Abstract
AIM
To reveal the research hotspots, trends, and future prospects of lacrimal duct obstruction disease (LDOD) from 1900 to 2024 through the bibliometric and visualized analysis, providing a directional guidance for research in this field.
METHODS
The Web of Science Core Collection database was used to retrieve relevant literature. Data analysis and visualization were conducted using VOSviewer 1.6.20 and CiteSpace 6.3.1, including annual publication volume, trends, research areas, country/region and institution distribution, journal and co-cited journal analysis, author and co-cited author analysis, keyword and burst keyword analysis, etc.
RESULTS
The study included a total of 1481 articles, revealing an overall upward trend in research on LDOD, with ophthalmology being the predominant field. While the United States previously led research efforts, India and China have emerged as key contributors since 2015. Mohammad Javed Ali stands out as the most influential author in this research area. Ophthalmic Plastic and Reconstructive Surgery has published the highest number of related articles, whereas Ophthalmology has the highest co-citation. The current focal points of research include minimally invasive and precise modifications to dacryocystorhinostomy, along with intubation, new materials for stents, and disease pathogenesis.
CONCLUSION
LDOD research has garnered widely attention and exhibits a steady upward trend. Since 1900, the United States, China, and India have been the leading contributors to this field. Ophthalmologists continue to be the primary driving force behind LDOD research. The findings of this study suggest that at the forefront of LDOD research, our focus has long been on refining and innovating surgical treatment. The minimally invasive and precise modification of lacrimal surgery, represented by dacryocystorhinostomy, is the ongoing developmental direction of this field. Rapid interdisciplinary integration and in-depth exploration of pathogenesis and allergic inflammation will lead to the emergence of new materials, innovative technologies, and safer clinical treatment protocols.
Keywords: lacrimal duct obstruction disease, dacryocystorhinostomy, lacrimal drainage system, tear drainage system, bibliometric analysis
INTRODUCTION
The lacrimal drainage system comprises the lacrimal puncta, lacrimal canaliculi, lacrimal sac, and nasolacrimal duct, responsible for draining tears from the eye to the nasal cavity[1]–[2]. Unobstructed flow through the lacrimal duct is essential for tear drainage to the nasal cavity[3]. Any obstruction or constriction in any part of the tear duct system may lead to tearing symptoms, which are a common manifestation of lacrimal duct obstruction disease (LDOD)[4]. LDOD is a prevalent and frequently-occurring disease in ophthalmology, and approximately 3% of patients seen in ophthalmologic clinics are affected by this condition according to some reports[5]. Obstructive lacrimal drainage system result in inflammation[6], leading to symptoms such as purulent discharge from the eye and ocular irritation[7], significantly impacting patients' physical and mental well-being. Among these situations, one common consequence of nasolacrimal duct obstruction is causing dacryocystitis, which may lead to acute inflammation with redness and pain around the inner canthus of the eye[8] and carries a risk of developing orbital cellulitis, orbital abscess or intracranial infection[9]–[10]. Therefore, restoring patency to the lacrimal drainage system through surgery is crucial for treating LDOD. In response to this challenge, ongoing innovation and development in lacrimal surgery have included dacryocystoplasty[11] and dacryocystorhinostomy[12]. Dacryocystorhinostomy was first proposed by Toti[13] in 1904 and has undergone over a century's worth of development becoming currently considered as an optimal solution for treating dacryocystitis induced by nasolacrimal duct obstruction[14]–[15]. However, due to complexities associated with ocular and nasal structures[16]–[18], implementing dacryocystorhinostomy still presents challenges[19]. In recent years, the advancement of technologies, like endoscopic navigation and laser[20]–[23], has propelled dacryocystorhinostomy towards achieving more precise, effective, and minimally invasive outcomes. Furthermore, the exploration into the pathogenesis of LDOD has provided us with a better understanding of the formation of lacrimal concretion[24]–[25] and the occurrence of nasolacrimal duct obstruction[26].
Utilizing bibliometric analysis enables us to visually depict not only present developments but also emerging themes and prospective direction for investigation within a specific area of study. Bibliometrics has been extensively applied in ophthalmologic and surgical research[27]–[30], steering advancements in associated disciplines while enriching scholars' comprehension regarding their professional landscape. Nevertheless, despite an abundance of studies on LDOD, there remains a dearth in terms of bibliometric scrutiny pertaining to its development tendency as well as contributing nations, prominent authors, key concepts, and citation. What are the primary subjects and future directions in investigations of LDOD? Does dacryocystorhinostomy continue to represent a promising avenue for research? What role does lacrimal stent play in treating LDOD? What is the LDOS's pathogenesis? These inquiries hold critical significance necessitating further exploration. Consequently, we undertook an inaugural bibliometric examination focused on LDOD employing specialized analytical tools with an objective to synthesize prevailing investigative tendencies and pivotal subject matters within this domain. Through meticulous scrutiny, our aspiration is to unveil this field's knowledge framework, identify principal scholarly institutions, authors, and nations, as well as probe prevalent keywords and co-citations, to ultimately aim at furnishing guidance for subsequent lines of research.
MATERIALS AND METHODS
Bibliometrics
Bibliometrics originated in the early 20th century and was established as a distinct discipline in 1969[31]. It is widely employed for literature analysis across various fields[32], offering quantitative methods for examining articles within specific domains[33] and conducting comprehensive performance analysis[34] through detailed bibliometric analysis of author keywords, institutions, and references. Furthermore, with the continuous advancement of computer technology, visualization analysis using modern software can enhance data interpretation, resulting in more comprehensive outcomes[35].
Data Sources and Search
We chose Web of Science Core Collection, a high-quality digital literature resource database widely recognized internationally, as the data source. Clarivate Analytics is considered the most suitable database for bibliometric analysis and has been widely used[36]. We used “TS=[lacrimal AND (obstruction OR obstructive)]” as the search term to search all articles from 1900 to the present, and selected research articles and review articles written in English. The detailed search situation and flow chart are shown in Table 1 and Figure 1.
Table 1. Summary of data source and selection.
| Category | Specific standard requirements |
| Research database | Web of Science Core Collection |
| Citation indexes | Science Citation Index Expanded (SCI-EXPENDED) |
| Searching period | 1900-01-01 to 2024-07-11 |
| Languages | English |
| Searching Keywords | TS=[lacrimal AND (obstruction OR obstructive)] |
| Document types | “Article” or “Review Article” |
| Sample size | 1481 |
Figure 1. Flowchart of research.
Data Analysis and Visual Analysis
The documents retrieved from the Web of Science Core Collection were downloaded in “Plain text file” and “Tab delimited file” formats for data analysis. Subsequently, Research Areas, Times Cited, and Publications Over Time were analyzed using Web of Science's “Analyze Result” and “Citation Report”. The authors, countries or regions, institutions, keywords, and cited references were then analyzed and visualized using VOSviewer 1.6.20 and CiteSpace 6.3.1 for the “Plain text file” format data. Meanwhile, the data in “Tab delimited file” format was imported into the “Bibliometric Online Analysis Platform” (https://bibliometric.com) to analyze annual changes in the number of articles of each country as well as cooperation relationships between countries. Additionally, the data processed by VOSviewer 1.6.20 was analyzed using Scimago Graphica 1.0.43 to generate a visual map of country distribution and country-to-country collaboration. We used Microsoft Excel (Redmond, WA, USA) to create a table that presents the author, country or region, institution, and reference information.
RESULTS
Annual Publications, Trends and Research Areas
A total of 1481 scholarly publications were analyzed; comprising of research articles (n=1394) and review articles (n=87), originating from diverse geographic locations encompassing over 60 countries and 1427 academic institutions. The comprehensive annual publications spanning from 1900 to 2024 for literature pertaining to LDOD is visually depicted in Figure 2A. It reveals a generally upward trend including two different peaks, the minor one in 1970S and 1980s and the major one Since the 1990s which culminates at its zenith around 2020 and subsequently taper off. Concurrently, citations also increased rapidly after 1990, reached its peak in 2020, and finally fell gradually, showing a similar trend with annual publications. Among the literature pertaining to LDOD, a total of 860 articles were categorized under ophthalmology, followed by surgery (n=320) and otorhinolaryngology (n=232; Figure 3).
Figure 2. Trends and countries of issuance.
Figure 3. Top 5 research areas (from Web of Science).

