Abstract
Background and Aim
Hydatid cysts are caused by Echinococcus larvae and are prevalent in endemic areas worldwide. We analyzed post-procedure complications and outcomes of patients with liver hydatid cysts.
Materials and Methods
We included patients who were managed either by surgery or percutaneous drainage (PAIR) for hydatid liver cysts at Harran University Faculty of Medicine Hospital between January 2017 and February 2021. We recorded age, sex, segmental location, size, number, Gharbi classification, treatment modality, length of hospital stays, and complications.
Results
We included a total of 209 patients who were managed by hydatid liver cysts. Among them, 74 post-procedural complications were developed in a total of 69 (33%) patients. Biliary fistula was the most prevalent complication (n=38,18.2%). Hospitalization duration was a median of 5 days (2–36) and was 5 days (2–36) in patients who underwent surgery and 3 days (range:2–7) in patients managed by PAIR. Patients with cyst diameter ≥9.5 cm were predicted to have an increased risk of complications with 70% sensitivity and 60% specificity. More patients experienced any difficulties in patients who were managed by PAIR than those who underwent surgery (65.4% vs 28.4%, p<0.001).
Conclusion
Our study showed that both surgery and PAIR are safe and effective management strategies for patients with liver cyst hydatid. PAIR was associated with more complications but a shorter duration of hospitalization.
Keywords: Liver hydatid cyst surgery, percutaneous hydatid cyst treatment, post-operative complications
Introduction
Regarding echinococci, Echinococcus granulosus frequently causes cystic echinococcosis, while E. multiocularis less frequently causes alveolar hydatid cyst.[1,2] Hydatid cysts can remain asymptomatic until they reach a certain size. Hydatid cysts may present with a variety of clinical manifestations ranging from right upper quadrant pain and hepatomegaly to cholestasis and rarely features of chronic liver disease such as portal hypertension, and ascites.
A history of living in endemic areas as well as clinical and laboratory findings are helpful to reach cyst hydatid diagnosis, but imaging techniques such as ultrasonography (USG), computed tomography (CT), and magnetic resonance imaging (MRI) are the main diagnostic methods.[3]
There are several treatment options for liver hydatid cysts, including medical treatment, surgery, and percutaneous drainage (PAIR). Combinations of these treatment options are more widely accepted strategies in the management of liver hydatid cysts.[4]
Several minor and major complications such as bleeding, surgical site infection, biliary fistula, anaphylaxis or secondary hydatidosis with intra-abdominal transplantation of cyst contents, sclerosing cholangitis, biliary tract injury, development of an abscess in the abdomen or cyst cavity, pleural effusion, and cyst recurrence can develop following surgery or PAIR in patients with hydatid cyst disease.[5]
This study aimed to present our experience with complications following surgery and PAIR in patients with cyst hydatid. Our data was derived from an endemic area for hydatid cysts and a tertiary hospital.
Materials and Methods
The present study included patients who underwent surgery or PAIR for liver hydatid cysts between January 2017 and February 2021 at Harran University Faculty of Medicine Hospital. The study was approved by the Harran University Faculty of Medicine Ethics Committee (01.03.2021 HRU 20/15/09) and conducted by the Declaration of Helsinki.
Information about the patients age, sex, segmental cyst location, cyst size, number of cysts, Gharbi classification, treatment modalities, and complications were recorded. The segmental location of the cysts was recorded based on the Couinaud classification, and the cyst size was recorded in centimeters. The number of cysts was grouped as 1, 2, and multiple. Operated patients underwent either open surgery or laparoscopy, depending on the patient’s suitability. Intraoperative bile leaks that could be repaired were closed by sutures. Cholecystectomy was added to the operation for gallstones in the gallbladder, which were adjacent to the cyst wall. All patients who underwent percutaneous procedure were treated with the same percutaneous technique. USG, CT, and MRI methods were used alone or in combination as imaging modalities during the patients’ pre-procedure evaluation (Fig. 1).
Figure 1.
