Abstract
Background
There is currently no consensus on the surgical treatment of lumbar spondylolysis in young adults, and the nonunion rate remains relatively high even after surgery. Therefore, in this study, we proposed a modified intravertebral screw-rod fixation technique within a single vertebral segment and investigated the clinical efficacy of this modified fixation system combined with autologous cancellous bone grafting in the treatment of lumbar spondylolysis in young adults.
Methods
This study included 28 young adults with lumbar spondylolysis who were treated at our center between 2021 and 2023. All patients underwent modified intravertebral screw-rod fixation within a single vertebral segment combined with autologous cancellous bone grafting. We performed postoperative follow-ups regularly to assess the patient’s pain status using the visual analog scale (VAS), Oswestry Disability Index (ODI), and radiological findings.
Results
All 28 patients successfully underwent the surgery with an average operation time and blood loss volume of 96.01 ± 21.3 min and 186.78 ± 63.43 mL, respectively. Postoperatively, patients experienced significant symptom relief, with notable decreases in VAS scores and ODI indices at 1, 3, 6, and 12 months compared with preoperative conditions. These differences were statistically significant (P < 0.05). Radiological findings revealed a healing rate of 92.86% for the 56 fractured pars interarticularis among the 28 patients. No implant-related complications, such as fracture, loosening, or pseudarthrosis, were observed.
Conclusions
The modified intravertebral screw-rod fixation system within a single vertebral segment combined with autologous cancellous bone grafting is a safe and effective treatment for lumbar spondylolysis in young adults. It significantly improves pain and functional disability as it promotes bone healing.
Keywords: Lumbar spondylolysis, Young adults, Bone healing, Clinical outcome, Internal fixation
Background
Lumbar spondylolysis is a specific spinal disorder characterized by a defect in the bone between the pedicle and lamina of the lumbar vertebrae. This defect results in pedicle discontinuity, affecting the overall structure and function of the spine. Notably, epidemiological studies indicate that the incidence of lumbar spondylolysis in the general population ranges from 5 to 6% [1]. However, the incidence may rise to 20–50% among athletes, particularly those involved in repetitive spinal loading activities [2]. This condition primarily affects males and most commonly occurs in the L5 vertebra. Its pathogenesis includes congenital dysplasia of the pars interarticularis, weakness in the bony connection between the pedicle and lamina, long-term repetitive excessive flexion and rotational loading of the spine, such as in weightlifting and gymnastics [3], and acute or chronic spinal injuries. Furthermore, the clinical manifestations are lower back pain, limited lumbar mobility, and muscle spasms [4]. However, in some cases, spondylolysis compresses the neural roots, causing lower limb pain or sensory abnormalities. Currently, conservative treatment remains the mainstream approach for lumbar spondylolysis, including physiotherapy, pharmacological therapy (e.g., nonsteroidal anti-inflammatory drugs), and lumbar bracing. However, surgical intervention may be considered for patients who do not respond to conservative treatment or develop neurological symptoms. Various surgical techniques to help repair defects and facilitate bone healing are available for lumbar spondylolysis. These techniques include simple pars repair with bone grafting, Scott wiring, Buck screw fixation, pedicle screw fixation combined with hook-rod systems, interbody fusion, dynamic fixation combined with pars repair, single-lag screw fixation, and hook-pars screw fixation [5]. One of these surgical methods is chosen based on the patient’s specific circumstances, including age, type, and severity of spondylolysis, and the presence of spondylolisthesis or other complications. Notably, conservative treatment may be the first option for younger patients with unilateral spondylolysis. However, surgery is required if conservative treatment fails, with surgical repair considered early for adults and patients with bilateral spondylolysis. Currently, lumbar spondylolysis surgery is primarily classified into segmental and transsegmental fixation; however, both methods have certain drawbacks. Transsegmental fixation is complex, involves significant trauma, results in greater blood loss, and restricts the mobility of the involved vertebral segments, hence potentially accelerating the degeneration of adjacent vertebral joints [6]. In contrast, implant breakage or disengagement, inadequate fixation strength, and suboptimal bone fusion may complicate segmental fixation [7, 8]. Consensus on the surgical approach has not been reached, and postoperative residual low back pain and a considerable nonunion rate remain prominent clinical issues. Therefore, in this study, we proposed an innovative modified intravertebral screw-rod fixation system within a single vertebral segment combined with autologous cancellous bone grafting for the treatment of lumbar spondylolysis in young adults.
