Abstract
Background
Ferroptosis is involved in the occurrence and development of inflammatory arthritis. RND1 has been reported to possess pro-ferroptosis activity.
Objective
This study was designed to explore the role and the molecular mechanism of RND1 in rheumatoid arthritis (RA).
Methods
DBA/1 mice were exposed to type II collagen immunization. The pathological damage of the knee joints of mice was observed with H&E staining and RND1 expression in synovial tissues was detected using Western blot. In vitro, Western blot was used to measure RND1, ferroptosis-, migration- and inflammation-related proteins. The cell proliferation, migration and invasion were detected using CCK-8 method, EdU staining, wound healing and transwell assays. The levels of inflammatory factors were detected with ELISA and RT-qPCR. Relative iron level, GSH and MDA concentrations were detected with corresponding assay kits. BODIPY 581/591 C11 kit measured lipid ROS. 4-HNE and GPX4 expression were detected using immunofluorescence assay.
Results
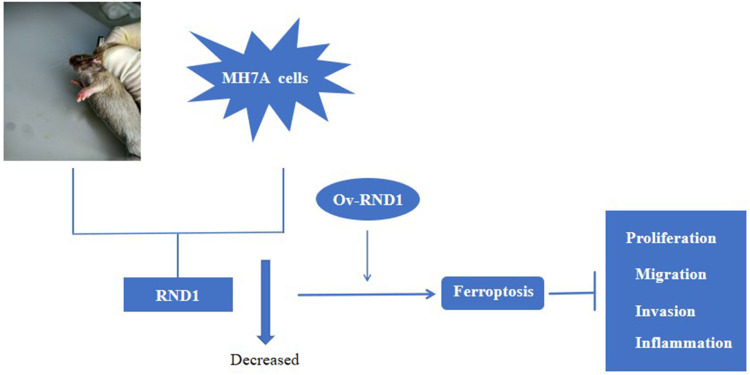
This study found that RND1 expression was reduced in the synovial tissues of RA mice and human fibroblast-like MH7A synoviocytes. It was also found that the upregulation of RND1 inhibited the proliferation, migration, invasion and inflammatory response in rheumatoid synovial cells via ferroptosis.
Conclusion
Collectively, RND1 exerted protective impacts on RA, which might be mediated by ferroptosis.
Keywords: rheumatoid arthritis, RND1, ferroptosis, fibroblast-like synoviocytes
Graphical Abstract
Introduction
As a chronic and systemic autoimmune disease, rheumatoid arthritis (RA) is characterized by continuous inflammation of the synovial joints, which leads to the proliferation of synovial tissues, the erosion of cartilage and consequent deformation of joints.1,2 It has been reported that RA fibroblast-like synoviocytes (RA-FLSs), which are proliferating cells similar to tumor cells, can cause abnormal synovial hyperplasia in patients when its viability is increased.3,4 In addition, existing researches have supported that the abnormal proliferation and apoptosis of FLSs are the primary pathological foundation of persistent synovitis and bone destruction.5,6 Therefore, RA-FLSs have been perceived as promising targeting cells to treat RA attributed to its biology.4
Ferroptosis, a type of regulatory cell death dependent on the aggregation of intracellular iron, is characterized by iron deposition, lipid peroxidation, GSH reduction, and GPX4 inactivation.7 Extensive researches have showed that ferroptosis, a significant regulatory factor in inflammatory responses, is closely associated with the initiation and progression of various inflammatory arthritis including RA and the induction of ferroptosis can inhibit synovium inflammation in RA.8,9 Iron can be extensively found in the synovium of patients with RA, thus facilitating inflammatory response.10,11 Furthermore, ferroptosis is an important event in synovium injury in RA and ferroptosis modulation in synovial cells is effective for RA treatment.12
It is reported that Rho family GTPase 1 (RND1) is expressed in various cells, including cancer cells13, cardiomyocytes14 and endothelial cells.14 RND1 is involved in many cellular activities, including cell proliferation, invasion and ferroptosis.15,16 Of note, RND3, which is a member of RND family, is lowly expressed in RA-FLSs and RND3 elevation can inhibit the proliferation, migration, invasion and inflammatory response in RA-FLSs.17 Moreover, according to rheumatoid arthritis dataset (GSE55457), RND1 expression is reduced in RA tissues. However, the role of RND1 in RA is unknown and whether RND1 can participate in inflammation, proliferation, migration and invasion in RA-FLSs via inducing ferroptosis yet to be investigated.
All in all, this study explored the role of RND1 in inflammation, proliferation, migration, invasion and ferroptosis in RA-FLSs and revealed the relevant molecular mechanisms, which might provide novel therapeutic targets for the treatment of RA.
Materials and Methods
Collagen-Induced Arthritis (CIA) Models
The animal experiments were performed under a project license (No. AHGDMU-LAC-A-202403-066) issued by the Ethics Committee of the Affiliated Hospital of Guangdong Medical University. Animal welfare and all experiments were approved by the Institutional Animal Care and Use Committee of the Affiliated Hospital of Guangdong Medical University. The male DBA/1 mice were obtained from Changzhou Cavens Laboratory Animals Technology Co., Ltd., (China). For acclimatization, the mice were housed in clean cages with a 12 h light/dark cycle and 44%-65% humidity. Mice were divided into two groups (n=6): Control and CIA. Mice were immunized subcutaneously at the base of the tail with 100 μL of bovine type II collagen (2 mg/mL) dissolved in 0.01 M acetic acid emulsified 1:1 with complete Freund’s adjuvant (Thermo Fisher Scientific). After 21 days, the mice were subcutaneously injected with 50 μg of bovine type II collagen emulsified 1:1 with incomplete Freund’s adjuvant (Thermo Fisher Scientific). On the 45th day, mice were sacrificed through cervical dislocation and the keen joints of mice were collected for subsequent analysis.
