Abstract
Purpose of Review
Limb alignment correction about the knee joint is crucial for the protection of the meniscus, particularly in the setting of meniscal root repairs and meniscal allograft transplantation. Distal femoral osteotomies and high tibial osteotomies have been described to restore the anatomic alignment to aid in meniscal preservation. This article provides a review of knee alignment and biomechanics, various surgical interventions to correct knee malalignment, and the effect of malalignment on the treatment of meniscal pathology.
Recent Findings
Both distal femoral and high tibial corrective osteotomies have been shown to slow the progression of osteoarthritis in the postoperative period. Moreover, corrective osteotomies have resulted in high patient satisfaction and good survival rates at mid- to long-term follow-up in patients with prior varus/valgus malalignment. Ongoing research is aimed to determine the best utilization for concomitant osteotomies in the setting and treatment of meniscal pathology with hopes of decreasing the progression of early-onset osteoarthritis, and ultimately, the conversion to total knee arthroplasty.
Summary
Neutral alignment at the level of the knee joint results in optimal force distributions. Corrective valgus and varus osteotomies aim to restore neutral alignment with the goal of ligamentous and meniscal preservation, ideally slowing osteoarthritis progression.
Keywords
meniscus; distal femoral osteotomy; high tibial osteotomy; varus malalignment; valgus malalignment; osteoarthritis.
Keywords: Varus malalignment, Valgus malalignment, Meniscal allograft transplant, Root repair, High tibial osteotomy, Distal femoral osteotomy
Introduction
The normal anatomic alignment of the knee is between 5° and 7° of valgus in relation to a neutral mechanical axis [1–4]. In terms of force distribution, the medial compartment—in an anatomic knee—may bear up to 70% of the total force [5–7]. When the mechanical axis shifts medially due to excess varus alignment, the total axial force applied to the medial compartment increases, which may have negative implications on the medial compartment including the medial meniscus. Conversely, when the knee has excess valgus alignment, more of the force is distributed through the lateral compartment including the lateral meniscus.
Excess varus alignment may possibly jeopardize certain meniscal procedures—particularly medial meniscal allograft transplants (MMATs) and medial meniscal posterior root tear (MMPRTs) repairs [8•,9•,10–12]. When there is ≥ 5° of correctable varus, a high tibial osteotomy (HTO) may be performed in the setting of MMPRT repair or MMAT to better protect the repair/transplant [13–16••,17–19,20•]. Moreover, failure to address the varus alignment may be associated with poorer meniscal healing rates and increased rates of postoperative meniscal extrusion [15••,21••,22•].
There is a paucity of literature describing increased risk of lateral meniscal injury or increased postoperative complications following lateral meniscus surgery with valgus malalignment; however, it is theorized that the lateral meniscus is more susceptible to tearing in a valgus-malaligned knee due to incumbent loss of meniscal mobility secondary to increased compressive forces on the lateral compartment [23••]. Nonetheless, due to the natural convexity and overall decreased surface area of the lateral compartment compared to the medial compartment, an increasing valgus deformity would place more force on a compartment that may not be equipped to handle such stresses [23••,24]. Therefore, in the setting of valgus-malalignment at the knee, it is important to consider correcting the mechanical axis to neutral with a distal femoral osteotomy (DFO) at the time of certain lateral meniscal procedures (for example lateral meniscus allograft transplantation [LMATs]) to ensure an optimal mechanical environment for healing [25].
It is crucial to consider knee alignment in the setting of posterior horn root meniscal tears or meniscal transplantation. Failure to do so may result in construct failure, continued progression of unicompartmental osteoarthritis (OA), and ultimately conversion to either a unicompartmental knee arthroplasty (UKA) or a total knee arthroplasty (TKA).
Alignment & Biomechanics
The mechanical axis of the lower limb is defined by a line extending from the center of the femoral head to the center of the tibiotalar joint, and the anatomical axes of the femur and tibia correspond to the mid-diaphyseal line of each bone [26]. Ideally, the mechanical axis should pass from the center of the femoral head, through the knee transecting the tibial eminences, to the center of the tibiotalar joint [27, 28]. Medial deviation of this line suggests varus alignment, while lateral deviation suggests valgus alignment [26, 27]. In relation to the mechanical axis, the normal anatomic axis of the knee lies between 5° and 7° of valgus [1–4, 27]. The tibial surface averages approximately 3° of varus whereas the femoral surface averages approximately 2° to 3° of valgus in relation to the mechanical axis [27, 29].
In neutral alignment, the medial compartment may bear up to 70% of the axial load which increases by 5% for every additional 1° of varus in a malaligned knee [27, 30, 31]. In a review by Dugdale et al., greater than 2° of varus malalignment substantially increased the risk of developing medial compartmental OA [32]. This highlights the importance of meticulous preoperative planning for MATs and meniscal root repairs, with the goal of neutral alignment restoration to preserve meniscus and articular cartilage.
