Highlights
-
•
Radiation therapists reported a high interest in learning about AI.
-
•
AI is perceived to enhance effectiveness in radiation therapy but is underutilized.
-
•
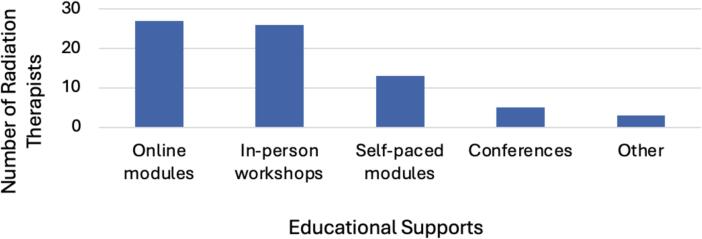
The preferred education methods were online modules and in-person workshops.
-
•
Radiation therapists expect AI to impact job satisfaction and clinical roles.
Keywords: Radiotherapy, Perception, Artificial Intelligence, Educational Support
Abstract
Introduction
In recent years, artificial intelligence (AI) technology has played an evolving role in radiation science, influencing the clinical practice of radiation therapists. This study aimed to explore the knowledge, attitude, clinical applications, and learning needs from the perspective of radiation therapists.
Materials and Methods
This study used a cross-sectional online survey with a population of radiation therapists from a single institution. The survey was developed iteratively and was based on past literature. The questions were constructed to measure perception using four themes: knowledge of AI, perceived utilization, job impact, clinical applications, learning needs, and educational support. The data was analyzed using descriptive statistics according to the key themes.
Results
Between 22nd December 2023 and 17th January 2024, 74 radiation therapists completed the survey. The majority (55.4 %) were 44 years or older (Baby Boomers and Generation X). Additionally, 37.8 % rated their knowledge of AI as none or limited, but 93.2 % expressed interest in learning more about AI. Many (79.7 %) perceived AI not to be fully used in radiation therapy but has increased its effectiveness in image registration, reconstruction, and contouring. With the increasing use of AI in healthcare, 96.0 % feel that AI may affect their role, and 82.4 % believe it may impact their job satisfaction. Educational supports indicated to be the most advantageous for their job were online modules (36.5 %) and in-person workshops (35.1 %).
Conclusion
Exploring the perspectives of radiation therapists has shown a strong interest in learning about AI and its role in radiation therapy. This information can help in understanding how to develop tailored strategies to mitigate potential barriers, leading to the successful implementation of AI in clinical radiation therapy practice.
Introduction
It is projected that by 2024, there will be approximately 247,100 new cancer cases diagnosed in Canada[1]. In Ontario alone, there has been a 157 % increase in cancer diagnoses from 1984 to 2018[2]. A critical component of cancer treatments is radiation therapy, which is used for approximately 50 % of cancer patients during their treatment care[3]. Radiation therapy is increasingly integrating advanced technologies into clinical practice, including artificial intelligence (AI), which has the potential to enhance treatment efficiency and precision[4], [5]. AI refers to algorithms using large datasets to solve human intelligence problems using machine learning, deep learning, or convolutional neural networks[6].
Within radiation therapy, AI-based methods are progressively being integrated into clinical practice including auto-segmentation, treatment planning, and synthetic computed tomography scan generation[7]. Research in healthcare AI has increased from one published scientific paper in the year 2000 to 5019 in 2021[8]. Despite this increase, there is limited research on the perception of AI among radiation therapists.
Research on innovations such as image-guided radiation therapy (IGRT) has shown that assessing the perception of radiation therapists can lead to increased confidence and successful adoption[9]. It is crucial to understand the perception of radiation therapists to ensure the successful implementation of new technology into practice. Against this background, this study aimed to evaluate the current perception of AI among radiation therapists at an urban academic cancer center with experience piloting AI-based technology.
Methods
From December 2023 to January 2024, an online survey was sent to a population of approximately 196 radiation therapists (including full-time and part-time) at a single institution. The population size was decided based on how many radiation therapists were currently employed and able to participate in the project. The sampling method for the project was convenience sampling due to the available population of radiation therapists and their willingness to participate.
