ABSTRACT
Objective
The study aimed to evaluate the prevalence and impact of low‐value diagnostic tests at a regional, major‐referral, mixed Emergency Department (ED).
Methods
A single‐site, cross‐sectional study was conducted at Townsville University Hospital in April 2022. Adult patients (aged 18 years and above) who underwent one of 10 specified diagnostic tests were included. The tests encompassed coagulation studies, urine cultures, blood cultures, cranial computed tomography (CT) in syncope, cranial CT in minor head injury, cervical spine CT in neck trauma, ankle X‐ray in acute ankle trauma, duplex lower extremity ultrasound in suspected deep vein thrombosis, CT pulmonary angiography in suspected pulmonary embolism, and CT kidney ureter bladder in renal colic. Tests were classified as low‐value based on Choosing Wisely recommendations, with their value determined by a research assistant using clinical documentation, prior to the availability of test results. Emergency clinicians were blinded to the study conduct.
Results
Of all diagnostic tests performed, 48.2% (276/572) were deemed low‐value, including 50.6% of laboratory tests (246/486) and 24.4% of imaging tests (21/86). The median ED length of stay was 6.1 h (IQR 3.9–8.5). Low‐value imaging tests contributed to 152 lost bed‐hours per 100 tests.
Conclusion
A substantial proportion of diagnostic tests were low‐value, exacerbating access block and reducing the availability of ED beds, thereby delaying timely emergency care. The implementation of evidence‐based, effective strategies is imperative to mitigate patient harm associated with low‐value diagnostic tests.
Keywords: access block, diagnostic tests, emergency medicine, low‐value care
1. Introduction
Low‐value care, defined as medical interventions that are ineffective, inefficient, and provide no benefit to patients, represents a significant challenge to global health systems [1, 2, 3, 4, 5]. The prevalence of such care varies widely, reported to be between 1% and 80%, and it imposes a substantial economic burden [5]. In the United States, the annual cost of low‐value care is estimated at A$423 billion [5] In Australia, the cost to NSW public hospitals alone is A$99.3 million [1].
Despite concerted efforts by professional organisations worldwide to eliminate low‐value care, including the Choosing Wisely campaign initiated by the American Board of Internal Medicine in 2012, Choosing Wisely Canada (CWC) since 2014 and subsequently Choosing Wisely Australia since 2015, the issue persists [6, 7, 8, 9]. The persistence of low‐value care necessitates a re‐evaluation of its framing, suggesting that it be considered a patient safety concern and a source of preventable harm, which may bolster engagement from clinicians and the community [10, 11]. However, robust evidence detailing patient harm resulting from low‐value care remains scarce [12].
In the Emergency Department (ED), low‐value care can exacerbate patient flow issues and contribute to access block. Access block is a critical problem in the Australasian health care system where admitted patients experience delays in transferring from the ED to inpatient beds due to capacity constraints [13, 14]. With Australasian EDs experiencing unprecedented demand, 46.1% of admitted patients experience access block [14], leading to compromised patient outcomes, increased clinical errors, and higher mortality rates [14, 15, 16]. The performance of low‐value diagnostic tests can further impede ED operations, prolong patient stays, and adversely impact patient flow [17, 18, 19].
In addition to impairing patient flow, low‐value tests can have other adverse patient outcomes. Low‐value imaging tests could reveal incidentalomas—imaging abnormality in an asymptomatic patient or imaging abnormality unrelated to symptoms in a symptomatic patient—necessitating further investigation [20]. Incidentalomas were common in the study by Davenport et al., who reported at least one incidental finding in 15%–30% of all imaging tests and 20%–40% of computed tomography (CT) scans [21]. Patients with incidental findings but low risk for disease are likely to experience length bias, lead‐time bias, overdiagnosis and overtreatment that create an illusion of benefit while conferring harm [21].
The aim of this study was to determine the prevalence and impact on patient flow of low‐value laboratory and imaging tests at Townsville University Hospital Emergency Department.
