Abstract
The American Heart Association (AHA) introduced public access defibrillation more than 30 years ago. Since then, we have seen the growth of public access defibrillation programs across many settings within communities. However, despite high expectations that the availability of automated external defibrillators (AEDs) and more integrated public access defibrillation programs would dramatically increase cardiac arrest survival, AEDs are used in the United States in only 4% of out‐of‐hospital cardiac arrests and survival rates have remained disappointingly low. In follow‐up to a recent International Liaison Committee on Resuscitation report, an AED Symposium was organized by members of the AHA Emergency Cardiovascular Care Committee to establish a strategic roadmap for AED technology, education and training, and real‐world use of these devices, including integration with public access defibrillation programs to meet the AHA's goal of doubling out‐of‐hospital cardiac arrests survival by 2030. The meeting brought together a diverse group of subject matter experts including representatives from the US Food and Drug Administration, the defibrillator industry, clinicians, and scientists. This paper summarizes the proceedings of the AED symposium and suggests a set of strategic recommendations to ultimately improve survival from cardiac arrest.
Keywords: automated external defibrillators (AEDs), cardiopulmonary resuscitation (CPR), human factors, lay responders, out‐of‐hospital cardiac arrest
Subject Categories: Sudden Cardiac Death, Ventricular Fibrillation, Cardiopulmonary Arrest
Nonstandard Abbreviations and Acronyms
- FDA
US Food and Drug Administration
- OHCA
out‐of‐hospital cardiac arrest
- PAD
public access defibrillation
Public access defibrillation (PAD) was first introduced by the American Heart Association (AHA) in 1990 with the creation of the Task Force on the Future of Cardiopulmonary Resuscitation 1 followed by the “Public Access Defibrillation: A New Strategy to Prevent Sudden Death” conference in 1994. The conference proceedings identified recommendations for the AHA, the US Food and Drug Administration (FDA), and the National Institutes of Health to facilitate the organization of PAD programs as well as continued technological development and approval of small, low cost, accurate and reliable devices. 2 A follow up statement, published in 1997, provided strategies to both industry representatives and regulatory agencies for the assessment of accuracy of rhythm algorithms, alternative techniques, and waveforms to ensure safety of Automated External Defibrillators (AEDs) when used by minimally trained lay rescuers. This latter paper established cardiac rhythm categories and provided sensitivity and specificity bounds for the AEDs to identify each of these categories so that shocks were appropriately given to victims. 3 That cornerstone reference continues to guide industry and FDA standards for the development of AED technology.
Following the successful randomized Public Access Defibrillation Trial in 2004, PAD programs have become more integrated within major transportation centers, large sports arenas, and large businesses where many people are present. 4 With the desire to make AEDs more accessible, AEDs are now placed in locations where the risk of cardiac arrest is lower, and a lay public response may be more likely. These sites include community centers, small businesses, schools, and places of worship.
AHA advocacy efforts are underway to improve access to AEDs and to make sure there are cardiac emergency response plans in place to optimize their use. CPR training programs for community members include instruction on the use of AEDs. However, despite high expectations that improved training and increased AED availability would dramatically increase cardiac arrest survival, use rates have remained disappointingly low; and AEDs are used in the United States in only about 4% of out‐of‐hospital cardiac arrests (OHCA). Many of the fundamental barriers to successful AED use and PAD programs, and novel strategies to overcome them, were outlined in a recent International Liaison Committee of Resuscitation scientific statement. 5 An important strategy may be leveraging advances in technology to enhance AED use. However, implementation of new technology can be challenging with multiple barriers including regulatory structures that rely on old standards for approval of advanced devices. As technology has advanced, previous AED standards (1997) have now become outdated and limiting the opportunity for further integration and implementation of innovative technology.
The AED Symposium was held in November 2023, in Philadelphia, PA, and included 102 participants representing sectors of science, industry, regulatory agencies, and health care professionals involved in PAD programs.
The goals of this scientific symposium were to:
Review the current state of the Public Access Defibrillation from the perspective of multiple stakeholders.
Identify innovative solutions to improve AED access and usage.
Identify innovative solutions to optimizing AED availability, usability, and community engagement in PAD program.
- Develop an actionable road map for the AHA, along with key stakeholders, for each of the key focus areas:
-
◦Advocacy and Policy;
-
◦Science and Technology;
-
◦Education and Community Engagement.
-
◦
SYMPOSIUM STRUCTURE
The symposium was organized by members of the AHA Emergency Cardiovascular Care Committee. The program included an opening keynote speaker that summarized the historical background of PAD, while providing a vision into the future. Speakers included invited subject matter experts from the FDA, industry, clinicians, and scientists. This was followed by panel discussions focused on access, patient and community awareness, human factors, and science and technology to shorten the time interval to successful defibrillation. Each panel had a designated moderator to facilitate dialogue between the audience and speakers to foster interactive discussions. The program also included small‐group breakout sessions on human factors to provide a more direct experience and understanding for participants on how human interaction influences systems and processes designed to achieve the desired outcome. Feedback was collected through pre‐ and post‐event interactive surveys to generate a priority list of focus areas to address gaps over the short‐ and long‐term. The summit proceedings were recorded for debriefing purposes and to summarize key content for wider dissemination or future reference. The summary of each panel discussion is presented here as current state, gaps identified and a summary table of recommendations.