Issuance by Country/Regions and Institutions
The data covers 60 countries/regions, and the annual publication changes of the top 10 countries in the term of total publication number are shown in Figure 2B. The United States occupied the dominant position in the field of LDOD research before 2015, but India and China began to surpass the United States in this term after 2015 and gradually became the main force in LDOD research. The intercountry cooperation is shown in Figure 2C, in which the United States is the country that participates in intercountry cooperation the most, but overall, there is less intercountry cooperation in LDOD. Among the continents, North America, Asia, Europe, and Oceania are active in this research. Figures 4A and 4B show the connections between countries and institutions, with the size of the circles indicating the number of publications, and the thickness of the lines indicating the degree of closeness of the connections between these entities. The United States is the country with the highest total number of publications, primarily focused on the period before the 2010s. However, after the 2010s, Asian countries such as India and China gradually became the main sources of articles. The top 10 countries and institutions in the term of total publication number are listed in Table 2, and L.V. Prasad Eye Institute is the institution with both the highest number of publications and the highest number of citations, and its publications are concentrated in the past decade. Among the 1427 institutions, the top 10 institutions come from 6 countries, with 3 institutions from South Korea, 2 institutions from the United States, and 2 institutions from Australia. In the term of total publication number, the top 10 institutions did not match the top 5 countries (Table 2), which may be related to the fact that China and Turkey have more publications but their institutions are more dispersed.
Figure 4. Visual analysis of the sending country and institution.
Table 2. Top 10 countries and institutions with publications on LDOD.
| Rank | Country | Count (%) | Citation | Institution | Count (%) | Citation |
| 1 | USA | 318 (21.47) | 8169 | L.V. Prasad Eye Institute | 72 (4.86) | 1009 |
| 2 | Turkey | 133 (8.98) | 1889 | The University of Adelaide | 29 (1.96) | 434 |
| 3 | India | 131 (8.85) | 1478 | Royal Adelaide Hospital | 25 (1.69) | 536 |
| 4 | China | 114 (7.70) | 1292 | Korea University | 19 (1.28) | 136 |
| 5 | South Korea | 105 (7.09) | 1429 | Moorfields Eye Hospital | 19 (1.28) | 608 |
| 6 | Japan | 100 (6.75) | 1194 | University of Ulsan | 19 (1.28) | 493 |
| 7 | United Kingdom | 99 (6.68) | 2661 | Tel Aviv University | 15 (1.01) | 128 |
| 8 | Australia | 78 (5.27) | 1729 | Harvard University | 14 (0.95) | 454 |
| 9 | Germany | 59 (3.98) | 833 | University of California-Los Angeles | 14 (0.95) | 468 |
| 10 | Italy | 57 (3.85) | 688 | The Catholic University of Korea | 13 (0.88) | 214 |
Analysis of Journals and Co-cited Journals
By July 11, 2024, a total of 269 journals had published literature related to LDOD. Ophthalmic Plastic and Reconstructive Surgery (n=191, 12.90%) had the highest number of publications, followed by Ophthalmology (n=64, 3.32%), British Journal of Ophthalmology (n=54, 3.65%), American Journal of Ophthalmology (n=53, 3.58%), and Journal of Craniofacial Surgery (n=43, 2.90%). Among the top 15 journals with the most articles related to LDOD, Ophthalmology [impact factor (IF)=13.1] has the highest IF in 2023, followed by American Journal of Ophthalmology (IF=4.1) and British Journal of Ophthalmology (IF=3.7; Table 3), all of which are among the top 5 journals in terms of publication volume. Of these 15 journals, 8 journals (53.33%) are classified as Q2 by the Journal Citation Reports (JCR), and there is not any journal classified as Q4 (Table 3). The total number of publications in Ophthalmic Plastic and Reconstructive Surgery is much higher than that in Ophthalmology, but the citations of the two are similar, which ranks first (n=3160) and second (n=3140) respectively (Table 3). The majority of the top 10 journals by total publication number, including Ophthalmic Plastic and Reconstructive Surgery, primarily published in the 2010s or before (Figure 5A). Some of the journals with lower total publication number, such as International Ophthalmology and Indian Journal of Ophthalmology, primarily published in the past decade (Figure 5A). Among the top 15 co-cited journals for LDOD, Ophthalmology (2689) the most frequently cited, followed by American Journal of Ophthalmology (n=1980) and Ophthalmic Plastic and Reconstructive Surgery (n=1732). Furthermore, among these 15 journals, 10 journals are in Q1, with only Orbit in Q4 (Table 4, Figure 5B).
Table 3. Top 15 journals of publications on LDOD (2023).
| Rank | Journal | Count (%) | Citation | IF | Q (JCR) |
| 1 | Ophthalmic Plastic and Reconstructive Surgery | 191 (12.90) | 3160 | 1.2 | 3 |
| 2 | Ophthalmology | 64 (4.32) | 3140 | 13.1 | 1 |
| 3 | British Journal of Ophthalmology | 54 (3.65) | 1611 | 3.7 | 1 |
| 4 | American Journal of Ophthalmology | 53 (3.58) | 1761 | 4.1 | 1 |
| 5 | Journal of Craniofacial Surgery | 43 (2.90) | 308 | 1.0 | 3 |
| 6 | European Journal of Ophthalmology | 39 (2.63) | 273 | 1.4 | 3 |
| 7 | Eye | 38 (2.57) | 792 | 2.8 | 1 |
| 8 | Graefes Archive for Clinical and Experimental Ophthalmology | 30 (2.03) | 313 | 2.4 | 2 |
| 9 | International Ophthalmology | 29 (1.96) | 72 | 1.4 | 3 |
| 10 | International Journal of Pediatric Otorhinolaryngology | 25 (1.69) | 420 | 1.2 | 3 |
| 11 | Archives of Ophthalmology | 23 (1.55) | 840 | 4.399 (2014)a | 1a |
| 12 | Indian Journal of Ophthalmology | 23 (1.55) | 204 | 2.1 | 2 |
| 13 | Journal of Laryngology and Otology | 22 (1.49) | 281 | 1.1 | 3 |
| 14 | Canadian Journal of Ophthalmology-Journal Canadien D Ophtalmologie | 21 (1.42) | 220 | 3.3 | 1 |
| 15 | European Archives of Oto-Rhino-Laryngology | 21 (1.42) | 242 | 1.9 | 2 |
aThe edition is the latest one showed in Web of Science. IF: Impact factor; JCR: Journal Citation Reports.
Figure 5. Visual analysis of journals and co-cited journals.
Table 4. Top 15 co-cited journals (2023).
| Rank | Journal | Co-citations | IF | Q (JCR) |
| 1 | Ophthalmology | 2689 | 13.1 | 1 |
| 2 | American Journal of Ophthalmology | 1980 | 4.1 | 1 |
| 3 | Ophthalmic Plastic and Reconstructive Surgery | 1732 | 1.2 | 3 |
| 4 | Archives of Ophthalmology | 1546 | 4.399 (2014)a | 1a |
| 5 | British Journal of Ophthalmology | 1358 | 3.7 | 1 |
| 6 | Ophthalmic Surgery Lasers & Imaging | 995 | 1.318 (2013)a | 3a |
| 7 | Ophthalmic Plastic and Reconstructive Surgery | 770 | 1.2 | 3 |
| 8 | Orbit | 760 | 0.9 | 4 |
| 9 | Radiology | 709 | 12.1 | 1 |
| 10 | Laryngoscope | 675 | 2.2 | 1 |
| 11 | Eye | 604 | 2.8 | 1 |
| 12 | Otolaryngology-Head and Neck Surgery | 378 | 2.6 | 1 |
| 13 | Canadian Journal of Ophthalmology-Journal Canadien D Ophtalmologie | 362 | 3.3 | 1 |
| 14 | Journal of AAPOS | 342 | 1.2 | 3 |
| 15 | Investigative Ophthalmology & Visual Science | 340 | 5.0 | 1 |
aThe edition is the latest one showed in Web of Science. IF: Impact factor; JCR: Journal Citation Reports.
Analysis of Authors and Co-cited Authors
Among all authors who have published literature related to LDOD from 1900 to the present, Table 5 lists the top 10 authors by publication volume and co-citation frequency. Mohammad Javed Ali has the highest publication volume (n=65), followed by Selva (n=31) and Baek (n=19). In research of LDOD, the author network with co-citations is shown in Figure 6, where node size is related to the number of articles published, and line thickness is related to the degree of author interaction. The three most co-cited author are Ali, Song, and Hurwitz (Table 5). In addition, we found that Mohammad Javed Ali from India ranked first in both authorship and co-cited authorship, mainly around 2020, indicating that this author is the most active and influential scholar recently in the field of LDOD globally.
