Abstract
Objective
To conduct a comparative analysis of the clinical efficacy and quality of life in elderly patients with lumbar degenerative disease (LDD) treated with TLIF (transforaminal lumbar interbody fusion) combined with either unilateral pedicle screw fixation (UPSF) or bilateral pedicle screw fixation (BPSF).
Methods
A total of 112 patients with single- or double-segment lumbar degenerative disease were divided into two groups. In the unilateral fixation cohort, 32 single-segment patients and 22 double-segment patients underwent TLIF combined with UPSF, whereas in the bilateral fixation cohort, 34 single-segment patients and 24 double-segment patients underwent TLIF combined with BPSF. Data on operative time, intraoperative blood loss, time to postoperative ambulation, length of hospital stay, and perioperative complications were collected and analysed. Pain and functional status were preoperatively evaluated, in addition to being postoperatively evaluated at 1, 6, and 12 months, using the visual analogue scale (VAS), Oswestry Disability Index (ODI), Japanese Orthopaedic Association (JOA) score, and Short Form-36 (SF-36) health survey questionnaire. Imaging follow-up was conducted for 1 year; at the final follow-up, the fusion rate was determined using the Bridwell fusion grading system, and clinical outcomes were assessed by using the modified MacNab criteria.
Results
All of the follow-up patients successfully completed the surgeries. There were no significant differences observed in average postoperative ambulation time or hospital stay between the UPSF and BPSF groups for either single- or double-segment patients. However, the UPSF group exhibited less average blood loss and a shorter surgery time (P < 0.05). At 12 months after surgery, there were no statistically significant differences observed in the VAS, ODI, or JOA scores between the UPSF and BPSF groups, although both scores were significantly improved compared with the preoperative scores. There were fewer perioperative complications observed in the UPSF group than in the BPSF group for both single-segment (P = 0.040) and double-segment (P = 0.009) patients. In terms of quality of life, the UPSF group exhibited better long-term physical and mental health outcomes compared with the BPSF group (single-segment PCS: preoperative, P = 0.694; 1 month, P = 0.310; 6 months, P = 0.022; 12 months, P = 0.020; MCS: preoperative, P = 0.849; 1 month, P = 0.655; 6 months, P = 0.022; 12 months, P < 0.001; double-segment PCS: preoperative, p = 0.890; 1 month, P = 0.374; 6 months, P = 0.022; 12 months, P = 0.023; MCS: preoperative, P = 0.447; 1 month, P = 0.419; 6 months, P = 0.023; 12 months, P < 0.001). At the final follow-up, there were no significant differences observed in fusion rates between the groups according to the Bridwell fusion grading system (P > 0.05), with both groups achieving satisfactory fusion rates. The modified MacNab criteria revealed that excellent and good results in each group were > 90%, with no significant differences being observed between the groups (P > 0.05).
Conclusions
For the treatment of LDD in elderly patients, both TLIF combined with UPSF and TLIF combined with BPSF can achieve favourable outcomes. However, UPSF demonstrates advantages compared with BPSF, including a shorter surgery time, reduced intraoperative blood loss, and greater postoperative quality of life.
Keywords: Lumbar degenerative diseases, TLIF, Unilateral pedicle screw fixation, Bilateral pedicle screw fixation, Clinical efficacy, Quality of life, Elderly
Introduction
With increased ageing of the global population, there are currently more than 962 million people aged 60 years and older (representing 13% of the world’s total population) [1]. As the elderly population continues to grow, the prevalence of LDD is also increasing [2]. LDD primarily includes lumbar disc herniation and lumbar spinal stenosis [3]; these conditions cause severe low back and leg pain, which often imposes a significant burden on individuals and society [4]. Lumbar interbody fusion surgery is the main surgical method for treating LDD [5]. Currently, TLIF is a routine and well-established surgical method for treating LDD; moreover, its efficacy is widely recognised [6–8].
TLIF achieves decompression and anterior spinal fusion by removing the lower facet of the upper vertebra and the upper facet of the lower vertebra to expose the intervertebral foramen window. This technique does not involve intradural manipulation, thereby reducing the risks of nerve and dural traction, injury, and postoperative scar formation. Additionally, it avoids the use of laminectomy, thus allowing for the preservation of intervertebral ligaments, the supraspinous ligament, and other midline supporting structures behind the dura mater, which minimises the impact on spinal stability [9].
Traditionally, TLIF is often combined with BPSF, thus providing strong internal fixation for fusion and yielding good clinical efficacy [10]. Recently, UPSF has been gradually applied in clinical practice due to the fact that it is less invasive, safer, does not interfere with the contralateral soft tissues, and further reduces intraoperative blood loss, operation times, and tissue damage [11, 12]. However, most related studies have not considered patient age, and almost no analysis of the elderly population has been conducted. Moreover, biomechanical studies on UPSF have partially confirmed its stability and reliability [13]. This study conducted a prospective randomised controlled trial to evaluate the clinical efficacy and quality of life in elderly LDD patients aged 60 years and older who were treated with UPSF compared with those treated with BPSF.
Methods
Patient population
This randomised controlled trial received approval from the Ethics Committee of the Affiliated Hospital of Zunyi Medical University. The study included 117 elderly patients admitted to the Second Affiliated Hospital of Zunyi Medical University between July 2021 and December 2023; these patients met the inclusion and exclusion criteria and underwent TLIF combined with either UPSF or BPSF. Among these patients, 5 patients were excluded because they refused to participate in long-term postoperative follow-up. The remaining 112 patients were randomly assigned to different groups. Specifically, 66 patients underwent single-level fusion, with 32 receiving TLIF combined with UPSF and 34 undergoing TLIF combined with BPSF. Additionally, 46 patients received double-level fusion, with 22 receiving TLIF combined with UPSF and 24 undergoing TLIF combined with BPSF. All of the participants successfully completed the study.
Inclusion criteria
Aged 60 years or older;
Single-segment or consecutive two-segment degenerative lumbar disc herniation or lumbar spinal stenosis with neurological symptoms;
Unilateral clinical symptoms consistent with imaging findings;
Ineffective conservative treatment and patient requests for surgical treatment.
Exclusion criteria
Presence of spinal deformities, tumours, tuberculosis, infections, or lumbar spondylolisthesis grade II or higher.
