Abstract
Introduction:
Infected gap non-union is a serious complication seen in cases of diaphyseal fracture of forearm bones. It carries high morbidity in the form of severe functional impairment and poses a challenge to treat due to the complex anatomical relationship and articulations involved. Though there are multiple treatment options available, there are no guidelines for its management. Each case is unique and requires a customized, patient-specific approach.
Case Report:
A 43-year-old man sustained a road traffic accident with closed both bone forearm fracture 6 months ago and was treated elsewhere with open reduction plate fixation of the radius, and Kirchner wire fixation of the ulna at an outside centre. Subsequently, he developed a purulent discharging sinus from the surgical site. After 7 months, following a trivial injury, the patient developed a deformity in his forearm. X-ray findings revealed a bent radial plate, signs of osteolysis, implant loosening along with displaced shaft of ulna fracture. The patient underwent implant removal with radial shortening and plate osteosynthesis for the radius and ulna.
Conclusion:
In cases of infected gap non-union of radius and ulna, the key for management is thorough debridement with retention of vascularity by minimal soft tissue damage, followed by rigid fixation of the fracture. Simultaneously, adequate steps should be taken to manage the infection, such as culture-specific antibiotics and monitoring of inflammatory markers such as complete blood count, Erythrocyte sedimentation rate, and C-reactive protein.
Keywords: Forearm, infected non-union, plate osteosynthesis, docking, radius, ulna
Learning Point of the Article:
In cases of infected gap non-union of both bones forearm, shortening and acute docking with plate osteosynthesis could be considered as a good alternative to current modalities of management with no recurrence of infection and good post-operative functional outcome.
Introduction
Infected gap non-unions of the forearm are difficult to treat. The presence of infection, lack of bone apposition, and unique forearm anatomy may lead to significant functional disability. Biological factors such as smoking, diabetes, and mechanical factors such as inadequate fixation can predispose to non-union [1, 2]. The presence of a gap between the fracture ends creates a dead space for the infection to persist. A stable forearm is necessary for the proper function of the hand. A gap non-union causes instability of the forearm, and alteration of the normal radius-ulna relation can cause reduction in pronation-supination. The function can further be reduced extraarticular or intraarticular stiffness of elbow, wrist, and hand joints with prolonged immobilization. Hence, the goals of management are infection control, restoration of forearm anatomy, and achieving bone union [3, 4]. Though there are multiple methods of treatment, there are no standard guidelines for the same. Treatment options include staged revision versus single-stage debridement and fixation. Fixation methods can be internal fixation or ring fixation or the Masquelet technique [5]. Ring fixators are reliable and stable but the treatment is prolonged. Ring fixators are necessary in severe bone loss needing bone lengthening [3]. Lesser defects can be managed by primary internal fixation with bone grafting but can risk recurrence of infection. Here, we report a case of infected gap non-union of radius and ulna with implant failure managed with radial shortening and acute docking with plate-osteosynthesis.
Case Report
A 43-year-old man presented to us with a complaint of discharging sinus for the past 7 months and deformity in his left forearm for the past month. The patient sustained a fracture in the mid-shaft of radius and ulna after a road traffic accident 8 months ago. The patient underwent open reduction and plate fixation of the radius with Kirchner wire (K-wire) fixation of the ulna in an outside centre (Fig.1). 15 days post-surgery, the patient developed a purulent discharging sinus from the surgical site from both surgical scares and was managed with debridement and the ulna K-wire removal (Fig. 2). The condition persisted for the next 7 months during which no antibiotics taken by the patient. later due to a trivial injury, the patient developed a deformity in his forearm. The patient had severe functional limitation and had a disabilities of the arm, shoulder, and hand (DASH) score of 86 [6]. X-ray findings revealed a bent radial plate, with osteolysis, implant loosening, and displaced shaft of ulna fracture(Fig. 3). The patient underwent implant removal with shortening of the radius by 2 cm with freshening the fracture site until bone with good vascularity was seen, and plate osteosynthesis for radius and ulna. The resected end of the radius was used as a bone graft (Fig. 4). Post-operatively patient’s grip strength was reduced but on subsequent follow-ups it progressively improved and at 1 year of follow up patient regained full grip strength. At 1-year follow-up, radiographs suggested union and there were no signs of infection (Fig. 5). On measurement the patient had a 2 cm shortening for both radius and ulna in the operated forearm, elbow range of motion is from 0 to 140°, wrist supination of 70, and pronation of 50°(Fig. 6-8). He is able to carry out his daily activities and has a post-operative DASH score of 5.8.
Figure 1.
X-ray anterior-posterior and lateral views for left forearm; Post-operative X-ray of left forearm after the first surgery.
Figure 2.
X-ray anterior-posterior and lateral views for left forearm; Post-operative X-ray of left forearm at the onset of pus discharge, the patient underwent debridement and ulna Kirchner wire removal.
Figure 3.