Envisioning Early Access to Defibrillation
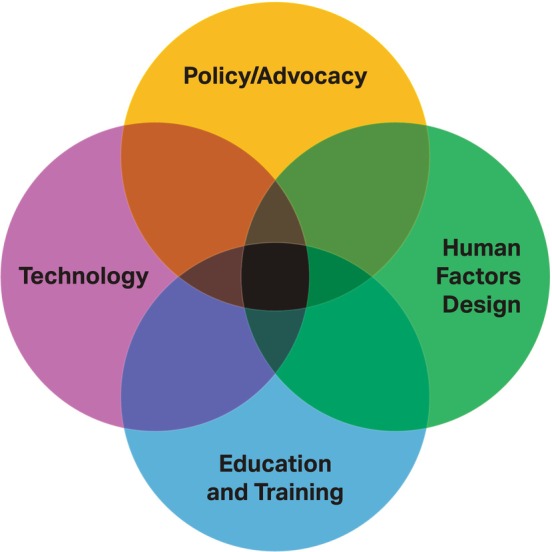
The symposium brought together participants who share the fundamental aspiration that every community, regardless of socioeconomic factors and geographic location, should have equitable and timely access to AEDs. A key aspect of examining the future use of AEDs was to rethink how PAD programs may improve OHCA outcomes, but also help mitigate historical disparities in access to defibrillation and bystander CPR. Bringing together a broad and diverse group of participants allows for the development of a roadmap that is needed to influence and coordinate meaningful change across all the areas of focus in this symposium (Figure 1).
Figure 1. AHA PAD symposium themes.
SCIENCE AND TECHNOLOGY
This panel focused on the current state of the FDA's guidance for AED manufacturers, as well as the need for updated recommendations from the scientific community to inform revised FDA guidance.
Current AED Manufacturer Guidance
The AHA Task Force on External Defibrillation, its subcommittee on AED Safety and Efficacy and the AED Manufacturers' Panel published recommendations for rhythm algorithm performance, incorporating new waveforms and enhancing safety to ensure safe use in public access defibrillation settings in 1997. 3 The recommendations of this landmark paper continue to serve as the core guide for manufacturers working in the development of new technology and devices and directs FDA approval. However, it has become increasingly clear that the recommendations are no longer adequate for manufacturers or the FDA.
Current Gaps in AED Technology
Given the advances in technological innovation in other industries, AED design continues to lag and has not changed dramatically in the past 30 years. Most AEDs do not currently include geolocation services which can easily identify AED location and integrate them into the 9‐1‐1 system. The use of automated notification would allow nearby lay responders to provide rapid response before emergency medical services (EMS) arrival. Secondly, most currently available AEDs are not able to identify shockable rhythms and deliver shocks during compressions, requiring long pauses during rhythm identification. If available, such new technology can increase chest compression fraction and shorten the pre‐shock delay. 6 In addition, AEDs are not currently interoperable with each other or with electronic health record systems creating a barrier to access. As such, the rhythms identified in the field before hospital arrival may not be available to health care personnel who are making determinations about short‐ and long‐term therapy. This lack of information to the treating physicians results in being unaware of the true cause of the collapse and potentially withholding appropriate therapy such as implantation of an implantable cardioverter defibrillator (ICD). 7 , 8
Table 1 summarizes the key recommendations related to science and technology identified during the AED Symposium.
Table 1.
Recommendations on Science and Technology
| Category | Problem | Solution |
|---|---|---|
| AED algorithms |
Review performance recommendations from Kerber et al Distinction between coarse and fine ventricular fibrillation Requirement for sensitivity and specificity of rhythms rarely seen during cardiac arrest, ie, NSR Regulations require small sample sizes No criteria for rhythm identification in the pediatric population 30–45 s required for rhythm identification |
Update Kerber paper Update AED performance standards for sample size, number of sample rhythms per patient, limit to actual rhythms of cardiac arrest Need for faster algorithms and shorter times to annotate rhythms during pauses Develop sensitivity and specificity criteria for rare or unlikely rhythms that will not present in cardiac arrest Validate the rhythm algorithms for pediatric population |
| Waveform optimization |
Most waveforms are based on existing waveforms with 20+ y of clinical use Research supporting defibrillation waveforms needs to be updated |
Update waveforms to the science of 2024 Provide more than a single option for defibrillation energy/waveform Update technology to account for artifact detection to include rhythm identification during chest compressions |
| Connectivity |
AEDs are deployed mostly at fixed facilities that are not interconnected with the community nor the public Majority of AED use data are simply lost and never used to study, analyze, and to promote new discoveries |
Equip AEDs with web and cellular connectivity to Enable GPS tracking, which could be wrapped into leading mobile apps like Google Maps to locate the nearest AED to the public, 911 dispatchers, and EMS personnel Wireless transmission of results to receiving hospital or central location or repository AED registry Make recommendations on standard case reporting and simple report extraction from AED through USB port or Bluetooth |
AED indicates automated external defibrillators; and NSR, non‐shockable rythm
HUMAN FACTORS
Humans are the end‐users of AEDs in the field and, as such, are an integral part of ensuring AED design allows for lay responders to use the device safely and appropriately during stressful situations.
