Abstract
Treatment of Massive rotator cuff tears (MRCT) is difficult, with high rates of retears. Using biological augmentation in the form of the highly vascular subacromial bursa, was used to improve tendon healing. This work aimed to evaluate the results of arthroscopic guided mini-open transosseous repair with bursal augmentation in the treatment of MRCTs in a five-step approach. Forty-eight patients, with a mean age of 63.15 years, were treated with this technique. The patients were evaluated with the constant, UCLA and VAS scores. Plain X-rays were performed to evaluate the CSA and MRI was done to confirm the diagnosis of MRCT and determine the degree of fatty degeneration. Ultrasound was done at 1 year post-operative to determine any retears. The mean follow-up period was 29 months ± 4.95. The Constant and UCLA mean scores improved from (52.52) to (89) and (13.2) to (30.5) respectively (p < 0.0001). The post-operative active flexion and abduction improved from a mean of (112° to 170°) and (136.2° to 167°) respectively, while ER improved from (62.8° to 70°) with their p values (p < 0.0001). Pain improved from a mean VAS of (5.85) to (0.5) (p < 0.0001). No deterioration of function was noted throughout the follow-up period, and no retears occurred on post-operative ultrasound evaluation. Mini-open transosseous repair with bursal augmentation in the treatment of MRCT is an effective and low-cost method that achieves satisfactory results with no retears.
Keywords: Mini-open, Massive rotator cuff tear, Biological bursa
Subject terms: Muscle, Tendons, Outcomes research
Introduction
Massive rotator cuff tears (MRCT) present significant treatment challenges, often leading to a high incidence of recurrent tears post-surgery1–3. The definition of MRCT varies4–6, but Gerber’s classification, which considers the number of tendons involved, is most commonly referenced in the literature7–9. It has been reported that the retear rate following surgical treatment ranges from 17.6 to 94% for large and massive tears2,10–13. Most of these retears occur in the first two years of follow-up, as mentioned in a recent meta-analysis study14. This high failure rate persists despite the introduction of arthroscopic techniques, with studies showing no statistically significant difference in outcomes compared to mini-open repairs15–17. Massive tears may also show varying grades of fatty degeneration which may improve after successful repair indicating that fatty degeneration is not an absolute contraindication for repair18,19. Massive tears compromise the biological healing environment, which may be a major cause of re-rupture. Several methods have been proposed to augment biological healing in MRCT repairs, including Subacromial balloon spacers20, Synthetic and bioengineered grafts21, tendon allograft patch augmentation22, Dermal allografts23, Applying platelet-rich plasma (PRP) over the repair site24, Biceps Tendon Autograft25 and the usage of Subacromial Bursa26–29. The subacromial bursa proved to possess considerable tendon-healing potential which may be owed to its pluripotent stem cells30, extensive blood supply31, which may enhance healing, and its lubricating property, reducing friction over the upper surface of the rotator cuff32. Other benefits include the ease of use and almost no additional expenses.
However, standardized surgical techniques for bursal mobilization, harvesting, and vascularity preservation remain lacking in the literature. .Preoperative imaging can predict the reparability of MRCTs33–35, yet intraoperative assessment of tendon quality and mobility often serves as the definitive determinant1,36–38. There is ongoing debate regarding the necessity of acromioplasty and tenotomy of the long head of the biceps tendon (LHBT) in treating MRCTs, with varying practices reported39–42. Transosseous (TO) repair originally described by McLaughlin in 194443 has been used in arthroscopic and mini-open rotator cuff repair by many authors and proved to be a better option for repair due to their lower cost, better healing interface, and avoidance of the complications regarding anchor failure44. Because most clinical studies in the literature do not present the surgical techniques for MRCT repairs in a step-by-step approach it is difficult for researchers to compare the results. This study aims to evaluate the clinical and radiological outcomes of a mini-open transosseous repair with bursal augmentation in treating MRCTs, and to establish a standardized five-step surgical approach for this technique.
Material
Forty-eight patients with massive rotator cuff tears were treated with our standardized five-step technique of arthroscopic guided mini-open transosseous repair with bursal augmentation. MRCT was defined as involving two or more tendons according to Gerber classification5. Exclusion criteria were designed to ensure a homogeneous sample and remove any associations that may affect function after treatment. They included patients with revision cases, rotator cuff tears associated with neurological lesions, osteoarthritis of the glenohumeral joint classified as grades 2 or 3 by the Samilson-Prieto classification45, rheumatoid arthritis, or postinfectious conditions. These patients were referred to our university hospital after the failure of several months of conservative treatment and had undergone surgery between September 2019 and December 2023.
Ethical consideration
All patients provided informed consent, and the study was conducted in accordance with the Declaration of Helsinki. The experimental protocols were approved by the institutional review board of Cairo University Hospital. The study was also registered on ClinicalTrials.gov with the identifier: NCT06242158.