In a biomechanical study examining the effect of lower limb alignment on tibiofemoral joint biomechanics following MMPRT repair, Berk et al. found that greater overall contact pressures and areas of localized contact pressures were elevated in varus knees [8•], which may reduce the effectiveness of root repair in delaying OA progression. In another biomechanical study looking at MMPRT repair following a 5° medial closing wedge DFO, Deichsel et al. found that an insufficiency of peripheral attachments and varus alignment led to increased forces acting on the root repair [9•]. These biomechanical studies highlight two important points to consider: (1) even if the meniscal root was repaired it may fail to heal due to elevated contact pressures, and (2) if there is residual varus malalignment, the forces on the articular surfaces are likely to be amplified.
In a historic study by Johnson et al., it was determined that even when OA patients have a mild-to-moderate valgus deformity, most of the force was still transmitted through the medial compartment [33]. Furthermore, they stated that predominant valgus moments were typically demonstrated by patients only if a severe valgus deformity was present. Conversely, it was found over 30 years later by the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative that patients–even those with mild-to-moderate valgus malalignment–demonstrated increased risk of lateral meniscus damage and lateral compartmental OA [23••]. Though not studied to the extent of varus malalignment, valgus malalignment may still have negative implications on the joint which must be considered at the time of certain lateral meniscal interventions.
Indications & Special Considerations
Whether an HTO is performed for a varus malalignment or a DFO for a valgus malalignment, it is generally accepted that there must be ≥ 5° of correctable deformity [13••,18], as correcting < 5° is technically challenging. If possible, the alignment correction and meniscus procedure should be performed in a one-stage setting to avoid the morbidity of two separate procedures and to immediately restore the biomechanical axis to provide the meniscus with the optimal environment to heal. If not possible, all bony work should be performed prior to soft tissue repair to prevent excessive contact pressures from placing stresses on the repair construct. Furthermore, any osteochondral defects amenable to surgical intervention should be addressed at the time of surgery, as failure to do so may result in clinical and/or anatomical failure of the meniscal procedure [13••].
Medial Meniscal Root Repair with High-Tibial Osteotomy
Medial meniscal root tears treated with partial meniscectomy have been shown to result in a progression to TKA in > 70% of patients and subjective failure in > 95% of patients at 10-year follow-up [34]. Poor clinical and radiographic outcomes have also been associated with nonoperative treatment of root tears [35], especially compared to operative treatment [10, 11].
Varus malalignment has been shown to lead to inferior outcomes following MMPRT repair [14••,21••,22•,36]. In a systematic review of 11 studies performed by Eseonu et al., it was found that baseline severity of varus malalignment was a predictor of poor functional outcomes in patients with medial meniscal root pathology [36, 37]. Additionally, preoperative varus alignment and persisting meniscal extrusion have been shown to be predictive of clinical failure and conversion to TKA at long-term follow-up [21••]. Lower extremity alignment closest to neutral correlates with improved patient outcomes [38]. Therefore, concomitant correction of varus malalignment with HTOs have been performed to restore a neutral mechanical axis thus protecting the medial meniscal intervention and preserving the medial compartment.
Medial Meniscal Allograft Transplantation with High-Tibial Osteotomy
The three indications for a meniscal transplant include (1) unicompartmental pain in a meniscus-deficient knee, (2) patients undergoing revision ACL reconstruction in the setting of an absent meniscus, and (3) post-meniscectomy increase in contact stress and decrease in joint-contact surface resulting in overloading and cartilage wear [39].
HTO in the setting of both MMATs and MMPRT repairs for patients with significant malalignment demonstrate results comparable to meniscal intervention in isolation in patients with neutral alignment [13–16••,20•,40,41]. In a matched case-control study performed by Grassi et al., concomitant HTO in the setting of MMAT with varus malalignment resulted in comparable failure rates and equivocal patient satisfaction compared to those who underwent an isolated MMAT without varus malalignment [14••]. Additionally, Lee et al. found that osteotomy in addition to MMAT resulted in less meniscal extrusion [42]. This finding implies that correcting varus malalignment results in the restoration of intra-articular biomechanics and further preserves the knee joint. Additional long-term studies (> 15–20 years) would offer insight into the longevity of medial meniscal interventions with concomitant HTOs as they compare to isolated medial meniscal surgery.
Lateral Meniscus Allograft Transplantation with Distal Femoral Osteotomy
There is a paucity of literature describing the detrimental clinical effects of valgus malalignment on meniscal preservation outcomes. However, given the understanding of normal knee biomechanics, kinematics, and load distribution, concomitant DFO in the setting of LMATs has been well-documented [43•,44]. In a small case series examining return to sports following concomitant LMAT and DFO, Puzzitiello et al. found that > 80% of patients were able to return to at least one sport postoperatively [43•]. In a similar study performed by Puzzitiello and colleagues looking at return to work, it was noted that in a young and active patient population undergoing LMAT and DFO the return-to-work rate was relatively high with most patients returning to work within three months [44]. However, patients with more physically demanding jobs took longer to return to work.
Case Examples
High Tibial Osteotomy and Medial Meniscal Allograft Transplantation
28-year-old male with a 2-year history of right knee pain, instability, and recurrent effusions. Significant medial joint line tenderness noted associated with catching and locking. Prior history of primary ACL reconstruction with hamstring tendon autograft and medial meniscus repair followed by a revision ACL reconstruction with bone-patellar tendon-bone (BTB) allograft and partial medial meniscectomy completed four months after the index procedure at an outside institution. Physical examination notes a slight varus alignment, tenderness to palpation on the medial joint line, and a 2 + Lachman and positive pivot shift.