2. Methods
This was a single‐site, cross‐sectional study conducted at Townsville University Hospital ED, a major‐referral, mixed ED located in regional Queensland. The hospital had an annual patient census of 95,362 for the calendar year 2022. The study was conducted over 20 weekdays (daytime hours), from 4 April to 29April 2022. Ethics approval, inclusive of a consent waiver, was granted by the Townsville Hospital and Health Service Human Research Ethics Committee (HREC/2021/QTHS/75339). The study adhered to the STROBE guidelines for reporting [22].
2.1. Participants
Individuals aged 18 years or older who underwent specific diagnostic laboratory or imaging tests ordered by an emergency clinician were considered eligible. The study focused on 10 tests: coagulation studies, urine cultures, blood cultures, cranial CT in syncope, cranial CT in minor head injury, cervical spine CT in neck trauma, ankle XR in acute ankle trauma, duplex lower extremity ultrasound in suspected deep vein thrombosis, CT pulmonary angiography in suspected pulmonary embolism, and CT Kidney Ureter Bladder in renal colic. These tests were selected based on the availability of evidence‐based guidelines to inform clinical practice (Table 1). The primary outcomes measured were the proportion of patients undergoing any tests, the proportion of low‐value tests, ED length of stay (LoS), and additional ED LoS attributable to low‐value tests termed ‘lost bed‐hours’. We defined ED LoS as the time from ED arrival to ED departure [23]. We defined lost bed‐hours as additional time spent by patients in emergency department bed space (including short stay unit) whilst awaiting results of low‐value laboratory and imaging tests (Figure 1). The concept of lost bed‐hours was informed by literature on lost bed‐days which has been used to quantify adverse patient outcomes from hospital acquired infections [24]. The term ‘bed’ refers to ED treatment spaces (bed or chair). We did not make a distinction between a bed or a chair and decided on the term bed (rather than treatment space) to align with prior literature on lost bed‐days.
TABLE 1.
Choosing Wisely recommendations for the 10 diagnostic tests of interest.
| Test | Choosing wisely recommendation |
|---|---|
| Cranial CT in syncope | Avoid CT of the head in asymptomatic adult patients in the emergency department with syncope, insignificant trauma, and a normal neurological evaluation. Choosing Wisely – Cranial CT in Syncope Recommendation |
| Cranial CT in minor head injury | Don't request CT head scans in patients with head injury, unless indicated by a validated clinical decision rule. Choosing Wisely – Cranial CT in Minor Head Injury Recommendation |
| Cervical CT | Don't request imaging of the cervical spine in trauma patients, unless indicated by a validated clinical decision rule. Choosing Wisely – Cervical CT Recommendation |
| CT KUB | Avoid requesting CT KUB in otherwise healthy ED patients, age < 50 years, with a known history of kidney stones, presenting with symptoms and signs consistent with uncomplicated renal colic. Choosing Wisely – CT KUB Recommendation |
| CTPA | Don't request any diagnostic test for suspected PE unless indicated by Wells Score (or Charlotte Rule) followed by PE rule‐out criteria (in patients not pregnant). Low risk patients in whom diagnostic testing is indicated should have PE excluded by a negative D dimer not imaging. Choosing Wisely – CTPA Recommendation |
| US DVT lower limbs |
Don't request duplex compression ultrasound for suspected lower limb DVT in ambulatory patients unless the wells score (DVT risk assessment score) is greater than 2, OR if less than 2 but D‐dimer assay is positive. Choosing Wisely – US DVT Lower Limb Recommendation |
| Ankle X‐ray | Don't request imaging for acute ankle trauma unless indicated by Ottawa Ankle Rules (localised bone tenderness or inability to weight‐bear as defined in the rules). Choosing Wisely – Ankle X‐ray Recommendation |
| Coagulation studies | Avoid coagulation studies in ED patients unless there is a clearly defined specific clinical indication, such as monitoring of anticoagulants, in patients with suspected severe liver disease, coagulopathy or in the assessment of snakebite envenomation. Choosing Wisely – Coagulation Studies Recommendation |
| Blood culture | Avoid blood cultures in patients who are not systemically septic, have a clear source of infection and in whom a direct specimen for culture (e.g., urine, wound swab, sputum, cerebrospinal fluid or joint aspirate) is possible. Choosing Wisely – Blood Culture Recommendation |
| Urine culture | Do not perform surveillance urine cultures or treat bacteriuria in elderly patients in the absence of symptoms or signs of infection. Choosing Wisely – Urine Culture Recommendation |
Abbreviations: CT, computed tomography; DVT, deep vein thombosis; KUB, kidney ureter bladder; PA, pulmonary angiography; PE, pulmonary embolus; US, ultrasound.