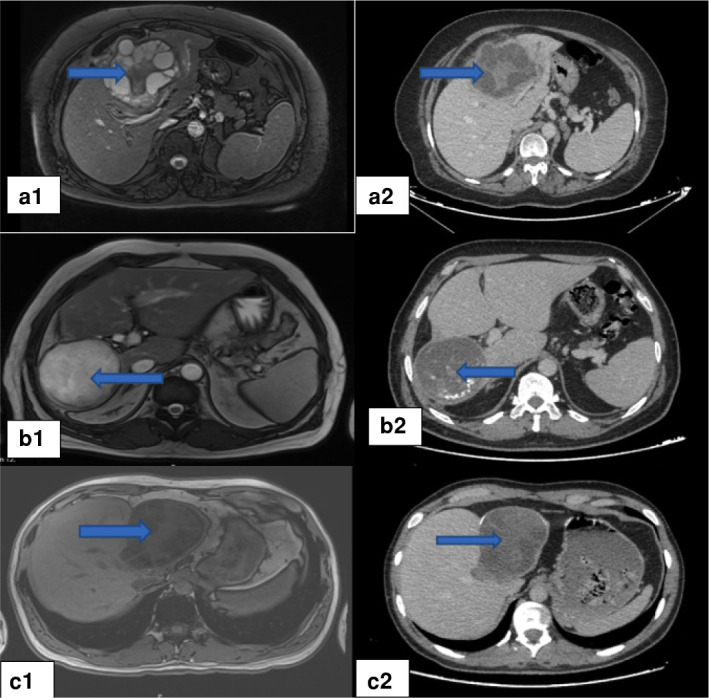
Computed tomography (CT) and magnetic resonance imaging (MRI) images of three patients included in the study during pre-operative evaluation [MRI on the left (a1, b1, c1), CT on the right (a2, b2, c2)]. The arrows indicate the location of the cysts.
Patients with hydatid cysts in other organs, younger than 18 years old, with incomplete data, and patients who underwent emergency procedures were excluded from the study. The data of patients were further analyzed for post-procedure complications.
The location of the cyst, the patient’s preference after preliminary information about the treatments, the stage of the cyst, and the patient’s pre-operative American Society of Anesthesiologists score.
The types of complications that occurred in patients upon surgical or percutaneous treatment were recorded as biliary fistula, disease recurrence, biloma, liver abscess, biliary stricture, pleural effusion, and perioperative anaphylaxis.
All of the patients underwent surgical and percutaneous treatment under operating room conditions. Based on the recommendation of the anesthesiology department, antihistamines, steroids, and epinephrine at appropriate doses were administered to patients with allergic reactions. All patients were started on albendazole (10 mg/kg/day) for 6 months post-operatively.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) Version 18.0 (SPSS® for Windows Chicago, IL, USA) was used for statistical analysis. Numerical data were presented in mean value standard deviation, whereas the non-numerical group data was in median value. Kolmogorov–Smirnov test was used to test the normal distribution hypothesis for all numerical data. Independent Samples t-test was used to compare paired groups when the numerical values met the normal distribution hypothesis, and the Mann–Whitney U test was used for comparison purposes in cases of non-normal distribution. A one-way analysis of variance (ANOVA) test was used to compare numerical data with normal distribution and three or more groups. The Bonferroni test was performed as a post hoc test in cases where the difference was significant. The Kruskal Wallis-H test was used to compare three or more groups in cases of non-normal numerical distribution. The Mann–Whitney U test was used for pairwise comparisons when the results were statistically significant. Pearson correlation test was performed to see whether there was a correlation between the numerical data. The Chi-squared or Fisher Exact test was used to compare ordinal and nominal data. ROC curve analysis was used to predict the development of postoperative complications. Results with a p-value of <0.05 were considered statistically significant.
