Abstract
Background: Age-related decline in musculoskeletal function is a significant concern, particularly in Western countries facing demographic shifts and increased healthcare demands. This review examines the typical trajectories of musculoskeletal deterioration with age and evaluates the effectiveness of various interventions in preventing or reversing these changes. Methods: The review analyzes documented rates of decline across multiple parameters, including muscle mass, Type II muscle fiber reduction, and decreased motor unit firing rates. It examines evidence from studies on targeted interventions aimed at reversing these trends or preventing further decline. Results: The evidence suggests that multimodal interventions, including strength training can effectively maintain or improve physical function in aging adults. These interventions have shown potential in altering the trajectory of age-related decline in musculoskeletal function. Conclusions. The findings of this review have important implications for healthcare providers and policymakers in addressing the challenges of an aging population. By providing a framework for understanding and addressing age-related physical decline through evidence-based interventions, this review offers potential strategies for reducing healthcare costs and improving the quality of life for older adults.
Keywords: healthy aging, physical performance tests, cognitive function, metabolic health, longevity interventions, cardiovascular fitness, musculoskeletal strength, quality of life in older people
1. Introduction
Aging typically is associated with decreases in musculoskeletal function, which results in greater degrees of physical disability, injury risk, and is associated with increased mortality [1]. Presently, Western countries are composed of a large proportion of older adults, who will be entering retirement. The economic implications of the upward shift in the average age is a commonly discussed issue [2,3,4], especially given that healthcare spending is heavily skewed towards end-of-life care [5]. For greater independence and health in the older population, it pays dividends to start interventions early, including physical and cognitive interventions. This review focuses on the musculoskeletal parameters which typically worsen with age, and how the magnitude of the expected decline compares with what can be achieved through modest interventions.
2. The Effect of Aging on Physical Capacity
Age-related declines in physical functioning are thought to be quite ubiquitous. Age-related decline in muscle mass occurs throughout the lifespan, at 0.37% per year in women and 0.47% per year in men [6]. This loss occurs mostly in Type II fast-twitch fibers, while Type I fibers are mostly maintained [7]. Protein synthesis rates also decrease with age [8]. Besides the important loss in strength, muscle mass also influences metabolism, and lower muscle mass has negative effects on metabolism.
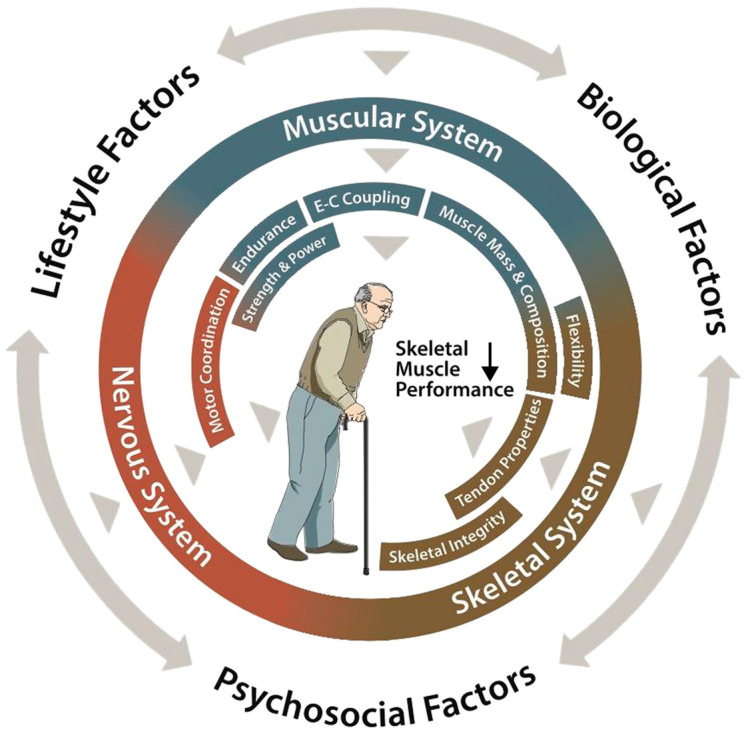
The skeletal system undergoes parallel deterioration, with decreasing bone mineral density and structural changes in the tendons and connective tissues [9] (see Figure 1). The tendons become less stiff and show decreased mechanical properties, affecting their ability to transfer force effectively from muscles to bones.
Figure 1.
Declining skeletal muscle performance in older people. Diagram by Tim Goheen, Associate Professor, Ohio University School of Visual Communication. Reproduced from [9] under a CC BY-NC 4.0 license (https://creativecommons.org/licenses/by-nc/4.0/, accessed on December 10, 2024).
The expected trends in the musculoskeletal system with aging are shown in Table 1. These trends show a gradual decline in the functional and structural parameters of muscle, bone, and tendon as aging progresses [9]. In addition, a limited number of these parameters are predictive of the lifespan, which suggests that they are associated with overall health.
For healthy aging, changes made early on can have significant impacts later on in life, especially if they are long-term changes in habits and practices, instead of short-term changes. Physical fitness, including musculoskeletal strength and integrity, is important in old age, as this enables older people to retain independence for longer, to have better overall health, to experience fewer accidents, and to recover quickly from injuries [10].
Falls are one example where physical fitness can mean the difference between life and death. The mortality after hip fractures in older adults varies from approximately 10% [11] up to about 35% [12,13,14]. Fitness can improve the dynamic balance and lower limb strength, which allows people to maintain balance in potential fall scenarios [15].
Table 1.
Trends in musculoskeletal parameters with increasing age and corresponding interventions for improving musculoskeletal parameters.