FIGURE 1.
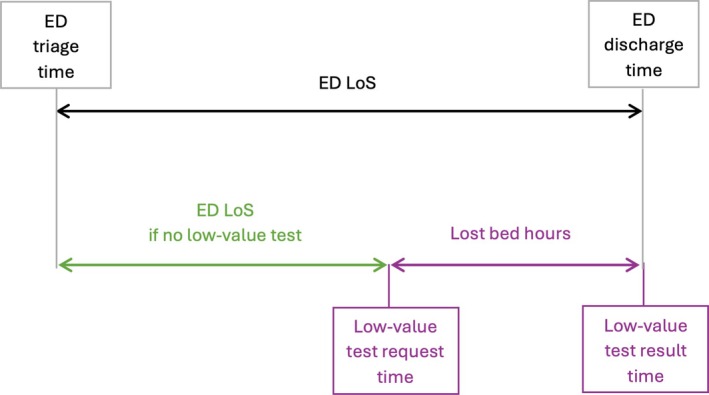
Timeline for calculating ED LoS and lost bed hours.
2.2. Data Collection
Recruitment occurred when a research assistant was present, utilising the FirstNet ED Information Software (Cerner Inc) to prospectively identify and enrol eligible participants. Tests were classified as low‐value if they did not align with the Choosing Wisely recommendations (Table 1). The research assistant, blinded to the test outcomes, assigned the value of tests based on the treating clinicians' documentation. The absence of explicit documentation for a low‐value test was interpreted as a lack of indication for that test. Emergency clinicians were blinded to the study, ensuring no change in the care provided to participants.
Data collection was executed by a single research assistant over 160 h throughout the study period. The assistant received training using practice medical records and was blinded to the study aims. A standardised form was employed for data collection, with clearly defined eligibility criteria and variables. Periodic meetings ensured performance monitoring, and any data ambiguities or conflicts were resolved through consensus among the investigators. Data variables included age, sex, ED triage time and date, ED presenting complaint, value of tests, results of tests, ED discharge diagnosis, ED discharge destination, ED LoS, test request time, and test result time.
2.3. Sample Size and Data Analysis
A sample size calculation was not performed and instead a convenience sampling approach was used. Data analysis was performed in STATA (StataCorp LLC. 2023. Stata Statistical Software: Release 18.0 College Station, TX, USA). Continuous variables were summarised as means and standard deviations (SD) or medians and inter‐quartile ranges (IQR), contingent upon the distribution's normality. Categorical variables were presented as counts and percentages. The metric of lost bed‐hours per 100 low‐value tests was also calculated.
3. Results
During the 20 weekday study period, encompassing 160 h, a total of 1871 patients presented to the study site, and 424 were recruited. Flowchart of participant inclusion is presented in Figure 2.
FIGURE 2.

Flow chart of patient inclusion.
The participants age range was 18–99 years, with a median age of 60 (IQR 37–74). Female participants accounted for 55% of the study cohort. Discharge outcomes were as follows: 41% were discharged home, 57% required hospital admission, and 2% were admitted to the Hospital in the Home (HITH) program. 1 patient (0.1%) died in ED, due to out‐of‐hospital cardiac arrest.
The prevalence and impact of low‐value tests are summarised in Table 2. The overall prevalence of low‐value tests was 48.2% (276/572) including 50.6% of laboratory tests (246/486) and 24.4% of imaging tests (21/86). Cranial CT scans for syncope were identified as low‐value in 100% of cases (5 out of 5 scans). Coagulation studies were the most frequently encountered low‐value laboratory test, accounting for 55.3% (89 out of 161 tests). None of the low‐value laboratory and imaging tests yielded positive results. The median ED LoS was 6.1 h (IQR 3.9–8.5). Low‐value imaging tests resulted in 152 lost bed‐hours per 100 tests.
