Abstract
Objective
The purpose of the study was to compare the impact of the mobilization techniques and mobilization with movement techniques on static balance in individuals with acute inversion ankle sprain.
Methods
Volunteers with acute inversion ankle sprain (N = 40) were equally and randomly assigned to 2 groups. Participants in intervention group I received the Mulligan mobilization with movement techniques, whereas participants in intervention group II underwent the Maitland mobilization techniques. Each participant received the intervention every other day for 2 consecutive weeks. To assess static balance, participants assumed a single-leg stance on the affected leg at the center of a force plate with eyes open or closed plate for 20 seconds. The displacement, velocity, and area of the center of pressure were recorded 1 day before and after the intervention.
Results
The velocity of the center of pressure in the anterior-posterior direction was significantly reduced only in group I during eyes open (P = .043) and closed (P = .004). However, the displacement of the center of pressure in the anterior-posterior direction was significantly decreased in both group I (P = .024) and group II (P = .028) with eyes open. No significant changes were found in the area of the center of pressure in either group during eyes open or closed (P > .053).
Conclusions
Both Mulligan's and Maitland's approaches significantly improved sway displacement. For the individuals with acute inversion ankle sprain who were included in this study, the Mulligan technique were more effective in improving static balance indicators compared to the Maitland technique.
Clinical Trial
The study was then registered in the Iranian Registry of Clinical Trials (17/02/2019) (IRCT20190108042292N2).
Key Indexing Terms: Ankle sprain, Manual therapy, Postural balance
Introduction
Inversion ankle sprains are one of the common lower limb injuries, especially among athletes and individuals with intense physical activities.1 The prevalence of this injury is notably high in contact sports such as basketball (41.1%), football (9.3%), soccer (7.9%), and volleyball (7 per 1000 exposures), as well as during activities involving running and jumping.2,3 Around 60% of lower limb injuries in basketball players are related to inversion ankle sprains.4 The common mechanism of inversion ankle sprain involves foot supination, which can lead to the rupture of the lateral ankle ligaments.5 Individuals with acute ankle instability often find it challenging to rely on their injured ankle and may be unable to participate in strenuous sports activities.6
Conditions that may ultimately lead to chronic ankle sprain include anatomical damage to the muscle-tendon units, positional faults at the talar joint, restricted range of ankle dorsiflexion, decreased muscle strength, and deficits in postural stability.6,7 In more than 70% of inversion ankle sprains, the combined mechanical and functional disorders may result in poor quality of life, an inability to perceive joint position, delayed reactions to sudden inversion stress, and recurrent ankle sprains.8, 9, 10, 11
Conservative treatment for ankle sprain includes electrotherapy modalities and therapeutic exercises. However, these approaches usually do not address neuromuscular deficits and joint instability.10,12, 13, 14 The study by de Ruvo et al. (2022) found that the combination of manual therapy and exercise significantly improved pain levels, range of motion, and functional outcomes in patients with lateral ankle sprains compared to exercise alone.15 The orthopedic section of the American Physical Therapy Association recommends incorporating manual therapy techniques in the treatment protocol for ankle sprain.16 Several ankle joint mobilization approaches commonly used in physiotherapy practice were developed by renowned manual therapists, such as Geoffrey Maitland, Freddy Kaltenborn, and Brian Mulligan.17
Based on Maitland's concept, an anterior-to-posterior force is exerted on the talus during talocrural joint mobilization, a commonly used technique for restoring ankle joint motion. However, previous studies exploring the impact of mobilization on balance have provided controversial results.18, 19, 20
Another therapeutic concept is mobilization combined with movement, referred to as Mulligan's concept. This approach involves applying a sustained passive accessory motion within the joint while the patient actively performs a cardinal motion identified as painful or restricted. For individuals with an ankle sprain, a posterior-to-anterior glide is employed to the tibia adjacent to the talocrural joint during active ankle dorsiflexion.21 This approach is believed to offer several advantages, including expedited recovery of ankle range of motion without discomfort, treatment in a dynamic condition, and improvement of functional posture.22,23 Two earlier studies24,25 have established the significant effect of mobilization combined with movement on dynamic balance. However, another study26 has argued that this technique does not have a significant effect on dynamic balance.
To our knowledge, no other study has been conducted to compare the impact of Maitland and Mulligan mobilization approaches on individuals with acute ankle sprain specifically emphasizing static balance measurements. Therefore, the purpose of the current study was to compare the impact of mobilization techniques and mobilization with movement techniques on the static balance in individuals with an acute inversion ankle sprain. It was hypothesized that static balance significantly differs between individuals with acute inversion ankle sprain treated with mobilization with movement techniques and those treated with mobilization techniques.
