Abstract
Background
Burnout, marked by emotional exhaustion and reduced clinical performance, may impair the effective application of noninvasive respiratory support (NIRS) and timely transition to invasive methods, potentially affecting patient outcomes. This study aims to identify the impact of burnout on the knowledge, attitudes, and practices (KAP) of healthcare professionals in the application of respiratory support, and further explore how other factors may influence these areas.
Method
A cross-sectional study was conducted from November 15, 2023, to December 14, 2023, at multiple hospitals in central China, involving key departments such as emergency, respiratory, cardiology, and critical care. Demographic information, alongside scores measuring KAP was gathered through the dissemination of questionnaires. Knowledge was assessed using a scoring system (range: 0–24), while attitude and practice were measured using 5-point Likert scales, with score ranges of 8–40 and 8–56, respectively. The Chinese version of the Maslach Burnout Inventory General Survey (MBI-GS) was used to assess occupational burnout.
Results
A total of 517 valid questionnaires were enrolled, including 284 (54.9%) nurses, and 269 (52%) had worked for less than 10 years. The median scores for knowledge, attitude, practice, and burnout were 20, 26, 38, and 40, respectively. Participants from private hospitals exhibited burnout scores higher than 50. Burnout was negatively correlated with both attitude (r = -0.289) and practice (r = -0.206). Multivariate logistic regression showed that practice, as the dependent variable, was independently associated with a knowledge score below 20 (OR = 0.441, 95% CI: [0.297, 0.657]), an attitude score below 26 (OR = 0.493, 95% CI: [0.335, 0.724]), and burnout scores below 40 (OR = 0.539, 95% CI: [0.364–0.796]) were independently associated with practice. Age above 40 years (OR = 0.470, 95% CI: [0.264, 0.837]), being a nurse (OR = 0.627, 95% CI: [0.424, 0.928]), and lack of recent training in respiratory support (OR = 0.590, 95% CI: [0.403, 0.866]) were also associated with lower practice scores.
Conclusions
Healthcare professionals had sufficient knowledge, positive attitudes, and proactive practices regarding the application of respiratory support. However, the impact of burnout must not be overlooked, even for those scoring below the threshold (50 points), as burnout can still significantly affect clinical performance. Healthcare institutions should prioritize continuous education and training programs focusing on respiratory support, especially for high stress environment professionals, to enhance clinical practice and patient outcomes.
Clinical trial number
not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-025-07302-8.
Keywords: Respiratory support, Healthcare professional, Knowledge, Attitude, Practice
Background
Reducing mortality from respiratory illnesses is critically dependent on effective respiratory support strategies [1]. These strategies encompass a range of techniques from oxygen therapy to both invasive and non-invasive mechanical ventilation. Noninvasive respiratory support (NIRS), which includes standard oxygen therapy (SOT), high-flow oxygen therapy (HFOT), and noninvasive ventilation (NIV), plays a pivotal role in the early management of patients with acute hypoxemic respiratory failure (AHRF) and acute respiratory distress syndrome (ARDS) [2, 3]. NIV encompasses modes such as continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP), typically delivered via a mask interface [4]. When NIRS proves insufficient, particularly in cases where the respiratory demand overwhelms the system’s capacity, transitioning to invasive mechanical ventilation is key [5, 6]. Invasive mechanical ventilation not only facilitates physiological gas exchange but also may provide lung and diaphragm protection under lung-protective strategies, thereby allowing time for the lungs to recover and preventing the progression of patient self-inflicted lung injury [7, 8]. However, it is imperative to carefully manage the transition between noninvasive and invasive respiratory support, as neglecting the underlying physiology of the respiratory system can lead to the exacerbation of lung injury [9]. Respiratory support is often administered in emergency and critical situations, which demands not only advanced technical skills but also tests the psychological resilience and operational competence of healthcare professionals [10]. Under such high-pressure conditions, burnout - characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment - can significantly hinder clinical decision-making and impair the ability to deliver high-quality care. Burnout increases the likelihood of errors, delays in care, and suboptimal management of respiratory support interventions, which ultimately affects patient safety and outcomes.
The Knowledge-Attitude-Practice (KAP) model is foundational in understanding and influencing health behaviors, serving as a crucial framework within health literacy to evaluate the knowledge, attitudes, and practices prevalent among specific populations, particularly in the healthcare sector [11]. Utilizing the KAP questionnaire, researchers can thoroughly assess the knowledge levels, attitudes, and practical approaches of target groups towards health-related topics, further analyzing the demand for and acceptance of pertinent information [12]. Central to this model is the principle that increased knowledge positively affects attitudes, which in turn, shape behaviors and practices [13]. In healthcare, professionals’ knowledge and perspectives are critical, as their decisions directly impact the selection and management of respiratory support techniques. Burnout, however, may disrupt this chain by undermining knowledge retention, fostering negative attitudes, and reducing engagement with best practices, thereby weakening the overall KAP framework.
Although previous studies have investigated the effects of burnout on specific clinical behaviors, such as communication and adherence to guidelines, research addressing its relationship with the integrated KAP model in the context of respiratory support is currently limited. Existing literature tends to focus either on the impact of burnout on general professional performance or on knowledge and practice regarding respiratory support, but seldom on their intersection [14, 15]. This study therefore aims to bridge this gap by examining how burnout may influence healthcare professionals’ knowledge, attitudes, and practices in the application of respiratory support, with the goal of informing strategies to improve clinical implementation and training in high-pressure environments.
Despite the critical importance of such an inquiry, research specifically targeting the KAP of healthcare professionals in the application of respiratory support has been conspicuously absent. This gap underscores the need for this study, which aims to explore the KAP of healthcare professionals regarding respiratory support, with particular attention to the influence of occupational burnout. This investigation not only seeks to illuminate the current state of professional understanding and application of respiratory support techniques but also to identify opportunities for improving healthcare delivery and outcomes for patients with respiratory conditions.
Materials and methods
Study design and participants
This cross-sectional study was conducted between November 15, 2023 and December 14, 2023, at multiple hospitals located in central China. The study primarily targeted physicians and nurses working in emergency, respiratory, cardiology, and intensive care departments. Demographic information, along with scores measuring knowledge, attitude, and practice related to the application of respiratory support, was collected through structured questionnaires. Ethical approval was obtained from the Ethics Committee of Taihe County People’s Hospital, and informed consent was obtained from all participants prior to questionnaire administration.
Inclusion criteria comprised individuals aged 18 years or older, primarily registered physicians and nurses, including emergency physicians, intensivists, respiratory physicians, cardiologists, and nurses engaged in frontline respiratory care, who were working in emergency, respiratory, cardiology, or critical care departments at the time of the survey. Approximately 650 physicians and nurses across the selected institutions were eligible to participate in this study. Additionally, participants were required to complete the questionnaire in its entirety and provide informed consent. Exclusion criteria encompassed completion times of less than 90 s and duplicate questionnaire submissions.
