Abstract
Background:
Opioid use disorder (OUD) is a global concern with a reported shift in changing demographic and biopsychosocial profiles. Characterization of clusters based on diagnostic symptom criteria can help to understand the underlying associations between these criteria.
Aim:
The present study identifies clusters based on OUD diagnostic criteria, which may reveal clinically relevant subgroups of individuals with OUDs.
Materials and Methods:
The DSM5 diagnostic system OUD diagnosis was made for 204 male participants. An unsupervised clustering analysis focused on the individual 11 DSM5 diagnostic criteria.
Results:
Using the DSM5 diagnostic criteria, we obtained two clusters based on severity. Further, analyzing clinical information along with DSM5 criteria, two groups varying in OUD severity, presence of injecting drug use, and employment were identified.
Conclusion:
Based on cluster analysis, two main clusters of DSM5 criteria emerged. Rather than DSM5 symptoms clustering with each other based on the similarity of symptomatology, they aggregate numerically reflecting severity.
Keywords: Clinical relevance, cluster analysis, Diagnostic and Statistical Manual of Mental Disorders, opioid-related disorders, phenotype
Opioid use disorder (OUD) is a significant public health issue that affects people all over the world. According to the World Drug Report 2023 published by the United Nations Office on Drugs and Crime,[1] opioids continue to have a significant impact on health and society. Globally, it has been estimated that about 40.5 million individuals were dependent on opioids, and more than 100,000 individuals died of opioid overdose.[2] According to a recent nationwide survey conducted in India, it was determined that around 23 million individuals use opioids, with a subset of 2.8 million individuals exhibiting dependence on opioids.[3,4] OUDs affect individuals across the Global North and South divide and lead to considerable health harm, loss of productivity, and adverse consequences for the individual, family, and community.[2,3]
Substance use disorders themselves seem to be heterogeneous groups, with different clusters of individuals being subsumed under a diagnostic rubric of a particular substance use disorder. Such clusters have been studied for various substance use disorders.[5,6,7,8,9,10] Babor classified alcohol use disorder into two types, A and B, based on their drinking pattern and alcohol-related problems.[5] Type A is characterized by the late onset of alcohol complications and a better prognosis, while type B is characterized by the early onset of alcoholism and increased childhood and familial risk factors. An Indian study examining alcohol use disorder patients found two distinct subtypes of alcohol use disorder with or without antisocial personality and attention deficit hyperactivity disorder.[9] Thus, cluster analysis techniques help to draw out underlying patterns and groupings, which may have clinical and service/policy-related implications.
OUD has also exhibited a certain degree of heterogeneity in its severity, co-morbidities, and potential for recovery.[7] Clustering has been explored in OUDs in various ways, including clinical and medico-legal profiles,[11] emergency department visit attributes,[12] withdrawal symptoms,[13] clinical profiles inclusive of personality attributes,[14] and clinical profiles of pregnant women who have OUD.[15] Looking at clustering helps to bring out the salient aspects of the different subsets of the population with substance use disorders and may have relevance to identifying specific attributes of vulnerability and outcomes.
The DSM5 individual criteria used for making a substance use disorder diagnosis provide an opportunity to understand the inherent clustering of the typologies of different diagnoses. The eleven criteria used for making a substance use disorder diagnosis provide a diverse range of potential combinations.[16] It is possible that two patients sharing no common diagnostic feature are diagnosed with the same DSM5 label of OUD. Understanding underlying clusters of such diagnoses based upon the congregation of diagnostic criteria may help to discern substance use disorder typologies. This may help to understand further the characteristics of the heterogeneous sample of opioid users and derive additional incremental insights into substance use disorder typologies. Thus, this study aimed to discover latent, more homogeneous groupings within individuals with OUD by unsupervised clustering analysis, primarily using diagnostic criteria data and basic socio-demographic information. Additionally, the study sought to analyze and compare the distinctions between these identified clusters.
