Abstract
Purpose
Substance use and traumatic events are prevalent in Afghanistan, but their relationship is under-investigated.
Methods
A nationally-representative, cross-sectional survey was conducted in 8 regions of Afghanistan in 2017 (N = 4474). First, we examined the burden of substance use, and demographic correlates (e.g., gender, age) in the Afghan general population; second, we examined the association between traumatic and stressful experiences, including PTSD, and any substance use, tobacco use and sedative use.
Results
Substance use disorder is prevalent in Afghanistan, with prevalence of any substance use at 5.03%, tobacco use at 21.82%, and sedative use prevalence at 6.71%. Women and people with middle and high economic status were less likely to use any substance and tobacco, however, women were more likely use sedative compared to men. People who had collective violence and experienced any traumatic event more likely to use any substances, tobacco and sedative compared to their counterparts. Finally, individuals with PTSD, depression and generalized anxiety were more likely to use any substances, tobacco and sedative compared to individuals without these psychiatric disorders.
Conclusion
Substance use and dependence are prevalent in Afghanistan, an area with exposure to conflict and trauma for a majority of the population, underscoring the pervasive impact of trauma exposure on population health in this area. As resources are deployed to assist the Afghan population through conflict, attention to substance use and psychiatric disorders is needed to fully address population health.
Keywords: Depression, Generalized anxiety, PTSD, Substance use, Tobacco use, Traumatic event
Introduction
Afghanistan is a country that has experienced more than 45 years of political and social unrest after the army revolution in 1978, and is a major source of cultivation and production of opium globally. Afghanistan accounted for approximately 85% of global opium production in 2020, supplying an estimated 80% of all illicit opioid users in the world [1]. Furthermore, during these decades most Afghans have been exposed to range of violence and traumatic events either experienced or witnessed. Two of three Afghan individuals (64.67%) experienced at least one type of traumatic event based on nationally representative survey reports in 2018 [2], and many experienced multiple traumatic events. This combination of high drug production and a heavily traumatized population raise concerns about the public health impact of substance use in Afghanistan.
Available data indicate that substance use remains prevalent in the Afghan general population. While use of any intoxicant is legally prohibited in Afghanistan, in practice there are limited sanctions on use except when associated with a drug-related crime such as a road accident or drug trafficking. A 2018 national mental health survey reported that approximately 1 in 5 adults in Afghanistan had moderate tobacco dependence, and 2.3% reporting high levels of tobacco dependence. Sedative use was also prevalent, with 3.7% of the population reporting moderate risk and 1.2% high risk. The alcohol and cannabis use in Afghanistan was low in prevalence and found to be 0.7% and 3.2% respectively [3]. Understanding how substance use potentially varies with and is shaped by traumas experienced in the Afghan general population is of importance to public health given the health consequences of heavy substance use, and the high exposure to trauma. Further, studies are needed that estimate substance use disorder and dependence risk, which is dimensional and can range from mild to severe based on the level of substance use and the problems experienced associated with use. Few studies in Afghanistan have estimated substance use disorder risks.
Many studies have documented that exposure to traumatic events is associated with risk for initiating substance use and developing a substance use disorders. Data from the World Health Organization World Mental Health Surveys documented that lifetime substance use disorders (SUD) prevalence almost three times higher among those traumatic exposed compared to those with no trauma exposure [4], and associations are strong between all types of traumas and the risk of several specific substance and behavioral dependences [5]. A systematic review of literature found that, across countries, the rates of lifetime trauma exposure vary from 21 to 98% and are correlated with increased rates of substance use and SUDs. As traumatic event experiences increase, so too does risk for substance use and SUDs, including in populations with high exposure to trauma such as reservation-based American Indian populations [6]. Further there is a higher prevalence of adverse childhood experiences (ACEs) in populations with SUD than in those without reported ACEs, and a positive association between ACEs and the development and severity of SUD in adolescence and adulthood [7]. Posttraumatic stress disorder (PTSD) and substance use disorders (SUDs) are prevalent and frequently co-occur [8], and surviving multiple traumas including sexual abuse is most highly associated with PTSD [9] as well as subsequent risk for substance use and SUDs [10, 11]. Indeed, while existing literature indicates comorbidity between SUDs and other mental health disorders [12, 13], few studies have documented the magnitude of the associations in the Afghan context.
More knowledge about the relationship between exposures to traumatic experiences and the risk of substance abuse in the Afghan population is important to document, given that Afghanistan is a low resource setting and understanding the extent of public health problems is critical to allocating resources improve the wellbeing of Afghan people both those who remain in and those who have emigrated. The present study analyzes the largest dataset of traumatic events and substance use conducted to date in the Afghan general population to address two aims: first, we examine the burden of substance use, and demographic correlates including gender and age, in the Afghan general population; and second, we examine the association of traumatic and stressful experiences with any substance use, tobacco use and sedative use. We also highlight the associations between substance use disorders and other mental health disorders, providing assessment of comorbidity in the Afghan context.
Methods
Sample
A cross-sectional household survey was implemented from April to October 2017 in each of the eight regions of Afghanistan: (1) Eastern; (2) South Eastern; (3) Southern; (4) Western; (5) North Western; (6) North Eastern; (7) Central Kabul; and (8) Central Bamiyan. A multi-stage stratified cluster sampling method was applied: in each region, two provinces were randomly selected totaling 16 provinces out of a possible 34. A random sampling of clusters within province was selected, based on maps of 320 clusters provided by the Central Statistical Organization. Within each cluster, 14 households were randomly selected, and eligibility criteria assessed [14]. In the household, a randomized adult selection was based on Kish selection before starting the interview. Eligibility included Afghan males and females, at least 15 years old, who were residents of the household and who had given consent to participate in the study. The study aimed to estimate prevalence of common mental health problems in the population aged 15 or older; thus, the study was powered to estimate predictors of an outcome with prevalence of at most 20% based on existing global literature. Based on an estimated 20% outcome, minimum total sample size per region was 246 using simple random sampling assumptions; because our design was multistage cluster sampling, considering the design effect of two, and anticipating the non-response to be 10%, the final target sample size in each region was 542, rendering a total sample size for the country of 4475 head of family members and 4474 individuals. A consent form was read aloud and accepted for each selected person before survey initiation; those who did not accept were excluded. Sampling weights were created based on the age and gender of the population based on census data and applied to the sample to approximate national distributions. A team of one female and one male was responsible to collect data from each household. Data collection was supervised by provincial supervisors, and regular monitoring visits were conducted by monitoring officers. Furthermore, the provincial public health directorate also conducted supervisory visits from the data collection process. The overall response rate for most of variables found to be at least 99%. Details of the study design and methodology can be found elsewhere [2].
The distributions of study demographics are found in our previous publications [2]. Briefly, 52.62% of the weighted individual sample completed no formal education and did not have any reading skills, 3.5% did not complete primary school, 6.4% completed primary, 8.5% secondary, 18.1% college, and 7.9% university. 53.5% of the sample declared no income, with distinct differences by sex; 84.6% of women and 22.6% of men reported no income. 13.7% of the sample reported working in agriculture or animal husbandry, 13.8% as a laborer, 9.1% salaried, and 3.7% in business or trading. Income was linked to the type of employment: those in agriculture, farming, or as laborer earned an average of 7200 AFS (100$), whereas those in business earned 12,982 AFS (200$) on average. Female disadvantage persisted for women who earned an income: 42% of women who worked were in the lowest income category versus 16% of men. Urban people reported to higher income groups compared with rural people. On the total weighted sample, 27.6% were Tajik, 47.82 were Pashtu, 11.4% Hazara, 6.6% Uzbek, 6.7% another ethnicity (for 0.1% the information was missing). As expected, ethnicities were very different across regions [2].
Instruments
The questionnaire collected pertinent socio-demographic information. Post-traumatic stress disorder was assessed with the life event checklist 5 (LEC-5) together with PTSD Check-List 5 (PCL) [15, 16]; using the DSM-5 algorithm. We categorized lifetime experiences of traumatic events in six groups: collective violence, sexual violence, accidental injury, cause/ witnessed harm, interpersonal violence, and any traumatic events. First, collective violence included those who experience or witness (1) fire or explosion; (2) assault with a weapon (for example, being shot, stabbed, threatened with a knife, gun, bomb); (3) combat or exposure to a warzone (in the military or as a civilian); and (4) captivity (for example, being kidnapped, abducted, held hostage, prisoner of war). Second, sexual violence included experience or witness of (1) sexual assault (rape, attempted rape, made to perform any type of sexual act through force or threat of harm); and (2) other unwanted or uncomfortable sexual experience (for example, doing sex during ministration, doing sex without your permission with your partner). Third, accidental injury included experience or witness of (1) natural disaster (for example, food, earthquake); (2) transportation accident (for example, car accident, plane crash); (3) serious accident at work, home, or during any activity; (4) exposure to toxic substance (for example, mercury, benzene); and (5) life-threatening illness or injury; and only witnessed of sudden accidental death. Forth, cause/witnessed harm included witness of (1) sudden violent death (for example, homicide, suicide) and (2) sudden accidental death. Fifth, interpersonal violence included experience or witness of physical assault (for example, being attacked, hit, slapped, kicked, beaten up); and finally, the sixth is any traumatic event who experienced and witnessed for any of events. This classification was previously used by other authors [17, 18]. It is worth noting that first all violence were categorized in three categories: total, experienced and witnessed and second, the number of traumatic events was classified into three groups: no traumatic events, 1 to 3 events and more than 3 events [18].
Information about substance abuse was collected by the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) [19]. Information on cigarette smoking, sedative use, and any other drug use was assessed, and problems related to substance use disorders were categorized based on established cut-points for the ASSIST into no risk, moderate, and high risk for smoking, sedative use, and any substance use. We defined any substance use as those who use cannabis, cocaine, amphetamine, inhalant, hallucinogen, opioids, narcotic and alcohol. Sedative and tobacco use were not included as part of the any substance use category.
Data management and analysis
All data were entered twice in the Census and Survey Processing System (CS-Pro), and both datasets were verified for any consistency. If inconsistencies were found, the original questionnaire was re-checked to validate the response and the corrective measures were taken. Finally, the clean dataset was integrated into STATA and further cleaning processes were conducted by a statistician and analyst. Analyses were done with STATA 17, and all analyses incorporated sampling weights. First, frequencies and prevalence were estimated for all study variables, including outcome variables (any substance abuse, and traumatic events). Second, the outcome variables were cross tabulated by independent variables to assess any bivariate relationship. Finally, logistic regression was run to determine the strength of association, adjusted for demographics and number of traumatic events.
Results
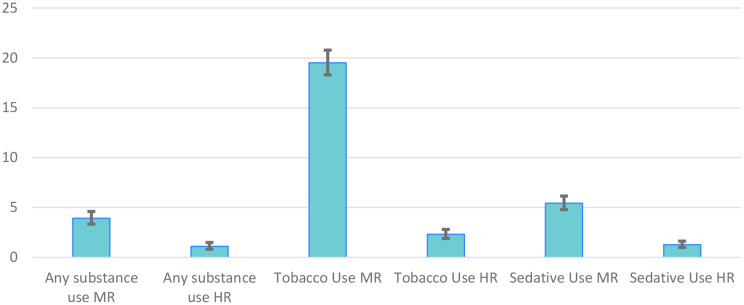
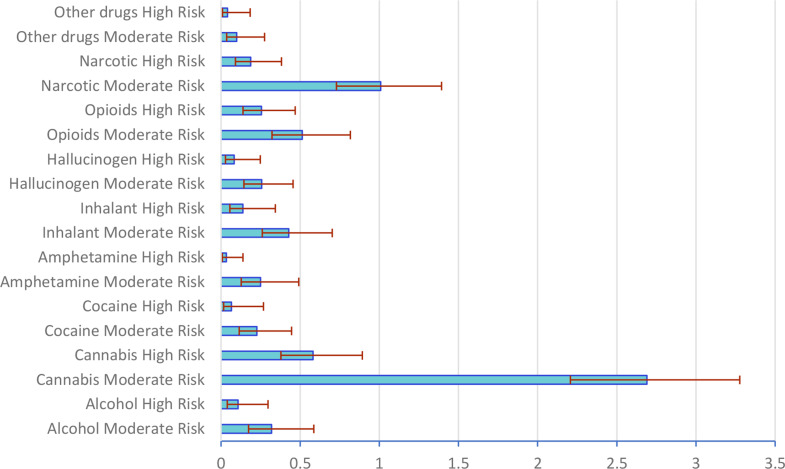
In the total sample, 3.9% (95% CI; 3.3,4.6) and 1.1% (95% CI, 0.8, 1.5) of respondents had moderate and high risk of substance use(Fig. 1). It was found that cannabis (combined moderate and high risk prevalence of 3.3%) was the most common substance used by Afghan population followed by narcotics (combined moderate and high risk prevalence of 1.2%) and opioids (combined moderate and high risk prevalence of 0.8%) (Fig. 2). By sex there was a significant difference of moderate and high risk of any substance use between male and female (6.2% vs. 1.7%: and 2% vs. 0.2%). There was a statistically significant difference between sex, various education levels; various ethnic groups; urban and rurality; different regions and socio-economic status across all outcomes: any substance use, tobacco use and sedative use. While age and marital status were found to be associated with tobacco and sedative use, they were not associated with the combined any substance use category. Furthermore, different occupations found to be associated with any substance use and tobacco use but they had no association with sedative use. Moreover, the cross tabulation suggested that there is a statistical difference for the collective violence, caused/witnessed harm, interpersonal violence, witness of sexual violence, accidental injury, witness of accidental death, any traumatic events and the number of traumatic events, depression, generalized anxiety and PTSDS across all outcomes: any substance use, tobacco use and sedative use risk. (Tables 1 and 2)
Fig. 1.
