ABSTRACT
Objective
This systematic review and meta‐analysis aimed to evaluate the effectiveness of different instrumentation systems in reducing postoperative pain following root canal preparation in primary teeth.
Material and Methods
The present study was conducted in accordance with PRISMA guidelines and registered on PROSPERO (CRD42020135904). The review aimed to determine whether there is a difference in postoperative pain incidence using various instrumentation systems (manual and mechanical) for root canal preparation of primary teeth during pulpectomy. An extensive database search was performed using specific MeSH terms to include clinical studies up to November 2024. Based on eligibility criteria, the selected articles were subjected to quality assessment and the risk of bias was conducted using the Cochrane Risk of Bias (RoB 2) tool. In addition, meta‐analyses were conducted on homogeneous studies.
Results
A total of 11 studies were included for qualitative assessments, and 7 studies underwent quantitative analysis. The results review indicated that mechanical instrumentation systems yielded better overall pain reduction compared to manual systems. The meta‐analysis further demonstrated statistically significant pain reduction at 6 (p < 0.01, 95% CI: 1.46) and 12 h (p < 0.01, 95% CI: 2.15). However, no notable pain reduction or significance were observed at other time points (p = 0.41, 95% CI: 1.66; p = 0.23, 95% CI: 1.67; p = 0.61, 95% CI: 1.25). The overall risk of bias was low for the included studies.
Conclusion
Rotary NiTi instrumentation systems were superior in reducing Postoperative pain incidence in primary teeth undergoing pulpectomy.
Clinical Relevance
Mechanical instrumentation is not only advantageous in decreasing overall treatment time, but also in reducing pain incidence after pulpectomy, which nowadays represents an important and widely used procedure to preserve primary teeth.
Keywords: endodontic treatment, mechanical instrumentation, pain, primary teeth, pulpectomy, root canal preparation
1. Introduction
The preservation of primary teeth until the eruption of permanent successors is of paramount importance for the space maintenance, good development of the oral apparatus, and correct masticatory function (Cleghorn et al. 2010). Irreversible pulp inflammation and involvement of periapical tissue of primary teeth in most cases require pulpectomy to retain the involved tooth until exfoliation and allow normal growth pattern of permanent element (Li et al. 2023). Although endodontic treatment is a widely accepted procedure even in primary dental elements, it's still considered challenging due to the wide range of anatomical variations of the root canal system of primary teeth (Ahmed et al. 2020). Moreover, the success of the therapy over time depends on several factors as proper removal of infected tissue, adequate preparation and disinfection of the root canals, and effective obturation and sealing (Girish Babu et al. 2024). Compared to traditional methods using manual K‐files and H‐files, modern rotary and reciprocating systems are mostly employed to facilitate root shaping (Manchanda et al. 2020; Schachter et al. 2023). Moreover, the introduction of nickel‐titanium (NiTi) files has significantly shortened treatment times in pediatric endodontics (Shetty et al. 2023). Even though some clinicians limit the use of rotary files due to concerns about iatrogenic errors or incomplete pulp tissue removal (Nisar et al. 2024), evidence‐based studies have shown that rotary NiTi files reduce overall treatment time, particularly instrumentation time, while promoting conservative dentin removal and more consistent conical root canal preparations (Panchal, Jeevanandan, and Erulappan 2019). The reciprocating files, as an alternative to the rotary ones, offer enhanced safety during instrumentation, contributing to more efficient canal cleaning (Marques et al. 2023).
It's been widely demonstrated within scientific literature that rotary and reciprocating systems are effective in post‐endodontic pain reduction in the case of permanent teeth (Sun et al. 2018; Martins et al. 2019; Rahbani Nobar et al. 2021); however, clinical data regarding their impact on postoperative pain in primary teeth remain limited (Manchanda et al. 2020; Lakshmanan et al. 2021). Post‐instrumentation pain in pediatric patients typically ranges from mild discomfort to moderate or severe pain, lasting from a few hours to several days (Lakshmanan et al. 2021). In general, posttreatment pain is due to several factors including patient‐related, operator‐related, and treatment protocol‐related factors (Arias et al. 2013). During root canal debridement, extruded dentin debris, combined with microbial agents and chemical disinfectants, can provoke an acute inflammatory response in the periapical tissue, leading to post‐endodontic pain (Sun et al. 2018; Ng et al. 2004). In vitro studies demonstrated that some degree of dentin debris extrusion is inevitable with any instrument design (Suresh et al. 2023).
Recent clinical trials have assessed the effects of different instrumentation systems on postoperative pain in pediatric patients (Asokan et al. 2021; Morankar et al. 2020); however, few data are available to reach a univocal agreement in terms of pain reduction. Therefore, the aim of the present systematic review and meta‐analysis was to evaluate the incidence of postoperative pain following root canal preparation in primary teeth using different manual or mechanical instrumentations.