This study used an online descriptive cross-sectional survey consisting of qualitative and quantitative items with a Likert scale and open-ended questions. The framework of the survey was based on the existing literature with feedback from radiation therapy clinical researchers [10], [11], [12]. Using these findings from the literature, this study used a multi-dimensional approach to define perception under four themes. The themes were radiation therapist’s knowledge, attitude, clinical applications, and learning needs.
This research project was approved by the institutional quality improvement committee. The quality improvement project aimed to understand the perspectives of radiation therapists’ on artificial intelligence. The participants were invited through an email that had the study and consent information. The email included the contact information of the research team for potential participants to ask questions or address any concerns. Following the expression of interest, the potential participants consented, and the first question of the survey confirmed consent. Reminder emails were sent out weekly starting at two weeks following the initial mail. To maintain confidentiality and anonymity, the questions were selected to avoid identifying information. Participants were informed that all data remained confidential and stored on REDCap, a secure online application that captured the data from the research project.
Data analysis
The results for each question were inputted and sorted in Microsoft Excel. The researchers reviewed the data to ensure completeness and check for duplicates in the raw data. The raw data from the survey was analyzed using standard descriptive statistics. Frequency distributions and visual graphs were created to determine the relative frequency of responses. The chi-square test was used to evaluate a statistically significant association (p < 0.05) between age and the themes of perception.
Results
During the data collection period, a total of 83 individuals consented to participate in the survey from a single institution between 22nd December 2023 and 17th January 2024. Nine did not complete the survey resulting in a total of 74 radiation therapists who completed the anonymized online survey. The response rate was 37.8 % among the 196 radiation therapists currently employed at the institution (including part-time and full-time employees).
Knowledge of AI
Results demonstrated that many radiation therapists had moderate (39.2 %) or limited (36.4 %) knowledge and awareness of AI, with only 1.4 % having no level of familiarity. Additionally, respondents showed a similar trend in ranking their understanding of educational AI terms (ex/ machine learning, deep learning, etc.), with 35.1 % indicating a moderate understanding and an equal percentage having limited understanding see Table 1.
Table 1.
Summarizes the results of demographics, perceptions of knowledge, and impact of AI.
| # (%) | |||
|---|---|---|---|
| Age | |||
| Baby Boomer (1946–1964) | 4 (5.4 %) | ||
| Generation X (1965–1980) | 37 (50.0 %) | ||
| Millennial/Generation Y (1981–1996) | 32(43.2 %) | ||
| Generation Z (1997 – 2012) | 1 (1.4 %) | ||
| Knowledge of AI | |||
| Level of AI knowledge | |||
| None | 1 (1.4 %) | ||
| Limited | 27 (36.4 %) | ||
| Moderate | 29 (39.2 %) | ||
| Good | 16 (21.6 %) | ||
| Expert | 1 (1.4 %) | ||
| Understanding of AI terms | |||
| None | 5 (6.8 %) | ||
| Limited | 26 (35.1 %) | ||
| Moderate | 26 (35.1 %) | ||
| Good | 16 (21.6 %) | ||
| Expert | 1 (1.4 %) | ||
| Perceived impact of AI | |||
| Fully implemented AI in radiation therapy | |||
| Strongly Disagree | 19 (25.7 %) | ||
| Disagree | 40 (54.1 %) | ||
| Neutral | 14 (18.9 %) | ||
| Agree | 0 (0 %) | ||
| Strongly Agree | 1 (1.4 %) | ||
| Job role | |||
| None | 3 (4.1 %) | ||
| Slightly | 14 (18.9 %) | ||
| Moderately | 31 (41.9 %) | ||
| Significantly | 16 (21.6 %) | ||
| Very significantly | 10 (13.5 %) | ||
| Job satisfaction | |||
| None | 13 (17.6 %) | ||
| Slightly | 12 (16.2 %) | ||
| Moderately | 32 (43.2 %) | ||
| Significantly | 12 (16.2 %) | ||
| Very significantly | 5 (6.8 %) | ||
Perceived utilization of AI & job impact
More than two-thirds of radiation therapists agreed with the statement that AI has not been fully implemented into radiation therapy, and most radiation therapists (95.9 %) perceived that the increasing use of AI would impact their role. Additionally, 17.6 % of respondents stated that using AI would not influence their job satisfaction when asked to what extent they believe the increased use of AI will change their perspective on their job satisfaction. This is more than a 4-fold increase compared to the small percentage (4.1 %) of radiation therapists who do not anticipate that AI would affect their role. The most common level of impact on job satisfaction was moderate, with 43.2 %, as shown in Table 1.
