Abstract
Prior studies showed the potential of a rigid fixation, such as a trans-syndesmotic screw, to produce tibiofibular malreduction. Flexible implants, although capable of allowing forgiveness, may not provide sufficient stability for all injury patterns. To assess the malreduction forgiveness of a two-phase syndesmotic device that is designed to transition from a rigid screw construct to a flexible suture-type. Cadaveric specimens were loaded in a frame under four conditions: native (control), syndesmotic instability (injured), malreduced with engaged syndesmotic device (malreduced), and post-disengagement (disengaged). The malreduction targets were 5 mm anterior displacement, 5 mm posterior displacement, 15° of rotation, and 140 N over-compressed. Fixation was performed with a single device 20 mm proximal to the ankle, manually disengaged to allow semi-constrained motion of the syndesmosis. Weightbearing Computed Tomography (WBCT) scans were obtained, and anatomic axes of the tibia and fibula extracted to calculate tibiofibular joint position with an established orthogonal system. A total of 42 specimens were included and allocated in the four groups. Anterior and posterior malreduction demonstrated 2.50 mm (SD: ±1.37 mm) and 5.04 mm (SD: ±2.23 mm) of average malreduction. The disengaged condition resulted in average recovery of 1.79 mm (95%CI: 0.72|2.85; p = 0.0034; 72% recovery) and 1.69 mm (95%CI: 0.09|3.28; p = 0.0006; 33% recovery) toward the control position, for anterior and posterior malreduction, respectively. Rotational malreduction demonstrated 2.44° (SD: ±2.09°) of average rotational malreduction, with 1.98° (95%CI: -0.13°|4.09°; p = 0.0707; 81%) of recovery. Over-compression specimens showed average medial translation of 0.89 mm (SD: ±1.10 mm), with 0.74 mm (95%CI: 0.05|1.51; p = 0.0128; 82%) of recovery when disengaged. The two-phase syndesmotic device was able to allow partial malreduction recovery in different scenarios after transitioning to the flexible state. The use of this implant might mitigate potential surgical tibiofibular malreductions while providing the mechanical and clinical advantages of both rigid and flexible devices. Level V. Controlled laboratory study.
Subject terms: Musculoskeletal system, Diagnostic markers, Computed tomography, Ligaments
Introduction
As important and challenging as properly diagnosing syndesmotic instability is, it is equally important to restore a stable and anatomically reduced ankle syndesmosis1. Syndesmosis malreduction can have a negative impact on the ankle joint and functionality2,3. Reduction clamps and screw fixation may also cause over-compression and malalignment4, particularly if positioned in more than 15–30° of angulation axially5,6. Tibiofibular reduction cannot be reliably determined by intraoperative fluoroscopy, particularly when considering fibular external rotation7. While radiographs exhibit limitations, computed tomography (CT) and weight-bearing computed tomography (WBCT) became important tools when investigating syndesmotic instability and malreduction8–10. Bone segmentation, three-dimensional (3D) distance and coverage mappings are promising technologies showing potential to increase diagnosis and tibiofibular interaction understanding11–13. A more extensive appreciation of the syndesmosis could add in the analysis on how treatments behave in a unstable joint.
The use of flexible fixation has been demonstrated to decrease syndesmotic malreduction incidence when compared to rigid screw fixation by allowing positional correction14,15. However, it is not indicated for all injury patterns, making more rigid fixations a clinical requirement16–18. Recently, hybrid systems have become available. These implants aim to combine the benefits of a screw fixation and the flexibility of suture construct. As such, two-phase syndesmotic devices are designed to maintain rigidity during early healing, and disengage after weightbearing is resumed, allowing restoration of physiologic motion and correction of possible malalignments19,20. Still, the fundamental concept of these hybrid devices and their true capacity (as well as rigid or flexible implants) to allow recuperation from a malreduced state have not yet been tested. Therefore, this study aimed to quantify the syndesmotic malreduction forgiveness of a two-phase syndesmotic device in a cadaveric model. We hypothesized that the disengaged configuration of the device would permit significant recovery of syndesmotic malreductions in different scenarios.
Methods
This cadaveric study, that complied with Declaration of Helsinki, applied four controlled malreductions to ankle syndesmosis. Permission for the use of cadavers was obtained from the University of Iowa, and specimens were obtained from Science Care® (Science Care, Phoenix, AZ, USA). They were stabilized with rigid fixation (device engaged phase), followed by permanently disengagement for flexible state conversion. The amount of fibular recovery toward the control joint position was measured. WBCT scans were obtained at control, injured, malreduced, and disengaged timepoints (Fig. 1).
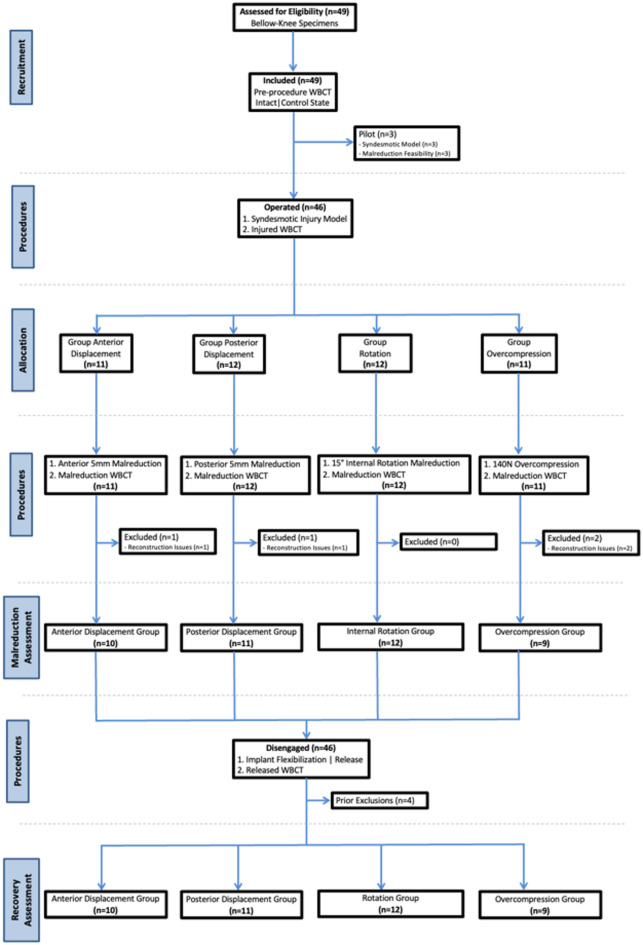
Fig. 1.
