Abstract
Background and Objective
Attrition in the medical training programs not only affects the specialty but also the hospital, the trainee’s career path, and the provision of care to patients. This study aims to determine the trends, annual rates, and reasons of attrition at the University of the Philippines-Philippine General Hospital (UP-PGH) from 2018-2022.
Methods
The study was carried out in two stages. A retrospective review of trainees’ records from the Office of the Deputy Director of Health Operations (ODDHO) and Human Resource Department (HRD) was initially done followed by a survey of the resident training officers (RTOs). Associations between physician and program attributes to attrition were analyzed using t-test and Chi-square at p <0.05 level of significance.
Results
There were 141 resignations recorded during the 5-year review (residents=113, fellows=28). The mean age for residents was 28.76 years ± 3.05, 55.75% were females, 59.29% graduated from non-UP College of Medicine (UPCM) schools, and 92.92% were single. Most left during their first year (53.98%); Ob-Gyne (n=20) and Anesthesiology (n=18) had the most number of drop-outs. For fellows, the mean age was 32.73 years ± 2.70, most were female (60.71%), single (71.43%), from non-UPCM schools (71.43%), left during their 1st year (78.57%) and not from PGH residency (78.57%). Pediatrics (n=13) and Internal Medicine (n=9) had the highest numbers of fellow resignations. The reasons cited were mental health, unmet expectation, change in specialty, and sickness. The mean resident attrition rate was 3.51% while for fellows it was 1.36%, an evident rise was seen during the COVID-19 years.
Conclusion
The decision to take postgraduate training is a personal journey for medical graduates. It is important to focus on strategies in identifying modifiable stressors during demanding times and be more receptive in addressing anxiety and mental health issues. Adjustments in the selection process must give applicants the real-world feel of the training environment, so a more realistic expectation will be met.
Keywords: attrition rate, post-graduate training, residents, fellows
INTRODUCTION
Balancing residency training and personal priorities has never been a daunting challenge in recent years particularly to the current generation of trainees. Well-being of physicians both within the hospital and home environment must be considered as it is essential in sustaining the overall system of healthcare. Medical specialty training in a tertiary government hospital like the University of the Philippines-Philippine General Hospital (UP-PGH), with a 1500-bed capacity, faces many difficulties and attrition is inevitably one of them. Identifying the factors resulting in attrition is central in addressing it because premature exit of a resident not only negatively impacts the training program but also disrupts the career path of the resident.1 A significant amount of time and resources are invested in recruiting and training every physician2-4 and the loss is not only logistically burdensome but costly to the hospital. Moreover, the increased clinical load and duties for the remaining residents result in lowered overall morale. Additional work and effort are also needed to reorganize workforce to minimize the effects on patient care and duty roster5, thus making the situation even more complicated.
Postgraduate residency is a choice that entails extensive decision-making process6 and is typically perceived as a demanding and stressful task for medical students7. Ultimately, the push factor to enter into specialty training is one that is subjective and personal. Several factors that may play substantial influence include family background, personal circumstances, prospective private practice, preferred lifestyle, number of working hours, financial gains, inherited family practice, and availability of future practice infrastructure. The residency selection process is arduous and labor-intensive for both the applicant and clinical training staff, as the medical graduate seeks to identify the residency program that is aligned with his or her long-term personal and career goals; the department training staff, on the other hand, is on the lookout for a suitable applicant that will likely perform well during the entire training period.6
Premature resignation definitely has ramifications and detrimental consequences to the provision of care to patients aside from the substantial and unquantifiable liability to manpower. Attrition in residency programs has been widely studied in recent decades in the Western countries but no definitive solutions have been identified. Paucity of literature on local setting particularly in UP-PGH makes it worth investigating. It is the primary objective of this pilot study to examine the trends, reasons, and annual rate of attrition in a major referral hospital with a wide range of residency and fellowship programs and to explore physician and program characteristics associated with it.
METHODS
Study Design and Population
This pilot study has two stages: Records of trainees who resigned from 01 January 2018 – 31 December 2022 from the UP-PGH Human Resource Department (HRD) and Office of Deputy Director for Health Operations (ODDHO) were initially reviewed. This aims to ensure sourcing of all available information on attrition by collecting basic data submitted during application and elicited from exit interviews. Information extracted include: for residents – age, sex, marital status, medical school, year level of attrition, undergraduate academic achievement, and pre-training medical condition; for fellows – additional information on residency hospital classification was also gathered. For the training program attributes, the following data were collected: clinical department, duration of training, type of clinical department, year of resignation (pre-COVID vs. COVID year) and reason for attrition.
The second stage entailed an online or physical survey of the Resident Training Officers (RTO) of all 17 departments and/or their respective subspecialty divisions. This, on the other hand, acquired more insights on the department's training program which cannot be retrospectively extracted from the trainee’s records or exit interviews. Data on the number of years respondent is serving as an RTO, presence of mentorship program for trainees, type of the prevailing work environment in the department for the last 5 years (2018-2022),8 average number of hours trainees go on duty, average number of duty days per week, general performance of trainees who resigned in the last 5 years (2018-2022) were asked. Residency work culture8 refers to how the culture of work environment is viewed by the RTOs and is classified into the following: clan, hierarchy, adhocracy, market (see Operational Definition of Variables).
Data collection was done from January to June 2023 and were encoded in a Microsoft Excel spreadsheet. Statistical analysis was performed using Stata Version 12 for Windows. Chi-square and T-test to measure associations between attrition and each categorical variable were utilized. Attrition rate for any year was calculated by using aggregate hospital data per department as the percentage of all residents or fellows who left compared to the total number of residents and fellows in training for the same year.9,10
The study was exempted from ethical review by the UP Manila-Review Ethics Board (UPM-REB 2022-0469-EX) as it involves negligible to minimal risks entailing only collection of data for educational evaluation activities.