Concurrent cognitive disorders or other diseases affecting functional evaluation;
Clinical symptoms not matching the imaging results.
Surgical techniques
A chief spinal surgeon performed all of the TLIF surgeries.
UPSF (Single Segment): The patient was placed into the prone position; after positioning, a longitudinal incision was performed 2 cm lateral to the posterior midline on the surgical side. The soft tissue was retracted bilaterally via the retractors, and the thoracolumbar fascia was incised under direct vision. Upon observing the natural separation between the longissimus and multifidus muscles, blunt dissection was performed to expose the lamina and facet joints of the surgical segment. Pedicle screws were inserted into the vertebral bodies above and below the segment. The inferior articular process was excised with rongeurs or chisels, and the lateral parts of the lamina and the ligamentum flavum were removed, thereby exposing the nerve root canal. The dural sac and nerve root were subsequently retracted, and the intervertebral disc was revealed. Complete decompression was achieved for the spinal canal and lateral recess stenosis, as well as for disc herniation, with the nerve root also being protected. The intervertebral disc was excised, and the corresponding TLIF instruments were used to prepare the endplate cartilage. Adequate bone fragments that were obtained during surgery, mixed with allograft bone, were filled in the anterior one-third of the intervertebral space, and a suitably sized cage was obliquely inserted. The position of the cage was confirmed using a C-arm X-ray machine. Finally, the rod and nut were installed and compressed for fixation, a drainage tube was placed in the wound, and the incision was sutured layer by layer.
BPSF (Single Segment): The patient was placed into the prone position; after positioning, a posterior midline incision was performed to expose the spine. The supraspinous and interspinous ligaments were preserved, and the paraspinal muscles were subperiosteally dissected to the tips of the transverse processes, with damage to the facet joint capsules being avoided. The bilateral paraspinal muscles were retracted to expose the entry points for pedicle screw insertion. After thorough decompression, anterior support was placed, the fixation was compressed, drainage tubes were placed in the wound, and the incision was sutured layer by layer.
Postoperative management
Patients were initially assigned to postoperative bed rest; additionally, they were assigned an appropriate thromboprophylaxis regimen based on their Caprini score. They were encouraged to turn over in bed, elevate their legs, perform ankle pump exercises, and undergo leg compression therapy to prevent thrombus formation. Lumbar spine anteroposterior and lateral X-rays were reviewed on the day of drain removal. If the positions of the internal fixation and interbody cage were satisfactory, patients were allowed to ambulate with the assistance of a lumbar brace. Discharged patients received monthly follow ups for the first three months and every three months thereafter.
Analyzed data
Indicators related to surgical safety, including surgical duration, intraoperative blood loss, postoperative time to ambulation after drainage tube removal, and length of hospital stay, were recorded in the medical records system. Common perioperative complications, including surgical site infection, nerve injury, cerebrospinal fluid leakage, hypostatic pneumonia, postoperative delirium, venous thrombosis, circulatory failure, and reoperation, were closely monitored. The VAS was used to assess the severity of lumbar and leg pain; moreover, the ODI was used to evaluate daily living disabilities, and the JOA score was used to assess spinal cord and nerve function [14]. The SF-36 was used to assess patients’ quality of life from both physical (via the physical component summary, or PCS) and psychological (via the mental component summary, or MCS) aspects [15]. The modified MacNab criteria [16] were used to evaluate surgical satisfaction at the final follow-up, and the Bridwell evaluation criteria [17] were used to measure the state of interbody fusion (Fig. 1).
Fig. 1.
Flowchart
Statistical analysis
Data analysis was conducted using SPSS 29.0 (IBM Corp., Armonk, NY, USA, Version 29.0). Continuous variables are expressed as the means ± standard deviations (x ± s) and were compared between the two groups using t tests for age, operation time, hospitalisation time, intraoperative blood loss, VAS score, ODI score, and JOA score. Categorical variables are expressed as numbers (n) and percentages (%) and were compared between the two groups via chi-square tests or Fisher’s exact tests for sex, surgical segment, and complications. A P value < 0.05 was considered to be statistically significant.
Results
Preoperative clinical data of the two groups: no statistically significant differences
A total of 112 patients with single- or double-level LDD who underwent TLIF combined with either UPSF or BPSF were included in the study (61 males and 51 females). The general patient characteristics are shown in Tables 1 and 2.
Table 1.
General information of single-segment patients
| Characteristic | Single-segment UPSF Group (n = 32) | Single-segment BPSF Group (n = 34) | P value |
|---|---|---|---|
| Mean Age (years) | 71.4 ± 4.2 | 68.4 ± 3.2 | 0.094 |
| Gender (n, %) | 0.432 | ||
| Male | 20 (62.5) | 18 (52.9) | |
| Female | 12 (37.5) | 16 (47.1) | |
| Surgical Segment (n, %) | 0.972 | ||
| L3/L4 | 6 (18.8) | 6 (17.6) | |
| L4/L5 | 16 (50.0) | 18 (52.9) | |
| L5/S1 | 10 (31.2) | 10 (29.4) | |
| Comorbidities (n, %) | |||
| Chronic Obstructive Pulmonary Disease (COPD) | 14 (43.8) | 10 (29.4) | 0.226 |
| Hypertension | 12 (37.5) | 10 (29.4) | 0.486 |
| Diabetes | 10 (31.3) | 8 (23.5) | 0.482 |
| Coronary Artery Disease | 6 (18.8) | 2 (5.9) | 0.221 |
| Chronic Renal Insufficiency | 4 (12.5) | 2 (5.9) | 0.613 |
| Osteoporosis | 18 (56.3) | 14 (41.2) | 0.221 |
| Preoperative VAS Score | 6.38 ± 0.96 | 6.88 ± 0.86 | 0.119 |
| Preoperative ODI Score | 61.88 ± 9.89 | 64.94 ± 6.13 | 0.290 |
| Preoperative JOA Score | 10.19 ± 1.28 | 9.76 ± 1.30 | 0.354 |
| Preoperative SF-36 Score | |||
| PCS | 26.00 ± 1.59 | 25.12 ± 1.76 | 0.142 |
| MCS | 19.50 ± 3.01 | 19.29 ± 3.14 | 0.447 |
Table 2.
