Abstract
Introduction:
The International Academy of Cytology (IAC) has developed a comprehensive and systematic method that defines five categories for reporting breast fine needle aspiration cytology. These categories stratify breast lesions by their risk of malignancy, providing guidance on management for each category. The aim of the study is to analyze the diagnostic utility of the IAC Yokohama system in breast cytology reporting with histopathological correlation.
Methods:
This was a cross-sectional observational study. The study included 55 patients with clinically suspected breast lumps who underwent Fine Needle Aspiration Cytology for provisional diagnosis, which was later confirmed by corresponding excisional biopsy and histopathology. The collected data following Fine Needle Aspiration Cytology (FNAC) and histopathology were entered into Microsoft Office Excel software 13. Data analysis was performed using SPSS 16. For diagnostic measurement, sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy were calculated. The probability of significance was set at the 5% level.
Results:
Among 55 cases of breast lesions on cytopathology as per the International Academy of Cytology Yokohama System, none of the cases were categorized as Insufficient (C1). Twenty-five cases (45.5%) were categorized as C2 (benign), 5 cases (9.1%) were categorized as C3 (atypia, probably benign), 4 cases (7.3%) were categorized as C4 (suspicious for malignancy), and 21 cases (38.3%) were categorized as C5 (malignant). The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for cytopathology compared with histopathology were 86.21% (95% CI: 73.76%–98.66%), 100% (95% CI: 100%–100%), 100% (95% CI: 100%–100%), 86.67% (95% CI: 74.29%–99.05%), and 92.7% (95% CI: 85.54%–99.93%), respectively.
Conclusion:
The IAC Yokohama system for reporting breast fine needle aspiration cytopathology effectively stratifies patients into five categories and has high sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy with regard to the gold standard histopathology.
Keywords: breast lesion, fine needle aspiration cytology, histopathology
Introduction
Fine Needle Aspiration Cytology (FNAC) is a rapid, cost-effective, atraumatic, and minimally invasive technique for disease site diagnosis[1]. Breast FNAC is a very accurate and common method of distinguishing breast lesions as benign or malignant before surgery with minimal complications, high sensitivity (90–95%), and a high positive predictive value (100%)[2]. Breast cancer survival rates have been connected to early detection programs. Lower survival rates have been attributed to an advanced stage of disease at the time of presentation, a lack of effective diagnostic and treatment facilities, and limited access to professional care. Clinical examination alone remains insufficient for the distinction of breast lesions as benign or malignant, therefore FNAC remains the first line of investigation in a country with limited resources and large, isolated, rural populations on the periphery with limited access to centralized health care[3].
HIGHLIGHTS
IAC Yokohama system of breast FNAC is better for reporting breast lesions as each diagnostic category conveys a specific risk of malignancy, which helps in planning the therapeutic approach for patients.
55 FNA samples from breast lumps, along with their corresponding histopathology samples, were enrolled in our study.
All the 55 samples were categorized according to the IAC Yokohama system of breast FNAC; Out of 55 cases 25 cases were categorized as C2 (Benign), 5 cases as C3 (Atypia, probably benign), 4 cases as C4 (suspicious of malignancy), and 21 cases as C5 (malignant). None of the cases were insufficient (C1).
The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for cytology (IAC) compared with histopathology were 86.21%, 100%, 100%, 86.67%, and 92.7%, respectively.
The International Academy of Cytology (IAC) Yokohama system was proposed to standardize breast cytology reporting, enhance the reproducibility of reports, and create uniformity in its assessment by clinicians. The IAC has developed a comprehensive and systematic method that defines five categories for reporting breast cytology. These categories stratify breast lesions by their risk of malignancy and provide guidance for management within each category[2]. IAC employs a five-stage stratification of breast lesions as follows: Code 1 – Insufficient material; Code 2 – Benign; Code 3 – Atypical, probably benign; Code 4 – Suspicious, probably in situ or invasive carcinoma; and Code 5 – Malignant[4]. Although the majority of breast lesions are benign, it can be difficult to tell whether a proliferative lesion in the atypia category is benign or malignant. In these cases, the Yokohama guidelines become helpful.