Operational Definition of Variables
| Variable | Definition |
|---|---|
| Attrition | – refers to a resident or fellow at any year level who tendered resignation and left a training program at UP-PGH during the 5-year study period of 2018-2022 |
|
| |
| Annual Attrition rate | – computed as the total number of residents/fellows who tendered resignation and left a training program anytime between official appointment as Medical Officer and prior to completion of entire duration of residency/fellowship divided by the total number of residents /fellows who are in residency/fellowship program for that year as listed by HRD |
|
| |
| Resident 11 | – a Filipino national who successfully passed the Philippine Licensure Examination and has been accepted to any of the 16 departments after submitting relevant requirements for residency training |
|
| |
| Fellow 12 | – a Filipino national who successfully hurdled the respective specialty examinations or at least passed the written component of their specialty board and has been accepted to any of the 15 departments offering fellowship after submitting relevant requirements for fellowship training – or a Foreign national after following the guidelines set in the Joint Professional Regulation Commission (PRC) and Department of Health Administrative Order No. 2015-01 |
|
| |
| Medical School | – where trainee finished basic medical education |
| UPCM | – from the University of the Philippines-College of Medicine |
| Non-UPCM | – not from the University of the Philippines-College of Medicine |
|
| |
| Pre-COVID Years | – from 2018-2019 when COVID-19 is non-existent |
|
| |
| COVID Years | – from 2020-2022 when COVID-19 pandemic is ongoing |
|
| |
| Type of Clinical Department | – stratified to 4 specialty choices based on general function, duration of training program, and number of years needed to be specialty board-eligible |
| Generalist | – includes Pediatrics, Family Medicine, Internal Medicine, each with a 3-year duration of training for specialty board certification |
| Surgical Specialty | – includes General Surgery, Plastic and Reconstructive Surgery, Thoraco-cardiovascular Surgery, Urology, Pediatric Surgery, Neurosurgery, each requiring a minimum of 5 years training prior to specialty board certification |
| 4-year Surgical Specialty | – includes Obstetrics and Gynecology, Orthopedics, Otorhinolaryngology, each with 4-year residency training prior to board certification eligibility |
| Other or Combination Specialty | – includes non-generalist or combined specialties namely Anatomic and Clinical Pathology, Adult Neurology, Anesthesiology, Emergency Medicine, Ophthalmology, Psychiatry, Diagnostic Radiology and Radiation Oncology, Nuclear Medicine, and Rehabilitation Medicine -each with at least 3 years of training prior to specialty board certification |
|
| |
| Mentorship Program | – refers to the relationship in any of the specialty training programs where a consultant physician takes the role of a “mentor” who guides, promotes the “mentee’s” career and professional development, who is either a resident or fellow |
| formal | – structured and evaluated regularly |
| informal | – no structure and not evaluated |
|
| |
| Residency/Fellowship Work Culture 8 | – refers to how the culture of work environment is viewed by the RTOs in their specialty department. Categorized into the ff: |
| Clan Culture | – reflects a more sociable working environment, and individuals view it as a ‘family’ |
| Hierarchy Culture | – focuses on structure and formality, with an emphasis on organizations functioning efficiently |
| Adhocracy Culture | – reflects a climate where risk is accepted in an innovative, energetic, and creative environment |
| Market Culture | – is results-oriented, and individual’s complete goals in a competitive manner |
RESULTS
During the 5-year review period, 141 trainees (2.74%) prematurely left their training programs (residents=113, fellows=28). The mean age of resignees for residents was 28.76 years ± 3.05, the median age is 28, the youngest being 25 years of age and the oldest was 50. More than half were females (55.75%), graduated from non-UPCM medical school (59.29%) and a vast majority being single (92.92%). The year level of attrition clustered around the earlier part or 1st two years of residency with the highest number leaving during their first year of training (53.98%). For fellows, the mean age of those who quit was32.73 years ± 2.70, median of 33 years, with age ranging from 29 to 40 years. Similarly, a considerable percentage was female (60.71%), single (71.43%), from non-UPCM medical school (71.43%), resigned on their 1st year (78.57%), and did not come from a PGH residency program (78.57%) with most having trained in a hospital within Metro Manila (50%). The resident and fellow attrition profile from 2018-2022 is detailed in Table 1.
Table 1.
Summary of Resident and Fellow Profile who Resigned from 2018-2022 (N=141)
| Variables | Residents | Fellows | ||
|---|---|---|---|---|
| n | 113 | n | 28 | |
| Age | ||||
| Mean | 28.76 ± 3.05 | 32.73 ± 2.70 | ||
| Median | 28 | 33 | ||
| Mode | 28 | 32 | ||
| Range | Min-25; Max-50 | Min-29; Max-40 | ||
| n | % | n | % | |
| Sex | ||||
| Male | 50 | 44.25 | 11 | 39.29 |
| Female | 63 | 55.75 | 17 | 60.71 |
|
| ||||
| Marital Status | ||||
| Single | 105 | 92.92 | 20 | 71.43 |
| Married | 7 | 6.19 | 8 | 28.57 |
| Not Identified | 1 | 0.88 | ||
|
| ||||
| Medical School | ||||
| UPCM | 46 | 40.71 | 8 | 28.57 |
| Non-UPCM | 67 | 59.29 | 20 | 71.43 |
|
| ||||
| Year Level at time of attrition | ||||
| 1st | 61 | 53.98 | 22 | 78.57 |
| 2nd | 33 | 29.20 | 6 | 21.43 |
| 3rd | 12 | 10.62 | ||
| 4th | 5 | 4.42 | ||
| 5th | 1 | 0.88 | ||
| 6th | 0 | 0.00 | ||
| 7th | 1 | 0.88 | ||
|
| ||||
| Residency Hospital Classification | ||||
| PGH | 6 | 21.43 | ||
| Non-PGH | 22 | 78.57 | ||
| Metro Manila hospital | 11 | 50.00 | ||
| Outside Metro Manila hospital | 3 | 13.63 | ||
| Not Identified | 8 | 36.36 | ||
For the specialty program characteristics of trainees (Table 2) who resigned, the following departments have the highest attrition percentage for residents from 2018-2022: Obstetrics-Gynecology (17.70%), Anesthesiology (15.93%), Family and Community Medicine (12.39%), Pediatrics (11.50%), and Surgery (10.62%). While the departments of Pediatrics (46.43%) and Internal Medicine (32.14%) have the highest proportion for fellows.
Table 2.
Training Program Attributes on Attrition (2018-2022)
| Attributes / Categories | Residents | Fellows | ||
|---|---|---|---|---|
| n | % | n | % | |
| Department | ||||
| Anesthesiology | 18 | 15.93 | 1 | 3.57 |
| Dermatology | 0 | 0 | 0 | 0 |
| Emergency Medicine (DEM) | 5 | 4.42 | 0 | 0 |
| Family Medicine (DFCM) | 14 | 12.39 | 1 | 3.57 |
| Laboratories | 1 | 0.88 | 0 | 0 |
| Medicine | 1 | 0.88 | 9 | 32.14 |
| Neurosciences | 9 | 7.96 | 0 | 0 |
| Obstetrics and Gynecology | 20 | 17.70 | 0 | 0 |
| Ophthalmology | 1 | 0.88 | 0 | 0 |
| Orthopedics | 8 | 7.08 | 0 | 0 |
| ORL/HNS | 2 | 1.77 | 0 | 0 |
| Pediatrics | 13 | 11.50 | 13 | 46.43 |
| Psychiatry | 6 | 5.31 | 1 | 3.57 |
| Radiology | 0 | 0 | 0 | 0 |
| Rehabilitation Medicine | 3 | 2.65 | 1 | 3.57 |
| Surgery | 12 | 10.62 | 1 | 3.57 |
| Toxicology | 1 | 3.57 | ||
|
| ||||
| Duration of training (in years) | ||||
| 1 | 1 | 3.57 | ||
| 2 | 5 | 17.86 | ||
| 3 | 62 | 54.87 | 8 | 28.57 |
| 4 | 33 | 29.20 | ||
| 5 | 12 | 10.62 | ||
| 6 | 6 | 5.31 | ||
| Not identified | 14 | 50.00 | ||
|
| ||||
| Type of Department | ||||
| Generalist | 28 | 24.78 | 22 | 78.57 |
| Surgical Department | 16 | 14.16 | 1 | 3.57 |
| 4-year surgical specialty | 28 | 24.78 | ||
| Others/Combined | 39 | 34.51 | 3 | 10.71 |
| Not identified | 2 | 1.77 | 2 | 7.14 |
|
| ||||
| Year of Resignation | ||||
| Pre-COVID | 35 | 30.97 | 7 | 25.00 |
| COVID | 78 | 69.03 | 21 | 75.00 |
|
| ||||
| Number of days a trainee goes on shift per week | ||||
| 1-2 days/week | 68 | 60.18 | 25 | 89.29 |
| 3-5 days/week | 33 | 29.20 | 1 | 3.57 |
| 6-7 days/week | 12 | 10.62 | 1 | 3.57 |
| Not identified | 1 | 3.57 | ||
|
| ||||
| Number of hours a trainee goes on duty | ||||
| ≤12 hours/day | 5 | 4.42 | 1 | 3.57 |
| >12 hours per day | 108 | 95.58 | 27 | 96.43 |
|
| ||||
| Presence of Mentoring | ||||
| Yes | 112 | 99.12 | 28 | 100 |
| No | 1 | 0.88 | ||
|
| ||||
| General Training Performance Evaluation | ||||
| Satisfactory | 24 | 21.24 | 11 | 39.29 |
| Unsatisfactory | 31 | 27.43 | 3 | 10.71 |
| Mixed Grading | 48 | 42.48 | ||
| Not Applicable | 3 | 8.85 | ||
| Not Identified | 7 | 14 | 50 | |
|
| ||||
| Training Work Culture Type | ||||
| Clan | 61 | 53.98 | 26 | 92.86 |
| Hierarchy | 36 | 31.86 | 2 | 7.14 |
| Adhocracy | 0 | 0 | ||
| Market | 16 | 14.16 | ||
The residency training with 3 years duration,1-2 days/week duty shift, more than 12 hours/day duty, and with a clan type of work culture had the most number of resignees both for residents and fellows. For residents, the combined type of department had the highest attrition at 34.51% followed by both the generalist and 4-year surgical specialty (24.78% for each). For fellows, the majority of attrition came from the generalist department. This trend may be because 9 out of 17 residency programs (53%) are 3 years long and fall under either the combined or generalist types. The general performance of residents as reported by the RTOs was either satisfactory or unsatisfactory (mixed grading) while half of the fellows’ evaluation were not cited. Expectedly, almost 1.5 times more residents and twice as many fellows resigned during the pandemic compared to the non-pandemic years.