General information of double-segment patients
| Characteristic | Double-segment UPSF Group (n = 22) | Double-segment BPSF Group (n = 24) | P value |
|---|---|---|---|
| Mean Age (years) | 71.6 ± 5.8 | 68.8 ± 3.0 | 0.171 |
| Gender (n, %) | 0.238 | ||
| Male | 13 (59.1) | 10 (41.7) | |
| Female | 9 (40.9) | 14 (58.3) | |
| Surgical Segment (n, %) | 0.829 | ||
| L3-L5 | 8 (36.4) | 8 (33.3) | |
| L4-S1 | 14 (63.6) | 16 (66.7) | |
| Comorbidities (n, %) | |||
| Chronic Obstructive Pulmonary Disease (COPD) | 10 (45.5) | 4 (16.7) | 0.072 |
| Hypertension | 8 (36.4) | 12 (50.0) | 0.351 |
| Diabetes | 8 (36.4) | 6 (25.0) | 0.403 |
| Coronary Artery Disease | 4 (18.2) | 2 (8.3) | 0.581 |
| Renal Insufficiency | 0 (0.0) | 0 (0.0) | - |
| Osteoporosis | 10 (45.5) | 16 (66.7) | 0.147 |
| Preoperative VAS Score | 6.18 ± 0.87 | 6.42 ± 0.79 | 0.507 |
| Preoperative ODI Score | 58.18 ± 7.45 | 62.50 ± 5.47 | 0.126 |
| Preoperative JOA Score | 8.82 ± 1.47 | 8.67 ± 1.23 | 0.791 |
| Preoperative SF-36 Score | |||
| PCS | 25.27 ± 2.05 | 26.00 ± 1.91 | 0.388 |
| MCS | 20.09 ± 3.24 | 19.08 ± 3.00 | 0.447 |
Among the single-level patients (n = 66), 32 underwent UPSF, including 20 males (62.5%) and 12 females (37.5%), with a mean age of 71.4 ± 4.2 years. The affected segments included L3/L4 in 6 patients (18.8%), L4/L5 in 16 patients (50.0%), and L5/S1 in 10 patients (31.2%). The comorbidities included chronic obstructive pulmonary disease (COPD) in 14 patients (43.8%), hypertension in 12 patients (37.5%), diabetes in 10 patients (31.3%), coronary artery disease (CAD) in 6 patients (18.8%), renal insufficiency in 4 patients (12.5%), and osteoporosis in 18 patients (56.3%). The preoperative scores included a VAS score of 6.38 ± 0.96, an ODI score of 61.88 ± 9.89, a JOA score of 10.19 ± 1.28, and SF-36 subscores of 26.00 ± 1.59 for PCS and 19.50 ± 3.01 for MCS. Among the 34 patients who underwent BPSF, 18 males (52.9%) and 16 females (47.1%) had a mean age of 68.4 ± 3.2 years. The affected segments included L3/L4 in 6 patients (17.6%), L4/L5 in 16 patients (52.9%), and L5/S1 in 10 patients (29.4%). The comorbidities included COPD in 10 patients (29.4%), hypertension in 10 patients (29.4%), diabetes in 8 patients (23.5%), CAD in 2 patients (5.9%), renal insufficiency in 2 patients (5.9%) and osteoporosis in 14 patients (41.2%). The preoperative scores included a VAS score of 6.88 ± 0.86, an ODI score of 64.94 ± 6.13, a JOA score of 9.76 ± 1.30, and SF-36 subscores of 25.12 ± 1.76 for PCS and 19.29 ± 3.14 for MCS.
Among the double-level patients (n = 46), 22 underwent UPSF, comprising 13 males (59.1%) and 9 females (40.9%), with a mean age of 71.6 ± 5.8 years. The affected segments included L3–L5 in 8 patients (36.4%) and L4–S1 in 14 patients (63.6%). The comorbidities included COPD in 10 patients (45.5%), hypertension in 8 patients (36.4%), diabetes in 8 patients (36.4%), CAD in 4 patients (18.2%), and osteoporosis in 10 patients (45.5%). The preoperative scores included a VAS score of 6.18 ± 0.87, an ODI score of 58.18 ± 7.45, a JOA score of 8.82 ± 1.47, and SF-36 subscores of 25.27 ± 2.05 for PCS and 20.09 ± 3.24 for MCS. Among the 24 patients who underwent BPSF, 10 males (41.7%) and 14 females (58.3%) had a mean age of 68.8 ± 3.0 years. The affected segments included L3–L5 in 8 patients (33.3%) and L4–S1 in 16 patients (66.7%). The comorbidities included COPD in 4 patients (16.7%), hypertension in 12 patients (50.0%), diabetes in 6 patients (25.0%), and osteoporosis in 16 patients (66.7%). The preoperative scores included a VAS score of 6.42 ± 0.79, an ODI score of 62.50 ± 5.47, a JOA score of 8.67 ± 1.23, and SF-36 subscores of 26.00 ± 1.91 for PCS and 19.08 ± 3.00 for MCS.
Comparative analysis of preoperative clinical parameters, including sex, age, affected segments, comorbidities, and VAS, ODI, JOA, PCS, and MCS scores, revealed no statistically significant differences between the single- and double-level groups (P > 0.05), thereby indicating comparability between the groups.
The results from both the single-level and double-level groups demonstrated that the UPSF group exhibited shorter operative times and reduced intraoperative blood loss
Comparisons of the perioperative data between the groups revealed that, for single-level patients, there were no significant differences observed in the time to ambulation after drainage tube removal or the length of hospital stay between the two groups (P > 0.05). However, operative times and intraoperative blood loss were significantly lower in the UPSF group (92.5 ± 7.9 min and 96.4 ± 20.1 mL, respectively) compared with the BPSF group (128.3 ± 6.5 min and 188.6 ± 13.5 mL, respectively) (P < 0.05) (Table 3).
Table 3.
