Abstract
Abstract
Objective
To examine whether influenza transmission risk decreased during summer and winter vacations and increased after vacations and statutory holiday.
Design
An ecological study.
Setting
Guangzhou, Guangdong Province of China.
Participants
A total of 458 343 influenza cases in school-aged children were included, including 160 067 (35.05%) in kindergarten, 223 817 (48.83%) in primary school, 50 053 (10.92%) in middle school and 23 801 (5.19%) in high school.
Data and methods
Data on influenza cases were obtained from the Notifiable Infectious Disease Surveillance System operated by Guangzhou Centre for Disease Control and Prevention. Influenza incidence rate ratio (IRR) by negative binomial regression model was used to analyse the influenza risk of school-age children during/after vacation to before/during breaks.
Results
In all four groups, there was significantly lower incidence of influenza during winter and summer vacations compared with the 4 weeks preceding vacations. Compared with the 2 weeks preceding return, kindergarten students experienced the highest influenza risk in the third week after summer vacation (IRR=3.40, 95% CI 2.43to 4.79). Primary school students had the highest risk in the fourth week after winter vacation (IRR=9.59, 95% CI 6.71 to 13.87). Middle school students had the highest risk in the fourth week after summer (IRR=11.60, 95% CI 6.17 to 22.62). High school students also experienced the highest risk in the fourth week following summer (IRR=17.96, 95% CI 8.10 to 42.05). Despite the risk of influenza increasing after returning to school, it remained lower compared with before vacations and holidays.
Conclusions
Due to changes in contact patterns, influenza incidence was high towards the end of term, significantly decreased during vacations and started to rise on returning to school, peaking in the third or fourth week. These findings suggested using holiday periods strategically to promote influenza vaccination and implementing enhanced non-pharmaceutical interventions on students returning to school.
Keywords: Epidemiology, Public health, Infection control, Schools
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study analysed the impact of winter vacations, summer vacations and short statutory holidays on influenza infection among school-age children separately.
Quantitative analyses were conducted to compare the risk of influenza infection among students before vacations, during vacations and after returning to school.
This study categorised school-age children into four groups and calculated the infection risk for each group, respectively: kindergarten, primary school, middle school and high school.
This study primarily classified cases based on the age of the patients, which, to a certain extent, reduced the accuracy of categorising student cases.
There was no comparator population to calculate incidence rates, and this study did not adjust for key confounders such as time, COVID-19 pandemic effects or changes in case detection methods.
Introduction
Schools are critical hubs for influenza transmission, with children playing a pivotal role in spreading the virus.1 2 During the 2009–2010 period, Chinese schools experienced 2498 influenza outbreaks, constituting 90.08% of all clustered outbreaks reported in China during that period.3 Due to high population density and frequent interpersonal contact, schools pose key and challenging fronts in influenza outbreak prevention and control. At the onset of each academic year, students often bring viruses from their hometowns to campuses, resulting in increased respiratory disease cases among school-age children.4 Several studies have documented influenza outbreaks coinciding with the beginning of the school term.5 6 However, this phenomenon remained inadequately recognised and studied in China.
School closures are usually implemented as emergency interventions in response to influenza outbreaks in China. According to the Guidelines for Influenza-like Illness Outbreak Management in China, class suspension (typically lasting 4 days) may be implemented when epidemiological risk assessment indicates potential for further spread and any of the following criteria are met: (1) ≥5 newly identified influenza-like illness (ILI) cases in the class within a single day; (2) current ILI cases constitute ≥30% of class enrolment; (3) occurrence of ≥2 laboratory-confirmed influenza-related hospitalisations or fatalities occurring within 1 week. When sustained influenza outbreaks disrupt regular educational activities, the educational authority should conduct risk evaluations and implement tiered class suspension measures.
However, such school closures are strictly confined to institutions experiencing active influenza outbreaks, demonstrating reactive implementation and geographical specificity. Moreover, school closures must weigh social and economic benefits and cannot be implemented as a routine preventive measure. In contrast, scheduled summer and winter vacations, along with statutory holidays, which involve regular and proactive school closures, also affect influenza epidemic dynamics.7 8 Previous research has primarily focused on the impacts of school closures during outbreaks of infectious diseases,9,14 such as the 2009 influenza pandemic and the 2020 COVID-19 epidemic. Consequently, there is a tendency to emphasise the significant findings that school holidays can reduce virus transmission and that the return to school may increase the incidence rate of diseases. Comparatively, limited attention has been given to studies focusing on non-epidemic periods or natural trends.7 15 16
This study used daily influenza case data from Guangzhou City spanning 14 years (2010–2023) to explore the following hypotheses and quantify effect sizes: (1) influenza transmission risk decreased during summer and winter vacations, (2) transmission increased after vacations and (3) despite the postvacation increase, the risk remained lower than prevacation levels.
Methods
Study area
Guangzhou, situated in southern China, serves as the capital city of Guangdong Province. The city is divided into 11 districts spanning a total area of 7434.4 km2. By the end of 2023, the permanent resident population reached 18.82 million and registered population reached 10.56 million, including 2.43 million (23.01%) individuals under the age of 18.