Study flowchart. WBCT weight-bearing computed tomography, N newtons, mm millimetres, n number of specimens.
Specimen preparation
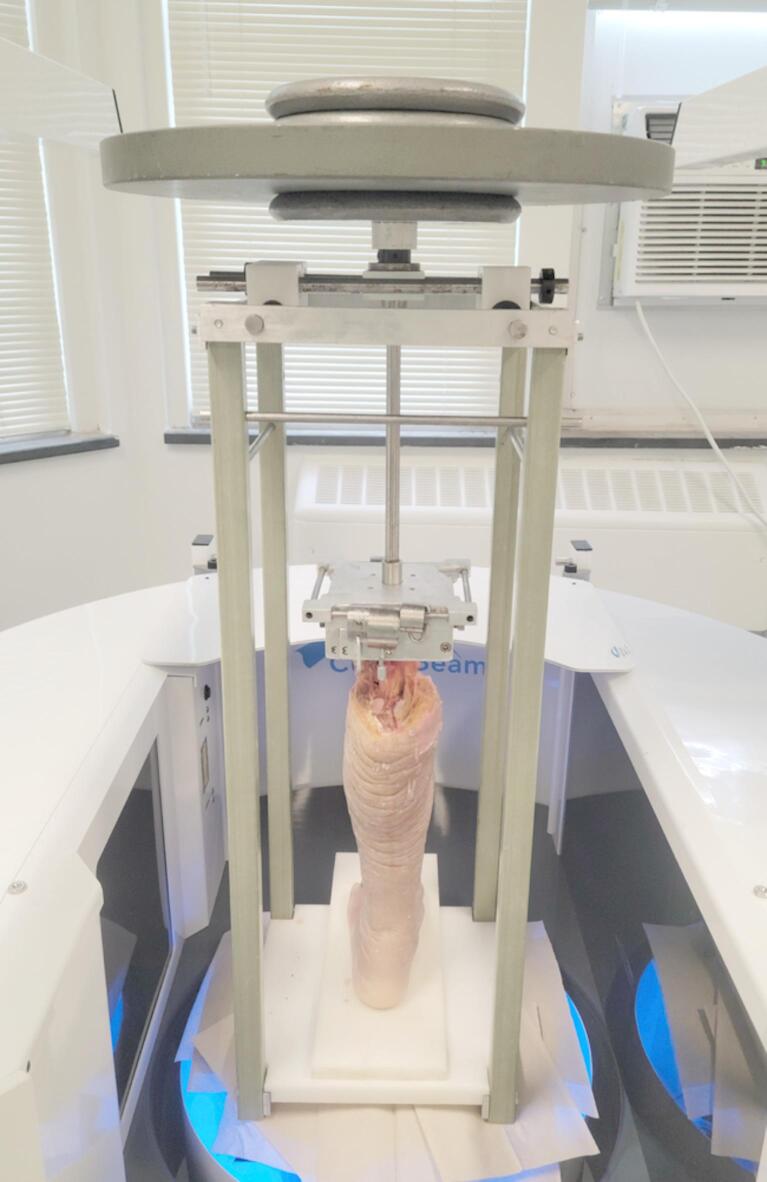
Through-knee specimens were thawed 36 h priorly the experiments and prepared resecting soft tissue (meniscus and muscle attachments) from the proximal leg while leaving the proximal tibiofibular joint intact. Specimens were examined clinically and fluoroscopically and excluded if any deformity/disease, previous fracture or surgery were found, or if imaging reconstruction issues were noted. The proximal tibia was then potted (polymethylmethacrylate) in a square block, utilized to fix the specimen vertically and in a plantigrade fashion to the external frame. The proximal fibula and tibiofibular articulation were not potted. The previously described radiolucent frame received 36.3 kg (350 N) of vertical load to replicate weightbearing (Fig. 2)21.
Fig. 2.
Broad view of the specimen placed inside WBCT scanner. The leg is secured in a simulated weightbearing state by the radiolucent external frame that hold the weights (36.3 kg) on top of the construct.
Weight-bearing CT imaging
The loaded frame with the specimen were placed in the WBCT scan (Hi-Rise™, CurveBeam LLC, Warrington), and images acquired using a metal artifact reduction sequence. Specimens were first scanned in uninjured control conditions and secondly following a syndesmotic injury model, as formerly described22,23. A third set of images was obtained after fixing an intentional fibular malpositioning with the syndesmotic device. Finally, the fourth and final scan was taken following device disengagement, allowing the malreduced fibula to potentially move into a more anatomical position.