MATERIALS AND METHODS
Data source
The data were obtained from our previously conducted study, which included patients with substance use disorders.[17] The original study used purposive sampling and assessed participants using a structured questionnaire. Individuals with substance use disorder were approached from the outpatient setting and offered participation. Purposive sampling was chosen as random or systematic sampling was not feasible. Outpatients were included if they had a history of any substance use disorder as per the Diagnostic and Statistical Manual of Mental Disorders (DSM5) 5 criteria, were willing to give informed consent, and were at least 18 years of age. While the previous study aimed to assess the pattern of self-harm attempts among individuals with substance use disorders, the participants were graded on each item of DSM5 criteria for substance use disorders for making a diagnosis. This enabled us to look at the clustering of these DSM5 criteria, which was not the focus of the initial study. The availability of this dataset provided us with an opportunity to answer the meaningful clinical research question of whether certain types of criteria (e.g., tolerance and withdrawal, which reflected physiological dependence) gelled well with others (e.g., social and interpersonal issues and reduced socio-occupational activities which are psychosocial-context dependent). The present analysis focuses on OUDs and performs clustering based on the DSM5 criteria, followed by evaluating differences across clusters in terms of socio-demographic factors and selected clinical variables (duration of opioid use and instances of injecting drug use). The original study adhered to the Declaration of Helsinki and was approved by the Institutional Ethics Committee.[17]
Cluster analysis
The dataset comprised 11 binary categorical variables, hence, hierarchical cluster analysis (Python version 3) was employed to identify hidden patterns within the data. We systematically compared various linkage methods (single, complete, average, and Ward) and distance metrics (Jaccard, Dice, and Hamming) to identify the most appropriate approach for clustering binary categorical data. The quality and robustness of the clustering solutions were evaluated using the silhouette score, which measures the cohesion and separation of clusters, and the cophenetic correlation coefficient, which assesses how well the hierarchical clustering preserves the pairwise distances between the original data points. The Hamming distance metrics with the Ward method were chosen as they gave the most optimum silhouette scores and cophenetic correlation coefficients. Therefore, clustering approach using this approach was prioritized and considered for further analysis.
Statistical analysis
Statistical analysis was performed using the statistical packages available in Python version 3. For comparisons among different clusters, we performed a non-parametric Mann–Whitney U test, used for continuous variables displaying non-normal distribution, and the Chi-square test for categorical variables. To evaluate the relationships among input parameters, correlation and association coefficients were determined and a heatmap was generated to visualize these relationships. Additionally, the Phi coefficient (φ) was calculated to estimate the strength and significance of the associations among the categorical variables.
RESULTS
A total of 364 patients were approached for participation in the original study, among whom 300 consented to partake. Among them, OUD was present in 204 which was included in the present analysis. Table 1 provides the clinical characteristics of these patients. We used 11 criteria of DSM5. Figure 1 gives the frequency distribution of DSM5 criteria for OUD in the present study.
Table 1.
Clinical characteristics of patients with opioid use disorder (n=204)
| Characteristics | Mean±SD/frequency (%) |
|---|---|
| Age (years) | 31.48±11.36 |
| Education (No. of completed years) | |
| 0.5 | 52 (25.5) |
| 6.10 | 99 (48.5) |
| >10 | 53 (26.0) |
| Marital Status | |
| Not Married | 105 (51.5) |
| Married | 99 (48.5) |
| Occupation | |
| Not Employed | 49 (24.0) |
| Employed | 155 (76.0) |
| Residence | |
| Urban | 150 (73.5) |
| Rural | 54 (26.5) |
| Family Type | |
| Living alone | 8 (3.9) |
| Nuclear | 114 (55.9) |
| Extended/joint | 82 (40.2) |
| Per capita income in INR per month | 5819±7713 |
| DSM5 Severity for opioid use disorder | |
| Mild | 5 (2.5) |
| Moderate | 30 (14.7) |
| Severe | 169 (82.8) |
| Opioid use duration (years) | 9.1±7.9 |
| History of injection drug use | |
| No | 136 (66.7) |
| Yes | 68 (33.3) |
INR - Indian Rupees, SD - Standard Deviation
Figure 1.