Study data
Influenza is classified as a statutory infectious disease in China, mandating clinicians to report diagnosed cases online. According to Chinese guidelines for diagnosis and treatment of influenza (2018 version),17 influenza cases can be categorised as clinically diagnosed cases or confirmed cases. Clinically diagnosed cases refer to patients meeting clinical criteria of influenza with epidemiological linkage and exclusion of alternative aetiologies for influenza-like symptoms. Confirmed cases refer to patients demonstrating influenza clinical manifestations with ≥1 positive pathogen detection result (nucleic acid test, virus culture or increased IgG antibody level). This study used data obtained from the Notifiable Infectious Disease Surveillance System operated by Guangzhou Centre for Disease Control and Prevention, covering influenza cases in Guangzhou from 2010 to 2023. The dataset comprised case numbers, birthdates, symptom onset dates, diagnosis dates, gender and population categories (occupation). All analysed data underwent anonymisation procedures, excluding all personal information (eg, names, national ID numbers, telephone number and residential addresses).
Study design
This study conducted an ecological design to analyse the impact of vacations and back-to-school periods on influenza transmission among school-age children in Guangzhou from 2010 to 2023. The primary variables of interest included the timing of summer and winter vacations, statutory holidays and the back-to-school periods. The outcome of interest was the risk of influenza infection among school-age children. The negative binomial regression model was chosen due to the overdispersion observed in the influenza case data, and the incidence rate ratio (IRR) was calculated to compare influenza risk before, during and after vacations.
Relevant definitions
School-age children
In China, the school year typically commences on 1 September. Children who reach the age of 3 years by the start of the school year are eligible for kindergarten, while those who turn 6 years old can enrol in primary school, 12 years for middle school and 15 years for high school. In this study, children were categorised based on their school entry age (calculated as the difference between the school year’s starting date and their birth date) into four groups: kindergarten (3–5 years), primary school (6–11 years), middle school (12–14 years) and high school (15–17 years). Collectively, these age groups constitute school-age children (excluding university students).
Winter and summer vacations and statutory holidays
An academic year is divided into two semesters in China. The first semester, generally from September to January, incorporates a winter vacation in February. The second semester spans from March to June, with a summer vacation in July and August. Details of the specific winter and summer vacations were provided in online supplemental table S1).
To differentiate between summer and winter vacations and statutory holidays, ‘vacation’ refers to the summer and winter breaks and ‘holiday’ pertains to statutory holidays. Statutory holidays include New Year’s Day, Spring Festival, Qingming Festival, Labour Day, Dragon Boat Festival, Mid-Autumn Festival and National Day. The Spring Festival invariably falls within the winter vacation; thus, it was excluded from the holiday analysis. Children’s Day is observed only by kindergarten and primary school students. Specific dates of statutory holiday were listed in online supplemental table S2).
Adjusted working days, a distinct holiday arrangement in China, involve connecting statutory holidays with adjacent weekends to create a longer, consecutive holiday period by compensating shifts on other rest days. For example, if New Year’s Day falls on a Thursday, the government mandates a day off on Friday, requiring work on Sunday to make up for it. This study exclusively analysed the impact of statutory holidays that involve rest periods exceeding 2 days in duration.
Other covariates
To minimise the risk of confounding, we adjusted the model by incorporating mean temperature and relative humidity as covariates, based on available dataset and previous research on the relationship between the meteorological factors and paediatric influenza in Guangzhou.18 19 Meteorological data were obtained from the Guangdong Provincial Meteorological Bureau (http://gd.cma.gov.cn/). We constructed multiple models incorporating 0, 1 or 2 covariates and selected the optimal model based on the Akaike Information Criterion, with detailed results provided in online supplemental table S3-S6).
Negative binomial regression model
The negative binomial regression model was employed to characterise and predict the distribution of discrete random variables, commonly applied in medical research to forecast disease incidence rates and analyse influencing factors. Influenza cases were treated as count data, and the overdispersion test confirmed the presence of overdispersion in the influenza data. The formula for the negative binomial regression model was presented below:
where log(y) represented the log odds of the event occurrence; in represented the number of observed events; β represented the regression coefficient and ki represented the coefficient of dispersion.
The negative binomial regression model was used for the following analyses: (1) to calculate the risk of influenza incidence during summer and winter vacations compared with the 4 weeks preceding vacations; (2) to calculate the risk of influenza incidence in the first 4 weeks after returning to school from vacations compared with the 2 weeks preceding return; (3) to assess the risk of influenza incidence during the first 4 weeks after returning to school compared with the 4 weeks preceding vacations; (4) to estimate the risk of influenza incidence within 2 weeks after statutory holidays compared with the 2 weeks before holidays.
Sensitivity analysis
Given the substantially higher influenza case numbers in 2023 compared with other years, we performed sensitivity analyses by excluding this period. Replicating the aforementioned statistical methodology, we analysed influenza infection risks among school-aged children during 2010–2022.
Software and analysis
Data collection and cleaning were performed using WPS Office. No missing values were identified in the case records used for statistical analysis. Time series plots and negative binomial regression models were constructed using the ‘ggplot2’ and ‘MASS’ packages in R (V.4.2.1), respectively. IRR achieved statistical significance when its 95% CI excluded 1. IRR of during/after to before vacation <1 indicated that the number of influenza cases during/after vacation was lower than those before vacation.
Patient and public involvement statement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Results
Time series of influenza cases
Between 2010 and 2023, Guangzhou reported 458 343 influenza cases in school-aged children, including 160 672 (35.05%) in kindergarten, 223 817 (48.83%) in primary school, 50 053 (10.92%) in middle school and 23 801 (5.19%) in high school (online supplemental table S7). The total number of male cases amounted to 263 450 (57.48%), with female cases accounting for 1 94 894 cases (42.52%). The year 2023 recorded the highest number of influenza cases among school-age children (n=2 46 260), followed by 2019 with 76 027 reported cases (online supplemental table S8). The increase in cases may be associated with population growth, reduced population immunity and revisions to diagnostic criteria outlined in the Diagnosis and Treatment Protocol for Influenza (2019 Edition) issued in November 2019. The protocol emphasises the importance of epidemiological history and early aetiological testing during influenza seasons, even in cases with atypical clinical manifestations, and recognises positive antigen detection results as one of the confirmed diagnostic criteria.
