Abstract
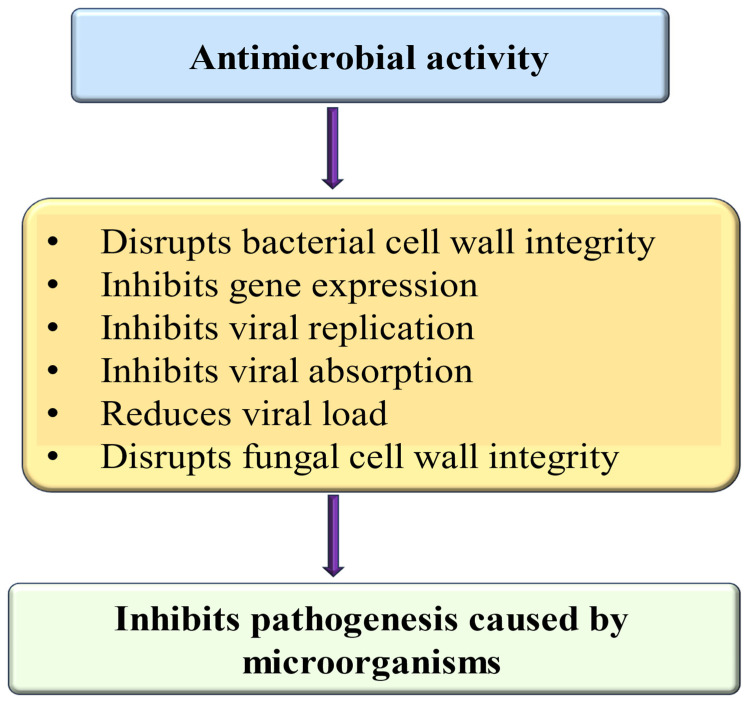
Myricetin is a natural flavonoid with powerful antioxidant and anti-inflammatory potential commonly found in vegetables, fruits, nuts, and tea. The vital role of this flavonoid in the prevention and treatment of various diseases is evidenced by its ability to reduce inflammation and oxidative stress, maintain tissue architecture, and modulate cell signaling pathways. Thus, this review summarizes recent evidence on myricetin, focusing precisely on its mechanisms of action in various pathogenesis, including obesity, diabetes mellitus, arthritis, osteoporosis, liver, neuro, cardio, and reproductive system-associated pathogenesis. Moreover, it has been revealed that myricetin exhibits anti-microbial properties due to obstructive virulence factors, preventing biofilm formation and disrupting membrane integrity. Additionally, synergistic potential with other drugs and the role of myricetin-based nanoformulations in different diseases are properly discussed. This review seeks to increase the understanding of myricetin’s pharmacological potential in various diseases, principally highlighting its effective mechanisms of action. Further wide-ranging research, as well as more randomized and controlled clinical trial studies, should be executed to reconnoiter this compound’s therapeutic value, safety, and usefulness against various human pathogenesis.
Keywords: myricetin, oxidative stress, inflammation, pathogenesis, nanoformulation
1. Introduction
Medicinal plants are commonly used in traditional cultures globally and are gaining acceptance in modern society as natural alternatives or complements to synthetic chemicals [1]. Moreover, medicinal plants are indispensable in curing most pathogeneses, as numerous human illnesses are treated with medications derived from plant components [2]. An estimated 80% of the worldwide population uses traditional medicine to treat as well as manage various diseases [3].
Medicinal plants are abundant in flavonoids, polyphenols, vitamins, and proteins, all significantly contributing to disease management. Additionally, natural products have been vital in the discovery of drugs, especially in the fields of cancer and infectious diseases [4,5]. In addition, natural products and their bioactive ingredients play a substantial role in disease management through different mechanisms [6,7,8,9,10]. Moreover, natural compounds and their bioactive constituents are abundant sources of polyphenols, phenolic acids, carotenoids, vitamins, minerals, and other nutrients, and all these constituents hold disease-management properties. Including these health-boosting substances in diets can provide better health and wellness. Flavonoids represent an important class of secondary metabolites that can be found across a wide range of sources, such as fruits, vegetables, grains, herbs, stems, seeds, nuts, and flowers [11]. More than 10,000 flavonoid compounds have been extracted and recognized [12]. Research has shown that foods high in flavonoids prevent disease development and progression. These foods/flavonoids possess numerous benefits, including anti-analgesic, anti-inflammatory, anti-cancer, anti-microbial, anti-proliferative, and neuroprotective properties [12,13,14].
Myricetin is a natural flavonoid derived from several plant sources, and its role in pathogenesis has been confirmed through different mechanisms of action, mainly through antioxidant and anti-inflammatory potential [15]. The pathogenesis prevention potential is described as myricetin, which was shown to restore the activity of the antioxidant enzymes. Additionally, the compound reduced lipid peroxidation caused by cisplatin, as well as the increase in xanthine oxidase activity and the activity of phase-II detoxifying enzymes. Myricetin also mitigated the damaging effects of cisplatin by regulating the levels of molecular inflammation markers (NF-κB, Nrf-2, TNF-α and IL-6), restoring Nrf-2 levels, and preventing the disintegration of goblet cells [16]. The study was designed to examine the beneficial role of myricetin in a diet-induced nonalcoholic steatohepatitis (NASH) model. C57BL/6J mice were administered either a standard chow diet or a choline-deficient, L-amino acid-defined, high-fat diet (CDAHFD) for a duration of 8 weeks. During this period, they received daily treatment with either myricetin (at a dose of 100 mg/kg) or vehicle by daily gavage. It was reported that myricetin ameliorated hepatic inflammation, steatosis, and inhibited hepatic macrophage infiltration in CDAHFD-fed mice. Also, myricetin-treated to CDAHFD-fed mice prevented liver fibrosis and hepatic stellate cell (HSC) activation as compared to vehicle-treated mice. Furthermore, myricetin inhibited M1 macrophage polarization as well as its relative markers in livers of NASH mice while causing the M2 polarization induction. Likewise, in in vitro findings, myricetin prevented the lipopolysaccharide (LPS)-induced mRNA expression of M1 macrophages marker genes as well as induced IL-4-induced M2 macrophage marker genes in RAW264.7 macrophages. Moreover, myricetin inhibited the expression of TLR2/4-MyD88 and triggering receptor expressed on myeloid cells-1 (TREM-1) signaling molecules in livers from NASH mice as well as in RAW264.7 macrophages stimulated by LPS [17].
Myricetin’s role in cancer is described as myricetin activating ferroptosis in gastric cancer cells by enhancing malondialdehyde production and Fe2+ accumulation while suppressing glutathione levels. Moreover, in vivo experiments confirmed that myricetin treatment meaningfully inhibited the growth of subcutaneous tumors in BALB/c nude mice [18]. Its role as a hepatoprotective was noticed as myricetin prevented hepatotoxicity via modulating the ethanol metabolizing enzymes, production of free radicals, and inflammatory markers in vivo. Myricetin maintains oxidant–antioxidant status, lipid membrane integrity, and histoarchitecture. After ethanol administration, there was an increase in the aspartate aminotransferase (AST), aspartate transaminase (AST), malondialdehyde (MDA); myricetin administration reduced the level of all these markers. Additionally, treatment of myricetin decreased ethanol-induced inflammatory markers [19]. This review described the role of myricetin in pathogenesis and how it influences different biological activities. Additionally, it discusses the synergistic effects when combined with other compounds, as well as the potential impact of nanoformulations in various pathogenesis.
2. Methodology
Search engines such as PubMed, Scopus, Google Scholar, and Web of Science were used to collect data concerning myricetin and its role in pathogenesis management. The keywords used to collect data included sources, intake of myricetin, oxidative stress, inflammation, cardioprotective effects, neuroprotective potential, and role in the respiratory and reproductive systems. Its role is in anti-obesity, wound healing, anti-cancer, bone disease, and inhibition of microorganisms. Nanoformulation based on myricetin and synergistic effect with other compounds was searched. The literature that was comprised of experimental findings, randomized controlled trials, and epidemiological studies associated with myricetin was included in this study, whereas case reports, editorials, and thesis were excluded.
3. Structure, Sources, Daily Intake, and Pharmacokinetics of Myricetin
Myricetin (3,5,7,3′,4′,5′-hexahydroxyflavone), with the chemical formula C15H10O8, has a relative molecular mass of 318.24. It is a member of the class of flavonoids/plant-derived flavonoids known as flavonols. This flavonoid is usually found in nature within berries, fruits and vegetables, typically as glycosides instead of free aglycones [20]. Additionally, flavonoids are predominantly found in their glycoside form in a variety of sources such as nuts, vegetables, herbs, fruits, plants, and beverages like tea, fruit juices, wine, and medicinal plants [21,22,23,24,25,26,27]. The amount present in various fruits and vegetables varies within different ranges. The quantities of myricetin in black fruits ranges between 14 and 142 mg/kg [24], and in honey, it ranges from 29.2 to 289 μg/100 g honey [28]. A quantity of 57.2 mg/g of myricetin per gram was extracted from the fruits of Lycium barbarum L. [29], while the skin of Carménère grapes contains 2.4 mg of myricetin per kg [30]. The concentration of myricetin in plants like Rosa canina L. (rose hip), Urtica dioica L. (nettle), and Portulaca oleracea L. (purslane) ranges from 3 to 58 mg/kg [25]. The estimated daily intake of myricetin is approximately 1.1 mg for males and around 0.98 mg for females [31]. The average daily consumption of myricetin is 2.2 ± 2.5 mg [32]. The average intake of myricetin for adults aged 18 to 64 years in the European Union is 2 mg per day, ranging between 1 and 4 mg per day [33]. The chemical structure of myricetin is shown in Figure 1.
Figure 1.
Chemical structure of myricetin (Chemical structure was made using the Chemical Sketch Tool: https://www.rcsb.org/chemical-sketch).
Myricetin’s influence on the pharmacokinetics of losartan and its active metabolite, EXP-3174, was studied in rats. The pharmacokinetic parameters for both losartan and EXP-3174 were assessed following the oral administration of losartan (9 mg/kg) to the rats, either with or without the presence of myricetin (at doses of 0.4, 2, and 8 mg/kg). Moreover, myricetin notably increased the cellular uptake of rhodamine 123 in MCF-7/ADR cells that overexpress P-glycoprotein, and this effect was dependent on the concentration. The pharmacokinetic parameters of losartan were significantly modified by myricetin in comparison to the control group. The addition of myricetin (at doses of 2 or 8 mg/kg) resulted in a 31.4–61.1% increase in the area under the plasma concentration-time curve for losartan, as well as a 31.8–50.2% rise in the peak plasma concentration of losartan. Accordingly, the absolute bioavailability of losartan in the presence of myricetin increased significantly compared with the control. As a result, the absolute bioavailability of losartan was significantly enhanced in the presence of myricetin compared to the control group. Moreover, the simultaneous administration of myricetin (8 mg/kg) led to a substantial 20% decrease in the ratio of the area under the plasma concentration-time curve for the metabolite to that of the parent drug. This advocates that myricetin might inhibit the cytochrome P450 (CYP)-mediated metabolism of losartan to its active metabolite (EXP-3174) [34]. A particular and precise ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) technique was established and verified for the detection and measurement of myricetin in rat plasma following both oral and intravenous administration. Followed by β-glucuronidase as well as sulfatase hydrolysis and liquid-liquid extraction with ethyl acetate, the analytes were separated on an Acquity UPLC BEH C18 column and studied in the selected ion recording with a negative electrospray ionization mode. The method was successfully employed to conduct a pharmacokinetic study of myricetin following both intravenous and oral administration in rats. The absolute bioavailability was found to be 9.62% for the 50 mg/kg dose and 9.74% for the 100 mg/kg dose, indicating that myricetin has limited absorption when administered orally [35].
4. Effects of Myricetin on Human Health
Scientific studies have established that myricetin offers various health benefits by modulating multiple biological activities. These benefits are mainly attributed to its anti-inflammatory and antioxidant properties, which play a significant role in the body’s response to stress as well as disease. The biological activities of myricetin are outlined below.
4.1. Antioxidant Potential
Oxidative stress (OS) is an imbalance between pro-oxidants and antioxidants, leading to dysregulation of redox processes and damage to macromolecules. Oxidative stress has harmful effects as free radicals interact with essential cellular components, for example lipids, proteins, and DNA [36]. Lipid peroxidation disrupts cell membranes, and oxidation of proteins leads to loss of function and structural integrity. Additionally, damage to DNA can lead to mutations and genomic instability [37].
Natural compounds play a substantial role in preventing pathogenesis through its antioxidant potential as well as reducing the oxidative stress [38,39,40]. Moreover, myricetin shows role in disease management through inhibition of oxidative stress related parameters. Supplementation of rat hepatocyte cultures with the myricetin directed to the formation of phenoxyl radical intermediates, as noticed in intact cells. These radicals corresponded to one-electron oxidation products of myricetin. The level of phenoxyl radicals was meaningfully decreased when myricetin-treated hepatocyte cultures were also supplemented with ferric iron nitrilotriacetate (Fe-NTA). This proposed that iron might accelerate the oxidation flux of myricetin. Furthermore, myricetin was found to be capable of preventing lipid peroxidation induced by iron in hepatocyte culture. Free malondialdehyde levels as well as the number of radicals derived from oxidized lipids were significantly decreased when myricetin was added to iron-treated cultures [41]. The antioxidant potential of myricetin on 5-fluorouracil (5-FU)-induced hepatotoxicity was examined. It was reported that the level of MDA was increased in those rats receiving the single intraperitoneal (IP)-dose of 5-FU as compared to the control group. Whereas those rats receiving the lower dose of myricetin alone caused an important reduction in MDA as compared to control group, that same difference does not appear amongst the higher dose of myricetin group. However, both groups of rats receiving both myricetin and 5-FU showed meaningfully reduced levels of MDA compared to 5-FU-only group. On the other hand, there was an important decrease in the hepatic tissue homogenate level of the superoxide dismutase (SOD) enzyme in the 5-FU-only group, whereas those rats receiving myricetin caused an important increase in SOD. The myricetin + 5-FU groups showed SOD levels that were meaningfully higher than those in the 5-FU-only group. Moreover, in the myricetin + 5-FU groups, a substantial increase in the levels of glutathione (GSH), as well as catalase (CAT), was noticed as compared to those in the 5-FU-only group [42].
The study examined the effects of toxic iron chelate, Fe-NTA, on oxidative DNA damage. This investigation was conducted both in the presence and absence of the myricetin at a concentration of 25–50–100 microM. The simultaneously increasing concentrations of myricetin, in addition to iron, effectively prevented lipid peroxidation [43]. The role of myricetin in colon toxicity was examined, and the effects of myricetin on cisplatin-caused colon toxicity were measured in terms of phase-II detoxification and enzyme antioxidant status. The results revealed that myricetin was found to restore the level of all the antioxidant enzymes, ameliorate lipid peroxidation, increase phase-II detoxifying enzyme activity, and increase xanthine oxidase activity [16]. Another study based on liver failure in mice reported that myeloperoxidase (MPO) and MDA levels were reduced, and SOD and CAT activities were improved with myricetin at doses of 50 and 100 mg/kg pretreatment. These findings suggest that myricetin protects against liver failure by regulating oxidative stress via Nrf2 signaling and that it might be a probable approach to avoid liver damage [44]. Abolfazl Barzegar 2016 demonstrated that intracellular reactive oxygen species (ROS) are highly toxic, and applying low concentrations of myricetin inhibited the cellular production of ROS. Because of the excellent correlation between cellular reactive oxygen species and their cell toxic effects, the higher antioxidant effectiveness of myricetin caused an efficient inhibited intracellular ROS and defended against cell death [45]. Treatment with aluminum phosphide increased cytotoxicity, cellular ROS formation, ATP depletion, and MDA level, and decreased the activities of antioxidant enzymes in cardiomyocytes. It was noticed that myricetin at a dose of 80 µM demonstrated ameliorated aluminum phosphide-caused cytotoxicity in isolated cardiomyocytes, meaningfully decreasing the aluminum phosphide-stimulated MDA production, intracellular ROS, and reduction of GSH, and increased the activities of SOD, catalase, and glutathione peroxidase (GSH-Px) [46]. The protective role of myricetin against tert-butylhydroperoxide (t-BHP) induced oxidative stress in human erythrocytes was examined. Incubating erythrocytes with t-BHP caused development of oxidative stress, as shown by enhancement in erythrocyte MDA and protein carbonyl content, and a reduction in intracellular-reduced GSH membrane sulphydryl (-SH) groups. Incubation of erythrocytes by myricetin, at the same time as t-BHP, protected the erythrocytes from oxidative stress [47]. A study was performed to reconnoiter the regressive effect of myricetin on pre-existing hepatic steatosis caused by a high-fat diet (HFD). Myricetin treatment meaningfully alleviated HFD-induced steatosis, reduced hepatic lipid accumulation, increased antioxidative enzyme activities and thiobarbituric acid reactive substance (TBARS) levels. Microarray analysis of hepatic gene expression profiles presented that myricetin suggestively altered the expression profiles of 177 genes which were participated in 12 biological pathways, with the peroxisome proliferator activated receptor (PPAR) signaling pathway as well as peroxisome [48]. The potential effect of myricetin on obesity was investigated. It was demonstrated that obesity-associated oxidative stress (total antioxidant capacity, glutathione peroxidase activity), malondialdehyde, and inflammation were ameliorated in mice treated with myricetin [49]. Another experiment was performed to inspect the hepatoprotective potential of myricetin against high-fat diet-induced hepatic steatosis mice, and 0.12% w/w myricetin in the diet was given to animals. Myricetin reduced HFD-induced steatosis, lipid accumulation, and TBARS levels and enhanced the glutathione peroxidase, SOD, and catalase antioxidant enzyme activities in the liver [50].
A vital study result reported that myricetin suggestively bettered diabetes-induced impairment in sensation, nerve blood flow, and nerve conduction velocities; furthermore, myricetin significantly decreased the generation of advanced glycation end-products (AGEs), elevated Na+, K+-ATPase activity and ROS, and antioxidant activities in nerves in diabetic animals. In addition, studies revealed that myricetin meaningfully elevated the hydrogen sulfide (H2S) levels and elevated the expression level of nuclear factor-E2-related factor-2 (Nrf2) as well as heme oxygenase-1 (HO-1) in diabetic rats [51].
4.2. Anti-Inflammatory Effects
Flavonoids and natural compounds exhibited anti-inflammatory effects [52,53,54] by reducing the production of pro-inflammatory agents and downregulating cyclooxygenase-2 (COX-2) expression. Moreover, the flavanols have confirmed the ability to inhibit lipoxygenase [55]. This action reduces the production of key inflammatory substances, including prostaglandins, leukotrienes, and nitric oxide [56]. Flavonoids also diminish the release of metabolites from arachidonic acid and chemokines, which helps to reduce leukocyte infiltration and edema [57]. Furthermore, flavonoids can chelate iron and inhibit the activation of the complement system, contributing to a decrease in inflammation [58].
Myricetin revealed its anti-inflammatory potential by reducing the production of pro-inflammatory agents and downregulating COX-2, inducible nitric oxide synthase (iNOS) expression, and other mechanisms. Myricetin reduced the production of pro-inflammatory mediators in LPS-stimulated RAW264.7 macrophages in a dose-dependent manner. The administration of myricetin also led to a decrease in the levels of iNOS, NO, IL-6, TNF-α, and IL-12 in mice. Furthermore, myricetin inhibited NF-κB activation by preventing the degradation of IκBα, nuclear translocation of the p65 subunit of NF-κB, and NF-κB DNA binding activity in LPS-stimulated RAW264.7 macrophages. Furthermore, myricetin reduced the phosphorylation of STAT1 as well as the production of IFN-β in LPS-stimulated RAW264.7 macrophages [59]. The effects of myricetin on the expression of cyclooxygenase 2 COX-2 in H9c2 cells treated with peptidoglycan (PGN) from Streptococcus sanguinis, a bacterial constituent of dental plaque linked with infective endocarditis, was investigated. Myricetin exposure caused in dose-dependent decrease of PGN-induced expression of COX-2 reduced phosphorylation of p38, extracellular signal regulated kinase 1/2, as well as c-Jun N-terminal kinase, and reduced IκB-α degradation, consistent with COX decreased -2 activity. The results advocate that myricetin is valuable in moderating the inflammatory response in infective endocarditis [60]. The potential of myricetin to modulate LPS-stimulated activation of mouse bone marrow-derived dendritic cells (DCs) was evaluated. It was reported that myricetin significantly reduced the secretion of tumor necrosis factor-α, interleukin-6, and interleukin-12p70 by LPS-stimulated DCs. Myricetin showed a role in the inhibition of expression of LPS-induced major histocompatibility class II, CD40, as well as CD86 on DCs, and the migratory and endocytic capacity of LPS-stimulated DCs was blocked by myricetin. Furthermore, by myricetin, LPS-stimulated DC-elicited allogeneic T-cell proliferation was reduced. Moreover, this outcome established that myricetin reduces the responses of LPS-stimulated activation of DCs through suppression of IκB kinase/nuclear factor-κB as well as mitogen-activated protein kinase-dependent pathways [61]. A study was made to explore whether myricetin was effective in improving sepsis-induced myocardial dysfunction in cardiomyocyte injury. Myricetin considerably produces inflammatory cytokines both in serum and cardiac tissue and inhibits degradation of IκBα, nuclear translocation of p65, and cellular apoptosis. This compound prevented the reduction of oxidoreductase activity and overexpression of iNOS. Furthremore, myricetin treatment could decrease inflammatory cytokines production of peritoneal macrophages stimulated with LPS in vitro [62]. This compound inhibits the upregulation of COX-2 by blocking IκB/NFκB, Akt, and mammalian target of rapamycin (mTOR) signaling. It also decreases the production of cytokines and chemokines in keratinocytes, ultimately mitigating skin inflammation caused by TNF-α and ultraviolet light [63,64]. An interesting study result reported that myricetin dose-dependently inhibited the production of pro-inflammatory mediators in LPS-stimulated RAW264.7 macrophages. Myricetin treatment decreased the production of tumor necrosis factor alpha (TNF-α), Interleukin- 6,12 (IL-6,12), nitric oxide (NO), and iNOS, in mice [59]. Pretreatment with myricetin and its effects on decreased the up-regulation of matrix metalloproteinase 1 (MMP-1) and IL-6, as well as inhibiting the phosphorylation of p38 and JNK in human synovial sarcoma cells in vitro [65]. The effects of apigenin and myricetin against cisplatin-induced nephrotoxicity were examined. Treatment of mice with cisplatin demonstrated a substantial increase in serum levels of IL-6 and TNFα. Then again, treatment with myricetin apigenin, or their combination, improved the above-mentioned increase in serum levels of TNFα [66]. An experiment was performed to explore the role of myricetin in colon toxicity and it was reported that myricetin reduced deteriorative effects by regulating the level of molecular markers of inflammation and controlling goblet cell disintegration [16]. Myricetin significantly reduced lung inflammation as marked by the reduced concentration of protein in the bronchoalveolar lavage fluid (BALF), wet-to-dry weight ratio of lungs, activity of MPO, cytokine production, and inflammatory cell migration. Moreover, the reduction was also noticed in toll-like receptor 4 (TLR4), nuclear factor-kappa B (NF-κB), and MyD88 expression [67].
