Abstract
Objective
This study assesses the diagnostic value of preoperative greyscale and Doppler imaging and their combinative use with simultaneous advanced Doppler imaging and cervical maneuvers in detecting central cervical lymph node metastasis in papillary thyroid carcinoma patients.
Methods
In this cross-sectional survey, we included candidates for total or partial thyroidectomy with concomitant cervical lymph node dissection who referred to the TIRAD imaging center from February 2022 to September 2023 with papillary thyroid carcinoma diagnosis. Patients underwent preoperative ultrasonographic examination using the Aixplorer device (Supersonic Imagine, France) with a linear array transducer of 7.5–16 MHz to identify potential metastasis within the cervical lymph nodes. Ultrasonic assessments are presented using the totaling attributes such as sensitivity, specificity, positive and negative predictive values, and likelihood ratios.
Results
The post-operation pathology results showed metastasis in 85 (42.5%) patients. Standard imaging protocol without cervical approaches and advanced Doppler imaging capability detected metastatic involvement in 34 (17.0%) subjects. Meanwhile, the modified approach utilizing advanced Doppler imaging capability and cervical maneuvers identified metastatic involvement in 84 (42.0%) cases. The preoperative sensitivity without advanced Doppler imaging and maneuvers was 35.3%, specificity – 96.5%, positive predictive value – 88.2%, and negative predictive value – 66.9%. The introduction of advanced Doppler imaging and maneuvers yielded a sensitivity of 97.6%, specificity – of 99.1%, positive predictive value – 98.8%, and negative predictive value – 98.3%.
Conclusion
Advanced Doppler imaging can improve the visualization of the cervical areas, due to its ultrafast and ultrasensitive perception qualities, facilitating the early recognition of vascular pattern changes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12880-025-01750-w.
Keywords: Papillary thyroid carcinoma, Ultrasonography, Lymph nodes, Neoplasm metastasis, Doppler ultrasonography
Introduction
Papillary thyroid carcinoma (PTC) is the predominant form of thyroid cancer, accounting for over 80% of reported cases [1]. Despite an increasing trend in its incidence in recent years, there has not been a significant rise in mortality rates. Notably, the overall 5-year survival rate remains impressively high at 98.3%, as documented by the Surveillance, Epidemiology, and End Results database [2].
Although PTC generally follows an indolent course and has a favorable prognosis, early metastatic lymph node involvement has been reported in up to 70% of patients [3]. The significance of cervical lymph node metastasis is pronounced, correlating with elevated risks of local recurrence, distant metastasis, and reduced patient survival [4]. Preoperative ultrasonographic evaluation is a standard component of surgical planning [5], and accurate preoperative lymph node metastatic involvement assessment can significantly influence the surgical strategy [6]. Central cervical lymph nodes serve as sentinels for thyroid cancer metastasis [7]. However, despite their simplicity and speed, conventional ultrasound methods have limited capabilities in detecting central cervical lymph node metastasis [8]. Due to these lymph nodes’ small size and anatomical position [6], studies have reported up to only 30% sensitivities [9] for central cervical lymph node metastatic detection with ultrasonography. Consequently, current guidelines recommend prophylactic central cervical lymph node dissection, which can lead to additional postoperative complications.
Advanced Doppler imaging is a novel capability in Doppler ultrasonography based on color flow imaging. This technology facilitates the identification of subtle changes in lymph node vascular patterns that were previously elusive [10, 11]. As a result, advanced Doppler imaging can potentially evaluate sensitive central lymph node metastasis and reduce the need for prophylactic lymph node dissection. The ability to accurately detect metastatic involvement of central cervical lymph nodes holds significant potential for promoting less radical lymph node dissection strategies. Furthermore, specific cervical maneuvers can enhance ultrasonographic visualization by minimizing acoustic shadowing, approximating deeper anatomical structures to the probe, and repositioning tissues to improve anatomical delineation and diagnostic clarity [12]. Therefore, this study aims to elucidate the diagnostic accuracy of preoperative advanced Doppler imaging capability with cervical maneuvers in detecting metastatic central cervical lymph nodes in patients with PTC.