Methods
Trial Design
This parallel, quasi-experimental, randomized clinical trial was conducted at the Neuromuscular Rehabilitation Research Center of Semnan University of Medical Sciences from May to July 2019. The study was approved by the Research Ethics Committee of Semnan University of Medical Sciences (IR.SEMUMS.REC.1397.205) and was subsequently registered in the Iranian Registry of Clinical Trials on February 17, 2019 (IRCT20190108042292N2).
Randomization and Blinding
The participants (N = 40) were randomly and equally assigned to 2 groups using a method that randomly generates odds and even numbers, which was administered by a colleague who was not involved in the treatment or assessment. The random allocation was conducted by selecting sealed envelopes that contained numbers between 1 and 40. Both groups were well-matched in terms of physical activity levels and body mass index (BMI).
A physical therapist with 4 years of clinical practice in manual therapy administered the intervention in both groups. Another physical therapist, blinded to group allocation, measured the outcome variables in both groups. The assessor and participants remained blinded to the groups in this double-blinded clinical trial.
Participants
Individuals (N = 44) who were referred to the NMRRC at SUMS with acute inversion ankle sprain were screened and enrolled in the study. Four volunteers were excluded from the study due to ankle immobilization for less than 2 weeks, diabetes mellitus, and a history of bone fractures in the affected lower limb. The intervention and evaluation procedures were explained to all volunteers using clear and simple language. Subsequently, all participants reviewed and signed an informed consent form before participating in the study.
The group I underwent ankle mobilization with active motion techniques, whereas the group II received ankle mobilization techniques. The variables were measured in both groups 1 day before and after the intervention.
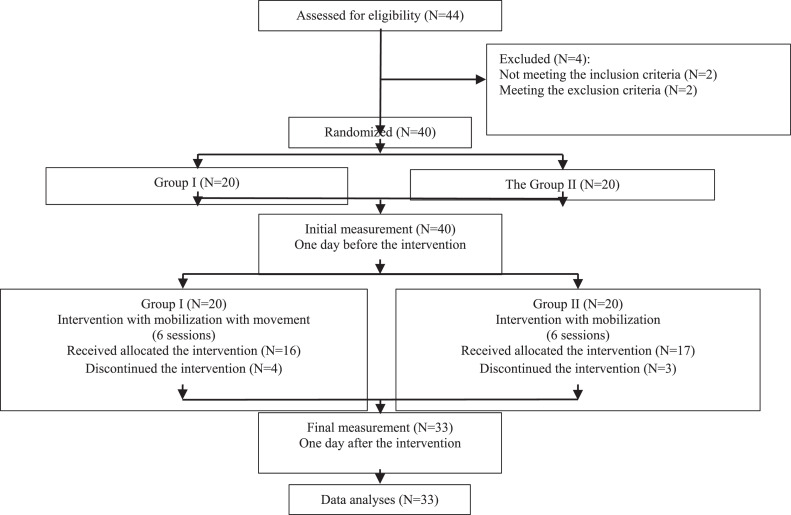
During the intervention, 3 subjects from group I and 1 subject from group II withdrew due to aggravated pain during the procedure. Additionally, 1 subject from group I and 2 subjects from group II were excluded due to intolerance to discomfort during the intervention (Fig 1).
Fig 1.
Flowchart of the study.
The Inclusion Criteria
The inclusion criteria consisted of young adults aged between 20 and 40 years who were experiencing their first unilateral inversion ankle sprain. Participants were required to have undergone ankle immobilization for a period of 14 to 28 days prior to the intervention. Grade II mechanical instability in the talocrural joint needed to be identified according to specific indicators. These indicators included moderate pain, rated 3 to 7 on the Visual Analog Scale (VAS), as well as greater anterior displacement of the talus on the injured side compared to the uninjured side during the anterior drawer test before ankle immobilization, with the anterior displacement required to measure between 3 and 10 mm. Additionally, moderate pain (rated 3 to 7 on the VAS) and greater inversion tilt of the talus on the injured side compared to the uninjured side during the talar tilt test before ankle immobilization needed to be observed, with the inversion tilt required to measure between 3 and 9 degrees.27, 28, 29, 30, 31
The Exclusion Criteria
The exclusion criteria encompassed systemic, neurological, or rheumatological diseases, history of fracture, dislocation, or subluxation in either lower limb, intra-articular steroid injection in either lower limb, medication intervention in the last 2 weeks, rehabilitation for the lower quadrant of the skeleton in the last 6 months, aggravation of pain during intervention, intolerance of discomfort during intervention.18,32,33
Interventions
Each patient received the intervention every other day for 2 consecutive weeks, comprising 3 sessions per week. Prior to the mobilization techniques, the therapist examined the pain-free accessory motion range of the talus and then implemented rhythmic oscillations equivalent to grade III with a large amplitude to exert a tensile force on the periarticular tissues.