X-ray anterior-posterior and lateral views for left forearm; X-ray of left forearm at presentation, with deformity due to the trivial trauma.
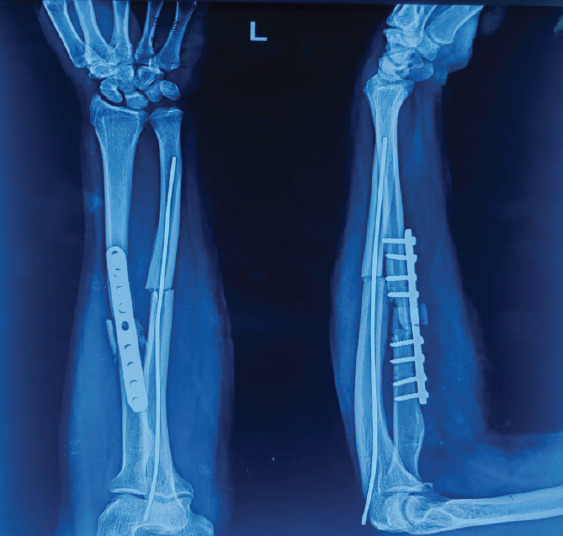
Figure 4.

X-ray anterior-posterior and lateral views for left forearm; immediate post-operative X-ray of left forearm.
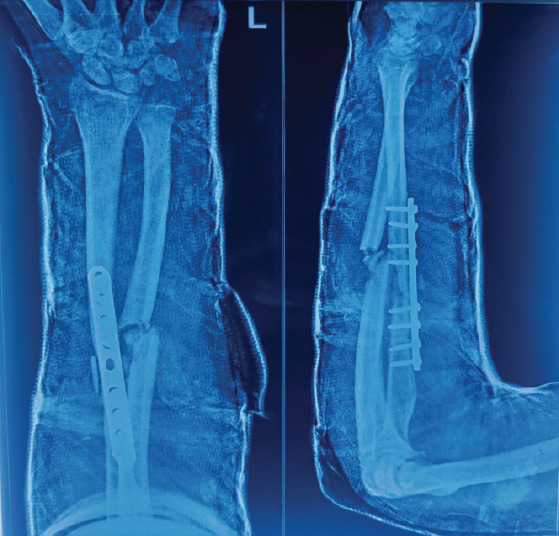
Figure 5.

X-ray anterior-posterior and lateral views for left forearm; 1-year follow-up post-operative X-ray of left forearm.
Figure 6.

Clinical picture of bilateral arms. Clinical picture of bilateral forearms showing shortening of the operated forearm.
Figure 8.

Clinical picture of the left arm. Clinical picture of left arm showing pronation and supination of the wrist at 1-year follow-up.
Figure 7.

