Abstract
Introduction
Internet-based interventions (IBI) increase access to evidence-based treatments for mental disorders, but knowledge of their mechanisms of change is limited. Self-efficacy, a key factor in psychotherapy, is especially relevant in IBI due to its self-help focus. We investigated self-efficacy and related constructs as outcomes, predictors/moderators, and mediators in randomized controlled trials.
Methods
A systematic search was conducted across PsycINFO, PubMed, CINAHL, and Web of Science. Two reviewers selected studies, extracted data, and assessed bias. Effects were quantified using random effect models and supplemented by narrative syntheses and box score visualizations.
Results
70 studies (N = 17,407 participants) were included. IBI showed moderate effects on self-efficacy in within (d = 0.47) and between (d = 0.46) comparisons, with guided interventions having the largest effect (d = 0.66). Findings on self-efficacy as a predictor/moderator were mixed, though some studies suggested individuals with lower self-efficacy benefit more. Self-efficacy emerged as a mediator through which IBI affected treatment outcomes.
Conclusion
Self-efficacy appears influential in IBI efficacy and may itself be a valuable treatment target. However, mixed results and methodological limitations in mediator studies highlight the need for further research, particularly on long-term effects.
Keywords: Internet-based interventions; Self-efficacy; Mastery, digital health; Systematic review; Meta-analysis
Highlights
-
•
Internet-based interventions potentially increase access to psychological treatment
-
•
Self-efficacy can be increased by internet-based interventions
-
•
Self-efficacy seems to have a mediating effect on treatment outcome
-
•
It remains unclear who could profit from self-efficacy enhancing interventions
1. Introduction
Mental disorders have high prevalence and comorbidity rates and are associated with significant individual, societal, and economic costs (Vigo et al., 2016). Psychotherapy is an effective treatment for mental disorders, but the demand already clearly exceeds treatment capacities (e.g., American Psychological Association, 2022). Internet-based interventions (IBI) are one way to meet the high demand for evidence-based treatment (Ebert et al., 2018). Terminology in the field of digital interventions is inconsistent, with various terms such as „e-mental health“, „web-based interventions“, and „internet-delivered therapy“used interchangeably (Smoktunowicz et al., 2020). While no universal consensus exists on a single preferred term, for the purposes of this manuscript, we adopt the term „IBI“. IBI predominantly function as self-help programs, accessible through websites or mobile applications, that help affected individuals cope with their mental health. They can be either guided with some degree of contact between professionals and participants, unguided without any human support, or an integrated element of a face-to-face treatment in blended approaches (Ebert et al., 2018). IBI offer several advantages over traditional face-to-face treatment, including ease of access (provided the individual has internet access and a compatible device), low cost, anonymity, time- and location-independent delivery, empowerment to manage one's health care, and flexibility of use (Donker et al., 2015; Ebert et al., 2018). Recent meta-analyses have found that IBI are effective in treating mental disorders and stress (Domhardt et al., 2020; Heber et al., 2017; Taylor et al., 2021) with guided interventions seeming more beneficial than those without guidance (Werntz et al., 2023). However, little is known about the underlying processes that influence the treatment success of IBI for mental disorders.
Given the self-help focus of IBI, which aims to empower patients to take their treatment into their own hands, Bandura's social learning theory provides a promising framework to examine mechanisms of change in the context of IBI (Bandura, 1977). Bandura (1977) assumes that therapeutic change derives from a common transdiagnostic cognitive mechanism, namely perceived self-efficacy, which is defined as the “beliefs in one's capabilities to organize and execute the courses of action required to produce given attainments” (Bandura, 1997, p. 3). In the context of IBI, this could imply that a patient's belief in their ability to effectively engage with and complete the IBI can influence the outcome of the intervention regarding symptom reduction. The construct strongly overlaps with a number of related psychological constructs that similarly focus on an individual's beliefs about their capacity to influence outcomes in their environment and the significance of these beliefs in navigating challenges and achieving goals. These concepts are locus of control (Rotter, 1966), mastery (Pearlin and Schooler, 1978), and attribution (Weiner, 1986). Another related but distinct construct is empowerment. While both concepts involve an individual's sense of agency, empowerment involves a broader sense of control over one's life, including social, political, and economic dimensions whereas self-efficacy is more centered on personal capabilities (Cattaneo and Chapman, 2010). In this, self-efficacy is often seen as an antecedent to empowerment (Rawlett, 2014). Self-efficacy can be measured on a general level or in specific domains. General self-efficacy refers to an individual's belief in their overall ability to succeed in a wide range of situations, reflecting a broad sense of confidence in handling life's challenges. In contrast, specific self-efficacy measures relate to the confidence an individual has in specific abilities or situations. Self-efficacy is considered a dynamic construct and, accordingly, also a possible target for interventions (Bandura, 1997). The hypothesized impact of self-efficacy on therapeutic outcomes is explained by its influence on thought processes, on the extent and duration of motivation, and affective states. Low levels of perceived self-efficacy are likely to lead to avoidance, pessimistic thoughts, low motivation, a tendency to give up quickly, and weak commitment to goals. High levels of perceived self-efficacy promote an individual's commitment to change one's behavior, as well as the setting of challenging goals and a high level of effort to achieve them despite obstacles and challenges (Bandura, 1997). Given the inherent nature of IBI in fostering autonomy and self-management, it is of interest to further explore the role of self-efficacy in the context of IBI. IBI require self-efficacy-related competencies, such as taking an active role in the treatment (Domhardt et al., 2018), meeting self-imposed goals (Zarski et al., 2023), and practicing and applying psychotherapeutic techniques on their own responsibility (Sextl-Plötz et al., 2023). They also require appropriate handling of stress and frustration that may arise from a tight treatment schedule or technical difficulties (Fenski et al., 2021; Rozental et al., 2015). Individuals with high self-efficacy could therefore more effectively utilize and benefit from such autonomous and self-guided interventions due to their belief in their ability to manage their mental health independently. Concurrently, the experience of working on one's mental health problems autonomously in IBI could enhance participants' self-efficacy which then positively influences the outcome of the intervention. Thus, self-efficacy in regard to psychotherapeutic interventions can be seen as a potential treatment target (outcome), a variable that predicts or influences the magnitude or direction of the effect (predictor/moderator), as well as a mechanism of how and why change appears (mediator).
Several studies investigated the role of self-efficacy in the context of mental health. Self-efficacy beliefs are negatively associated with symptoms of mental disorders, such as depression, anxiety, and stress (Iancu et al., 2015; Tahmassian and Jalali Moghadam, 2011; Wicke et al., 2022). A review of IBI for health behavior change with 20 included studies showed that the interventions had a small positive effect of g = 0.190 on self-efficacy as an outcome (Newby et al., 2021). Samoocha et al. (2010) found in a meta-analysis that IBI have a small positive effect of a Standardized Mean Difference = 0.23 on self-efficacy measured with disease-specific self-efficacy scales (k = 9), while no effects were found for self-efficacy measured with general self-efficacy scales (k = 3). In a recent review of predictors of therapy outcome in guided IBI by Haller et al. (2023) six studies that examined self-efficacy as a predictor of outcome were identified and yielded inconsistent results. Self-efficacy is considered to be an important common factor of psychotherapy (Pfammatter and Tschacher, 2016). A recent meta-analysis on mechanisms of change in digital interventions for depression with 25 included trials (Angerer et al., 2025) identified self-related factors, including self-efficacy and perceived control (measured by the Pearlin Mastery Scale), as the most robust mediators of symptom improvement. Previous systematic reviews on mechanisms of change in IBI for depression with 26 included studies (Domhardt et al., 2021) and PTSD with 33 included studies (Steubl et al., 2021) partially supported a mediating role of cognitive variables, including self-efficacy, mastery and perceived control.
Despite the crucial role that self-efficacy may play in therapeutic change, little systematic research has been done, especially in the context of IBI. Understanding factors contributing to change in mental disorders is crucial for the development of more effective, engaging, and personalized IBI. To our knowledge, there has been no comprehensive review or meta-analysis of the role of self-efficacy in IBI for mental disorders. The aim of this review is to provide insight into the role of self-efficacy and related constructs in IBI. To provide a comprehensive analysis and to account for conceptual overlap between constructs, we include closely related constructs. Subgroup analyses tested our assumption that these constructs should be considered together. We will explore the role of self-efficacy and related constructs as an outcome, predictor or moderator, and mediator in IBI that are applied stand-alone (guided and unguided) as well as in conjunction with face-to-face therapy as blended care. Our systematic review and meta-analysis aim at answering the following questions:
-
1.
Are IBI efficacious in increasing self-efficacy and related constructs (self-efficacy as an outcome)?
-
•
1.a Does the effect remain consistent across short-, mid-, and long-term follow-up periods?
-
•
1.b Are there differences in the efficacy regarding different treatment settings, mental disorders, or control groups?
-
•
1.c Do the effects differ when considering related constructs collectively compared to self-efficacy alone?
-
2.
Are self-efficacy and related constructs predictors/moderators of treatment outcome? Do individuals with higher or lower levels of self-efficacy and related constructs benefit more or less from treatment?
-
3.
Do self-efficacy and related outcomes account for all or part of the effect of the intervention outcomes? (self-efficacy as a mediator)?
To conclude: In adults (Population), what is the effect of IBI aiming at improving symptoms of mental disorders (Intervention) on self-efficacy and related constructs (Outcome) compared with a waitlist, treatment-as-usual (TAU), and active interventions (Comparison) at post-treatment and short-, mid- and long-term follow-up? Is there evidence that self-efficacy and related outcomes act as a predictor, moderator, or mediator in IBI?
2. Methods
This review and meta-analysis was registered with PROSPERO (CRD42023405543) and is reported according to the PRISMA guidelines (Page et al., 2021). Differing from the original preregistration, we included only RCTs to elevate the quality of our findings, after it became clear that this would still result in a sufficient body of studies. No separate review study protocol was published.
2.1. Search strategy
We conducted a systematic literature search with a predefined set of search strings via the following databases: PsycINFO, PubMed/MEDLINE, CINAHL, and Web of Science. The electronic database search was completed on the 29th of April 2024 without restrictions on the publication date. In a second step, we manually searched the reference lists of all eligible studies, to identify other relevant studies. In a third step, we searched the registries ISRCTN and clinicaltrials for eligible studies. The search terms included a combination of keywords concerning treatment, setting, and key psychological constructs. Two members of the review team met with experts of the field at their respective institutions to refine the search. The predefined set of search strings optimized for each database can be found in the appendix (Table A).
2.2. Inclusion criteria
Studies published in English were eligible for inclusion if the intervention was delivered to adults. We included studies in which IBI (stand-alone, guided, unguided, or combined with face-to-face sessions) were applied to improve mental health problems, such as depression, anxiety, and stress. IBI were defined as psychological interventions delivered via digital platforms, including web-based programs, mobile applications (apps), and other online self-help tools. Synchronous teletherapy sessions conducted via video or phone calls were excluded. We included clinical samples as well as non-clinical samples. Randomized controlled trials with any kind of control group were included. Studies were eligible if they quantitively assessed (1) self-efficacy, defined as the belief in one's ability to exercise control over events that affect one's life, or over one's own mental states or to successfully perform behavior required to achieve certain results (Bandura, 1997); or related constructs including perceived control, defined as the belief in one's ability to determine one's internal states and behavior, influence one's environment, or bring about desired outcomes (Wallston et al., 1987); mastery, defined as a global feeling to have control over one's life situations (Pearlin and Schooler, 1978); or attribution, defined as an individual's causal attributions of achievement, which affects behaviors and motivation (Weiner, 1986); and (2) quantitively assessed symptoms of mental disorders (e.g., depression, stress, anxiety) through an established instrument (e.g., self-report or clinical interview).
2.3. Exclusion criteria
We excluded studies that were aimed (1) specifically at a population with somatic diseases or somatic conditions (e.g., pregnancy) and (2) at other outcomes, besides symptoms of mental health (e.g., parental skills, weight loss).
2.4. Data extraction
We conducted the study selection using the Rayyan tool (Ouzzani et al., 2016). Two reviewers (EK, JL) screened all titles and abstracts and excluded irrelevant articles. Afterward, the full texts of the remaining references were screened according to the eligibility criteria by pairs of two independent reviewers (EK, JL, SB, LMG, MP). The inter-rater reliability across all studies of the fulltext-screening resulted in a Cohen's Kappa of 0.92, which is an almost perfect agreement (Landis and Koch, 1977). Disagreements were resolved through discussion with the study lead (SB). Pairs of two independent reviewers extracted the data of the included study and discussed any differences that may have occurred (JL, EK, SB, LMG, MP). If not reported in the publication, study authors were contacted twice and asked for the missing data. We extracted study characteristics, means and standard deviations of self-reported self-efficacy and of symptoms of mental disorders at all available time points and saved them in an excel spreadsheet. When studies reported more than one outcome measure for one construct, we used the primary outcome measure defined by the study authors or, if this was unclear, the most used measure across studies.
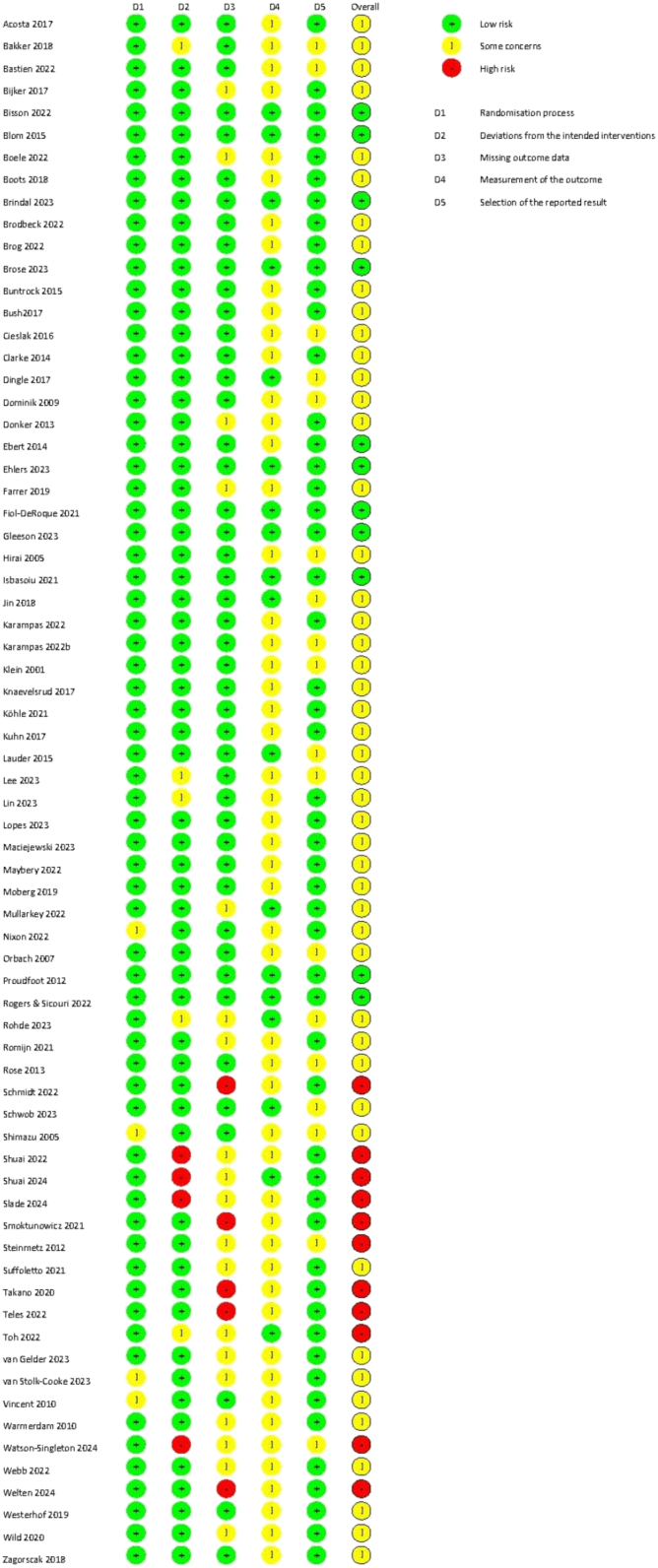
2.5. Quality assessment
We used the Cochrane Collaboration's tool for assessing risk of bias in RCTs (RoB 2.0) (Sterne et al., 2019). The methodological quality of the included studies was assessed independently by pairs of two reviewers (SB, LMG, JL, EK), who independently rated each study for bias and coded the criteria. Final assessments were crosschecked, and disagreements were resolved through discussion. We rated each study on the five domains: (1) bias arising from the randomization process, (2) bias due to deviations from intended interventions, (3) bias due to missing outcome data, (4) bias in the measurement of the outcome, (5) bias in the selection of the reported result, leading to a judgment of either “low risk of bias”, “some concerns”, or “high risk of bias”.