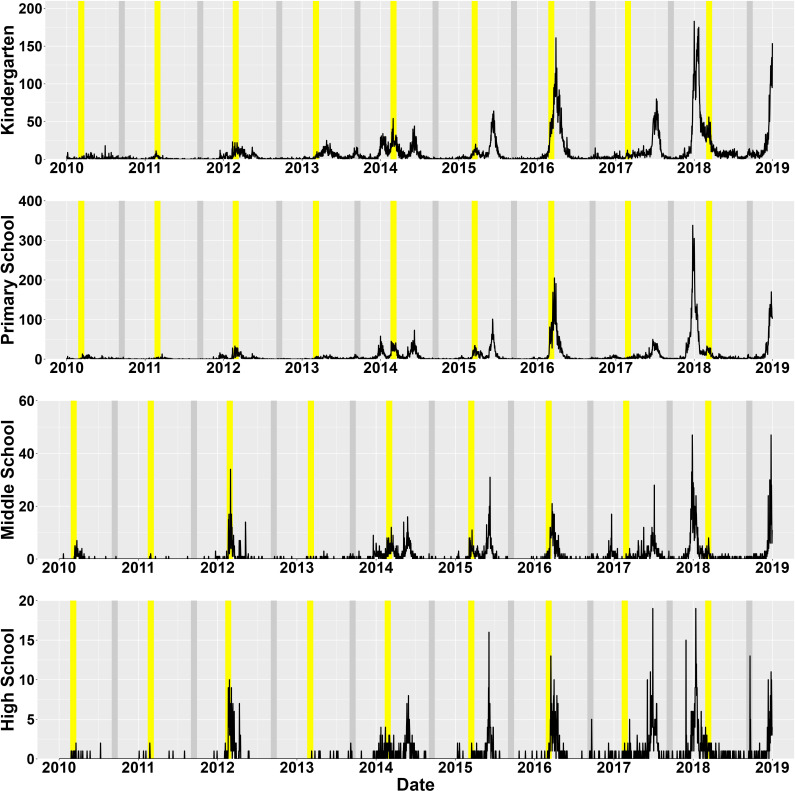
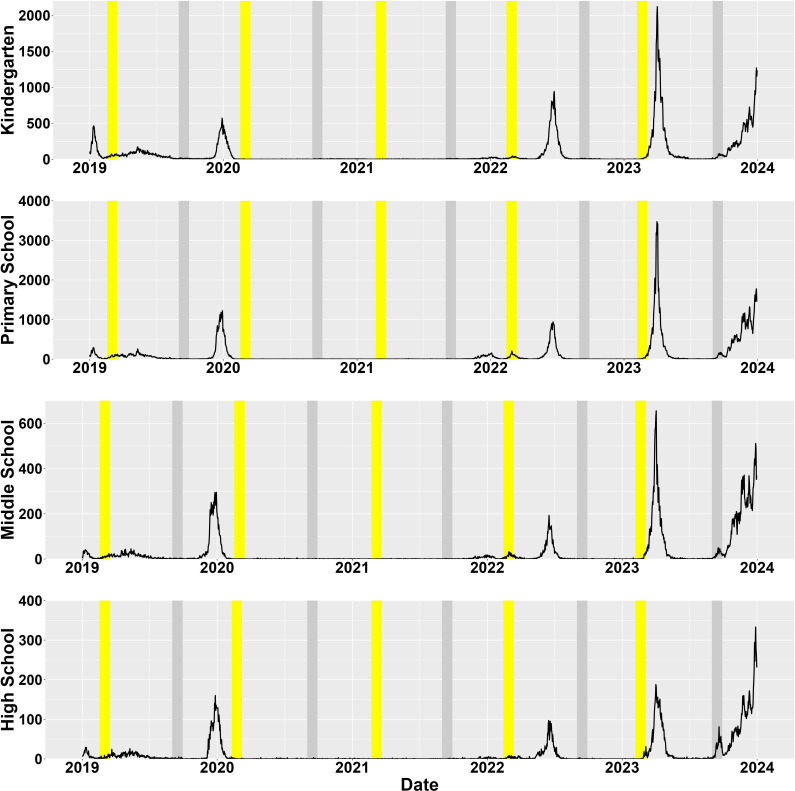
The trend in influenza cases among these age groups was similar, showing an overall fluctuating upward trend. Excluding the COVID-19 pandemic period (2020–2021), influenza case numbers during 2010–2018 (figure 1) were substantially lower than those in the 2019–2023 period (figure 2). Each year experienced a peak in winter or spring, with additional summer peaks observed in 2014, 2015, 2018 and 2023. The influenza season typically coincided with the winter vacation, and in most years, a new influenza outbreak could be observed within 4 weeks after the end of the winter vacation.
Figure 1. Time-series graph of influenza cases (per week) among school-age children in Guangzhou from 2010 to 2018. The yellow area represented the first four weeks after returning to school from winter vacations, and the grey area represented the first four weeks after returning to school from summer vacations.
Figure 2. Time-series graph of influenza cases (per week) among school-age children in Guangzhou from 2019 to 2023. The yellow area represented the first four weeks after returning to school from winter vacations, and the grey area represented the first four weeks after returning to school from summer vacations.