Percent of moderate and high risk of any substance, tobacco and sedative use along with 95% CI
Fig. 2.
Prevalence of substance use with 95% CI
Table 1.
Prevalence of moderate and high risk scores for any substance use, tobacco use, and sedative use by general characteristics in the Afghan general population
| Variables/Characteristics | Any substance use | Tobacco Use | Sedative Use | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | No | Moderate | High | P-value | n | No | Moderate | High | P-value | n | No | Moderate | High | P-value | ||||||||||||
| Sex | ||||||||||||||||||||||||||
| Female | 2561 | 98.13 | [97.47,98.61] | 1.66 | [1.20,2.29] | 0.21 | [0.09,0.50] | < 0.001 | 2561 | 92.03 | [90.92,93.02] | 6.64 | [5.73,7.67] | 1.33 | [0.95,1.86] | < 0.001 | 2559 | 91.32 | [90.13,92.38] | 6.97 | [6.02,8.07] | 1.71 | [1.27,2.28] | < 0.001 | ||
| Male | 1864 | 91.83 | [90.45,93.03] | 6.17 | [5.12,7.41] | 2.00 | [1.45,2.75] | 1865 | 64.43 | [62.19,66.61] | 32.29 | [30.17,34.48] | 3.29 | [2.59,4.17] | 1864 | 95.24 | [94.17,96.12] | 3.91 | [3.10,4.91] | 0.85 | [0.54,1.34] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| Education | ||||||||||||||||||||||||||
| No Education | 2690 | 95.43 | [94.47,96.24] | 3.16 | [2.51,3.97] | 1.41 | [0.98,2.02] | < 0.001 | 2690 | 77.88 | [76.16,79.52] | 19.33 | [17.77,20.99] | 2.79 | [2.20,3.52] | 0.002 | 2689 | 92.06 | [90.95,93.04] | 6.18 | [5.31,7.19] | 1.75 | [1.33,2.31] | 0.017 | ||
| Less than Primary and Primary | 394 | 90.4 | [86.75,93.12] | 7.51 | [5.11,10.90] | 2.1 | [1.03,4.21] | 394 | 71.52 | [66.64,75.93] | 25.1 | [20.91,29.82] | 3.38 | [1.93,5.87] | 394 | 94.10 | [91.32,96.03] | 4.80 | [3.11,7.33] | 1.10 | [0.40,2.98] | |||||
| Secondary and High School | 907 | 95.47 | [93.82,96.70] | 3.9 | [2.77,5.48] | 0.63 | [0.27,1.42] | 908 | 80.45 | [77.71,82.92] | 17.74 | [15.37,20.40] | 1.81 | [1.15,2.84] | 907 | 95.13 | [93.53,96.35] | 4.11 | [2.99,5.63] | 0.76 | [0.38,1.51] | |||||
| University and other | 416 | 95.46 | [92.84,97.15] | 4.54 | [2.85,7.16] | 0 | 416 | 80.31 | [76.00,84.01] | 19.34 | [15.68,23.61] | 0.35 | [0.05,2.43] | 415 | 93.71 | [90.95,95.67] | 5.84 | [3.94,8.57] | 0.45 | [0.14,1.41] | ||||||
| Total | 4407 | 94.95 | [94.19,95.62] | 3.94 | [3.35,4.63] | 1.11 | [0.82,1.51] | 4408 | 78.2 | [76.88,79.47] | 19.48 | [18.26,20.75] | 2.32 | [1.91,2.82] | 4405 | 93.26 | [92.48,93.97] | 5.46 | [4.81,6.18] | 1.28 | [1.00,1.64] | |||||
| Occupation | ||||||||||||||||||||||||||
| Service/Salaried/Business/Trading | 523 | 94.42 | [91.99,96.14] | 4.74 | [3.18,7.01] | 0.84 | [0.31,2.30] | < 0.001 | 523 | 69.96 | [65.73,73.86] | 28.02 | [24.20,32.19] | 2.03 | [1.14,3.56] | < 0.001 | 523 | 93.92 | [91.55,95.66] | 5.16 | [3.56,7.43] | 0.92 | [0.41,2.05] | 0.321 | ||
| Labor | 555 | 90.72 | [87.84,92.97] | 6.31 | [4.49,8.79] | 2.97 | [1.78,4.91] | 556 | 65.09 | [60.89,69.07] | 31.08 | [27.25,35.18] | 3.83 | [2.50,5.82] | 555 | 94.55 | [92.27,96.19] | 4.48 | [3.01,6.62] | 0.97 | [0.42,2.21] | |||||
| Agriculture/Rearing Animals | 585 | 93.16 | [90.64,95.03] | 5.32 | [3.65,7.68] | 1.53 | [0.82,2.83] | 585 | 62.68 | [58.54,66.64] | 33.22 | [29.39,37.29] | 4.10 | [2.78,6.01] | 584 | 94.67 | [92.46,96.26] | 4.33 | [2.89,6.44] | 1.00 | [0.48,2.09] | |||||
| No Source of Income | 2491 | 97.04 | [96.18,97.71] | 2.46 | [1.85,3.27] | 0.5 | [0.27,0.91] | 2491 | 87.78 | [86.32,89.10] | 10.67 | [9.42,12.06] | 1.55 | [1.12,2.15] | 2490 | 92.49 | [91.38,93.47] | 6.06 | [5.17,7.09] | 1.45 | [1.07,1.97] | |||||
| Other | 223 | 91.95 | [87.01,95.12] | 6.57 | [3.74,11.28] | 1.48 | [0.47,4.55] | 223 | 73.8 | [67.44,79.31] | 23.7 | [18.43,29.92] | 2.50 | [1.10,5.59] | 223 | 94.26 | [90.65,96.52] | 3.61 | [2.02,6.36] | 2.14 | [0.83,5.38] | |||||
| Total | 4377 | 95.01 | [94.25,95.68] | 3.9 | [3.32,4.59] | 1.08 | [0.80,1.47] | 4378 | 78.1 | [76.77,79.37] | 19.57 | [18.35,20.85] | 2.33 | [1.92,2.84] | 4044 | 93.36 | [92.58,94.06] | 5.35 | [4.71,6.07] | 1.29 | [1.01,1.65] | |||||
| Age | ||||||||||||||||||||||||||
| 15–24 Yrs | 1101 | 95.25 | [93.78,96.38] | 4.08 | [3.04,5.46] | 0.67 | [0.32,1.41] | 0.063 | 1102 | 87.00 | [84.83,88.90] | 11.89 | [10.07,14.00] | 1.11 | [0.63,1.94] | < 0.001 | 1100 | 95.09 | [93.65,96.22] | 4.56 | [3.48,5.95] | 0.35 | [0.13,0.94] | < 0.001 | ||
| 25–34 Yrs | 1043 | 93.99 | [92.16,95.41] | 4.3 | [3.12,5.89] | 1.71 | [1.01,2.89] | 1043 | 76.02 | [73.06,78.75] | 21.68 | [19.05,24.57] | 2.30 | [1.49,3.54] | 1043 | 93.81 | [92.21,95.10] | 4.94 | [3.80,6.40] | 1.25 | [0.75,2.09] | |||||
| 35–44 Yrs | 980 | 94.3 | [92.46,95.72] | 3.66 | [2.56,5.21] | 2.04 | [1.25,3.31] | 980 | 72.09 | [68.99,75.00] | 24.70 | [21.91,27.72] | 3.21 | [2.20,4.67] | 979 | 90.19 | [88.16,91.91] | 7.70 | [6.19,9.54] | 2.11 | [1.36,3.25] | |||||
| 45–54 Yrs | 734 | 95.28 | [93.39,96.66] | 4.11 | [2.84,5.91] | 0.61 | [0.23,1.62] | 734 | 73.47 | [70.01,76.67] | 23.44 | [20.38,26.80] | 3.09 | [2.03,4.67] | 734 | 92.4 | [90.28,94.09] | 5.74 | [4.28,7.65] | 1.86 | [1.12,3.08] | |||||
| 55 + Yrs | 567 | 96.44 | [94.53,97.70] | 2.85 | [1.74,4.62] | 0.71 | [0.27,1.87] | 567 | 66.69 | [62.66,70.49] | 29.08 | [25.45,33.00] | 4.22 | [2.86,6.19] | 567 | 91.46 | [88.85,93.51] | 5.93 | [4.28,8.16] | 2.61 | [1.53,4.42] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| Marital Status | ||||||||||||||||||||||||||
| Never married | 868 | 94.67 | [92.93,96.01] | 4.66 | [3.43,6.32] | 0.66 | [0.29,1.51] | 0.144 | 869 | 86.37 | [83.87,88.53] | 12.39 | [10.32,14.81] | 1.25 | [0.68,2.26] | < 0.001 | 867 | 94.85 | [93.15,96.14] | 4.58 | [3.37,6.21] | 0.57 | [0.24,1.31] | < 0.001 | ||
| Married | 3345 | 95.01 | [94.12,95.76] | 3.63 | [2.99,4.39] | 1.37 | [0.99,1.88] | 3345 | 74.32 | [72.70,75.87] | 22.91 | [21.42,24.48] | 2.77 | [2.24,3.41] | 3344 | 92.95 | [92.03,93.76] | 5.69 | [4.95,6.53] | 1.36 | [1.04,1.79] | |||||
| Widowed / Divorce or separated | 200 | 96.31 | [92.23,98.28] | 3.69 | [1.72,7.77] | 0 | 200 | 83.97 | [77.80,88.67] | 13.48 | [9.20,19.34] | 2.55 | [1.00,6.33] | 200 | 86.94 | [81.32,91.05] | 7.73 | [4.87,12.06] | 5.34 | [2.71,10.23] | ||||||
| Total | 4413 | 94.96 | [94.20,95.62] | 3.93 | [3.34,4.62] | 1.11 | [0.82,1.50] | 4414 | 78.18 | [76.86,79.44] | 19.5 | [18.29,20.78] | 2.32 | [1.90,2.82] | 4411 | 93.27 | [92.49,93.98] | 5.45 | [4.80,6.17] | 1.28 | [1.00,1.64] | |||||
| Ethnicity | ||||||||||||||||||||||||||
| Tajik | 1186 | 95 | [93.53,96.15] | 4.33 | [3.25,5.74] | 0.67 | [0.34,1.30] | 0.037 | 1186 | 84.31 | [82.02,86.37] | 13.51 | [11.60,15.69] | 2.17 | [1.46,3.22] | < 0.001 | 1186 | 92.06 | [90.37,93.47] | 7.09 | [5.75,8.72] | 0.85 | [0.47,1.51] | < 0.001 | ||
| Pashtun | 2136 | 94.27 | [93.07,95.28] | 4.05 | [3.21,5.10] | 1.68 | [1.17,2.39] | 2136 | 72.99 | [70.92,74.96] | 24.45 | [22.55,26.47] | 2.56 | [1.95,3.34] | 2135 | 93.45 | [92.31,94.44] | 4.54 | [3.71,5.54] | 2.01 | [1.51,2.66] | |||||
| Hazara | 490 | 97.22 | [95.06,98.45] | 2.78 | [1.55,4.94] | 0 | 490 | 83.07 | [79.33,86.24] | 16.08 | [12.97,19.76] | 0.85 | [0.34,2.11] | 489 | 93.1 | [90.69,94.91] | 6.51 | [4.74,8.88] | 0.39 | [0.13,1.22] | ||||||
| Uzbek | 286 | 94.86 | [90.89,97.16] | 4.69 | [2.52,8.59] | 0.44 | [0.06,3.08] | 287 | 79.8 | [74.49,84.24] | 18.36 | [14.12,23.53] | 1.84 | [0.76,4.39] | 286 | 93.67 | [89.82,96.13] | 6.33 | [3.87,10.18] | 0 | 0 | |||||
| Other | 284 | 96.27 | [92.60,98.16] | 2.15 | [0.87,5.24] | 1.57 | [0.51,4.79] | 284 | 78.54 | [73.15,83.10] | 17.61 | [13.45,22.71] | 3.85 | [2.10,6.92] | 284 | 96.99 | [94.05,98.50] | 3.01 | [1.50,5.95] | 0 | 0 | |||||
