Significance
The US overweight/obesity epidemic and the resulting chronic disease burden are an unfolding, diet-driven existential disaster. This has been obvious for decades, but the epidemic keeps getting worse. As managing and reversing this crisis demands more fruit and vegetable intake, it also demands more fruit and vegetable production, particularly the most healthful kinds. This makes horticulture research and production just as crucial as nutritional and medical research and practice. From now on, horticulture, nutrition, and medicine must therefore work together to transform the food system, dietary patterns, and health. Changes in institutional culture and federal funding priorities will be needed.
Keywords: horticulture, fruits and vegetables, obesity, type 2 diabetes, food is medicine
Abstract
It is clear that the escalating epidemic of insulin resistance and type 2 diabetes has reached a crisis level in the United States, that overweight and obesity are drivers, and that diets and the food system have major roles. It is also clear that nutrition and medical research point to increased healthful fruit and vegetable intake as a key part of any strategy to manage the crisis. But although increasing healthful intake entails both expanding production of fruits and vegetables and improving their healthful characteristics, horticulture has generally been sidelined or taken for granted when strategies are envisioned. This article makes the case that horticulture research and practice can and should be equal partners with nutrition and medicine in the pressing search for effective crisis-management strategies. To do so, it first “runs the numbers” for the scale of the crisis, for trends in fruit and vegetable intake and production, for the scant federal support for horticultural crop production and research, and for horticulture research’s high return on investment. The article then sketches a roadmap to integrate horticulture research and community outreach with nutrition and healthcare, stressing new opportunities. The goal is a US food system that i) makes healthful fruits and vegetables accessible, affordable, and appealing for all and ii) complements a healthcare system spanning patient-based to population-based nutrition.
US diets and the food system are major drivers of the ongoing epidemic of overweight and obesity, insulin resistance, diabetes, and associated diseases, and the changes needed to deal with this crisis are decades overdue (1, 2). The modest changes advised by nine successive editions of the Dietary Guidelines for Americans (DGA) have not reversed or even slowed the epidemic. The numbers are now dire: 73% of adults and 35% of children and adolescents have overweight or obesity, 15% of adults have diabetes, and 37% of adults and 18% of adolescents have prediabetes (3, 4) (Fig. 1A). This crisis situation calls for new ways of doing things because the old ones clearly are not working. But changes of the scale needed only happen when there is enough political will and public will (5).
Fig. 1.
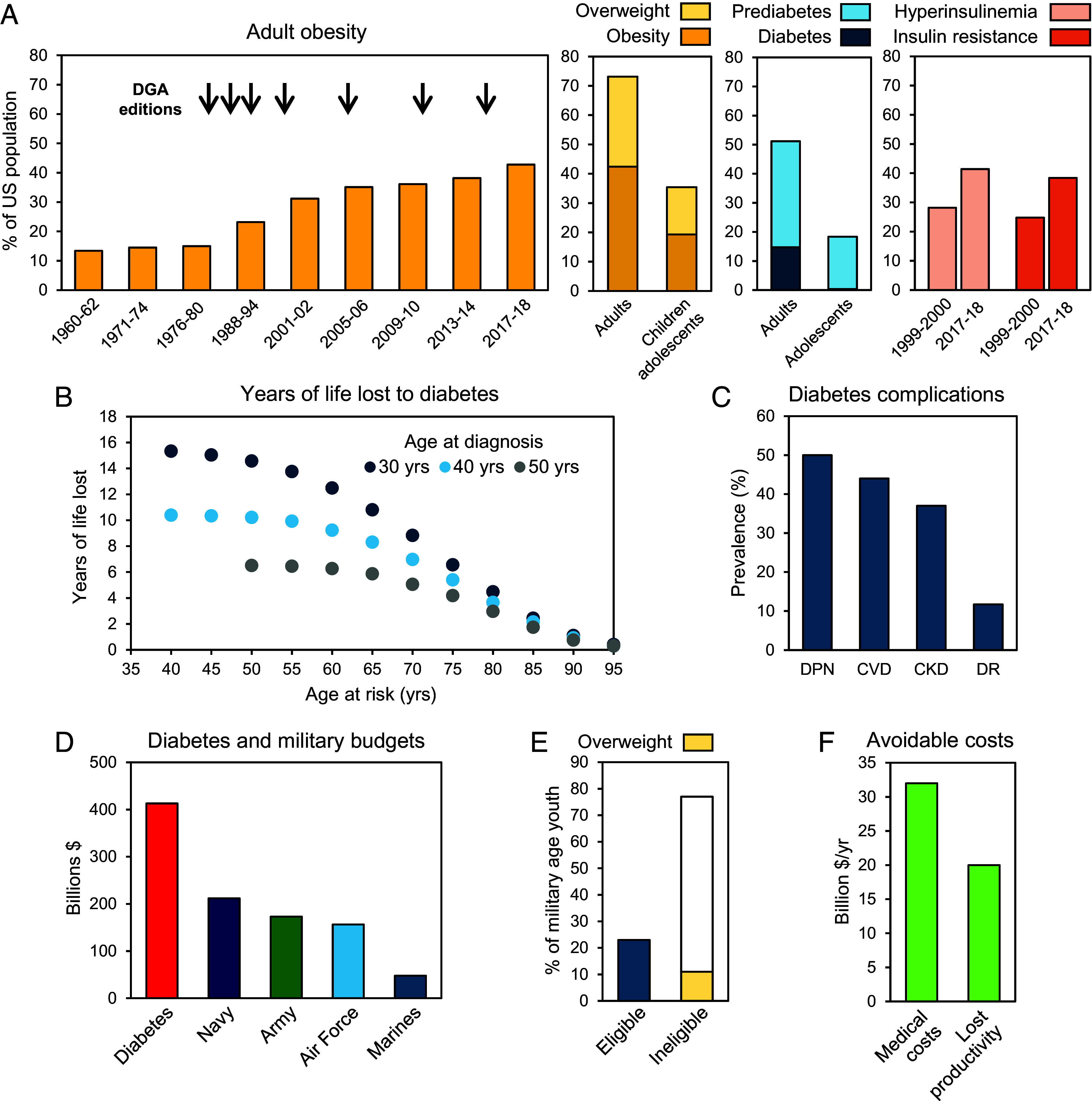
The US obesity/overweight/diabetes epidemic by the numbers. (A) 60 y trend in adult obesity (arrows mark the release dates of editions of the DGA; percent of adults and young people with overweight or obesity (2017 to 18); percent of adults (2017 to 20) and adolescents (2005 to 16) with diabetes and prediabetes. (B) Estimated years of life lost according to age at diagnosis of type 2 diabetes relative to people without diabetes. (C) Prevalence of diabetes complications among people diagnosed with diabetes: peripheral neuropathy (DPN), cardiovascular disease (CVD), chronic kidney disease (CKD), and retinopathy (DR). Data are for various years 2007 to 2018. (D) Total economic costs of diabetes (direct medical costs and attributable indirect costs) relative to military spending in 2022. (E) Percent of youth eligible/ineligible for military service in 2020. (F) Estimated economic impacts of not meeting the US recommended daily fruit and vegetable intake on cardiovascular deaths alone (2018). Data sources are in Dataset S1.
