Abstract
Preoperative anxiety and postoperative pain pose significant challenges in surgical settings, often leading to various physical and psychological complications. This study aimed to assess the impact of multimedia education on anxiety levels and pain among candidates undergoing laparoscopic cholecystectomy. In a clinical trial employing Solomon’s four-group design, 80 candidates for laparoscopic cholecystectomy were enrolled. They were selected through convenience sampling and randomly allocated to four groups: intervention group with pre-test (E1), intervention group without pre-test (E2), control group with pre-test (C1), and control group without pre-test (C2). Multimedia education was administered to the intervention groups. Data were collected using the State-Trait Anxiety Inventory (STAI) for anxiety assessment and the Visual Analog Scale (VAS) for pain measurement, then analyzed using SPSS-22 software. Preoperative state anxiety levels in groups E1 and E2 were significantly lower compared to C1 and C2 (38.6 ± 7.32, 38.1 ± 8.83, 46.3 ± 11.57, and 45.8 ± 9.57, respectively; p = 0.006). However, there was no significant difference in state anxiety levels 24 h post-surgery nor in trait anxiety levels before and 24 h after surgery. Moreover, there was no significant difference in mean pain scores 24 h post-surgery among the groups. The findings indicate that multimedia education can effectively reduce preoperative anxiety in patients undergoing surgery. However, it did not significantly impact anxiety and pain levels post-surgery. Multimedia education may be considered as a supplementary approach to standard preoperative care protocols.
Keywords: Patient education, Multimedia, Preoperative anxiety, Pain, Laparoscopic cholecystectomy
Subject terms: Health care, Medical research
Introduction
Cholelithiasis, a prevalent ailment of the digestive system, exhibits a rising incidence rate attributable to shifts in lifestyle1. Notably, cholelithiasis poses substantial economic burdens and serves as a significant predisposing factor for gallbladder cancer2. Laparoscopic cholecystectomy stands as the standard therapeutic modality for cholelithiasis, offering diminished postoperative complications and expedited patient recovery compared to open cholecystectomy3,4.
Despite the minimally invasive nature of laparoscopic cholecystectomy, postoperative pain remains a prominent challenge associated with this surgical approach5 and the most common complaints during the post-surgery period are pain at the surgical incision site and shoulder pain6. Pain perception post-surgery elicits the release of catecholamines and activation of the sympathetic nervous system, precipitating physiological responses such as hypertension, tachycardia, elevated respiratory rate, and heightened cardiac oxygen consumption7. Postoperative pain management following laparoscopic cholecystectomy often involves the use of opioid medications, which can lead to various adverse effects5. A systematic review suggests using a combination of interventions for pain management, involving basic analgesia with non-steroidal anti-inflammatory drugs (NSAIDs) or selective cyclo-oxygenase-2 (COX-2) inhibitors, as well as paracetamol, administered before or during surgery and continued for up to 72 h postoperatively. Intraoperative interventions, such as intravenous dexamethasone administration and specific surgical techniques like three-port laparoscopy, low-pressure pneumoperitoneum, gallbladder removal through the umbilical port, and normal saline irrigation, are also recommended. This study emphasizes that opioid medications should only be used as a last resort if other interventions prove ineffective8. Additionally, non-pharmacological strategies, such as breathing exercises and preoperative education, have shown effectiveness in managing postoperative pain9–11. Therefore, a combination of pharmacological and non-pharmacological interventions may be a suitable approach for pain management following laparoscopic cholecystectomy. Inadequate pain management post-surgery may culminate in complications, including delayed wound healing, atelectasis, pneumonia, deep vein thrombosis, prolonged recovery duration, extended hospitalization, chronic pain, and diminished quality of life for patients12. Post-laparoscopic cholecystectomy pain is attributed to local irritation, augmented intra-abdominal pressure, and diaphragmatic stretching induced by insufflation of carbon dioxide gas into the peritoneum during surgery13. Furthermore, within the biopsychosocial model of pain, psychological variables such as anxiety exert a notable influence on pain perception14.
A considerable proportion of preoperative patients experience varying degrees of anxiety; the prevalence rates of preoperative anxiety in children and adults range from 40 to 60% and 11–80%, respectively15,16. Anxiety precipitates adverse effects, including stimulation of the endocrine and autonomic systems, engendering subsequent hemodynamic instability. Furthermore, inadequate anxiety management correlates with escalated usage of anesthetic agents pre- and intraoperatively, heightening the likelihood of postoperative complications such as nausea, vomiting, respiratory compromise, and tachycardia16,17.
Patients awaiting surgery harbor anxiety stemming from diverse factors, including inadequate comprehension of the surgical procedure and anesthesia administration, apprehension regarding surgical outcomes, fear of postoperative complications and pain, anxiety pertaining to consciousness recovery post-surgery, fear of dependency and loss of autonomy, and uncertainty regarding hospitalization experiences16–18. Additionally, preoperative anxiety may exacerbate postoperative anxiety19. Consequently, the provision of comprehensive, patient-tailored information, fostering psychological preparedness for surgery, and proficient pain management assume paramount importance in the patient recovery trajectory18,20. Preoperative education not only enhances patient understanding regarding the disease and available therapeutic modalities but also promotes active patient engagement in the treatment process, thereby mitigating postoperative complications such as anxiety and pain21. Previous research underscores the favorable impact of preoperative education on anxiety reduction, postoperative complications, and heightened patient satisfaction11,21,22.
Traditional patient education modalities, such as verbal communication and written materials like pamphlets, may fall short due to temporal constraints, omission of pertinent information, lack of clarity, or inadequacy stemming from healthcare providers’ communication skills18,22. Multimedia education emerges as a contemporary approach to patient information dissemination, encompassing diverse media types, including text, symbols, images, sound, video, and animations, typically delivered via digital platforms23,24. This mode of education permits information review at the convenience of patients and facilitates comprehension of complex concepts through judicious integration of textual, visual, and auditory elements18,25. Grounded in the cognitive theory of multimedia learning’s dual-channel assumption, an amalgamation of auditory and visual stimuli enhances cognitive capacity, comprehension, and retention, thereby augmenting audience engagement and knowledge acquisition26. Enhanced comprehension of content, including therapeutic interventions, consequentially attenuates patient anxiety25. However, findings from prior studies regarding the efficacy of multimedia education and educational videos in anxiety reduction and knowledge enhancement among patients exhibit variability27–29.