Table 5. Ranking of the top 10 authors and co-cited authors.
| Rank | Authors | Count | Co-cited authors | Citations |
| 1 | Ali, MJ | 65 | Ali, MJ | 499 |
| 2 | Selva, D | 31 | Song, HY | 290 |
| 3 | Baek, S | 19 | Hurwitz, JJ | 248 |
| 4 | Song, HY | 16 | Jones, LT | 233 |
| 5 | Kakizaki, H | 15 | Linberg, JV | 228 |
| 6 | Naik, Milind N | 13 | Welham, RAN | 200 |
| 7 | Paulsen, F | 12 | Tsirbas, A | 198 |
| 8 | Singh, S | 12 | Becker, BB | 195 |
| 9 | Takahashi, Y | 12 | Kashkouli, MB | 189 |
| 10 | Trimarchi, M | 12 | Hartikainen, J | 180 |
Figure 6. Visual analysis of authors and co-cited authors.
Analysis of Co-cited References
The co-cited references were visualized by adjusting the size of the nodes and the thickness of the connecting lines (Figure 7A). Table 6 shows the 10 most frequently co-cited references[13],[37]–[45]. The articles we included was in English, but the co-cited references in those papers were not all in English. Therefore, the non-English co-cited references were retained to truly demonstrate the studies making the significant contributions to the field, without contradicting the aforementioned content. Among them, “Primary acquired nasolacrimal duct obstruction—a clinicopathological report and biopsy technique” stands out as the article with the highest citation (n=127).
Figure 7. Visual analysis of co-cited references.
Table 6. Top 10 co-cited references.
| Rank | Title | Citation | Publication year | First author | Journal, IF | Quartile in category |
| 1 | Primary acquired nasolacrimal duct obstruction—a clinicopathological report and biopsy technique | 127 | 1986 | Linberg, JV | Ophthalmology (IF=13.1) | 1 |
| 2 | Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus | 122 | 1990 | Munk, PL | Radiology (IF=12.1) | 1 |
| 3 | External dacryocystorhinostomy—surgical success, patient satisfaction, and economic cost | 114 | 1995 | Tarbet, KJ | Ophthalmology (IF=13.1) | 1 |
| 4 | Endoscopic transnasal dacryocystorhinostomy | 107 | 1989 | Mcdonogh, M | Journal of Laryngology and Otology (IF=1.1) | 3 |
| 5 | Nuovo metodo conservatore di cura radicale delle suppurazioni croncihe del sacco lacrimale (dacriocistorinostomia) | 97 | 1904 | Toti, A | Clinica Moderna (Firenze) (No IF) | None |
| 6 | Endonasal laser dacryocystorhinostomy. A new approach to nasolacrimal duct obstruction | 96 | 1990 | Massaro, BM | Archives of Ophthalmology (IF=4.399, 2014)a | 1a |
| 7 | Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction | 84 | 1987 | Katowitz, JA | Ophthalmology (IF=13.1) | 1 |
| 8 | Management of unsuccessful lacrimal surgery | 79 | 1987 | Welham, RAN | British Journal of Ophthalmology (IF=3.7) | 1 |
| 9 | Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy | 75 | 1998 | Hartikainen, J | Ophthalmology (IF=13.1) | 1 |
| 10 | Dacryocystorhinostomy failure—association with nasolacrimal silicone intubation | 74 | 1989 | Allen, K | Ophthalmic Plastic and Reconstructive Surgery (IF=1.2) | 3 |
aThe edition is the latest one showed in Web of Science. IF: Impact factor.
In addition, we carried out co-citation analysis on the references on the timeline (Figure 7B), and the size of nodes was related to the number of co-citations. A total of 18 clusters are showed, which can be divided into 4 types: surgical technique studies (cluster 0, 1, 2, 5, 6, 7, 12, 14), therapeutic effect studies (cluster 4, 9, 13), etiological pathology studies (clusters 15, 16, 18), and others (cluster 3, 8, 10, 11). Figure 7B shows that surgical technique studies were carried out throughout the entire timeline, but were mainly concentrated before 2005, while treatment effect studies and etiological pathology studies were mainly distributed after 2000. At the same time, we have observed that since the beginning of the 21st century, Major hotspots in the study of lacrimal duct obstructive diseases include “mitomycin C” (cluster 0), “paediatric endoscopic endonasal dacryocystorhinostomy (EnDCR)” (cluster 2), “prospective” comparison (cluster 4), punctal stenosis (cluster 1), systematic review (cluster 3).
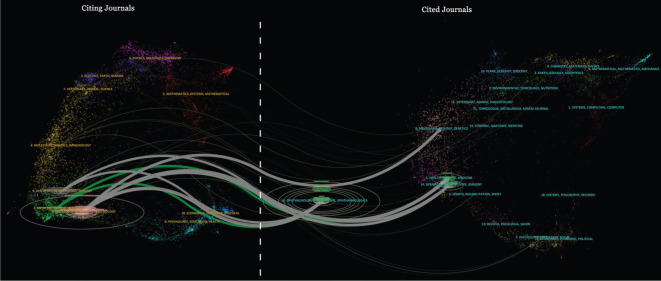
Double-map superposition of journals enables the visualization of topic distribution and orientation within academic journals. On either side of the graph are the citing journals and the cited journals (Figure 8). This curve is the cited curve, which indicates the source of the subject and show the fields advancing the LDOD research. “Dentistry/dermatology/surgery”, “medicine/medical/clinical” and “neurology/sport/ophthalmology” is derived from “ophthalmology/ophthalmic/ophthalmologica”, “health/nursing/medicine” and “dermatology/dentistry/surgery”. In addition, “neurology/sport/ophthalmology” research also from “molecular/biology/genetics”.
Figure 8. Double graph superposition of periodicals.
Analysis of Keywords and Burst Keywords
VOSviewer is used to analyze the frequency of keywords and the strength of their associations, with the aim of revealing the core topics and potential trends in the research field. With the set parameters, the minimum appearance frequency of keywords is 15, and the statistical result shows that a total of 91 keywords have been included. Subsequently, in order to focus on the core concepts more clearly, we increased the threshold for the appearance frequency to 22, at which point, the number of keywords was reduced to 60. The most frequently occurring keywords are dacryocystorhinostomy (n=302), followed by nasolacrimal duct obstruction (n=291), epiphora (n=242), management (n=194), and obstruction (193; Figure 9).
Figure 9. Visual analysis of keyword.

In order to further analyze the research frontier, we use CiteSpace to identify keywords that suddenly appear in the academic literature and quickly attract attention, the so-called “burst keyword”. Of the top 25 cited burst words (Figure 10), The top 3 words for explosive strength were “lacrimal gland and duct” (strength of 14.88), “dacryocystoplasty” (strength of 10.6), and “lacrimal surgery” (strength of 10.08). Breakout words that lasted 10y or more were “dilation” (14y), “outcome” (11y), “dacryocystoplasty” (10y), and “system” (10y). We have paid special attention to keywords that have burst in recent years. These include “outcome” (strength of 8.27), “dry eye” (strength of 5.89), “lacrimal sac” (strength of 5.92), and “silicone tube. Intubation” (strength of 4.19).
Figure 10. Analysis of keyword burst.

DISCUSSION
Basic Information Exploration
We searched and obtained 1481 articles related to LDOD published since 1900, the majority of which were released after 1970, with a significant surge in publication emerging after 1990. The general trend indicates a gradual increase in publication. The lacrimal drainage system, as a structure at the junction of the eye and the nose, has been paid much attention by the academic circles of ophthalmology and otolaryngology. However, through the analysis of research fields, we found that ophthalmology occupies a clear dominant position, with the highest proportion of 58.11%. By analyzing the number and trends of publications by country, we find that the United States is the clear leader in terms of the overall number of publications, with 21.47%. Its number of publications is higher than the combined total of Turkey and India, which are ranked second and third respectively, and its citations are significantly higher than the combined total of other top 5 countries. In terms of timeline and geographical distribution, the United States gradually declined after 2015, while Asian countries represented by India and China gradually became the research center of LDOD. The finding suggests that some Asian countries have progressively surpassed North America and European nations in this particular research domain recently, and are anticipated to emerge as the future frontrunners.
Among the top 10 global publishing institutions, 90% are from developed countries, with only L.V. Prasad Eye Institute coming from a developing country. But L.V. Prasad Eye Institute has the highest number of publications and citations to become the most influential institution globally. This shows that developed countries, represented by the United States, still play a key role in research on LDOD, while developing countries, represented by India, have great potential for development and growing influence. Although Turkey and China are among the top 5 countries in publication, their research institutions are not among the top 10 institutions in publication. Therefore, research institutions in Turkey and China are widely distributed, and their cooperation networks are not tight.