Both wills seem at last to have strengthened sufficiently in the United States to spur meaningful change (6). This article takes this to be the case and explores opportunities to do things differently, especially from the standpoint of horticulture. This is not a parochial standpoint. Increasing fruit and vegetable intake has been emphasized over and over again as a key part of dietary strategies to manage the crisis (1, 2, 7, 8). Yet horticulture research and production have historically taken a backseat to nutrition and medical research and practice when strategies to manage the crisis are envisioned (9–12), and federal funding has long mirrored this (2, 13). Horticultural products have also taken a backseat to other agricultural products in funding support (1). One effect of the overshadowing of horticulture has been a lack of systematic, sustained cooperation with the nutrition and health sciences, and this is aggravated by career and funding structures for academic researchers that incentivize individual programs, i.e., fragmentation (14). To quote the late Charlie Munger: “Show me the incentive and I'll show you the outcome.”
In plotting a course forward, step one is to grasp clearly where we are now, which means getting a feel for the numbers. Accordingly, taking inspiration from Ron Milo’s “by the numbers” approach (e.g., ref. 15), we start by laying out the stark US numbers on i) the health and economic impacts of the epidemic, ii) fruit and vegetable intake and production, and iii) federal support for horticulture research and for growers. We do this in three figures (Figs. 1–3) with short matching text sections. While some of the numbers are widely known to horticulture, nutrition, or medical professionals, they tend to be siloed in each discipline; they must all be put side-by-side to see how interdependent they are. We close with a scheme (Fig. 4) and text that envision next-gen collaborations between horticulture, nutrition, and medicine that—through research and practice—deliver solutions to manage the health crisis. Overall, this article aims to be a straightforward one-stop resource for decision-makers and concerned citizens.
Fig. 2.
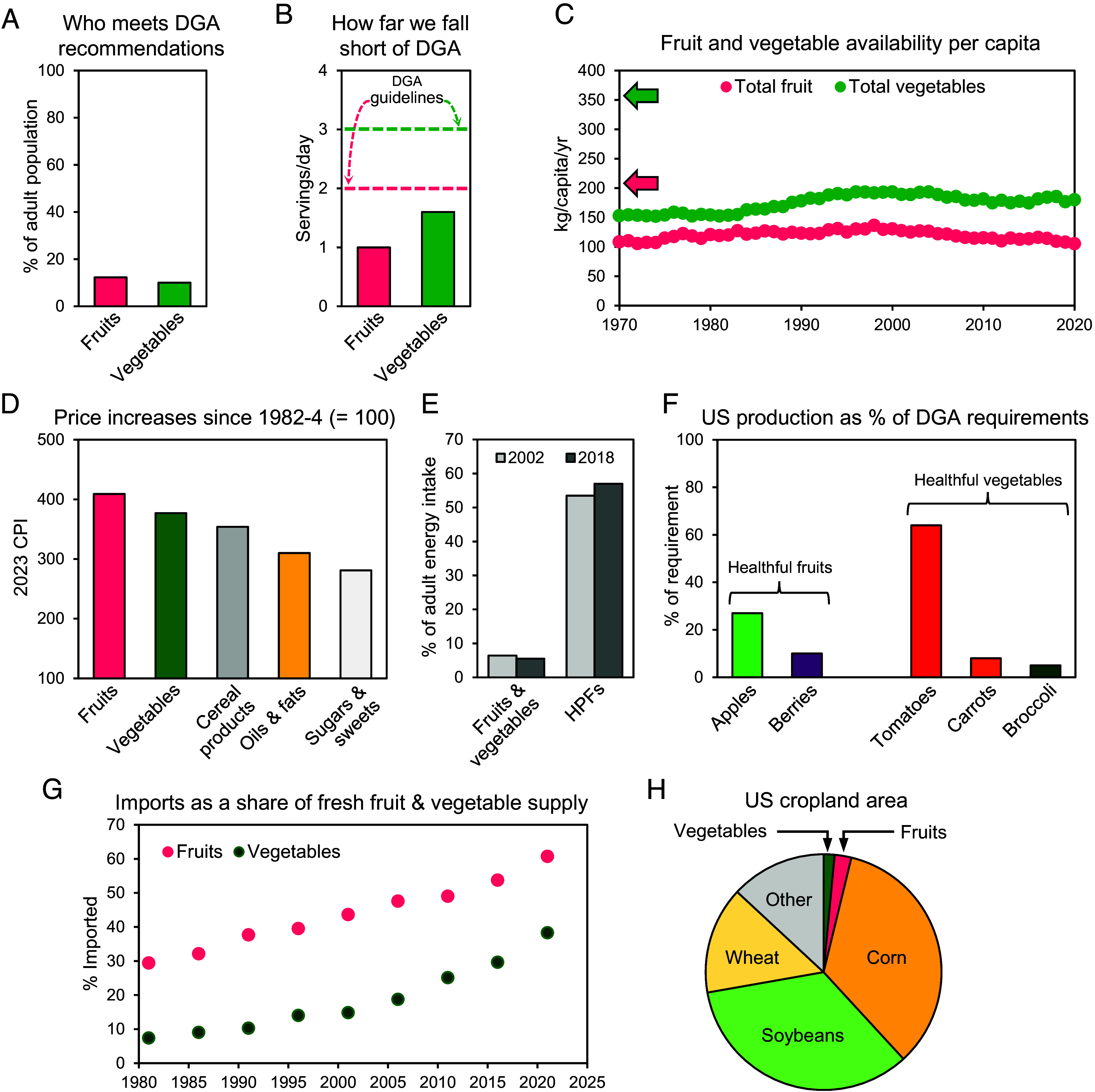
US fruit and vegetable intake and production by the numbers. (A) Percent of adults in 2019 getting the DGA recommended daily intake of fruits (2 servings) and vegetables (3 servings). (B) Median frequencies in 2019 of fruit and vegetable intake among adults. (C) 50 y trends in per capita fruit and vegetable availability. Arrows next to the vertical axis show roughly what fruit (pink) and vegetable (green) supplies would need to be to meet recommended intakes for the whole US population. (D) Increases over 40 y in real costs of fruits and vegetables vs. commodity crop-based foods as reflected by the Consumer Price Index (CPI, 1982-4 = 100). (E) Consumption of fruits and vegetables vs. ultraprocessed foods (UPFs) by US adults in 2002 and 2018, expressed as percentages of total energy (kcal) intake. (F) Approximate estimates of shortfalls in US domestic production of representative healthful fruits and vegetables relative to amounts needed to give the population 1 serving per day. (G) 40 y trends in imports as a share of the US supply of fresh fruits and vegetables. (H) Area of US cropland planted to fruits and vegetables in 2017 relative to major commodity crops. Data sources are in Dataset S2.