| System | Component | Changes | Rate/Magnitude | Association with Healthspan/QOL Measures | Intervention | Magnitude of Change | Mechanism of Adaptation |
|---|---|---|---|---|---|---|---|
| Muscular System | Muscle Mass | Overall muscle mass decline | Women: 0.37%/year Men: 0.47%/year Over 75 years: Women: 0.64–0.70%/year Men: 0.80–0.98%/year [6] |
Correlation between thigh muscle area and telomere length [16] Association of appendicular lean mass normalized to body mass index and 10-year health-related quality of life [17] Muscle mass not associated with overall quality of life [18,19] Muscle mass correlated with physical vitality, emotional functioning, and physical functioning in older breast cancer survivors [20] |
Strength training (2× per week for 24 weeks) | 3.8% [1.6%, 6.1%] increase in bone mineral-free lean tissue mass [21] | Activation of anabolic pathways [22] Satellite cell activation [23] Hormonal response [24] |
| Muscle Fibers | Type II (fast twitch) fiber reduction | 10–40% reduction in Type II fiber size [25] | In animal models, Type II muscle fibers help to regulate glucose metabolism [26] | Resistance training 3× per week for 12 weeks | 28% increase in area [27] | ||
| Type I (slow twitch) preservation | Decrease is much slower than for Type II [28] | Resistance training 3× per week for 12 weeks | Non-significant increase in Type I muscle fiber size [27] | ||||
| Muscle Function | Reduced force per unit area | Strong association between grip strength and mortality risk [29] Grip strength associated with level of independence in old age [30,31] |
Leg press trained 3× per week for 12 weeks | 22% increase in leg press power [32] | |||
| Reduced motor unit firing | Maximum voluntary contraction (MVC) decreases by ~50 points or 9% per decade [33] Maximum firing rate 30–35% lower in older adults [34] |
6 weeks of resistance exercise | Maximal motor unit discharge rates were 49% higher for the older adults [35] | Increase in neural drive from CNS to activate muscle fibers [36] | |||
| 6 to 12 weeks of resistance training | Voluntary activation of knee extensors increased 1.8% following resistance training [37] | ||||||
| Impaired calcium handling | 33% reduction in calcium reuptake [38] | Unknown | Selenium supplementation and training | Improvement in calcium release in older mice [39] | Effect mediated through ryanodine receptor [39] and selenoprotein N [40] | ||
| Acute exercise training | Improvements in calcium release rate [41] | Modification of calcitropic hormone levels [42] | |||||
| 12 weeks of high-resistance strength training | Partial reversal of reduction in sarcoplasmic reticulum Ca 2+ uptake in skeletal muscle [38]. | ||||||
| Muscle Quality | Increased fat infiltration | Non-contractile area in leg anterior compartment approximately 2.5-fold larger in older subjects than in young subjects [43,44] | Arm fat mass index association with increased non-cardiovascular mortality [45] Low fat mass and high muscle mass associated with a 62% [32%,78%] decrease in total mortality [46] Skeletal muscle fat infiltration associated with higher all-cause and cardiovascular mortality [47] |
12-week resistance training program | 11% decrease in thigh intramuscular adipose tissue [48] | Increases fatty acid oxidation [49] Improves insulin sensitivity [50] Reduces adipogenic signaling [51] |
|
| High-effort single-set exercise training 2×/week for 16 months | Fat infiltration stable in exercise group but increased in control group [52] | ||||||
| Greater fibrosis | Increase in tissue fibrosis observed in aging mouse model [53] Increase in muscle fibrosis biomarkers in humans [54] | Metformin | Lowered biomarkers of muscle fibrosis [55] | Inhibits TGF-β1 signaling, alters fate of myofibroblasts [56] | |||
| Nintedanib | Decreased expression of fibrotic genes [57] | Reduces proliferation and migration of fibroblasts [57], downregulation of extracellular matrix production [57], interference with profibrotic signaling [58] | |||||
| Resistance training and Dioscorea esculenta | Circulating levels of C1q, a biomarker associated with fibrosis, lower in experimental group [59] | Lowers C1q [59] | |||||
| Losartan | Decreases fibrosis and fibrotic biomarkers in animal models [60] | Interferes with TGF-β1 signaling [61] | |||||
| Suramin | Decreases fibrosis in animal models [60] | Reduces TGF-β signaling [62] | |||||
| Decorin | Decreases fibrosis in animal models [60] | Inhibits TGF-β [63] | |||||
| Halofuginone | Decreases fibrosis in animal models [60] | Inhibits collagen synthesis [64] | |||||
| Reduced sensitivity to anabolic stimuli | Decreased muscle protein synthesis after insulin infusion in older people compared to younger people [65] | N/A | Leucine | Leucine supplementation stimulates muscle protein synthesis [66] | Potent stimulator of mTORC1 and protein synthesis [67] | ||
| High protein intake | Doubling the recommended daily intake of protein increased muscle protein synthesis by 19% [68] | Increasing muscle protein synthesis [69] | |||||
| Pennation angle | Decrease in pennation angle | 4% decline per decade in vastus lateralis pennation angle [70] | No direct correlation, but pennation angle is correlated with age with r = −0.50 [70] | Leg press training for 10 weeks | 30% increase in pennation angle of vastus lateralis (VL) muscle [71] | Remodeling [72] | |
| Mitochondrial number | Decrease with age | Older participants (71+/−2 years) have 57% reduction in mitochondria compared to younger individuals (23+/−2 years) or 1.74% reduction per year. [73] | Association with VO2 max [74] | 30 to 60 min 3× per week for 4 months at moderate intensity (75% of maximum heartrate) | Increase in muscle mitochondrial density by 50.7% in exercise group [75] | Increases muscle GLUT−4 levels and insulin action [76,77] | |
| Energy expenditure at rest | Decreased basal metabolic rate | 4% decline per decade after 50 years of age [53,78] | Genetically predicted basal metabolic rate negatively associated with lifespan [79] | Fish oil with resistance training | Significant increase in resting metabolic rate [80] | Increases in the phosphorylation status of kinases related to the mTORC-1 signaling, increased muscle mass [81] | |
| Nutritional consultation and physical training | Increase in RMR [82] | Maximizes muscle protein synthesis (MPS) through the activation of mammalian target of rapamycin (mTOR) [83] | |||||
| Skeletal System | Bone Structure | Accelerated bone mineral density loss | Cortical zone in upper femoral neck declined by 6.4% per decade [84] | One standard deviation difference in bone mineral density is associated with a 1.39-fold increase in mortality [85] 1 SD increase in total hip BMD associated with a 0.77 [0.61,0.91] relative risk of overall mortality [86] |
Physical exercise program | No decrease in bone mineral density of exercise group, decrease of 1.1% [0.1%,2.1%] in control group [87] | Activating mTORC1 and Mitogen-active protein kinases signaling for growth, repair, and adaptation [88] |
| Elastic modulus | 2.3% reduction per decade of life past age 35 [89] | Unknown | N/A | N/A | |||
| Bone strength | Reduction by 3.7% each decade after age 35 [89] | Unknown | Physical exercise | Reduction in fracture risk by 51% in the exercise group [90] | |||
| Fracture toughness | Kc: 4.1% reduction per decade after age 35 [89] | Unknown | |||||
| Work of fracture | 8.7% reduction per decade after age 35 [89] | Unknown | |||||
| Tendons | Reduced stiffness | Decreased maximum shortening velocity of tendons between older (75 years) and younger (20 years) adults by 16% [91] | Unknown | 14 weeks of high-load resistance training | Increase in tendon stiffness by 65% [92,93] | Tendon hypertrophy [94,95] | |
| Decreased shock absorption | F20 of occiput (inverse proxy for shock absorption capacity) roughly doubles between third and fifth decade of life, and between the fifth and seventh decade of life [96] | Decreased shock absorption capacity may contribute to greater risk from falls [97] | 14 weeks of high-load resistance training | Tendon Young’s modulus increased by 69% [92,93] | |||
| Function | Flexibility | 5–6 degree decline per decade in shoulder abduction [98] | Not associated with mortality [99]. | Dynamic and static stretching exercises for 12 weeks | Sit and reach test improvement by 23 +/−10% [100] | Stretching promotes the addition of sarcomeres in series, increasing the functional length of muscle fibers and improving the ability to generate an extended ROM [101], improved muscle–tendon unit (MTU) compliance [102,103] |
3. Interventions for Improving the Aging Musculoskeletal System
Resistance training produces many important benefits for aging bodies, across a wide degree of systems, organs, and tissue types. Some training specificity may be necessary to target certain parameters, though the benefits of resistance training manifest across a wide variety of training regimens. Table 1 includes interventions that can improve the musculoskeletal parameters that secularly decline with age, and the magnitude of their impact.