Surgical & study procedures
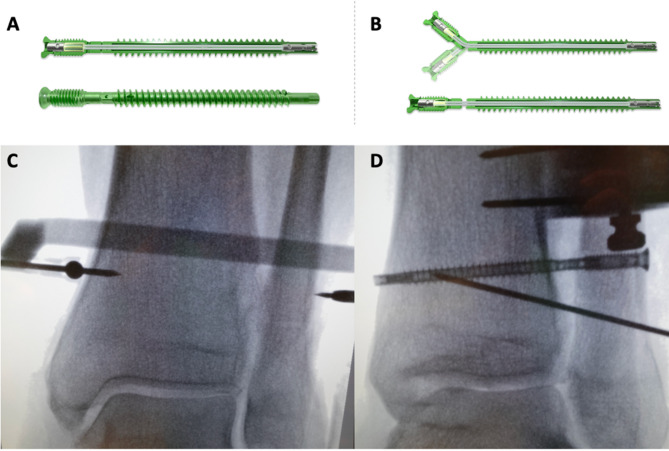
Interventions were performed by a fellowship-trained orthopedic foot and ankle surgeon. After release of all distal syndesmotic ligaments, direct confirmation of tibiofibular instability was obtained22,24,25. Fixation was performed following controlled malpositioning of the distal fibula at the incisura (anterior, posterior, rotation, over-compression). All steps were performed under fluoroscopy and provisional fixation carried with a 0.062” K-wires in a malreduced position as described below. Rigid fixation was established by inserting a single two-phase syndesmotic device (R3ACT™ Stabilization System, Paragon 28®, Englewood), placed quadri-cortically, 20 mm proximally and parallel to the ankle joint. For precise placement, a small medial approach proximal to medial malleolus apex was done. A ball tipped wire was inserted 20 mm proximally the ankle joint, five millimeters anterior to the distal tibia midline14,26. An external targeting guide was then attached to the ball-tipped wire controlling the guidewire insertion and drilling, parallel to the ankle joint, aiming 5°-10o anteriorly.
The utilized device transitions from a rigid screw construct to a flexible implant by allowing the fibular portion of the device to permanently disengage from the tibial portion within the syndesmotic space. It retains relative stability due to the internal suture contained inside the screw housing, which remains intact despite disengagement of the metal components. A thermoplastic polyurethane bumper within the device fibular portion acts as a spring-like element. It works in conjunction with the suture to allow for diastatic motion, providing up to 3 mm between the tibial and fibular sections in all directions22,27,28. The device has a 4.2 mm major diameter, with a minor of 3.2 mm in the fibula and 2.8 mm in the tibia. It was inserted through the fibula, making sure that the notch designed for disengagement was positioned in the syndesmotic joint space. Longer implants (60–70 mm in length) were utilized to ensure that the tip was quadricortical and visible through the medial approach, facilitating manual disengagement (Fig. 3). While device disengagement in-vivo is designed to occur with cyclical weightbearing, manual disengagement was required given the cadaveric nature of our investigation.
Fig. 3.
Graphical representation of the two-phase syndesmotic device. The screw housing contains an internal suture loop with a disengaging mechanism that allows the device (rigid fixation—A) to become flexible, turning into a dynamic/flexible suture-type fixation (B). The screws were 4.2 mm in external major diameter, with an internal major diameter of 3.3 mm in the fibula and 2.8 mm in the tibia. The screws were solid and had an internal suture loop with a disengaging mechanism that allowed the screw (rigid fixation) to become flexible, turning into a dynamic/flexible suture-type fixation. Repetitive cycling (load, motion) would disengage the internal mechanism. Fluoroscopic image showing the external ball-tipped guide wire and the targeting guide for the syndesmotic device (C) and the device inserted through the fibula and tibia with the disengagement notch positioned in the syndesmotic space (D).
After WBCT imaging in the malreduced position, the fibular and tibial portions were separated by applying opposing torque to both ends of the device. For each specimen, a sequence of 10 full range of motion cycles from maximum plantarflexion to dorsiflexion was performed manually to allow full device release and fibula mobilization. The final WBCT was then performed to assess fibular recovery from the malreduced state toward the control position.
Induced syndesmotic malreduction
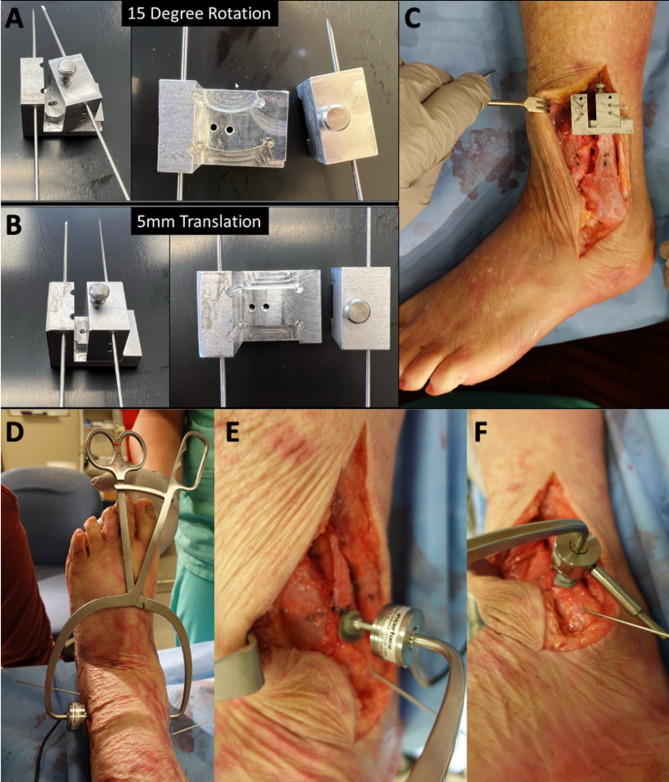
Four types of syndesmotic malreduction were induced in the specimens: anterior displacement, posterior displacement, internal rotation, and over-compression (Figs. 4 and 5)4,29. Anterior displacement was performed using a custom jig designed to translate the fibula in a single direction. The jig was positioned on the lateral aspect of the ankle, two 0.062” k-wires were introduced through the jig holes into the fibula and two into the tibia before ligaments section. After release, the jig was opened, allowing controlled fibular anterior translation by 5 mm30,31. Posterior displacement was performed similarly, with jig opening in the opposite direction.