The aim of the study is to analyze the diagnostic utility of the IAC Yokohama system in breast cytology reporting with histopathological correlation. The comparison between cytology reports using IAC and histological reports helps in evaluating the IAC’s effectiveness in identifying the aggressiveness of tumors and the possibility of its use as a prognostic factor for better management of patients and guidance for further neo-adjuvant therapy.
Methods
This was a cross-sectional observational study carried out in Nepal. Ethical approval from the Institutional Review Committee was obtained under the number “IRC/1944/020.” This study included 55 patients with clinically suspected breast lumps who underwent FNAC for provisional diagnosis, later confirmed by corresponding excisional biopsy and histopathology. All patients presenting with breast lumps whose FNAC was performed and whose histopathological samples were available after FNAC were included in this study for a period of one year, from February 2021 to February 2022. Patients who were unwilling to participate and who did not consent to the study were not included. Written informed consent was obtained from the participants. No control groups were assigned, and samples were selected following a simple random sampling method using a random number table.
The study considered a 95% confidence interval and 80% power to estimate the sample size
In the study conducted by Panwar, et al, concordant rate of histopathology report and FNAC grading was 89%. Using one proportion formula:
n = Z²pq/d2, where Z = 1.96 at 95% confidence interval, p = 89%, q = 11%. Now d = 10% of p = 8.9 at 80% power.
Putting the value in equation:
n = (1.96 × 1.96 × 89 × 11)/(8.9 × 8.9) = 47.46–48 to reduce various bias.
Now, when 10% was added to the calculated sample size, the number became 53 samples. To further strengthen the study, 55 samples were thus used.
Following fine needle aspiration, two smears, made by gently pressing one clean slide over the slide with the specimen material, were air-dried and stained with Giemsa stain. Another two smears were immediately fixed with Papanicolaou stain. Light microscopy technique was used to examine the specimens, and breast lesions on cytopathology (FNAC) were categorized as per the IAC Yokohama System. Either lumpectomy or mastectomy was performed on patients as clinically indicated. Later, for histopathological examination, grossing of specimens was done. Hematoxylin and eosin staining was performed, and the slides were examined with a Nikon Eclipse E600 microscope under 4×, 10×, and 40× objective lenses. To eliminate inter-observer bias, a multi-view microscope was used to simultaneously visualize the slides, ensuring that all the pathologists viewed the same area of the slide with the same features of the specimen before reaching a final diagnosis. The collected data was entered into Microsoft Office Excel software 13. Data analysis was conducted by using SPSS 16 (Statistical Package for Social Sciences).
For descriptive statistics: percentage (%), mean, and standard deviation were calculated, along with graphical and tabular presentations. For inferential statistics: chi-square test and proportion test were used to find the significant association between the variables. For diagnostic measurement: sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy were calculated. The probability of significance was set at the 5% level.
The methods are stated in accordance with the STROCSS 2021 guidelines[5].
Results
Among 55 cases of breast lesions on cytopathology as per the IAC Yokohama System, none of the cases were insufficient (C1), 25 cases (45.5%) were categorized as C2 (benign), 5 cases (9.1%) were categorized as C3 (atypia probably benign), 4 cases (7.3%) were categorized as C4 (suspicious for malignancy), and 21 cases (38.3%) as C5 (malignant). Therefore, 30 cases (54.5%) were benign, and 25 cases (45.5%) were malignant on FNAC (Table 1).
Table 1.