Methods
This cross-sectional study aimed to assess the preoperative diagnostic accuracy of cervical ultrasonography in detecting lymph node metastasis among patients with PTC. Patients diagnosed with PTC who were referred to the TIRAD imaging center from February 2022 to September 2023 and who were candidates for total or partial thyroidectomy with cervical lymph node excision were enrolled. The diagnosis of PTC was confirmed by preoperative fine needle aspiration cytology. Patients were excluded from the study if they had a history of previous malignancies, cervical surgeries, neck area radiotherapy, lymphatic system diseases, low-quality ultrasonographic images, or non-diagnostic pathological reports. All patients underwent surgical intervention in accordance with established international guidelines [13]. Furthermore, lymph node dissection adequacy was ensured by the removal of a minimum of six lymph nodes in each case [14]. In our study, lymph node dissections from different cervical zones were submitted separately for pathological evaluation as distinct segments. Consequently, prominent lymph nodes were reported separately in the pathology reports and correlated with ultrasonographic findings. All procedures were conducted by the 1964 Declaration of Helsinki and its later extensions. Written informed consent was obtained from all participants. The ethics committee of AJA University of Medical Sciences reviewed and approved this study (IR.AJAUMS.REC.1402.036).
Ultrasonographic evaluation
Patients underwent preoperative ultrasonographic evaluation to assess central cervical lymph node metastasis. The patients were supine with minimally extended necks tilted backward, and coupling gel was applied. Ultrasonography was performed in greyscale and color Doppler modes, with and without the utilization of advanced Doppler imaging, using an Aixplorer device (Supersonic Imagine, France) with a linear array transducer operating at a frequency of 7.5–16 MHz. Advanced Doppler imaging is integrated into Supersonic Imagine devices as Angio Planewave Ultrasensitive (Angio PL.U.S) capability. Initially, patients were evaluated for metastatic lymph nodes using greyscale and Doppler modes without maneuvering. Subsequently, probe pushing, cervical rotation, and swallowing or coughing maneuvers were performed to enhance visualization.
Cervical lymph nodes exhibiting irregular cystic appearance, internal microcalcifications, a round shape with increased anteroposterior diameter, increased echogenicity and heterogeneity, irregular margins, absence or narrowing of the hilum, irregular contour, focal asymmetry, and cortical thickening on greyscale mode were considered suspicious for metastatic involvement [15]. In Doppler mode, increased central vascularity and abnormal lymph node vascular patterns, such as vessels entering the lymph node from the periphery or focal increased vascularity in the periphery, suggested metastatic involvement. Presence of any of these diagnostic criteria was considered a suspicion of metastatic involvement.
Given that small, round, hypoechoic, and low-vascular lymph nodes are commonly observed in the central cervical region as normal findings, particularly in cases of chronic lymphocytic thyroiditis, careful differentiation between normal and metastatic lymph nodes was necessary. Comparing suspected lymph nodes with their counterparts on the contralateral side of the neck helped favor metastatic involvement in unilateral findings.
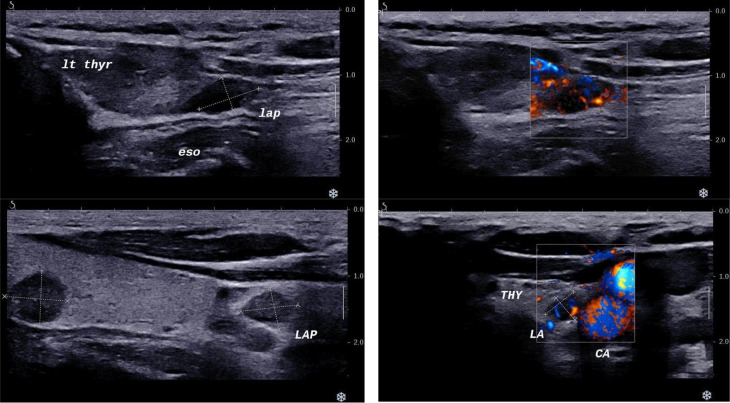
All ultrasonographic evaluations were conducted by a radiology specialist with 18 years of diagnostic and 11 years of interventional thyroid ultrasonography experience. Figure 1 provides examples of greyscale and color Doppler modes using advanced Doppler imaging capability.
Fig. 1.