| Total | 4382 | 94.98 | [94.22,95.65] | 3.9 | [3.31,4.59] | 1.12 | [0.83,1.51] | 4383 | 78.08 | [76.75,79.35] | 19.63 | [18.41,20.91] | 2.29 | [1.88,2.80] | 4380 | 93.28 | [92.49,93.99] | 5.48 | [4.84,6.21] | 1.24 | [0.96,1.59] | |||||
| Rurality | ||||||||||||||||||||||||||
| Urban | 1157 | 97.42 | [96.17,98.27] | 2.13 | [1.36,3.31] | 0.45 | [0.18,1.13] | < 0.001 | 1158 | 87.38 | [85.21,89.27] | 11.17 | [9.39,13.25] | 1.45 | [0.89,2.34] | < 0.001 | 1156 | 95.21 | [93.79,96.32] | 4.13 | [3.09,5.50] | 0.66 | [0.35,1.22] | 0.004 | ||
| Rural | 3268 | 94.07 | [93.11,94.90] | 4.58 | [3.85,5.44] | 1.35 | [0.98,1.86] | 3268 | 74.8 | [73.18,76.35] | 22.57 | [21.08,24.14] | 2.63 | [2.12,3.26] | 3267 | 92.58 | [91.63,93.44] | 5.91 | [5.14,6.79] | 1.51 | [1.15,1.97] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| Region | ||||||||||||||||||||||||||
| Central | 539 | 96.45 | [94.27,97.81] | 2.87 | [1.67,4.86] | 0.69 | [0.21,2.18] | < 0.001 | 539 | 88.61 | [85.38,91.20] | 9.68 | [7.29,12.75] | 1.71 | [0.87,3.32] | < 0.001 | 539 | 94.32 | [92.07,95.96] | 5.17 | [3.60,7.38] | 0.51 | [0.19,1.37] | < 0.001 | ||
| South | 560 | 95.7 | [93.37,97.24] | 2.12 | [1.14,3.91] | 2.18 | [1.15,4.10] | 560 | 64.95 | [60.50,69.16] | 31.25 | [27.17,35.64] | 3.80 | [2.40,5.96] | 560 | 93.83 | [91.62,95.49] | 3.23 | [2.06,5.03] | 2.93 | [1.89,4.53] | |||||
| East | 554 | 94.94 | [92.58,96.57] | 3.35 | [2.06,5.40] | 1.72 | [0.88,3.33] | 554 | 72.76 | [68.78,76.41] | 24.49 | [21.00,28.35] | 2.75 | [1.64,4.57] | 554 | 95.85 | [93.77,97.25] | 3.07 | [1.90,4.92] | 1.08 | [0.47,2.49] | |||||
| Southwest | 559 | 97.27 | [95.16,98.47] | 1.96 | [0.97,3.95] | 0.77 | [0.28,2.09] | 559 | 79.31 | [75.42,82.73] | 18.33 | [15.06,22.14] | 2.36 | [1.42,3.90] | 559 | 92.67 | [90.07,94.63] | 4.5 | [3.00,6.71] | 2.82 | [1.71,4.63] | |||||
| West | 552 | 89.74 | [86.65,92.19] | 8.07 | [5.90,10.94] | 2.19 | [1.22,3.91] | 552 | 75.69 | [71.78,79.21] | 20.93 | [17.60,24.70] | 3.38 | [2.20,5.17] | 550 | 91.61 | [88.85,93.73] | 6.21 | [4.38,8.75] | 2.18 | [1.26,3.73] | |||||
| North | 550 | 98.26 | [96.44,99.16] | 1.6 | [0.74,3.43] | 0.14 | [0.02,0.96] | 551 | 86.68 | [83.44,89.36] | 11.81 | [9.30,14.90] | 1.51 | [0.72,3.14] | 550 | 97.52 | [95.88,98.52] | 2.21 | [1.27,3.80] | 0.27 | [0.07,1.08] | |||||
| Central High Land | 556 | 94.88 | [92.62,96.48] | 4.42 | [2.95,6.57] | 0.7 | [0.26,1.88] | 556 | 80.15 | [76.44,83.40] | 19.14 | [15.93,22.82] | 0.71 | [0.29,1.72] | 556 | 91.29 | [88.81,93.25] | 8.19 | [6.28,10.61] | 0.53 | [0.19,1.42] | |||||
| Northeast | 555 | 93.4 | [90.76,95.32] | 6.2 | [4.34,8.79] | 0.4 | [0.10,1.61] | 555 | 77.05 | [73.17,80.51] | 20.65 | [17.33,24.41] | 2.31 | [1.32,4.00] | 555 | 89.31 | [86.35,91.69] | 10.5 | [8.15,13.47] | 0.17 | [0.02,1.19] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| Economic Status (self-reporting) | ||||||||||||||||||||||||||
| Poor | 1701 | 93.7 | [92.30,94.87] | 4.8 | [3.78,6.07] | 1.5 | [0.99,2.26] | 0.021 | 1700 | 75.05 | [72.81,77.17] | 21.52 | [19.52,23.66] | 3.43 | [2.63,4.44] | < 0.001 | 1701 | 93.06 | [91.73,94.20] | 5.41 | [4.40,6.63] | 1.53 | [1.06,2.20] | 0.572 | ||
| Middle and Rich | 2657 | 95.76 | [94.83,96.54] | 3.33 | [2.65,4.18] | 0.9 | [0.58,1.40] | 2659 | 80.03 | [78.36,81.60] | 18.38 | [16.86,20.00] | 1.60 | [1.18,2.16] | 2655 | 93.35 | [92.34,94.24] | 5.49 | [4.68,6.43] | 1.16 | [0.83,1.62] | |||||
| Total | 4358 | 94.99 | [94.23,95.66] | 3.88 | [3.29,4.57] | 1.13 | [0.83,1.52] | 4359 | 78.16 | [76.83,79.44] | 19.56 | [18.33,20.84] | 2.28 | [1.87,2.78] | 4356 | 93.25 | [92.45,93.96] | 5.46 | [4.81,6.19] | 1.3 | [1.01,1.66] | |||||
Table 2.
Prevalence of moderate and high risk scores for any substance use, tobacco use, and sedative use by traumatic events in the Afghan general population
| Variables/Characteristics | Any substance use | Tobacco Use | Sedative Use | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | No | Moderate | High | P-value | n | No | Moderate | High | P-value | n | No | Moderate | High | P-value | ||||||||||||
| % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | % row | 95% CI | |||||||||
| Collective Violence (Total) | ||||||||||||||||||||||||||
| No | 1778 | 97.9 | [96.97,98.55] | 1.97 | [1.34,2.88] | 0.13 | [0.03,0.60] | < 0.001 | 1779 | 87.56 | [85.83,89.10] | 11.43 | [9.95,13.11] | 1.01 | [0.64,1.59] | < 0.001 | 1777 | 94.74 | [93.58,95.70] | 4.66 | [3.75,5.78] | 0.60 | [0.35,1.02] | < 0.001 | ||
| Yes | 2627 | 93.13 | [92.00,94.10] | 5.17 | [4.32,6.18] | 1.7 | [1.25,2.32] | 2627 | 72.13 | [70.28,73.90] | 24.75 | [23.05,26.54] | 3.12 | [2.51,3.88] | 2626 | 92.31 | [91.22,93.27] | 5.97 | [5.12,6.95] | 1.72 | [1.30,2.27] | |||||
| Total | 4405 | 95 | [94.24,95.66] | 3.92 | [3.33,4.60] | 1.09 | [0.80,1.47] | 4406 | 78.18 | [76.86,79.45] | 19.53 | [18.31,20.80] | 2.29 | [1.88,2.79] | 4403 | 93.26 | [92.48,93.97] | 5.46 | [4.81,6.18] | 1.28 | [1.00,1.64] | |||||
| Collective Violence (Experienced) | ||||||||||||||||||||||||||
| No | 3199 | 96.98 | [96.25,97.57] | 2.59 | [2.04,3.28] | 0.44 | [0.25,0.76] | < 0.001 | 3200 | 82.75 | [81.31,84.09] | 15.60 | [14.30,16.99] | 1.65 | [1.26,2.16] | < 0.001 | 3198 | 94.27 | [93.42,95.02] | 4.92 | [4.21,5.73] | 0.81 | [0.57,1.14] | < 0.001 | ||
| Yes | 1193 | 89.74 | [87.70,91.48] | 7.45 | [5.97,9.27] | 2.8 | [1.95,4.02] | 1193 | 66.20 | [63.33,68.97] | 29.80 | [27.14,32.60] | 4.00 | [2.99,5.32] | 1192 | 90.53 | [88.68,92.10] | 6.93 | [5.58,8.58] | 2.54 | [1.79,3.59] | |||||
| Total | 4392 | 94.98 | [94.22,95.65] | 3.93 | [3.34,4.62] | 1.09 | [0.80,1.48] | 4393 | 78.19 | [76.86,79.45] | 19.51 | [18.30,20.79] | 2.30 | [1.89,2.80] | 4390 | 93.24 | [92.45,93.95] | 5.47 | [4.83,6.20] | 1.29 | [1.00,1.65] | |||||
| Collective Violence (Witnessed) | ||||||||||||||||||||||||||
| No | 2048 | 97.19 | [96.25,97.90] | 2.47 | [1.80,3.37] | 0.34 | [0.16,0.74] | < 0.001 | 2049 | 85.72 | [84.03,87.25] | 13.07 | [11.59,14.71] | 1.21 | [0.82,1.78] | < 0.001 | 2047 | 94.18 | [93.06,95.13] | 4.99 | [4.10,6.05] | 0.83 | [0.54,1.29] | 0.019 | ||
| Yes | 2352 | 93.2 | [92.01,94.22] | 5.11 | [4.22,6.16] | 1.69 | [1.22,2.36] | 2352 | 72.01 | [70.06,73.89] | 24.81 | [23.01,26.69] | 3.18 | [2.53,3.99] | 2351 | 92.49 | [91.36,93.49] | 5.85 | [4.97,6.89] | 1.65 | [1.23,2.22] | |||||
| Total | 4400 | 94.99 | [94.23,95.66] | 3.92 | [3.33,4.61] | 1.09 | [0.80,1.47] | 4401 | 78.17 | [76.85,79.44] | 19.53 | [18.32,20.81] | 2.30 | [1.88,2.79] | 4398 | 93.25 | [92.47,93.96] | 5.46 | [4.82,6.19] | 1.28 | [1.00,1.64] | |||||
| Caused/Witnessed Harm (Total) | ||||||||||||||||||||||||||
| No | 3785 | 95.45 | [94.66,96.13] | 3.7 | [3.09,4.42] | 0.85 | [0.58,1.24] | < 0.001 | 3786 | 79.77 | [78.38,81.08] | 18.22 | [16.95,19.56] | 2.02 | [1.60,2.53] | < 0.001 | 3783 | 93.42 | [92.57,94.17] | 5.57 | [4.87,6.36] | 1.01 | [0.75,1.38] | < 0.001 | ||
| Yes | 614 | 91.89 | [89.12,94.00] | 5.32 | [3.62,7.78] | 2.79 | [1.69,4.57] | 614 | 68.39 | [64.32,72.19] | 27.35 | [23.71,31.33] | 4.26 | [2.93,6.15] | 614 | 92.28 | [89.91,94.13] | 4.75 | [3.28,6.83] | 2.97 | [1.97,4.46] | |||||
| Total | 4399 | 94.96 | [94.19,95.62] | 3.93 | [3.34,4.62] | 1.12 | [0.83,1.51] | 4400 | 78.18 | [76.86,79.45] | 19.49 | [18.28,20.77] | 2.33 | [1.91,2.83] | 4397 | 93.26 | [92.47,93.97] | 5.45 | [4.81,6.18] | 1.29 | [1.00,1.65] | |||||
| Caused/Witnessed Harm (Experienced) | ||||||||||||||||||||||||||
| No | 4371 | 95.2 | [94.46,95.86] | 3.76 | [3.18,4.44] | 1.04 | [0.76,1.42] | < 0.001 | 4372 | 78.54 | [77.22,79.80] | 19.16 | [17.95,20.43] | 2.30 | [1.89,2.80] | < 0.001 | 4369 | 93.29 | [92.51,94.00] | 5.46 | [4.82,6.19] | 1.24 | [0.96,1.60] | 0.054 | ||