Presenting radiographs demonstrated medial compartmental osteoarthritis with periarticular osteophytes (Fig. 1).
Fig. 1.

Standing AP radiograph of bilateral knees demonstrating medial joint space narrowing of the right knee (yellow arrow) compared to the left. Suture buttons from a previous ACL procedure noted on both the femur and tibia. The femoral tunnel is noted to be 10.9-mm wide, and the tibial tunnel is noted to be 11.9-mm wide
In addition to the confirmation of an ACL graft rupture, magnetic resonance imaging (MRI) demonstrates medial tibial plateau subchondral edema with normal lateral compartment cartilage as well as medial meniscal deficiency (Fig. 2).
Fig. 2.
Magnetic resonance imaging of the right knee demonstrating: (A) medial compartment subchondral edema of the medial tibial plateau with normal lateral compartment cartilage on the coronal, (B) medial compartment subchondral edema, and (C) medial meniscal deficiency on the sagittal views
Long leg standing (HKA) films were also obtained which demonstrated slight varus alignment of the right lower extremity compared to the left. A two-staged approach was planned with the first procedure consisting of bone grafting of the femoral and tibial tunnels, and a medial opening wedge high tibial osteotomy to offload the medial compartment [17, 18]. Postoperative long-leg films depict a 6° correction (Fig. 3).
Fig. 3.
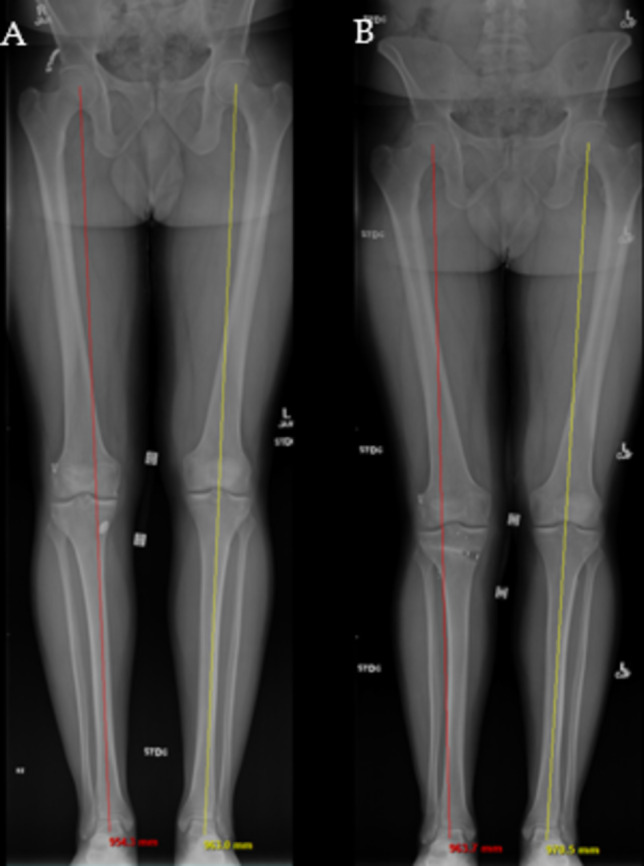
(A) Preoperative standing long films demonstrating a slight varus alignment (red line) of the right leg compared to neutral alignment (yellow line) of the left leg. (B) Postoperative long-leg radiographs after HTO demonstrating slight valgus alignment (red line) of the right leg compared to neutral alignment (yellow line) of the left leg
The second stage of the procedure was performed 9 months following the initial procedure and included ACL reconstruction with a BTB autograft, and an MMAT for medial meniscal deficiency (Fig. 4) [45].
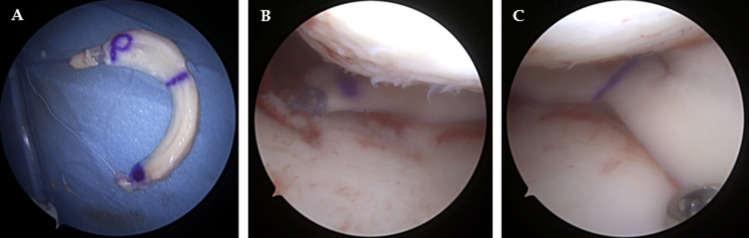
Fig. 4.
The medial meniscus allograft. (A) overhead view of the meniscal allograft with a posterior bone plug (P). (B) Arthroscopic view through the anterolateral portal of the medial compartment of the right knee posterior root fixation and (C) meniscal graft body fixation
High Tibial Osteotomy & Medial Meniscal Root Repair
16-year-old female volleyball and track athlete presenting with persistent instability and varus thrust. She has a history of posterior cruciate ligament (PCL) and posterolateral corner (PLC) reconstruction following a hyperextension injury during hurdles two years prior.
Physical examination demonstrated full ROM with a stable Lachman. There was tenderness to palpation along the posterior third of the medial joint line. There was a 2 + reverse Lachman, 2 + posterior drawer, 2 + positive posterior sag, and 2 + quad activation test. Dial test was symmetric at 30° but had about 10° of asymmetric opening at 90°. There was minimal laxity at 30° of flexion with varus stress, but a firm endpoint was noted. The LCL was palpable and taut in the figure-four position.