Influenza risk during winter and summer vacations
In all four groups, there was significantly lower incidence of influenza during winter and summer vacations compared with the 4 weeks preceding vacations. The longer the summer vacation period, the greater the reduction in influenza incidence risk among school-aged children. Primary school students had an IRR of 0.08 (95% CI: 0.06 to 0.11) during the whole summer vacation, indicating a substantial reduction in influenza risk compared with the prevacation period (table 1).
Table 1. Risk of influenza during vacations compared with the 4 weeks preceding vacations.
| Group | Summer vacation (first 4 weeks) | Summer vacation (whole vacation) | Winter vacation (whole vacation) | |||
|---|---|---|---|---|---|---|
| Irr (95% CI) | Adjusted IRR (95% CI) | Irr (95% CI) | Adjusted IRR (95% CI) | Irr (95% CI) | Adjusted IRR (95% CI) | |
| Kindergarten | 0.17 (0.13 to 0.23) | 0.19 (0.15 to 0.26) | 0.12 (0.09 to 0.15) | 0.12 (0.10 to 0.15) | 0.24 (0.18 to 0.31) | 0.28 (0.21 to 0.36) |
| Primary school | 0.12 (0.09 to 0.17) | 0.14 (0.10 to 0.19) | 0.08 (0.06 to 0.11) | 0.08 (0.06 to 0.11) | 0.09 (0.07 to 0.12) | 0.11 (0.08 to 0.15) |
| Middle school | 0.11 (0.08 to 0.17) | 0.13 (0.08 to 0.19) | 0.08 (0.06 to 0.11) | 0.08 (0.06 to 0.12) | 0.08 (0.05 to 0.11) | 0.10 (0.07 to 0.15) |
| High school | 0.12 (0.08 to 0.18) | 0.14 (0.09 to 0.21) | 0.09 (0.07 to 0.13) | 0.10 (0.07 to 0.15) | 0.10 (0.07 to 0.16) | 0.14 (0.09 to 0.22) |
Adjustment models incorporated average temperature and relative humidity.
IRR, incidence rate ratio.
Risk of back-to-school after winter and summer vacations
Following both winter and summer vacations, the influenza risks within the first 4 weeks back to school compared with the 2 weeks preceding return were statistically significant and exhibited hazardous effects across all age groups. Adjusted for temperature and humidity, the IRRs were comparable to those in the unadjusted models. Kindergarten students experienced the highest influenza risk in the third week after summer vacation (IRR=3.40, 95% CI=2.43 to 4.79) and in the fourth week after winter vacation (IRR=2.98, 95% CI=2.18 to 4.12). Primary school students had the highest risk in the third week after summer vacation (IRR=9.11, 95% CI=5.88 to 14.35) and in the fourth week after winter vacation (IRR=9.59, 95% CI=6.71 to 13.87). Middle school students had the highest risk in the fourth week after both summer (IRR=11.60, 95% CI=6.17 to 22.62) and winter vacation (IRR=10.08, 95% CI=6.51 to 15.82). High school students also experienced the highest risk in the fourth week following both summer (IRR=17.96, 95% CI=8.10 to 42.05) and winter vacation (IRR=5.92, 95% CI=3.87 to 9.16) (table 2).
Table 2. Risk of influenza in the first 4 weeks after returning to school from vacations compared with the 2 weeks preceding return.
| Back to school (weeks) | Summer vacation | Winter vacation | |||
|---|---|---|---|---|---|
| IRR (95% CI) | Adjusted IRR (95% CI) | IRR (95% CI) | Adjusted IRR (95% CI) | ||
| Kindergarten | 1 | 1.55 (1.10 to 2.22) | 1.68 (1.19 to 2.39) | 1.58 (1.15 to 2.20) | 1.48 (1.08 to 2.05) |
| 2 | 2.17 (1.54 to 3.08) | 2.17 (1.55 to 3.07) | 2.40 (1.75 to 3.34) | 2.32 (1.70 to 3.21) | |
| 3 | 3.12 (2.22 to 4.43) | 3.40 (2.43 to 4.79) | 2.57 (1.87 to 3.57) | 2.34 (1.71 to 3.24) | |
| 4 | 2.87 (2.05 to 4.08) | 3.39 (2.42 to 4.79) | 3.01 (2.19 to 4.18) | 2.98 (2.18 to 4.12) | |
| 1–4 | 2.43 (1.88 to 3.12) | 2.64 (2.05 to 3.39) | 2.39 (1.89 to 3.01) | 2.29 (1.81 to 2.87) | |
| Primary school | 1 | 2.12 (1.35 to 3.41) | 2.44 (1.56 to 3.88) | 2.88 (2.02 to 4.14) | 2.74 (1.93 to 3.93) |
| 2 | 3.34 (2.13 to 5.33) | 3.10 (1.99 to 4.92) | 5.95 (4.20 to 8.55) | 6.12 (4.32 to 8.77) | |
| 3 | 7.58 (4.86 to 12.06) | 9.11 (5.88 to 14.35) | 7.57 (5.34 to 10.88) | 8.05 (5.63 to 11.66) | |
| 4 | 6.69 (4.29 to 10.64) | 8.79 (5.69 to 13.81) | 8.45 (5.96 to 12.12) | 9.59 (6.71 to 13.87) | |
| 1–4 | 4.93 (3.50 to 6.89) | 5.80 (4.12 to 8.12) | 6.21 (4.77 to 8.04) | 6.14 (4.72 to 7.94) | |
