Abstract
Introduction
Vasectomy is a widely used, safe, effective method of permanent contraception and contributes to healthy sexuality.
Aims
We have conducted a 3-step observational clinical study to develop a vasectomy regret risk score and guide patients and clinicians when discussing a vasectomy.
Methods
A 3-step approach has been followed. First, experts involved in male health have proposed risk factors for regret (remorse) after vasectomy, defined by a vasectomy reversal surgery or medically assisted reproduction. The selected factors were evaluated in 1200 patients vasectomized in the last 15 years. Finally, the expert panel has constructed a score for predicting regret after vasectomy.
Results
Fifty-two international experts identified 17 risk factors for vasectomy regret. Five of the risk factors were significant: an age <35 years old, a high Barrat Impulsivity Score, a low level of education, and a patient who didn’t understand that the vasectomy might not be reversible or for whom the contraception responsibility is ideally feminine, or no responsible partner. On multivariate analysis, 3 risk factors and 2 “sine qua non” conditions were used to build the decision algorithm. A risk score ≥ 4 required information on sperm cryopreservation before vasectomy, and those with a risk score ≥ 7 required extra time for reflection. The scoring system was proposed to 52 international experts and accepted with 86.7% strongly agreeing. The model’s sensitivity and specificity were 0.98 and 0.53, respectively.
Conclusion
A decisional algorithm was established to identify patients requiring information on sperm cryopreservation before vasectomy or additional time for reflection to reduce the risk of vasectomy regret. The algorithm contains 3 risk factors and 2 “sine qua non” conditions.
Keywords: vasectomy, regret risk factors, scoring system, semen cryopreservation, reflection time, male fertility, male contraception
Introduction
Vasectomy is a widely used, safe, effective method of permanent contraception and contributes to healthy sexuality.1-3 Thermal or hormonal methods are sometimes offered as alternative treatments but are not yet recommended as a standard approach.3 Surgical complications are rare.4,5
In men who have undergone vasectomy, the desire for a child is estimated between 5% and 7%.6 Among partners of vasectomized patients, a wish for pregnancy is estimated at around 6.1%.7 Being childless or single, having an age <30 years, having a severe intercurrent illness, or having chronic scrotal pain are relative contraindications to vasectomy.8 It is crucial to identify patients with a potential increased risk for vasectomy regret.
Patients who wish to restore their fertility following vasectomy may be offered vasectomy reversal (VR).9-11 The pregnancy rate after VR varies from 50% to 75%.6 Medically assisted reproduction (MAR), ideally from the patient’s cryopreserved sperm, is the last option.10 French Association of Urology guidelines recommend providing information on sperm cryopreservation and a 4-month reflection period for patients requesting vasectomy.3,12,13
We have conducted a 3-stage study with a panel of experts to identify patients at risk of vasectomy regret—remorse (emotional response to a decision that now feels wrong or ill-suited to the new situation) and developed a pre-vasectomy regret risk score. This score will guide clinicians when counseling these men to consider semen cryopreservation or a period of reflection before surgery.
Material and methods
Panel of experts
Between January and May 2023, an international panel of 52 experts in men’s health has been invited to propose potential risk factors for vasectomy regret—change of mind after vasectomy (Table S1; supplementary material). The Barratt Impulsivity Score in its short 15-questions form (BIS-15) was included as a possible risk factor. The risk factors were then rated by the experts via an online consultation conducted from May 2023 to June 2023 (Table S2; supplementary material). Expert recommendations were graded as very strong, strong, weak, and no/neutral according to the level of agreement among the panelists. Very strong was defined as “mandatory before vasectomy.”
Patient survey
An online questionnaire of 34 items was developed, including the 17 selected risk factors and epidemiological characteristics (Table S3; supplementary material). The questionnaire was circulated to 1200 men who had undergone vasectomy or VR in the last 15 years in 3 Belgian academic hospitals. The survey was approved by the local ethical committee (B0392022000072), and informed consent was obtained before as the first step. The survey was conducted anonymously using SurveyMonkey.