Radiographs demonstrated excessive tunnel/socket widening up to 15-mm. Long-leg films demonstrated 6° of varus malalignment (Fig. 5).
Fig. 5.

Standing long-films demonstrating 6° of varus alignment of the left leg compared to neutral alignment of the right leg
A two-stage approach was planned with the first procedure consisting of bone grafting of the femoral and tibial tunnels, and a medial opening wedge HTO to offload the medial compartment and prevent a varus thrust from the chronic PLC deficiency (Fig. 6) [17, 18].
Fig. 6.

Intraoperative fluoroscopy of the left knee following an opening wedge high tibial osteotomy
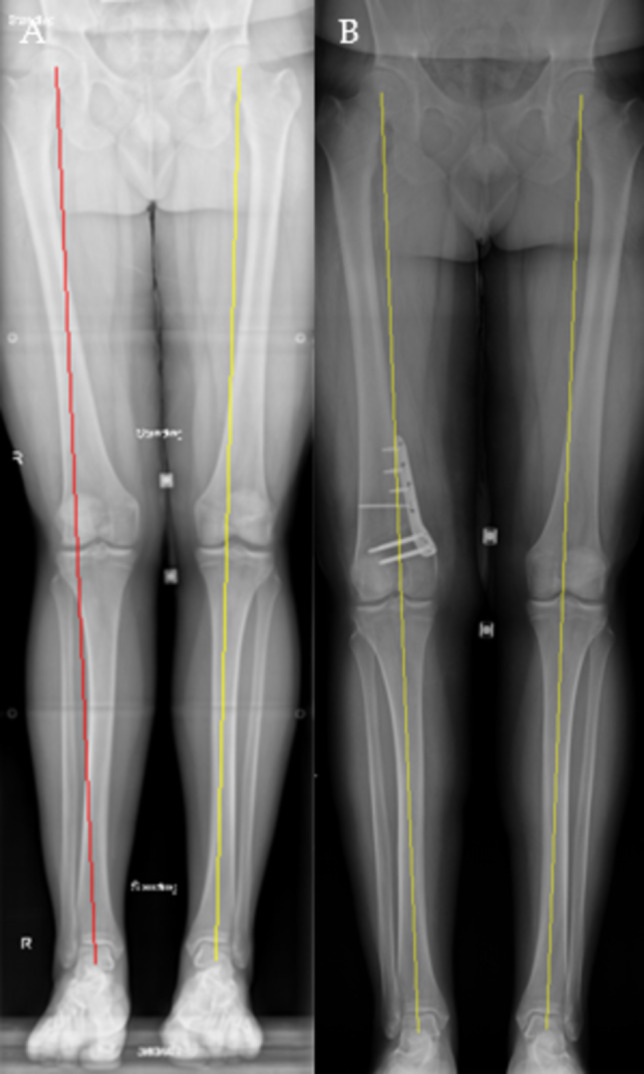
The second stage of the procedure was performed eight months following the initial procedure and included PCL reconstruction with an allograft, and a medial meniscal root repair (Fig. 7) [46, 47].
Fig. 7.
Arthroscopic view through the anterolateral portal of the medial compartment of the left knee demonstrating (A) a posterior root tear and (B) final fixation following repair using the transtibial pullout method
Distal Femoral Osteotomy & Lateral Meniscal Allograft Transplantation
22-year-old male who sustained a twisting injury to the right knee after being ejected from a motorcycle which was associated with knee pain, instability, and locking. Past surgical history positive for bilateral arthroscopic partial lateral meniscectomies and saucerizations. Additionally, it was noted that the patient has had several right knee injuries while playing basketball resulting in intermittent right knee pain and instability.
Physical examination demonstrated well-healed arthroscopy portals with no signs of infection, a mild 1 + effusion, 2 + Lachman with a soft endpoint, slight lateral pseudolaxity, and tenderness over the lateral joint line. Additionally, ROM was from full extension to 120° of knee flexion compared to full extension and 140° of knee flexion of the contralateral knee. The remainder of the exam was unremarkable. The patient was otherwise neurovascularly intact.
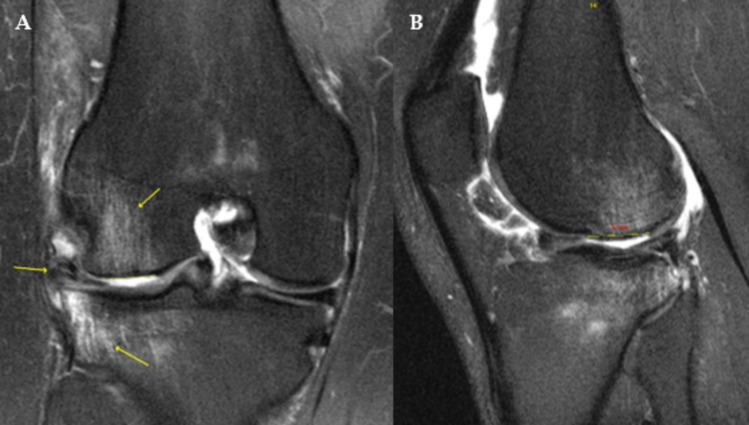
Radiographs on initial presentation were unremarkable. MRI of the right knee demonstrated injuries to the ACL and lateral meniscus, as well as subchondral edema on the lateral tibial plateau and lateral femoral condyle (LFC); furthermore, there was a chondral injury noted of the LFC (Fig. 8).