The study employed a convenience sampling method and enlisted ten trained medical research assistants to assist in questionnaire distribution and collection. The questionnaires were disseminated through WeChat workgroups across various departments at at Taihe County People’s Hospital, Anhui Medical University First Affiliated Hospital, Fuyang People’s Hospital, Taihe County Huayuan Hospital, and Taihe County Second People’s Hospital. Participants completed the questionnaires online using the Wenjuanxing platform (https://www.wjx.cn/app/survey.aspx).
Questionnaire introduction
The questionnaire design was guided by pertinent guidelines and literature. The content was formulated based on relevant national guidelines including: 2017 COPD exacerbation consensus, 2019 high-flow oxygen therapy consensus, and 2020 ECMO clinical practice expert consensus [16–18]. Feedback was solicited from two experts: Dr. Jun Chen, Deputy Chief Physician of the Respiratory Department at the First Affiliated Hospital of the University of Science and Technology of China, and Dr. Min Shao, Director of the Intensive Care Medicine Department at the First Affiliated Hospital of Anhui Medical University. Their expert feedback focused on ensuring the content validity, clarity of the questions, and alignment with clinical practices.
A pilot study was conducted after the initial development phase with 50 healthcare professionals to assess the questionnaire’s clarity, structure, and reliability. During this phase, modifications were made to improve question phrasing and response options based on participant feedback. The internal consistency of the questionnaire was evaluated using Cronbach’s α coefficient which yielded 0.809 for the pilot version, indicating commendable reliability. Additionally, the final version was tested for construct validity using exploratory factor analysis to confirm the alignment of the items with the intended dimensions. These steps ensured both the credibility and reliability of the self-developed questionnaire.
The final questionnaire encompassed four dimensions: demographic information, knowledge, attitude, and practice (appendix). The knowledge dimension comprised 11 questions, with correct responses earning 2 points, and incorrect or uncertain responses earning 1 point, resulting in a score range of 11–22 points. The attitude dimension comprised 7 questions, utilizing a five-point Likert scale ranging from “Strongly Agree” (5 points) to “Strongly Disagree” (1 point), yielding a score range of 7–35 points. Similarly, the practice dimension comprised 9 questions, employing a five-point Likert scale ranging from " Very much so " (5 points) to " Very inconsistent " (1 point), with a score range of 9–45 points. These three dimensions were designed to assess knowledge, attitudes, and practices related to the application of respiratory support. Scores exceeding 70% of the total possible value were interpreted as indicative of satisfactory knowledge, favorable attitudes, and proactive practices. This criterion was based on the absolute score range rather than the actual distribution within the study population and was applied for descriptive analysis. For logistic regression, the median score of the total population was used as the cut-off to reduce group imbalance and ensure comparability between categories [19]. The Chinese version of the Maslach Burnout Inventory General Survey (MBI-GS) was used to assess occupational burnout [20, 21]. For the assessment of occupational burnout, the MBI-GS Occupational Burnout Scale employed a 7-point Likert scale ranging from “Always” (6 points) to “Never” (0 points). Standardized scoring involved the summation of total scores divided by 15, then multiplied by 20. While a score ≥ 50 generally indicates the presence of burnout, we adopted a threshold of 40 in multivariate regression analysis due to the imbalanced group sizes that resulted from using the standard cut-off, which impeded statistical analysis.
Statistical analysis
Statistical analysis was conducted using SPSS 26.0 (IBM Corp., Armonk, N.Y., USA). Continuous variables were described using median (25th percentile, 75th percentile), and between-group comparisons were performed using Wilcoxon-Mann-Whitney tests or Kruskal-Wallis analysis of variance. Categorical variables were presented as n (%). Spearman correlation analysis was employed to assess the correlations between knowledge, attitude, and practice scores. In multivariate analysis, the median score of the total population was used as the cut-off point to minimize group imbalance and enhance statistical robustness. Variables with P < 0.1 in univariable analysis were entered into multivariate regression using a forward stepwise selection method. To explore the relationship between burnout and KAP, the low burnout group was used as the reference category in regression models. Although an additional analysis using the standard burnout threshold of 50 was considered, the resulting sample imbalance between groups prevented its inclusion in logistic regression. The dependent variable for the multivariate logistic regression was practice, dichotomized using a median score of 38. Structural equation modeling (SEM) was used to validate hypotheses regarding the interrelationships among KAP and burnout. Two-sided p < 0.05 were considered statistically significant in this study.
Results
Initially, = 550 questionnaires were collected, with approximately 650 physicians and nurses estimated to be eligible across the participating institutions. After excluding 20 questionnaires that took less than 90 s or more than 1,800 s to complete, and 13 questionnaires with incomplete responses, a total of 517 valid questionnaires were included, yielding a validity rate of 94%. The Cronbach’s α coefficient for the formal experiment feedback questionnaire was 0.812; the Kaiser-Meyer-Olkin (KMO) value for the self-made questionnaire was 0.886; and the KMO value for the MBI-GS Occupational Burnout Scale was 0.932.
Out of 517 participants, 245 (47.4%) were aged 30–39 years, 284 (54.9%) were nurses, 328 (63.4%) were females, 328 (63.4%) had Bachelor’s Degree, 326 (63.1%) were working in public tertiary hospitals, 269 (52.0%) had worked for less than 10 years, 440 (85.1%) of care providers had experience with respiratory support patients, and 316 (61.1%) had received training related to respiratory support in the last six months. The median (IQR) of knowledge, attitude, practice, and MBI-GS scores were 20 (19, 21) (possible range: 11–22), 26 (23, 28) (possible range: 7–35), 38 (35, 44) (possible range: 9–45), and 40 (18.7, 53.3) (possible range: 0–120), separately. Participants with different age, education, nature of institution, years of work experience, department/ward, frequency of respiratory support for patients, and availability of respiratory support related training were more likely to have different knowledge scores. Participants with different education, nature of institution, position, and department/ward were more likely to have different attitude scores. Those with different education, position, and availability of respiratory support related training were more likely to have different practice scores. Moreover, those with different age, education, nature of institution, years of work experience, and departmental frequency of respiratory support were more likely to have different MBI-GS Scale score (P < 0.005) (Table 1).
Table 1.