Mulligan Mobilization
The patients assumed a standing position in front of the therapist at the end of the treatment table and slightly advanced their affected lower extremity. The therapist securely wrapped a belt around her pelvis and the patient's distal tibia and fibula. To stabilize the talus, the therapist placed her hands one on top of the other on the patient's talus. The therapist then displaced her pelvis backward with oscillation, causing a forward displacement of the patient's distal tibia and fibula. The patients concurrently dorsiflexed their ankles to a pain-free end range (Fig 2A).34 Within each session, the patients received 8 bouts, with each bout lasting 30 seconds, followed by a 1-minute rest interval.35
Fig 2.
Mobilization techniques; (A) mobilization with movement approach (Mulligan's mobilization techniques) and (B) mobilization approach (Maitland's mobilization techniques).
Maitland Mobilization
The patients were instructed to lie down, with the knee and hip joints of the affected lower limb placed at 90º and 60º flexion, respectively. The opposite lower limb was positioned in a neutral position. A wooden board was used to support the affected ankle joint at 20º plantar flexion. At the end of the treatment table, the therapist placed her first web space on the talus. The mobilizing force was directed parallel to the articular surface of the tibia (Fig 2B). Within each session, the patients underwent 2 bouts, and each bout lasted 2 minutes, with a 1-minute rest interval.36
Outcome Measures
The Static Balance Tests
To assess static balance, participants assumed a barefoot single-leg stance at the center of a force plate (9260AA6, Kistler Group, Switzerland) and carried out 3 trials with eyes open and 3 trials with eyes closed on the affected leg. The balance tests were conducted in random order to prevent fatigue and minimize learning effects.
The test protocol was designed to minimize movement interference. This protocol was rehearsed several times prior to recording. Initially, the participants wore a soft collar to prevent additional small motions in the craniocervical vertebrae. Subsequently, the participants crossed their upper extremities on their chests, elevated the unaffected leg at 30 degrees of hip flexion and 45 degrees of knee flexion, and aimed to remain motionless throughout each 20-second trial. During the single-leg stance with eyes open, participants were instructed to focus their gaze on a cross marked on the wall located 3 meters away from them. If any part of the suspended leg touched the ground, the trial was repeated.37,38
The center of pressure (CoP) data was collected at a sampling rate of 120 Hz, 1 day before and after the intervention. These parameters encompassed the sway displacement, velocity, and area in both the medial-lateral and anterior-posterior directions during single-leg stance on the affected leg, with eyes open and eyes closed. The mean sway displacement, velocity, and area were calculated from the 3 trials.
Sample Size
To our knowledge, no study was conducted to compare the impact of the Mulligan and Maitland mobilization approaches on static balance. Therefore, it was decided to rely on the data obtained from the present study to estimate the sample size. The change in the CoP area during single-leg stance with eyes closed was identified as the primary outcome in individuals with an acute inversion ankle sprain. The G*Power software was used to calculate the sample size. The effect size difference between the 2 groups was conservatively assumed to be 1. Considering a 95% confidence interval and 80% power for 2-tailed independent samples t-test, the estimated sample size was 17 individuals in each group. Furthermore, a 20% dropout rate was taken into account for each group.
Statistical Analyses
In this study, mean and standard deviation values for quantitative variables and frequency distribution for the sex variable were reported for each group. The Chi-square test was employed to examine the frequency distribution of sex between the 2 groups. The normal distribution of quantitative variables was assessed using the Shapiro–Wilk test. Based on the results of the Shapiro–Wilk test, the means of the background variables between the 2 groups was compared using the independent samples t-test, while the means of the dependent variables between the 2 groups was compared using either the Mann–Whitney U test or the independent samples t-test. The general linear model approach with repeated measures was employed to compare the mean of the dependent variables at 2 measurements, before and after the intervention. The data were analysed using SPSS software at a significance level of 0.05.
Results
The group I, which received the Mulligan mobilization techniques, consisted of 16 participants (6 females, 10 males) with a mean age of 29.12 ± 7.50 years and a BMI of 26.12 ± 3.77 kg/m², while group II, which underwent the Maitland mobilization techniques, comprised 17 subjects (9 females, 8 males) with a mean age of 33.29 ± 5.75 years and a BMI of 27.00 ± 3.55 kg/m². There was no significant difference in sex (P = .373), age (P = .082), and BMI (P = .498) between the individuals in the 2 groups.
Table 1 presents the mean and standard deviation of the center of pressure (CoP) velocity in the anterior-posterior and medial-lateral directions during single-leg stance on the affected leg, with eyes open and closed, for each group before and after the intervention. Prior to the intervention, there was no significant difference (P > .149) in the CoP velocity between the 2 groups in both directions, with eyes open and closed. The CoP velocity in the anterior-posterior direction was significantly reduced within groups with eyes open (P = .020) and closed (P = .003). These changes were statistically significant in group I with eyes open (P = .043) and closed (P = .004), while they were not significant in group II with eyes open (P = .203) and closed (P = .179).