Nurses bear a significant responsibility in patient education, imparting comprehensive information regarding diseases, treatment modalities, and associated dimensions, thereby alleviating patient apprehension and facilitating optimal postoperative complication management. However, time constraints hinder nurses’ ability to deliver exhaustive education through traditional means, such as face-to-face interactions, posing limitations. Multimedia-based education presents a promising avenue for effective patient instruction, potentially mitigating surgical anxiety and postoperative complications. Nevertheless, existing literature yields conflicting findings concerning the efficacy of multimedia education modalities on patient knowledge and anxiety levels. Hence, this study aims to ascertain the impact of multimedia education on anxiety levels and pain among candidates undergoing laparoscopic cholecystectomy.
Materials and methods
Study design
The present study employed a randomized controlled clinical trial utilizing a Solomon four-group design with an allocation ratio of 1:1:1:1. Patients were randomly assigned to four groups, including two intervention groups and two control groups. One intervention group underwent a pre-test, while the other intervention group did not. Similarly, one control group received a pre-test, while the other did not. Post-tests and follow-ups were conducted across all four groups. The study duration spanned from May 29, 2023, to November 6, 2023. Adherence to the CONSORT (Consolidated Standards of Reporting Trials) checklist guided the study report.
Participants
The research population comprised all patients diagnosed with cholelithiasis slated for laparoscopic cholecystectomy at the general surgery departments of a hospital affiliated to Kermanshah University of Medical Sciences, Kermanshah, western Iran. Inclusion criteria encompassed willingness to participate in the research, age between 19 and 65 years, ability to communicate effectively, absence of severe visual or auditory impairments, lack of psychological disorders, absence of respiratory ailments, absence of substance addiction, and proficiency in reading and writing. Exclusion criteria included the conversion of laparoscopic surgery to laparotomy, administration of sedatives pre-and post-surgery, and emergency surgery.
Sample size
According to the study by Toğaç and Yılmaz11, the mean and standard deviation of post-operative state anxiety (24 h after surgery) in the intervention and control groups were 39 ± 3.5 and 44.4 ± 4.8, respectively. Considering a confidence level of 95% and a test power of 90% based on the formula provided below, the sample size was estimated to be 13 participants per group. To ensure more precise results, the sample size was increased to 20 participants per group (a total of 80 participants).
 |
Randomization
Convenience sampling was utilized to select patients, who were then randomly allocated to four groups: intervention group with pre-test (E1), intervention group without pre-test (E2), control group with pre-test (C1), and control group without pre-test (C2). Randomization was achieved using a random sequence generated by https://www.randomizer.org. Random numbers were assigned to 80 cards in sequential order, concealed within sealed opaque envelopes, and placed in a box. A separate individual, distinct from the researcher, handled the generation and recording of random sequences onto cards, as well as the placement of cards into envelopes. Allocation concealment was ensured until patient allocation. Following consent acquisition of eligible patients, envelopes were opened sequentially at their bedside to determine group allocation. Due to the nature of the intervention, blinding was not feasible.
Procedures
Patients consenting to participate were enrolled a day before surgery, and written informed consent was obtained. Subsequently, patients were randomized into the four groups. Demographic information was collected, and hemodynamic parameters (including systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and arterial blood oxygen saturation (SpO2)) were measured for all groups. Participants in E1 and C1 completed the Spielberger State and Trait Anxiety Inventory (STAI). After that, multimedia education was administered to intervention groups, while control groups received standard care. On the morning of surgery, hemodynamic parameters were reassessed, and STAI was completed for all groups. Additionally, 24 h post-surgery, hemodynamic parameters were reevaluated, STAI was completed, and pain levels were assessed for all groups. All interventions and measurements were conducted at the patient’s bedside within the ward setting. Data collection occurred on the day preceding surgery (prior to intervention) between 18:00 to 20:00 h and on the morning of surgery (pre-operatively) between 06:00 to 07:30 h.
Patient education and data collection at all three time points were conducted by a single researcher (the first author), who was present at the patients’ bedside throughout the intervention and data collection process. Participants completed the demographic information form and the STAI themselves, with the researcher available to address any questions or ambiguities that arose, providing clarification as needed. Hemodynamic parameters were assessed using a sphygmomanometer and pulse oximeter. To quantify pain levels, patients were provided with a Visual Analog Scale (VAS) and were asked to mark a point corresponding to their perceived pain level on a 10-cm line. Furthermore, patient education was delivered through multimedia approach, including the presentation of videos on a tablet device.
All patients received intravenous acetaminophen at a dose of 1000 mg, three times a day (every 8 h), and intravenous administration of 25 mg of pethidine, twice a day (every 12 h), as part of routine post-operative care regarding the analgesics used in the post-operative period.
Multimedia groups
Educational content was developed based on prior research10,11 and structured into seven PowerPoint files, subsequently presented in video format (MP4). The video content comprised textual and visual elements, predominantly emphasizing images. BANDICAM screen recording software (https://www.bandicam.com) facilitated video creation from prepared PowerPoint slides with added audio. Videos adhered to Mayer’s multimedia principles30 and incorporated two videos filmed within the hospital’s operating room. Video and photographic material, including operating room visuals, were captured using a video camera and edited by a professional studio. Samsung Galaxy S6 Lite tablets and Lito L-9 wireless headphones facilitated video presentation. The educational content was disseminated across nine separate videos totaling 30 min and 56 s (00:30:56) in the following sequence:
Gallbladder anatomy and function (01:41).
Advantages of laparoscopic cholecystectomy over open surgery and potential postoperative complications (03:24).
Pre-surgical procedures upon entering the operating room, encompassing patient monitoring, general anesthesia administration, and associated complications (05:13).
Roles of the surgical team and equipment overview within the operating room setting (03:02).
Surgical procedure walkthrough, inclusive of abdominal preparation, trocar insertion, instrument placement, drain insertion, and incision closure, followed by postoperative recovery procedures (05:22).
Operating room processes, including gowning, glove donning, equipment preparation, and laparoscopic setup (03:03) (which was filmed within the hospital’s operating room).
Administration of carbon dioxide into the abdominal cavity and overview of the surgical team during the procedure (01:04) (trocar and port insertion video excluded) (which was filmed within the hospital’s operating room).
Postoperative care protocols, encompassing vital sign monitoring, NPO status, mobilization restrictions, drain management, wound care, medication administration, and hospitalization duration (05:35).
Instruction on postoperative deep breathing exercises (02:32), followed by supervised practice with the researcher’s guidance.
Upon completion of the intervention, patients received four pamphlets elucidating gallbladder anatomy and function, laparoscopic cholecystectomy benefits, postoperative care protocols, and postoperative deep breathing exercises, mirroring video content in summarized form with accompanying images. Pamphlets were printed in color on A4-sized paper.
Materials preparation drew from reference books, related articles, and insights from surgical department heads, nurses, operating room experts, and intelligence field professionals.