There were varied reasons why the trainees prematurely left during the 5-year analysis; unfortunately, the majority for both groups cannot be retrospectively extracted from available records. For the residents, the following were gathered as the reasons for resignation (Figure 1): mental health, unmet expectation, change in chosen specialty, sickness, change in career plan or interest, burnout, heavy workload or pressure at workload, family reason, and academic integrity.
Figure 1.
Reasons for resident attrition (2018-2022).
Meanwhile for fellows; mental health, unmet expectation, sickness/illness, change in interest, and burnout were cited as the motives for leaving (Figure 2).
Figure 2.
Reasons for fellow attrition (2018-2022).
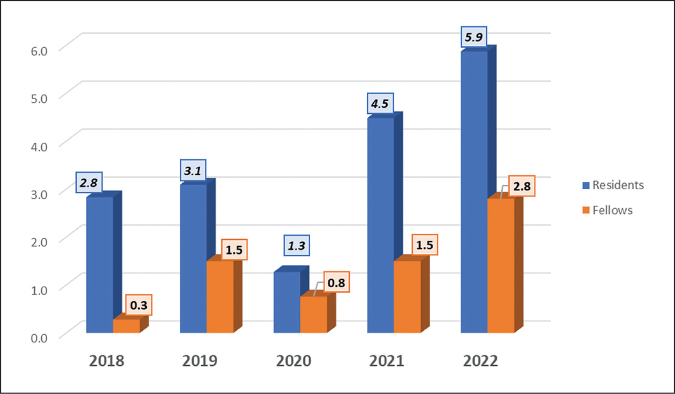
The annual attrition rate (Table 3) increased markedly during the last two years of COVID pandemic from 2021-2022 for the residents and in 2022 for the fellows. Pre-pandemic, the annual rates for residents were 2.83% and 3.09% for 2018 and 2019, respectively; dipped in 2020, the 1st year of COVID, at 1.27% but increased to 1.5 to 2 times in 2021-2022. The fellow’s attrition rate showed a similar trend; 0.27% to 1.50% pre-COVID years, went down to 0.76% in 2020 then increased to 1.50% and 2.80% in 2021 and 2022, respectively (Figure 3). The annual attrition rate summarized in Table 3 revealed an average of 3.51% for residents and 1.36% for fellows from 2018 to 2022.
Table 3.
Annual Attrition Rate, Residents and Fellows (2018-2022)
| Year | Residents | Fellows | ||||
|---|---|---|---|---|---|---|
| Total Residents | Attrition (n) | Attrition Rate (%) | Total Residents | Attrition (n) | Attrition Rate (%) | |
| 2018 | 565 | 16 | 2.83 | 368 | 1 | 0.27 |
| 2019 | 614 | 19 | 3.09 | 401 | 6 | 1.50 |
| 2020 | 629 | 8 | 1.27 | 397 | 3 | 0.76 |
| 2021 | 669 | 30 | 4.48 | 399 | 6 | 1.50 |
| 2022 | 682 | 40 | 5.87 | 429 | 12 | 2.80 |
|
| ||||||
| Total | 3,159 | 113 | Ave.: 3.51 | 1,994 | 28 | Ave.: 1.36 |
Figure 3.
Five-year attrition rate trends, Residents and Fellows (2018-2022).
Eight clinical specialties surpassed the overall 3.51 mean attrition rate (Figure 4); with Orthopedics being the highest followed by Department of Family and Community Medicine (DFCM), Psychiatry, Anesthesiology, Ob-Gyne, Neurosciences, Emergency Medicine (EM), and Pediatrics. During the pandemic years, Psychiatry (2020) and FCM (2022) reported the highest rate at 16.67% and 21.05%, respectively. On the other hand, pre-pandemic, only the Department of EM (DEM) registered a relatively high rate at 11.76%.
Figure 4.
Average resident attrition rate in the clinical departments.
*Overall average attrition rate
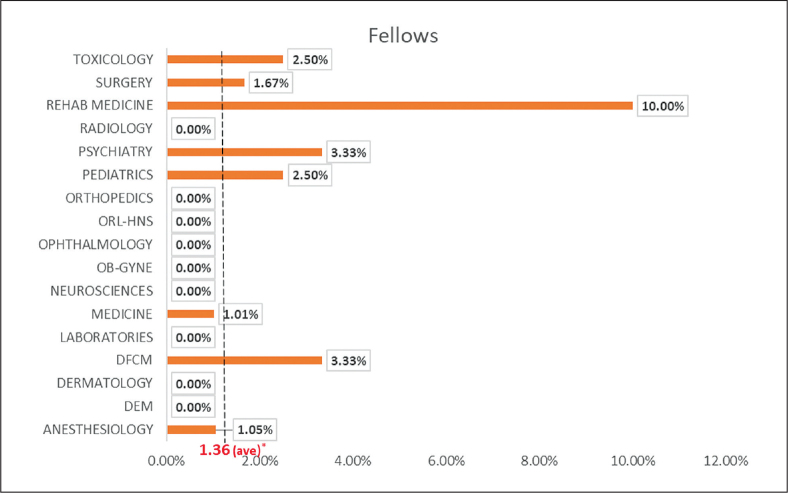
The annual attrition average across all departments for fellows was 1.36 and only six out of the 17 specialties exceeded this level (Figure 5), namely: Rehabilitation Medicine (10%), Psychiatry (3.33%), DFCM (3.33%), Pediatrics (2.5%), Toxicology (2.5%), and Surgery (1.67%). It is important to note that Surgery and Pediatrics are relatively considered big departments compared to the other medium-sized (e.g., DFCM, Psychiatry) and smaller specialties (e.g., Toxicology, Rehab Med) in terms of the number of fellows.