Current FDA Guidance
The FDA published guidance for medical device manufacturers in 2016, “Applying Human Factors and Usability Engineering to Medical Devices,” which provides recommended methodology for human factors validation studies when providing evidence to the Agency that a device can be used safely and effectively for the intended users, uses, and use environments. 9 The FDA also has recommendations for medical device manufacturers to consider when developing their human factors validation protocol for AEDs to be used by lay responders. A critical task for a device is defined as, “A user task which, if performed incorrectly or not performed at all, would or could cause serious harm to the patient or user, where harm is defined to include compromised medical care.” In the context of AEDs, examples of these critical tasks are: removal of patient clothing, appropriate pad/electrode placement, not touching the patient when delivering a shock, and time to treatment (eg, shock) delivery. For example, as compared with other medical device usability assessments, the FDA guidance recommends medical device manufacturers include a timing component in the success criteria when assessing the usability of AEDs. Time to treatment delivery is especially critical when considering AED use by lay rescuers because timeliness of treatment is directly related to successful outcomes. Furthermore, medical device manufacturers should consider including human factors in the validation studies, stratified user groups such as older and younger lay participants, a purchaser group, and a representative lay responder group. Ultimately, by assessing all critical tasks in the human factors validation study, medical device manufacturers are providing evidence to the Agency that the risk mitigations are effective in preventing critical use errors.
How Human Factors Data Are Tracked
The FDA relies heavily on the MAUDE (Manufacturer and User Facility Device Experience) database to analyze incoming device reports by mandatory reporters (manufacturers, importers, and device user facilities) and voluntary reporters such as health care professionals, patients and consumers. This serves as the basis for identifying critical issues that may impact device function. However, ongoing research showcases how important qualitative research and real‐time case data may be in understanding more granular issues with AEDs. Data presented by Peel Regional Paramedic Services in Ontario, Canada gathered through the use of the Lay Responder debriefing program 10 exemplify how the real‐world experience of using an AED by lay rescuers can provide critical insights into more human‐centered design of the devices. 11 Unlike fire extinguishers, a common comparison, every AED on the market is designed with different cases, covers, and screens, different voice prompts, order of the prompts, and overall inconsistent imagery, naming conventions, or language. To make AEDs easier to use, their design must be simple, transparent, and standardized. Then, when education and training is deployed in the community, people should feel confident that the available AED will be recognizable in a time‐sensitive, highly stressful situation.
Use of Simulation to Improve AED Design
Research from simulation‐based studies assessing a lay rescuers' abilities to accurately use AEDs is critical to improve design. Comparisons of different AEDs have shown that user‐friendliness was significantly different across different models. This was highlighted by interviewing laypersons after use of AEDs in a simulated setting showing that intuitiveness and improved visual cues were considered important by laypersons. 12 For example, poor imagery of electrode placement on the device, resulting in less effective shock delivery was reported by both lay rescuers and health care professionals. The illustrations on the electrodes show inaccurate placement with the lateral pad in the anterior axillary line, rather than mid‐axillary. In addition, following defibrillation, some laypersons remove the electrodes after only 1 shock or do not resume chest compressions. This may be related to inadequate training or uncontextualized translation of abbreviations into other languages. Moreover, these issues are only compounded when simulations include activation of the pediatric mode to defibrillate because of different solutions from various manufacturers (separate electrodes or buttons in the device).
Gaps in Human Factors
To date, there has been a lack of integration of human factors research to inform a more robust understanding of how consumers use AEDs in real‐world settings. Such research could make AEDs more acceptable to the public, more user‐friendly and ensure that skill training transfers directly to real‐life situations when users are under duress.
Table 2 summarizes the key recommendations related to human factors identified during the AED Symposium.
Table 2.
Recommendations on Human Factors
| Category | Problem | Solution |
|---|---|---|
| Data collection | MAUDE is not an effective way to understand real‐world challenges to AED use and treatment delivery |
Better real‐world data collection using qualitative and quantitative methods Research on stratified groups who are more likely to have difficulty with the device (eg, older, younger, non‐English speaking) |
| AED design | Confusing designs for lay rescuers ie, if you have seen one AED, you have seen one AED |
Standardization of AED look and feel Design must be transparent, simple, with interoperability of electrodes Standard method to activate pediatric mode |
| Electrode design | Visual cues are difficult to interpret and electrodes are often poorly placed |
Better visual cues on devices Electrodes should be similar in design and application to standardize training |
| Voice prompts | AED voice prompts are different for each device and can be confusing in a highly stressful situation for lay rescuers |
‐Standardization of AED voice prompts and ordering ‐Ability to “teach to the prompts” in CPR training courses and contextualize training |
AED indicates automated external defibrillators; CPR, cardiopulmonary resuscitation; and MAUDE, Manufacturer and User Facility Device Experience.
Education and Training
Education and training of lay responders is an integral part of increasing the willingness to respond, critical skills in performing CPR and using the AED, as well as how to handle the stress related to the event.
Current Educational Efforts
Major training organizations like the AHA are focused on providing hands‐on education for lay responders to better understand how to use AEDs. Despite focused training efforts, CPR and AED training has been found to be lower in counties with a higher proportion of rural, Black, Hispanic, and lower income residents. 13 The focus is on developing a framework for which community members can anticipate presence of an AED will prompt them to act. However, because of high variability in how AEDs are designed, as well as voice prompts, generic actions are covered in these courses, which may mean that the lay responder may have a completely different interaction with the device in a real‐life situation. 11 Finally, equity, diversity, and inclusiveness considerations are absent from current training paradigms and presents significant challenges for certain groups, especially those in underserved and vulnerable populations.