Fig. 3.
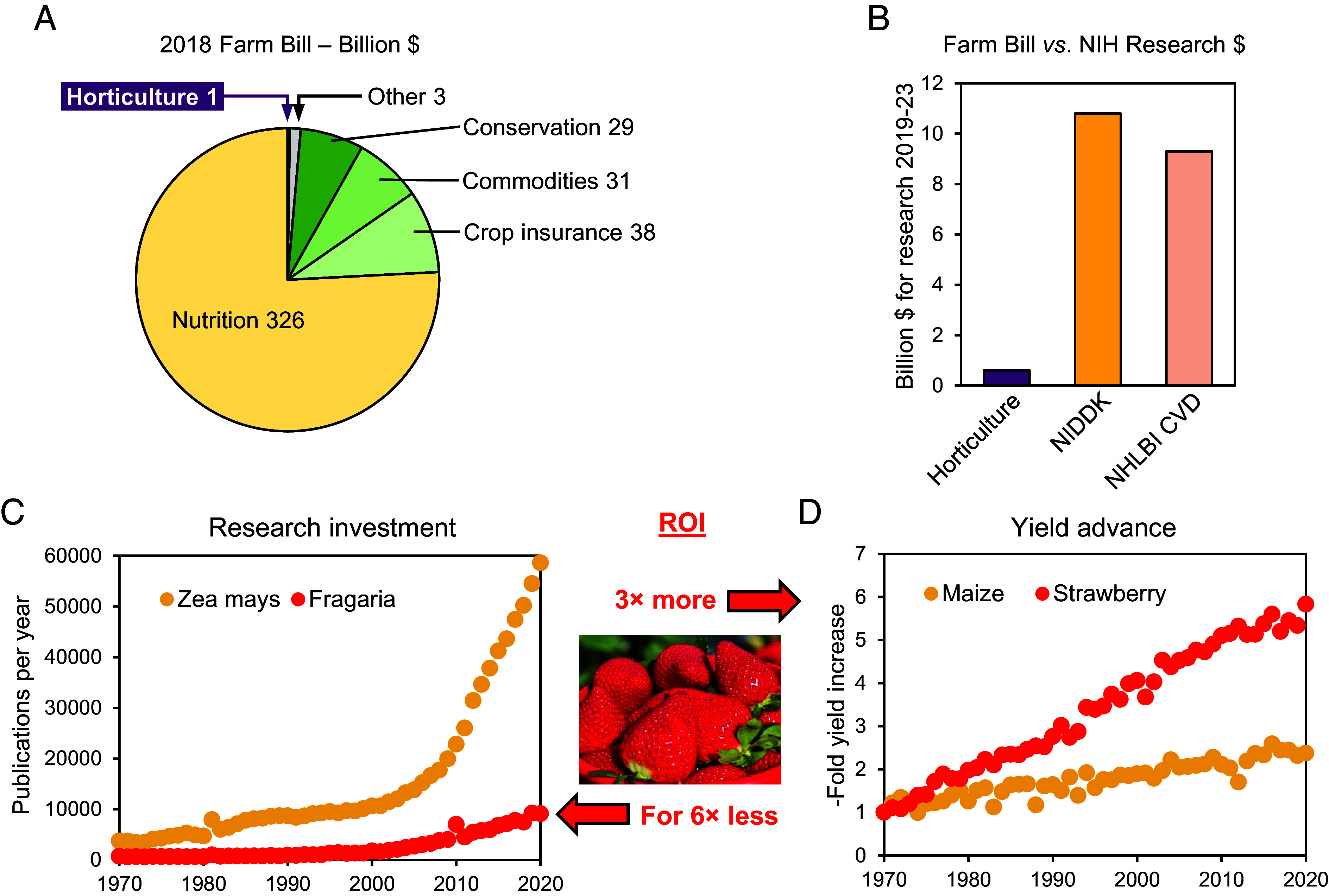
US federal support for fruit and vegetable research and production by the numbers. (A) Breakdown of the 2018 Farm Bill showing the small fraction for support of horticultural crop research and production relative to nutrition programs and commodity crops. (B) Approximate estimates of research funding for horticulture from the 5 y 2018 Farm Bill vs. NIH research funding for the same 5 y from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and for cardiovascular disease (CVD) from the National Heart, Lung, and Blood Institute (NHLBI); CVD research was estimated as 50% of the NHLBI total. (C) 50 y trends in publications per year (a proxy for research investment quantification) for Zea mays (maize) and Fragaria (cultivated strawberries and close relatives). (D) 50 y trends in US average yield per acre for maize and strawberries relative to yields in 1970 (= 1). A rough estimate of the 18-fold greater ROI on research on strawberry vs. maize (3× more yield advance for 6× less research) is between C and D. Data sources are in Dataset S3.
Fig. 4.
Roadmap for integrating horticulture research and practice with healthcare and nutrition with respect to research needs and opportunities and practical needs and opportunities.
The Obesity/Overweight/Diabetes Epidemic by the Numbers
Here, we use key numbers to drive home the magnitude of the epidemic. First, a few clarifications. The diabetes we refer to is Type 2 diabetes (T2D), which is caused by insulin resistance in muscle, liver, and fat tissue. T2D is characterized by chronically high blood glucose levels and is strongly associated with obesity and aging. Prediabetes occurs when blood glucose levels are slightly above the normal range and carries a high risk of progression to full-blown T2D. Hyperinsulinemia is an abnormally high level of insulin in the blood and can be both a cause and a consequence of insulin resistance (16). Obesity in adults is defined by a Body Mass Index (BMI) ≥30; overweight is a BMI >25 and <30. In this and other sections, sources of the numbers in the text and figures are in Datasets S1–S3.