Results
A total of 209 patients (145 female, 69%) with a median age of 33 years (range: 18–77) were included in the study. PAIR was performed in 26 (12.5%) patients while 183 (87.5%) patients underwent surgery. A total of 148 of the cysts were localized in the right lobe (71%), 44 in the left lobe (21%), and 17 in the right and left lobes (8%). The mean size of the cysts was 10.1±2.89 cm. Based on the Gharbi classification, type 1 (n=76, 36.4%), type 2 (n=70, 33.5%), type 3 (n=61, 29.2%) and type 4 (n=2, 0.9%). USG was performed in 173 patients, both USG and CT in 164 patients, and USG, CT, and MRI combined in 31 patients.
A total of 74 post-procedure complications were observed in 69 patients (33%). Five patients had more than one complication. Post-procedure complications developed in 52 (28.4%) patients who were surgically treated and in 17 (65.4%) patients who underwent PAIR. Biliary fistula was the most prevalent complication in the acute period, as seen in 38 (18.2%) patients. Biloma occurred in 11 (5.3%), liver abscess in 4 (1.9%), pleural effusion in 6 (2.9%), perioperative anaphylaxis in 2 (1%) patients, and biliary stricture in 1 (0.5%) patient included in the study. Twelve patients (5.7%) had recurred disease as a long-term complication.
The mean size of cysts with post-procedure complications was 10.9±3.05 cm. To predict the development of postoperative complications in hydatid cyst patients, the cut-off value of cyst diameter was determined using ROC curve analysis. Patients with cyst diameter ≥9.5 cm were predicted to have an increased risk of complications with 70% sensitivity and 60% specificity (Area under the curve: 0.624, 95% confidence interval, CI: 0.546–0.703, p=0.003) (Fig. 2).
Figure 2.

Graph showing the cut-off value of cyst diameter using ROC curve analysis to predict the development of postoperative complications according to cyst diameter.
There was no correlation between the number, localization, and Gharbi classification of the cyst and the occurrence of post-operative complications. One-way ANOVA test indicated a significant correlation between cyst size and the types of post-operative complications (p=0.015). Based on the results, the cyst size was the highest in the pleural effusion group (13.16±5.7 cm). The distribution of post-operative complications with cyst size is given in Table 1.
Table 1.
Mean cyst sizes in patients with post-operative complications
| Type of complication | Cyst size | ||||
|---|---|---|---|---|---|
| Number of patients | Mean | SD | Minimum | Maximum | |
| No | 135 | 9.64 | 2.71 | 5 | 20 |
| Biliary fistula | 38 | 10.73 | 2.78 | 6 | 20 |
| Biloma | 11 | 11.9 | 3.01 | 7 | 16 |
| Liver abscess | 4 | 9.5 | 1.91 | 8 | 12 |
| Biliary stricture | 1 | 12 | – | 12 | 12 |
| Recurrence | 12 | 10.25 | 2.34 | 7 | 14 |
| Pleural effusion | 6 | 13.16 | 5.70 | 7 | 22 |
| Perioperative anaphylaxis | 2 | 9 | 2.82 | 7 | 11 |
SD: Standard deviation.
Endoscopic retrograde cholangiopancreatography (ERCP) was performed in 29 (76.3%) patients with biliary fistula, while biliary fistulae spontaneously closed upon conservative follow-up in 9 (23.7%) patients. Percutaneous drainage catheterization was performed in all 11 patients with biloma. Biliary fistula occurred in 8 (72.7%) patients who underwent percutaneous drainage catheterization, and they were treated with ERCP. The most prevalent hepatic location of the cysts in the patients who developed biliary tract complications was segment 6, and the mean cyst size was 11±2.82 cm (Fig. 3).
Figure 3.

A distribution of cysts according to liver segments in patients with post-operative biliary tract complications.
All six patients with pleural effusion were drained with a percutaneous catheter. One of these patients had multiple cysts, whereas the cysts were localized in the right lobe and were single in five patients. The mean size of the cysts of our patients with pleural effusion was 13.16±5.7 cm.