Clinical applications
When asked about the effectiveness and productivity of clinical applications that use AI in radiation therapy, 77.0 % of radiation therapists believed that AI has increased effectiveness in image registration and reconstruction. Similarly, in treatment planning contouring (organs at risk (OAR) and targets), 78.4 % of radiation therapists believed AI would improve effectiveness. The quality assurance process had inconclusive outcomes as there was no unanimous consensus on the effectiveness, resulting in an equal distribution (see Fig. 1).
Fig. 1.
Opinion of AI effectiveness on clinical applications.
Learning needs and educational supports
Ninety-three percent of participants were interested in learning more about AI, with many preferring online modules (36.5 %) or in-person workshops (35.1 %) as their learning method. Few respondents indicated that conferences (6.8 %) and self-paced modules (17.6 %) would be advantageous to enhance their learning or ability to use AI technologies (see Fig. 2). Three respondents indicated “other” in an open-ended question and mentioned a combination of methods or no interest in any education.
Fig. 2.
Preferred learning methods and educational supports.
The majority (87.8 %) of participants believed that students studying radiation therapy should learn about AI and its clinical applications in radiation therapy (55.4 %). Other aspects of AI that were shown to be important for students to learn were the fundamentals of AI (17.6 %) and ethical considerations and policy (16.2 %) (see Fig. 3). Eight respondents indicated “other” in an open-ended question with the comments having a common theme of a combination of clinical applications, fundamentals, ethical considerations, and policy.
Fig. 3.
Aspects of AI that radiation therapists would like students to learn.
Age
Majority of the radiation therapists 41/74 (55.4 %) were 44 years or older (Baby Boomers and Generation X) and the remaining (44.6 %) were 43 years or younger (Millennials or Generation Z) see Table 1. Table 2 demonstrates that when using the chi-square test on the themes of knowledge of AI terms there were statistically significant results (p < 0.05) between the two age groups.
Table 2.
Age analysis – Assessing knowledge and perception of AI using the chi-square test.
| Theme & Question | Groups | Categories | Chi-Square p-value | |
|---|---|---|---|---|
| Knowledge | Limited + None | Good + Moderate + Expert | ||
| Rate your current level of knowledge of Artificial Intelligence (AI) | Baby Boomers & Generation X (44 years or older) |
16 | 25 | 0.8 |
| Millennial/Generation Y & Generation Z (43 years or younger) |
12 | 21 | ||
| Rate your current level of understanding of AI terms (ex/Machine Learning, Deep Learning…) |
Baby Boomers & Generation X (44 years or older) |
13 | 28 | <0.05 |
| Millennial/Generation Y & Generation Z (43 years or younger) |
18 | 15 | ||
| Perception of Utilization & Job Impact | Strongly Disagree + Disagree | Strongly Agree + Agree + Neutral | ||
| Do you feel AI has been fully implemented in radiation therapy? | Baby Boomers & Generation X (44 years or older) |
32 | 9 | 0.7 |
| Millennial/Generation Y & Generation Z (43 years or younger) |
27 | 6 | ||
| Do you think the increased use of AI in radiation therapy will affect your role as a radiation therapist? | Baby Boomers & Generation X (44 years or older) |
7 | 34 | 0.2 |
| Millennial/Generation Y & Generation Z (43 years or younger) |
10 | 23 | ||
| To what extent do you believe that the increased use of AI will change your perspective on your job satisfaction? | Baby Boomers & Generation X (44 years or older) |
13 | 28 | 0.7 |
| Millennial/Generation Y & Generation Z (43 years or younger) |
12 | 21 | ||
Discussion
With the fast-paced movement of the AI industry, healthcare professionals seem to be “cautiously optimistic” about AI[12]. Similarly to when other innovations were introduced into radiation therapy, it significantly changed clinical practice, patient care, and safety frameworks[9]. AI will likely have this same “disruptive transformation” as it evolves and integrates into radiation oncology[13]. It is crucial to understand the perception of healthcare professionals to implement new technology into practice successfully[9]. The research has shown that insights into the perception of AI will allow for informed decisions on education, adoption strategies, and clinical applications[14]. Thus, research should expand on the existing knowledge and prioritize understanding how radiation therapists perceive AI[10], [15], [16], [17]. This project aimed to capture the perception of radiation therapists regarding the implementation of AI in radiation medicine using the themes of knowledge, impact on role and job satisfaction, clinical applications, and learning needs.