The consensus meeting
A consensus meeting with the expert was held on September 21, 2023 in Brussels to analyze the clinical study’s results. Based on the clinical trials, a scoring system was developed and validated by the experts.
Statistical analysis
The primary endpoint of the study is the rate of objective regret, defined by a decision to have VR or MAR. Regret was also subjectively assessed by the question 26 “Do you have any regret since your vasectomy: yes or no?” (Table S3). The vasectomy regret algorithm was developed based on the risk factors identified in the survey using a multivariate logistic regression model to quantify the impact of different potential risk factors on the probability of vasectomy regret. The independent variables relevant to the model were selected based on exploratory analyses and univariate models (hypothesis testing between the regret and no-regret groups and univariate logistic regression to explain regret). The ROC curve and area under the curve (AUC) were used to assess the model's performance, sensitivity, and specificity. Results are expressed as median (range) unless otherwise stated. Statistics were done on SPSS package.
Results
Expert consultation
Firstly, the experts have individually proposed 17 potential factors they suspected may lead to vasectomy regret: a new partner (78%); desire for child (48.1%); chronic postoperative pain (30.8%); young age (28.8%); death of a child (25%); childlessness (17.3%); change of mind (11.5%); single, separated, or divorced relationship status (9.6%;); low socio-economic status (7.7%); external pressure to perform vasectomy—for example, “where the partner was the first to suggest that the man has a vasectomy” (5.8%); psychological initial status—“psychiatric/psychological co-morbidity” (5.8%); low number of children defined as ≤1 child (3.8%); (3.8%); religious (3.8%); belief in reversibility (3.8%); ecological concerns (1.9%); and lack of partner consultation before vasectomy (1.9%). The word regret may not always be taken literal and describes the act of feeling sorrow or remorse for past actions due to change of circumstances.
The above 17 factors were further reviewed via an online consultation, and a strength level was determined for each by consensus.
The panel of experts concluded (with >75% agreement considered a strong recommendation) that reasons for vasectomy, number of children, and patient age are questions that should be included during the pre-vasectomy consultation (Table S4; supplementary material).
Recognized risk factors for vasectomy regret include (with >75% agreement considered as a strong recommendation): men <30 years old, wish to have a child in the future, and external pressure (Table S4; supplementary material).
Patient survey
Population
Twelve hundred patients from 3 academic centers were contacted: 1129 (94.1%) after a vasectomy and 71 (5.9%) after a VR surgery. This analysis is based on the 594 (49.5%) who signed the informed consent form and answered the questionnaire. The patient characteristics are summarized in Table 1.
Table 1.
Patients’ characteristics.
| Regret rate | |||||
|---|---|---|---|---|---|
| VR - P+ | VR - P- | MAR - P+ | MAR - P- | FSU - P+ | FSU - P- |
| 36 (8.9%), | 14 (3.4%) | 4 (1%), | |||
| 25 (69.4%) | 11 (30.6%) | 10 (71.4%) | 4 (28.6%) | 2 (50%) | 2 (50%) |
| Marital status | |||||
| Single | Married | Legal cohabitors | Separated | Divorced | Widowed |
| 27 (6.6%) | 1248 (60.3%) | 70 (17%) | 11 (2.7%) | 54 (13.1%) | 1 (0.24%) |
| Educational level | |||||
| No diploma | Elementary school | Secondary school | Bachelor’s degree from college | Bachelor’s degree from university | Master from university |
| 5 (1.2%) | 5 (1.2%) | 130 (31.6%) | 109 (26.5%) | 19 (4.6%) | 144 (35%) |
Abbreviations: VR, vasectomy reversal (-no, + yes); MAR, medically assisted reproduction (-no, + yes); FSU, frozen sperm used (-no, + yes); P+, pregnancy (-no, + yes).
Regret characteristics
Seventy-three patients (12.3%) answered positively to the question “Do you have any regret since your vasectomy?” (Table S3; Patient questionnaire, q26). Among them 32 (5.8%) have regret objectified by VR or MAR. The main regret reason was a child desire in 47 patients (64.4%), chronic testicular pain ≥1 year in 22 (30.1%), restoration of fertility potential because too young age at the time of vasectomy in 4 (5.5%), and death of child in 1 (1.4%). The median time before expressing regret was 4 years (1-15).