After preparing the educational content, content validity was assessed. A form with 16 items was created and given to 12 specialists, including two surgeons, a head nurse of the surgical department, two nursing professors, three nurses from the surgical department, a psychiatric nurse, two operating room experts, and an anesthesia expert. The Content Validity Index (CVI) was calculated as 0.9. Initially, the educational video was 37 min and 43 s long, but based on expert feedback, it was reduced to 30 min and 56 s.
In this study, face validity was also conducted to evaluate the clarity, appropriateness of sentences, and applicability of the educational content for patients. The videos were shown to five patients, and they were asked to express their opinions. One patient suggested an addition to the educational content. Following content and face validity assessments, the videos were finalized.
Control groups
Control groups received standard care devoid of intervention, comprising preoperative consultations, consent acquisition, necessary tests, surgical site preparation, and preoperative fasting protocols.
Outcome measures
Data collection instruments included a demographic information form, the STAI, and a VAS for pain assessment.
Primary outcomes
Anxiety and pain served as primary study endpoints.
STAI, comprising 40 questions, assessed anxiety levels, with 20 questions dedicated to state anxiety and 20 to trait anxiety; higher scores denoted increased anxiety11.
Pain intensity was evaluated using a VAS featuring a 10-cm horizontal line denoting minimum and maximum pain scores, with 0 indicating no pain and 10 representing maximal pain intensity11.
Secondary outcomes
Secondary outcomes encompassed hemodynamic indices, including SBP, DBP, HR, and SpO2. SBP and DBP were measured using a sphygmomanometer (model no. BP AG1-20; Microlife, Widnau, Switzerland) by applying the cuff to the patient’s arm. HR and SpO2 were assessed using a pulse oximeter (MD300 C2; ChoiceMMed, Beijing, China) placed on the index finger.
Ethical considerations
The study received approval from the Ethics Committee of Kermanshah University of Medical Sciences (code: IR.KUMS.REC.1401.503) at 24/01/2023 available at https://ethics.research.ac.ir/PortalProposalListEn.php?code=&title=&name=rostam+jalali&stat=&isAll=. All methods were performed in accordance with the guidelines and regulations of Iran National Committee for Ethics in Biomedical Research. It was registered with the Iranian Registry of Clinical Trials IRCT20130603013568N7 at 13/02/2023 available at https://irct.behdasht.gov.ir/. Participants were briefed on study objectives and assured of voluntary participation and confidentiality maintenance. Written informed consent was obtained from all participants, and assurance was provided regarding the confidential handling of their data. Control group participants received videos and pamphlets at the study’s conclusion.
Statistical analysis
Statistical analysis was performed using SPSS version 22 software. The normality of data distribution was assessed using the Kolmogorov-Smirnov test. Descriptive statistics, including mean and standard deviation for continuous variables and frequency for categorical variables, were computed. The homogeneity of variables across the four groups was examined using chi-square and Fisher’s exact tests. Inter-group comparisons utilized independent samples t-test, one-way analysis of variance (ANOVA), followed by Scheffe post hoc test for significant results. Intra-group comparisons employed paired samples t-test and repeated measures ANOVA, with Bonferroni post hoc test for significant findings. Statistical significance was set at p < 0.05.
Results
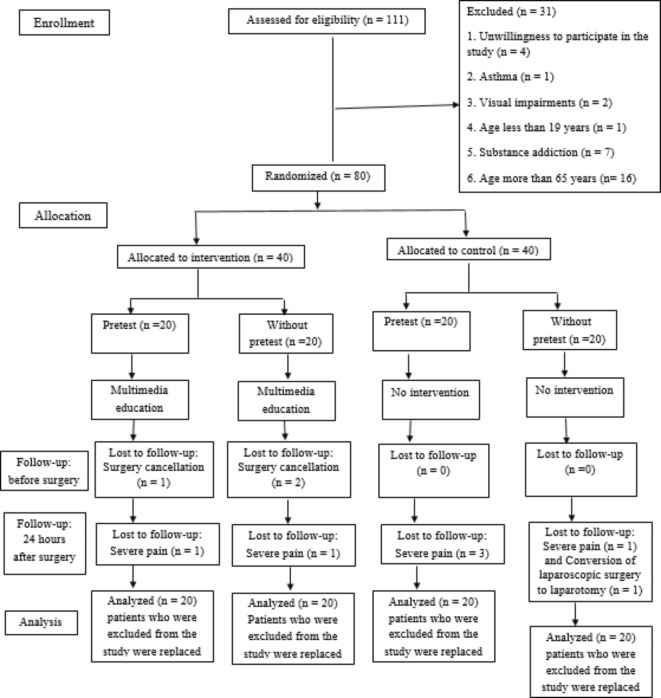
The study initially included 80 eligible patients, with ten individuals subsequently excluded due to various reasons. Replacement was performed, resulting in a final sample size of 80 participants (Fig. 1). The mean age was 40.66 ± 12.18 years, with the majority being female (80%) and having a history of surgery (74%). No significant differences were observed among study groups concerning demographic variables (p > 0.05; Table 1).
Fig. 1.
Study flow diagram.
Table 1.
Comparison of demographic variables between study groups.
| Variable | Variable levels | Group | |||||
|---|---|---|---|---|---|---|---|
| E1 (n = 20) |
E2 (n = 20) |
C1 (n = 20) |
C2 (n = 20) |
Total (n = 80) | Test result | ||
|
Age (years) Mean ± SD |
40.9 ± 10.07 | 40.55 ± 13.01 | 39.95 ± 12.74 | 41.25 ± 13.52 | 40.66 ± 12.18 |
F = 0.04 P = 0.989 |
|
|
Gender N (%) |
Female | 17 (85) | 15 (75) | 16 (80) | 16 (80) | 64 (80) |
F = 0.73 P = 0.890 |
| Male | 3 (15) | 5 (25) | 4 (20) | 4 (20) | 16 (20) | ||
|
Marital status N (%) |
Single | 2 (10) | 1 (5) | 1 (5) | 0 (0) | 4 (5) |
F = 3.07 P = 0.863 |
| Married | 16 (80) | 18 (90) | 18 (90) | 18 (90) | 70 (87.5) | ||
| Divorced or widowed | 2 (10) | 1 (5) | 1 (5) | 2 (10) | 6 (7.5) | ||
| Educational level N (%) | Primary and secondary school | 16 (80) | 13 (65) | 11 (55) | 13 (65) | 53 (66.2) |
X2 = 2.85 P = 0.415 |
| Diploma and university education | 4 (20) | 7 (35) | 9 (45) | 7 (35) | 27 (33.8) | ||
| Occupational status N (%) | Self-employed/ employed | 3 (15) | 3 (15) | 5 (25) | 3 (15) | 14 (17.5) |
F = 1.94 P = 0.969 |
| Housemaker | 16 (80) | 15 (75) | 14 (70) | 16 (80) | 61 (76.2) | ||
| Retired | 1 (5) | 2 (10) | 1 (5) | 1 (5) | 5 (6.3) | ||
|
Surgery history N (%) |
Yes | 15 (75) | 17 (85) | 15 (75) | 12 (60) | 59 (74) |
X2 = 3.29 P = 0.349 |
| No | 5 (25) | 3 (15) | 5 (25) | 8(40) | 21 (26) | ||
|
Comorbidity N (%) |
With Comorbidity | 8 (40) | 10 (50) | 6 (30) | 8 (40) | 32 (40) |
X2 = 1.67 P = 0.644 |
| Without Comorbidity | 12 (60) | 10 (50) | 14 (70) | 12 (60) | 48 (60) | ||
|
Smoking N (%) |
Yes | 3 (15) | 2 (10) | 0 (0) | 4 (20) | 9 (11.2) |
F = 4.59 P = 0.228 |
| No | 17 (85) | 18 (90) | 20 (100) | 16 (80) | 71 (88.8) | ||
E1 = Experiment 1 (intervention with pretest), E2 = Experiment 2 (intervention without pretest), C1 = Control 1 (control with pretest), C2 = Control 2 (control without pretest), SD = Standard deviation, P value significant at P < 0.05.