Central cervical region ultrasound, left panel, greyscale mode, right panel, advanced Doppler imaging mode. The upper left image illustrates an axial ultrasonographic view of a metastatic lymph node. The left thyroid lobe and cervical esophagus are visible, confirming the lymph node’s posterior position relative to the thyroid, located in level VI of the neck. The upper right image with color Doppler reveals abnormal vascularity and microvascular flow, indicative of metastatic involvement. The lower left image shows a sagittal view of a TIRADS 5 left thyroid nodule and lymphadenopathy in the lower portion of the left thyroid lobe. The lower right image suggests the lymph node is positioned posterior to the thymus, within the central neck (levels VI and VII. LT, left; THYR, thyroid; ESO, esophagus; LAP, lymphadenopathy; THY, thymus; CA, carotid sheath
Data collection
Clinical information, including demographic data (age, sex, body mass index (BMI)), preoperative ultrasonographic evaluations of the suspicious lymph nodes, and postoperative pathology reports (tumor size, tumor location, tumor staging, and metastatic lymph node involvement), were collected from the patient’s medical records using a data collection form.
Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) version 27 (IBM, USA). Quantitative data are presented as mean with standard deviation or median with interquartile range. Qualitative data are presented as counts and percentages. Pearson’s Chi-square test and Fisher’s Exact test were used to compare qualitative data, while the Independent Samples T-test and Wilcoxon Rank Sum Test were used to compare quantitative data. Diagnostic accuracy criteria are presented as sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratios (LR) [16]. To compare the diagnostic performance of the two techniques, as well as their agreement with the pathological gold standard, the McNemar test was employed. A p-value of less than 0.05 was considered statistically significant.
Definitions
Angio PL.U.S
Angio Planewave Ultrasensitive imaging is a Doppler imaging-based capability that uses unfocused waves and 3D wall filtering to evaluate fine vascular structures that cannot be detected with power Doppler evaluations.
Results
Two hundred patients with PTC were enrolled in the final assessment. Postoperative pathological assessments revealed metastatic involvement in 85 cases, constituting 42.5% of the total population.
Demographic findings
The mean age of the patients was 40.50 ± 6.55 years, with 78.5% being female. The mean age of patients with metastatic lymph nodes was 39.49 ± 6.59 years, with 66 (77.6%) females, while the mean age of patients without metastatic involvement was 41.24 ± 6.46 years, with 91 (79.1%) females. The patients’ mean BMI was 24.29 ± 2.44 kg/m², and a history of diabetes mellitus was observed in 16 (8.0%) participants, with a mean time to diagnosis of 10.25 ± 3.60 years. No statistically significant differences regarding demographic characteristics and medical history between patients with and without metastatic lymph node involvement were observed between patients with and without metastatic lymph node involvement. Table 1 presents a summary of the patient demographics.
Table 1.
Baseline characteristics of the participants
| Characteristics | Group | P-value1 | |
|---|---|---|---|
| With Metastasis (N = 85) |
Metastasis free (N = 115) |
||
| Age, years | 39.49 ± 6.59 | 41.24 ± 6.46 | 0.062 |
| Sex, female | 66 (77.6) | 91 (79.1) | 0.862 |
| Height, cm | 162.00 (161.00, 166.00) | 165.00 (160.00, 166.00) | 0.735 |
| Weight, Kg | 70.00 (61.00, 76.00) | 66.00 (63.00, 72.00) | 0.237 |
| Body Mass Index, Kg/m2 | 26.39 (23.00, 28.11) | 24.24 (22.86, 28.04) | 0.114 |
| Diabetes Mellitus | 9 (10.6) | 7 (6.1) | 0.296 |
| Diabetes Mellitus Duration, years 2 | 10.67 ± 3.90 | 9.71 ± 3.42 | 0.617 |
| Smoking | 10 (11.8) | 10 (8.7) | 0.635 |
1: Independent Sample T-test, Pearson’s Chi-Square Test, and Wilcoxon Rank-Sum Test
2: Since diabetes mellitus duration is only assessed in patients with the disease, the sample size in the metastatic group is 9 and in the group without metastasis is 7 persons
Continuous data are provided as mean with standard deviation or median with interquartile range
Categorical data are provided as frequencies and percentages
Pathologic findings
All participants had PTC without distant metastasis (M0). The average size of the thyroid tumors in pathologic evaluations was 1.96 ± 1.08 cm, predominantly located in the right lobe. The metastatic group exhibited a slightly larger average size of 2.12 ± 1.18 cm compared to the non-metastatic group, with a size of 1.84 ± 0.99 cm. The right thyroid lobe was the prominent tumor site in both groups, with 53 (62.4%) cases in the metastatic group and 69 (60%) cases in the non-metastatic group. Most patients (69.0%) were categorized as T1 stage at the time of diagnosis, with 52 (61.2%) cases in the metastatic group and 86 (74.8%) in the non-metastatic group. The average number of dissected lymph nodes was 11.20 ± 3.12. Among patients with confirmed lymph node metastasis, the mean number of metastatically involved lymph nodes was 1.55 ± 0.86. No statistically significant differences were identified between the two groups concerning tumor size, location, and stage. Additional pathologic details are provided in Table 2.