In Canada, radiation therapists operate linear accelerators, perform quality assurance, provide patient care, train students, and prepare radiation treatment plans. Most radiation therapists who participated in this study were Generation X (1965–1980) 44 years and older (55.4 %), a similar demographic to other studies[10]. The Canadian radiation therapy workforce often has radiation therapists from the ages of 18 to 65 years old[18]. This study had slightly more radiation therapists aged 44 years and older, possibly due to familiarity with the institution or an increased sense of value to contribute to research or improved education methods. Age stratification suggested that radiation therapists 44 years or older were more likely to have a good, moderate, or expert understanding of AI terms. This result complemented the study by Batumalai et al., who found that Generation X felt the most empowered to make decisions regarding AI automation[12]. Additionally, an international survey on AI in radiology revealed that an increased adoption of AI into clinical practice may be associated with an intermediate to advanced level of AI knowledge[19]. Together these results could suggest that age coupled with clinical experience and increased understanding of AI allows individuals to be more empowered to implement AI.
The overall understanding of AI from this study data was identified as moderate or limited. While this was a self-assessment question, these findings were similar to the literature[11]. The gap in knowledge mirrors Coakley et al., where there was a general awareness of AI but a lack of familiarity with the technical components (i.e., deep learning, machine learning)[20]. Given that AI systems are sometimes referred to as black-box machines it is important to have questions that can differentiate AI understanding from specific AI terms. Patient-centred medicine requires informed decision-making, and a general AI understanding is not sufficient. Understanding the terms AI algorithm systems use is vital to avoid the risk of black-box medicine[21], [22]. Thus, there is an appreciable need for further education and awareness of AI to improve the knowledge of radiation therapists. Many studies have noticed these trends and note a consistent willingness and readiness to learn[10], [11], [20], [23].
With the need for further training and the ambiguity of the term AI, it has the potential to influence job roles and satisfaction. The question will remain if the overarching feelings from radiation therapists are positive or negative. AI has an increasing ability to enhance treatment planning in radiation therapy, which has been recognized and studied[24], [25]. Similar to the literature, most respondents in this study agreed that AI has not been fully implemented in radiation therapy but recognizes its potential to increase productivity in image registration and contouring[13], [26]. Additionally, radiation therapists perceive that AI would impact their job satisfaction. International studies found this consensus among their populations where the majority believe AI will alter the radiographer practice[20]. Further clarification is needed to learn what aspects of AI are perceived as positive and negative concerning their clinical role. Previous studies in radiological technology have reported mixed opinions, possibly due to how AI is used in radiology and the awareness of clinical applications[27], [28].
The rise of AI in radiation therapy should prompt educators to evaluate their curriculum and incorporate AI-related concepts into the curriculum if this is not currently being done. This study had a strong interest in participants learning about AI (93.2 %) through online modules or in-person workshops. These two methods may have been preferred by radiation therapists due to the convenience of online modules and the hands-on experience of in-person workshops. A future education model to learn about AI in radiation therapy may want to incorporate a hybrid of these approaches to align with the interests of radiation therapists. Additionally, many (87.8 %) indicated that students should be educated on the use of AI in clinical practice, and these results are echoed in the literature[23]. Furthermore, a review by Chamunyonga et al., suggested that future radiation therapy education needs to provide students with the confidence, knowledge, skills, and competency to use AI safely and ethically in clinical applications[29]. To ensure positive awareness and integration of AI, radiation therapists must have an active role in the application and clinical validation of AI[30]. Thus, gaining a better understanding of the perception and gaps in knowledge will inform successful implementation strategies and education of our future clinicians.