Basic characteristics of participants and their KAP and burnout scores
| N(%) | Knowledge (K) | Attitude (A) | Practice (P) | MBI-GS Scale | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median (25th percentile, 75th percentile) | P | Median (25th percentile, 75th percentile) | P | Median (25th percentile, 75th percentile) | P | Median (25th percentile, 75th percentile) | P | |||
| Total | 20(19, 21) | 26(23, 28) | 38(35, 44) | 40(18.7, 53.3) | ||||||
| Age | 0.001 | 0.821 | 0.088 | 0.002 | ||||||
| Below 30 years | 180(34.8) | 20(19, 21) | 26(23, 28) | 39(34, 45) | 44(21.3, 56) | |||||
| 30–39 years | 245(47.4) | 21(19, 21) | 26(23, 29) | 38(36, 44) | 41.3(20, 54.7) | |||||
| 40 years and above | 92(17.8) | 19(18, 21) | 26(24, 28) | 36(35, 41.5) | 30(12.7, 42.7) | |||||
| Gender | 0.112 | 0.766 | 0.120 | 0.962 | ||||||
| Male | 189(36.6) | 21(19, 21) | 26(23, 28) | 38(36, 45) | 41.3(18.7, 53.3) | |||||
| Female | 328(63.4) | 20(19, 21) | 26(23, 28.5) | 37.5(35, 44) | 40(18.7, 54.7) | |||||
| Marital status | 0.105 | 0.170 | 0.587 | 0.172 | ||||||
| Married | 374(72.3) | 20(19, 21) | 26(23, 29) | 38(35, 44) | 40(18.7, 52) | |||||
| Other | 143(27.7) | 21(19, 21) | 26(23, 28) | 37(34, 45) | 44(20, 54.7) | |||||
| Education | <0.001 | 0.002 | 0.049 | <0.001 | ||||||
| College | 139(26.9) | 20(18, 21) | 25(23, 28) | 36(34, 42) | 29.3(10.7, 49.3) | |||||
| Bachelor’s degree | 346(66.9) | 20(19, 21) | 26(23, 29) | 38(35, 45) | 41.3(20, 54.7) | |||||
| Master’s degree and above | 32(6.2) | 21(20, 21) | 26(24.5, 29) | 38.5(36, 43.5) | 48(36, 62.7) | |||||
| Professional title | 0.112 | 0.104 | 0.651 | 0.667 | ||||||
| No title | 34(6.6) | 19(17, 21) | 26.5(23, 29) | 39.5(31, 43) | 38.7(18.7, 50.7) | |||||
| Junior | 239(46.2) | 21(19, 21) | 26(23, 28) | 37(35, 45) | 37.3(17.3, 54.7) | |||||
| Intermediate | 209(40.4) | 20(19, 21) | 27(23, 29) | 38(35, 44) | 41.3(20, 53.3) | |||||
| Senior | 35(6.8) | 21(19, 21) | 27(24, 28) | 37(34, 44) | 40(18.7, 50.7) | |||||
| Nature of institution | <0.001 | 0.008 | 0.286 | <0.001 | ||||||
| Public tertiary | 326(63.1) | 21(19, 21) | 27(23, 29) | 38(36, 45) | 42.7(22.7, 56) | |||||
| Public secondary | 154(29.8) | 19.5(18, 21) | 26(23, 28) | 36(34, 43) | 29.3(10.7, 48) | |||||
| Public primary | 19(3.7) | 18(17, 21) | 24(23, 29) | 40(34, 44) | 28(16, 44) | |||||
| Private hospital | 18(3.5) | 20(19, 21) | 24(22, 26) | 38.5(33, 44) | 50.7(41.3, 62.7) | |||||
| Years of work experience | <0.001 | 0.633 | 0.353 | 0.008 | ||||||
| Less than 10 years | 269(52) | 21(19, 21) | 26(23, 29) | 39(35, 45) | 42.7(18.7, 56) | |||||
| 10–19 years | 183(35.4) | 20(19, 21) | 26(23, 28) | 37(35, 44) | 40(21.3, 53.3) | |||||
| 20 years and above | 65(12.6) | 19(18, 21) | 26(24, 27) | 36(35, 42) | 29.3(13.3, 42.7) | |||||
| Position | 0.542 | 0.018 | 0.008 | 0.593 | ||||||
| Physician | 233(45.1) | 20(19, 21) | 27(23, 29) | 39(36, 45) | 41.3(18.7, 54.7) | |||||
| Nurse | 284(54.9) | 20(19, 21) | 26(23, 28) | 37(34.5, 44) | 38.7(18.7, 52) | |||||
| Department/Ward | <0.001 | 0.005 | 0.665 | 0.056 | ||||||
| Emergency Department | 261(50.5) | 20(19, 21) | 26(23, 28) | 38(35, 45) | 38.7(17.3, 52) | |||||
| Respiratory Department | 76(14.7) | 21(19, 21) | 26(24, 29) | 37(35, 43) | 42.7(26.7, 56) | |||||
| Cardiology Department | 100(19.3) | 20(18, 21) | 25(23, 27) | 36.5(35, 43) | 37.3(13.3, 53.3) | |||||
| Intensive Care Unit | 80(15.5) | 21(20, 21) | 27(24, 29.5) | 39(36, 43.5) | 42.7(30.7, 53.3) | |||||
| Frequency of Respiratory Support for Patients | <0.001 | 0.179 | 0.703 | <0.001 | ||||||
| No contact | 78(15.1) | 19(17, 21) | 25(23, 28) | 37(34, 45) | 26(10.7, 46.7) | |||||
| 0–20% | 211(40.8) | 20(19, 21) | 26(23, 28) | 38(36, 44) | 40(18.7, 52) | |||||
| 21–50% | 88(17) | 20(19, 21) | 26(24, 28) | 37.5(35, 43.5) | 40(18.7, 54.7) | |||||
| More than 50% | 140(27.1) | 21(20, 21) | 26(23, 29) | 38(34.5, 44) | 46.7(28.7, 56) | |||||
| Respiratory Support Related Training in the Past Six Months | 0.012 | 0.414 | <0.001 | 0.082 | ||||||
| Yes | 316(61.1) | 21(19, 21) | 26(23, 28) | 40(36, 45) | 40(17.3, 52) | |||||
| No | 201(38.9) | 20(18, 21) | 26(23, 28) | 36(34, 43) | 41.3(24, 54.7) | |||||
Note: Continuous variables are presented as median (interquartile range, IQR); categorical variables are presented as n (%). Frequency of respiratory support for patients was determined based on the reported proportion of respiratory support cases in each participant’s department
Legend: KAP = Knowledge, Attitude, Practice; MBI-GS = Maslach Burnout Inventory-General Survey
The distribution of knowledge dimensions shown that the two knowledge items with the highest correctness rates were “Respiratory support techniques include oxygen therapy, non-invasive mechanical ventilation, and invasive mechanical ventilation.” (K2) with 95.6% and “Patients with acute left heart failure accompanied by significant hypoxemia and respiratory distress (especially with peripheral oxygen saturation < 90%) should receive oxygen therapy early.” (K4) with 93.8%. However, 36.6% of participants were unsure how to adjust the parameters of non-invasive ventilation for patients with severe pancreatitis (K12) (Table 2).
Table 2.