Table 1.
The Mean and Standard Deviation of the Center of Pressure Velocity in the Anterior-Posterior and Medial-Lateral Directions During Single Leg Stance on the Affected Leg With Eyes Open and Closed for Each Group Before and After the Intervention
| Variables | Before Intervention | After Intervention | Effect Size | P* | P⁎⁎ | P⁎⁎⁎ | |||
|---|---|---|---|---|---|---|---|---|---|
| CoP velocity (cm/s) | Eyes open | AP | Group I | 4.96 ± 1.87 | 3.87 ± 1.76 | 0.247 | .705 | .020 | .628 |
| Group II | 4.58 ± 2.36 | 3.85 ± 1.38 | 0.099 | ||||||
| ML | Group I | 4.61 ± 2.19 | 3.77 ± 1.20 | 0.139 | .560 | .178 | .408 | ||
| Group II | 4.02 ± 1.64 | 3.82 ± 1.65 | 0.009 | ||||||
| Eyes closed | AP | Group I | 11.26 ± 3.03 | 7.57 ± 3.85 | 0.438 | .556 | .003 | .313 | |
| Group II | 9.76 ± 4.04 | 7.86 ± 4.30 | 0.110 | ||||||
| ML | Group I | 7.66 ± 2.94 | 7.12 ± 3.83 | 0.012 | .964 | .101 | .341 | ||
| Group II | 8.42 ± 2.88 | 6.43 ± 3.07 | 0.266 | ||||||
Between group effect,
within group effect, and
within and between group interaction effect in ANOVA with repeated measurements, significant at P ≤ .05.
Data are presented as mean ± standard deviation (M ± SD).
Group I; intervention with Mulligan's mobilization approach, Group II; intervention with Maitland's mobilization approach, AP; anterior-posterior direction, ML; medial-lateral direction, CoP velocity; center of pressure velocity.
Table 2 presents the mean and standard deviation of the CoP displacement in the anterior-posterior and medial-lateral directions during single-leg stance on the affected leg, with eyes open and closed, for each group before and after the intervention. Prior to the intervention, there was no significant difference (P > .181) in the CoP displacement between the 2 groups in both directions, with eyes open and closed. The CoP displacement in the anterior-posterior direction exhibited a significant reduction within groups with eyes open (P = .002) and closed (P = .010). These changes were found to be statistically significant in group I (P = .024) and group II (P = .028) with eyes open, while with eyes closed, these changes were not significant in either group I (P = .068) and group II (P = .077).
Table 2.
The Mean and Standard Deviation of the Center of Pressure Displacement in the Anterior-Posterior and Medial-Lateral Directions During Single Leg Stance on the Affected Leg With Eyes Open and Closed for Each Group Before and After the Intervention
| Variables | Before Intervention | After Intervention | Effect Size | P* | P⁎⁎ | P⁎⁎⁎ | |||
|---|---|---|---|---|---|---|---|---|---|
| CoP displacement (cm) | Eyes open | AP | Group I | 79.08 ± 37.80 | 53.73 ± 19.23 | 0.295 | .960 | .002 | .862 |
| Group II | 78.28 ± 41.00 | 55.36 ± 17.67 | 0.267 | ||||||
| ML | Group I | 63.95 ± 21.07 | 55.52 ± 25.16 | 0.089 | .604 | .113 | .911 | ||
| Group II | 68.67 ± 35.78 | 58.99 ± 25.44 | 0.074 | ||||||
| Eyes closed | AP | Group I | 180.42 ± 64.83 | 129.01 ± 78.50 | 0.205 | .487 | .010 | .731 | |
| Group II | 161.72 ± 69.70 | 121.89 ± 71.08 | 0.183 | ||||||
| ML | Group I | 125.19 ± 51.15 | 120.09 ± 81.02 | 0.003 | .345 | .293 | .443 | ||
| Group II | 153.44 ± 65.99 | 121.25 ± 65.38 | 0.099 | ||||||
Between group effect,
within group effect, and
within and between group interaction effect in ANOVA with repeated measurements, significant at P ≤ .05.
Data are presented as mean ± standard deviation (M ± SD).
Group I; intervention with Mulligan's mobilization approach, Group II; intervention with Maitland's mobilization approach, AP; anterior-posterior direction, ML; medial-lateral direction, CoP displacement; center of pressure displacement.
Table 3 presents the mean and standard deviation of the CoP area during single-leg stance on the affected leg, with eyes open and closed, for each group before and after the intervention. Prior to the intervention, there was no significant difference (P > .829) in the CoP area between the 2 groups with eyes open and closed.
Table 3.