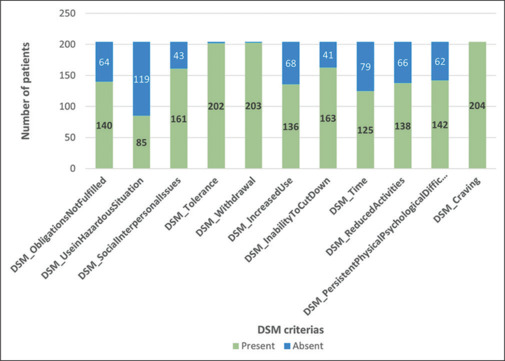
Frequency of DSM5 criteria for opioid use disorder. DSM_Tolerance-Tolerance as defined by either a need for markedly increased amounts to achieve intoxication or desired effect or markedly diminished effect with continued use of the same amount, DSM_Withdrawal-Withdrawal manifesting as either a characteristic syndrome or the substance is used to avoid withdrawal, DSM_IncreasedUse-Taken in larger amounts or longer period than intended, DSM_InabilityToCutDown-Persistent desire or unsuccessful efforts to cut down or control substance use, Time - A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects, DSM_Craving-Craving or a strong desire to use substances, DSM_ObligationsNotFulfilled-Substance use resulting in a failure to fulfill major role obligations at work, school, or home, DSM_SocialInterpersonalIssues-Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance, DSM_ReducedActivities Stopping or reducing important social, occupational, or recreational activities due to substance use, DSM_UseinHazardousSituation-Recurrent use of substances in physically hazardous situations, DSM_PersistentPhysicalPsychologicalDifficulties- The substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the use of the substance.
Based on multivariate analysis, we identified several key associations among different DSM5 criteria in the study population [Figure 2a]. The strongest positive correlation is between tolerance and withdrawal (φ =0.71; P < 0.05). The inability to cut down use and time spent on drugs also shows a high correlation (φ =0.68; P < 0.05), suggesting that individuals who have difficulty cutting down on opioid use tend to spend significant time on activities related to obtaining, using, or recovering from opioids. A significant correlation was found between use in hazardous situations and reduced socio-occupational activity (φ =0.64; P < 0.05), indicating that recurrent opioid use in hazardous situations is strongly linked to reducing important social, occupational, or recreational activities due to substance use. Additionally, moderate positive associations were identified between reduced socio-occupational activity and time spent on drugs (φ =0.63; P < 0.05), as well as social and interpersonal issues and persistent physical and psychological difficulties (φ =0.57; P < 0.05), showing connections between reduced activities and time spent on opioid-related activities, and indicating that interpersonal problems are related to ongoing physical or psychological challenges faced by individuals with OUD. Figure 2b reveals the intricate web of associations among the DSM5 criteria, emphasizing the strongest connections indicated by Phi coefficients (φ) values ranging from 0.705 to 0.523. The solid edges indicate statistically significant (P < 0.05) stronger associations, while dotted lines show moderate to weaker associations (craving was present in all; hence, it was not included in the network map).
Figure 2.