In Table 2, we include four aspects of fitness that are helpful for older people and where the secular trend declines with aging. These may also be assessed using either biomarker- or function-based tests, and training interventions prescribed accordingly.
Table 2.
Intervention classes for maintaining physical function with age and means of training.
| Training Type | Trend (Absent Training) | System | Associated Tests | Training | Adaptations |
|---|---|---|---|---|---|
| Strength Training | Sarcopenia, muscle loss, bone loss | Musculoskeletal | Grip strength [104] | Weightlifting | Increase in muscle mass and bone density |
| Endurance training | Lower VO2 max | Metabolic, cardiopulmonary | Resting metabolic rate, creatine phosphokinase [105] |
Running, swimming, walking, cycling, cross-country skiing, hiking, etc. | Increased mitochondrial size, greater ability to metabolize fat, increased (heart) stroke volume |
| Balance training | Poorer coordination | Musculoskeletal, nervous | Self-selected gait velocity [106], chair rise test (timed 5 chair rises), tandem standing and walking, timed up and go test, clinical gait analysis with special focus on regularity, mechanography [107] | Yoga | Neuromuscular control [108] |
| Flexibility | Decrease in joint flexion [98,109] | Musculoskeletal, tendons, fascia | Flexibility tests: Flexindex [109] | Yoga, pilates | Improved flexibility and stability [110] |
Adaptation to interventions (including physical training) is characterized by a wide range of molecular mechanisms (Table 1). For certain parameters like strength, the value can be improved through multiple mechanisms, including nervous system adaptations as well as hypertrophy of the relevant muscles [22]. Other aspects of fitness which this article has only briefly covered include endurance training, balance training, and flexibility. Endurance training can be important for developing cardiorespiratory fitness, which is highly associated with lifespan [111]. Balance training is important in the context of fall prevention, which can carry a significant mortality risk for older people [112]. Flexibility is associated with functional ability in adults [113]. Overall, the fitness level is associated with greater independence and capability into old age.
4. Conclusions
This review demonstrates how the trajectory of age-related physical decline can be improved through targeted interventions. Research shows meaningful improvements across various physiological parameters when using multiple strategies, from resistance training to nutritional optimization. Physical exercise has demonstrated remarkable effects on both muscular and skeletal health, while proper nutrition supports muscle synthesis and overall function.
The integration of functional and biomarker testing with personalized interventions offers a practical framework for promoting healthy aging. This approach is particularly relevant given the growing demographic of older adults in Western societies and their associated healthcare challenges. Looking ahead, there is a clear need for continued research to refine these interventions and explore their synergistic effects.
Healthcare providers and policymakers can leverage these insights to test adults for their physical capacities and prescribe training programs to bring up the parameter values, which will result in greater health outcomes. People are more likely to follow an individualized program than a generic program, more so than vague advice to ‘eat right’ and ‘move more’ [114,115]. These training programs can be used with a wearable device, which allows for gamification, accountability, and allows for the monitoring of progress [116], as well as the development of more effective programs supporting healthy aging, potentially reducing the burden of age-related chronic diseases and associated healthcare costs. Through the systematic application of these findings, we can work toward a future where aging is characterized by maintained functionality and enhanced quality of life rather than decline.
While this review has focused mostly on physical interventions, other interventions, such as nutritional supplementation and novel therapeutics practices, may also be of interest, especially as they may reduce the time taken to engage in a program designed to decrease the rate of decline in musculoskeletal function with age. The potential limitations of this approach are that older people may not have access to a gym, but many exercise interventions can be performed with minimal or no equipment. Furthermore, this study relies on the findings in the cited studies being robust, which is a challenge inherent to providing guidelines based on clinical research.
Additionally, examining the impact of interventions and the association between musculoskeletal parameters and healthspan or, inversely, mortality. Each intervention creates a change in the expected trend for an aging person, which can improve health outcomes. This can further be extrapolated to financial costs and may alleviate the cost of old-age care.
Acknowledgments
A preprint version of this article exists in [117].
Author Contributions
Conceptualization, M.H. and P.M.; methodology, M.H.; validation, M.H., P.M., and J.T.; investigation, M.H.; writing—original draft preparation, M.H.; writing—review and editing, M.H., P.M., J.V., and J.T. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding Statement
The Article Processing Charge was funded by the Frontline COVID-19 Critical Care Alliance.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Trombetti A., Reid K.F., Hars M., Herrmann F.R., Pasha E., Phillips E.M., Fielding R.A. Age-Associated Declines in Muscle Mass, Strength, Power, and Physical Performance: Impact on Fear of Falling and Quality of Life. Osteoporos. Int. 2016;27:463–471. doi: 10.1007/s00198-015-3236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho D., Lee K. Population Aging and Fiscal Sustainability: Nonlinear Evidence from Europe. J. Int. Money Financ. 2022;126:102665. doi: 10.1016/j.jimonfin.2022.102665. [DOI] [Google Scholar]
- 3.Cristea M., Noja G.G., Stefea P., Sala A.L. The Impact of Population Aging and Public Health Support on EU Labor Markets. Int. J. Environ. Res. Public Health. 2020;17:1439. doi: 10.3390/ijerph17041439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Žokalj M. The Impact of Population Aging on Public Finance in the European Union. Financ. Theory Pract. 2016;40:383–412. doi: 10.3326/fintp.40.4.2. [DOI] [Google Scholar]