Fig. 8.
Magnetic resonance imaging of the right knee demonstrated disruption to the (A) lateral meniscus and anterior cruciate ligament with subchondral edema noted of the lateral tibial plateau and lateral femoral condyle on the coronal view, and a (B) 23-mm chondral injury noted on the sagittal view
HKA films demonstrated valgus malalignment of the right knee compared to the left (Fig. 9a). A two-stage procedure was planned with the first stage consisting of a diagnostic scope and a DFO. The second stage consisted of an ACL reconstruction, LMAT, and matrix-induced autologous chondrocyte implantation (MACI) of the lateral femoral condyle. Correction of the valgus malalignment was confirmed with postoperative HKA films (Fig. 9b).
Fig. 9.
(A) Long-leg films demonstrating valgus malalignment (red line) of the right leg compared to a slight varus (yellow line) left leg. (B) Postoperative long-leg films following an 8° varus-producing closing wedge distal femoral osteotomy
The lateral meniscal allograft can be visualized in Fig.10.
Fig. 10.

Overhead view of the lateral meniscal allograft prior to transplantation
The LMAT can be visualized in Fig. 11 [48].
Fig. 11.
Arthroscopic view through the (A) anteromedial portal demonstrating lateral meniscal deficiency. (B) Arthroscopic view through the anterolateral portal demonstrating a lateral meniscal allograft transplant following fixation
The MACI can be visualized in Fig. 12.
Fig. 12.

Intraoperative photograph demonstrating matrix-induced autologous chondrocyte implantation of the lateral femoral condyle
Concluding Remarks
There is much more to consider when addressing meniscus pathology than just the meniscus itself. To most adequately protect certain meniscal procedures such as posterior root repairs and MATs, knee alignment must be assessed and managed accordingly. In patients with significant varus malalignment with concomitant medial meniscal pathology necessitating either a root repair or an MAT, it is crucial to first correct the malalignment with an opening wedge HTO. Conversely, in the setting of considerable valgus malalignment with concomitant lateral meniscal pathology requiring a root repair or LMAT, it is important to also perform a varus-producing DFO.
There are other factors that may also need to be scrutinized at the time of alignment correction/meniscal procedures. These include the potential need to perform concomitant chondral procedures such as OCATs. Furthermore, in the setting of ligamentous injuries (i.e., ACL rupture), it is crucial to perform concomitant ACL reconstruction to restore stability. Failure to address ligamentous instability or chondral defects in addition to the knee malalignment will result in persistent abnormal anatomy of the knee and may jeopardize the success of the meniscal procedure which may ultimately accelerate the progression of osteoarthritis.
Key References
• Berk AN, Cregar WM, Wang S, et al. The Effect of Lower Limb Alignment on Tibiofemoral Joint Contact Biomechanics after Medial Meniscus Posterior Root Repair: A Finite-Element Analysis. J Am Acad Orthop Surg. 2024;32(11):e558-e567. doi:10.5435/JAAOS-D-23-00702.
Demonstrated that varus knees exhibited greater peak contact pressures and areas of local contact pressure which may reduce the effectiveness of root repair in delaying or preventing the development of medial compartmental OA.
• Deichsel A, Peez C, Raschke MJ, et al. Arthroscopic Centralization of the Medial Meniscus Reduces Load on a Posterior Root Repair Under Dynamic Varus Loading: A Biomechanical Investigation. Am J Sports Med. Published online September 15, 2024. doi:10.1177/03635465241274791.
Demonstrated that varus alignment resulted in increased forces acting on a posterior medial meniscal root repair.
•• Husen M, Poudel K, Wang A, et al. Survivorship of 157 Arthroscopic Meniscal Allograft Transplants Using Bone Fixation at a Mean of 7 Years and Prognostic Factors Analysis. Am J Sports Med. 2024;52(1):96–108. doi:10.1177/03635465231212667.
Demonstrated that MATs have a lasting beneficial effect both in isolation and in complex cases with ≥ 1 concurrent procedure including but not limited to osteotomies.
•• Grassi A, Lucidi GA, Di Paolo S, et al. Clinical Outcomes of Medial Meniscal Allograft Transplantation With or Without High Tibial Osteotomy: A Case-Control Study Up to 8 Years of Follow-up. Am J Sports Med. 2024;52(7):1813–1819. doi:10.1177/03635465241248822.
Demonstrated that surgically addressed malalignment does not represent a contraindication for MMAT.
•• Choi YS, Chang MJ, Lee JH, et al. Repair of medial meniscus posterior root tear is effective for root healing and cartilage regeneration in opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5799–5811. doi:10.1007/s00167-023-07637-z.
Demonstrated that medial meniscal posterior root tear repair in the setting of opening wedge HTO might improve root repair healing.
•• Liu JN, Agarwalla A, Garcia GH, et al. Return to Sport and Work After High Tibial Osteotomy With Concomitant Medial Meniscal Allograft Transplant. Arthroscopy. 2019;35(11):3090–3096. doi:10.1016/j.arthro.2019.05.053.