The extracts as well as active compounds of Chinese bayberry were used to check the chemical antioxidant potential and anti-inflammatory activities in Propionibacterium acnes (P. acnes)-stimulated human SZ95 sebocytes. Consequently, the flavonols, myricetin and myricitrin, were found to be rich in the unhydrolyzed and hydrolyzed extracts of Chinese bayberry fruits, correspondingly. The anthocyanin cyanidin-3-glucoside was also mainly found in the unhydrolyzed extracts. Quantification of human inflammatory cytokines designated that cell-free extracts of P. acnes stimulated IL-8 and IL-6 production, which was prevented by myricetin. Myricetin also showed inhibitory effects in P. acnes-stimulated gene expression of TLR2 as well as protein phosphorylation of p70 S6 kinase [68]. Cells treated with myricetin prevented anti-Fas IgM-induced apoptosis and blocked the synergetic effect of anti-Fas IgM with TNF-alpha or IL-1beta on cell death [69]. A pioneer study reported that myricetin effectively reduced the expression of several indicators of the neuroinflammatory response in LPS-induced activated microglia [70]. Myricetin effectively enhanced the inflammatory response by blocking the AKT/IKK/NF-κB signaling pathway and restoring the integrity of the blood–milk barrier in mice with LPS-induced mastitis [71].
4.3. Hepatoprotective Effects
Liver diseases contribute significantly to global rates of illness and death [72]. Chronic liver diseases have become a substantial cause of death and morbidity over the last decade, leading to approximately two million deaths each year worldwide [73]. The primary contributors to chronic liver disease include non-alcoholic fatty liver disease, hepatitis B and C, cirrhosis, and hepatocellular carcinoma. These conditions, along with their complications, play a major role in liver-related mortality [74]. Various types of drugs, including synthetic drugs, are used to treat this pathogenesis. Unfortunately, such treatment leads to negative side effects. Various natural compounds and their bioactive constituents have been confirmed to show a hepatoprotective role by reducing oxidative stress and inflammation and maintaining liver tissue morphology [75,76,77]. The role of myricetin in the inhibition of liver pathogenesis through modulation of different mechanisms is presented in Figure 2.
Figure 2.
Hepatoprotective potential of myricetin through different mechanisms (the liver image used in the figure is from our lab). The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
Moreover, the role of myricetin as a hepatoprotective is summarized in Table 1 as per the previous studies. To explore the role of myricetin in vivo, carbon tetrachloride (CCl4) was induced to develop liver fibrosis. Hematoxylin and eosin (H&E), and Sirius-red staining reported a noticeable increase in the amount of liver fibrosis. Myricetin treatment reduced the amount of liver fibrosis and ameliorated the increase in serum ALT and AST activity caused by CCl4. The anti-fibrotic potential of myricetin in CCl4-treated mice was reported by measuring the effects of myricetin on α-smooth muscle actin (α-SMA) and collagen type I (Col1) protein expression. The Col1 and α -SMA expression were meaningfully reduced in fibrotic mice treated with myricetin [78]. Study findings described that myricetin improved high-fat diet (HFD)-induced hepatic steatosis and TH levels, increased hepatic type 1 deiodinase activities, and elevated energy expenditure concerning the HFD mice. At the same time, myricetin inhibite the upregulation of miR-205 and miR-146b caused by a HFD [79]. Another study finding exhibited that myricetin efficiently protects from LPS/D-GalN-induced fulminant hepatitis by lowering AST and ALT levels and improving oxidative stress, histopathological changes, hepatic apoptosis, and inflammation; furthermore, myricetin efficiently mediates multiple signaling pathways. Myricetin relieved hepatotoxicity excited by H2O2 and was inhibited by Nrf2-null and AMPK inhibitors [80]. Myricetin decreased the fatality rate of animals, pathological liver changes, improved liver function enzymes (ALT, AST, and ALP), decreased apoptotic, inflammatory factors, and oxidative, and enhanced some antioxidants. In addition, myricetin improved the activity of sirtuin 1 and hepatic level and reversed inappropriate alterations of autophagic parameters [81]. Myricetin inhibited hepatotoxicity by modulating the production of free radicals and inflammatory markers in vivo. Myricetin maintained oxidant–antioxidant status, lipid membrane integrity, and liver tissue architecture. Administration of ethanol increases the hepatotoxicity biomarkers, and myricetin administration reduces the level of these markers [19]. The role of myricetin supplementation on HFD-induced nonalcoholic fatty liver disease (NAFLD) in rats was examined. The 12-week supplementation with myricetin and fecal microbiota transplantation indicates that myricetin significantly decelerates the progression of NAFLD. Myricetin reduces hepatic lipid synthesis and inflammation by modulating the gut microbiota related to fecal butyric acid [82]. Another finding reported that myricetin and apigenin pretreatments increased liver GSH levels and CAT and SOD activities, albumin and total protein levels, and decreased serum liver function enzymes in LPS-treated mice.
Table 1.
Hepatoprotective activities of myricetin through different mechanisms.
| Activity | Study Types | Dose | Outcome | Ref. |
|---|---|---|---|---|
| Hepatoprotective effect | In vivo, mice model | 50 mg/kg |
|
[78] |
| In vivo, mice model | 100 mg/kg |
|
[79] | |
| In vivo, mice model | 25, 50, 100 mg/kg |
|
[80] | |
| In vivo, mice model | 25 or 100 mg/kg |
|
[81] | |
| In vivo, rat model | 25, 50 mg/kg |
|
[19] | |
| In vivo, rat model | HFD containing 0.5% myricetin |
|
[82] | |
| In vivo, mice model | 100, 200 mg/kg |
|
[83] | |
| In vivo, mice model | 25, 50, 100 mg/kg |
|
[44] | |
| In vivo, mice model | Diet containing 0.04% or 0.08% myricetin |
|
[84] | |
| In vivo, mice model | 100 mg/kg |
|
[17] | |
| In vitro, LPS-stimulated RAW264.7 macrophages | 50 μM |
|
[17] | |
| In vivo, rats | 25, 50 mg/kg |
|
[19] |
Myricetin and apigenin administration also maintained the hepatic architecture disrupted during LPS administration [83]. Xia Wang et al., 2023 reported as myricetin pretreatment decreased serum ALT and AST and improved the pathological changes of liver tissues induced by lipopolysaccharide (LPS)/D-galactosamine (D-Gal). Furthermore, MPO and MDA levels were reduced, SOD and CAT activities were increased with myricetin (50 and 100 mg/kg) pretreatment [44]. The beneficial effects of myricetin against non-alcoholic fatty liver disease were noticed by the regulation of hepatic lipid metabolism transcription factors, pro-inflammatory cytokines, and the antioxidant system [84]. Myricetin improved hepatic inflammation and steatosis and inhibited hepatic macrophage infiltration in CDAHFD-fed mice [17]. Sheikh Bilal Ahmad et al., 2022 reported that myricetin prevented hepatotoxicity by modifying the production of free radicals and inflammatory markers in vivo. Myricetin maintained oxidant–antioxidant status, lipid membrane integrity, and liver tissue architecture [19].
4.4. Anti-Diabetic Potential
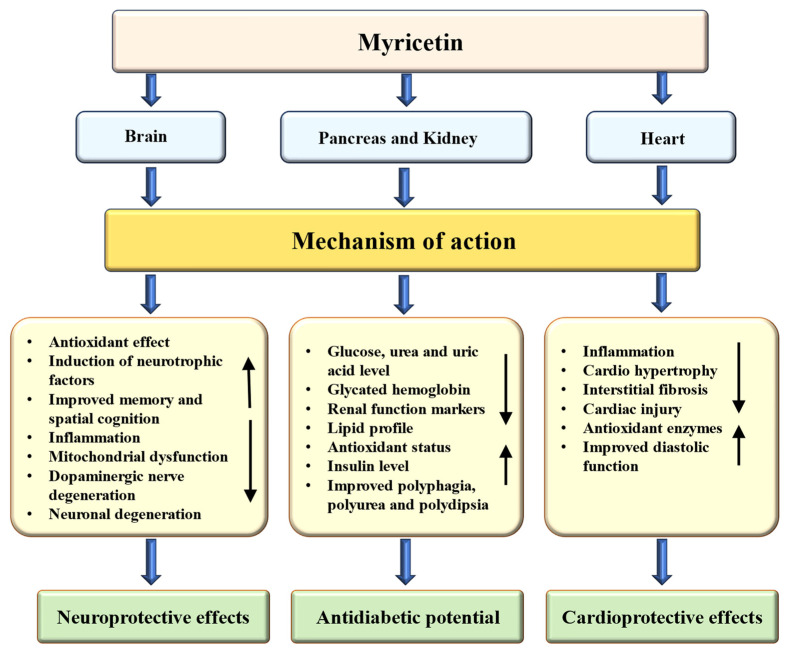
Fruits, leaves, seeds, bark, and peels are frequently acknowledged as rich sources of bioactive phytochemicals that may aid in addressing various health concerns [85,86]. A range of natural compounds and their bioactive components have been shown to have anti-diabetic effects by decreasing inflammation and oxidative stress while preserving the structure of liver and kidney tissues [87,88,89]. The role of myricetin in the management of diabetes and its associated complications is summarized in Table 2. Myricetin’s role as an anti-diabetic through the modulation of different mechanisms is presented in Figure 3.
Figure 3.
Anti-diabetic, neuroprotective and cardioprotective potential of myricetin through various mechanisms. The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
The role of myricetin was examined by enzymes of carbohydrate metabolism and renal function markers in streptozotocin (STZ)-cadmium (Cd) induced diabetic nephrotoxic animals. The innovative finding was noted as a substantial rise of plasma glucose, urea, uric acid, hemoglobin, and creatinine, and a substantial decrease of plasma insulin, hexokinase, hemoglobin, and glycogen were noticed in the STZ-Cd-induced diabetic rats. The administration of myricetin meaningfully normalizes the carbohydrate metabolic products like gluconeogenic enzymes, glycated hemoglobin, glucose, and glycogen phosphorylase, and renal function markers with increased insulin, glycogen, and glycogen synthase [90]. Diabetic nephrotoxic rats exhibited meaningfully elevated levels of urinary albumin along with altered lipid profiles. Alongside this, there was a decrease in the activities of lecithin cholesterol acyl transferase and lipoprotein lipase. Treatment with myricetin was found to normalize these parameters. Furthermore, the administration of myricetin led to a decrease in interstitial fibrosis glomerulosclerosis and an expansion of the extracellular mesangial matrix in diabetic nephrotoxic rats. Also, myricetin confirmed considerable protective effects against the lipid metabolism alterations induced by STZ-Cd, thereby mitigating diabetic nephropathy in the experimental rats [91].
To prove the role of myricetin in improving the symptoms of type 2 diabetes, as well as controlling the intestinal flora in a type 2 diabetes mouse model, Iit was noticed that fasting blood glucose and blood lipid levels of Type 2 diabetes mellitus (T2DM) mice were significantly decreased by myricetin treatment, whereas there were increased SOD levels. Myricetin improved polydipsia, polyuria, polyphagia and weight loss in T2DM mice [92]. It was reported that myricetin reduced diabetic cardiomyopathy-associated cardiac damage in mice subjected to streptozotocin and in neonatal rat cardiomyocytes challenged with high glucose. Myricetin treatment meaningfully alleviated cardiac hypertrophy and interstitial fibrosis apoptosis mechanically. Myricetin treatment increased the activity of the Nrf2/HO-1 pathway, strengthening antioxidative stress capacity and decreasing MDA production. These beneficial effects of myricetin treatment protected cardiomyocytes from apoptosis [93]. Myricetin alleviated renal dysfunction, oxidative damage, and fibrosis induced by diabetes mellitus while enhancing the expression of Nrf2 and its target genes. After Nrf2 was knocked down, myricetin treatment still significantly reduced diabetes-induced renal dysfunction and fibrosis. It was concluded that myricetin prevented the diabetes-associated decrease in expression of Nrf2 and the IκB/NF-κB (P65) signaling pathway was inhibited [94].
A recent finding reported that myricetin improves cardiac function in diabetic cardiomyopathy mice by decreasing interstitial fibrosis and cardiomyocyte hypertrophy. Moreover, myricetin caused an increase in occludin expression and the number of goblet cells in diabetic cardiomyopathy mice. Compared with diabetic cardiomyopathy mice unfed with gut content, the expression of occludin, the cardiac function, and the number of goblet cells in diabetic cardiomyopathy mice fed by gut contents were higher, whereas TLR4/MyD88 pathway-related proteins and cardiomyocyte hypertrophy were reduced [95]. The mechanism of myricetin, on a high-fat diet (HFD) fed streptozotocin (STZ) induced diabetic rats was investigated. The results exhibited that administration of myricetin in HFD/STZ-induced diabetic rats dose-dependently reduced the serum glucose as well as insulin. Moreover, myricetin protected pancreatic tissue from HFD-fed STZ-induced apoptosis. The experimental results indicate that myricetin offers noteworthy health benefits and could be measured an auspicious dietary complement for supporting treatment of hypoglycemic [96].
A study was made to reconnoiter the role of myricetin on insulin resistance in rats fed with a diet containing fructose. Frequent intravenous injection of myricetin was found to reduce the high triglyceride and glucose levels. Moreover, the higher degree of insulin resistance in fructose-chow-fed rats was diminished by myricetin treatment. Also, treatment with myricetin reversed the decreased insulin action on the phosphorylation of insulin receptors, insulin receptor substrate 1, and Akt in the soleus muscle of rats [97]. Diabetic nephrotoxic rats exhibited a significant increase in the activities of hepatic and renal functional markers in their plasma. This was accompanied by an increase in albumin levels and urine volume. After 30 days of treatment with intraperitoneal administration of myricetin, the diabetic nephrotoxic rats showed significant protective effects on all the biochemical parameters examined. The results indicate that myricetin at a 1.0 mg/kg body weight dose demonstrates a greater antihyperglycemic and renoprotective effect [98]. Filiz Ozcan et al. (2012) reported that myricetin treatment reduced blood urea nitrogen (BUN) and urinary volume, decreased glomerulosclerosis, and decreased protein excretion, which was intensely increased in diabetic rats. Reduced creatinine clearance measured in diabetic rats was increased after treatment of myricetin. The study revealed that myricetin restored renal activities of glutathione peroxidase (GPx) and xanthine oxidase (XO), and improved altered renal functions in diabetic rats [99]. Myricetin, administered at an effective dose of 1.0 mg/kg, decreased the rise in plasma glucose levels. Additionally, myricetin demonstrated a concentration-dependent stimulatory effect on glucose uptake in the soleus muscles isolated from STZ-diabetic rats [100].
Table 2.
Anti-diabetic activities of myricetin through different mechanisms.
| Activity | Types of Study | Doses | Findings | Ref. |
|---|---|---|---|---|
| Anti-diabetic potential | Male albino Wistar rats, in vivo | 1.0 mg/kg bw |
|
[90] |
| Male albino Wistar rats, in vivo | 1.0 mg/kg bw |
|
[91] | |
| Male mice, in vivo | 75, 150 and 300 mg/kg |
|
[92] | |
| Mice model, in vivo | 200 mg/kg/day |
|
[93] | |
| Mice model, in vivo | 100 mg/kg/day |
|
[94] | |
| Rat model, in vivo | 50 and 200 mg/kg body weight |
|
[96] | |
| Rats model, in vivo | 1 mg/kg per injection |
|
[97] | |
| Rats model, in vivo | 0.5, 1.0 and 1.5 mg/kg bw |
|
[98] | |
| Rats model, in vivo | 6 mg/day |
|
[99] | |
| Rats model, in vivo | 1.0 mg/kg |
|
[100] |
4.5. Cardioprotective Effects
Cardiovascular diseases (CVDs) rank among the top causes of illness and death worldwide, with increasing incidence rates and declining age of onset in recent years [101]. Various biochemical, genetic, environmental, as well as behavioral factors can play a role in the emergence of cardiovascular diseases [102]. As far back as the 1990s, epidemiological studies showed a link between higher consumption of flavonoid-rich diets and a reduced incidence of cardiovascular disease [103]. The role of myricetin in the management of cardio-associated pathogenesis is summarized in Table 3. Myricetin’s role as cardioprotective through the modulation of different mechanisms is presented in Figure 3.
Recently, numerous studies have highlighted the preventive and therapeutic benefits of flavonoids for the cardiovascular system, both on their own and in combination with other agents [104]. Lipopolysaccharide significantly impaired the mouse cardiac function, but myricetin administration markedly improved it. Myricetin also substantially decreased the production of inflammatory cytokines in both serum and cardiac tissue. Myricetin has been shown to inhibit the degradation of IκBα, nuclear translocation of p65, and cellular apoptosis, both in vivo and in vitro [62]. Pretreatment with myricetin (100 mg/kg and 300 mg/kg, both administered orally) for 21 days significantly reduced the effects of isoproterenol on heart rate, as well as levels of AST, LDH, CK, and SOD, and CAT [105]. A study found that myricetin significantly reduced the overexpression of IL-1beta, IL-6, and TNF-alpha by inhibiting the NF-κB/P65 signaling pathway. Additionally, treatment with myricetin resulted in lower levels of reactive oxygen species (ROS) and increased the expression of superoxide dismutase and glutathione peroxidase [106]. In comparison to the I/R group, pretreatment with 5μM myricetin improved several cardiovascular parameters. This treatment enhanced the maximum up/down rate of left ventricular pressure (dp/dtmax) and coronary flow, increased left ventricular developed pressure, and reduced levels of creatine kinase. Additionally, myricetin was found to have beneficial effects by decreasing both infarct size and cardiomyocyte apoptosis. It also demonstrated antioxidant properties, evidenced by a reduction in malondialdehyde (MDA) levels, alongside an increase in superoxide dismutase (SOD) levels and an improved glutathione (GSH)/glutathione disulfide (GSSG) ratio [107]. In vivo studies showed that myricetin treatment alleviated cardiac hypertrophy, apoptosis, and interstitial fibrosis. Mechanistically, myricetin significantly enhanced the activity of the Nrf2/HO-1 pathway, which improved oxidative stress resistance. This was evidenced by increased activity of GPx and SOD, alongside decreased production of MDA. The protective effects of myricetin treatment on cardiomyocytes were demonstrated by a reduction in terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL)-positive nuclei, c-caspase 3, and Bax, indicating decreased apoptosis [93]. In vitro, studies demonstrated that pretreatment with myricetin notably lowered the expression of inflammatory cytokines triggered by advanced glycation end-products (AGEs), while also reducing cell apoptosis, fibrosis, and hypertrophy in H9c2 cells. In vivo investigations demonstrated that oral administration of myricetin markedly lowered the expression of enzymes linked to cardiomyopathy. Additionally, myricetin improved diastolic dysfunction and alleviated histological changes [108]. Myricetin may enhance cardiac function in mice with diabetic cardiomyopathy by reducing cardiomyocyte hypertrophy and interstitial fibrosis. It has been shown to increase the expression of occludin and the number of goblet cells in these mice. When comparing diabetic cardiomyopathy (DCM) mice that were not fed gut content with those that were, the latter demonstrated improved cardiac function, increased goblet cells, and higher occludin expression. Conversely, the DCM mice that were fed gut content exhibited a decrease in cardiomyocyte hypertrophy and in the levels of proteins related to the TLR4/MyD88 pathway [95].
Myricetin reduced cardiac injury caused by doxorubicin, leading to decreased levels of cardiac troponin I (cTnI), AST, lactate dehydrogenase (LDH), and brain natriuretic peptide (BNP). It also improved myocardial injury and fibrosis. Furthermore, myricetin effectively prevented doxorubicin-induced oxidative stress by increasing the activities of GSH, SOD, CAT, and lowered MDA levels [109]. After 21 days of treatment, it was observed that myricetin significantly reduced myocardial injury in mice with experimental autoimmune myocarditis and the treatment led to a decrease in serum levels of anti-cardiac myosin antibodies [110]. A study was planned to explore the effects of myricetin against 5-FU-caused cardiac injury in rats. It was noticed that 5-FU injection caused inflammation, extensive cardiac damage and oxidative stress. However, myricetin lessened markers of inflammation, oxidative stress, apoptosis, and cardiac toxicity [111]. Myricetin exposure caused dose-dependent suppression of PGN-induced COX-2 expression and reduced IκB-α degradation, consistent with decreased COX-2 activity. The above-mentioned results advise that myricetin is useful for regulating the inflammatory response in infective endocarditis [60].
Table 3.
Cardioprotective activities of myricetin through different mechanisms.
| Activity | Model | Dose | Outcome | Ref. |
|---|---|---|---|---|
| Mice, in vivo | 100 mg/kg |
|
[62] | |
| Wistar rats, in vivo | 100 and 300 mg/kg, p.o |
|
[105] | |
| H9c2 cardiomyocyte cell line, in vitro | 5, 10, 20, 40 Μm |
|
[106] | |
| Rat model, in vivo | 5 μM |
|
[107] | |
| Mice model, in vivo | 200 mg/kg/d |
|
[93] | |
| H9c2 cells, in vitro | 25 μg/mL |
|
[108] | |
| Mice model, in vivo | 300 mg/kg/day |
|
[108] | |
| Male rats, in vivo | 2.5 mg/kg and 5 mg/kg |
|
[109] | |
| Rats model, in vivo | 25 and 50 mg/kg |
|
[111] | |
| H9c2 cells, in vitro | 1, 5, 10, & 15 μM |
|
[60] |
4.6. Neuroprotective Effects
Neurodegenerative diseases are a heterogeneous group of disorders considered by progressive damage as well as loss of neurons in different areas of the central or peripheral nervous system [112]. Neurodegenerative disorders such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis affect millions of people worldwide, resulting in substantial socio-economic challenges [113]. There are several medications available for treating this pathogenesis; however, these drugs may lead to undesirable side effects. However, safe alternative medicines are needed to overcome these adverse effects and play a role in preventing this condition. The role of myricetin in the management of neuro-associated pathogenesis is summarized in Table 4. Myricetin’s role as neuroprotective through the modulation of different mechanisms is presented in Figure 3.