- 5.Zhang Y., Gupta A., Nicholson S., Li J. Elevated End-of-Life Spending: A New Measure of Potentially Wasteful Health Care Spending at the End of Life. Health Serv. Res. 2023;58:186–194. doi: 10.1111/1475-6773.14093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell W.K., Williams J., Atherton P., Larvin M., Lund J., Narici M. Sarcopenia, Dynapenia, and the Impact of Advancing Age on Human Skeletal Muscle Size and Strength; a Quantitative Review. Front. Physiol. 2012;3:260. doi: 10.3389/fphys.2012.00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martel G.F., Roth S.M., Ivey F.M., Lemmer J.T., Tracy B.L., Hurlbut D.E., Metter E.J., Hurley B.F., Rogers M.A. Age and Sex Affect Human Muscle Fibre Adaptations to Heavy-Resistance Strength Training. Exp. Physiol. 2006;91:457–464. doi: 10.1113/expphysiol.2005.032771. [DOI] [PubMed] [Google Scholar]
- 8.Koopman R., van Loon L.J.C. Aging, Exercise, and Muscle Protein Metabolism. J. Appl. Physiol. 2009;106:2040–2048. doi: 10.1152/japplphysiol.91551.2008. [DOI] [PubMed] [Google Scholar]
- 9.Tieland M., Trouwborst I., Clark B.C. Skeletal Muscle Performance and Ageing. J. Cachexia Sarcopenia Muscle. 2018;9:3–19. doi: 10.1002/jcsm.12238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miri S., Farhadi B., Takasi P., Ghorbani Vajargah P., Karkhah S. Physical Independence and Related Factors among Older Adults: A Systematic Review and Meta-Analysis. Ann. Med. Surg. 2024;86:3400. doi: 10.1097/MS9.0000000000002100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Raichandani K., Agarwal S., Jain H., Bharwani N. Mortality Profile after 2 Years of Hip Fractures in Elderly Patients Treated with Early Surgery. J. Clin. Orthop. Trauma. 2021;18:1–5. doi: 10.1016/j.jcot.2021.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee A., Xi I.L., Ahn J., Bernstein J. Median Survival Following Geriatric Hip Fracture among 17,868 Males from the Veterans Health Administration. Front. Surg. 2023;10:1090680. doi: 10.3389/fsurg.2023.1090680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu E., Killington M., Cameron I.D., Li R., Kurrle S., Crotty M. Life Expectancy of Older People Living in Aged Care Facilities after a Hip Fracture. Sci. Rep. 2021;11:20266. doi: 10.1038/s41598-021-99685-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morri M., Ambrosi E., Chiari P., Orlandi Magli A., Gazineo D., D’ Alessandro F., Forni C. One-Year Mortality after Hip Fracture Surgery and Prognostic Factors: A Prospective Cohort Study. Sci. Rep. 2019;9:18718. doi: 10.1038/s41598-019-55196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sadaqa M., Németh Z., Makai A., Prémusz V., Hock M. Effectiveness of Exercise Interventions on Fall Prevention in Ambulatory Community-Dwelling Older Adults: A Systematic Review with Narrative Synthesis. Front. Public Health. 2023;11:1209319. doi: 10.3389/fpubh.2023.1209319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques A., Peralta M., Marconcin P., Henriques-Neto D., Gouveia É.R., Ferrari G., Martins J., Sarmento H., Ihle A. A Systematic Review of the Association Between Muscular Fitness and Telomere Length Across the Adult Lifespan. Front. Physiol. 2021;12:706189. doi: 10.3389/fphys.2021.706189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balogun S., Winzenberg T., Wills K., Scott D., Jones G., Callisaya M.L., Aitken D. Prospective Associations of Low Muscle Mass and Strength with Health-Related Quality of Life over 10-Year in Community-Dwelling Older Adults. Exp. Gerontol. 2019;118:65–71. doi: 10.1016/j.exger.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 18.da Costa Pereira J.P., Freire Y.A., da Silva A.M.B., de Lucena Alves C.P., de Melo Silva R., Câmara M., Browne R.A.V., Costa E.C., Trussardi Fayh A.P. Associations of Upper- and Lower-Limb Muscle Strength, Mass, and Quality with Health-Related Quality of Life in Community-Dwelling Older Adults. Geriatr. Gerontol. Int. 2024;24:683–692. doi: 10.1111/ggi.14912. [DOI] [PubMed] [Google Scholar]
- 19.Haider S., Luger E., Kapan A., Titze S., Lackinger C., Schindler K.E., Dorner T.E. Associations between Daily Physical Activity, Handgrip Strength, Muscle Mass, Physical Performance and Quality of Life in Prefrail and Frail Community-Dwelling Older Adults. Qual. Life Res. 2016;25:3129–3138. doi: 10.1007/s11136-016-1349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morishita S., Kasahara R., Yamamoto Y., Jinbo R., Takano A., Yasuda M., Tsubaki A., Aoki O., Fu J.B., Tsuji T. Differences in the Relationships Between Muscle Strength, Muscle Mass, Balance Function, and Quality of Life for Middle-Aged and Older Breast Cancer Survivors. Integr. Cancer Ther. 2022;21:15347354221138574. doi: 10.1177/15347354221138574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taaffe D.R., Duret C., Wheeler S., Marcus R. Once-Weekly Resistance Exercise Improves Muscle Strength and Neuromuscular Performance in Older Adults. J. Am. Geriatr. Soc. 1999;47:1208–1214. doi: 10.1111/j.1532-5415.1999.tb05201.x. [DOI] [PubMed] [Google Scholar]
- 22.Schiaffino S., Reggiani C., Akimoto T., Blaauw B. Molecular Mechanisms of Skeletal Muscle Hypertrophy. J. Neuromuscul. Dis. 2021;8:169–183. doi: 10.3233/JND-200568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kadi F., Charifi N., Denis C., Lexell J., Andersen J.L., Schjerling P., Olsen S., Kjaer M. The Behaviour of Satellite Cells in Response to Exercise: What Have We Learned from Human Studies? Pflug. Arch.-Eur. J. Physiol. 2005;451:319–327. doi: 10.1007/s00424-005-1406-6. [DOI] [PubMed] [Google Scholar]
- 24.Schoenfeld B.J. The Mechanisms of Muscle Hypertrophy and Their Application to Resistance Training. J. Strength Cond. Res. 2010;24:2857. doi: 10.1519/JSC.0b013e3181e840f3. [DOI] [PubMed] [Google Scholar]