Pre-operative characteristics
The level of education (P = .0036), an age <30 years (P = .0039) (Figure 1), a Barratt impulsiveness score >30/45 (P = .0266), and a lack of information on the irreversibility (P = .0068) were statistically significantly (P < .05) associated with vasectomy regret. The median Barratt impulsiveness score (BIS-15) was 26 [15-45].
Figure 1.

Age at the time of vasectomy and regret (individual value and logistic regression).
Contraception viewpoint
Most of the patients (62%) confirmed discussing contraception options with their partners, and 89% believed that both partners were responsible for the contraception. Interestingly, the rate of regret was significantly higher in patients considering that contraception was the partner’s concern (P = .0003).
Pre-operative sperm cryopreservation
Half the patients had received information about sperm cryopreservation possibilities (n = 205). Sixteen of them (7.8%) had used a sperm bank before vasectomy, but only 4 patients used their sample (Table 1). Patients expressed significantly more regret after vasectomy if they had not stored their sperm (P < .0001).
Multivariate analysis
Five risk factors were significantly associated with vasectomy regret: (<35 years old at the time of vasectomy), a Barrat Impulsivity Score (BIS-15) >30, a low level of education, misunderstanding the concept of “definitive,” and patient relying on female contraception or no contraception at all.
Among those risk factors, 3 were confirmed as significant in the multivariate analysis: the partner in charge of contraception (partner or neither) (P = .0027; OR 4.07), an age <35 years old (P = .0137; OR 3.03), and a BIS-15 score > 30) (P = .0398; OR 2.30). The level of education was not significant (P = .0672, OR = 2) and was excluded from the model. Understanding the definitive nature of the procedure was considered by the expert’s panel as a “sine qua non”—“mandatory” condition to obtain informed consent before surgery.
A risk score for each criterion was defined according to their OR in the model. A decision algorithm was elaborated to identify the patient at risk of regret. The AUC of these 3 criteria of multivariate analysis was 0.64 for a risk score ≥4 and 0.77 for a risk score ≥7 (Figure 2). The final logistic regression model had a sensitivity of 0.98 and a specificity of 0.53 (Figure 2—Table S5; supplementary material).
Figure 2.
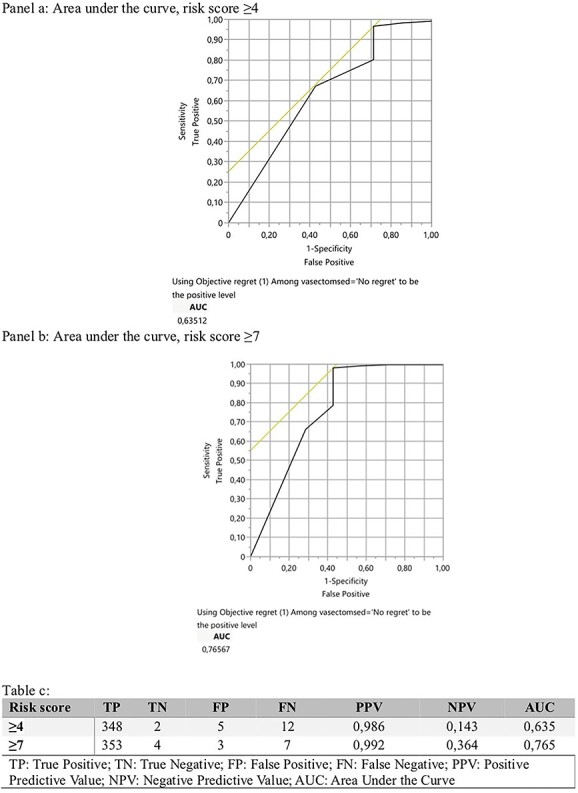
Logistic regression mode—multivariate analysis.