2. Materials and Methods
The present systematic review was conducted following the PRISMA guidelines (Page et al. 2021), and the protocol was registered on PROSPERO (CRD42020135904). The review aimed to answer the following question: “Is there a difference in postoperative pain incidence when using different instrumentation systems during root canal preparation of primary teeth undergoing pulpectomy?” The PICO framework was as follows:
Population: Subjects with primary teeth underwent pulpectomy.
Intervention: Mechanical root canal preparation with different NiTi instrumentation systems.
Comparison: Manual preparation of the root canal system.
Outcome: Postoperative pain incidence.
2.1. Search Strategy
A comprehensive literature search was performed through multiple electronic databases including PubMed, Scopus, Embase, Google Scholar, Web of Science, and Cochrane up to November 2024. Relevant MeSH terms were used as follows: ((((Primary teeth) OR (Deciduous teeth)) AND (((((Root canal preparation) OR (Endodontic treatment)) OR (Root canal therapy)) OR (Pulp therapy)) OR (Pulpectomy))) AND (((Manual instrumentation) OR (Rotary instrumentation)) OR (Reciprocating instrumentation))) AND (((Postoperative pain) OR (Posttreatment pain)) OR (Post‐endodontic pain)).
In addition, reference lists of the evaluated articles were manually searched to identify other studies for potential inclusion.
2.2. Eligibility Criteria
The following inclusion and exclusion criteria were used to select the studies.
2.2.1. Inclusion Criteria
– Studies published in Peer‐reviewed Journals.
– Studies published in English language.
– Studies reporting clinical trials: randomized clinical trials, prospective comparative clinical trials;‐ Studies reporting on root canal preparation of primary teeth with different instrumentation systems (hand files, rotary, or reciprocating instrumentation) and evaluating postoperative pain incidence.
2.2.2. Exclusion Criteria
– Laboratory‐based studies and ex vivo studies.
– Studies on animal samples.
– Trials involving permanent teeth.
– Case series, case report, reviews and retrospective studies.
– Gray literature.
2.3. Study Selection
Screening and selection of papers were performed by two independent reviewing authors (K.V.T. and K.A.V.) following the eligibility criteria. After the removal of duplicates, studies were assessed by title and abstract. Then, potentially relevant full texts were retrieved for reading and data extraction. Any discrepancies in the study selection process were solved by a third reviewer (G.S.).
2.4. Data Extraction and Qualitative Analysis
The collected data were independently reported by the two reviewers in Excel sheets for further analysis. The following information for each included study was described: authors, year, study design, sample size, age, tooth type, pulpal/periapical condition, instrumentation technique, number of treatment sessions, obturation material used, irrigants or intracanal medicaments, pain assessment scale, prescription of posttreatment analgesics, evolution period, comparison between experimental groups.
Qualitative assessments were conducted on the selected articles using a revised Cochrane risk‐of‐bias tool for randomized trials (RoB 2) (Sterne et al. 2019) by means of Review Manager 5.4 software (RevMan, The Nordic Cochrane Centre, Copenhagen, Denmark). Based on the 5 assessed domains, the selected studies were categorized as having low risk of bias (all domains were satisfied), some concerns (in at least one domain), or high risk of bias (high risk in at least one domain or some concerns for multiple domains).
2.5. Quantitative Synthesis
Meta‐analyses were conducted only on homogeneous studies using Review Manager 5.4 software (RevMan, The Nordic Cochrane Centre, Copenhagen, Denmark). The risk ratio (RR) was calculated to compare the pain rate between the manual instrumentation group and the mechanical instrumentation group, and the results were reported with 95% confidence intervals (CIs). Analysis of overall pain incidence that pooled together all subjects who experienced pain after manual or mechanical instrumentation was performed. In addition, subgroup analyses were carried out based on the time intervals after pulpectomy (6, 12, 24, 48, and 72 h after treatment). Statistical heterogeneity among studies was assessed using the chi‐squared test and the Higgins index (I2). The I2 statistic represents the percentage of diversity in effect estimates due to heterogeneity, rather than sampling error. Pooled estimates were calculated using the Mantel–Haenszel fixed‐effects model of analysis if I2 ≤ 50%; otherwise, a random‐effects model of analysis was applied. All results were expressed as RRs with 95% CIs and shown in forest plots.
3. Results
The search strategy identified a total of 168 studies. Following duplicates removal, 116 papers were screened for title and abstract reading, and 20 studies underwent full‐text reading. According to eligibility criteria, 11 papers were included in the present systematic review and processed for qualitative analysis (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021; Moudgalya et al. 2024; Divya et al. 2019; Bohidar et al. 2024); in addition, 7 studies (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Divya et al. 2019) underwent quantitative evaluation (meta‐analysis) (Figure 1). Characteristics and outcomes of included papers are summarized in Tables 1 and 2.
Figure 1.