| Yes | 38 | 70.24 | [53.23,83.04] | 21.25 | [10.70,37.81] | 8.51 | [2.68,23.91] | 38 | 43.95 | [28.61,60.55] | 51.86 | [35.66,67.68] | 4.19 | [1.04,15.42] | 38 | 91.82 | [79.31,97.05] | 2.85 | [0.40,17.67] | 5.32 | [1.66,15.81] | |||||
| Total | 4409 | 94.95 | [94.19,95.62] | 3.94 | [3.35,4.62] | 1.11 | [0.82,1.51] | 4410 | 78.18 | [76.86,79.45] | 19.49 | [18.28,20.77] | 2.32 | [1.91,2.82] | 4407 | 93.28 | [92.49,93.99] | 5.44 | [4.80,6.16] | 1.28 | [1.00,1.64] | |||||
| Caused/Witnessed Harm (Witnessed) | ||||||||||||||||||||||||||
| No | 3806 | 95.28 | [94.48,95.97] | 3.84 | [3.22,4.57] | 0.89 | [0.61,1.28] | 0.003 | 3807 | 79.56 | [78.17,80.88] | 18.41 | [17.14,19.75] | 2.03 | [1.61,2.55] | < 0.001 | 3804 | 93.45 | [92.60,94.20] | 5.53 | [4.84,6.32] | 1.02 | [0.75,1.39] | < 0.001 | ||
| Yes | 593 | 92.86 | [90.18,94.86] | 4.52 | [2.93,6.89] | 2.62 | [1.56,4.35] | 593 | 69.24 | [65.12,73.08] | 26.48 | [22.81,30.51] | 4.27 | [2.92,6.22] | 593 | 92.06 | [89.60,93.98] | 4.95 | [3.42,7.11] | 3.00 | [1.97,4.54] | |||||
| Total | 4399 | 94.96 | [94.19,95.62] | 3.93 | [3.34,4.62] | 1.12 | [0.83,1.51] | 4400 | 78.18 | [76.86,79.45] | 19.49 | [18.28,20.77] | 2.33 | [1.91,2.83] | 4397 | 93.26 | [92.47,93.97] | 5.45 | [4.81,6.18] | 1.29 | [1.00,1.65] | |||||
| Inter-personal Violence (Total) | ||||||||||||||||||||||||||
| No | 2583 | 96.35 | [95.46,97.07] | 3.24 | [2.56,4.08] | 0.42 | [0.22,0.79] | < 0.001 | 2584 | 82.89 | [81.30,84.37] | 15.75 | [14.32,17.29] | 1.36 | [0.97,1.90] | < 0.001 | 2582 | 93.83 | [92.82,94.70] | 5.47 | [4.64,6.43] | 0.71 | [0.45,1.10] | < 0.001 | ||
| Yes | 1821 | 93.18 | [91.79,94.34] | 4.82 | [3.84,6.03] | 2.01 | [1.42,2.83] | 1821 | 71.88 | [69.65,74.02] | 24.57 | [22.53,26.73] | 3.55 | [2.78,4.51] | 1820 | 92.57 | [91.27,93.68] | 5.37 | [4.41,6.53] | 2.06 | [1.53,2.77] | |||||
| Total | 4404 | 94.99 | [94.23,95.66] | 3.91 | [3.32,4.60] | 1.09 | [0.81,1.48] | 4405 | 78.19 | [76.87,79.46] | 19.51 | [18.30,20.79] | 2.29 | [1.88,2.79] | 4402 | 93.29 | [92.50,93.99] | 5.43 | [4.79,6.15] | 1.28 | [1.00,1.64] | |||||
| Inter-personal Violence (Experienced) | ||||||||||||||||||||||||||
| No | 3327 | 96.26 | [95.49,96.91] | 3.12 | [2.53,3.84] | 0.61 | [0.38,0.99] | < 0.001 | 3328 | 81.52 | [80.09,82.87] | 16.78 | [15.49,18.17] | 1.70 | [1.31,2.20] | < 0.001 | 3326 | 94.01 | [93.14,94.77] | 4.96 | [4.27,5.76] | 1.03 | [0.75,1.42] | 0.002 | ||
| Yes | 1077 | 91.19 | [89.14,92.88] | 6.27 | [4.84,8.10] | 2.54 | [1.71,3.75] | 1077 | 68.21 | [65.17,71.11] | 27.7 | [24.92,30.66] | 4.09 | [3.03,5.50] | 1076 | 91.13 | [89.26,92.71] | 6.82 | [5.43,8.54] | 2.04 | [1.38,3.02] | |||||
| Total | 4404 | 94.99 | [94.23,95.66] | 3.91 | [3.32,4.60] | 1.09 | [0.81,1.48] | 4405 | 78.19 | [76.87,79.46] | 19.51 | [18.30,20.79] | 2.29 | [1.88,2.79] | 4402 | 93.29 | [92.50,93.99] | 5.43 | [4.79,6.15] | 1.28 | [1.00,1.64] | |||||
| Inter-personal Violence (Witnessed) | ||||||||||||||||||||||||||
| No | 3012 | 95.55 | [94.65,96.31] | 3.76 | [3.07,4.60] | 0.68 | [0.43,1.10] | 0.002 | 3013 | 81.08 | [79.55,82.53] | 17.2 | [15.81,18.69] | 1.71 | [1.30,2.26] | < 0.001 | 3011 | 93.6 | [92.66,94.43] | 5.48 | [4.71,6.37] | 0.92 | [0.65,1.30] | 0.009 | ||
| Yes | 1392 | 93.86 | [92.35,95.09] | 4.21 | [3.21,5.52] | 1.93 | [1.29,2.87] | 1392 | 72.32 | [69.78,74.72] | 24.21 | [21.91,26.66] | 3.47 | [2.62,4.58] | 1391 | 92.65 | [91.15,93.91] | 5.33 | [4.25,6.66] | 2.02 | [1.42,2.86] | |||||
| Total | 4404 | 94.99 | [94.23,95.66] | 3.91 | [3.32,4.60] | 1.09 | [0.81,1.48] | 4405 | 78.19 | [76.87,79.46] | 19.51 | [18.30,20.79] | 2.29 | [1.88,2.79] | 4402 | 93.29 | [92.50,93.99] | 5.43 | [4.79,6.15] | 1.28 | [1.00,1.64] | |||||
| Sexual Violence (Total) | ||||||||||||||||||||||||||
| No | 4153 | 95.17 | [94.40,95.84] | 3.81 | [3.21,4.51] | 1.03 | [0.74,1.42] | 0.013 | 4154 | 78.67 | [77.32,79.96] | 19.17 | [17.93,20.47] | 2.17 | [1.75,2.67] | < 0.001 | 4152 | 93.55 | [92.74,94.26] | 5.3 | [4.64,6.04] | 1.16 | [0.88,1.52] | < 0.001 | ||
| Yes | 204 | 91.61 | [85.81,95.17] | 4.76 | [2.21,9.94] | 3.63 | [1.58,8.12] | 204 | 69.22 | [61.87,75.70] | 24.43 | [18.46,31.58] | 6.35 | [3.62,10.92] | 203 | 87.12 | [82.10,90.89] | 8.13 | [5.22,12.46] | 4.75 | [2.68,8.26] | |||||
| Total | 4357 | 95.03 | [94.26,95.69] | 3.85 | [3.26,4.53] | 1.13 | [0.83,1.53] | 4358 | 78.29 | [76.96,79.56] | 19.38 | [18.16,20.66] | 2.33 | [1.91,2.84] | 4355 | 93.29 | [92.50,94.00] | 5.41 | [4.77,6.14] | 1.30 | [1.02,1.66] | |||||
| Sexual Violence (Experienced) | ||||||||||||||||||||||||||
| No | 4259 | 95.01 | [94.24,95.69] | 3.87 | [3.28,4.57] | 1.12 | [0.82,1.52] | 0.770 | 4260 | 78.33 | [76.99,79.61] | 19.38 | [18.15,20.67] | 2.30 | [1.88,2.81] | 0.492 | 4258 | 93.45 | [92.66,94.16] | 5.30 | [4.66,6.03] | 1.25 | [0.96,1.61] | < 0.001 | ||
| Yes | 98 | 95.8 | [87.22,98.71] | 2.48 | [0.56,10.23] | 1.72 | [0.24,11.15] | 98 | 76.2 | [65.97,84.10] | 19.49 | [12.41,29.28] | 4.3 | [1.48,11.88] | 97 | 84.03 | [75.74,89.87] | 11.5 | [6.72,19.11] | 4.43 | [1.83,10.33] | |||||
| Total | 4357 | 95.03 | [94.26,95.69] | 3.85 | [3.26,4.53] | 1.13 | [0.83,1.53] | 4358 | 78.29 | [76.96,79.56] | 19.38 | [18.16,20.66] | 2.33 | [1.91,2.84] | 4355 | 93.29 | [92.50,94.00] | 5.41 | [4.77,6.14] | 1.30 | [1.02,1.66] | |||||
| Sexual Violence (Witnessed) | ||||||||||||||||||||||||||
| No | 4227 | 95.23 | [94.47,95.89] | 3.76 | [3.17,4.45] | 1.01 | [0.73,1.40] | < 0.001 | 4228 | 78.68 | [77.35,79.96] | 19.12 | [17.89,20.41] | 2.20 | [1.79,2.70] | < 0.001 | 4226 | 93.43 | [92.63,94.15] | 5.38 | [4.73,6.12] | 1.19 | [0.91,1.55] | < 0.001 | ||
| Yes | 129 | 87.54 | [79.35,92.78] | 7.07 | [3.30,14.49] | 5.39 | [2.36,11.87] | 129 | 63.9 | [54.44,72.39] | 28.93 | [20.99,38.40] | 7.18 | [3.80,13.14] | 128 | 88.18 | [81.86,92.50] | 6.45 | [3.41,11.86] | 5.38 | [2.77,10.16] | |||||
| Total | 4356 | 95.02 | [94.26,95.69] | 3.85 | [3.26,4.53] | 1.13 | [0.84,1.53] | 4357 | 78.29 | [76.96,79.56] | 19.38 | [18.16,20.66] | 2.33 | [1.92,2.84] | 4354 | 93.29 | [92.50,94.00] | 5.41 | [4.77,6.14] | 1.30 | [1.02,1.66] | |||||
| Accidental Injury (Total) | ||||||||||||||||||||||||||
| No | 965 | 98.44 | [97.28,99.11] | 1.32 | [0.72,2.43] | 0.24 | [0.06,0.97] | < 0.001 | 966 | 84.55 | [81.98,86.81] | 14.26 | [12.07,16.76] | 1.19 | [0.68,2.09] | < 0.001 | 964 | 95.71 | [94.28,96.79] | 3.77 | [2.75,5.15] | 0.52 | [0.25,1.10] | 0.001 | ||
| Yes | 3444 | 94.04 | [93.11,94.85] | 4.62 | [3.90,5.46] | 1.34 | [0.99,1.83] | 3444 | 76.43 | [74.90,77.90] | 20.95 | [19.54,22.43] | 2.62 | [2.12,3.22] | 3443 | 92.69 | [91.76,93.52] | 5.83 | [5.08,6.68] | 1.48 | [1.14,1.92] | |||||
| Total | 4409 | 94.95 | [94.19,95.62] | 3.93 | [3.34,4.62] | 1.11 | [0.82,1.51] | 4410 | 78.12 | [76.80,79.39] | 19.56 | [18.34,20.83] | 2.32 | [1.91,2.82] | 4407 | 93.31 | [92.53,94.02] | 5.40 | [4.76,6.12] | 1.28 | [1.00,1.64] | |||||
| Accidental Injury (Experienced) | ||||||||||||||||||||||||||
| No | 2198 | 96.99 | [96.09,97.69] | 2.39 | [1.78,3.22] | 0.61 | [0.34,1.09] | < 0.001 | 2199 | 81.05 | [79.24,82.74] | 17.4 | [15.76,19.16] | 1.55 | [1.12,2.15] | < 0.001 | 2197 | 94.78 | [93.77,95.63] | 4.45 | [3.66,5.40] | 0.78 | [0.50,1.20] | < 0.001 | ||
| Yes | 2192 | 92.94 | [91.67,94.03] | 5.45 | [4.50,6.60] | 1.61 | [1.13,2.29] | 2192 | 75.23 | [73.28,77.09] | 21.69 | [19.92,23.56] | 3.08 | [2.42,3.92] | 2191 | 91.87 | [90.64,92.96] | 6.34 | [5.38,7.47] | 1.78 | [1.32,2.40] | |||||
| Total | 4390 | 94.93 | [94.16,95.60] | 3.95 | [3.36,4.64] | 1.12 | [0.83,1.51] | 4391 | 78.09 | [76.76,79.36] | 19.58 | [18.36,20.86] | 2.33 | [1.92,2.83] | 4388 | 93.3 | [92.51,94.01] | 5.41 | [4.77,6.14] | 1.29 | [1.01,1.65] | |||||
| Accidental Injury (Witnessed) | ||||||||||||||||||||||||||