Ali (n=65) published the most articles on LDOD, and is also the author with the highest number of co-citations, indicating that he is the most influential author in the field of LDOD. By July 11, 2024, 269 journals had published 1481 articles related to LDOD. Ophthalmic Plastic and Reconstructive Surgery (12.90%, 3160) has the most related articles and citations, followed by Ophthalmology (4.32%, 3140). Although the former has about three times as many articles as the latter, Ophthalmology has a similar number of citations with the former and the most co-citations. Therefore, researchers can find the most research and potential collaborators in the field in Ophthalmic Plastic and Reconstructive Surgery, while it is easier to learn about high-quality research in this field in Ophthalmology. In addition, among the top 15 journals in publication volume, Journal of Craniofacial Surgery, International Ophthalmology, and Indian Journal of Ophthalmology, have a high frequency of articles on this field in recent years, which can also help researchers understand related progress.
In the analysis of co-cited references, the cited references were categorized into 18 clusters, which can be further classified into four types. It can be seen from the timeline that surgical technique studies have always been the focus of research on LDOD, while the research on therapeutic effects and pathogenesis and physiology has gradually gained importance since the 21st century. By sorting and analyzing the top 10 cited articles, we found that the term “dacryocystorhinostomy” appeared repeatedly in the titles (60%), which is a widely used method for treating nasolacrimal duct obstruction and dacryocystitis, and has always been a subject of interest. To understand the hotpots and scope of academic discussions in the field of LDOD, we used VOSviewer and Citespace to conduct the analysis of keywords and burst keywords on the data we obtained. We found that 60% of the top 5 burst keywords were related to surgical techniques, and that surgery-related words have repeatedly appeared since the 1990s, further indicating that this direction of research has always been a hotpot in the field of LDOD. Meanwhile, “dilation” (14y), “outcome” (11y), and “dacryocystoplasty” (10y) have persisted for 10y or more, which to some extent reflects the need for a longer period of practice and discussion for surgical techniques and scientific efficacy evaluation for tear duct obstructive diseases. The burst keywords “outcome”, “dry eye”, “lacrimal sac”, and “silicone tube intubation” appeared after 2013 and have continued to the present, indicating that scientific evaluation of treatment outcomes, the relationship between LDOD and dry eye, the management of different types of lacrimal sacs and their etiological studies, and the materials and applications of intubation may become hotpots in the future. High-frequency keywords such as “dacryocystorhinostomy”, “nasolacrimal duct obstruction”, “epiphora”, “management”, and “obstruction” suggest that discussions on nasolacrimal duct obstruction and its treatments and efficacy are the focus of research on LDOD, and are also a direction worthy of further exploration and in-depth study in the future.
When focusing on research conducted in the past 20y, a large number of studies on therapeutic effect studies and etiological pathology studies have been cited, particularly in terms of long-term effects, safer treatments, and disease mechanisms, reflecting the future development direction of LDOD research that is becoming increasingly deepened. At the same time, in the burst keywords of the past 20y, the words “endonasal”, “endoscopic”, and “laser” have been closely associated with “dacryocystorhinostomy”, indicating that research on dacryocystorhinostomy is developing towards minimally invasive direction in order to reduce appearance damage and pursue smaller injuries and better outcomes.
Dacryocystorhinostomy
Dacryocystorhinostomy in the modern sense has been proposed for 120y[12], has been tested in many clinical practices, and has been widely recognized as the standard treatment option for nasolacrimal duct obstruction[46]. The surgical approaches include transcutaneous, transnasal and transcanalicular approaches[46], so dacryocystorhinostomy can be divided into transcutaneous external dacryocystorhinostomy (ExDCR) and endoscopic dacryocystorhinostomy[47]. ExDCR is a classic and versatile surgical approach that uses an open approach, which is less restricted by factors such as nasal cavity, fractures, and tumors[48]–[49]. It has a high success rate and is considered the gold standard for surgical treatment of LDOD[50]. It is often designed as a control group in the research of new surgical techniques[46],[51].
Compared with ExDCR, endoscopic dacryocystorhinostomy has the advantage of no facial scar and has attracted wide attention[52]. EnDCR has a good effect on the treatment of LDOD[53]–[54], and a few studies showed superior results than ExDCR[55]. Meanwhile, EnDCR has also achieved significant results in the study of pathological or special lacrimal sacs[56]–[57]. With the development of endoscopic navigation and virtual reality technology, EnDCR has great potential in treating traumatic and congenital nasolacrimal duct obstruction[58]–[60]. Transcanalicular dacryocystorhinostomy requires assistance from an endoscope and a laser device. During the procedure, the optical fiber cable was inserted into the lacrimal sac via the lacrimal canaliculus, and then a passage connecting the lacrimal sac to the nasal cavity was established with assistance from a nasal endoscope. In recent years, many studies have shown that this technology has great potential, but the success rate varies greatly in different studies[61]–[63], indicating that further research is still needed on the factors affecting the success rate. The fibrosis and stenosis of the newly established passage pose significant challenges in the postoperative management of dacryocystorhinostomy. Studies have demonstrated that the application of mitomycin can effectively inhibit the formation of inflammatory granulation and enhance surgical success rates[64]–[65].
Intubation
Intubation is a commonly performed surgical procedure for treating LDOD, involving the insertion of a lacrimal stent into the lacrimal drainage system. It can be utilized independently[66] or in conjunction with other surgical techniques to address obstructions or constrictions at various points within the system, including the lacrimal punctum, lacrimal canaliculi, or nasolacrimal duct. Research on combining intubation with dacryocystoplasty or dacryocystorhinostomy has produced numerous favorable outcomes[11],[66]–[67]. Nevertheless, some studies have indicated that the impact of stents on surgical success rates remains contentious[68]–[69].
In response to various situations in the treatment of LDOD, lacrimal stents have undergone continuous improvement, including the development of mini-Monoka stents[70], Crawford stents[71], and others. Furthermore, the ideal material for tear duct stents should possess biocompatibility, resistance to biofilm formation, and elasticity for self-expansion[72]. Silicone stents are widely used in clinical practice due to their excellent material properties. Additionally, new types of stents composed of polymer materials have demonstrated significant advantages. These include Shape Memory Polymer stent[73] with improved anti-biofilm formation and self-expanding elasticity, as well as more cost-effective polyurethane stents. Moreover, the novel stent with drug-carrying coating can impart anti-inflammatory, antifibrotic, antibacterial, and antithrombotic properties. This has been validated in rabbit experiments showing a reduction in postoperative stenosis of the nasolacrimal duct after intubation[74].
Current Understanding of the Etiopathogenesis of LDOD
Research on the pathogenesis of LDOD is of great significance for treatment and prevention[75]. However, the specific pathogenesis of LDOD is still unknown. Primary acquired nasolacrimal duct obstruction (PANDO) disease is the most prevalent form of LDOD[76], and there is active research into its pathogenesis[26]. Its primary pathological manifestations involve recurrent inflammation and fibrosis of the lacrimal duct, ultimately resulting in dysfunction of the lacrimal drainage system[77]–[78]. Meanwhile, PANDO has a multifaceted etiology, encompassing anatomical constriction, microbial influence, and alterations in tear protein profiles, among other contributing factors[79]–[81]. These elements interact and collectively impact the functionality and health of the nasolacrimal duct. Some researches indicate that prolactin and prolactin receptors may play a significant role in the pathogenesis of PANDO, suggesting that they could serve as crucial targets for further investigation[80],[82]. There is evidence to suggest that PANDO is linked with allergic conjunctivitis, allergic rhinitis, and gastroesophageal reflux disease[83]–[85]. Furthermore, PANDO has also been associated with the administration of radiation therapy and the utilization of specific medications[86]–[91].
Obstruction of lacrimal canaliculi and lacrimal punctum can result from various factors, such as congenital anomalies, infections, tumors, concretion, and medications[92]–[95]. Research shows that the etiology plays a crucial role in surgical management of canalicular obstruction, as different etiological types respond differently to specific surgical interventions[96]. Additionally, genetic research on congenital LDOD has provided new insights for the treatment and prevention of the disease. Zhang et al[97] and Wang et al[98] discovered that mutations in the IGSF3 gene and FGF10 gene are linked to congenital LDOD, while Feng et al[99] observed that mutations in the FGF10 gene can result in obstructive nasolacrimal duct stenosis, indicating a potential significant role of these genes in lacrimal duct development. Furthermore, the ongoing research on tear proteinomics, lacrimal system concretion, and microbiological profiles is continuously advancing the academic community's understanding of the pathogenesis of LDOD[24],[80],[97],[100]–[102].