| Middle school | 1 | 2.24 (1.16 to 4.45) | 2.96 (1.54 to 5.82) | 1.93 (1.23 to 3.08) | 1.77 (1.12 to 2.82) |
| 2 | 4.29 (2.27 to 8.40) | 3.63 (1.93 to 6.98) | 5.19 (3.37 to 8.09) | 5.11 (3.32 to 7.96) | |
| 3 | 7.97 (4.25 to 15.46) | 11.30 (6.05 to 21.83) | 7.98 (5.22 to 12.39) | 8.06 (5.18 to 12.70) | |
| 4 | 7.21 (3.84 to 13.99) | 11.60 (6.17 to 22.62) | 9.17 (6.00 to 14.21) | 10.08 (6.51 to 15.82) | |
| 1–4 | 5.43 (3.29 to 8.85) | 6.96 (4.21 to 11.48) | 6.07 (4.29 to 8.55) | 5.85 (4.14 to 8.25) | |
| High school | 1 | 1.57 (0.66 to 3.93) | 1.89 (0.78 to 4.82) | 1.31 (0.80 to 2.15) | 1.20 (0.73 to 1.97) |
| 2 | 6.94 (3.06 to 16.76) | 3.76 (1.64 to 8.94) | 1.95 (1.23 to 3.13) | 1.94 (1.22 to 3.10) | |
| 3 | 13.84 (6.14 to 33.23) | 17.34 (7.81 to 40.78) | 3.50 (2.25 to 5.50) | 3.28 (2.11 to 5.13) | |
| 4 | 12.55 (5.57 to 30.14) | 17.96 (8.10 to 42.05) | 5.95 (3.88 to 9.25) | 5.92 (3.87 to 9.16) | |
| 1–4 | 8.73 (4.48 to 16.54) | 9.75 (5.01 to 18.65) | 3.18 (2.21 to 4.56) | 3.09 (2.15 to 4.43) | |
Adjustment models incorporated average temperature and relative humidity.
IRR, incidence rate ratio.
The impact of summer and winter vacations on the spread of influenza
Following summer or winter vacations, the influenza risk decreased markedly across all age groups compared with prevacation levels. Summer vacations exerted a more substantial influence on influenza prevalence among kindergarten, primary and middle school students, whereas winter vacations had a more pronounced effect on high school students (table 3).
Table 3. Risk of influenza during the first 4 weeks after returning to school compared with the 4 weeks preceding vacations.
| Group | Summer vacation | Winter vacation | ||
|---|---|---|---|---|
| IRR (95% CI) | Adjusted IRR (95% CI) | IRR (95% CI) | Adjusted IRR (95% CI) | |
| Kindergarten | 0.12 (0.09 to 0.16) | 0.13 (0.10 to 0.16) | 0.30 (0.23 to 0.38) | 0.24 (0.19 to 0.31) |
| Primary school | 0.17 (0.12 to 0.23) | 0.16 (0.12 to 0.22) | 0.32 (0.25 to 0.42) | 0.27 (0.21 to 0.35) |
| Middle school | 0.25 (0.17 to 0.37) | 0.24 (0.16 to 0.36) | 0.24 (0.17 to 0.32) | 0.19 (0.14 to 0.26) |
| High school | 0.52 (0.33 to 0.83) | 0.50 (0.32 to 0.78) | 0.17 (0.12 to 0.25) | 0.15 (0.11 to 0.22) |
Adjustment models incorporated average temperature and relative humidity.
IRR, incidence rate ratio.
The impact of statutory holidays on the spread of influenza
In the first week following the statutory holidays, statistically significant results were observed only among high school students in the univariate model. However, in the multivariate model, all four age groups exhibited lower incidence rates. By the second week, none of the adjusted models were statistically significant for any school-age group. Cumulative effects over 2 weeks showed lower incidence rates on middle (IRR=0.76, 95%CI=0.60 to 0.97) and high school students (IRR=0.64, 95%CI=0.49 to 0.84), while no statistical significance was observed for kindergarten and primary school students (table 4).
Table 4. The risk of influenza within 2 weeks after statutory holidays compared with the 2 weeks before the holidays.
| Group | 1 week | 2 week | 1–2 week | |||
|---|---|---|---|---|---|---|
| IRR (95% CI) | Adjusted IRR (95% CI) | IRR (95% CI) | Adjusted IRR (95% CI) | IRR (95% CI) | Adjusted IRR (95% CI) | |
| Kindergarten | 0.92 (0.75 to 1.13) | 0.71 (0.58 to 0.87) | 1.35 (1.10 to 1.66) | 1.11 (0.91 to 1.37) | 1.13 (0.96 to 1.34) | 0.91 (0.77 to 1.08) |
| Primary school | 0.87 (0.70 to 1.09) | 0.72 (0.58 to 0.91) | 1.18 (0.94 to 1.47) | 1.06 (0.85 to 1.34) | 1.02 (0.85 to 1.23) | 0.89 (0.74 to 1.08) |
| Middle school | 0.77 (0.59 to 1.03) | 0.59 (0.45 to 0.79) | 1.10 (0.83 to 1.46) | 0.93 (0.71 to 1.24) | 0.94 (0.74 to 1.18) | 0.76 (0.60 to 0.97) |
| High school | 0.57 (0.41 to 0.80) | 0.46 (0.34 to 0.65) | 0.91 (0.66 to 1.28) | 0.81 (0.59 to 1.13) | 0.74 (0.56 to 0.98) | 0.64 (0.49 to 0.84) |
Adjustment models incorporated average temperature and relative humidity.
IRR, incidence rate ratio.