Perioperative factors for single-segment patients
| Variable | UPSF Group | BPSF Group | P value |
|---|---|---|---|
| Surgical Time (min) | 92.5 ± 7.9 | 128.3 ± 6.5 | < 0.001 |
| Intraoperative Blood Loss (mL) | 96.4 ± 20.1 | 188.6 ± 13.5 | < 0.001 |
| Time to Ambulation (days) | 2.94 ± 0.44 | 2.82 ± 0.39 | 0.439 |
| Hospital Stay (days) | 11.1 ± 4.3 | 13.5 ± 3.1 | 0.075 |
Similarly, for double-level patients, no statistically significant differences were observed in the time to ambulation after drainage tube removal or the length of hospital stay between the two groups (P > 0.05). However, the UPSF group demonstrated significantly shorter operative times (124.8 ± 9.3 min) and reduced intraoperative blood loss (120.8 ± 14.9 mL) compared with the BPSF group (198.5 ± 12.8 min and 358.8 ± 10.9 mL, respectively) (P < 0.05) (Table 4).
Table 4.
Perioperative factors for double-segment patients
| Variable | UPSF Group | BPSF Group | P value |
|---|---|---|---|
| Surgical Time (min) | 124.8 ± 9.3 | 198.5 ± 12.8 | < 0.001 |
| Intraoperative Blood Loss (mL) | 120.8 ± 14.9 | 358.8 ± 10.9 | < 0.001 |
| Time to Ambulation (days) | 2.82 ± 0.41 | 2.83 ± 0.58 | 0.943 |
| Hospital Stay (days) | 13.6 ± 4.1 | 13.3 ± 3.3 | 0.891 |
Lower intraoperative and postoperative complication rates were observed in the UPSF group across Single- and Double-Level patients
Among the single-level patients, 3 had surgical site infections, all of which were successfully controlled via wound dressing changes and antibiotic therapy. One patient experienced postoperative radiating pain in the ipsilateral thigh, which was attributed to intraoperative nerve root traction, and the symptoms were resolved after treatment with dehydrating agents, steroids, and neurotrophic medications. Three cases of cerebrospinal fluid (CSF) leakage occurred and were resolved with compression drainage. One patient developed lower limb deep vein thrombosis (DVT), which was resolved following heparin treatment, with thrombus recanalisation confirmed at discharge. One case of postoperative circulatory failure required transfer to the intensive care unit (ICU), after which the patient returned to the general ward within 3 days and was subsequently safely discharged. The incidence of complications in the UPSF group was lower than that in the BPSF group (P = 0.040) (Table 5).
Table 5.
Perioperative complications for single-segment patients
| Parameter | UPSF Group | BPSF Group | P value |
|---|---|---|---|
| Surgical Site Infection(n, %) | 1 (3.13%) | 2 (5.88%) | 0.040 |
| Nerve Injury(n, %) | 0 | 1 (2.94%) | |
| Cerebrospinal Fluid Leakage(n, %) | 0 | 3 (8.82%) | |
| Postoperative Delirium(n, %) | 0 | 0 | |
| Hypostatic Pneumonia(n, %) | 0 | 0 | |
| Deep Vein Thrombosis(n, %) | 0 | 1 (2.94%) | |
| Circulatory Failure(n, %) | 0 | 1 (2.94%) | |
| Reoperation(n, %) | 0 | 0 |
For double-level patients, there were 4 cases of surgical site infection, which were effectively managed via timely wound care and antibiotic treatment. Two cases of CSF leakage occurred and were healed via compression drainage. One patient developed postoperative delirium, which improved after 2 days of neuropharmacological treatment. Two patients developed hypostatic pneumonia, which was treated with postural drainage, back percussion to promote sputum clearance, nebulisation therapy, and antibiotics. The symptoms of these patients (including coughing and sputum production) were resolved, and follow-up chest CT scans confirmed that the pneumonia had resolved by the time of discharge. Two cases of postoperative lower limb DVT were treated with heparin, thus resulting in thrombus recanalisation at discharge. The analysis demonstrated that the BPSF group experienced a greater incidence of complications than did the UPSF group (P = 0.009). There were no reoperations in any of the patients (Table 6).
Table 6.
Perioperative complications for double-segment patients
| Parameter | UPSF Group | BPSF Group | P value |
|---|---|---|---|
| Surgical Site Infection(n, %) | 1 (4.55%) | 3 (12.5%) | 0.009 |
| Nerve Injury(n, %) | 0 | 0 | |
| Cerebrospinal Fluid Leakage(n, %) | 0 | 2 (8.33%) | |
| Postoperative Delirium(n, %) | 0 | 1 (4.17%) | |
| Hypostatic Pneumonia(n, %) | 0 | 2 (8.33%) | |
| Deep Vein Thrombosis(n, %) | 0 | 2 (8.33%) | |
| Circulatory Failure(n, %) | 0 | 0 | |
| Reoperation(n, %) | 0 | 0 |
Progressive improvement in postoperative VAS, ODI, and JOA scores
Both the single-level and double-level patient groups demonstrated significant immediate pain relief, as evidenced by the postoperative VAS scores (P < 0.001). Pain levels remained low and continued to progressively decrease throughout the follow-up period, with further improvements being observed until the final assessment (P < 0.05).
There were no statistically significant differences observed in the VAS scores between the UPSF and BPSF groups. In the single-level group, the preoperative VAS score was 6.38 ± 0.96 for the UPSF group and 6.88 ± 0.86 for the BPSF group (P = 0.119). At 1 month after surgery, the VAS scores were 1.94 ± 0.68 vs. 2.06 ± 0.75 (P = 0.630); at 6 months, the scores were 1.06 ± 0.68 vs. 1.18 ± 0.81 (P = 0.665); and at 12 months, the scores were 0.75 ± 0.68 vs. 0.76 ± 0.75 (P = 0.954). Similarly, for the double-level group, the preoperative VAS score was 6.18 ± 0.87 for the UPSF group and 6.42 ± 0.79 for the BPSF group (P = 0.507). At 1 month after surgery, the scores were 1.82 ± 0.75 vs. 2.00 ± 0.74 (P = 0.565); at 6 months, the scores were 1.00 ± 0.76 vs. 1.17 ± 0.84 (P = 0.626); and at 12 months, the scores were 0.64 ± 0.51 vs. 0.75 ± 0.74 (P = 0.687) (Figs. 2 and 3).
Fig. 2.
VAS scores for single-segment patients
Fig. 3.
VAS scores for double-segment patients
These findings underscore the sustained and significant pain relief that was postoperatively achieved, with no substantial difference being observed between the UPSF and BPSF groups across both single-level and double-level cases.