Fig. 4.
External jigs for induced malrotation (A) and anterior/posterior displacement (B). Example of induced posterior fibular displacement (C). Example of overcompression (D) with the load-cell controlled compression (E, F) clamp (above 140 N).
Fig. 5.
Examples of weightbearing CT images (axial plane) of control and injured ankles as well as induced over-compression, rotation, posterior displacement, and anterior displacement. Top row images demonstrating displacement 1 cm proximal to the ankle, middle row at the level of the device, and bottom row with the disengaged state, demonstrating partial correction of the syndesmotic malreduction.
Another custom jig was used for internal rotation of the fibula. It was also positioned on the lateral ankle and fixed with four 0.062” k-wires into tibia and fibula before injury. Once ligaments were released, the jig was opened, rotating the fibula internally by 15°32. Over-compression malreduction was performed using a custom reduction clamp that allowed continuous control of the applied compression torque. The clamp was equipped with a 500 N load cell calibrated for a 0–180 N range. It had two tines that were positioned in the distal aspects of the medial tibia and lateral fibula. To decrease the chances of bone failure at the clamp tines, washers were utilized to increase contact area between clamp and bone. Provisional and final fixation were performed while maintaining the clamp compression force at 140 N4,33.
Anatomical axes
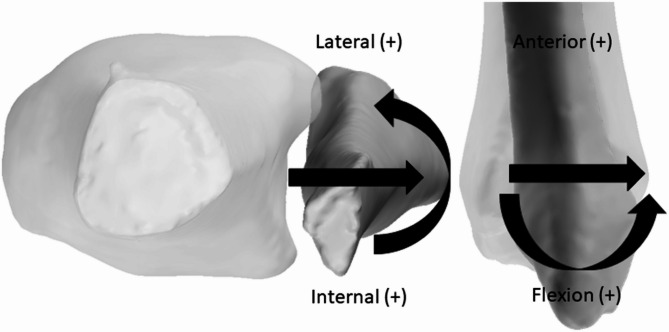
Semi-automated segmentation of the tibia and fibula using a software package (Bonelogic™, Disior®, Paragon 28®, Englewood) was carried. Models were verified and finalized to remove imperfections. Custom MATLAB code (MathWorks Inc®, Natick) was used to calculate tibiofibular joint pose using extracted automatic bony axes with an established orthogonal joint coordinate system (Fig. 6)34. Control bones/axes from tibia and fibula were registered to other conditions (injured, malreduced, and disengaged) to improve axes correspondence between different trials. Output data was normalized to control states and compared across specimens and malreduction scenarios. The tibiofibular position, and the amount of recovery (difference between malreduced and disengaged states) achieved along of the primary axis of the induced malignment were calculated. Secondarily, a binary evaluation (closer or further to control state) was carried to assess change in pose between malreduced and disengaged states. The tibia was overlaid for different limb conditions to visualize and verify kinematic descriptions.
Fig. 6.
Visualization of anatomical joint coordinate system and positive translations and rotations as perceived by the fibula. Figure was created using MATLAB R2022b (Mathworks, Natick, MA. https://www.mathworks.com/).
Statistical analysis
Shapiro-Wilk tests were conducted to assess normality of the data. Mean changes between malreduced and disengaged states were compared using paired t-tests or Wilcoxon signed rank test. Analyses were performed using RStudio (v2023.09.01, Posit®, PBC, Boston, MA). Confidence intervals were calculated, and statistical significance was determined for p values under 0.05.
Results
From the initial 49 limbs, 3 were used in the pilot and 4 were excluded due to imaging reconstruction issues. The 42 final sample (13 female) had a mean age of 73.37 years (31–91) and a BMI of 24.92 kg/m2 (SD: 5.28). A total of 10 specimens were assessed in the anterior displacement, 11 in the posterior displacement, 12 in the rotation and 9 in the over-compression groups (Fig. 1). Findings from the groups’ post-hoc analysis yielded power values (1-β) of 0.936 for the anterior, 0.993 for the posterior, 0.445 for the rotation and 0.894 for the over-compression.
Anterior displacements specimens demonstrated 2.50 mm (SD: ±1.37 mm) of average translation relative to the control at the rigid malreduced timepoint. The disengaged condition showed 0.71 mm (SD: ±1.04 mm) anterior translation relative to control position, resulting in a significant recovery (p = 0.0034) of 1.79 mm (95%CI: 0.72 mm, 2.85 mm); a 72% change (Table 1). All specimens (100%) achieved an anterior/posterior (AP) position that was closer to the control after disengagement. The posterior displacement group sustained 5.04 mm (SD: ±2.23 mm) translation relative to the control, while the disengaged state had 3.35 mm (SD: ±1.52 mm) posterior translation relative to control. A significant decrease (p = 0.0006) of 1.69 mm (95%CI: 0.09 mm, 3.28 mm) was noted, 33% of recovery. The AP position after disengagement of was closer to the intact position in 91% (10/11) of the limbs.
Table 1.