Elements of a Successful PAD Program
Summit participants recognized community education and engagement as a critical element to a successful PAD program. The importance of creating a culture of valuing CPR and AED training and use in a community as a whole is a crucial reframing of how we talk about CPR training, and schoolchildren are a target population of interest to drive sustainable change within a population.
CPR and AED use education can be integrated into school curricula. Schoolchildren, even in the absence of formalized training, have demonstrated successful use of an AED in simulated conditions. 14 , 15 , 16 Schoolteachers are in a unique position to integrate CPR and AED use education in the classroom. Previous research has shown how schoolteachers can teach basic life support content after proper training. 14 , 15 , 16 , 17 Summit participants noted that it is important that schoolchildren are a priority population to be educated in CPR and use of an AED. Examples of take‐home resources to help engage and educate schoolchildren were shared at the symposium.
Table 3 summarizes the key recommendations related to education and training identified during the AED Symposium.
Table 3.
Recommendations on Education and Training
| Category | Problem | Solution |
|---|---|---|
| Compliance with CPR training in schools | Lack of funding, time, and interest |
Gamification of CPR and AED education Student record/report card has a separate course record showing completion of training BLS Peer Training Engage public school systems Legislative efforts to provide funding assistance for CPR and AED training |
| Train personnel in schools | Educators, and staff are not required to have or maintain certification |
Require CPR and AED training as a prerequisite for employment in school systems Annual training as part of the educator's professional development pathway BLS Peer Training |
| Equipment | Training devices not available or accessible | Find alternate methods:
|
AED indicates automated external defibrillators; BLS, basic life support, and CPR, cardiopulmonary resuscitation.
Policy Gap Analysis
The Emergency Cardiovascular Care Systems of Care subcommittee completed a comprehensive analysis of policies influencing access to AEDs. The policy gap analysis revealed a complex landscape of laws and regulations governing the use of Automated External Defibrillators (AEDs) in public places. Significant heterogeneity was observed across different jurisdictions, highlighting inconsistencies and gaps in standards and requirements (Figure 2). Key findings included variations in AED accessibility mandates, training and certification requirements for AED operators, liability protection for AED use, and reporting obligations. The analysis emphasized the need for harmonization and standardization of AED‐related policies to ensure widespread deployment, effective use, and legal protection in emergency situations across diverse settings. Universal AED public policy would inform training and education efforts which provide the foundation of new interventions to increase bystander participation, including AED utilization as part of an effort to evolve PAD programs.
Figure 2. Distribution of number of laws, policies, and regulations by state in the United States.

AED indicates automated external defibrillators.
Table 4 summarizes the key recommendations related to policies and regulations during the AED Symposium.
Table 4.
Recommendations on Policies and Regulations
| Category | Problem | Solution |
|---|---|---|
| Laws, policies, and regulation in general |
‐Complex, variable, and strict regulations create barriers to AED placement, maintenance, and use ‐Liability concerns may deter individuals and organizations from deploying or using AEDs |
‐Need for harmonization across complex laws and regulations ‐Need for clear liability protections ‐Federal regulations should serve as a floor, but not a ceiling, for the legal framework across states |
| AED deployment |
‐No clear guidance on optimal placement ‐AEDs are currently located in buildings that are not necessarily accessible to the public |
‐Leverage technology to inform deployment ‐AED registration locally ‐Inclusion of AED locations in telephone apps |
| AED accessibility |
‐No universal guidance on signage and packaging for deployment ‐The current most common AED location is in a cabinet ‐Cost, including the expense of AED acquisition, training, and maintenance can limit access |
‐Optimal deployment strategies must consider equity and account for areas with a higher risk ‐Local jurisdictions should offer incentives, grants to expand accessibility ‐Placement with 24/7 accessibility ‐Lower cost ‐Recommend or legislate ILCOR endorsed universal AED signage already in use in many other countries |
| AED readiness | No clear and universal standards or plan for the maintenance and upkeep of AEDs |
‐Standardization and simplicity on maintenance plans to ensure readiness ‐Potential to implement readiness plans based on prevention models created for fire safety and extinguishing devices requiring a regular inspection and testing ‐Wi‐Fi notification to inform owners of expiring batteries and pads |
AED indicates automated external defibrillators; and ILCOR, International Liaison Committee on Resuscitation.
Innovative Approaches to Improve Public Access to Defibrillation
The final panel of the AED Symposium was a presentation of several programs which have developed novel methods to improve PAD within their communities. These sites include the City of San Diego, Denmark, City of Pittsburgh, and Holland. During the presentations, several themes were consistent across the sites. These include wide‐spread CPR education and AED training, high density of availability of AEDs, government buy‐in for the programs, dispatch telephone apps to quickly notify lay rescuers and attention to equity in both CPR training and AED availability. Below are some of the specifics which have made each program unique and successful within their communities. The panel also included a presentation about the potential benefit of drones to deliver AEDs in a timely manner.
San Diego Project Heart Beat
Created in 2001, the goals of the project are to save lives by establishing awareness, education, and making AEDs as accessible as fire extinguishers throughout the city and county of San Diego. Every high school student graduates with compression‐only CPR and AED training. Other unique aspects of the program include use of 30‐second Public Service Announcement videos and social media posts, ability to purchase AEDs at reduced costs, post‐incident management with EMS teams responding to downloaded AED data and provide critical incident debriefing for responders. Since the project's inception, 10 000 AEDs have been distributed and 208 lives, including 5 children have been saved.