TABLE 2.
Prevalence of and lost‐bed‐hours from low‐value diagnostic tests at TUH‐ED.
| Diagnostic test | Prevalence | Lost bed‐hours |
|---|---|---|
| Cranial CT in syncope | 100% (5/5) | 6.2 |
| Cranial CT in minor head injury | 37% (7/19) | 7.0 |
| Cervical CT | 17.6% (3/17) | 3.4 |
| Ankle X‐ray | 7% (1/15) | 1.1 |
| CT KUB | 0% (0/14) | 0 |
| CTPA | 31.3% (5/16) | 14.2 |
| US DVT lower limbs | 0% (0/0) | a |
| Coagulation studies | 55.3% (89/161) | b |
| Blood cultures | 51.6% (48/93) | b |
| Urine culture | 47.0% (109/232) | b |
Abbreviations: CT, computed tomography; DVT, deep vein thrombosis; KUB, kidney ureter bladder; PA, pulmonary angiography; TUH‐ED, Townsville University Hospital Emergency Department; US, ultrasound.
No US scans were performed during the study period.
Lost bed‐hours could not be calculated due to contemporaneous alternative diagnostic test requests.
4. Discussion
Our study found that a large proportion of laboratory and imaging tests were low‐value. This finding is consistent with the prevalence of low‐value tests highlighted in recent ED studies [8, 25, 26, 27]. For example, a Canadian study across four provinces found no decrease in the 30% rate of chest radiographs for infants with bronchiolitis since 2014–2015 [25]. Comparable rates were observed for cranial CT scans in adults with minor head injuries without red flags [25]. Similarly, Friere et al. reported that 39.5% of paediatric ED presentations for constipation had low‐value abdominal radiographs [26, 27], and Venkatesh et al. identified a low‐value lumbar spine imaging rate of 34.7% in a study of adult patient presentations with atraumatic low‐back pain across 305 United States EDs [8]. A similar prevalence was noted in a single‐site Australian study which reported an imaging rate of 39.3% in adult patient presentations with non‐specific low‐back pain [27].
Our study further indicates that low‐value imaging tests contribute to prolonged ED stays, escalating the risk of patient harm. We introduced ‘lost bed‐hours’ as a metric to quantify the additional ED LoS and the associated patient harm resulting from low‐value tests. This concept parallels ‘lost bed‐days’, traditionally used to measure the hospital‐level impact of healthcare‐associated infections [28]. The ‘lost bed‐hours’ metric reflects that diminished availability of ED beds could be exacerbating the negative consequences of access block. The potential impact of low‐value tests on access block will need to be explored in a multisite, prospective study.
Jones et al. found that a 10% increase in admitted ED patients experiencing access block led to a 10% rise in the risk of mortality within 7 days for new patients presenting to ED [16]. This is echoed by a United States study linking ED overcrowding to longer stays and higher mortality rates [29]. Low‐value tests can thus harm patients by compounding access block. Reducing low‐value tests could mitigate this compounding effect and associated patient harm.
Overuse of testing appears to be common, driven by availability, apparent objectiveness, and the increasing sensitivity of tests to detect disease [6]. Overuse of diagnostic testing is a particular problem in emergency medicine. Emergency physicians cite fear of missing a diagnosis, fear of lawsuits, and perceived patient expectations as key contributors [30].
Risk‐aversion and intolerance for uncertainty are unsurprising, given the context in which Emergency Physicians function. Emergency Medicine pairs high‐stakes decision making with a unique set of challenges. These include lack of time and space (limiting the opportunity to gather a thorough history, learn potentially relevant psychosocial or other contextual factors, and establish trust), lack of an ongoing relationship between physician and patient, and uncertain access by patients to appropriate follow‐up [30].
While our study did not examine other adverse outcomes of low‐value tests, such as patient pain, emotional stress, unnecessary follow‐up procedures, clinician burnout, and financial costs, these are well‐documented concerns [12, 31].