Mean and standard deviation of the malreduced and disengaged joint pose information relative to the control state. Recovery is the difference between malreduced and the disengaged. Anterior, posterior, and rotation malreduction results are described along the respective degree of freedom, over-compression is described along the medial-lateral degree of freedom.
| Malreduction patterns | n | Malreduced | Disengaged | Recovery | Recovery significance |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p-value | ||
| Anterior (mm) | |||||
| A(+) P(−) | 10 | 2.50 (1.37) | 0.71 (1.04) | − 1.79 (1.44) | 0.0034 |
| Posterior (mm) | |||||
| A(+) P(−) | 11 | − 5.04 (2.23) | − 3.35 (1.52) | 1.69 (1.14) | 0.0006 |
| Rotation (°) | |||||
| I(+) E(−) | 12 | 2.44 (2.09) | 0.46 (2.70) | 1.97 (3.42) | 0.0707 |
| Over-compression (mm) | |||||
| L(+) M(−) | 9 | − 0.89 (1.10) | − 0.16 (0.49) | 0.74 (0.78) | 0.0128 |
mm: millimeters; n: number of specimens; A: anterior (positive values); P: posterior (negative values); I: internal (positive values); E: external (negative values); L: lateral (positive values). M: medial (negative values).
Rotational malreduction specimens demonstrated 2.44° (SD: ±2.09°) of malreduction relative to the control state. After disengagement, internal rotation was 0.46° (SD: ±2.70°) relative to control. A non-significant (p = 0.0707) 1.98° (95%CI: -0.13°, 4.09°) change was found, 81% of recovery. Seven of 12 specimens had a position closer to the control after disengagement. Over-compression specimens demonstrated average medial translation of 0.89 mm (SD: ±1.10 mm) relative to the control position at the malreduced timepoint and 0.16 mm (SD: ±0.49 mm) relative to the control at the disengaged timepoint. A 0.73 mm (95%CI: 0.05 mm, 1.51 mm) significant (p = 0.0128) positional change was noted, a 82% recovery (Table 1). After disengagement, the medial/lateral position was closer to the intact position in 89% (8/9) of the limbs (Fig. 7).
Fig. 7.
Anatomic axes configurations exemplified by each malreduction pattern and situation. In these examples, axes were compared between the control (grey) and malreduction (purple) states. Vectors and positions are represented by colored lines. (A) Anterior malreduction. (B) Posterior malreduction. (C) Malrotation. (D) Over-compression. Figure was created using MATLAB R2022b (Mathworks, Natick, MA. https://www.mathworks.com/).
Discussion
This cadaveric study aimed to assess the capability of a two-phase syndesmotic device in allowing recovery after syndesmotic malreduction using 3D WBCT bone axis. The device permitted partial restoration towards the native joint position when anterior displacement, posterior displacement and over-compression were induced; however, it did not show significant improvement with malrotation. These results do not fully confirm our hypothesis.
Several studies have examined syndesmotic malreduction employing different measurement techniques35–39. Using a CT axial view 1 cm proximal to the joint, Gardner et al. defined differences among the fibula and the anterior and posterior tibial facets above 2 mm as abnormal38. Nault et al. proposed several measurements to assess the tibiofibular interface, including distances and angulations, settling normality on 8.70° (SD: ±3.1°) internal rotation39. Hennings et al. used over 2 mm in tibiofibular clear space and a 5° in translation as characterizations for a malreduced syndesmosis35. By using this metric, they could not find differences among treatments with screws and suture buttons35. However, Kubik et al. tested current measurements in normal bilateral ankles with conventional CT, finding that 35% of normal ankles would be considered false positives for syndesmotic malalignment if compared to its contralateral side37. This highlights the differences and particularities of the measurements utilized to assess syndesmotic malpositioning, emphasizing the need for a more comprehensive 3D evaluation of tibiofibular alignment.
The potential advantage of flexible syndesmotic fixation for correction of iatrogenic syndesmotic malreduction has been discussed40,41. Song et al. analyzed nine patients initially malreduced with screws, finding that 89% restored proper alignment after screw removal38,40. Baek et al. observed no changes in radiographic parameters after screw removal; however, using CT, a 71.4% spontaneous syndesmotic reduction was noted36,41. The theoretical superiority of flexible devices in allowing natural motion and, therefore, lower malreduction rates was challenged by recent studies showing a number of mispositioned syndesmoses42–44. Kortekangas et al., in a clinical trial involving 43 patients with Weber C fractures, found one malreduction in the screw group and seven in the flexible group using intraoperative CT43. Subsequent open exploration noticed good reduction in all flexible patients when in dorsiflexion, demonstrating some recoverability for suture-bottons43. Two-year postoperative WBCT indicated three malreductions with screws and one with flexibles43. Although having a 10.4% hardware removal rate, no study have assessed syndesmotic position changes following suture-type fixation removal44. Our results demonstrate partial recovery between the rigidly fixed malpositioned and the disengaged dynamic states, sustaining the concept of a closer anatomical positioning return once the device was disengaged. Most importantly, the amount of percentual recovery (72% for anterior, 33% for posterior, 81% for rotation, and 82% for over-compression) also indicates a closer control position after the rigid fixation transitioned to the suture. Although these findings lack direct clinical correlation, they support the argument that controlled motion afforded by the flexible device may provide improved tibiofibular positioning without the need for secondary hardware removal.
While significant fibular recovery was noted, complete return to the control/uninjured state was not observed. These results imply that the tibiofibular relation was not entirely reestablished, echoing previously published data. Spindler et al., retrospectively analyzed bone tunnels produced by flexible implants, observing a 35.4% intraoperative malreduction rate45. That was decreased to 17% postoperatively, showing the implants’ compensatory nature, but not a complete recovery45. Using postoperative CT, Hennings et al. noticed malreductions in 18% of suture-buttons and 37% of screws46. Unlike other studies, we present cadaveric data that cannot be extrapolated to an in vivo situation, as motion and ligament healing might contribute to a more stable and anatomical final fibular position.
