Abstract
Objectives
The aim of this study was to describe the safety and effectiveness of thoracic or lumbar partial lateral corpectomy (PLC) in cats with spinal cord compression due to intervertebral disc herniation (IVH).
Methods
A retrospective study was conducted of 12 client-owned cats from two academic and one private referral veterinary centres. Cross-sectional imaging was available in 12 cats for evaluation of disc herniation. Nine cats had postoperative imaging for evaluation of slot creation and decompression. Neurological examination was performed for assessment of pre- and postoperative status. Complications were evaluated.
Results
Seven cats had severe (>50%), four moderate (>20 to <50%) and one mild (<20%) spinal cord compression on cross-sectional imaging. IVH occurred at Th12–13 in five cases, at L1–2 in two cases and at Th3–4, Th13–L1, L4–5 and L5–6 in one case each. After PLC, two cats had insufficient decompression (>20% remaining spinal cord compression), five had good decompression (<20% remaining spinal cord compression) and complete decompression (normal shape of the spinal cord) was achieved in two cats. Outcomes included five cats with an excellent result, three with significant improvement, one with mild improvement and three cats that died intra- or postoperatively due to extensive intraoperative bleeding. One cat was euthanased as a result of neurological deterioration 5 months postoperatively. The median follow-up period was 13.2 months (range 0 days to 84 months).
Conclusions and relevance
PLC in cats offers a potential treatment option for IVH to decompress the spinal cord. Fatal haemorrhage associated with this surgery is a significant risk, as occurred in 25% of the cats in this study. Surgeons should especially be aware of the potential for intraoperative haemorrhage and the need for sufficient slot creation to achieve sufficient spinal cord decompression and avoid complications.
Keywords: Neurosurgery, disc disease, partial lateral corpectomy, complications
Introduction
Intervertebral disc disease (IVDD) is uncommon in cats, with a reported general prevalence in the range of 0.12–0.26% upon admission to veterinary hospitals.1–5 Although it is well known that intervertebral disk degeneration is a common finding in post-mortem examinations in cats, with an increasing incidence in older cats, associated clinical signs are rare.6–10 In cases of chronic disc disease where protruded material is firmly attached to the remaining annulus fibrosus, which is secured to the dorsal and ventral longitudinal ligaments, the vertebral body and its cartilaginous end plate through Sharpey’s fibres, the removal of herniated material becomes a challenging task. This process may pose a risk of iatrogenic spinal cord trauma and incomplete removal of extruded or protruded disc material. In 2004, Moissonnier et al 11 initially introduced and described the thoracolumbar lateral corpectomy (TLLC) as an innovative technique in dogs to remove disc material ventral to the spinal cord while minimising or avoiding spinal cord trauma by creation of a lateral slot through the vertebral epiphyses of two adjacent vertebral bodies and the intervertebral disc. This approach has become a surgical option in dogs for treating chronic protrusive and extrusive thoracolumbar IVDD, with the primary complication being haemorrhage from the venous vertebral sinus(es).12,13 In contrast, only three case reports of partial lateral corpectomies (PLCs) in cats have been published.14–16 The first PLC for a ventral extradural thoracic spinal cord compression at Th3–4 in a cat was reported in 2008. 14 Two more recent case reports describe a combination of hemilaminectomy and partial corpectomy for resection of a vertebral vascular hamartoma at Th13 and a lateral corpectomy combined with a foraminotomy at L1–2 because of chronic intervertebral disc herniation (IVH) associated with fused vertebrae.15,16
The aims of this retrospective study were to assess preoperative neurological presentation, characterise disc cross-sectional imaging features, analyse slot morphometry as thoroughly as possible, evaluate the outcomes of PLC in cats and to report complications. We hypothesised that PLC in cats would be a safe and an effective treatment option for IVDD, similar to dogs.