Discussion
Complications that may occur after surgical or percutaneous treatment of hydatid cyst include hemorrhage, surgical site infection, biliary fistula, anaphylaxis or secondary hydatidosis with intra-abdominal transplantation of cyst contents, sclerosing cholangitis, common bile duct injury, abscess in the abdomen or cyst cavity, pleural effusion, and recurrence.[5] All the aforementioned complications, except for hemorrhage, surgical site infection, sclerosing cholangitis, and biliary tract injury, were seen in the patients included in the present study.
Conflicting results have been reported in the literature regarding the effect of age on complications. A retrospective study by Baraket et al.[6] reported the median age as 33 years (14–83), the rate of female patients as 55%, and that age did not affect the occurrence of complications. In a retrospective study by Daradkeh et al.,[7] morbidity increased in patients aged above 40 years. The fact that 145 out of 209 patients included in our study were female (69.4%) is consistent with the previous reports. The fact that hydatid cyst disease is more common in women is an issue that needs to be investigated. The mean age of our patients was 36.51±14.83 years. There was no statistically significant correlation between the older age and morbidity in the patients included in the present study (p=0.770).
There are studies in the literature investigating the relationship between the location of the cyst in the liver and the risk of complications. El Malki et al.[8] reported in a retrospective study that cysts in the left lobe and liver dome were associated with a higher risk of complications. In the present study, there was no statistically significant difference between the location of the cyst in the liver and the risk of complications. Understanding the relationship between liver cyst size and the risk of complications provides us with useful information to predict possible complications. A retrospective study by El Malki et al.[8] and a study by Atli et al.[9] reported that cyst sizes of >10 cm and >10.5 cm, respectively, increased the risk of complications. In the present study, the mean size of the cysts with post-operative complications was 10.9 cm (6–22 cm), and there was a statistically significant relationship between the increased cyst size and the occurrence of complications. We also mentioned in the results section that the cut-off value was ≥9.5 cm.
Among our patients, 81.8% had one cyst, 11.9% had two cysts, and 6.2% had multiple cysts. Previous studies did not report any correlation between the number of cysts and the risk of complications.[10] In the present study, no statistically significant relationship existed between the number of cysts and the risk of complications.
Gharbi classification guides us on how to treat the cyst rather than determining the risk of complications of the cyst. Demircan et al.[11] reported that cysts classified as Type 3 based on Gharbi classification were a risk factor for the occurrence of complications. In the present study, 36.3% of the cysts were Type 1, 33.4% were Type 2, and 29.1% were Type 3. There was no significant difference between the type of cyst by Gharbi classification and the occurrence of post-operative complications (p=0.086).
Percutaneous hydatid cyst treatment offers a more minimally invasive treatment option for suitable patients. Although the percutaneous treatment method is defined as a minimally invasive method, there are cases in the literature that require liver transplantation after sclerosing cholangitis secondary to protoscolicidal agents used in percutaneous treatment and care should be taken in terms of complications.[12] Deniz et al.[13] reported a complication rate of 15% upon percutaneous treatment. In the present study, 26 (12.4%) patients underwent percutaneous treatment. In another study, patients treated with different percutaneous techniques reported a high success rate of 94.5%, no abscesses or fistulas as complications, and a low complication rate with only 2 patients developing anaphylaxis.[14] Complications were seen in 17 (65.4%) patients who received percutaneous treatment. The present study’s complication rate of 65.4% in patients who underwent percutaneous treatment is inconsistent with previous reports. We think that this may be associated with the relatively small total number of patients who underwent the PAIR procedure.
The prevalence of complications of rupture of the bile ducts is between 3%–17%. Increased intra-cystic pressure subsequently leads to compression and necrosis of the wall, causing rupture into adjacent bile ducts.[15] In the present study, 29 out of 38 patients (76.3%) with biliary fistula were treated with ERCP. In 9 (23.7%) patients, the complication stopped spontaneously after conservative follow-up.