Frequency of breast lesion on cytopathology (FNAC) categorized as per IAC Yokohama system
| Diagnosis | Frequency | Percentage |
|---|---|---|
| C1; insufficient | 0 | 0.0% |
| C2; benign | 25 | 45.5% |
| C3; atypia probably benign | 5 | 9.1% |
| C4; suspicious for malignancy | 4 | 7.3% |
| C5; malignant | 21 | 32.8% |
| Total | 55 | 100.0% |
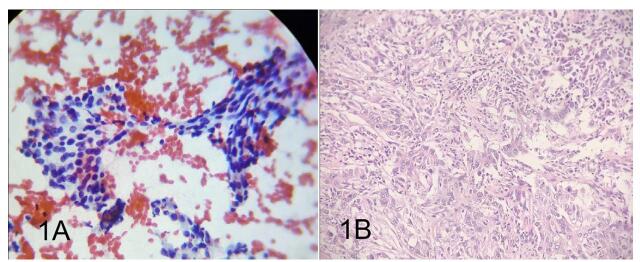
On final histopathology, 26 cases (47.3%) were benign, and 29 cases (52.7%) were malignant. Among the 26 cases of benign breast lesion diagnoses on final histopathology, 17 cases (65.38%) were fibroadenoma, followed by fibrocystic change with intraductal papilloma, fibrocystic changes, and breast abscess, each constituting one case (3.84%). Among the 29 cases of malignant breast lesion diagnoses on final histopathology, 25 cases (86.2%) were invasive carcinoma, no special type. The remaining four cases were invasive lobular carcinoma, invasive papillary carcinoma, metaplastic and mucinous breast carcinoma which constituted 3.44% (Tables 2, 3, and 4). Out of 30 benign cases on cytopathology, four cases reported as C3 (Atypia, probably benign) were found to be malignant on final histopathology (Fig. 1). Thus, among the 55 cases, in the FNAC diagnosis, the number of cases with true positive, true negative, false positive, and false negative results was 25, 26, 0, and 4, respectively.
Table 2.
Frequency of breast lesion (benign versus malignant) in histopathology
| Final histopathology | Frequency | Percentage |
|---|---|---|
| Benign | 26 | 47.3% |
| Malignant | 29 | 52.7% |
| Total | 55 | 100.0% |
Table 3.
Frequency of spectrum of benign disease on final histopathology
| Diagnosis | Frequency | Percentage |
|---|---|---|
| Breast abscess | 1 | 3.84% |
| Fibrocystic changes with intraductal papilloma | 1 | 3.84% |
| Fibroadenoma | 17 | 65.38% |
| Fibroadenoma with lactational changes | 1 | 3.84% |
| Fibro adenomatoid hyperplasia | 3 | 11.53% |
| Fibrocystic change | 3 | 11.53% |
| Total | 26 | 100.00% |
Table 4.
Frequency of spectrum of malignant disease on final histopathology
| Diagnosis | Frequency | Percentage |
|---|---|---|
| IBC, NOS | 25 | 86.20% |
| Invasive lobular carcinoma | 1 | 3.44% |
| Invasive papillary carcinoma | 1 | 3.44% |
| Metaplastic carcinoma | 1 | 3.44% |
| Mucinous breast carcinoma | 1 | 3.44% |
| Total | 29 | 100.00% |
Figure 1.
Discrepant case in FNAC (IAC) and excisional biopsy. A shows smear from FNAC breast, C3 (pap 40X obj). B shows excisional biopsy IBC, NOS (malignant) (H and E 40X obj).
The sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for cytopathology compared with histopathology was 86.21% (95% CI: 73.76%–98.66%), 100% (95% CI: 100%–100%), 100% (95% CI: 100%–100%), 86.67% (95% CI: 74.29%–99.05%), and 92.7% (95% CI: 85.54%–99.93%), respectively (Table 5).
Table 5.
Cross-tabulation of benign and malignant lesions on cytopathology and histopathology
| Histopathology | |||
|---|---|---|---|
| Benign | Malignant | Total | |
| Benign | 26 | 4 | 30 |
| Malignant | 0 | 25 | 25 |
| Total | 26 | 29 | 55 |
Discussion
The present study reconsiders the diagnostic accuracy of FNAB in diagnosing breast lesions and validates the IAC Yokohama system.
The study includes 55 cases of breast lumps where two procedures, FNAC and final histopathology, were obtained. Final histopathology diagnosis is the gold standard for confirming breast lesions. Final histopathology here refers to excisional biopsy (EB) and mastectomy specimen study. FNAC is an outpatient procedure with minimal complications and very high diagnostic accuracy. Yokohama stratifies breast lesions into five categories and ensures high-quality reporting, which helps in the appropriate management of patients. The upper outer quadrant was the most commonly involved site in our study which was similar to the study by Sundar, et al[6]. All of 55 cases were categorized according to the standardized reporting of breast FNAC as per the IAC Yokohama. In this study, the highest percentage of breast disease was categorized as benign (C2) at 45.5%, followed by the malignant category (C5) at 38.5%. Another common category C3 (Atypia, probably benign) was 9.1%. There were no insufficient cases due to the better skills of the practitioner performing FNAC and the skill of making smears. The insufficient rate was reduced by better initial training with hands-on experience and the use of ultrasound guidance for FNAC.