The rotational recovery did not reach statistical significance (p = 0.0707), what may be attribute in part due to difficulties attempting to rotate the fibula. Average malrotation was 2.44°, well short of the planned 15°. Induced malrotation relative to the injured condition of less than 1° was seen in 4 limbs. Anterior displacement also did not reach the full translation in some specimens (2.50 mm; SD ± 1.37 mm). These challenges were likely due to the inherent tibiofibular morphological conformity and constraints from remaining structures (proximal ligaments). It is also possible that the applied rotation led to torsion of the fibula or deformation of the k-wires, leading to a discrepancy between applied and calculated angulation. Another aspect might be the inherent device capability to allow recovery to a certain amount, potentially falling short in severe scenarios such as the study’s. Maximal tension of the inner sutures and implant edges shearing are potential explanations.
Our work has other important limitations. Initially, it was a cadaveric study using a syndesmotic instability model that might not represent the myriad of injury scenarios47,48. Secondly, fixation was carried with only one type of implant, making the data less applicable to other fixations. However, the utilization of a device composed of a screw and a suture allowed us to assess rigid and dynamic fixation in the same specimens. Further, although we performed a post-hoc power analysis, our study might be underpowered to detect subtle (and potentially clinically relevant) changes when comparing subgroups. WBCT portrays a static assessment of the tibiofibular interaction and might not completely capture the dynamics of the ankle and the syndesmosis. Finally, we were unable to malrotate the fibula as desired, which could explain the lack of difference in this group.
Conclusion
In this cadaveric study without healing, dynamization of a hybrid syndesmosis fixation device resulted in partial passive correction of syndesmotic malreduction. The findings support the recovery concept in multiple planes, potentially impacting the clinical management of these injuries. Questions about limits of passive correction and comparative performance with rigid or flexible implants are yet to be answered. Assessment of the device in a cohort of patients using this methodology is also a paramount to support in vitro results.
Author contributions
NSBM: had full access to all the data in the study and takes responsibility for the integrity and accuracy of the data analysis. Literature revision, study design, writing, paper submissions and data collecting.DH: writing, data collecting and paper submission. JK: co- supervisor, literature revision, data collecting, writing.KAMC: experimentations, literature revision, writing.KD: experimentations, data collecting literature revision.CCN: supervisor. Literature revision, writing, study design and paper submissions.
Funding
This study was partially funded by a Paragon 28 research Grant.
Data availability
According to the ICMJE data sharing police, the datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Competing interests
The study was partially funded by a Paragon 28 grant. Implants used in this study were also from Paragon 28.Individual Competing Interests: Nacime Salomao Barbachan Mansur, MD, PhDBrazilian Foot and Ankle Society: Board or committee memberAmerican Orthopaedic Foot and Ankle Society: Board or committee memberJohn Y Kwon, MDDJ Orthopaedics: IP royalties; Paid consultantMedline: IP royaltiesParagon 28: IP royalties; Paid consultantRestor3D: Paid consultantTrimed: IP royaltiesCesar De Cesar Netto, MD, PhDAmerican Orthopaedic Foot and Ankle Society: Board or committee memberCurveBeam: Paid consultant; Stock or stock OptionsFoot and Ankle International: Editorial or governing boardNextremity: Paid consultantOssio: Paid consultantParagon 28: IP royalties; Paid consultantWeightbearing CT International Study Group: Board or committee memberZimmer: Paid consultant The other authors have nothing to disclosure.All authors have completed the ICMJE uniform disclosure form (www.icmje.org/coi_disclosure) and declare no support from any organization for the submitted work; Other authors have no financial relationships with any organizations that might have an interest in the submitted work in the previous ten years; no other relationships or activities that could appear to have influenced the submitted work.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harris, M. C. et al. Prospective results of the modified glide path technique for improved syndesmotic reduction during ankle fracture fixation. Foot Ankle Int.43 (7), 923–927. 10.1177/10711007221081868 (2022). [DOI] [PubMed] [Google Scholar]
- 2.Veen, E. J. & Zuurmond, R. G. Mid-term results of ankle fractures with and without syndesmotic rupture. Foot Ankle Surg.21 (1), 30–36. 10.1016/j.fas.2014.09.001 (2015). [DOI] [PubMed] [Google Scholar]
- 3.Hunt, K. J., Goeb, Y., Behn, A. W., Criswell, B. & Chou, L. Ankle joint contact loads and displacement with progressive syndesmotic injury. Foot Ankle Int.36 (9), 1095–1103. 10.1177/1071100715583456 (2015). [DOI] [PubMed] [Google Scholar]