Data distribution conformed to normality based on the Kolmogorov-Smirnov test.
One-way ANOVA revealed a statistically significant difference in mean preoperative state anxiety among groups (p = 0.006), while postoperative state anxiety at 24 h did not yield significance (p = 0.091). No significant differences were noted in preoperative trait anxiety and postoperative trait anxiety at 24 h among the groups, nor in mean postoperative pain (p = 0.897, p = 0.754, and p = 0.865, respectively). Intra-group analysis showed significant differences only in the E1 group’s state anxiety (p = 0.001) (Table 2).
Table 2.
Comparison of mean scores of state and trait anxiety and pain in study groups.
| Variable | Stage | Group | Test result | |||
|---|---|---|---|---|---|---|
| E1* | E2* | C1* | C2* | |||
| State anxiety | Before education | 44.5 ± 9.78 | 42.1 ± 10.43 |
t = 0.75 P = 0.46a |
||
| Before surgery | 38.6 ± 7.32 | 38.1 ± 8.83 | 46.3 ± 11.57 | 45.8 ± 9.57 |
F = 4.45 P = 0.006b |
|
| 24 h after surgery | 39.95 ± 8.04 | 39.05 ± 8.02 | 45.85 ± 13.13 | 44.35 ± 9.52 |
F = 2.238 P = 0.091b |
|
| Test result |
F = 11.131 P = 0.001c |
t = -0.55 P = 0.592d |
F = 1.94 P = 0.158c |
t = 0.81 P = 0.43d |
||
| Trait anxiety | Before education | 45.15 ± 8.01 | 42.65 ± 9.91 |
t = 0.88 P = 0.38a |
||
| Before surgery | 43.45 ± 7.24 | 41.55 ± 6.41 | 42.95 ± 11.33 | 43.25 ± 8.71 |
F = 0.198 P = 0.897b |
|
| 24 h after surgery | 43.6 ± 7.94 | 41.15 ± 5.88 | 42.35 ± 10.13 | 43.4 ± 7.32 |
F = 0.399 P = 0.754b |
|
| Test result |
F = 1.38 P = 0.26c |
t = 0.41 P = 0.684d |
F = 0.08 P = 0.923c |
t = -0.1 P = 0.926d |
||
| Pain | 24 h after surgery | 4.48 ± 1.8 | 4.45 ± 1.43 | 4.82 ± 1.7 | 4.75 ± 1.91 |
F = 0.245 P = 0.865b |
E1 = Experiment 1 (intervention with pretest), E2 = Experiment 2 (intervention without pretest), C1 = Control 1 (control with pretest), C2 = Control 2 (control without pretest), *Expressed as mean ± standard deviation, aAnalyzed using independent sample t-test, b Analyzed using one way ANOVA, c Analyzed using repeated measures ANOVA, dAnalyzed using paired samples t-test, P value significant at P < 0.05.
Scheffe post hoc test revealed significantly lower mean preoperative state anxiety in intervention groups compared to control groups, with no significant differences between intervention and control pairs (Table 3). Bonferroni post hoc test indicated significantly reduced preoperative and postoperative state anxiety in the E1 group compared to pre-intervention levels (p = 0.001 and p = 0.023, respectively) (Table 4).
Table 3.
The results of Scheffe post hoc test in terms of state anxiety before surgery.
| Group | Group | MD | P value |
|---|---|---|---|
| E1 | E2 | 0.50 | 0.999 |
| C1 | -7.70 | 0.012 | |
| C2 | -7.20 | 0.011 | |
| E2 | C1 | -8.20 | 0.016 |
| C2 | -7.70 | 0.012 | |
| C1 | C2 | 0.50 | 0.13 |
E1 = Experiment 1 (intervention with pretest), E2 = Experiment 2 (intervention without pretest), C1 = Control 1 (control with pretest), C2 = Control 2 (control without pretest), MD = Mean difference, P value significant at P < 0.05.
Table 4.
The results of Bonferroni post hoc test in terms of state anxiety in E1 group.
| Stage | Stage | MD | P value |
|---|---|---|---|
| Before surgery | Before education | -5.90 | 0.001 |
| 24 h after surgery | -1.35 | 0.65 | |
| 24 h after surgery | Before education | -4.55 | 0.032 |
MD = Mean difference, P value significant at P < 0.05.
No significant differences were observed among the four study groups regarding mean hemodynamic parameters (SBP, DBP, HR, SpO2) across all study phases. Repeated measures ANOVA indicated significant differences in SBP in the E1 and E2 groups, DBP in the E1 group, and HR and SpO2 across all groups during all study phases (Table 5). Bonferroni post hoc analysis revealed significantly decreased SBP in E1 and E2 groups pre-operatively and at 24 h post-surgery compared to pre-intervention levels. DBP in the E1 group was significantly reduced pre-operatively and at 24 h post-surgery compared to pre-intervention levels (p = 0.046 and p = 0.041, respectively). HR in E1 and E2 groups exhibited significantly lower preoperative levels compared to pre-intervention levels (p = 0.008 and p = 0.001, respectively). Additionally, HR in all groups significantly increased 24 h post-surgery compared to preoperative levels (p = 0.006, p = 0.002, p = 0.005, and p = 0.004 in E1, E2, C1, and C2 groups, respectively). Moreover, SpO2 significantly decreased 24 h post-surgery in all groups compared to pre-intervention and preoperative levels (Table 6).
Table 5.