To mitigate low‐value testing, diagnostic stewardship—administering the right test for the right patient at the right time—has been advocated [32, 33]. This approach necessitates disrupting habitual testing behaviours, as noted by Grimshaw et al., who recommend population and system‐level de‐implementation strategies [34]. The Choosing Wisely De‐Implementation Framework provides a structured method for designing interventions based on behavioural change theories, encompassing the identification of low‐value tests, local priorities, drivers, interventions, and rigorous evaluation [35]. This could guide future efforts to eliminate low‐value testing and enhance patient safety [35].
A strength of our study is the blinding of emergency clinicians to study conduct. This blinding likely eliminated Hawthorne bias, where clinicians might alter their behaviour due to the awareness of being observed. Our study method reduces the risk of post hoc rationalisation, where tests with negative results might be deemed low‐value and those with positive outcomes considered high‐value.
The single‐site, in‐hours design limits the generalizability of our study findings. The relatively small number of individual tests reduces the strength of our conclusions. There is a high risk of bias from the method of determination of test value by a single rater. Exclusion of 215 patients at the screening stage increases the risk of bias due to missing data. The reliance on clinical documentation to determine test value could have led to an overestimation of low‐value test prevalence due to the absence of documentation in patients who had a valid indication. Exclusion of patients presenting overnight—when decision‐making is not supported by Emergency Physicians—who were present in ED between 0800 and 2300 h‐ may have resulted in an underestimation of the prevalence of low‐value tests.
As imaging tests accounted for a small proportion (15%) of all tests in our study, the use of low‐value imaging tests alone to calculate lost‐bed‐hours is a key limitation of our study. The concurrent performance of low‐value laboratory tests with other diagnostic tests posed a challenge in quantifying their impact in terms of lost‐bed‐hours. This limitation reinforces the need for further research into better measures of quantification of the impact of low‐value laboratory tests on patient care, outcomes, and safety.
In summary, our study contributes to the body of emergency medicine literature by highlighting the prevalence and impact of low‐value diagnostic tests. The limitations noted above underscore the need for larger, multi‐site studies to more accurately quantify the patient, clinician, and system harm associated with low‐value tests. Such studies could further enhance clinician and community engagement in efforts to reduce such tests and improve patient safety. Reframing value‐based health care as a resource sustainability issue could bolster efforts to reduce low‐value tests. Future research should focus on the design, implementation, and evaluation of evidence‐based interventions aimed at de‐implementing low‐value diagnostic tests.
5. Conclusion
Low‐value diagnostic tests are prevalent and contribute to extended ED LoS, exacerbating access block and potentially increasing patient harm. The development and implementation of evidence‐based interventions are crucial to reduce low‐value tests and mitigate their negative impact on patient care.
Conflicts of Interest
The authors declare no conflicts of interest.
Walker H., West C., Lawton L., Emeto T. I., and Gangathimmaiah V., “Could Low‐Value Diagnostic Tests be Compounding Access Block? A Single‐Site, Cross‐Sectional Study,” Emergency Medicine Australasia 37, no. 4 (2025): e70100, 10.1111/1742-6723.70100.
Funding: This work was supported by the Townsville Hospital and Health Service Study, Education and Research Trust Account (SERTA) Fund.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Badgery‐Parker T., Pearson S. A., Chalmers K., et al., “Low‐value care in Australian public hospitals: Prevalence and trends over time,” BMJ Quality and Safety 28, no. 3 (2019): 205–214, 10.1136/bmjqs-2018-008338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Badgery‐Parker T., Pearson S. A., Dunn S., and Elshaug A. G., “Measuring Hospital‐Acquired Complications Associated With Low‐Value Care,” JAMA Internal Medicine 179, no. 4 (2019): 499–505, 10.1001/jamainternmed.2018.7464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shrank W. H., Rogstad T. L., and Parekh N., “Waste in the US Health Care System: Estimated Costs and Potential for Savings,” JAMA 322, no. 15 (2019): 1501–1509, 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 4. Gledstone‐Brown L. and McHugh D., “Review Article: Idle 'just‐in‐Case' Peripheral Intravenous Cannulas in the Emergency Department: Is Something Wrong?,” Emergency Medicine Australasia 30, no. 3 (2018): 309–326, 10.1111/1742-6723.12877. [DOI] [PubMed] [Google Scholar]
- 5. Brownlee S., Chalkidou K., Doust J., et al., “Evidence for Overuse of Medical Services Around the World,” Lancet 390, no. 10090 (2017): 156–168, 10.1016/S0140-6736(16)32585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. “Choosing Wisely. Our Mission,” accessed February 2, 2022, https://www.choosingwisely.org/our‐mission/.