Sensitivity analysis
Analysis of vacation and back-to-school on influenza infection among school-age children from 2010 to 2022 was presented in online supplemental table S9-S11). A marginal elevation in infection risk was observed among students after summer vacations compared with the 2 weeks preceding return (online supplemental table S10). A notably lower incidence of influenza was observed after summer vacation compared with prevacation periods (online supplemental table S11). Other results were consistent with those from 2010 to 2023. It suggested that the substantial increase in summer 2023 cases had a huge influence on the outcomes, highlighting the necessity for enhanced containment measures when students return to school after the summer vacation.
Discussion
This study revealed a notable decrease in the risk of influenza among school-age children during summer and winter vacations. The decrease in the incidence of influenza was more pronounced with longer vacation durations, but risk increased on returning to school. This finding was consistent with research from various global contexts, primarily attributing to changes in contact patterns—reduced exposure during vacations and heightened exposure post return to school.16 20 A study in South Korea reported a 27%–39% reduction in influenza transmission during spring vacation, with an overall estimated reduction in transmission rates of 6%–23%.7 Cauchemez et al analysing surveillance data from France found that school holidays potentially lowered influenza infection rates among children by 20%–29%.21 Tamerius et al estimated an average of 14% reduction (95% CI: 10% to 19%) in influenza transmission during the spring and summer vacations in Mexico in 2009.5 Furthermore, an increase in the incidence of other diseases has been observed on returning to school. A clear association existed between the prevalence of asthma in September and the return to school after summer vacation, as evidenced in studies from Canada and the UK.22 23 Another study conducted in the UK identified an increase in rhinovirus infections among adults following the summer vacation, suggesting the potential role of children in the transmission of rhinovirus.24
This study also indicated that although the risk of influenza increased after returning to school, it remained lower compared with before the break. Similar findings were reported in other studies. Research conducted in the Oregon School District demonstrated a nearly 50% decrease in influenza A cases after winter and spring vacations compared with before the vacations.25 In contrast to the persistently high influenza incidence observed prior to holidays, school resumption was associated with a progressive increase in case numbers, requiring several weeks to return to preholiday baseline levels. These findings underscore once again the critical role of school closures in mitigating influenza transmission risks.
All four groups of school-age children in this study experienced the highest IRRs during the fourth week after winter vacations, but this did not signify the epidemic peak occurred during that week. Preliminary simulation models indicated that the heightened influenza risk post return to school could persist for 8–10 weeks, closely correlating with the annual influenza epidemic pattern across the entire population. Moreover, the accuracy of simulated risk assessments may diminish with longer study durations. On the other hand, the fifth week after summer vacation coincided with National Day, a statutory holiday entailing a 7-day break for students and workers. This may be an inflection point in the influenza epidemic curve, weakening the impact of back-to-school on influenza transmission. Therefore, this study specifically analysed the influenza risk among school-age children during the first 4 weeks following vacations.
Kindergarten students are more active and engage more frequently in community activities, coupled with poorer hygiene practices and lower innate immunity, which partly explained the relatively high incidence of influenza during summer and winter vacations among this group.26 In contrast to other school-age children, high school students experienced shorter vacation periods and faced enormous academic pressure, leading them to reduce outdoor activities considerably. They were more inclined to rest or study at home during vacations and holidays. Additionally, high school students generally exhibit stronger immune capabilities and better health awareness. However, middle and high school students exhibited higher IRR values in the third week and fourth week following winter and summer vacations compared with kindergarten and primary school students. This discrepancy could be attributed to fewer cases among middle and high school students, where even a slight increase in numbers can amplify disease risk. Therefore, although the postresumption elevation in infection risk among kindergarten and primary school students was less pronounced compared with junior and senior high school students, implementing targeted protection measures for these younger cohorts remains crucial from a public health perspective.
This study also demonstrated that, even brief statutory holidays significantly reduced influenza infection risk among school-aged children during the first postholiday week, with risk normalisation occurring by the second week. This phenomenon was similar to the ‘weekend effect’, primarily attributable to synchronised closures of workplaces and schools during holidays, which reduced interpersonal contact.27 28 Liang demonstrated that extended weekend strategies (≥3 consecutive days) effectively suppressed seasonal influenza transmission.29 Therefore, these findings suggested that statutory holidays effectively mitigate influenza transmission among students. Meanwhile, the reinforcement of postholiday preventive measures on back to school remains imperative.
School closures during influenza outbreaks typically involve additional non-pharmaceutical interventions, such as home isolation, reduced outings, frequent handwashing and active mask wearing. When combined with these measures, school closures can greatly reduce influenza cases.30 Some studies suggested that school closure may only delay the peak of influenza epidemics and had limited effectiveness in reducing total epidemic sizes.231,33 Other research indicated that if no time is appropriately or implemented without other interventions like vaccination, school closures may not effectively control outbreaks.34,36
School closures during influenza outbreaks typically involve additional non-pharmaceutical interventions, such as home isolation, reduced outings, frequent handwashing, and active mask wearing. When combined with these measures, school closures can greatly reduce influenza cases.30 Some studies suggested that school closure may only delay the peak of influenza epidemics and had limited effectiveness in reducing total epidemic sizes.231,33 Other research indicated that if no time is appropriately or implemented without other interventions like vaccination, school closures may not effectively control outbreaks.34,36
This study had substantial practical implications. First, during vacations, people do not deliberately reduce outings, self-isolate at home or wear masks voluntarily, yet vacations and holidays still reduce the risk of influenza among school-age children. This indicates that vacations notably influence influenza epidemiological patterns, suggesting that extending or adjusting vacations during influenza seasons may be advisable and beneficial. Second, influenza cases among students often increase gradually on returning to school, potentially leading to outbreaks thereafter. Vaccinating students during vacations can establish herd immunity within schools, which may substantially suppress influenza outbreaks, thereby alleviating both health and economic burdens on the population.31 Vacations provide ample time for both vaccine production and vaccination, and vaccinating children during these periods can yield maximum benefits.30 Therefore, governments should enhance vaccination policies, promote vaccines and encourage student vaccination during vacations. We hope this study will contribute to the development of influenza prevention and control policies worldwide, appealing to policymakers to prioritise respiratory infectious diseases among school-age children on their return to school and implement timely interventions.