- 25.Nilwik R., Snijders T., Leenders M., Groen B.B., van Kranenburg J., Verdijk L.B., van Loon L.J.C. The Decline in Skeletal Muscle Mass with Aging Is Mainly Attributed to a Reduction in Type II Muscle Fiber Size. Exp. Gerontol. 2013;48:492–498. doi: 10.1016/j.exger.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Castorena C.M., Arias E.B., Sharma N., Bogan J.S., Cartee G.D. Fiber Type Effects on Contraction-Stimulated Glucose Uptake and GLUT4 Abundance in Single Fibers from Rat Skeletal Muscle. Am. J. Physiol. Endocrinol. Metab. 2015;308:E223–E230. doi: 10.1152/ajpendo.00466.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kryger A.I., Andersen J.L. Resistance Training in the Oldest Old: Consequences for Muscle Strength, Fiber Types, Fiber Size, and MHC Isoforms. Scand. J. Med. Sci. Sports. 2007;17:422–430. doi: 10.1111/j.1600-0838.2006.00575.x. [DOI] [PubMed] [Google Scholar]
- 28.Miljkovic N., Lim J.-Y., Miljkovic I., Frontera W.R. Aging of Skeletal Muscle Fibers. Ann. Rehabil. Med. 2015;39:155–162. doi: 10.5535/arm.2015.39.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Leong D.P., Teo K.K., Rangarajan S., Lopez-Jaramillo P., Avezum A., Orlandini A., Seron P., Ahmed S.H., Rosengren A., Kelishadi R., et al. Prognostic Value of Grip Strength: Findings from the Prospective Urban Rural Epidemiology (PURE) Study. Lancet. 2015;386:266–273. doi: 10.1016/S0140-6736(14)62000-6. [DOI] [PubMed] [Google Scholar]
- 30.Carson R.G. Get a Grip: Individual Variations in Grip Strength Are a Marker of Brain Health. Neurobiol. Aging. 2018;71:189–222. doi: 10.1016/j.neurobiolaging.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 31.Rantanen T., Guralnik J.M., Foley D., Masaki K., Leveille S., Curb J.D., White L. Midlife Hand Grip Strength as a Predictor of Old Age Disability. JAMA. 1999;281:558–560. doi: 10.1001/jama.281.6.558. [DOI] [PubMed] [Google Scholar]
- 32.Earles D.R., Judge J.O., Gunnarsson O.T. Velocity Training Induces Power-Specific Adaptations in Highly Functioning Older Adults. Arch. Phys. Med. Rehabil. 2001;82:872–878. doi: 10.1053/apmr.2001.23838. [DOI] [PubMed] [Google Scholar]
- 33.Ling S.M., Conwit R.A., Ferrucci L., Metter E.J. Age-Associated Changes in Motor Unit Physiology: Observations from the Baltimore Longitudinal Study of Aging. Arch. Phys. Med. Rehabil. 2009;90:1237–1240. doi: 10.1016/j.apmr.2008.09.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kamen G., Sison S.V., Du C.C., Patten C. Motor Unit Discharge Behavior in Older Adults during Maximal-Effort Contractions. J. Appl. Physiol. 1995;79:1908–1913. doi: 10.1152/jappl.1995.79.6.1908. [DOI] [PubMed] [Google Scholar]
- 35.Kamen G., Knight C.A. Training-Related Adaptations in Motor Unit Discharge Rate in Young and Older Adults. J. Gerontol. Ser. A. 2004;59:1334–1338. doi: 10.1093/gerona/59.12.1334. [DOI] [PubMed] [Google Scholar]
- 36.Gabriel D.A., Kamen G., Frost G. Neural Adaptations to Resistive Exercise: Mechanisms and Recommendations for Training Practices. Sports Med. 2006;36:133–149. doi: 10.2165/00007256-200636020-00004. [DOI] [PubMed] [Google Scholar]
- 37.Arnold P., Bautmans I. The Influence of Strength Training on Muscle Activation in Elderly Persons: A Systematic Review and Meta-Analysis. Exp. Gerontol. 2014;58:58–68. doi: 10.1016/j.exger.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 38.Hunter S.K., Thompson M.W., Ruell P.A., Harmer A.R., Thom J.M., Gwinn T.H., Adams R.D. Human Skeletal Sarcoplasmic Reticulum Ca2+ Uptake and Muscle Function with Aging and Strength Training. J. Appl. Physiol. 1999;86:1858–1865. doi: 10.1152/jappl.1999.86.6.1858. [DOI] [PubMed] [Google Scholar]
- 39.Fodor J., Al-Gaadi D., Czirják T., Oláh T., Dienes B., Csernoch L., Szentesi P. Improved Calcium Homeostasis and Force by Selenium Treatment and Training in Aged Mouse Skeletal Muscle. Sci. Rep. 2020;10:1707. doi: 10.1038/s41598-020-58500-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wesolowski L.T., Semanchik P.L., White-Springer S.H. Beyond Antioxidants: Selenium and Skeletal Muscle Mitochondria. Front. Vet. Sci. 2022;9:1011159. doi: 10.3389/fvets.2022.1011159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gejl K.D., Andersson E.P., Nielsen J., Holmberg H.-C., Ørtenblad N. Effects of Acute Exercise and Training on the Sarcoplasmic Reticulum Ca2+ Release and Uptake Rates in Highly Trained Endurance Athletes. Front. Physiol. 2020;11:810. doi: 10.3389/fphys.2020.00810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maïmoun L., Sultan C. Effect of Physical Activity on Calcium Homeostasis and Calciotropic Hormones: A Review. Calcif. Tissue Int. 2009;85:277–286. doi: 10.1007/s00223-009-9277-z. [DOI] [PubMed] [Google Scholar]
- 43.Kragstrup T.W., Kjaer M., Mackey A.L. Structural, Biochemical, Cellular, and Functional Changes in Skeletal Muscle Extracellular Matrix with Aging. Scand. J. Med. Sci. Sports. 2011;21:749–757. doi: 10.1111/j.1600-0838.2011.01377.x. [DOI] [PubMed] [Google Scholar]
- 44.Kent-Braun J.A., Ng A.V., Young K. Skeletal Muscle Contractile and Noncontractile Components in Young and Older Women and Men. J. Appl. Physiol. 2000;88:662–668. doi: 10.1152/jappl.2000.88.2.662. [DOI] [PubMed] [Google Scholar]
- 45.Guo J., Wei Y., Heiland E.G., Marseglia A. Differential Impacts of Fat and Muscle Mass on Cardiovascular and Non-Cardiovascular Mortality in Individuals with Type 2 Diabetes. J. Cachexia Sarcopenia Muscle. 2024;15:1930–1941. doi: 10.1002/jcsm.13542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Srikanthan P., Horwich T.B., Tseng C.H. Relation of Muscle Mass and Fat Mass to Cardiovascular Disease Mortality. Am. J. Cardiol. 2016;117:1355–1360. doi: 10.1016/j.amjcard.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 47.Miljkovic I., Kuipers A.L., Cauley J.A., Prasad T., Lee C.G., Ensrud K.E., Cawthon P.M., Hoffman A.R., Dam T.-T., Gordon C.L., et al. Greater Skeletal Muscle Fat Infiltration Is Associated with Higher All-Cause and Cardiovascular Mortality in Older Men. J. Gerontol. Ser. A. 2015;70:1133–1140. doi: 10.1093/gerona/glv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marcus R.L., Addison O., Kidde J.P., Dibble L.E., Lastayo P.C. Skeletal Muscle Fat Infiltration: Impact of Age, Inactivity, and Exercise. J. Nutr. Health Aging. 2010;14:362–366. doi: 10.1007/s12603-010-0081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mika A., Macaluso F., Barone R., Di Felice V., Sledzinski T. Effect of Exercise on Fatty Acid Metabolism and Adipokine Secretion in Adipose Tissue. Front. Physiol. 2019;10:26. doi: 10.3389/fphys.2019.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Turcotte L.P., Fisher J.S. Skeletal Muscle Insulin Resistance: Roles of Fatty Acid Metabolism and Exercise. Phys. Ther. 2008;88:1279–1296. doi: 10.2522/ptj.20080018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamrick M.W., McGee-Lawrence M.E., Frechette D.M. Fatty Infiltration of Skeletal Muscle: Mechanisms and Comparisons with Bone Marrow Adiposity. Front. Endocrinol. 2016;7:69. doi: 10.3389/fendo.2016.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ghasemikaram M., Chaudry O., Nagel A.M., Uder M., Jakob F., Kemmler W., Kohl M., Engelke K. Effects of 16 Months of High Intensity Resistance Training on Thigh Muscle Fat Infiltration in Elderly Men with Osteosarcopenia. GeroScience. 2021;43:607–617. doi: 10.1007/s11357-020-00316-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brack A.S., Conboy M.J., Roy S., Lee M., Kuo C.J., Keller C., Rando T.A. Increased Wnt Signaling during Aging Alters Muscle Stem Cell Fate and Increases Fibrosis. Science. 2007;317:807–810. doi: 10.1126/science.1144090. [DOI] [PubMed] [Google Scholar]