Figure 5.
Average fellow attrition rate in the clinical departments.
*Overall average attrition rate
Analysis of the trainees’ attrition characteristics (Table 4) showed no significant difference in sex, marital status, and year level of attrition among the residents who resigned before and during the pandemic. However, residents who resigned during the COVID years were significantly younger (p=0.04) than those during pre-pandemic. Furthermore, there were significantly more non-UPCM resignees than there were UPCM (p=0.03), pre-pandemic. It can also be noted that attrition was comparable among UPCM and non-UPCM residents from 2020-2022. No specific individual profile of fellows was associated with resignations before and during the COVID years.
Table 4.
Comparison of Trainee Characteristics between those who Resigned pre-COVID-19 vs. COVID-19 years
| Variable | Residents | Fellows | ||||
|---|---|---|---|---|---|---|
| Resigned Pre-COVID year (n=35) | Resigned COVID year (n=78) | p-value | Resigned Pre-COVID year (n=7) | Resigned COVID year (n=21) | p-value | |
| Age | Mean=29.65 SD=4.09 | Mean=28.36 SD=2.37 | 0.04* | Mean=34 SD=3.42 | Mean=32.85 SD=2.46 | 0.34 |
|
| ||||||
| Sex | 0.15§ | 0.19§ | ||||
| Male | 19 | 31 | 1 | 10 | ||
| Female | 16 | 47 | 6 | 11 | ||
|
| ||||||
| Marital Status | 0.78§ | 0.37§ | ||||
| Single | 33 | 72 | 4 | 16 | ||
| Married | 2 | 5 | 3 | 5 | ||
| Other/s | 0 | 1 | ||||
|
| ||||||
| Medical School | 0.03§ | |||||
| UPCM | 9 | 37 | ||||
| Non-UPCM | 26 | 41 | ||||
|
| ||||||
| Year Level of Attrition | Mean=1.91 SD=0.98 | Mean=1.64 SD=1.04 | 0.19* | Mean=1.14 SD=0.38 | Mean=1.24 SD=0.44 | 0.61§ |
|
| ||||||
| Residency Hospital Classification | - | - | 0.08§ | |||
| PGH | 2 | 4 | ||||
| Non-PGH | 5 | 17 | ||||
| Metro Manila hospital | 6 | |||||
| Outside Metro Manila hospital | 0 | 3 | ||||
| Not Identified | 0 | 8 | ||||
t-test
chi-square
p <0.05, significant
Table 5 details the training program attributes of residents and fellows who resigned before and during the COVID-19 period. Findings with statistical significance during the pandemic for fellows include those programs with 3 years duration (p=0.02) and generalist department type (p=0.03); no program feature appears to be associated with resident attrition.
Table 5.
Comparison of Training Program Characteristics between those who Resigned pre-COVID-19 vs. COVID-19 years; Residents vs Fellows
| Attributes / Categories | Residents | Fellows | ||||
|---|---|---|---|---|---|---|
| Pre-COVID (n=35) | COVID (n=78) | p-value § | Pre-COVID (n=7) | COVID (n=21) | p-value § | |
| Department | 0.94 | 0.88 | ||||
| Anesthesiology | 7 | 11 | 0 | 1 | ||
| Dermatology | 0 | 0 | 0 | 0 | ||
| Emergency Medicine | 3 | 2 | 0 | 0 | ||
| Family Medicine | 2 | 12 | 0 | 1 | ||
| Laboratories | 0 | 1 | 0 | 0 | ||
| Obstetrics and Gynecology | 6 | 14 | 0 | 1 | ||
| Internal Medicine | 0 | 1 | 2 | 7 | ||
| Neurosciences | 3 | 6 | 0 | 0 | ||
| Ophthalmology | 0 | 1 | 0 | 0 | ||
| Orthopedics | 2 | 6 | 0 | 0 | ||
| ORL/HNS | 1 | 1 | 0 | 0 | ||
| Psychiatry and Behavioral Medicine | 2 | 4 | 0 | 1 | ||
| Pediatrics | 4 | 9 | 4 | 9 | ||
| Surgery | 4 | 8 | 1 | 0 | ||
| Rehabilitation Medicine | 1 | 2 | 0 | 1 | ||
| Toxicology | 0 | 1 | ||||
|
| ||||||
| Duration of training (in years) | 0.73 | 0.02 | ||||
| 1 | 0 | 1 | ||||
| 2 | 4 | 1 | ||||
| 3 | 19 | 43 | 1 | 7 | ||
| 4 | 9 | 24 | ||||
| 5 | 4 | 8 | ||||
| 6 | 3 | 3 | ||||
| Not identified | 2 | 12 | ||||
|
| ||||||
| Type of Department | 0.19 | 0.03 | ||||
| Generalist | 6 | 22 | 4 | 18 | ||
| Surgical Department | 5 | 11 | 1 | 0 | ||
| 4-year surgical specialty | 8 | 20 | 0 | 0 | ||
| Others / Combined | 14 | 25 | 0 | 3 | ||
| Not identified | 2 | 0 | 2 | 0 | ||
|
| ||||||
| Number of days a trainee goes on shift per week | 0.68 | 0.59 | ||||
| 1-2 days/week | 19 | 49 | 6 | 19 | ||
| 3-5 days/week | 12 | 21 | 0 | 1 | ||
| 6-7 days/week | 4 | 8 | 1 | 1 | ||
|
| ||||||
| Number of hours a trainee goes on duty | 0.17 | 1.00 | ||||
| ≤12 hours/day | 3 | 2 | 0 | 1 | ||
| >12 hours per day | 32 | 76 | 7 | 20 | ||
|
| ||||||
| Type Training Work Culture | 0.99 | 0.44 | ||||
| Clan | 19 | 42 | 6 | 20 | ||
| Hierarchy | 11 | 25 | 1 | 1 | ||
| Adhocracy | 0 | 0 | ||||
| Market | 5 | 11 | ||||
chi-square
p <0.05, significant
Although most of the reasons (62%) for premature exit from the training program were not identified, mental health was cited as the most compelling one during the COVID years particularly for the residents (Table 6). The other push factors during the pandemic were unmet expectations, change in specialty, and personal health reasons.
Table 6.
Comparison of Reason for Attrition, Pre-COVID vs. COVID years
| Reason | Residents | Fellows | ||
|---|---|---|---|---|
| Pre-COVID (n=35) | COVID (n=78) | Pre-COVID (n=7) | COVID (n=21) | |
| Burnout | 0 | 3 | 1 | |
|
| ||||
| Change in specialty | 0 | 7 | ||
|
| ||||
| Change in Career plan/Interest | 0 | 3 | 0 | 1 |
|
| ||||
| Personal Health Reason | 0 | 3 | 0 | 3 |
|
| ||||
| Family Reason | 0 | 1 | ||
|
| ||||
| Mental health | 0 | 14 | 4 | |
|
| ||||
| Heavy Workload/Pressure | 0 | 2 | ||
|
| ||||
| Unmet Expectation | 0 | 7 | 0 | 3 |
|
| ||||
| Academic Integrity | 0 | 1 | ||
|
| ||||
| Not Identified | 35 | 37 | 7 | 9 |
DISCUSSION
Medical specialty training is perceived as one of the most physically and mentally demanding stage of a doctor’s journey of being a specialist. In most cases, the newly graduated medical student needs to adjust to the heavier workload, and the substantial increase in the level of responsibility, not to mention the other requirements set by the training program necessary for completion of training. There will inevitably be trainees who cannot keep up with these demands. Some will realize that the specialization they initially chose to train in is not for them. A few will develop an illness, either physical or mental, or will end up with a family circumstance that they will have to prioritize their health or family over completion of training.