Expert consensus
The scoring system was proposed to the 52 experts and was accepted after 2 rounds of discussion with 2 levels of recommendation: information on sperm cryopreservation before vasectomy (risk score ≥4) or extra time for reflection (risk score ≥7). The majority of experts (86.7%) strongly agreed and 6.7% weakly agreed on the final consensus (Table S5; supplementary material). According to the Focus group (FG)- results, a pre-vasectomy questionnaire was proposed to the experts during the Delphi consensus and strongly recommended by 80% (Table S6; supplementary material).
Discussion
The recommendation for cryopreservation prior to vasectomy significantly varies among European urologists. In the absence of clear guidelines, it is mainly driven by local practices and financial coverage of the country’s healthcare system. An international consensus was thus needed to standardize practices and guide patients’ (and couples’) choice.
The satisfaction rate after vasectomy is high, mostly due to taking responsibility for the partner and the reliability and ease of this surgical technique. However, previous publications demonstrated possible psychological complications, including depression, irritability, or somatic symptoms.14
Twelve percent of our sample described subjective regret, twice as many as those with an objective regret defined as a genuine procreation project (VR, MAR, or cryopreserved sperm use).15
In the present study, we developed a simple preoperative questionnaire to anticipate future regret and selectively recommend cryopreservation or delay the surgery to further discussion We used a modified Delphi panel methodology to identify factors for vasectomy regret. Five hundred ninety-four patients evaluated these factors via an online survey. A prediction algorithm was then developed.
The prediction algorithm includes patient characteristics, information about the couple, and family composition (Table S5; supplementary material). This algorithm is not developed to contraindicate vasectomy but rather to provide targeted information and, more importantly, to suggest sperm cryopreservation.
We propose a scoring system based on 6 criteria to evaluate the risk of post-vasectomy regret. Two factors were identified as “sine qua non” conditions by experts: Absence of wish to have children in the future and acceptance of the potential irreversibility of the procedure (understood as permanent infertility). Patients should understand that VR can offer good results (70% pregnancy rate in our study), but these remain uncertain and depend on the time elapsed since vasectomy.6,16
The 4 reminder criteria are based on experts’ suggestions evaluated by our clinical study.
Young age was identified by the FG to be a risk factor of vasectomy regret. This in line with current literature.15 Our clinical study identified 39 years old as the most sensitive and specific threshold for avoiding post-operative regret (Figure 1). The most significant impact was observed in participants aged 35 years old and under (Figure 1).
We used the impulsivity-validated score of Barratt (BIS-15; supplementary material) for the first time in this scenario and found a significant impact on regret after vasectomy.
Our findings are in line with available research, which confirms that this tool is suitable for identifying the tendency to make wrong choices that one may later regret.17 It evaluates non-planning, motor, and attentional impulsivity. BIS-15 was confirmed to maintain good reliability and validity for evaluating prefrontal structure, serotonergic function, and impulsivity-related behaviors in healthy individuals.17
Level of education was not identified as a vasectomy regret risk factor in the literature but was found to be significant in our study. This criterion may reflect the couple’s socio-economic level and could be linked to greater instability within the couple.18 Vasectomy reversal was significantly higher in patients with a different partner from the one at the time of vasectomy. These criteria may also be linked to medical literacy and a better understanding of the possible irreversible post-operative sterility, identified as a crucial risk factor.
The ideal partner who should be responsible for contraception in the relationship is an important criterion. It demonstrates the involvement and motivation of men. A patient considering the woman to be responsible for contraception in their relationship may request this surgery in the event of external pressure.
Experts identified childlessness as a potential vasectomy regret risk factor. Our clinical study did not confirm this correlation as no statistical difference was found between the childless population and those with offspring. Similar results were published previously.19 This may demonstrate a lifestyle choice. This lifestyle choice may mitigate the desire to father a new child with a different partner in the event of separation.