Cell Culture and Treatment
The normal human FLSs (cat. CP-H241) and human fibroblast-like MH7A synoviocytes (cat. no. CP-H248) were procured from BeNa Culture Collection and incubated in DMEM supplemented with 10% FBS and 1% penicillin-streptomycin at 37°C with 5% CO2. To explore the mechanism of RND1 associated with ferroptosis in RA, ferroptosis inhibitors Fer-1 (1 μM) or DFO (100 μM) were used to treat fibroblast-like MH7A synoviocytes.
Cell Transfection
To increase RND1 expression, plasmids carrying RND1 (Ov-RND1) and pcDNA3.1 empty vector (Ov-NC) were constructed by GenePharma (Shanghai, China). When cell confluence reached 70%, the plasmids were transfected into MH7A cells using Lipofectamine 3000 Transfection Reagent for 48 h according to the manufacturer’s instructions. After 48 h, MH7A cells were harvested for follow-up experiments.
H&E Staining
The collected knee joints of mice were fixed with 10% formalin, decalcified in 10% formic acid at 37°C for 1 week with shaking, embedded in paraffin and then cut into 5-μm-thick sections. Subsequently, processed sections were exposed to H&E staining according to the manufacturer’s instructions and a fluorescence microscope was used for observation.
Western Blot
The proteins were extracted from the collected synovial tissues and MH7A cells with RIPA buffer. The protein concentration was determined using BCA assay kits according to the manufacturer’s instructions. Separated by 8% SDS-PAGE, the proteins were transferred to PVDF membranes. Inhibited by 5% BSA, the membranes were incubated with primary antibodies specific to RND1, GPX4, ACSL4, SLC7A11, MMP2, MMP9, p-p65, p65, COX2, or GAPDH overnight at 4°C. On the next day, the membranes were incubated with HRP-conjugated anti-rabbit IgG secondary antibodies at room temperature for 2 h. The protein bans were visualized using ECL detection reagent and the grey values were determined with ImageJ software (version 1.49; National Institutes of Health).
Immunohistochemical Analysis
The collected synovial tissues were processed in 5-μm-thick sections, fixed in 4% methanol at 4°C for 24 h, washed by PBS and then treated with retrieval solution for 20 min at 90°C.18 Inhibited by 5% BSA, the sections were incubated with GPX4 primary antibody overnight at 4°C. On the next day, the sections were incubated with HRP-conjugated anti-rabbit IgG secondary antibody at room temperature for 1 h. Hematoxylin solution was used for nuclear staining for 5 min at room temperature. Finally, the images were observed using an Olympus CX43 microscope.
RT-qPCR
The total RNA was extracted from MH7A cells using Trizol reagent, and then reverse transcription into cDNA using PrimeScript RT kit according to the manufacturer’s instructions. The real-time PCR was performed with an ABI 7900HT Sequence Detection system. The relative gene expression was determined using the 2−ΔΔCt method.
CCK-8 Assay
The fibroblast-like MH7A synoviocytes were inoculated into 96-well plates for incubation. Thereafter, each well was added with 10 μL CCK-8 reagent and cells were incubated for additional 3 h at 37 °C. The absorbance was determined at 450 nm with a microplate reader.
EdU Staining
The fibroblast-like MH7A synoviocytes were injected into 6-well plates for incubation. Each well was supplemented with 10 µM EdU solution to incubate cells for another 2 h. Following the staining with DAPI, a fluorescence microscope was used for observation.
Wound Healing
The fibroblast-like MH7A synoviocytes were injected into 6-well plates and incubated till 80–90% cell confluence was obtained. The wounds were created using a sterile pipette tip. Subsequently, the cells were incubated for 24 h. The cell images were observed with a light microscope and ImageJ software was used for the analysis of cell migration rate.
Transwell
The fibroblast-like MH7A synoviocytes were injected into the upper chamber of the transwell with Matrigel gel treatment while DMEM supplemented with 10% FBS were placed on the lower chamber of the transwell, followed by the incubation for 24 h. The uninvaded cells were removed while the invaded cells were fixed with 4% paraformaldehyde and stained by crystal violet. A light microscope was used for the observation of cell invasion and the number of invaded cells was analyzed.
Elisa
The fibroblast-like MH7A synoviocytes were centrifuged at 2000 x g for 4 min at 4°C. The levels of TNF-α, IL-1β and IL-6 in the culture supernatant were detected using ELISA-related TNFα assay kits, IL-1β assay kits and IL-6 assay kits according to the manufacturer’s instructions.
Measurement of Iron, MDA and GSH
The relative iron, MDA and GSH concentration in cell lysates were detected using iron assay kits, MDA assay kits, and GSH assay kits according to the manufacturer’s instructions.