| No | 1417 | 97.87 | [96.86,98.57] | 1.64 | [1.05,2.55] | 0.49 | [0.21,1.13] | < 0.001 | 1418 | 84.59 | [82.50,86.46] | 13.91 | [12.12,15.92] | 1.50 | [0.97,2.33] | < 0.001 | 1416 | 94.85 | [93.59,95.87] | 4.25 | [3.32,5.41] | 0.91 | [0.54,1.52] | 0.019 | ||
| Yes | 2984 | 93.65 | [92.62,94.54] | 4.96 | [4.17,5.89] | 1.39 | [1.01,1.92] | 2984 | 75.2 | [73.53,76.81] | 22.11 | [20.57,23.73] | 2.69 | [2.16,3.34] | 2983 | 92.66 | [91.66,93.55] | 5.88 | [5.08,6.81] | 1.45 | [1.10,1.92] | |||||
| Total | 4401 | 94.94 | [94.18,95.61] | 3.94 | [3.35,4.63] | 1.12 | [0.83,1.51] | 4402 | 78.08 | [76.75,79.35] | 19.60 | [18.38,20.88] | 2.32 | [1.91,2.83] | 4399 | 93.33 | [92.55,94.04] | 5.38 | [4.74,6.10] | 1.28 | [1.00,1.64] | |||||
| Witness of Accidental Death | ||||||||||||||||||||||||||
| No | 3677 | 95.9 | [95.13,96.55] | 3.31 | [2.73,4.01] | 0.79 | [0.53,1.18] | < 0.001 | 3678 | 80.29 | [78.90,81.61] | 17.82 | [16.55,19.17] | 1.89 | [1.48,2.41] | < 0.001 | 3675 | 93.23 | [92.37,94.01] | 5.59 | [4.88,6.39] | 1.18 | [0.89,1.56] | 0.207 | ||
| Yes | 732 | 90.33 | [87.73,92.43] | 6.99 | [5.20,9.33] | 2.68 | [1.69,4.23] | 732 | 67.84 | [64.14,71.33] | 27.95 | [24.59,31.57] | 4.21 | [3.00,5.87] | 732 | 93.71 | [91.68,95.27] | 4.51 | [3.19,6.33] | 1.79 | [1.06,2.99] | |||||
| Total | 4409 | 94.95 | [94.19,95.62] | 3.93 | [3.34,4.62] | 1.11 | [0.82,1.50] | 4410 | 78.18 | [76.86,79.44] | 19.54 | [18.33,20.82] | 2.28 | [1.87,2.78] | 4407 | 93.31 | [92.53,94.02] | 5.4 | [4.76,6.13] | 1.28 | [1.00,1.64] | |||||
| Any traumatic Event | ||||||||||||||||||||||||||
| No | 644 | 99.07 | [97.69,99.63] | 0.93 | [0.37,2.31] | 0 | < 0.001 | 645 | 91.76 | [89.23,93.74] | 7.70 | [5.78,10.19] | 0.54 | [0.20,1.44] | < 0.001 | 643 | 97.68 | [96.19,98.60] | 1.99 | [1.14,3.44] | 0.33 | [0.11,1.03] | < 0.001 | |||
| Yes | 3757 | 94.31 | [93.44,95.07] | 4.43 | [3.75,5.21] | 1.26 | [0.93,1.71] | 3757 | 75.98 | [74.51,77.40] | 21.44 | [20.08,22.86] | 2.58 | [2.11,3.15] | 3756 | 92.6 | [91.71,93.40] | 5.97 | [5.24,6.78] | 1.44 | [1.12,1.85] | |||||
| Total | 4401 | 94.97 | [94.21,95.64] | 3.94 | [3.35,4.63] | 1.09 | [0.80,1.47] | 4402 | 78.17 | [76.85,79.44] | 19.53 | [18.32,20.81] | 2.30 | [1.89,2.79] | 4399 | 93.3 | [92.52,94.01] | 5.42 | [4.77,6.14] | 1.29 | [1.00,1.64] | |||||
| Total traumatic Event (experienced) | ||||||||||||||||||||||||||
| No | 1582 | 97.89 | [96.93,98.55] | 1.85 | [1.23,2.77] | 0.26 | [0.10,0.70] | < 0.001 | 1583 | 85.5 | [83.57,87.23] | 13.21 | [11.54,15.08] | 1.29 | [0.84,2.00] | < 0.001 | 1581 | 95.21 | [94.04,96.16] | 4.1 | [3.22,5.22] | 0.69 | [0.40,1.18] | < 0.001 | ||
| Yes | 2774 | 93.37 | [92.28,94.32] | 5.07 | [4.24,6.05] | 1.56 | [1.13,2.14] | 2774 | 74.22 | [72.46,75.91] | 22.93 | [21.31,24.63] | 2.85 | [2.28,3.55] | 2773 | 92.28 | [91.22,93.22] | 6.09 | [5.24,7.05] | 1.63 | [1.24,2.15] | |||||
| Total | 4356 | 94.97 | [94.20,95.64] | 3.93 | [3.34,4.63] | 1.1 | [0.81,1.49] | 4357 | 78.21 | [76.88,79.48] | 19.49 | [18.27,20.78] | 2.3 | [1.89,2.80] | 4354 | 93.32 | [92.53,94.03] | 5.39 | [4.74,6.11] | 1.3 | [1.01,1.66] | |||||
| Total traumatic Event (witnessed) | ||||||||||||||||||||||||||
| No | 1007 | 97.98 | [96.79,98.74] | 1.77 | [1.06,2.93] | 0.25 | [0.08,0.80] | < 0.001 | 1008 | 88.59 | [86.34,90.51] | 10.63 | [8.76,12.84] | 0.78 | [0.40,1.51] | < 0.001 | 1006 | 96.15 | [94.74,97.20] | 3.14 | [2.21,4.45] | 0.71 | [0.33,1.49] | < 0.001 | ||
| Yes | 3369 | 94.11 | [93.17,94.92] | 4.57 | [3.85,5.41] | 1.32 | [0.97,1.81] | 3369 | 75.22 | [73.65,76.73] | 22.05 | [20.60,23.57] | 2.73 | [2.22,3.35] | 3368 | 92.51 | [91.57,93.35] | 6.04 | [5.27,6.90] | 1.45 | [1.12,1.89] | |||||
| Total | 4376 | 94.94 | [94.17,95.61] | 3.97 | [3.37,4.66] | 1.09 | [0.81,1.48] | 4377 | 78.1 | [76.78,79.37] | 19.59 | [18.37,20.87] | 2.31 | [1.90,2.81] | 4374 | 93.29 | [92.51,94.00] | 5.41 | [4.77,6.14] | 1.29 | [1.01,1.65] | |||||
| Exposure to traumatic events | ||||||||||||||||||||||||||
| No | 668 | 98.9 | [97.51,99.52] | 0.89 | [0.36,2.22] | 0.2 | [0.03,1.42] | < 0.001 | 669 | 91.31 | [88.75,93.33] | 7.98 | [6.04,10.47] | 0.72 | [0.29,1.75] | < 0.001 | 667 | 97.43 | [95.89,98.40] | 2.25 | [1.34,3.76] | 0.32 | [0.10,0.99] | < 0.001 | ||
| 1 to 3 events | 1658 | 97.12 | [96.07,97.89] | 2.73 | [1.98,3.77] | 0.15 | [0.05,0.47] | 1658 | 82.55 | [80.55,84.39] | 16.02 | [14.24,17.97] | 1.43 | [0.97,2.11] | 1658 | 93.26 | [91.96,94.36] | 6 | [4.96,7.23] | 0.74 | [0.43,1.28] | |||||
| 4 or more events | 2099 | 92.18 | [90.84,93.34] | 5.71 | [4.72,6.90] | 2.11 | [1.54,2.88] | 2099 | 71 | [68.91,73.01] | 25.55 | [23.62,27.58] | 3.45 | [2.73,4.35] | 2098 | 92.09 | [90.84,93.19] | 5.94 | [4.98,7.08] | 1.96 | [1.48,2.61] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| PTSD | ||||||||||||||||||||||||||
| No | 4157 | 95.48 | [94.73,96.13] | 3.61 | [3.03,4.29] | 0.91 | [0.64,1.29] | < 0.001 | 4157 | 78.66 | [77.32,79.95] | 19.1 | [17.87,20.40] | 2.23 | [1.82,2.74] | 0.004 | 4155 | 93.87 | [93.09,94.56] | 5.2 | [4.56,5.92] | 0.94 | [0.69,1.26] | < 0.001 | ||
| Yes | 268 | 85.84 | [80.45,89.92] | 9.5 | [6.18,14.35] | 4.66 | [2.54,8.40] | 269 | 69.65 | [63.36,75.28] | 26.65 | [21.25,32.86] | 3.70 | [2.01,6.69] | 268 | 82.97 | [77.64,87.23] | 9.65 | [6.41,14.28] | 7.38 | [4.77,11.25] | |||||
| Total | 4425 | 94.97 | [94.21,95.63] | 3.92 | [3.33,4.61] | 1.11 | [0.82,1.50] | 4426 | 78.18 | [76.86,79.45] | 19.51 | [18.29,20.78] | 2.31 | [1.90,2.81] | 4423 | 93.29 | [92.51,93.99] | 5.43 | [4.79,6.16] | 1.28 | [1.00,1.63] | |||||
| Depression | ||||||||||||||||||||||||||
| No | 3817 | 95.8 | [95.05,96.45] | 3.32 | [2.75,4.00] | 0.88 | [0.61,1.26] | < 0.001 | 3817 | 79.30 | [77.91,80.63] | 18.69 | [17.41,20.05] | 2.00 | [1.60,2.51] | < 0.001 | 3815 | 94.48 | [93.70,95.17] | 4.74 | [4.10,5.48] | 0.78 | [0.56,1.09] | < 0.001 | ||
| Yes | 542 | 89.4 | [86.06,92.02] | 7.62 | [5.41,10.64] | 2.98 | [1.73,5.07] | 543 | 70.25 | [66.01,74.18] | 24.84 | [21.19,28.88] | 4.91 | [3.29,7.28] | 542 | 84.68 | [81.30,87.55] | 10.5 | [8.07,13.44] | 4.87 | [3.35,7.02] | |||||
| Total | 4359 | 95.05 | [94.29,95.72] | 3.82 | [3.24,4.50] | 1.13 | [0.83,1.52] | 4360 | 78.24 | [76.91,79.51] | 19.42 | [18.20,20.69] | 2.34 | [1.93,2.85] | 4357 | 93.33 | [92.55,94.04] | 5.41 | [4.76,6.13] | 1.26 | [0.98,1.61] | |||||
| Generalized Anxiety | ||||||||||||||||||||||||||
| No | 4252 | 95.2 | [94.44,95.86] | 3.78 | [3.19,4.47] | 1.02 | [0.74,1.40] | 0.002 | 4253 | 78.47 | [77.13,79.75] | 19.34 | [18.10,20.63] | 2.19 | [1.78,2.69] | 0.007 | 4251 | 93.94 | [93.18,94.62] | 4.96 | [4.34,5.67] | 1.1 | [0.84,1.44] | < 0.001 | ||
| Yes | 160 | 88.79 | [81.87,93.28] | 7.44 | [3.91,13.71] | 3.78 | [1.53,8.99] | 160 | 69.35 | [61.30,76.38] | 25.34 | [18.85,33.15] | 5.31 | [2.67,10.27] | 159 | 74.03 | [66.27,80.53] | 19.5 | [13.79,26.78] | 6.48 | [3.51,11.68] | |||||
| Total | 4412 | 94.98 | [94.22,95.65] | 3.9 | [3.32,4.59] | 1.11 | [0.82,1.50] | 4413 | 78.16 | [76.84,79.43] | 19.54 | [18.32,20.81] | 2.30 | [1.89,2.80] | 4410 | 93.27 | [92.48,93.98] | 5.45 | [4.81,6.17] | 1.28 | [1.00,1.64] | |||||
Any substance use
In logistic regression (Table 3), women had lower moderate (RR = 0.32; 95% CI = 0.18, 0.58) and high risk (RR = 0.05; 95% CI = 0.01, 0.18) of any substance use compared to the men. Individual who lived in south region had lower risk of moderate use of any substance use compared to those who lived in central regions of the country (RR = 0.23; 95% CI = 0.09, 0.61). Furthermore, people who reported their socio-economic status as middle and rich had lower risk of moderate use of any substance use compared to those who reported their socio-economic status as poor (RR = 0.66; 95% CI = 0.45, 0.96).
Table 3.