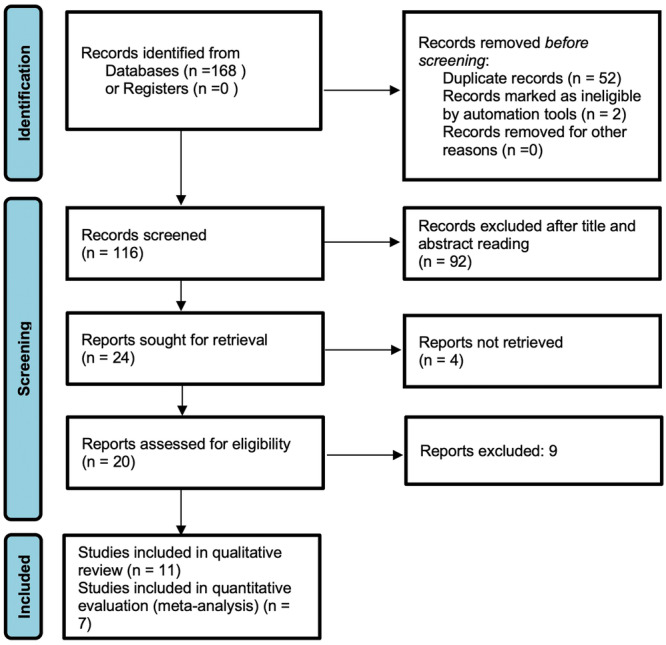
PRISMA flow chart describing the search strategy.
Table 1.
Characteristics of the included studies.
| Study | Type of study | Sample size | Age | Teeth type | Pulpal/periapical condition | Groups' distribution | Instrumentation technique | Number of treatment sessions/obtuartion material | Irrigants or intracanal medicaments | Pain assessment scale | Posttreatment analgesic prescribed |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Marques et al. (2023) | Randomized controlled trial | 151 teeth | 3–9 years | Primary molars | Irreversible pulpitis or apical periodontitis |
Group I: Manual K‐files Group II: Kedo‐S Square rotary files Group III: WaveOne Gold files |
Crown‐down technique | Single visit/Obturation: iodoform‐calcium hydroxide (Vitapex) | 1% NaOCl during instrumentation + final rinse EDTA | Wong‐Baker pain rating scale | Unclear |
| Hadwa et al. (2023) | Randomized controlled trial | 60 teeth | 4–7 years | Mandibular primary second molars | Non‐vital pulp |
Group I: Kedo‐S Square rotary files Group II: Fanta AF_ rotary system Group III: Manual K‐files |
Rotary files: crown down technique; Manual files: Quarter‐turn‐pull technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | 17% EDTA before instrumentation, 1% NaOCl in between files + final flush with normal saline | Four‐point pain intensity scale | Unclear |
| Thakur et al. (2023) | Randomized controlled trial | 75 teeth | 4–9 years | Mandibular primary molars | Pulpitis/absence of periapical lesions |
Group I: XP Endo shaper files Group II: Kedo SG Blue files Group III: Manual K‐files |
XP Endo shaper: continuous rotary movement; Rotary files: crown down technique; Manual files: quarter‐turn‐pull technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | 2.5% NaOCl during instrumentation + final rinse of 17% EDTA + final flush normal saline | Wong‐Baker pain rating scale | Ibuprofen or paracetamol |
| Panchal, Jeevanandan, and Subramanian (2019) | Randomized controlled trial | 75 teeth | 4–6 years | Posterior primary teeth | Pulpal necrosis |
Group I: Manual K‐file Group II: Manual H‐ file Group III: Kedo S files |
Rotary files: crown down technique; Manual K‐files: quarter‐turn‐pull technique; Manual H‐files: retraction technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | Normal saline solution | Modified Wong‐Baker pain rating scale | Ibuprofen or paracetamol |
| Jeevanandan et al. (2020) | Randomized controlled trial | 60 patients | 6–8 years | Maxillary primary teeth | Asymptomatic irreversible pulpitis/absence of periapical lesion |
Group I: Manual NiTi K‐flex files Group II: Reciprocating NiTi flex K‐files Group III: Kedo S rotary files |
Rotary files: crown down technique; Manual K‐files: quarter‐turn‐pull technique; Manual H‐files: retraction technique |
Single visit/Obturation: iodoform‐zinc‐oxide (Endoflas) | 1% NaOCl + EDTA Gel during instrumentation + final rinse of 2% CHX + final flush normal saline | Four‐point pain intensity scale | Ibuprofen or paracetamol |
| Topçuoğlu et al. (2017) | Randomized controlled trial | 106 patients | 6–8 years | Maxillary primary molars | Pulpal necrosis/absence of periapical lesion | Group I: Manual hand K‐file Group II: Revo‐S rotary files | Rotary files: crown down technique, Manual K‐ files: quarter‐turn‐pull technique | Single visit/Obturation: zinc‐oxide eugenol paste | 1% NaOCl between each file. | Four‐point pain intensity scale | Ibuprofen or paracetamol |
| Barasuol et al. (2021) | Randomized controlled trial | 88 patients | 4–9 years | Primary molars | Pulp necrosis or irreversible pulpitis/with or without periapical lesion |
Group I: Manual hand K‐file Group II: ProDesign Logic rotary files |
Rotary files: crown down technique; Manual K‐files: crown down rotation and traction technique |
Single visit/Obturation: zinc‐oxide eugenol paste | 2.5% NaOCl during instrumentation + final rinse of 17% EDTA and 2.5% NaOCl. | Faces Pain Scale Revised | Unclear |
| Tyagi et al. (2021) | Randomized controlled trial | 75 teeth | 4–8 years | Primary molars | Irreversible pulpits, pulpal necrosis, apical periodontitis |
Group I: Manual hand K‐file NiTi flex Group II: ProAF baby gold rotary files Group III: WaveOne Gold reciprocating files |