Methods
Patient selection and inclusion criteria
In this study, we aimed to provide an innovative modified intravertebral screw-rod fixation system within a single vertebral segment combined with autologous cancellous bone grafting for the treatment of lumbar spondylolysis in young adults. We enrolled 28 young patients with lumbar spondylolysis who underwent surgery using a modified single-vertebral segmental internal fixation system combined with autologous cancellous bone grafting at our center between 2021 and 2023. The diagnosis of lumbar spondylolysis in all patients was confirmed through anteroposterior, lateral, oblique, and dynamic lumbar radiography, along with lumbar computed tomography (CT) and magnetic resonance imaging (MRI). Patients were included if they were aged ≥ 18 years and had a confirmed diagnosis of unilateral or bilateral lumbar spondylolysis at a single segment and spondylolisthesis not exceeding grade I. All participants had failed to achieve satisfactory outcomes after at least 6 months of conservative treatment, with some exhibiting neurological symptoms. The exclusion criteria were the presence of other spinal diseases such as scoliosis or spondylolisthesis exceeding grade I, severe systemic diseases such as heart disease or diabetes that could potentially affect surgical outcomes, and patients who declined to participate in the study. This study was approved by the Biomedical Ethics Committee of the 900th Hospital of the Joint Logistics Support Force (Ethics Batch No. 2021-061), and all patients provided signed informed consent.
Technical key points
The modified intravertebral screw-rod fixation system is a minor optimization of the existing fixation techniques for lumbar spondylolysis. It involves placing a 3.5-mm pedicle screw within the pedicle on one side of the affected vertebra, followed by inserting another 3.5-mm pedicle screw along the direction of the lumbar isthmus on the same side of the lamina, with the isthmic screw spanning both ends of the fracture. The two screws were connected using a titanium rod to form a unilateral triangular stable fixation structure, as illustrated in Fig. 1. We simultaneously performed autologous cancellous bone grafting on the isthmic defect area to facilitate bone healing. A similar surgical procedure was performed on the contralateral side. However, reduction and repositioning of the vertebral body should be performed before inserting the bilateral isthmic screws for isthmus fixation in cases of concurrent vertebral spondylolisthesis.
Fig. 1.
Modified intravertebral screw-rod fixation system for a single vertebral segment. (A) Schematic diagram. (B, C) Model illustrations
Surgical procedure
Patients were positioned in the prone position under general anesthesia. A posterior midline incision (4–6 cm) was made to expose the affected vertebrae. Furthermore, the autologous iliac cancellous bone was harvested and grafted into the isthmic bone-grafting trough after grinding the sclerotic bone at the bilateral lumbar isthmic defects until the fresh bleeding bone surfaces were exposed. Subsequently, we used a modified single-vertebral segmental pedicle screw-rod fixation system to place and fix the screw. Additionally, fluoroscopic guidance using a C-arm machine was used to ensure stable fixation of the screw-rod system, with no nerve root compression observed. Subsequently, the incision was closed in layers. The intraoperative images of screw placement and incision are shown in Fig. 2.
Fig. 2.
