-monitoring of blood pressure promotes achievement of blood pressure target in primary health care. Am J Hypertens. 2005;18:1415–20. [DOI] [PubMed] [Google Scholar]
- 17.Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). J Gen Intern Med. 2005;20:1091–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marquez-Contreras E, Martell-Claros N, Gil-Guillen V, de la Figuera-Von Wichmann M, Casado-Martinez JJ, Martin-de Pablos JL, et al. Efficacy of a home blood pressure monitoring programme on therapeutic compliance in hypertension: the EAPACUM-HTA study. J Hypertens. 2006;24:169–75. [DOI] [PubMed] [Google Scholar]
- 19.Verberk WJ, Thien T, Kroon AA, Lenders JW, van Montfrans GA, Smit AJ, et al. Prevalence and persistence of masked hypertension in treated hypertensive patients. Am J Hypertens. 2007;20:1258–65. [DOI] [PubMed] [Google Scholar]
- 20.Kauric-Klein Z, Artinian N. Improving blood pressure control in hypertensive hemodialysis patients. CANNT J. 2007;17:24–8. [PubMed] [Google Scholar]
- 21.Artinian NT, Flack JM, Nordstrom CK, Hockman EM, Washington OG, Jen KL, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007;56:312–22. [DOI] [PubMed] [Google Scholar]
- 22.Tobe SW, Hunter K, Geerts R, Raymond N, Pylypchuk G, Canadian Hypertension S. IMPPACT: Investigation of Medical Professionals and Patients Achieving Control Together. Can J Cardiol. 2008;24:205–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Madsen LB, Kirkegaard P, Pedersen EB. Blood pressure control during telemonitoring of home blood pressure. a randomized controlled trial during 6 months. Blood Press. 2008;17:78–86. [DOI] [PubMed] [Google Scholar]
- 24.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parati G, Omboni S, Albini F, Piantoni L, Giuliano A, Revera M, et al. Home blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare study. J Hypertens. 2009;27:198–203. [DOI] [PubMed] [Google Scholar]
- 26.da Silva GV, de Barros S, Abensur H, Ortega KC, Mion D Jr, Cochrane Renal Group Prospective Trial Register CRG. Home blood pressure monitoring in blood pressure control among haemodialysis patients: an open randomized clinical trial. Nephrol Dial Transpl. 2009;24:3805–11. [DOI] [PubMed] [Google Scholar]
- 27.Dejesus RS, Chaudhry R, Leutink DJ, Hinton MA, Cha SS, Stroebel RJ. Effects of efforts to intensify management on blood pressure control among patients with type 2 diabetes mellitus and hypertension: a pilot study. Vasc Health Risk Manag. 2009;5:705–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bosworth HB, Olsen MK, Grubber JM, Neary AM, Orr MM, Powers BJ, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009;151:687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rinfret S, Lussier MT, Peirce A, Duhamel F, Cossette S, Lalonde L, et al. The impact of a multidisciplinary information technology-supported program on blood pressure control in primary care. Circ Cardiovasc Qual Outcomes. 2009;2:170–7. [DOI] [PubMed] [Google Scholar]
- 30.Godwin M, Lam M, Birtwhistle R, Delva D, Seguin R, Casson I, et al. A primary care pragmatic cluster randomized trial of the use of home blood pressure monitoring on blood pressure levels in hypertensive patients with above target blood pressure. Fam Pract. 2010;27:135–42. [DOI] [PubMed] [Google Scholar]
- 31.McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet. 2010;376:163–72. [DOI] [PubMed] [Google Scholar]
- 32.Varis J, Kantola I. The choice of home blood pressure result reporting method is essential: Results mailed to physicians did not improve hypertension control compared with ordinary office-based blood pressure treatment. Blood Press. 2010;19:319–24. [DOI] [PubMed] [Google Scholar]
- 33.Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011;171:1173–80. [DOI] [PubMed] [Google Scholar]
- 34.Magid DJ, Ho PM, Olson KL, Brand DW, Welch LK, Snow KE, et al. A multimodal blood pressure control intervention in 3 healthcare systems. Am J Manag Care. 2011;17:e96–103. [PubMed] [Google Scholar]