Since the 1980s, adult obesity has steadily increased, reaching 43% of the population by 2018, with an additional 30% classified as overweight; even more alarming, youth obesity and overweight have risen to 35% (Fig. 1A). Given that obesity is a major risk factor for T2D (17) it is unsurprising that T2D and prediabetes have tracked the rising obesity. Today, these conditions affect around one in two adults and one in five adolescents (Fig. 1A). Because insulin resistance is a driver of T2D (18), it is no surprise either that insulin resistance and hyperinsulinemia also rose between 2000 and 2018 (Fig. 1A). The arrows in the adult obesity chart in Fig. 1A mark successive editions of the DGA, which have come out every 5 y since 1980. Matching the arrows with the timing of the obesity rise might suggest that DGAs have actually driven the rise! While this seems absurd, it is not entirely wrong (1, 19), e.g., the DGA’s 1992 Food Guide Pyramid recommended 6–11 servings of grains per day. This was moderated in 2011 by MyPlate, the Pyramid’s successor, which emphasized consumption of whole grain foods (20).
A T2D diagnosis is not just about diabetes itself; it forecasts a substantially shortened life. For instance, at age 50 (a typical age for T2D onset), having T2D is associated with a life expectancy loss of 6 y (21). And the younger the age of onset, the greater the loss; it increases to 10 y of life lost for onset at age 40 and to 15 y for onset at age 30 (Fig. 2B). But this is only half the story. For T2D, the years of life lost (YLL) are at least equaled by years lived with disability (YLD) (22). Hence, someone diagnosed at 30 is likely to die 15 y early and to be disabled in some way for their last 15-plus years of life. This is all the more concerning because—consistent with the rise in obesity among the young—early-onset T2D (i.e., diagnosed below age 40) is becoming increasingly common (23).
T2D shortens life and worsens health through its complications. These include peripheral neuropathy (which can lead to toe, foot, or leg amputation), cardiovascular disease (heart attack and stroke), chronic kidney disease, and retinopathy (vision loss). Many adults with diabetes experience one or more of these complications: 50% are afflicted by peripheral neuropathy, 44% by cardiovascular disease, 37% by chronic kidney disease, and 12% by retinopathy (Fig. 1C). T2D is the leading cause of kidney failure (which can require dialysis or a kidney transplant) and a leading cause of blindness.
The burden of individual suffering from obesity and its health consequences is thus huge and growing. The broader societal consequences are likewise huge and growing, as the following snapshots show. First, the medical costs and indirect costs of diabetes in the United States totaled $413 billion in 2022 (24), which is more than the 2022 US Army and Navy budgets combined (Fig. 1D). Second, staying with the military, a new high of 77% of youth were disqualified for service in 2020, with having overweight the largest single reason (Fig. 1E). Third, total cost accounting puts the costs of not meeting the recommended fruit and vegetable intake at $52 billion in 2018 for cardiovascular deaths alone (Fig. 1F), and the cost to human life attributable to today’s unhealthy food system is reckoned to exceed the cost of the food itself (25). These snapshots capture how urgently we need effective interventions to manage and prevent obesity and T2D to protect healthcare systems, national security, and lives. Increasing fruit and vegetable intake is an effective intervention—but it is not straightforward, as covered next.
Fruit and Vegetable Intake and Production by the Numbers
Fruits and vegetables are essential for health, not luxuries. However, current US intakes fall far short of the recommended two daily servings of fruit plus three of vegetables (“5-a-day”) (26). Only about one in ten adults meets these recommendations (Fig. 2A), and median fruit and vegetable intakes for adults are just half the recommended amounts (Fig. 2B). These dismal numbers in reality understate the nutritional shortfall as they include items that are not healthy choices for everyone (27, 28). Given the law of supply and demand, low consumption of fruits and vegetables should be matched by low production—which indeed it is (Fig. 2C). Overall, the supply of fruits and vegetables is no more than about half what would be needed to give everyone their 5-a-day (Fig. 2C). Fruit and vegetable production therefore has to be at least doubled domestically to meet this demand. There is nothing new about this; the same was true 20 y ago (9, 29), yet availability on a per capita basis has fallen, not risen since then (Fig. 2C). And fruit and vegetable supplies are not alone in having gone in the wrong direction for decades; prices have too. Since the 1980s, fresh fruit and vegetable prices have risen more than for any other foods, especially less-healthy foods based on commodity crops (Fig. 2D), and more than half of fruits and vegetables now cost over $1 per serving (30). Inflation has thus helped turn fruits and vegetables into exactly what they should not be: a luxury that only wealthier families can afford. Given these factors, it is no wonder that the consumption of cheap ultraprocessed foods that are made from commodity crops—and are strongly linked to obesity—has risen as fruit and vegetable consumption has fallen (Fig. 2E), and that ultraprocessed food consumption is highest among some of the most socioeconomically disadvantaged demographic groups (31).
There is more bad news. First, while overall production of fruits and vegetables needs doubling, US domestic production of some notably healthful and readily consumed ones, e.g., berries, carrots, and broccoli, would need to increase 10- to 20-fold (Fig. 2F). Thus, the shortfalls are greatest for the types of produce that could most benefit health. Another bad news item is the word “domestic” in the term “domestic production” above. In 40 y, domestic fruit and vegetable production has fallen to the point that imports now make up about 40% of the vegetable supply and 60% of the fruit supply (Fig. 2G). The main reasons for the domestic decline are the availability and cost of labor (32). Labor typically comprises one-third to one-half of the cost of growing and marketing fresh produce (33).
The above numbers explain our earlier statement that increasing US fruit and vegetable production is “not straightforward.” This does not mean it cannot be done, but rather that deep, system-wide changes are needed. We suggest such changes in this article’s last section. For now, note that there is plenty of room to maneuver: the United States has ample land to grow more fruits and vegetables. These crops currently take only about 3% of cropland; corn and soybeans (commodity crops) take 68% (Fig. 2H).
Federal Support for Fruit and Vegetable Research and Production by the Numbers
As with the cropland areas, so with federal support for research and production. A breakdown of the most recent (2018) Farm Bill—the main source of support for horticultural crop research and production—shows just $1 billion (0.2% of the $428 billion total) went to horticulture (Fig. 3A). In contrast, $69 billion went to commodity crops, much of it as crop insurance, revenue support, and disaster assistance (Fig. 3A). The relative lack of federal support for horticulture research is even more starkly clear when the Farm Bill’s horticulture research funding, about $0.6 billion for 2019–23, is set beside the 2019–23 research budgets for the two NIH Divisions with most responsibility for obesity, T2D, and their complications (Fig. 3B). The budget of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) is $10.8 billion; the part of the budget of the National Heart, Lung, and Blood Institute (NHLBI) dedicated to cardiovascular disease research is about $9.3 billion. Added together, these NIH research budgets are over 30 times that for horticulture. And yet horticultural produce—in quantity and quality—can be as effective as medication in managing obesity and T2D downstream of diagnosis (e.g., ref. 34) and can be even more effective upstream before these conditions ever develop (e.g., ref. 35). The 2020-30 Strategic Plan for NIH Nutrition Research (36) and recent proposals to strengthen and coordinate US nutrition research (12, 37) do not yet integrate horticulture, but could evolve to do so.