For both single-level and double-level patients, a significant improvement in daily living ability was postoperatively observed compared with preoperative levels (P < 0.001). Over the course of follow-up, the ODI scores continuously decreased (P < 0.05).
There were no statistically significant differences observed in the ODI scores between the UPSF and BPSF groups. In the single-level group, the preoperative ODI scores were 61.88 ± 9.89 and 64.94 ± 6.13 for the UPSF and BPSF groups, respectively (P = 0.290). At 1 month after surgery, the scores were 19.13 ± 4.50 vs. 17.06 ± 4.80 (p = 0.212); at 6 months, the scores were 8.13 ± 2.47 vs. 6.94 ± 2.36 (P = 0.169); and at 12 months, the scores were 6.38 ± 1.67 vs. 6.24 ± 1.99 (P = 0.829). Similarly, in the double-level group, the preoperative ODI score was 58.18 ± 7.45 for the UPSF group and 62.50 ± 5.47 for the BPSF group (P = 0.126). At 1 month after surgery, the scores were 20.73 ± 5.61 vs. 17.17 ± 5.51 (P = 0.127); at 6 months, the scores were 8.00 ± 2.19 vs. 7.00 ± 2.00 (p = 0.265); and at 12 months, the scores were 6.55 ± 2.21 vs. 6.50 ± 1.73 (P = 0.957) (Figs. 4 and 5).
Fig. 4.
ODI scores for single-segment patients
Fig. 5.
ODI scores for double-segment patients
These results demonstrate a significant postoperative improvement in functional outcomes, with ODI scores progressively decreasing over time; moreover, no significant differences were observed between the UPSF and BPSF groups in either single-level or double-level patients.
For both single-level and double-level patients, postoperative JOA scores were significantly better compared with the preoperative JOA scores (P < 0.05), thereby indicating enhanced spinal cord and nerve function after surgery.
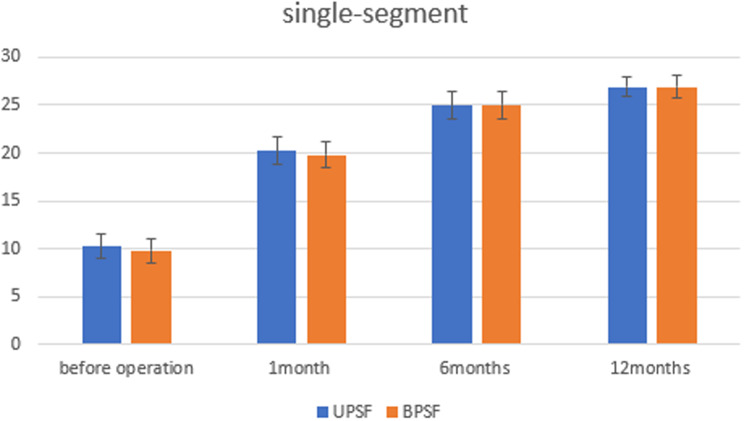
There were no statistically significant differences observed in the JOA scores between the UPSF and BPSF groups. In the single-level group, the preoperative JOA score was 10.19 ± 1.28 for the UPSF group and 9.76 ± 1.30 for the BPSF group (P = 0.354). At 1 month after surgery, the scores were 20.25 ± 1.48 vs. 19.82 ± 1.38 (P = 0.399); at 6 months, the scores were 24.94 ± 1.44 vs. 25.00 ± 1.41 (P = 0.873); and at 12 months, the scores were 26.94 ± 1.06 vs. 26.94 ± 1.14 (P = 0.992). Similarly, in the double-level group, the preoperative JOA score was 8.82 ± 1.47 for the UPSF group and 8.67 ± 1.23 for the BPSF group (P = 0.791). At 1 month after surgery, the scores were 18.27 ± 1.35 vs. 18.75 ± 1.14 (P = 0.368); at 6 months, the scores were 23.91 ± 1.30 vs. 24.42 ± 1.51 (P = 0.399); and at 12 months, the scores were 26.00 ± 0.78 vs. 26.42 ± 0.79 (P = 0.217) (Figs. 6 and 7).
Fig. 6.
JOA scores for single-segment patients
Fig. 7.
JOA scores for double-segment patients
These findings demonstrate a marked enhancement in postoperative neurological function, with no significant differences being observed between the UPSF and BPSF groups in either the single-level or the double-level patients.
Higher Long-Term quality of life scores in the UPSF group among Single- and Double-Level patients
In terms of the SF-36 score, both PCS and MCS scores were significantly improved after surgery compared with the preoperative scores for single-level patients (P < 0.05), with no statistically significant differences being preoperatively observed between the groups. However, long-term follow-up revealed that the UPSF group achieved higher PCS and MCS scores compared with the BPSF group. For PCS, the preoperative scores were not significantly different between the groups (P = 0.694), nor were the 1-month postoperative scores (P = 0.310). At 6 months, the PCS scores were significantly greater in the UPSF group (P = 0.022), and this trend persisted at 12 months (P = 0.020). Similarly, for MCS, there was no difference observed before surgery (P = 0.849) or at 1 month after surgery (P = 0.655). However, significant differences emerged at 6 months (P = 0.022) and at 12 months (P < 0.001) (Figs. 8).
Fig. 8.
PCS and MCS scores for single-segment patients
A comparable trend was observed for double-level patients. During long-term follow-up, both the PCS and MCS scores were greater in the UPSF group than in the BPSF group. For PCS, the preoperative scores were similar between the groups (P = 0.890), with no difference being observed at 1 month after surgery (P = 0.374). Significant differences were noted at 6 months (p = 0.022) and at 12 months (P = 0.023). The MCS scores followed a similar pattern, demonstrating no difference before surgery (P = 0.447) or at 1 month after surgery (P = 0.419); however, significantly higher scores were obtained for the UPSF group at 6 months (P = 0.023) and at 12 months (P < 0.001) (Figs. 9).
Fig. 9.
PCS and MCS scores for double-segment patients
These findings underscore the notion that patients in the UPSF group experienced better long-term improvements in quality of life, as reflected by both PCS and MCS scores, regardless of whether they underwent single- or double-level procedures.