The scoring system was statistically developed with a sensitivity of 0.98. It aimed to identify patients likely to regret vasectomy procedure. They need pre-operative information about sperm cryopreservation options if their risk score is ≥4. Sperm cryopreservation is not an obligation. The patient must just receive information. A man who cannot afford sperm cryopreservation should not, however, be ineligible for vasectomy. If the score is ≥7, an extra period of 4 months to allow time for reflection is proposed in line with the French recommendations proposing this time for reflection for all patients.20 The aim is also to reduce the rate of sperm cryopreservation in some countries, such as France, which offer this security option for all patients prior vasectomy.6 An excessive rate of sperm cryopreservation is linked to cost for patients and time for specialists. Identifying patients at risk of regret is of utmost importance.
Conclusion
Vasectomy is intended to be a definitive male contraception. Although minimal, the risk of post-operative regret does exist and is related to various factors. A decisional algorithm could help identify patients at risk of vasectomy regret who could then be offered sperm cryopreservation and/or more time to consider their options before surgery. This could help to reduce the rate of regret and avoid excessive sperm cryopreservation.
External validation of this proposed decision-making algorithm is needed before clinical implementation.
Supplementary Material
Acknowledgments
Belgian Society of Urology and Foundation Mont-Godinne.
Contributor Information
Amandine Degraeve, Department of Urology, Centre Hospitalier Universitaire, Université Catholique de Louvain, 5000 Namur, Belgium; Department of Urology, Cliniques Universitaires Saint-Luc, 1200 Bruxelles, Belgium.
Lorenzo Tosco, Université libre de Bruxelles (ULB), Hôpital Universitaire de Bruxelles (H.U.B), Erasme Hospital, 1070 Brussels, Belgium.
Bertrand Tombal, Department of Urology, Cliniques Universitaires Saint-Luc, 1200 Bruxelles, Belgium.
Thierry Roumeguere, Université libre de Bruxelles (ULB), Hôpital Universitaire de Bruxelles (H.U.B), Erasme Hospital, 1070 Brussels, Belgium.
Jeanne Beirnaert, Université libre de Bruxelles (ULB), Hôpital Universitaire de Bruxelles (H.U.B), Erasme Hospital, 1070 Brussels, Belgium.
Robin Hamal, Department of Urology, Cliniques Universitaires Saint-Luc, 1200 Bruxelles, Belgium.
Céline Bugli, Plateforme Technologique de Support en Méthodologie et Support Statistique (SMCS), Université catholique de Louvain (UCLouvain), 1348 Louvain-la-Neuve, Belgium.
Marco Cosentino, Andrology Department, Casa di Cura Villa Maria, 35100 Padova, Italy.
Lee Wai Gin (Don), Institute of Andrology, Department of Urology, University College London Hospital NHS Trust, London NW1 2PG, United Kingdom.
Marta Skrodzka, Department of Urology, St. Georges University Hospital, London SW17 0QT, United Kingdom.
Maarten Albersen, Department of Urology, Universitair Ziekenhuis Leuven (UZ Leuven), 3000 Leuven, Belgium.
Koenraad van Renterghem, Department of Urology, Jessa Hospital, 3500 Hasselt, Belgium.
Maxime Sempels, Department of Urology, CHU Liège, 4000 Liège, Belgium.
David Penning, Department of Fertility, Université Libre de Bruxelles (ULB), Hôpital Universitaire de Bruxelles (HUB), CUB Hôpital Erasme, 1070 Brussels, Belgium.
Mikkel Fode, Department of Urology, Copenhagen University Hospital - Herlev and Gentofte Hospital, 2100 Copenhagen, Denmark.
Antoine Faix, Department of Urology, Department of Andrology, Clinique du Millénaire, 34000 Montpellier, France.
Marjan Waterloos, Department of Urology, AZ Maria Middelares, 9000 Ghent, Belgium.
Borja Garcia Gomez, Department of Urology, Hospital Universitario 12 de Octubre, 28041 Madrid, Spain.
Damien Carnicelli, Department of Urology, CHU Lyon sud, 69495 Lyon, France.
Jean-Pierre Graziana, Department of Urology Andrology, Clinique mutualiste de la porte de l'Orient, 56100 Lorient, France.