Detection of Lipid ROS
We used BODIPY 581/591 C11 kits to detect lipid ROS. In brief, the fibroblast-like MH7A synoviocytes were trypsinized and re-suspended in 400 µL of serum-free medium containing 2 μM C11-BODIPY (581/591) in the dark. Subsequently, the cells were labeled with Hoechst nuclear staining and then washed by PBS. The cell images were observed using a laser scanning confocal microscope and the fluorescence ratio of green/red was detected using ImageJ software.
Immunofluorescence Assay
The fibroblast-like MH7A synoviocytes were fixed with 4% paraformaldehyde and permeated with 0.2% Triton X-100 for 10 min. Then, the cells were incubated with primary antibodies targeting 4-HNE, GPX4, goat anti-rabbit IgG and goat anti-mouse IgG. DAPI was used for cell nucleus staining and a fluorescence microscope was used for observation.
Statistical Analysis
The experimental data were presented as mean ± SD after the statistical analysis with GraphPad Prism 8.0 software (GraphPad software, Inc). The differences among groups were demonstrated with Student’s t-test (for two groups) and one-way ANOVA with Tukey’s post hoc test (for three or more groups). P-values ≤ 0.05 were indicative of statistical significance.
Results
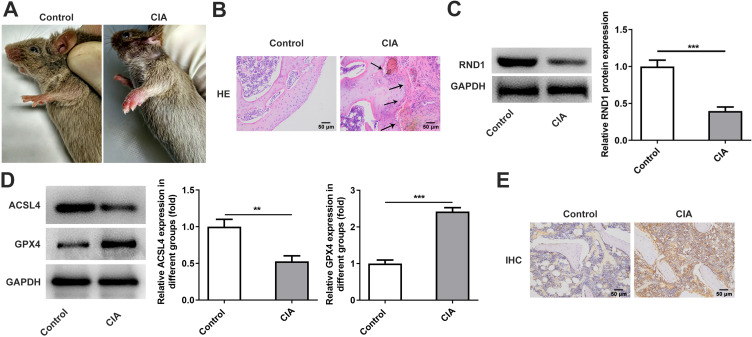
RND1 Expression Is Downregulated in the Joint Tissues of RA Mice
As Figure 1A depicted, the frontpaws of CIA mice exhibited serious swelling of the paws and all digits. H&E staining was used to observe the histological changes of the keen joints of CIA mice. Obviously, synovial hyperplasia with a quantity of infiltrating inflammatory cells was observed, pannus was formed and cartilage and bone were seriously destructed (Figure 1B). The protein expression of RND1 in synovial tissues was detected with Western blot and it was found that RND1 expression was significantly reduced in CIA mice (Figure 1C). Besides, Western blot was used to detect the expressions of ferroptosis-related proteins and it was found that GPX4 expression was increased in CIA mice while ACSL4 expression was significantly decreased (Figure 1D). Moreover, the results of immunohistochemical analysis for GPX4 showed that GPX4 expression was significantly increased in CIA mice (Figure 1E).
Figure 1.
RND1 expression is downregulated in the joint tissues of RA mice. (A) The symptoms of CIA mice were observed. (B) The pathological features of the keen joints of CIA mice were detected using H&E staining. The black arrows point to the pannus. (C) The protein expression of RND1 in synovial tissues of CIA mice was detected using Western blot. (D) The expressions of ferroptosis-related proteins were detected using Western blot. (E) Immunohistochemical analysis for GPX4. **P<0.01 and ***P<0.001.
RND1 Expression Is Downregulated in RA-FLSs
The expression of RND1 was also detected in rheumatoid synovial cells in vitro using RT-qPCR and Western blot. Similarly, the mRNA and protein expressions of RND1 in RA-FLSs were significantly decreased (Figure 2A). The expressions of proteins implicated in ferroptosis (GPX4 and SLC7A11) were also investigated and the results showed that GPX4 and SLC7A11 expressions were significantly elevated in RA-FLSs (Figure 2B).
Figure 2.
RND1 expression is downregulated in RA-FLSs. (A) The mRNA and protein expressions of RND1 in RA-FLSs were detected using RT-qPCR and Western blot. (B) The expressions of ferroptosis-related proteins were detected using Western blot. **P<0.01 and ***P<0.001.