Limitations
In addition to this study being only conducted in a single institutional, it did have limitations, including the response rate. This was a challenge encountered with the timing of the study done during a period of holidays and vacations at the institution which may have indirectly impacted the staff available to participate. The single institution was also a limitation, however, this institution has done some research in AI, allowing this population of radiation therapists to give their clinically relevant perspective on real-world AI applications. Additionally, to comply with ethics the online survey could only be done using the institution’s virtual private network (VPN) which may have negatively impacted the response rate.
Future directions
Healthcare is recognizing the impact of new technology as many organizations, like the Canadian Artificial Intelligence and big Data in Radiotherapy Alliance (CADRA), understand that research is needed to facilitate the successful integration of healthcare and technology. The Canadian Association of Medical Radiation Technologists (CAMRT), the Canadian Organization of Medical Physicists (COMP), and the Canadian Association of Radiation Oncology (CARO) have joined together to form CADRA[31]. CADRA is taking the necessary steps to promote education and collaboration regarding AI among inter-professional practices and patients. Future research may wish to evaluate practicing radiation therapists nationally at multiple provincial sites. This approach would allow for a more representative sample that would reduce bias and increase generalizability and study validity. Additionally, other healthcare professionals who are involved in radiation therapy, such as radiation oncologists, nurses, radiation therapy patient flow coordinators, and physicists, would give a more comprehensive understanding and practical, relevant data. Students and trainees would provide a different perspective and inform educational interventions that could help future generations of healthcare professionals[32]. Another stakeholder that should be considered in future research is the patient perspective which could explore patients’ knowledge, values and communication or education preferences when AI is integrated into their treatments. There are some studies regarding the patient perspective on the use of AI in radiology, but limited information is known on how patients perceive AI integration into their radiation therapy treatments[33]. Using the information from these types of studies could improve the profession and person-centered care.
Conclusion
Transformation is occurring in healthcare, and new technological advancements are being rapidly integrated into clinical practice. This project aimed to explore the knowledge, attitude, clinical applications, and learning needs of AI from the perspective of radiation therapists. The results revealed a consensus among radiation therapists that AI has the potential to increase effectiveness in radiation therapy and has room to grow in the profession. They perceived AI to increase effectiveness in some aspects of radiation therapy and could impact their clinical practice. There was a strong interest in learning about AI and for future students to have AI integrated into their undergraduate curriculum and available continuing education after their undergraduate training. Learning about the perception of AI from radiation therapists allows for tailored strategies to mitigate potential barriers, leading to successful implementation and adoption.
Contributions
All authors contributed to the work, acquisition and analysis of the data. All authors were involved in drafting and commenting on the paper and have approved the final version.
Ethical approval
Informed written consent was obtained from all participants. The University Health Network (UHN) Quality Improvement Review Committee (QIRC) approved the study (QIRC 23-0699).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank all the radiation therapists at the institution who participated in this study. We acknowledge the support from Dr Tara Rosewell and Ms Kieng Tan from Princess Margaret Cancer Centre for their assistance and encouragement.
References
- 1.Brenner D.R., et al. Projected estimates of cancer in Canada in 2024. CMAJ. May 2024;196(18):E615–E623. doi: 10.1503/CMAJ.240095/TAB-RELATED-CONTENT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ontario Health (Cancer Care Ontario), “Ontario Cancer Statistics 2022,” Toronto, 2022. [Online]. Available: https://www.cancercareontario.ca/en/data-research/view-data/statistical-reports/ontario-cancer-statistics-2022.