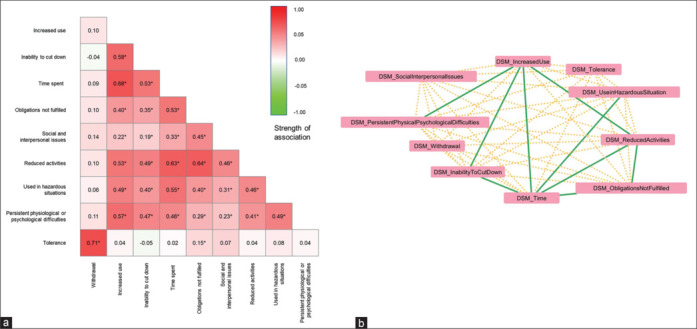
Relationship of DSM criteria. (a) Heatmap showing the correlation/association among DSM5 criteria [*Significant at 0.05 significance level (2-tailed)]. (b) Network map showing strongest associations among DSM5 criteria. DSM_Tolerance-Tolerance as defined by either a need for markedly increased amounts to achieve intoxication or desired effect or markedly diminished effect with continued use of the same amount, DSM_Withdrawal-Withdrawal manifesting as either a characteristic syndrome or the substance is used to avoid withdrawal, DSM_IncreasedUse-Taken in larger amounts or longer period than intended, DSM_InabilityToCutDown-Persistent desire or unsuccessful efforts to cut down or control substance use, DSM_Time- A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from its effects, DSM_Craving-Craving or a strong desire to use substances, DSM_ObligationsNotFulfilled-Substance use resulting in a failure to fulfill major role obligations at work, school, or home, DSM_SocialInterpersonalIssues-Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance, DSM_ReducedActivities Stopping or reducing important social, occupational, or recreational activities due to substance use, DSM_UseinHazardousSituation-Recurrent use of substances in physically hazardous situations, DSM_PersistentPhysicalPsychologicalDifficulties-The substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the use of the substance
The hierarchical clustering based on 11 DSM5 criteria, utilizing Hamming metrics and the Ward method, resulted in two distinct and robust clusters. The silhouette measure of cohesion and separation is 0.58, indicating well-defined clusters. Additionally, the cophenetic correlation coefficient is 0.79, suggesting a good representation of the original data structure. Cluster 1 (n = 118) is characterized by a significantly higher number of applicable diagnostic criteria (Cramer V = 0.380, P < 0.001), greater employment rates (φ =0.155, P = 0.041), and the largest proportion of patients without a history of injecting drug use (φ =0.161, P = 0.031). In contrast, Cluster 2 (n = 86) has fewer patients with a history of injecting drug use and met fewer DSM criteria, indicating a lower severity level compared to Cluster 1 in which all the patients exhibited higher severity of substance use disorder. Other clinical and socio-demographic parameters were comparable between the two clusters [Table 2].
Table 2.
Comparison between two clusters formed using 11 DSM5 criteria
| Variable | Cluster 1 (n=118) | Cluster 2 (n=86) | P |
|---|---|---|---|
| Age (years) | 30.6 | 32.6 | 0.350* |
| Per capita income (INR per month) | 6377.8 | 5052.7 | 0.206* |
| Marital Status | 0.285# | ||
| Not Married | 55.1% | 46.5% | |
| Married | 44.9% | 53.5% | |
| Occupation | 0.041# | ||
| Not Employed | 29.7% | 16.3% | |
| Employed | 70.3% | 83.7% | |
| Education (No. of completed years) | 0.179# | ||
| 0.5 | 21.2% | 31.4% | |
| 6.10 | 53.4% | 41.9% | |
| >10 | 25.4% | 26.7% | |
| Residence | 0.065# | ||
| Urban | 78.8% | 66.3% | |
| Rural | 21.2% | 33.7% | |
| Family Type | 0.395# | ||
| Living alone | 5.1% | 2.3% | |
| Nuclear | 52.5% | 60.5% | |
| Extended/joint | 42.4% | 37.2% | |
| Injecting Drug Use | 0.031# | ||
| No | 60.2% | 75.6% | |
| Yes | 39.8% | 24.4% | |
| Duration of opioid use in years | 9.25 | 9.10 | 0.246* |
| DSM Severity | 0.001# | ||
| Mild | 0.0% | 6.0% | |
| Moderate | 0.0% | 35.7% | |
| Severe | 100.0% | 58.3% |
INR - Indian Rupees, Statistical tests: #Chi-square test, *Mann–Whitney U. Significant associations have been highlighted
DISCUSSION
The present study looked for any hidden clusters of DSM5 diagnostic criteria of OUD, which might differ in profile to help develop more targeted care. We obtained two significant clusters of individuals while using only the DSM5 criteria for unsupervised cluster analysis. One of them has a greater number of diagnostic criteria applicable, injecting drug use, and greater chances of being unemployed. This group had a higher severity of substance use disorder. The age did not differ significantly across these two clusters based only on the DSM5 criteria. This implies that clinically we may have differential patient subgroups, and the diagnostic criteria-based clustering primarily yields severe and less severe categories. This extends onto the generic sub-divisions of DSM5 criteria of mild, moderate, and severe substance use disorder to the context of opiates. The three-group classification is generically a good proposition, especially when considering substance use disorders like nicotine use disorder and cannabis use disorder may find diagnostic space in mild categories.[18,19] However, where OUD, primarily two groups emerge on severity, more severe and less severe. This may be due to the quick development of tolerance and withdrawal with OUD, quicker transition from initiation of use to disordered use, and range of impairments that may develop.[20]