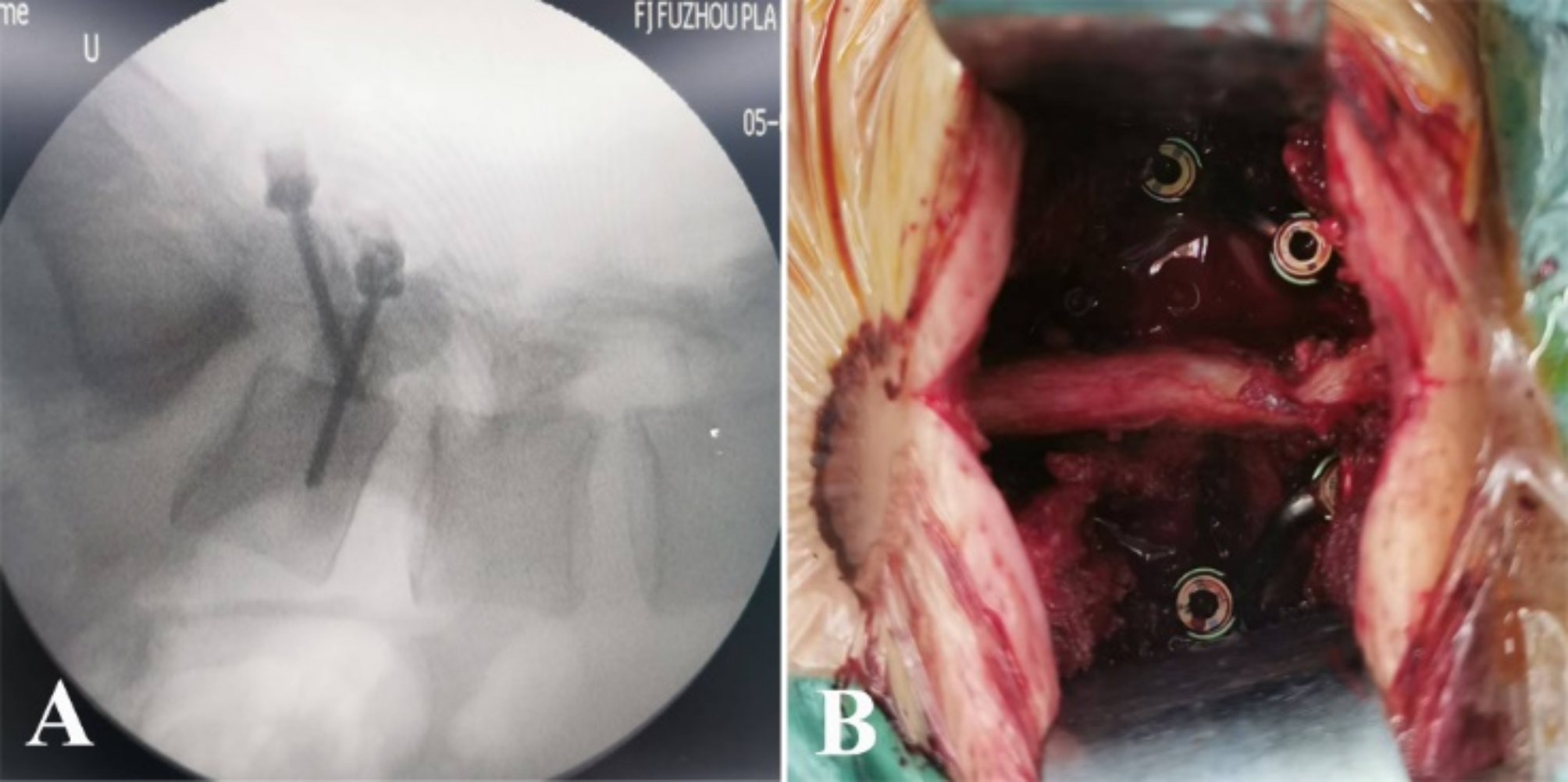
Peg placement. (A) Intraoperative peg placement. (B) Surgical incision view
Postoperative management
After surgery, the patients were required to wear a lumbar brace for 4–6 weeks to protect the surgical site and restrict excessive flexion and extension movements. We initiated physical therapy, including isometric contraction training of the lumbar muscles and progressive activities, within 1 week postoperatively. Gradual weight-bearing exercises and aerobic activities were introduced 3 months after surgery to enhance lumbar muscle strength and endurance.