Multinomial logistic regression of risk of substance use disorders by socio-demographic characteristics
| Variables | Any substance use | Tobacco Use | Sedative Use | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderate Risk | High Risk | Moderate Risk | High Risk | Moderate Risk | High Risk | |||||||||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | |||||||||||||||||||||||||||||
| RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | |||||||||||
| Sex | ||||||||||||||||||||||||||||||||||
| Male | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Female | 0.32 | 0.18 | 0.58 | < 0.001 | 0.05 | 0.01 | 0.18 | < 0.001 | 0.10 | 0.08 | 0.14 | < 0.001 | 0.20 | 0.10 | 0.41 | < 0.001 | 2.22 | 1.51 | 3.28 | < 0.001 | 2.12 | 0.88 | 5.13 | 0.095 | ||||||||||
| Education | ||||||||||||||||||||||||||||||||||
| No Education | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Less than Primary and Primary | 1.62 | 0.96 | 2.76 | 0.073 | 0.92 | 0.38 | 2.24 | 0.862 | 1.06 | 0.77 | 1.45 | 0.737 | 1.26 | 0.65 | 2.44 | 0.490 | 0.96 | 0.55 | 1.67 | 0.872 | 0.76 | 0.22 | 2.60 | 0.660 | ||||||||||
| Secondary and High School | 0.96 | 0.56 | 1.66 | 0.891 | 0.32 | 0.10 | 1.01 | 0.052 | 0.79 | 0.60 | 1.05 | 0.103 | 0.72 | 0.35 | 1.47 | 0.370 | 0.98 | 0.62 | 1.55 | 0.931 | 1.33 | 0.56 | 3.18 | 0.521 | ||||||||||
| University and other | 1.23 | 0.62 | 2.44 | 0.550 | 0.00 | 0.00 | 0.00 | 0.000 | 0.73 | 0.51 | 1.05 | 0.090 | 0.12 | 0.02 | 0.94 | 0.044 | 1.27 | 0.75 | 2.14 | 0.371 | 0.69 | 0.16 | 2.93 | 0.612 | ||||||||||
| Occupation | ||||||||||||||||||||||||||||||||||
| Service/Salaried/Business/Trading | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Labor | 1.15 | 0.61 | 2.16 | 0.673 | 2.16 | 0.60 | 7.79 | 0.242 | 1.07 | 0.77 | 1.50 | 0.682 | 1.41 | 0.64 | 3.08 | 0.390 | 0.92 | 0.50 | 1.67 | 0.778 | 0.98 | 0.29 | 3.33 | 0.971 | ||||||||||
| Agriculture/Rearing Animals | 0.81 | 0.42 | 1.54 | 0.518 | 1.04 | 0.30 | 3.58 | 0.952 | 0.89 | 0.64 | 1.24 | 0.481 | 1.13 | 0.51 | 2.47 | 0.765 | 0.74 | 0.41 | 1.36 | 0.338 | 1.01 | 0.29 | 3.58 | 0.984 | ||||||||||
| No Source of Income | 0.91 | 0.46 | 1.77 | 0.770 | 3.68 | 0.84 | 16.18 | 0.084 | 1.30 | 0.91 | 1.85 | 0.156 | 1.65 | 0.69 | 3.98 | 0.264 | 0.85 | 0.51 | 1.44 | 0.555 | 1.21 | 0.43 | 3.38 | 0.713 | ||||||||||
| Other | 1.21 | 0.55 | 2.66 | 0.635 | 1.61 | 0.31 | 8.24 | 0.567 | 0.82 | 0.54 | 1.26 | 0.377 | 0.88 | 0.28 | 2.81 | 0.831 | 0.70 | 0.34 | 1.46 | 0.342 | 1.46 | 0.36 | 5.90 | 0.597 | ||||||||||
| Age | ||||||||||||||||||||||||||||||||||
| 15–24 Yrs | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| 25–34 Yrs | 1.34 | 0.70 | 2.54 | 0.373 | 2.47 | 0.75 | 8.15 | 0.136 | 1.85 | 1.31 | 2.61 | < 0.001 | 2.44 | 0.92 | 6.43 | 0.072 | 1.16 | 0.72 | 1.87 | 0.545 | 8.02 | 2.92 | 22.00 | < 0.001 | ||||||||||
| 35–44 Yrs | 1.18 | 0.58 | 2.38 | 0.653 | 2.27 | 0.65 | 7.95 | 0.200 | 2.15 | 1.49 | 3.10 | < 0.001 | 2.79 | 1.02 | 7.63 | 0.046 | 2.08 | 1.26 | 3.45 | 0.004 | 13.64 | 4.46 | 41.67 | < 0.001 | ||||||||||
| 45–54 Yrs | 1.25 | 0.59 | 2.63 | 0.564 | 0.62 | 0.14 | 2.79 | 0.531 | 1.89 | 1.29 | 2.78 | 0.001 | 2.91 | 1.03 | 8.27 | 0.044 | 1.53 | 0.88 | 2.67 | 0.131 | 10.41 | 3.19 | 33.99 | < 0.001 | ||||||||||
| 55 + Yrs | 0.85 | 0.37 | 1.95 | 0.704 | 0.72 | 0.15 | 3.48 | 0.682 | 2.73 | 1.84 | 4.04 | < 0.001 | 4.04 | 1.37 | 11.91 | 0.011 | 1.80 | 0.98 | 3.30 | 0.056 | 15.17 | 4.78 | 48.16 | < 0.001 | ||||||||||
| Marital Status | ||||||||||||||||||||||||||||||||||
| Never married | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Married | 0.66 | 0.36 | 1.24 | 0.196 | 1.89 | 0.55 | 6.57 | 0.314 | 1.65 | 1.15 | 2.35 | 0.006 | 1.21 | 0.48 | 3.09 | 0.684 | 0.91 | 0.56 | 1.48 | 0.711 | 0.52 | 0.21 | 1.27 | 0.152 | ||||||||||
| Widowed / Divorce or separated | 1.21 | 0.43 | 3.39 | 0.718 | NR | 1.37 | 0.74 | 2.52 | 0.313 | 1.19 | 0.26 | 5.43 | 0.824 | 0.86 | 0.40 | 1.84 | 0.694 | 1.42 | 0.43 | 4.73 | 0.566 | |||||||||||||
| Ethnicity | ||||||||||||||||||||||||||||||||||
| Tajik | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Pashtun | 1.18 | 0.70 | 1.96 | 0.535 | 1.31 | 0.51 | 3.33 | 0.577 | 1.54 | 1.12 | 2.12 | 0.008 | 0.71 | 0.38 | 1.32 | 0.282 | 0.92 | 0.58 | 1.45 | 0.714 | 1.06 | 0.48 | 2.34 | 0.893 | ||||||||||
| Hazara | 0.57 | 0.19 | 1.67 | 0.305 | NR | 1.07 | 0.65 | 1.75 | 0.787 | 0.93 | 0.28 | 3.13 | 0.906 | 0.75 | 0.41 | 1.37 | 0.346 | 0.39 | 0.07 | 2.25 | 0.290 | |||||||||||||
| Uzbek | 0.90 | 0.41 | 1.97 | 0.801 | 1.77 | 0.14 | 22.04 | 0.659 | 0.92 | 0.59 | 1.44 | 0.723 | 0.70 | 0.22 | 2.29 | 0.557 | 0.60 | 0.32 | 1.12 | 0.110 | NR | |||||||||||||
| Other | 0.77 | 0.27 | 2.20 | 0.623 | 3.00 | 0.43 | 20.89 | 0.266 | 1.24 | 0.78 | 1.97 | 0.367 | 2.47 | 1.00 | 6.12 | 0.051 | 0.62 | 0.29 | 1.35 | 0.231 | NR | |||||||||||||
| Rurality | ||||||||||||||||||||||||||||||||||
| Urban | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Rural | 2.72 | 1.48 | 4.99 | 0.001 | 2.12 | 0.69 | 6.53 | 0.193 | 1.56 | 1.19 | 2.04 | 0.001 | 1.66 | 0.96 | 2.84 | 0.067 | 1.50 | 1.00 | 2.25 | 0.052 | 1.73 | 0.80 | 3.74 | 0.162 | ||||||||||
| Region | ||||||||||||||||||||||||||||||||||
| Central | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| South | 0.23 | 0.09 | 0.61 | 0.003 | 1.18 | 0.27 | 5.11 | 0.827 | 2.35 | 1.47 | 3.76 | < 0.001 | 2.11 | 0.85 | 5.24 | 0.108 | 0.52 | 0.25 | 1.06 | 0.071 | 2.75 | 0.74 | 10.20 | 0.131 | ||||||||||
| East | 0.45 | 0.20 | 1.03 | 0.059 | 0.61 | 0.14 | 2.74 | 0.518 | 1.38 | 0.88 | 2.16 | 0.160 | 1.12 | 0.47 | 2.69 | 0.797 | 0.41 | 0.19 | 0.88 | 0.022 | 1.50 | 0.34 | 6.60 | 0.595 | ||||||||||
| Southwest | 0.39 | 0.14 | 1.07 | 0.068 | 0.55 | 0.12 | 2.59 | 0.45 | 1.45 | 0.90 | 2.32 | 0.127 | 1.30 | 0.52 | 3.21 | 0.576 | 0.70 | 0.36 | 1.37 | 0.298 | 2.43 | 0.67 | 8.88 | 0.178 | ||||||||||
| West | 1.61 | 0.77 | 3.37 | 0.204 | 1.32 | 0.34 | 5.17 | 0.692 | 2.04 | 1.30 | 3.19 | 0.002 | 1.79 | 0.77 | 4.14 | 0.176 | 1.24 | 0.70 | 2.22 | 0.463 | 4.14 | 1.15 | 14.83 | 0.029 | ||||||||||
| North | 0.47 | 0.17 | 1.26 | 0.133 | 0.10 | 0.01 | 1.56 | 0.101 | 0.85 | 0.52 | 1.40 | 0.524 | 0.54 | 0.15 | 1.90 | 0.336 | 0.56 | 0.29 | 1.09 | 0.090 | 1.15 | 0.19 | 7.14 | 0.879 | ||||||||||
| Central High Land | 1.08 | 0.43 | 2.67 | 0.876 | 0.77 | 0.12 | 4.88 | 0.783 | 1.49 | 0.88 | 2.54 | 0.137 | 0.23 | 0.07 | 0.81 | 0.022 | 1.62 | 0.89 | 2.96 | 0.117 | 1.25 | 0.21 | 7.54 | 0.806 | ||||||||||
| Northeast | 1.24 | 0.55 | 2.80 | 0.611 | 0.19 | 0.02 | 1.50 | 0.116 | 1.48 | 0.91 | 2.41 | 0.111 | 0.72 | 0.26 | 1.98 | 0.522 | 2.25 | 1.26 | 4.02 | 0.006 | 0.43 | 0.04 | 4.03 | 0.456 | ||||||||||
| Economic Status (self-reporting) | ||||||||||||||||||||||||||||||||||
| Poor | Ref | Ref | Ref | |||||||||||||||||||||||||||||||
| Middle and Rich | 0.66 | 0.45 | 0.96 | 0.031 | 0.90 | 0.45 | 1.78 | 0.759 | 0.89 | 0.74 | 1.08 | 0.238 | 0.54 | 0.35 | 0.84 | 0.007 | 1.04 | 0.78 | 1.39 | 0.781 | 0.90 | 0.53 | 1.54 | 0.704 | ||||||||||
|
The model is adjusted or controlled for sex, education, occupation, age, marital status, ethnicity, area of residence, region, economic status, and numbers of traumatic events. NR = Not Reliable |
||||||||||||||||||||||||||||||||||
For traumatic events (Table 4), people who experienced of collective violence more likely to have moderate (RR = 1.76; 95% CI = 1.15, 2.72) and high (RR = 3.08; 95% CI = 1.38, 6.84) risk of any substance use compared to those who did not have experience of collective violence. People who experienced caused/witnessed harm had greater moderate risk of (RR = 3.75; 95% CI = 1.41, 9.98) of any substance use comparedto those who did not have experience of cause/witness harm. People who had total and witnessed interpersonal violence had lower risk of moderate use of any substance use comparing to those did not have total and witness of interpersonal violence (RR = 0.64; 95% CI = 0.42, 0.98) and (RR = 0.42; 95% CI = 0.28, 0.64) respectively. People who witnessed of sexual violence had high risk of any addition comparing to those who did not witness of sexual violence (RR = 3.42; 95% CI = 1.18, 9.89). Furthermore, individuals with any traumatic event had more risk of moderate (RR = 4.69; 95% CI = 1.53, 14.38) any addition comparing those who did not have any traumatic events.
Table 4.