The two severity-based clusters differed from each other based on injecting drug use and employment. Other studies have also found injecting drug use to be an independent marker of substance use disorder severity.[21] Injecting drug use can produce a greater “rush” and hence repeated substance intake, and hence a more entrenched use and difficulty in quitting. The consequences of injecting drug use like overdose and contracting secondary infections may also impair functioning and lead to stigma. Thus, injecting drug use may be a direct or indirect determinant of the severity in the clinical population with OUD. The proportion of unemployed people was higher in the cluster of higher severity. This finding suggests that probably greater severity produced more impairment and did not enable individuals to work regularly. Alternately, the individual with severe OUD may not have been able to secure work due to prior history or stigma associated with their condition. We are unable to clarify the directionality of this association due to the limits of the dataset.
We found that tolerance and withdrawal showed the highest correlation among the different parameters. Tolerance and withdrawal signify physiological dependence, and these features are also present in chronic opioid users who are not necessarily substance dependent.[22] The reason for these features developing is the pharmacodynamic adaptation of the body to the increasing doses of opioids, and hence the occurrence of withdrawal symptoms on opioid cessation. A range of methods are being used to understand the genesis of tolerance and subsequent withdrawal from the cellular to organismic level.[23] We also found that craving was a ubiquitous symptom in the sample, signifying the intense desire to consume opioids was probably a defining feature of OUD.
The implication of the two-cluster solution in the clinical setting primarily entails differentiating patients based on severity. Those individuals who have more severe OUD are more likely to inject drugs and are more likely to be unemployed. In absolute terms, in both the clusters, non-injecting drug users and employed individuals predominate. However, on a relative basis, these two features are more common in the more severe OUD cluster. Thus, severe OUD patients may require additional harm reduction measures like needle–syringe exchange programs (NSEP) and greater awareness of the transmission of blood-borne viruses. Similarly, this more severe group may require greater employment support or engagement in alternate vocations. Nonetheless, the less severe group may also be recipients of such focus. We also explored other cluster solutions (three cluster solution and four cluster solution), but clinically meaningful differentiations did not emerge on the other cluster solution. With the present analysis, the two clusters may have some implications in the treatment focus, for example, in patients with injecting drug use, we may need to focus on employment as well. With the constraints of clinical sample, and heterogeneity of DSM criteria fulfilled, the analysis is helpful in conceptualization of segregation of patients on some of the features easily discernible in the clinical setting.
While this research is an important step toward identifying clinically distinct subgroups of OUD based upon primarily DSM5 diagnostic criteria, future studies should validate these clusters and assess treatment outcomes associated with these clusters. Doing so would enable researchers and clinicians to identify patients based on vulnerabilities and individualize the treatment decision and delivery accordingly. From the treatment perspective, it may help us select more tailored approaches for participants from a particular cluster (as above, higher severity cases). It might also enable other stakeholders involved in treatment provision to plan or allocate resources more appropriately, especially in resource-limited settings and situations. For example, the individuals with injecting drug use, being representative of the severe cluster, would benefit from more comprehensive and wraparound services, referral for testing for blood-borne viruses, and ensuring continuity of care.