Rotary and reciprocating file: crown down technique; Manual K‐files NiTi flex: quarter‐turn‐pull technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | 1% NaOCl followed by normal saline | Four‐point pain intensity scale | Unclear |
| Divya et al. (2019) | Randomized controlled trial | 45 teeth | 6–8 years | Mandibular primary molars | Asymptomatic irreversible pulpitis |
Group I: Manual K‐files Group II: Kedo‐S rotary files Group III: K3 rotary files |
Rotary files: crown down technique; Manual K‐files: quarter‐turn‐pull technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | 3% NaOCl during instrumentation + normal saline | Four‐point pain intensity scale | Unclear |
| Moudgalya et al. (2024) | Randomized controlled trial | 75 patients | 5–9 years | Primary molars | Pulpitis or apical periodontitis |
Group I: Kedo S rotary files Group II: Rotary K‐flex files Group III: Hand K‐file or H‐files |
Crown down technique | Two visits/Unclear medication/Obturation: iodoform‐calcium hydroxide (Metapex) |
0.2% CHX and normal saline alternatively in Groups II and III. 17% EDTA gel during instrumentation in Group I. |
Unclear | Unclear |
| Bohidar et al. (2024) | Clinical trial with random allocation | 36 teeth | 4–8 years | Primary molars | Unclear |
Group I: Manual hand K‐file Group II: Kedo S rotary files |
Rotary files: crown down technique; Manual K‐files: balanced force technique |
Single visit/Obturation: iodoform‐calcium hydroxide (Metapex) | 3% NaOCl during instrumentation + normal saline | Four‐point pain intensity scale | Unclear |
Table 2.
Outcomes reported by the included studies.
| Study | Groups | Evaluation period | Preoperative pain | Pain assessments | Analgesic intake |
|---|---|---|---|---|---|
| Marques et al. (2023) |
Group I: Manual K‐files Group I: Kedo‐S Square rotary files Group III: Wave One Gold files |
48 h | Not reported | Manual Hand K‐files = WaveOne Gold files | Manual Hand K‐ files = WaveOne Gold files |
| Hadwa et al. (2023) |
Group I: Kedo‐S Square rotary files Group II: Fanta AF_ rotary system Group III: Manual K‐files |
6, 12, 24, 48 h | Not reported | Kedo‐S Square rotary files > Fanta AF_ rotary system > Manual K‐files | Not assessed |
| Thakur et al. (2023) |
Group I: XP Endo shaper files Group II: Kedo SG Blue files Group III: Manual K‐files |
6, 12, 24, 48, and 72 h | Reported | XP‐ Endo shaper > Kedo‐S Square rotary files > Manual K‐files | Not assessed |
| Panchal, Jeevanandan, and Subramanian (2019) |
Group I: Manual K‐file Group II: Manual H‐ file Group III: Kedo S files |
6, 12, 24, 48 and 72 h | Not reported | Kedo‐S Square rotary files > Manual K‐files > Manual H‐files | Not assessed |
| Jeevanandan et al. (2020) |
Group I: Manual NiTi K‐flex files Group II: Reciprocating NiTi flex K‐files Group III: Kedo S rotary files |
6, 12, 24, 48, and 72 h | Reported | Kedo‐S Square rotary files > Reciprocating NiTi K‐flex files > Manual H‐files | Not assessed |
| Topçuoğlu et al. (2017) |
Group I: Manual hand K‐file Group II: Revo‐S rotary files |
12, 24, 48, 72 h, and one week | Not reported | Revo‐S rotary files > Manual K‐files | Not assessed |
| Barasuol et al. (2021) |
Group I: Manual hand K‐file Group II: ProDesign Logic rotary files |
6 and 72 h (data was pooled together and dichotomized) | Not reported | Manual hand K‐file = ProDesign Logic rotary files | Manual hand K‐file = ProDesign Logic rotary files |
| Tyagi et al. (2021) |
Group I: Manual hand K‐file NiTi flex Group II: ProAF baby gold rotary files Group III: WaveOne Gold reciprocating files |
6, 24, 72 h and 1 week | Reported |
At 6 h: WaveOne gold reciprocating files > ProAF baby gold rotary files > Manual hand K‐file NiTi flex At other time intervals: WaveOne Gold reciprocating files = ProAF baby gold rotary files = Manual hand K‐file NiTi flex |
Not assessed |
| Divya et al. (2019) |
Group I: Manual K‐files Group II: Kedo‐S rotary files Group III: K3 rotary files |
6, 12, 24, 48, and 72 h | Not reported |
Manual K‐files = Kedo‐S rotary files = K3 rotary files |
Not assessed |
| Moudgalya et al. (2024) |
Group I: Kedo S rotary files Group II: Rotary K‐flex files Group III: Hand K‐file or H‐files |
3‐day time intervals (unclear on the actual time intervals assessed) | Not reported |