- 35.Hebert PL, Sisk JE, Tuzzio L, Casabianca JM, Pogue VA, Wang JJ, et al. Nurse-led disease management for hypertension control in a diverse urban community: a randomized trial. J Gen Intern Med. 2012;27:630–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fuchs SC, Ferreira-da-Silva AL, Moreira LB, Neyeloff JL, Fuchs FC, Gus M, et al. Efficacy of isolated home blood pressure monitoring for blood pressure control: randomized controlled trial with ambulatory blood pressure monitoring - MONITOR study. J Hypertens. 2012;30:75–80. [DOI] [PubMed] [Google Scholar]
- 37.Piette JD, Datwani H, Gaudioso S, Foster SM, Westphal J, Perry W, et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed E Health. 2012;18:613–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Williams A, Manias E, Walker R, Gorelik A. A multifactorial intervention to improve blood pressure control in co-existing diabetes and kidney disease: a feasibility randomized controlled trial. J Adv Nurs. 2012;68:2515–25. [DOI] [PubMed] [Google Scholar]
- 39.Kerry SM, Markus HS, Khong TK, Cloud GC, Tulloch J, Coster D, et al. Home blood pressure monitoring with nurse-led telephone support among patients with hypertension and a history of stroke: a community-based randomized controlled trial. CMAJ. 2013;185:23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist-led, American Heart Association Heart360 Web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes. 2013;6:157–63. [DOI] [PubMed] [Google Scholar]
- 41.McKinstry B, Hanley J, Wild S, Pagliari C, Paterson M, Lewis S, et al. Telemonitoring based service redesign for the management of uncontrolled hypertension: multicentre randomised controlled trial. BMJ. 2013;346:f3030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Margolis KL, Asche SE, Bergdall AR, Dehmer SP, Groen SE, Kadrmas HM, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ogedegbe G, Tobin JN, Fernandez S, Cassells A, Diaz-Gloster M, Khalida C, et al. Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects. Circulation. 2014;129:2044–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stewart K, George J, Mc Namara KP, Jackson SL, Peterson GM, Bereznicki LR, et al. A multifaceted pharmacist intervention to improve antihypertensive adherence: a cluster-randomized, controlled trial (HAPPy trial). J Clin Pharm Ther. 2014;39:527–34. [DOI] [PubMed] [Google Scholar]
- 45.McManus RJ, Mant J, Haque MS, Bray EP, Bryan S, Greenfield SM, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. [DOI] [PubMed] [Google Scholar]
- 46.Hosseininasab M, Jahangard-Rafsanjani Z, Mohagheghi A, Sarayani A, Rashidian A, Javadi M, et al. Self-monitoring of blood pressure for improving adherence to antihypertensive medicines and blood pressure control: a randomized controlled trial. Am J Hypertens. 2014;27:1339–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim KB, Han HR, Huh B, Nguyen T, Lee H, Kim MT. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27:1199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yi SS, Tabaei BP, Angell SY, Rapin A, Buck MD, Pagano WG, et al. Self-blood pressure monitoring in an urban, ethnically diverse population: a randomized clinical trial utilizing the electronic health record. Circ Cardiovasc Qual Outcomes. 2015;8:138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hanley J, Fairbrother P, Krishan A, McCloughan L, Padfield P, Paterson M, et al. Mixed methods feasibility study for a trial of blood pressure telemonitoring for people who have had stroke/transient ischaemic attack (TIA). Trials. 2015;16:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aekplakorn W, Suriyawongpaisal P, Tansirisithikul R, Sakulpipat T, Charoensuk P. Effectiveness of self-monitoring blood pressure in primary care: a randomized controlled trial. J Prim Care Community Health. 2016;7:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim JY, Wineinger NE, Steinhubl SR. The influence of wireless self-monitoring program on the relationship between patient activation and health behaviors, medication adherence, and blood pressure levels in hypertensive patients: a substudy of a randomized controlled trial. J Med Internet Res. 2016;18:e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tzourio C, Hanon O, Godin O, Soumare A, Dufouil C. Impact of home blood pressure monitoring on blood pressure control in older individuals: a French randomized study. J Hypertens. 2017;35:612–20. [DOI] [PubMed] [Google Scholar]