The Mean and Standard Deviation of Center of Pressure area During Single Leg Stance With Eyes Open and Closed for Each Group Before and After Intervention
| Variables | Before Intervention | After Intervention | Effect Size | P* | P⁎⁎ | P⁎⁎⁎ | ||
|---|---|---|---|---|---|---|---|---|
| CoP area (cm2) | Eyes open | Group I | 10.34 ± 4.86 | 8.26 ± 5.06 | 0.115 | .755 | .266 | .614 |
| Group II | 10.14 ± 6.36 | 9.35 ± 5.31 | 0.009 | |||||
| Eyes closed | Group I | 24.16 ± 16.55 | 16.79 ± 13.39 | 0.076 | .833 | .053 | .826 | |
| Group II | 25.62 ± 11.75 | 16.42 ± 13.70 | 0.176 | |||||
Between group effect,
within group effect, and
within and between group interaction effect in ANOVA with repeated measurements, significant at P ≤ .05.
Data are presented as mean ± standard deviation (M ± SD).
Group I; intervention with Mulligan's mobilization approach, Group II; intervention with Maitland's mobilization approach, CoP area; center of pressure area.
Discussion
In the present study, the comparison of Mulligan's and Maitland's approaches in individuals with acute inversion ankle sprain revealed encouraging outcomes in terms of stability and balance. Both Mulligan's and Maitland's approaches significantly improved sway displacement. However, sway velocity was exclusively reduced in individuals who received the Mulligan approach. The Mulligan approach demonstrated slightly greater effects, implying subtle distinctions in the impact of the 2 approaches.
Previous studies did not explore the impact of Mulligan mobilization on static balance and primarily concentrated on its effects on dynamic balance. For instance, Ayad et al.24 and Cruz-Diaz et al.25 observed significant effects of mobilization with movement on dynamic balance. On the contrary, Gilbreath et al. assessed balance indicators 24-48 hours postmobilization and did not identify a significant effect on dynamic balance.26
In the 2009 study by Hopper et al., a cross-sectional investigation was conducted to explore the impact of Mulligan's ankle taping on static balance, postural sway recovery patterns, and dynamic tracking balance tasks in patients with unilateral chronic ankle instability.39
They discovered that Mulligan ankle taping did not have an effect on static balance indicators. The disparity between the findings of the mentioned studies and the present study can be attributed to the difference in interventions. Specifically, in the present study, the Mulligan mobilization techniques were utilized, whereas in the Hopper study, Mulligan ankle taping was employed.
It appears that the techniques employed in the current study may have a more pronounced impact on central mechanisms of movement and postural control, potentially leading to an improvement in static balance through the provision of articular stimulus.25,33,40 Additionally it is worth noting that they measured sway area as an index of static balance for 10 seconds, whereas in the present study, the measurement was extended to 20 seconds. This difference in measurement duration could contribute to variations in the observed results between the 2 studies.
The results of the present study align with the findings of Cruz-Díaz et al. in 2020.41 Cruz-Díaz and colleagues explored the impact of incorporating self-mobilization of the ankle joint, specifically focusing on posterior gliding of the talus and enhanced by the active movement of the patient, alongside CrossFit training in individuals with chronic ankle instability. They observed that after 3 months of intervention, the combination of self-mobilization and CrossFit training was more effective than CrossFit training alone.
Upon analyzing the static balance indicators, it can be concluded that the intervention using the Maitland's method did not result in a significant improvement in the subjects' static balance across the majority of the indexes.
In the existing published literature, the effectiveness of Maitland mobilization techniques on dynamic balance has been explored.42 For example, Wells et al. conducted a study on 17 individuals aged 18 to 35 years with chronic ankle sprain. Their findings did not reveal a significant effect of 1 session of Maitland grade 4 mobilization on dynamic balance.43 Likewise, in another study by Harkey et al., the application of Maitland's third-degree mobilization for ankle sprain showed no significant effect on the subjects' dynamic balance.44
In the study by Hoch et al., involving 12 patients with chronic ankle sprain, the Maitland mobilization techniques was applied in 6 sessions over a 2-week treatment period with 1 day in between each session. Balance measurements were taken 24-72 hours after the last therapeutic session.45 The results indicated that this intervention did not lead to an improvement in static balance. Consistent with their findings, it was observed that 6 sessions of Maitland's intervention did not have a significant effect on static balance in the present study.
In another study, Hoch et al. used a third-degree Maitland mobilization session on 20 patients with chronic ankle sprain, and examined the balance indices immediately after using the time-to-boundary method.46 Their conclusion suggested that this intervention had positive effects on static balance but did not yield positive effects on dynamic balance. The observed inconsistency in results between this study and the present one may be attributed to differences in study characteristics and methodologies.