Denmark
Denmark instituted the Danish AED Network, linking information about individual AEDs to all emergency medical dispatch centers across the country, enabling identification of the nearest accessible AED in the event of an OHCA. 18 Their program uses text‐messages or smartphone applications to activate citizen responders and linked them to an available AED. This resulted in a 76% increase in bystander CPR and tripling the rate of bystander defibrillation. 19 Dispatching volunteers to the scene of cardiac arrest with AEDs 20 ; optimizing AED placement in the community through spatiotemporal and mathematical modeling 21 , 22 ; and new AED smart screens that alert lay rescuers to the event and location of a cardiac arrest were critical factors leading to this change. Publicly available AEDs have increased from 0 to 20 943 since 2006, and AEDs with 24/7 access have increased from 2775 in 2015 to 12 923 in 2021. Through the telephone app, volunteer responders now number 150 000 distributed throughout the entire country. When a citizen responder arrives first, the odds ratio of bystander CPR and defibrillation is 3.73 (2.04–6.84). Additional interventions which support the PAD programs include legislative mandates to report all cardiac arrests to the Danish Cardiac Arrest Registry, CPR training in schools, workplaces and before receiving a driver's license, and public campaigns associated with Restart a Heart Day.
The Netherlands
Holland started their PAD project in 2005 with the adoption of a telephone alert app notifying citizens of a suspected cardiac arrest in both public and private homes. Responders must have an active CPR certification. Refresher courses are required every year to remain active in the program. Two thirds of located volunteers are directed to the AED first, one third directed to the victim to initiate or continue CPR.
To increase awareness, the Netherlands Heart Foundation supported frequent radio and TV announcements and created a “6 minutes” campaign to encourage local communities to organize themselves with volunteers and AEDs. These volunteers, along with an increased response from first responders, resulted in AED application in >50% of victims before EMS arrival. There has been a reduction of the delay from emergency‐call to first defibrillation from any device (AED or EMS) from 11.7 to 9.3 minutes in residential areas and from 9.2 to 8 minutes in public places. Consequently, survival from OHCA with a shockable rhythm in residential areas (60%–70% of all OHCA) increased from 26% to 39% and in public (38% of all OHCA) remained at 51%. 23 , 24 This indicates that community rescuers indeed contribute primarily to increased survival of patients in residential areas where most OHCAs occur.
Pittsburgh, PA
The PAD program in Pittsburgh also uses a telephone‐dispatch app including a defined and managed responder program, making the distribution of AEDs and trainers equitable across the city, recognizing that residential neighborhoods need coverage even more than commercial areas and that the AEDs can be co‐located with other life‐saving tools, such as Narcan and Stop the Bleed supplies. An ideal responder program includes law enforcement, designated off‐duty responders, as well as the general public. AEDs must be registered to the telephone app with a sustainable system‐level plan for management and maintenance. System analytics are collected from the start to measure the effectiveness of the program and identify underserved or underutilizing in areas. Post‐event surveys including all elements of response (ie, alert received or missed, arrival at scene, chest compressions, locate and/or use AED and psychological stress) are instrumental in improving the program.
Equity is fundamental to a successful PAD program and every residential neighborhood is different. Thus, any program cannot be “one size fits all” and each neighborhood needs a stakeholder group to own the effort. System analytics from the telephone app has identified the areas at highest risk for cardiac arrest and correlates this with the number of responders and AEDs. Responding to these disparities is crucial to improving outcomes. As geolocation can disincentivize participation within specific populations, the telephone app offers an alternative called AED responders whereby the proximity trigger for an alert is the nearest AED and the geolocation of the responder is not recorded. Within the city of Pittsburgh, bystander CPR in telephone app public associated areas was 60% versus 36% in non‐telephone app associated OHCA. 25
Drone AED Delivery
Drones, or unmanned aerial vehicles, hold promise for rapidly delivering AEDs to bystanders for OHCA treatment. 26 International research has advanced our understanding of this technology to deliver AEDs in a timely manner first through mathematical optimization research, then simulated drone AED deliveries, and now with real‐time and safe beyond visual line of sight operations within controlled air space. Sweden has done this on more than 200 suspected cardiac arrests. 27 , 28 , 29 , 30 , 31 The first report of a patient who was successfully defibrillated by a drone‐delivered AED occurred in Sweden in January of 2022. 32
In the United States, simulation research has demonstrated that bystanders can successfully apply and use a drone‐delivered AED with telephone dispatch assistance. 33 This study demonstrated that a drone needed to arrive at least 1:59 minutes ahead of EMS in order for the bystander to have time to retrieve, apply, and defibrillate an OHCA patient. Mathematical optimization research demonstrated that a state‐wide drone network, along with first responders carrying an AED, could potentially achieve a median AED arrival time (time from 9‐1‐1 call to AED arrival) of 4.8 (interquartile range, 4.3–5.2) minutes 34 , 35 with a median of 7 (interquartile range, 5–8) drones per county, with greatest median arrival time benefit in urban areas compared with rural regions.