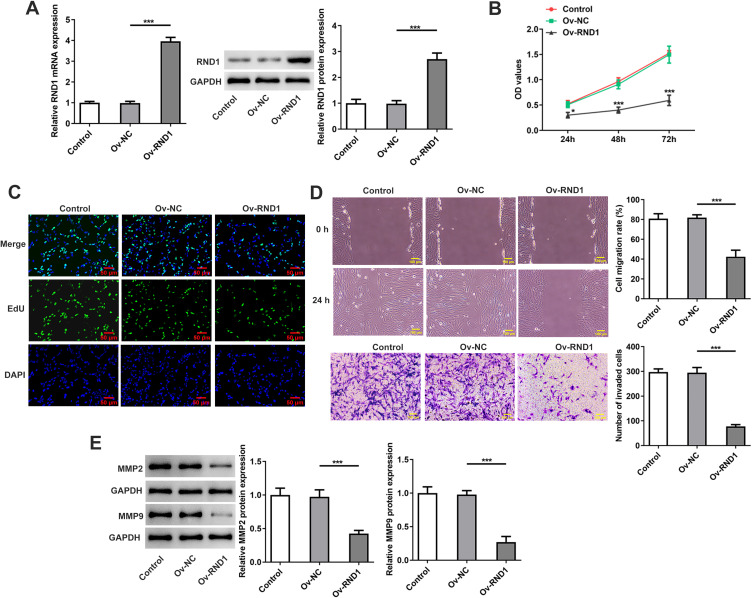
RND1 Overexpression Inhibits the Proliferation, Migration and Invasion in RA-FLSs
We transfected Ov-RND1 into FA-FLSs and RT-qPCR and Western blot were used to detect RND1 expression. It was found that RND1 expression was significantly increased in RND1-overexpressed FA-FLSs (Figure 3A). In RA pathogenesis, activated RA-FLSs show similar proliferating and invasive characteristics with tumor cells, which eventually leads to aberrant hyperplasia and joint damage.19 To explore the role of RND1 in the proliferation, migration and invasion in RA, Ov-RND1 was transfected into RA-FLSs and relevant assays were performed. It was found that RND1 overexpression significantly reduced the viability and the proliferation of RA-FLSs (Figure 3B and C). Similarly, the migration and invasion of RA-FLSs were significantly inhibited after overexpressing RND1 (Figure 3D). MMPs are critical mediators in wound healing.20 Results of Western blot showed that the protein expressions of MMP2 and MMP9 in RA-FLSs were increased by RND1 elevation (Figure 3E).
Figure 3.
RND1 overexpression inhibits the proliferation, migration and invasion in RA-FLSs. (A) The transfection efficacy of Ov-RND1 was detected using RT-qPCR and Western blot. (B) The cell viability was detected using CCK-8 assay. (C) The cell proliferation was detected using EdU staining. (D) The cell migration and invasion were detected using wound healing and transwell. (E) The expressions of MMP2 and MMP9 were detected using Western blot. *P<0.05 and ***P<0.001.
RND1 Overexpression Inhibits the Inflammatory Release in RA-FLSs
The continuous inflammation in damaged joints can pathogenically change cell activity in RA.21 The effects of RND1 upregulation on the release of inflammatory factor were detected with ELISA and RT-qPCR. It was found that the levels of TNF-α, IL-1β and IL-6 in RA-FLSs were significantly decreased following the transfection of Ov-RND1 (Figure 4A and B). Western blot was used for the detection of inflammation-implicated proteins and it was found that RND1 overexpression significantly decreased the expressions of p-p65 and COX2 (Figure 4C).
Figure 4.
RND1 overexpression inhibits the inflammatory release in RA-FLSs. (A) The levels of inflammatory factors were detected using ELISA. (B) The mRNA expressions of inflammatory factors were detected using RT-qPCR. (C) The expressions of inflammation-related proteins were detected using Western blot. ***P<0.001.
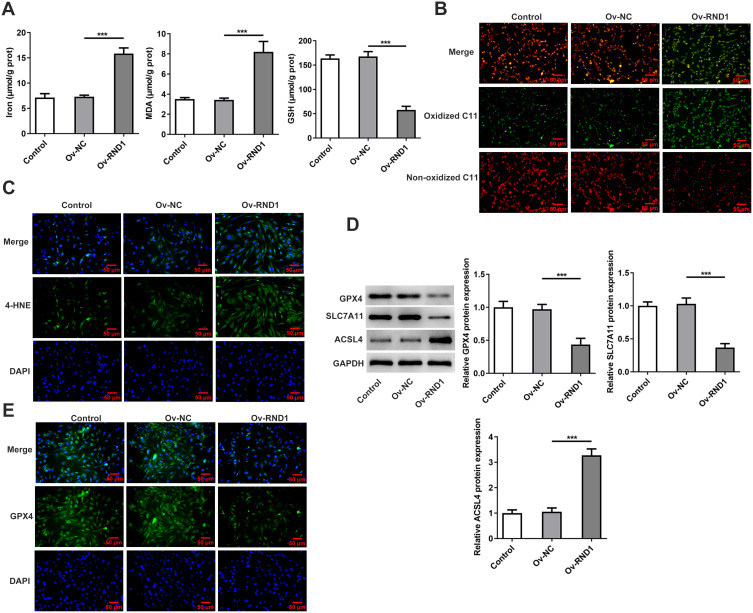
RND1 Overexpression Promotes Ferroptosis in RA-FLSs
The role of ferroptosis has been highlighted in inflammatory arthritis pathogenesis.22 Compared with the Ov-NC group, RND1 overexpression significantly increased iron level and MDA concentration whereas it reduced GSH concentration in RA-FLSs (Figure 5A). Results of BODIPY 581/591 C11 kits showed that the bound to peroxidized lipids turned into green fluorescence, indicating that RND1 overexpression increased the fluorescent intensity in RA-FLSs (Figure 5B). Besides, the level of 4-HNE, which is a stable product of lipid peroxidation, was also increased by RND1 elevation (Figure 5C). Additionally, the overexpression in RND1 decreased GPX4 and SLC7A11 expressions while increasing ACSL4 expression in RA-FLSs (Figure 5D). Moreover, GPX4 intensity in RA-FLSs was significantly decreased after overexpressing RND1 (Figure 5E).
Figure 5.