2.6. Data analysis
All quantitative analyses were conducted in R (RStudio Team, 2020), using the metafor (Viechtbauer, 2010), meta (Balduzzi et al., 2019), and dmetar package (Harrer et al., 2019). In this meta-analysis, we opted for a random effects model to pool effect sizes as we anticipated considerable between-study heterogeneity among the included studies based on previous work (Moshe et al., 2021; Taylor et al., 2021). Statistical heterogeneity was evaluated with the I2- and Cochran's Q-Statistics, and by visual inspection of forest plots. A p-value of the Q-statistic below 0.05 indicates heterogeneity (Cochran, 1954). I2 up to 25 % represents low, 50 % moderate and 75 % high heterogeneity (Higgins and Thompson, 2002). We addressed heterogeneous effect sizes by conducting subgroup analyses when at least three studies per subgroup were available. In studies with multiple intervention arms, we analyzed each intervention separately while using the same control group for comparison. This approach allowed us to retain distinct intervention effects and conduct more detailed subgroup analyses.
The following analysis methods were applied for the different study aims: To evaluate the effect of IBIs on self-efficacy and related constructs as outcome, we calculated uncontrolled effect sizes from pre- to post-treatment, and from pre-treatment to follow-up assessments, as well as controlled effect sizes for the difference between the IBI and the control conditions at post-treatment and follow-up assessments. Results for self-efficacy and related constructs (attribution, perceived control, and mastery) were analyzed together. Follow-up assessments were grouped into short-term (FU1, 4–23 weeks), mid-term (FU2, 24–51 weeks), and long-term (FU3, 52 and more weeks). For uncontrolled effects, the re-test correlation between time points was set at 0.5 (Borenstein, 2009). To investigate the influence of different re-test correlations sensitivity analyses were conducted for a correlation of 0.3 and 0.7. We further conducted sensitivity analyses investigating whether excluding outliers impacted effect sizes and heterogeneity. Subgroup analyses were performed for the type of assessed self-efficacy (general or specific), the type of control group, the type of guidance, and the type of disorder or population the intervention targeted. For the metanalytic pooling, disorders were grouped into mood disorders (depression and bipolar), substance abuse (including nicotine), trauma (Post-Traumatic Stress Disorder (PTSD) and grief), transdiagnostic, non-clinical (e.g. students, workers, or community samples without a formal diagnosis), and other (including stress, insomnia, and anxiety). Self-efficacy measures were grouped into general self-efficacy (including general self-efficacy, perceived control, mastery, attribution) and specific self-efficacy (e.g., mental health self-efficacy, caregiver mastery, coping self-efficacy). To test our assumption that the related constructs should be considered together, we conducted a subgroup analysis regarding only studies that applied self-efficacy measures (General: General Self-Efficacy Scale, New General Self-Efficacy Scale and the General Self-Efficacy Subscale of the Self-Efficacy Scale; Specific: e.g. Coping Self-Efficacy Scale, Mental Health Self-Efficacy Scale, Emotional Self-Efficacy). Hereafter, the term “self-efficacy” will refer to both self-efficacy and included related constructs unless specified otherwise. As for the type of control group, we categorized enhanced care and enhanced treatment as usual as TAU, and for the type of guidance, we categorized contact on demand as unguided. Publication bias was assessed by inspecting the funnel plot on the self-efficacy measures as well as calculating rank correlations and Egger's tests. Additionally, Duval and Tweedie's Trim and Fill procedure was applied (Duval and Tweedie, 2004).
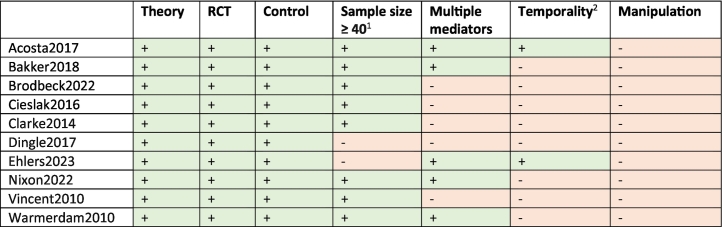
The results for self-efficacy as a predictor or moderator are synthesized narratively due to a limited number of studies and heterogenous outcomes. To determine the role of self-efficacy as a mediator in IBI, we aggregated the reported statistical significance in the primary studies following a box score approach with the three categories yes, mixed, and no for those studies that performed a mediator analysis with a self-efficacy measure. In these, we aggregated the results as subgroup-analyses when three or more studies were available. We extracted a measure of explained variance (R2) wherever possible as recommended by the Cochrane Handbook (Higgins et al., 2011). Given the large heterogeneity of the studies, this can only serve as a rough estimate. Additionally, we rated mediation studies in reference to their quality applying the criteria originally proposed by Kazdin (2007), which were adapted to psychotherapy research by Lemmens et al. (2016) and have been utilized in IBI research (Domhardt et al., 2021; Steubl et al., 2021). The criteria are rated as fulfilled (+) or not fulfilled (−) and include: (1) a theoretical foundation, (2) RCT as the study design, (3) inclusion of a control group, (4) a sample size of at least 40 per group, (5) the inclusion of multiple mediators, (6) evaluation of temporality (two or more assessments of mediators and outcome variables during the treatment phase), and (7) the direct experimental manipulation of the mediator. Given the significant heterogeneity among the included studies, alongside varied analyses and outcome measures, pooling effect sizes from the mediator studies was not feasible.
2.7. Data availability
All data for this project, including the data extraction sheet and relevant R code, have been made publicly available and can be accessed at: https://osf.io/5qz4e/?view_only=2b6c48d99ca448fba9b6ab7e9731ef25.
3. Results
3.1. Study characteristics
The systematic database search yielded 5676 initial hits. Two additional records were identified through backward search, three studies were identified through clinical trial registries, and four studies were sent to us directly by the authors. After screening of titles and abstracts, 244 studies were assessed for eligibility in full-text review. Of those, 70 studies met the criteria for inclusion. The corresponding flow chart is presented in Fig. 1. The included studies were published between 2001 and 2024. Half of the studies were carried out in Europe (k = 35; 50.00 %). Regarding the other half, most were conducted in North America (k = 18; 25.71 %) and Australia (k = 12; 17.14 %), while the remaining were conducted in Asia (k = 4; 5.71 %) and South America (k = 1; 1.43 %). In total, N = 17,407 participants were included in this review. Sample sizes ranged between 21 and 2304 participants, with a mean sample size of n = 248 participants (SD = 349).
Fig. 1.
PRISMA flow chart.
Regarding the sample's characteristics, the mean percentage of women was 70.72 % (SD = 17.49) and the mean age of participants ranged from 18.7 to 71.4 (M = 38.25; SD = 12.39). Most of the included studies assessed an Internet-based intervention (k = 59; 84.29 %) while the remaining evaluated a mobile app-based intervention (k = 9; 12.86 %), a Chat-Bot (k = 1; 1.43 %) or an ecological momentary intervention (k = 1; 1.43 %). Regarding the treatment setting, most of the included studies evaluated unguided interventions (k = 44; 62.86 %), about one third evaluated guided interventions (k = 19; 27.14 %), a small proportion focused on blended approaches (k = 5; 7.14 %) and two studies investigated multiple treatment groups with both guided and unguided interventions (k = 2; 2.86 %). Most of the included studies compared IBI against an active control condition (k = 29; 41.43 %) or a waiting list (k = 26; 37.14 %). The remaining studies compared IBI against (enhanced) TAU (k = 15; 21.43 %). Three studies included two control conditions. In one of them, it was two active control conditions, in another, it was an active condition and waiting list and in the third, it was an active condition and TAU. Regarding the type of population and symptomatology evaluated in the included studies, 17 studies (24.29 %) examined non-clinical samples (e.g., students, workers, community samples), evaluating mainly anxious, depressive and/or stress symptomatology. Eight studies (11.43 %) focused specifically on non-professional caregivers or relatives of individuals with somatic or mental disorders. The majority of studies focused on clinical populations with mood disorders (k = 12; 17.14 %), trauma or grief symptoms (k = 9; 12.86 %), transdiagnostic symptoms (k = 7; 10 %), substance abuse problems (k = 6; 8.57 %) and anxiety disorders (k = 5; 7.14 %). Other studies (k = 6; 8.57 %) focused on elevated stress symptoms, insomnia, or suicidal ideation. The majority of assessed interventions are based on a CBT approach (including Acceptance and Commitment Therapy, Dialectical Behavior Therapy, Problem Solving, and Stress Management) or on CBT combined with other approaches (e.g., Mindfulness, Self-compassion, Positive Psychology) (k = 48; 68.57 %). Few interventions were based on Psychoeducation (k = 4; 5.71 %). Other studies investigated interventions based on other or mixed approaches (e.g., interpersonal therapy, narrative therapy, resilience, emotion regulation through music; k = 20; 28.57 %). Two studies (2.86 %) did not specify the approach on which the applied intervention was based. The duration of the intervention ranged from a single 45-min session to 52 weeks. A detailed overview of the studies characteristics is outlined in Table 1.
Table 1.
Study Characteristics.