The study group included (22 men and 26 women) with a mean age of 63.15 years with a range of (53–69) years. Twelve of the patients were diabetics and one was diagnosed with chronic kidney disease that required regular dialysis. Patients were evaluated clinically for the active range of movements of the shoulder in foreword flexion, abduction, and internal and external rotation. The Constant score and University of California-Los Angeles (UCLA) scores were used for functional evaluation. The Constant Score assessed overall shoulder function, incorporating pain, range of motion, strength, and daily activity levels. The UCLA Shoulder Score evaluated pain, function, active range of motion, and patient satisfaction. The Visual Analogue Scale (VAS) score was used to assess pain. An outpatient ultrasound was used to evaluate the condition of the rotator cuff. Standard plain X-rays of the shoulder were performed to assess the Critical shoulder angle (CSA)46. Nineteen (39%) patients had associated type II or III Bigliani acromions. MRI was performed to confirm diagnoses of MRCT (see Fig. 1) and to evaluate the degree of fatty degeneration according to the Goutallier classification47.
Fig. 1.
MRI coronal cut section showing a complete tear of the suprapinatus tendon.
Most of our cases (73%) presented with Collins-type D tears. Regarding fatty degeneration, 36 patients (75%) exhibited grade 1, 2, or 3 fatty degeneration, while only 12 patients (25%) showed no signs of fatty degeneration.
The demographic data are summarized in (Table 1)
Table 1.
Shows the baseline data of the included patients.
| Number of cases | Age (years) | Gender | Side | Dominance | Follow-up period (months) | |||
|---|---|---|---|---|---|---|---|---|
| N = 48 |
63.15 ± 4.38 (53–69) |
Men | 22 | Right | 22 | Dominant | 21 | 29.46 ± 4.95 (24–38) |
| Women | 26 | Left | 26 | Non-dominant | 27 | |||
| Type of tear (Collins classification) | Fatty degeneration (Goutallier) | Bigliani Acromions | Tenotomy or Tenodesis | |||||
|---|---|---|---|---|---|---|---|---|
| A | 6 (12.5%) | 0 | 12 (25%) | Type I | 29 (60.42%) | None | 38 | |
| B | 6 (12.5%) | 1 | 19 (39.58%) | |||||
| C | 1 (2.08%) | 2 | 11 (22.92%) | Type II | 8 (16.67%) | Tenotomy | 8 | |
| D | 35 (72.92%) | 3 | 6 (12.5%) | |||||
| E | 0 | 4 | 0 | Type III | 11 (22.92%) | Tenodesis | 2 | |
Surgical technique
In conjunction with general anesthesia, an interscalene brachial plexus block was given for the operation. Patients were placed in a semisetting position. Conventional posterior, lateral, and anterolateral portals for arthroscopy were used for both glenohumeral and subacromial spaces. The posterior portal was made 2 cm inferior and medial to the posterolateral corner of the acromion. In the same anteroposterior plane as the distal clavicle, the anterolateral portal is situated 2 cm lateral to the distal acromion. Off the anterolateral margin of the acromion, an accessory lateral portal was formed to facilitate instrumentation if necessary.
Surgery was performed in a five-step approach including:
Step one: Identifying the type of tear, if repairable and reducible
A posterior subacromial portal was used to identify the size and quality of the rotator cuff tear. Using a shaver, minimal removal of the bursa and gentle mobilization of the tendon was done. A grasper was then applied to pull the tendon to determine if it was reducible to the footprint area. If the tendon was friable or if the released pulled tendon did not cover more than 50% of the bare bone of the footprint, a shift to tendon transfer surgery would be decided.
Step two: Preparing both the subacromial space and footprint together with identifying the biceps tendon pathology
Acromioplasty, with removing the anterior and lateral part of the acromion was performed in all type II and III Bigliani acromions, to reach a capacious subacromial space in different positions testing shoulder forward flexion and abduction. Minimal removal of the coracoacromial ligament was considered to prevent superior instability together with minimal removal of the anterior deltoid fibers to prevent further detachment when later performing an anterolateral mini-open approach. The LHBT was palpated and mobilized, looking for any signs of degeneration and fraying or instability. The LHBT was inspected either through the tear using the same subacromial portal or through the glenohumeral portal. For patients aged 65 years or older, when indicated, tenotomy was performed close to the origin of the glenoid labrum. For active and younger patients, tenodesis was added using non-absorbable sutures to fix the LHBT to the insertion of the pectoralis major tendon by a separate incision. Lastly, the footprint was prepared with a slow-speed burr.
Step three: Mini open anterolateral surgical approach
An anterolateral mini-open approach was used through a longitudinal 4 cm skin incision aligned with the anterior acromion. Followed by splitting the deltoid muscle between the anterior and middle fibers through the anterolateral raphe. A blunt deltoid retractor was applied, and the involvement and configuration of the torn tendon were confirmed and visualized by rotating the arm in different positions. (see Fig. 2).
Fig. 2.
Photograph showing the exposure of the torn tendon after applying a blunt retractor to retract the deltoid muscle. A Cobb dissector is a useful tool to gently mobilize the tendon to its footprint.