In the treatment of liver hydatid cysts, it is possible to predict the risk of cystobiliary fistula development according to the cyst size. Ramia et al.[16] reported the risk factors for cysto-biliary fistula as cysts >7.5 cm in size, cysts located in the central liver segment, and advanced cysts (Type 3–4) based on Gharbi classification. The mean cyst size in our patients with biliary fistula was 10.73±2.78 cm, the highest number of cysts was found in segment 6 (11 patients), and the highest number of cysts was found in Type 3 (16 patients), which is consistent with previous reports.
Biliary stricture is a rare but challenging post-operative complication of hydatid cyst disease. Yılmaz et al.[17] reported that 27% of all post-operative biliary strictures were secondary to hydatid cyst disease. Sclerosing cholangitis associated with scolicidal agents, secondary biliary infections, and centrally located hydatid cysts have been suggested as predisposing factors. In the present study, biliary stricture occurred in a patient operated on for a liver hydatid cyst associated with segment five localized biliary tract. Surgery was decided upon failed percutaneous transhepatic cholangiography and ERCP. Portoenterostomy was performed upon stenosis detection at the main hepatic duct bifurcation level.
Cysts associated with the bile ducts may present as bilomas after the procedure. Percutaneous drainage and subsequent ERCP may be required for these patients. The cure is usually achieved after these procedures. Baydar et al.[18] reported that 6 (22.2%) out of 27 patients had post-operative biloma upon liver hydatid cyst surgery and achieved a 92.6% success rate after percutaneous drainage in patients with biloma. In the present study, 11 patients (5.3%) had post-operative biloma. All the patients included in the study underwent percutaneous drainage. Eight out of eleven patients who underwent percutaneous drainage for biloma had biliary fistula, which was treated with ERCP.
A liver abscess may occur after surgical and percutaneous treatment or due to the cyst’s biliary tract relationship. It is required to cease the biliary tract connection by surgical or interventional procedures, to conduct surgical or interventional drainage of the abscess, and to administer medical albendazole and anti-biotherapy as an addition to the treatment.[19] In the present study, post-operative liver abscesses occurred in 4 patients (1.9%). All of these patients were treated with percutaneous drainage and cured.
Pleural effusion is frequently seen in most hepatobiliary surgery patients, not just hydatid cysts. Cobanoglu et al.[20] reported that 40.4% of patients with post-operative pleural effusion after upper abdominal surgery included the patients who underwent hepatobiliary surgery. In the present study, six patients had post-operative pleural effusion and were treated with percutaneous catheter drainage. Although there was no correlation between the types of complications and age upon statistical analysis (p=0.859), pleural effusion was seen in relatively older patients included in the study. In the present study, there was a significant difference between cyst size and the types of complications (p=0.015). Based on the study results, patients with pleural effusion had the highest cyst size (13.16±5.7 cm). Furthermore, there was a significant correlation between the types of post-operative complications and the duration of hospitalization (p<0.001). The longest hospital stay was seen in the pleural effusion group (15.50±11.04 days).
When an interventional procedure is performed in the treatment of hydatid cysts regardless of the organ, anaphylactic reactions are among the most feared complications. Inal et al.[21] reported that the rate of allergic reactions during the administration of anesthesia for liver hydatid cyst operations ranged between 1/5000 and 1/25000, and the mortality rate was 3%–5%. In the present study, 2 patients (0.9%) had anaphylactic reaction perioperatively and recovered upon medical treatment. There was no mortality in our patients. Collado-Aliaga et al.[22] reported in a 20-year cohort analysis that anaphylactic reaction was a risk factor in younger patients (<60 years) and patients with multiple cysts. In the present study, a clear comparison was not possible due to the relatively smaller size of the sample group.
Our study’s limitations include its retrospective design, the difficulty of making comparisons due to the large difference in the number of patients included in the PAIR procedure and surgery groups, and the loss of data in patients whose retrospective data were unavailable.