In a recent systematic review conducted by Weerasekara et al. in 2018, the clinical benefits of joint mobilization were explored. The findings of the review suggested that the Mulligan techniques are more likely to yield clinical benefits compared to Maitland mobilization, traction, and manipulation. Furthermore, when compared to other manual therapy techniques such as Maitland and manipulation, fewer studies reported no positive outcomes with Mulligan techniques.23 The results of the present study align with the conclusions drawn in the aforementioned systematic review, indicating consistency with the idea that the Mulligan techniques are more likely to produce clinical benefits compared to Maitland mobilization and other manual therapy techniques.
Limitations and Recommendations
The present study recognizes several limitations that should be considered when interpreting the findings. A key limitation is the lack of comprehensive guidelines for manual therapy techniques in previous research, including the number of treatment bouts, duration, and intervals, which complicates the determination of optimal dosages and their effects. Additionally, the current study only conducted a postintervention evaluation due to time constraints, highlighting the need for future research to include follow-up assessments to better understand the long-term impact of interventions.
This study is the first of its kind, with a sample size calculated using standard statistical assumptions (alpha 0.05, power 80%). While the study met its estimated sample size, it remains relatively small, which may limit the generalizability of findings and increase the risk of Type I errors. The small sample size can reduce statistical power, making it harder to detect true effects, especially if effect sizes are small. Additionally, limited sample diversity may affect the results' applicability to broader populations. Using different statistical assumptions and variables would have resulted in a larger required sample size. Future research should aim for larger, more diverse samples to address these limitations.
Another significant limitation is the involvement of the same therapist in treating both groups, which may introduce bias due to individual treatment styles and the rapport established with participants. This bias cannot be easily mitigated in a small study, and the subjective judgment of the therapist may also influence perceived treatment efficacy. However, it is important to acknowledge that having the same therapist offers certain advantages as well. It ensures a consistent level of pressure and maintains a uniform skill level throughout the treatment process, which may help control for variability in treatment delivery. Future studies should consider employing multiple therapists or randomizing therapist assignments to enhance reliability and generalizability.
To provide a more holistic evaluation, future research should incorporate subjective measures of functional outcomes and patient-reported outcomes, allowing for a better understanding of the interventions' overall impact on patients' well-being. Additionally, applying the Maitland and Mulligan approaches to a diverse range of injuries, age groups, and populations is recommended to further explore the effectiveness and applicability of these techniques. Addressing these limitations will enhance the reliability and relevance of future findings, leading to more effective and personalized treatment approaches for patients with ankle sprains.
Conclusion
In the present study, the included individuals with acute inversion ankle sprain who received either Mulligan's and Maitland's approaches showed significantly improved sway displacement. However, sway velocity was exclusively reduced in individuals who received the Mulligan approach.
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Human Subjects or Animals
The study protocol was reviewed and approved by the Research Ethics Board of SUMS (IR.SEMUMS.REC.1397.205).
Funding Sources and Conflicts of Interest
The research and technology deputy of Semnan University of Medical Sciences (Grant number: 1639) funded this project. The Neuromuscular Rehabilitation Research Center of Semnan University of Medical Sciences provided the work place and instruments. No conflicts of interest were reported for this study.
Contributorship Information
Concept development: CTD, PA, RB, AN; Design: CTD, PA, RB, AN; Supervision: CTD, AN; Data collection/processing: CTD, PA, RB, AN; Analysis/interpretation: CTD, PA, MM, RB, AN; Literature search: CTD, PA, AN; Writing: CTD, PA; Critical review: CTD, PA, MM, RB, AN.
Practical Applications.
-
•
Both Mulligan's and Maitland's approaches improved sway displacement.
-
•
However, sway velocity was exclusively reduced in individuals who received Mulligan's approach.
-
•
The Mulligan's approach demonstrated slightly greater effects, thereby implying subtle distinctions in the impact of the two approaches.