There is a growing body of evidence that in a controlled environment in both urban and rural regions drones can deliver an AED faster than the current EMS services. However, the effectiveness of drone delivery of AEDs on improving cardiac arrest survival is currently dependent on resolving several supporting factors including, but not limited to Federal and local aviation regulations, practical considerations of operation and maintenance of a drone network, weather effects on flight operations, community education, AED literacy, the optimal drone model, and cost.
CONCLUSIONS
The AED summit successfully brought together a multidisciplinary group of subject matter experts from the FDA, industry, clinicians, and scientists to collaboratively discuss the current state of knowledge, identify gaps, and establish strategic recommendations for the future of AED technology and PAD. These strategic recommendations serve as a roadmap to transform how we think about PAD, AED devices, program implementation, and ultimately improve survival from OHCA.
Sources of Funding
The AED Symposium was made possible by the AHA with support from Philips Healthcare, Stryker Corporation, and ZOLL Medical Corporation.
Disclosures
Benjamin S. Abella MD MPhil reports research funding from the National Institute Health, Avive, Becton Dickinson, Consulting: Becton Dickinson, Zoll, Stryker, Neuroptics; Tom P. Aufderheide, MD, MS, grants from: The National Heart, Lung, and Blood Institute and National Institute for Neurological Disorders and Stroke for ARREST Trial and, Influence of Cooling duration on Efficacy in Cardiac Arrest Patients. Zoll Medical inc. for Ventilation Monitoring in Out‐of‐Hospital Emergency Care. Consulting: Medtronics, Inc. Volunteer: Citizen CPR Foundation, Resuscitation Science Symposium Planning Committee, and 3CPR Leadership Committee; Lance B. Becker MD, institutional grants from Nihon Kohden, Philips Medical Systems, and ZOLL Medical Corp. Serves on the scientific advisory boards for Nihon Kohden and Philips; Katie N. Dainty PhD, member Medical Advisory Board for Philips Healthcare; Carolina Malta‐Hansen MD, PhD, grants from TrygFonden, Helsefonden, Independent Research Fund Denmark, Laerdal Foundation, Novo Nordisk Foundation, Capital Region of Denmark Research Fund, Member of International Liaison Committee on Resuscitation Basic Life Support Task Force and RACE‐CARS (Regional Approaches to Cardiovascular Emergencies—Cardiac Arrest) trial steering committee; Rudolph W. Koster, MD, PhD, medical advisor for Stryker Emergency Care (Redmond, WA), and Heartsine (Belfast, UK); Michael R. Sayre, MD, Consultant, Stryker Emergency Care (Redmond, WA); Monique A. Starks MD, MHS, reports grants on AHA Health Equity Research Network—Improving Access to Care and other Health Inequities in Rural America—Developing and Testing Drone‐Delivered AEDs for Cardiac Arrests In Rural America, The National Heart, Lung, and Blood Institute K23 Award—Evaluation of the Requirements and Critical Features of a Drone‐Deployed AED Network to Improve Community‐Level Survival after out‐of‐hospital cardiac arrest, and UH3 Cluster Randomized Trial, RACE‐CARS. The remaining authors have no disclosures to report.
Acknowledgments
We would like to express our gratitude to all AHA Emergency Cardiovascular Care staff and Systems of Care subcommittee members for their hard work in planning the AED Summit. Also, our heartfelt appreciation to all participants and collaborators for their active engagement and insightful contributions, which made the summit a huge success.
This manuscript was sent to Saket Girotra, MD, SM, Associate Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 9.
REFERENCES
- 1. Cobb LA, Eliastam M, Kerber RE, Melker R, Moss AJ, Newell L, Paraskos JA, Weaver WD, Weil M, Weisfeldt ML. Report of the American Heart Association task force on the future of cardiopulmonary resuscitation. Circulation. 1992;85:2346–2355. doi: 10.1161/01.CIR.85.6.2346 [DOI] [PubMed] [Google Scholar]
- 2. Weisfeldt ML, Kerber RE, McGoldrick RP, Moss AJ, Nichol G, Ornato JP, Palmer DG, Riegel B, Smith SC Jr. American Heart Association report on the public access defibrillation conference December 8–10, 1994. Automatic external defibrillation task force. Circulation. 1995;92:2740–2747. [DOI] [PubMed] [Google Scholar]
- 3. Kerber RE, Becker LB, Bourland JD, Cummins RO, Hallstrom AP, Michos MB, Nichol G, Ornato JP, Thies WH, White RD, et al. Automatic external defibrillators for public access defibrillation: recommendations for specifying and reporting arrhythmia analysis algorithm performance, incorporating new waveforms, and enhancing safety. A statement for health professionals from the American Heart Association Task Force on Automatic External Defibrillation, Subcommittee on AED Safety and Efficacy. Circulation. 1997;95:1677–1682. [DOI] [PubMed] [Google Scholar]
- 4. Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M, et al. Public‐access defibrillation and survival after out‐of‐hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566 [DOI] [PubMed] [Google Scholar]
- 5. Brooks SC, Clegg GR, Bray J, Deakin CD, Perkins GD, Ringh M, Smith CM, Link MS, Merchant RM, Pezo‐Morales J, et al. Optimizing outcomes after out‐of‐hospital cardiac arrest with innovative approaches to public‐access defibrillation: a scientific statement from the International Liaison Committee on Resuscitation. Circulation. 2022;145:e776–e801. doi: 10.1161/CIR.0000000000001013 [DOI] [PubMed] [Google Scholar]
- 6. de Graaf C, Beesems SG, Oud S, Stickney RE, Piraino DW, Chapman FW, Koster RW. Analyzing the heart rhythm during chest compressions: performance and clinical value of a new AED algorithm. Resuscitation. 2021;162:320–328. doi: 10.1016/j.resuscitation.2021.01.003 [DOI] [PubMed] [Google Scholar]
- 7. Homma PCM, de Graaf C, Tan HL, Hulleman M, Koster RW, Beesems SG, Blom MT. Transfer of essential AED information to treating hospital (TREAT). Resuscitation. 2020;149:47–52. doi: 10.1016/j.resuscitation.2020.01.033 [DOI] [PubMed] [Google Scholar]
- 8. Hansen MB, Lippert FK, Rasmussen LS, Nielsen AM. Systematic downloading and analysis of data from automated external defibrillators used in out‐of‐hospital cardiac arrest. Resuscitation. 2014;85:1681–1685. doi: 10.1016/j.resuscitation.2014.08.038 [DOI] [PubMed] [Google Scholar]
- 9. Food and Drug Administration . Applying Human Factors and Usability Engineering to Medical Devices: Guidance for Industry and Food and Drug Administration Staff . 2016. Accessed June 1, 2024. https://www.fda.gov/media/80481/download.