RND1 overexpression promotes ferroptosis in RA-FLSs. (A) The iron level and MDA and GSH concentrations were detected using corresponding assay kits. (B) The lipid ROS was detected using BODIPY 581/591 C11 kit. (C) 4-HNE expression was detected using immunofluorescence assay. (D) The expressions of ferroptosis-related proteins were detected using Western blot. (E) The GPX4 expression was detected using immunofluorescence assay. ***P<0.001.
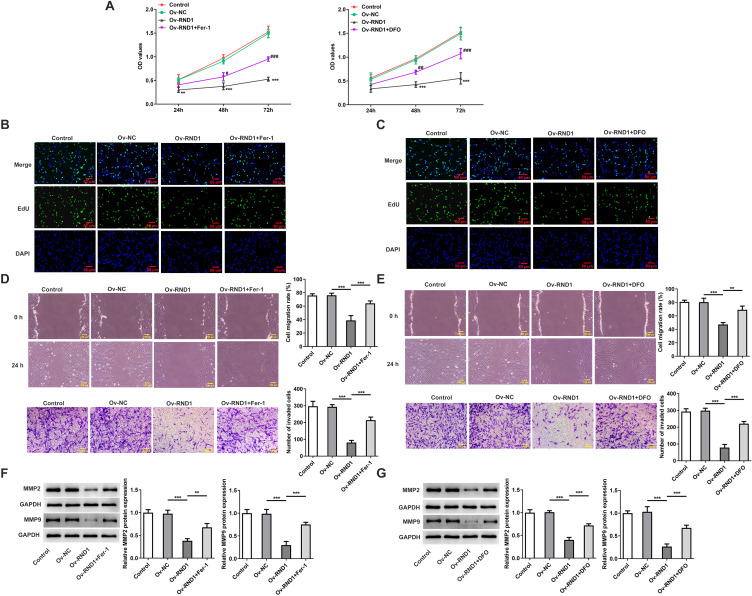
RND1 Overexpression Inhibits the Proliferation, Migration and Invasion in RA-FLSs via Ferroptosis
To investigate the mechanism of RND1 related with ferroptosis in RA, RA-FLSs were transfected with Ov-RND1 and treated with ferroptosis inhibitor Fer-1 or DFO. It was found that the reduced cell viability and proliferation in RA-FLSs due to RND1 overexpression were partially revived following the pre-treatment of Fer-1 or DFO (Figure 6A–C). Consistently, Fer-1 or DFO pre-treatment also promoted the inhibited migration and invasion of RND1-overexpressed RA-FLSs (Figure 6D and E). Furthermore, the decreased expressions of MMP2 and MMP9 in RA-FLSs because of RND1 overexpression were partially increased following the pre-treatment of Fer-1 or DFO (Figure 6F and G).
Figure 6.
RND1 overexpression inhibits the proliferation, migration and invasion in RA-FLSs via ferroptosis. (A) The cell viability was detected using CCK-8 assay. (B and C) The cell proliferation was detected using EdU staining. (D and E) The cell migration and invasion were detected using wound healing and transwell. (F and G) The expressions of MMP2 and MMP9 were detected using Western blot. **P<0.01 and ***P<0.001, #P<0.01 ##P<0.01 and ###P<0.001.
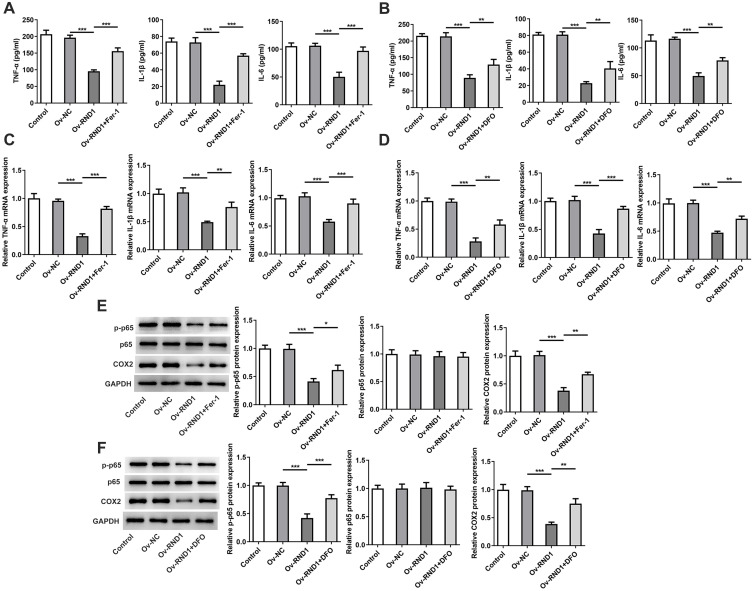
RND1 Overexpression Inhibits the Inflammatory Release in RA-FLSs via Ferroptosis
Results of ELISA and RT-qPCR showed that the pre-treatment of Fer-1 or DFO increased the levels of TNF-α, IL-1β and IL-6 in RA-FLSs with RND1 overexpression (Figure 7A–D). Moreover, the reduced protein expressions of p-p65 and COX2 in RA-FLSs due to RND1 overexpression were partially increased by Fer-1 or DFO treatment (Figure 7E and F).
Figure 7.