Comparable outcomes in fusion and functional recovery between the UPSF and BPSF groups
According to the Bridwell fusion evaluation criteria, for single-level patients at the final follow-up, 28 patients in the UPSF group (87.5%) were classified as Grade I, and 4 patients (12.5%) were classified as Grade II, whereas 26 patients in the BPSF group (76.5%) were classified as Grade I, and 8 patients (23.5%) were classified as Grade II (P = 0.400). For double-level patients, the UPSF group included 16 patients (72.7%) classified as Grade I and 6 patients (27.3%) as Grade II, whereas the BPSF group included 20 patients (83.3%) classified as Grade I and 4 cases (16.7%) as Grade II (P = 0.608). No statistically significant differences were observed between the groups.
The modified MacNab evaluation at the final follow-up revealed that among single-level patients, 22 patients in the UPSF group were rated as excellent, 8 as good, and 2 as fair, with an excellent-to-good rate of 93.8%. The BPSF group included 24 patients rated as excellent and 10 as good, which resulted in an excellent-to-good rating of 100% (P = 0.520). For double-level patients, the UPSF group included 14 patients rated as excellent, 6 as good, and 2 as fair, with an excellent-to-good rate of 90.9%. The BPSF group included 18 patients rated as excellent, 4 as good, and 2 as fair, with an excellent-to-good rating of 91.7% (P = 0.724). No statistically significant differences were observed between the groups in these assessments.
A typical case
A 74-year-old male presented with a 5 + year history of lower back pain radiating to the right lower limb, which had worsened in the past month. His medical history included coronary atherosclerotic heart disease, hypertension, type 2 diabetes, and COPD. The patient had previously sought treatment at other hospitals, where the high surgical and anaesthetic risks led to repeated conservative treatments, including physical therapy, oral nonsteroidal anti-inflammatory drugs (NSAIDs), and acupuncture, none of which provided significant symptom relief. Upon admission, physical examination revealed reduced skin sensation and muscle strength in the L5 nerve root distribution area. The patient scored 8 on the lumbar JOA scale and 8 on the VAS for pain; moreover, the patient demonstrated an ODI score of 65. Imaging studies indicated spinal segment instability and nerve compression due to an L4/5 disc herniation. Based on the patient’s symptoms, physical findings, and imaging results, the affected segment was identified as L4/5. After meticulous preoperative planning, the patient underwent a scheduled L4/5 TLIF combined with UPSF under general anaesthesia. The surgery was completed within 100 min, and the patient was safely transferred back to the ward after surgery. On postoperative day two, the drainage tube was removed, and follow-up imaging was performed. The patient was mobilised with a lumbar brace. After surgery, the patient’s pain markedly improved; moreover, his VAS score decreased to 1 at two weeks after surgery, and no complications were observed. At the 6-month follow-up, the patient’s VAS score was 0, the ODI score was 6, and the JOA score had improved to 26 (Fig. 10: A-D: Preoperative anteroposterior and lateral lumbar X-rays and dynamic radiographs. E: Preoperative axial MRI of the L4/5 segment. F: Preoperative sagittal MRI of the lumbar spine. G-H: Postoperative radiographic evaluation).
Fig. 10.
Typical case study
Discussion
Age is the most critical factor contributing to LDD, regardless of whether it affects bone structure or soft tissue [18]. With the accelerating trend of global population ageing [19], the prevalence of LDD is increasing. This condition not only causes significant physical and psychological pain and dysfunction but also severely impacts patients’ quality of life. For patients with lumbar degenerative diseases, if conservative treatment is ineffective, lumbar fusion surgery becomes necessary [20]. Currently, TLIF is the most common method of lumbar fusion surgery [18], and it was first introduced by Harms in 1982 [21]. TLIF is indicated for the treatment of all LDDs, including degenerative disc disease, disc herniation, and spinal stenosis.
Elderly patients constitute a unique cohort. Currently, elderly individuals enjoy longer life expectancies, more active lifestyles, and higher expectations for quality of life, whereby they aim to live their remaining years free of pain [22]. However, due to their functional status, independence level, comorbidities, and frailty, elderly patients experience increased risks of surgery and postoperative complications [23, 24]. Therefore, when elderly patients with LDD are surgically treated, it is imperative to not only ensure basic clinical efficacy but also focus on improving their postoperative quality of life.
As patients age, their physiological functions (particularly those of the cardiovascular and respiratory systems) tend to decline [25]. The selection of surgical methods is crucial for treatment efficacy and postoperative recovery. Surgery can impose a significant psychological burden on elderly patients [26], especially those exhibiting potential cognitive decline or emotional instability. The reduction of the psychological impact of surgery can help patients to more quickly adapt to and accept posttreatment statuses [27]. Therefore, surgical decisions should fully consider the patient’s overall health status and postoperative quality of life to ensure the selection of the most appropriate surgical method, thereby maximising treatment efficacy and the patient’s quality of life.
Reports have indicated that the use of UPSF in TLIF offers advantages over BPSF in terms of reduced blood loss and shorter operation times while also ensuring similar vertebral fusion rates [28, 29]. However, these findings are primarily limited to single-segment cases, and specific research on patient age, comorbidities, and quality of life has not been thoroughly conducted. UPSF, which involves the treatment of only one side of the pedicle or lamina, entails a relatively small surgical scope, thereby reducing physical trauma to the patient. Conversely, BPSF, which is a more traditional fixation method [30], involves extensive bilateral fixation and requires significant intraoperative exposure of paravertebral muscles around the target segment, thereby leading to increased risks of trauma, longer operation times, higher infection risks, greater intraoperative blood loss, and postoperative incision and muscle damage [31]. Thus, for elderly patients with poorer health statuses and multiple comorbidities, UPSF may be a more advantageous option.