Kedo S rotary files > Rotary K‐flex files > Hand K‐file or H‐files |
Not assessed |
| Bohidar et al. (2024) |
Group I: Manual hand K‐file Group II: Kedo S rotary files |
6, 12, 24, 48, and 72 h | Reported | Kedo S files > Manual hand K‐files | Not assessed |
A total of 10 included studies were randomized controlled trials (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021; Moudgalya et al. 2024; Divya et al. 2019), while 1 study was a clinical trial (Bohidar et al. 2024). The age range of the study participants was 3–9 years. Regarding evaluated primary teeth, 6 studies included unspecified primary molars (Marques et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Barasuol et al. 2021; Tyagi et al. 2021; Moudgalya et al. 2024; Bohidar et al. 2024), 3 studies focused on mandibular primary molars (Hadwa et al. 2023; Thakur et al. 2023; Divya et al. 2019), and 2 studies specifically analyzed maxillary primary posterior teeth (Jeevanandan et al. 2020; Topçuoğlu et al. 2017). In 10 out 11 studies, the entire pulpectomy procedure was completed in a single visit (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021; Divya et al. 2019; Bohidar et al. 2024), while in 1 article a two‐visit protocol was adopted (Moudgalya et al. 2024). Regarding postoperative pain levels evaluation after pulpectomy, observational time intervals were different. Indeed, 5 studies analyzed pain levels from 6 h to 3 days postoperatively (Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Divya et al. 2019) and 2 studies assessed pain only up to 2 days postoperatively (Marques et al. 2023; Hadwa et al. 2023). Only 2 papers reported outcomes after 1 week (Topçuoğlu et al. 2017; Tyagi et al. 2021). Finally, 2 studies reported pooled and dichotomized 3‐day pain evaluations (Barasuol et al. 2021; Moudgalya et al. 2024), although the specific time intervals used for evaluations were unclear.
Sample sizes varied across the included studies. Precisely, some of them considered the number of patients (Moudgalya et al. 2024), while others evaluated the number of teeth underwent pulpectomy (Marques et al. 2023; Hadwa et al. 2023; Tyagi et al. 2021; Divya et al. 2019; Bohidar et al. 2024). The statistical power of the included studies ranged from 80% (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Jeevanandan et al. 2020; Tyagi et al. 2021; Moudgalya et al. 2024) to 95% (Panchal, Jeevanandan, and Subramanian 2019; Divya et al. 2019). The study by Bohidar et al. (2024) did not provide a sample size calculation.
Regarding preoperative conditions, 4 studies enrolled only teeth with pulpal necrosis (Hadwa et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021), while others also included cases of pulpitis or apical periodontitis (Marques et al. 2023; Thakur et al. 2023; Jeevanandan et al. 2020; Divya et al. 2019; Moudgalya et al. 2024); the diagnostic inclusion criteria were unclear in one study (Bohidar et al. 2024).
Rotary canal instrumentation was obtained by Kedo‐S rotary files (Marques et al. 2023; Hadwa et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Divya et al. 2019; Moudgalya et al. 2024; Bohidar et al. 2024), Fanta files (Hadwa et al. 2023), Revo‐S (Topçuoğlu et al. 2017), Rotary K‐flex files (Moudgalya et al. 2024), K3 Rotary files (Divya et al. 2019), ProDesign Logic rotary files (Barasuol et al. 2021), ProAF Baby Gold rotary files (Tyagi et al. 2021), and XP Endo Shaper file systems (Thakur et al. 2023). The reciprocating motion was used in 3 out 11 studies such as WaveOne Gold file system (Marques et al. 2023; Tyagi et al. 2021) and NiTi Flex file system (Jeevanandan et al. 2020). On the other hand, manual root canal preparation was carried out with K‐files (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Topçuoğlu et al. 2017; Barasuol et al. 2021; Divya et al. 2019; Moudgalya et al. 2024), K‐Niti Flex files (Jeevanandan et al. 2020; Tyagi et al. 2021), or H‐files (Panchal, Jeevanandan, and Subramanian 2019; Moudgalya et al. 2024).
Hand K‐files employed the quarter‐turn and pull motion, while H‐files employed the retraction and pull technique; only Bohidar et al. (2024) used a balanced force technique with manual K‐files. All studies using rotary or reciprocating file systems employed a crown‐down technique.