Limitations
Our study has a few limitations, first, as we only included male opioid-dependent participants, it may not be a representative sample of the opioid users. Generally, women are under-represented among substance users in the geographic context,[24] probably both due to lower actual prevalence of substance use disorders and entry barriers for treatment. Second, no treatment-related data was included, and the study was cross-sectional. Information on the outcomes might have been helpful in understanding the salient characteristics of the clusters over a time horizon. Third, ascertainment biases and inaccuracies applicable to routine clinical psychiatric diagnostic assessment cannot be entirely ruled out. Furthermore, the sample represents a non-random treatment-seeking population in a medically oriented setup and may not be generalizable to other settings.
CONCLUSION
To conclude, we identified distinct profiles of OUD based on different approaches. Based on the DSM5 diagnostic criteria of OUDs, we found only two clusters, primarily based on severity. These clustering approaches are illuminative of differential and heterogeneous population subgroups of individuals with OUDs, with potentially different treatment “needs.” The present analysis furthers the data on the clusters of individuals with OUDs based on diagnostic criteria, which may be helpful for nosological characterization and refinement.
Data availability statement
The data would be available from the corresponding author on reasonable request.
Author contributions
Conceptualization, Methodology, Software, Formal analysis, Writing -review and editing. SB, DG, YPB, SS Writing original draft. VP Investigation, Writing -review and editing. RG.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Department of Biotechnology (DBT) [grant numbers BT/PR40151/BTIS/137/5/2021].
REFERENCES
- 1.UNODC . United Nations Office of Drugs and Crime; Geneva: 2023. World Drug Report. [Google Scholar]
- 2.Degenhardt L, Grebely J, Stone J, Hickman M, Vickerman P, Marshall BDL, et al. Global patterns of opioid use and dependence: Harms to populations, interventions, and future action. Lancet. 2019;394:1560–79. doi: 10.1016/S0140-6736(19)32229-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ambekar A, Agrawal A, Rao R, Mishra AK, Khandelwal S, Chadda R Kumar. Magnitude of Substance Use in India. 2019. Available from: https://www.muktangan.org/pdf/Magnitude_Substance_Use_India_REPORT.pdf. [Last accessed on 2023 Aug 21]
- 4.Strang J, Volkow ND, Degenhardt L, Hickman M, Johnson K, Koob GF, et al. Opioid use disorder. Nat Rev Dis Primer. 2020;6:1–28. doi: 10.1038/s41572-019-0137-5. [DOI] [PubMed] [Google Scholar]
- 5.Babor TF. The classification of alcoholics. Alcohol Health Res World. 1996;20:6–14. [PMC free article] [PubMed] [Google Scholar]
- 6.Bogenschutz MP, Scott Tonigan J, Pettinati HM. Effects of alcoholism typology on response to naltrexone in the COMBINE study. Alcohol Clin Exp Res. 2009;33:10–8. doi: 10.1111/j.1530-0277.2008.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carroll KM. The profound heterogeneity of substance use disorders: Implications for treatment development. Curr Dir Psychol Sci. 2021;30:358–64. doi: 10.1177/09637214211026984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Vaddiparti K, Cheong J, Cottler LB. Identification of typologies of cocaine use based on quantity, frequency, and duration of use: A latent profile analysis. J Addict Med. 2021;15:211–8. doi: 10.1097/ADM.0000000000000749. [DOI] [PubMed] [Google Scholar]
- 9.Malhotra S, Basu D, Ghosh A, Khullar M, Kakkar N. Subtyping of alcohol dependence in Indian males: A cluster analytic approach. Indian J Psychiatry. 2016;58:372. doi: 10.4103/0019-5545.196707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schlaff G, Walter H, Lesch OM. The Lesch alcoholism typology – psychiatric and psychosocial treatment approaches. Ann Gastroenterol Q Publ Hell Soc Gastroenterol. 2011;24:89–97. [PMC free article] [PubMed] [Google Scholar]