Follow-up evaluation and statistical analysis
Patients underwent regular follow-up visits at 1, 3, and 6 months and 1 year postoperatively. The specific follow-up content included pain scores assessed using the Visual Analog Scale (VAS), Oswestry Disability Index (ODI) questionnaire, and radiological evaluations (radiography, CT, or MRI to assess isthmic healing). All data were statistically analyzed using SPSS 22.0 (IBM Corp., Armonk, NY, USA). Normally distributed and homogeneous variance measurement data were expressed as mean ± standard deviation (x ± s). Additionally, repeated measure analysis of variance was used to compare preoperative and postoperative data, with further pairwise comparisons conducted using Dunnett’s t-test. Statistical significance was set at P < 0.05.
Results
Basic patient information is presented in Table 1. We included 28 patients (27 males and 1 female) in this study. The mean age and body mass index were 24.41 ± 3.37 years and 23.13 ± 1.89 kg/m², respectively. Among these patients, 22 had bilateral isthmic defects at the L5 vertebra, whereas six had this defect at the L4 vertebra. Currently, the clinically used isthmic classifications are the Morita (based on radiography), Sairyo (based on CT), and Kaneko classifications. In this study, we used the Kaneko classification to categorize lumbar isthmic spondylolysis into type A (complete fracture), type B (incomplete fracture), and type C (pre-fracture with visible radiolucent defects in the isthmic cortical bone) [9, 10]. Of the 28 patients, 27 were diagnosed with type A lumbar isthmic spondylolysis, and 1 with type B. All 28 patients underwent successful surgery, with a mean operation duration and blood loss volume of 96.01 ± 21.3 min and 186.78 ± 63.43 mL, respectively. No complications occurred during surgery, and the patients recovered well postoperatively with no infections, nerve injuries, or other surgery-related complications.
Table 1.
Baseline characteristics of the included patients
| Number (n) | 28 |
|---|---|
| Gender (n) | |
| Male | 27 |
| Female | 1 |
| Number of Lumbar Isthmus Fractures (n) | 56 |
| Kaneko Classification (n) | |
| Type A | 27 |
| Type B | 1 |
| Location of Lumbar Isthmus Fracture | |
| L4 (bilateral) | 6 |
| L5 (bilateral) | 22 |
| Age (y) | 24.41 ± 3.37 |
| Body Mass Index (kg/m2) | 23.13 ± 1.89 |
| Operation Duration (min) | 96.01 ± 21.3 |
| Blood Loss Volume (mL) | 186.78 ± 63.43 |
| Number of Lumbar Isthmus Healing Cases (n) | 52 |
| Healing Rate of Lumbar Isthmus (%) | 92.86 |
Pain scores (VAS)
The mean preoperative VAS score was 6.77 ± 0.82, which decreased to 3.23 ± 0.59 1 month postoperatively, further decreasing to 2.15 ± 0.54 3 months postoperatively and to 1.46 ± 0.51 and 1.23 ± 0.43 at 6 months and 1 year postoperatively, respectively. Notably, compared with the preoperative scores, the VAS scores at 1, 3, and 6 months and 1 year postoperatively were significantly reduced, and these changes were statistically significant (P < 0.05).
ODI
The mean preoperative ODI was 19.92% ± 2.64%, decreased to 10.15% ± 2.26% 1 month postoperatively, also decreased to 7.85% ± 1.54% 3 months postoperatively, and further decreased to 4.39% ± 0.85% and 3.08% ± 0.74% at 6 months and 1 year postoperatively, respectively, indicating a significant reduction in functional impairment in daily life. The detailed statistical analyses are presented in Table 2.
Table 2.
Comparison of clinical outcomes pre- and postoperatively
| VSA Score | ODI (%) | |
|---|---|---|
| Preoperative | 6.77 ± 0.82 | 19.92 ± 2.64 |
| 1-month Postoperative | 3.23 ± 0.59* | 10.15 ± 2.26* |
| 3-month Postoperative | 2.15 ± 0.54* | 7.85 ± 1.54* |
| 6-month Postoperative | 1.46 ± 0.51* | 4.39 ± 0.85* |
| 1-year Postoperative | 1.23 + 0.43* | 3.08 ± 0.74* |
| F-value | 380.63 | 369.05 |
| P-value | < 0.05 | < 0.05 |
* Statistically significant difference compared with preoperative values (P < 0.05). VAS, Visual Analog Scale; ODI, Oswestry Disability Index
Radiological assessment
One patient did not experience healing in the bone of both isthmic defects after more than 2 years of follow-up. Additionally, two patients still had unilateral isthmic nonunion after more than 2 years of follow-up. The remaining patients had bone healing in the isthmic defect area on radiography, CT, or MRIs at 6 months or 1 year postoperatively. Notably, the healing rate of 56 isthmic defects in 28 patients was 92.86%.