Matin Ramezani et al., 2016, investigated the potential effects of myricetin and it significantly improved learning and memory impairments and increased the number of hippocampal CA3 pyramidal neurons in rats with Alzheimer’s disease [114].
Myricetin treatment improved learning memory and ameliorated tau phosphorylation and reduced pre- and postsynaptic proteins in Aβ42 oligomer-treated neuronal SH-SY5Y cells and 3 × Tg mice [115]. The effect of myricetin on Alzheimer’s disease (AD) and its causal mechanisms were studied. Myricetin efficiently reduced Fe2+-induced cell death in SH-SY5Y cells in vitro. In a mouse model of AD, myricetin treatment meaningfully reversed scopolamine-induced cognitive deficits and down-regulating brain iron. Consequently, it was suggested that myricetin treatment reduced mice’s cognitive deficits by preventing AChE and brain iron regulation [116]. The Parkinson’s disease (PD) models were made by treating SH-SY5Y cells with 1-methyl-4-phenylpyridinium (MPP+) and injecting 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) into rats, correspondingly. The results confirmed that myricetin treatment efficiently mitigated MPTP-triggered motor impairment, α-synuclein (α-Syn) accumulation, and dopamine neuronal death in PD models. In vitro, myricetin treatment restored SH-SY5Y cell viability as well as alleviated MPP+-induced SH-SY5Y cell ferroptosis [117]. The role of myricetin in Parkinson’s disease models based on in vivo and in vitro experiments was explored. Myricetin treatment suppressed the expression of pro-inflammatory mediators, the activation of microglia, and the reduction in the number of dopaminergic neurons, as well as ameliorated the rats’ motor dysfunction. Also, myricetin inhibited the activation of the mitogen-activated protein kinase (MAPK) and NF-κB pathways and the production of pro-inflammatory mediators in activated microglia. Based on these results, myricetin inhibits dopaminergic neuron degeneration via inhibiting microglial neuroinflammation [118]. Rotenone administration caused dopaminergic neuronal degeneration, memory decline, impaired muscular coordination, dopamine depletion, gait disturbances, oxidative stress, and apoptosis. The ingestion of myricetin by Drosophila meaningfully prevented neuronal degeneration caused by rotenone [119]. Myricetin demonstrated a dose-dependent increase in antioxidative activity. When PD flies were exposed to various concentrations of myricetin, there was a significant dose-dependent rise in dopamine levels compared to unexposed PD flies. Additionally, myricetin helped protect against the loss of dopaminergic neurons in the brains of the PD flies [120]. The effects of myricetin on 6-hydroxydopamine (6-OHDA)-induced neurodegeneration was tested. The dopamine content in the striatum was reduced after 6-OHDA treatment, which was restored by myricetin treatment. Moreover, it showed that myricetin prevented the 6 -OHDA-induced decrease of tyrosine hydroxylase positive neurons [121]. The role of the myricetin, in a pentylenetetrazole (PTZ)-induced mouse model of epilepsy was examined. Myricetin treatment reduced the mortality rate and seizures. Elevated expression levels of apoptotic proteins and increased apoptotic cell count caused by PTZ were downregulated following myricetin treatment. The results of the study showed that myricetin may cause protective effects via regulating the molecular events associated with epileptogenesis [122]. It significantly enhanced the activities of antioxidant enzymes and lowered markers of oxidative stress. Myricetin also effectively decreased the levels of pro-inflammatory cytokines, showing its anti-inflammatory properties. Behavioral evaluations indicated that myricetin improved motor functions and cognitive abilities in PTZ-treated mice, leading to a notable reduction in mortality rates and severity of seizures [123].
Table 4.
Neuroprotective activities of myricetin through different mechanisms.
| Disease | Types of Study | Model | Doses | Outcome | Ref. |
|---|---|---|---|---|---|
| Alzheimer’s disease | In vivo | Rat models | 5 or 10 mg/kg |
|
[114] |
| In vivo | Mice model | 20 mg/kg |
|
[115] | |
| In vitro | SH-SY5Y cells | 5–20 µM |
|
[115] | |
| In vitro | SH-SY5Y | 4, 1, 0.25, 0.063, 0.016 µM |
|
[116] | |
| In vivo | Mice model | 25 or 50 mg/kg |
|
[116] | |
| Parkinson’s disease | In vitro | SH-SY5Y cells | 50 µM |
|
[117] |
| In vivo | Rat model | 25 g/kg |
|
[117] | |
| In vivo | Rat model | 2.5, 5, or 10 mg/kg |
|
[118] | |
| In vitro | SH-SY5Y cells | 12.5, 25, 50 µM |
|
[118] | |
| In vivo | Drosophila model | 250, 500, 750, 1000 µM |
|
[119] | |
| In vivo | Drosophila Model | 10, 20 and 40 μM |
|
[120] | |
| Epilepsy | In vivo | Mice model | 50, 100 mg/kg |
|
[122] |
| In vivo | Mice model | 200 mg/kg |
|
[123] |
4.7. Anti-Cancer Potential
Cancer poses a severe threat to both physical and mental health, with high incidence and mortality rates globally [124,125]. Presently, the leading treatments for cancer consist of radiotherapy, chemotherapy, and surgical procedures. Despite their effectiveness, these approaches have limited efficacy and may also lead to negative side effects. Ongoing research and development efforts are focused on discovering new cytotoxic compounds from medicinal plants that exhibit antiproliferative activity [126] and in vitro studies have shown the activities of flavonoids on tumor cells, such as the inhibition of cell growth and alteration of tumor invasive behavior [127]. Various medicinal plants and their bioactive compounds, including myricetin, demonstrate anti-cancer potential both in vivo and in vitro by modulating cell signaling pathways. Natural compounds and their bioactive compound role in cancer management have been established through their ability to target several molecules and signaling pathways, including those involved in angiogenesis, cell cycle, apoptosis, autophagy, tumor suppressor genes, and inflammation [128,129,130]. Myricetin’s role as an anti-cancer through the modulation of different mechanisms is presented in Figure 4. Moreover, the role of myricetin in the management of cancer is summarized in Table 5. A study focused on ovarian cancer found that myricetin inhibited the secretion of the angiogenesis mediator vascular endothelial growth factor (VEGF) and reduced the levels of p-Akt and hypoxia-inducible factor-1α (HIF-1α) proteins in ovarian cancer cells. Additionally, an innovative pathway involving p21/HIF-1α/VEGF was involved in myricetin’s repressing effect on angiogenesis in cancer cells [131]. Another study based on both in vivo and in vitro experiments revealed that myricetin reduced vascular endothelial growth factor levels. Additionally, Western blot analysis indicated that myricetin downregulated the expression of p38MAPK and VEGFR2 [132].
Figure 4.
Anti-cancerous effects of myricetin via modulation of cell signaling molecules. The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
Table 5.
The potential role of myricetin in prevention of cancer.
| Cancer | Modulation | Study Types | Model | Mechanism | Outcome | Refs. |
|---|---|---|---|---|---|---|
| Ovarian | Angiogenesis | In vitro | OVCAR-3 and A2780/CP70 | VEGF ↓ Angiogenesis ↓ |
|
[131] |
| Breast | Angiogenesis | In vitro and in vivo | MDA-MB-231,4T1 & in vivo tumor xenograft model | VEGF ↓ VEGFR ↓ Angiogenesis ↓ |
|
[132] |
| Breast | Nrf-2/GPX4 pathway | In vitro and in vivo | Breast tumors mice model 4 T1 | Nrf-2 ↓, GPX4 ↓ |
|
[133] |
| Gastric | Apoptosis | In vitro and in vivo | AGS & Xenograft | Bcl-2/Bax ratio ↓ Bax ↑ Bcl2 ↓ |
|
[134] |
| Gastric | PI3K/Akt/mtor | In vitro | AGS | p-PI3K, p-Akt and p-mTOR ↓ |
|
[134] |
| Gastric | Apoptosis | In vitro | In vitro | Bcl-2 ↓ and pro-caspase-3 Bax and cleaved caspase-3 ↑ |
|
[135] |
| Pancreatic cancer | Apoptosis | In vitro | MIA PaCa-2, Panc-1 and S2-013 | Caspase-3 and 9 ↑ Induction of apoptosis |
|
[136] |
| Brain | Apoptosis | In vitro | U251 | Bax and Bad levels ↑ Bcl-2 and Bcl-xl ↓ |
|
[137] |
| Liver | Cell cycle | In vitro | Hep3B and HepG2i | Blocking cell cycle at the G2/M phase cell number in the G0/G1 phase ↓ |
|
[138] |
| Liver | Cell cycle | In vitro | HepG2 | Accumulation of cells in the G2/M phase ↑ Protein levels of the p53/p21 cascade ↑ |
|
[139] |
| Liver | Autophagy | In vitro | SMMC-7721 and Hep3B | Ratio of LC3-II/LC3-I ↑ autophagic flux ↑ |
|
[140] |
| Ovarian | PI3K/AKT | In vitro | A2780 and HO8910 | Phosphorylated ERK and PI3K/AKT ↓ |
|
[141] |
| Bile duct | STAT3 pathway | In vitro | KKU-100 | STAT3 ↓ |
|
[142] |
The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
The role of myricetin in the induction of ferroptosis in breast cancer cells was explored. It was noticed that myricetin could inhibit 4 T1 tumor cell viability and colony-forming activity, increasing the level of ROS, MDA, Fe2+, and within these cells. From a mechanistic perspective, this bioactive compound induced ferroptotic 4 T1 cell death by downregulating glutathione peroxidase 4 (GPX4) and Nrf-2. Moreover, in vivo, findings established that myricetin treatment was enough to decrease the growth of subcutaneous breast tumors in female mice, as noticed by decreases in tumor volume and weight [133]. A study was conducted to evaluate the role of myricetin in inducing apoptosis in gastric cancer cells. It was found that myricetin decreased the survival rate of these cells by inhibiting the phosphoinositide 3 kinase (PI3K)/Akt/mammalian (or mechanistic) target of rapamycin (mTOR) pathway, thereby triggering apoptosis. Similar findings were observed in vivo, where tumor growth was also suppressed [134]. A study on gastric cancer indicated that the percentage of apoptotic cells was higher in the treatment groups compared to the control groups. Additionally, the levels of the anti-apoptotic protein Bcl-2 and pro-caspase-3 were reduced in the myricetin treatment group. In contrast, the pro-apoptotic protein Bax and cleaved caspase-3 were meaningfully elevated in the myricetin-treated groups [135].
A study based on pancreatic cancer reported that the presence of myricetin considerably reduced cell viability in all pancreatic cancer cells tested (S2-013MIA and PaCa-2, Panc-1,) in a dose-dependent behavior, while little effect was detected on the viability of normal pancreatic ductal cells; it was noticed that myricetin-induced cell death in pancreatic cancer cells is facilitated by apoptosis. The incubation of S2-013 and MIA PaCa-2 cells by myricetin inhibited the phosphorylation of Akt and results indicate that myricetin causes apoptosis through the inhibition of the PI-3 kinase signaling pathway. Furthermore, myricetin inhibits tumor growth in an orthotopic mouse model of pancreatic cancer [136]. Myricetin employs anticancer effects in human glioma cells by inducing mitochondrial-mediated apoptosis, ROS generation, G2/M phase cell cycle arrest, and cell migration inhibition [137]. Myricetin promotes autophagy and halts the cell cycle at the G2/M phase, which helps inhibit the growth of HCC cells by lowering MARCH 1 levels. In both Hep3B and HepG2 cells, myricetin decreases the membrane-associated RING-CH finger protein 1 (MARCH1) protein. Additionally, myricetin suppresses HCC growth both in vitro and in vivo by inhibiting the p38 MAPK and Stat3 signaling pathways through the downregulation of MARCH 1 [138]. Another study result based on MTT assay proved that exposure of HepG2 cells to myricetin activated G2/M phase arrest. Myricetin evidently diminished Cdc2 and cyclin B1 protein levels and increased the protein levels of the p53/p21 cascade in HepG2 cells. Furthermore, treatment by myricetin caused in the Thr14/Tyr15 phosphorylated (inactive) p27 and Cdc2 up-regulation, and the downregulation of cyclin-dependent kinase 7 (CDK7) kinase protein, as well as CDK7-facilitated Thr161 phosphorylated (active) Cdc2 [139].
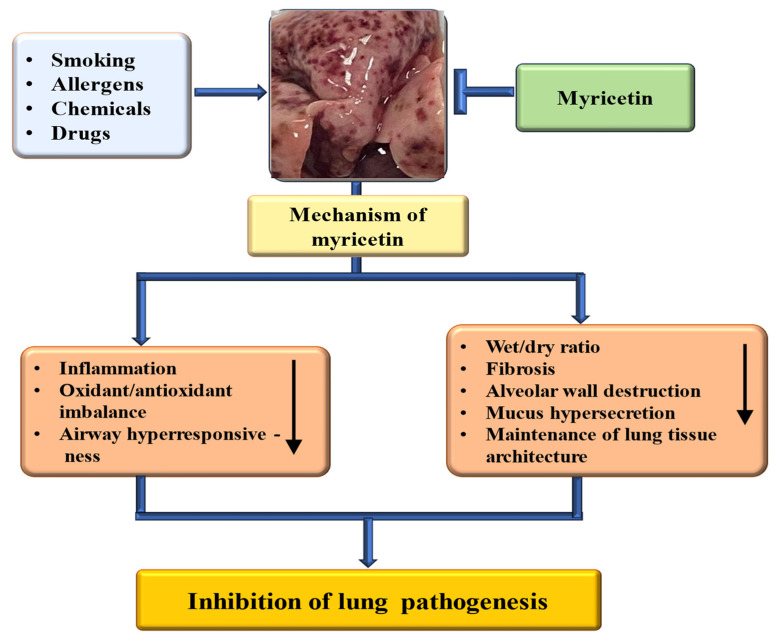
4.8. Role in Respiratory Disease
The rising incidence of chronic respiratory diseases (CRDs) has led to higher rates of illness and death globally [143]. The existing treatment approach is costly and can lead to adverse side effects. Therefore, there is a need for safer and more affordable treatment options to tackle this pathogenesis. Natural compounds and their bioactive have a proven role in managing lung-associated pathogenesis [144,145]. Myricetin’s role in lung pathogenesis through the modulation of the different mechanisms is presented in Figure 5. Moreover, the role of myricetin in the management of respiratory system-associated pathogenesis is summarized in Table 6. The murine sepsis model was made by cecal ligation and puncture (CLP), and the role of myricetin in this pathogenesis was examined. The survival rate test designated that myricetin suggestively improved the vitality of CLP-operated mice. Moreover, myricetin showed significant inhibitory effects on pathological changes in morphology, oxidative stress response biomarkers of inflammatory response, and mitochondrial damage in CLP-induced mice [146]. Myricetin reduced lung inflammation, as evidenced by the reduced wet-to-dry weight ratio of lungs, MPO activity, and protein concentration in the BALF, inflammatory cell migration, and cytokine production. A decrease was also seen in TLR4, NF-κB, and MyD88 expressions. Moreover, an elevated antioxidant enzyme activity of catalase, superoxide dismutase, and glutathione peroxidase was observed in all the treatment groups [67]. The results of another study reported that compared with the model group, the levels of neutrophils and macrophages in BALF in the myricetin and active groups decreased, whereas the wet/dry ratio of the lung tissue and total protein decreased [147].
Figure 5.
The role of myricetin in managing lung pathogenesis through different mechanisms (the lung image used in the figure is from our lab). The downward-pointing arrow shows downregulation.
A study was performed to inspect whether myricetin reduced airway hyperresponsiveness, eosinophil infiltration, and airway inflammation in the lungs of asthmatic mice. It was reported that myricetin efficiently mitigated eosinophil infiltration, goblet cell hyperplasia, and airway hyperresponsiveness (AHR) in the lungs, and it reduced the expression of Th2 cytokine in BALF from asthmatic mice. Myricetin reduced ROS and the production of proinflammatory cytokines, eotaxins, in BEAS-2B cells [148]. The in vivo studies showed that myricetin effectively alleviated bleomycin (BLM)-induced pulmonary fibrosis. In vitro studies designated that myricetin dose-dependently suppresses TGF-β1/Smad signaling and reduces epithelial-mesenchymal transition and TGF-β1-induced fibroblast activation [149].
4.9. Effects of Myricetin on Digestive System/Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is characterized by recurrent episodes of gastrointestinal inflammation caused by an atypical immune response to the intestinal microbiota [150]. Inflammatory bowel disease chiefly involves two distinct clinical phenotypes: Crohn’s disease (CD) and ulcerative colitis (UC) [151]. Since the year 2000, the global incidence of IBDs has been on the rise, now impacting approximately 1 in 200 people in Western nations [152]. Myricetin’s role in the digestive system and associated pathogenesis is presented in Table 6. The protective potential of myricetin was assessed in a murine model of colitis induced by dextran sulphate sodium. The results demonstrated that myricetin treatment reduced histology scores and ameliorated body weight loss in a dose-dependent means. Myricetin diminished myeloperoxidase production while increasing the activity of glutathione peroxidase and superoxide dismutase. Additionally, the levels of the cytokine’s interleukin-6 interleukin-1 decreased [153]. The M10 derivative of myricetin, administered orally, demonstrated a reduction in ulcerative colitis, significantly lowering the disease activity index. Pathological examination indicated that M10 alleviated the extent of colonic inflammation in the affected tissues and helped restore the integrity of the intestinal barrier that had been compromised by Dextran sulphate sodium (DSS) [154]. Myricetin ameliorated the severity of inflammation in acute ulcerative colitis and meaningfully improved the condition. Myricetin elevated the levels of transforming growth factor β and IL-10. Furthermore, the proportion of regulatory T cells increased in mice in the treatment of the myricetin group [155]. M10, a derivative of myricetin, enhanced the populations of CD8+ T and CD4+ T cells while inhibiting the infiltration of myeloid-derived suppressor cells into colorectal tissues. Additionally, there was a decrease in pro-inflammatory mediators, including granulocyte-macrophage colony-stimulating factor/macrophage colony-stimulating factor, IL-6, and TNF-α within the colonic mucosa [156].
4.10. Anti-Obesity Properties
Obesity is a substantial worldwide public health issue, described as having a Body Mass Index of 30 kg/m2 or higher [157]. Individuals who are obese face an increased risk of developing various chronic diseases. Bioactive compounds are present in small amounts in these food items, and they are effective in treating obesity [158,159]. Myricetin’s role in anti-obesity through modulation of different mechanisms is presented in Figure 6. Moreover, the role of myricetin in anti-obesity is summarized in Table 6. A study was performed to examine myricetin’s role in reducing mice’s body weight induced by a high-fat diet (HFD). Administration of myricetin intensely decreased the body weight of diet-induced obese mice. Numerous parameters linked to obesity, including serum triglyceride, glucose, and cholesterol, were reduced in myricetin-treated mice. Furthermore, obesity-linked oxidative stress was ameliorated in myricetin-treated mice [49]. A study finding revealed that myricetin inhibited the differentiation of 3 T3-L1 preadipocytes in a concentration-dependent way. It was observed that myricetin lowered both the mRNA and protein levels of key adipogenic transcription factors. Additionally, myricetin treatment resulted in a reduction of mRNA levels for several other transcription factors related to adipogenesis. These results indicate that myricetin exhibits anti-obesity effects in adipocytes [160].
Figure 6.
Role of myricetin in eye disease, bone disease, obesity, and wound healing. The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
After 14 weeks of myricetin treatment, db/db mice showed improvements in systemic insulin resistance, hepatic steatosis, and a reduction in body weight. Myricetin also improved plasma lipid profiles, increased energy expenditure, and reduced adiposity. In inguinal white adipose tissue (Iwat), treatment with myricetin prompted the formation of beige adipocytes, activated mitochondrial biogenesis, and elevated the expression of thermogenic proteins. Moreover, the expression levels of adiponectin were elevated in C3H10T1/2 cells and in adipose tissues and plasma following myricetin treatment [161]. Research indicated that myricetin decreased the intracellular buildup of triglycerides in 3T3-L1 adipocytes from rats on a high-fat diet. Its impact on reducing body weight and visceral fat pad weights in fat-fed rats was comparable to that of fenofibrate administered at a dose of 100 mg/kg/day [162].
4.11. Wound Healing Effects
Numerous studies have investigated the wound-healing abilities of natural products that exhibit antioxidant, collagen-promoting, anti-inflammatory, and antibacterial properties [163]. The role of myricetin in wound healing through modulation of different mechanisms are presented in Figure 6. Moreover, the wound-healing role of myricetin is summarized in Table 6. A topical application of naturally isolated myricetin from the shoots of Tecomaria capensis v. aurea on wound healing was made in albino rats. It was reported that the percentage of wound closure as well as contraction was delayed in wounded rats (67.35%) and was increased after treatment of wounded rats with myricetin; the treatment with myricetin (20%) was the most powerful (98.76%). Histological studies indicated that treatment with 10% myricetin resulted in a significant area of scarring at the wound site, similar to the control group. In contrast, the 20% myricetin treatment showed a reduced scarring area and re-epithelialization accompanied by a higher density of fibroblasts at the wound site. Therefore, it can be proposed that the enhancements in inflammatory cytokines as well as systemic reorganization after treatment of myricetin may be suggested to play a vital part in the promotion of wound healing [164]. Results presented that the topical application of myricetin-3-O-rhamnoside decreased inflammatory cells infiltration and increased wound healing [165]. An in vitro model of inflammation was created using monolayers of scratched fibroblasts or keratinocytes that were exposed to LPS from Pseudomonas aeruginosa. Subsequently, myricetin and dihydromyricetin were administered to the cells at sub-toxic concentrations ranging from 5 to 15 µM. It was reported that myricetin and dihydromyricetin inhibit the production of pro-inflammatory cytokines in LPS-stimulated skin cells and level of MMP-1 decreased in fibroblasts [166].