Demonstrated that HTO plus MMAT provided high rates of return to sports and return to work.
• Perry AK, Lavoie-Gagne O, Knapik DM, et al. Examining the Efficacy of Medial Meniscus Posterior Root Repair: A Meta-analysis and Systematic Review of Biomechanical and Clinical Outcomes. Am J Sports Med. 2023;51(7):1914–1926. doi:10.1177/03635465221077271.
Demonstrated that medial meniscal posterior root repair generally improved biomechanical outcomes and led to improved PROs with greater improvements noted in patients undergoing concomitant HTO.
•• Chung KS, Ha JK, Ra HJ, Kim JG. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4122–4130. doi:10.1007/s00167-020-06405-7.
Demonstrated that preoperative varus alignment and increased meniscal extrusion postoperatively were found to be predictive for a clinical failure after meniscal root repair at long-term follow-up.
• Lee DW, Lee SH, Kim JG. Outcomes of Medial Meniscal Posterior Root Repair During Proximal Tibial Osteotomy: Is Root Repair Beneficial?. Arthroscopy. 2020;36(9):2466–2475. doi:10.1016/j.arthro.2020.04.038.
Demonstrated that concurrent medial meniscal posterior root repair during HTO resulted in improved arthroscopic appearance during second-look arthroscopy.
•• Felson DT, Niu J, Gross KD, et al. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum. 2013;65(2):355–362. doi:10.1002/art.37726.
Demonstrated that valgus malalignment was associated with increased risk of disease progression in the lateral compartment including progressive lateral meniscal and cartilage damage.
• Puzzitiello RN, Liu JN, Garcia GH, et al. Return to Sport and Outcomes After Concomitant Lateral Meniscal Allograft Transplant and Distal Femoral Varus Osteotomy. Arthroscopy. 2020;36(1):253–260. doi:10.1016/j.arthro.2019.07.022.
Demonstrated that concomitant LMAT and DFO resulted in a high rate of return to sport as well as a significant decrease in VAS pain scores.
Author Contributions
A.V.D. wrote the main manuscript text and prepared all of the figures. A.J.W., L.E.B, A.D.C, A.S.K., and B.A.L. all reviewed, edited, and made additions to the manuscript.
Funding
No funding was received.
Data Availability
No datasets were generated or analysed during the current study.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing Interest
Bruce A. Levy has received consulting fees from Arthrex; nonconsulting fees from Arthrex and Smith+Nephew; royalties from Arthrex; and has stock/stock options in COVR Medical.Andrew D. Carbone has received funding grants from Arthrex and Medical Device Business Services Inc; speaking and lecture fees from Arthrex, Smith+Nephew, Medwest Associates Inc, Micromed Inc, and Saxum Surgical Inc.Abhishek S. Kannan has received consulting fees from Linvatec Corporation; and speaking and lecture fees from Arthrex.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Whiteside LA. Soft tissue balancing: the knee. J Arthroplasty. 2002;17(4 Suppl 1):23–7. 10.1054/arth.2002.33264. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Zeng Y, Dai K, Zhu Z, Xie L. Normal lower-extremity alignment parameters in healthy Southern Chinese adults as a guide in total knee arthroplasty. J Arthroplasty. 2010;25(4):563–70. 10.1016/j.arth.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Micicoi G, Jacquet C, Sharma A, et al. Neutral alignment resulting from tibial vara and opposite femoral valgus is the main morphologic pattern in healthy middle-aged patients: an exploration of a 3D-CT database. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):849–58. 10.1007/s00167-020-06030-4. [DOI] [PubMed] [Google Scholar]
- 4.Uquillas C, Rossy W, Nathasingh CK, Strauss E, Jazrawi L, Gonzalez-Lomas G. Osteotomies about the knee: AAOS exhibit selection. J Bone Joint Surg Am. 2014;96(24):e199. 10.2106/JBJS.N.00270. [DOI] [PubMed] [Google Scholar]
- 5.Fantini Pagani CH, Potthast W, Brüggemann GP. The effect of valgus bracing on the knee adduction moment during gait and running in male subjects with varus alignment. Clin Biomech (Bristol Avon). 2010;25(1):70–6. 10.1016/j.clinbiomech.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Reeves ND, Bowling FL. Conservative biomechanical strategies for knee osteoarthritis. Nat Rev Rheumatol. 2011;7(2):113–22. 10.1038/nrrheum.2010.212. [DOI] [PubMed] [Google Scholar]
- 7.Zhang L, Liu G, Han B et al. Knee Joint Biomechanics in Physiological Conditions and How Pathologies Can Affect It: A Systematic Review. Appl Bionics Biomech. 2020;2020:7451683. Published 2020 Apr 3. 10.1155/2020/7451683 [DOI] [PMC free article] [PubMed]
- 8.Berk AN, Cregar WM, Wang S, et al. The Effect of Lower Limb Alignment on Tibiofemoral Joint Contact Biomechanics after medial Meniscus posterior Root repair: a finite-element analysis. J Am Acad Orthop Surg. 2024;32(11):e558–67. 10.5435/JAAOS-D-23-00702. [DOI] [PubMed] [Google Scholar]