This study had several limitations. First, cases of school-age children were categorised based on enrolment date and birthdate, thus children who had dropped out of school may not be identified and could be included in the study, and some children who started school earlier or later may be overlooked or misclassified. Second, we lacked detailed data on influenza virus strains. Virus strains were linked to epidemic patterns, and we could not further analyse whether different influenza strains were associated with vacations and back to school. Third, there was no comparator population to calculate incidence rates, which limits the ability to generalise the findings. Fourth, this study did not adjust for key confounders such as time, COVID-19 pandemic effects, socioeconomic levels, vaccination rates or changes in case detection methods. These factors may have influenced the observed trends in influenza incidence. Finally, we did not differentiate between influenza seasons. Winter vacations generally align with the influenza seasons in Guangzhou, and occasional years may experience a second peak in summer. Statutory holidays are spread across various seasons and are shorter in duration, possibly exerting less impact on influenza epidemic patterns. Therefore, the significance of distinguishing influenza seasons may be limited.
Conclusion
Due to changes in contact patterns, both long winter and summer vacations, as well as short statutory holidays, could reduce the risk of influenza transmission. Influenza incidence was high towards the end of term, significantly decreased during vacations and started to rise on returning to school, peaking in the third or fourth week. These findings suggested using holiday periods strategically to promote influenza vaccination and implementing enhanced non-pharmaceutical interventions on students returning to school.
Supplementary material
Footnotes
Funding: This work was supported by the Natural Science Foundation of Guangdong Province (2019A1515011407), Medical Science and Technology Project of Guangzhou (20201A011067, 20211A011059, 20241A011048), Guangdong Medical Science and Technology Research Project (A2019379, A2020399, B2021244). The Key Project of Medicine Discipline of Guangzhou (No. 2025–2027-11), Science and Technology Project of Guangzhou (202206080003, 2023A03J0457, 2025A03J3771).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-096341).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Ethics approval: This study involves human participants and was approved by the Ethics Committee of Guangzhou Center for Disease Control and Prevention (reference GZCDC-2018018). Case information is routinely collected through the infectious disease information system as part of infectious disease surveillance. Patient consent was not required.
Data availability statement
Data are available upon reasonable request.
References
- 1.Mossong J, Hens N, Jit M, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ewing A, Lee EC, Viboud C, et al. Contact, Travel, and Transmission: The Impact of Winter Holidays on Influenza Dynamics in the United States. J Infect Dis. 2017;215:732–9. doi: 10.1093/infdis/jiw642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shi J, Xiang N, Zhang Y, et al. Epidemiological characteristics on the clustering nature of pandemic (H1N1) 2009 in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33:62–6. [PubMed] [Google Scholar]
- 4.Perry Markovich M, Glatman-Freedman A, Bromberg M, et al. Back-to-school upper respiratory infection in preschool and primary school-age children in Israel. Pediatr Infect Dis J. 2015;34:476–81. doi: 10.1097/INF.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 5.Tamerius J, Viboud C, Shaman J, et al. Impact of School Cycles and Environmental Forcing on the Timing of Pandemic Influenza Activity in Mexican States, May-December 2009. PLoS Comput Biol. 2015;11:e1004337. doi: 10.1371/journal.pcbi.1004337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lucero MG, Inobaya MT, Nillos LT, et al. National Influenza Surveillance in the Philippines from 2006 to 2012: seasonality and circulating strains. BMC Infect Dis. 2016;16:762. doi: 10.1186/s12879-016-2087-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryu S, Ali ST, Cowling BJ, et al. Effects of School Holidays on Seasonal Influenza in South Korea, 2014-2016. J Infect Dis. 2020;222:832–5. doi: 10.1093/infdis/jiaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luca GD, Kerckhove KV, Coletti P, et al. The impact of regular school closure on seasonal influenza epidemics: a data-driven spatial transmission model for Belgium. BMC Infect Dis. 2018;18:29. doi: 10.1186/s12879-017-2934-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chowell G, Echevarría-Zuno S, Viboud C, et al. Characterizing the epidemiology of the 2009 influenza A/H1N1 pandemic in Mexico. PLoS Med. 2011;8:e1000436. doi: 10.1371/journal.pmed.1000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang KE, Lipsitch M, Shaman J, et al. The US 2009 A(H1N1) influenza epidemic: quantifying the impact of school openings on the reproductive number. Epidemiology. 2014;25:203–6. doi: 10.1097/EDE.0000000000000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chao DL, Halloran ME, Longini IM., Jr School opening dates predict pandemic influenza A(H1N1) outbreaks in the United States. J Infect Dis. 2010;202:877–80. doi: 10.1086/655810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu JT, Cowling BJ, Lau EHY, et al. School closure and mitigation of pandemic (H1N1) 2009, Hong Kong. Emerg Infect Dis . 2010;16:538–41. doi: 10.3201/eid1603.091216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsueh P-R, Lee P-I, Hsiang Chiu A-W, et al. Pandemic (H1N1) 2009 vaccination and class suspensions after outbreaks, Taipei City, Taiwan. Emerg Infect Dis . 2010;16:1309–11. doi: 10.3201/eid1608.100310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzpatrick T, Wilton A, Cohen E, et al. School Reopening And COVID-19 In The Community: Evidence From A Natural Experiment In Ontario, Canada. Health Aff (Millwood) 2022;41:864–72. doi: 10.1377/hlthaff.2021.01676. [DOI] [PubMed] [Google Scholar]