- 11.Flórez G, López-Durán A, Triñanes Y, Osorio J, Fraga J, Fernández JM, et al. First-time admissions for opioid treatment: Cross-sectional and descriptive study of new opioid users seeking treatment. Neuropsychiatr Dis Treat. 2015;11:2431–40. doi: 10.2147/NDT.S84431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor RA, Gilson A, Schulz W, Lopez K, Young P, Pandya S, et al. Computational phenotypes for patients with opioid-related disorders presenting to the emergency department. PLoS One. 2023;18:e0291572. doi: 10.1371/journal.pone.0291572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunn KE, Weerts EM, Huhn AS, Schroeder JR, Tompkins DA, Bigelow GE, et al. Preliminary evidence of different and clinically meaningful opioid withdrawal phenotypes. Addict Biol. 2020;25:e12680. doi: 10.1111/adb.12680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De B, Mattoo SK, Basu D. Age at onset typology in opioid-dependent men: An exploratory study from India. Am J Addict. 2003;12:336–45. [PubMed] [Google Scholar]
- 15.Charron E, Yu Z, Lundahl B, Silipigni J, Okifuji A, Gordon AJ, et al. Cluster analysis to identify patient profiles and substance use patterns among pregnant persons with opioid use disorder. Addict Behav Rep. 2023;17:100484. doi: 10.1016/j.abrep.2023.100484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lane SP, Sher KJ. Limits of current approaches to diagnosis severity based on criterion counts: An example with DSM-5 alcohol use disorder. Clin Psychol Sci. 2015;3:819–35. doi: 10.1177/2167702614553026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta R, Narnoli S, Das N, Sarkar S, Balhara YPS. Patterns and predictors of self-harm in patients with substance-use disorder. Indian J Psychiatry. 2019;61:431–8. doi: 10.4103/psychiatry.IndianJPsychiatry_578_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nielsen S, Bruno R, Lintzeris N, Fischer J, Carruthers S, Stoové M. Pharmaceutical opioid analgesic and heroin dependence: How do treatment-seeking clients differ in Australia? Drug Alcohol Rev. 2011;30:291–9. doi: 10.1111/j.1465-3362.2011.00302.x. [DOI] [PubMed] [Google Scholar]
- 19.Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012–2013: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions–III. Am J Psychiatry. 2016;173:588–99. doi: 10.1176/appi.ajp.2015.15070907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chou SP, Goldstein RB, Smith SM, Huang B, Ruan WJ, Zhang H, et al. The epidemiology of DSM-5 nicotine use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Clin Psychiatry. 2016;77:6529. doi: 10.4088/JCP.15m10114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marel C, Sunderland M, Mills KL, Slade T, Teesson M, Chapman C. Conditional probabilities of substance use disorders and associated risk factors: Progression from first use to use disorder on alcohol, cannabis, stimulants, sedatives and opioids. Drug Alcohol Depend. 2019;194:136–42. doi: 10.1016/j.drugalcdep.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 22.Tun S, Vicknasingam B, Singh D. Factors affecting addiction severity index (ASI) among clients enrolled in methadone maintenance treatment (MMT) program in Myanmar. Harm Reduct J. 2021;18:1–2. doi: 10.1186/s12954-021-00523-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morgan MM, Christie MJ. Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human. Br J Pharmacol. 2011;164:1322–34. doi: 10.1111/j.1476-5381.2011.01335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nebhinani N, Sarkar S, Gupta S, Mattoo SK, Basu D. Demographic and clinical profile of substance abusing women seeking treatment at a de-addiction center in north India. Ind Psychiatry J. 2013;22:12–6. doi: 10.4103/0972-6748.123587. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data would be available from the corresponding author on reasonable request.