- 7. Müskens J. L. J. M., Kool R. B., van Dulmen S. A., and Westert G. P., “Overuse of Diagnostic Testing in Healthcare: A Systematic Review,” BMJ Quality and Safety 31, no. 1 (2022): 54–63, 10.1136/bmjqs-2020-012576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Venkatesh A. K., Scofi J. E., Rothenberg C., et al., “Choosing Wisely in Emergency Medicine: Early Results and Insights From the Acep Emergency Quality Network (E‐QUAL),” American Journal of Emergency Medicine 39 (2021): 102–108, 10.1016/j.ajem.2020.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen K. J., Thiruganasambandamoorthy V., Campbell S. G., Upadhye S., Dowling S., and Chartier L. B., “Choosing Wisely Canada: Scratching the 7‐Year Itch,” CJEM 24, no. 6 (2022): 569–573, 10.1007/s43678-022-00349-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marcotte L. M., Zech J. M., and Liao J. M., “Key Features Underlying Low‐Value Care Recommendations,” American Journal of Medical Quality 36, no. 2 (2021): 99–102, 10.1177/1062860620930329. [DOI] [PubMed] [Google Scholar]
- 11. Brownlee S. M. and Korenstein D., “Better Understanding the Downsides of Low Value Healthcare Could Reduce Harm,” BMJ 372 (2021): 372, 10.1136/bmj.n117. [DOI] [PubMed] [Google Scholar]
- 12. Korenstein D., Harris R., Elshaug A. G., et al., “To Expand the Evidence Base About Harms from Tests and Treatments,” Journal of General Internal Medicine 36, no. 7 (2021): 2105–2110, 10.1007/s11606-021-06597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. ACEM , Access Block: Australasian College for Emergency Medicine (ACEM, accessed May 28, 2022, 2022), https://acem.org.au/Content‐Sources/Advancing‐Emergency‐Medicine/Better‐Outcomes‐for‐Patients/Access‐Block. [Google Scholar]
- 14. Richardson D. B., “Access Block in Australian Emergency Departments 2017‐2020,” Emergency Medicine Australasia 33, no. 3 (2021): 529–533, 10.1111/1742-6723.13738. [DOI] [PubMed] [Google Scholar]
- 15. Javidan A. P., Hansen K., Higginson I., Jones P., Lang E., and the IFEM Task Force on Emergency Department Crowding, Access Block , “The International Federation for Emergency Medicine Report on Emergency Department Crowding and Access Block: A Brief Summary,” CJEM 23, no. 1 (2021): 26–28, 10.1007/s43678-020-00065-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jones P. G. and van der Werf B., “Emergency Department Crowding and Mortality for Patients Presenting to Emergency Departments in New Zealand,” Emergency Medicine Australasia 33, no. 4 (2021): 655–664, 10.1111/1742-6723.13699. [DOI] [PubMed] [Google Scholar]
- 17. “Choosing Wisely Champion Hospital: Victorian Agency for Health Information,” 2023, https://www.bettersafercare.vic.gov.au/improvement/projects/mtip/choosing‐wisely‐champion‐hospital.
- 18. “What is Patient Flow?: NEJM Catalyst Innovations in Care Delivery,” 2018, nejm.org.
- 19. “Good Practice Guide: Focus on Improving Patient Flow,” 2017.