Materials and methods
Between 2005 and 2023, 12 client-owned cats with IVH underwent thoracolumbar PLC (TLPLC) in two teaching veterinary hospitals and one private referral hospital. The inclusion criteria comprised a complete medical evaluation, including physical and neurological examinations at presentation, spinal cord imaging, PLC as treatment, assessment of intra- and postoperative complications, and postoperative outcome. Recorded information for each cat included breed, age, weight and sex, clinical course before presentation, neurological evaluation before surgery, diagnostic imaging findings before and after surgery if available, surgery performed, intra- and postoperative complications, postoperative care, postoperative neurological status, outcome and follow-up period. The clinical course before presentation was categorised as acute if neurological signs developed within 1 week, and progressive if clinical signs developed over more than 1 week. Retrospective assessment of medical treatment or physical therapy before surgery was not possible owing to limited available data. The neurological status of each cat was classified using a Modified Frankel Score (MFS) before and after surgery: 5 = pain, without neurological deficits; 4 = proprioceptive deficits only; 3 = ataxia or ambulatory paraparesis; 2 = non-ambulatory paraparesis; 1 = paraplegia and intact nociception; and 0 = paraplegia without intact nociception. Spinal imaging techniques (Figure 1) included three different MRI systems (Vantage Elan 1.5 Tesla, Toshiba Corporation; Ingenia 3.0 Tesla, Philips Healthcare; Magnetom vida 3.0 Tesla, Siemens Healthcare). Contrast agents were used for every MRI study (gadoteric acid, Dota Mr 0.5 mmol/ml, Consentis Diagnostics; gadoteric acid, Clariscan 0.5 mmol/ml, GE Healthcare, Buchler). Two different CT systems were used for CT and myelo-CT, respectively (IQon Spectral CT, Koninklijke Philips; Aquilion RXL, Toshiba). Contrast agents were used for every CT and myelo-CT (Iobitridol, Xenetix 350 mg/ml, Guerbet; Iopamidol, Solutrast 200M, Bracco Imaging Germany). The IVH site was recorded and PLC was performed, as described by Moissonnier et al, 11 based on the diagnostic imaging results. All cats were examined, and surgery was performed by specialist surgeons (DECVS and one non-diplomate surgeon who is highly experienced in neurosurgery). The degree of compression of the spinal cord before and after surgery was measured, lateralisation and mineralisation of the herniated disc material were evaluated, and slot morphometry was calculated if imaging data were available (Figures 2 and 3). Compression of the spinal cord was classified as mild compression (<20%), moderate compression (>20 to <50%) or severe compression (>50%). Lateralisation was recorded as central if there was no obvious lateralisation of the herniated disc material, slightly lateralised if most compression was ventral and a minor lateral component was visible, and obvious lateralisation if most compression was ventral but a marked or obvious lateral component was visible. The mineralisation of the herniated disc material was categorised as follows: no mineralisation if the disc material had the same signal intensity as the spinal cord on imaging; moderate mineralisation if the disc material was visibly mineralised but did not have the same signal intensity as vertebral cortical bone; and pronounced mineralisation if the disc material matched the same signal intensity as the vertebral cortical bone on imaging (Figure 3). Postoperative spinal cord compression was assessed using CT or MRI and categorised as complete decompression if the spinal cord shape was normal, good decompression if the remaining compression was below 20% and insufficient decompression if compression exceeded 20%. Slot morphometry was calculated in three ways, using CT or MRI images (Figure 2). The depth of the slot was measured based on the laterolateral extension of the vertebral body measured at the level of the cranial endplate of the caudal vertebra adjacent to affected disc space on transverse preoperative images. The remaining bone was measured at the same location on the postoperative images and the difference was expressed as percentage of the preoperative value. The height of the slot was calculated based on the dorsoventral extension of the vertebral body measured on transverse preoperative images at the level of the cranial endplate of the caudal vertebra adjacent to the affected disc space. The remaining bone was again measured at the same location on postoperative images and the difference expressed as percentage of the preoperative value. The length of the slot was calculated based on the craniocaudal extension of the two vertebral bodies adjacent to the affected disc and the intervertebral disc measured on sagittal preoperative images. The remaining bone was measured at the same location on postoperative images and the difference was again expressed as a percentage of the preoperative value. The recorded outcomes were correlated with the preoperative status and categorised using a grading scheme (0 = excellent, no neurological abnormalities; 1 = good, significant improvement; 2 = satisfactory, mild improvement; 3 = unsatisfactory, no improvement; 4 = worse, neurological deterioration; 5 = death). Intra- and postoperative complications were evaluated and the follow-up period was defined as the time from surgery until the last presentation or owner communication. In addition, cases were examined to determine any correlation between the MFS at presentation, the location of affected intervertebral disc space, preoperative spinal cord compression, mineralisation and lateralisation of the herniated disc material, postoperative spinal cord decompression, slot morphometry and the outcome.