Irrigation agents varied among the included studies. 1% NaOCl was the most commonly used primary irrigant (Marques et al. 2023; Hadwa et al. 2023; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Tyagi et al. 2021), followed by 3% NaOCl (Divya et al. 2019; Bohidar et al. 2024) and 2.5% NaOCl without dilution (Thakur et al. 2023; Barasuol et al. 2021). Two studies (Jeevanandan et al. 2020; Moudgalya et al. 2024) reported the use of 2% CHX, either as an irrigant or a final flush. Final rinse of 17% EDTA was used in 5 studies (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Barasuol et al. 2021; Moudgalya et al. 2024), while in 2 papers, EDTA was applied as gel during instrumentation (Jeevanandan et al. 2020; Moudgalya et al. 2024). Only one study used saline solution as irrigant from the initial instrumentation phase up to final shaping (Panchal, Jeevanandan, and Subramanian 2019).
Regarding obturation materials, Ca(OH)₂ with iodoform (Metapex or Vitapex) was the most commonly used agent (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Tyagi et al. 2021; Moudgalya et al. 2024; Divya et al. 2019; Bohidar et al. 2024). Combinations of zinc oxide and iodoform (Endoflas) was used in 1 study (Jeevanandan et al. 2020), while 2 studies applied zinc oxide eugenol as final obturation (Topçuoğlu et al. 2017; Barasuol et al. 2021).
Pain rating scales used to evaluate pain level were different among studies. Specifically, 7 papers used a four‐point pain intensity scale for pain analysis (Hadwa et al. 2023; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021; Divya et al. 2019; Bohidar et al. 2024), 2 studies used the Wong‐Baker pain rating scale (Marques et al. 2023; Thakur et al. 2023), and 1 study used the Modified Wong‐Baker scale (Panchal, Jeevanandan, and Subramanian 2019). Unclear pain scale was reported in only 1 study (Moudgalya et al. 2024). Preoperative pain was clearly assessed in 4 papers (Thakur et al. 2023; Jeevanandan et al. 2020; Tyagi et al. 2021; Bohidar et al. 2024). Prescribed postoperative analgesics were unspecified in 7 studies (Marques et al. 2023; Hadwa et al. 2023; Barasuol et al. 2021; Tyagi et al. 2021; Divya et al. 2019; Moudgalya et al. 2024; Bohidar et al. 2024), whereas 4 studies (Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017) prescribed ibuprofen or paracetamol as an alternative in case of hypersensitivity. None of the included studies clearly specified the dosages. The effect of postoperative analgesic intake on pain was evaluated in just 2 studies (Marques et al. 2023; Barasuol et al. 2021), without reporting any significant differences among assessed groups.
3.1. Risk of Bias
The quality of the included articles was assessed using the Cochrane Risk of Bias tool (RoB 2). Among the included studies, 5 demonstrated some concerns (Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Divya et al. 2019; Moudgalya et al. 2024; Bohidar et al. 2024) while the remaining 6 had been categorized as having low risk of bias (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Topçuoğlu et al. 2017; Barasuol et al. 2021; Tyagi et al. 2021). The shortcomings mostly concerned the randomization process or deviations from the intended interventions (Figure 2). The overall risk of biased judgment of all studies was classified as low risk (Figure 3).
Figure 2.
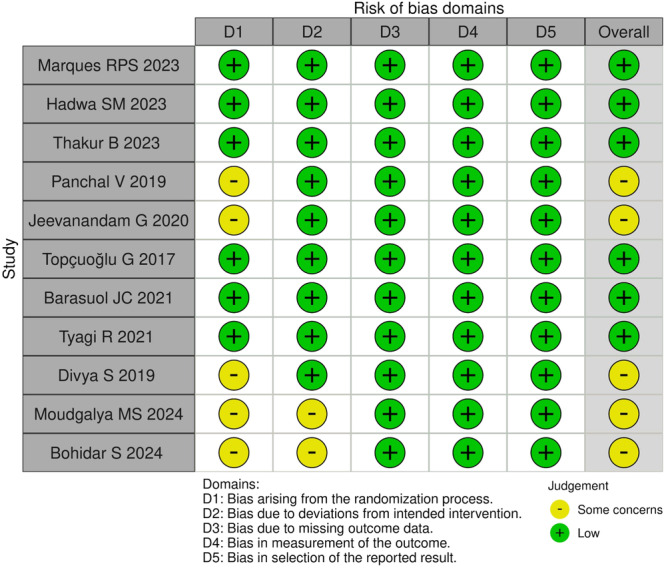
Risk of Bias Graph obtained by revised Cochrane risk‐of‐bias tool for randomized trials (RoB 2).
Figure 3.
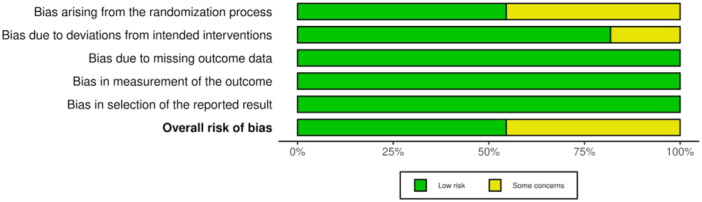
Risk of Bias Summary obtained by revised Cochrane risk‐of‐bias tool for randomized trials (RoB 2).