In our study, for elderly patients (regardless of whether they were single-segment or double-segment patients), there were no significant differences observed between the UPSF and BPSF groups in terms of average postoperative ambulation time or hospital stay duration. However, the UPSF group exhibited significantly reduced average blood loss and shorter operation times (P < 0.05), thereby indicating a lower incidence of intraoperative adverse events [32]. In terms of intraoperative and postoperative complications, the UPSF group demonstrated fewer complications compared with the BPSF group, regardless of whether patients underwent single-level (P = 0.040) or double-level (P = 0.009) procedures. All of the patients successfully completed surgery and were discharged without requiring reoperation. At the 12-month follow-up, both groups demonstrated significant improvements in the VAS, ODI, and JOA scores compared with the preoperative scores, with no statistically significant differences being observed between the groups. Follow-up indicated that in the long term, the UPSF group demonstrated better physical and mental health outcomes (as measured via the SF-36 PCS and MCS scores) compared with the BPSF group. Specifically, in single-segment patients, PCS scores were observed before surgery (P = 0.694) and at 1 month (P = 0.310), 6 months (P = 0.022), and 12 months (P = 0.020) after surgery. Moreover, MCS scores were observed before surgery (p = 0.849) and at 1 month (P = 0.655), 6 months (P = 0.022), and 12 months (P < 0.001) after surgery. In double-segment patients, PCS scores were observed before surgery (P = 0.890) and at 1 month (P = 0.374), 6 months (P = 0.022), and 12 months (P = 0.023) after surgery. Moreover, MCS scores were observed before surgery (P = 0.447) and at 1 month (P = 0.419), 6 months (P = 0.023), and 12 months (P < 0.001) after surgery. These results suggest that patients in the UPSF group had a greater quality of life than did those in the BPSF group. During the follow-up period, no instances of internal fixation loosening or breakage were observed in either group. At the final follow-up, based on the Bridwell fusion evaluation criteria, there were no statistically significant differences observed in the fusion rates between the groups, with both groups achieving excellent fusion results. The modified MacNab evaluation results revealed that the percentages of excellent and good outcomes were greater than 90% in all of the groups, with no significant differences being observed between the groups (P > 0.05).
Several limitations were noted in this study. First, the sample size was relatively small. Given that the study population consisted of elderly individuals, there was a limited number of elderly surgical patients included in this study. Thus, we plan to expand the sample size in future studies. Second, the follow-up period was relatively short (12 months), which is insufficient for exploring the long-term clinical outcomes and quality of life of elderly patients. Long-term follow-up is still necessary. Third, our study focused on patients who underwent surgical treatment and did not compare these patients with elderly patients who received conservative treatment. Future research should include comparisons with elderly patients undergoing conservative treatment. Fourth, the imaging evaluations were limited to vertebral fusion rates. Future studies should incorporate additional imaging data, such as lumbar mobility and intervertebral height. Finally, there was no information available on postoperative rehabilitation; thus, the effects of rehabilitation were not included in this study. Future research will enhance the statistical analysis in this area. Despite these limitations, the strengths of this study include the comprehensive follow-up of the enrolled patients, as well as the uses of randomised treatments, a single diagnosis, and treatments administered by a single team, thereby minimising confounding variables.
Conclusion
Our findings indicate that both surgical techniques can effectively improve the clinical outcomes and quality of life of elderly patients with LDD at the 1-year follow-up. Compared with TLIF combined with BPSF, the UPSF technique offers statistically significant advantages in terms of shorter operative times and reduced intraoperative blood loss. Moreover, this technique is associated with lower rates of intraoperative and postoperative complications. Long-term follow-ups at 6 and 12 months further demonstrated that patients in the UPSF group achieved better quality-of-life outcomes.
Acknowledgements
Not applicable.
Abbreviations
- TLIF
Transforaminal Lumbar Interbody Fusion
- UPSF
Unilateral Pedicle Screw Fixation
- BPSF
Bilateral Pedicle Screw Fixation
- LDD
Lumbar Degenerative Diseases
- VAS
Visual Analog Scale
- ODI
Oswestry Disability Index
- JOA
Japanese Orthopaedic Association
- SF-36
Short form-36 health survey questionnaire
- PCS
Physical component summary
- MCS
Mental component summary
- COPD
Chronic Obstructive Pulmonary Disease
- CAD
coronary artery disease
- CSF
Cerebrospinal fluid
- DVT
Deep vein thrombosis
- ICU
intensive care unit
- NSAIDs
nonsteroidal anti-inflammatory drugs
Author contributions
Cheng-Peng Li and Kai-Kai Feng performed all the researches and wrote the manuscript, they are first authors. Cheng-Peng Li contributed to writing original draft preparation. Xiao-Bing Xiang, Kai-Yin Gao, Zhen-Yu Nie and Wei-Wei Zhang participated in the collection of researchful data. Guang-Ru Cao conceived and designed the study. Dong Zhao and Wen-Xin Liao contributed to methodology. All authors read and approved the final manuscript. All involved subjects and the authors listed have approved the publication of the manuscript.
Funding
Project: Provincial and Ministry Jointly-Constructed Collaborative Innovation Center Project (Education and Science Technology Letter [2020] No. 39)
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The methodology and ethics were reviewed and approved of by the institutional review board of Zunyi Medical University. written informed consent was obtained from all the participants prior to the enrollment of this study.
Consent for publication
Written informed consent for publication was obtained from the participant.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
First authors: Cheng-Peng Li and Kai-Kai Feng.