Figure 1.
Different imaging modalities of disc protrusion: (a) transverse CT image (soft tissue window); (b) horizontal myelo-CT image (soft tissue window); and (c) MRI T2-weighted image; respective disc protrusion marked with arrows
Figure 2.

(a) Transverse CT image of a slightly lateralised severe compressive disc protrusion (arrow); (b) sagittal CT image of the same disc protrusion (arrow) with cranial extension; (c) transverse CT image after partial lateral corpectomy (PLC); and (d) sagittal CT image after PLC. x = laterolateral slot extension; y = dorsoventral slot extension; z = craniocaudal slot extension
Figure 3.
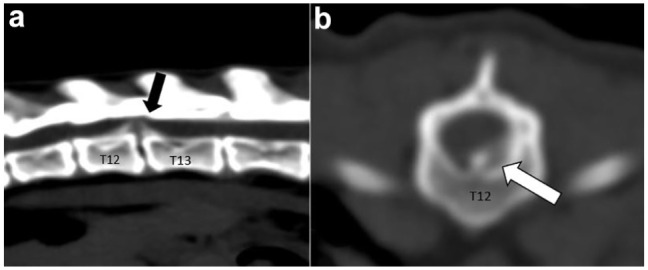
(a) Sagittal and (b) horizontal CT imaging of a pronounced mineralised disc herniation at T12–13 (arrows), classified as obvious lateralised and severe compressive
Results
A total of 12 client-owned cats underwent PLC at two teaching veterinary hospitals and one private referral clinic. This group included nine purebred cats (five Persian, two Birman, one Exotic Shorthair, one British Shorthair) and three domestic shorthair cats. Among them, seven cats were spayed females, three were castrated males, one was male entire and one was female entire. The mean age of the cats was 7.8 years (range 5–12) and the mean body weight was 4.3 kg (range 2.9–9). Preoperative neurologic assessment and imaging results are listed in Table 1. Postoperative imaging data sets were available for nine cases (Table 2). The mean depth of the created slots was 46.1% (range 26–63) and the mean height of the slot was 52.4% (range 37–66). The mean length of the slot was 28.8% (range 17–56). Final postoperative outcomes were available for 12 cats. Postoperative imaging data sets were available for nine cats and are listed in Table 2. Complete decompression was achieved in two cats, good decompression in five cats and insufficient decompression in two cats. Four cats had an excellent outcome, three cats showed significant improvement and one cat had mild improvement in neurological signs. Two cats (cats 4 and 12) died during surgery, and one cat (cat 10) died during the postoperative period due to excessive haemorrhage from the vertebral sinus intraoperatively. One cat (cat 5), initially showing improvement, deteriorated 5 months postoperatively and was euthanased at the owner’s request. The follow-up period for all patients was in the range of 0 days to 7 years (mean 13.2 months). Owing to the limited number of cases, no statistical analyses were performed.
Table 1.
Preoperative neurological assessment and imaging results
| Case number | Age (years) | Clinical course* | MFS | Imaging technique | Localisation | Compression † | Lateralisation | Mineralisation ‡ |
|---|---|---|---|---|---|---|---|---|
| 1 | 7 | Progressive (>1 week) | 3 | MRI § | Th12–13 | 3 | Slightly lateralised | 2 |
| 2 | 12 | Progressive (12 days) | 3 | Myelo-CT** | Th3–4 | 2 | Obvious lateralised | 1 |
| 3 | 11 | Progressive (7 days) | 3 | Myelo-CT** | L5–6 | 1 | Slightly lateralised | 2 |
| 4 | 12 | Acute (1 day) | 2 | Myelo-CT** | L4–5 | 2 | Slightly lateralised | 2 |
| 5 | 6 | Progressive (9 days) | 3 | Myelo-CT** | Th12–13 | 2 | Slightly lateralised | 2 |
| 6 | 6 | Acute (1 day) | 3 | Myelo-CT** | Th12–13 | 3 | Obvious lateralised | 3 |
| 7 | 5 | Progressive (3 weeks) | 3 | MRI †† | Th12–13 | 2 | Slightly lateralised | 2 |
| 8 | 8 | Progressive (12 days) | 3 | MRI ‡‡ | L6–7 | 3 | Slightly lateralised | 3 |
| 9 | 5 | Progressive (2 months) | 4 | MRI ‡‡ and CT §§ | Th12–13 | 3 | Central | 2 |
| 10 | 6 | Progressive (3 weeks) | 3 | MRI ‡‡ and CT §§ | L1–2 | 3 | Slightly lateralised | 2 |
| 11 | 6 | Acute (1 day) | 0–1 | MRI ‡‡ and CT §§ | Th13–L1 | 3 | Slightly lateralised | 1 |
| 12 | 9 | Acute (1 day) | 3 | CT § | L1–2 | 3 | Slightly lateralised | 3 |
The value in parentheses is the time between onset of clinical signs and surgery
1 = mild compression (<20%), 2 = moderate compression (>20 to <50%), 3 = severe compression (>50%)
1 = no mineralisation, 2 = moderate mineralisation, 3 = pronounced mineralisation
Magnetom vida 3.0 Tesla, Siemens Healthcare
IQon Spectral CT, Koninklijke Philips
Ingenia 3.0 Tesla, Philipps Healthcare
Vantage Elan, 1.5 Tesla, Toshiba
Aquilion RXL, Toshiba
MFS = Modified Frankel Score
Table 2.