Step four: Transosseous repair of rotator cuff
To ensure even tension distribution, three or four size two FiberWire® sutures were first passed equidistant through the tendon with horizontal stitches used when necessary. The giant needle was then introduced taking one strand of the suture to penetrate the bone at equidistance on the footprint and emerging from the skin, about 5 cm from the tip of the greater tuberosity. Having the shoulder free allows movements of the humerus to help localize the whole bare area according to the anatomical footprints as well as showing any anterosuperior or posterosuperior tears. The sutures passed using the Giant needle were retrieved subdeltoid, superficial to the bursa by a right-angle hook. Before tightening the sutures, the subacromial bursa was mobilized gently from the medial and posterior sides toward the tendon ends. (see Fig. 3-I to IV).
Fig. 3.
I) Photo shows the rotator cuff tear and the subacromial bursa after mobilization; II) Passing the sutures through the tendon and bone then retrieving its end superficial to the bursa; III) Pushing the sliding knot at the lateral side of the humerus so the bursa overlaps the repair; IV) Final coverage of the tendon with the bursa.
Step five: Biological bursa augmentation
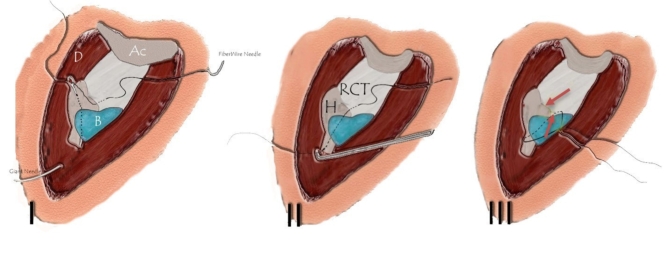
The subacromial bursa was used for biological augmentation of the repair by covering the repaired tendon. Mobilizing the subacromial bursa without jeopardizing its vascular supply is a critical step. The Cobb dissector proved to be a valuable tool, enabling blunt mobilization of the bursa while preserving the supplying vessels. This technique allows the bursa to be advanced from the medial and posterior sides to cover the localized repair site without causing any soft tissue trauma. This was done by pushing the sliding knot at the lateral side of the humerus so the bursa overlaps the repair. The sutures pull the tendon down to the bone and overlap the bursa without additional sutures. (see Fig. 4-I to III)
Fig. 4.
I) Diagram shows passing the FiberWire® through the tendon and then a giant needle is introduced to penetrate the bone with the distal strand of the sutures; II) The suture is pulled subdeltoid superficial to the bursa with a right-angled hook; III) Tightening the knot pushes the bursa to cover the repair without extra sutures. [Ac:Acromion; D:Deltoid; B:Bursa; RCT:Rotator Cuff Tendon; H:Humerus].
Postoperative care routine: Patients were fitted with abduction braces to ensure proper shoulder positioning and immobilization. Starting from the first week postoperatively, patients began passive range-of-motion (ROM) exercises and pendulum exercises to promote joint mobility and reduce stiffness.
At six weeks post-surgery, active-assisted and active free ROM exercises according to the pain tolerance of the patient were allowed. This phase aimed to gradually restore functional movement while avoiding undue stress on the healing tissues.
At three months postoperatively, patients started muscle-strengthening exercises and occupation therapy to return to their original jobs and sports.
Results
The mean follow-up period for the patients was 29 months ± 4.95 with a range between 24 and 38 months. The functional scores, outpatient shoulder ultrasound, and VAS scores were recorded at six, twelve, and twenty-four months post-operatively (see Table 2).
Table 2.
Shows the outcome data of the included patients.
| (VAS) score | Constant score | (UCLA) score | Active Anterior flexion angle degrees | Active abduction degrees | Active external rotation degrees | Active internal rotation degrees | |
|---|---|---|---|---|---|---|---|
| Pre-operative | 5.85 ± 1.3 | 52.52 ± 3.7 | 13.2 ± 3.7 | 112 ± 30 | 136.2 ± 20.4 | 62.8 ± 11 | 56.25 ± 5.78 |
| Post-operative 6 months | 2.18 ± 1.1 | 84.3 ± 3.3 | 26.8 ± 5.8 | 155 ± 28 | 160 ± 18 | 65 ± 6 | 59.27 ± 7.14 |
| Post-operative 12 months | 1 ± 0.66 | 87.6 ± 3.32 | 29.1 ± 4.4 | 168 ± 11 | 167 ± 14 | 69 ± 2 | 71.08 ± 6.4 |
| Post-operative 24 months | 0.5 ± 0.5 | 89 ± 3 | 30.5 ± 5.2 | 170 ± 9 | 167 ± 14 | 70 ± 2 | 71.1 ± 3.1 |
Results showed a mean improvement in Constant score from 52.52 ± 3.7 preoperatively to 89 ± 3 postoperatively, and was statistically significant (p < 0.001), with a 95% confidence interval (CI) for the difference ranging from 34.2 to 38.1. Similarly, the UCLA score improved from 13.2 ± 3.7 to 30.5 ± 5.2 (p < 0.001; 95% CI 16.1–18.3), and the VAS score decreased from 5.85 ± 1.3 to 0.5 ± 0.5 (p < 0.001; 95% CI −5.4 to −4.8).