Conclusion
In conclusion, post-operative complications are prevalent in liver hydatid disease and are still associated with significant health problems. Pre-operative identification of risk factors may ensure the prediction of post-operative complications in liver hydatid disease. Therefore, a pre-operative evaluation of hydatid cyst patients should be cautious regarding the risk of post-operative complications. To manage post-operative complications, a multidisciplinary approach by general surgery, interventional radiology, thoracic surgery, anesthesia, and gastroenterology departments is required.
Footnotes
How to cite this article: Erkmen F, Yilmaz M, Yonder H, Tatli F, Ozgonul A, Karaca E, et al. Complications and management of patients with liver hydatid cyst: A single center experience. Hepatology Forum 2025; 6(2):52–56.
Ethics Committee Approval
The Harran University Faculty of Medicine Ethics Committee granted approval for this study (date: 01.03.2021, number: HRU 20/15/09).
Author Contributions
Concept – FE, MY, HY, FT, EB, AO, EK, AU; Design – FE, MY, HY, FT, EB, AO, EK, AU; Supervision – FE, MY, HY, FT, EB, AO, EK, AU; Fundings – FE, EK, HY, AU; Materials – FE, EK, HY, EB; Data Collection and/or Processing – FT, MY, AO, AU; Analysis and/or Interpretation – FT, MY, HY, EB; Literature Search – FE, FT, AU, AO; Writing – FE, FT, EK, MY; Critical Reviews – FE, AU, AO, HY.
Conflict of Interest
The authors have no conflict of interest to declare.
Use of AI for Writing Assistance
Not declared.
Financial Disclosure
The authors declared that this study has received no financial support.
Peer-review
Externally peer-reviewed.
References
- 1.Eckert J, Gemmell M, Meslin Fo-X, Pawlowski Z. 2001. WHO/OIE manual on echinococcosis in humans and animals: a public health problem of global concern World Organisation for Animal Health. [Google Scholar]
- 2.Thompson RCA. Biology and Systematics of Echinococcus. In: Thompson RCA, lymbery AJ, editors. Echinococcus and hydatid disease. Guilford: Biddles Ltd; 1995. pp. 1–37. [Google Scholar]
- 3.Yılmaz GR, Babur C. Diagnosis of echinococcosis. Turk Bullet Hygiene Exp Biol. 2007;64(3):35–44. [Google Scholar]
- 4.Çaycı M, Tihan D. Karaciğer kist hidatik tedavisinde güncel yaklaşım. Uludağ Üniv Tıp Fak Derg. 2016;42(1):53–59. [Google Scholar]
- 5.Bedioui H, Bouslama K, Maghrebi H, Farah J, Ayari H, Hsairi H, et al. Predictive factors of morbidity after surgical treatment of hepatic hydatid cyst. Pan Afr Med J. 2012;13:1–10. [PMC free article] [PubMed] [Google Scholar]
- 6.Baraket O, Moussa M, Ayed K, Kort B, Bouchoucha S. Predictive factors of morbidity after surgical treatment of hydatid cyst of the liver. Arab J Gastroenterol. 2014;15(3-4):119–122. doi: 10.1016/j.ajg.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Daradkeh S, El-Muhtaseb H, Farah S, Sroujieh A, Abu-Khalaf M. Predictors of morbidity and mortality in surgical management of hydatid cyst of the liver. Langenbecks Arch Surg. 2007;392(1):35–39. doi: 10.1007/s00423-006-0064-2. [DOI] [PubMed] [Google Scholar]
- 8.El Malki HO, El Mejdoubi Y, Souadka A, Moshine R, Ifrine L, Abouqal R, et al. Predictive factors of deep abdominal complications after operation for hydatid cyst of the liver: 15 years of experience with 672 patients. J Am Coll Surg. 2008;206(4):629–637. doi: 10.1016/j.jamcollsurg.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 9.Atli M, Kama NA, Yuksek YN, Doganay M, Gozalan U, Kologlu M, et al. Intrabiliary rupture of a hepatic hydatid cyst: Associated clinical factors and proper management. Arch Surg. 2001;136(11):1249–1255. doi: 10.1001/archsurg.136.11.1249. [DOI] [PubMed] [Google Scholar]