A positive take-home on funding is the stellar return on investment (ROI) from fruit and vegetable crop research. To gauge this roughly but robustly, similarly to (38), we tracked a proxy for research investment, the number of publications per year (Fig. 3C), and yield advance over a 50 y period (Fig. 3D). We took strawberry (Fragaria × ananassa) as an example of a healthful fruit and maize (Zea mays) as a benchmark crop that has long profited greatly from research (39). Relative to maize, strawberry research delivered threefold more yield advance from sixfold less investment (Fig. 3 C and D). Strawberry research thus has a recent ROI 18 times that of maize research, whose ROI is already good.
What, Then, Should We Do Differently?
Running the numbers side-by-side on the health, nutrition, and horticulture dimensions of the crisis suggests what to do differently from here on out. Changes are needed in three areas: foundations, research, and practice (Fig. 4). We cover each below, stressing actionable ideas. The overall goal is a food system that i) makes healthful fruits and vegetables accessible, affordable, and appealing for all, and ii) is integrated with healthcare spanning patient-based to population-based nutrition (Fig. 4).
Foundations.
Underpinning everything else is the need for breadth as well as depth in today’s mindsets and tomorrow’s training. This is neatly captured by the idea of “T-shaped” professionals who have both traditional disciplinary expertise (the T’s upright stroke) and awareness and understanding of other expertise (the T’s cross stroke) (40). Such actors are critical when dealing with “wicked problems” (41), of which the current health crisis is surely one. US Land Grant universities are particularly well placed to foster T-shaped thinking and education. Their triple mandate for research, teaching, and extension—which faces outward to the real world—is inherently T-shaped and gives them a high level of public trust, which is crucial in times of change. Further, Land Grant universities can have medicine, nutrition, and horticulture on the same campus. As Tony Robbins said: “Proximity is power”.
T-shaped thinking can only turn into effective action if it is incentivized. The incentives must be massive because “Team Science” has already been encouraged for a decade or more (42) but has never really taken hold. At the university level, incentives could be tenure and promotion criteria that require cross-disciplinary work, and joint appointments, e.g., between medicine or nutrition and horticulture. This could be reinforced by “cluster hires” (multiple faculty hired simultaneously into a “cluster” focused on a specific interdisciplinary area). At the federal level, incentives could be inter- or intra-agency programs that fund only work that integrates medicine, nutrition, and horticultural science. In any case, the resulting next-gen collaborations must be deeper, better resourced, and more powerful than ever before if we are to break free of small, disparate studies and inconclusive intervention trials (43).
Research.
Here, we suggest five broad areas with potential backed by evidence. They are examples of the opportunities; there are many others.
Prioritize health in research on fruits and vegetables. The term “health” here has three parts: which fruits and vegetables are most beneficial to which people (and why), which ones patients and other consumers are most likely to eat (and why, i.e., behavior and economic research), and which ones are most readily produced cost-effectively at scale (and where). Red, orange, and blue fruits and vegetables, as well as dark green leafy vegetables, are clearly healthful (44) but essentially any fruit or vegetable can be made more healthful if this is prioritized based on dialog among physicians, nutritionists, and horticultural scientists. A key goal is to move beyond traditional research strategies that often fail to demonstrate clear health benefits to strategies that directly connect horticultural produce to health outcomes.
Within each target crop, define and prioritize key traits for improvement via classical and molecular breeding (45, 46) and synthetic biology (47), and by management (48). Key traits include palatability and its interaction with preferences (49), reducing food waste by minimizing or repurposing nonconsumable plant parts and extending shelf life (50–52), increasing nutrient density (10), and antioxidant content (53), lowering the glycemic index (54), and exploring natural lower-glycemic plant sugars (55). Besides these traits, an overarchingly important issue is to reduce labor costs. The long-term prospects for AI-driven mechanical harvesting are excellent (56), and meanwhile much can be done by breeding for greater ease—and hence lower cost—of manual harvesting (57).
Develop and spread evidence-based, nutritionally and therapeutically relevant information on the interactions between intake of whole fruits and vegetables, gut microbiomes, health, and disease, and on behavioral factors that affect healthful dietary patterns. Research in these areas is exploding (36, 58–60) and enabling interventions to maintain health and prevent and treat diseases at individual patient and population levels. The prebiotics (dietary fibers), antioxidants, and other compounds in fruits and vegetables are clearly pivotal to gut microbiome composition, but mechanisms are still speculative. Cross-disciplinary discoveries need to be made.
Develop and clinically trial fruit- and vegetable-rich diets that reverse insulin resistance before and after T2D is diagnosed. Such preventive and therapeutic dietary interventions have had local, short-term success, notably in the Food Is Medicine movement (12, 60). But research is needed on their long-term effects (61), on benefits based on age of implementation (62), and on how to roll them out at scale with the flexibility needed to account for preferences, for different household budgets, and for seasonal shifts in fresh produce availability.
Develop and clinically test diets for brain health that prevent or slow neurodegeneration and optimize function at any stage. At least one in five older US adults with T2D experiences some degree of cognitive impairment or dementia, and this fraction is rising along with the prevalence of T2D (63). As for insulin resistance, there is evidence that high fruit and vegetable consumption sustains cognition in later life, but which ones, in what amounts, and why, all need more research (64). More broadly, T2D being a risk factor for heart disease and stroke, a reduction in T2D would also reduce the risk of these comorbidities, which can affect quality of life and cognition.
Practice.
In this area, we include horticultural production itself and the extension activities that transfer research findings to producers and consumers. Production and consumption patterns cannot change without effective community outreach, as is provided by extension educators from Land Grant universities (65). Before suggesting changes, we stress that the food and healthcare systems are rat’s nests of complexity in which opposing and competing interests, overlapping mandates, and clashing economic and social philosophies vie for power and federal support (1, 5). For the people these systems should serve, roadblocks to healthy fruit and vegetable intake include costs, poor geographic access, lack of time or skills needed for food preparation, cultural norms, and personal preferences (66). In such a complex arena, actors with siloed approaches who are ignorant about, or lose sight of, the interplay of the different components will be ineffectual, and their actions will likely lead to unintended consequences (67). Hence, in part, our emphasis above on the need for T-shaped actors.