- 4.Goetz, J. E., Rungprai, C., Rudert, M. J., Warth, L. C. & Phisitkul, P. Screw fixation of the syndesmosis alters joint contact characteristics in an axially loaded cadaveric model. Foot Ankle Surg.25 (5), 594–600. 10.1016/j.fas.2018.05.003 (2019). [DOI] [PubMed] [Google Scholar]
- 5.Miller, A. N., Barei, D. P., Iaquinto, J. M., Ledoux, W. R. & Beingessner, D. M. Iatrogenic syndesmosis malreduction via clamp and screw placement. J. Orthop. Trauma.27 (2), 100–106. 10.1097/BOT.0b013e31825197cb (2013). [DOI] [PubMed] [Google Scholar]
- 6.Miller, A. N. et al. Direct visualization for syndesmotic stabilization of ankle fractures. Foot Ankle Int.30 (5), 419–426. 10.3113/FAI.2009.0419 (2009). [DOI] [PubMed] [Google Scholar]
- 7.Marmor, M., Hansen, E., Han, H. K., Buckley, J. & Matityahu, A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot Ankle Int.32 (6), 616–622. 10.3113/fai.2011.0616 (2011). [DOI] [PubMed] [Google Scholar]
- 8.de Cesar Netto, C., Valderrabano, V. & Mansur, N. S. B. Multidirectional Chronic Ankle Instability: What Is It? Foot and Ankle Clinics. (2023). 10.1016/j.fcl.2023.01.012 [DOI] [PubMed]
- 9.Elghazy, M. A. et al. Screw versus suture button in treatment of syndesmosis instability: comparison using weightbearing CT scan. Foot Ankle Surg.27 (3), 285–290. 10.1016/j.fas.2021.01.001 (2021). [DOI] [PubMed] [Google Scholar]
- 10.Abdelaziz, M. E. et al. Evaluation of syndesmosis reduction on CT scan. Foot Ankle Int.40 (9), 1087–1093. 10.1177/1071100719849850 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Ashkani Esfahani, S. et al. Volume measurements on weightbearing computed tomography can detect subtle syndesmotic instability. J. Orthop. Res.40 (2), 460–467. 10.1002/jor.25049 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beisemann, N. et al. Detection of fibular rotational changes in cone beam CT: experimental study in a specimen model. BMC Med. Imaging. 22 (1), 181. 10.1186/s12880-022-00913-3 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhimani, R. et al. Utility of volumetric measurement via Weight-Bearing computed tomography scan to diagnose syndesmotic instability. Foot Ankle Int.41 (7), 859–865. 10.1177/1071100720917682 (2020). [DOI] [PubMed] [Google Scholar]
- 14.Westermann, R. W. et al. The effect of suture-button fixation on simulated syndesmotic malreduction: a cadaveric study. J. Bone Joint Surg. Am.96 (20), 1732–1738. 10.2106/JBJS.N.00198 (2014). [DOI] [PubMed] [Google Scholar]
- 15.Güvercin, Y., Abdioğlu, A. A., Dizdar, A., Yaylacı, E. U. & Yaylacı, M. Suture button fixation method used in the treatment of syndesmosis injury: A Biomechanical analysis of the effect of the placement of the button on the distal tibiofibular joint in the mid-stance phase with finite elements method. Injury53 (7), 2437–2445. 10.1016/j.injury.2022.05.037 (2022). [DOI] [PubMed] [Google Scholar]
- 16.Barbachan Mansur, N. S., Godoy-Santos, A. L. & Schepers, T. High-Ankle sprain and syndesmotic instability: how Far have we come with diagnosis and treatment?? Foot and ankle clinics. (2023). 10.1016/j.fcl.2023.01.006 [DOI] [PubMed]
- 17.Regauer, M., Mackay, G., Nelson, O., Böcker, W. & Ehrnthaller, C. Evidence-Based surgical treatment algorithm for unstable syndesmotic injuries. J. Clin. Med.11 (2), 331. 10.3390/jcm11020331 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schermann, H. et al. Comparison of several combinations of suture tape reinforcement and suture button constructs for fixation of unstable syndesmosis. J. Am. Acad. Orthop. Surg.30 (10), e769–e78. 10.5435/jaaos-d-21-00508 (2022). [DOI] [PubMed] [Google Scholar]
- 19.Gadomski, B. C. et al. A large animal model for orthopedic foot and ankle research. Front. Veterinary Sci.910.3389/fvets.2022.816529 (2022). [DOI] [PMC free article] [PubMed]
- 20.Gennis, E., Koenig, S., Rodericks, D., Otlans, P. & Tornetta, P. 3 The fate of the fixed syndesmosis over time. Foot Ankle Int.36 (10), 1202–1208. 10.1177/1071100715588186 (2015). [DOI] [PubMed] [Google Scholar]
- 21.Lalevée, M. et al. Impact of first metatarsal hyperpronation on first ray alignment: A study in cadavers. Clin. Orthop. Relat. Res.10.1097/corr.0000000000002265 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Cesar Netto, C. et al. Syndesmotic malreduction assessment using Three-Dimensional distance mapping: A cadaveric WBCT study. Foot Ankle Orthop.7 (4), 2473011421S00646. 10.1177/2473011421S00646 (2022). [Google Scholar]
- 23.de Cesar Netto, C. et al. Cadaveric diagnostic study of subtle syndesmotic instability using a 3-Dimensional Weight-Bearing CT distance mapping algorithm. J. Bone Joint Surg. Am.10.2106/jbjs.24.00199 (2024). [DOI] [PubMed] [Google Scholar]
- 24.Takahashi, K. et al. Comparison of treatment methods for syndesmotic injuries with posterior tibiofibular ligament ruptures: A cadaveric Biomechanical study. Orthop. J. Sports Med.10 (9), 23259671221122811. 10.1177/23259671221122811 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mococain, P. et al. Biomechanical effect on joint stability of including deltoid ligament repair in an ankle fracture soft tissue injury model with deltoid and syndesmotic disruption. Foot Ankle Int.41 (9), 1158–1164. 10.1177/1071100720929007 (2020). [DOI] [PubMed] [Google Scholar]
- 26.McBryde, A. et al. Syndesmotic screw placement: a Biomechanical analysis. Foot Ankle Int.18 (5), 262–266. 10.1177/107110079701800503 (1997). [DOI] [PubMed] [Google Scholar]