- 10. Snobelen PJ, Pellegrino JL, Nevils GS, Dainty KN. Helping those who help. Circ Cardiovasc Qual Outcomes. 2018;11:e004702. doi: 10.1161/CIRCOUTCOMES.118.004702 [DOI] [PubMed] [Google Scholar]
- 11. Mausz J, Snobelen P, Tavares W. “Please. Don't. Die.”: a grounded theory study of bystander cardiopulmonary resuscitation. Circ Cardiovasc Qual Outcomes. 2018;11:e004035. doi: 10.1161/CIRCOUTCOMES.117.004035 [DOI] [PubMed] [Google Scholar]
- 12. Stærk M, Bødtker H, Lauridsen KG, Løfgren B. Automated external defibrillation training on the left or the right side: a randomized simulation study. Open Access Emerg Med. 2017;9:73–79. doi: 10.2147/OAEM.S140220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Anderson ML, Cox M, Al‐Khatib SM, Nichol G, Thomas KL, Chan PS, Saha‐Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, et al. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. doi: 10.1001/jamainternmed.2013.11320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Martínez‐Isasi S, Abelairas‐Gómez C, Pichel‐López M, Barcala‐Furelos R, Varela‐Casal C, Vázquez‐Santamariña D, Sánchez‐Santos L, Rodríguez‐Núñez A. Learning to resuscitate at school: study in 8–12 year‐old schoolchildren. Ann Pediatr (Eng Ed). 2022;96:17–24. doi: 10.1016/j.anpede.2020.09.013 [DOI] [PubMed] [Google Scholar]
- 15. Abelairas‐Gómez C, Martinez‐Isasi S, Barcala‐Furelos R, Varela‐Casal C, Carballo‐Fazanes A, Pichel‐López M, Fernández Méndez F, Otero‐Agra M, Sanchez Santos L, Rodriguez‐Nuñez A. Training frequency for educating schoolchildren in basic life support: very brief 4‐month rolling‐refreshers versus annual retraining‐a 2‐year prospective longitudinal trial. BMJ Open. 2021;11:e052478. doi: 10.1136/bmjopen-2021-052478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Varela‐Casal C, Abelairas‐Gómez C, Otero‐Agra M, Barcala‐Furelos R, Rodríguez‐Núñez A, Greif R. Teaching basic life support to 5‐ to 8‐year‐old children: a cluster randomized trial. Pediatrics. 2021;148:e2021051408. doi: 10.1542/peds.2021-051408 [DOI] [PubMed] [Google Scholar]
- 17. Abelairas‐Gómez C, Rodríguez‐Núñez A, Greif R. Now it is time to teach to schoolteachers: the long road to the Schoolteacher BLS Teaching Curriculum. Resuscitation. 2021;165:66–67. doi: 10.1016/j.resuscitation.2021.06.005 [DOI] [PubMed] [Google Scholar]
- 18. Hansen CM, Lippert FK, Wissenberg M, Weeke P, Zinckernagel L, Ruwald MH, Karlsson L, Gislason GH, Nielsen SL, Køber L, et al. Temporal trends in coverage of historical cardiac arrests using a volunteer‐based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130:1859–1867. doi: 10.1161/CIRCULATIONAHA.114.008850 [DOI] [PubMed] [Google Scholar]
- 19. Andelius L, Malta Hansen C, Lippert FK, Karlsson L, Torp‐Pedersen C, Kjær Ersbøll A, Køber L, Collatz Christensen H, Blomberg SN, Gislason GH, et al. Smartphone activation of citizen responders to facilitate defibrillation in out‐of‐hospital cardiac arrest. J Am Coll Cardiol. 2020;76:43–53. doi: 10.1016/j.jacc.2020.04.073 [DOI] [PubMed] [Google Scholar]
- 20. Folke F, Shahriari P, Hansen CM, Gregers MCT. Public access defibrillation: challenges and new solutions. Curr Opin Crit Care. 2023;29:168–174. doi: 10.1097/MCC.0000000000001051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Siddiq AA, Brooks SC, Chan TCY. Modeling the impact of public access defibrillator range on public location cardiac arrest coverage. Resuscitation. 2013;84:904–909. doi: 10.1016/j.resuscitation.2012.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sun CLF, Karlsson L, Torp‐Pedersen C, Morrison LJ, Folke F, Chan TCY. Spatiotemporal AED optimization is generalizable. Resuscitation. 2018;131:101–107. doi: 10.1016/j.resuscitation.2018.08.012 [DOI] [PubMed] [Google Scholar]
- 23. Zijlstra JA, Stieglis R, Riedijk F, Smeekes M, van der Worp WE, Koster RW. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out‐of‐hospital cardiac arrest dispatch system. Resuscitation. 2014;85:1444–1449. doi: 10.1016/j.resuscitation.2014.07.020 [DOI] [PubMed] [Google Scholar]