Devise and implement ways to integrate horticultural sciences with medicine and nutrition, e.g., as pioneered at Texas A&M University’s Vegetable and Fruit Improvement Center (68). Besides university reforms to drive integration (see above), opportunities include cotaught, cross-disciplinary courses, e.g., lectures for doctors on why fruits and vegetables are healthful and how they are grown, and for horticultural scientists on health issues that fruits and vegetables help prevent or treat. In parallel, more extension programs can be designed to fix disconnects between trustworthy medical and academic information on fruit and vegetable intake and what the public hears. The public is bombarded with poor information promoting skepticism about the safety and health attributes of fruits and vegetables. A promising intervention opportunity is to leverage the surge in use of subcutaneously injected glucagon-like peptide-1 receptor (Glp-1) agonists (e.g., Wegovy®, Zepbound®) to treat obesity (69). These injections could be combined with nutrition counseling and support programs, potentially reinforced by continuous glucose monitoring (70, 71), to help patients replace calorie-dense, processed foods (for which Glp-1 agonists reduce intake) with healthful fruits and vegetables (72). As Drs. Sarah Berry and Tim Spector quip: “You can’t out-inject a bad diet; Glp-1 still requires healthy eating” (73).
Create five NIH-supported Food Is Medicine centers that equally support medical, nutritional, and horticultural research and extension. Centers in the South, Northeast, Midwest, Southwest, and Northwest are needed because each region differs in demographics, food preferences, and fruit and vegetable production. In the South, for instance, Florida has an aging population and migration patterns that foreshadow national trends and is the number two State in horticultural production. These features make Florida an ideal sandbox in which to take Food Is Medicine to the next level.
Scale Food Is Medicine from its present local and patient-treatment-centric form to the population level with an emphasis on prevention. The size of the crisis (Fig. 1) makes this upshift from treating individuals to population health essential (60). The massive expansion of domestic fruit and vegetable production needed to support the upshift (Fig. 2) makes horticultural science just as essential.
Align production expansion with evolving healthful eating guidelines. This imperative has an extension part and a federal funding part. Extension is within this article’s scope (see above). The politics of the Farm Bill and of NIH support for horticultural research and production are not. With that said, a glance at Fig. 3 is enough to show the lopsided nature of current Farm Bill and NIH funding and of commodity funding vs. horticultural funding within the Farm Bill.
Work with food processors to make increased fruit and vegetable intake a plus for them, not a minus. Although the food industry is often blamed for the obesity epidemic and its effects on health (e.g., refs. 1, 5, and 66) there is no escaping TINA: there Is No Alternative to having this industry on board. As with federal funding, formulating how to achieve this is beyond this article’s scope. We can nonetheless point to evidence-based marketing and to extending the usability and value of fruits and vegetables to maximize access and minimize waste by canning, freezing, extract preparation, and other means (74, 75).
Epilogue
This article’s authors are horticultural scientists, physicians, nutritionists, extension specialists, and administrators from the same university. We came together to write the article as a call to action, to be followed up by specific, transdisciplinary action plans. The United States and many other countries are in the grip of a population health crisis brought on by interlocking failures in the food and healthcare systems. Ways to manage and even reverse the crisis are at hand. Implementing them demands new tools: institutional structures and funding programs that are fit for a challenging purpose. As Winston Churchill said: “Give us the tools and we will finish the job.”
Supplementary Material
Dataset S01 (XLSX)
Dataset S02 (XLSX)
Dataset S03 (XLSX)
Acknowledgments
We thank Drs. Suzanne D. Thornsbury and Lisa House for guidance on food economics, Eva Sailly for graphic design support, and the following colleagues for thoughtful comments on manuscript drafts: Dr. Deep Saini, Dr. Romeena Lee, Dr. Amy Sheer, Dr. James Manley, and Leann Manley.
Author contributions
C.C.G., D.D.T., and A.D.H. designed research; C.C.G., D.D.T., M.F.R.R., V.M.W., K.M.B., K.P.S., P.R.B., J.E.A., R.G.-S., A.V.B., W.T.D., M.S.J., J.S.A., and A.D.H. performed research; C.C.G., D.D.T., and A.D.H. analyzed data; and C.C.G., D.D.T., and A.D.H. wrote the paper.
Competing interests
The authors declare no competing interest.
Footnotes
Reviewers: M.F., Virginia Polytechnic Institute and State University; E.M., University of California Davis; B.S.P., Texas A&M University; and L.R., Purdue University System.
Data, Materials, and Software Availability
All study data are included in the article and/or supporting information. Previously published data were used for this work (Datasets S1–S3).
Supporting Information
References
- 1.Jackson R. J., Minjares R., Naumoff K. S., Shrimali B. P., Martin L. K., Agriculture policy is health policy. J. Hunger Environ. Nutr. 4, 393–408 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muller M., Schoonover H., Wallinga D., Considering the Contribution of U.S. Food and Agricultural Policy to the Obesity Epidemic: Overview and Opportunities (Institute for Agriculture and Trade, 2007), https://healthyeatingresearch.org/wp-content/uploads/2013/12/Considering-the-contribution-of-U.S.-Food-and-Agricultural-Policy.pdf. [Google Scholar]
- 3.National Institute of Diabetes and Digestive and Kidney Diseases, Health Statistics (2023), https://www.niddk.nih.gov/health-information/health-statistics. Accessed December 23, 2024.
- 4.Andes L. J., Cheng Y. J., Rolka D. B., Gregg E. W., Imperatore G., Prevalence of prediabetes among adolescents and young adults in the United States, 2005–2016. JAMA Pediatr. 174, e194498 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cullerton K., Donnet T., Lee A., Gallegos D., Playing the policy game: A review of the barriers to and enablers of nutrition policy change. Public Health Nutr. 19, 2643–2653 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed T., The political lens on food is changing Axios (2024) https://www.axios.com/2024/12/18/american-diet-politics-chronic-disease. Accessed December 24, 2024.