Table 2.
Summary of pathologic findings of the thyroid tumor
| Characteristics | Levels | Groups | P-value1 | |
|---|---|---|---|---|
| Metastatic (N = 85) |
Metastatic free (N = 115) |
|||
| Thyroid Tumor size, cm | 2.00 (1.10, 3.05) | 1.80 (0.90, 2.70) | 0.104 | |
| Thyroid Tumor Location | Right Lobe | 53 (62.4) | 69 (60.0) | 0.458 |
| Left Lobe | 23 (27.1) | 25 (21.7) | ||
| Bilateral | 7 (8.2) | 17 (14.8) | ||
| Isthmus | 2 (2.4) | 4 (3.5) | ||
| Thyroid Tumor stage (TNM) | T1 | 52 (61.2) | 86 (74.8) | 0.172 |
| T2 | 19 (22.4) | 14 (12.2) | ||
| T3 | 10 (11.8) | 11 (9.6) | ||
| T4 | 4 (4.7) | 4 (3.5) | ||
1: Fisher Exact Test, and Wilcoxon Rank-Sum Test
Continuous data are provided as median with interquartile range
Categorical data are provided as frequencies and percentages
Ultrasonographic findings
Using greyscale and Doppler imaging without maneuvers and advanced Doppler imaging capability (conventional technique), suspicious metastatic involvement was observed in 34 (17.0%) patients. However, employing advanced Doppler imaging capability with maneuvers revealed metastatic involvement in 84 (42.0%) cases.
Using the conventional ultrasound technique, evaluation of 34 suspected lymph nodes demonstrated the following sonographic features: irregular margins in 15 cases (44.1%), absence of hilar architecture in 9 cases (26.5%), hilar narrowing in 7 cases (20.6%), calcification in 14 cases (41.2%), necrosis in 5 cases (14.7%), nodal matting in 8 cases (23.5%), cortical thickening in 11 cases (32.4%), abnormal vascular pattern in 19 cases (55.9%), abnormal nodular flow in 2 cases (5.9%), lymphovascular invasion in 10 cases (29.4%), perineural invasion in 10 cases (29.4%), and extrathyroidal extension in 8 cases (23.5%).
Assessment of 84 lymph nodes using advanced Doppler imaging combined with cervical maneuvers, which were identified as suspicious for metastasis, revealed the following characteristics: irregular margins in 37 cases (44.0%), absence of hilar architecture in 19 cases (22.6%), hilar narrowing in 22 cases (26.2%), calcification in 31 cases (36.9%), necrosis in 14 cases (16.7%), nodal matting in 28 cases (33.3%), cortical thickening in 31 cases (36.9%), abnormal vascular pattern in 50 cases (59.5%), abnormal nodular flow in 12 cases (14.3%), lymphovascular invasion in 22 cases (26.2%), perineural invasion in 23 cases (27.4%), and extrathyroidal extension in 20 cases (23.8%).
In the conventional technique, the average count of lymph nodes observed in each person with central cervical lymph node metastatic involvement was 3.24 ± 1.4. In contrast, using the advanced Doppler imaging technique, the mean number of metastatic lymph nodes detected was 2.50 ± 1.92. The mean size of the lymph nodes in the conventional evaluation was 13.96 ± 2.27 mm, while it was 8.90 ± 4.40 mm with the advanced Doppler imaging capability. Most central cervical lymph node metastases were observed in the right paratracheal region, exhibiting a round shape and hypoechoic characteristics. Table 3 demonstrates the sonographic findings of metastatic lymph nodes in patients using the conventional technique, with and without cervical maneuvers, and the advanced Doppler imaging capability.