3.2. Meta‐Analysis
Quantitative evaluation was performed on 7 studies (Marques et al. 2023; Hadwa et al. 2023; Thakur et al. 2023; Panchal, Jeevanandan, and Subramanian 2019; Jeevanandan et al. 2020; Topçuoğlu et al. 2017; Divya et al. 2019). Studies conducted by Barasuol et al. (2021) and Moudgalya et al. (2024) were excluded due to a lack of clarity in pain assessment during different time points. In addition, papers by Tyagi et al. (2021) and Bohidar et al. (2024) were excluded since pain scores were provided only as mean values and standard deviations. A random effects model was employed due to variations in patients' demographic data, initial pulpal diagnosis, irrigation protocol, instrumentation technique, and intracanal medicaments used. Follow‐up time periods, as well as the pain assessment scales, varied among the studies. A statistically significant difference in the overall pain incidence was observed between manual and mechanical instrumentation systems, with favorable outcomes for the latter after pulpectomy procedures (Heterogeneity: Tau² = 0.0648; Chi² = 19.16, df = 6 (p < 0.01); I 2 = 69%, Z = 2.65 (p < 0.01)) (Figure 4).
Figure 4.
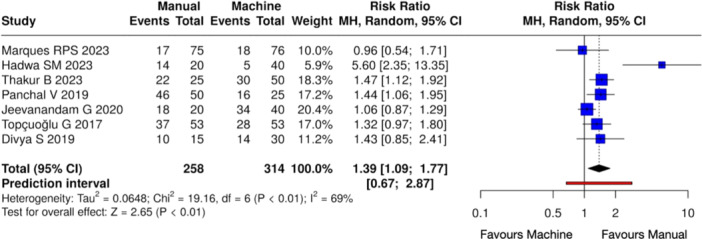
Forest plot of overall postoperative pain incidence between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. Pain occurrence was statistically higher in the case of manual instrumentation.
Meta‐analyses at different time intervals showed a statistically significant difference in pain occurrence in the manual instrumentation groups at 6 h (Heterogeneity: Tau² = 0.0795; Chi² = 20.05, df = 5 (p < 0.01); I 2 = 75%, Z = 2.71 (p < 0.01)) (Figure 5) and 12 h (Heterogeneity: Tau² = 0.2606; Chi² = 15.78, df = 5 (p < 0.01); I 2 = 68%, Z = 2.93 (p < 0.01)) (Figure 6) when compared with mechanical shaping. On the other hand, no notable variations were observed between the manual and mechanical instrumentation groups at 24 h (Heterogeneity: Tau² = 0.9957; Chi² = 11.68, df = 3 (p < 0.01); I 2 = 74%, Z = 0.83 (p = 0.41)) (Figure 7), 48 h (Heterogeneity: Tau² = 0.3833; Chi² = 8.29, df = 3 (p = 0.04); I 2 = 64%, Z = 1.21 (p = 0.23)) (Figure 8), and 72 h (Heterogeneity: Tau² = NA; Chi² = 0.00, df = 0 (p = NA); I 2 = NA%, Z = 0.52 (p = 0.61)) (Figure 9).
Figure 5.
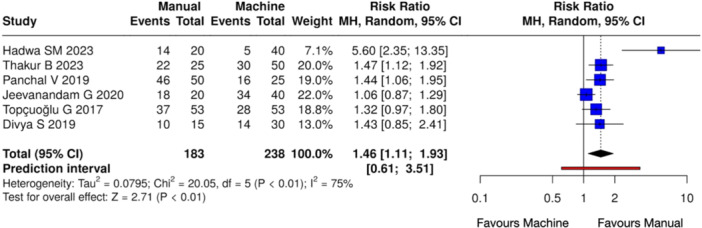
Forest plot of overall postoperative pain incidence at 6 h between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. Pain occurrence was statistically higher in the case of manual instrumentation.
Figure 6.
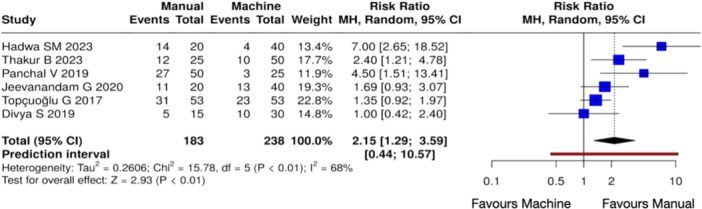
Forest plot of overall postoperative pain incidence at 12 h between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. Pain occurrence was statistically higher in the case of manual instrumentation.
Figure 7.