- 9.Deichsel A, Peez C, Raschke MJ et al. Arthroscopic Centralization of the Medial Meniscus Reduces Load on a Posterior Root Repair Under Dynamic Varus Loading: A Biomechanical Investigation. Am J Sports Med. Published online September 15, 2024. 10.1177/03635465241274791 [DOI] [PMC free article] [PubMed]
- 10.Krych AJ, Song BM, Nauert RF 3rd, et al. Prospective consecutive clinical outcomes after Transtibial Root repair for posterior meniscal Root tears: a Multicenter Study. Orthop J Sports Med. 2022;10(2):23259671221079794. 10.1177/23259671221079794. Published 2022 Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernard CD, Kennedy NI, Tagliero AJ, et al. Medial Meniscus posterior Root tear treatment: a matched cohort comparison of Nonoperative Management, partial meniscectomy, and repair. Am J Sports Med. 2020;48(1):128–32. 10.1177/0363546519888212. [DOI] [PubMed] [Google Scholar]
- 12.Ozeki N, Seil R, Krych AJ, Koga H. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS. 2021;6(1):35–45. 10.1136/jisakos-2019-000380. [DOI] [PubMed] [Google Scholar]
- 13.Husen M, Poudel K, Wang A, et al. Survivorship of 157 arthroscopic meniscal allograft transplants using bone fixation at a Mean of 7 years and prognostic factors analysis. Am J Sports Med. 2024;52(1):96–108. 10.1177/03635465231212667. [DOI] [PubMed] [Google Scholar]
- 14.Grassi A, Lucidi GA, Di Paolo S, et al. Clinical outcomes of Medial Meniscal Allograft Transplantation with or without high tibial osteotomy: a case-control study up to 8 years of follow-up. Am J Sports Med. 2024;52(7):1813–9. 10.1177/03635465241248822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi YS, Chang MJ, Lee JH, et al. Repair of medial meniscus posterior root tear is effective for root healing and cartilage regeneration in opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5799–811. 10.1007/s00167-023-07637-z. [DOI] [PubMed] [Google Scholar]
- 16.Liu JN, Agarwalla A, Garcia GH, et al. Return to Sport and work after high tibial osteotomy with concomitant medial meniscal allograft transplant. Arthroscopy. 2019;35(11):3090–6. 10.1016/j.arthro.2019.05.053. [DOI] [PubMed] [Google Scholar]
- 17.Keyt LK, Hevesi M, Levy BA, Krych AJ, Camp CL, Stuart MJ. High tibial osteotomy with a modern polyetheretherketone (PEEK) System: mid-term results at a Mean of 6 years Follow-Up. J Knee Surg. 2022;35(8):916–21. 10.1055/s-0040-1721090. [DOI] [PubMed] [Google Scholar]
- 18.Hevesi M, Macalena JA, Wu IT, et al. High tibial osteotomy with modern PEEK implants is safe and leads to lower hardware removal rates when compared to conventional metal fixation: a multi-center comparison study. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1280–90. 10.1007/s00167-018-5329-0. [DOI] [PubMed] [Google Scholar]
- 19.Husen M, Wang AS, Levy BA, Saris DBF, Stuart MJ, Krych AJ. Influence of concomitant meniscal allograft transplantation on Midterm outcomes after Osteochondral Allograft transplantation: a comparative matched-pair analysis. Am J Sports Med. 2024;52(5):1238–49. 10.1177/03635465241234534. [DOI] [PubMed] [Google Scholar]
- 20.Perry AK, Lavoie-Gagne O, Knapik DM, et al. Examining the efficacy of medial Meniscus posterior Root repair: a Meta-analysis and systematic review of Biomechanical and Clinical outcomes. Am J Sports Med. 2023;51(7):1914–26. 10.1177/03635465221077271. [DOI] [PubMed] [Google Scholar]
- 21.Chung KS, Ha JK, Ra HJ, Kim JG. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4122–30. 10.1007/s00167-020-06405-7. [DOI] [PubMed] [Google Scholar]
- 22.Lee DW, Lee SH, Kim JG. Outcomes of medial meniscal posterior Root Repair during Proximal Tibial Osteotomy: is Root Repair Beneficial? Arthroscopy. 2020;36(9):2466–75. 10.1016/j.arthro.2020.04.038. [DOI] [PubMed] [Google Scholar]
- 23.Felson DT, Niu J, Gross KD, et al. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum. 2013;65(2):355–62. 10.1002/art.37726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fu FF, Thompson WO. Motion of the meniscus during knee flexion. In: Mow VC, Arnoczky SP, Jackson DW, editors. Knee Meniscus: Basic and Clinical foundations. New York: Raven Press, Ltd; 1992. pp. 75–89. [Google Scholar]
- 25.Duethman NC, Bernard CD, Camp CL, Krych AJ, Stuart MJ. Medial closing wedge distal femoral osteotomy. Clin Sports Med. 2019;38(3):361–73. 10.1016/j.csm.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Michalska-Foryszewska A, Modzelewski P, Sklinda K, Mruk B, Walecki J. Radiological Approach to Assessment of Lower-Limb alignment-coronal and transverse plane analysis. J Clin Med. 2024;13(22):6975. 10.3390/jcm13226975. Published 2024 Nov 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu X, Chen Z, Gao Y, Zhang J, Jin Z. High tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. 2019;2019:8363128. 10.1155/2019/8363128. Published 2019 May 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):197–205. 10.1007/s00167-012-2122-3. [DOI] [PubMed] [Google Scholar]