Table 3.
Summary of sonographic findings of metastatic lymph nodes
| Feature | Levels | Groups | p-value1 | |
|---|---|---|---|---|
| Conventional Technique (N = 34) |
Advanced Technique (N = 84) |
|||
| Count | 3.00 (3.00, 3.00) | 2.00 (1.00, 4.00) | < 0.001 | |
| Size | 14.00 (13.00, 15.00) | 7.00 (5.00, 13.75) | < 0.001 | |
| Location | Right Paratracheal | 21 (61.8) | 41 (48.4) | 0.185 |
| Left Paratracheal | 17 (50.0) | 39 (46.4) | 0.718 | |
| Pretracheal | 0 (0) | 26 (31.0) | < 0.001 | |
| Suprasternal Notch | 26 (76.5) | 37 (44.0) | < 0.001 | |
| Shape | Round | 25 (73.5) | 30 (35.7) | < 0.001 |
| Oval | 9 (26.5) | 54 (64.3) | ||
| Echo | Hypoecho | 25 (73.5) | 51 (60.7) | 0.182 |
| Mixed | 9 (26.5) | 33 (39.3) | ||
| Abnormal Findings | Irregular Margins | 15 (44.1) | 37 (44.0) | 0.993 |
| Hilar Absence | 9 (26.5) | 19 (22.6) | 0.644 | |
| Hilar Narrowing | 7 (20.6) | 22 (26.2) | 0.506 | |
| Calcification | 14 (41.2) | 31 (36.9) | 0.659 | |
| Necrosis | 5 (14.7) | 14 (16.7) | 0.793 | |
| Matting | 8 (23.5) | 28 (33.3) | 0.288 | |
| Cortical Thickness | 11 (32.4) | 31 (36.9) | 0.637 | |
| Abnormal Vascular Pattern | 19 (55.9) | 50 (59.5) | 0.712 | |
| Abnormal Nodular Flow | 2 (5.9) | 12 (14.3) | 0.042 | |
| Lymphovascular Invasion | 10 (29.4) | 22 (26.2) | 0.718 | |
| Perineural Invasion | 10 (29.4) | 23 (27.4) | 0.825 | |
| Extrathyroidal Extension | 8 (23.5) | 20 (23.8) | 0.974 | |
1: Wilcoxon Rank Sum Test, Pearson’s Chi-Square Test, Fisher’s Exact Test
Continuous data are provided as median with interquartile range
Categorical data are provided as frequencies and percentages
Diagnostic accuracy
Preoperative conventional sonographic imaging without maneuvers yielded a sensitivity of 35.29%, a specificity of 96.52%, a PPV of 88.23%, and an NPV of 66.86%. In contrast, the simultaneous implementation of advanced Doppler imaging capability and cervical maneuvers yielded a sensitivity of 97.64%, a specificity of 99.13%, a PPV of 98.80%, and an NPV of 98.27%. A comparison between the two techniques revealed a statistically significant difference in their agreement (Chi-Square = 42.875, p < 0.001). Furthermore, when evaluating their diagnostic performance relative to the pathological gold standard, advanced Doppler imaging capability with cervical maneuvers demonstrated significantly superior diagnostic accuracy (Chi-Square = 54.018, p < 0.001). Table 4 summarizes their diagnostic accuracy parameters.
Table 4.
Diagnostic accuracy of sonographic evaluation modalities
| Feature | Conventional Technique (N = 34) |
Advanced Technique (N = 84) |
|---|---|---|
| Sensitivity, % | 35.29 | 97.64 |
| Specificity, % | 96.52 | 99.13 |
| PPV, % | 88.23 | 98.80 |
| NPV, % | 66.86 | 98.27 |
| LR+ | 10.14 | 112.22 |
| LR- | 0.67 | 0.023 |
PPV, Positive Predictive Value; NPV, Negative Predictive Value; LR, Likelihood Ratio
Discussion
This study investigated the diagnostic performance of advanced Doppler imaging for detecting metastatic central cervical lymph nodes in patients with papillary thyroid carcinoma (PTC). The findings demonstrated excellent diagnostic accuracy, with sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) all exceeding 95%, highlighting the potential utility of this technique in preoperative staging. Furthermore, comparison of the advanced technique with the conventional technique yielded significantly higher diagnostic capability, further supporting our findings.