Postoperative imaging data sets and outcome
| Case number | Imaging technique | Slot morphometry* (%) | Remaining bone † (%) | Decompression ‡ | Outcome § | Follow-up |
|---|---|---|---|---|---|---|
| 1 | Not performed | – | – | – | 0 | 3 months |
| 2 | CT | 63, 56, 56 | 37, 44, 44 | 2 | 0 | 12 months |
| 3 | CT | 32, 53, 21 | 68, 47, 79 | 2 | 0 | 6 months |
| 4 | Not performed | – | – | – | 5 | not available |
| 5 | Myelo-CT | 63, 37, 21 | 37, 63, 79 | 1 | 5 | 5 months |
| 6 | Not performed | – | – | – | 2 | 6 weeks (1.4 months) |
| 7 | MRI | 60, 39, 36 | 40, 61, 64 | 1 | 0 | 3 weeks (0.7 months) |
| 8 | CT | 49, 65, 33 | 51, 35, 67 | 3 | 1 | 7 years (84 months) |
| 9 | CT | 48, 66, 20 | 52, 34, 80 | 2 | 1 | 3 years (36 months) |
| 10 | CT | 26, 53, 17 | 74, 47, 83 | 3 | 5 | not available |
| 11 | CT | 38, 56, 19 | 62, 44, 81 | 2 | 1 | 10 months |
| 12 | CT | 36, 47, 36 | 64, 53, 64 | 2 | 5 | not available |
Laterolateral, dorsoventral and craniocaudal dimensions
Laterolateral, dorsoventral and craniocaudal dimensions
1 = complete decompression, 2 = good decompression, 3 = insufficient decompression
0 = excellent, no neurological abnormalities; 1 = good, significant improvement; 2 = satisfactory, mild improvement; 3 = unsatisfactory, no improvement; 4 = worse, neurological deterioration; 5 = bad, death
Discussion
The study hypothesis that PLC is a safe and effective treatment option for IVDH in cats was only partially supported by our data.
In our study, 25% of the cats (cats 4, 10 and 12) treated with PLC did not survive surgery or the perioperative period, and one cat (cat 5) deteriorated 5 months later. To the authors’ knowledge, no fatal outcomes due to intraoperative haemorrhage in decompressive thoracolumbar spinal surgery in cats and dogs have been reported previously. Haemorrhage is a well-known complication of TLPLC in dogs in addition to spinal nerve injury, wound infection, incomplete spinal cord decompression, postoperative instability and pneumothorax in the thoracic region.11,13,17 Intraoperative blood loss during spinal surgeries is often due to disruption of the internal vertebral venous plexus, leading to significant haemorrhage.18,19 In two studies on TLPLC in dogs, haemorrhage due to vertebral sinus injury occurred in 24.3% and 25% of cases, respectively, without any fatal outcome. To minimise the risk in dogs, haemorrhage can be prevented by stopping the drilling once the dorsal longitudinal ligament is reached.12,13 Blood loss must be taken into account in cats, given their lower body weight and the physiological characteristic of having proportionately less blood volume relative to their body size. 20 In this study, three cats (cats 4, 10 and 12) had intra- or postoperative cardiac arrest, likely due to an underestimation of the degree of intraoperative haemorrhage. Cautious slot drilling, particularly in the dorsal area, and avoiding disruption of the dorsal longitudinal ligament seem to be essential in preventing haemorrhage. In addition, close monitoring of blood loss during the procedure is crucial. The immediate availability of blood products for transfusion in cases of major haemorrhage could mitigate this critical complication and ensure the procedure’s success by allowing for adequate slot creation.