Complications
During the follow-up period, no patient experienced complications, such as implant fracture, loosening, or pseudarthrosis.
Statistical analysis
The results of the analysis showed that there were significant differences in VAS scores and ODI at various postoperative time points compared with preoperative values (P < 0.05), indicating that surgery had a significant effect on improving pain, lumbar mobility, and functional impairment.
Illustrative case
A 21-year-old male patient presented with a history of recurrent lower back pain lasting more than 1 year. Radiographic and CT examinations revealed bilateral isthmic defects of the L5 vertebra with grade I spondylolisthesis (Fig. 3). The patient’s symptoms gradually worsened despite more than 1 year of conservative treatment at a rehabilitation center, which prompted his visit to our hospital. At presentation, his VAS score was 6, and his ODI was 19%.
Fig. 3.
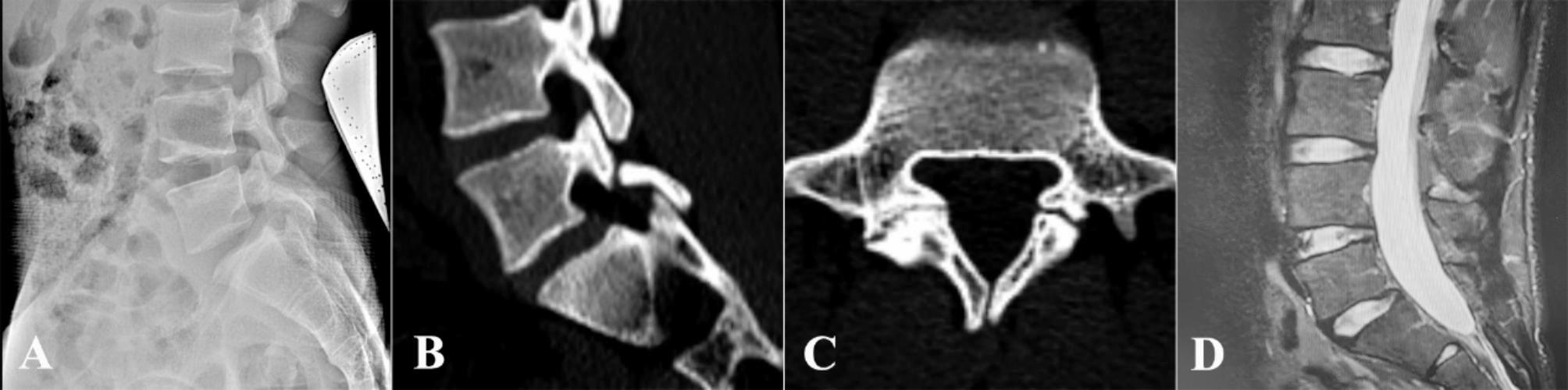
Preoperative radiographic and imaging studies of a case with lumbar spondylolysis at L5. (A) Preoperative radiographic lateral view. (B) Preoperative computed tomography (CT) sagittal view. (C) Preoperative CT coronal view. (D) Preoperative lumbar magnetic resonance imaging
Furthermore, on January 6, 2022, the patient underwent surgery under general anesthesia to “treat the bilateral isthmic defects of the L5 vertebra with a modified single-segment pedicle screw and rod fixation system combined with autologous cancellous bone grafting.” Postoperatively, the patient experienced relief from lower back pain compared to preoperative levels. At 1, 3, and 9 months postoperatively, the VAS scores were 4, 2, and 1, respectively, and the ODI scores were 11%, 7%, and 3%, respectively. Nine months post-surgery, the patient reported no significant discomfort in the lower back. Follow-up lumbar X-ray radiography and CT scans demonstrated bone fusion at the defect site of the pars interarticularis of the L5 vertebra. MRI indicated no notable degeneration of the intervertebral disc compared to pre-operative findings (Fig. 4).