Preoperative ultrasonography is a standard component in managing patients with PTC [17]. However, due to the small size of the lymph nodes and the anatomical complexity of the neck, which includes gas and bony structures, the diagnostic accuracy of ultrasonography for detecting metastatic involvement is limited [18]. Metastatic involvement in the lateral cervical lymph nodes is more likely to be detected compared to the central region using non-invasive imaging modalities. However, despite having higher sensitivity, the specificity of lateral cervical lymph node metastasis detection is lower compared to the central cervical region [19].
Accurate detection of metastatic involvement in cervical lymph nodes is crucial for surgical strategy development [20]. Since PTC tends to metastasize through the lymphatic system, cervical lymph node metastasis is prevalent [7]. While the central cervical region is the primary site of metastatic involvement, its structural complexities make lateral cervical lymph nodes the most common site for detecting metastatic involvement [21]. As a result, prophylactic central cervical lymph node dissection was recommended in previous guidelines. However, its necessity, due to the increased risk of postoperative complications such as injury to the recurrent laryngeal nerve, is currently under debate [15].
Various non-invasive diagnostic techniques, such as computed tomography [22](CT) scans, magnetic resonance imaging [20], (MRI), and different ultrasonographic evaluations, such as color Doppler imaging, power Doppler imaging, and elastography [23] have been utilized to assess metastatic involvement. However, ultrasonography is preferred due to its simplicity, relative speed, and real-time capabilities. Moreover, the non-inferiority of ultrasonography for detecting metastatic cervical lymph nodes has been reported [9]. Despite its favorable characteristics, its capabilities are limited in detecting lymph node metastatic involvement, and efforts have been made to address this issue. These efforts include integrating artificial intelligence algorithms in computer-assisted devices and radiomics analyses [18, 24].
Angio PL.U.S is a Doppler-based imaging capability that allows visualization of very fine vessels and slow blood flow. These properties allow for early abnormal vascular pattern assessments and improved visualizations. The implementation of this technique has been successful in thyroid nodule diagnosis [11], and a study by Bin Wang et al. [25] reported a significant difference in vascular pattern assessment of cervical metastatic and non-metastatic lymph nodes in PTC patients using advanced Doppler imaging.
In our study, integrating advanced Doppler imaging with cervical maneuvers significantly outperformed conventional greyscale and color Doppler imaging in diagnostic accuracy. Importantly, the smaller mean size and reduced count of detected metastatic lymph nodes in the advanced Doppler group suggest that this technique can identify smaller lesions that would otherwise go unnoticed with standard ultrasound.
To our knowledge, this is one of the first studies to specifically evaluate the use of advanced Doppler imaging for detecting central cervical lymph node metastasis preoperatively in PTC. A frequent challenge with conventional imaging is the underdiagnosis of nodes located near the thoracic inlet and thymus due to their similar echogenicity. To address this, we employed a comprehensive scanning technique, ensuring thorough visualization of these anatomically challenging regions. Despite the promising results, this study has several limitations. A single experienced radiologist performed all ultrasonographic assessments with 18 years of diagnostic and 11 years of interventional thyroid imaging expertise. Given the operator-dependent nature of ultrasound, reproducibility across other practitioners with varying experience levels may be limited. Future multicenter studies with larger sample sizes and multiple observers are needed to validate these findings and assess generalizability. As the imaging assessments were conducted by a single radiology specialist, inter-observer variability and inter-rater reliability could not be analyzed. Moreover, the current study evaluated the combined application of advanced Doppler imaging and cervical maneuvers against conventional greyscale and Doppler imaging. Future studies can investigate the individual contribution of each technique to better understand their diagnostic value. Moreover, although lymph node dissections from different cervical zones were submitted and analyzed as separate segments, specific matching of each lymph node between imaging and pathology was not performed. Additionally, while lateral neck lymph node involvement is clinically significant, this study focused exclusively on the central cervical compartment and did not assess the potential correlation between central and lateral nodal metastases. The single-center design and relatively small sample size may limit the generalizability of our findings. Furthermore, data on the total number of lymph nodes detected during ultrasonography and the number classified as suspicious were not recorded, which could have provided more insights. Addressing these limitations in future research may yield more comprehensive and generalizable conclusions.