RND1 overexpression inhibits the inflammatory release in RA-FLSs via ferroptosis. (A and B) The levels of inflammatory factors were detected using ELISA. (C and D) The mRNA expressions of inflammatory factors were detected using RT-qPCR. (E and F) The expressions of inflammation-related proteins were detected using Western blot. *P<0.05, **P<0.01 and ***P<0.001.
Discussion
RA is an autoimmune disease characterized by proliferated synovial tissues and infiltrated inflammatory cells, eventually leading to the severe destruction of cartilage and bone and the swelling and the dysfunction of joints.23 During RA development, FLSs in synovium turn into aggressive phenotypes and generate pathogenic factors, making synovial tissues become hyperplastic invasiveness.24 The present study showed that RND1 expression was significantly decreased in the synovial tissues of CIA mice and RA-FLSs. RND1 elevation alleviated the severity of RA via inhibiting the proliferation, migration and invasion of RA-FLSs. Mechanistically, RND1 overexpression inhibited the development of RA through the induction of ferroptosis.
CIA, which is a major investigated animal mode, possesses various pathological and immunological features showing similarities with human RA.25 Thus, we also established CIA mice models in this research and serious swelling of the paws and all digits of CIA mice, synovial hyperplasia, pannus formation and the destruction of cartilage and bone in keen joints could be observed. FLSs, a type of unique cells in synovium, are critical modulators in RA pathogenesis.6 The activated FLSs manifest strong invasiveness and migration ability, increased proliferation and anti-apoptotic property.26 Additionally, FLSs stimulate inflammatory response via promoting the release of pro-inflammatory cytokines, MMPs, and chemokines.27 Thence, targeting the hyper-activation of pathogenic FLSs might be a prospective method for RA relieve.
RA is an inflammatory disease characterized by excessive production of pro-inflammatory factors. Kondo et al have corroborated that TNFα and IL-6 levels were significantly increased in the synovial fluid and serum of patients with RA, which are critical regulators in RA pathogenesis.25 More importantly, extensive researches have elucidated that inflammatory cytokines in RA-FLSs exert regulatory effects on the proliferation and migration of RA-FLSs.28 Therefore, inhibiting the inflammatory response, the proliferation, migration and invasion in RA-FLSs may be a promising method to ameliorate RA. It is reported that RND1 can inhibit cell proliferation, migration and invasion in hepatocellular carcinoma.29 Cao et al have evidenced that RND1 plays an important role in inflammation.30 Of note, RND3, which is a member of the RND family, is supported to suppress the inflammation, proliferation, invasion and migration in RA-FLSs when its expression is overexpressed.17 Our data found that RND1 overexpression could inhibit the proliferation, migration, invasion and inflammatory response in RA-FLSs, accompanied by decreased MMP2 and MMP9 expressions, reduced levels of pro-inflammatory cytokines TNF-α, IL-1β and IL-6 and decreased expressions of inflammation-related proteins p-p65 and COX2.
Ferroptosisin, which is characterized by excessive iron accumulation and lipid peroxidation, plays an important role in the pathogenesis of inflammatory arthritis.31 Some antirheumatic drugs, such as sulfasalazine and auranofin, demonstrate ferroptosis-regulatory effects, revealing that the modulatory mechanism of ferroptosis in inflammatory arthritis pathogenesis and ferroptosis-targeted treatment modalities deserve further exploration.32 In the synovial fluid and synovium of patients with RA, increased iron level, ROS and lipid peroxidation can be observed.9,33 In the cartilage of RA patients and adjuvant arthritis rat model, reduction in ACSL4 can be found and elevation in GPX4 can be observed, indicating an association between chondrocyte ferroptosis and RA development.34 Notably, RND1 overexpression stimulates the lipid peroxidation and ferroptosis of glioblastoma via SLC7A11.15 The present study showed that the overexpression of RND1 could increase iron level and elevated lipid peroxidation (MDA, 4-HNE, and lipid ROS) in RA-FLSs, suggested that RND1 overexpression could promote ferroptosis in RA. Besides, it is revealed that ACSL4 can promote ferroptosis.35 The reduction of SLC7A11 can decrease GPX4 activity, contributing to the accumulation of lethal lipid peroxides and the activation of ferroptosis.36 Considering this, we also detected the expressions of major mediators implicated in ferroptosis and our data found that RND1 upregulation increased ACLS4 expression whereas it decreased the expressions of GPX4 and SLC7A11 in RA-FLSs, which further confirming the promoting role of RND1 elevation in ferroptosis in RA.
It is reported that the suppression of ferroptosis by Semaphorin 5A can facilitate the activation of RA-FLSs.37 In CIA mice, TNF antagonist can induce the ferroptosis in FLSs and inhibit the development of RA.33 Evidently, these findings revealed that the effective promotion of ferroptosis in FLSs can inhibit RA development. In this study, to further explore the mechanism of RND1 related with ferroptosis in RA, ferroptosis inhibitors Fer-1 and DFO were used for the pre-treatment of RA-FLSs and functional experiments were performed again. The results demonstrated that Fer-1 or DFO treatment partially abolished the inhibitory effects of RND1 upregulation on the proliferation, migration, invasion and inflammatory release in RA-FLSs, indicating that RND1 overexpression exhibits its protective role in RA-FLSs via the regulation of ferroptosis.
To summarize, this study revealed the regulatory role of RND1 in the proliferation, migration, invasion, inflammatory release and ferroptosis in RA-FLSs and unprecedentedly identified the protective mechanism of RND1 in RA.