Knowledge dimension of the participants
| A yes | B no | C unclear | ||||
|---|---|---|---|---|---|---|
| K1 In most cases, respiratory support is merely a supportive therapy aimed at “buying time” while alleviating the respiratory failure associated with the underlying disease. | 465(89.9) | 35(6.8) | 17(3.3) | / | / | / |
| K2 Respiratory support techniques include oxygen therapy, non-invasive mechanical ventilation, and invasive mechanical ventilation. | 494(95.6) | 10(1.9) | 13(2.5) | / | / | / |
| K3 Non-invasive positive pressure ventilation refers to a technique where the patient is connected to a ventilator through interfaces such as nasal masks, nasal-oral masks, full-face masks, or helmets, without the need for invasive or endotracheal intubation or tracheostomy. | 469(90.7) | 26(5.0) | 22(4.3) | / | / | / |
| K4 Patients with acute left heart failure accompanied by significant hypoxemia and respiratory distress (especially with peripheral oxygen saturation < 90%) should receive oxygen therapy early. | 485(93.8) | 10(1.9) | 22(4.3) | / | / | / |
| K5 Mechanical ventilation is not suitable for patients undergoing cardiopulmonary resuscitation for cardiac arrest or patients with type I or type II respiratory failure. | 193(37.3) | 272(52.6) | 52(10.1) | / | / | / |
| K6 Absolute contraindications for non-invasive ventilation in heart failure include cardiac arrest, facial anatomical abnormalities, agitation or non-cooperation, altered consciousness, and persistent hypotension. | 403(77.9) | 67(13.0) | 47(9.1) | / | / | / |
| K7 For patients with exacerbations of chronic obstructive pulmonary disease who meet the indications for non-invasive positive pressure ventilation and have no contraindications, early application of non-invasive positive pressure ventilation should be considered to reduce the intubation rate and mortality rate. | 458(88.6) | 26(5.0) | 33(6.4) | / | / | / |
| K8 Non-invasive ventilation should not be routinely used in acute heart failure with cardiogenic pulmonary edema. | 298(57.6) | 165(31.9) | 54(10.4) | / | / | / |
| K9 During non-invasive positive pressure ventilation, it is advisable to avoid wearing the mask (nasal) at high inspiratory pressure levels. | 422(81.6) | 46(8.9) | 49(9.5) | / | / | / |
| K10 Compared to non-invasive ventilation, patients are more likely to tolerate high-flow oxygen therapy. | 371(71.8) | 96(18.6) | 50(9.7) | / | / | / |
| K11 Compared to non-invasive ventilation and invasive mechanical ventilation, high-flow oxygen therapy has less impact on circulation. | 355(68.7) | 92(17.8) | 70(13.5) | / | / | / |
| K12 In a patient with severe pancreatitis, height 1.68 m, weight 63 kg, bladder pressure 25 cmH2O, and using non-invasive ventilation with parameters IPAP 10 cmH2O, EPAP 4 cmH2O, FIO2 50%, with an actual respiratory rate of 28 breaths/minute, VT 453 ml, minute ventilation 7.3 L/min, blood gas analysis: pH 7.52, PCO2 36 mmHg, PO2 65 mmHg, how would you adjust the parameters? | A. increase IPAP | B. increase EPAP | C. Shorten inspiratory time | D. Lengthen inspiratory time | E. Shorten pressure rise time | F. Not sure |
| 113(21.9) | 74(14.3) | 54(10.4) | 79(15.3) | 8(1.5) | 189(36.6) |
K5 correct answer is B; K1-K4,K6-K11 correct answers are all A
Responses to the attitude items showed that 76.8% strongly agreed that it is important to consider the choice of respiratory support techniques based on the patient’s specific condition (A1), and 37.3% agreed that patients’ wishes and preferences often lead to unnecessary distress and influence medical decision-making (A4). Regarding whether guidelines and criteria for respiratory support techniques are confusing and challenging to implement, 34.2% were neutral (A5). On the other hand, 41.8% disagreed that the choice of respiratory support technique can significantly impact outcomes, especially for patients with chronic illnesses (A2) (Table S1).
Participants’ overall practice was proactive and positive, specifically, 54.2% adhered to choosing respiratory support techniques based on the patient’s condition and prognosis (P1), 49.9% adhered to adjusting ventilator parameters based on the patient’s oxygenation and ventilation indexes (P3), and 48.9% always analyzed the choice of ventilator based on the patient’s specific condition (P8) (Table S2).
Responses to the burnout scale showed that 37.7% always care about whether their work makes a contribution (M9) and 35.4% never doubt the significance of the work they do (M8). 35.6% believed that they were very good at what they did on a daily basis (M12) and 35.0% were always very happy when they accomplished something at their work (M13). However, it is worth noting that also 35.0% occasionally feel that the whole day’s work is really stressful for them (M4), and 34.4% occasionally feel that their work makes them feel physically and mentally exhausted (M1) (Table S3).
Correlation analysis showed that knowledge (r = 0.252, P<0.001) and attitude (r = 0.235, P<0.001) were positively correlated with practice, while attitude (r = -0.289, P<0.001) and practice (r = -0.206, P<0.001) were negatively correlated with MBI-GS Scale score (Table 3).
Table 3.
Correlation analysis of KAP scores and burnout (MBI-GS)
| Knowledge | Attitude | Practice | MBI-GS Scale | |
|---|---|---|---|---|
| Knowledge | 1.000 | 0.086(P = 0.051) | 0.252(P<0.001) | 0.010(P = 0.817) |
| Attitude | 0.086(P = 0.051) | 1.000 | 0.235(P<0.001) | -0.289(P<0.001) |
| Practice | 0.252(P<0.001) | 0.235(P<0.001) | 1.000 | -0.206(P<0.001) |
| MBI-GS Scale | 0.010(P = 0.817) | -0.289(P<0.001) | -0.206(P<0.001) | 1.000 |
Legend: KAP = Knowledge, Attitude, Practice; MBI-GS = Maslach Burnout Inventory-General Survey
Spearman’s rank correlation coefficients are presented with corresponding p-values in parentheses
Multivariate logistic regression showed that lower than 20 of knowledge score (OR = 0.441, 95% CI: [0.297, 0.657], P < 0.001), lower than 26 of attitude score (OR = 0.493, 95% CI: [0.335, 0.724], P < 0.001), lower than 40 of MBI-GS Scale score (OR = 0.539, 95% CI: [0.364, 0.796], P = 0.002), aged 40 years and above (OR = 0.470, 95% CI: [0.264, 0.837], P = 0.010), being nurse (OR = 0.627, 95% CI: [0.424, 0.928], P = 0.020), and no training in respiratory support in the last six months (OR = 0.590, 95% CI: [0.403, 0.866], P = 0.007) were independently associated with practice (Table 4).
Table 4.