For range of motion outcomes, active forward flexion improved from 112° ± 30 to 170° ± 9 (p < 0.001; 95% CI 50.3° to 63.8°), abduction from 136.2° ± 20.4 to 167° ± 14 (p < 0.001; 95% CI 26.5° to 37.3°), and external rotation from 62.8° ± 11 to 70° ± 2 (p < 0.001; 95% CI 5.8° to 9.6°). These statistical analyses indicate the significant functional improvements achieved with our technique.
All patients had a good level of internal rotation and could turn the dorsum of the hand to T12 or between their shoulder blades. Patients were able to return to their normal life and activities within an average of 6 months (See Table 2).
All patients showed complete healing with no deterioration of function or retears confirmed by ultrasound evaluation. None of our cases experienced complications such as elbow flexion weakness, deltoid function impairment, or axillary nerve injury after the repair of these massive rotator cuff tears.
Discussion
MRCTs are challenging to treat due to the poor tissue quality, limited healing potential and the high retear rate48. Several surgical techniques have been proposed to address these issues however none of these techniques have shown consistent and satisfactory results, and each has its limitations and complications37. This work presents a novel technique that combines several advantages of different methods while avoiding their drawbacks. This technique of mini-open transosseous repair with bursal augmentation is presented in a standardized five-step approach to be easily reproducible and compared with other studies.
First, we performed arthroscopic identification of the tear and its reparability, which allowed for a precise assessment of the tear size, shape, location, and tissue quality. We did not consider preoperative limited flexion less than 90 degrees as an indication of tendon transfer as recommended by some authors49,50, and agreed with other authors that good results were achieved with successful repair and healing51,52. We did not consider fatty degeneration as an absolute indication for tendon transfer or reversed shoulder arthroplasty. We followed the recommendations of different studies that analyzed the relation between presurgical fatty degeneration of the rotator cuff and retears and showed no statistically significant difference51,53. In our work, the indication for shifting to other salvage procedures was arthroscopic identification of a non-repairable or non-reducible tendon to the footprint. The LHBT was also arthroscopically identified and was sacrificed only in cases with subluxation or dislocation, partial lesions affecting more than 25% of the thickness, or superior labrum lesions of types 2, 3, or 441,42. Intraarticular tenotomy was performed for older patients with limited activities while tenodesis was performed for younger and more active patients. In this study, a total of 8 tenotomies and 2 tenodesis procedures were performed during the repair operation.
Second, we performed acromioplasty only in cases of Bigliani type II and III acromions, with a critical shoulder angle CSA of more than 35 degrees to decrease the re-rupture rates following the current consensus in the literature39,54. A total of 19 (39%) cases either had Bigliani type II or III acromions and underwent acromioplasty during repair. We believe that acromioplasty should be performed selectively and judiciously based on the acromion morphology and the tear characteristics. Special concerns were directed to remove as little as possible of either the coracoacromial ligament or anterior fibers of the Deltoid during acromioplasty to prevent later superior migration of the humeral head or deltoid fibers disruption.
Third, we used an anterolateral longitudinal mini-open approach to access the rotator cuff and perform the repair. This approach proved to be more favorable than the lateral approach as it allowed the identification of all types of tears with anterior or posterior extension55. Also, it preserves the deltoid muscle integrity and reduces the risk of deltoid detachment, by splitting the fibers at the raphe between the anterior and middle fibers.
Fourth, we performed the transosseous repair with a giant needle as described by Fleega56. Because of the large size of the core of the giant needle which may cause injury to the tendon or if there is a need to pass horizontal sutures in atrophied sections, we first passed the needle of the FiberWire® through the tendon side then used the giant needle to penetrate the bone under vision in its appropriate footprint site. Great care was taken not to pinch the long head of the biceps if it was preserved. Also, a meticulous suturing technique ensured smooth and even edges without any wrinkling. We believe that proper pull and direction of the tendon to cover the whole footprint is important for good functional results.
Fifth, we performed biological augmentation of the repair with the subacromial bursa, which is a novel and innovative technique that has not been reported before in MRCTs by a mini-open technique. The exact cause of retear was not fully discussed in the literature; however, trying to augment the repair with biological materials has improved results21–24,26,57. The rationale behind using the subacromial bursa to enhance the healing potential of the rotator cuff can be categorized into three primary functions. First, it serves as a source of mesenchymal stem cells thus creating a favorable environment for tissue regeneration and repair58–61. Second, its vascularity plays a crucial role in the healing process31,62, further supporting the repair process. Third, the bursa’s natural lubricating effect prevents adhesions and minimizes impingement on the acromial surface29,32. By covering the repaired cuff, the bursa reduces friction and shear forces under the acromion, thereby lowering the risk of adhesions and subsequent retears. Additionally, the use of the subacromial bursa as an autologous tissue is cost-effective, eliminating the need for additional graft materials and avoiding the risks associated with allografts or synthetic implants, such as immune reactions or implant failures. Although the use of the subacromial bursa proved to be effective, to our knowledge, the technique of dissection and mobilization either arthroscopic or mini-open was not thoroughly investigated. In this work, we described how to mobilize the bursa from medial and posterior with its blood supply to cover the repaired tendon with minimal sutures.