- 54.Parker L., Caldow M.K., Watts R., Levinger P., Cameron-Smith D., Levinger I. Age and Sex Differences in Human Skeletal Muscle Fibrosis Markers and Transforming Growth Factor-β Signaling. Eur. J. Appl. Physiol. 2017;117:1463–1472. doi: 10.1007/s00421-017-3639-4. [DOI] [PubMed] [Google Scholar]
- 55.Petrocelli J.J., McKenzie A.I., de Hart N.M.M.P., Reidy P.T., Mahmassani Z.S., Keeble A.R., Kaput K.L., Wahl M.P., Rondina M.T., Marcus R.L., et al. Disuse-Induced Muscle Fibrosis, Cellular Senescence, and Senescence-Associated Secretory Phenotype in Older Adults Are Alleviated during Re-Ambulation with Metformin Pre-Treatment. Aging Cell. 2023;22:e13936. doi: 10.1111/acel.13936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu M., Xu H., Liu J., Tan X., Wan S., Guo M., Long Y., Xu Y. Metformin and Fibrosis: A Review of Existing Evidence and Mechanisms. J. Diabetes Res. 2021;2021:6673525. doi: 10.1155/2021/6673525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Piñol-Jurado P., Suárez-Calvet X., Fernández-Simón E., Gallardo E., de la Oliva N., Martínez-Muriana A., Gómez-Gálvez P., Escudero L.M., Pérez-Peiró M., Wollin L., et al. Nintedanib Decreases Muscle Fibrosis and Improves Muscle Function in a Murine Model of Dystrophinopathy. Cell Death Dis. 2018;9:776. doi: 10.1038/s41419-018-0792-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rangarajan S., Kurundkar A., Kurundkar D., Bernard K., Sanders Y.Y., Ding Q., Antony V.B., Zhang J., Zmijewski J., Thannickal V.J. Novel Mechanisms for the Antifibrotic Action of Nintedanib. Am. J. Respir. Cell Mol. Biol. 2016;54:51–59. doi: 10.1165/rcmb.2014-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Iemitsu K., Fujie S., Uchida M., Inoue K., Shinohara Y., Iemitsu M. Dioscorea Esculenta Intake with Resistance Training Improves Muscle Quantity and Quality in Healthy Middle-Aged and Older Adults: A Randomized Controlled Trial. Nutrients. 2023;15:2438. doi: 10.3390/nu15112438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Garg K., Corona B.T., Walters T.J. Therapeutic Strategies for Preventing Skeletal Muscle Fibrosis after Injury. Front. Pharmacol. 2015;6:87. doi: 10.3389/fphar.2015.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Miguel-Carrasco J.L., Beaumont J., San José G., Moreno M.U., López B., González A., Zalba G., Díez J., Fortuño A., Ravassa S. Mechanisms Underlying the Cardiac Antifibrotic Effects of Losartan Metabolites. Sci. Rep. 2017;7:41865. doi: 10.1038/srep41865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chan Y.-S., Li Y., Foster W., Fu F.H., Huard J. The Use of Suramin, an Antifibrotic Agent, to Improve Muscle Recovery after Strain Injury. Am. J. Sports Med. 2005;33:43–51. doi: 10.1177/0363546504265190. [DOI] [PubMed] [Google Scholar]
- 63.Li Y., Li J., Zhu J., Sun B., Branca M., Tang Y., Foster W., Xiao X., Huard J. Decorin Gene Transfer Promotes Muscle Cell Differentiation and Muscle Regeneration. Mol. Ther. 2007;15:1616–1622. doi: 10.1038/sj.mt.6300250. [DOI] [PubMed] [Google Scholar]
- 64.Turgeman T., Hagai Y., Huebner K., Jassal D.S., Anderson J.E., Genin O., Nagler A., Halevy O., Pines M. Prevention of Muscle Fibrosis and Improvement in Muscle Performance in the Mdx Mouse by Halofuginone. Neuromuscul. Disord. 2008;18:857–868. doi: 10.1016/j.nmd.2008.06.386. [DOI] [PubMed] [Google Scholar]
- 65.Dickinson J.M., Volpi E., Rasmussen B.B. Exercise and Nutrition to Target Protein Synthesis Impairments in Aging Skeletal Muscle. Exerc. Sport Sci. Rev. 2013;41:216–223. doi: 10.1097/JES.0b013e3182a4e699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deane C.S., Cox J., Atherton P.J. Critical Variables Regulating Age-Related Anabolic Responses to Protein Nutrition in Skeletal Muscle. Front. Nutr. 2024;11:1419229. doi: 10.3389/fnut.2024.1419229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ham D.J., Caldow M.K., Lynch G.S., Koopman R. Leucine as a Treatment for Muscle Wasting: A Critical Review. Clin. Nutr. 2014;33:937–945. doi: 10.1016/j.clnu.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 68.Kim I.-Y., Schutzler S., Schrader A., Spencer H., Kortebein P., Deutz N.E.P., Wolfe R.R., Ferrando A.A. Quantity of Dietary Protein Intake, but Not Pattern of Intake, Affects Net Protein Balance Primarily through Differences in Protein Synthesis in Older Adults. Am. J. Physiol.-Endocrinol. Metab. 2015;308:E21–E28. doi: 10.1152/ajpendo.00382.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Garlick P.J., McNurlan M.A., Patlak C.S. Adaptation of Protein Metabolism in Relation to Limits to High Dietary Protein Intake. Eur. J. Clin. Nutr. 1999;53((Suppl. S1)):S34–S43. doi: 10.1038/sj.ejcn.1600742. [DOI] [PubMed] [Google Scholar]
- 70.Jacob I., Johnson M.I., Jones G., Jones A., Francis P. Age-Related Differences of Vastus Lateralis Muscle Morphology, Contractile Properties, Upper Body Grip Strength and Lower Extremity Functional Capability in Healthy Adults Aged 18 to 70 Years. BMC Geriatr. 2022;22:538. doi: 10.1186/s12877-022-03183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Franchi M.V., Atherton P.J., Reeves N.D., Flück M., Williams J., Mitchell W.K., Selby A., Beltran Valls R.M., Narici M.V. Architectural, Functional and Molecular Responses to Concentric and Eccentric Loading in Human Skeletal Muscle. Acta Physiol. 2014;210:642–654. doi: 10.1111/apha.12225. [DOI] [PubMed] [Google Scholar]