Given the high mortality rate associated with this surgery, other treatment options should be considered. A recent study by Amey et al 5 showed no significant difference in outcomes between surgical and conservative/medical treatment of thoracolumbar and lumbosacral IVDH in cats, regardless of IVDH type. This should be taken into account when making treatment recommendations in the management of IVDH in cats especially when neurological abnormalities are mild. There were no data provided for the cats included in this study as to whether any medical treatment had been undertaken before the recommendation for surgical treatment.
Regarding the effectiveness of this surgical procedure, in our study, thoracolumbar PLC improved neurological status in all cats that survived surgery and the perioperative period. Decompression of the spinal cord was achieved after PLC in nine cases and was complete or regarded as good in seven cats. In two cats (cats 8 and 10), decompression was assessed as insufficient. Of these two cats, one (cat 8) showed postoperative improvement, while the other cat (cat 10) died in the postoperative period. In cat 10, the created slot was smaller in all three dimensions as intraoperative hypotension due to bleeding resulted in the premature termination of surgery. For the other cat with insufficient decompression, slot morphometry revealed a shorter craniocaudal extension than that recommended by Moissonnier. 17 Consequently, it appears that sufficient slot creation in all three directions is necessary to achieve adequate decompression. Moissonnier’s recommended slot dimension for dogs range from a quarter of the caudal vertebral body length for the caudal margin, a quarter of the cranial vertebral body length for the cranial margin, half to two-thirds of the vertebral body width for the depth margin and half the vertebral body height for the ventral margin. 11 Comparing these recommendations with our results, only the mean dorsoventral dimension of the slot was large enough; however, the mean depth and craniocaudal distension of the slot were shorter. The creation of smaller slots in cats, with a mean weight of 4.3 kg in our cohort, may be attributed to their small size and little experience of PLC in this species. Furthermore, the length:width:height ratio of the feline vertebra differs from that of dogs, which likely influences both the creation and dimension of the slot required for adequate decompression. Currently, there are no studies investigating the slot dimension necessary for sufficient spinal cord decompression or possible instability after TLPLC in feline vertebrae, making it challenging to compare the recommended slot dimensions for PLC in dogs with those investigated in our study. Böttcher et al 14 assumed that there is no need to modify the surgical technique for cats, as their anatomical structures are quite similar to those of dogs. Considering the small size of the vertebral bodies in cats, creating a higher slot is recommended to ensure safe access and sufficient visibility. 14 In this study, the small sample size, along with varying or missing postoperative imaging studies, limited the evaluation of slot dimension and the effectiveness of spinal cord decompression. Nevertheless, the recommended slot dimensions appear to be adequate references for achieving effective spinal cord decompression based on the current data.
In general, middle-aged and purebred cats comprised the majority of cases of this survey. This finding is consistent with those in previous studies, which also reported a higher prevalence of IVDH in purebred cats compared with non-purebred cats, and a similar mean age pattern of 8–9.5 years.1,5,21,22
In our study, most cats presented with progressive onset of mild neurological signs within 3 weeks, and four cats (cats 4, 6, 11 and 12) showed acute onset, with more severe neurological abnormalities in two cats (cats 4 and 11). This matches previous studies, which shows that ambulatory paraparesis is the main neurological sign in cats with IVDH and that acute, progressive and non-progressive neurological signs are associated with intervertebral disc disease.5,22,23 It should be noted that the assessment of the clinical course in this survey was largely based on owners’ reports, and surgery as a treatment was chosen immediately after diagnostic imaging. This limited the assessment of the clinical course and evaluation of any medical treatment before surgery.