4.12. Anti-Analgesic Activity
The analgesic activity of myricetin, a chief compound in Myrica rubra Sieb. et Zucc. leaves were examined. It was reported that myricetin displayed a noteworthy inhibition on chemical nociceptive models. Additionally, myricetin lowered the levels of prostaglandin E2 (PGE2) in the peritoneal fluid and inhibited platelet aggregation induced by collagen and arachidonic acid in vitro [167]. The role of myricetin as an anti-analgesic is presented in Table 6. The analgesic effect of myricetin in a neuropathic pain model was examined. In vivo, a single injection of myricetin decreased SNL-induced mechanical allodynia as well as thermal hyperalgesia. In vitro, I(Ca(V)) (depolarization from −80 to 0 mV) was decreased by low concentrations of myricetin [168]. The antinociceptive effects of myricitrin in models of overt nociception was examined. The nociception induced by bradykinin was stopped by prior treatment with myricitrin. The myricetin dose of 100 mg/kg caused a 57% decrease in cinnamaldehyde-induced nociception [169]. Myricetin exhibited a notable inhibition in chemical nociceptive models, including the acetic acid-induced writhing response. It also reduced the levels of PGE2 in the peritoneal fluid and decreased platelet aggregation triggered by collagen and arachidonic acid. These findings collectively indicate that myricetin has strong analgesic properties, which are associated with peripheral analgesia [167].
4.13. Anti-Platelet Aggregation Potential
Studies indicate that flavonoids and phenolic acids function as anti-platelet aggregation agents [170,171], and myricetin also contributes to this effect. The antagonistic potential of myricetin on platelet activating factor (PAF) was evaluated. The specific binding of [3H] PAF to rabbit platelet receptors was examined via radioligand binding assay (RLBA). It was reported that the specific binding inhibition potency of myricetin was noticed to be concentration dependent. The platelet-activating factor-induced reactions of rabbit platelet adhesion, as well as polymorphonuclear leukocytes’ inner free calcium concentration increase, were prevented by myricetin [172]. The inhibitory effects of myricetin on the aggregation as well as secretion of platelets were examined. The flavonoid prevented platelet aggregation and ATP release of rabbit platelets brought by arachidonic acid or collagen, and somewhat those by platelet-activating factor [173]. Myricetin triggered an increase in platelet adenosine 3′,5′-cyclic monophosphate (cyclic-AMP) levels through prostacyclin stimulation. The anti-aggregating effect was due to modification in platelet cyclic-AMP metabolism, which involved the inhibition of phosphodiesterase activity [174]. It was reported that myricetin presented an important inhibition on chemical nociceptive models, such as the licking time on the late phase in the formalin test and acetic acid-induced writhing response in a dose-dependent way. Furthermore, myricetin inhibited the amount of PGE2 in the peritoneal fluid, and platelet aggregation was caused by collagen and arachidonic acid in vitro [167]. A recent finding reported that polyphenol-rich extract decreased platelet activation as well as aggregation induced by different agonists. Myricetin employed effective antiplatelet effects and reduced the capacity of platelets to spread on collagen [175].
4.14. Effect on Bone Disease
Myricetin’s role in glucocorticoid-induced osteoporosis was made, and outcomes exhibited that myricetin might reduce dexamethasone-induced osteoporosis by enhancing osteogenic differentiation and matrix mineralization through the ERK signaling pathway [176]. Myricetin’s role in bone disease is presented in Table 6. The myricetin treatment group’s bone mineral density (BMD) increased more than that of the diabetic group. Furthermore, myricetin treatment intensely improves trabecular bone microarchitecture by increasing bone mass and diminishing trabecular separation and structure model index compared to the control group [177]. The research focused on the protective effects of myricetin against destruction in human gingival fibroblasts (HGF) subjected to inflammatory conditions induced by lipopolysaccharide (LPS). Additionally, the study explored the role of myricetin in inhibiting osteoclastogenesis in cells caused by receptor activator of NF-κB ligand (RANKL) RAW264.7. Myricetin prevented the formation of TRAP (+) multinucleated cells. It also suppressed the activation of p-38, ERK, and cSrc signaling pathways and the degradation of I(k)B induced by RANKL in the RAW264.7 cells. Myricetin reduced the mRNA expression of osteoclast-linked genes, including cFOS, cathepsin K, and tartrate-resistant acid phosphatase (TRAP) [178]. Study results reported that mineralization of hBMSCs were improved by myricetin treatment. Myricetin raised the mRNA expression of osteocalcin, alkaline phosphatase, and collagen type I [179]. Myricetin, whether administered in high or low doses, effectively prevented the resorption of alveolar bone and enhanced the height of the alveolar crest in a mouse model. It also inhibited osteoclast formation and bone resorption. Notably, the high dose of myricetin showed greater efficacy than the low dose. This research indicated that myricetin positively influenced alveolar bone resorption in the mouse periodontitis model, suggesting its potential as a treatment option for both periodontitis and osteoporosis [180]. The effect of various flavonoids on bone calcium content and osteoclastogenesis were examined to compare action of flavonoid on bone formation as well as bone resorption. Mouse bone marrow cells were cultured in the presence of parathyroid hormone (PTH). Culture with PTH caused a substantial increase in osteoclast-like cell formation. This increase was meaningfully inhibited in the presence of quercetin, myricetin isorhamnetin, kaempferol, or curcumin in the range of 10−8−10–6 M. Furthermore, culture with PTH caused a noteworthy decrease in diaphyseal calcium content. This decrease was completely inhibited in the presence of myricetin, quercetin, kaempferol, or isorhamnetin of 10−6 M [181].
4.15. Effect on Eye Disease
The impact of myricetin on the physiological characteristics and viability of cultured human retinal pigment epithelial (RPE) cells was examined. Myricetin was found to dose-dependently decrease RPE cell proliferation, VEGF secretion, and cell migration. Treatment with myricetin at low concentrations resulted in a reduction of VEGF gene expression, while higher concentrations led to an increase in its expression [182]. Myricetin’s role in wound healing through modulation of different mechanisms is presented in Figure 7. Moreover, the wound-healing role of myricetin is summarized in Table 6. The study was executed to check the intraocular pressure (IOP)-dropping activity of myricetin. It was reported that myricetin at doses of 1 mg reduced IOP to below control levels [183].
Figure 7.
Role of myricetin as renoprotective, anti-arthritis, and in reproductive system. The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
An important study examined the effect of myricetin on A2E and blue light-induced photoreceptor death in primary retinal cell cultures. Myricetin protected photoreceptors (100%) against blue-light-mediated damage. Myricetin also protected against A2E-induced photoreceptors and bipolar cell death. These results suggest that myricetin functions as a potent and effective neuroprotective agent for photoreceptor cells against A2E and light damage [184]. The role of myricetin on the trabecular meshwork cells in primary open-angle glaucoma (POAG) was examined. POAG TM cells exposed to myricetin showed lowered lipid peroxidation products and reactive oxidative species (ROS) levels. Myricetin effectively inhibited IOP elevation in glaucoma-induced rats and reduced inflammatory cytokines in the aqueous humor and POAG TM cells of glaucoma-induced rats [185]. The study examined whether gallic acid and myricetin-rich Labisia pumila extract (LP) consumption prevents diabetic eye disorders. The diabetic rats consuming LP revealed dose-dependent, histopathologically decreased eye abnormalities. The LP suppressed inflammation, vascular leakage, abnormal vascularization, oxidative tension, and hyperglycemia of the diabetic rats [186].
4.16. Effect on Osteoarthritis
Osteoarthritis (OA) is the most common progressive musculoskeletal condition that can affect joints, but it chiefly affects the knees and hips as predominant weight-bearing joints [187,188,189]. The currently used drugs are effective but also cause side effects. Myricetin has a confirmed role as an anti-arthritis agent through different mechanisms, including its anti-inflammatory potential. Myricetin inhibited IL-1β-induced production of PGE2 and nitric oxide (NO), expression of ADAMTS5, and degradation of collagen-II in mouse chondrocytes. Also, in vivo, myricetin decreased OA in the mouse model of osteoarthritis [190]. Myricetin reduced cartilage degeneration in vitro and in vivo. Moreover, myricetin decreased the IL-1β-induced inflammatory cytokines production. Myricetin-treated mice showed a less severe OA phenotype than vehicle-treated mice. More notably, myricetin intensely reduced the expression of chondrocyte catabolic and increased the secretion of chondrocyte anabolism agents, including proteoglycans and collagen [191]. Myricetin inhibited the generation of cytokines and inflammatory mediators and suppressed the production of cyclooxygenase-2, inducible nitric oxide synthase, and in human chondrocytes under IL-1β stimulation. Moreover, an in vivo study established that myricetin ameliorated the progression of osteoarthritis in mice [192].
4.17. Renoprotective Effects
The renoprotective role of myricetin was confirmed through different mechanisms. The myricetin nephroprotective role against cisplatin-caused nephrotoxicity was investigated. It was demonstrated that apigenin, myricetin, and their combination reduced serum creatinine (Cr), blood urea nitrogen (BUN), TNF-α, and MDA levels, and increased catalase and GSH levels parallel to histopathological improvement in kidney tissues. Myricetin showed a protective and hopefully a preventive strategy against nephrotoxicity due to their anti-inflammatory and antioxidant effects [66]. Myricetin’s renoprotective role through modulation of different mechanisms is presented in Figure 7. Moreover, the wound-healing role of myricetin is summarized in Table 6. The research investigated the nephroprotective properties of myricetin on the oxidant–antioxidant balance in the kidneys of mice that were given a high-fat diet along with ethanol. This combination elevated malondialdehyde levels in the kidneys, signifying oxidative stress and disrupting the antioxidant system. Myricetin significantly reduced renal oxidative damage by restoring malondialdehyde levels, increasing the activities of antioxidant enzymes, and rebalancing glutathione stores in the kidneys. These findings indicate that myricetin has nephroprotective effects by enhancing the renal antioxidative defense system [193]. The administration of myricetin was found to restore albumin and lipid profiles to normal levels. Histopathological examinations of kidney samples revealed that myricetin treatment suppressed extracellular mesangial matrix expansion, glomerulosclerosis, and interstitial fibrosis in diabetic nephrotoxic rats. Furthermore, results indicate that myricetin provided noteworthy protection against alterations in lipid metabolism induced by STZ-Cd, which reduced the incidence of diabetic nephropathy in experimental rats [91].
Table 6.
The effects of myricetin in diverse pathogeneses via different mechanisms.
| Activity | Study Types | Model | Dose | Outcomes | Ref. |
|---|---|---|---|---|---|
| Lung injury protective effects | In vivo | Mice model/murine sepsis model | 100 mg/kg |
|
[146] |
| In vivo | Rat model | 10, 20 and 40 mg/kg |
|
[67] | |
| In vivo | Mice model | 50 mg/kg |
|
[147] | |
| Anti-ulcerative colitis effects | In vivo | Mice model | 200, 100 or 50 mg/kg |
|
[153] |
| In vivo | Mice model | 80 mg/kg |
|
[155] | |
| Anti-obesity potential | In vivo | Mice model | 150 mg/kg |
|
[49] |
| In vivo | Mice model | 400 mg/kg |
|
[161] | |
| Wound healing effects | In vivo | Rat model | 10 and 20% myricetin |
|
[164] |
| Anti-allodynic effect | In vivo | Rat model | 0.1–10 mg/kg |
|
[168] |
| Anti-osteoporosis effects | In vivo | Rat model | 1 or 2.5 mg/kg |
|
[176] |
| In vitro | MC3T3-E1 cells | 20 μM |
|
[176] | |
| In vivo | Rat model | 50 mg/kg |
|
[177] | |
| Role in periodontitis and osteoporosis | In vivo | Mice model | 2 or 5 mg/kg |
|
[180] |
| Intraocular pressure-lowering activity | In vivo | Rabbit model | 1 mg |
|
[183] |
| Role in glaucoma | In vivo | Rat model | 25, 50 or 100 mg/kg |
|
[185] |
| Anti-osteoarthritis effects | In vitro | Mouse chondrocyte | 12.5, 25 and 50 μM |
|
[190] |
| In vivo | Mouse model | 10 mg/kg |
|
[190] | |
| Renoprotective effects | In vivo | Mice model | 3 mg/kg |
|
[66] |
| In vivo | Mice model | 50 and 200 mg/kg |
|
[193] | |
| Role in the reproductive system | In vitro | VK2 and End1 | 5, 10, 20, 50 and 100 μM |
|
[194] |
4.18. Role in the Reproductive System
The antigrowth potential of myricetin in endometriosis was tested. Myricetin inhibited cell cycle progression and cell proliferation of human VK2/E6E7 and End1/E6E7 cells and induction of apoptosis, with accumulation of reactive oxygen species, calcium ions, and the loss of mitochondrial membrane potential. Additionally, myricetin reduced lesion size in the endometriosis mouse model by inhibiting Ccne1. Therefore, myricetin exhibits antiproliferative effects on endometriosis through cell cycle regulation [194]. The role of myricetin in the reproductive system through modulation of different mechanisms is presented in Figure 7. Moreover, the wound-healing role of myricetin is summarized in Table 6. Relative uterus weights of rats in 100 mg/kg/day dose group of myricetin were increased according to vehicle control as well as positive control groups. Moreover, uterine heights were increased in positive control groups and myricetin 100 mg/kg/day dose group [195]. It was reported that myricetin treatment improved metabolic capacity as well as insulin sensitivity by activating BAT in dehydroepiandrosterone (DHEA)-induced polycystic ovary syndrome (PCOS) mice. Additionally, decreased cystic formation and an increased number of corpus luteum were observed in PCOS mice. Myricetin decidedly improved reproductive deficiencies in PCOS mice [196].
4.19. Anti-Microbial Effects
Despite various initiatives aimed at decreasing consumption and regulating prescriptions, the prevalence of antibiotic resistance in clinical settings remains significant, and the emergence of bacterial pathogens with multidrug resistance is on the increase [197]. As a result, developing new approaches to combat antimicrobial resistance is essential for society. Focusing on the discovery of bioactive or natural compounds with antimicrobial properties could provide a sustainable solution to address this issue. The role of myricetin as an anti-bacterial, anti-fungal and anti-viral is presented in Figure 8. The role of myricetin microorganism-associated pathogenesis is summarized in Table 7. Antimicrobial potential, including antibacterial, antiviral, and antifungal properties, is explained here.
-
I.
Anti-bacterial potential
Myricetin oxidation products were generated via enzymatic oxidation of myricetin using horseradish peroxidase. It was reported that enzymatic oxidation enhanced the antibacterial activity and water solubility against Staphylococcus aureus of myricetin. Both myricetin and MYRoo could disturb the cell membrane, affect protein synthesis and degradation, and change the ROS levels in S. aureus. This study showed that enzymatic oxidation effectively improves MYR’s water solubility and antibacterial activity, enhancing its potential for food preservation [198]. Myricetin has been shown to inhibit the DnaB helicase of E. coli with a half-maximal inhibitory concentration (IC50) value of 11.3 μM. This crucial enzyme is vital for DNA replication and elongation [199]. A recent study was performed to assess the inhibitory potential of myricetin against Type II NADH oxidoreductase (NDH-2) as well as its effect on the expression and growth of virulence factors in S. aureus. It was demonstrated that myricetin was found to be an inhibitor of NDH-2 with a half-maximal inhibitory concentration of 2 μM. Time–kill assays exhibited that myricetin was a bactericidal agent against S. aureus. In line with being a competitive of NDH-2 substrate menadione (MK) inhibitor, the anti-staphylococcal potential of myricetin was antagonized through MK-4. Additionally, myricetin was shown to suppress the gene expression of enterotoxin SeA and decrease the hemolytic activity caused by S. aureus on rabbit erythrocytes in a dose-dependent way [200].
The effects of flavonols on recombinant sortase A (SrtA) as well as B (SrtB) prepared from S. aureus ATCC6538p were studied and it was noticed that these compounds inhibited the activity of sortases, without showing antibacterial activities. Among the flavonols tested, myricetin, morin, and quercetin showed strong sortase inhibitory activities [201]. Myricetin can effectively inhibit the activity of ClpP without affecting bacterial growth. Notably, myricetin reduced the pathogenicity of Staphylococcus aureus in vivo and enhanced the effectiveness of the traditional antibiotic oxacillin against methicillin-resistant Staphylococcus aureus (MRSA) infections. Additionally, it provided protection to mice from fatal lung infections caused by MRSA [202]. Myricetin notably decreases the production of various virulence factors in Staphylococcus aureus. This reduction encompasses diminished biofilm formation, adhesion, hemolysis, and staphyloxanthin production. Furthermore, myricetin offers significant protection against staphylococcal infections in the Galleria mellonella model [203]. Myricetin has been identified as an effective inhibitor of NDH-2, with a IC50 of 2 μM. The minimum inhibitory concentrations (MICs) of myricetin against S. aureus strains were found to be between 64 and 128 μg/mL. Furthermore, time-kill assays demonstrated that myricetin functions as a bactericidal agent against S. aureus [200] and myricetin demonstrated significant antimicrobial activity against foodborne pathogens [204].
-
II.
Anti-viral effects
The study was performed to assess the pharmacological efficiency and the mechanisms of action of myricetin against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection both in vivo and in vitro. Myricetin meaningfully inhibited SASR-CoV-2 infection as well as replication in Vero E6 cells. Furthermore, myricetin showed a noticeable suppressive action on the receptor-interacting serine/threonine protein kinase 1 (RIPK1)-driven inflammation as well as NF-kappa B signaling in THP1 macrophages. In animal model studies, myricetin remarkably ameliorated carrageenan-caused paw edema in rats, delayed-type hypersensitivity (DTH) induced auricle edema in mice, and LPS-induced acute lung injury (ALI) in mice [205]. Myricetin demonstrated strong antiviral effects against the pseudorabies virus (PRV) by directly inactivating the virus in vitro and hindering its adsorption, replication, and penetration into cells. In a mouse model infected with PRV, myricetin treatment enhanced the survival rate by 40% five days after infection. Furthermore, treatment with myricetin reduced the pathological changes associated with PRV infection [206]. Papain-like protease (PLpro) was selected as the target to screen antiviral agents against infectious bronchitis virus (IBV). It was reported that myricetin exhibited the robust inhibitory effect on IBV PLpro. Moreover, myricetin suggestively inhibits IBV replication in primary chicken embryo kidney cells and it can upregulate the transcription levels in the IRF7 and NF-κB signaling pathways [207]. It was reported that myricetin effectively inhibited transmissible gastroenteritis virus (TGEV)-induced cytopathic effects in a dose-dependent way. Myricetin meaningfully reduced TGEV viral load and at 100 μM concentration directly inactivated TGEV and suppressed its intracellular replication stage. In addition, treating PK-15 cells with 100 μM myricetin demonstrated a protective benefit against TGEV infection. Myricetin acted as a competitive inhibitor of PLpro, exhibiting an IC50 value of 6.563 μM [208]. The findings revealed that myricetin demonstrated anti-HSV-1 and HSV-2 properties with minimal toxicity, outperforming the effects of acyclovir [209].
-
III.
Anti-fungal effects
Heung-Shick Lee and Younhee Kim, 2022 reported that myricetin showed antifungal activity against Candida albicans via damaging the cell wall integrity and remarkably increasing the membrane permeability [210]. In vitro and vivo, myricetin’s anti-biofilm effect and its ability to increase miconazole nitrate’s (MN) antifungal effects were investigated. Myricetin exhibited a significantly inhibitory effect on biofilm formation and myricetin showed no effect on Candida albicans cell viability. MIC50 and MIC80 of MN were correspondingly reduced when used in combination with myricetin. Myricetin efficiently prevented the mouse periprosthetic joint infection (PJI), and MN was incorporated into thermosensitive hydrogel (TSH) [211].
Figure 8.
Antimicrobial potential of myricetin through different mechanisms.
Table 7.
Anti-microbial potential of myricetin.
| Activities | Species | Key Findings | Ref. |
|---|---|---|---|
| Anti-bacterial | Staphylococcus aureus |
|
[198] |
| Escherichia coli |
|
[199] | |
| S. aureus |
|
[201] | |
| S. aureus |
|
[200] | |
| SARS-CoV-2 |
|
[205] | |
| Anti-viral | Pseudorabies virus |
|
[206] |
| Transmissible gastroenteritis virus |
|
[208] | |
| Herpes simplex virus |
|
[209] | |
| Candida albicans |
|
[210] | |
| Anti-fungal | Candida albicans |
|
[211] |
5. Synergetic Effects of Myricetin with Other Drugs
Natural compounds and their bioactive components contribute to disease management mainly by exhibiting antioxidant and anti-inflammatory properties, as well as by influencing various biological functions. The impact of foods on human biological systems varies significantly when consumed as part of a whole matrix, compared to the effects of individual food constituents [212]. Physiological synergy occurs when plant compounds work together to enhance absorption, bioavailability, and metabolism while also reducing potential adverse effects [213]. Studies have indicated that drug combinations can improve effectiveness through different mechanisms, such as boosting antioxidant, anti-inflammatory, and anti-cancer properties while minimizing the side effects or toxicity associated with the individual drugs. Synergetic effects of myricetin with other drugs are summarized in Table 8. CuMy-12 (Cucurbitacin E (CuE) and myricetin (Myr), a combination of CuE as well as Myr from C. colocynthis, inhibited cell proliferation and caused cell cycle arrest in the G0/G1 phase and induced apoptosis, revealing a synergistic effect [214]. The effect of the combination of myricetin with vancomycin and oxacillin against vancomycin intermediate resistant S. aureus (VISA) and methicillin resistant S. aureus (MRSA) strains was investigated. Checkerboard assessments showed a decrease in the minimum inhibitory concentration (MIC) of antibacterials when myricetin was present, while time-kill tests confirmed the synergistic effects of these combinations, with the exception of the VISA strain when myricetin was combined with vancomycin. In vivo assessments demonstrated that the combination of oxacillin and myricetin was effective in treating MRSA-infected larvae, leading to a 20% increase in host survival compared to the control groups [215]. As per the results of the microdilution test, the bacterial strains used in this study (except for MRSA) were commonly sensitive to antibiotics. The interaction study revealed encouraging findings about the synergistic effects of antibiotics combined with flavonoids. Notably, myricetin demonstrated a synergistic interaction exclusively with levofloxacin [216]. A study was made to investigate the combined anti-diabetic effect of myricetin and kaempferol in streptozotocin (STZ)-activated diabetes in rats. The study demonstrated that combined treatment restored the measured parameters including inflammatory cytokines, glucose levels, oxidative markers, and liver and lipid enzymes in diabetic rats. The findings indicate that the combined treatment of myricetin and kaempferol offers positive effects against diabetes, suggesting that this combination could be therapeutically effective in managing the condition [217]. To investigate whether myricetin (MYR) and methyl eugenol (MEG) can enhance the anticancer effects of cisplatin (CP) on cervical cancer cells, HeLa cells were treated with MYR and MEG either individually or in combination with cisplatin and then assessed for cell growth and apoptosis. The results indicated that the combination of MYR or MEG with CP was more effective in suppressing cancer cell growth and promoting apoptosis compared to treatment with each drug alone. Furthermore, the loss of mitochondrial membrane potential (ΔΨm) and Caspase-3 activity were substantially greater in the combination treatment than in the single drug treatment [218]. Another study was executed to examine whether sulforaphane (SFN) and myricetin (Myr) synergistically induce apoptosis in adipocytes. As compared with the effects of each compound alone, the combination of SFN and Myr synergistically induced apoptosis, and reduced cell viability [219]. It was established that myricetin showed a strong affinity for CD147 as well as down-regulating the protein level of CD147 by facilitating its proteasome-dependent degradation. Furthermore, synergistic antitumor effects of myricetin and cisplatin were noticed in both in vivo and in vitro [220].