Univariable and multivariable logistic regression with practice as the dependent variable
| Cutoff value: ≥38 /<38 | Univariable | Multivariable (P<0.1) | |||
|---|---|---|---|---|---|
| No. | OR(95%CI) | P | OR(95%CI) | P | |
| Knowledge score | |||||
| High (≥ 20) | 197/336 | ref. | ref. | ||
| Low (<20) | 66/181 | 0.405(0.279, 0.588) | <0.001 | 0.441(0.297, 0.657) | <0.001 |
| Attitude score | |||||
| High (≥ 26) | 176/293 | ref. | ref. | ||
| Low (<26) | 87/224 | 0.422(0.296, 0.603) | <0.001 | 0.493(0.335, 0.724) | <0.001 |
| MBI-GS Scale score | |||||
| High (≥ 40) | 116/267 | 0.538(0.380–0.763) | 0.539(0.364–0.796) | ||
| Low (<40) | 147/250 | ref. | 0.001 | ref. | 0.002 |
| Age | |||||
| Below 30 years | 96/180 | ref. | ref. | ||
| 30–39 years | 133/245 | 1.039(0.706, 1.528) | 0.846 | 0.999(0.661, 1.510) | 0.996 |
| 40 years and above | 34/92 | 0.513(0.307, 0.858) | 0.011 | 0.470(0.264, 0.837) | 0.010 |
| Gender | |||||
| Male | 99/189 | ref. | |||
| Female | 164/328 | 0.909(0.635, 1.301) | 0.602 | ||
| Marital status | |||||
| Married | 193/374 | ref. | |||
| Other | 70/143 | 0.899(0.612, 1.322) | 0.589 | ||
| Education | |||||
| College | 57/139 | ref. | |||
| Bachelor’s degree | 188/346 | 1.712(1.149, 2.550) | 0.008 | ||
| Master’s degree and above | 18/32 | 1.850(0.851, 4.018) | 0.120 | ||
| Professional title | |||||
| No title | 18/34 | ref. | |||
| Junior | 118/239 | 0.867(0.422, 1.780) | 0.697 | ||
| Intermediate | 112/209 | 1.026(0.496, 2.122) | 0.944 | ||
| Senior | 15/35 | 0.667(0.258, 1.723) | 0.403 | ||
| Nature of institution | |||||
| Public tertiary | 175/326 | ref. | |||
| Public secondary | 68/154 | 0.682(0.464, 1.003) | 0.052 | ||
| Public primary | 10/19 | 0.959(0.380, 2.421) | 0.929 | ||
| Private hospital | 10/18 | 1.079(0.415, 2.802) | 0.877 | ||
| Years of work experience | |||||
| Less than 10 years | 145/269 | ref. | |||
| 10–19 years | 91/183 | 0.846(0.581, 1.232) | 0.383 | ||
| 20 years and above | 27/65 | 0.608(0.351, 1.052) | 0.075 | ||
| Position | |||||
| Physician | 128/233 | ref. | ref. | ||
| Nurse | 135/284 | 0.743(0.525, 1.052) | 0.094 | 0.627(0.424, 0.928) | 0.020 |
| Department/Ward | |||||
| Emergency Department | 132/261 | ref. | |||
| Respiratory Department | 36/76 | 0.880(0.527, 1.467) | 0.623 | ||
| Cardiology Department | 48/100 | 0.902(0.569, 1.431) | 0.662 | ||
| Intensive Care Unit | 47/80 | 1.392(0.838, 2.311) | 0.201 | ||
| Frequency of Respiratory Support for Patients | |||||
| No contact | 35/78 | ref. | |||
| 0–20% | 110/211 | 1.338(0.794, 2.254) | 0.274 | ||
| 21–50% | 44/88 | 1.229(0.667, 2.264) | 0.509 | ||
| More than 50% | 74/140 | 1.377(0.790, 2.402) | 0.259 | ||
| Respiratory Support Related Training in the Past Six Months | |||||
| Yes | 179/316 | ref. | ref. | ||
| No | 84/201 | 0.549(0.384, 0.786) | 0.001 | 0.590(0.403, 0.866) | 0.007 |
Legend: OR = Odds Ratio; CI = Confidence Interval; KAP = Knowledge, Attitude, Practice
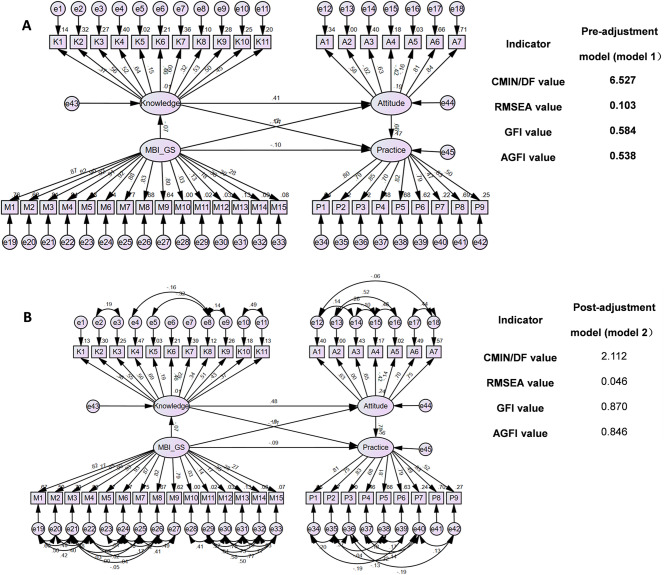
After adjustment, the fit Indices reached the target interval, showing that an ideal model was achieved (Fig. 1, from model 1 to model 2). The SEM results show that knowledge directly affected attitude (β = 0.475, P = 0.010) and attitude directly affected practice (β = 0.775, P = 0.010). Concurrently, knowledge has an indirect effect on practice through attitude (β = 0.368, P = 0.010), and the MBI-GS Scale also has an indirect effect on practice (β = -0.099, P = 0.037) (Table 5; Fig. 1).
Fig. 1.
The Structural Equation Model (SEM) Before and After Model Adjustment; (A) Before Model Adjustment; (B) After Model Adjustment. Rectangle shows observed variables, ellipses indicate potential variables, and circles represent residual terms
Table 5.
Bootstrap analysis of mediating effect significance test for the final mode
| Pre-adjustment model | Standardized direct effects | P | 95%CI | Standardized indirect effects | P | 95%CI | ||
|---|---|---|---|---|---|---|---|---|
| LLCI | ULCI | LLCI | ULCI | |||||
| K-A | 0.410 | 0.010 | 0.244 | 0.535 | / | / | / | / |
| K-P | 0.008 | 0.980 | -0.116 | 0.111 | 0.270 | 0.010 | 0.153 | 0.383 |
| M-K | -0.073 | 0.313 | -0.213 | -0.067 | / | / | / | / |
| A-P | 0.660 | 0.010 | 0.558 | 0.787 | / | / | / | / |
| M-A | -0.120 | 0.032 | -0.232 | -0.015 | -0.030 | 0.240 | -0.097 | 0.023 |
| M-P | -0.104 | 0.090 | -0.200 | 0.006 | -0.100 | 0.018 | -0.169 | -0.024 |
| Post-adjustment model | Standardized direct effects | P | 95%CI | Standardized indirect effects | P | 95%CI | ||
| LLCI | ULCI | LLCI | ULCI | |||||
| K-A | 0.475 | 0.010 | 0.265 | 0.622 | / | / | / | / |
| K-P | -0.109 | 0.162 | -0.314 | 0.027 | 0.368 | 0.010 | 0.185 | 0.575 |
| M-K | -0.073 | 0.351 | -0.227 | 0.064 | / | / | / | / |
| A-P | 0.775 | 0.010 | 0.656 | 0.963 | / | / | / | / |
| M-A | -0.103 | 0.065 | -0.223 | 0.005 | -0.035 | 0.352 | -0.123 | 0.024 |
| M-P | -0.092 | 0.204 | -0.198 | 0.042 | -0.099 | 0.037 | -0.194 | -0.012 |
Legend: LLCI = Lower Limit of the Confidence Interval; ULCI = Upper Limit of the Confidence Interval; K = Knowledge; A = Attitude; P = Practice; M = Maslach Burnout Inventory-General Survey
Discussion
Key findings and implications
Healthcare professionals demonstrate sufficient knowledge, positive attitudes, and proactive practices regarding respiratory support. Given the observed correlations and associations, interventions targeting continuous education, particularly for nurses and highly educated, high stress environment professionals, alongside addressing burnout through targeted interventions, could further enhance the implementation of personalized respiratory support in clinical settings.