Originally, PLC was devised to address compressive disc herniations located ventral to the spinal cord without the need to manipulate or move the spinal cord during surgery. Initially described as a procedure for removing chronic disc herniations resistant to conventional approaches, PLC has also found widespread application in the treatment of acute disc herniations. 24 The majority of cases presented in this study met these criteria, showing slightly lateralised (cats 1, 3–5, 7, 8, 10–12) or central located (cat 9) disc herniation, whereas two cats (cats 2 and 6) showed obvious lateralisation. Concerning the mineralisation of the herniated disc material, differentiation between acute and chronic herniated discs can be achieved, with more mineralised material commonly found in chronic herniations. 25 This aligns with another proposed indication for PLC in dogs, suggesting that chronically prolapsed disc material being firmly attached to the vertebra and removing it by PLC is advantageous. 11 However, there is also the possibility of acute intervertebral disc extrusion (IVDE) occurring on a chronic intervertebral disc protrusion (IVDP), which appears to be more common in cats. A recently published study demonstrated that some IVDH had imaging and surgical characteristics of both IVDP and IVDE. 5 Upon investigating the mineralisation of herniated disc material and spinal cord compression, we observed that all cats with pronounced mineralised disc material also showed severe spinal cord compression. In addition, one of the two cases with low mineralised herniated disc material showed severe spinal cord compression. In both cats with low mineralised herniated disc material, decompression was good and the outcome was excellent or good, whereas in cases of pronounced mineralised herniated disc material, a low degree of decompression and poorer outcome was achieved.
The distribution of affected discs was predominantly located in the caudal thoracic and cranial lumbar vertebral column, aligning closely with the well-established primary location of symptomatic IVDH in cats, typically between T3–L3.3,23,26–28 In addition, two studies investigated L4–5 and L6–7, respectively, as the primary locations for IVDH.21,22 The reasons for this are attributed to the unique configuration of the vertebral column and the high range of motion in this area of the vertebral column. The feline vertebral column shows mild extension in the lower lumbar segments, pronounced flexion in the lower thoracic and upper lumbar regions, and significant extension in the cranial thoracic (above T9) and cervical segments. During stance, the lower lumbar joints (L4–5 to L6–7) are nearly maximally extended, and the joints from T10 to T13 are maximally flexed, while the remaining joints are maintained in a mid-range position. This biomechanical positioning may contribute to the increased prevalence of intervertebral disc disease at T12–L1 and L4–6 in clinically affected cats. 29 In addition, it is suggested that the strain on the lower back during jumping may increase the incidence of clinically significant IVDH in cats. 21 Further reasons for clinically significant IVDH in the region caudally to T11 include the absence of the intercapital ligament, which provides additional dorsal support to the disc and enhances stability. 26
In this study, MRI was the preferred imaging modality for most of the cats preoperatively. When MRI was performed, an additional CT scan was conducted for better imaging of bone structures and surgical planning preoperatively, except in two cases. However, additional CT scans pre- and postoperatively provide valuable information and should be considered for adequate planning and to ensure successful decompression. Myelo-CT was the second most used imaging modality. Both MRI and myelo-CT are highly sensitive in detecting IVDH up to 98.5% and 97%, respectively, in small-sized dogs.30,31 Compared with myelo-CT, MRI is a non-invasive technique and can provide more prognostic information than other imaging modalities. 32 This is particularly important in cats, where disc herniation is a less common cause for spinal disorders compared with other conditions, such as neoplasia, inflammatory/infectious disease, traumatic injuries and vascular diseases. 33
This study has some limitations. The most significant limitation is its retrospective nature and the absence of control groups with similar presentation and imaging findings that were managed non-surgically (ie, medical/conservative treatment) or treated with a different surgical decompressive technique. Neurological assessment, diagnostic imaging, surgical technique, postoperative evaluation and follow-up varied among cases and could not be standardised. Imaging data sets were obtained using different methods, which could lead to inaccurate measurements. The slice thickness of CT scans was not standardised and there could be different measurement results between MRI and CT scans. Moreover, the sample size of 12 cases is small, precluding statistical analysis; however, given the limited number of PLCs performed in cats, the authors believe that this case series study provides valuable preliminary evidence for further assessment of whether this technique should be considered as a decompressive surgery in cats and whether this technique should be recommended over other treatments for IVDH in cats. Further prospective studies with standardised protocol and precise postoperative short- and long-term follow-up are warranted. In particular, the intraoperative monitoring of blood loss is critical given the consequences of haemorrhage in some cats in this study.