Comparison of mean values of hemodynamic parameters in study groups.
| Variable | Stage | Group | Test result | |||
|---|---|---|---|---|---|---|
| E1* | E2* | C1* | C2* | |||
| SBP (mmHg) | Before education | 117.3 ± 12.28 | 117.05 ± 17.37 | 118.2 ± 23.4 | 119.75 ± 21.78 |
F = 0.081 P = 0.97a |
| Before surgery | 108.8 ± 14.34 | 108.85 ± 15.17 | 118.4 ± 20.35 | 118.25 ± 19.75 |
F = 1.94 P = 0.13a |
|
| 24 h after surgery | 109.85 ± 12.95 | 109.4 ± 15.76 | 113.1 ± 19.86 | 113.55 ± 16.42 |
F = 0.343 P = 0.794a |
|
| Test result |
F = 7.64 P = 0.002b |
F = 6.85 P = 0.003b |
F = 1.35 P = 0.271b |
F = 2.003 P = 0.149b |
||
| DBP (mmHg) | Before education | 77 ± 10.27 | 76.35 ± 10.26 | 77.5 ± 16.06 | 78.65 ± 12.79 |
F = 0.119 P = 0.948a |
| Before surgery | 71.1 ± 10.57 | 70.65 ± 13.31 | 78.3 ± 16.22 | 78 ± 13.25 |
F = 1.95 P = 0.129a |
|
| 24 h after surgery | 71.4 ± 10.86 | 70.3 ± 12.13 | 74.6 ± 15.78 | 74.2 ± 12.43 |
F = 0.53 P = 0.663a |
|
| Test result |
F = 4.46 P = 0.018b |
F = 2.56 P = 0.091b |
F = 0.66 P = 0.52b |
F = 1.96 P = 0.154b |
||
| HR (per minute) | Before education | 82.65 ± 15.46 | 83 ± 12.9 | 79.05 ± 9.8 | 82.6 ± 14.64 |
F = 0.386 P = 0.76a |
| Before surgery | 74.55 ± 12.54 | 75.1 ± 9.37 | 78.8 ± 11.8 | 78.45 ± 12.48 |
F = 0.724 P = 0.54a |
|
| 24 h after surgery | 82.95 ± 13.2 | 82.7 ± 11.14 | 88.15 ± 7.82 | 87.75 ± 11.47 |
F = 1.433 P = 0.24a |
|
| Test result |
F = 7.88 P = 0.001b |
F = 9.77 P = 0.001b |
F = 9.48 P = 0.001b |
F = 4.197 P = 0.023b |
||
| SpO2 (%) | Before education | 96.3 ± 1.45 | 96.4 ± 1.35 | 96.2 ± 1.47 | 96.25 ± 1.65 |
F = 0.066 P = 0.978a |
| Before surgery | 96.5 ± 1.15 | 96.65 ± 1.27 | 96.35 ± 1.09 | 96.3 ± 1.13 |
F = 0.371 P = 0.774a |
|
| 24 h after surgery | 94 ± 2.03 | 94.15 ± 1.69 | 93.85 ± 1.81 | 93.95 ± 2.06 |
F = 0.086 P = 0.967a |
|
| Test result |
F = 23.61 P = 0.001b |
F = 31.21 P = 0.001b |
F = 36.71 P = 0.001b |
F = 17.58 P = 0.001b |
||
SBP = Systolic blood pressure, DBP = Diastolic blood pressure, HR = Heart rate, SpO2 = Oxygen saturation, E1 = Experiment 1 (intervention with pretest), E2 = Experiment 2 (intervention without pretest), C1 = Control 1 (control with pretest), C2 = Control 2 (control without pretest), *Expressed as mean ± standard deviation, a Analyzed using one way ANOVA, b Analyzed using repeated measures ANOVA, P value significant at P < 0.05.
Table 6.
The results of Bonferroni post hoc test in terms of hemodynamic parameters in study groups.
| Variable | Group | Stage | Stage | MD | P value |
|---|---|---|---|---|---|
| SBP | E1 | Before surgery | Before education | -8.50 | 0.01 |
| 24 h after surgery | -1.05 | 1.00 | |||
| 24 h after surgery | Before education | -7.45 | 0.012 | ||
| E2 | Before surgery | Before education | -8.20 | 0.012 | |
| 24 h after surgery | -0.55 | 1.00 | |||
| 24 h after surgery | Before education | -7.65 | 0.022 | ||
| DBP | E1 | Before surgery | Before education | -5.90 | 0.046 |
| 24 h after surgery | -0.30 | 1.00 | |||
| 24 h after surgery | Before education | -5.60 | 0.041 | ||
| HR | E1 | Before surgery | Before education | -8.10 | 0.008 |
| 24 h after surgery | -8.40 | 0.006 | |||
| 24 h after surgery | Before education | 0.30 | 1.00 | ||
| E2 | Before surgery | Before education | -7.90 | 0.001 | |
| 24 h after surgery | -7.60 | 0.002 | |||
| 24 h after surgery | Before education | -0.30 | 1.00 | ||
| C1 | Before surgery | Before education | -0.25 | 1.00 | |
| 24 h after surgery | -9.35 | 0.005 | |||
| 24 h after surgery | Before education | 9.10 | 0.001 | ||
| C2 | Before surgery | Before education | -4.15 | 0.56 | |
| 24 h after surgery | -9.30 | 0.004 | |||
| 24 h after surgery | Before education | 5.15 | 0.63 | ||
| SpO2 | E1 | Before surgery | Before education | 0.20 | 1.00 |
| 24 h after surgery | 2.50 | 0.001 | |||
| 24 h after surgery | Before education | -2.30 | 0.001 | ||
| E2 | Before surgery | Before education | 0.25 | 0.86 | |
| 24 h after surgery | 2.50 | 0.001 | |||
| 24 h after surgery | Before education | -2.25 | 0.001 | ||
| C1 | Before surgery | Before education | 0.15 | 1.00 | |
| 24 h after surgery | 2.50 | 0.001 | |||
| 24 h after surgery | Before education | -2.35 | 0.001 | ||
| C2 | Before surgery | Before education | 0.05 | 1.00 | |
| 24 h after surgery | 2.35 | 0.001 | |||
| 24 h after surgery | Before education | -2.30 | 0.001 |
SBP = Systolic blood pressure, DBP = Diastolic blood pressure, HR = Heart rate, SpO2 = Oxygen saturation, E1 = Experiment 1 (intervention with pretest), E2 = Experiment 2 (intervention without pretest), C1 = Control 1 (control with pretest), C2 = Control 2 (control without pretest), MD = Mean difference, P value significant at P < 0.05.