| Authors / Year / Country | Sample N, mean age, % female |
Population and assessed symptoms | Intervention(s) description (setting, duration, approach) | Control group(s) | Self-Efficacy measure | Role of self-efficacy in the study | Assessment times | Attrition |
|---|---|---|---|---|---|---|---|---|
| Acosta et al., 2017 / United States | 162 (81 IG, 81 CG), 32, 7 % | Veterans; Substance abuse and Trauma | Unguided, 12 weeks, CBT | TAU: Medical, behavioral health, pharmacy, weight management, and social work services. |
Brief Situational Confidence Questionnaire (BSCQ) | Mediator | pre, 4w, 8w, post, 16wFU, 24wFU | IG: 32.1 % CG: 14.8 % |
| Bakker et al., 2018/ Australia | 312 (78 IG1, 78 IG2, 78 IG3, 78 CG), 34.2, 81 % | Non-clinical sample; Depression and Anxiety | IG1: Unguided, 4 weeks, CBT IG2: Unguided, 4 weeks, CBT IG3: Unguided, 4 weeks, CBT |
WL | Coping Self-Efficacy Scale (CSES) | Mediator | pre, post | IG1: 50 % IG2: 66,7 % IG3: 70,5 % CG: 32,1 % |
| Bastien et al., 2022 / Canada | 217 (69 IG1, 73 IG2, 75 CG), 20.44, 78.8 % | Non-clinical sample of university students; Stress | IG1: Unguided, 4 weeks, mental health resilience-building (provider–presented) IG2: Unguided, 4 weeks, mental health resilience-building (peer–presented) |
WL | Coping Self-efficacy Scale (CSES) | Outcome | pre, post, 10wFU | IG1: 12.2 % IG2: 12.2 % CG: 8.9 % |
| Bijker et al., 2017 / Netherlands | 80 (41 IG, 39 CG), 49.9, 77.45 % | Caregivers of depressed patients; assessment of GAD | Guided, 6 weeks, CBT | WL | Pearlin Mastery Scale (PMS) | Outcome | pre, post | IG: 34.1 % CG: 12.8 % |
| Bisson et al., 2022 / United Kingdom | 196 (99 IG, 97 CG), 36.5, 63.8 % | Trauma | Blended, 8 weeks, CBT | AC: up to 12 f2f sessions individual CBT | General Self-Efficacy Scale (GSES) | Outcome | pre, post, 52wFU | IG: 20.6 % CG: 16.2 % |
| Blom et al., 2015 / Netherlands | 245 (149 IG, 96 CG), 61.2, 69.4 % | Caregivers of people with dementia; Depression and Anxiety | Guided, 24 weeks, CBT | AC: minimal intervention consisting of e-bulletins | Pearlin Mastery Scale (PMS; abbreviated 5-item version) | Outcome | pre, post | IG: 39.6 % CG: 11.5 % |
| Boele et al., 2022 / United Kingdom | 120 (40 IG1, 40 IG2, 40 CG), 52.2, 70.7 % | Caregivers of adult cancer patients; Depression | IG1: Guided, 8 weeks, Representational Approach IG2: Guided, 8 weeks, CBT |
Enhanced care as usual (ECAU): attention-control emails every 2 weeks, and access to a psychoeducational webpage | Mastery Scale | Outcome | pre, 8wFU, 16wFU | IG: 36 % CG: 13 % |
| Boots et al., 2018 / Netherlands | 81 (41 IG, 40 CG), 69, 65.4 % | Caregivers of People with Early-Stage Dementia; Stress, Depression and Anxiety | Blended, 8 weeks, CBT-SM | TAU: Waitlist receiving usual care consisting of nonfrequent counseling | Caregiver Self-Efficacy Scale (CSES) |
Outcome | pre, post | IG: 24.39 % CG: 7.5 % |
| Brindal et al., 2023 / Australia | 166 (81 IG, 85 CG), 38.48, 67.5 % | Healthy adults aged 25 to 50 years; Stress | Unguided, 4 weeks, Conservation of Resource theory |
AC: Mood monitoring | Coping Self-Efficacy Scale (CSE) | Outcome | Pre, 2w, post | IG: 23.46 % CG: 25.88 % |
| Brodbeck et al., 2022 / Switzerland | 110 (69 IG, 41 CG), 51.11, 69 % | Prolonged grief | Guided, 23 weeks, Dual Process Model of Coping | WL | 3 Self-developed items | Mediator | pre, post | IG: 34.1 % CG: 12.8 % |
| Brog et al., 2022b / Switzerland | 107 (53 IG, 54 CG), 40.36, 81.3 % | Depression | Unguided, 3 weeks, CBT | TAU: can range from no treatment at all to psychotherapy and/or drug therapy | General Self-Efficacy Scale (GSE) | Outcome | pre, post, 6wFU (only IG) | IG: 15.1 % CG: 3.7 % |
| Brose et al., 2023 / Germany | 2304 (1113 IG, 1191 CG), 42.3, 59.2 % | Depression | Guided, 6 weeks, CBT | AC: The same intervention with a different order of modules | General Self-Efficacy Scale (GSE) | Outcome | pre, post, 12wFU, 24wFU, 52wFU | IG: 27 % CG: 26 % |
| Buntrock et al., 2015 / Germany | 406 (202 IG, 204 CG), 45, 73.9 % | Depression | Guided, 3-6 weeks, CBT | eTAU: care-as-usual + a web-based psycho-educational intervention | Pearlin Mastery Scale (PMS) | Outcome | pre, post, 24wFU | IG: 9.9 % CG: 9.9 % |
| Bush et al., 2017 / United States | 118 (58 IG, 60 CG), 47.59, 31.5 % | Veterans; Suicidal ideation | Blended, 12-weeks, CBT | eTAU: active mental health treatment + printed materials about coping with suicidality | Coping Self-Efficacy Scale (CSE) | Outcome | pre, 3w, 6w, 12w | IG: 9.9 % CG: 9.9 % |
| Cieslak et al., 2016 / Poland | 168 (87 IG, 81 CG), 37.49, 78 % | Health and human services professionals; Trauma | Contact on demand, 4 weeks, CBT | AC: read-only educational materials | Secondary Trauma Self-Efficacy Scale (STSE) | Outcome; Mediator |
pre, post, 4wFU | IG: 52.87 % CG: 49.38 % |
| Clarke et al., 2014 / Australia | 720 (242 IG, 248 CG1, 230 CG2), 38.9, 69.6 % | Mild-to severe symptoms of Depression, Anxiety and/or Stress | Unguided, 7 weeks, CBT + Interpersonal Psychotherapy+Problem-solving Therapy+Positive Psychology | CG1: AC - fact sheet of information about depression, anxiety or stress via email + weekly SMS with brief factual statements CG2: WL |
Mental Health Self-Efficacy Scale (MHSES) | Mediator; Moderator |
pre, 7 post, 19 FU | IG: 47.9 % CG1: 21.4 % CG2: 13.9 % |
| Dingle and Carter, 2017 / Australia | 55 (19 IG1, 18 IG2, 18 CG), 40.61, 45 % | Substance abuse | IG1: Guided, 6 weeks, Emotion Regulation through Music IG2: Guided, 6 weeks, CBT |
TAU: Telephone CBT program without IBI | Three self-report questions | Outcome; Mediator |
pre, post | IG1: 42.11 % IG2: 22.2 % CG: 27.78 % |
| Dominick et al., 2009 / United States | 67 (33 IG, 34 CG), 47, 86.6 % | Recently bereaved; Grief | Unguided, 1 week, Psychoeducation | TAU: usual care | 3 items to assess self-efficacy | Outcome | pre, post | IG: 0 % CG: 0 % |
| Donker et al., 2013 / Australia & Netherlands | 1843 (620 IG1, 610 IG2, 613 CG), N.I., 72.4 % | Non-clinical sample; Depression and Anxiety | IG1: Unguided, 4 weeks, Interpersonal therapy IG2: Unguided, 4 week, CBT |
AC: short-version CBT-based IBI | Pearlin Mastery Scale (PMS) | Predictor; Moderator |
pre, 4 post, 28 FU | IG1: 66.8 % IG2: 70.3 % CG: 73.6 % |
| Ebert et al., 2014 / | 150 (75 IG, 75 CG), 47.1, 83.3 % | Teachers; Depression | Guided, 4 weeks, Problem solving training | WL | General Self-Efficacy Scale (GSE) | Outcome | pre, post, 12wFU, 24wFU | IG: 14.66 % CG: 8 % |
| Ehlers et al., 2023 / United Kingdom | 217 (92 IG1, 93 IG2, 32 CG), 36.36 73 % | Trauma | IG1: Guided, 13 weeks (26 incl. Booster phase), CBT IG2: Guided, 13 weeks (26 incl. Booster phase), Stress management |
WL: Waiting list with usual clinical care | General Self-Efficacy Scale (GSES) | Mediator | pre, 6w, 13w (post), 26w, 39w, and 65w | IG1: 5.43 % IG2: 1.08 % CG: 3.13 % |
| Farrer et al., 2019 / Australia | 200 (102 IG, 98 CG), 22.10, 77.5 % | University students with clinically significant mental distress; Depression, GAD, SAD and psychological distress | Contact on demand, 6 weeks, CBT + mindfulness | WL | General Self Efficacy (GSE-10); College Self-Efficacy Inventory (CSEI) | Outcome | pre, post, 18wFU | IG: 39.2 % CG: 16.3 % |
| Fiol-DeRoque et al., 2021 / Spain | 482 (248 IG, 234 CG), 41.37, 83.2 % | Health care providers of COVID-19 patients; Depression, Anxiety, Stress | Unguided, 2 weeks, CBT + mindfulness | AC: App with brief information about the mental health care of health care workers during COVID-19 | General self-efficacy scale (GSE) | Outcome | pre, post | IG: 10.9 % CG: 8.1 % |
| Gleeson et al., 2023 / Australia | 164 (82 IG, 82 CG), 51.04, 75 % | Family carers of first-episode psychosis patients; Stress | Guided, 52 weeks, Psychoeducational family intervention | eTAU: Specialized treatment as usual | Parental Self-Efficacy (Me as a Parent, MaaP) | Outcome | pre, 24w, post | IG: 25.61 % CG: 18.29 % |
| Hirai and Clum, 2005 / United States | 27 (13 IG, 14 CG), 20.40, 77.8 % | Individuals who had experienced a traumatic event: Trauma, Anxiety and Depression |
Unguided, 8 weeks, CBT | WL | Self-Efficacy Scale (SES); General self-efficacy subscale of the Active coping With Trauma Scale (ACTS) | Outcome | pre, post | IG: 27.8 % CG: 22.2 % |
| Isbăşoiu et al., 2021 / Romania | 284 (142 IG, 142 CG), 33.2, 84.5 % | Depression and/or Anxiety | Guided, 9 weeks, Unified Protocol with added self-enhancement strategies | AC: guided IBI, standard Unified Protocol | New General Self-Efficacy Scale (NGSE) | Outcome | pre, post, 33wFU | IG: 45.1 % CG: 45.8 % |
| Jin, 2017 / United States | 21 (11 IG, 10 CG), 20.14, 42.9 % | Asian international students in the US; Depression | Unguided, 7 weeks, CBT + Interpersonal Psychotherapy+Problem-solving Therapy+Positive Psychology with culturally tailored messages | AC: IBI based on CBT + Interpersonal Psychotherapy+Problem-solving Therapy+Positive Psychology without culturally tailored messages | Mental Health Self-Efficacy Scale (MHSES) | Outcome | pre, 3w, post | IG: 36.4 % CG: 40 % |
| Karampas, Pezirkianidis and Stalikas, 2022a, Karampas, Pezirkianidis and Stalikas, 2022b/ Greece | 26 (12 IG, 14 CG), 24.46, 96.2 % | Non-clinical sample of undergraduate Psychology students; Depression, Anxiety and Stress | Unguided, 5 weeks, CBT + ACT | WL | Perceived Stress Scale (PSS): Self-efficacy against stress | Outcome | pre, post, 17wFU | IG: 0 % CG: 0 % |
| Karampas et al., 2022b / Greece | 35 (17 IG, 18 CG), 22.68, 91.7 % | Non-clinical sample of undergraduate psychology students; Depression, Anxiety and Stress | Unguided, 5 weeks, CBT + ACT | WL | Perceived Stress Scale (PSS): Self-efficacy against stress | Outcome | pre, post | N.I. |
| Klein and Richards, 2001 / Australia | 23 (11 IG, 12 CG), 43, 86.36 % | Panic disorder | Unguided, 1 week, CBT | AC: Self-monitoring | Self Efficacy Questionnaire composed by six pairs of statements. | Outcome | pre, post | N.I. |
| Knaevelsrud et al., 2017 / Germany | 94 (47 IG, 47 CG), 71.4, 64.9 % | World War II survivors; Trauma | Guided, 6 weeks, CBT | WL | General Self-efficacy Scale (GSES) | Outcome | pre, post, 12wFU, 24wFU, 48wFU | IG: 12.8 % CG: 6.4 % |
| Köhle et al., 2021/ Netherlands | 103 (67 IG1, 60 IG2, 66 CG.), 55.89, 70.4 % | Partners of cancer patients/survivors; Anxiety and Depression | IG1: Guided, 6-12 weeks, ACT+Self-compassion IG2: Unguided, 6-12 weeks, ACT+Self-compassion |
WL | Pearlin Mastery Scale (PMS - abbreviated 5-item version) | Outcome | pre, post | IG1: 28.36 % IG2: 44.29 % CG: 21.21 % |
| Kuhn et al., 2017 / United States | 120 (62 IG, 58 CG), 39, 69.2 % | Trauma | Unguided, 12 weeks, CBT | WL | 9-item self-report measure developed for the study: PTSD symptom coping self-efficacy | Outcome | pre, post, 24wFU | IG: 17.7 % CG: 10.3 % |
| Lauder et al., 2015 / Australia | 129 (71 IG, 58 CG), 40.61, 74,5 % | Bipolar I & II | Unguided, 10 weeks, CBT | AC: unguided IBI, Psychoeducation | Levenson's Internal, Powerful Others and Chance Locus of Control scale | Outcome | pre, post, 24wFU, 52wFU | IG: 64.79 % CG: 47.46 % |
| Lee et al., 2023 / United States | 131 (66 IG, 65 CG), NI, 80.9 % | Non-clinical sample of college students; Depression, Anxiety and Stress | Unguided, 45-min single session, DBT-informed stress and anxiety management | WL | Anxiety Self-Efficacy (ASE): 2-item self-report measure created for the study | Outcome | pre, post | IG: 24.67 % CG: 27.3 % |
| Lin et al., 2023 / China | 84 (40 IG, 44 CG), 30.82, 62 % | Depression | Unguided, 8 weeks, CBT | WL | General Self-Efficacy Scale (GSES) | Outcome | pre, post | IG: 7.5 % CG: 2.27 % |
| Lopes et al., 2023 / Brazil | 189 (94 IG, 95 CG), 36.44, 79 % | Depression | Unguided, 13 weeks, CBT | TAU: other psychological or psychopharmaco-logical treatments | General Self-Efficacy Scale (GSES) | Outcome | pre, post | IG: 53.19 % CG: 30.53 % |
| Maciejewski and Smoktunowicz, 2023 / Poland | 372 (186 IG, 186 CG), 20.98, 85 % | Non-clinical sample of university students; Stress | Unguided, chatbot, 1 week, Conservation of Resources theory | WL | Coping Self-Efficacy Scale (CSES) | Outcome | pre, post, 4wFU | IG: 47.31 % CG: 21.51 % |
| Maybery et al., 2022 / Australia | 41 (22 IG, 19 CG), 21.83, 92.7 % | Young adults with parents with a mental illness; Depression, Anxiety, and Stress | Guided, 6 weeks, CBT | WL | General Self-efficacy Scale (GSES) | Outcome | pre, post, 6wFU | IG: 8.33 % CG: 4.76 % |
| Moberg et al., 2019 / United States | 500 (253 IG, 247 CG), 30.2, 75 % | Depression and Anxiety | Unguided, 4 weeks, CBT + mindfulness | WL | General Self-efficacy Scale (GSES) | Outcome | pre, post, 12wFU | IG: 68.8 % CG: 59.1 % |
| Mullarkey et al., 2022 / United States | 522 (261 IG, 261 CG), 46.11, 48.5 % | GAD | Unguided, 1 single session, NI | AC: 1 single session containing scientific information about how soap kills the SARS-CoV-2 |
Anxiety Control Questionnaire-Emotion Control (ACQ-EC) | Outcome | pre, post, 2wFU | IG: 6.9 % CG: 9.6 % |
| Nixon et al., 2022 / Germany | 262 (130 IG, 132 CG), 42.20, 69.5 % | Stress | Contact-on-demand, 4-7 weeks, Stress management and problem solving training | WL | Occupational Self-efficacy Scale (OSS-SF) | Mediator | pre, post | IG: 12 % CG: 8 % |
| Orbach et al., 2007 / United Kingdom | 90 (47 IG, 43 CG), 23.63, 73 % | College students; Test anxiety | Unguided, 6 weeks, CBT | AC: IBI with relaxation, diary, and puzzles | General Self-efficacy Scale (GSES) | Outcome | pre, post, 16wFU | IG: 27.66 % CG: 34.88 % |