Patients were followed up for a mean of 29 months and evaluated as regards their clinical outcomes using the Constant-Murley score, the UCLA score, and the visual analog scale for pain and radiologically by shoulder ultrasound. This technique of mini-open transosseous repair with bursal augmentation resulted in significant improvements in pain, function, and range of motion, as well as no retear rates. These results are superior to those reported by previous studies using different techniques for massive RCTs in regards to the rates of retears of functional deterioration during follow-up13,51,63–65. Studies using arthroscopic techniques report retear rates ranging from 17.6 to 94% due to limited healing potential and anchor-related complications2,10–13,66,67. This transosseous repair avoids anchors entirely, eliminating anchor failure as a potential complication, while biological augmentation with the subacromial bursa proved to enhance healing, contributing to the absence of retears in our study. In this study, it was also observed that there was no deterioration of function reaching the final follow-up period. Regarding functional outcomes, our UCLA score improved from 13.2 to 30.5, demonstrating results comparable to those achieved with other techniques for MRCTs, as reported by several authors in the literature11,68–70. Our simpler, cost-effective mini-open approach offers similar outcomes, making it more accessible in resource-limited settings. Incorporating the bursa as biological augmentation in the repair of MRCT holds great potential. The preliminary evidence supports its effectiveness in enhancing tendon healing and improving clinical outcomes. Continued research and clinical trials will be crucial in establishing its role as a standard adjunct in rotator cuff repair surgeries. In our study, all procedures were performed by the same surgical team, led by the senior author, a highly experienced orthopedic surgeon specializing in the treatment of massive rotator cuff tears. This consistency in surgical expertise ensured procedural standardization and minimized variability in outcomes. This study divided the technique into a 5-step technique to be straightforward and reproducible.
This study has some limitations in the form of the lack of a control group. While our results demonstrate significant improvements in functional outcomes and the absence of retears with the mini-open transosseous repair and bursal augmentation technique, a direct comparison with alternative methods would provide stronger evidence for its efficacy. A control group using standard repair techniques, with or without other forms of biological augmentation, could highlight the specific contributions of bursal augmentation to healing and retear prevention. Therefore, further studies with larger cohorts, randomized controlled designs, and longer follow-up periods are needed to confirm the efficacy and safety of this technique. Future research could also explore the incorporation of nanomaterials into the subacromial bursa during augmentation to potentially enhance its regenerative properties71. Diagnosing MRCTs accurately is challenging, particularly regarding classification and factors like tear patterns, tendon quality, and fatty degeneration. Implementing artificial intelligence in imaging could improve diagnostic precision. Finally, postoperative evaluations relied on ultrasound, which, while practical, may lack the sensitivity of MRI for detecting subtle structural changes.
In conclusion, this technique of mini-open transosseous repair with bursal augmentation in the treatment of MRCT is a feasible, safe, and effective method that achieves satisfactory functional outcomes with no retears.
Acknowledgements
Rana Ali Ahmed, Noureldin Mostafa.
Author contributions
YES and AOS were responsible for writing the main manuscript and collecting the data. YES were responsible for analyzing and interpreting the patient data. AOS was responsible for statistical analysis and revising the manuscript. All authors reviewed the manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Data availability
The data supporting the findings of this study are available upon reasonable request from the corresponding author.
Competing interests
The authors declare no competing interests.