Alt-text: Unlabelled box
References
- 1.Beynnon BD, Renström PA, Haugh L, Uh BS, Barker H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34(9):1401–1412. doi: 10.1177/0363546506288676. [DOI] [PubMed] [Google Scholar]
- 2.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 3.Cavazos GJ Jr, Harkless LB. The epidemiology, evaluation, and assessment of lateral ankle sprains in athletes. J Sports Med Ther. 2021;6:8–17. [Google Scholar]
- 4.Dick R, Hertel J, Agel J, Grossman J, Marshall SW. Descriptive epidemiology of collegiate men's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athlet Train. 2007;42(2):194. [PMC free article] [PubMed] [Google Scholar]
- 5.Witjes S, Gresnigt F, Van Den Bekerom MP, Olsman JG, Van Dijk NC. The ANKLE TRIAL (ANKLE treatment after injuries of the ankle ligaments): what is the benefit of external support devices in the functional treatment of acute ankle sprain?: a randomised controlled trial. BMC Musculoskeletal Disord. 2012;13(1):1–8. doi: 10.1186/1471-2474-13-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Mohrej OA, Al-Kenani NS. Chronic ankle instability: current perspectives. Avicenna J Med. 2016;6(04):103–108. doi: 10.4103/2231-0770.191446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: a critical review. Foot Ankle Special. 2014;7(4):298–326. doi: 10.1177/1938640014539813. [DOI] [PubMed] [Google Scholar]
- 8.Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29(5):361–371. doi: 10.2165/00007256-200029050-00005. [DOI] [PubMed] [Google Scholar]
- 9.Konradsen L, Ravn JB. Ankle instability caused by prolonged peroneal reaction time. Acta Orthopaed Scand. 1990;61(5):388–390. doi: 10.3109/17453679008993546. [DOI] [PubMed] [Google Scholar]
- 10.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19(10):653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 11.Hubbard TJ, Wikstrom EA. Ankle sprain: pathophysiology, predisposing factors, and management strategies. Open Access J Sports Med. 2010;1:115. doi: 10.2147/oajsm.s9060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wikstrom EA, Hubbard TJ. Talar positional fault in persons with chronic ankle instability. Arch Phys Med Rehab. 2010;91(8):1267–1271. doi: 10.1016/j.apmr.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 13.Petersen W, Rembitzki IV, Koppenburg AG, et al. Treatment of acute ankle ligament injuries: a systematic review. Arch Orthop Trauma Surg. 2013;133(8):1129–1141. doi: 10.1007/s00402-013-1742-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKeon P, Booi M, Branam B, Johnson D, Mattacola C. Lateral ankle ligament anesthesia significantly alters single limb postural control. Gait Post. 2010;32(3):374–377. doi: 10.1016/j.gaitpost.2010.06.016. [DOI] [PubMed] [Google Scholar]
- 15.de Ruvo R, Russo G, Lena F, et al. The effect of manual therapy plus exercise in patients with lateral ankle sprains: a critically appraised topic with a meta-analysis. Journal of Clinical Medicine. 2022;11(16):4925. doi: 10.3390/jcm11164925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin RL, Davenport TE, Paulseth S, et al. Ankle stability and movement coordination impairments: ankle ligament sprains: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2013;43(9):A1–A40. doi: 10.2519/jospt.2013.0305. [DOI] [PubMed] [Google Scholar]
- 17.Pettman E. A history of manipulative therapy. J Manual Manipulat Ther. 2007;15(3):165–174. doi: 10.1179/106698107790819873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30(11):1798–1804. doi: 10.1002/jor.22150. [DOI] [PubMed] [Google Scholar]
- 19.Chevutschi A, d'Houwt J, Pardessus V, Thevenon A. Immediate effects of talocrural and subtalar joint mobilization on balance in the elderly. Physiother Res Int. 2015;20(1):1–8. doi: 10.1002/pri.1582. [DOI] [PubMed] [Google Scholar]
- 20.Cho B, Ko T, Lee D. Effect of ankle joint mobilization on range of motion and functional balance of elderly adults. J Phys Ther Sci. 2012;24(4):331–333. [Google Scholar]
- 21.Mulligan BR. Mobilisations with movement (MWM'S) J Manual Manipulat Ther. 1993;1(4):154–156. [Google Scholar]
- 22.Exelby L. Peripheral mobilisations with movement. Manual Ther. 1996;1(3):118–126. doi: 10.1054/math.1996.0259. [DOI] [PubMed] [Google Scholar]
- 23.Weerasekara I, Osmotherly P, Snodgrass S, Marquez J, de Zoete R, Rivett DA. Clinical benefits of joint mobilization on ankle sprains: a systematic review and meta-analysis. Arch Phys Med Rehab. 2018;99(7) doi: 10.1016/j.apmr.2017.07.019. 1395-412.e5. [DOI] [PubMed] [Google Scholar]
- 24.Ayad K, Abdelaal A, Elazizi H, Abdelgalil A. Efficacy of mobilization with movement in treatment of chronic ankle sprain. Physiotherapy. 2015;101:e96–ee7. [Google Scholar]
- 25.Cruz-Díaz D, Lomas Vega R, Osuna-Pérez MC, Hita-Contreras F, Martínez-Amat A. Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Disab Rehab. 2015;37(7):601–610. doi: 10.3109/09638288.2014.935877. [DOI] [PubMed] [Google Scholar]