| Proudfoot et al., 2012 / Australia | 407 (139 IG1, 134 IG2, 134 CG), NI, 69 % | Bipolar Disorder | IG1: Unguided, 8 weeks, Psychoeducation IG2: Guided (peer support), 8 weeks, Psychoeducation |
AC: weekly emails containing links to simple information about bipolar disorder | Health Locus of Control (MHLC) | Outcome | pre, post, 20Wfu, 32wFU | IG1: 38.3 % IG2: 35.3 % CG: 35.3 % |
| Rogers and Sicouri, 2022 / Australia | 45 (23 IG, 22 CG), 19.67, 55 % | College students with mild symptoms of Anxiety, Stress or Depression | Unguided, 1 single session, CBT | AC: online session without CBT elements | Attribution Style Questionnaire (ASQ) | Outcome | pre, post, 1wFU | IG: 0 % CG: 4.5 % |
| Rohde et al., 2023 / Switzerland | 93 (54 IG, 39 CG), 23.72, 78.49 % | College students; Stress | Unguided, 1 week, Ecological momentary intervention training self-efficacy | WL | General Self-efficacy Scale (GSES) | Outcome | pre, post | IG: 11.48 % CG: 15.22 % |
| Romijn et al., 2021 / Netherlands | 114 (52 IG, 62 CG), 36.3, 60.5 % | Panic disorder (with or without agoraphobia), SAD and GAD | Blended, 15 weeks, CBT | TAU: f2f sessions with standard disorder specific CBT | Mastery Scale (5-item version) | Outcome | pre, 7w, post, 52wFU | IG: 34.62 % CG: 30.65 % |
| Rose et al., 2013 / United States | 66 (34 IG, 32 CG), 27.32, 50 % | Graduate students; Stress | Unguided, 6 weeks, CBT (Stress management training) | AC: 6 weekly sessions where they receive material on stress and stress management | Stress and Perception of Control Scale | Outcome | pre, post | IG: 11.76 % CG: 9.38 % |
| Schmidt et al., 2022 / Germany | 59 (30 IG, 28 CG), 44.47, 86 % | Prolonged grief | Guided, 5 weeks, CBT | WL | General Self-Efficacy Scale (GSES) | Predictor | pre, post | IG: 13.33 % CG: 3.57 % |
| Schwob and Newman, 2023 / United States | 82 (39 IG, 43 CG), 19.40, 53.65 % | Social Anxiety | Unguided, 1 week, CBT | AC: Self-monitoring | General Self-Efficacy Scale (GSES) | Outcome | pre, post, 4wFU | IG: 2.54 % CG: 4.65 % |
| Shimazu et al., 2005 / Japan | 225 (112 IG, 113 CG), 42.95, 16.91 % | Non-clinical sample of workers; Stress | Unguided, 4 weeks, Psychoeducation | WL | Self-efficacy scale (17 items | Outcome | pre, post, 6wFU | IG: 8.26 % CG: 5.45 % |
| Shuai et al., 2022 / United Kingdom | 52 (24 IG, 28 CG), 42.95, 16.91 % | Students; Alcohol use disorder | Unguided, 2 weeks, functional imagery training | AC: PowerPoint Video containing binge drinking risk information | Controlled Drinking Self-Efficacy Scale | Outcome | pre, post | IG: 36.8 % CG: 26.3 % |
| Shuai et al., 2024 / United Kingdom | 120 (59 IG, 61 CG), | Students in South Africa; Alcohol use disorder | Unguided, 2 weeks, functional imagery training | AC: PowerPoint Video containing binge drinking risk information | Controlled Drinking Self-Efficacy Scale | Outcome | pre, post | IG: 32.43 % CG: 21.87 % |
| Slade et al.* /, 2024 / United Kingdom | 1023 (507 IG, 516 CG), 38.4, 79.3 % | Depression, Anxiety, Stress | Unguided, NI, Recorded recovery narratives | TAU: usual care | Mental Health Confidence Scale | Outcome | pre, 1w, 12w, 52w (post) | |
| Smoktunowicz et al., 2021/ Poland | 1240 (311 IG1, 311 IG2, 309 CG1, 309 CG2), 36.2, 86.61 % | Non-clinical sample of medical professionals; Depression, Job related traumatic stress, Job burnout and Job stress | IG1: Unguided, 6 weeks, self-efficacy and social support sequential enhancement IG2: Unguided, 6 weeks, social support and self-efficacy sequential enhancement |
AC (CG1): unguided IBI with self-efficacy enhancement AC (CG2): unguided IBI with social support enhancement |
Work Stress and Job Burnout Self-Efficacy Scale | Outcome | pre, post, 30wFU | IG1: 89.3 % IG2: 83.6 % CG1: 77.7 % CG2: 79 % |
| Steinmetz et al., 2012 / United States | 56 (18 IG, 19 CG1, 19, CG2), 43, 85.7 % | Hurricane Ike survivors; Depression, Stress and Trauma | Unguided, 4 weeks, Social Cognitive Theory and Human Agency | AC (CG1): Information-only intervention TAU (CG2) |
Coping Self-Efficacy Scale for Trauma (CSE) | Outcome | pre, post | IG: 22 % CG1: 32 % CG2: 5.3 % |
| Suffoletto et al., 2021 / United States | 52 (34 IG, 18 CG), 18.7, 85 % | Young adults with a current mental health diagnosis; Anxiety and Depression | Unguided, 12 weeks, positive psychology+CBT + DBT | eTAU: TAU + web link with psychoeducational videos | Mental Health Self-Efficacy Scale (MHSES) | Outcome | pre, 4w, 8w, 12w (post) | IG: 5.9 % CG: 5.6 % |
| Takano et al., 2020 / Japan | 48 (23 IG, 25 CG), 38.25, 31.55 % | Substance abuse | Guided, 8 weeks, NI | AC: limited content of the IG IBI | Self-efficacy Scale for Drug Dependence (SSDD) | Outcome | pre, post, 20wFU, 32wFU | IG: 17.4 % CG: 4 % |
| Teles et al., 2022 / Portugal | 42 (21 IG, 21 CG), 53.6, 78.6 % | Caregivers of people with dementia; Depression and Anxiety | Unguided, 12 weeks, CBT + problem solving | AC: education-only ebook | Self-efficacy Scale for Drug Dependence (SSDD) | Outcome | pre, post, 36wFU | IG: 28.6 % CG: 4.8 % |
| Toh et al., 2022 / Singapore | 321 (162 IG, 159 CG), 22.5, 71.2 % | Undergraduate university students; Depression, Anxiety and Stress | Unguided, 1 week, CBT | AC: Psychoeducation IBI | Coping Self-Efficacy Scale (CSES) | Moderator | pre, post, 5wFU | IG: 1.9 % CG: 3.1 % |
| van Gelder et al., 2023 / Netherlands | 198 (99 IG, 99 CG), 35, 100 % | Women experiencing Intimate Partner Violence and Abuse; Anxiety, Depression | Unguided, 4modules, NI | AC: minimal intervention with only the most essential static information |
General Self-Efficacy Scale (GSES) | Outcome | pre, 12w, post, 52wFU | IG: 0 % CG: 2.02 % |
| van Stolk-Cooke et al., 2023 / United States | 200 (104 IG, 96 CG), 39, 97 % | Veteran Family Members; Stress | Unguided, 4 weeks, CBT | AC: the psychoedu-cation and support resources from PTSD Family Coach 1.0 | Partner Self-Efficacy scale (PSE) | Outcome | pre, post | IG: 33.65 % CG: 43.75 % |
| Vincent et al., 2010 / Canada | 118 (59 IG, 59 CG), 51.1, 71 % | Insomnia | Unguided, 5 weeks, CBT | WL | Sleep Locus of Control Scale (SLOC) | Mediator | pre, post, 4wFU | IG: 24.6 % CG: 24.6 % |
| Watson-Singleton and Pennefather* / 2024 / United States | 212 (106 IG, 106 CG), 36.06, 54,1 % | Non-clinical sample of Black/African American individuals; Stress, Depression, and Anxiety | Unguided, 12 weeks, Mindfulness | WL | Mindfulness Self Efficacy Scale (MSES) | Outcome | pre, post | IG: 20.75 % CG: 18.87 |
| Warmerdam et al., 2010 / Netherlands | 263 (88 IG1, 88 IG2, 87 CG), 45, 71 % | Depression | IG1: Guided, 8 weeks, CBT IG2: Guided, 5 weeks, problem-solving therapy |
WL | Pearlin Mastery Scale (PMS) | Mediator | pre, post, 8wFU | IG1: 19.32 % IG2: 29.55 % CG: 18.39 % |
| Webb et al., 2022 / United States | 556 (277 IG, 279 CG), 41, 45.1 % | Non-clinical sample; Tobacco use | Guided, 52 weeks, CBT | AC: A very brief advice (VBA) to stop smoking, an evidence-based intervention designed to facilitate quit attempts + referral to a cessation service | Smoking Abstinence Self-Efficacy Questionnaire | Outcome | pre, post, 26wFU, 52wFU | IG: 15 % CG: 13 % |
| Welten et al., 2024 / Netherlands | 120 (59 IG, 61 CG), 59.3, 74.2 % | Partners of patients with aquired brain injury; Stress, Depression, and Anxiety | Blended, 20 weeks, CBT | TAU: education and counseling tailored to individual needs. This could involve individual consultation(s) with a social worker or psychologist, or a peer support group. | Caregiver Mastery Scale (CMS) | Outcome | pre, post, 40wFU | IG: 28.81 % CG: 18.03 % |
| Westerhof et al., 2019 / Netherlands | 58 (19 IG1, 20 IG2, 19 CG), 53.8, 77.6 % | Sub-clinical sample of 40 years or older; Depression | IG1: Guided, 12 weeks, Narrative therapy IG2: Guided (peer support), 12 weeks, Narrative therapy |
WL | Pearlin Mastery Scale (PMS) | Outcome | pre, post, 24wFU, 48wFU | IG1: 31.6 % IG2: 30 % CG: 38.8 % |
| Wild et al., 2020 / United Kingdom | 430 (317 IG, 113 CG), 41.4, 58.1 % | Non-clinical sample of emergency workers; Depression, Anxiety, and Trauma | IG: Unguided, 6 weeks, Psychoeducation+mindfulness | AC: f2f sessions in group format | General Self-Efficacy Scale (GSES) | Outcome | pre, post, 18wFU | IG: 18.6 % CG: 19.2 % |
| Zagorscak et al., 2018 / Germany | 1089 (555 IG, 534 CG), 45.7, 65.6 % | Depression | Guided, 6 weeks, CBT | AC: Contact on Demand version of the same intervention | General Self-Efficacy Scale (GSE) | Outcome | pre, post, 12wFU, 24wFU, 52wFU | IG: 18.40 % CG: 21.20 % |
Note: *included in the meta-analytic pooling; 1In the original study, experimental and control group are reversed; AC: Active Control; ACT: Acceptance and Commitment Therapy; CBT: Cognitive Behavioral Therapy; CBT-SM: Cognitive Behavioral Therapy - Self-Management; CG: Control Group; DBT: Dialectical Behavior Therapy; f2f: face-to-face; FU: Follow Up; GAD: Generalized Anxiety Disorder; IG: Intervention Group; NI: No Information; PTSD: Post Traumatic Stress Disorder; SAD: Social Anxiety Disorder; (e)TAU: (enhanced) treatment as usual; w: weeks; WL: Waitlist.
For the meta-analytic analysis of self-efficacy as an outcome, we excluded 14 studies because the data was not available or because self-efficacy was not assessed at post-measurement time points, which resulted in a total N = 10,297 individuals in 56 publications for the meta-analytic calculations.
3.2. Risk of bias assessment
An overview of the results of the risk of bias assessments is provided in Fig. 2. In summary, the quality of the included studies can be considered satisfactory, with 59 studies (84.29 %) having low or moderate overall risk of bias. The domains with the lowest risk of bias across studies were the “randomization process” and “selection of the reported result”, whereas the criteria least met were “missing outcome data” and “measurement of the outcome”.
Fig. 2.
Risk of bias assessment.
3.3. Role of self-efficacy
3.3.1. Self-efficacy as an outcome
Our meta-analysis reviewed 67 comparisons from 56 publications focusing on the effect of IBI on self-efficacy compared to various controls.
Table 2 shows the between effect sizes and heterogeneity (Q-statistic, I2) for the overall and subgroup analyses from post-assessment, short-, mid-, and long-term follow-up for IBI on self-efficacy compared to control groups. The forest plot (Fig. 3) additionally visualizes the effect sizes and confidence intervals comparing IBI with the different settings to control groups. The overall comparison of IBI with control groups at post assessment yielded a moderate effect on self-efficacy (k = 67, d = 0.46, 95 % CI = 0.27–0.65) with high heterogeneity between studies (I2 = 95.13 %, Q = 504.72). There was a large effect on general self-efficacy (k = 29, d = 0.75, CI = 0.31–1.20) and a small effect on specific self-efficacy (k = 38, d = 0.21, CI = 0.12–0.30). The heterogeneity for general self-efficacy was very high (I2 = 98.05 %, Q = 416.17) while it was moderate (I2 = 48.1 %, Q = 81.01) for specific self-efficacy. We conducted subgroup analyses without related constructs, which yielded similar patterns in effects and heterogeneity (general: k = 20, d = 0.65, CI = 0.06–1.23, I2 = 98.58 %, Q = 288.52; specific: k = 30, d = 0.20, CI = 0.00–0.10, I2 = 53,12 %, Q = 73.40). The overall effect decreased in the follow-up assessments leading to non-significant effects in the short- and long-term follow-ups (FU1: k = 13, d = 0.16, 95 % CI = −0.00 - 0.33; FU3: k = 6, d = 0.12, 95 % CI = −0.09 - 0.33) and a small effect in the mid -term follow-up (FU2: k = 14, d = 0.16, 95 % CI = 0.03–0.29). All effect sizes reported for the subgroup analyses in the next section refer to post-assessment results. Follow-up results can be found in Table 2. In a subgroup of 28 studies comparing IBI to waitlist controls, a moderate effect was observed (d = 0.64, 95 % CI = 0.40–0.89). However, the heterogeneity remained high (I2 = 89.53 %), suggesting variability in the effect sizes within this subgroup. No significant advantage was found for IBI compared to TAU (k = 15, d = 0.66, 95 % CI = −0.08–1.39), and active controls (k = 24, d = 0.10, 95 % CI = −0.03 - 0.23). Guided interventions showed higher effect sizes (k = 19, d = 0.61, 95 % CI = 0.24–0.97) than unguided (k = 44, d = 0.42, 95 % CI = 0.17–0.68) and blended approaches (k = 4, d = 0.19. 95 % CI = −0.15 - 0.52). As for what kind of symptoms or populations the interventions targeted, there was a large effect for interventions targeting mood disorders (k = 11, d = 1.17, 95 % CI = 0.09–2.26), moderate effects for IBI targeting caregivers of relatives (k = 8, d = 0.68, 95 % CI = 0.08–1.29) and for interventions targeting trauma and grief (k = 9, d = 0.64, 95 % CI = 0.16–1.12). A small effect was found for interventions aiming at non-clinical populations (k = 20, d = 0.14, 95 % CI = 0.06–0.23) and other symptoms (e.g., stress and insomnia; k = 9, d = 0.37, 95 % CI = 0.18–0.56). Non-significant effects were found for transdiagnostic interventions (k = 5, d = 0.33, 95 % CI = −0.03 - 0.69), and interventions aiming at substance abuse (k = 5, d = 0.03, 95 % CI = -0.38–0.45). Removing outliers in the sensitivity analyses (Appendix Table D) lowered heterogeneity and showed overall smaller effect sizes (k = 55, d = 0.29, 95 % CI = 0.22–0.36). Within group effect sizes can be found in the appendix (Table B & Fig. A).
Table 2.