LDOD and Allergic Inflammation
The lacrimal duct is closely connected with the conjunctiva and nasal mucosa, especially the similarity between the epithelial cells of the lacrimal duct and fornical conjunctiva[103], which indicates a strong correlation between the health of conjunctiva and nasal cavity and the health of the lacrimal drainage system. Especially when allergic inflammation affects the nose or conjunctiva, the incidence and treatment difficulty of LDOD significantly increase[83],[104]. Due to the anatomical relationship, allergic inflammation in the nasal cavity or sinuses can cause swelling, which can block the opening of the nasolacrimal duct, leading to LDOD[105]–[106]. Additionally, several studies have shown that this type of LDOD is predominantly unilateral[105]. The pathological process may start with an allergic inflammation that leads to functional blockage, gradually progressing to fibrosis induced by inflammation, and finally resulting in a complete anatomical obstruction[106]–[107]. Meanwhile, nasal allergic inflammation can affect the effect of lacrimal surgery[108]. When allergic inflammation is not properly managed, the risk of LDOD recurrence increases. However, anti-allergic treatment before and after surgery may improve outcomes[109]. It is worth noting that some of these patients can alleviate the symptom of tearing by receiving anti-allergic treatment only[110], therefore, the timing of surgical treatment needs further discussion. It is evident that the prevention and treatment of LDOD caused by nasal sinusitis is a problem that needs to be solved.
In 1988, there was a report in the article linking allergic conjunctivitis to LDOD[111], and subsequent studies found that many chronic allergic conjunctivitis patients survived stenosis of lacrimal punctum[112]. Recent studies suggest that silicone stent exhibited good performance in for the management of LDOD in patients with allergic conjunctivitis[113]–[114], but unresolved conjunctival inflammation increases the risk of surgical failure or LDOD recurrence. In addition, the available evidence suggests a potential remission of conjunctivitis and epiphora after intubation[115], indicating that the relationship between LDOD and allergic conjunctival disease may be intricate and necessitates further investigation. Nasal or conjunctival inflammation can cause eye symptoms similar to LDOD, such as tears, red eyes, etc., which can easily lead to clinical misdiagnosis[116]. Therefore, it is very important to develop the further research on the relationship between LDOD and allergic inflammation, which is of great significance for clinical diagnosis and treatment.
Possible Future Trends and Directions in Research of LDOD
Upon summarizing and analyzing the aforementioned data, we posit the forthcoming trends and avenues for LDOD research to be as follows: 1) Dacryocystorhinostomy is a significant lacrimal surgery, and the ongoing trend towards minimally invasive and precise enhancements holds significant importance. Consequently, improving the therapeutic efficacy of endoscopic dacryocystorhinostomy and its application in complex cases will remain the primary focus of long-term research. 2) The utilization of intubation and the advancement of novel stents warrant further deliberation. 3) The in-depth investigation into the pathogenesis of LDOD is in its early stages and will continue to advance at the cellular, protein, and genetic levels, particularly in research related to PANDO. 4) From a current clinical perspective, exploring the link between LDOD and allergic inflammation, as well as their impact on diagnosis and treatment, will also be a challenging and highly relevant topic. 5) The integration of medicine and engineering is an emerging trend, with computer science, materials science, tissue engineering, and other disciplines playing the roles in advancing the prevention and treatment of LDOD.
Advantages and Disadvantages
Due to the relatively limited scope of keyword indexing, our research is somewhat constrained in its comprehensiveness. We have exclusively relied on data from the Web of Science platform and focused on English literature exploration. While it's possible that not all relevant studies were included in our specific data source selection, this approach ensures a thorough and professional analysis. Nonetheless, employing bibliometric analysis methods has produced highly reliable results with excellent reproducibility features, offering trustworthy data support and the evidence for the academic community.
In conclusion, at the forefront of LDOD research, our focus has long been on refining and innovating surgical treatment. As a result, the minimally invasive and precise modification of lacrimal surgery, represented by dacryocystorhinostomy, will be the future direction of development in this field. With rapid interdisciplinary integration and in-depth exploration of pathogenesis and allergic inflammation, novel materials, innovative technologies, and new solutions will offer more effective and safe treatment options for clinical practice in the future.
Footnotes
Foundation: Supported by Research Project (No.BLB23C003).
Conflicts of Interest: Chen MH, None; Bai F, None; Tao H, None.
REFERENCES
- 1.Xiao B, Guo DL, Liu R, et al. Obstruction of the tear drainage altered lacrimal gland structure and function. Invest Ophthalmol Vis Sci. 2023;64(10):13. doi: 10.1167/iovs.64.10.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura J, Kamao T, Mitani A, et al. Analysis of lacrimal duct morphology from cone-beam computed tomography dacryocystography in a Japanese population. Clin Ophthalmol. 2022;16:2057–2067. doi: 10.2147/OPTH.S370800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trimarchi M, Vinciguerra A, Resti AG, et al. Multidisciplinary approach to lacrimal system diseases. Acta Otorhinolaryngol Ital. 2021;41(Suppl. 1):S102–S107. doi: 10.14639/0392-100X-suppl.1-41-2021-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhan XY, Guo X, Liu R, et al. Intervention using a novel biodegradable hollow stent containing polylactic acid-polyprolactone-polyethylene glycol complexes against lacrimal duct obstruction disease. PLoS One. 2017;12(6):e0178679. doi: 10.1371/journal.pone.0178679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raslan OA, Ozturk A, Pham N, et al. A comprehensive review of cross-sectional imaging of the nasolacrimal drainage apparatus: what radiologists need to know. Am J Roentgenol. 2019;213(6):1331–1340. doi: 10.2214/AJR.19.21507. [DOI] [PubMed] [Google Scholar]
- 6.Engelsberg K, Sadlon M. First-onset dacryocystitis: characterization, treatment, and prognosis. Ophthalmol Ther. 2022;11(5):1735–1741. doi: 10.1007/s40123-022-00544-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bayuk EG, Malkoç Şen E, Çorak Eroğlu F, et al. Long-term follow-up results of primary canaliculitis patients. Turk J Ophthalmol. 2023;53(3):149–153. doi: 10.4274/tjo.galenos.2022.37659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann J, Lipsett S. Acute dacryocystitis. N Engl J Med. 2018;379(5):474. doi: 10.1056/NEJMicm1713250. [DOI] [PubMed] [Google Scholar]
- 9.Martins MC, Ricardo JR, Akaishi PM, et al. Orbital abscess secondary to acute dacryocystitis: case report. Arq Bras Oftalmol. 2008;71(4):576–578. doi: 10.1590/s0004-27492008000400020. [DOI] [PubMed] [Google Scholar]
- 10.Park MM, Ahmed OM, Ng JD, et al. Simultaneous orbital and intracranial abscesses in 17 cases. Ophthalmic Plast Reconstr Surg. 2021;37(3):212–216. doi: 10.1097/IOP.0000000000001760. [DOI] [PubMed] [Google Scholar]
- 11.Lai CC, Yang CJ, Lin CC, et al. Balloon dacryocystoplasty with pushed monocanalicular intubation as a primary management for primary acquired nasolacrimal duct obstruction. J Pers Med. 2023;13(3):564. doi: 10.3390/jpm13030564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mrittika S, Ali MJ. Lacrimal history–part III: doyens of dacryology series–addeo toti and external dacryocystorhinostomy. Semin Ophthalmol. 2024;39(7):491–492. doi: 10.1080/08820538.2024.2308957. [DOI] [PubMed] [Google Scholar]