In conclusion, ultrasonography is an important non-invasive preoperative assessment modality; however, conventional ultrasonography approaches do not yield high sensitivity despite their reasonable specificity. With the introduction of advanced Doppler imaging capability in Doppler imaging, due to its ultrafast and ultrasensitive capabilities, improved visualization of the cervical lymph nodes is achieved, enabling early and enhanced detection of vascular pattern changes. This study reports promising results regarding using advanced Doppler imaging capability with cervical maneuvers in detecting central cervical lymph node metastatic involvement; however, more comprehensive studies with larger sample sizes are required further to investigate the diagnostic value of advanced Doppler imaging capability.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank everyone who participated in this study.
Author contributions
H.C., Writing- Original Draft, Data Curation, Methodology; V.K., Writing- Original Draft, Data Curation, Formal Analysis; J.K., Writing- Review & Editing, Conceptualization; A.A., Writing- Review & Editing, Visualization; K.S., Writing- Review & Editing, Supervision; R.G. and H.E., Project Administration, Supervision.
Funding
This study did not receive any funds or grants.
Data availability
The study data are available upon reasonable request from the corresponding author. The data will be provided after anonymization.
Declarations
Ethical approval
All procedures were conducted by the 1964 Declaration of Helsinki and its later extensions. Written informed consent was obtained from all participants. The ethics committee of AJA University of Medical Sciences reviewed and approved this study (IR.AJAUMS.REC.1402.036).
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agyekum EA, Ren YZ, Wang X, Cranston SS, Wang YG, Wang J et al. Evaluation of cervical lymph node metastasis in papillary thyroid carcinoma using Clinical-Ultrasound radiomic machine Learning-Based model. Cancers (Basel). 2022;14(21). [DOI] [PMC free article] [PubMed]
- 2.Surveillance E, and End Results Program Cancer Stat Facts: Thyroid Cancer: National Cancer Institute 2024 [Available from: https://seer.cancer.gov/statfacts/html/thyro.html]
- 3.Liu RR, Chen SJ, Chen SJ, Guo XH. Utility of the multi-modality ultrasound scoring scale in evaluating cervical lymph node metastasis in patients with papillary thyroid cancer. Asian J Surg. 2023;46(7):2701–2. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal MA, Wang X, Guoliang Z, Moazzam NF, Shahid AD, Qian X, Qian W. A comparison of the efficiency of diagnostic ultrasound and magnetic resonance imaging of cervical lymph nodes in papillary thyroid carcinoma. J Xray Sci Technol. 2021;29(6):1033–44. [DOI] [PubMed] [Google Scholar]
- 5.Lee JY, Yoo RE, Rhim JH, Lee KH, Choi KS, Hwang I et al. Validation of ultrasound risk stratification systems for cervical lymph node metastasis in patients with thyroid Cancer. Cancers (Basel). 2022;14(9). [DOI] [PMC free article] [PubMed]
- 6.Tao L, Zhou W, Zhan W, Li W, Wang Y, Fan J. Preoperative prediction of cervical lymph node metastasis in papillary thyroid carcinoma via conventional and Contrast-Enhanced ultrasound. J Ultrasound Med. 2020;39(10):2071–80. [DOI] [PubMed] [Google Scholar]
- 7.Wen Q, Wang Z, Traverso A, Liu Y, Xu R, Feng Y, Qian L. A radiomics nomogram for the ultrasound-based evaluation of central cervical lymph node metastasis in papillary thyroid carcinoma. Front Endocrinol (Lausanne). 2022;13:1064434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li F, Pan D, He Y, Wu Y, Peng J, Li J, et al. Using ultrasound features and radiomics analysis to predict lymph node metastasis in patients with thyroid cancer. BMC Surg. 2020;20(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen YH, Zhang YQ. Diagnostic potential of ultrasonography and computed tomography in differentiating cervical lymph node metastasis of thyroid cancer: a systematic review and meta-analysis. Arch Med Sci. 2023;19(4):965–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang B, Yang J, Tang Y-L, Chen Y-Y, Luo J, Cui X-W, et al. The value of microvascular doppler ultrasound technique, qualitative or quantitative shear-wave elastography of breast lesions for predicting axillary nodal burden in patients with breast cancer. Quant Imaging Med Surg. 2024;14(1):408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chambara N, Liu SYW, Lo X, Ying M. Diagnostic value of AngioPLUS microvascular imaging in thyroid nodule diagnosis using quantitative and qualitative vascularity grading. Biomedicines. 