Training attrition may be a result of one or a combination of factors that include the trainees’ innate characteristics, background and personal immersions, the training program’s attributes such as its requirements and everyday activities, and the training environment as in the hospital facility, its physical set up, its processes, and its staff. At societal level, attrition may imply the loss of highly qualified personnel in the medical manpower affecting healthcare.13 At the same time, at the program level, the remaining group of trainees and their consultant staff may feel the weight adversely in terms of declining morale14 and inadvertent practical concerns such as scheduling and replacement issues.
Attrition may be associated with some demographic factors. In this study, the mean age of attrition of 28.76 years ± 3.05 for residents is expectedly lower than the mean age for fellows of 32.73 years ± 2.70 as the latter are older and are already in their post-residency specialization. Our present study also revealed that most of those who left training were females, single, and graduated from institutions other than UPCM, which is the medical school affiliated with UP-PGH. The findings were consistent with the reported significantly higher pooled attrition rate of 25% for female residents compared to 15% for men.15 A 2019 study by Lee et al. on Obstetrics and Gynecology resident attrition in Singapore showed that female and married residents were more likely to consider leaving specialty training, possibly due to expectations in the traditional setting of a nuclear family in their country.2 Similarly, more female EM residents left residency in the US between 2006-2007 and 2015-201616 due to health or family reasons. The circumstances that female trainees face in other countries are comparable to those in the local setting with most being of reproductive age when they enter residency. They also have responsibilities such as child-rearing, homemaking, being caretakers of sick and elderly members of the family, and other innately assigned obligations in a tightly-knit Filipino family culture.
Attrition occurred during the first two years of residency, majority on the 1st year level which showed similar findings for fellows who also quit on their 1st year of training. The result that attrition mainly occurred during the first two years of training across the different clinical departments is supported heavily in the literature.17,18 The timing may stem from adjustments to a highly demanding training atmosphere, steep learning curve, acclimatization to a new job, adaptation to the hectic duty schedules, and familiarization with hospital processes while getting to know their workmates. Although these adjustments are familiar to everyone, the ease and/or time frame may vary. Non-UPCM graduates setting foot for the first time in a busy and sometimes harsh tertiary hospital milieu may have more difficulty with this. Thus, a higher percentage was noted in this group. Being the National University Hospital, post-graduate training entails additional non-clinical work and administrative duties. These include performing research and supervising junior trainees and medical students. Others include clerical errands in keeping different patient registries and hospital logbooks up-to-date, filling up various laboratory forms, legwork for departmental conferences and arranging logistical requirements for lectures, didactics, conventions, and other departmental leisure gatherings. These are additional assignments to an already tight and heavy clinical workload. The administrative tasks become a burden to the medical workforce in general.19 As reported by Woolhandler et al. in 2014, US physicians devote one-sixth of their working hours, spending 8.7 hours per week, on administration which eventually lowers career satisfaction.20 Furthermore, administrative load is hard to quantify and even evaluate.
The program attributes in UP-PGH that were associated with higher trainee resignation rates are those with a 3-year program, with 1-2 duty days/week, more than 12 hours shift/day, and clan type of work culture. The combined type of department or those with non-generalist or combined specialties requiring at least three years of training had the highest attrition rate. This was followed by both the 3-year generalist and 4-year surgical specialty type. It should be noted though, that more than half of the specialty programs are three years in duration (53%) belonging to either combined or generalist type. These departments may exhibit an atmosphere where stressors are existent and expectations of residents or fellows are not met. Admittedly, most programs have heavy clinical workload requiring trainees to go on shift for more than 12 hours a day. Being a tertiary referral center, PGH caters to a large volume of patients with more complex problems or who present at the later stage of disease. These mentally and even emotionally demanding conditions further complicate the already physically demanding working conditions. A 2019 study by Chen et al. reported that vascular and cardiothoracic surgery residents in the US who seriously thought of quitting their training cited work conditions on specific rotations rather than overall working hours as reasons for contemplating resignations.21 Thus, as can be deduced, the type of work done in a particular posting that is more than the number of hours spent in that post should be differentiated in evaluating the factors to attrition. This may be a reasonable consideration in curriculum design and workforce scheduling.
The clinical learning environment is an important aspect that may have an influence on meeting the expectations of trainees. According to a cross-sectional study by Bin-You et al.8 on the interplay between residency program culture and feedback culture, ‘Clan’ culture was the foremost and preferred by residents in three institutions in the US. The clan type of work environment is characterized as a more sociable training environment, generally viewed to be similar to ‘family’.22 This sets a venue for having more informal feedback for employees, for a higher level of interaction between superiors and subordinates, and underscores employee development.23 The parental figures exhibited by program leaders in clan culture is highly desired by residents. It provides a strong support and encouragement system similar to an extended family which is appreciated in a highly demanding and rigorous workplace. Based on the survey done among RTOs, the clan culture is the most prevalent working milieu in PGH. Whether this type affects the attrition rate was not determined by this study. It only reflects the most dominant working atmosphere in the different specialties. Further scrutiny into the effect of this program variable may be required. In an analysis of attrition from Neurosurgery residency in Canada by Cusimano et al.,7 low-attrition programs placed more emphasis on the relationships built by residents and to the interpersonal aspects of training than programs with reported high resignations. The more personal approach and associations established in a more familial setting like in a clan culture are seen as positive engagements during specialty training.
The general performance of residents did not seem to factor in attrition. Most of the RTOs reported mixed performance evaluations for residents who dropped out of training. A consideration could be the difficulty of recalling the actual clinical and academic appraisals of resignees when the survey was conducted. Moreover, the questions included in the survey were not specific to each trainee but more on general terms regarding trainee and program characteristics. In a 2020 Singapore study on Anesthesia residents who quit, majority did not require remediation nor were dismissed because of unfavorable training evaluation or clinical incompetency but rather due to other reasons in the training environment.5
Numerous and diverse reasons for leaving training have been cited across clinical specialties. These are disturbed work-life balance, job discontent, excessive workload, switching career or specialty, unappealing work culture, and mismatch expectation.2,5-7,16,24,25 Results of our present investigation showed mental health as one of the compelling factors for leaving both the residency and fellowship. Notwithstanding the compounding effect of the pandemic on the mental wellbeing of hospital employees, this undoubtedly placed significant stress on the healthcare workers, particularly the residents and fellows tasked to be at the frontlines. It should be noted, however, that even before the pandemic, burnout and lack of adequate social support remained major contributors in trainees' mental health challenges. Burnout is known to be associated with poor work-life balance, unhealthy working hours, heavy workload, and unrealized academic expectation which are oftentimes coupled with the external demands of family and private life.2,25,26 For those who willingly resigned, the social sacrifice of isolation from family and friends, personal costs e.g., skipped meals, less attention to personal care or sleep deprivation, and the delay in financial compensation due to long training duration offset intrinsic rewards expected in future private practice. During residency, the daily tasks and clinical demands are apparently seen as disproportionate when compared to the anticipated remuneration and satisfaction in the offing.