Table 8.
Synergistic effects of myricetin with other drugs.
| Drugs/Compound | Activity | Key Finding | Ref. | |
|---|---|---|---|---|
| Myricetin | Cucurbitacin E | Anti-lung cancer |
|
[214] |
| Oxacillin | Antibacterial |
|
[215] | |
| Levofloxacin | Antibacterial |
|
[216] | |
| Kaempferol | Anti-diabetic |
|
[217] | |
| Methyl eugenol | Anti-cancerous |
|
[218] | |
| Sulforaphane | Anti-obesity |
|
[219] | |
| Cisplatin | Anti-cancerous |
|
[220] | |
| Piceatannol | Anti-cancerous |
|
[221] |
6. Myricetin-Based Nanoformulation and Its Role in Disease Management
Although myricetin is beneficial in managing pathogenesis, its main challenge is low bioavailability. However, various nanoformulations have been developed to enhance the bioavailability, depletion of toxicity, solubility, and targeted delivery of drugs. Nanoformulations also enhance the pharmacokinetic properties of bioactive compounds, leading to improved therapeutic effects. Moreover, nanoformulations can be introduced into the body through inhalation, ingestion, skin penetration, or injection, interacting with biological systems [222]. Additionally, nanoformulations can reduce the required administration doses by enabling targeted delivery and site-specific release, thereby enhancing the therapeutic effects of drugs [223]. The role of myricetin-based nanoformulations in disease are presented in Figure 9 and Table 9. A study was performed to synthesize the silver nanoparticles labelled with myricetin. It was reported that myricetin was capable of killing human colorectal cancer cell lines [224]. Myricetin-mediated silver nanoparticles (MY-AgNPs) were produced. These nanoparticles showed potent antibacterial activity against Salmonella and Escherichia coli, with minimum inhibitory concentrations of 10−4 and 10−5 g/L, respectively. Moreover, MY-AgNPs showed better antioxidant potential [225]. The gold nanoparticles (AuNPs) with myricetin (Myr) were synthesized and Myr-AuNPs-treated cells presented a good proportion of dead cells demonstrated with formation of pro-apoptotic bodies [226]. The study presents liposomal nanoformulations of myricetin showed to enhance its bioavailability while minimizing pro-oxidant activity. The impact of nanoencapsulated myricetin on developing zebrafish embryos was investigated. Results from the cumulative hatchability, developmental studies, and antioxidant assays indicated that the liposomal nanoformulation of myricetin exhibited enhanced antioxidant activity, offering protection against oxidative stress [227]. The study was planned to promote bioavailability as well as the therapeutic efficacy of myricetin through pro-liposome formulations. The better pharmacological effects, particularly the hepatoprotective and antioxidant activity of myricetin, were achieved through TPGS-modified pro-liposome formulation [228]. Myricetin was incorporated into pH-sensitive liposomes to improve its bioavailability and anti-hyperuricemic activity. The release rate of myricetin liposomes exceeded that of free myricetin, with the cumulative value responding to pH. Additionally, the maximum concentration (Cmax) of myricetin liposomes was measured at 4.92 ± 0.20 μg/mL. In the M-L-H group (200 mg/kg), the uric acid level decreased by 54.74% w/v compared to the model group [229]. High-bioavailability liposomes encapsulating dihydromyricetin (DHM) were developed and evaluated for their therapeutic effects and regulatory mechanisms in a model of hepatic inflammatory injury. The encapsulation of DHM in liposomes enhanced its bioavailability, resulting in a more effective reduction in liver inflammation. Additionally, DHM liposomes specifically targeted hepatic macrophages and polarization of macrophages into an anti-inflammatory phenotype [230]. A study was performed to formulate myricetin in the form of solid lipid nanoparticles (SLN), decorated with chitosan (CS) as well as active-targeted with folic acid (FA). The cytotoxicity assay displayed that myricetin-solid lipid nanoparticles (SLN)-chitosan (CS)- folic acid (FA) killed cancer cells, and the highest level of apoptosis was shown at the concentration of 45 µg/mL. The anti-angiogenic activities of the formulations showed a decrease in the number and length of the vessels and also affected VEGFR and VEGF genes involved in angiogenesis. The antitumor studies designated the effects of formulation on reducing tumor volume [231]. The myricetin nanofiber (MyNF) system, which combines hydroxypropyl-β-cyclodextrin (HPBCD) and polyvinylpyrrolidone K120 (PVP), has been developed to load myricetin, enhancing its water solubility and skin penetration by altering its physicochemical properties. The results revealed that these myricetin nanofibers significantly reduced cytotoxicity in HaCaT keratinocytes when compared to free myricetin [232].
Figure 9.
Myricetin-based nanoformulation and their role in disease management. The downward-pointing arrow shows downregulation, whereas the upward arrow represents upregulation.
The nanoemulsion of Myricetin (Myr-NE) was developed and assess its benefit over myricetin alone in Triple-negative breast cancer (TNBC) cells. It was reported that Myr-NE showed noteworthy inhibition of cell proliferation, clonogenicity, and increased apoptosis with ~2.5-fold lower IC50 as compared to myricetin. Mechanistic study demonstrated that nanoemulsion improved the anti-cancer effectiveness of Myricetin, probable through inhibiting the PI3K/AKT/mTOR pathway, ultimately leading to enhanced cell death in TNBC cells [233]. A nanoformulation was prepared with myricetin encapsulated within chitosan nanoparticles (CHT-NPs) such as MYR-CHT-NPs. In vivo, pharmacodynamic study followed by oral administration in rats exhibited better glycaemic control than existing drugs. The nanoparticles also showed a controlled increase in weight compared to Metformin. The nanoformulation reduced the levels of several pathological biomarkers and showed no toxicity or changes in the section of the organ as compared to normal control, suggesting safe oral administration of the encapsulated myricetin [234]. A Kolliphor HS15-based myricetin-loaded (HS15-Myr) nanomicelle was prepared to evaluate its effectiveness against cisplatin-induced acute kidney injury (AKI). In vitro results indicated that this formulation improved the antioxidant activity of myricetin and countered the proliferation inhibition of HK-2 cells caused by cisplatin. Additionally, the HS15-Myr nanomicelles effectively reduced the accumulation of reactive oxygen species, DNA damage, and decreased mitochondrial membrane potential induced by cisplatin. In an in vivo study involving mice, the results showed that the formulation reversed the adverse effects of cisplatin, including reductions in renal indices and body weight, as well as increased levels of blood urea nitrogen and serum creatinine. Moreover, the pretreatment with the nanomicelles significantly affected the activities of antioxidant enzymes altered by cisplatin. Furthermore, the formulation successfully inhibited the inflammatory responses triggered by cisplatin in the kidney tissue of mice [235]. A study developed a myricetin-coated zinc oxide nanocomposite, reporting that the tested C. perfringens isolates were sensitive to myricetin-loaded zinc oxide (ZnO)/polyvinyl alcohol (PVA), with minimum inhibitory concentrations ranging from 0.125 to 2 µg/mL [236].
Table 9.
Myricetin-based nanoformulation and their role in disease.
| Nanoformulations | Activity | Key Findings | Ref. |
|---|---|---|---|
| Myricetin-mediated silver nanoparticles | Antibacterial |
|
[225] |
| Myricetin-gold nanoparticles | Anti-cancerous |
|
[226] |
| Myricetin liposomal nanoformulation | Antioxidant |
|
[227] |
| TPGS modified pro-liposome of myricetin | Hepatoprotective |
|
[228] |
| MYR pH-sensitive liposomes | Anti-hyperuricemic |
|
[229] |
| Myricetin-loaded solid lipid nanoparticles | Anti-cancerous |
|
[231] |
| Myricetin nanofibers | Photoprotective |
|
[232] |
| Myricetin encapsulated chitosan nanoformulation | Diabetes management |
|
[234] |
| Myricetin-loaded nanomicelles | Nephroprotective |
|
[235] |
7. Conclusions and Future Perspectives
Around 80% of the global population depends on plant-based extracts for their primary healthcare needs, highlighting the vital role of traditional medicine in various cultures. These natural remedies are often the first line of defense against various pathogenesis, providing relief and health-promoting potential. Natural products, including stems, fruits, leaves, and seeds, play a significant role in disease management by modulating various biological activities. Flavonoids have also been demonstrated to significantly contribute to disease prevention due to their antioxidant and anti-inflammatory properties.
Flavonoids have emerged as important agents in disease prevention, largely due to their powerful antioxidant and anti-inflammatory properties. These compounds help combat oxidative stress by neutralizing free radicals, which can lead to cellular damage and numerous chronic diseases. Their anti-inflammatory effects also contribute to the decrease of inflammation-related pathogenesis. By modulating various biochemical and physiological pathways, flavonoids increase the body’s defense mechanisms. Based on evidence from in vitro and in vitro studies, flavonoids play a significant role in disease cure through various mechanisms. Myricetin is a member of the class of flavonoids/plant-derived flavonoids known as flavonols and is commonly found in vegetables and fruits. The amount present in various fruits and vegetables varies within different ranges. Its role in disease management is confirmed through potential mechanisms, including anti-inflammatory and antioxidant effects, lowering lipid and cholesterol levels, enhancement of insulin, and preservation of the structural integrity of tissues. This review emphasizes the recent findings regarding myricetin and its potential use in different diseases. Further research with adequate, randomized, and controlled clinical trials should be performed to explore this compound’s therapeutic importance, safety, and efficacy against human pathogenesis.
Acknowledgments
The researchers would like to thank the Deanship of Graduate Studies and Scientific Research at Qassim University for financial support (QU-APC-2025).
List of Abbreviations
| GSH | Glutathione |
| T-AOC | Total antoxidant capacity |
| SOD | Superoxide dismutase |
| CAT | Catalase |
| MDA | Malondialdehyde |
| NAFLD | Nonalcoholic fatty liver disease |
| ROS | Reactive oxygen species |
| AGEs | Advanced glycation end-products |
| Nrf2 | Nuclear factor erythroid 2–related factor 2 |
| iNOS | Inducible nitric oxide synthase |
| ALP | Alkaline phosphatase |
| ALT | Alanine transaminase |
| AST | Aspartate aminotransferase |
| COX-2 | Cyclooxygenase-2 |
| TNF-α | Tumor necrosis factor-α |
| NF-κB | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| IL | Interleukin |
| STAT | Signal transducer and activator of transcription |
| MMP | Matrix metalloproteinase |
| Cmax | Maximum concentration |
| IBD | Inflammatory bowel diseases |
| 5-FU | 5-Fluorouracil |
| CCl4 | Carbon tetrachloride |
| LPS | Lipopolysaccharide |
| BALF | Bronchoalveolar Lavage Fluid |
| STZ | Streptozotocin |
| HFD | High-fat diet |
| MAPK | Mitogen-activated protein kinase |
| TLR | Toll-like receptor |
| OA | Osteoarthritis |
| BUN | Blood Urea Nitrogen |
| VEGF | Vascular endothelil growth factor |
| PTZ | Pentylenetetrazole |
| PCO | Polycystic Ovary Syndrome |
| HIF-1α | Hypoxia-inducible factor-1α |
| IOP | Intraocular pressure |
| MPO | Myeloperoxidase |
| POAG | Primary open-angle glaucoma |
| MIC | Minimum inhibitory concentration |
| AuNP | Gold nanoparticle |
| AgNP | Silver nanoparticle |
| SLN | Solid nanoparticle |
| CDAHFD | Choline-deficient, L-amino acid-defined, high-fat diet |
| HSC | Hepatic stellate cells |
| NASH | Nonalcoholic steatohepatitis |
| TREM-1 | Triggering receptor expressed on myeloid cells-1 |
| Pi3k/Akt/mTOR | Phosphoinositide 3 kinase/Akt/mTOR |
| CDK | Cyclin-dependent kinase |
| Fe-NTA | Ferric iron nitrilotriacetate |
| GSH-Px | Glutathione peroxidase |
| TBARS | Thiobarbituric acid reactive substance |
| PGN | Peptidoglycan |
| mTOR | Mammalian target of rapamycin |
Author Contributions
Conceptualization, S.A.A. and A.H.R.; methodology, S.A.A. and A.H.R.; writing—original draft preparation, S.A.A. and A.H.R.; writing—review and editing, S.A.A. and A.H.R.; funding acquisition, S.A.A. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Funding was provided by the Deanship of Graduate Studies and Scientific Research Qassim University.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.van Wyk A., Prinsloo G. Medicinal plant harvesting, sustainability and cultivation in South Africa. Biol. Conserv. 2018;227:335–342. doi: 10.1016/j.biocon.2018.09.018. [DOI] [Google Scholar]
- 2.Torres-León C., Ramírez F.R., Aguirre-Joya J.A., Ramírez-Moreno A., Chávez-González M.L., Aguillón-Gutierrez D.R., Camacho-Guerra L., Ramírez-Guzmán N., Vélez S.H., Aguilar C.N. Medicinal plants used by rural communities in the arid zone of Viesca and Parras Coahuila in northeast Mexico. Saudi Pharm. J. 2023;31:21–28. doi: 10.1016/j.jsps.2022.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) World Health Organization Traditional Medicine Strategy 2014–2023. WHO; Geneva, Switzerland: 2013. pp. 1–78. [Google Scholar]
- 4.Harvey A.L., Edrada-Ebel R., Quinn R.J. The re-emergence of natural products for drug discovery in the genomics era. Nat. Rev. Drug Discov. 2015;14:111–129. doi: 10.1038/nrd4510. [DOI] [PubMed] [Google Scholar]
- 5.Atanasov A.G., Waltenberger B., Pferschy-Wenzig E.-M., Linder T., Wawrosch C., Uhrin P., Temml V., Wang L., Schwaiger S., Heiss E.H., et al. Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol. Adv. 2015;33:1582–1614. doi: 10.1016/j.biotechadv.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anwar S., Raut R., Alsahli M.A., Almatroudi A., Alfheeaid H., Alzahrani F.M., Khan A.A., Allemailem K.S., Almatroodi S.A., Rahmani A.H. Role of Ajwa Date Fruit Pulp and Seed in the Management of Diseases through In Vitro and In Silico Analysis. Biology. 2022;11:78. doi: 10.3390/biology11010078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anwar S., Almatroodi S.A., Almatroudi A., Allemailem K.S., Joseph R.J., Khan A.A., Alrumaihi F., Alsahli MAHusain Rahmani A. Biosynthesis of silver nanoparticles using Tamarix articulata leaf extract: An effective approach for attenuation of oxidative stress mediated diseases. Int. J. Food Prop. 2021;24:677–701. doi: 10.1080/10942912.2021.1914083. [DOI] [Google Scholar]
- 8.Barakat H., Aljutaily T., Almujaydil M.S., Algheshairy R.M., Alhomaid R.M., Almutairi A.S., Alshimali S.I., Abdellatif A.A. Amygdalin: A review on its characteristics, antioxidant potential, gastrointestinal microbiota intervention, anticancer therapeutic and mechanisms, toxicity, and encapsulation. Biomolecules. 2022;12:1514. doi: 10.3390/biom12101514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almatroodi S.A., Khan A.A., Aloliqi A.A., Syed M.A., Rahmani A.H. Therapeutic potential of Tamarix aphylla in the prevention of lung injury through the regulation of inflammation, oxidative stress and cell-signaling molecules. Appl. Sci. 2022;12:9925. doi: 10.3390/app12199925. [DOI] [Google Scholar]
- 10.Mani V., Arfeen M., Dhaked D.K., Mohammed H.A., Amirthalingam P., Elsisi H.A. Neuroprotective effect of methanolic Ajwa seed extract on lipopolysaccharide-induced memory dysfunction and neuroinflammation: In vivo, molecular docking and dynamics studies. Plants. 2023;12:934. doi: 10.3390/plants12040934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Santos E.L., Maia B., Ferriani A.P., Teixeira S.D. Flavonoids: From Biosynthesis to Human Health. Volume 13. IntechOpen; London, UK: 2017. Flavonoids: Classification, biosynthesis and chemical ecology; pp. 78–94. [Google Scholar]
- 12.Ullah A., Munir S., Badshah S.L., Khan N., Ghani L., Poulson B.G., Emwas A.-H., Jaremko M. Important Flavonoids and Their Role as a Therapeutic Agent. Molecules. 2020;25:5243. doi: 10.3390/molecules25225243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferraz C.R., Carvalho T.T., Manchope M.F., Artero N.A., Rasquel-Oliveira F.S., Fattori V., Casagrande R., Verri W.A. Therapeutic Potential of Flavonoids in Pain and Inflammation: Mechanisms of Action, Pre-Clinical and Clinical Data, and Pharmaceutical Development. Molecules. 2020;25:762. doi: 10.3390/molecules25030762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng X., Zhang X., Zeng F. Biological Functions and Health Benefits of Flavonoids in Fruits and Vegetables: A Contemporary Review. Foods. 2025;14:155. doi: 10.3390/foods14020155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta G., Siddiqui M.A., Khan M.M., Ajmal M., Ahsan R., Rahaman A., Ahmad A., Arshad, Khushtar M. Current Pharmacological Trends on Myricetin. Drug Res. 2020;70:448–454. doi: 10.1055/a-1224-3625. [DOI] [PubMed] [Google Scholar]
- 16.Rehman M.U., Rather I.A. Myricetin abrogates cisplatin-induced oxidative stress, inflammatory response, and goblet cell disintegration in colon of wistar rats. Plants. 2019;9:28. doi: 10.3390/plants9010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yao Q., Li S., Li X., Wang F., Tu C. Myricetin modulates macrophage polarization and mitigates liver inflammation and fibrosis in a murine model of nonalco-holic steatohepatitis. Front. Med. 2020;7:71. doi: 10.3389/fmed.2020.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lu Y., Sun J., Yang M., Xing Y., Zhu W., Zhu J., Ma X., Wang Y., Wang L., Jia Y. Myricetin Induces Ferroptosis and Inhibits Gastric Cancer Progression by Targeting NOX4. J. Agric. Food Chem. 2024;72:6178–6188. doi: 10.1021/acs.jafc.3c05243. [DOI] [PubMed] [Google Scholar]
- 19.Rashid S.M., Wali A.F., Ali S., Rehman M.U., Maqbool M.T., Nadeem A., Ahmad S.F., Siddiqui N. Myricetin (3,3′,4′,5,5′,7-hexahydroxyflavone) prevents ethanol-induced biochemical and inflammatory damage in the liver of Wistar rats. Hum. Exp. Toxicol. 2022;41:09603271211066843. doi: 10.1177/09603271211066843. [DOI] [PubMed] [Google Scholar]
- 20.Ong K.C., Khoo H.E. Biological effects of myricetin. Gen Pharmacol. 1997;29:121–126. doi: 10.1016/S0306-3623(96)00421-1. [DOI] [PubMed] [Google Scholar]
- 21.Sultana B., Anwar F. Flavonols (kaempeferol, quercetin, myricetin) contents of selected fruits, vegetables and medicinal plants. Food Chem. 2008;108:879–884. doi: 10.1016/j.foodchem.2007.11.053. [DOI] [PubMed] [Google Scholar]
- 22.ahan N., Khalil-Ur-Rahman A.S., Asi M.R. Phenolic acid and flavonol contents of gemmo-modified and native extracts of some indigenous medicinal plants. Pak. J. Bot. 2013;45:1515–1519. [Google Scholar]
- 23.Mustafa R., Hamid A.A., Mohamed S., Abu Bakar F. Total phenolic compounds, flavonoids, and radical scavenging activity of 21 selected tropical plants. J. Food Sci. 2010;75:C28–C35. doi: 10.1111/j.1750-3841.2009.01401.x. [DOI] [PubMed] [Google Scholar]
- 24.Häkkinen S.H., Kärenlampi S.O., Heinonen I.M., Mykkänen H.M., Törrönen A.R. Content of the flavonols quercetin, myricetin, and kaempferol in 25 edible berries. J. Agric. Food Chem. 1999;47:2274–2279. doi: 10.1021/jf9811065. [DOI] [PubMed] [Google Scholar]
- 25.Ozcan C., Yaman M. Determination of Myricetin in medicinal plants by high-performance liquid chromatography. Instrum. Sci. Technol. 2015;43:44–52. doi: 10.1080/10739149.2014.940533. [DOI] [Google Scholar]