Conclusions
Our findings confirm the feasibility of PLC as a decompressive spinal surgery in cats. The risk of surgical complication in this cohort was high, with a 25% mortality rate. Meticulous attention to adequate slot creation in all three dimensions to obtain adequate decompression and management of intraoperative haemorrhage were identified as important factors in achieving a favourable outcome. For cases without intra- or postoperative complications, our study suggests a favourable prognosis for cats undergoing PLC.
Acknowledgments
The authors would especially like to thank the University of Bern, Leipzig University and the Tierklinik Hofheim for providing the cases, as well as Dr Jan Wennemuth for evaluating the imaging data sets.
Footnotes
Accepted: 25 September 2024
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: The work described in this manuscript involved the use of non-experimental (owned or unowned) animals. Established internationally recognised high standards (‘best practice’) of veterinary clinical care for the individual patient were always followed and/or this work involved the use of cadavers. Ethical approval from a committee was therefore not specifically required for publication in JFMS. Although not required, where ethical approval was still obtained, it is stated in the manuscript.
Informed consent: Informed consent (verbal or written) was obtained from the owner or legal custodian of all animal(s) described in this work (experimental or non-experimental animals, including cadavers, tissues and samples) for all procedure(s) undertaken (prospective or retrospective studies). No animals or people are identifiable within this publication, and therefore additional informed consent for publication was not required.
ORCID iD: Florian Tyroller  https://orcid.org/0009-0009-0309-7200
https://orcid.org/0009-0009-0309-7200
References
- 1. De Decker S, Warner A-S, Volk HA. Prevalence and breed predisposition for thoracolumbar intervertebral disc disease in cats. J Feline Med Surg 2017; 19: 419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Marioni-Henry K, Vite CH, Newton AL, et al. Prevalence of diseases of the spinal cord of cats. J Vet Intern Med 2004; 18: 851–858. [DOI] [PubMed] [Google Scholar]
- 3. Bibbiani L, Gelendi S, Bernardini M, et al. Prevalence, clinical presentation and MRI of intervertebral disc herniations in cats. J Feline Med Surg 2022; 24: e443–e452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hamilton-Bennett S, Behr S. Clinical presentation, magnetic resonance imaging features, and outcome in 6 cats with lumbar degenerative intervertebral disc extrusion treated with hemilaminectomy. Vet Surg 2019; 48: 556–562. [DOI] [PubMed] [Google Scholar]
- 5. Amey JA, Liatis T, Cherubini GB, et al. Outcomes of surgically and conservatively managed thoracolumbar and lumbosacral intervertebral disc herniations in cats. J Vet Intern Med 2024; 38: 247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. King AS. Protrusion of the intervertebral disc in the cat. Vet Rec 1958; 70: 509–515. [Google Scholar]
- 7. King AS, Smith RN. Disc protrusion in the cat: ventral protrusions and radial splits. Res Vet Sci 1960; 1: 301–308. [Google Scholar]
- 8. King AS. Disc protrusion in the cat: age incidence of dorsal protrusions. Vet Rec 1960; 72: 381–383. [Google Scholar]
- 9. Butler WF. Histological age changes in the ruptured intervertebral disc of the cat. Res Vet Sci 1968; 9: 130–137. [PubMed] [Google Scholar]
- 10. King A, Smith RN. Degeneration of the intervertebral disc in the cat. Acta Orthop Scand 1964; 34: 139–158. [DOI] [PubMed] [Google Scholar]
- 11. Moissonnier P, Meheust P, Carozzo C. Thoracolumbar lateral corpectomy for treatment of chronic disk herniation: technique description and use in 15 dogs. Vet Surg 2004; 33: 620–628. [DOI] [PubMed] [Google Scholar]
- 12. Ferrand FX, Moissonnier P, Filleur A, et al. Thoracolumbar partial lateral corpectomy for the treatment of chronic intervertebral disc disease in 107 dogs. Ir Vet J 2015; 68: 27. DOI: 10.1186/s13620-015-0056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Salger F, Ziegler L, Böttcher IC, et al. Neurologic outcome after thoracolumbar partial lateral corpectomy for intervertebral disc disease in 72 dogs. Vet Surg 2014; 43: 581–588. [DOI] [PubMed] [Google Scholar]