- 13.Toti A. Nuovo metodo conservatore dicura radicale delle suppurazione croniche del Sacco lacrimale (Dacriocistorinostomia) Clinica Moderna (Firenze) 1904;10:385–387. [Google Scholar]
- 14.Vinciguerra A, Resti AG, Rampi A, et al. Endoscopic and external dacryocystorhinostomy: a therapeutic proposal for distal acquired lacrimal obstructions. Eur J Ophthalmol. 2023;33(3):1287–1293. doi: 10.1177/11206721221132746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heichel J, Dettmer W, Paulsen F, et al. Transcutaneous (external) dacryocystorhinostomy with reconstruction of the ductus nasolacrimalis. Klin Monbl Augenheilkd. 2024;241(1):30–38. doi: 10.1055/a-2158-5422. [DOI] [PubMed] [Google Scholar]
- 16.Gore SK, Naveed H, Hamilton J, et al. Radiological comparison of the lacrimal sac fossa anatomy between black africans and caucasians. Ophthalmic Plast Reconstr Surg. 2015;31(4):328–331. doi: 10.1097/IOP.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 17.Bedi DG, Salmon A, Winsett MZ, et al. Ruptured uterus: sonographic diagnosis. J Clin Ultrasound. 1986;14(7):529–533. doi: 10.1002/jcu.1870140706. [DOI] [PubMed] [Google Scholar]
- 18.Shams PN, Wormald PJ, Selva D. Anatomical landmarks of the lateral nasal wall: implications for endonasal lacrimal surgery. Curr Opin Ophthalmol. 2015;26(5):408–415. doi: 10.1097/ICU.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 19.Alicandri-Ciufelli M, Lucidi D, Aggazzotti Cavazza E, et al. Classical vs. retrograde endoscopic dacryocystorhinostomy: analyses and comparison of the results. J Clin Med. 2024;13(13):3824. doi: 10.3390/jcm13133824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Güven YZ, Akay F. Primary transcanalicular diode laser-assisted dacryocystorhinostomy: long-term success rates and risk factors for recurrence. Can J Ophthalmol. 2023;58(2):118–124. doi: 10.1016/j.jcjo.2022.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Tokat T, Tokat S, Kusbeci T. Long-term outcomes of transcanalicular laser dacryocystorhinostomy versus endonasal dacryocystorhinostomy and a review of the literature. Niger J Clin Pract. 2023;26(8):1069–1074. doi: 10.4103/njcp.njcp_349_22. [DOI] [PubMed] [Google Scholar]
- 22.Reichel O, Taxeidis M. Use of an image-guided navigation system for routine endonasal endoscopic dacryocystorhinostomy. J Laryngol Otol. 2019;133(8):685–690. doi: 10.1017/S0022215119001567. [DOI] [PubMed] [Google Scholar]
- 23.Chen RX, Liu S, Jiang AX, et al. A simple and efficient technique for suturing and knotting during endoscopic dacryocystorhinostomy. Int Ophthalmol. 2023;43(1):63–71. doi: 10.1007/s10792-022-02388-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stein M, Bethmann D, Viestenz A, et al. Concrements of the lacrimal apparatus. Klin Monbl Augenheilkd. 2023;240(1):44–52. doi: 10.1055/a-1975-0190. [DOI] [PubMed] [Google Scholar]
- 25.Repp DJ, Burkat CN, Lucarelli MJ. Lacrimal excretory system concretions: canalicular and lacrimal sac. Ophthalmology. 2009;116(11):2230–2235. doi: 10.1016/j.ophtha.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 26.Ali MJ. Etiopathogenesis of primary acquired nasolacrimal duct obstruction (PANDO) Prog Retin Eye Res. 2023;96:101193. doi: 10.1016/j.preteyeres.2023.101193. [DOI] [PubMed] [Google Scholar]
- 27.Lin F, Xie MY, Sheng XN, et al. Research trends in the field of retinitis pigmentosa from 2002 to 2021: a 20 years bibliometric analysis. Int Ophthalmol. 2023;43(6):1825–1833. doi: 10.1007/s10792-022-02581-2. [DOI] [PubMed] [Google Scholar]
- 28.Cai YR, Zhou JX, Xu XY, et al. Global trends and prospects in research of artificial cornea over past 20 years: a bibliometric and visualized analysis. Int Ophthalmol. 2023;43(6):2003–2015. doi: 10.1007/s10792-022-02600-2. [DOI] [PubMed] [Google Scholar]
- 29.Yang SJ, Zhang MT, Wei H, et al. Research prospects for kidney xenotransplantation: a bibliometric analysis. Ren Fail. 2024;46(1):2301681. doi: 10.1080/0886022X.2023.2301681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song WP, Wang H, Wang XY. Research hotspots and emerging trends in the treatment of Sjogren's syndrome: a bibliometric analysis from 1900 to 2022. Heliyon. 2024;10(1):e23216. doi: 10.1016/j.heliyon.2023.e23216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pritchard A. Statistical bibliography or bibliometrics. J Doc. 1969;25(4):348–349. [Google Scholar]
- 32.Diem A, Wolter SC. The use of bibliometrics to measure research performance in education sciences. Res High Educ. 2013;54(1):86–114. [Google Scholar]
- 33.Mayr P, Scharnhorst A. Scientometrics and information retrieval: weak-links revitalized. Scientometrics. 2015;102(3):2193–2199. [Google Scholar]
- 34.Abramo G, D'Angelo CA, Viel F. The field-standardized average impact of national research systems compared to world average: the case of Italy. Scientometrics. 2011;88(2):599–615. [Google Scholar]
- 35.van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi: 10.1007/s11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ding X, Yang Z. Knowledge mapping of platform research: a visual analysis using VOSviewer and CiteSpace. Electron Commer Res. 2022;22(3):787–809. [Google Scholar]
- 37.Allen K, Berlin AJ. Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthalmic Surg. 1989;20(7):486–489. [PubMed] [Google Scholar]
- 38.Katowitz JA, Welsh MG. Timing of initial probing and irrigation in congenital nasolacrimal duct obstruction. Ophthalmology. 1987;94(6):698–705. doi: 10.1016/s0161-6420(87)33392-5. [DOI] [PubMed] [Google Scholar]
- 39.Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995;102(7):1065–1070. doi: 10.1016/s0161-6420(95)30910-4. [DOI] [PubMed] [Google Scholar]
- 40.Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986;93(8):1055–1063. doi: 10.1016/s0161-6420(86)33620-0. [DOI] [PubMed] [Google Scholar]
- 41.Welham RA, Wulc AE. Management of unsuccessful lacrimal surgery. Br J Ophthalmol. 1987;71(2):152–157. doi: 10.1136/bjo.71.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Massaro BM, Gonnering RS, Harris GJ. Endonasal laser dacryocystorhinostomy. A new approach to nasolacrimal duct obstruction. Arch Ophthalmol. 1990;108(8):1172–1176. doi: 10.1001/archopht.1990.01070100128048. [DOI] [PubMed] [Google Scholar]
- 43.Munk PL, Lin DT, Morris DC. Epiphora: treatment by means of dacryocystoplasty with balloon dilation of the nasolacrimal drainage apparatus. Radiology. 1990;177(3):687–690. doi: 10.1148/radiology.177.3.2243969. [DOI] [PubMed] [Google Scholar]
- 44.Hartikainen J, Grenman R, Puukka P, et al. Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology. 1998;105(6):1106–1113. doi: 10.1016/S0161-6420(98)96015-8. [DOI] [PubMed] [Google Scholar]
- 45.McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989;103(6):585–587. doi: 10.1017/s0022215100109405. [DOI] [PubMed] [Google Scholar]
- 46.Panda BB, Nayak B, Mohapatra S, et al. Success and complications of endoscopic laser dacryocystorhinostomy vs. external dacryocystorhinostomy: a systematic review and meta-analysis. Indian J Ophthalmol. 2023;71(10):3290–3298. doi: 10.4103/IJO.IJO_3334_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu S, Zhang H, Zhang YR, et al. The efficacy of endoscopic dacryocystorhinostomy in the treatment of dacryocystitis: a systematic review and meta-analysis. Medicine. 2024;103(11):e37312. doi: 10.1097/MD.0000000000037312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ali MJ, Gupta H, Honavar SG, et al. Acquired nasolacrimal duct obstructions secondary to naso-orbito-ethmoidal fractures: patterns and outcomes. Ophthalmic Plast Reconstr Surg. 2012;28(4):242–245. doi: 10.1097/IOP.0b013e31823f3266. [DOI] [PubMed] [Google Scholar]
- 49.Vinciguerra A, Nonis A, Giordano Resti A, et al. Role of anaesthesia in endoscopic and external dacryocystorhinostomy: a meta-analysis of 3282 cases. Eur J Ophthalmol. 2022;32(1):66–74. doi: 10.1177/11206721211035616. [DOI] [PubMed] [Google Scholar]