Between-group effect sizes for IBI on self-efficacy at baseline compared to the end of treatment and follow-up (FU).
| Post | FU1 | FU2 | FU3 | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| k | dSMC | LL | UL | I2 | Q | k | dSMC | LL | UL | I2 | Q | k | dSMC | LL | UL | I2 | Q | k | dSMC | LL | UL | I2 | Q | |
| IBI (all) | 67 | 0.46 | 0.27 | 0.65 | 95.13 | 504.72 | 13 | 0.16 | −0.00 | 0.33 | 76.19 | 35.48 | 14 | 0.16 | 0.03 | 0.29 | 43.17 | 27.27 | 6 | 0.12 | −0.09 | 0.33 | 40.46 | 8.07 |
| Type of Self-Efficacy Measure | ||||||||||||||||||||||||
| General | 29 | 0.75 | 0.31 | 1.20 | 98.05 | 416.17 | 6 | 0.25 | −0.11 | 0.61 | 88.86 | 24.79 | 8 | 0.31 | 0.02 | 0.60 | 78.86 | 22.80 | ||||||
| Specific | 38 | 0.21 | 0.12 | 0.30 | 48.10 | 81.01 | 7 | 0.11 | −0.06 | 0.28 | 47.31 | 10.57 | 6 | 0.07 | −0.08 | 0.20 | 9.55 | 4.07 | ||||||
| Type of Control | ||||||||||||||||||||||||
| Waitlist | 28 | 0.64 | 0.40 | 0.89 | 89.53 | 173.31 | 7 | 0.15 | −0.13 | 0.43 | 72.42 | 19.91 | 3 | 0.97 | 0.22 | 1.73 | 71.16 | 7.87 | ||||||
| TAU | 15 | 0.66 | −0.08 | 1.39 | 98.27 | 180.93 | ||||||||||||||||||
| Active Control | 24 | 0.10 | −0.03 | 0.23 | 71.40 | 62.78 | 6 | 0.17 | −0.04 | 0.39 | 78.78 | 14.98 | 10 | 0.02 | −0.07 | 0.11 | 0.00 | 4.99 | ||||||
| Type of Setting | ||||||||||||||||||||||||
| Unguided | 44 | 0.42 | 0.17 | 0.68 | 94.71 | 285.41 | 8 | 0.16 | −0.09 | 0.42 | 76.51 | 24.26 | 6 | 0.15 | −0.05 | 0.36 | 0.00 | 2.34 | ||||||
| Guided | 19 | 0.61 | 0.24 | 0.97 | 96.21 | 204.13 | 5 | 0.15 | −0.07 | 0.36 | 70.61 | 9.74 | 8 | 0.28 | 0.00 | 0.55 | 85.62 | 24.34 | ||||||
| Blended | 4 | 0.19 | −0.15 | 0.52 | 63.02 | 7.90 | ||||||||||||||||||
| Type of Disorder | ||||||||||||||||||||||||
| Mood | 11 | 1.17 | 0.09 | 2.26 | 99.46 | 237.86 | ||||||||||||||||||
| Trauma | 9 | 0.64 | 0.16 | 1.12 | 91.38 | 66.90 | ||||||||||||||||||
| Transdiagnostic | 5 | 0.33 | −0.03 | 0.69 | 80.25 | 16.83 | ||||||||||||||||||
| Substance | 5 | 0.03 | −0.38 | 0.45 | 52.26 | 8.25 | ||||||||||||||||||
| Relationship | 8 | 0.68 | 0.08 | 1.29 | 91.67 | 82.46 | ||||||||||||||||||
| Non-clinical | 20 | 0.14 | 0.06 | 0.23 | 15.36 | 21.63 | ||||||||||||||||||
| Other | 9 | 0.37 | 0.18 | 0.56 | 35.95 | 11.90 | ||||||||||||||||||
FU1 = short-term follow-up between 1 and 5 months, FU2 = mid-term follow-up between 6 and 12 months, and FU3 = long-term follow-up over 12 months, dSMC = standardized mean changes, LL = lower limit of 95 % confidence interval, UL = upper limit of 95 % confidence interval. I2 values are reported in percent (%). k = number of comparisons. Comparisons with k < 3 studies are not reported.
Fig. 3.
Forest Plot between effects.
The Egger's test and the Rank Correlation Test indicated the presence of funnel plot asymmetry both for uncontrolled effects (Kendall's tau = 0.22, p < 0.01; Egger's test: Z = 5.81, p < 0.0001) as well as controlled effects (Kendall's tau = 0.27, p = 0.001; Egger's test: Z = 4.57, p < 0.0001), suggesting potential publication bias. However, when applying the trim and fill method, it estimated no missing studies, indicating that the observed effect sizes might not be substantially influenced by unreported studies.
3.3.2. Self-efficacy as a predictor or moderator
Six studies were identified examining self-efficacy as a predictor or moderator with mixed results. Three studies provide evidence that low self-efficacy pre-treatment is predictive of better outcomes while one study shows the opposite effect and two studies finding no significant effect. Clarke et al. (2014) examined the effects of mental health self-efficacy on outcomes of an IBI relative to an active control and a waitlist in a transdiagnostic clinical sample. They observed a significant moderation effect of self-efficacy: people with low pretreatment mental health self-efficacy reported the greatest post-intervention improvements in depression, anxiety, and stress (p = 0.013). Donker et al. (2013) conducted a noninferiority trial comparing two IBI to an active control condition in a non-clinical community sample. They found that lower mastery predicted better outcomes at post-test regardless of intervention (p < 0.001; i.e., predictor), while they found no significant interaction effect of mastery on depression (i.e., moderator). The third study by Toh et al. (2022) examined the potential efficacy of an IBI compared to an active control in a non-clinical student sample and found that participants with lower coping self-efficacy experienced the fastest post-test decline in perceived stress levels (p = 0.005). This moderation effect was found only for the outcome stress and not for depression and anxiety. In contrast, the study by Schmidt et al. (2022) investigated self-efficacy as a predictor in internet-based grief therapy for people bereaved by suicide compared to a waitlist. They found that higher self-efficacy was associated with a greater reduction in grief (p = 0.001). A study by Brog et al. (2022a)2 examined predictors of treatment outcome of an unguided IBI for COVID-19 related psychological distress and found no significant effect from pre-treatment self-efficacy on the outcome. Similar findings were shown by Böttche et al. (2016)3 in a study investigating predictors for treatment outcomes of an IBI for PTSD in older adults, that showed non-significance for self-efficacy as a predictor.
3.3.3. Self-efficacy as a mediator
Ten mediator studies with a total of twelve investigated IBI were identified. As visualized in Table 3 seven comparisons (58.33 %) reported overall support for self-efficacy as a mediator, although it is important to note that three of them came from the same study. Four studies yielded mixed results (33.33 %). In three of those studies, self-efficacy was only found to be a significant mediator for some of the primary outcomes but not all (Brodbeck et al., 2022; Clarke et al., 2014; Vincent et al., 2010). In one study, self-efficacy only partially mediated the effect (Acosta et al., 2017). One study (8.33 %) showed no significant evidence for self-efficacy as a mediator (Ehlers et al., 2023). Five studies provided sufficient data to calculate an estimate of variance explained by self-efficacy as a mediator, with a mean R2 of 0.32 (SD = 0.15). Table 4 gives an overview of to which extent the studies met quality criteria for investigating mediators as proposed by Kazdin (2007) and Lemmens et al. (2016).
Table 3.
Box score results and mean R2 for self-efficacy as a mediator.
| Subgroups | SE as a mediator | Mean R2 effect size estimate |
|---|---|---|
| Overall | +2a +2a +2a +4a +6a +8 +10a ?1 ?3 ?5 ?9a −7 | 0.32 (SD = 0.15, k = 5) |
| Unguided | +2 +2 +2 +4 +8 ?1 ?5 ?9 | |
| Guided | +6 +10 ?3 −7 |
Acosta2017, 2Bakker2018 (all 3 intervention groups), 3Brodbeck2022, 4Cieslak2016, 5Clarke2014, 6Dingle2017, 7Ehlers2023, 8Nixon2022, 9Vincent2010, 10Warmerdam2010; + significant mediator effect,? mixed results, – no significant mediator effect; astudies included in the calculation of the mean R2 effect size estimate.
Table 4.
Quality assessment mediator studies.
1 per group; 2Temporality is defined as >2 assessments during the treatment phase; − = requirement is not met; + = requirement is met.
4. Discussion
The use and research of IBI have grown rapidly in the past years, offering a new way for people to access mental health treatment. To our knowledge, this is the first systematic review and meta-analysis specifically addressing the role of self-efficacy in IBI for mental disorders. In this review, a total of 70 RCTs with N = 17,407 participants were included. Notably, 16 (over 20 %) of these studies were published in 2023 or 2024, highlighting the recent surge in interest and research activity in this area. The included studies investigated self-efficacy as an outcome, a predictor or moderator, or as a mediator in IBI aiming at reducing symptoms of mental disorders in adults.
Findings addressing the first research question concerning the impact of IBI on self-efficacy as an outcome showed overall moderate effects. In this study, there was a larger effect on general self-efficacy measures (e.g., general self-efficacy, attribution, perceived control, mastery) than specific self-efficacy measures (e.g., mental health self-efficacy, caregiver mastery, coping self-efficacy). This is in contrast to Bandura's (2006) recommendations to measure self-efficacy as specifically as possible and previous findings that IBI have a positive effect on self-efficacy measured with disease-specific self-efficacy scales, while no effects were found for self-efficacy measured with general self-efficacy scales (Samoocha et al., 2010). These results should, however, be interpreted with caution, because of the high heterogeneity among studies that assessed general self-efficacy measures. This could be an indication that the measures in this category assessing constructs related to self-efficacy, such as mastery, were not comparable. However, in a subgroup analysis regarding only studies that applied self-efficacy measures we found similar results in effects and heterogeneity as when we included related constructs. The actual overlap among these constructs should be investigated empirically to clarify their distinctions. Nonetheless, we consider it a strength of our analysis to have included related constructs broadly, as this approach offers a more comprehensive understanding given their inherent conceptual overlap. Results for the effects of IBI on self-efficacy at follow-up were mixed with stable moderate effects at short- and mid-term follow-up for within group comparisons and small or non-significant effects for between group comparisons. The sample sizes for long-term follow-ups were very small. Thus, the sustained effectiveness of IBI on self-efficacy beyond the immediate post-treatment period remains unclear.
As expected, the effect sizes were largest for comparisons with waitlist controls, while IBI were shown to be not more efficacious in enhancing self-efficacy than active controls or TAU. Clinical trials with waitlist controls yield limited conclusions, as they tend to overestimate the treatment effect sizes (Mohr et al., 2014). The reasons that the active controls were also effective could be due to non-specific or common therapeutic factors (e.g., positive expectations of treatment benefits, hope, and structure provided by treatment), which may arise due to the receipt of any psychological intervention (Mulder et al., 2017). Moreover, the content of the active control interventions often consisted of therapeutic material, such as the basic version of the intervention or the same content in a different order and were offered in a similar delivery mode. The non-significant effect size for IBI compared to TAU is in line with other meta-analysis that showed comparable efficacy of both treatment settings on mental health outcomes (Carlbring et al., 2018; Schaeuffele et al., 2024). Our findings suggest that IBI and TAU (e.g., face-to-face psychotherapy, telephone CBT, and nonfrequent counseling) can be similarly effective in improving self-efficacy offering a promising alternative in contexts where more costly traditional treatments are less accessible. The classification of control conditions is critical for interpreting the effectiveness of IBI. As Goldberg et al. (2023) emphasize, inconsistencies in control group definitions can impact effect size estimates and complicate cross-study comparisons. Our study categorized control groups into waitlist, active control, and treatment-as-usual conditions, aligning with conventional approaches. However, future research may benefit from adopting a more standardized classification.
Guided interventions appear to offer more benefits in increasing self-efficacy, while unguided interventions showed smaller effects. The level of guidance necessary in IBI for mental health remains a current debate. While the majority of studies demonstrate a superiority of guided over unguided IBI on mental health outcomes, some studies do not support these findings, making it unclear at this point how much human support is needed in IBI. The superiority of guided interventions on self-efficacy, observed in this study, could potentially be explained by the supportive nature that personalized feedback often entails. Participants might be able to overcome difficulties that occur during the intervention and develop more positive beliefs about their abilities through encouraging messages. Additionally, guided interventions motivate participants to engage fully and persistently with the intervention and practice skills regularly, which is crucial for a sense of achievement and the development of self-efficacy. However, the high heterogeneity in this group suggests that factors such as the extent and nature of guidance play a crucial role. Blended interventions showed a slightly larger effect than unguided but smaller effect than guided IBI in the within group comparisons, whilst there was a non-significant effect of blended interventions in the between group comparisons. The findings are particularly interesting regarding the construct of self-efficacy because they indicate that guidance within IBI is important to improve self-efficacy, an attribute strongly related to autonomy and self-motivation. It suggests that a moderate level of support enhances the intervention's effectiveness without the need for the more intensive face-to-face-support applied in blended approaches, offering a balance between independence, and directed help. However, the limited number of studies investigating blended interventions call for cautious interpretation. More research is needed regarding the necessary level of guidance in IBI, especially for secondary outcomes like self-efficacy.
IBI seemed to be effective in enhancing self-efficacy regardless of the mental disorder targeted. The smallest effects were found for interventions targeting individuals with substance abuse (including smoking) and non-clinical populations. Individuals with more severe symptoms of mental health disorders tend to have lower self-efficacy expectancies (Kim, 2003; Muris, 2002) which may result in larger gains in self-efficacy. However, it is unclear how non-clinical so-called community samples are. For example, Donker et al. (2013) recruited a community sample that reported a mean depression baseline score indicative of major depression.
The results for self-efficacy as a potential predictor or moderator were inconsistent. Three studies found evidence that individuals with low self-efficacy at baseline benefit more from IBI. These results were unexpected, as social learning theory assumes greater therapeutic benefit for people with high pretreatment self-efficacy (Bandura, 1997). Clarke et al. (2014) suggested that the increase may have been greatest in users with low self-efficacy because their higher depression scores at the start of the intervention offered them greater potential for improvement, or that an IBI to increase self-efficacy was particularly well suited to these individuals. On the other hand, one study found that higher self-efficacy was associated with a greater reduction in grief and two studies found no significant result for self-efficacy as a predictor. These conflicting results are in line with the review on transdiagnostic predictors of therapy outcome in guided IBI by Haller et al. (2023) that yielded inconsistent results for self-efficacy. In our study, a trend for the benefit of low self-efficacy at baseline was observed but given the small number of studies and the different symptoms of mental disorders they investigated, no firm conclusions can be drawn about whether high or low self-efficacy at baseline contributes to the response to IBI and for whom and under what conditions IBIs have different effects.
We found evidence for self-efficacy as a mediator in IBI. Seven comparisons in five studies showed a significant mediation effect for self-efficacy on outcomes, while four studies yielded mixed results, such as there was only a mediating effect found for some of the outcomes but not for others or self-efficacy turned out to be only partially mediating the outcome. Only one study showed no significant effect. These results are in correspondence with previous systematic reviews on mechanisms of change in IBI for depression (Domhardt et al., 2021) and PTSD (Steubl et al., 2021) that found self-efficacy as a mediator. Overall, the quality assessment for process research of the included mediation studies revealed significant room for improvement. Only two of the ten studies met the criteria of temporality (Kazdin, 2007). All five studies that found a significant mediation effect in this review did not meet the criteria of temporality and thus are insufficient to make a statement about the causal relationship of changes in self-efficacy and the outcomes. Furthermore, only five of the ten studies included multiple mediators and none of the studies employed an experimental design by manipulating self-efficacy. The findings of this review suggest that IBI may work in part by increasing the participants' self-efficacy and that because of this, precise targeting of self-efficacy may have the potential to increase the efficacy of IBI for mental disorders. However, the quality of studies is too poor to draw final conclusions, and the small mean R2 effect size estimate should therefore be interpreted with caution.