- 15.Qiao M, Zhu F, Chen J, et al. Effects of scheduled school breaks on the circulation of influenza in children, school-aged population, and adults in China: A spatio-temporal analysis. Int J Infect Dis. 2024;140:78–85. doi: 10.1016/j.ijid.2024.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Jackson C, Vynnycky E, Mangtani P. The Relationship Between School Holidays and Transmission of Influenza in England and Wales. Am J Epidemiol. 2016;184:644–51. doi: 10.1093/aje/kww083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Health Family Planning Commission of The People′s Republic of China Chinese guidelines for diagnosis and treatment of influenza (2018 version) Chin J Viral Dis. 2018;8:81–5. [Google Scholar]
- 18.Chen Z, Liu Y, Yue H, et al. The role of meteorological factors on influenza incidence among children in Guangzhou China, 2019-2022. Front Public Health. 2023;11:1268073. doi: 10.3389/fpubh.2023.1268073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guo Q, Dong Z, Zeng W, et al. The effects of meteorological factors on influenza among children in Guangzhou, China. Influenza Other Respir Viruses. 2019;13:166–75. doi: 10.1111/irv.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Litvinova M, Liu Q-H, Kulikov ES, et al. Reactive school closure weakens the network of social interactions and reduces the spread of influenza. Proc Natl Acad Sci U S A. 2019;116:13174–81. doi: 10.1073/pnas.1821298116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cauchemez S, Valleron A-J, Boëlle P-Y, et al. Estimating the impact of school closure on influenza transmission from Sentinel data. Nature. 2008;452:750–4. doi: 10.1038/nature06732. [DOI] [PubMed] [Google Scholar]
- 22.Johnston NW, Johnston SL, Norman GR, et al. The September epidemic of asthma hospitalization: school children as disease vectors. J Allergy Clin Immunol. 2006;117:557–62. doi: 10.1016/j.jaci.2005.11.034. [DOI] [PubMed] [Google Scholar]
- 23.Bundle N, Verlander NQ, Morbey R, et al. Monitoring epidemiological trends in back to school asthma among preschool and school-aged children using real-time syndromic surveillance in England, 2012-2016. J Epidemiol Community Health. 2019;73:825–31. doi: 10.1136/jech-2018-211936. [DOI] [PubMed] [Google Scholar]
- 24.Poole S, Brendish NJ, Tanner AR, et al. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med. 2020;8:e92–3. doi: 10.1016/S2213-2600(20)30502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.He C, Norton D, Temte JL, et al. Effect of planned school breaks on student absenteeism due to influenza-like illness in school aged children-Oregon School District, Wisconsin September 2014-June 2019. Influenza Other Respir Viruses. 2024;18:e13244. doi: 10.1111/irv.13244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ip DK, Lau EH, So HC, et al. A Smart Card-Based Electronic School Absenteeism System for Influenza-Like Illness Surveillance in Hong Kong: Design, Implementation, and Feasibility Assessment. JMIR Public Health Surveill. 2017;3:e67. doi: 10.2196/publichealth.6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee BY, Bedford VL, Roberts MS, et al. Virtual epidemic in a virtual city: simulating the spread of influenza in a US metropolitan area. Transl Res. 2008;151:275–87. doi: 10.1016/j.trsl.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooley P, Ganapathi L, Ghneim G, et al. Using Influenza-Like Illness Data to Reconstruct an Influenza Outbreak. Math Comput Model. 2008;48:929–39. doi: 10.1016/j.mcm.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao L. Agent-based simulation for weekend-extension strategies to mitigate influenza outbreaks. BMC Public Health. 2011;11:522. doi: 10.1186/1471-2458-11-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferguson NM, Cummings DAT, Fraser C, et al. Strategies for mitigating an influenza pandemic. Nature. 2006;442:448–52. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee BY, Brown ST, Cooley P, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16:252–61. doi: 10.1097/PHH.0b013e3181ce594e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bin Nafisah S, Alamery AH, Al Nafesa A, et al. School closure during novel influenza: A systematic review. J Infect Public Health. 2018;11:657–61. doi: 10.1016/j.jiph.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Eames KTD. The influence of school holiday timing on epidemic impact. Epidemiol Infect. 2014;142:1963–71. doi: 10.1017/S0950268813002884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cowling BJ, Lau EHY, Lam CLH, et al. Effects of school closures, 2008 winter influenza season, Hong Kong. Emerg Infect Dis . 2008;14:1660–2. doi: 10.3201/eid1410.080646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis BM, Markel H, Navarro A, et al. The effect of reactive school closure on community influenza-like illness counts in the state of Michigan during the 2009 H1N1 pandemic. Clin Infect Dis. 2015;60:e90–7. doi: 10.1093/cid/civ182. [DOI] [PubMed] [Google Scholar]
- 36.Hollingsworth TD, Klinkenberg D, Heesterbeek H, et al. Mitigation strategies for pandemic influenza A: balancing conflicting policy objectives. PLoS Comput Biol. 2011;7:e1001076. doi: 10.1371/journal.pcbi.1001076. [DOI] [PMC free article] [PubMed] [Google Scholar]