References
- 1.Zhang Y, Gu Z, Xu Y, Global scientific trends in healthy aging in the early 21st century: a data-driven scientometric and visualized analysis. Heliyon. 2024;10(1):e23405. [DOI] [PMC free article] [PubMed]
- 2.Wu PH, Kim HS, Il-Tae J. Intervertebral disc diseases PART 2: a review of the current diagnostic and treatment strategies for intervertebral disc Disease. Int J Mol Sci. 2020;21(6):2135. [DOI] [PMC free article] [PubMed]
- 3.Kim HS, Wu PH, Jang IT, Lumbar degenerative disease part 1. Anatomy and pathophysiology of intervertebral discogenic pain and radiofrequency ablation of basivertebral and sinuvertebral nerve treatment for chronic discogenic back pain: A prospective case series and review of Literature. Int J Mol Sci. 2020;21(4). [DOI] [PMC free article] [PubMed]
- 4.Yuan S, Huang C, Xu Y et al. Acupuncture for lumbar disc herniation: Protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2020;99(9):e19117. [DOI] [PMC free article] [PubMed]
- 5.Lee N, Kim KN, Yi S et al. Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg. 2017;101:216–226. [DOI] [PubMed]
- 6.Hu X, Yan L, Jin X et al. Endoscopic lumbar interbody fusion, minimally invasive transforaminal lumbar interbody fusion, and open transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: a systematic review and network meta-analysis. Global Spine J. 2024;14(1):295–305. [DOI] [PMC free article] [PubMed]
- 7.Rathbone J, Rackham M, Nielsen D et al. A systematic review of anterior lumbar interbody fusion (ALIF) versus posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), posterolateral lumbar fusion (PLF). Eur Spine J. 2023;32(6):1911–1926. [DOI] [PubMed]
- 8.Mobbs Ralph J, Phan K, Malham G et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2–18. [DOI] [PMC free article] [PubMed]
- 9.Wong AX. Jie, Tang Derek Haowen, Kaliya-Perumal Arun-Kumar, The evolution of lateral lumbar interbody fusion: A Journey from Past to Present. Medicina (Kaunas). 2024;60(3):378. [DOI] [PMC free article] [PubMed]
- 10.Essa A, Shehade M, Rabau O et al. Fusion’s Location and quality within the fixated segment following transforaminal interbody fusion (TLIF). Healthcare (Basel). 2023;11(21). [DOI] [PMC free article] [PubMed]
- 11.Lu P. Pan Ting, Dai Teng, Is unilateral pedicle screw fixation superior than bilateral pedicle screw fixation for lumbar degenerative diseases: a meta-analysis. J Orthop Surg Res. 2018;13(1):296. [DOI] [PMC free article] [PubMed]
- 12.Liu F, Feng Z, Zhou X, et al. Unilateral versus bilateral pedicle screw fixation in transforaminal lumbar interbody fusion: a monocentric study of 215 patients with a minimum of 4-Year Follow-up. Clin Spine Surg. 2017;30(6):E776–83. [DOI] [PubMed] [Google Scholar]
- 13.Feng KK, Xiang XB, Li CP et al. The biomechanical effects of treating double-segment lumbar degenerative diseases with unilateral fixation through interlaminar fenestration interbody fusion surgery: a three-dimensional finite element study. BMC Musculoskelet Disord. 2025;26(1):40. [DOI] [PMC free article] [PubMed]
- 14.Chen X. Zheng Z, Lin J. clinical effectiveness of Conservative treatments on lumbar spinal stenosis: a network Meta-Analysis. Front Pharmacol. 2022;13:859296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang SK, Gu ML, Zhang T et al. Effects of exercise therapy on disability, mobility, and quality of life in the elderly with chronic low back pain: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2023;18(1):513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53(5):891–903. [PubMed]
- 17.Bridwell KH, Lenke LG, McEnery KW et al. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 1995;20(12):1410–8. [PubMed]
- 18.Huang Y, Chen J, Gao P et al. A comparison of the bilateral decompression via unilateral approach versus conventional approach transforaminal lumbar interbody fusion for the treatment of lumbar degenerative disc disease in the elderly. BMC Musculoskelet Disord. 2021;22(1):156. [DOI] [PMC free article] [PubMed]
- 19.Gietel-Basten S. Contemporary demographic challenges and population policies. Bull World Health Organ. 2024;102(4):227–A227. [DOI] [PMC free article] [PubMed]
- 20.Bydon M, Alvi MA, Goyal A. Degenerative Lumbar Spondylolisthesis. Definition, natural history, Conservative management, and surgical Treatment. Neurosurg Clin N Am. 2019;30(3):299–304. [DOI] [PubMed] [Google Scholar]
- 21.Harms J. Rolinger H. [A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl)].Z Orthop Ihre Grenzgeb. 1982;120(3):343–7. [DOI] [PubMed]
- 22.Liu C, Guo C, Meng F et al. Perioperative risk factors related to complications of lumbar spine fusion surgery in elderly patients. BMC Musculoskelet Disord. 2023;24(1):573. [DOI] [PMC free article] [PubMed]
- 23.Schenk A, Kowark A, Berger M. Pre-Interventional risk assessment in the elderly (PIRATE): development of a scoring system to predict 30-day mortality using data of the Peri-Interventional outcome study in the elderly. PLoS One. 2023;18(12):e0294431. [DOI] [PMC free article] [PubMed]
- 24.Lim BG, Lee IO. Anesthetic management of geriatric patients. Korean J Anesthesiol. 2020;73(1):8–29. [DOI] [PMC free article] [PubMed]
- 25.Izquierdo M, Merchant RA, Morley JE et al. International exercise recommendations in older adults (ICFSR): expert consensus Guidelines. J Nutr Health Aging. 2021;25(7):824–53. [DOI] [PubMed]
- 26.Srifuengfung M, Abraham J, Avidan Michael S, et al. Perioperative Anxiety and Depression in Older Adults: Epidemiology and Treatment. Am J Geriatr Psychiatry. 2023;31(11):996–1008. [DOI] [PMC free article] [PubMed]
- 27.Mennig Eva F, Schäfer, Sarah K, Eschweiler Gerhard W et al. The relationship between pre-surgery self-rated health and changes in functional and mental health in older adults: insights from a prospective observational study. BMC geriatr. 2023;23(1):203. [DOI] [PMC free article] [PubMed]
- 28.Xu LL, Xu,Wu, Chao et al. Is unilateral pedicle screw fixation as effective as bilateral pedicle screw fixation in transforaminal lumbar interbody fusion: a meta-analysis of randomized controlled trials. Eur Spine J. 2023;32(2):700–711. [DOI] [PubMed]
- 29.Cheng X, Zhang K, Sun X et al. Unilateral versus bilateral pedicle screw fixation with transforaminal lumbar interbody fusion for treatment of lumbar foraminal stenosis. Spine J. 2022;22(10):1687–1693. [DOI] [PubMed]
- 30.Chen DJ, Yao C, Song Q et al. Unilateral versus bilateral pedicle screw fixation combined with transforaminal lumbar interbody fusion for the treatment of low lumbar degenerative disc diseases: analysis of clinical and radiographic results. World Neurosurg. 2018;115:e516-e522. [DOI] [PubMed]
- 31.Motosuneya T, Asazuma T, Tsuji T et al. Postoperative change of the cross-sectional area of back musculature after 5 surgical procedures as assessed by magnetic resonance imaging. J Spinal Disord Tech. 2006;19(5):318–22. [DOI] [PubMed] [Google Scholar]
- 32.Monetta A, Griffoni C, Falzetti L et al. Prolonged operative time significantly impacts on the incidence of complications in spinal surgery. J Orthop Surg Res. 2024;19(1):567. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.