Ethical consideration
All patients had undergone informed consent and the study was registered on clinicaltrials.gov with the identifier: NCT06242158.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ardebol, J. et al. A step-by-step approach to arthroscopic repair of massive rotator cuff tears. Arthrosc Tech12, e377–e382. 10.1016/j.eats.2022.11.019 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Galatz, L. M. et al. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am86, 219–224. 10.2106/00004623-200402000-00002 (2004). [DOI] [PubMed] [Google Scholar]
- 3.Di Benedetto, P. et al. Treatment options for massive rotator cuff tears: a narrative review. Acta Biomed92, e2021026. 10.23750/abm.v92iS3.11766 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nobuhara, K., Hata, Y. and Komai, M. Surgical procedure and results of repair of massive tears of the rotator cuff. Clin. Orthop. Relat. Res. 1994, 54–59. [PubMed]
- 5.Gerber, C., Fuchs, B. & Hodler, J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am82, 505–515. 10.2106/00004623-200004000-00006 (2000). [DOI] [PubMed] [Google Scholar]
- 6.Cofield, R. H. Subscapular muscle transposition for repair of chronic rotator cuff tears. Surg Gynecol Obstet154, 667–672 (1982). [PubMed] [Google Scholar]
- 7.Ladermann, A., Denard, P. J. & Collin, P. Massive rotator cuff tears: Definition and treatment. Int Orthop39, 2403–2414. 10.1007/s00264-015-2796-5 (2015). [DOI] [PubMed] [Google Scholar]
- 8.Conaire, E. O. et al. Massive irreparable rotator cuff tears: Which patients will benefit from physiotherapy exercise programs? A narrative review. Int J Environ Res Public Health10.3390/ijerph20075242 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheth, M. M. & Shah, A. A. Massive and irreparable rotator cuff tears: A review of current definitions and concepts. Orthop J Sports Med11, 23259671231154452. 10.1177/23259671231154452 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huijsmans, P. E. et al. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am89, 1248–1257. 10.2106/JBJS.E.00743 (2007). [DOI] [PubMed] [Google Scholar]
- 11.Sugaya, H. et al. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair: A prospective outcome study. J Bone Joint Surg Am89, 953–960. 10.2106/JBJS.F.00512 (2007). [DOI] [PubMed] [Google Scholar]
- 12.Park, J. Y. et al. Does an arthroscopic suture bridge technique maintain repair integrity?: A serial evaluation by ultrasonography. Clin Orthop Relat Res468, 1578–1587. 10.1007/s11999-009-0990-8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paxton, E. S. et al. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: Minimum ten-year follow-up. J Bone Joint Surg Am95, 627–632. 10.2106/JBJS.L.00255 (2013). [DOI] [PubMed] [Google Scholar]
- 14.Longo, U. G. et al. Conservative versus accelerated rehabilitation after rotator cuff repair: A systematic review and meta-analysis. BMC Musculoskelet Disord22, 637. 10.1186/s12891-021-04397-0 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ide, J., Maeda, S. & Takagi, K. A comparison of arthroscopic and open rotator cuff repair. Arthroscopy21, 1090–1098. 10.1016/j.arthro.2005.05.010 (2005). [DOI] [PubMed] [Google Scholar]
- 16.Musil D and Sadovsky P. Massive tears of the rotator cuff--comparison of mini-open and arthroscopic techniques. Part 2. Arthroscopic repair. Acta Chir. Orthop. Traumatol. Cech.74, 318–325 (2007). [PubMed]
- 17.Osti, L. et al. Arthroscopic vs mini-open rotator cuff repair: A quality of life impairment study. Int Orthop34, 389–394. 10.1007/s00264-009-0796-z (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burkhart, S. S. et al. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy23, 347–354. 10.1016/j.arthro.2006.12.012 (2007). [DOI] [PubMed] [Google Scholar]
- 19.Russell, R. D. et al. Structural integrity after rotator cuff repair does not correlate with patient function and pain: A meta-analysis. J Bone Joint Surg Am96, 265–271. 10.2106/JBJS.M.00265 (2014). [DOI] [PubMed] [Google Scholar]
- 20.Dasari, S. P. et al. Subacromial balloon spacer: Indications, rationale, and technique. JBJS Essent Surg Tech12(e21), 00069. 10.2106/JBJS.ST.21.00069 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu, Z. et al. Hydrogel development for rotator cuff repair. Front Bioeng Biotechnol10, 851660. 10.3389/fbioe.2022.851660 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chalmers, P. N. et al. All-arthroscopic patch augmentation of a massive rotator cuff tear: Surgical technique. Arthrosc Tech2, e447-451. 10.1016/j.eats.2013.07.003 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta, A. K. et al. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med40, 141–147. 10.1177/0363546511422795 (2012). [DOI] [PubMed] [Google Scholar]
- 24.Antuna, S. et al. Platelet-rich fibrin in arthroscopic repair of massive rotator cuff tears: A prospective randomized pilot clinical trial. Acta Orthop Belg79, 25–30 (2013). [PubMed] [Google Scholar]