Discussion
The current study aimed to assess the impact of multimedia education on anxiety and pain levels in candidates undergoing laparoscopic cholecystectomy. Results indicated a significant reduction in mean preoperative anxiety among intervention group patients compared to controls. Furthermore, the within-group analysis revealed a notable decrease in pre-surgery anxiety levels post-intervention compared to the day preceding surgery. These findings align with previous research demonstrating the anxiety-reducing efficacy of multimedia and video-based education across various procedural contexts11,31–34.
Educating patients not only supplements their understanding of the disease and treatment processes but also diminishes anxiety, fostering active collaboration with the care team and facilitating subsequent recovery21. Traditional teaching methods, such as face-to-face instruction and written materials, while commonplace, possess limitations that may exacerbate patient anxiety18,32. Multimedia-based education, encompassing digital video discs, compact discs, videos, and the Internet, enhances comprehension and retention of complex concepts through a multimodal approach, thereby alleviating patient anxiety23,25,35. However, it’s important to note that the mere juxtaposition of text and images doesn’t guarantee optimal learning outcomes; Mayer has 12 principles for multimedia design36 and adherence to these principles is crucial for effective knowledge transfer and anxiety reduction.
The effectiveness of our intervention can be attributed to the application of these multimedia principles, facilitating improved comprehension and reduced anxiety among participants. Prior studies have indicated that multimedia education surpasses verbal and written methods in enhancing disease and surgical knowledge and mitigating pre-procedure anxiety34,37.
Despite the documented efficacy of multimedia education in anxiety reduction, some studies have reported inconclusive findings regarding its effectiveness prior to procedures27,29. For instance, Omezli et al. observed increased anxiety levels in dental surgery candidates post-multimedia intervention38. Factors such as clinical context, the type of procedure, content quality, and standardization may contribute to the varying impact of education interventions39.
Our study revealed no significant difference in mean state anxiety levels among the four groups 24 h post-surgery, suggesting that multimedia training did not affect anxiety levels at this juncture. Similarly, Wu et al. reported no significant difference in state anxiety 24 h post-surgery between multimedia intervention and routine care groups40. Conversely, other studies have demonstrated reduced state anxiety following multimedia education11,41,42. Post-surgery anxiety may stem from factors like physical limitations, body image concerns, pain anticipation, and vocational constraints43. Notably, patients in the control group may have acquired post-surgery care information independently, potentially confounding our results.
Regarding trait anxiety, no significant differences were observed among the groups pre-and post-surgery, consistent with previous findings indicating the limited efficacy of multimedia and audio-visual education in mitigating trait anxiety levels11,32,44. Trait anxiety, constituting a stable individual characteristic45, may remain unaffected by interventions focused solely on procedural awareness.
Analysis of pain scores yielded no significant differences among the four groups, contrasting with prior studies indicating the efficacy of multimedia education in reducing pain post-laparoscopic cholecystectomy11,34. Notably, our intervention included instruction on post-surgery breathing exercises, which have been shown to alleviate procedural pain7,9. Additionally, surgical technique may influence postoperative pain, with the three-port method associated with lower pain levels4,46.
Hemodynamic indicators, including SBP, DBP, HR, and SpO2, exhibited no significant differences among the groups pre-and post-surgery, consistent with previous findings on the ineffectiveness of multimedia education on these variables37,47. However, some studies have reported decreased SBP, DBP, and HR following multimedia education11,41,42, suggesting potential variability in intervention outcomes.
SpO2 levels significantly decreased 24 h post-surgery across all groups, consistent with literature documenting post-laparoscopic cholecystectomy reductions in SpO248. Surgical factors, such as phrenic nerve stimulation and pneumoperitoneum, alongside anesthesia and pain medication side effects, may compromise respiratory function post-surgery49,50. The observed increase in HR post-surgery may be attributed to pain-induced sympathetic nervous system activation51, shallow breathing, anesthesia side effects, bleeding, and dehydration.
Limitations
This study utilized both dimensions of anxiety (state and trait) from the Spielberger questionnaire, comprising 40 questions. The high number of questions, particularly for time points such as preoperative assessment and assessments at three different stages (the day before surgery, pre-operation, and 24 h post-operation), may have impacted accurate completion due to potential patient impatience and reduced precision. While the researcher emphasized the importance of accurately completing the questionnaire and its impact on research findings, efforts were made to maximize patient cooperation. Nonetheless, the potential for incomplete or inaccurate responses remains a limitation.
Previous research has highlighted the influence of the number of ports on postoperative pain following laparoscopic cholecystectomy, with the three-port technique associated with less postoperative pain. However, this study did not account for the effect of port numbers on postoperative pain, as surgeries were performed using both three-port and four-port methods.
Recommendations for future studies
It is necessary to conduct longitudinal studies to assess the sustained impact of multimedia education on anxiety and pain levels beyond the immediate preoperative period. Long-term follow-up evaluations would provide valuable insights into the enduring effects of such interventions. Comparing various multimedia formats (e.g., video, interactive modules, virtual reality) to identify the most effective mode of delivery in reducing preoperative anxiety and postoperative pain is essential. Understanding which formats yield optimal outcomes can inform the design of future interventions. Incorporating patient preferences and feedback in the development and implementation of multimedia education programs is crucial. Tailoring interventions to individual preferences and learning styles may enhance engagement and efficacy. Investigating the potential synergistic effects of combining multimedia education with other non-pharmacological interventions (e.g., mindfulness-based techniques, relaxation exercises) or pharmacological approaches to optimize anxiety and pain management outcomes is important. Considering the impact of surgical factors, such as operative technique (e.g., number of ports in laparoscopic procedures), on postoperative pain outcomes is necessary. Future studies should stratify analyses based on surgical variables to elucidate their contribution to pain severity. Augmenting self-reported measures of anxiety and pain with objective assessments, such as physiological parameters (e.g., cortisol levels, heart rate variability), to provide a comprehensive understanding of patients’ psychological and physiological responses to surgery and educational interventions is recommended. Exploring the role of healthcare provider training in delivering multimedia education to patients is also important. Assessing providers’ competency in multimedia delivery techniques and communication skills may enhance intervention effectiveness. Conducting cost-effectiveness analyses to evaluate the economic implications of implementing multimedia education programs in clinical practice is crucial. Assessing the cost per quality-adjusted life year gained can inform resource allocation decisions and policy recommendations.
By addressing these recommendations, future studies can advance our understanding of the role of multimedia education in preoperative anxiety and postoperative pain management, ultimately improving patient outcomes and enhancing the quality of surgical care.
Conclusions
Anxiety is a common experience among individuals awaiting surgery, often leading to various physical and psychological complications. Effective pain management post-surgery remains a significant challenge for healthcare providers. Pre-surgery patient education holds promise in mitigating anxiety and reducing postoperative complications.