Several limitations must be considered when interpreting the results of this review and meta-analysis. First, as most of the primary studies were conducted in Western countries and recruited mainly female participants, the samples included were not representative of different ethnicities and genders. Only studies published in English were included, which may introduce language bias. Secondly, we may have missed relevant studies where self-efficacy was assessed but not mentioned in the titles or abstracts. Another important limitation of our results is the high heterogeneity of effects, which partly persisted in the subgroup analysis and limits the generalizability of our findings. This is probably due to the broad inclusion of different samples (i.e., different targeted symptoms, clinical- and non-clinical samples, caregivers, etc.) and IBI settings. Another reason could be that the included studies examine self-efficacy heterogeneously, including general and specific self-efficacy and related constructs such as perceived control and mastery. Other meta-analyses on IBI for specific mental disorders have also reported high heterogeneity (Domhardt et al., 2021; Steubl et al., 2021), suggesting that IBI is a very broad term for interventions differing greatly in terms of intensity, content, and delivery. The third limitation is regarding the results of the mediator analyses. The box-scoring approach can only be considered for visualization and effect size estimates did not account for study sample differences. Future research should apply meta-analytic structural equation modeling if possible. Fourthly, although the quality of the included studies can be considered satisfactory, risk of bias was a concern, particularly due to self-reported outcomes and limited documentation of blinding procedures. This is consistent with previous findings that blinding is rarely used in randomized clinical trials of psychological interventions, which can lead to an overestimation of the beneficial effects of the experimental interventions studied and an underestimation of the harmful effects (Juul et al., 2021). While participant and personnel blinding is often impractical in psychotherapy research, it may be more feasible in IBI (Domhardt et al., 2021). Given these challenges, we rated the risk of bias in outcome measurement as raising some concerns. Furthermore, we didn't assess an inter-rater reliability for the risk of bias rating. Lastly, the majority of included studies reported high dropout rates, which is a common problem in IBI (Moshe et al., 2021). We did not examine the relationship between adherence and self-efficacy, but future research should explore how self-efficacy influences adherence and whether enhancing it can improve engagement in IBI (Smoktunowicz et al., 2024). Besides the limitations, this study has notable strengths, including its comprehensive approach that integrates self-efficacy and related constructs to provide a holistic understanding of their roles in internet-based interventions. Additionally, we have ensured transparency and reproducibility by making all project data, including the data extraction sheet and relevant R code, publicly available.
Given that the overall effects of IBI on self-efficacy were moderate in the included RCTs, the reach of such scalable, low-intensity interventions could yield important public health advantages by engaging individuals who may not typically pursue or have access to traditional forms of treatment (Bennett-Levy et al., 2010). More research is needed on the long-term efficacy of IBI on self-efficacy. From a clinical standpoint this is of crucial relevance because self-efficacy is conceptualized as a component of resilience (Schwarzer and Warner, 2013) and thus, enhancing self-efficacy sustainably could be an important goal of treatment to prevent future episodes of mental disorders. The findings of our study also suggest that self-efficacy might be a mediator of improved mental health outcomes in IBI. Expanding the evidence base with component studies investigating the active ingredients of treatment as well as mediation studies following methodological recommendations for process research and using appropriate statistical methods for mediation analysis, will further improve our knowledge on mechanisms of change of IBI for mental disorders (Domhardt et al., 2021). Given the positive influence of high self-efficacy on mental health and its potential role as a mediator for treatment success, it could be of interest to target enhancing self-efficacy as an outcome. Given the mixed evidence for self-efficacy as a predictor or moderator for treatment outcomes, more research is needed to determine for whom self-efficacy enhancing intervention components could be beneficial. Here it would be advantageous to conduct an individual patient data meta-analysis for more precise analysis of how self-efficacy influences treatment outcomes and adherence across different populations. We included a diverse range of self-efficacy measurement tools in our study. Future research could focus specifically on the impact of different self-efficacy measurement instruments within IBI research to determine whether certain measures are more sensitive to change or better suited for digital interventions.
Overall, results from this systematic review and meta-analysis suggest that IBI can be as effective as traditional treatment in improving self-efficacy. Given the scalability and cost-effectiveness of IBI, they could serve as a viable alternative to face-to-face treatments, particularly for individuals who prefer digital interventions. Self-efficacy may play an important role in the context of IBI as a mediator and could therefore itself be a valuable target to increase the efficacy of IBI for symptoms of mental disorders. More research is needed on long-term effects of IBI on self-efficacy, self-efficacy as a predictor or moderator, and more studies with appropriate study designs for process research are needed to further investigate the role of self-efficacy in IBI.
Declaration of Generative AI and AI-assisted technologies in the writing process
During the preparation of this work the corresponding author used ChatGPT to improve clarity and readability for some individual sentences (OpenAI, 2024). After using this tool, the author reviewed and edited the content as needed and takes full responsibility for the content of the published article.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2025.100821.
The paper is a secondary analysis of the paper by Brog et al. (2022b)
The paper is a secondary analysis of the paper by Knaevelsrud et al. (2017)
Contributor Information
Solveig Behr, Email: s.behr@fu-berlin.de.
Laura Martinez Garcia, Email: l.martinez@unizar.es.
Marie Puetz, Email: m.puetz@stud.phb.de.
Johanna Boettcher, Email: johanna.boettcher@phb.de.
Carmen Schaeuffele, Email: carmen.schaeuffele@fu-berlin.de.
Christine Knaevelsrud, Email: christine.knaevelsrud@fu-berlin.de.
Appendix A. Supplementary data
Supplementary material
References
- Acosta M.C., Possemato K., Maisto S.A., Marsch L.A., Barrie K., Lantinga L., Fong C., Xie H., Grabinski M., Rosenblum A. Web-delivered CBT reduces heavy drinking in OEF-OIF veterans in primary care with symptomatic substance use and PTSD. Behav. Ther. 2017;48(2):262–276. doi: 10.1016/j.beth.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association 2022 COVID-19 practitioner impact survey: psychologist workload. APA Reports. 2022 https://www.apa.org/pubs/reports/practitioner/2022-covid-psychologist-workload [Google Scholar]
- Angerer F., Mennel V., Grund S., Mayer A., Büscher R., Sander L.B., Cuijpers P., Terhorst Y., Baumeister H., Domhardt M. Mechanisms of change in digital interventions for depression: a systematic review and meta-analysis of six mediator domains. J. Affect. Disord. 2025;368:615–632. doi: 10.1016/j.jad.2024.09.055. [DOI] [PubMed] [Google Scholar]
- Bakker D., Kazantzis N., Rickwood D., Rickard N. A randomized controlled trial of three smartphone apps for enhancing public mental health. Behav. Res. Ther. 2018;109:75–83. doi: 10.1016/j.brat.2018.08.003. [DOI] [PubMed] [Google Scholar]
- Balduzzi S., Rücker G., Schwarzer G. meta: General Package for Meta-Analysis. R package version 4.11-0. 2019. https://cran.r-project.org/package=meta URL.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84(2):191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. W H Freeman/Times Books/ Henry Holt & Co.; 1997. Self-Efficacy: The Exercise of Control. [Google Scholar]
- Bandura A. In: Self-Efficacy Beliefs of Adolescents. Pajares F., Urdan T.C., editors. vol. 5. Information Age Publishing; 2006. Guide for constructing self-efficacy scales; pp. 307–337. [Google Scholar]
- Bastien, L., Boke, B. N., Mettler, J., Zito, S., Di Genova, L., Romano, V., Lewis, S. P., Whitley, R., Iyer, S. N., & Heath, N. L. (2022). Peer-Presented Versus Mental Health Service Provider–Presented Mental Health Outreach Programs for University Students: Randomized Controlled Trial [Original Paper]. JMIR Ment Health, 9(7), e34168. doi: 10.2196/34168. [DOI] [PMC free article] [PubMed]
- Bennett-Levy, J., Richards, D. A., & Farrand, P. (2010). 3Low intensity CBT interventions: a revolution in mental health care. In J. Bennett-Levy, P. Farrand, J. Bennett-Levy, D. Richards, P. Farrand, H. Christensen, K. Griffiths, D. Kavanagh, B. Klein, M. A. Lau, J. Proudfoot, L. Ritterband, J. White, & C. Williams (Eds.), Oxford Guide to Low Intensity CBT Interventions (pp. 0). Oxford University Press. 10.1093/med:psych/9780199590117.003.0001. [DOI]
- Bijker L., Kleiboer A., Riper H.M., Cuijpers P., Donker T. A pilot randomized controlled trial of E-care for caregivers: an internet intervention for caregivers of depressed patients. Internet Interv. 2017;9:88–99. doi: 10.1016/j.invent.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisson J.I., Ariti C., Cullen K., Kitchiner N., Lewis C., Roberts N.P., Simon N., Smallman K., Addison K., Bell V., Brookes-Howell L., Cosgrove S., Ehlers A., Fitzsimmons D., Foscarini-Craggs P., Harris S.R.S., Kelson M., Lovell K., McKenna M., Williams-Thomas R. Guided, internet based, cognitive behavioural therapy for post-traumatic stress disorder: pragmatic, multicentre, randomised controlled non-inferiority trial (RAPID) BMJ. 2022;377 doi: 10.1136/bmj-2021-069405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blom M., Zarit S., Zwaaftink R., Cuijpers P., Pot A.M. Effectiveness of an internet intervention for family caregivers of people with dementia: results of a randomized controlled trial. PLoS One. 2015;13 doi: 10.1371/journal.pone.0116622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boele F.W., Weimer J.M., Marsland A.L., Armstrong T.S., Given C.W., Drappatz J., Donovan H.S., Sherwood P.R. The effects of SmartCare© on neuro-oncology family caregivers’ distress: a randomized controlled trial. Support Care Cancer. 2022;30(3):2059–2068. doi: 10.1007/s00520-021-06555-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boots L.M., de Vugt M.E., Kempen G.I., Verhey F.R. Effectiveness of a blended care self-management program for caregivers of people with early-stage dementia (partner in balance): randomized controlled trial [original paper] J. Med. Internet Res. 2018;20(7) doi: 10.2196/10017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M. John Wiley & Sons; 2009. Introduction to meta-Analysis. [Google Scholar]
- Böttche M., Kuwert P., Pietrzak R.H., Knaevelsrud C. Predictors of outcome of an Internet-based cognitive-behavioural therapy for post-traumatic stress disorder in older adults. Psychol. Psychother. 2016;89(1):82–96. doi: 10.1111/papt.12069. [DOI] [PubMed] [Google Scholar]
- Brindal E., Kakoschke N., Golley S., Rebuli M., Baird D. Effectiveness and feasibility of a self-guided Mobile app targeting emotional well-being in healthy adults: 4-week randomized controlled trial [original paper] JMIR Ment Health. 2023;10 doi: 10.2196/44925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodbeck J., Berger T., Biesold N., Rockstroh F., Schmidt S.J., Znoj H. The role of emotion regulation and loss-related coping self-efficacy in an internet intervention for grief: mediation analysis [original paper] JMIR Ment Health. 2022;9(5) doi: 10.2196/27707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brog N.A., Hegy J.K., Berger T., Znoj H. Age, motivation, and emotion regulation skills predict treatment outcome in an internet-based self-help intervention for COVID-19 related psychological distress [original research] Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.835356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brog N.A., Hegy J.K., Berger T., Znoj H. Effects of an internet-based self-help intervention for psychological distress due to COVID-19: results of a randomized controlled trial. Internet Interv. 2022;27 doi: 10.1016/j.invent.2021.100492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brose A., Heinrich M., Bohn J., Kampisiou C., Zagorscak P., Knaevelsrud C. Sequencing effects of behavioral activation and cognitive restructuring in an internet-based intervention for depressed adults are negligible: results from a randomized controlled trial. J. Consult. Clin. Psychol. 2023;91(3):122–138. doi: 10.1037/ccp0000789. [DOI] [PubMed] [Google Scholar]
- Buntrock C., Ebert D., Lehr D., Smit F., Cuijpers P., Berking M. Effectiveness of a web-based cognitive Behavioural intervention for subthreshold depression: pragmatic randomised controlled trial. Psychother. Psychosom. 2015;84:348–358. doi: 10.1159/000438673. [DOI] [PubMed] [Google Scholar]
- Bush N.E., Smolenski D.J., Denneson L.M., Williams H.B., Thomas E.K., Dobscha S.K. A virtual Hope box: randomized controlled trial of a smartphone app for emotional regulation and coping with distress. Psychiatr. Serv. 2017;68(4):330–336. doi: 10.1176/appi.ps.201600283. [DOI] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn. Behav. Ther. 2018;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- Cattaneo L.B., Chapman A.R. The process of empowerment: a model for use in research and practice. Am. Psychol. 2010;65(7):646–659. doi: 10.1037/a0018854. [DOI] [PubMed] [Google Scholar]
- Cieslak R., Benight C.C., Rogala A., Smoktunowicz E., Kowalska M., Zukowska K., Yeager C., Luszczynska A. Effects of internet-based self-efficacy intervention on secondary traumatic stress and secondary posttraumatic growth among health and human services professionals exposed to indirect trauma [original research] Front. Psychol. 2016;7 doi: 10.3389/fpsyg.2016.01009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke J., Proudfoot J., Birch M.R., Whitton A.E., Parker G., Manicavasagar V., Harrison V., Christensen H., Hadzi-Pavlovic D. Effects of mental health self-efficacy on outcomes of a mobile phone and web intervention for mild-to-moderate depression, anxiety and stress: secondary analysis of a randomised controlled trial. BMC Psychiatry. 2014;14:272. doi: 10.1186/s12888-014-0272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran W.G. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–129. [Google Scholar]
- Dingle G.A., Carter N.A. Smoke into sound: a pilot randomised controlled trial of a music cravings management program for chronic smokers attempting to quit. Music. Sci. 2017;21(2):151–177. doi: 10.1177/1029864916682822. [DOI] [Google Scholar]
- Domhardt, M., Ebert, D. D., & Baumeister, H. (2018). Internet- und mobilebasierte Interventionen. In.