Afonso Morgado, Department of Urology, ULS São João, 4050-377 Porto, Portugal.
Kathleen D’Hauwers, Department of Urology, Radboud University Medical Center, 6525 Nijmegen, The Netherlands.
Ege Serefoglu, Department of Urology, Biruni Üniversitesi, 34015 Istanbul, Türkiye.
Celeste Manfredi, Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania “Luigi Vanvitelli”, 80138 Naples, Italy.
Emmanuel Weyne, Department of Urology, AZ Sint-Blasius, 9200 Sint-Niklaas, Belgium.
Jack Beck, Department of Urology, St. Antoniusziekenhuis, 3435 Nieuwegein, The Netherlands.
Daniar Osmonov, Department of Urology, University Hospital Schleswig Holstein, Campus Lübeck, 23562 Lübeck, Germany.
Chris Roller, Department of Urology, Hôpitaux Robert Schuman, L-2540 Luxembourg, Luxembourg.
Ludovic Ferreti, Department of Urology, Maison de Santé Protestante de Bagatelle, 33401 Talence, France.
Giogio Russo, Urology Section, University of Catania, 95124 Catania, Italy.
Faysal A Yafi, Department of Urology, University of California Irvine, CA92697 Irvine, United States.
Beatrice Cuzin, Department of Urology and Transplantation, University E. Herriot Hospital, 69003 Lyon, France.
François-Xavier Madec, Department of Urology, Foch Hospital, 92150 Suresnes, France; UMR 1179, Inserm Faculty of Medicine, 78000 Versailles, France; Department of Urology, Saint Quentin University, Paris Saclay, 78180 Montigny le Bretonneux, France.
Geoffroy Vanoverschelde, Department of Urology, Cliniques Saint-Jean, 1000 Bruxelles, Belgium.
François Hervé, Department of Urology, ERN Accredited Centrum, Ghent University Hospital, 9000 Ghent, Belgium.
Eric Chung, Department of Urology, Princess Alexandra Hospital, University of Queensland, and the AndroUrology Centre, Brisbane, QLD_4102 Queensland, Australia.
Ulla Nordström, Department of Urology, Rigshospitalet, 4000 Roskilde, Denmark.
Andrea Cocci, Department of Urology, University of Florence, Careggi Hospital, 50134 Florence, Italy.
Rawad Abou Zahr, Department of Urology, Cliniques Universitaires Saint-Luc, 1200 Bruxelles, Belgium.
François Triffaux, Department of Urology, CHU Liège, 4000 Liège, Belgium.
Minhas Suks, Department of Urology, Imperial College Healthcare, Fulham Palace Road, London W6 8RF, United Kingdom.
Hussain Alnajjar, Institute of Andrology, Department of Urology, University College London Hospital NHS Trust, London NW1 2PG, United Kingdom.
Julien Van Damme, Department of Urology, Cliniques Universitaires Saint-Luc, 1200 Bruxelles, Belgium.
Sam Ward, Department of Urology, Cliniques Saint-Jean, 1000 Bruxelles, Belgium.
Author contributions
Lorenzo Tosco, Julien Van Damme and Sam Ward same author importance.
Funding
None declared.
Conflicts of interest
None declared.
Disclosure
Partially retrospective study. Development of a risk score to be implemented in clinical practice to assess its effectiveness in identifying patients at risk of regret. Need for external validation.