- 14. Böttcher P, Flegel T, Böttcher IC, et al. Partial lateral corpectomy for ventral extradural thoracic spinal cord compression in a cat. J Feline Med Surg 2008; 10: 291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ito D, Shiozawa N, Sekiguchi N, et al. Repeated surgical treatment and long-term outcome of a cat with vertebral vascular hamartoma. J Vet Med Sci 2020: 82; 721–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Malik Y, Konar M, Wernick M, et al. Chronic intervertebral disk herniation associated with fused vertebrae treated by vertebral lateral corpectomy in a cat. Vet Comp Orthop Traumatol 2009; 22: 170–173. [DOI] [PubMed] [Google Scholar]
- 17. Moissonnier P. Thoracolumbar lateral corpectomy. In: Shores A, Brisson BA. (eds). Current techniques in canine and feline neurosurgery. Hoboken, NJ: Wiley, 2017, pp 199–204. [Google Scholar]
- 18. Smith B, Hosgood G, Kerwin S. Ventral slot decompression for cervical intervertebral disc disease in 112 dogs. Aust Vet Pract 1997; 27: 58–64. [Google Scholar]
- 19. Clark D. An analysis of intraoperative and early postoperative mortality associated with cervical spinal decompressive surgery in the dog. J Am Anim Hosp Assoc 1986; 22: 739–744. [Google Scholar]
- 20. Turnwald G, Pichler M. Blood transfusion in dogs and cats part II. Administration, adverse effects and component therapy. Compend Contin Educ Pract Vet 1985; 7: 115. [Google Scholar]
- 21. Muñana KR, Olby N, Sharp N, et al. Intervertebral disk disease in 10 cats. J Am Anim Hosp Assoc 2001; 37: 384–389. [DOI] [PubMed] [Google Scholar]
- 22. Fowler KM, Pancotto TE, Werre SR, et al. Outcome of thoracolumbar surgical feline intervertebral disc disease. J Feline Med Surg 2021; 24: 473–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rayward R. Feline intervertebral disc disease: a review of the literature. Vet Comp Orthop Traumatol 2002; 15: 137–144. [Google Scholar]
- 24. Jeffery ND, Harcourt-Brown TR, Barker AK, et al. Choices and decisions in decompressive surgery for thoracolumbar intervertebral disk herniation. Vet Clin North Am Small Anim Pract 2018; 48: 169–186. [DOI] [PubMed] [Google Scholar]
- 25. Olby NJ, Müntana KR, Sharp NJ, et al. The computed tomographic appearance of acute thoracolumbar intervertebral disc herniations in dogs. Vet Radiol Ultrasound 2000; 41: 396–402. [DOI] [PubMed] [Google Scholar]
- 26. King A. Disc protrusions in the cat: distribution of dorsal protrusions along the vertebral column. Vet Rec 1960; 72: 335–337. [Google Scholar]
- 27. Kathmann I, Cizinauskas S, Rytz U, et al. Spontaneous lumbar intervertebral disc protrusion in cats: literature review and case presentations. J Feline Med Surg 2000; 2: 207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mella SL, Cardy TJ, Volk HA, et al. Clinical reasoning in feline spinal disease: which combination of clinical information is useful? J Feline Med Surg 2020; 22: 521–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Macpherson J, Ye Y. The cat vertebral column: stance configuration and range of motion. Exp Brain Res 1998; 119: 324–332. [DOI] [PubMed] [Google Scholar]
- 30. Cooper JJ, Young BD, Griffin IV, et al. Comparison between noncontrast computed tomography and magnetic resonance imaging for detection and characterization of thoracolumbar myelopathy caused by intervertebral disk herniation in dogs. Vet Radiol Ultrasound 2014; 55: 182–189. [DOI] [PubMed] [Google Scholar]
- 31. Dennison SE, Drees R, Rylander H, et al. Evaluation of different computed tomography techniques and myelography for the diagnosis of acute canine myelopathy. Vet Radiol Ultrasound 2010; 51: 254–258. [DOI] [PubMed] [Google Scholar]
- 32. Olby N, Moore S, Brisson B, et al. ACVIM consensus statement on diagnosis and management of acute canine thoracolumbar intervertebral disc extrusion. J Vet Intern Med 2022; 36: 1570–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gonçalves R, Platt SR, Llabrés-Díaz FJ, et al. Clinical and magnetic resonance imaging findings in 92 cats with clinical signs of spinal cord disease. J Feline Med Surg 2009; 11: 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]