- 26.Sarker U., Oba S. Antioxidant constituents of three selected red and green color Amaranthus leafy vegetable. Sci. Rep. 2019;9:18233. doi: 10.1038/s41598-019-52033-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nardini M., Garaguso I. Characterization of bioactive compounds and antioxidant activity of fruit beers. Food Chem. 2020;305:125437. doi: 10.1016/j.foodchem.2019.125437. [DOI] [PubMed] [Google Scholar]
- 28.Martos I., Ferreres F., Yao L., D’Arcy B., Caffin N., Tomás-Barberán F.A. Flavonoids in monospecific eucalyptus honeys from Australia. J. Agric. Food Chem. 2000;48:4744–4748. doi: 10.1021/jf000277i. [DOI] [PubMed] [Google Scholar]
- 29.Ali M.C., Chen J., Zhang H., Li Z., Zhao L., Qiu H. Effective extraction of flavonoids from Lycium barbarum L. fruits by deep eutectic solvents-based ultrasound-assisted extraction. Talanta. 2019;203:16–22. doi: 10.1016/j.talanta.2019.05.012. [DOI] [PubMed] [Google Scholar]
- 30.Huamán-Castilla N.L., Mariotti-Celis M.S., Pérez-Correa J.R. Polyphenols of Carménère grapes. Mini-Rev. Org. Chem. 2017;14:176–186. doi: 10.2174/1570193X14666170206151439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lin J., Zhang S.M., Wu K., Willett W.C., Fuchs C.S., Giovannucci E. Flavonoid intake and colorectal cancer risk in men and women. Am. J. Epidemiology. 2006;164:644–651. doi: 10.1093/aje/kwj296. [DOI] [PubMed] [Google Scholar]
- 32.Mullie P., Clarys P., Deriemaeker P., Hebbelinck M. Estimation of daily human intake of food flavonoids. Plant Foods Hu-Man Nutr. 2007;62:93–98. doi: 10.1007/s11130-007-0047-7. [DOI] [PubMed] [Google Scholar]
- 33.Vogiatzoglou A., Mulligan A.A., Lentjes M.A.H., Luben R.N., Spencer J.P.E., Schroeter H., Khaw K.-T., Kuhnle G.G.C. Flavonoid intake in European adults (18 to 64 years) PLoS ONE. 2015;10:e0128132. doi: 10.1371/journal.pone.0128132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choi D.-H., Li C., Choi J.-S. Effects of myricetin, an antioxidant, on the pharmacokinetics of losartan and its active metabo-lite, EXP-3174, in rats: Possible role of cytochrome P450 3A4, cytochrome P450 2C9 and P-glycoprotein inhibition by myricetin. J. Pharm. Pharmacol. 2010;62:908–914. doi: 10.1211/jpp.62.07.0012. [DOI] [PubMed] [Google Scholar]
- 35.Dang Y., Lin G., Xie Y., Duan J., Ma P., Li G., Ji G. Quantitative Determination of Myricetin in Rat Plasma by Ultra Performance Liquid Chromatography Tandem Mass Spectrometry and Its Absolute Bioavailability. Drug Res. 2014;64:516–522. doi: 10.1055/s-0033-1363220. [DOI] [PubMed] [Google Scholar]
- 36.Lobo V., Patil A., Phatak A., Chandra N. Free radicals, antioxidants and functional foods: Impact on human health. Pharmacogn. Rev. 2010;4:118–126. doi: 10.4103/0973-7847.70902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ayala A., Muñoz M.F., Argüelles S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell. Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alzohairy M.A., Khan A.A., Alsahli M.A., Almatroodi S.A., Rahmani A.H. Protective effects of thymoquinone, an active compound of nigella sativa, on rats with Benzo (a) pyrene-Induced Lung injury through regulation of oxidative stress and inflammation. Molecules. 2021;26:3218. doi: 10.3390/molecules26113218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alharbi H.O.A., Alshebremi M., Babiker A.Y., Rahmani A.H. The Role of Quercetin, a Flavonoid in the Management of Pathogenesis Through Regulation of Oxidative Stress, Inflammation, and Biological Activities. Biomolecules. 2025;15:151. doi: 10.3390/biom15010151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rahmani A.H., Almatroudi A., Allemailem K.S., Alharbi H.O.A., Babiker A.Y., Althwab S.A., Alsuhaymi N., Alsugoor M.H., Khan A.A., Al-Megrin W.A.I. Oleuropein, a phenolic component of Olea europaea L. ameliorates CCl 4-induced liver injury in rats through the regulation of oxidative stress and inflammation. Eur. Rev. Med. Pharmacol. Sci. 2024;28:1259–1271. doi: 10.26355/eurrev_202402_35447. [DOI] [PubMed] [Google Scholar]
- 41.Morel I., Abaléa V., Sergent O., Cillard P., Cillard J. Involvement of phenoxyl radical intermediates in lipid antioxidant action of myricetin in iron-treated rat hepatocyte culture. Biochem. Pharmacol. 1998;55:1399–1404. doi: 10.1016/S0006-2952(97)00648-5. [DOI] [PubMed] [Google Scholar]
- 42.Hassan F.A., Al-Shawi N.N. Antioxidant and Anti-Inflammatory Effects of Myricetin on 5-Fluorouracil-Induced Hepatotoxicity in Male Rats. Afr. J. Biomed. Res. 2024;27:3705–3713. [Google Scholar]
- 43.Abalea V., Cillard J., Dubos M.-P., Sergent O., Cillard P., Morel I. Repair of iron-induced DNA oxidation by the flavonoid myricetin in primary rat hepatocyte cultures. Free. Radic. Biol. Med. 1999;26:1457–1466. doi: 10.1016/S0891-5849(99)00010-6. [DOI] [PubMed] [Google Scholar]
- 44.Wang X., Sun Y., Li P., Wu Z., Chen Y., Fu Y., Wu H., Ye Y., Wang J., Yang Z., et al. The protective effects of myricetin against acute liver failure via inhibiting inflammation and regulating oxidative stress via Nrf2 signaling. Nat. Prod. Res. 2023;37:798–802. doi: 10.1080/14786419.2022.2089138. [DOI] [PubMed] [Google Scholar]
- 45.Barzegar A. Antioxidant activity of polyphenolic myricetin in vitro cell- free and cell-based systems. Mol. Biol. Res. Commun. 2016;5:87–95. [PMC free article] [PubMed] [Google Scholar]
- 46.Salimi A., Jamali Z., Shabani M. Antioxidant potential and inhibition of mitochondrial permeability transition pore by myricetin reduces aluminium phosphide-induced cytotoxicity and mitochondrial impairments. Front. Pharmacol. 2021;12:719081. doi: 10.3389/fphar.2021.719081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pandey K.B., Mishra N., Rizvi S.I. Protective role of myricetin on oxidative stress markers in human erythrocytes subjected to oxidative stress. Nat. Prod. Commun. 2009;4:1934578X0900400211. doi: 10.1177/1934578X0900400211. [DOI] [PubMed] [Google Scholar]
- 48.Xia S.-F., Le G.-W., Wang P., Qiu Y.-Y., Jiang Y.-Y., Tang X. Regressive effect of myricetin on hepatic steatosis in mice fed a high-fat diet. Nutrients. 2016;8:799. doi: 10.3390/nu8120799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Su H.-M., Feng L.-N., Zheng X.-D., Chen W. Myricetin protects against diet-induced obesity and ameliorates oxidative stress in C57BL/6 mice. J. Zhejiang Univ. B. 2016;17:437–446. doi: 10.1631/jzus.B1600074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choi H.-N., Kang M.-J., Lee S.-J., Kim J.-I. Ameliorative effect of myricetin on insulin resistance in mice fed a high-fat, high-sucrose diet. Nutr. Res. Pr. 2014;8:544–549. doi: 10.4162/nrp.2014.8.5.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ma J., Liu J., Chen Y., Yu H., Xiang L. Myricetin Improves Impaired Nerve Functions in Experimental Diabetic Rats. Front. Endocrinol. 2022;13:915603. doi: 10.3389/fendo.2022.915603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rahmani A.H., A Alharbi H.O., Khan A.A., Babiker A.Y., Alam Rizvi M.M. Therapeutic potential of resveratrol, a polyphenol in the prevention of liver injury induced by diethylnitrosamine (DEN) through the regulation of inflammation and oxidative stress. Funct. Foods Health Dis. 2024;14:898–920. doi: 10.31989/ffhd.v14i12.1502. [DOI] [Google Scholar]
- 53.Rahmani A.H., Babiker A.Y. Review on role of honey in disease prevention and treatment through modulation of biological activities. Open Life Sci. 2025;20:20251069. doi: 10.1515/biol-2025-1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alzohairy M.A., Khan A.A., Ansari M.A., Babiker A.Y., Alsahli M.A., Almatroodi S.A., Rahmani A.H. Protective effect of quercetin, a Flavonol against benzo (a) pyrene-induced lung injury via inflammation, oxidative stress, angiogenesis and Cyclooxygenase-2 Signalling molecule. Appl. Sci. 2021;11:8675. doi: 10.3390/app11188675. [DOI] [Google Scholar]
- 55.Serafini M., Peluso I., Raguzzini A. Flavonoids as Anti-Inflammatory Agents. Proc. Nutr. Soc. 2010;69:273–278. doi: 10.1017/S002966511000162X. [DOI] [PubMed] [Google Scholar]
- 56.García-Lafuente A., Guillamón E., Villares A., Rostagno M.A., Martínez J.A. Flavonoids as Anti-Inflammatory Agents: Implications in Cancer and Cardiovascular Disease. Inflamm. Res. 2009;58:537–552. doi: 10.1007/s00011-009-0037-3. [DOI] [PubMed] [Google Scholar]
- 57.Read M.A. Flavonoids: Naturally occurring anti-inflammatory agents. Am. J. Pathol. 1995;147:235–237. [PMC free article] [PubMed] [Google Scholar]
- 58.Ferrali M., Signorini C., Caciotti B., Sugherini L., Ciccoli L., Giachetti D., Comporti M. Protection against oxidative damage of erythrocyte membrane by the flavonoid quercetin and its relation to iron chelating activity. FEBS Lett. 1997;416:123–129. doi: 10.1016/S0014-5793(97)01182-4. [DOI] [PubMed] [Google Scholar]
- 59.Cho B.O., Yin H.H., Park S.H., Byun E.B., Ha H.Y., Jang S.I. Anti-inflammatory activity of myricetin from Diospyros lotus through suppression of NF-κB and STAT1 activation and Nrf2-mediated HO-1 induction in lipopolysaccharide-stimulated RAW264.7 macrophages. Biosci. Biotechnol. Biochem. 2016;80:1520–1530. doi: 10.1080/09168451.2016.1171697. [DOI] [PubMed] [Google Scholar]
- 60.Rosas-Martínez M., Gutiérrez-Venegas G. Myricetin Inhibition of Peptidoglycan-Induced COX-2 Expression in H9c2 Cardiomyocytes. Prev. Nutr. Food Sci. 2019;24:202–209. doi: 10.3746/pnf.2019.24.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fu R.H., Liu S.P., Chu C.L., Lin Y.H., Ho Y.C., Chiu S.C., Lin W.Y., Shyu W.C., Lin S.Z. Myricetin attenuates lipopolysaccharide-stimulated activation of mouse bone marrow-derived dendritic cells through suppression of IKK/NF-κB and MAPK sig-nalling pathways. J. Sci. Food Agric. 2013;93:76–84. doi: 10.1002/jsfa.5733. [DOI] [PubMed] [Google Scholar]
- 62.Zhang N., Feng H., Liao H., Chen S., Yang Z., Deng W., Tang Q. Myricetin attenuated LPS induced cardiac injury in vivo and in vitro. Phytotherapy Res. 2018;32:459–470. doi: 10.1002/ptr.5989. [DOI] [PubMed] [Google Scholar]
- 63.Lee C.S. Flavonoid myricetin inhibits TNF-stimulated production of inflammatory mediators by suppressing the Akt, mTOR and NF-κB pathways in human keratinocytes. Eur. J. Pharmacol. 2016;784:164–172. doi: 10.1016/j.ejphar.2016.05.025. [DOI] [PubMed] [Google Scholar]
- 64.Xie J., Zheng Y. Myricetin protects keratinocyte damage induced by UV through IκB/NFκb signaling pathway. J. Cosmet. Dermatol. 2017;16:444–449. doi: 10.1111/jocd.12399. [DOI] [PubMed] [Google Scholar]
- 65.Lee Y.S., Choi E.M. Myricetin inhibits IL-1β-induced inflammatory mediators in SW982 human synovial sarcoma cells. Int. Immunopharmacol. 2010;10:812–814. doi: 10.1016/j.intimp.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 66.Hassan S.M., Khalaf M.M., Sadek S.A., Abo-Youssef A.M. Protective effects of apigenin and myricetin against cisplatin-induced nephrotoxicity in mice. Pharm. Biol. 2017;55:766–774. doi: 10.1080/13880209.2016.1275704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mao M., Huang M. Myricetin attenuates lung inflammation and provides protection against lipopolysaccharide-induced acute lung injury by inhibition of NF-κB pathway in rats. Trop. J. Pharm. Res. 2017;16:2585. doi: 10.4314/tjpr.v16i11.3. [DOI] [Google Scholar]
- 68.Chen K., Yang C., Li T., Zouboulis C.C., Huang Y. Suppression of Propionibacterium acnes-stimulated proinflammatory cytokines by Chinese bayberry extracts and its active constituent myricetin in human sebocytes in vitro. Phytotherapy Res. 2019;33:1104–1113. doi: 10.1002/ptr.6304. [DOI] [PubMed] [Google Scholar]
- 69.Kuo P.L. Myricetin inhibits the induction of anti-Fas IgM-, tumor necrosis factor-alpha- and interleukin-1beta-mediated apoptosis by Fas pathway inhibition in human osteoblastic cell line MG-63. Life Sci. 2005;77:2964–2976. doi: 10.1016/j.lfs.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 70.Jang J.-H., Lee S.H., Jung K., Yoo H., Park G. Inhibitory Effects of Myricetin on Lipopolysaccharide-Induced Neuroinflammation. Brain Sci. 2020;10:32. doi: 10.3390/brainsci10010032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kan X., Liu B., Guo W., Wei L., Lin Y., Guo Y., Gong Q., Li Y., Xu D., Cao Y., et al. Myricetin relieves LPS-induced mastitis by inhibiting inflammatory response and repairing the blood–milk barrier. J. Cell. Physiol. 2019;234:16252–16262. doi: 10.1002/jcp.28288. [DOI] [PubMed] [Google Scholar]
- 72.Rehm J., Samokhvalov A.V., Shield K.D. Global burden of alcoholic liver diseases. J. Hepatol. 2013;59:160–168. doi: 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 73.Devarbhavi H., Asrani S.K., Arab J.P., Nartey Y.A., Pose E., Kamath P.S. Global burden of liver disease: 2023 update. J. Hepatol. 2023;79:516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 74.Adewusi E., Afolayan A. A review of natural products with hepatoprotective activity. J. Med. Plants Res. 2010;4:1318–1334. [Google Scholar]
- 75.Almatroodi S.A., Alsahli M.A., Alharbi H.M., Khan A.A., Husain Rahmani A. Epigallocatechin-3-gallate (EGCG), an active con-stituent of green tea: Implications in the prevention of liver injury induced by diethylnitrosamine (DEN) in rats. Appl. Sci. 2019;9:4821. doi: 10.3390/app9224821. [DOI] [Google Scholar]
- 76.Abushady E.A., Elagaty S.M., Nassef N.A., Abdelhamid G.S. The potential hepatoprotective effect of quercetin on cholestatic liver injury in rats. Qjm Int. J. Med. 2020;113((Suppl. S1)):hcaa065-002. doi: 10.1093/qjmed/hcaa065.002. [DOI] [Google Scholar]
- 77.Oke G.O., Abiodun A.A., Imafidon C.E., Monsi B.F. Zingiber officinale (Roscoe) mitigates CCl4-induced liver histopathology and biochemical derangements through antioxidant, membrane-stabilizing and tissue-regenerating potentials. Toxicol. Rep. 2019;6:416–425. doi: 10.1016/j.toxrep.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Geng Y., Sun Q., Li W., Lu Z., Xu H., Shi J., Xu Z. The common dietary flavonoid myricetin attenuates liver fibrosis in carbon tetrachloride treated mice. Mol. Nutr. Food Res. 2017;61:1600392. doi: 10.1002/mnfr.201600392. [DOI] [PubMed] [Google Scholar]
- 79.Xia S.F., Qiu Y.Y., Chen L.M., Jiang Y.Y., Huang W., Xie Z.X., Tang X., Sun J. Myricetin alleviated hepatic steatosis by acting on microRNA-146b/thyroid hormone receptor b pathway in high-fat diet fed C57BL/6J mice. Food Funct. 2019;10:1465–1477. doi: 10.1039/C8FO01452C. [DOI] [PubMed] [Google Scholar]
- 80.Lv H., An B., Yu Q., Cao Y., Liu Y., Li S. The hepatoprotective effect of myricetin against lipopolysaccharide and D-galactosamine-induced fulminant hepatitis. Int. J. Biol. Macromol. 2020;155:1092–1104. doi: 10.1016/j.ijbiomac.2019.11.075. [DOI] [PubMed] [Google Scholar]
- 81.Rostami A., Baluchnejadmojarad T., Roghani M. Hepatoprotective Effect of Myricetin following Lipopolysaccharide/DGalactosamine: Involvement of Autophagy and Sirtuin 1. Curr. Mol. Pharmacol. 2023;16:419–433. doi: 10.2174/1874467215666220614101721. [DOI] [PubMed] [Google Scholar]
- 82.Sun W.-L., Li X.-Y., Dou H.-Y., Wang X.-D., Li J.-D., Shen L., Ji H.-F. Myricetin supplementation decreases hepatic lipid synthesis and inflammation by modulating gut microbiota. Cell Rep. 2021;36:109641. doi: 10.1016/j.celrep.2021.109641. [DOI] [PubMed] [Google Scholar]
- 83.Berköz M., Ünal S., Karayakar F., Yunusoğlu O., Özkan-Yılmaz F., Özlüer-Hunt A., Aslan A. Prophylactic effect of myricetin and apigenin against lipopolysaccharide-induced acute liver injury. Mol. Biol. Rep. 2021;48:6363–6373. doi: 10.1007/s11033-021-06637-x. [DOI] [PubMed] [Google Scholar]
- 84.Choi H.-N., Shin J.-Y., Kim J.-I. Ameliorative Effect of Myricetin on Nonalcoholic Fatty Liver Disease in ob/ob Mice. J. Med. Food. 2021;24:1092–1099. doi: 10.1089/jmf.2021.K.0090. [DOI] [PubMed] [Google Scholar]
- 85.Zamljen T., Medič A., Veberič R., Hudina M., Štampar F., Slatnar A. Apple Fruit (Malus domestica Borkh.) Metabolic Re-sponse to Infestation by Invasive Brown Marmorated Stink Bug (Halyomorpha halys Stal.) Horticulturae. 2021;7:212. doi: 10.3390/horticulturae7080212. [DOI] [Google Scholar]
- 86.Emon N.U., Alam S., Rudra S., Al Haidar I.K., Farhad M., Rana M.E.H., Ganguly A. Antipyretic activity of the leaves ex-tract of Caesalpinia digyna Rottl along with phytoconstituent’s binding affinity to COX-1, COX-2 and mPGES-1 receptors: An in vivo and in silico approaches (Antipyretic activity of Caesalpinia digyna Rottl) Saudi J. Biol. Sci. 2021;28:5302–5309. doi: 10.1016/j.sjbs.2021.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rahmani A.H., Alsahli M.A., Khan A.A., Almatroodi S.A. Quercetin, a plant flavonol attenuates diabetic complications, renal tissue damage, renal oxidative stress and inflammation in streptozotocin-induced diabetic rats. Metabolites. 2023;13:130. doi: 10.3390/metabo13010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Almatroodi S.A., Alnuqaydan A.M., Babiker A.Y., Almogbel M.A., Khan A.A., Husain Rahmani A. 6-Gingerol, a bioactive compound of ginger attenuates renal damage in streptozotocin-induced diabetic rats by regulating the oxidative stress and in-flammation. Pharmaceutics. 2021;13:317. doi: 10.3390/pharmaceutics13030317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alsulaim A.K., Almutaz T.H., Albati A.A., Rahmani A.H. Therapeutic Potential of Curcumin, a Bioactive Compound of Turmeric, in Prevention of Streptozotocin-Induced Diabetes through the Modulation of Oxidative Stress and Inflammation. Molecules. 2023;29:128. doi: 10.3390/molecules29010128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kandasamy N., Ashokkumar N. Protective effect of bioflavonoid myricetin enhances carbohydrate metabolic enzymes and insulin signaling molecules in streptozotocin–cadmium induced diabetic nephrotoxic rats. Toxicol. Appl. Pharmacol. 2014;279:173–185. doi: 10.1016/j.taap.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 91.Kandasamy N., Ashokkumar N. Renoprotective effect of myricetin restrains dyslipidemia and renal mesangial cell proliferation by the suppression of sterol regulatory element binding proteins in an experimental model of diabetic nephropathy. Eur. J. Pharmacol. 2014;743:53–62. doi: 10.1016/j.ejphar.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 92.Zhao Z., Chen Y., Li X., Zhu L., Wang X., Li L., Sun H., Han X., Li J. Myricetin relieves the symptoms of type 2 diabetes mice and regulates intestinal microflora. Biomed. Pharmacother. 2022;153:113530. doi: 10.1016/j.biopha.2022.113530. [DOI] [PubMed] [Google Scholar]
- 93.Liao H.H., Zhu J.X., Feng H., Ni J., Zhang N., Chen S., Liu H.J., Yang Z., Deng W., Tang Q.Z. Myricetin possesses potential protective effects on diabetic cardiomyopathy through inhibiting IκBα/NFκB and enhancing Nrf2/HO-1. Oxidative Med. Cell. Longev. 2017;2017:8370593. doi: 10.1155/2017/8370593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.yang Z.J., Wang H.R., Wang Y.I., Zhai Z.H., Wang L.W., Li L., Zhang C., Tang L. Myricetin Attenuated Diabetes-Associated Kidney Injuries and Dysfunction via Regulating Nuclear Factor (Erythroid Derived 2)-Like 2 and Nuclear Factor-κB Signaling. Front. Pharmacol. 2019;10:647. doi: 10.3389/fphar.2019.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhu J., Bao Z., Hu Z., Wu S., Tian C., Zhou Y., Ding Z., Tan X. Myricetin alleviates diabetic cardiomyopathy by regulating gut microbiota and their metabolites. Nutr. Diabetes. 2024;14:10. doi: 10.1038/s41387-024-00268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Qian J., Zhang J., Chen Y., Dai C., Fan J., Guo H. Hypoglycemic activity and mechanisms of myricetin. Nat. Prod. Res. 2022;36:6177–6180. doi: 10.1080/14786419.2022.2058941. [DOI] [PubMed] [Google Scholar]