- 24. Stieglis R, Zijlstra JA, Riedijk F, Smeekes M, van der Worp WE, Tijssen JGP, Zwinderman AH, Blom MT, Koster RW. Alert system‐supported lay defibrillation and basic life‐support for cardiac arrest at home. Eur Heart J. 2022;43:1465–1474. doi: 10.1093/eurheartj/ehab802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Smida T, Salerno J, Weiss L, Martin‐Gill C, Salcido DD. PulsePoint dispatch associated patient characteristics and prehospital outcomes in a mid‐sized metropolitan area. Resuscitation. 2022;170:36–43. doi: 10.1016/j.resuscitation.2021.11.007 [DOI] [PubMed] [Google Scholar]
- 26. Boutilier JJ, Brooks SC, Janmohamed A, Byers A, Buick JE, Zhan C, Schoellig AP, Cheskes S, Morrison LJ, Chan TCY. Optimizing a drone network to deliver automated external defibrillators. Circulation. 2017;135:2454–2465. doi: 10.1161/circulationaha.116.026318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Claesson A, Bäckman A, Ringh M, Svensson L, Nordberg P, Djärv T, Hollenberg J. Time to delivery of an automated external defibrillator using a drone for simulated out‐of‐hospital cardiac arrests vs emergency medical services. JAMA. 2017;317:2332–2334. doi: 10.1001/jama.2017.3957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Claesson A, Fredman D, Svensson L, Ringh M, Hollenberg J, Nordberg P, Rosenqvist M, Djarv T, Österberg S, Lennartsson J, et al. Unmanned aerial vehicles (drones) in out‐of‐hospital‐cardiac‐arrest. Scand J Trauma Resusc Emerg Med. 2016;24:124. doi: 10.1186/s13049-016-0313-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Schierbeck S, Hollenberg J, Nord A, Svensson L, Nordberg P, Ringh M, Forsberg S, Lundgren P, Axelsson C, Claesson A. Automated external defibrillators delivered by drones to patients with suspected out‐of‐hospital cardiac arrest. Eur Heart J. 2021;43:1478–1487. doi: 10.1093/eurheartj/ehab498 [DOI] [PubMed] [Google Scholar]
- 30. Schierbeck S, Nord A, Svensson L, Rawshani A, Hollenberg J, Ringh M, Forsberg S, Nordberg P, Hilding F, Claesson A. National coverage of out‐of‐hospital cardiac arrests using automated external defibrillator‐equipped drones—a geographical information system analysis. Resuscitation. 2021;163:136–145. doi: 10.1016/j.resuscitation.2021.02.040 [DOI] [PubMed] [Google Scholar]
- 31. Schierbeck S, Nord A, Svensson L, Ringh M, Nordberg P, Hollenberg J, Lundgren P, Folke F, Jonsson M, Forsberg S, et al. Drone delivery of automated external defibrillators compared with ambulance arrival in real‐life suspected out‐of‐hospital cardiac arrests: a prospective observational study in Sweden. Lancet Digit Health. 2023;5:e862–e871. doi: 10.1016/S2589-7500(23)00161-9 [DOI] [PubMed] [Google Scholar]
- 32. Schierbeck S, Svensson L, Claesson A. Use of a drone‐delivered automated external defibrillator in an out‐of‐hospital cardiac arrest. N Engl J Med. 2022;386:1953–1954. doi: 10.1056/NEJMc2200833 [DOI] [PubMed] [Google Scholar]
- 33. Starks MA, Blewer AL, Chow C, Sharpe E, van Vleet L, Arnold E, Buckland DM, Joiner A, Simmons D, Green CL, et al. Incorporation of drone technology into the chain of survival for OHCA: estimation of time needed for bystander treatment of OHCA and CPR performance. Circ Cardiovasc Qual Outcomes. 2024;17:e010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Starks MACJ, Leung B, Chan T, Blewer AL, Simmons D, Joiner A, Cabanas JG, Harmody M, Nelson D, Clark T, et al. Accelerating AED use in out‐of‐hospital cardiac arrest with combinations of first responder and drone delivery to achieve 5‐minute AED deployment. Circulation. 2022;146:244. [Google Scholar]
- 35. Chu JL, Blewer AL, Konstantin K, Nelson D, Powell S, McNally BF, Granger CB, Ornato JP, Mark DB, Chan TY, et al. Rural–urban differences for integrated first responder and drone automated external defibrillator delivery in North Carolina. Circulation. 2023;148:148. doi: 10.1161/circ.148.suppl_1.105 [DOI] [Google Scholar]