The association between higher educational attainment and better knowledge, more positive attitudes, and enhanced practices, however increased burnout levels among healthcare professionals in personalized respiratory support, reveals a multifaceted dynamic within professional development and workplace stressors [22, 23]. Professionals with advanced degrees often exhibit a deeper understanding of theoretical concepts and possess advanced skills pertinent to respiratory care, fostering positive attitudes and proactive engagement in their practice. However, the pursuit of higher education may entail additional academic and professional responsibilities, leading to heightened workload and stress levels [24]. Additionally, individuals in roles requiring advanced degrees may face greater expectations for leadership, decision-making, and research, intensifying job-related pressures [25].
Descriptive analysis showed that healthcare professionals more frequently exposed to respiratory support reported higher burnout scores. This aligns with previous research indicating that prolonged exposure to workplace stressors can lead to increased burnout. Furthermore, years of work experience exhibited a negative correlation with knowledge and burnout, indicating a potential decline in competencies and increased susceptibility to burnout over time, which resonates with the findings of previous study [26]. Bivariate analysis revealed differences in attitudes and practices between physicians and nurses, with physicians showing higher median scores in both domains. While these differences do not necessarily imply superiority, they may reflect the distinct clinical responsibilities and decision-making roles associated with each profession. This observation highlights the importance of understanding profession-specific needs when designing interventions aimed at optimizing respiratory support practices and addressing burnout. Further subgroup analysis by profession may help tailor strategies more effectively.
Moreover, the institutional setting was found to significantly influence knowledge, attitudes, and burnout levels, with professionals in public tertiary institutions scoring higher across these domains compared to those in other settings. This disparity may stem from differences in organizational culture, resource availability, and institutional support systems. Public tertiary institutions often possess more advanced medical equipment, robust training opportunities, and standardized clinical protocols, which not only enhance knowledge acquisition but also foster positive attitudes and proactive practices. In contrast, private or lower-tier institutions may face resource limitations, higher workloads, and less access to formal training, potentially contributing to higher burnout levels and suboptimal clinical practices. Furthermore, the organizational culture in tertiary institutions may prioritize evidence-based practices and provide structured mentorship programs, which can mitigate burnout by promoting collaboration and professional development. Addressing these institutional disparities by ensuring equitable resource allocation and providing tailored support could help optimize KAP and reduce burnout among healthcare professionals in different settings. This could be attributed to differences in resources, organizational culture, and support systems available in various types of healthcare institutions.
Correlation analysis and SEM results offer insights into the relationships among healthcare professionals’ knowledge, attitudes, practices, and burnout levels regarding personalized respiratory support. Positive correlations between knowledge, attitudes, and practices, alongside negative correlations between attitudes/practices and burnout, reflect the influence of various individual and organizational factors. Professionals with a stronger understanding of personalized respiratory support are more likely to have positive attitudes, leading to more proactive practices. Conversely, healthcare experiencing burnout may exhibit negative attitudes, such as emotional exhaustion and reduced personal accomplishment, which can lead to diminished engagement in their work and compromised clinical practices [27, 28].
Comparison with existing literature
Our study findings are consistent with previous research, showing that even lower levels of burnout negatively impact healthcare professionals’ performance. The SEM analysis confirms the correlation between knowledge, attitudes, and practices (KAP), with attitudes mediating the link between knowledge and practice. This highlights the need to foster positive attitudes to enhance the implementation of evidence-based practices in clinical settings [29, 30].Burnout also showed an indirect effect on practice, impacting KAP. Emotional exhaustion from burnout can weaken attitudes, leading to reduced engagement with best practices and lower care quality. This aligns with studies linking burnout to diminished performance and patient outcomes [31, 32]. Addressing burnout is crucial to improving both professional well-being and clinical practices [33, 34].
Practical applications
In examining healthcare professionals’ understanding, attitudes, and practices regarding respiratory support, it’s clear that while fundamental concepts such as oxygen therapy and non-invasive ventilation are well understood, gaps remain in areas like the appropriate use of mechanical ventilation in specific scenarios. To bridge these knowledge gaps, targeted educational initiatives should be implemented, focusing on case-based learning and scenario simulations. These sessions could involve multidisciplinary discussions, drawing insights from real-life experiences and clinical guidelines to enhance professionals’ confidence and competence in decision-making regarding respiratory support interventions [35, 36]. Attitudes towards patient-centered care are generally positive, but challenges persist in navigating clinical guidelines. Healthcare organizations should foster environments that promote shared decision-making and provide continuous access to updated guidelines and decision-support tools [37–39]. In translating knowledge and attitudes into practice, it is essential to align with evidence-based recommendations. Gaps in emergency airway management during urgent situations suggest the need for enhanced training through simulation-based learning and crisis resource management, which will improve both practitioner confidence and patient outcomes [40–43]. Tailored interventions should also consider the distinct needs of different professional roles. For instance, nurses, who often report higher burnout levels due to frequent patient interactions, may benefit from resilience training and peer support programs. On the other hand, physicians could benefit from leadership training and decision-support tools to alleviate the cognitive load associated with high-stakes clinical decisions. Similarly, work environments with limited resources, such as private or lower-tier hospitals, may require additional investment in training opportunities and mental health support to address these disparities effectively.
The prevalence of burnout symptoms among healthcare professionals underscores the urgent need for proactive strategies to support workforce well-being. However, existing literature highlights the significant burden of burnout among healthcare professionals, which warrants attention [44, 45]. This study emphasizes that even low levels of burnout can still negatively affect healthcare professionals’ practices and clinical performance, underscoring the importance of addressing burnout at all levels. Chronic stress and exhaustion not only jeopardize individual health but also compromise patient care quality and safety [46, 47]. To mitigate burnout, organizations should adopt a holistic approach that addresses both individual and systemic factors contributing to workplace stress. Implementing regular staff well-being assessments and providing access to confidential counseling services can empower professionals to prioritize self-care and seek support when needed [48, 49]. Moreover, fostering a culture of appreciation and recognition, alongside workload optimization strategies and opportunities for professional development, can cultivate a resilient workforce capable of delivering high-quality care while maintaining personal well-being [50–52].