- 3.Baskar R., Lee K.A., Yeo R., Yeoh K.W. Cancer and radiation therapy: current advances and future directions. Int J Med Sci. Feb. 2012;9(3):193. doi: 10.7150/IJMS.3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiorino C., Guckemberger M., Schwarz M., van der Heide U.A., Heijmen B. Technology‐driven research for radiotherapy innovation. Mol Oncol. Jul. 2020;14(7):1500. doi: 10.1002/1878-0261.12659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giuliani M., Gospodarowicz M. Radiation oncology in Canada. Jpn J Clin Oncol. Jan. 2018;48(1):22–25. doi: 10.1093/JJCO/HYX148. [DOI] [PubMed] [Google Scholar]
- 6.Jarrett D., Stride E., Vallis K., Gooding M.J. Applications and limitations of machine learning in radiation oncology. Br J Radiol. 2019;92(1100):1–12. doi: 10.1259/bjr.20190001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vandewinckele L., et al. Overview of artificial intelligence-based applications in radiotherapy: recommendations for implementation and quality assurance. Radiother Oncol. Dec. 2020;153:55–66. doi: 10.1016/J.RADONC.2020.09.008. [DOI] [PubMed] [Google Scholar]
- 8.Jimma B.L. Artificial intelligence in healthcare: a bibliometric analysis. Telematics Informatics Rep. Mar. 2023;9 doi: 10.1016/J.TELER.2023.100041. [DOI] [Google Scholar]
- 9.Li W., Harnett N., Moseley D.J., Higgins J., Chan K., Jaffray D.A. Investigating user perspective on training and clinical implementation of volumetric imaging. J Med Imaging Radiat Sci. Jun. 2010;41(2):57–65. doi: 10.1016/J.JMIR.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Wong K., Gallant F., Szumacher E. Perceptions of Canadian radiation oncologists, radiation physicists, radiation therapists and radiation trainees about the impact of artificial intelligence in radiation oncology - national survey. J Med Imaging Radiat Sci. Mar. 2021;52(1):44–48. doi: 10.1016/J.JMIR.2020.11.013. [DOI] [PubMed] [Google Scholar]
- 11.J. O’Shaughnessey and M. L. Collins, “Radiation therapist perceptions on how artificial intelligence may affect their role and practice,” J Med Radiat Sci, vol. 70 Suppl 2, no. Suppl 2, pp. 6–14, Apr. 2023, doi: 10.1002/JMRS.638. [DOI] [PMC free article] [PubMed]
- 12.Batumalai V., et al. Cautiously optimistic: a survey of radiation oncology professionals’ perceptions of automation in radiotherapy planning. Tech Innov Patient Support Radiat Oncol. Dec. 2020;16:58–64. doi: 10.1016/J.TIPSRO.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson R.F., et al. Artificial intelligence in radiation oncology: a specialty-wide disruptive transformation? Radiother Oncol. Dec. 2018;129(3):421. doi: 10.1016/J.RADONC.2018.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nieboer M.E., van Hoof J., van Hout A.M., Aarts S., Wouters E.J.M. Professional values, technology and future health care: the view of health care professionals in The Netherlands. Technol Soc. Nov. 2014;39:10–17. doi: 10.1016/J.TECHSOC.2014.05.003. [DOI] [Google Scholar]
- 15.Castagno S., Khalifa M. Perceptions of artificial intelligence among healthcare staff: a qualitative survey study. Front Artif Intell. Oct. 2020;3 doi: 10.3389/FRAI.2020.578983/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gillan C., Milne E., Harnett N., Purdie T.G., Jaffray D.A., Hodges B. Professional implications of introducing artificial intelligence in healthcare: an evaluation using radiation medicine as a testing ground. J Radiother Pract. Mar. 2019;18(1):5–9. doi: 10.1017/S1460396918000468. [DOI] [Google Scholar]
- 17.Q. Miró Catalina et al., “Knowledge and perception of primary care healthcare professionals on the use of artificial intelligence as a healthcare tool,” 2023, doi: 10.1177/20552076231180511. [DOI] [PMC free article] [PubMed]