Funding Statement
There is no funding to report.
Data Sharing Statement
The data underlying this article are available in the article.
Ethics Approval
The animal experiments were approved by the Institutional Animal Care and Use Committee of the Affiliated Hospital of Guangdong Medical University and performed according to the National Institutes of Health Guidelines for the care and use of experimental animals.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no competing interests in this work.
References
- 1.Xiao F, Han M, Rui K, et al. New insights into follicular helper T cell response and regulation in autoimmune pathogenesis. Cell mol Immunol. 2021;18(6):1610–1612. doi: 10.1038/s41423-021-00688-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aletaha D, Smolen JS. Diagnosis and management of rheumatoid arthritis: a review. JAMA. 2018;320(13):1360–1372. doi: 10.1001/jama.2018.13103 [DOI] [PubMed] [Google Scholar]
- 3.Bottini N, Firestein GS. Duality of fibroblast-like synoviocytes in RA: passive responders and imprinted aggressors. Nat Rev Rheumatol. 2013;9(1):24–33. doi: 10.1038/nrrheum.2012.190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang R, Zhang Y, Wang L, et al. Increased autophagy in fibroblast-like synoviocytes leads to immune enhancement potential in rheumatoid arthritis. Oncotarget. 2017;8(9):15420–15430. doi: 10.18632/oncotarget.14331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim EK, Kwon JE, Lee SY, et al. IL-17-mediated mitochondrial dysfunction impairs apoptosis in rheumatoid arthritis synovial fibroblasts through activation of autophagy. Cell Death Dis. 2017;8(1):e2565. doi: 10.1038/cddis.2016.490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Z, Ma D, Yang H, et al. Fibroblast-like synoviocytes in rheumatoid arthritis: surface markers and phenotypes. Int Immunopharmacol. 2021;93:107392. doi: 10.1016/j.intimp.2021.107392 [DOI] [PubMed] [Google Scholar]
- 7.Xie Z, Hou H, Luo D, An R, Zhao Y, Qiu C. ROS-dependent lipid peroxidation and reliant antioxidant ferroptosis-suppressor-Protein 1 in rheumatoid arthritis: a covert clue for potential therapy. Inflammation. 2021;44(1):35–47. doi: 10.1007/s10753-020-01338-2 [DOI] [PubMed] [Google Scholar]
- 8.Stockwell BR. Ferroptosis turns 10: emerging mechanisms, physiological functions, and therapeutic applications. Cell. 2022;185(14):2401–2421. doi: 10.1016/j.cell.2022.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ling H, Li M, Yang C, et al. Glycine increased ferroptosis via SAM-mediated GPX4 promoter methylation in rheumatoid arthritis. Rheumatology. 2022;61(11):4521–4534. doi: 10.1093/rheumatology/keac069 [DOI] [PubMed] [Google Scholar]
- 10.Baker JF, Ghio AJ. Iron homoeostasis in rheumatic disease. Rheumatology. 2009;48(11):1339–1344. doi: 10.1093/rheumatology/kep221 [DOI] [PubMed] [Google Scholar]
- 11.Telfer JF, Brock JH. Proinflammatory cytokines increase iron uptake into human monocytes and synovial fibroblasts from patients with rheumatoid arthritis. Med Sci Monit. 2004;10(4):Br91–5. [PubMed] [Google Scholar]
- 12.Luo H, Zhang R. Icariin enhances cell survival in lipopolysaccharide-induced synoviocytes by suppressing ferroptosis via the Xc-/GPX4 axis. Exp Ther Med. 2021;21(1):72. doi: 10.3892/etm.2020.9504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Y, Chen H, Yan J, et al. FOXA2 activates RND1 to regulate arachidonic acid metabolism pathway and suppress cisplatin resistance in lung squamous cell carcinoma. Clin Respir J. 2024;18(8):e13814. doi: 10.1111/crj.13814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swaminathan B, Youn SW, Naiche LA, et al. Endothelial Notch signaling directly regulates the small GTPase RND1 to facilitate Notch suppression of endothelial migration. Sci Rep. 2022;12(1):1655. doi: 10.1038/s41598-022-05666-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun Q, Xu Y, Yuan F, et al. Rho family GTPase 1 (RND1), a novel regulator of p53, enhances ferroptosis in glioblastoma. Cell Biosci. 2022;12(1):53. doi: 10.1186/s13578-022-00791-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Komatsu H, Iguchi T, Masuda T, et al. Attenuated RND1 expression confers malignant phenotype and predicts poor prognosis in hepatocellular carcinoma. Ann Surg Oncol. 2017;24(3):850–859. doi: 10.1245/s10434-016-5573-9 [DOI] [PubMed] [Google Scholar]
- 17.Dai L, Chen X, Zhang H, et al. RND3 transcriptionally regulated by FOXM1 inhibits the migration and inflammation of synovial fibroblasts in rheumatoid arthritis through the Rho/ROCK pathway. J Interferon Cytokine Res. 2022;42(6):279–289. doi: 10.1089/jir.2021.0228 [DOI] [PubMed] [Google Scholar]