Study limitations and future directions
This study had limitations. Firstly, the study’s cross-sectional design restricts the establishment of causal relationships between variables, limiting the ability to determine temporal sequences or causality. Secondly, the study was conducted at a single area, potentially limiting the generalizability of findings to broader healthcare settings. Thirdly, the use of convenience sampling and online questionnaire dissemination introduced challenges in calculating an accurate response rate, as the exact number of potential participants reached through this method was not recorded. Lastly, reliance on self-reported measures through questionnaires may introduce response bias or social desirability bias, potentially influencing the accuracy and reliability of the collected data.
Future research should prioritize comparative studies across diverse healthcare settings, including urban and rural hospitals, as well as public and private institutions, to evaluate the generalizability of findings. Such studies could explore how variations in organizational culture, resource allocation, and professional training impact KAP and burnout levels. Additionally, longitudinal studies are needed to establish causal relationships between burnout, KAP, and clinical outcomes. Expanding sample sizes and employing stratified sampling methods could also improve the robustness and external validity of future investigations. These efforts will help refine targeted interventions and promote evidence-based strategies to support healthcare professionals in diverse contexts.
Conclusions
In conclusion, healthcare professionals exhibited satisfactory levels of knowledge, positive attitudes, and proactive practices regarding the application of respiratory support. Although a cutoff score of 50 is commonly used to define burnout, the imbalance between groups in our sample limited the feasibility of applying this threshold in regression analysis. Nevertheless, higher burnout scores were associated with poorer attitudes and practices, suggesting that psychological burden may affect clinical performance even in the absence of clinically defined burnout. To further enhance the quality of care and address burnout risks, targeted interventions, including regular training sessions and mental health support, should be implemented. These efforts should focus particularly on older healthcare professionals and nurses, ensuring sustained competence, reducing burnout, and promoting overall well-being in clinical practice.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- SOT
standard oxygen therapy
- NIRS
Noninvasive respiratory support
- HFOT
high-flow oxygen therapy
- CPAP
continuous positive airway pressure
- NIV
noninvasive ventilation
- AHRF
acute hypoxemic respiratory failure
- ARDS
acute respiratory distress syndrome
- KAP
Knowledge-Attitude-Practice
- MBI-GS
Maslach Burnout Inventory General Survey
- SEM
structural equation modeling
Author contributions
Tao Cui and Jie Lu carried out the studies, participated in collecting data, and drafted the manuscript. Bin Chen and Chuangwei Yu performed the statistical analysis and participated in its design. Yunli Hu and Chuanfei Bao, Shuguang Zhao participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information file.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Taihe County People’s Hospital, and informed consent was obtained from the participants for the study through an online questionnaire. I confirm that all methods were performed in accordance with the relevant guidelines. All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tao Cui and Jie Lui contributed equally to this work.
References
- 1.Bjorklund AR, Odongkara Mpora B, Steiner ME, Fischer G, Davey CS, Slusher TM. Use of a modified bubble continuous positive airway pressure (bCPAP) device for children in respiratory distress in low- and middle-income countries: a safety study. Paediatr Int Child Health. 2019;39:160–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grieco DL, Maggiore SM, Roca O, Spinelli E, Patel BK, Thille AW, et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med. 2021;47:851–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munshi L, Mancebo J, Brochard LJ. Noninvasive respiratory support for adults with acute respiratory failure. N Engl J Med. 2022;387:1688–98. [DOI] [PubMed] [Google Scholar]
- 4.Popowicz P, Leonard K. Noninvasive ventilation and oxygenation strategies. Surg Clin North Am. 2022;102:149–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Esperanza JA, Sarlabous L, de Haro C, Magrans R, Lopez-Aguilar J, Blanch L. Monitoring asynchrony during invasive mechanical ventilation. Respir Care. 2020;65:847–69. [DOI] [PubMed] [Google Scholar]
- 6.Walter JM, Corbridge TC, Singer BD. Invasive mechanical ventilation. South Med J. 2018;111:746–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017;195:438–42. [DOI] [PubMed] [Google Scholar]
- 8.Szafran JC, Patel BK. Invasive mechanical ventilation. Crit Care Clin. 2024;40:255–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cutuli SL, Grieco DL, Michi T, Cesarano M, Rosà T, Pintaudi G et al. Personalized respiratory support in ARDS: A Physiology-to-Bedside review. J Clin Med. 2023;12. [DOI] [PMC free article] [PubMed]
- 10.Colville GA, Smith JG, Brierley J, Citron K, Nguru NM, Shaunak PD, et al. Coping with staff burnout and Work-Related posttraumatic stress in intensive care. Pediatr Crit Care Med. 2017;18:e267–73. [DOI] [PubMed] [Google Scholar]
- 11.Tan J, Luo L, Zhang M, Chen H, Zhang D, Dong C, et al. A Chinese and Western medication adherence scale in patients with chronic kidney disease. Patient Prefer Adherence. 2019;13:1487–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li L, Zhang J, Qiao Q, Wu L, Chen L. Development, reliability, and validity of theKnowledge-Attitude-Practice questionnaire of foreigners on traditional Chinese medicine treatment. Evid Based Complement Alternat Med. 2020;2020:8527320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khalid A, Haque S, Alvi S, Ferdous M, Genereux O, Chowdhury N, et al. Promoting health literacy about cancer screening among Muslim immigrants in canada: perspectives of imams on the role they can play in community. J Prim Care Community Health. 2022;13:21501319211063051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angeli MC, Rausa F, Satta E, Salvatelli ML, Pollara I, Rapina C, et al. Underestimated sleep breathing disorders in a cohort of patients admitted to post-COVID-19 follow-up program: A single center experience. J Neurol Sci. 2021;429:118656. [Google Scholar]
- 15.Cabrera-Aguilera I, Benito B, Tajes M, Farré R, Gozal D, Almendros I, et al. Chronic sleep fragmentation mimicking sleep apnea does not worsen Left-Ventricular function in healthy and heart failure mice. Front Neurol. 2019;10:1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chinese Thoracic Society COPD Working Group. Expert consensus on the diagnosis and treatment of acute exacerbation of chronic obstructive pulmonary disease in China (2017 revised edition) [J]. Chin J Tuberculosis Respiratory Dis. 2017;40(4):241–55. 10.3760/cma.j.issn.1001-0939.2017.04.001. [Google Scholar]
- 17.Chinese Society of Critical Care Medicine, Chinese Medical Association. Expert consensus on the clinical application of high-flow nasal cannula oxygen therapy in adults (2019) [J]. Chin Crit Care Med. 2019;31(4):391–8. 10.3760/cma.j.issn.2095-4352.2019.04.001. [Google Scholar]
- 18.Extracorporeal Life Support Committee of the Chinese Medical Doctor Association, Chinese Society of Critical Care Medicine, Chinese Medical Association. Expert consensus on clinical practice of extracorporeal membrane oxygenation for adult respiratory failure [J]. Chin Crit Care Med. 2020;32(10):1169–81. 10.3760/cma.j.cn121430-20200810-00578. [Google Scholar]
- 19.Lee F, Suryohusodo AA. Knowledge, attitude, and practice assessment toward COVID-19 among communities in East Nusa Tenggara, Indonesia: A cross-sectional study. Front Public Health. 2022;10:957630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maslach C, Jackson SEJJ. The measurement of experienced burnout. 1981;2:99–113.