Fig. 4.

Nine-month postoperative radiological follow-up, showing bony fusion at both isthmic defects of L5. (A) Postoperative radiographic lateral view. (B) Postoperative computed tomography (CT) sagittal view. (C) Postoperative CT coronal view. (D) Postoperative lumbar magnetic resonance imaging
Discussion
Currently, there is no consensus regarding the management of young adults with isolated bilateral lumbar isthmic spondylolysis [9]. Surgical intervention is considered for patients whose symptoms persist after rigorous conservative treatment for more than 6 months [10]. Reconstructing the isthmic structure, maintaining spinal stability, alleviating symptoms, and restoring motor function are the primary goals of current surgical interventions [11]. Additionally, surgical options for isolated isthmic spondylolysis primarily include trans-segmental fixation and intrasegmental isthmic repair with internal fixation [12, 13]. Notably, transsegmental fixation is the most widely used and classic surgical approach in spinal surgery, particularly in patients with isthmic spondylolysis accompanied by spondylolisthesis, spinal stenosis, or radicular symptoms. This approach promotes isthmic healing by reconstructing a stable spinal environment [13]. However, the mobility of the corresponding vertebrae is sacrificed using this method, potentially reducing the quality of life and athletic performance of young adults [14]. In addition, it accelerates the degeneration of adjacent vertebrae and intervertebral discs. Notably, transsegmental fixation is a complex procedure with significant tissue damage and blood loss and multiple postoperative complications [6]. Intra-segmental isthmic repair achieves bony healing through internal fixation combined with bone grafting of the isthmic fissure. It is now widely used in clinical practice [15].
There are various surgical approaches for the internal fixation of lumbar spondylolysis segments, each with its own advantages. However, there is controversy regarding which procedure is more suitable for isolated lumbar spondylolysis. Buck screw fixation was proposed based on isolated pars interarticularis surgery, utilizing lag screws for uniaxial fixation of the bone at both ends of the pars to ensure the continuity and stability of its structure [16]. However, when effective connection between the two screws is lacking, it reduces the restriction of the axial rotation and lateral bending relative motion between the vertebral bodies [17], preserving a certain degree of mobility. Currently, minimally invasive modified Buck techniques combined with computer navigation are used to treat spondylolysis [18]. These methods result in shorter operation times, more precise surgery, and reduced blood loss. However, Li et al. observed 16 patients who underwent pedicle screw fixation and found complete bony fusion in the pars of all these patients, whereas among 15 patients who underwent the Buck procedure, four had no bony fusion [7]. The stability achieved with the Buck method is relatively low when compared with pedicle screws, which may be detrimental to bony fusion between the fractured ends of the pars. Additionally, a single screw has weak torsional resistance and may even become internally loose because of the movement. The screw itself also occupies the fracture healing area, which can lead to healing difficulties and, ultimately, internal fixation failure [19]. Currently, the clinical use of intrasegmental “V”-shaped and “U”-shaped rod internal fixation techniques has achieved satisfactory therapeutic effects [20, 21]. However, conditions such as lamina and spinous process hypoplasia significantly reduce the effectiveness of compression fixation, thereby affecting the healing of the pars.
Therefore, we propose an improved single-vertebral pedicle screw-rod fixation system based on the Buck and screw-hook fixation techniques. Using the Buck method, a 3.5-mm pedicle screw was inserted along the direction of the lumbar isthmus through the lamina, directly fixing the isthmic fracture segments. Another screw was simultaneously placed in the ipsilateral pedicle and connected via a titanium rod to form a stable triangle that indirectly compressed the bone surface of the isthmic fracture segment. Furthermore, this dual approach, both direct and indirect, ensures the stability of the lumbar isthmus, providing greater stability than the unilateral Buck method and facilitating later bone healing. Findings from our research show that patients with isthmic spondylolysis treated with this improved surgical method achieved a bone healing rate of 92.86%, which indirectly reflects the structural stability of this surgical approach and its high bone fusion rate. The postoperative VAS and ODI scores of patients in this study significantly decreased, indicating notable relief from symptoms such as low back pain and a substantial improvement in quality of life. This method preserves spinal mobility, reduces the incidence of adjacent vertebral pathologies, and mitigates adjacent disc degeneration because it involves segmental internal fixation. Additionally, the surgical technique is relatively simple, with low intraoperative blood loss. Furthermore, pedicle screw technology is well-established for spinal applications and provides robust fixation. It exhibits a lower probability of implant loosening or fracture and fewer complications compared with the Scott method and screw-hook fixation, hence facilitating postoperative recovery.