- 97.Liu I.-M., Tzeng T.-F., Liou S.-S., Lan T.-W. Myricetin, a naturally occurring flavonol, ameliorates insulin resistance induced by a high-fructose diet in rats. Life Sci. 2007;81:1479–1488. doi: 10.1016/j.lfs.2007.08.045. [DOI] [PubMed] [Google Scholar]
- 98.Kandasamy N., Ashokkumar N. Myricetin, a natural flavonoid, normalizes hyperglycemia in streptozotocin-cadmium-induced experimental diabetic nephrotoxic rats. Biomed. Prev. Nutr. 2012;2:246–251. doi: 10.1016/j.bionut.2012.04.003. [DOI] [Google Scholar]
- 99.Ozcan F., Ozmen A., Akkaya B., Aliciguzel Y., Aslan M. Beneficial effect of myricetin on renal functions in streptozotocin-induced diabetes. Clin. Exp. Med. 2012;12:265–272. doi: 10.1007/s10238-011-0167-0. [DOI] [PubMed] [Google Scholar]
- 100.Liu I.-M., Liou S.-S., Lan T.-W., Hsu F.-L., Cheng J.-T. Myricetin as the active principle of Abelmoschus moschatus to lower plasma glucose in streptozotocin-induced diabetic rats. Planta Medica. 2005;71:617–621. doi: 10.1055/s-2005-871266. [DOI] [PubMed] [Google Scholar]
- 101.Roth G.A., Mensah G.A., Johnson C.O., Addolorato G., Ammirati E., Baddour L.M., Barengo N.C., Beaton A.Z., Benjamin E.J., Benziger C.P., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the gbd 2019 study. J. Am. Coll. Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Andersson C., Johnson A.D., Benjamin E.J., Levy D., Vasan R.S. 70-year legacy of the framingham heart study. Nat. Rev. Cardiol. 2019;16:687–698. doi: 10.1038/s41569-019-0202-5. [DOI] [PubMed] [Google Scholar]
- 103.Mozaffarian D., Wu J.H.Y. Flavonoids, dairy foods, and cardiovascular and metabolic health: A review of emerging biologic pathways. Circ. Res. 2018;122:369–384. doi: 10.1161/CIRCRESAHA.117.309008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Khan J., Deb P.K., Priya S., Medina K.D., Devi R., Walode S.G., Rudrapal M. Dietary Flavonoids: Cardioprotective Potential with Antioxidant Effects and Their Pharmacokinetic, Toxicological and Therapeutic Concerns. Molecules. 2021;26:4021. doi: 10.3390/molecules26134021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tiwari R., Mohan M., Kasture S., Maxia A., Ballero M. Cardioprotective potential of myricetin in isoproterenol-induced myocardial infarction in Wistar rats. Phytother Res. 2009;23:1361–1366. doi: 10.1002/ptr.2688. [DOI] [PubMed] [Google Scholar]
- 106.Chen S., Fan B. Myricetin protects cardiomyocytes from LPS-induced injury. Herz. 2018;43:265–274. doi: 10.1007/s00059-017-4556-3. [DOI] [PubMed] [Google Scholar]
- 107.Qiu Y., Cong N., Liang M., Wang Y., Wang J. Systems Pharmacology Dissection of the Protective Effect of Myricetin Against Acute Ischemia/Reperfusion-Induced Myocardial Injury in Isolated Rat Heart. Cardiovasc. Toxicol. 2017;17:277–286. doi: 10.1007/s12012-016-9382-y. [DOI] [PubMed] [Google Scholar]
- 108.Zhang B., Shen Q., Chen Y., Pan R., Kuang S., Liu G., Sun G., Sun X. Myricitrin Alleviates Oxidative Stress-induced Inflammation and Apoptosis and Protects Mice against Diabetic Cardiomyopathy. Sci. Rep. 2017;7:srep44239. doi: 10.1038/srep44239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Li J., Luo T., Zhao Y., Wang D., Jin Y., Wu Z., Yang G., Qi X. Cardioprotective potentials of myricetin on doxorubicin-induced cardiotoxicity based on biochemical and transcriptomic analysis. Biomed. Pharmacother. 2024;175:116748. doi: 10.1016/j.biopha.2024.116748. [DOI] [PubMed] [Google Scholar]
- 110.Nie N., Li Z., Li W., Huang X., Jiang Z., Shen Y. Myricetin ameliorates experimental autoimmune myocarditis in mice by modulating immune response and inhibiting MCP-1 expression. Eur. J. Pharmacol. 2023;942:175549. doi: 10.1016/j.ejphar.2023.175549. [DOI] [PubMed] [Google Scholar]
- 111.Arafah A., Rehman M.U., Ahmad A., AlKharfy K.M., Alqahtani S., Jan B.L., Almatroudi N.M. Myricetin (3,3′,4′,5,5′,7-Hexahydroxyflavone) Prevents 5-Fluorouracil-Induced Cardiotoxicity. ACS Omega. 2022;7:4514–4524. doi: 10.1021/acsomega.1c06475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Feigin V.L., Abajobir A.A., Abate K.H., Abd-Allah F., Abdulle A.M., Abera S.F., Abyu G.Y., Ahmed M.B., Aichour A.N., Aichour I., et al. Global, Regional, and National Burden of Neurological Disorders During 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Selkoe D.J., Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol. Med. 2016;8:595–608. doi: 10.15252/emmm.201606210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ramezani M., Darbandi N., Khodagholi F., Hashemi A. Myricetin protects hippocampal CA3 pyramidal neurons and improves learning and memory impairments in rats with Alzheimer’s disease. Neural Regen. Res. 2016;11:1976–1980. doi: 10.4103/1673-5374.197141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang L., Tang Z., Li B., Peng Y., Yang X., Xiao Y., Ni R., Qi X.-L. Myricetin ameliorates cognitive impairment in 3×Tg Alzheimer’s disease mice by regulating oxidative stress and tau hyperphosphorylation. Biomed. Pharmacother. 2024;177:116963. doi: 10.1016/j.biopha.2024.116963. [DOI] [PubMed] [Google Scholar]
- 116.Wang B., Zhong Y., Gao C., Li J. Myricetin ameliorates scopolamine-induced memory impairment in mice via inhibiting acetylcholinesterase and down-regulating brain iron. Biochem. Biophys. Res. Commun. 2017;490:336–342. doi: 10.1016/j.bbrc.2017.06.045. [DOI] [PubMed] [Google Scholar]
- 117.Gu S.-C., Xie Z.-G., Gu M.-J., Wang C.-D., Xu L.-M., Gao C., Yuan X.-L., Wu Y., Hu Y.-Q., Cao Y., et al. Myricetin mitigates motor disturbance and decreases neuronal ferroptosis in a rat model of Parkinson’s disease. Sci. Rep. 2024;14:15107. doi: 10.1038/s41598-024-62910-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Huang B., Liu J., Ma D., Chen G., Wang W., Fu S. Myricetin prevents dopaminergic neurons from undergoing neuroinflammation-mediated degeneration in a lipopolysaccharide-induced Parkinson’s disease model. J. Funct. Foods. 2018;45:452–461. doi: 10.1016/j.jff.2018.04.018. [DOI] [Google Scholar]
- 119.Karuppaiah J., Dhanraj V., Balakrishnan R., Elangovan N. Myricetin attenuates neurodegeneration and cognitive impairment in Parkinsonism. Front. Biosci. 2018;10:481–494. doi: 10.2741/e835. [DOI] [PubMed] [Google Scholar]
- 120.Ara G., Afzal M., Jyoti S., Naz F., Rahul, Siddique Y.H. Effect of Myricetin on the loss of dopaminergic neurons in the transgenic Drosophila model of Parkinson’s disease. Curr. Drug Ther. 2019;14:58–64. doi: 10.2174/1574885513666180529114546. [DOI] [Google Scholar]
- 121.Ma Z.-G., Wang J., Jiang H., Liu T.-W., Xie J.-X. Myricetin reduces 6-hydroxydopamine-induced dopamine neuron degeneration in rats. NeuroReport. 2007;18:1181–1185. doi: 10.1097/WNR.0b013e32821c51fe. [DOI] [PubMed] [Google Scholar]
- 122.Sun Z.Q., Meng F.H., Tu L.X., Sun L. Myricetin attenuates the severity of seizures and neuroapoptosis in pentylenetetrazole kindled mice by regulating the of BDNF-TrkB signaling pathway and modulating matrix metalloproteinase-9 and GABAA. Exp. Ther. Med. 2019;17:3083–3091. doi: 10.3892/etm.2019.7282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Demyashkin G., Blinova E., Grigoryan M., Parshenkov M., Skovorodko P., Ius V., Lebed A., Shegay P., Kaprin A. Neuroprotective Effects of Myricetin on PTZ-Induced Seizures in Mice: Evaluation of Oxidation, Neuroinflammation and Metabolism, and Apoptosis in the Hippocampus. Curr. Issues Mol. Biol. 2024;46:8914–8944. doi: 10.3390/cimb46080527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bhatt A.P., Redinbo M.R., Bultman S.J. The role of the microbiome in cancer development and therapy. CA A Cancer J. Clin. 2017;67:326–344. doi: 10.3322/caac.21398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Cronin K.A., Lake A.J., Scott S., Sherman R.L., Noone A.M., Howlader N., Henley S.J., Anderson R.N., Firth A.U., Ma J., et al. Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics. Cancer. 2018;124:2785–2800. doi: 10.1002/cncr.31551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Madhuri S., Pandey G. Some anticancer medicinal plants of foreign origin. Curr. Sci. 2009;25:779–783. [Google Scholar]
- 127.Cragg G.M., Pezzuto J.M. Natural Products as a Vital Source for the Discovery of Cancer Chemotherapeutic and Chemopreventive Agents. Med. Princ. Pract. 2016;25((Suppl. S2)):41–59. doi: 10.1159/000443404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Almatroodi S.A., Alsahli M.A., Rahmani A.H. Berberine: Berberine: An important emphasis on its anticancer effects through modulation of various cell signaling pathways. Molecules. 2022;27:5889. doi: 10.3390/molecules27185889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Almajali B., Al-Jamal H.A., Taib W.R., Ismail I., Johan M.F., Doolaanea A.A., Ibrahim W.N. Thymoquinone, as a novel therapeutic candidate of cancers. Pharmaceuticals. 2021;14:369. doi: 10.3390/ph14040369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Almatroodi S.A., Syed M.A., Rahmani A.H. Potential therapeutic targets of curcumin, most abundant active compound of turmeric spice: Role in the management of various types of cancer. Recent Pat. Anti-Cancer Drug Discov. 2021;16:3–29. doi: 10.2174/1574892815999201102214602. [DOI] [PubMed] [Google Scholar]
- 131.Huang H., Chen A.Y., Rojanasakul Y., Ye X., Rankin G.O., Chen Y.C. Dietary compounds galangin and myricetin suppress ovarian cancer cell angiogenesis. J. Funct. Foods. 2015;15:464–475. doi: 10.1016/j.jff.2015.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhou Z., Mao W., Li Y., Qi C., He Y. Myricetin inhibits breast tumor growth and angiogenesis by regulating VEGF/VEGFR2 and p38MAPK signaling pathways. Anat. Rec. 2019;302:2186–2192. doi: 10.1002/ar.24222. [DOI] [PubMed] [Google Scholar]
- 133.Niu X., Ding X., Tong Q., Huang X., Ma X., Li Z., Wang Q., Wang Y. Myricetin inhibits 4 T1 breast tumor growth in mice via induc-tion of Nrf-2/GPX4 pathway-mediated Ferroptosis. Toxicol. Appl. Pharmacol. 2024;3:116990. doi: 10.1016/j.taap.2024.116990. [DOI] [PubMed] [Google Scholar]
- 134.Han S.-H., Lee J.-H., Woo J.-S., Jung G.-H., Jung S.-H., Han E.-J., Kim B., Cho S.D., Nam J.S., Che J.H., et al. Myricetin induces apoptosis and autophagy in human gastric cancer cells through inhibition of the PI3K/Akt/mTOR pathway. Heliyon. 2022;8:e09309. doi: 10.1016/j.heliyon.2022.e09309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Feng J., Chen X., Wang Y., Du Y., Sun Q., Zang W., Zhao G. Myricetin inhibits proliferation and induces apoptosis and cell cycle arrest in gastric cancer cells. Mol. Cell. Biochem. 2015;408:163–170. doi: 10.1007/s11010-015-2492-1. [DOI] [PubMed] [Google Scholar]
- 136.Phillips P., Sangwan V., Borja-Cacho D., Dudeja V., Vickers S., Saluja A. Myricetin induces pancreatic cancer cell death via the induction of apoptosis and inhibition of the phosphatidylinositol 3-kinase (PI3K) signaling pathway. Cancer Lett. 2011;308:181–188. doi: 10.1016/j.canlet.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li H.G., Chen J.X., Xiong J.H., Zhu J.W. Myricetin exhibits anti-glioma potential by inducing mitochondrial-mediated apoptosis, cell cycle arrest, inhibition of cell migration and ROS generation. J BUON. 2016;21:182–190. [PubMed] [Google Scholar]
- 138.Yang W., Su J., Li M., Li T., Wang X., Zhao M., Hu X. Myricetin induces autophagy and cell cycle arrest of HCC by inhibiting MARCH1-regulated Stat3 and p38 MAPK signaling pathways. Front. Pharmacol. 2021;12:709526. doi: 10.3389/fphar.2021.709526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang X.H., Zou Z.Q., Xu C.W., Shen Y.Z., Li D. Myricetin induces G2/M phase arrest in HepG2 cells by inhibiting the activity of the cyclin B/Cdc2 complex. Mol. Med. Rep. 2011;4:273–277. doi: 10.3892/mmr.2011.417. [DOI] [PubMed] [Google Scholar]
- 140.Ji A., Hu L., Ma D., Qiang G., Yan D., Zhang G., Jiang C. Myricetin Induces Apoptosis and Protective Autophagy through Endoplasmic Reticulum Stress in Hepatocellular Carcinoma. Evid. Based Complement. Altern. Med. 2022;2022:3115312. doi: 10.1155/2022/3115312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yang H.-W., Lan Y., Li A., Wu H., Song Z.-W., Wan A.-L., Wang Y., Li S.-B., Ji S., Wang Z.-C., et al. Myricetin suppresses TGF-β-induced epithelial-to-mesenchymal transition in ovarian cancer. Front. Pharmacol. 2023;14:1288883. doi: 10.3389/fphar.2023.1288883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Senggunprai L., Tuponchai P., Kukongviriyapan V., Prawan A., Kongpetch S. Myricetin ameliorates cytokine-induced migration and invasion of cholangiocarcinoma cells via suppression of STAT3 pathway. J. Cancer Res. Ther. 2019;15:157–163. doi: 10.4103/jcrt.JCRT_287_17. [DOI] [PubMed] [Google Scholar]
- 143.Xie M., Liu X., Cao X., Guo M., Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir. Res. 2020;21:49. doi: 10.1186/s12931-020-1291-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rahman M., Bibi S., Rahaman S., Rahman F., Islam F., Khan M.S., Hasan M.M., Parvez A., Hossain A., Maeesa S.K., et al. Natural therapeutics and nutraceuticals for lung diseases: Traditional significance, phytochemistry, and pharmacology. Biomed. Pharmacother. 2022;150:113041. doi: 10.1016/j.biopha.2022.113041. [DOI] [PubMed] [Google Scholar]
- 145.Abdulaal W.H., Omar U.M., Zeyadi M., El-Agamy D.S., Alhakamy N.A., Almalki N.A., Asfour H.Z., Al-Rabia M.W., Alzain A.A., Mohamed G.A., et al. Protective effect of kaempferol glucoside against lipopolysaccharide-caused acute lung injury via targeting Nrf2/NF-κB/NLRP3/GSDMD: Integrating experimental and computational studies. Saudi Pharm. J. 2024;32:102073. doi: 10.1016/j.jsps.2024.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Xu H., Qi Q., Yan X. Myricetin ameliorates sepsis-associated acute lung injury in a murine sepsis model. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2021;394:165–175. doi: 10.1007/s00210-020-01880-8. [DOI] [PubMed] [Google Scholar]
- 147.Yang W., Li B., Yang G. The protective effects and mechanisms of myricetin on LPS-induced acute lung injury of BALB/c mice. Int. J. Tradit. Chin. Med. 2019;6:154–159. [Google Scholar]
- 148.Huang W.-C., Wu S.-J., Yeh K.-W., Huang T., Liou C.-J. Protective effects of myricetin on airway inflammation and oxidative stress in ovalbumin-induced asthma mice. J. Nutr. Biochem. 2024;123:109485. doi: 10.1016/j.jnutbio.2023.109485. [DOI] [PubMed] [Google Scholar]
- 149.Li X., Yu H., Liang L., Bi Z., Wang Y., Gao S., Wang M., Li H., Miao Y., Deng R., et al. Myricetin ameliorates bleomycin-induced pulmonary fibrosis in mice by inhibiting TGF-β signaling via targeting HSP90β. Biochem. Pharmacol. 2020;178:114097. doi: 10.1016/j.bcp.2020.114097. [DOI] [PubMed] [Google Scholar]
- 150.Dmochowska N., Wardill H.R., Hughes P.A. Advances in Imaging Specific Mediators of Inflammatory Bowel Disease. Int. J. Mol. Sci. 2018;19:2471. doi: 10.3390/ijms19092471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Gubatan J., Kulkarni C.V., Talamantes S.M., Temby M., Fardeen T., Sinha S.R. Dietary Exposures and Interventions in Inflammatory Bowel Disease: Current Evidence and Emerging Concepts. Nutrients. 2023;15:579. doi: 10.3390/nu15030579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ng S.C., Shi H.Y., Hamidi N., Underwood F.E., Tang W., Benchimol E.I., Panaccione R., Ghosh S., Wu J.C.Y., Chan F.K.L., et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet. 2017;390:2769–2778. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 153.Zhao J., Hong T., Dong M., Meng Y., Mu J. Protective effect of myricetin in dextran sulphate sodium-induced murine ulcerative colitis. Mol. Med. Rep. 2013;7:565–570. doi: 10.3892/mmr.2012.1225. [DOI] [PubMed] [Google Scholar]
- 154.Zhou X.-L., Yang J., Qu X.-J., Meng J., Miao R.-R., Cui S.-X. M10, a Myricetin-3-O-b-D-Lactose Sodium Salt, Prevents Ulcerative Colitis Through Inhibiting Necroptosis in Mice. Front. Pharmacol. 2020;11:557312. doi: 10.3389/fphar.2020.557312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Qu X., Li Q., Song Y., Xue A., Liu Y., Qi D., Dong H. Potential of myricetin to restore the immune balance in dextran sulfate sodium-induced acute murine ulcerative colitis. J. Pharm. Pharmacol. 2020;72:92–100. doi: 10.1111/jphp.13197. [DOI] [PubMed] [Google Scholar]
- 156.Wang F., Song Z.-Y., Qu X.-J., Li F., Zhang L., Li W.-B., Cui S.-X. M10, a novel derivative of Myricetin, prevents ulcerative colitis and colorectal tumor through attenuating robust endoplasmic reticulum stress. Carcinogenesis. 2018;39:889–899. doi: 10.1093/carcin/bgy057. [DOI] [PubMed] [Google Scholar]
- 157.Lin X., Li H. Obesity: Epidemiology, pathophysiology, and therapeutics. Front. Endocrinol. 2021;12:706978. doi: 10.3389/fendo.2021.706978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Kim S., Jin Y., Choi Y., Park T. Resveratrol exerts anti-obesity effects via mechanisms involving down-regulation of adipogenic and inflammatory processes in mice. Biochem. Pharmacol. 2011;81:1343–1351. doi: 10.1016/j.bcp.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 159.Aguirre L., Milton-Laskibar I., Hijona E., Bujanda L., Rimando A.M., Portillo M.P. Effects of pterostilbene in brown adipose tissue from obese rats. J. Physiol. Biochem. 2016;73:457–464. doi: 10.1007/s13105-017-0556-2. [DOI] [PubMed] [Google Scholar]
- 160.Wang Q., Wang S.-T., Yang X., You P.-P., Zhang W. Myricetin suppresses differentiation of 3 T3-L1 preadipocytes and enhances lipolysis in adipocytes. Nutr. Res. 2015;35:317–327. doi: 10.1016/j.nutres.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 161.Hu T., Yuan X., Wei G., Luo H., Lee H.J., Jin W. Myricetin-induced brown adipose tissue activation prevents obesity and insulin resistance in db/db mice. Eur. J. Nutr. 2018;57:391–403. doi: 10.1007/s00394-017-1433-z. [DOI] [PubMed] [Google Scholar]
- 162.Chang C.J., Tzeng T.-F., Liou S.-S., Chang Y.-S., Liu I.-M. Myricetin increases hepatic peroxisome proliferator-activated receptor protein expression and decreases plasma lipids and adiposity in rats. Evid. Based Complement. Altern. Med. 2012;2012:787152. doi: 10.1155/2012/787152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Trinh X.-T., Long N.-V., Van Anh L.T., Nga P.T., Giang N.N., Chien P.N., Nam S.-Y., Heo C.-Y. A Comprehensive Review of Natural Compounds for Wound Healing: Targeting Bioactivity Perspective. Int. J. Mol. Sci. 2022;23:9573. doi: 10.3390/ijms23179573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Elshamy A.I., Ammar N.M., Hassan H.A., El-Kashak W.A., Al-Rejaie S.S., Abd-ElGawad A.M., Farrag A.H. Topical Wound Healing Activity of Myricetin Isolated from Tecomaria capensis v. aurea. Molecules. 2020;25:4870. doi: 10.3390/molecules25214870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Elloumi W., Mahmoudi A., Ortiz S., Boutefnouchet S., Chamkha M., Sayadi S. Wound healing potential of quercetin-3-O-rhamnoside and myricetin-3-O-rhamnoside isolated from Pistacia lentiscus distilled leaves in rats model. Biomed. Pharmacother. 2022;146:112574. doi: 10.1016/j.biopha.2021.112574. [DOI] [PubMed] [Google Scholar]
- 166.Sklenářová R., Svrčková M., Hodek P., Ulrichová J., Franková J. Effect of the natural flavonoids myricetin and dihydromyricetin on the wound healing process in vitro. J. Appl. Biomed. 2021;19:149–158. doi: 10.32725/jab.2021.017. [DOI] [PubMed] [Google Scholar]
- 167.Tong Y., Zhou X.-M., Wang S.-J., Yang Y., Cao Y.-L. Analgesic activity of myricetin isolated from Myrica rubra Sieb. et Zucc. leaves. Arch. Pharmacal Res. 2009;32:527–533. doi: 10.1007/s12272-009-1408-6. [DOI] [PubMed] [Google Scholar]