2022;10(7):1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang W, Tang L, Lu C, Wu M, Chen M. Shear wave elastography in the evaluation of level VI lymph nodes in papillary thyroid carcinoma: combined with gray-scale ultrasound ex vivo. BMC Cancer. 2018;18:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid Cancer. Thyroid. 2016;26(1):1–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sancho JJ, Lennard TWJ, Paunovic I, Triponez F, Sitges-Serra A. Prophylactic central neck disection in papillary thyroid cancer: a consensus report of the European society of endocrine surgeons (ESES). Langenbeck’s Archives Surg. 2014;399:155–63. [DOI] [PubMed] [Google Scholar]
- 15.Abboud B, Smayra T, Jabbour H, Ghorra C, Abadjian G. Correlations of neck ultrasound and pathology in cervical lymph node of papillary thyroid carcinoma. Acta Chir Belg. 2020;120(4):238–44. [DOI] [PubMed] [Google Scholar]
- 16.Šimundić A-M. Measures of diagnostic accuracy: basic definitions. Ejifcc. 2009;19(4):203. [PMC free article] [PubMed] [Google Scholar]
- 17.Liu L, Li G, Jia C, Du L, Shi Q, Wu R. Preoperative strain ultrasound elastography can predict occult central cervical lymph node metastasis in papillary thyroid cancer: a single-center retrospective study. Front Oncol. 2023;13:1141855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao HN, Yin H, Liu JY, Song LL, Peng YL, Ma BY. Deep learning-assisted ultrasonic diagnosis of cervical lymph node metastasis of thyroid cancer: a retrospective study of 3059 patients. Front Oncol. 2024;14:1204987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee D, Ji Y, Sung E, Park J, Lee Y, Park D, Tae K. Roles of ultrasonography and computed tomography in the surgical management of cervical lymph node metastases in papillary thyroid carcinoma. Eur J Surg Oncol (EJSO). 2013;39(2):191–6. [DOI] [PubMed] [Google Scholar]
- 20.Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope. 2011;121(3):487–91. [DOI] [PubMed] [Google Scholar]
- 21.Jiang LH, Chen C, Tan Z, Lu XX, Hu SS, Wang QL, et al. Clinical characteristics related to central lymph node metastasis in cN0 papillary thyroid carcinoma: A retrospective study of 916 patients. Int J Endocrinol. 2014;2014:385787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Albuck AL, Issa PP, Hussein M, Aboueisha M, Attia AS, Omar M, et al. A combination of computed tomography scan and ultrasound provides optimal detection of cervical lymph node metastasis in papillary thyroid carcinomas: A systematic review and meta-analysis. Head Neck. 2023;45(9):2173–84. [DOI] [PubMed] [Google Scholar]
- 23.Xu JM, Xu XH, Xu HX, Zhang YF, Guo LH, Liu LN, et al. Prediction of cervical lymph node metastasis in patients with papillary thyroid cancer using combined conventional ultrasound, strain elastography, and acoustic radiation force impulse (ARFI) elastography. Eur Radiol. 2016;26(8):2611–22. [DOI] [PubMed] [Google Scholar]
- 24.Mu J, Cao Y, Zhong X, Diao W, Jia Z. Prediction of cervical lymph node metastasis in differentiated thyroid cancer based on radiomics models. Br J Radiol. 2024. [DOI] [PMC free article] [PubMed]
- 25.Wang B, Cao Q, Cui XW, Dietrich CF, Yi AJ. A model based on clinical data and multi-modal ultrasound for predicting cervical lymph node metastasis in patients with thyroid papillary carcinoma. Front Endocrinol (Lausanne). 2022;13:1063998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study data are available upon reasonable request from the corresponding author. The data will be provided after anonymization.