The most common benign breast disease in our study was fibroadenoma. It was diagnosed in final histopathology in 65.38% of benign breast lesions (17 out of 26). It was followed by a minor percentage of Fibro adenomatoid hyperplasia, fibrocystic change in breast disease, fibrocystic breast disease with intra ductal papilloma, fibrocystic disease with lactational change and breast abscess. These findings were similar to studies by Sundar, et al (30.75%)[6] and Agrawal, et al (58.1%)[7].
The most common malignant breast disease in the study was invasive breast carcinoma, no special type (IBC, NST). It was diagnosed in final histopathology in 52.7% of malignant breast lesions (29 out of 55). A similar result was observed in the study done by Makhija, et al, where out of 102 malignant breast lesions, 82 cases were ductal carcinoma[8]. In a similar study done by Panwar, et al, most of the malignant diseases were ductal carcinoma[9].
In our study, sensitivity, specificity, positive predictive value, negative predictive value, and accuracy for cytopathology in comparison with histopathology were 86.21%, 100%, 100%, 86.67%, and 92.7%, respectively, which is comparable to the study by Chauhan, et al, where sensitivity was 89.66%, specificity was 100%, positive predictive value (PPV) was 100%, negative predictive value (NPV) was 90.2%, and accuracy was 94.69%[10].
In our study, four out of five cases categorized as C3 (atypia probably benign) which turned out to be malignant in final histopathology. This implies that four cases which were supposed to be atypia probably benign, were actually malignant. The risk of malignancy for atypia category varies in the literature from 17.2% to 26.3% and is even higher – 80% in this study. This disparity in results might be due to the small sample size and the smaller number of atypical cases in our study. Additionally, the difference in the risk of malignancy in our study can be attributed to interobserver variability in assigning an atypical category. In our study, invasive breast carcinoma and benign fibrocystic changes with intraductal papilloma were categorized as atypia probably benign (C3) in FNAC, as C3 includes high cellularity, poorly cohesive tissue fragment nuclei with moderate atypia, and the absence of myoepithelial cells.
This study highlights the effectiveness of the IAC Yokohama system in accurately classifying breast lesions, but the study does have certain limitations. First, the small sample size of 55 cases may limit the generalizability of the findings. A larger sample size would strengthen the validation of the system’s predictive value and allow for a more detailed analysis of variability among different breast lesions and their subtypes as classified by the IAC Yokohama System. The restricted population and lower disease prevalence in Nepal led to the smaller sample size and limited study population. Additionally, the research was conducted at a single institution, and differences in FNAC techniques and instruments, staining methods, and observer interpretation across laboratories could affect the reproducibility of the results in other settings. To eliminate inter-observer bias, a multi-view microscope was used to simultaneously visualize the slides so that all the pathologists could view the same area of the slide with the same features of specimen. This further allowed immediate peer-review and the ability for observers to discuss observations in real-time and provide immediate feedback, helping to resolve disagreements or uncertainties before reaching a final diagnosis.
The IAC Yokohama System aids in monitoring the risk of malignancy in patients classified under various IAC categories, allowing pathologists to better identify situations that require additional histopathological confirmation and to provide more robust suggestions to treating surgeons[7]. The reporting system provides an improved structured format for reporting breast lesions by giving comprehensive definitions and descriptions, as well as the risk of malignancy for the standardized five categories.
Conclusion
The IAC Yokohama system demonstrates high diagnostic accuracy for breast lesions, with a sensitivity of 86.21% (95% CI: 73.76–98.66%), specificity and PPV of 100%, NPV of 86.67% (74.29–99.05%), and overall accuracy of 92.7% (85.54–99.93%). These results validate its utility in stratifying lesions and guiding clinical management, particularly in resource-limited settings. However, the study’s relatively small sample size (n = 55) and unicentric design limit its generalizability. Furthermore, the elevated malignancy rate (80%) in the atypia (C3) category may be a reflection of interobserver variability or sampling constraints due to the smaller sample size. Multicenter studies with larger cohorts are essential to confirm reproducibility across diverse populations and refine risk stratification for atypical lesions in the future.