Multinomial logistic regression of risk of substance use disorders by traumatic events and psychiatric disorders
| Variables | Any substance use | Tobacco Use | Sedative Use | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Moderate Risk | High Risk | Moderate Risk | High Risk | Moderate Risk | High Risk | ||||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | 95% CI | ||||||||||||||||||||||||
| RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | RRR | LL | UL | P-value | ||||||
| Collective Violence (Total) | 1.25 | 0.65 | 2.4 | 0.501 | 6.74 | 0.91 | 49.9 | 0.062 | 1.25 | 0.95 | 1.65 | 0.118 | 1.35 | 0.65 | 2.79 | 0.417 | 1.22 | 0.79 | 1.88 | 0.362 | 0.91 | 0.36 | 2.30 | 0.838 | |||||
| Collective Violence (Experienced) | 1.76 | 1.15 | 2.72 | 0.010 | 3.08 | 1.38 | 6.84 | 0.006 | 1.29 | 1.04 | 1.60 | 0.022 | 1.52 | 0.98 | 2.35 | 0.064 | 1.44 | 1.01 | 2.06 | 0.045 | 2.27 | 1.20 | 4.30 | 0.012 | |||||
| Collective Violence (Witnessed) | 0.91 | 0.53 | 1.56 | 0.734 | 1.26 | 0.58 | 2.75 | 0.560 | 1.22 | 0.95 | 1.58 | 0.121 | 1.41 | 0.75 | 2.66 | 0.281 | 0.99 | 0.66 | 1.47 | 0.947 | 0.59 | 0.30 | 1.19 | 0.142 | |||||
| Caused/Witnessed Harm (Total) | 0.94 | 0.57 | 1.56 | 0.815 | 1.01 | 0.50 | 2.06 | 0.980 | 0.94 | 0.73 | 1.23 | 0.672 | 1.2 | 0.69 | 2.07 | 0.520 | 0.81 | 0.5 | 1.28 | 0.363 | 1.09 | 0.58 | 2.03 | 0.788 | |||||
| Caused/Witnessed Harm (Experienced) | 3.75 | 1.41 | 9.98 | 0.008 | 3.17 | 0.84 | 11.96 | 0.089 | 2.63 | 1.22 | 5.66 | 0.013 | 1.6 | 0.35 | 7.34 | 0.546 | 0.55 | 0.07 | 4.43 | 0.571 | 2.21 | 0.67 | 7.28 | 0.194 | |||||
| Caused/Witnessed Harm (Witnessed) | 0.74 | 0.43 | 1.28 | 0.278 | 0.86 | 0.42 | 1.77 | 0.678 | 0.87 | 0.66 | 1.14 | 0.312 | 1.15 | 0.66 | 2.01 | 0.619 | 0.85 | 0.54 | 1.36 | 0.508 | 1.08 | 0.58 | 2.03 | 0.808 | |||||
| Inter-personal Violence (Total) | 0.64 | 0.42 | 0.98 | 0.038 | 1.22 | 0.51 | 2.92 | 0.661 | 0.94 | 0.75 | 1.19 | 0.630 | 1.81 | 1.07 | 3.06 | 0.026 | 0.69 | 0.50 | 0.96 | 0.029 | 1.60 | 0.89 | 2.89 | 0.119 | |||||
| Inter-personal Violence (Experienced) | 1.20 | 0.80 | 1.80 | 0.390 | 1.64 | 0.80 | 3.34 | 0.178 | 1.50 | 1.19 | 1.88 | < 0.001 | 2.04 | 1.26 | 3.28 | 0.004 | 1.04 | 0.74 | 1.47 | 0.820 | 1.25 | 0.70 | 2.23 | 0.448 | |||||
| Inter-personal Violence (Witnessed) | 0.42 | 0.28 | 0.64 | < 0.001 | 1.02 | 0.45 | 2.29 | 0.964 | 0.79 | 0.63 | 0.98 | 0.035 | 1.3 | 0.77 | 2.2 | 0.322 | 0.72 | 0.51 | 1.02 | 0.068 | 1.19 | 0.67 | 2.13 | 0.552 | |||||
| Sexual Violence (Total) | 1.11 | 0.46 | 2.65 | 0.822 | 2.43 | 0.80 | 7.33 | 0.116 | 1.08 | 0.69 | 1.69 | 0.747 | 1.82 | 0.88 | 3.8 | 0.108 | 1.24 | 0.68 | 2.27 | 0.473 | 1.29 | 0.58 | 2.86 | 0.534 | |||||
| Sexual Violence (Experienced) | 0.92 | 0.22 | 3.89 | 0.906 | 0.97 | 0.12 | 7.97 | 0.980 | 1.27 | 0.67 | 2.39 | 0.460 | 1.25 | 0.33 | 4.69 | 0.739 | 1.70 | 0.78 | 3.68 | 0.181 | 0.81 | 0.26 | 2.52 | 0.714 | |||||
| Sexual Violence (Witnessed) | 1.46 | 0.60 | 3.50 | 0.402 | 3.42 | 1.18 | 9.89 | 0.023 | 1.11 | 0.66 | 1.87 | 0.698 | 1.88 | 0.85 | 4.15 | 0.119 | 0.98 | 0.45 | 2.12 | 0.959 | 1.71 | 0.75 | 3.88 | 0.199 | |||||
| Accidental Injury (Total) | 1.69 | 0.61 | 4.7 | 0.311 | 1.38 | 0.17 | 10.97 | 0.760 | 0.52 | 0.37 | 0.73 | < 0.001 | 0.67 | 0.29 | 1.57 | 0.355 | 0.62 | 0.38 | 1.01 | 0.056 | 1.81 | 0.51 | 6.39 | 0.356 | |||||
| Accidental Injury (Experienced) | 1.46 | 0.91 | 2.33 | 0.113 | 1.58 | 0.79 | 3.17 | 0.193 | 0.94 | 0.76 | 1.16 | 0.548 | 1.25 | 0.80 | 1.96 | 0.321 | 1.26 | 0.93 | 1.72 | 0.143 | 1.89 | 1.07 | 3.34 | 0.029 | |||||
| Accidental Injury (Witnessed) | 1.49 | 0.78 | 2.83 | 0.226 | 0.57 | 0.19 | 1.73 | 0.323 | 0.81 | 0.61 | 1.07 | 0.137 | 0.78 | 0.36 | 1.68 | 0.524 | 0.75 | 0.49 | 1.13 | 0.163 | 0.69 | 0.28 | 1.68 | 0.412 | |||||
| Witness of any accidental death | 1.44 | 0.92 | 2.23 | 0.107 | 1.05 | 0.52 | 2.12 | 0.886 | 1.05 | 0.82 | 1.35 | 0.689 | 1.48 | 0.89 | 2.45 | 0.127 | 0.72 | 0.46 | 1.13 | 0.155 | 0.50 | 0.26 | 0.96 | 0.038 | |||||
| Any traumatic event | 4.69 | 1.53 | 14.38 | 0.007 | 6.28 | 3.42 | 11.50 | < 0.001 | 2.43 | 1.69 | 3.48 | < 0.001 | 6.23 | 2.06 | 18.83 | 0.001 | 2.68 | 1.46 | 4.92 | 0.001 | 3.45 | 0.99 | 11.98 | 0.051 | |||||
| Any traumatic event (Experienced) | 1.39 | 0.80 | 2.41 | 0.239 | 1.95 | 0.66 | 5.76 | 0.228 | 1.30 | 1.01 | 1.66 | 0.041 | 1.24 | 0.7 | 2.19 | 0.456 | 1.13 | 0.79 | 1.61 | 0.508 | 1.46 | 0.68 | 3.12 | 0.334 | |||||
| Any traumatic event (Witnessed) | 0.83 | 0.38 | 1.8 | 0.641 | 0.41 | 0.11 | 1.51 | 0.179 | 1.11 | 0.75 | 1.65 | 0.589 | 1.83 | 0.71 | 4.68 | 0.210 | 0.84 | 0.46 | 1.53 | 0.565 | 0.61 | 0.2 | 1.88 | 0.387 | |||||
| PTSD | 2.46 | 1.28 | 4.74 | < 0.001 | 5.06 | 2.01 | 12.74 | < 0.001 | 1.35 | 0.9 | 2.03 | 0.145 | 0.98 | 0.46 | 2.09 | 0.954 | 1.16 | 0.67 | 2.01 | 0.590 | 2.76 | 1.37 | 5.54 | 0.004 | |||||
| Depression | 1.61 | 0.92 | 2.81 | 0.093 | 1.57 | 0.69 | 3.58 | 0.283 | 1.32 | 0.99 | 1.76 | 0.061 | 2.09 | 1.19 | 3.65 | 0.010 | 2.03 | 1.37 | 3.01 | < 0.001 | 2.54 | 1.38 | 4.69 | 0.003 | |||||
| Generalized Anxiety | 1.19 | 0.54 | 2.65 | 0.666 | 2.21 | 0.66 | 7.44 | 0.201 | 1.22 | 0.75 | 2.00 | 0.423 | 1.74 | 0.73 | 4.15 | 0.213 | 3.19 | 1.81 | 5.62 | < 0.001 | 2.97 | 1.40 | 6.27 | 0.004 | |||||
| Number of traumatic events | |||||||||||||||||||||||||||||
| None | Ref. | ||||||||||||||||||||||||||||
| 1 to 3 events | 3.43 | 1.11 | 10.6 | 0.033 | 0.6 | 0.06 | 6.15 | 0.667 | 2.07 | 1.45 | 2.96 | < 0.001 | 2.25 | 0.82 | 6.18 | 0.115 | 2.28 | 1.29 | 4.02 | 0.004 | 1.95 | 0.53 | 7.21 | 0.316 | |||||
| 4 or more events | 4.93 | 1.6 | 15.2 | 0.006 | 4.19 | 0.56 | 31.2 | 0.162 | 2.35 | 1.65 | 3.34 | < 0.001 | 4.75 | 1.74 | 13 | 0.002 | 2.34 | 1.31 | 4.17 | 0.004 | 3.49 | 1 | 12.1 | 0.050 | |||||
The model is adjusted or controlled for sex, education, occupation, age, marital status, ethnicity, area of residence, region, economic status, numbers of traumatic events, PTSD, Depression, and generalized anxiety disorders
People with PTSD more likely to have moderate (RR = 2.46; 95% CI = 1.28, 4.74) and high risk (RR = 5.06; 95% CI = 2.01, 12.74) of any substance use comparing those who did not have PTSD.
Tobacco use
In the total sample, 19.51% (95% CI; 18.29, 20.78) and 2.31% (95% CI; 1.90, 2.81) of respondent had moderate and high risk of tobacco use (Fig. 1).
Based on logistic regression results, women compared to men were less likely to have moderate (RR = 0.10; 95% CI = 0.08, 0.14) and high (RR = 0.20; 95% CI = 0.10, 0.41) tobacco use. However, the study did not find any risk reduction for various categories of education; only individuals who had university or other type of education had less likely the high risk of using tobacco (RR = 0.12; 95%CI = 0.02, 0.94). Age was associated with tobacco use (see Table 3), as was marital status, ethnicity, and region. People who reported themselves as middle or rich socioeconomic class less likely had the high risk of tobacco use (RR = 0.54; 95%CI = 0.35, 0.84). (Table 3)
Table 4 shows that people who had total interpersonal violence had high risk of tobacco dependence (RR = 1.81; 95%CI = 1.07, 3.06), and moderate risk increases were documented for specific violent exposures including collective violence (RR = 1.29; 95%CI = 1.04, 1.60) and experiencing cause/witnessed harm (RR = 2.63; 95%CI = 1.22, 5.66). In addition, people who have experienced of interpersonal violence were more likely to have moderate (RR = 1.50; 95%CI = 1.19, 1.88) and high (RR = 2.04; 95%CI = 1.26, 3.28) risk of tobacco use compared to those who did not experienced it. Furthermore, people who witnessed for interpersonal violence had lower moderate risk of tobacco use comparing those who did not witness it (RR = 0.79; 95%CI = 0.63, 0.98). Individuals who had total accidental injury were less likely to have a moderate risk of tobacco use compared to those who did not have total accidental injury (RR = 0.52; 95%CI = 0.37, 0.73). Moreover, it was found that people with any traumatic event were more likely to have moderate (RR = 2.43; 95%CI = 1.69, 3.48) and high (RR = 6.23; 95%CI = 2.06, 18.83) risk of tobacco use compared to those who did not have any traumatic events. In addition, people who experienced of any traumatic event were more likely to have moderate risk of tobacco use compared to those who did not experience any traumatic event (RR = 1.30; 95%CI = 1.01, 1.66).
Finally, people with depression were more likely to have high risk of tobacco use compared to those who did not have depression. (RR = 2.09% CI = 1.19, 3.65). (Table 3)
Sedative use
In the total sample, 5.43% (95% CI; 4.79, 6.16) and 1.28% (95% CI; 1.00, 1.63) of respondent had moderate and high risk of sedative use (Fig. 1).
Women more likely to have moderate risk of sedative use compared to men (RR = 2.22; 95%CI = 1.51, 3.28), and risk generally increased with age. In addition, people who resided in East (RR = 0.41; 95%CI = 0.19, 0.88) were less likely to have moderate risk of sedative use while people who resided in North East (RR = 2.25; 95%CI = 1.26, 4.02) and West (RR = 4.14; 95%CI = 1.15, 14.83) regions were more likely to have moderate and high risk of sedative use respectively compared to people who resided in the Central region.
People who experienced the collective violence were more likely to have moderate (RR = 1.44; 95%CI = 1.01, 2.06) and high (RR = 2.27; 95%CI = 1.20, 4.30) risk of sedative use compared to those who did not experience collective violence. People who had total interpersonal violence were less likely to have sedative use compared to those who did not have it (RR = 0.69; 95%CI = 0.50, 0.96). In addition, it was observed that people who experienced the accidental injury were more likely to have high risk of sedative use compared to those who did not experience it (RR = 1.89; 95%CI = 1.07, 3.34). People who witnessed of accidental death were less likely to have high risk of sedative use compared to those who did not witnessed it (RR = 0.50; 95% CI = 0.26, 0.96). Furthermore, people who have any traumatic event were more likely to have moderate risk of sedative use compared to those who did not have any traumatic event (RR = 2.68; 95%CI = 1.46, 4.92).
People who had PTSD were more likely to have high risk of sedative use compared to those who did not have PTSD (RR = 2.76; 95%CI = 1.37, 5.54). In addition, people with depression were more likely to have moderate (RR = 2.03% CI = 1.37, 3.01) and high (RR = 2.54; 95% CI = 1.38, 4.69) risk of sedative use compared to those who did not have depression. Furthermore, individual with generalized anxiety were more likely to have moderate (RR = 3.19; 95% CI = 1.81, 5.62) and high (RR = 2.97; 95% CI = 1.40, 6.27) risk of sedative use compared to those without generalized anxiety. (Table 4)
Discussion
The present study documents that substance use disorder is prevalent in the general population of Afghanistan, with prevalence of any substance use of 5.%. Tobacco use was particularly prevalent in this sample, with moderate to high risk of use of 21.8%, and sedative use prevalence at 6.7%. Risk of dependence was heightened among individuals with exposure to traumatic events and with co-occurring mental health disorders, which were also prevalent in the sample, highlighting the potential public health consequences of continued trauma exposure in the Afghan population. The current study determined that individual with collective violence, having experience of caused/witnessed of harm, sexual violence, having any traumatic events and with PTSD had greater risk of any substance use while people who witness of interpersonal violence found to be in lower risk of any substance use. Further, social determinants of health were correlated with substance use and dependence, with significant differences based on respondents’ sex, various education level, across occupation, ethnicity, residential area, various regions, and economic status.
These results are in line with previous research in other countries, documenting that the number of traumatic events as well as qualitative aspects of specific traumatic experiences can impact the relationship between traumatic experiences and substance abuse [18, 20, 21]. The direction and magnitude of the estimates in our study are comparable to those found in other countries, with traumatic events increasing the risk of substance use and substance related problems in the order of magnitude of approximately 1.5 to 2.5 for most comparisons, yet our results suggest some associations that are stronger in magnitude than other studies, with traumatic event exposure increasing the risk of substance use problems in orders of magnitude upward of 4–6 times the risk. This may be due to the lower overall prevalence of substance use in Afghan general population, thus risk factors such as traumatic event exposure have stronger links to substance use. Further, some unique correlates did emerge in the context of the Afghan population. Specifically, while people experiencing collective violence, experience of sexual violence, accidental injury, any traumatic events, depression, generalized anxiety and PTSD had higher risk of sedative use comparing to their counterparts, people with total interpersonal violence and those who witnessed for any accidental death less like to have risk of sedative use comparing their counterparts. While there is not sufficient literature to provide mechanisms that may underlie these unique patterns of results, it may be given the high level of trauma exposure in Afghanistan, including interpersonal violence, and witnessing death, there may be a range of alternative ways of coping with trauma, such as processing with family and community, and less need to cope with substances such as sedatives. Further research in the context of Afghanistan to understand patterns of trauma coping is an important next step in the research.