- Domhardt M., Letsch J., Kybelka J., Koenigbauer J., Doebler P., Baumeister H. Are internet- and mobile-based interventions effective in adults with diagnosed panic disorder and/or agoraphobia? A systematic review and meta-analysis. J. Affect. Disord. 2020;276:169–182. doi: 10.1016/j.jad.2020.06.059. [DOI] [PubMed] [Google Scholar]
- Domhardt M., Steubl L., Boettcher J., Buntrock C., Karyotaki E., Ebert D.D., Cuijpers P., Baumeister H. Mediators and mechanisms of change in internet- and mobile-based interventions for depression: a systematic review. Clin. Psychol. Rev. 2021;83 doi: 10.1016/j.cpr.2020.101953. [DOI] [PubMed] [Google Scholar]
- Dominick S.A., Irvine A.B., Beauchamp N., Seeley J.R., Nolen-Hoeksema S., Doka K.J., Bonanno G.A. An internet tool to normalize grief. Omega (Westport) 2009;60(1):71–87. doi: 10.2190/om.60.1.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T., Batterham P.J., Warmerdam L., Bennett K., Bennett A., Cuijpers P., Griffiths K.M., Christensen H. Predictors and moderators of response to internet-delivered interpersonal psychotherapy and cognitive behavior therapy for depression. J. Affect. Disord. 2013;151(1):343–351. doi: 10.1016/j.jad.2013.06.020. [DOI] [PubMed] [Google Scholar]
- Donker T., Blankers M., Hedman E., Ljótsson B., Petrie K., Christensen H. Economic evaluations of internet interventions for mental health: a systematic review. Psychol. Med. 2015;45(16):3357–3376. doi: 10.1017/S0033291715001427. [DOI] [PubMed] [Google Scholar]
- Duval S., Tweedie R. Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication Bias in Meta-analysis. Biometrics. 2004;56(2):455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Ebert D.D., Daele T.V., Nordgreen T., Karekla M., Compare A., Zarbo C., Brugnera A., Øverland S., Trebbi G., Jensen K.L., Kaehlke F., Baumeister H. Internet- and Mobile-based psychological interventions: applications, efficacy, and potential for improving mental health. Eur. Psychol. 2018;23(2):167–187. doi: 10.1027/1016-9040/a000318. [DOI] [Google Scholar]
- Ebert D.D., Lehr D., Boß L., Riper H., Cuijpers P., Andersson G., Thiart H., Heber E., Berking M. Efficacy of an internet-based problem-solving training for teachers: results of a randomized controlled trial. Scandinavian Journal of Work, Environment &. 2014;Health(6):582–596. doi: 10.5271/sjweh.3449. [DOI] [PubMed] [Google Scholar]
- Ehlers A., Wild J., Warnock-Parkes E., Grey N., Murray H., Kerr A., Rozental A., Thew G., Janecka M., Beierl E.T., Tsiachristas A., Perera-Salazar R., Andersson G., Clark D.M. Therapist-assisted online psychological therapies differing in trauma focus for post-traumatic stress disorder (STOP-PTSD): a UK-based, single-blind, randomised controlled trial. Lancet Psychiatry. 2023;10(8):608–622. doi: 10.1016/S2215-0366(23)00181-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrer L.M., Gulliver A., Katruss N., Fassnacht D.B., Kyrios M., Batterham P.J. A novel multi-component online intervention to improve the mental health of university students: randomised controlled trial of the Uni virtual clinic. Internet Interv. 2019;18 doi: 10.1016/j.invent.2019.100276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenski F., Rozental A., Heinrich M., Knaevelsrud C., Zagorscak P., Boettcher J. Negative effects in internet-based interventions for depression: a qualitative content analysis. Internet Interv. 2021;26 doi: 10.1016/j.invent.2021.100469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiol-DeRoque, M. A., Serrano-Ripoll, M. J., Jiménez, R., Zamanillo-Campos, R., Yáñez-Juan, A. M., Bennasar-Veny, M., Leiva, A., Gervilla, E., García-Buades, M. E., García-Toro, M., Alonso-Coello, P., Pastor-Moreno, G., Ruiz-Pérez, I., Sitges, C., García-Campayo, J., Llobera-Cánaves, J., & Ricci-Cabello, I. (2021). A Mobile Phone–Based Intervention to Reduce Mental Health Problems in Health Care Workers During the COVID-19 Pandemic (PsyCovidApp): Randomized Controlled Trial [Original Paper]. JMIR Mhealth Uhealth, 9(5), e27039. doi: 10.2196/27039. [DOI] [PMC free article] [PubMed]
- Gleeson J.F.M., Koval P., Zyphur M., Lederman R., Herrman H., Eleftheriadis D., Bendall S., Cotton S.M., Gorelik A., Alvarez-Jimenez M. A randomized controlled trial of moderated online social therapy for family carers of first-episode psychosis patients in a specialist treatment setting. Schizophr. Res. 2023;255:203–212. doi: 10.1016/j.schres.2023.03.019. [DOI] [PubMed] [Google Scholar]
- Goldberg S.B., Sun S., Carlbring P., Torous J. Selecting and describing control conditions in mobile health randomized controlled trials: a proposed typology. npj Digital Medicine. 2023;6:181. doi: 10.1038/s41746-023-00923-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller K., Becker P., Niemeyer H., Boettcher J. Who benefits from guided internet-based interventions? A systematic review of predictors and moderators of treatment outcome. Internet Interv. 2023;33 doi: 10.1016/j.invent.2023.100635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrer M., Cuijpers P., Furukawa T.A., Ebert D.D. dmetar: Companion R Package for the Guide 'Doing Meta-Analysis in R'. R package version 0.0.9000. 2019. https://github.com/MathiasHarrer/dmetar URL.
- Heber E., Ebert D.D., Lehr D., Cuijpers P., Berking M., Nobis S., Riper H. The benefit of web- and computer-based interventions for stress: a systematic review and Meta-analysis [original paper] J. Med. Internet Res. 2017;19(2) doi: 10.2196/jmir.5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savović J., Schulz K.F., Weeks L., Sterne J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirai M., Clum G.A. An internet-based self-change program for traumatic event related fear, distress, and maladaptive coping. J. Trauma. Stress. 2005;18(6):631–636. doi: 10.1002/jts.20071. [DOI] [PubMed] [Google Scholar]
- Iancu I., Bodner E., Ben-Zion I.Z. Self esteem, dependency, self-efficacy and self-criticism in social anxiety disorder. Compr. Psychiatry. 2015;58:165–171. doi: 10.1016/j.comppsych.2014.11.018. [DOI] [PubMed] [Google Scholar]
- Isbăşoiu A.B., Tulbure B.T., Rusu A., Sava F.A. Can we boost treatment adherence to an online Transdiagnostic intervention by adding self-enhancement strategies? Results from a randomized controlled non-inferiority trial [original research] Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.752249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin L. 2017. A web-based intervention with culturally tailored messages to improve mental health among Asian international students with mild-to-moderate depression: A pilot randomized controlled trial [Doctoral dissertation] [Google Scholar]
- Juul S., Gluud C., Simonsen S., Frandsen F.W., Kirsch I., Jakobsen J.C. Blinding in randomised clinical trials of psychological interventions: a retrospective study of published trial reports. BMJ Evidence-Based Medicine. 2021;26(3):109. doi: 10.1136/bmjebm-2020-111407. [DOI] [PubMed] [Google Scholar]
- Karampas K., Pezirkianidis C., Stalikas A. In: Emerging Adulthood in the COVID-19 Pandemic and Other Crises: Individual and Relational Resources. Leontopoulou S., Delle Fave A., editors. Springer International Publishing; 2022. Combining stress mindset training with acceptance and commitment therapy (ACT): An internet-delivered intervention for emerging adults during the pandemic; pp. 295–314. [DOI] [Google Scholar]
- Karampas K., Pezirkianidis C., Stalikas A. ReStress mindset: an internet-delivered intervention that changes university students’ mindset about stress in the shadow of the COVID-19 pandemic [original research] Front. Psychol. 2022;13 doi: 10.3389/fpsyg.2022.1036564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin A.E. Mediators and mechanisms of change in psychotherapy research. Annu. Rev. Clin. Psychol. 2007;3(1):1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- Kim Y.-H. Correlation of mental health problems with psychological constructs in adolescence: final results from a 2-year study. Int. J. Nurs. Stud. 2003;40(2):115–124. doi: 10.1016/S0020-7489(02)00037-8. [DOI] [PubMed] [Google Scholar]
- Klein B., Richards J.C. A brief internet-based treatment for panic disorder. Behav. Cogn. Psychother. 2001;29(1):113–117. doi: 10.1017/S1352465801001138. [DOI] [Google Scholar]
- Knaevelsrud C., Böttche M., Pietrzak R.H., Freyberger H.J., Kuwert P. Efficacy and feasibility of a therapist-guided internet-based intervention for older persons with childhood traumatization: a randomized controlled trial. Am. J. Geriatr. Psychiatry. 2017;25(8):878–888. doi: 10.1016/j.jagp.2017.02.024. [DOI] [PubMed] [Google Scholar]
- Köhle N., Drossaert C.H.C., ten Klooster P.M., Schreurs K.M.G., Hagedoorn M., Van Uden-Kraan C.F., Verdonck-de Leeuw I.M., Bohlmeijer E.T. Web-based self-help intervention for partners of cancer patients based on acceptance and commitment therapy and self-compassion training: a randomized controlled trial with automated versus personal feedback. Support Care Cancer. 2021;29(9):5115–5125. doi: 10.1007/s00520-021-06051-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn E., Kanuri N., Hoffman J.E., Garvert D.W., Ruzek J.I., Taylor C.B. A randomized controlled trial of a smartphone app for posttraumatic stress disorder symptoms. J. Consult. Clin. Psychol. 2017;85(3):267–273. doi: 10.1037/ccp0000163. [DOI] [PubMed] [Google Scholar]
- Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- Lauder S., Chester A., Castle D., Dodd S., Gliddon E., Berk L., Chamberlain J., Klein B., Gilbert M., Austin D.W., Berk M. A randomized head to head trial of MoodSwings.net.au: an internet based self-help program for bipolar disorder. J. Affect. Disord. 2015;171:13–21. doi: 10.1016/j.jad.2014.08.008. [DOI] [PubMed] [Google Scholar]
- Lee C.S., Bowman M., Wu J.L. Preliminary outcomes from a single-session, asynchronous, online stress and anxiety management workshop for college students. Trends Psychiatry Psychother. 2023;45 doi: 10.47626/2237-6089-2021-0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemmens L., Müller V., Arntz A., Huibers M.J.H. Mechanisms of change in psychotherapy for depression: an empirical update and evaluation of research aimed at identifying psychological mediators. Clin. Psychol. Rev. 2016;50:95–107. doi: 10.1016/j.cpr.2016.09.004. [DOI] [PubMed] [Google Scholar]
- Lin Z., Cheng L., Han X., Wang H., Liao Y., Guo L., Shi J., Fan B., Teopiz K.M., Jawad M.Y., Zhang H., Chen Y., Lu C., McIntyre R.S. The effect of internet-based cognitive behavioral therapy on major depressive disorder: randomized controlled trial [original paper] J. Med. Internet Res. 2023;25 doi: 10.2196/42786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes R.T., da Rocha G.C., Svacina M.A., Meyer B., Šipka D., Berger T. Effectiveness of an internet-based self-guided program to treat depression in a sample of Brazilian users: randomized controlled trial [original paper] JMIR Form Res. 2023;7 doi: 10.2196/46326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejewski J., Smoktunowicz E. Low-effort internet intervention to reduce students’ stress delivered with Meta’s messenger chatbot (Stressbot): a randomized controlled trial. Internet Interv. 2023;33 doi: 10.1016/j.invent.2023.100653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maybery D., Reupert A., Bartholomew C., Cuff R., Duncan Z., McAuliffe C., McLean L., Pettenuzzo L., Swing A., Foster K. An online intervention for 18–25-year-old youth whose parents have a mental illness and/or substance use disorder: a pilot randomized controlled trial. Early Interv. Psychiatry. 2022;16(11):1249–1258. doi: 10.1111/eip.13274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberg C., Niles A., Beermann D. Guided self-help works: randomized waitlist controlled trial of Pacifica, a Mobile app integrating cognitive behavioral therapy and mindfulness for stress, anxiety, and depression [original paper] J. Med. Internet Res. 2019;21(6) doi: 10.2196/12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr D.C., Ho J., Hart T.L., Baron K.G., Berendsen M., Beckner V., Cai X., Cuijpers P., Spring B., Kinsinger S.W., Schroder K.E., Duffecy J. Control condition design and implementation features in controlled trials: a meta-analysis of trials evaluating psychotherapy for depression. Transl. Behav. Med. 2014;4(4):407–423. doi: 10.1007/s13142-014-0262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshe I., Terhorst Y., Philippi P., Domhardt M., Cuijpers P., Cristea I., Pulkki-Råback L., Baumeister H., Sander L.B. Digital interventions for the treatment of depression: a meta-analytic review. Psychol. Bull. 2021;147(8):749–786. doi: 10.1037/bul0000334. [DOI] [PubMed] [Google Scholar]
- Mulder R., Murray G., Rucklidge J. Common versus specific factors in psychotherapy: opening the black box. Lancet Psychiatry. 2017;4(12):953–962. doi: 10.1016/s2215-0366(17)30100-1. [DOI] [PubMed] [Google Scholar]
- Mullarkey M., Dobias M., Sung J., Ahuvia I., Shumake J., Beevers C., Schleider J. Web-based single session intervention for perceived control over anxiety during COVID-19: randomized controlled trial [original paper] JMIR Ment Health. 2022;9(4) doi: 10.2196/33473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P. Relationships between self-efficacy and symptoms of anxiety disorders and depression in a normal adolescent sample. Personal. Individ. Differ. 2002;32(2):337–348. doi: 10.1016/S0191-8869(01)00027-7. [DOI] [Google Scholar]
- Newby K., Teah G., Cooke R., Li X., Brown K., Salisbury-Finch B., Kwah K., Bartle N., Curtis K., Fulton E., Parsons J., Dusseldorp E., Williams S.L. Do automated digital health behaviour change interventions have a positive effect on self-efficacy? A systematic review and meta-analysis. Health Psychol. Rev. 2021;15(1):140–158. doi: 10.1080/17437199.2019.1705873. [DOI] [PubMed] [Google Scholar]
- Nixon P., Ebert D.D., Boß L., Angerer P., Dragano N., Lehr D. The efficacy of a web-based stress management intervention for employees experiencing adverse working conditions and occupational self-efficacy as a mediator: randomized controlled trial [original paper] J. Med. Internet Res. 2022;24(10) doi: 10.2196/40488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OpenAI . OpenAI; San Francisco, CA: 2024. ChatGPT.https://chat.openai.com/ URL. [Google Scholar]
- Orbach G., Lindsay S., Grey S. A randomised placebo-controlled trial of a self-help internet-based intervention for test anxiety. Behav. Res. Ther. 2007;45(3):483–496. doi: 10.1016/j.brat.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016;5 doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I., Schooler C. The structure of coping. J. Health Soc. Behav. 1978;19(1):2–21. doi: 10.2307/2136319. [DOI] [PubMed] [Google Scholar]