- 27.Cassinelli, S. J. et al. Use of anatomical landmarks in ankle arthroscopy to determine accuracy of syndesmotic reduction: A cadaveric study. Foot Ankle Spec.13 (3), 219–227. 10.1177/1938640019846972 (2020). [DOI] [PubMed] [Google Scholar]
- 28.LaMothe, J. et al. Effect of complete syndesmotic disruption and deltoid injuries and different reduction methods on ankle joint contact mechanics. Foot Ankle Int.38 (6), 694–700. 10.1177/1071100717696360 (2017). [DOI] [PubMed] [Google Scholar]
- 29.Boszczyk, A., Kwapisz, S., Krummel, M., Grass, R. & Rammelt, S. Correlation of Incisura anatomy with syndesmotic malreduction. Foot Ankle Int.39 (3), 369–375. 10.1177/1071100717744332 (2018). [DOI] [PubMed] [Google Scholar]
- 30.Bhimani, R. et al. Arthroscopic assessment of syndesmotic instability: are we pulling correctly in the coronal plane? Foot Ankle Surg.29 (1), 67–71. 10.1016/j.fas.2022.09.007 (2023). [DOI] [PubMed] [Google Scholar]
- 31.Gebremeskel, M. et al. Quantification of manipulation forces needed for robot-assisted reduction of the ankle syndesmosis: an initial cadaveric study. Int. J. Comput. Assist. Radiol. Surg.17 (12), 2263–2267. 10.1007/s11548-022-02705-0 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beisemann, N. et al. Detection of fibular rotational changes in cone beam CT: experimental study in a specimen model. BMC Med. Imaging. 22 (1). 10.1186/s12880-022-00913-3 (2022). [DOI] [PMC free article] [PubMed]
- 33.Haynes, J. et al. Increased reduction clamp force associated with syndesmotic overcompression. Foot Ankle Int.37 (7), 722–729. 10.1177/1071100716634791 (2016). [DOI] [PubMed] [Google Scholar]
- 34.Grood, E. S. & Suntay, W. J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J. Biomech. Eng.105 (2), 136–144. 10.1115/1.3138397 (1983). [DOI] [PubMed] [Google Scholar]
- 35.Hennings, R. et al. Suture button versus syndesmotic screw in ankle fractures - evaluation with 3D imaging-based measurements. BMC Musculoskelet. Disord.22 (1). 10.1186/s12891-021-04834-0 (2021). [DOI] [PMC free article] [PubMed]
- 36.Pelton, K., Thordarson, D. B. & Barnwell, J. Open versus closed treatment of the fibula in Maissoneuve injuries. Foot Ankle Int.31 (7), 604–608. 10.3113/fai.2010.0604 (2010). [DOI] [PubMed] [Google Scholar]
- 37.Kubik, J. F. et al. Assessment of malreduction standards for the syndesmosis in bilateral CT scans of uninjured ankles. Bone Joint J.103-b (1), 178–183. 10.1302/0301-620x.103b1.Bjj-2020-0844.R1 (2021). [DOI] [PubMed] [Google Scholar]
- 38.Gardner, M. J., Demetrakopoulos, D., Briggs, S. M., Helfet, D. L. & Lorich, D. G. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int.27 (10), 788–792. 10.1177/107110070602701005 (2006). [DOI] [PubMed] [Google Scholar]
- 39.Nault, M-L., Hébert-Davies, J., Laflamme, G-Y. & Leduc, S. CT scan assessment of the syndesmosis: A new reproducible method. J. Orthop. Trauma. 27 (11), 638–641. 10.1097/BOT.0b013e318284785a (2013). [DOI] [PubMed] [Google Scholar]
- 40.Song, D. J. et al. The effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint. Foot Ankle Int.35 (6), 543–548. 10.1177/1071100714524552 (2014). [DOI] [PubMed] [Google Scholar]
- 41.Baek, J. H., Kim, T. Y., Kwon, Y. B. & Jeong, B. O. Radiographic change of the distal tibiofibular joint following removal of transfixing screw fixation. Foot Ankle Int.39 (3), 318–325. 10.1177/1071100717745526 (2018). [DOI] [PubMed] [Google Scholar]
- 42.T, K., B, J. E., K, K. & H, M. J. COMPLICATIONS OF ANKLE SYNDESMOSIS STABILISATION USING A TIGHTROPE. Orthop. Proc.93-B (SUPP_I), 62. 10.1302/0301-620X.93BSUPP_I.0930062e (2011). [Google Scholar]
- 43.Kortekangas, T. et al. A prospective randomised study comparing tightrope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury46 (6), 1119–1126. 10.1016/j.injury.2015.02.004 (2015). [DOI] [PubMed] [Google Scholar]
- 44.Schulte, S. S. et al. Suture button versus screw fixation for distal tibiofibular injury and expected value decision analysis. Cureus10.7759/cureus.19890 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Spindler, F. T., Gaube, F. P., Böcker, W., Polzer, H. & Baumbach, S. F. Compensation of dynamic fixation systems in the quality of reduction of distal tibiofibular joint in acute syndesmotic complex injuries: A CT-Based analysis. Foot Ankle Int.43 (11), 1393–1401. 10.1177/10711007221115193 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hennings, R. et al. Flexible nature of fixation in syndesmotic stabilization of the inferior tibiofibular joint affects the radiological reduction outcome. Int. Orthop.10.1007/s00264-022-05550-7 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.de Cesar Netto, C. CORR Insights®: can weightbearing Cone-beam CT reliably differentiate between stable and unstable syndesmotic ankle injuries?? A systematic review and Meta-Analysis. Clin. Orthop. Relat. Res.10.1097/corr.0000000000002223 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raheman, F. J. et al. Can weightbearing Cone-beam CT reliably differentiate between stable and unstable syndesmotic ankle injuries?? A systematic review and Meta-analysis. Clin. Orthop. Relat. Res.10.1097/corr.0000000000002171 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
According to the ICMJE data sharing police, the datasets used and analyzed during the current study are available from the corresponding author on reasonable request.