- 20. O'Sullivan J. W., Muntinga T., Grigg S., et al., “Prevalence and Outcomes of Incidental Imaging Findings: Umbrella Review,” BMJ 361 (2018): k2387, 10.1136/bmj.k2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Davenport M. S., “Incidental Findings and Low‐Value Care,” AJR. American Journal of Roentgenology 221 (2023): 1–7, 10.2214/ajr.22.28926. [DOI] [PubMed] [Google Scholar]
- 22. von Elm E., Altman D. G., Egger M., Pocock S. J., Gøtzsche P. C., and Vandenbroucke J. P., “The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines For Reporting Observational Studies,” Lancet 370, no. 9596 (2007): 1453–1457, 10.1016/s0140-6736(07)61602-x. [DOI] [PubMed] [Google Scholar]
- 23. Australasian College for Emergency Medicine , “Policy on Standard Terminology, Version 7,” 2023.
- 24. Morris A. J., Hensen M., Graves N., et al., “The Burden Of Healthcare‐Associated Infections in New Zealand Public Hospitals 2021,” Infection Control and Hospital Epidemiology 45, no. 10 (2024): 1–1182, 10.1017/ice.2024.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Information CIfH , Overuse of Tests and Treatments in Canada‐Progress Report (CIHI, 2022). [Google Scholar]
- 26. Freire G. C., Diong C., Gandhi S., et al., “Variation in Low‐Value Radiograph Use for Children in the Emergency Department: A Cross‐Sectional Study of Administrative Databases,” CMAJ Open 10, no. 4 (2022): E889–E899, 10.9778/cmajo.20210140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Buchbinder R., Bourne A., Staples M., et al., “Management of Patients Presenting With Low Back Pain to a Private Hospital Emergency Department in Melbourne, Australia,” Emergency Medicine Australasia 34, no. 2 (2022): 157–163, 10.1111/1742-6723.13814. [DOI] [PubMed] [Google Scholar]
- 28. Manoukian S., Stewart S., Graves N., et al., “Bed‐Days and Costs Associated With the Inpatient Burden of Healthcare‐Associated Infection in the UK,” Journal of Hospital Infection 114 (2021): 43–50, 10.1016/j.jhin.2020.12.027. [DOI] [PubMed] [Google Scholar]
- 29. Sun B. C., Hsia R. Y., Weiss R. E., et al., “Effect of Emergency Department Crowding on Outcomes of Admitted Patients,” Annals of Emergency Medicine 61, no. 6 (2013): 605–611, 10.1016/j.annemergmed.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Newton E., “Addressing Overuse in Emergency Medicine: Evidence of a Role For Greater Patient Engagement,” Clinical and Experimental Emergency Medicine 4, no. 4 (2017): 189–200, 10.15441/ceem.17.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Blokzijl J., Dodd R. H., Copp T., et al., “Understanding Overuse of Diagnostic Imaging for Patients With Low Back Pain in the Emergency Department: A Qualitative Study,” Emergency Medicine Journal 38, no. 7 (2021): 529–535, 10.1136/emermed-2020-210345. [DOI] [PubMed] [Google Scholar]
- 32. Morgan D. J., Malani P. N., and Diekema D. J., “Diagnostic Stewardship to Prevent Diagnostic Error,” JAMA 329, no. 15 (2023): 1255–1256, 10.1001/jama.2023.1678. [DOI] [PubMed] [Google Scholar]
- 33. Fabre V., Carroll K. C., and Cosgrove S. E., “Blood Culture Utilization in the Hospital Setting: a Call for Diagnostic Stewardship,” Journal of Clinical Microbiology 60, no. 3 (2022): e01005–e01021, 10.1128/jcm.01005-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grimshaw J. M. and Levinson W., “Reducing Low Value Care: Opportunities and Challenges for Choosing Wisely Campaigns,” BMJ Evidence‐Based Medicine 29 (2023): 215–218, 10.1136/bmjebm-2023-112271. [DOI] [PubMed] [Google Scholar]
- 35. Grimshaw J. M., Patey A. M., Kirkham K. R., et al., “De‐Implementing Wisely: Developing the Evidence Base to Reduce Low‐Value Care,” BMJ Quality and Safety 29, no. 5 (2020): 409–417, 10.1136/bmjqs-2019-010060. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