- 25.Endell, D., Ruttershoff, K. & Scheibel, M. Biceps smash technique: Biceps tendon autograft augmentation for arthroscopic rotator cuff reconstruction. Arthrosc Tech12, e383–e386. 10.1016/j.eats.2022.11.020 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freislederer, F., Dittrich, M. & Scheibel, M. Biological augmentation with Subacromial Bursa in arthroscopic rotator cuff repair. Arthrosc Tech8, e741–e747. 10.1016/j.eats.2019.03.010 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steinert, A. F. & Gohlke, F. Editorial commentary: Subacromial bursa-friend or foe within the shoulder? An old debate with new insights. Arthroscopy35, 2989–2991. 10.1016/j.arthro.2019.08.019 (2019). [DOI] [PubMed] [Google Scholar]
- 28.Bhatia, D. N. Arthroscopic bursa-augmented rotator cuff repair: A vasculature-preserving technique for subacromial bursal harvest and tendon augmentation. Arthrosc Tech10, e1203–e1209. 10.1016/j.eats.2021.01.013 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klatte-Schulz, F. et al. Subacromial bursa: A neglected tissue is gaining more and more attention in clinical and experimental research. Cells10.3390/cells11040663 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gregory, J. M. et al. Clinical outcomes of rotator cuff repair with subacromial bursa reimplantation: A retrospective cohort study. JSES Int.7, 763–767. 10.1016/j.jseint.2023.05.010 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Põldoja, E. et al. Blood supply of the subacromial bursa and rotator cuff tendons on the bursal side. Knee Surg Sports Traumatol Arthrosc25, 2041–2046. 10.1007/s00167-016-4379-4 (2017). [DOI] [PubMed] [Google Scholar]
- 32.Funakoshi, T. et al. Distribution of lubricin in the ruptured human rotator cuff and biceps tendon: A pilot study. Clin Orthop Relat Res468, 1588–1599. 10.1007/s11999-009-1108-z (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dwyer, T. et al. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc23, 415–422. 10.1007/s00167-013-2745-z (2015). [DOI] [PubMed] [Google Scholar]
- 34.Kim, J. Y., Park, J. S. & Rhee, Y. G. Can preoperative magnetic resonance imaging predict the reparability of massive rotator cuff tears?. Am J Sports Med45, 1654–1663. 10.1177/0363546517694160 (2017). [DOI] [PubMed] [Google Scholar]
- 35.Yoo, J. C. et al. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy25, 573–582. 10.1016/j.arthro.2008.12.015 (2009). [DOI] [PubMed] [Google Scholar]
- 36.Kaitlyn-Guadagno, U. S., Huish, E. G. Jr. & Best, M. J. Massive rotator cuff tears: Algorithmic approach to surgical treatment. Ann. Joint8, 38. 10.21037/aoj-23-7 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kovacevic, D. et al. Management of irreparable massive rotator cuff tears: A systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg29, 2459–2475. 10.1016/j.jse.2020.07.030 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kany, J. Tendon transfers in rotator-cuff surgery. Orthop Traumatol Surg Res106, S43–S51. 10.1016/j.otsr.2019.05.023 (2020). [DOI] [PubMed] [Google Scholar]
- 39.Milano, G. et al. Arthroscopic rotator cuff repair with and without subacromial decompression: A prospective randomized study. Arthroscopy23, 81–88. 10.1016/j.arthro.2006.10.011 (2007). [DOI] [PubMed] [Google Scholar]
- 40.Waterman, B. R. et al. Randomized trial of arthroscopic rotator cuff with or without acromioplasty: No difference in patient-reported outcomes at long-term follow-up. Arthroscopy37, 3072–3078. 10.1016/j.arthro.2021.04.041 (2021). [DOI] [PubMed] [Google Scholar]
- 41.Malavolta, E. A. et al. Biceps tenotomy or tenodesis in association with rotator cuff repair: is there an influence on functional results? A retrospective cohort study. Sao Paulo Med J140, 237–243. 10.1590/1516-3180.2021.0219.R1.28062021 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Srinivasan, R. C. et al. Outcomes of biceps tenotomy versus tenodesis during arthroscopic rotator cuff repair: An analysis of patients from a large multicenter database. Orthop J Sports Med10.1177/23259671221110851 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McLaughlin, H. L. Lesions of the musculotendinous cuff of the shoulder. The exposure and treatment of tears with retraction. Clin. Orthop. Relat. Res. 1994; 3–9. [PubMed]
- 44.Sanders, B. True transosseous hybrid rotator cuff repair. Arthrosc Tech8, e1013–e1018. 10.1016/j.eats.2019.05.012 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Samilson, R. L. & Prieto, V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am65, 456–460 (1983). [PubMed] [Google Scholar]
- 46.Moor, B. K., Bouaicha, S., Rothenfluh, D. A., et al. Is there an association between the individual anatomy of the scapula and the development of rotator cuff tears or osteoarthritis of the glenohumeral joint?: A radiological study of the critical shoulder angle. Bone Joint J 2013; 95-b: 935–941. 10.1302/0301-620x.95b7.31028. [DOI] [PubMed]
- 47.Goutallier, D., Postel, J. M., Bernageau, J., et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994: 78–83. [PubMed]
- 48.Kucirek, N. K., Hung, N. J. & Wong, S. E. Treatment options for massive irreparable rotator cuff tears. Curr Rev Musculoskelet Med14, 304–315. 10.1007/s12178-021-09714-7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahmed, A. F. et al. Tendon transfers in rotator cuff deficiency. Oper. Tech. Sports Med.31, 150986. 10.1016/j.otsm.2023.150986 (2023). [Google Scholar]