Clinical picture of the left arm. Clinical picture of left arm showing flexion and extension of the elbow at 1-year follow-up.
Discussion
At present, there are no standardized guidelines for treating infected gap non-union of forearm bones. Given the individualized nature of each patient’s presentation, personalized care is needed. Treatment options for this condition vary widely and can be tailored based on factors such as the extent of bone gap, fracture pattern, stage of infection, skin condition, and the patient’s overall health. Ebied et al. conducted a case series of nine patients suffering from infected non-union of diaphyseal fractures of the radius and ulna, which were managed by a two-staged treatment strategy: First, radical debridement followed by an interval of antibiotics and application of a ring external fixator in the final stage. All fractures achieved union with improved functional outcomes [3]. Perna et al. conducted a retrospective study on 18 patients with infected non-union of forearm bones, which were managed by a two-staged surgical treatment: First, debridement and temporary stabilization of the non-union until infection has cleared, followed by a new synthesis with plate, opposite bone graft strut, and intercalary graft. Resolution of the infectious process and union with good functional results and a low rate of complications were achieved [4]. In our case, on pre-operative evaluation and intraoperatively, it appeared that the infection had resolved. Therefore, we did a single-stage procedure following radical debridement. Liu et al. conducted a retrospective study to evaluate the outcomes in 21 cases of infected non-union of forearm bones, which were treated with debridement followed by bone transport using a unilateral external fixator. All patients achieved bony union with satisfactory functional and cosmetic outcomes [7]. Dhar et al. conducted a case series involving twelve cases of infected non-union of the forearm, all managed with the two-staged induced membrane technique. All twelve bones united uneventfully within a range of 6–12 months [8]. Parihar et al. described treating a 42-year-old woman with infected non-union of the radius and ulna. After initial surgery with a compression plate, she underwent debridement and intramedullary nail placement, followed by vascularized fibula grafting and plate fixation. 1 year later, she had a favorable outcome [9]. In our case, rather than planning bone transport for the ulna to address the bone gap, we opted to shorten the radius to achieve cortical contact, followed by rigid fixation, and excised cortical bone from the radius was used as a bone graft. Baringa et al. conducted a cadaveric study in which they sequentially shortened the forearm by 2, 4, and 6 cm and internal fixation, they concluded that progressive shortening progressively leads to a greater reduction in supination and pronation due to radial bow and radio-ulnar gap [10], in our case 2 cm shortening was done. After radical debridement, the shortening of the bones help in achieving reduction without a need for extensive traction or soft tissue dissection and its complications. Although the forearm length is reduced there is no strain on the distal and proximal radioulnar joint, resulting in a favorable range of motion of the wrist and elbow.
Conclusion
For cases of infected gap non-union of both bones forearm, shortening and acute docking with plate osteosynthesis and bone grafting is an alternative, offering a recurrence-free outcome and favorable post-operative functional results.
Clinical Message.
Effective management of infected gap non-union in the radius and ulna involves thorough debridement with preservation of vascularity, followed by rigid fracture fixation and bone grafting. Concurrently, address infection with culture-specific antibiotics and monitor inflammatory markers for optimal outcomes.
Biography


Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Mills L, Tsang J, Hopper G, Keenan G, Simpson AH. The multifactorial aetiology of fracture nonunion and the importance of searching for latent infection. Bone Joint Res. 2016;5:512–9. doi: 10.1302/2046-3758.510.BJR-2016-0138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nicholson J, Makaram N, Simpson A, Keating J. Fracture nonunion in long bones:A literature review of risk factors and surgical management. Injury. 2021;52:S3–11. doi: 10.1016/j.injury.2020.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Ebied AM, Elseedy AI. Treatment of Infected Nonunion of Forearm Bones by Ring External Fixator. [[Last accessed on 5 Nov 2024]]. Available from: https://journals.lww.com/egoj/fulltext/2018/53040/treatment_of_infected_nonunion_of_forearm_bones_by.9.aspx .
- 4.Perna F, Pilla F, Nanni M, Berti L, Lullini G, Traina F, et al. Two-stage surgical treatment for septic non-union of the forearm. World J Orthop. 2017;8:471–7. doi: 10.5312/wjo.v8.i6.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dimartino S, Pavone V, Carnazza M, Cuffaro ER, Sergi F, Testa G. Forearm fracture nonunion with and without bone loss:An overview of adult and child populations. J Clin Med. 2022;11:4106. doi: 10.3390/jcm11144106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire:Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu T, Liu Z, Ling L, Zhang X. Infected forearm nonunion treated by bone transport after debridement. BMC Musculoskelet Disord. 2013;14:273. doi: 10.1186/1471-2474-14-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhar SA, Dar TA, Mir NA. Management of infected nonunion of the forearm by the masquelet technique. Strategies Trauma Limb Reconstr. 2019;14:1–5. doi: 10.5005/jp-journals-10080-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parihar M, Ahuja D. Infected nonunion of radius and ulna-strategy of approach. J Orthop Case Rep. 2012 Oct-Dec;2(4):26–31. [PMC free article] [PubMed] [Google Scholar]
- 10.Barinaga G, Rodriguez-Feo C, Rasmussen E, Telfer S, Iannuzzi N. The effect of forearm shortening on forearm range of motion. J Hand Surg. 2022;47:87–e1-7. doi: 10.1016/j.jhsa.2021.03.017. [DOI] [PubMed] [Google Scholar]