- 7.Mozaffarian D., Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: A comprehensive review. Circulation 133, 187–225 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hood R., Selfridge N., Fruits and vegetables lower the risk of type 2 diabetes. Integr. Med. Alert 23, 12 (2020). [Google Scholar]
- 9.Buzby J. C., Wells H. F., Vocke G., Possible Implications for U.S. Agriculture from Adoption of Select Dietary Guidelines Economic Research Report no. 31 (U.S. Department of Agriculture, Washington, DC, 2006). https://ageconsearch.umn.edu/record/7230. [Google Scholar]
- 10.Simon P. W., Progress toward increasing intake of dietary nutrients from vegetables and fruits: The case for a greater role for the horticultural sciences. HortScience 49, 112–115 (2014). [Google Scholar]
- 11.Rehm C. D., Peñalvo J. L., Afshin A., Mozaffarian D., Dietary intake among US adults, 1999–2012. JAMA 315, 2542–2553 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleischhacker S. E., et al. , Strengthening national nutrition research: Rationale and options for a new coordinated federal research effort and authority. Am. J. Clin. Nutr. 112, 721–769 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reinhardt S., Where’s the federal funding for food systems research? Curr. Dev. Nutr. 5, 87 (2021). [Google Scholar]
- 14.Cummings J. N., Kiesler S., Collaborative research across disciplinary and organizational boundaries. Soc. Stud. Sci. 35, 703–722 (2005). [Google Scholar]
- 15.Chure G., et al. , Anthroponumbers.org: A quantitative database of human impacts on Planet Earth. Patterns 3, 100552 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janssen J. A., Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer. Int. J. Mol. Sci. 22, 7797 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abdelaal M., le Roux M. C. W., Docherty N. G., Morbidity and mortality associated with obesity. Ann. Transl. Med. 5, 161 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taylor R., Insulin resistance and type 2 diabetes. Diabetes 6, 778 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Putnam J., Allshouse J., Kantor L. S., US per capita food supply trends: More calories, refined carbohydrates, and fats. Food Rev. 25, 2–15 (2002). [Google Scholar]
- 20.USDA MyPlate, What is MyPlate? https://www.myplate.gov/eat-healthy/what-is-myplate. Accessed 23 December 2024. [Google Scholar]
- 21.Kianmehr H., et al. , Potential gains in life expectancy associated with achieving treatment goals in US adults with type 2 diabetes. JAMA Netw. Open 5, e227705 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kotwas A., Karakiewicz B., Zabielska P., Wieder-Huszla S., Jurczak A., Epidemiological factors for type 2 diabetes mellitus: Evidence from the global burden of disease. Arch. Public Health 79, 110 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee C., Boye K., Bergman B., Williamson S. E., Nelson D. R., Early-onset Type 2 diabetes in the US – prevalence from national health and nutrition examination survey (NHANES) data. Diabetes 73, 1999–2020 (2024). [Google Scholar]
- 24.Parker E. D., et al. , Economic costs of diabetes in the U.S. in 2022. Diabetes Care 47, 26–43 (2024). [DOI] [PubMed] [Google Scholar]
- 25.World Economic Forum, Transforming the Global Food System for Human Health and Resilience (World Economic Forum, 2023), https://www3.weforum.org/docs/WEF_New_Frontiers_of_Nutrition_2023.pdf. [Google Scholar]
- 26.Lee S. H., Adults meeting fruit and vegetable intake recommendations – United States, 2019 MMWR. Morb. Mortal. Wkly Rep. 71, 1–9 (2022), https://www.cdc.gov/mmwr/volumes/71/wr/mm7101a1.htm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Veronese N., et al. , Fried potato consumption is associated with elevated mortality: An 8-y longitudinal cohort study. Am. J. Clin. Nutr. 106, 162–167 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guasch-Ferré M., Hu F. B., Are fruit juices just as unhealthy as sugar-sweetened beverages? JAMA Netw. Open 2, e193109 (2019). [DOI] [PubMed] [Google Scholar]
- 29.Finley J., et al. , Perspective: Understanding the intersection of climate/environmental change, health, agriculture, and improved nutrition–A case study: Type 2 diabetes. Adv. Nutr. 10, 731–738 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young S., Hyman J., Stewart H., Satisfying Fruit and Vegetable Recommendations Possible for under $3 A Day, data analysis shows (Amber Waves, 2024) https://www.ers.usda.gov/amber-waves/2024/september/satisfying-fruit-and-vegetable-recommendations-possible-for-under-3-a-day-data-analysis-shows. [Google Scholar]
- 31.Juul F., Parekh N., Martinez-Steele E., Monteiro C. A., Chang V. W., Ultra-processed food consumption among US adults from 2001 to 2018. Am. J. Clin. Nutr. 115, 211–221 (2022). [DOI] [PubMed] [Google Scholar]
- 32.Ribera L. A., Young L. K., “Outlook of fresh fruits and vegetables in the United States” (CNAS Rep. 2024-01, Center for North American Studies, 2024; https://www.freshproduce.com/siteassets/files/advocacy/2024.01.outlook-of-fresh-fruits-and-vegetables-in-the-united-states-luis-final.pdf). Accessed 23 December 2024.
- 33.Astill G., Food Loss: Why Food Stays on The Farm or off The Market (USDA Economic Research Service, Amber Waves, 2020). [Google Scholar]
- 34.Unwin D., Delon C., Unwin J., Tobin S., Taylor R., What predicts drug-free type 2 diabetes remission? Insights from an 8-year general practice service evaluation of a lower carbohydrate diet with weight loss BMJ Nutr. Prev. Health 6, 46–55 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertoia M. L., et al. , Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: Analysis from three prospective cohort studies. PLoS Med. 12, e1001878 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rodgers G. P., Collins F. S., Precision nutrition – the answer to “what to eat to stay healthy”. JAMA 324, 735–736 (2020). [DOI] [PubMed] [Google Scholar]
- 37.Nicastro H. L., et al. , Opportunities to advance implementation science and nutrition research: A commentary on the Strategic Plan for NIH Nutrition Research. Transl. Behav. Med. 13, 1–6 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bloom N., Jones C. I., Van Reenen J., Webb M., Are ideas getting harder to find? Am. Econ. Rev. 110, 1104–1144 (2020). [Google Scholar]
- 39.Duvick D. N., The contribution of breeding to yield advances in maize (Zea mays L.). Adv. Agron. 86, 83–145 (2005). [Google Scholar]
- 40.Conley S. N., Foley R. W., Gorman M. E., Denham J., Coleman K., Acquisition of T-shaped expertise: An exploratory study. Soc. Epistemol. 31, 165–183 (2017). [Google Scholar]
- 41.Peters B. G., What is so wicked about wicked problems? A conceptual analysis and a research program Policy Soc. 36, 385–396 (2017). [Google Scholar]