However, this study had certain limitations. First, the number of cases was relatively small, leading to potential data bias. Therefore, future research should increase the sample size to enhance data accuracy. Meanwhile, as a single-center study, the improved single-vertebral segmental pedicle screw-rod fixation system, which is a segmental internal fixation method, included a limited number of cases and excluded patients with vertebral slips greater than grade I. Hence, the effectiveness of this approach in severe isthmic spondylolysis requires further evaluation. Moreover, whether this fixation method contributes to the degeneration of facet joints and intervertebral discs remains unknown and warrants further follow-up. Future studies should conduct finite element analysis or biomechanical experiments to verify the mechanical stability of this fixation method.
Conclusions
In summary, an improved single-vertebral segmental pedicle screw-rod fixation system combined with autologous cancellous bone grafting has emerged as a novel and effective surgical approach for the treatment of isthmic spondylolysis in young adults. It effectively increases the bone healing rate of isthmic spondylolysis and offers patients a better prognosis for recovery while ensuring segmental lumbar mobility, alleviating pain symptoms, maintaining spinal stability, reducing complications, and accelerating postoperative recovery.
Acknowledgements
Not applicable.
Abbreviations
- CT
Computed tomography
- MRI
Magnetic resonance imaging
- ODI
Oswestry Disability Index
- VAS
Visual analog scale
Author contributions
Conceptualization, Xiu Yang; Funding acquisition, Xiu Yang; Supervision, Shun-Lin; Visualization, Jie Liang; Writing – original draft, Xiu Yang, Shun-Lin, Han-Lin Chen; Writing – review and editing, Jie Xiao and Jin-Shui Chen. All the authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the hospital-level project of the 900th Hospital of the Joint Logistics Support Force of PLA (2021JQ06); the Startup Fund for Scientific Research, Fujian Medical University (Grant number: 2023QH1355); and the Natural Science Foundation of Fujian Province (Grant number: 2024J011149 and 2024J011158). The sponsors played no role in the design, execution, interpretation, or writing of the study.
Data availability
The datasets used and analyses relevant to this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Biomedical Ethics Committee of the 900th Hospital of the Joint Logistics Support Force (Ethics Batch No. 2021-061). Informed consent was obtained from all the participants (or their guardians) included in the study.
Consent for publication
The patient described in the “Illustrative case” provided informed consent for the publication of the report and accompanying images.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiu Yang, Shun Lin and Han-Lin Chen contributed equally to this work.
Contributor Information
Jie Xiao, Email: 395994607@qq.com.
Jin-Shui Chen, Email: cjswater1@163.com.