- 10.Uzunkoy A. Percutaneous Treatment Management Liver Hydatid Cyst Turkiye Klinikleri. J Gen Surg-Special. 2010;Topics 3(2):38–50. [Google Scholar]
- 11.Demircan O, Baymus M, Seydaoglu G, Akinoglu A, Sakman G. Occult cystobiliary communication presenting as postoperative biliary leakage after hydatid liver surgery: Are there significant preoperative clinical predictors? Can J Surg. 2006;49(3):177–184. [PMC free article] [PubMed] [Google Scholar]
- 12.Okut G, Saglam K, Kocaaslan H, Kayaalp C. First two cases of literature: Caustic sclerosing cholangitis due to percutaneous treatment of hydatid liver disease causing liver transplantation. Hepatol Forum. 2024;5(2):90–92. doi: 10.14744/hf.2023.2023.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deniz MA, Taş Deniz Z, Hattapoğlu S, Çetinçakmak MG. Retrospective evaluation of percutaneous treated liver cyst hydatic cases. Van Tıp Derg. 2020;27(3):267–273. doi: 10.5505/vtd.2020.48991. [DOI] [Google Scholar]
- 14.Örmeci N, Asiller ÖÖ Parmaksız A, Kalkan Ç Üstüner E, Altınel A, et al. Percutaneous treatment of hydatid cysts with the Örmeci technique. Turk J Gastroenterol. 2024;35(5):398–407. doi: 10.5152/tjg.2024.23286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bektaş A, Örmeci N. Kist hidatik komplikasyonları ve peritoneal kist hidatik. TKIin Cerrahi. 1998;3(3):199–201. [Google Scholar]
- 16.Ramia JM, Figueras J, De la Plaza R, Garcia-Parreno J. Cysto-biliary communication in liver hydatidosis. Langenbecks Arch Surg. 2012;397(6):881–887. doi: 10.1007/s00423-012-0926-8. [DOI] [PubMed] [Google Scholar]
- 17.Yilmaz U, Sakin B, Boyacioglu S, Saritas U, Cumhar T, Akoglu M. Management of postoperative biliary strictures secondary to hepatic hydatid disease by endoscopic stenting. Hepatogastroenterology. 1998;45(19):65–69. [PubMed] [Google Scholar]
- 18.Baydar B, Alper E, Akpınar Z, Aslan F, Serin Aİ Buyraç Z, et al. Percutaneous drainage of postoperative bilomas reduces the requirement of a second operation. Ege J Med. 2010;49(3):149–152. [Google Scholar]
- 19.Alghofaily KA, Saeedan MB, Aljohani IM, Alrasheed M, McWilliams S, Aldosary A, et al. Hepatic hydatid disease complications: review of imaging findings and clinical implications. Abdom Radiol (NY) 2017;42(1):199–210. doi: 10.1007/s00261-016-0860-2. [DOI] [PubMed] [Google Scholar]
- 20.Çobanoğlu U, Bartın M, Mergan D, Yılmaz/ D, Yılmaz Ö, Demir A, Toktaş O. Pleural effusion resultant after upper abdom inal surgery: Analysis of 47 cases. J Clin Anal Med. 2011;2(3):16–20. doi: 10.4328/JCAM.305. [DOI] [Google Scholar]
- 21.İnal MT, Memiş D, Akın F, Sezer A. Allergic reaction during hydatid cyst operation: Case report. Trakya Univ Tip Fak Derg. 2008;25(3):238–240. [Google Scholar]
- 22.Collado-Aliaga J, Romero-Alegría Á, Alonso-Sardón M, Muro A, López-Bernus A, Velasco-Tirado V, et al. Complications Associated with Initial Clinical Presentation of Cystic Echinococcosis: A 20-year Cohort Analysis. Am J Trop Med Hyg. 2019;101(3):628–635. doi: 10.4269/ajtmh.19-0019. [DOI] [PMC free article] [PubMed] [Google Scholar]