- 42.National Research Council, Enhancing the Effectiveness of Team Science (The National Academies Press, Washington, DC, 2015). [PubMed] [Google Scholar]
- 43.Ioannidis J. P., Implausible results in human nutrition research. BMJ 347, f6698 (2013). [DOI] [PubMed] [Google Scholar]
- 44.Blumfield M., et al. , Should we “Eat a Rainbow”? An umbrella review of the health effects of colorful bioactive pigments in fruits and vegetables. Molecules 27, 4061 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumar M., et al. , Breeding approaches for quality improvement in fruit crops: Strategies and achievements. Int. J. Environ. Clim. Chang. 13, 75–93 (2023). [Google Scholar]
- 46.Natalini A., Acciarri N., Cardi T., Breeding for nutritional and organoleptic quality in vegetable crops: The case of tomato and cauliflower. Agriculture 11, 606 (2021). [Google Scholar]
- 47.Oliveira-Filho E. R., Voiniciuc C., Hanson A. D., Adapting enzymes to improve their functionality in plants: Why and how. Biochem. Soc. Trans. 51, 1957–1966 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rouphael Y., et al. , Vegetable quality as affected by genetic, agronomic and environmental factors. J. Food Agric. Environ. 10, 680–688 (2012). [Google Scholar]
- 49.Fan Z., et al. , Strawberry sweetness and consumer preference are enhanced by specific volatile compounds. Hort. Res. 8, 66 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pop C., Suharoschi R., Pop O. L., Dietary fiber and prebiotic compounds in fruits and vegetables food waste. Sustainability 13, 7219 (2021). [Google Scholar]
- 51.Kumar K., Yu Q., Bhatia D., Honsho C., Gmitter F. G. Jr., Construction of a high density genetic linkage map to define the locus conferring seedlessness from Mukaku Kishu mandarin. Front. Plant Sci. 14, 1087023 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chase K., et al. , Examining preharvest genetic and morphological factors contributing to lettuce (Lactuca sativa L.) shelf-life. Sci. Rep. 14, 6618 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mattia M. R., et al. , Genome-wide association study of healthful flavonoids among diverse Mandarin accessions. Plants 11, 317 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ek K. L., Wang S., Copeland L., Brand-Miller J. C., Discovery of a low-glycaemic index potato and relationship with starch digestion in vitro. Br. J. Nutr. 111, 699–705 (2014). [DOI] [PubMed] [Google Scholar]
- 55.Hough L., Stacey B. E., Biosynthesis and metabolism of allitol and D-allulose in Itea plants; Incorporation of 14CO2. Phytochemistry 5, 215–222 (1966). [Google Scholar]
- 56.Kaleem A., et al. , Development challenges of fruit-harvesting robotic arms: A critical review. AgriEngineering 5, 2216–2237 (2023). [Google Scholar]
- 57.Whitaker V. M., et al. , ‘Florida brilliance’ strawberry. HortScience 54, 2073–2077 (2019). [Google Scholar]
- 58.Gérard P., Li G. G., Bhuyan D. J., Fruits, vegetables, and biotics for a healthy gut microbiome. Front. Nutr. 11, 1468453 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Valles-Colomer M., et al. , Cardiometabolic health, diet and the gut microbiome: A meta-omics perspective. Nat. Med. 29, 551–561 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ridberg R. A., et al. , Food is medicine national summit: Transforming health care. Am. J. Clin. Nutr. 120, 1441–1456 (2024). [DOI] [PubMed] [Google Scholar]
- 61.Firman C. H., Mellor D. D., Unwin D., Brown A., A, Does a ketogenic diet have a place within diabetes clinical practice? Review of current evidence and controversies Diabetes Ther. 15, 77–97 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Voss C. H., Loughnan R. C., Food as medicine in early childhood: A critical review of the evidence and future directions. J. Nutr. Sci. 9, e51 (2020).33240495 [Google Scholar]
- 63.Kotecha P., et al. , Continuous glucose monitoring and all-cause mortality in insulin-using population with diabetes and cognitive impairment. Diabetes Obes. Metab. 26, 4795–4798 (2024). [DOI] [PubMed] [Google Scholar]
- 64.Haskell-Ramsay C. F., Docherty S., Role of fruit and vegetables in sustaining healthy cognitive function: Evidence and issues. Proc. Nutr. Soc. 82, 305–314 (2023). [DOI] [PubMed] [Google Scholar]
- 65.Bickell E. G., The agricultural cooperative extension system: An overview. Congress. Res. Ser. R48071, (2024), https://crsreports.congress.gov. [Google Scholar]
- 66.Reinhardt S., Delivering on the dietary guidelines. https://www.ucs.org/resources/delivering-dietary-guidelines. Accessed 23 December 2024.
- 67.Castilleja G., “Why true cost accounting” in True Cost Accounting for Food – Balancing the Scale, Gemmill-Herren B., Baker L. E., Daniels P. A., Eds. (Taylor and Francis, 2021), pp. xxxi–xxxv. [Google Scholar]
- 68.Vegetable and Fruit Improvement Center (Texas A&M University; ) https://vfic.tamu.edu/. [Google Scholar]
- 69.Celletti F., Branca F., Farrar J., Obesity and glucagon-like peptide-1 receptor agonists. JAMA 333, 561–562, (2024), 10.1001/jama.2024.25872. [DOI] [PubMed] [Google Scholar]
- 70.Miller E., Miller K., Detection and intervention: Use of continuous glucose monitoring in the early stages of Type 2 diabetes. Clin. Diabetes 42, 398–407 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Tan Y. Y., Suan E., Koh G. C. H., Suhairi S. B., Tyagi S., Effectiveness of continuous glucose monitoring in patient management of Type 2 Diabetes Mellitus: An umbrella review of systematic reviews from 2011 to 2024. Arch. Public Health 82, 1–23 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hristakeva S., Liaukonyte J., Feler L., The No-Hunger Games: How GLP-1 Medication Adoption is Changing Consumer Food Purchases (Cornell SC Johnson College of Business Research Paper, 2024). [Google Scholar]
- 73.ZOE Science and Nutrition Podcast, How to eat in 2025: 7 science-backed tips | Prof. Tim Spector and Prof. Sarah Berry. (2025), https://youtu.be/iRxbxmjjjdw?si=0VEMyGf49vZJE6oU. Accessed January 5, 2025.
- 74.Rickman J. C., Bruhn C. M., Barrett D. M., Nutritional comparison of fresh, frozen, and canned fruits and vegetables II. Vitamin A and carotenoids, vitamin E, minerals and fiber. J. Sci. Food Agric. 87, 1185–1196 (2007). [Google Scholar]
- 75.Salas-Millán J. Á., Aguayo E., Fermentation for revalorisation of fruit and vegetable by-products: A sustainable approach towards minimising food loss and waste. Foods 13, 3680 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dataset S01 (XLSX)
Dataset S02 (XLSX)
Dataset S03 (XLSX)
Data Availability Statement
All study data are included in the article and/or supporting information. Previously published data were used for this work (Datasets S1–S3).