- 50.Locatello LG, De Zan ER, Tarantini A, et al. External dacryocystorhinostomy: a critical overview of the current evidence. Eur J Ophthalmol. 2025;35(1):12–22. doi: 10.1177/11206721241249214. [DOI] [PubMed] [Google Scholar]
- 51.Taskin U, Yigit O, Sisman A, et al. Comparison of outcomes between endoscopic and external dacryocystorhinostomy with a Griffiths nasal catheter. J Otolaryngol Head Neck Surg. 2011;40(3):216–220. [PubMed] [Google Scholar]
- 52.Yang J, Cao ZW, Gu ZW. Modified endoscopic dacryocystorhinostomy using the middle uncinate process approach. J Craniofac Surg. 2020;31(5):1464–1466. doi: 10.1097/SCS.0000000000006493. [DOI] [PubMed] [Google Scholar]
- 53.Pietris J, Tong JY, Selva D. Primary dacryocystorhinostomy for acute dacryocystitis: a systematic review. Semin Ophthalmol. 2024:1–9. doi: 10.1080/08820538.2024.2344714. [DOI] [PubMed] [Google Scholar]
- 54.Rajabi MT, Shahraki K, Nozare A, et al. External versus endoscopic dacryocystorhinostomy for primary acquired nasolacrimal duct obstruction. Middle East Afr J Ophthalmol. 2022;29(1):1–6. doi: 10.4103/meajo.meajo_238_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ben Simon GJ, Joseph J, Lee S, et al. External versus endoscopic dacryocystorhinostomy for acquired nasolacrimal duct obstruction in a tertiary referral center. Ophthalmology. 2005;112(8):1463–1468. doi: 10.1016/j.ophtha.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 56.Yu B, Mao B, Tu Y, et al. Endoscopic dacryocystorhinostomy with and without bicanalicular silicone tube in patients with a small lacrimal sac: a comparative study. Rhinology. 2024;62(5):623–630. doi: 10.4193/Rhin22.151. [DOI] [PubMed] [Google Scholar]
- 57.Campobasso G, Ragno MS, Monda A, et al. Exclusive or combined endoscopic approach to tumours of the lower lacrimal pathway: review of the literature. Acta Otorhinolaryngol Ital. 2024;44(Suppl. 1):S67–S81. doi: 10.14639/0392-100X-suppl.1-44-2024-N2966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ali MJ, Naik MN. Image-guided dacryolocalization (IGDL) in traumatic secondary acquired lacrimal drainage obstructions (SALDO) Ophthalmic Plast Reconstr Surg. 2015;31(5):406–409. doi: 10.1097/IOP.0000000000000502. [DOI] [PubMed] [Google Scholar]
- 59.Ali MJ, Singh S, Naik MN. Image-guided lacrimal drainage surgery in congenital arhinia-microphthalmia syndrome. Orbit. 2017;36(3):137–143. doi: 10.1080/01676830.2017.1280059. [DOI] [PubMed] [Google Scholar]
- 60.Nowak R, Nowak-Gospodarowicz I, Rękas M, et al. Virtual reality and mixed reality-assisted endoscopic DCR in extremely complex lacrimal obstructions. Laryngoscope. 2024;134(8):3508–3515. doi: 10.1002/lary.31399. [DOI] [PubMed] [Google Scholar]
- 61.Mourya D, Rijal RK. Transcanalicular laser-assisted dacryocystorhinostomy with diode laser. Orbit. 2017;36(6):370–374. doi: 10.1080/01676830.2017.1337189. [DOI] [PubMed] [Google Scholar]
- 62.Drnovsek-Olup B, Beltram M. Transcanalicular diode laser-assisted dacryocystorhinostomy. Indian J Ophthalmol. 2010;58(3):213–217. doi: 10.4103/0301-4738.62646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nowak R, Rekas M, Gospodarowicz IN, et al. Long-term outcomes of primary transcanalicular laser dacryocystorhinostomy. Graefes Arch Clin Exp Ophthalmol. 2021;259(8):2425–2430. doi: 10.1007/s00417-021-05165-5. [DOI] [PubMed] [Google Scholar]
- 64.Kim SY, Chambers CB, Ahn JH. Efficacy of adjuvant mitomycin-C and triamcinolone-impregnated nasal packing for endoscopic dacryocystorhinostomy. Int J Ophthalmol. 2024;17(3):480–484. doi: 10.18240/ijo.2024.03.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nair AG, Ali MJ. Mitomycin-C in dacryocystorhinostomy: from experimentation to implementation and the road ahead: a review. Indian J Ophthalmol. 2015;63(4):335–339. doi: 10.4103/0301-4738.158082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zimmermann JA, Storp JJ, Merté RL, et al. Retrospective analysis of bicanalicular lacrimal silicone tube intubation in patients with congenital nasolacrimal duct obstruction: a long-term follow-up study. Klin Monbl Augenheilkd. 2024;241(12):1328–1334. doi: 10.1055/a-2237-1139. [DOI] [PubMed] [Google Scholar]
- 67.Lai CC, Yang CJ, Lin CC, et al. Surgical outcomes of balloon dacryocystoplasty combined with pushed-type monocanalicular intubation as the primary management for congenital nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 2021;58(6):365–369. doi: 10.3928/01913913-20210414-01. [DOI] [PubMed] [Google Scholar]
- 68.Maldhure SV, Golhar PS, Moon PP. Endonasal dacryocystorhinostomy: results with or without stenting. Cureus. 2023;15(1):e33470. doi: 10.7759/cureus.33470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bahner L, Zebralla V, Dietz A, et al. Prospective, randomised clinical trial on the necessity of using a silicone intubarium in the context of endonasal-endoscopic dacryocystorhinostomy (EN-DCR) in patients with postsaccal lacrimal duct stenosis. Int Ophthalmol. 2024;44(1):293. doi: 10.1007/s10792-024-03205-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Srivatsan S, Mirza M, Imayama I, et al. Use of a nasolacrimal stent to treat air regurgitation after dacryocystorhinostomy in a patient using a continuous positive airway pressure device. J Clin Sleep Med. 2023;19(12):2123–2124. doi: 10.5664/jcsm.10744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lin L, Yang L, Jin XM, et al. Management lacrimal sac abscesses using lacrimal probe and Crawford silicon tube. BMC Ophthalmol. 2016;16(1):211. doi: 10.1186/s12886-016-0378-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wu KY, Fujioka JK, Goodyear E, et al. Polymers and biomaterials for posterior lamella of the eyelid and the lacrimal system. Polymers. 2024;16(3):352. doi: 10.3390/polym16030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park JY, Lee JB, Shin WB, et al. Nasolacrimal stent with shape memory as an advanced alternative to silicone products. Acta Biomater. 2020;101:273–284. doi: 10.1016/j.actbio.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 74.Xiao WZ, Wang BJ, Wang XM, et al. Two-electron oxidized polyphenol chemistry-inspired superhydrophilic drug-carrying coatings for the construction of multifunctional nasolacrimal duct stents. J Mater Chem B. 2024;12(11):2877–2893. doi: 10.1039/d3tb02668j. [DOI] [PubMed] [Google Scholar]
- 75.Ali MJ, Paulsen F. Human lacrimal drainage system reconstruction, recanalization, and regeneration. Curr Eye Res. 2020;45(3):241–252. doi: 10.1080/02713683.2019.1580376. [DOI] [PubMed] [Google Scholar]
- 76.Das AV, Rath S, Naik MN, et al. The incidence of lacrimal drainage disorders across a tertiary eye care network: customization of an indigenously developed electronic medical record system-eyeSmart. Ophthalmic Plast Reconstr Surg. 2019;35(4):354–356. doi: 10.1097/IOP.0000000000001257. [DOI] [PubMed] [Google Scholar]
- 77.Jang JK, Choi SE, Lew H. Liquid-based thin-prep cytology study of lacrimal drainage system in primary acquired nasolacrimal duct obstruction. Graefes Arch Clin Exp Ophthalmol. 2022;260(9):3053–3059. doi: 10.1007/s00417-022-05667-w. [DOI] [PubMed] [Google Scholar]
- 78.Paulsen FP, Thale AB, Maune S, et al. New insights into the pathophysiology of primary acquired dacryostenosis. Ophthalmology. 2001;108(12):2329–2336. doi: 10.1016/s0161-6420(01)00946-0. [DOI] [PubMed] [Google Scholar]
- 79.Prokosch V, Prokosch JE, Promesberger J, et al. Bacterial spectrum and antimicrobial susceptibility patterns in acquired and connatal lacrimal duct stenosis. Curr Eye Res. 2014;39(11):1069–1075. doi: 10.3109/02713683.2014.898312. [DOI] [PubMed] [Google Scholar]
- 80.Wang D, Xiang N, Hu WK, et al. Detection & analysis of inflammatory cytokines in tears of patients with lacrimal duct obstruction. Indian J Med Res. 2021;154(6):888–894. doi: 10.4103/ijmr.IJMR_1435_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zolli CL, Shannon GM. Dacryocystorhinostomy: a review of 119 cases. Ophthalmic Surg. 1982;13(11):905–910. [PubMed] [Google Scholar]