Formal and structured mentoring has been associated with lower levels of burnout and may be considered as first-line strategy to address this problem.26 However, having a dedicated mentor does not automatically translate to a favorable support system27 but interactions derived from the mentor-mentee relationship have been linked to increased resident satisfaction and less desire to leave prematurely4. An overwhelming majority of RTOs reported presence of mentoring programs in their respective departments but this, however, cannot be construed as a major factor against attrition; its actual extent and implementation may need further qualitative investigation to fully decipher its impact.
The unmet expectations of trainees noted in our study also put a heavy toll on their mental health causing them to drop out early. The attrition factors are evidently intertwined and cannot be taken in isolation which, if not addressed, will result in a vicious downhill trend. Data from SingHealth on attrition cites program mismatch as the leading cause of resident departure from hospital-based training.28 Recognizing that incompatible expectations are vital to attrition risk, creating realistic ones could help reduce attrition. Unmet expectations could be tempered by providing considerable prior exposure and work experience either during medical school or pre-residency period for individuals with equivocal motivation in entering postgraduate specialization. Furthermore, job satisfaction is achieved if expectation is consistent with actual experience.29 All stakeholders will benefit if potential mismatch between trainee and specialty is timely recognized and resolved to avert considerations of premature resignation.
Another identified reason is switching specialty or total change of interest from the medical field. A possible explanation for the change of heart in a trainee’s chosen program may stem from the desire for work-life balance and a more controllable lifestyle. Schwartz et al. defined controllable lifestyle specialties as those that allow the physician to control the number of hours devoted to practicing the specialty.30 Inability to balance and manage lifestyle, in turn, pushes their decision to leave. Personal variables like age, gender, marital status, lifestyle, family responsibilities, coping mechanism, psyche, and long-term career goals may influence this. The effect of long working hours on lifestyle and the financial burden remained issues of constant contemplation for leaving.31
The mean attrition rate of 3.51% for the PGH residents and 1.36% for fellows may differ from the recorded rates by several authors. Baldwin et al. put the overall attrition rate for all American residents at 1.8% three decades ago32 but has since increased to around 4% in 2000-2009.9 Recent systematic review and meta-analysis done by Hope and colleagues in 2020 registered a pooled overall attrition estimate as high as 17% for surgical training programs.33 A nationwide survey investigating factors involved in attrition at the Netherlands from 2014 to 2017 registered an overall attrition rate from hospital-based specialties at 11%, ranging from 2.2% to as high as 24.3%.25 The reported dropout rate among Florida’s family practice residency programs from 1976 to 1979 is 20% to 33%.34 The SingHealth Anesthesiology Residency Programme (SHARP) had an overall attrition prevalence of 17% over a 7-year period from 2011-2018.5 This is comparable to the attrition prevalence of 18% described among general surgery residents,15,35 with uncontrollable lifestyle cited as the most common reason for not finishing residency.15 The literature is silent about attrition rates that are acceptable or within manageable limits. Although our institution percentage may not seem to be that high, it generally represents a considerable number if seen in the context of trainee shortage affecting the workforce of a tertiary hospital with a wide catchment area. Furthermore, looking at the trends over the 5-year study duration, the significant increase has been a concern.
The reported rates greatly vary in different countries and types of sponsoring institution; however, Dermatology consistently had the lowest attrition rate with the primary care specialties including Family Medicine, Ob-Gyne and Pediatrics, having difficulty retaining trainees.36 This is consistent with our findings with Dermatology registering no resignations and the three mentioned departments exceeding the PGH 5-year mean attrition of 3.51%. Psychiatry is also one of the clinical departments with a relatively high attrition rate. This review noted an average of 6.52% for the last 5 years which is comparable to 6.0% [5.7%-6.3%] cited by Lu et al.16 and the 7.53% [6.74%-8.60%] noted in the study by Wang et al.36 This could possibly be attributed to the long duty hours and stressful work environment in Psychiatry with the deluge of consults and referrals from within the university and hospital staff on top of the usual patient base during the height of COVID-19 scare.
Although having academic honors were not extracted in our review due to non-documentation on the entry and exit interviews of individuals who resigned, its presence yielded interesting results in several studies. Academic achievements prior to entry to residency have not shown a definitive role on either attrition or retention to postgraduate specialty programs. Kron and colleagues found that an honors performance in medical school predicted retention in their surgical residency program,37 but Papp et al. showed no correlation between medical school academic records and subsequent performance evaluations among surgical residents38. To fully elucidate if possession of Latin or other academic honors has an impact on the motivation, retention or attrition, further study is needed.
Another significant influence to be considered in understanding the trends and reasons for attrition at UP-PGH in the last five years is the effect of the pandemic from 2020 to 2022. The unexpected added demands on the clinical workload brought about by COVID-19 were evidently reflected in the larger number of resignations during the pandemic both among the residents (69.03%) and fellows (75%). Interestingly, the attrition rate actually dropped during the 1st year of the pandemic in 2020 but almost doubled compared to pre-pandemic figures in the following years. Although it is quite puzzling why a dip in 2020 occurred, against what is naturally expected because of the uncertainty of the disease, the most likely impact of COVID-19 was felt in the following years due to the protracted exposure to an exhausting course of the infection and the unpredictable virus behavior.
It was also noted that residents who left during the pandemic were significantly younger compared to the pre-pandemic year. The attrition rate from graduates of non-UPCM medical schools was significantly higher during the pre-pandemic years but the rate between UPCM and non-UPCM residents was already comparable during the COVID period. It can be surmised that during the pandemic, the non-UPCM graduates who were unfamiliar with the PGH processes and culture found it hard to adjust, particularly in their 1st year, resulting in early departure. As expected, the younger residents were more inclined to leave when COVID struck due to a combination of reasons previously cited. It should be noted that the year level 1 residents during the data collection period were the medical interns and clerks when the pandemic hit. During that time, the medical students were barred from the clinical rotations and were shifted to online learning. This significantly affected exposure to clinical work and delayed adjustments to the stressful work environment. Their age could have also made it easier for them to decide to quit and delay entry into specialty training.
For fellows, most resignations were from programs classified under the generalist type and those with 3-year programs. Most of the PGH fellowship programs have a duration of 3 years and these are concentrated in the Internal Medicine and Pediatrics both classified as generalist departments. These two specialties, together with Family and Community Medicine, bear the burden of the clinical load during the pandemic by the sheer number and high acuity of patients. It is possible that fellows from these departments decided to leave because employment-wise, they can already engage in private clinical practice given that they already finished residency. Furthermore, there were impressions that the quality of training for some fields of specialization might have been compromised when PGH was designated as a COVID referral center. As the case-mix and procedures contracted with the priority given to COVID cases, some trainees felt anxious and uncertain about not getting what they came for in PGH. Given all these observations, the challenge to instigate measures to address attrition must be multifaceted commencing in the latter years of medical schooling, during the selection process and recruitment period, adjusting modifiable aspects of the training curriculum e.g., scheduling, varying rotations, creating a more engaging learning and work environment to strategies on retaining existing trainees, but most importantly, being able to identify early on who may be at risk of attrition.
Limitations
Since the study entailed secondary data review, information gathered was limited to what was available in the trainee’s records from HRD and ODDHO. This pilot investigation was conducted on broad terms in an attempt to generate initial trends from available hospital reports which may find value when instituting changes or policies on training. As the study relied on HRD appointment records, exit interviews of ODDHO, and general responses of RTOs, as well as limited qualitative data that were not granular were obtained.