- 53.Klarskov P, Bang LE, Schultz-Larsen P, Gregers Petersen H, Benee Olsen D, Berg RMG, et al. Intensive versus conventional blood pressure monitoring in a general practice population. The Blood Pressure Reduction in Danish General Practice trial: a randomized controlled parallel group trial. Fam Pract. 2018;35:433–9. [DOI] [PubMed] [Google Scholar]
- 54.Martinez MA, Garcia-Puig J, Loeches MP, Mateo MC, Utiel I, Torres R, et al. Home blood pressure vs. clinic blood pressure measurement-based follow up in type ii diabetics: effect on 24-h ambulatory BP and albuminuria. Randomised trial. Med Clin. 2018;150:413–20. [DOI] [PubMed] [Google Scholar]
- 55.McManus RJ, Mant J, Franssen M, Nickless A, Schwartz C, Hodgkinson J, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet. 2018;391:949–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pan F, Wu H, Liu C, Zhang X, Peng W, Wei X, et al. Effects of home telemonitoring on the control of high blood pressure: a randomised control trial in the Fangzhuang Community Health Center, Beijing. Aust J Prim Health. 2018;24:398–403. [DOI] [PubMed] [Google Scholar]
- 57.Skolarus LE, Cowdery J, Dome M, Bailey S, Baek J, Byrd JB, et al. Reach out churches: a community-based participatory research pilot trial to assess the feasibility of a mobile health technology intervention to reduce blood pressure among African Americans. Health Promot Pract. 2018;19:495–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cuffee YL, Sciamanna C, Gerin W, Lehman E, Cover L, Johnson AA, et al. The effectiveness of home blood pressure on 24-hour blood pressure control: a randomized controlled trial. Am J Hypertens. 2019;32:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gu Y, Bao X, Wang Y, Meng G, Wu H, Zhang Q, et al. Effects of self-monitoring devices on blood pressure in older adults with hypertension and diabetes: a randomised controlled trial. J Epidemiol Community Health. 2020;74:137–43. [DOI] [PubMed] [Google Scholar]
- 60.Ojji DB, Baldridge AS, Orji AI, Shedul LG, Ojji OI, Egenti NB, et al. Feasibility and effect of community health worker support and home monitoring for blood pressure control in Nigeria: a randomised pilot trial. Cardiovasc J Afr. 2020;31:213–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zha P, Qureshi R, Porter S, Chao YY, Pacquiao D, Chase S, et al. Utilizing a mobile health intervention to manage hypertension in an underserved community. West J Nurs Res. 2020;42:201–9. [DOI] [PubMed] [Google Scholar]
- 62.Ionov MV, Zhukova OV, Yudina YS, Avdonina NG, Emelyanov IV, Kurapeev DI, et al. Value-based approach to blood pressure telemonitoring and remote counseling in hypertensive patients. Blood Press. 2021;30:20–30. [DOI] [PubMed] [Google Scholar]
- 63.McManus RJ, Little P, Stuart B, Morton K, Raftery J, Kelly J, et al. Home and online management and evaluation of blood pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ. 2021;372:m4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang D, Huang QF, Li Y, Wang JG. A randomized controlled trial on home blood pressure monitoring and quality of care in stage 2 and 3 hypertension. Hypertens Res. 2021;44:533–40. [DOI] [PubMed] [Google Scholar]
- 65.Akl C, Rashidi N, Akik C, Hitti E, Hamadeh G, Badr K, et al. Self-monitoring of blood pressure to improve hypertension management in a middle-income country: a proof of concept study. 2020. 10.21203/rs.3.rs-25446/v1.