The findings of this study demonstrate that multimedia education significantly reduces preoperative anxiety among laparoscopic cholecystectomy candidates. However, its effectiveness in alleviating anxiety and pain post-surgery was not evident. Nevertheless, multimedia-based training presents a cost-effective, non-pharmacological, and complication-free approach to anxiety reduction in the preoperative period, complementing standard care protocols.
Author contributions
RJ contributed to the design, participated in most of the study steps. RJ and NarS prepared the manuscript and gathered data. NadS analyzed the data.
Funding
Kermanshah University of Medical Sciences, grant no 4020116.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The study received approval from the Ethics Committee of Kermanshah University of Medical Sciences (code: IR.KUMS.REC.1401.503) and was registered with the Iranian Registry of Clinical Trials (IRCT20130603013568N7). Written informed consent was obtained from all participants.
Consent for publication
All authors read and confirmed the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dan, W. Y., Yang, Y. S., Peng, L. H., Sun, G. & Wang, Z. K. Gastrointestinal microbiome and cholelithiasis: current status and perspectives. World J. Gastroenterol.29 (10), 1589–1601 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen, L. et al. Insights into modifiable risk factors of cholelithiasis: a mendelian randomization study. Hepatology. 75 (4), 785–796 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cianci, P. & Restini, E. Management of cholelithiasis with choledocholithiasis: endoscopic and surgical approaches. World J. Gastroenterol.27 (28), 4536–4554 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin, H., Zhang, J., Li, X., Li, Y. & Su, S. Comparative outcomes of single-incision laparoscopic, mini-laparoscopic, four-port laparoscopic, three-port laparoscopic, and single-incision robotic cholecystectomy: a systematic review and network meta-analysis. Updates Surg.75(1), 41–51 (2023). [DOI] [PubMed] [Google Scholar]
- 5.Wang, W., Wang, L. & Gao, Y. A. Meta-analysis of randomized controlled trials concerning the efficacy of transversus abdominis plane block for pain control after laparoscopic cholecystectomy. Front. Surg.8, 700318 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulita, F. et al. Comparison of analgesic efficacy of acetaminophen monotherapy versus acetaminophen combinations with either pethidine or parecoxib in patients undergoing laparoscopic cholecystectomy: a randomized prospective study. Med. Glas (Zenica). 18(1), 27–32 (2021). [DOI] [PubMed] [Google Scholar]
- 7.Jarrah, M. I. et al. The effect of slow deep breathing relaxation exercise on pain levels during and post chest tube removal after coronary artery bypass graft surgery. Int. J. Nurs. Sci.9(2), 155–161 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourgeois, C. et al. Pain management after laparoscopic cholecystectomy: a systematic review and procedure-specific postoperative pain management (PROSPECT) recommendations. Eur. J. Anaesthesiol. (2024). [DOI] [PubMed]
- 9.Bastamizad, N., Abbasi, P., Salari, N. & Jalali, R. Comparing the effect of incentive spirometry and deep breathing exercises on the level of shoulder pain and nausea following laparoscopic cholecystectomy surgery: a clinical Trial Study. Gastroenterol. Nurs.46(1), 14–22 (2023). [DOI] [PubMed] [Google Scholar]
- 10.Sadati, L. et al. Effect of preoperative nursing visit on preoperative anxiety and postoperative complications in candidates for laparoscopic cholecystectomy: a randomized clinical trial. Scand. J. Caring Sci.27(4), 994–998 (2013). [DOI] [PubMed] [Google Scholar]
- 11.Toğaç, H. K. & Yılmaz, E. Effects of preoperative individualized audiovisual education on anxiety and comfort in patients undergoing laparoscopic cholecystectomy: randomised controlled study. Patient Educ. Couns.104 (3), 603–610 (2021). [DOI] [PubMed] [Google Scholar]
- 12.Thurston, K. L., Zhang, S. J., Wilbanks, B. A., Billings, R. & Aroke, E. N. A systematic review of race, sex, and socioeconomic status differences in postoperative pain and pain management. J. Perianesth. Nurs.38(3), 504–515 (2023). [DOI] [PubMed] [Google Scholar]
- 13.Gin, E., Lowen, D., Tacey, M. & Hodgson, R. Reduced laparoscopic intra-abdominal pressure during laparoscopic cholecystectomy and its effect on post-operative pain: a double-blinded randomised control trial. J. Gastrointest. Surg.25(11), 2806–2813 (2021). [DOI] [PubMed] [Google Scholar]
- 14.Coppes, O. J. M., Yong, R. J., Kaye, A. D. & Urman, R. D. Patient and surgery-related predictors of acute postoperative pain. Curr. Pain Headache Rep.24(4), 12 (2020). [DOI] [PubMed] [Google Scholar]
- 15.Shawahna, R. et al. Prevalence of preoperative anxiety among hospitalized patients in a developing country: a study of associated factors. Perioper Med. (Lond). 12(1), 47 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang, R., Huang, X., Wang, Y. & Akbari, M. Non-pharmacologic approaches in preoperative anxiety, a comprehensive review. Front. Public. Health. 10, 854673 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agüero-Millan, B. & Abajas-Bustillo, R. & Ortego-Maté, C. Efficacy of nonpharmacologic interventions in preoperative anxiety: a systematic review of systematic reviews. J. Clin. Nurs. (2023). [DOI] [PubMed]
- 18.Tom, K. & Phang, P. T. Effectiveness of the video medium to supplement preoperative patient education: a systematic review of the literature. Patient Educ. Couns.105(7), 1878–1887 (2022). [DOI] [PubMed] [Google Scholar]
- 19.Madsen, B. K., Zetner, D., Møller, A. M. & Rosenberg, J. Melatonin for preoperative and postoperative anxiety in adults. Cochrane Database Syst. Rev.12(12), Cd009861 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tola, Y. O., Chow, K. M. & Liang, W. Effects of non-pharmacological interventions on preoperative anxiety and postoperative pain in patients undergoing breast cancer surgery: a systematic review. J. Clin. Nurs.30 (23–24), 3369–3384 (2021). [DOI] [PubMed] [Google Scholar]
- 21.Wang, Y., Huang, X. & Liu, Z. The effect of preoperative health education, delivered as animation videos, on postoperative anxiety and pain in femoral fractures. Front. Psychol.13, 881799 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi, H. & Kim, J. Effects of multimedia-based information on anxiety, discomfort and satisfaction with care among patients undergoing cerebral angiography: a quasi-experimental study. J. Clin. Nurs.31 (7–8), 949–957 (2022). [DOI] [PubMed] [Google Scholar]