The authors were also aware of the possible inexact estimation of the attrition figures with just the examination of available attrition statistics; thus, the only intention was to present a more general perspective of the overall attrition picture of PGH. As most of the variables needed were not retrospectively extracted, a more robust, granular, and standardized database that would include details on pre-training medical conditions, individual performance evaluation, and reason for resignation must be part of application forms and resignation interview checklists.
Recall bias is also a concern with regard to data gathered from RTOs on the activities and performance of trainees five years ago. This was addressed with clear definitions of terms in the survey introduction and only basic information was asked regarding the department’s training program.
CONCLUSION AND RECOMMENDATIONS
This preliminary study identified trainee-specific and training program attributes related to attrition and the reasons and trends in the last five years in PGH. Female, single trainees from non-UP College of Medicine medical schools were more likely to leave residency and fellowship. Departure from clinical training usually occurs during the first two years and the leading reasons for this were mental health, unmet expectations, change in specialty, and sickness. The mean resident attrition rate was 3.51% while for fellows the average rate was 1.36%, with a noticeable increase during the COVID years.
A better understanding of the impact of attrition will help new medical graduates transition to post-graduate training and prevent early departure. It may be worthwhile to revisit the medical school curriculum to integrate extensive career counseling as early as clinical clerkship with actual exposure to the rigors of residency and considerable immersion in the ward work. It is essential to advise medical students and assist them in their career decisions, underscoring the need for clear expectations and motivation as to why they are proceeding to hospital-based specialization.
The present investigation recognizes the need to improve screening and selection process of applicants which will encourage self-evaluation to have more realistic expectations of the grueling years ahead. Hospital administrators, department chairs, and training officers must also be cognizant that the conventional training model of “one size fits all” may no longer be the best template due to the changing preferences of residents and fellows. During training, regular feedback and self-reflection must enhance “career adaptability” as part of character development. Healthy and positive interactions with colleagues must also be encouraged, ensuring access to support systems like consultant advisers, mentors, family, peers, and significant others. Anxiety and expectations must be managed during the early years of training by identifying modifiable stressors when the learning curve is expected to be steep. Although logistically difficult, an individualized training approach tailored to the evolving demands of the trainees and program can be considered. This may include extended leave credits, predictability in working hours, protected “me-time”, a more open and nurturing department culture, fostering camaraderie, and accommodating personal needs when attending to other priorities like family or health reasons.
Attrition, even though considered disruptive, must not always be seen as unfavorable especially if potential expectation mismatch between the trainee and the specialty is identified in a timely manner. It can be an opportunity to assess individual motivations, doubts, and intentions; for the program directors, it may also be a good time to finetune the training curriculum to better prepare the next generation of specialists by adapting to the changing learning landscape because at the macro level, the future of the healthcare system is also at stake.
Acknowledgments
The authors would like to express their gratitude to UP-PGH for the financial support to conduct this paper under the 2023 PGH Research Grant for Medical Specialists/Consultants.
Statement of Authorship
Both authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
One of the authors is the PGH Coordinator for Training, who implements the rules and policies of the different training programs of the hospital. She did not participate in the data gathering; no other conflict of interest is declared.
REFERENCES
- 1.Naylor RA, Reisch JS, Valentine RJ. Factors related to attrition in surgery residency based on application data. Arch Surg. 2008. Jul;143(7):647-51; discussion 651-2. doi: 10.1001/archsurg.143.7.647. PMID: 18645106. [DOI] [PubMed] [Google Scholar]
- 2.Lee JC, Kee JX, Ogilvie SW, Chern B, Chin CY. What drives attrition amongst obstetrics and gynaecology residents in Singapore. The Asia Pacific Scholar. 2019;4(1):34-41. doi: 10.29060/TAPS.2019-4-1/OA2005. [DOI] [Google Scholar]
- 3.Avery DMJ, Harrell AG, Wallace JC, Burkhardt J, Bell JV, Geno CE, et al. Why do residents quit general surgery residencies? A study of 789 graduates from 3 campuses who matched into general surgery over 40 years: 1974 to 2015. Clin Surg. 2017;2(1):1-5.doi: 10.33582/2639-9229/1003. [DOI] [Google Scholar]
- 4.Sullivan MC, Yeo H, Roman SA, Ciarleglio MM, Cong X, Bell RH Jr, et al. Surgical residency and attrition: defining the individual and programmatic factors predictive of trainee losses. J Am Coll Surg. 2013. Mar;216(3):461-71. doi: 10.1016/j.jamcollsurg.2012.11.005. PMID: 23266420. [DOI] [PubMed] [Google Scholar]
- 5.Moo D, Siow WS, Ong ET. Why residents quit: Prevalence of and reasons for attrition among anaesthesia residents in a single sponsoring institution. Proceedings of Singapore Healthcare. 2020;29(2):94-103. doi: 10.1177/2010105820908296. [DOI] [Google Scholar]
- 6.Andriole DA, Jeffe DB, Hageman HL, Klingensmith ME, McAlister RP, Whelan AJ. Attrition during graduate medical education: medical school perspective. Arch Surg. 2008. Dec;143(12):1172-7; discussion 1177. doi: 10.1001/archsurg.143.12.1172. PMID: 19075168. [DOI] [PubMed] [Google Scholar]
- 7.Cusimano MD, Yonke AM, Tucker WS. An analysis of attrition from Canadian neurosurgery residency programs. Acad Med. 1999. Aug;74(8):925-31. doi: 10.1097/00001888-199908000-00019. PMID: 10495735. [DOI] [PubMed] [Google Scholar]
- 8.Bing-You R, Ramani S, Ramesh S, Hayes V, Varaklis K, Ward D, et al. The interplay between residency program culture and feedback culture: a cross-sectional study exploring perceptions of residents at three institutions. Med Educ Online. 2019. Dec;24(1):1611296. doi: 10.1080/10872981.2019.1611296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kennedy KA, Brennan MC, Rayburn WF, Brotherton SE. Attrition rates between residents in obstetrics and gynecology and other clinical specialties, 2000-2009. J Grad Med Educ. 2013. Jun;5(2):267-71. doi: 10.4300/JGME-D-12-00141.1. PMID: 24404271; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brockberg M, Mittelman A, Dugas J, McCabe K, Spector J, Liu J, et al. Rate of programs affected by resident attrition and program factors associated with attrition in Emergency Medicine. J Grad Med Educ. 2019. Dec;11(6):663-7. doi: 10.4300/JGME-D-19-00248.1. PMID: 31871566; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sio-Aguilar JO, Jose SML, Sacdalan MDP, Ebina BA. Residency Training Programs. In: PGH Training Manual. Manila: University of the Philippines Manila-Philippine General Hospital; 2021. pp. 9-14. [Google Scholar]