- 82.Mircheff AK, Wang YR, Ding CQ, et al. Potentially pathogenic immune cells and networks in apparently healthy lacrimal glands. Ocul Surf. 2015;13(1):47–81. doi: 10.1016/j.jtos.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nemet AY, Vinker S. Associated morbidity of nasolacrimal duct obstruction—a large community based case-control study. Graefes Arch Clin Exp Ophthalmol. 2014;252(1):125–130. doi: 10.1007/s00417-013-2484-3. [DOI] [PubMed] [Google Scholar]
- 84.Rim TH, Ko J, Kim SS, et al. Lacrimal drainage obstruction and gastroesophageal reflux disease: a nationwide longitudinal cohort study. J Clin Gastroenterol. 2019;53(4):277–283. doi: 10.1097/MCG.0000000000001005. [DOI] [PubMed] [Google Scholar]
- 85.Mayo-Yáñez M, Viña-Vázquez S, Lechien JR, et al. Involvement of laryngopharyngeal reflux in ocular diseases: a state-of-the-art review. J Voice. 2023;37(4):586–597. doi: 10.1016/j.jvoice.2021.03.010. [DOI] [PubMed] [Google Scholar]
- 86.Zhou XY, Zhang XY, Zhou DM, et al. A narrative review of ocular surface disease related to anti-glaucomatous medications. Ophthalmol Ther. 2022;11(5):1681–1704. doi: 10.1007/s40123-022-00557-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seider N, Miller B, Beiran I. Topical glaucoma therapy as a risk factor for nasolacrimal duct obstruction. Am J Ophthalmol. 2008;145(1):120–123. doi: 10.1016/j.ajo.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 88.Ortiz-Basso T, Galmarini A, Vigo RL, et al. The relationship between topical anti-glaucoma medications and the development of lacrimal drainage system obstruction. Arq Bras Oftalmol. 2018;81(6):490–493. doi: 10.5935/0004-2749.20180095. [DOI] [PubMed] [Google Scholar]
- 89.Kim N, Kim JW, Baek JH, et al. S-1-induced lacrimal drainage obstruction and its association with ingredients/metabolites of S-1 in tears and plasma: a prospective multi-institutional study. Cancer Res Treat. 2018;50(1):30–39. doi: 10.4143/crt.2016.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kubo N, Kubota Y, Kawamura H, et al. Dosimetric parameters predictive of nasolacrimal duct obstruction after carbon-ion radiotherapy for head and neck carcinoma. Radiother Oncol. 2019;141:72–77. doi: 10.1016/j.radonc.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 91.Bothra N, Lin LY, Yoon MK. Radiation-induced acquired lacrimal drainage obstructions: management and outcomes. Semin Ophthalmol. 2025;40(1):30–34. doi: 10.1080/08820538.2024.2376620. [DOI] [PubMed] [Google Scholar]
- 92.Pal SS, Alam MS. Lacrimal canaliculitis: a major review. Semin Ophthalmol. 2024;39(8):586–594. doi: 10.1080/08820538.2024.2354689. [DOI] [PubMed] [Google Scholar]
- 93.Nghiem AZ, Ameen M, Koutroumanos N. Canalicular obstruction associated with dupilumab. Int Ophthalmol. 2023;43(12):4791–4795. doi: 10.1007/s10792-023-02880-2. [DOI] [PubMed] [Google Scholar]
- 94.Lee DH, Cohen LM, Yoon MK, et al. Punctal stenosis associated with dupilumab therapy for atopic dermatitis. J Dermatolog Treat. 2021;32(7):737–740. doi: 10.1080/09546634.2019.1711010. [DOI] [PubMed] [Google Scholar]
- 95.Dohlman JC, Habib LA, Freitag SK. Punctal agenesis: embryology, presentation, management modalities and outcomes. Anat Anz. 2019;224:113–116. doi: 10.1016/j.aanat.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 96.Ağaçkesen A, Yazıcıoğlu T, Oklar M, et al. Importance of etiology in canalicular obstruction surgery. Int Ophthalmol. 2023;43(9):3193–3198. doi: 10.1007/s10792-023-02719-w. [DOI] [PubMed] [Google Scholar]
- 97.Zhang HY, Zhang CY, Wang F, et al. Identification of a novel mutation in the FGF10 gene in a Chinese family with obvious congenital lacrimal duct dysplasia in lacrimo-auriculo-dento-digital syndrome. Int J Ophthalmol. 2023;16(4):499–504. doi: 10.18240/ijo.2023.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wang F, Tao H, Han C, et al. Preliminary report on screening IGSF3 gene mutation in families with congenital absence of lacrimal puncta and canaliculi. Int J Ophthalmol. 2020;13(9):1351–1355. doi: 10.18240/ijo.2020.09.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Feng ZX, Liu W, Li ZS, et al. Bony congenital nasolacrimal duct obstruction: a novel phenotype of aplasia of lacrimal and major salivary glands. Ophthalmology. 2024;131(5):589–594. doi: 10.1016/j.ophtha.2023.12.003. [DOI] [PubMed] [Google Scholar]
- 100.Ponzini E, Santambrogio C, de Palma A, et al. Mass spectrometry-based tear proteomics for noninvasive biomarker discovery. Mass Spectrom Rev. 2022;41(5):842–860. doi: 10.1002/mas.21691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Luo B, Li M, Xiang N, et al. The microbiologic spectrum of dacryocystitis. BMC Ophthalmol. 2021;21(1):29. doi: 10.1186/s12886-020-01792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Muthumalai M, Alam MS, Shrirao N, et al. A case-control study to determine the microbiological spectrum and antibiotic sensitivity patterns in congenital nasolacrimal duct obstruction. J Curr Ophthalmol. 2022;34(2):251–256. doi: 10.4103/joco.joco_216_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Xie C, Li XY, Cui HG. Potential candidate cells for constructing tissue-engineered lacrimal duct epithelium: a histological and cytological study in rabbits. J Zhejiang Univ Sci B. 2015;16(11):904–913. doi: 10.1631/jzus.B1500113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ghasemi H, Asghari Asl S, Yarmohammadi ME, et al. External dacryocystorhinostomy; success rate and causes of failure in endoscopic and pathologic evaluations. Iran J Pathol. 2017;12(3):189–194. [PMC free article] [PubMed] [Google Scholar]
- 105.Kubba H, Robson AK, Bearn MA. Epiphora: the role of rhinitis. Am J Rhinol. 1998;12(4):273–274. doi: 10.2500/105065898781389967. [DOI] [PubMed] [Google Scholar]
- 106.Jones LT. An anatomical approach to problems of the eyelids and lacrimal apparatus. Arch Ophthalmol. 1961;66:111–124. doi: 10.1001/archopht.1961.00960010113025. [DOI] [PubMed] [Google Scholar]
- 107.Kallman JE, Foster JA, Wulc AE, et al. Computed tomography in lacrimal outflow obstruction. Ophthalmology. 1997;104(4):676–682. doi: 10.1016/s0161-6420(97)30252-8. [DOI] [PubMed] [Google Scholar]
- 108.Dietze J, Suh D. Risk factors for poor surgical outcome of pediatric nasolacrimal duct obstruction. J Pediatr Ophthalmol Strabismus. 2019;56(4):261–264. doi: 10.3928/01913913-20190506-01. [DOI] [PubMed] [Google Scholar]
- 109.Tugrul S, Senturk E, Doğan R, et al. Effect of allergic rhinitis on the outcomes of diode laser dacryocystorhinostomy. Am J Otolaryngol. 2021;42(6):103127. doi: 10.1016/j.amjoto.2021.103127. [DOI] [PubMed] [Google Scholar]
- 110.Sanke RF. Pseudonasolacrimal duct obstruction caused by nasal allergy. Ophthalmic Surg. 1989;20(1):63–67. [PubMed] [Google Scholar]
- 111.Wojno TH. Allergic lacrimal obstruction. Am J Ophthalmol. 1988;106(1):48–52. doi: 10.1016/s0002-9394(14)76387-1. [DOI] [PubMed] [Google Scholar]
- 112.Leonardi A, Castegnaro A, Valerio AL, et al. Epidemiology of allergic conjunctivitis: clinical appearance and treatment patterns in a population-based study. Curr Opin Allergy Clin Immunol. 2015;15(5):482–488. doi: 10.1097/ACI.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 113.Or L, Zadok D, Hartstein ME. Mini-monoka stenting for patients with perennial allergic conjunctivitis. Orbit. 2019;38(4):285–289. doi: 10.1080/01676830.2018.1518465. [DOI] [PubMed] [Google Scholar]
- 114.Alsulaiman N, Alsuhaibani AH. Bicanalicular silicone intubation for the management of punctal stenosis and obstruction in patients with allergic conjunctivitis. Ophthalmic Plast Reconstr Surg. 2019;35(5):451–455. doi: 10.1097/IOP.0000000000001315. [DOI] [PubMed] [Google Scholar]
- 115.Gabbay IE, Nahum Y, Yassur Y, et al. Resolution of recalcitrant chronic papillary conjunctivitis associated with Epiphora following punctoplasty and lacrimal stenting. Can J Ophthalmol. 2018;53(4):380–383. doi: 10.1016/j.jcjo.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 116.Gündüz K, Günalp I, Gürses Ozden R. Chronic dacryoadenitis misdiagnosed as eyelid edema and allergic conjunctivitis. Jpn J Ophthalmol. 1999;43(2):109–112. doi: 10.1016/s0021-5155(98)00078-1. [DOI] [PubMed] [Google Scholar]