- 50.Collin, P. et al. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg23, 1195–1202. 10.1016/j.jse.2013.11.019 (2014). [DOI] [PubMed] [Google Scholar]
- 51.Yokoya, S. et al. Outcomes of arthroscopic rotator cuff repair with muscle advancement for massive rotator cuff tears. J Shoulder Elbow Surg28, 445–452. 10.1016/j.jse.2018.08.038 (2019). [DOI] [PubMed] [Google Scholar]
- 52.Denard, P. J. et al. Pseudoparalysis from a massive rotator cuff tear is reliably reversed with an arthroscopic rotator cuff repair in patients without preoperative glenohumeral arthritis. Am J Sports Med43, 2373–2378. 10.1177/0363546515597486 (2015). [DOI] [PubMed] [Google Scholar]
- 53.Cho, N. S. & Rhee, Y. G. The factors affecting the clinical outcome and integrity of arthroscopically repaired rotator cuff tears of the shoulder. Clin Orthop Surg1, 96–104. 10.4055/cios.2009.1.2.96 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meissner-Haecker, A. et al. Critical shoulder angle and failure of conservative treatment in patients with atraumatic full thickness rotator cuff tears. BMC Musculoskelet Disord23, 561. 10.1186/s12891-022-05519-y (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cho, C. H. et al. Anterolateral approach for mini-open rotator cuff repair. Int Orthop36, 95–100. 10.1007/s00264-011-1305-8 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fleega, B. A. Arthroscopic transhumeral rotator cuff repair: Giant needle technique. Arthroscopy18, 218–223. 10.1053/jars.2002.30661 (2002). [DOI] [PubMed] [Google Scholar]
- 57.Guler, Y. et al. Arthroscopic biological augmentation with Subacromial Bursa for bursal-sided partial-thickness rotator cuff tears. Orthop J Sports Med10.1177/23259671231190335 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Steinert, A. F. et al. Characterization of bursa subacromialis-derived mesenchymal stem cells. Stem Cell Res Ther6, 114. 10.1186/s13287-015-0104-3 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morikawa, D. et al. Comparison of preparation techniques for isolating Subacromial Bursa-derived cells as a potential augment for rotator cuff repair. Arthroscopy36, 80–85. 10.1016/j.arthro.2019.07.024 (2020). [DOI] [PubMed] [Google Scholar]
- 60.Uhthoff, H. K., Sarkar, K. Surgical repair of rotator cuff ruptures. The importance of the subacromial bursa. J. Bone Joint Surg. Br. 1991; 73: 399–401. 10.1302/0301-620X.73B3.1670436. [DOI] [PubMed]
- 61.Dyrna, F. et al. Human subacromial bursal cells display superior engraftment versus bone marrow stromal cells in murine tendon repair. Am J Sports Med46, 3511–3520. 10.1177/0363546518802842 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marshall, B. P., Levine, W. N. & Thomopoulos, S. The role of the subacromial bursa in rotator cuff healing: friend or foe?. J Bone Joint Surg Am105, 417–425. 10.2106/jbjs.22.00680 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Konig, M. A. & Braunstein, V. A. Tendon repair leads to better long-term clinical outcome than debridement in massive rotator cuff tears. Open Orthop J11, 546–553. 10.2174/1874325001611010546 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zumstein, M. A. et al. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am90, 2423–2431. 10.2106/JBJS.G.00677 (2008). [DOI] [PubMed] [Google Scholar]
- 65.Collin, P. et al. Clinical and structural outcome 20 years after repair of massive rotator cuff tears. J Shoulder Elbow Surg29, 521–526. 10.1016/j.jse.2019.07.031 (2020). [DOI] [PubMed] [Google Scholar]
- 66.Kim, J., Ryu, Y. & Kim, S. H. Surgical options for failed rotator cuff repair, except arthroplasty: Review of current methods. Clin Shoulder Elb23, 48–58. 10.5397/cise.2019.00416 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cummins, C. A. & Murrell, G. A. C. Mode of failure for rotator cuff repair with suture anchors identified at revision surgery. J. Shoulder Elbow Surg.12, 128–133. 10.1067/mse.2003.21 (2003). [DOI] [PubMed] [Google Scholar]
- 68.Denard, P. J. et al. Long-term outcome of arthroscopic massive rotator cuff repair: The importance of double-row fixation. Arthroscopy28, 909–915. 10.1016/j.arthro.2011.12.007 (2012). [DOI] [PubMed] [Google Scholar]
- 69.Papadopoulos, P. et al. Functional outcome and structural integrity following mini-open repair of large and massive rotator cuff tears: A 3–5 year follow-up study. J Shoulder Elbow Surg20, 131–137. 10.1016/j.jse.2010.05.026 (2011). [DOI] [PubMed] [Google Scholar]
- 70.Rush, L. N., Savoie, F. H. & Itoi, E. Double-row rotator cuff repair yields improved tendon structural integrity, but no difference in clinical outcomes compared with single-row and triple-row repair: A systematic review. Journal of ISAKOS2, 260–268. 10.1136/jisakos-2016-000069 (2017). [Google Scholar]
- 71.Hao, X. et al. Nanomaterials for bone metastasis. J Control Release373, 640–651. 10.1016/j.jconrel.2024.07.067 (2024). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available upon reasonable request from the corresponding author.