References
- 1. Abbe CR, Page ST, Thirumalai A. Male contraception. Yale J Biol Med. 2020;93(4):603–613 [PMC free article] [PubMed] [Google Scholar]
- 2. Jamieson DJ, Costello C, Trussell J, Hillis SD, Marchbanks PA, Peterson HB. The risk of pregnancy after vasectomy. Obstet Gynecol. 2004;103(5, Part 1):848–850. 10.1097/01.AOG.0000123246.11511.e4 [DOI] [PubMed] [Google Scholar]
- 3. Dohle GR, Diemer T, Kopa Z, et al. European Association of Urology guidelines on vasectomy. Eur Urol. 2012;61(1):159–163. 10.1016/j.eururo.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 4. Fainberg J, Kashanian JA. Vasectomy. Vasectomy Jama. 2018;319(23):2450. 10.1001/jama.2018.6514 [DOI] [PubMed] [Google Scholar]
- 5. Auyeung AB, Almejally A, Alsaggar F, Doyle F. Incidence of post-vasectomy pain: systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(5):1788. 10.3390/ijerph17051788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Degraeve A, Roumeguere T, Tilmans G, et al. European countries have different rates of sperm cryopreservation before vasectomy and at the time of reversal. Andrology. 2022;10(7):1286–1291. 10.1111/andr.13182 [DOI] [PubMed] [Google Scholar]
- 7. Brannigan RE. Vasectomy and vasectomy reversal: a comprehensive approach to the evolving spectrum of care. Fertil Steril. 2021;115(6):1363–1364. 10.1016/j.fertnstert.2021.04.029 [DOI] [PubMed] [Google Scholar]
- 8. Clinic Mayo, Mayo Foundation for Medical Education and Research (MFMER), Vasectomy Reversal .2020. (https://www.mayoclinic.org/tests-procedures/vasectomy-reversal/about/pac-20384537).
- 9. Jequier AM. Vasectomy related infertility: a major and costly medical problem. Hum Reprod. 1998;13(7):1757–1759. 10.1093/humrep/13.7.1757 [DOI] [PubMed] [Google Scholar]
- 10. Potts JM, Pasqualotto FF, Nelson D, Thomas AJ Jr, Agarwal A. Patient characteristics associated with vasectomy reversal. J Urol. 1999;161(6):1835–1839. 10.1016/S0022-5347(05)68819-2 [DOI] [PubMed] [Google Scholar]
- 11. Amory JK. Male contraception. Fertil Steril. 2016;106(6):1303–1309. 10.1016/j.fertnstert.2016.08.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sharlip ID, Belker AM, Honig S, et al. Vasectomy: AUA guideline. J Urol. 2012;188(6S):2482–2491. 10.1016/j.juro.2012.09.080 [DOI] [PubMed] [Google Scholar]
- 13. Hupertan V, Graziana JP, Schoentgen N, et al. Recommendations of the Committee of Andrology and Sexual Medicine of the AFU concerning the management of vasectomy. Prog Urol. 2023;33(5):223–236. 10.1016/j.purol.2022.12.014 [DOI] [PubMed] [Google Scholar]
- 14. Zhao K, Wu L, Kong X, et al. Long-term safety, health and mental status in men with vasectomy. Sci Rep. 2018;8(1):15703. 10.1038/s41598-018-33989-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Anderson DJ, Lucero M, Vining S, et al. Vasectomy regret or lack thereof. Health Psychol Res. 2022;10(3):38241. 10.52965/001c.38241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Uvin V, de Brucker S, de Brucker M, et al. Pregnancy after vasectomy: surgical reversal or assisted reproduction? Hum Reprod. 2018;33(7):1218–1227. 10.1093/humrep/dey101 [DOI] [PubMed] [Google Scholar]
- 17. Spinella M. Normative data and a short form of the Barratt impulsiveness scale. Int J Neurosci. 2007;117(3):359–368. 10.1080/00207450600588881 [DOI] [PubMed] [Google Scholar]
- 18. Karney BR. Socioeconomic status and intimate relationships. Annu Rev Psychol. 2021;72(1):391–414. 10.1146/annurev-psych-051920-013658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Charles DK, Anderson DJ, Newton SA, Dietrich PN, Sandlow JI. Vasectomy regret among childless men. Urology. 2023;172:111–114. 10.1016/j.urology.2022.11.027 [DOI] [PubMed] [Google Scholar]
- 20.Hupertan V, Graziana JP, Schoentgen N, et al. Recommandations du Comité d’Andrologie et de Médecine Sexuelle de l’AFU concernant la prise en charge de la vasectomie, Progrès en Urologie, 2023;33(5):223–236. 10.1016/j.purol.2022.12.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