Furthermore, consistent with prior studies, we found that in general, traumatic events increased the risk for high-risk substance use more than moderate risk substance use, although sample sizes in our studies for high-risk substance use were often small thus results imprecise. Collective violence, sexual violence, and reports of PTSD were most strongly associated with high-risk substance use in the Afghan population. Specific mechanisms for the role of trauma in substance use has been extensively explored, including use of substances to numb or cope with intrusive thoughts and anxiety around trauma [22, 23], as well as to self-medicate other mental health disorders [24]. Providing mental health treatment and trauma-informed therapy are critically necessary to reduce unregulated substance use, including in settings where access to care can be a challenge including in many areas of Afghanistan. This is especially important as recent increased political conflicts in the region are likely to perpetuate exposures to violence as well as social determinants of health such as economic distress.
Tobacco use remains highly prevalent in Afghanistan, and as a global contributor to disease and mortality, efforts to provide smoking cessation are critical. Moderate and high-risk prevalence of tobacco use was 21.82% in our data, with significant difference across sex, various education levels, different occupations, age groups, marital status, ethnicity, residential area, various regions, socio-economic status, most type of traumatic events, depression, generalized anxiety and PTSD. Tobacco cessation efforts can include relatively cost effective measures such as therapy and behavioral intervention [25], as well as medication and other pharmacological treatment [26]. Expanding access to smoking cessation to rural regions and focusing on high risk groups such as men, those with fewer economic resources, and providing culturally-competent and acceptable interventions by ethnicity may accelerate progress.
Sedative use also remains prevalent in Afghanistan, with prevalence of 6.71%. Use of and dependence to sedatives was higher among women, especially those in young adulthood and older age, and with specific regional and ethnic differences. The increased prevalence among women is unique compared with other substance use which is often more prevalent among men, and may be indicative of cultural norms around use of sedatives for women, increased healthcare access, as well as coping with traumas that may include gender-based violence [27]. Women in Afghanistan are more likely to utilize health care services than men, especially due to conditions such as pregnancy, which might precipitate more evaluation for potential sedative use [28], and worldwide women are more likely than men to be prescribed sedative [29], thus may have higher likelihood for non-medical use based on exposure. Indeed, use of sedatives was correlated with exposure to traumas and psychiatric morbidities that are concentrated among women compared with men, including experience of sexual violence, depression, generalized anxiety and PTSD, suggesting that interventions to treat and improve women’s health throughout Afghanistan, especially in rural regions, may reduce sedative abuse. Given that prolonged and high-dose sedative use are associated with increased risk of injury and overdose death [30, 31], a concentrated public-health approach to gender-specific intervention and care is warranted.
Limitations of the study should be noted. All data are based on self-report, as is common in epidemiological surveys, and substance use was not confirmed with toxicological testing. We anticipate that this may lead to under-reporting, given the stigmatized nature of drug use and potential for social desirability bias as interviews were conducted face-to-face. Further, we selected areas for sampling based on a clustered approach, which was not accounted for in the analysis, thus standard errors may be underestimated, although we do not anticipate that clustering would have a demonstrable impact on results or conclusions. Additionally, we note that we controlled for fixed effects of province in regression models, which provides some adjustment for any area-level correlation. Data were collected in 2017, prior to the increased political unrest in Afghanistan and increased migration of Afghan people in 2021, thus the extent to which results generalize to current prevalence estimates among the population in Afghanistan, as well as those who emigrated, is unknown. Given that increased distress and trauma are associated with increased risk of substance use and disorder, we anticipate that prevalence likely has increased in the population in recent years. Finally, data collection was cross-sectional, thus the directions of associations could not be confirmed. It may be the case that substance use increases exposure to traumatic events; further analysis in longitudinal data are an important next step to validate results.
Finally, our recommendations based on these analyses is increased treatment and other support throughout Afghanistan, which is a challenge given limited resources in some areas. While challenging due to health care infrastructure, brief screening and referral to treatment is possible in low resources settings [32–34], and even brief interventions for substance use problems have demonstrated efficacy. Thus, incorporating substance use assessments into routine care should be considered. In conclusion, substance use and dependence is prevalent in Afghanistan, an area with historical and current exposure to conflict and trauma for a majority of the population [2], and underscores the pervasive impact of trauma exposure on population health in this critically important area. As resources are deployed to assist the Afghan population through a period of high conflict, attention to substance use and psychiatric disorders is needed to fully address population health.
Acknowledgements
We thank the participants who take part in this study and sharing their information. We acknowledge the implementation of this research would not be possible if we did not receive support from the Afghanistan Ministry of Public Health, the Conseil Santé and the Governance institute of Afghanistan. We thank the excellent team of data collectors and provincial team supervisors, the data management office as well as individuals who support IT, administrative, and logistic support to the study. Furthermore, we would also thank the department of epidemiology of Mailman School of Public Health, and LPPS, University of Paris for providing opportunities to further analyze the data and its dissemination.
Author contributions
Ajmal Sabawoon has received the contract service. Has been managing the data collection and management process. Conducted the analysis and draft the manuscript. Has revised the work bringing important intellectual content. Approved the final version. Agreed on accountability of all aspects. Riley M. Nesheim-Case designed plan for the analysis and has been involved in primary data analysis including literature review. Approved the final version. Agreed on accountability of all aspects. Katherine M. Keyes participated to the interpretation of data for the work. Has revised the work bringing important intellectual content. Approved the final version. Agreed on accountability of all aspects. Elie Karam Participated to the interpretation of data for the work. Has revised the work bringing important intellectual content. Approved the final version. Agreed on accountability of all aspects. Viviane Kovess-Masfety has designed the work and conducted the analyses. Has been contracted by Conseil Santé to supervise the work. Has drafted the work. Approved the final version. Agreed on accountability of all aspects.
Funding
This survey was supported by the European Union (EU) (Grant number is EuropeAid/137–728/ DH/SER/AF/).
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the mandatory request of authorizations from the funder and the Afghan ministry of public health but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The project was approved by the Afghanistan Institutional Review Board, National Public Health Institute, Ministry of Public health the 12/31/2016: IRB n° 335541. Informed Consent was provided by all the participants in the study. All methods were performed in accordance with the ethical standards as laid down in the Declaration of Helsinki and its later amendments or comparable ethical standards.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNODC. Drug Situation in Afghanistan: Latest Findings and Emerging Threats. UNODC. 2021. https://www.unodc.org/documents/data-and-analysis/Afghanistan/Afghanistan_brief_Nov_2021.pdf
- 2.Kovess-Masfety V, Keyes K, Karam E, Sabawoon A, Sarwari BA. A National survey on depressive and anxiety disorders in Afghanistan: A highly traumatized population. BMC Psychiatry. 2021;21:314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cottler LB, Ajinkya S, Goldberger BA, Ghani MA, Martin DM, Hu H, et al. Prevalence of drug and alcohol use in urban Afghanistan: epidemiological data from the Afghanistan National urban drug use study (ANUDUS). Lancet Glob Heal. 2014;2:e592–600. [DOI] [PubMed] [Google Scholar]
- 4.Degenhardt L, Bharat C, Glantz MD, Bromet EJ, Alonso J, Bruffaerts R, et al. The associations between traumatic experiences and subsequent onset of a substance use disorder: findings. Drug Alcohol Depend. 2022;240:109574. from the World Health Organization World Mental Health surveys. [DOI] [PubMed] [Google Scholar]
- 5.Levin Y, Bar-Or RL, Forer R, Vaserman M, Kor A, Lev-Ran S. The association between type of trauma, level of exposure and addiction. Addict Behav. 2021;118:106889. [DOI] [PubMed] [Google Scholar]
- 6.Herron JL, Venner KL. A systematic review of trauma and substance use in American Indian and Alaska native individuals: incorporating cultural considerations. J Racial Ethn Heal Disparities. 2023;10:603–32. [DOI] [PMC free article] [PubMed]
- 7.Leza L, Siria S, López-Goñi JJ, Fernandez-Montalvo J. Adverse childhood experiences (ACEs) and substance use disorder (SUD): a scoping review. Drug Alcohol Depend. 2021;221:108563. [DOI] [PubMed] [Google Scholar]
- 8.McCauley JL, Killeen T, Gros DF, Brady KT, Back SE. Posttraumatic stress disorder and co-occurring substance use disorders: advances in assessment and treatment. Clin Psychol Sci Pract. 2012;19:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ehlers CL, Gizer IR, Gilder DA, Yehuda R. Lifetime history of traumatic events in an American Indian community sample: heritability and relation to substance dependence, affective disorder, conduct disorder and PTSD. J Psychiatr Res. 2013;47:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carliner H, Gary D, McLaughlin KA, Keyes KM. Trauma exposure and externalizing disorders in adolescents: results from the National comorbidity survey adolescent supplement. J Am Acad Child Adolesc Psychiatry. 2017;56:755–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carliner H, Keyes KM, McLaughlin KA, Meyers JL, Dunn EC, Martins SS. Childhood trauma and illicit drug use in adolescence: A population-based National comorbidity survey replication–adolescent supplement study. J Am Acad Child Adolesc Psychiatry. 2016;55:701–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, et al. Epidemiology of DSM-5 drug use disorder: results from the National epidemiologic survey on alcohol and related Conditions–III. JAMA Psychiatry. 2016;73:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the world health organization world mental health surveys. Arch Gen Psychiatry. 2009;66:785–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kish L. A procedure for objective respondent selection within the household. J Am Stat Assoc. 1949;44:380–7. [Google Scholar]
- 15.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–98. [DOI] [PubMed] [Google Scholar]
- 16.Weathers F, Blake D, Schnurr P, Kaloupek D, Marx B, Keane T. The Life Events Checklist for DSM-5 (LEC-5). 2013.
- 17.Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, et al. Trauma and PTSD in the WHO world mental health surveys. Eur J Psychotraumatol. 2017;8:1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karam EG, Friedman MJ, Hill ED, Kessler RC, McLaughlin KA, Petukhova M, et al. Cumulative traumas and risk thresholds: 12-month PTSD in the world mental health (WMH) surveys. Depress Anxiety. 2014;31:130–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro MG, Organization WH. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): manual for use in primary care. 2010.
- 20.Brown PJ, Wolfe J. Substance abuse and post-traumatic stress disorder comorbidity. Drug Alcohol Depend. 1994;35:51–9. [DOI] [PubMed] [Google Scholar]
- 21.Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addict Behav. 1998;23:827–40. [DOI] [PubMed] [Google Scholar]
- 22.Haller M, Chassin L. Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol Addict Behav. 2014;28:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark HW, Masson CL, Delucchi KL, Hall SM, Sees KL. Violent traumatic events and drug abuse severity. J Subst Abuse Treat. 2001;20:121–7. [DOI] [PubMed] [Google Scholar]
- 24.Pericot-Valverde I, Elliott RJ, Miller ME, Tidey JW, Gaalema DE. Posttraumatic stress disorder and tobacco use: A systematic review and meta-analysis. Addict Behav. 2018;84:238–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reisinger SA, Kamel S, Seiber E, Klein EG, Paskett ED, Wewers ME. Peer reviewed: Cost-Effectiveness of Community-Based tobacco dependence treatment interventions: initial findings of a systematic review. Prev Chronic Dis. 2019;16. [DOI] [PMC free article] [PubMed]
- 26.Patnode CD, Henderson JT, Coppola EL, Melnikow J, Durbin S, Thomas RG. Interventions for tobacco cessation in adults, including pregnant persons: updated evidence report and systematic review for the US preventive services task force. JAMA. 2021;325:280–98. [DOI] [PubMed] [Google Scholar]
- 27.Zhong S, Yu R, Fazel S. Drug use disorders and violence: associations with individual drug categories. Epidemiol Rev. 2020;42:103–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tawfiq E, Azimi MD, Feroz A, Hadad AS, Soroush MS, Jafari M, et al. Predicting maternal healthcare seeking behaviour in Afghanistan: exploring sociodemographic factors and women’s knowledge of severity of illness. BMC Pregnancy Childbirth. 2023;23:561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van de Boyd A, Pivette M, Ten Have M, Florescu S, O’Neill S, et al. Gender differences in psychotropic use across Europe: results from a large cross-sectional, population-based study. Eur Psychiatry. 2015;30:778–88. [DOI] [PubMed] [Google Scholar]
- 30.Votaw VR, Geyer R, Rieselbach MM, McHugh RK. The epidemiology of benzodiazepine misuse: a systematic review. Drug Alcohol Depend. 2019;200:95–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tardelli VS, Bianco MCM, Prakash R, Segura LE, Castaldelli-Maia JM, Fidalgo TM, et al. Overdose deaths involving non-BZD hypnotic/sedatives in the USA: trends analyses. Lancet Reg Heal. 2022;10:100190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.n der Westhuizen C, Malan M, Naledi T, Roelofse M, Myers B, Stein DJ, et al. Patient outcomes and experience of a task-shared screening and brief intervention service for problem substance use in South African emergency centres: a mixed methods study. Addict Sci Clin Pract. 2021;16:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moberg DP, Paltzer J. Clinical recognition of substance use disorders in medicaid primary care associated with universal screening, brief intervention and referral to treatment (SBIRT). J Stud Alcohol Drugs. 2021;82:700–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mattoo SK, Prasad S, Ghosh A. Brief intervention in substance use disorders. Indian J Psychiatry. 2018;60(Suppl 4):S466. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the mandatory request of authorizations from the funder and the Afghan ministry of public health but are available from the corresponding author on reasonable request.