- 23.Abdulrahaman, M. D. et al. Multimedia tools in the teaching and learning processes: a systematic review. Heliyon. 6(11), e05312 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vagg, T., Balta, J. Y., Bolger, A. & Lone, M. Multimedia in education: what do the students think? Health Prof. Edu. 6(3), 325–333 (2020). [Google Scholar]
- 25.Huang, H. et al. Clinical application value of multimedia education and nursing intervention in a coronary computed tomography angiography. Clin. Nurs. Res.31(4), 607–614 (2022). [DOI] [PubMed] [Google Scholar]
- 26.Cavanagh, T. M. & Kiersch, C. Using commonly-available technologies to create online multimedia lessons through the application of the cognitive theory of multimedia learning. Educ. Technol. Res. Dev. 1–21 (2022). [DOI] [PMC free article] [PubMed]
- 27.Bernard, A. L. et al. The impact of an interactive multimedia educational platform on patient comprehension and anxiety during fertility treatment: a randomized controlled trial. F S Rep.3 (3), 214–222 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanyeki, T., Mung’ayi, V., Bal, R. & Odaba, D. Effect of video-based information on preoperative state trait anxiety inventory scores in adult patients presenting for elective caesarean section: a randomized controlled trial. Afr. Health Sci.22 (3), 117–124 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Metterlein, T. et al. Effectiveness of pre-anesthetic video information on patient anxiety and economical aspects. Saudi J. Anaesth.15 (2), 127–130 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mayer, R. E. How multimedia can improve learning and instruction. In: (eds Dunlosky, J. & Rawson, K. A.) The Cambridge Handbook of Cognition and Education. New York, NY, US: Cambridge University Press; 460–479. (2019). [Google Scholar]
- 31.Hou, H. et al. Effect of interactive, multimedia-based home-initiated education on preoperative anxiety inchildren and their parents: a single-center randomized controlled trial. BMC Anesthesiol. 23 (1), 95 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karalar, M., Demirbas, A., Gercek, O., Topal, K. & Keles, I. Impact of preoperative video-based education on anxiety levels in patients with renal stones scheduled for flexible ureteroscopic lithotripsy: a comparative study using APAIS and STAI. Med. Sci. Monit.29, e941351 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rajput, S. K., Tiwari, T. & Chaudhary, A. K. Effect of preoperative multimedia based video information on perioperative anxiety and hemodynamic stability in patients undergoing surgery under spinal anesthesia. J. Family Med. Prim. Care. 10 (1), 237–242 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stergiopoulou, A., Birbas, K., Katostaras, T. & Mantas, J. The effect of interactive multimedia on preoperative knowledge and postoperative recovery of patients undergoing laparoscopic cholecystectomy. Methods Inf. Med.46 (4), 406–409 (2007). [DOI] [PubMed] [Google Scholar]
- 35.Aydal, P., Uslu, Y. & Ulus, B. The effect of preoperative nursing visit on anxiety and pain level of patients after surgery. J. Perianesth. Nurs.38 (1), 96–101 (2023). [DOI] [PubMed] [Google Scholar]
- 36.Grech, V. The application of the Mayer multimedia learning theory to medical PowerPoint slide show presentations. J. Vis. Commun. Med.41 (1), 36–41 (2018). [DOI] [PubMed] [Google Scholar]
- 37.Gökçe, E. & Arslan, S. Possible effect of video and written education on anxiety of patients undergoing coronary angiography. J. Perianesth. Nurs.34 (2), 281–288 (2019). [DOI] [PubMed] [Google Scholar]
- 38.Omezli, M. M., Torul, D. & Kahveci, K. Does watching videos increase the perioperative anxiety in patients undergoing third molar surgery? A randomized trial. J. Oral Maxillofac. Surg.78(2), 216e211–216e219 (2020). [DOI] [PubMed] [Google Scholar]
- 39.Shreyas, K. et al. Effect of multimedia teaching tools in parental anxiety and comprehension of informed consent procedure in pediatric surgical procedures: a single centre randomized control trial. J. Pediatr. Surg.58 (10), 2000–2005 (2023). [DOI] [PubMed] [Google Scholar]
- 40.Wu, K. L. et al. The effectiveness of an accessibility-enhanced multimedia informational educational programme in reducing anxiety and increasing satisfaction of patients undergoing cardiac catheterisation. J. Clin. Nurs.23 (13–14), 2063–2073 (2014). [DOI] [PubMed] [Google Scholar]
- 41.Liu, Y. et al. The effects of video based nursing education on perioperative anxiety and depression in patients with gastric cancer. Psychol. Health Med.26(7), 867–876 (2021). [DOI] [PubMed] [Google Scholar]
- 42.Shao, J. et al. Effect of multimedia-based nursing visit on perioperative anxiety in esophageal squamous cell carcinoma patients undergoing video-assisted thoracoscopic surgery. Psychol. Health Med.24(10), 1198–1206 (2019). [DOI] [PubMed] [Google Scholar]
- 43.Jellish, W. S. & O’Rourke, M. Anxiolytic use in the postoperative care unit. Anesthesiol .Clin.30(3), 467–480 (2012). [DOI] [PubMed] [Google Scholar]
- 44.Rau, N. M. et al. Multimedia tablet or paper handout to supplement counseling during preterm birth hospitalization: a randomized controlled trial. Am. J. Obstet. Gynecol. MFM. 5(4), 100875 (2023). [DOI] [PubMed] [Google Scholar]
- 45.Saviola, F. et al. Trait and state anxiety are mapped differently in the human brain. Sci. Rep.10(1), 11112 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hajibandeh, S. et al. Meta-analysis and trial sequential analysis of three-port vs four-port laparoscopic cholecystectomy (level 1 evidence). Updates Surg.73(2), 451–471 (2021). [DOI] [PubMed] [Google Scholar]
- 47.Çallıoğlu, N. et al. The effect of informing the patient about the procedure with video imaging before office hysteroscopy on pain. J. Obstet. Gynaecol. Res.49(9), 2387–2392 (2023). [DOI] [PubMed] [Google Scholar]
- 48.Osman, Y. et al. The comparison of pulmonary functions in open versus laparoscopic cholecystectomy. J. Pak Med. Assoc.59(4), 201–204 (2009). [PubMed] [Google Scholar]
- 49.Bablekos, G. D., Michaelides, S. A., Analitis, A. & Charalabopoulos, K. A. Effects of laparoscopic cholecystectomy on lung function: a systematic review. World J. Gastroenterol.20(46), 17603–17617 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lee, S. Y. et al. The effect of ultrasound-guided transversus abdominis plane block on pulmonary function in patients undergoing laparoscopic cholecystectomy: a prospective randomized study. Surg. Endosc. 36(10), 7334–7342 (2022). [DOI] [PubMed] [Google Scholar]
- 51.Fernandez Rojas, R., Brown, N., Waddington, G. & Goecke, R. A systematic review of neurophysiological sensing for the assessment of acute pain. NPJ Digit. Med.6(1), 76 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.