- 26.Gilbreath JP, Gaven SL, Van Lunen BL, Hoch MC. The effects of mobilization with movement on dorsiflexion range of motion, dynamic balance, and self-reported function in individuals with chronic ankle instability. Manual Ther. 2014;19(2):152–157. doi: 10.1016/j.math.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Vereeck L, Wuyts F, Truijen S, Van de Heyning P. Clinical assessment of balance: normative data, and gender and age effects. Int J Audiol. 2008;47(2):67–75. doi: 10.1080/14992020701689688. [DOI] [PubMed] [Google Scholar]
- 28.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51(2):113–125. doi: 10.1136/bjsports-2016-096178. [DOI] [PubMed] [Google Scholar]
- 29.Hubbard TJ, Hertel J. Mechanical contributions to chronic lateral ankle instability. Sports Med. 2006;36(3):263–277. doi: 10.2165/00007256-200636030-00006. [DOI] [PubMed] [Google Scholar]
- 30.Landrum EL, Kelln BM, Parente WR, Ingersoll CD, Hertel J. Immediate effects of anterior-to-posterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Manual Manipulat Ther. 2008;16(2):100–105. doi: 10.1179/106698108790818413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gribble PA. Evaluating and differentiating ankle instability. J Athlet Train. 2019;54(6):617–627. doi: 10.4085/1062-6050-484-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitman JM, Cleland JA, Mintken P, et al. Predicting short-term response to thrust and nonthrust manipulation and exercise in patients post inversion ankle sprain. J Orthop Sports Phys Ther. 2009;39(3):188–200. doi: 10.2519/jospt.2009.2940. [DOI] [PubMed] [Google Scholar]
- 33.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. doi: 10.2519/jospt.2006.2265. [DOI] [PubMed] [Google Scholar]
- 34.Loudon JK, Reiman MP, Sylvain J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med. 2014;48(5):365–370. doi: 10.1136/bjsports-2013-092763. [DOI] [PubMed] [Google Scholar]
- 35.Hing W, Bigelow R, Bremner T. Mulligan's mobilisation with movement: a review of the tenets and prescription of MWMs. New Zealand J Physiother. 2008;36(3):144–165. [Google Scholar]
- 36.Silva RD, Teixeira LM, Moreira TS, Teixeira-Salmela LF, de Resende MA. Effects of anteroposterior talus mobilization on range of motion, pain, and functional capacity in participants with subacute and chronic ankle injuries: a controlled trial. J Manipulat Physiol Therap. 2017;40(4):273–283. doi: 10.1016/j.jmpt.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 37.López-Rodríguez S, de-Las-Peñas CF, Alburquerque-Sendín F, Rodríguez-Blanco C, Palomeque-del-Cerro L. Immediate effects of manipulation of the talocrural joint on stabilometry and baropodometry in patients with ankle sprain. J Manipulat Physiol Therap. 2007;30(3):186–192. doi: 10.1016/j.jmpt.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 38.Bernier JN, Perrin DH. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27(4):264–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]
- 39.Hopper D, Samsson K, Hulenik T, Ng C, Hall T, Robinson K. The influence of Mulligan ankle taping during balance performance in subjects with unilateral chronic ankle instability. Phys Ther Sport. 2009;10(4):125–130. doi: 10.1016/j.ptsp.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 40.Reid A, Birmingham TB, Alcock G. Efficacy of mobilization with movement for patients with limited dorsiflexion after ankle sprain: a crossover trial. Physiother Canada. 2007;59(3):166–172. [Google Scholar]
- 41.Cruz-Díaz D, Hita-Contreras F, Martínez-Amat A, Aibar-Almazán A, Kim K-M. Ankle-joint self-mobilization and CrossFit training in patients with chronic ankle instability: a randomized controlled trial. J Athlet Train. 2020;55(2):159–168. doi: 10.4085/1062-6050-181-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weerasekara I, Deam H, Bamborough N, et al. Effect of Mobilisation with Movement (MWM) on clinical outcomes in lateral ankle sprains: a systematic review and meta-analysis. Foot. 2020;43 doi: 10.1016/j.foot.2019.101657. [DOI] [PubMed] [Google Scholar]
- 43.Wells AM. Effects of joint mobilization on ankle dorsiflexion range of motion, dynamic postural control, and self-reported patient outcomes in individuals with chronic ankle instability. *Master's thesis*. Toledo, OH: University of Toledo; 2012.
- 44.Harkey M, McLeod M, Van Scoit A, et al. The immediate effects of an anterior-to-posterior talar mobilization on neural excitability, dorsiflexion range of motion, and dynamic balance in patients with chronic ankle instability. J Sport Rehab. 2014;23(4):351–359. doi: 10.1123/jsr.2013-0085. [DOI] [PubMed] [Google Scholar]
- 45.Hoch MC, Mullineaux DR, Andreatta RD, et al. Effect of a 2-week joint-mobilization intervention on single-limb balance and ankle arthrokinematics in those with chronic ankle instability. J Sport Rehab. 2014;23(1):18–26. doi: 10.1123/jsr.2012-0125. [DOI] [PubMed] [Google Scholar]
- 46.Hoch MC, McKeon PO. Joint mobilization improves spatiotemporal postural control and range of motion in those with chronic ankle instability. J Orthop Res. 2011;29(3):326–332. doi: 10.1002/jor.21256. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.