- Pfammatter M., Tschacher W. Klassen allgemeiner Wirkfaktoren der Psychotherapie und ihr Zusammenhang mit Therapietechniken. Z. Klin. Psychol. Psychother. 2016;16:1–13. doi: 10.1026/1616-3443/a000331. [DOI] [Google Scholar]
- Proudfoot J., Parker G., Manicavasagar V., Hadzi-Pavlovic D., Whitton A., Nicholas J., Smith M., Burckhardt R. Effects of adjunctive peer support on perceptions of illness control and understanding in an online psychoeducation program for bipolar disorder: a randomised controlled trial. J. Affect. Disord. 2012;142(1):98–105. doi: 10.1016/j.jad.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Rawlett K. Journey from self-efficacy to empowerment. Health Care. 2014;2:1–9. doi: 10.12966/hc.02.01.2014. [DOI] [Google Scholar]
- Rogers J., Sicouri G. A single-session online cognitive Bias modification of interpretations modified for adults with anxiety and depressive symptoms. Behav. Ther. 2022;53(5):967–980. doi: 10.1016/j.beth.2022.04.006. [DOI] [PubMed] [Google Scholar]
- Rohde J., Marciniak M.A., Henninger M., Homan S., Paersch C., Egger S.T., Seifritz E., Brown A.D., Kleim B. Investigating relationships among self-efficacy, mood, and anxiety using digital technologies: randomized controlled trial [original paper] JMIR Form Res. 2023;7 doi: 10.2196/45749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romijn G., Batelaan N., Koning J., van Balkom A., de Leeuw A., Benning F., Hakkaart van Roijen L., Riper H. Acceptability, effectiveness and cost-effectiveness of blended cognitive-behavioural therapy (bCBT) versus face-to-face CBT (ftfCBT) for anxiety disorders in specialised mental health care: a 15-week randomised controlled trial with 1-year follow-up. PLoS One. 2021;16(11) doi: 10.1371/journal.pone.0259493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose R.D., Buckey J.C., Zbozinek T.D., Motivala S.J., Glenn D.E., Cartreine J.A., Craske M.G. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav. Res. Ther. 2013;51(2):106–112. doi: 10.1016/j.brat.2012.11.003. [DOI] [PubMed] [Google Scholar]
- Rotter J.B. Generalized expectancies for internal versus external control of reinforcement. Psychol. Monogr. Gen. Appl. 1966;80(1):1–28. doi: 10.1037/h0092976. [DOI] [PubMed] [Google Scholar]
- Rozental A., Boettcher J., Andersson G., Schmidt B., Carlbring P. Negative effects of internet interventions: a qualitative content analysis of Patients’ experiences with treatments delivered online. Cogn. Behav. Ther. 2015;44(3):223–236. doi: 10.1080/16506073.2015.1008033. [DOI] [PubMed] [Google Scholar]
- RStudio Team . RStudio, PBC; Boston, MA: 2020. RStudio: Integrated Development for R.http://www.rstudio.com/ URL. [Google Scholar]
- Samoocha D., Bruinvels D.J., Elbers N.A., Anema J.R., van der Beek A.J. Effectiveness of web-based interventions on patient empowerment: a systematic review and meta-analysis. J. Med. Internet Res. 2010;12(2) doi: 10.2196/jmir.1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaeuffele C., Meine L.E., Schulz A., Weber M.C., Moser A., Paersch C., Recher D., Boettcher J., Renneberg B., Flückiger C., Kleim B. A systematic review and meta-analysis of transdiagnostic cognitive behavioural therapies for emotional disorders. Nat. Hum. Behav. 2024 doi: 10.1038/s41562-023-01787-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt V., Treml J., Linde K., Peterhänsel C., Kersting A. Predictors of prolonged grief in an internet-based grief therapy for people bereaved by suicide. J. Psychiatr. Res. 2022;149:162–167. doi: 10.1016/j.jpsychires.2022.02.023. [DOI] [PubMed] [Google Scholar]
- Schwarzer R., Warner L.M. In: Resilience in Children, Adolescents, and Adults: Translating Research into Practice. Prince-Embury S., Saklofske D.H., editors. Springer; New York: 2013. Perceived self-efficacy and its relationship to resilience; pp. 139–150. [DOI] [Google Scholar]
- Schwob J.T., Newman M.G. Brief imaginal exposure exercises for social anxiety disorder: a randomized controlled trial of a self-help momentary intervention app. J. Anxiety Disord. 2023;98 doi: 10.1016/j.janxdis.2023.102749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sextl-Plötz T., Franke M., Baumeister H., Ebert D.D. In: Digitale Gesundheitsinterventionen: Anwendungen in Therapie Und Prävention. Ebert D.D., Baumeister H., editors. Springer; Berlin Heidelberg: 2023. Affektive Störungen; pp. 39–54. [DOI] [Google Scholar]
- Shimazu A., Kawakami N., Irimajiri H., Sakamoto M., Amano S. Effects of web-based psychoeducation on self-efficacy, problem solving behavior, stress responses and job satisfaction among workers: a controlled clinical trial. J. Occup. Health. 2005;47(5):405–413. doi: 10.1539/joh.47.405. [DOI] [PubMed] [Google Scholar]
- Shuai R., Ahmed-Leitao F., Bloom J., Seedat S., Hogarth L. Brief online negative affect focused functional imagery training (FIT) improves four-week drinking outcomes in hazardous student drinkers: a pilot randomised controlled trial replication in South Africa. Addict. Behav. Rep. 2024;19 doi: 10.1016/j.abrep.2024.100540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuai R., Bakou A.E., Andrade J., Hides L., Hogarth L. Brief online negative affect focused functional imagery training improves 2-week drinking outcomes in hazardous student drinkers: a pilot randomised controlled trial. Int. J. Behav. Med. 2022;29(3):346–356. doi: 10.1007/s12529-021-10019-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade M., Rennick-Egglestone S., Elliott Rachel A., Newby C., Robinson C., Gavan S.P., Paterson L., Ali Y., Yeo C., Glover T., Pollock K., Callard F., Priebe S., Thornicroft G., Repper J., Keppens J., Smuk M., Franklin D., Walcott R., group, t. N. s Effectiveness and cost-effectiveness of online recorded recovery narratives in improving quality of life for people with non-psychotic mental health problems: a pragmatic randomized controlled trial. World Psychiatry. 2024;23(1):101–112. doi: 10.1002/wps.21176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoktunowicz E., Barak A., Andersson G., Banos R.M., Berger T., Botella C., Dear B.F., Donker T., Ebert D.D., Hadjistavropoulos H., Hodgins D.C., Kaldo V., Mohr D.C., Nordgreen T., Powers M.B., Riper H., Ritterband L.M., Rozental A., Schueller S.M., Titov N., Weise C., Carlbring P. Consensus statement on the problem of terminology in psychological interventions using the internet or digital components. Internet Interv. 2020;21 doi: 10.1016/j.invent.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoktunowicz E., Lesnierowska M., Carlbring P., Andersson G., Cieslak R. Resource-based internet intervention (med-stress) to improve well-being among medical professionals: randomized controlled trial. J. Med. Internet Res. 2021;23(1) doi: 10.2196/21445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoktunowicz E., Maciejewski J., Lesnierowska M., Carlbring P. Bridging the adherence gap in internet interventions: a randomized controlled trial study protocol investigating context-specific self-efficacy. Internet Interv. 2024;35 doi: 10.1016/j.invent.2023.100697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmetz S.E., Benight C.C., Bishop S.L., James L.E. My disaster recovery: a pilot randomized controlled trial of an internet intervention. Anxiety Stress Coping. 2012;25(5):593–600. doi: 10.1080/10615806.2011.604869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.Y., Corbett M.S., Eldridge S.M., Emberson J.R., Hernán M.A., Hopewell S., Hróbjartsson A., Junqueira D.R., Jüni P., Kirkham J.J., Lasserson T., Li T., Higgins J.P.T. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366 doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Steubl L., Sachser C., Baumeister H., Domhardt M. Mechanisms of change in internet- and mobile-based interventions for PTSD: a systematic review and meta-analysis. Eur. J. Psychotraumatol. 2021;12(1) doi: 10.1080/20008198.2021.1879551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B., Goldstein T., Gotkiewicz D., Gotkiewicz E., George B., Brent D. Acceptability, engagement, and effects of a Mobile digital intervention to support mental health for young adults transitioning to college: pilot randomized controlled trial [original paper] JMIR Form Res. 2021;5(10) doi: 10.2196/32271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahmassian K., Jalali Moghadam N. Relationship between self-efficacy and symptoms of anxiety, depression, worry and social avoidance in a normal sample of students. Iran J Psychiatry Behav Sci. 2011;5(2):91–98. [PMC free article] [PubMed] [Google Scholar]
- Takano A., Miyamoto Y., Shinozaki T., Matsumoto T., Kawakami N. Effect of a web-based relapse prevention program on abstinence among Japanese drug users: a pilot randomized controlled trial. J. Subst. Abus. Treat. 2020;111:37–46. doi: 10.1016/j.jsat.2019.12.001. [DOI] [PubMed] [Google Scholar]
- Taylor C.B., Graham A.K., Flatt R.E., Waldherr K., Fitzsimmons-Craft E.E. Current state of scientific evidence on internet-based interventions for the treatment of depression, anxiety, eating disorders and substance abuse: an overview of systematic reviews and meta-analyses. Eur. J. Pub. Health. 2021;31(31 Suppl 1):i3–i10. doi: 10.1093/eurpub/ckz208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teles S., Ferreira A., Paúl C. Feasibility of an online training and support program for dementia carers: results from a mixed-methods pilot randomized controlled trial. BMC Geriatr. 2022;22(1):173. doi: 10.1186/s12877-022-02831-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toh S.H.Y., Tan J.H.Y., Kosasih F.R., Sündermann O. Efficacy of the mental health app intellect to reduce stress: randomized controlled trial with a 1-month follow-up. JMIR Form Res. 2022;6(12) doi: 10.2196/40723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Gelder N.E., Ligthart S.A., van Rosmalen-Nooijens K.A., Prins J.B., Oertelt-Prigione S. Effectiveness of the SAFE eHealth intervention for women experiencing intimate partner violence and abuse: randomized controlled trial, quantitative process evaluation, and open feasibility study [original paper] J. Med. Internet Res. 2023;25 doi: 10.2196/42641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Stolk-Cooke K., Wielgosz J., Hallenbeck H.W., Chang A., Rosen C., Owen J., Kuhn E. The PTSD family coach app in veteran family members: pilot randomized controlled trial [original paper] JMIR Form Res. 2023;7 doi: 10.2196/42053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viechtbauer W. metafor: Meta-Analysis Package for R. R package version 2.5-7. 2010. https://cran.r-project.org/package=metafor URL.
- Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/s2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- Vincent N., Walsh K., Lewycky S. Sleep locus of control and computerized cognitive-behavioral therapy (cCBT) Behav. Res. Ther. 2010;48(8):779–783. doi: 10.1016/j.brat.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Wallston K.A., Wallston B.S., Smith S., Dobbins C.J. Perceived control and health. Curr. Psychol. 1987;6(1):5–25. doi: 10.1007/BF02686633. [DOI] [Google Scholar]
- Warmerdam L., van Straten A., Jongsma J., Twisk J., Cuijpers P. Online cognitive behavioral therapy and problem-solving therapy for depressive symptoms: exploring mechanisms of change. J. Behav. Ther. Exp. Psychiatry. 2010;41(1):64–70. doi: 10.1016/j.jbtep.2009.10.003. [DOI] [PubMed] [Google Scholar]
- Watson-Singleton N.N., Pennefather J. Using a randomized clinical trial to test the efficacy of a culturally responsive Mobile health application in African Americans. Behav. Ther. 2024 doi: 10.1016/j.beth.2023.12.002. [DOI] [PubMed] [Google Scholar]
- Webb J., Peerbux S., Ang A., Siddiqui S., Sherwani Y., Ahmed M., MacRae H., Puri H., Majeed A., Glasner S. Long-term effectiveness of a clinician-assisted digital cognitive behavioral therapy intervention for smoking cessation: secondary outcomes from a randomized controlled trial. Nicotine Tob. Res. 2022;24(11):1763–1772. doi: 10.1093/ntr/ntac113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner B. In: An Attributional Theory of Motivation and Emotion. Weiner B., editor. Springer US; 1986. An attributional theory of achievement motivation and emotion; pp. 159–190. [DOI] [PubMed] [Google Scholar]
- Welten J.J.E., Cox V.C.M., van Eijk R.P.A., van Heugten C.M., Visser-Meily J.M.A., Schepers V.P.M. The effects of a blended care intervention in Partners of Patients with Acquired Brain Injury - results of the CARE4Carer randomized controlled trial. Arch. Phys. Med. Rehabil. 2024;105(2):352–358. doi: 10.1016/j.apmr.2023.08.024. [DOI] [PubMed] [Google Scholar]
- Werntz A., Amado S., Jasman M., Ervin A., Rhodes J.E. Providing human support for the use of digital mental health interventions: systematic Meta-review. J. Med. Internet Res. 2023;25 doi: 10.2196/42864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westerhof G.J., Lamers S.M.A., Postel M.G., Bohlmeijer E.T. Online therapy for depressive symptoms: an evaluation of counselor-led and peer-supported life review therapy. Gerontologist. 2019;59(1):135–146. doi: 10.1093/geront/gnx140. [DOI] [PubMed] [Google Scholar]
- Wicke F.S., Dinh T.S., Riedel-Heller S., Weyerer S., König H.-H., Gensichen J., Schön G., Wegscheider K., Bickel H., Fuchs A., Schäfer I., van den Bussche H., Scherer M., Mergenthal K. Predictors of change in depressive symptoms in older and multimorbid patients: a longitudinal analysis of the multicare cohort. Aging Ment. Health. 2022;26(4):818–827. doi: 10.1080/13607863.2021.1902470. [DOI] [PubMed] [Google Scholar]
- Wild J., El-Salahi S., Degli Esposti M., Thew G.R. Evaluating the effectiveness of a group-based resilience intervention versus psychoeducation for emergency responders in England: a randomised controlled trial. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagorscak P., Heinrich M., Sommer D., Wagner B., Knaevelsrud C. Benefits of individualized feedback in internet-based interventions for depression: a randomized controlled trial. Psychother. Psychosom. 2018;87(1):32–45. doi: 10.1159/000481515. [DOI] [PubMed] [Google Scholar]
- Zarski A.-C., Baumeister H., Ebert D.D. In: Digitale Gesundheitsinterventionen: Anwendungen in Therapie Und Prävention. Ebert D.D., Baumeister H., editors. Springer; Berlin Heidelberg: 2023. Technische Umsetzung, inhaltliche Gestaltung und Implementierungsmöglichkeiten; pp. 3–12. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
All data for this project, including the data extraction sheet and relevant R code, have been made publicly available and can be accessed at: https://osf.io/5qz4e/?view_only=2b6c48d99ca448fba9b6ab7e9731ef25.