- 21.Li C, Shi K. The influence of distributive equity and procedural equity on job burnout. Acta psychologica sinica.
- 22.Royce TJ, Davenport KT, Dahle JM. A burnout reduction and wellness strategy: personal financial health for the medical trainee and early career radiation oncologist. Pract Radiat Oncol. 2019;9:231–8. [DOI] [PubMed] [Google Scholar]
- 23.Batanda I. Prevalence of burnout among healthcare professionals: a survey at fort portal regional referral hospital. Npj Mental Health Res. 2024;3:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anandarajah AP, Quill TE, Privitera MR. Adopting the quadruple aim: the university of Rochester medical center experience: moving from physician burnout to physician resilience. Am J Med. 2018;131:979–86. [DOI] [PubMed] [Google Scholar]
- 25.Zhang M, Li S, Han D, Wu Y, Zhao J, Liao H, et al. Association of job characteristics and burnout of healthcare workers in different positions in rural China: A Cross-Sectional study. Int J Public Health. 2023;68:1605966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guteta M. Factors affecting cardiopulmonary resuscitation practice among nurses in Mizan Tepi university teaching hospital, Tepi general hospital, and Gebretsadik Shawo hospital, Southwest Ethiopia. Open Access Emerg Med. 2022;14:165–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koutsimani P, Montgomery A. Burnout and cognitive functioning: are we underestimating the role of visuospatial functions?? Front Psychiatry. 2022;13:775606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lal S, Khan E. Pseudo-teams in healthcare: the perils of impersonating a cohesive unit. Pak J Med Sci. 2023;39:1194–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jun J, Ojemeni MM, Kalamani R, Tong J, Crecelius ML. Relationship between nurse burnout, patient and organizational outcomes: systematic review. Int J Nurs Stud. 2021;119:103933. [DOI] [PubMed] [Google Scholar]
- 30.Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N, Gómez-Urquiza JL, Monsalve-Reyes C et al. Cañadas-De la Fuente GA,. Prevalence, Risk Factors and Burnout Levels in Intensive Care Unit Nurses: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2021;18. [DOI] [PMC free article] [PubMed]
- 31.Eo SK, Kim C, Park KH, Eo EK. The effectiveness of emotion-focused Art therapy on the resilience and self-image of emergency physicians. World J Emerg Med. 2022;13:479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seo JH, Bae HO, Kim BJ, Huh S, Ahn YJ, Jung SS, et al. Burnout of faculty members of medical schools in Korea. J Korean Med Sci. 2022;37:e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hwang E, Kim J. Factors affecting academic burnout of nursing students according to clinical practice experience. BMC Med Educ. 2022;22:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagasaki K, Seo E, Maeno T, Kobayashi H. Diagnostic accuracy of the Single-item measure of burnout (Japanese version) for identifying medical resident burnout. J Gen Fam Med. 2022;23:241–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernando SM, Tran A, Sadeghirad B, Burns KEA, Fan E, Brodie D, et al. Noninvasive respiratory support following extubation in critically ill adults: a systematic review and network meta-analysis. Intensive Care Med. 2022;48:137–47. [DOI] [PubMed] [Google Scholar]
- 36.Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An official American thoracic society and European respiratory society technical statement. Am J Respir Crit Care Med. 2019;200:e70–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huppert LA, Matthay MA, Ware LB. Pathogenesis of acute respiratory distress syndrome. Semin Respir Crit Care Med. 2019;40:31–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meyer NJ, Gattinoni L, Calfee CS. Acute respiratory distress syndrome. Lancet. 2021;398:622–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Munshi L, Brodie D, Fan E. Extracorporeal support for acute respiratory distress syndrome in adults. NEJM Evid. 2022;1:EVIDra2200128. [DOI] [PubMed] [Google Scholar]
- 40.Karamchandani K, Wheelwright J, Yang AL, Westphal ND, Khanna AK, Myatra SN. Emergency airway management outside the operating room: current evidence and management strategies. Anesth Analg. 2021;133:648–62. [DOI] [PubMed] [Google Scholar]
- 41.Myatra SN, Divatia JV, Brewster DJ. The physiologically difficult airway: an emerging concept. Curr Opin Anaesthesiol. 2022;35:115–21. [DOI] [PubMed] [Google Scholar]
- 42.Inglis R, Ayebale E, Schultz MJ. Optimizing respiratory management in resource-limited settings. Curr Opin Crit Care. 2019;25:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tola DH, Rojo A, Morgan B. Basic airway management for the professional nurse. Nurs Clin North Am. 2021;56:379–88. [DOI] [PubMed] [Google Scholar]
- 44.Al-Mugheed K, Bayraktar N, Al-Bsheish M, AlSyouf A, Jarrar M, AlBaker W et al. Patient safety attitudes among Doctors and nurses: associations with workload, adverse events, experience. Healthcare (Basel). 2022;10. [DOI] [PMC free article] [PubMed]
- 45.Gu W, Liu Y, Lu Z, Wang J, Che X, Xu Y, et al. Associated factors of burnout among Chinese vaccination staff during COVID-19 epidemic: A cross-sectional study. Front Public Health. 2023;11:1086889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Al Houri HN, Jomaa S, Arrouk DMN, Nassif T, Al Ata Allah MJ, Al Houri AN, et al. The prevalence of stress among medical students in Syria and its association with social support: a cross-sectional study. BMC Psychiatry. 2023;23:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hong Y, Zhang L, Liu N, Xu X, Liu D, Tu J. The central nervous mechanism of Stress-Promoting Cancer progression. Int J Mol Sci. 2022;23. [DOI] [PMC free article] [PubMed]
- 48.Cohen C, Pignata S, Bezak E, Tie M, Childs J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: a systematic review. BMJ Open. 2023;13:e071203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lall MD, Gaeta TJ, Chung AS, Chinai SA, Garg M, Husain A, et al. Assessment of physician Well-being, part two: beyond burnout. West J Emerg Med. 2019;20:291–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lauden SM, Wilson PM, Faust MM, Webber S, Schwartz A, Mahan JD, et al. Global health experiences, Well-Being, and burnout: findings from a National longitudinal study. Acad Pediatr. 2020;20:1192–7. [DOI] [PubMed] [Google Scholar]
- 51.Taylor CE, Scott EJ, Owen K. Physical activity, burnout and quality of life in medical students: A systematic review. Clin Teach. 2022;19:e13525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.West CP, Dyrbye LN, Sinsky C, Trockel M, Tutty M, Nedelec L, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open. 2020;3:e209385. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information file.