Acknowledgements
The authors would like to acknowledge the Department of Pathology of B.P. Koirala Institute of Health Sciences for all the help and support in making this study possible. The authors would also like to express their warmest thanks to Dr. Paricha Upadhyaya, Professor, Department of Pathology, BPKIHS, Dharan, who made this work possible. Additionally, the authors would like to thank Prof. Dr. Smriti Karki, Dr. Niharika Shah, and Dr. Mona Dahal for their constant support.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 22 April 2025
Contributor Information
Khushbu Sah, Email: drkhushbu2017@gmail.com.
Brinda Kharel, Email: brinda-kharel105@icloud.com.
Nirmal Prasad Sah, Email: drnirmalshah12@gmail.com.
Ethical approval
Ethical approval from the Institutional Review Committee of the B.P. Koirala Institute of Health Sciences (BPKIHS-IRC) was obtained under the number “IRC/1944/020.”
Consent
Written informed consent was obtained from the patient’s parents/legal guardian in their native language for the publication of this case series. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None.
Author contributions
K.S.: conceptualization, supervision, resources, data curation, writing original draft; B.K.: data curation, writing original draft, writing and reviewing; N.S.: writing and reviewing.
Conflicts of interest disclosure
None.
Research registration unique identifying number (UIN)
researchregistry10958. https://researchregistry.knack.com/researchregistry#home/registrationdetails/677a2f038da6bd030b4454d9/.
Guarantor
Khushbu Sah.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data availability statement
Anonymized data will be made available on request. All values are provided in the form of tables within the manuscript.
References
- [1].Lever JV, Trott PA, Webb AJ. Fine needle aspiration cytology. J Clin Pathol 1985;38:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Field AS, Raymond WA, Schmitt FC. The international academy of cytology Yokohama system for reporting breast fine needle aspiration biopsy cytopathology. Acta Cytol 2019;63:255–56. [DOI] [PubMed] [Google Scholar]
- [3].Agnani B, Hemrajani D, Mathur K, et al. Breast cytopathology reporting using the newly proposed IAC Yokohama system: a single institutional retrospective study of the application of the system and utility of breast FNAC. Int J Sci Res 2020;1–3. doi: 10.36106/ijsr/4801280. [DOI] [Google Scholar]
- [4].Field AS, Schmitt F, Vielh P. IAC standardized reporting of breast fine-needle aspiration biopsy cytology. Acta Cytol 2017;61:3–6. [DOI] [PubMed] [Google Scholar]
- [5].Mathew G, Agha R, Albrecht J, et al. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- [6].Sundar PM, Shanmugasundaram S, Nagappan E. The role of the IAC Yokohama system for reporting breast fine needle aspiration biopsy and the ACR breast imaging-reporting and data system in the evaluation of breast lesions. Cytopathology 2022;33:185–95. [DOI] [PubMed] [Google Scholar]
- [7].Agrawal N, Kothari K, Tummidi S, et al. Fine-needle aspiration biopsy cytopathology of breast lesions using the international academy of cytology Yokohama system and rapid on-site evaluation: a single-institute experience. Acta Cytol 2021;65:463–77. [DOI] [PubMed] [Google Scholar]
- [8].Makhija S, Patil S. Cytology of breast-lesions. IP Arch Cytol Histopathol Res 2020;5:81–85. doi: 10.18231/j.achr.2020.016. [DOI] [Google Scholar]
- [9].Panwar H, Ingle P, Santosh T, et al. FNAC of breast lesions with special reference to IAC standardized reporting and comparative study of cytohistological grading of breast carcinoma. J Cytol 2020;37:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chauhan V, Pujani M, Agarwal C, et al. IAC standardized reporting of breast fine-needle aspiration cytology, Yokohama 2016: a critical appraisal over a 2 year period. Breast Dis 2019;38:109–15. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data will be made available on request. All values are provided in the form of tables within the manuscript.