- 66.Margolis KL, Bergdall AR, Crain AL, JaKa MM, Anderson JP, Solberg LI, et al. Comparing pharmacist-led telehealth care and clinic-based care for uncontrolled high blood pressure: the hyperlink 3 pragmatic cluster-randomized trial. Hypertension. 2022;79:2708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Okoro RN, Umate I, Ohieku JD, Yakubu SI, Adibe MO. The impact of pharmacist-led interventions on blood pressure control among patients with chronic kidney disease: a randomized controlled trial. JACCP J Am Coll Clin Pharm. 2022;5:1062–74. [Google Scholar]
- 68.Muijsers HEC, Wu P, van der Heijden OWH, Wijnberger LDE, van Bijsterveldt C, Buijs C, et al. Home blood pressure monitoring detects unrevealed hypertension in women with a history of preeclampsia: results of the BP-PRESELF study. Am J Prev Cardiol. 2022;12:100429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Calderon-Anyosa R, Tincopa JP, Raza M, Carcamo CP. Randomized controlled trial of home telemonitoring of blood pressure with an adapted tensiometer with SMS capability. Eur J Investig Health Psychol Educ. 2023;13:440–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Doogue R, Hayes P, Hebert R, Sheikhi A, Rai T, Morton K, et al. Towards an integrated blood pressure self-monitoring solution for stroke/TIA in Ireland: a mixed methods feasibility study for the TASMIN5S IRL randomised controlled trial. Pilot Feasibility Stud. 2023;9:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hoppe KK, Smith M, Birstler J, Kim K, Sullivan-Vedder L, LaMantia JN, et al. Effect of a telephone health coaching intervention on hypertension control in young adults: the MyHEART randomized clinical trial. JAMA Netw Open. 2023;6:e2255618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Leupold F, Karimzadeh A, Breitkreuz T, Draht F, Klidis K, Grobe T, et al. Digital redesign of hypertension management with practice and patient apps for blood pressure control (PIA study): a cluster-randomised controlled trial in general practices. EClinicalMedicine. 2023;55:101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martinez-Ibanez P, Marco-Moreno I, Peiro S, Martinez-Ibanez L, Barreira-Franch I, Bellot-Pujalte L, et al. Home blood pressure self-monitoring plus self-titration of antihypertensive medication for poorly controlled hypertension in primary care: the ADAMPA randomized clinical trial. J Gen Intern Med. 2023;38:81–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nejamis A, Chaparro M, Gibbons L, Poggio R, Moyano DL, Irazola V. Effectiveness of peer mentoring and self-monitoring to improve blood pressure control in a vulnerable population in Argentina: pragmatic randomized open-label controlled trial. Chronic Illn. 2023. 10.1177/17423953231187170. [DOI] [PubMed]
- 75.Ramos-Zavala MG, Grover-Paez F, Cardona-Munoz EG, Cardona-Muller D, Alanis-Sanchez AG, Pascoe-Gonzalez S, et al. Comparison of the use of blood pressure telemonitoring versus standard medical care in the achievement of short-term therapeutic goals in blood pressure in patients with uncontrolled hypertension: an open-label clinical trial. JRSM Cardiovasc Dis. 2023;12:20480040231178585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Satoh M, Maeda T, Hoshide S, Ohkubo T. Is antihypertensive treatment based on home blood pressure recommended rather than that based on office blood pressure in adults with essential hypertension? (meta-analysis). Hypertens Res. 2019;42:807–16. [DOI] [PubMed] [Google Scholar]
- 77.Fletcher BR, Hartmann-Boyce J, Hinton L, McManus RJ. The effect of self-monitoring of blood pressure on medication adherence and lifestyle factors: a systematic review and meta-analysis. Am J Hypertens. 2015;28:1209–21. [DOI] [PubMed] [Google Scholar]
- 78.Sundstrom J, Lind L, Nowrouzi S, Hagstrom E, Held C, Lytsy P, et al. Heterogeneity in blood pressure response to 4 antihypertensive drugs: a randomized clinical trial. JAMA. 2023;329:1160–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Blood Pressure Lowering Treatment Trialists Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors declare that all supporting data are available in the article and online Supplementary files.