References
- 1.Aoki Y, Takahashi H, Nakajima A, Kubota G, Watanabe A, Nakajima T, et al. Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep. 2020;10:6739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pan JH, Chen CS, Liu CL, Chou PH. Biomechanical effects of a novel pedicle screw W-type rod fixation for lumbar spondylolysis: a finite element analysis. Bioeng (Basel). 2023;10:451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang JP, Zhong ZC, Cheng CK, Chen CS, Yu CH, Chang TK, et al. Finite element analysis of the spondylolysis in lumbar spine. Biomed Mater Eng. 2006;16:301–8. [PubMed] [Google Scholar]
- 4.Minor A, Klein BR, Sowah MN, Etienne K, Levi AD. Pars interarticularis fractures treated with minimally invasive surgery: a literature review. J Clin Med. 2024;13:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ye Y, Jin S, Zou Y, Fang Y, Xu P, Zhang Z, et al. Biomechanical evaluation of lumbar spondylolysis repair with various fixation options: a finite element analysis. Front Bioeng Biotechnol. 2022;10:1024159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung CC, Shimer AL. Lumbosacral spondylolysis and spondylolisthesis. Clin Sports Med. 2021;40:471–90. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Li H, Chang X, Hu Z, Mu X, Liu C, et al. Retrospective comparative study of pedicle screw fixation via quadrant retractor and Buck’s technique in the treatment of adolescent spondylolysis. Orthop Surg. 2022;14:111–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicol RO, Scott JH. Lytic spondylolysis. Repair by wiring. Spine. 1986;11:1027–30. [DOI] [PubMed] [Google Scholar]
- 9.Schlenzka D, Seitsalo S, Poussa M, Osterman K. Operative treatment of symptomatic lumbar spondylolysis and mild isthmic spondylolisthesis in young patients: direct repair of the defect or segmental spinal fusion? Eur Spine J. 1993;2:104–12. [DOI] [PubMed] [Google Scholar]
- 10.Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: I. diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006;14:417–24. [DOI] [PubMed] [Google Scholar]
- 11.Li Q, Hu B, Zhang Z, et al. Clinical outcomes of Isobar TTL System with Isthmic Bone Grafting and Pedicle Screw-Vertebral plate hook with direct repair of defect for lumbar spondylolysis: a matched-pair Case Control Study. Orthop Surg. 2023;15:2582–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammed N, Patra DP, Narayan V, Savardekar AR, Dossani RH, Bollam P, et al. A comparison of the techniques of direct pars interarticularis repairs for spondylolysis and low-grade spondylolisthesis: a meta-analysis. Neurosurg Focus. 2018;44:E10. [DOI] [PubMed] [Google Scholar]
- 13.Verma R, Virk S, Qureshi S. Interbody fusions in the lumbar spine: a review. HSS J. 2020;16:162–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Said E, Abdel-Wanis ME, Ameen M, Sayed AA, Mosallam KH, Ahmed AM, et al. Posterolateral fusion versus posterior lumbar interbody fusion: a systematic review and meta-analysis of randomized controlled trials. Global Spine J. 2022;12:990–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mohile NV, Kuczmarski AS, Lee D, Warburton C, Rakoczy K, Butler AJ. Spondylolysis and isthmic spondylolisthesis: a guide to diagnosis and management. J Am Board Fam Med. 2022;35:1204–16. [DOI] [PubMed] [Google Scholar]
- 16.Bonnici AV, Koka SR, Richards DJ. Results of Buck screw fusion in grade I spondylolisthesis. J R Soc Med. 1991;84:270–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai SHL, Chang CW, Chen WC, et al. Does Direct Surgical Repair Benefit pars Interarticularis fracture? A systematic review and Meta-analysis. Pain Physician. 2022;25:265–82. [PubMed] [Google Scholar]
- 18.Yurac R, Bravo JT, Silva Á, Marré B. Spondylolysis repair using a minimally invasive modified Buck technique with neuronavigation and neuromonitoring in high school and professional athletes: technical notes, case series, and literature review. World Neurosurg. 2021;155:54–63. [DOI] [PubMed] [Google Scholar]
- 19.Ye Y, Yang H, Ma T, Zhu K, Xu G, Han Z, et al. Buck technique supplemented by temporary intersegmental pedicle screw fixation to repair lumbar spondylolysis in youth. J Orthop Surg Res. 2024;19:340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tatsumura M, Okuwaki S, Gamada H, Asai R, Eto F, Nagashima K, et al. A novel technique for pars defect direct repair with a modified Smiley face rod for spondylolysis and isthmic spondylolisthesis. Spine Surg Relat Res. 2023;7:396–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koptan WMT, ElMiligui YH, ElSharkawi MM. Direct repair of spondylolysis presenting after correction of adolescent idiopathic scoliosis. Spine J. 2011;11:133–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyses relevant to this study are available from the corresponding author upon reasonable request.