- 18.Gillies C., Bristow B., Gallant F., Osmar K., Lange-Mechlen I., Tran W.T. Results of a Canadian study examining the prevalence and potential for developing compassion fatigue and burnout in radiation therapists. J Radiother Pract. Sep. 2014;13(4):383–392. doi: 10.1017/S1460396914000144. [DOI] [Google Scholar]
- 19.Huisman M., et al. An international survey on AI in radiology in 1,041 radiologists and radiology residents part 1: fear of replacement, knowledge, and attitude. Eur Radiol. Sep. 2021;31(9):7058–7066. doi: 10.1007/S00330-021-07781-5/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coakley S., et al. Radiographers’ knowledge, attitudes and expectations of artificial intelligence in medical imaging. Radiography (Lond) Nov. 2022;28(4):943–948. doi: 10.1016/J.RADI.2022.06.020. [DOI] [PubMed] [Google Scholar]
- 21.Amann J., Blasimme A., Vayena E., Frey D., Madai V.I. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak. Dec. 2020;20(1):1–9. doi: 10.1186/S12911-020-01332-6/PEER-REVIEW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bjerring J.C., Busch J. Artificial intelligence and patient-centered decision-making. Philos Technol. Jun. 2021;34(2):349–371. doi: 10.1007/S13347-019-00391-6/METRICS. [DOI] [Google Scholar]
- 23.Ryan M.L., O’Donovan T., McNulty J.P. Artificial intelligence: the opinions of radiographers and radiation therapists in Ireland. Radiography (Lond) Oct. 2021;27(Suppl 1):S74–S82. doi: 10.1016/J.RADI.2021.07.022. [DOI] [PubMed] [Google Scholar]
- 24.Tsang D.S., et al. A prospective study of machine learning-assisted radiotherapy planning for patients receiving 54 Gy to the brain. Int J Radiat Oncol Biol Phys. Mar. 2024 doi: 10.1016/J.IJROBP.2024.02.022. [DOI] [PubMed] [Google Scholar]
- 25.Pillai M., et al. Using artificial intelligence to improve the quality and safety of radiation therapy. J Am Coll Radiol. 2019;16:1267–1272. doi: 10.1016/j.jacr.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 26.Liang S., et al. Deep-learning-based detection and segmentation of organs at risk in nasopharyngeal carcinoma computed tomographic images for radiotherapy planning. Eur Radiol. Apr. 2019;29(4):1961–1967. doi: 10.1007/S00330-018-5748-9/TABLES/4. [DOI] [PubMed] [Google Scholar]
- 27.Botwe B.O., et al. The integration of artificial intelligence in medical imaging practice: perspectives of African radiographers. Radiography (Lond) Aug. 2021;27(3):861–866. doi: 10.1016/J.RADI.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 28.M. M. Abuzaid, W. Elshami, H. Tekin, and B. Issa, “Assessment of the Willingness of Radiologists and Radiographers to Accept the Integration of Artificial Intelligence Into Radiology Practice,” 2022, doi: 10.1016/j.acra.2020.09.014. [DOI] [PubMed]
- 29.Chamunyonga C., Edwards C., Caldwell P., Rutledge P., Burbery J. The impact of artificial intelligence and machine learning in radiation therapy: considerations for future curriculum enhancement. J Med Imaging Radiat Sci. Jun. 2020;51(2):214–220. doi: 10.1016/j.jmir.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 30.Murphy A., Liszewski B. Artificial intelligence and the medical radiation profession: how our advocacy must inform future practice. J Med Imaging Radiat Sci. Dec. 2019;50(4):S15–S19. doi: 10.1016/j.jmir.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 31.CADRA, “Canadian Artificial Intelligence and big Data in Radiotherapy Alliance (CADRA).” Accessed: Dec. 11, 2024. [Online]. Available: https://www.cadra-acadr.ca/.
- 32.Wartman S.A., Combs C.D. Reimagining medical education in the age of AI. AMA J Ethics. Feb. 2019;21(2):146–152. doi: 10.1001/AMAJETHICS.2019.146. [DOI] [PubMed] [Google Scholar]
- 33.Haan M., Ongena Y.P., Hommes S., Kwee T.C., Yakar D. A qualitative study to understand patient perspective on the use of artificial intelligence in radiology. J Am Coll Radiol. Oct. 2019;16(10):1416–1419. doi: 10.1016/J.JACR.2018.12.043. [DOI] [PubMed] [Google Scholar]