- 29.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470(1):45–53. 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–9. 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 31.Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, Bergmann G. Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am. 2012;94(11):1023–9. 10.2106/JBJS.K.00927. [DOI] [PubMed] [Google Scholar]
- 32.Dugdale TW, Noyes FR, Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res. 1992;(274):248–64. [PubMed]
- 33.Johnson F, Leitl S, Waugh W. The distribution of load across the knee. A comparison of static and dynamic measurements. J Bone Joint Surg Br. 1980;62(3):346–9. 10.1302/0301-620X.62B3.7410467. [DOI] [PubMed] [Google Scholar]
- 34.Lamba A, Regan C, Levy BA, Stuart MJ, Krych AJ, Hevesi M. Long-term outcomes of partial meniscectomy for degenerative medial Meniscus posterior Root tears. Orthop J Sports Med. 2024;12(9):23259671241266593. 10.1177/23259671241266593. Published 2024 Sep 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krych AJ, Lamba A, Wang AS, et al. Nonoperative Management of degenerative medial Meniscus posterior Root tears: poor outcomes at a minimum 10-Year follow-up. Am J Sports Med. 2023;51(10):2603–7. 10.1177/03635465231185132. [DOI] [PubMed] [Google Scholar]
- 36.Eseonu KC, Neale J, Lyons A, Kluzek S. Are outcomes of Acute Meniscus Root tear Repair Better Than Debridement or Nonoperative Management? A systematic review. Am J Sports Med. 2022;50(11):3130–9. 10.1177/03635465211031250. [DOI] [PubMed] [Google Scholar]
- 37.Jiang EX, Abouljoud MM, Everhart JS, et al. Clinical factors associated with successful meniscal root repairs: a systematic review. Knee. 2019;26(2):285–91. 10.1016/j.knee.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 38.Ridley TJ, Ruzbarsky JJ, Dornan GJ, et al. Minimum 2-Year clinical outcomes of Medial Meniscus Root tears in relation to coronal alignment. Am J Sports Med. 2022;50(5):1254–60. 10.1177/03635465221080167. [DOI] [PubMed] [Google Scholar]
- 39.Getgood A, LaPrade RF, Verdonk P, et al. International Meniscus Reconstruction experts Forum (IMREF) 2015 Consensus Statement on the practice of Meniscal Allograft Transplantation. Am J Sports Med. 2017;45(5):1195–205. 10.1177/0363546516660064. [DOI] [PubMed] [Google Scholar]
- 40.Harris JD, Cavo M, Brophy R, Siston R, Flanigan D. Biological knee reconstruction: a systematic review of combined meniscal allograft transplantation and cartilage repair or restoration. Arthroscopy. 2011;27(3):409–18. 10.1016/j.arthro.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 41.Harris JD, McNeilan R, Siston RA, Flanigan DC. Survival and clinical outcome of isolated high tibial osteotomy and combined biological knee reconstruction. Knee. 2013;20(3):154–61. 10.1016/j.knee.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 42.Lee DW, Kang SJ, Kim RJ, et al. Clinical and radiological outcomes of Medial Meniscal Allograft Transplantation Combined with Realignment surgery. Am J Sports Med. 2024;52(9):2260–9. 10.1177/03635465241255346. [DOI] [PubMed] [Google Scholar]
- 43.Puzzitiello RN, Liu JN, Garcia GH, et al. Return to Sport and outcomes after concomitant lateral meniscal allograft transplant and distal femoral Varus Osteotomy. Arthroscopy. 2020;36(1):253–60. 10.1016/j.arthro.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 44.Puzzitiello RN, Liu JN, Garcia GH, et al. Return to work after distal femoral Varus Osteotomy. Orthop J Sports Med. 2020;8(12):2325967120965966. 10.1177/2325967120965966. Published 2020 Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ow ZGW, Cheong CK, Hai HH, et al. Securing transplanted Meniscal allografts using bone plugs results in Lower risks of Graft failure and reoperations: a Meta-analysis. Am J Sports Med. 2022;50(14):4008–18. 10.1177/03635465211042014. [DOI] [PubMed] [Google Scholar]
- 46.Krych AJ, Bernard CD, Kennedy NI, et al. Medial versus lateral Meniscus Root tears: is there a difference in Injury Presentation, Treatment decisions, and Surgical Repair outcomes? Arthroscopy. 2020;36(4):1135–41. 10.1016/j.arthro.2019.11.098. [DOI] [PubMed] [Google Scholar]
- 47.Blackman AJ, Stuart MJ, Levy BA, McCarthy MA, Krych AJ. Arthroscopic meniscal Root Repair using a Ceterix NovoStitch suture Passer. Arthrosc Tech. 2014;3(5):e643–6. 10.1016/j.eats.2014.07.006. Published 2014 Oct 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Woodmass JM, Johnson NR, Levy BA, Stuart MJ, Krych AJ. Lateral Meniscus allograft transplantation: the Bone Plug technique. Arthrosc Tech. 2017;6(4):e1215–20. 10.1016/j.eats.2017.04.016. Published 2017 Aug 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.