- 72.Vieira A., Blazevich A., Souza N., Celes R., Alex S., Tufano J.J., Bottaro M. Acute Changes in Muscle Thickness and Pennation Angle in Response to Work-Matched Concentric and Eccentric Isokinetic Exercise. Appl. Physiol. Nutr. Metab. 2018;43:1069–1074. doi: 10.1139/apnm-2018-0055. [DOI] [PubMed] [Google Scholar]
- 73.Crane J.D., Devries M.C., Safdar A., Hamadeh M.J., Tarnopolsky M.A. The Effect of Aging on Human Skeletal Muscle Mitochondrial and Intramyocellular Lipid Ultrastructure. J. Gerontol. Ser. A. 2010;65A:119–128. doi: 10.1093/gerona/glp179. [DOI] [PubMed] [Google Scholar]
- 74.Lee M.J.-C., Saner N.J., Ferri A., García-Domínguez E., Broatch J.R., Bishop D.J. Delineating the Contribution of Ageing and Physical Activity to Changes in Mitochondrial Characteristics across the Lifespan. Mol. Asp. Med. 2024;97:101272. doi: 10.1016/j.mam.2024.101272. [DOI] [PubMed] [Google Scholar]
- 75.Broskey N.T., Greggio C., Boss A., Boutant M., Dwyer A., Schlueter L., Hans D., Gremion G., Kreis R., Boesch C., et al. Skeletal Muscle Mitochondria in the Elderly: Effects of Physical Fitness and Exercise Training. J. Clin. Endocrinol. Metab. 2014;99:1852–1861. doi: 10.1210/jc.2013-3983. [DOI] [PubMed] [Google Scholar]
- 76.Yu J., Zheng J., Liu X.F., Feng Z.L., Zhang X.P., Cao L.L., Zhou Z.P. Exercise Improved Lipid Metabolism and Insulin Sensitivity in Rats Fed a High-Fat Diet by Regulating Glucose Transporter 4 (GLUT4) and Musclin Expression. Braz. J. Med. Biol. Res. 2016;49:e5129. doi: 10.1590/1414-431x20165129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hughes V.A., Fiatarone M.A., Fielding R.A., Kahn B.B., Ferrara C.M., Shepherd P., Fisher E.C., Wolfe R.R., Elahi D., Evans W.J. Exercise Increases Muscle GLUT-4 Levels and Insulin Action in Subjects with Impaired Glucose Tolerance. Am. J. Physiol.-Endocrinol. Metab. 1993;264:E855–E862. doi: 10.1152/ajpendo.1993.264.6.E855. [DOI] [PubMed] [Google Scholar]
- 78.Kim T.N., Park M.S., Ryu J.Y., Choi H.Y., Hong H.C., Yoo H.J., Kang H.J., Song W., Park S.W., Baik S.H., et al. Impact of Visceral Fat on Skeletal Muscle Mass and Vice Versa in a Prospective Cohort Study: The Korean Sarcopenic Obesity Study (KSOS) PLoS ONE. 2014;9:e115407. doi: 10.1371/journal.pone.0115407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ng J.C.M., Schooling C.M. Effect of Basal Metabolic Rate on Lifespan: A Sex-Specific Mendelian Randomization Study. Sci. Rep. 2023;13:7761. doi: 10.1038/s41598-023-34410-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee S.-R., Directo D., Khamoui A.V. Fish Oil Administration Combined with Resistance Exercise Training Improves Strength, Resting Metabolic Rate, and Inflammation in Older Adults. Aging Clin. Exp. Res. 2022;34:3073–3081. doi: 10.1007/s40520-022-02250-5. [DOI] [PubMed] [Google Scholar]
- 81.McGlory C., Calder P.C., Nunes E.A. The Influence of Omega-3 Fatty Acids on Skeletal Muscle Protein Turnover in Health, Disuse, and Disease. Front. Nutr. 2019;6:144. doi: 10.3389/fnut.2019.00144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lammes E., Rydwik E., Akner G. Effects of Nutritional Intervention and Physical Training on Energy Intake, Resting Metabolic Rate and Body Composition in Frail Elderly. A Randomised, Controlled Pilot Study. J. Nutr. Health Aging. 2012;16:162–167. doi: 10.1007/s12603-011-0157-7. [DOI] [PubMed] [Google Scholar]
- 83.Fujita S., Dreyer H.C., Drummond M.J., Glynn E.L., Cadenas J.G., Yoshizawa F., Volpi E., Rasmussen B.B. Nutrient Signalling in the Regulation of Human Muscle Protein Synthesis. J. Physiol. 2007;582:813–823. doi: 10.1113/jphysiol.2007.134593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mayhew P.M., Thomas C.D., Clement J.G., Loveridge N., Beck T.J., Bonfield W., Burgoyne C.J., Reeve J. Relation between Age, Femoral Neck Cortical Stability, and Hip Fracture Risk. Lancet. 2005;366:129–135. doi: 10.1016/S0140-6736(05)66870-5. [DOI] [PubMed] [Google Scholar]
- 85.Johansson C., Black D., Johnell O., Odén A., Mellström D. Bone Mineral Density Is a Predictor of Survival. Calcif. Tissue Int. 1998;63:190–196. doi: 10.1007/s002239900513. [DOI] [PubMed] [Google Scholar]
- 86.Trivedi D.P., Khaw K.T. Bone Mineral Density at the Hip Predicts Mortality in Elderly Men. Osteoporos. Int. 2001;12:259–265. doi: 10.1007/s001980170114. [DOI] [PubMed] [Google Scholar]
- 87.Korpelainen R., Keinänen-Kiukaanniemi S., Heikkinen J., Väänänen K., Korpelainen J. Effect of Impact Exercise on Bone Mineral Density in Elderly Women with Low BMD: A Population-Based Randomized Controlled 30-Month Intervention. Osteoporos. Int. 2006;17:109–118. doi: 10.1007/s00198-005-1924-2. [DOI] [PubMed] [Google Scholar]
- 88.Thomas A.C.Q., Stead C.A., Burniston J.G., Phillips S.M. Exercise-Specific Adaptations in Human Skeletal Muscle: Molecular Mechanisms of Making Muscles Fit and Mighty. Free Radic. Biol. Med. 2024;223:341–356. doi: 10.1016/j.freeradbiomed.2024.08.010. [DOI] [PubMed] [Google Scholar]
- 89.Zioupos P., Currey J.D. Changes in the Stiffness, Strength, and Toughness of Human Cortical Bone with Age. Bone. 1998;22:57–66. doi: 10.1016/S8756-3282(97)00228-7. [DOI] [PubMed] [Google Scholar]
- 90.Kemmler W., Häberle L., von Stengel S. Effects of Exercise on Fracture Reduction in Older Adults. Osteoporos. Int. 2013;24:1937–1950. doi: 10.1007/s00198-012-2248-7. [DOI] [PubMed] [Google Scholar]
- 91.Narici M.V., Maffulli N., Maganaris C.N. Ageing of Human Muscles and Tendons. Disabil. Rehabil. 2008;30:1548–1554. doi: 10.1080/09638280701831058. [DOI] [PubMed] [Google Scholar]
- 92.Grosset J.-F., Breen L., Stewart C.E., Burgess K.E., Onambélé G.L. Influence of Exercise Intensity on Training-Induced Tendon Mechanical Properties Changes in Older Individuals. AGE. 2014;36:9657. doi: 10.1007/s11357-014-9657-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Reeves N.D., Maganaris C.N., Narici M.V. Effect of Strength Training on Human Patella Tendon Mechanical Properties of Older Individuals. J. Physiol. 2003;548:971–981. doi: 10.1113/jphysiol.2002.035576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Radovanović G., Bohm S., Peper K.K., Arampatzis A., Legerlotz K. Evidence-Based High-Loading Tendon Exercise for 12 Weeks Leads to Increased Tendon Stiffness and Cross-Sectional Area in Achilles Tendinopathy: A Controlled Clinical Trial. Sports Med.-Open. 2022;8:149. doi: 10.1186/s40798-022-00545-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jerger S., Centner C., Lauber B., Seynnes O., Friedrich T., Lolli D., Gollhofer A., König D. Specific Collagen Peptides Increase Adaptions of Patellar Tendon Morphology Following 14-Weeks of High-Load Resistance Training: A Randomized-Controlled Trial. Eur. J. Sport Sci. 2023;23:2329–2339. doi: 10.1080/17461391.2023.2232758. [DOI] [PubMed] [Google Scholar]