- 18.Wang X, Tang K, Wang Y, et al. Elevated microRNA‑145‑5p increases matrix metalloproteinase‑9 by activating the nuclear factor‑κB pathway in rheumatoid arthritis. Mol Med Rep. 2019;20(3):2703–2711. doi: 10.3892/mmr.2019.10499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu Y, Pan YF, Xue YQ, et al. uPAR promotes tumor-like biologic behaviors of fibroblast-like synoviocytes through PI3K/Akt signaling pathway in patients with rheumatoid arthritis. Cell mol Immunol. 2018;15(2):171–181. doi: 10.1038/cmi.2016.60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu P, Wang G, Lu X, et al. Elevated matrix metalloproteinase 9 supports peripheral nerve regeneration via promoting Schwann cell migration. Exp Neurol. 2022;352:114020. doi: 10.1016/j.expneurol.2022.114020 [DOI] [PubMed] [Google Scholar]
- 21.Yang X, Zhang W, Wang L, Zhao Y, Wei W. Metabolite-sensing GPCRs in rheumatoid arthritis. Trends Pharmacol Sci. 2024;45(2):118–133. doi: 10.1016/j.tips.2023.12.001 [DOI] [PubMed] [Google Scholar]
- 22.Chang S, Tang M, Zhang B, Xiang D, Li F. Ferroptosis in inflammatory arthritis: a promising future. Front Immunol. 2022;13:955069. doi: 10.3389/fimmu.2022.955069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Woude D, van der Helm-van Mil AHM. Update on the epidemiology, risk factors, and disease outcomes of rheumatoid arthritis. Best Pract Res. 2018;32(2):174–187. doi: 10.1016/j.berh.2018.10.005 [DOI] [PubMed] [Google Scholar]
- 24.Bustamante MF, Garcia-Carbonell R, Whisenant KD, Guma M. Fibroblast-like synoviocyte metabolism in the pathogenesis of rheumatoid arthritis. Arthritis Res Therapy. 2017;19(1):110. doi: 10.1186/s13075-017-1303-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kondo N, Kuroda T, Kobayashi D. Cytokine networks in the pathogenesis of rheumatoid arthritis. Int J mol Sci. 2021;22(20):10922. doi: 10.3390/ijms222010922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu D, Li R, Xu S, et al. SMOC2 promotes aggressive behavior of fibroblast-like synoviocytes in rheumatoid arthritis through transcriptional and post-transcriptional regulating MYO1C. Cell Death Dis. 2022;13(12):1035. doi: 10.1038/s41419-022-05479-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Falconer J, Murphy AN, Young SP, et al. Review: synovial Cell Metabolism and Chronic Inflammation in Rheumatoid Arthritis. Arthritis Rheumatol. 2018;70(7):984–999. doi: 10.1002/art.40504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang B, Ge Y, Zhou Y, et al. miR-124a inhibits the proliferation and inflammation in rheumatoid arthritis fibroblast-like synoviocytes via targeting PIK3/NF-κB pathway. Cell Biochem Funct. 2019;37(4):208–215. doi: 10.1002/cbf.3386 [DOI] [PubMed] [Google Scholar]
- 29.Qin CD, Ma DN, Zhang SZ, et al. The Rho GTPase Rnd1 inhibits epithelial-mesenchymal transition in hepatocellular carcinoma and is a favorable anti-metastasis target. Cell Death Dis. 2018;9(5):486. doi: 10.1038/s41419-018-0517-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cao S, Mao X, Liu D, Buck M. Backbone assignment and secondary structure of Rnd1, an unusual Rho family small GTPase. Biomol NMR Assignments. 2013;7(2):121–128. doi: 10.1007/s12104-012-9391-0 [DOI] [PubMed] [Google Scholar]
- 31.Li J, Cao F, Yin HL, et al. Ferroptosis: past, present and future. Cell Death Dis. 2020;11(2):88. doi: 10.1038/s41419-020-2298-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.He X, Zhang J, Gong M, et al. Identification of potential ferroptosis-associated biomarkers in rheumatoid arthritis. Front Immunol. 2023;14:1197275. doi: 10.3389/fimmu.2023.1197275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu J, Feng Z, Chen L, et al. TNF antagonist sensitizes synovial fibroblasts to ferroptotic cell death in collagen-induced arthritis mouse models. Nat Commun. 2022;13(1):676. doi: 10.1038/s41467-021-27948-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou R, Chen Y, Li S, et al. TRPM7 channel inhibition attenuates rheumatoid arthritis articular chondrocyte ferroptosis by suppression of the PKCα-NOX4 axis. Redox Biol. 2022;55:102411. doi: 10.1016/j.redox.2022.102411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Y, Zhang M, Bi R, et al. ACSL4 deficiency confers protection against ferroptosis-mediated acute kidney injury. Redox Biol. 2022;51:102262. doi: 10.1016/j.redox.2022.102262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yuan Y, Zhai Y, Chen J, Xu X, Wang H. Kaempferol ameliorates oxygen-glucose deprivation/reoxygenation-induced neuronal ferroptosis by activating Nrf2/SLC7A11/GPX4 axis. Biomolecules. 2021;11(7):923. doi: 10.3390/biom11070923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheng Q, Chen M, Liu M, et al. Semaphorin 5A suppresses ferroptosis through activation of PI3K-AKT-mTOR signaling in rheumatoid arthritis. Cell Death Dis. 2022;13(7):608. doi: 10.1038/s41419-022-05065-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article.