- 168.Hagenacker T., Hillebrand I., Wissmann A., Büsselberg D., Schäfers M. Anti-allodynic effect of the flavonoid myricetin in a rat model of neuropathic pain: Involvement of p38 and protein kinase C mediated modulation of Ca2+channels. Eur. J. Pain. 2010;14:992–998. doi: 10.1016/j.ejpain.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 169.Córdova M.M., Werner M.F.d.P., da Silva M.D., Ruani A.P., Pizzolatti M.G., Santos A.R. Further antinociceptive effects of myricitrin in chemical models of overt nociception in mice. Neurosci. Lett. 2011;495:173–177. doi: 10.1016/j.neulet.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 170.Sharifi-Rad J., Quispe C., Shaheen S., El Haouari M., Azzini E., Butnariu M., Sarac I., Pentea M., Ramírez-Alarcón K., Martorell M., et al. Flavonoids as potential anti-platelet aggregation agents: From biochemistry to health promoting abilities. Crit. Rev. Food Sci. Nutr. 2022;62:8045–8058. doi: 10.1080/10408398.2021.1924612. [DOI] [PubMed] [Google Scholar]
- 171.Sharifi-Rad J., Quispe C., Zam W., Kumar M., Cardoso S.M., Pereira O.R., Ademiluyi A.O., Adeleke O., Moreira A.C., Živković J., et al. Phenolic bioactives as antiplatelet aggregation factors: The pivotal ingredients in maintaining cardiovascular health. Oxidative Med. Cell. Longev. 2021;2021:2195902. doi: 10.1155/2021/2195902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Zang B.-X., Jin M., Wu W., Chen W.-M., Piao Y.-Z., Li J.-R. Antagonistic effect of myricetin on platelet activing factor. Yao Xue Xue Bao Acta Pharm. Sin. 2003;38:831–833. [PubMed] [Google Scholar]
- 173.Tzeng S.-H., Ko W.-C., Ko F.-N., Teng C.-M. Inhibition of platelet aggregation by some flavonoids. Thromb. Res. 1991;64:91–100. doi: 10.1016/0049-3848(91)90208-E. [DOI] [PubMed] [Google Scholar]
- 174.Landolfi R., Mower R.L., Steiner M. Modification of platelet function and arachidonic acid metabolism by bioflavonoids. Biochem. Pharmacol. 1984;33:1525–1530. doi: 10.1016/0006-2952(84)90423-4. [DOI] [PubMed] [Google Scholar]
- 175.Gaspar R.S., da Silva S.A., Stapleton J., Fontelles J.L.d.L., Sousa H.R., Chagas V.T., Alsufyani S., Trostchansky A., Gibbins J.M., Paes A.M.d.A. Myricetin, the Main Flavonoid in Syzygium cumini Leaf, Is a Novel Inhibitor of Platelet Thiol Isomerases PDI and ERp5. Front. Pharmacol. 2020;10:1678. doi: 10.3389/fphar.2019.01678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Fan S., Gao X., Chen P., Li X. Myricetin ameliorates glucocorticoid-induced osteoporosis through the ERK signaling pathway. Life Sci. 2018;207:205–211. doi: 10.1016/j.lfs.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 177.Ying X., Chen X., Wang T., Zheng W., Chen L., Xu Y. Possible osteoprotective effects of myricetin in STZ induced diabetic osteo-porosis in rats. Eur. J. Pharmacol. 2020;866:172805. doi: 10.1016/j.ejphar.2019.172805. [DOI] [PubMed] [Google Scholar]
- 178.Ko S.Y. Myricetin suppresses LPS-induced MMP expression in human gingival fibroblasts and inhibits osteoclastogenesis by downregulating NFATc1 in RANKL-induced RAW 264.7 cells. Arch. Oral Biol. 2012;57:1623–1632. doi: 10.1016/j.archoralbio.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 179.Ying X., Chen X., Feng Y., Xu H.Z., Chen H., Yu K., Cheng S., Peng L. Myricetin enhances osteogenic differentiation through the activation of canonical Wnt/β-catenin signaling in human bone marrow stromal cells. Eur. J. Pharmacol. 2014;738:22–30. doi: 10.1016/j.ejphar.2014.04.049. [DOI] [PubMed] [Google Scholar]
- 180.Huang J., Wu C., Tian B., Zhou X., Ma N., Qian Y. Myricetin prevents alveolar bone loss in an experimental ovariectomized mouse model of periodontitis. Int. J. Mol. Sci. 2016;17:422. doi: 10.3390/ijms17030422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Yamaguchi M., Hamamoto R., Uchiyama S., Ishiyama K. Effects of flavonoid on calcium content in femoral tissue culture and parathyroid hormone-stimulated osteoclastogenesis in bone marrow culture in vitro. Mol. Cell. Biochem. 2007;303:83–88. doi: 10.1007/s11010-007-9458-x. [DOI] [PubMed] [Google Scholar]
- 182.Chen R., Hollborn M., Grosche A., Reichenbach A., Wiedemann P., Bringmann A., Kohen L. Effects of the vegetable polyphenols epigallocatechin-3-gallate, luteolin, apigenin, myricetin, quercetin, and cyanidin in primary cultures of human retinal pigment epithelial cells. Mol. Vis. 2014;20:242–258. [PMC free article] [PubMed] [Google Scholar]
- 183.Hodges L.C., Kearse E.C., Green K. Intraocular pressure-lowering activity of phenolic antioxidants in normotensive rabbits. Curr. Eye Res. 1999;19:234–240. doi: 10.1076/ceyr.19.3.234.5320. [DOI] [PubMed] [Google Scholar]
- 184.Laabich A., Manmoto C.C., Kuksa V., Leung D.W., Vissvesvaran G.P., Karliga I., Kamat M., Scott I.L., Fawzi A., Kubota R. Protective effects of myricetin and related flavonols against A2E and light mediated-cell death in bovine retinal primary cell culture. Exp. Eye Res. 2007;85:154–165. doi: 10.1016/j.exer.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 185.Qing Y., Li Y., Luo L. Effect of myricetin on primary open-angle glaucoma. Transl. Neurosci. 2018;9:132–141. doi: 10.1515/tnsci-2018-0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Nahar N., Mohamed S., Mustapha N.M., Fong L.S., Ishak N.I.M. Gallic acid and myricetin-rich Labisia pumila extract mitigated multiple diabetic eye disorders in rats. J. Food Biochem. 2021;45:e13948. doi: 10.1111/jfbc.13948. [DOI] [PubMed] [Google Scholar]
- 187.Bortoluzzi A., Furini F., Scirè C.A. Osteoarthritis and its management—Epidemiology, nutritional aspects and environmental factors. Autoimmun. Rev. 2018;17:1097–1104. doi: 10.1016/j.autrev.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 188.Mabey T., Honsawek S. Cytokines as biochemical markers for knee osteoarthritis. World J. Orthop. 2015;6:95–105. doi: 10.5312/wjo.v6.i1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Nelson A. Osteoarthritis year in review 2017: Clinical. Osteoarthr. Cartil. 2018;26:319–325. doi: 10.1016/j.joca.2017.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Yan Z., Lin Z., Wu Y., Zhan J., Qi W., Lin J., Shen J., Xue X., Pan X. The protective effect of myricitrin in osteoarthritis: An in vitro and in vivo study. Int. Immunopharmacol. 2020;84:106511. doi: 10.1016/j.intimp.2020.106511. [DOI] [PubMed] [Google Scholar]
- 191.Liu X., Fang H., Zeng C., Cai D. Myricetin attenuates osteoarthritis by blockade of the IL-1β/MAPK pathway. Osteoarthr. Cartil. 2018;26:S84. doi: 10.1016/j.joca.2018.02.181. [DOI] [Google Scholar]
- 192.Pan X., Chen T., Zhang Z., Chen X., Chen C., Chen L., Wang X., Ying X. Activation of Nrf2/HO-1 signal with Myricetin for attenuating ECM degradation in human chondrocytes and ameliorating the murine osteoarthritis. Int. Immunopharmacol. 2019;75:105742. doi: 10.1016/j.intimp.2019.105742. [DOI] [PubMed] [Google Scholar]
- 193.Sriset Y., Sukkasem N., Chatuphonprasert W., Jarukamjorn K. Nephroprotective Effects of Hesperidin and Myricetin Against High-Fat Diet Plus Ethanol-Induced Renal Oxidative Damage in Mice. Rev. Bras. De Farm. 2022;32:555–562. doi: 10.1007/s43450-022-00275-5. [DOI] [Google Scholar]
- 194.Park S., Song G., Lim W. Myricetin inhibits endometriosis growth through cyclin E1 down-regulation in vitro and in vivo. J. Nutr. Biochem. 2020;78:108328. doi: 10.1016/j.jnutbio.2019.108328. [DOI] [PubMed] [Google Scholar]
- 195.Barlas N., Özer S., Karabulut G. The estrogenic effects of apigenin, phloretin and myricetin based on uterotrophic assay in immature Wistar albino rats. Toxicol. Lett. 2014;226:35–42. doi: 10.1016/j.toxlet.2014.01.030. [DOI] [PubMed] [Google Scholar]
- 196.Zheng N., Wang C., Li Y., Fu H., Hu T. Myricetin ameliorates polycystic ovary syndrome in mice by brown adipose tissue activation. Reproduction. 2024;167:e240034. doi: 10.1530/REP-24-0034. [DOI] [PubMed] [Google Scholar]
- 197.Golkar T., Bassenden A.V., Maiti K., Arya D.P., Schmeing T.M., Berghuis A.M. Structural basis for plazomicin antibiotic action and resistance. Commun. Biol. 2021;4:729. doi: 10.1038/s42003-021-02261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Li J., Sun M., Pan Y., Cui X., Li C. Enzymatic oxidation increases the antibacterial activity of myricetin against Staphylococcus aureus. Food Chem. 2025;463:141250. doi: 10.1016/j.foodchem.2024.141250. [DOI] [PubMed] [Google Scholar]
- 199.Griep M.A., Blood S., Larson M.A., Koepsell S.A., Hinrichs S.H. Myricetin inhibits Escherichia coli DnaB helicase but not primase. Bioorganic Med. Chem. 2007;15:7203–7208. doi: 10.1016/j.bmc.2007.07.057. [DOI] [PubMed] [Google Scholar]
- 200.Zhou J.-L., Chen H.-H., Xu J., Huang M.-Y., Wang J.-F., Shen H.-J., Shen S.-X., Gao C.-X., Qian C.-D. Myricetin acts as an inhibitor of type II NADH Dehydrogenase from Staphylococcus aureus. Molecules. 2024;29:2354. doi: 10.3390/molecules29102354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Kang S.S., Kim J.G., Lee T.H., Oh K.B. Flavonols inhibit sortases and sortase-mediated Staphylococcus aureus clumping to fibrinogen. Biol. Pharm. Bull. 2006;29:1751–1755. doi: 10.1248/bpb.29.1751. [DOI] [PubMed] [Google Scholar]
- 202.Jing S., Wang L., Wang T., Fan L., Chen L., Xiang H., Shi Y., Wang D. Myricetin protects mice against MRSA-related lethal pneumonia by targeting ClpP. Biochem. Pharmacol. 2021;192:114753. doi: 10.1016/j.bcp.2021.114753. [DOI] [PubMed] [Google Scholar]
- 203.Silva L.N., Da Hora G.C.A., Soares T.A., Bojer M.S., Ingmer H., Macedo A.J., Trentin D.S. Myricetin protects Galleria mellonella against Staphylococcus aureus infection and inhibits multiple virulence factors. Sci. Rep. 2017;7:2823. doi: 10.1038/s41598-017-02712-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Cetin-Karaca H., Newman M.C. Antimicrobial efficacy of plant phenolic compounds against Salmonella and Escherichia Coli. Food Biosci. 2015;11:8–16. doi: 10.1016/j.fbio.2015.03.002. [DOI] [Google Scholar]
- 205.Pan H., He J., Yang Z., Yao X., Zhang H., Li R., Xiao Y., Zhao C., Jiang H., Liu Y., et al. Myricetin possesses the potency against SARS-CoV-2 infection through blocking viral-entry facilitators and suppressing inflammation in rats and mice. Phytomedicine. 2023;116:154858. doi: 10.1016/j.phymed.2023.154858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Hu H., Hu Z., Zhang Y., Wan H., Yin Z., Li L., Liang X., Zhao X., Yin L., Ye G., et al. Myricetin inhibits pseudorabies virus infection through direct inactivation and activating host antiviral defense. Front. Microbiol. 2022;13:985108. doi: 10.3389/fmicb.2022.985108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Peng S., Fang C., He H., Song X., Zhao X., Zou Y., Li L., Jia R., Yin Z. Myricetin exerts its antiviral activity against infectious bronchitis virus by inhibiting the deubiquitinating activity of papain-like protease. Poult. Sci. 2022;101:101626. doi: 10.1016/j.psj.2021.101626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Fan J., Xi P., Liu H., Song X., Zhao X., Zhou X., Zou Y., Fu Y., Li L., Jia R., et al. Myricetin inhibits transmissible gastroenteritis virus replication by targeting papain-like protease deubiquitinating enzyme activity. Front. Microbiol. 2024;15:1433664. doi: 10.3389/fmicb.2024.1433664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Li W., Xu C., Hao C., Zhang Y., Wang Z., Wang S., Wang W. Inhibition of herpes simplex virus by myricetin through targeting viral gD protein and cellular EGFR/PI3K/Akt pathway. Antivir. Res. 2020;177:104714. doi: 10.1016/j.antiviral.2020.104714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Lee H.-S., Kim Y. Myricetin Disturbs the Cell Wall Integrity and Increases the Membrane Permeability of Candida albicans. J. Microbiol. Biotechnol. 2022;32:37–45. doi: 10.4014/jmb.2110.10014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Mo F., Ma J., Yang X., Zhang P., Li Q., Zhang J. In vitro and in vivo effects of the combination of myricetin and miconazole nitrate incorporated to thermosensitive hydrogels, on C. albicans biofilms. Phytomedicine. 2020;71:153223. doi: 10.1016/j.phymed.2020.153223. [DOI] [PubMed] [Google Scholar]
- 212.Jacobs Jr D.R., Gross M.D., Tapsell L.C. Food synergy: An operational concept for understanding nutrition. Am. J. Clin. Nutr. 2009;89:1543S–1548S. doi: 10.3945/ajcn.2009.26736B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Ganora L. Herbal Constituents: Foundations of Phytochemistry. 1st ed. Lisa Ganora; Louisville, KY, USA: 2009. [Google Scholar]
- 214.Zhang J., Aray B., Zhang Y., Bai Y., Yuan T., Ding S., Xue Y., Huang X., Li Z. Synergistic effect of cucurbitacin E and myricetin on Anti-Non-Small cell lung cancer: Molecular mechanism and therapeutic potential. Phytomedicine. 2023;111:154619. doi: 10.1016/j.phymed.2022.154619. [DOI] [PubMed] [Google Scholar]
- 215.Pinto H.B., Brust F.R., Macedo A.J., Trentin D.S. The antivirulence compound myricetin possesses remarkable synergistic effect with antibacterials upon multidrug resistant Staphylococcus aureus. Microb. Pathog. 2020;149:104571. doi: 10.1016/j.micpath.2020.104571. [DOI] [PubMed] [Google Scholar]
- 216.Hanci H., Igan H. Antimicrobial synergistic effects of apigenin,(-)-epigallocatechin-3-gallate, myricetin and luteolin in combination with some antibiotics. Ann. Agric. Environ. Med. 2023;30:61–64. doi: 10.26444/aaem/161220. [DOI] [PubMed] [Google Scholar]
- 217.Al-Abbasi F.A., Kazmi I. Therapeutic role of kaempferol and myricetin in streptozotocin-induced diabetes synergistically via modulation in pancreatic amylase, glycogen storage and insulin secretion. Mol. Cell. Biochem. 2023;478:1927–1937. doi: 10.1007/s11010-022-04629-4. [DOI] [PubMed] [Google Scholar]
- 218.Yi J.-L., Shi S., Shen Y.-L., Wang L., Chen H.-Y., Zhu J., Ding Y. Myricetin and methyl eugenol combination enhances the anticancer activity, cell cycle arrest and apoptosis induction of cis-platin against HeLa cervical cancer cell lines. Int. J. Clin. Exp. Pathol. 2015;8:1116–1127. [PMC free article] [PubMed] [Google Scholar]
- 219.Yao A., Shen Y., Zhang Z., Zou Z., Wang A., Chen S., Zhang H., Chen F., Zhao J., Chen Z., et al. Sulforaphane and myricetin act synergistically to induce apoptosis in 3T3-L1 adipocytes. Mol. Med. Rep. 2018;17:2945–2951. doi: 10.3892/mmr.2017.8235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Chen L., Fan T., Wang M., Zhu C.Y., Feng W.Y., Li Y., Yang H. Myricetin, a natural inhibitor of CD147, increases sensitivity of cis-platin in ovarian cancer. Expert Opin. Ther. Targets. 2024;28:83–95. doi: 10.1080/14728222.2024.2306345. [DOI] [PubMed] [Google Scholar]
- 221.Morales P., Haza A.I. Selective apoptotic effects of piceatannol and myricetin in human cancer cells. J. Appl. Toxicol. 2012;32:986–993. doi: 10.1002/jat.1725. [DOI] [PubMed] [Google Scholar]
- 222.Jeevanandam J., Chan Y.S., Danquah M.K. Nano-formulations of drugs: Recent developments, impact and challenges. Biochimie. 2016;128:99–112. doi: 10.1016/j.biochi.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 223.Patra J.K., Das G., Fraceto L.F., Campos E.V.R., del Pilar Rodriguez-Torres M., Acosta-Torres L.S., Diaz-Torres L.A., Grillo R., Swamy M.K., Sharma S., et al. Nano based drug delivery systems: Recent developments and future prospects. J. Nanobiotechnol. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Anwer S.T., Mobashir M., Fantoukh O.I., Khan B., Imtiyaz K., Naqvi I.H., Alam Rizvi M.M. Synthesis of Silver Nano Particles Using Myricetin and the In-Vitro Assessment of Anti-Colorectal Cancer Activity: In-Silico Integration. Int. J. Mol. Sci. 2022;23:11024. doi: 10.3390/ijms231911024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Li Z., Ma W., Ali I., Zhao H., Wang D., Qiu J. Green and facile synthesis and antioxidant and antibacterial evaluation of dietary myricetin-mediated silver nanoparticles. ACS Omega. 2020;5:32632–32640. doi: 10.1021/acsomega.0c05002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mohan U.P., Sriram B., Panneerselvam T., Devaraj S., MubarakAli D., Parasuraman P., Palanisamy P., Premanand A., Arunachalam S., Kunjiappan S. Utilization of plant-derived Myricetin molecule coupled with ultrasound for the synthesis of gold nanoparticles against breast cancer. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2020;393:1963–1976. doi: 10.1007/s00210-020-01874-6. [DOI] [PubMed] [Google Scholar]
- 227.Agraharam G., Girigoswami A., Girigoswami K. Nanoencapsulated myricetin to improve antioxidant activity and bioavailabil-ity: A study on zebrafish embryos. Chemistry. 2021;4:1–17. doi: 10.3390/chemistry4010001. [DOI] [Google Scholar]
- 228.Thant Y., Wang Q., Wei C., Liu J., Zhang K., Bao R., Zhu Q., Weng W., Yu Q., Zhu Y., et al. TPGS conjugated pro-liposomal nano-drug delivery system potentiate the antioxidant and hepatoprotective activity of Myricetin. J. Drug Deliv. Sci. Technol. 2021;66:102808. doi: 10.1016/j.jddst.2021.102808. [DOI] [Google Scholar]
- 229.Li C., Du M., Meng L., Adu-Frimpong M., Gong C., Zheng S., Shi W., Wang Q., Toreniyazov E., Ji H., et al. Preparation, characterisation, and pharmacodynamic study of myricetin pH-sensitive liposomes. J. Microencapsul. 2024;41:269–283. doi: 10.1080/02652048.2024.2337461. [DOI] [PubMed] [Google Scholar]
- 230.Zhou X., Yi L., Lang H., Zhang J., Zhang Q., Yu L., Zhu J., Mi M. Dihydromyricetin-encapsulated liposomes inhibit exhaustive exercise-induced liver inflammation by orchestrating M1/M2 macrophage polarization. Front. Pharmacol. 2022;13:887263. doi: 10.3389/fphar.2022.887263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Khatamian N., Motavalizadehkakhky A., Tabrizi M.H., Mehrzad J., Zhiani R. Preparation and characterization of the myricetin-loaded solid lipid nanoparticles decorated with folic acid-bound chitosan and evaluation of its antitumor and anti-angiogenic activities in vitro and in vivo in mice bearing tumor models. Cancer Nanotechnol. 2023;14:9. doi: 10.1186/s12645-023-00160-3. [DOI] [Google Scholar]
- 232.Lin T.-C., Yang C.-Y., Wu T.-H., Tseng C.-H., Yen F.-L. Myricetin Nanofibers Enhanced Water Solubility and Skin Penetration for Increasing Antioxidant and Photoprotective Activities. Pharmaceutics. 2023;15:906. doi: 10.3390/pharmaceutics15030906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Sharma P., Chaturvedi S., Khan M.A., Rai Y., Bhatt A.N., Najmi A.K., Akhtar M., Mishra A.K. Nanoemulsion potentiates the anti-cancer activity of Myricetin by effective inhibition of PI3K/AKT/mTOR pathway in triple-negative breast cancer cells. Med. Oncol. 2024;41:56. doi: 10.1007/s12032-023-02274-5. [DOI] [PubMed] [Google Scholar]
- 234.Upadhyay M., Hosur R.V., Jha A., Bharti K., Mali P.S., Jha A.K., Mishra B., Kumar A. Myricetin encapsulated chitosan nanoformulation for management of type 2 diabetes: Preparation, optimization, characterization and in vivo activity. Biomater. Adv. 2023;153:213542. doi: 10.1016/j.bioadv.2023.213542. [DOI] [PubMed] [Google Scholar]
- 235.Qi X., Wang J., Fei F., Gao X., Wu X., Shi D., Guo C. Myricetin-loaded nanomicelles protect against cisplatin-induced acute kidney injury by inhibiting the DNA damage-cGAS–STING signaling pathway. Mol. Pharm. 2022;20:136–146. doi: 10.1021/acs.molpharmaceut.2c00520. [DOI] [PubMed] [Google Scholar]
- 236.Gomaa N.H., El-Aziz N.K.A., El-Naenaeey E.-S.Y., Abdelaziz W.S., Sewid A.H. Antimicrobial potential of myricetin-coated zinc oxide nanocomposite against drug-resistant Clostridium perfringens. BMC Microbiol. 2023;23:79. doi: 10.1186/s12866-023-02800-5. [DOI] [PMC free article] [PubMed] [Google Scholar]