- 96.Brzuszkiewicz-Kuźmicka G., Szczegielniak J., Bączkowicz D. Age-Related Changes in Shock Absorption Capacity of the Human Spinal Column. Clin. Interv. Aging. 2018;13:987–993. doi: 10.2147/CIA.S156298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Santello M. Review of Motor Control Mechanisms Underlying Impact Absorption from Falls. Gait Posture. 2005;21:85–94. doi: 10.1016/j.gaitpost.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 98.Stathokostas L., McDonald M.W., Little R.M.D., Paterson D.H. Flexibility of Older Adults Aged 55–86 Years and the Influence of Physical Activity. J. Aging Res. 2013;2013:e743843. doi: 10.1155/2013/743843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Perrone F., Jommi C., Di Maio M., Gimigliano A., Gridelli C., Pignata S., Ciardiello F., Nuzzo F., de Matteis A., Del Mastro L., et al. The Association of Financial Difficulties with Clinical Outcomes in Cancer Patients: Secondary Analysis of 16 Academic Prospective Clinical Trials Conducted in Italy†. Ann. Oncol. 2016;27:2224–2229. doi: 10.1093/annonc/mdw433. [DOI] [PubMed] [Google Scholar]
- 100.Greca S.L., Rapali M., Ciaprini G., Russo L., Vinciguerra M.G., Giminiani R.D. Acute and Chronic Effects of Supervised Flexibility Training in Older Adults: A Comparison of Two Different Conditioning Programs. Int. J. Environ. Res. Public Health. 2022;19:16974. doi: 10.3390/ijerph192416974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Warneke K., Keiner M., Wohlann T., Lohmann L.H., Schmitt T., Hillebrecht M., Brinkmann A., Hein A., Wirth K., Schiemann S. Influence of Long-Lasting Static Stretching Intervention on Functional and Morphological Parameters in the Plantar Flexors: A Randomized Controlled Trial. J. Strength Cond. Res. 2023;37:1993–2001. doi: 10.1519/JSC.0000000000004513. [DOI] [PubMed] [Google Scholar]
- 102.Panidi I., Bogdanis G.C., Terzis G., Donti A., Konrad A., Gaspari V., Donti O. Muscle Architectural and Functional Adaptations Following 12-Weeks of Stretching in Adolescent Female Athletes. Front. Physiol. 2021;12:701338. doi: 10.3389/fphys.2021.701338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Longo S., Cè E., Bisconti A.V., Rampichini S., Doria C., Borrelli M., Limonta E., Coratella G., Esposito F. The Effects of 12 Weeks of Static Stretch Training on the Functional, Mechanical, and Architectural Characteristics of the Triceps Surae Muscle–Tendon Complex. Eur. J. Appl. Physiol. 2021;121:1743–1758. doi: 10.1007/s00421-021-04654-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cui M., Zhang S., Liu Y., Gang X., Wang G. Grip Strength and the Risk of Cognitive Decline and Dementia: A Systematic Review and Meta-Analysis of Longitudinal Cohort Studies. Front. Aging Neurosci. 2021;13:625551. doi: 10.3389/fnagi.2021.625551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kim S., Jazwinski S.M. Quantitative Measures of Healthy Aging and Biological Age. Healthy Aging Res. 2015;4:26. doi: 10.12715/har.2015.4.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hirase T., Okubo Y., Delbaere K., Menant J.C., Lord S.R., Sturnieks D.L. Risk Factors for Falls and Fall-Related Fractures in Community-Living Older People with Pain: A Prospective Cohort Study. Int. J. Environ. Res. Public Health. 2023;20:6040. doi: 10.3390/ijerph20116040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Runge M., Hunter G. Determinants of Musculoskeletal Frailty and the Risk of Falls in Old Age. J. Musculoskelet. Neuronal Interact. 2006;6:167–173. [PubMed] [Google Scholar]
- 108.Zech A., Hübscher M., Vogt L., Banzer W., Hänsel F., Pfeifer K. Balance Training for Neuromuscular Control and Performance Enhancement: A Systematic Review. J. Athl. Train. 2010;45:392–403. doi: 10.4085/1062-6050-45.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Araújo C.G.S.D. Flexibility Assessment: Normative Values for Flexitest from 5 to 91 Years of Age. Arq. Bras. Cardiol. 2008;90:280–287. doi: 10.1590/S0066-782X2008000400008. [DOI] [PubMed] [Google Scholar]
- 110.Polsgrove M.J., Eggleston B.M., Lockyer R.J. Impact of 10-Weeks of Yoga Practice on Flexibility and Balance of College Athletes. Int. J. Yoga. 2016;9:27. doi: 10.4103/0973-6131.171710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Duizer D. Cardiorespiratory Fitness Assessment and Treatment for Health Span and Lifespan. CAND J. 2020;27:22–25. doi: 10.54434/candj.76. [DOI] [Google Scholar]
- 112.Costa J.N.A., Ribeiro A.L.A., Ribeiro D.B.G., Neri S.G.R., Barbosa D.F., Avelar B.P., Safons M.P. Balance Exercise Circuit for Fall Prevention in Older Adults: A Randomized Controlled Crossover Trial. J. Frailty Sarcopenia Falls. 2022;7:60–71. doi: 10.22540/JFSF-07-060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Stathokostas L., Little R.M.D., Vandervoort A.A., Paterson D.H. Flexibility Training and Functional Ability in Older Adults: A Systematic Review. J. Aging Res. 2012;2012:306818. doi: 10.1155/2012/306818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ghanvatkar S., Kankanhalli A., Rajan V. User Models for Personalized Physical Activity Interventions: Scoping Review. JMIR mHealth uHealth. 2019;7:e11098. doi: 10.2196/11098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Davergne T., Meidinger P., Dechartres A., Gossec L. The Effectiveness of Digital Apps Providing Personalized Exercise Videos: Systematic Review with Meta-Analysis. J. Med. Internet Res. 2023;25:e45207. doi: 10.2196/45207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Monroe C.M., Cai B., Edney S., Jake-Schoffman D.E., Brazendale K., Bucko A., Armstrong B., Yang C.-H., Turner-McGrievy G. Harnessing Technology and Gamification to Increase Adult Physical Activity: A Cluster Randomized Controlled Trial of the Columbia Moves Pilot. Int. J. Behav. Nutr. Phys. Act. 2023;20:129. doi: 10.1186/s12966-023-01530-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Halma M., Marik P. Preventing Functional Decline with Age: Biomarkers and Best Practices-[V1] Preprints. 2024 doi: 10.20944/preprints202403.0667.v1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.