- 12.Sio-Aguilar JO, Jose SML, Sacdalan MdP, Ebina BA. Postresidency Fellowship Training Programs. In: PGH Training Manual. Manila: University of the Philippines Manila-Philippine General Hospital; 2021. pp. 15-20. [Google Scholar]
- 13.Ginther DN, Dattani S, Miller S, Hayes P. Thoughts of quitting general surgery residency: factors in Canada. J Surg Educ. 2016. May-Jun;73(3):513-7. doi: 10.1016/j.jsurg.2015.11.008. PMID: 26708490. [DOI] [PubMed] [Google Scholar]
- 14.Schwed AC, Lee SL, Salcedo ES, Reeves ME, Inaba K, Sidwell RA, et al. Association of general surgery resident remediation and program director attitudes with resident attrition. JAMA Surg. 2017. Dec 1;152(12):1134-40. doi: 10.1001/jamasurg.2017.2656. PMID: 28813585; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoushhal Z, Hussain MA, Greco E, Mamdani M, Verma S, Rotstein O, et al. Prevalence and causes of attrition among surgical residents: a systematic review and meta-analysis. JAMA Surg. 2017. Mar 1;152(3):265-72. doi: 10.1001/jamasurg.2016.4086. PMID: 27973673. [DOI] [PubMed] [Google Scholar]
- 16.Lu DW, Hartman ND, Druck J, Mitzman J, Strout TD. Why residents quit: National rates of and reasons for attrition among emergency medicine physicians in training. West J Emerg Med. 2019. Mar;20(2):351-6. doi: 10.5811/westjem.2018.11.40449. PMID: 30881556; PMCID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris JB, Leibrandt TJ, Rhodes RS. Voluntary changes in surgery career paths: a survey of the program directors in surgery. J Am Coll Surg. 2003. Apr;196(4):611-6. doi: 10.1016/S1072-7515(02)01832-X. PMID: 12691942. [DOI] [PubMed] [Google Scholar]
- 18.Manriquez Gilpin M. Residency attrition rate in obstetrics and gynecology: are we losing more postgraduates today? Am J Obstet Gynecol. 2005. Nov;193(5):1804-6. doi: 10.1016/j.ajog.2005.07.083. PMID: 16260238. [DOI] [PubMed] [Google Scholar]
- 19.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009. Nov 14;374(9702):1714-21. doi: 10.1016/S0140-6736(09)61424-0. PMID: 19914516. [DOI] [PubMed] [Google Scholar]
- 20.Woolhandler S, Himmelstein DU. Administrative work consumes one-sixth of U.S. physicians' working hours and lowers their career satisfaction. Int J Health Serv. 2014;44(4):635-42. doi: 10.2190/HS.44.4.a. PMID: 25626223. [DOI] [PubMed] [Google Scholar]
- 21.Chen H, Reddy RM, Palmer SW, Coleman DM, Hoch JR, DiMusto PD, et al. Attrition rates in integrated vascular and cardiothoracic surgery residency and fellowship programs. J Vasc Surg. 2019; 69(1):236-41. doi: 10.1016/j.jvs.2018.07.074. PMID: 30455051. [DOI] [PubMed] [Google Scholar]
- 22.Steelman LA, Levy PE, Snell AF. The Feedback Environment Scale: construct definition, measurement, and validation. Educ Psychol Meas. 2004;64(1): 165-84.doi: 10.1177/0013164403258440. [DOI] [Google Scholar]
- 23.Kerr J, Slocum JW. Managing corporate culture through reward systems. Acad Manage Exec. 1987;1(2):99-107. doi: 10.5465/ame.1987.4275817. [DOI] [Google Scholar]
- 24.Nadeem M, Effendi MS, Ather MH. Attrition in surgical residency programmes: causes and effects. Arab J Uro. 2014;12(1):25-9. doi: 10.1016/j.aju.2013.07.002. PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bustraan J, Dijkhuizen K, Velthuis S, van der Post R, Driessen E, van Lith JMM, et al. Why do trainees leave hospital-based specialty training? A nationwide survey study investigating factors involved in study investigating factors involved in attrition and subsequent career choices in the Netherlands. BMJ Open.2019;9:e028631. doi: 10.1136/bmjopen-2018-028631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Phillips D. 'Alarming' Burnout Rate in General Surgery Residents. Medscape. 2016. [Google Scholar]
- 27.Bongiovanni T, Yeo H, Sosa JA, Yoo PS, Long T, Rosenthal M, et al. Attrition from surgical residency training: perspectives from those who left. Am J Surg. 2015;210(4):648-54. doi: 10.1016/j.amjsurg.2015.05.014. PMID: 26238074. [DOI] [PubMed] [Google Scholar]
- 28.Tamil Mannan SD, Heng JMJ, Andrada JA, Choon PH, Yeo HSH, Lim BL. Improving resident selection through analysis of attrition rate in SingHealth Residency. Poster presented at the Accreditation Council for Graduate Medical Education Annual Education Conference; 2018; Orlando, FL. [Google Scholar]
- 29.Oraman Y, Unakitan G, Selen U. Measuring employee expectations in a strategic human resource management research: job satisfaction. Procedia – Soc Behav Sci. 2011;24:413-20. doi: 10.1016/j.sbspro.2011.09.022. [DOI] [Google Scholar]
- 30.Schwartz RW, Haley JV, Williams C, Jarecky RK, Strodel WE, Young B, et al. The controllable lifestyle factor and students' attitudes about specialty selection. Acad Med. 1990. Mar;65(3):207-10. doi: 10.1097/00001888-199003000-00016. PMID: 2306321. [DOI] [PubMed] [Google Scholar]
- 31.Lum SK, Crisostomo AC. A comparative study of surgical training in South East Asia, Australia and the United Kingdom. Asian J Surg. 2009. Jul;32(3):137-42. doi: 10.1016/S1015-9584(09)60384-5. PMID: 19656752. [DOI] [PubMed] [Google Scholar]
- 32.Baldwin DC Jr, Daugherty SR, Eckenfels EJ. Casualties of residency training: a national study of loss and attrition. Res Med Educ. 1988; 27:112-7. PMID: 3218844. [PubMed] [Google Scholar]
- 33.Hope C, Reilly JJ, Griffiths G, Lund J, Humes D. Factors associated with attrition and performance throughout surgical training: a systematic review and meta-analysis. World J Surg. 2021. Feb;45(2):429-42. doi: 10.1007/s00268-020-05844-0. PMID: 33104833; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dallman JJ, Crandall LA, Haas WH. Factors affecting residency program dropouts. A longitudinal study. J Fla Med Assoc. 1980. Sep;67(9):833-5. PMID: 7411085. [PubMed] [Google Scholar]
- 35.Dodson TF, Webb AL. Why do residents leave general surgery? The hidden problem in today's programs. Curr Surg. 2005. Jan-Feb;62(1):128-31. doi: 10.1016/j.cursur.2004.07.009. PMID: 15708164. [DOI] [PubMed] [Google Scholar]
- 36.Wang X, Zhang W, Sheng S, Sharma R, Kamran M, Pakanati AR, et al. Residency attrition and associated characteristics, a 10-year cross specialty comparative study. Brain and Neurological Disorders. 2022;5(4). doi: 10.31579/2642-973X/028. [DOI] [Google Scholar]
- 37.Kron IL, Kaiser DL, Nolan SP, Rudolf LE, Muler WHJ, Jones RS. Can success in the surgical residency be predicted from preresidency evaluation? Ann Surg. 1985;202(6):694-5.doi: 10.1097/00000658-198512000-00005. PMID: 4073981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Papp KK, Polk HC Jr, Richardson JD. The relationship between criteria used to select residents and performance during residency. Am J Surg. 1997. Apr;173(4):326-9. doi: 10.1016/s0002-9610(96)00389-3. PMID: 9136789. [DOI] [PubMed] [Google Scholar]