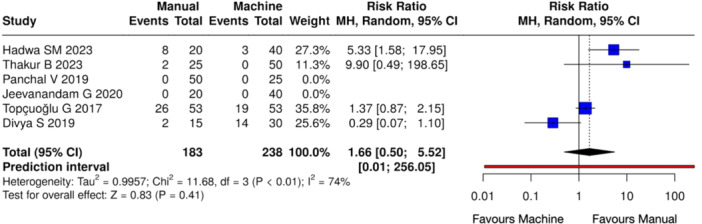
Forest plot of overall postoperative pain incidence at 24 h between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. There was no statistically significant difference between manual and mechanical instrumentation.
Figure 8.
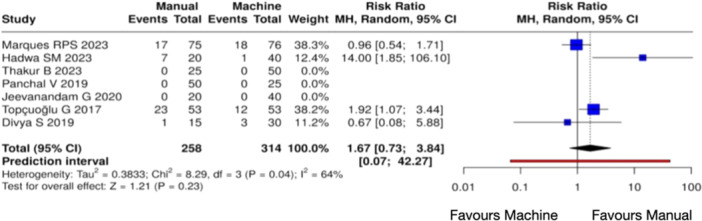
Forest plot of overall postoperative pain incidence at 48 h between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. There was no statistically significant difference between manual and mechanical instrumentation.
Figure 9.
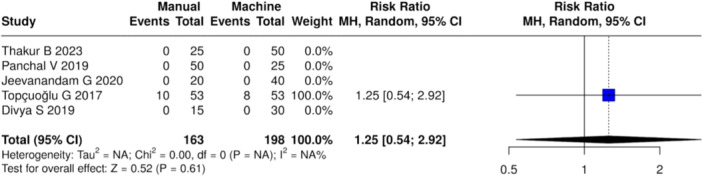
Forest plot of overall postoperative pain incidence at 72 h between manual and mechanical instrumentation systems after pulpectomy procedures of primary teeth. There was no statistically significant difference between manual and mechanical instrumentation.
4. Discussion
The current systematic review and meta‐analysis were conducted to evaluate the effectiveness of manual and mechanical root canal instrumentations in reducing postoperative pain incidence following pulpectomy procedures. Previous systematic reviews have analyzed various aspects of root canal treatment, including success rates, quality of root canal filling, instrumentation, cleaning efficacy and postoperative pain occurrence (Manchanda et al. 2020; Lakshmanan et al. 2021; Asokan et al. 2021; Padmawar et al. 2025; Chugh et al. 2021; Kalaskar et al. 2024).
Regarding pain incidence following the use of various instrumentation systems, a previous study (Lakshmanan et al. 2021) reported data only on 3 papers, while the present paper provided a comprehensive review analyzing 11 studies from a qualitative point of view and 7 studies were further quantitatively evaluated. In accordance with scientific literature, it's been demonstrated that rotary instrumentation was significantly superior to hand instrumentation in reducing overall postoperative pain. It should be considered that primary teeth are more predisposed to debris apical extrusion due to root anatomy as well as physiological root resorption; in this light, mechanical instrumentation seemed to reduce the amount of debris pushed into periapical tissue (Rahbani Nobar et al. 2021) and, thanks to better cutting abilities, decrease the instrumentation time, contributing to lesser pain incidence than manual techniques (Panchal, Jeevanandan, and Erulappan 2019; Khadmi et al. 2025). Although in permanent dentition differences of apical extrusion of debris caused by rotary and reciprocating systems are reported (Alhayki 2025; Villani et al. 2024; Western and Dicksit 2017), regarding primary teeth, the degree of extruded debris by different mechanical instrumentations should be better elucidated. A lesser extent of apical extrusion has been observed when using dedicated pediatric rotary systems (Kamatchi et al. 2024).
The analysis of root canals of primary teeth after instrumentation revealed a higher preservation of remaining dentin thickness caused by manual preparation and the production of less dentin cracks when compared to rotary and reciprocating systems (Saha and Singh 2022), even though iatrogenic errors such as canal transportation and apical blockage have been observed (George et al. 2016). On the other hand, the reciprocating systems significantly reduced the instrumentation time and the rotary ones produced lesser canal transportation (Saha and Singh 2022), obtaining a better canal shaping as well as tridimensional space for correct obturation (Kumaran et al. 2024). Limitations of mechanical instrumentation are commonly due to instrument fracture, overheating, and loss of hard tissue, mostly in the case of thinner root dentin. These drawbacks might be overcome by new thermal treatments and motions to increase mechanical performances, limit the risks of iatrogenic complications, and mitigate posttreatment pain incidence (Azizi and Azizi 2021; Pelliccioni et al. 2023; Tabassum et al. 2019; Zupanc et al. 2018).
The conducted meta‐analyses suggested a significant pain reduction in the case of mechanical instrumentation 6 and 12 h after endodontic treatment. On the other hand, no significant differences were observed at 24, 42, 72 h. As for permanent dentition, pain following root canal therapy is most commonly experienced 6 and 12 h after treatment (Smith et al. 2017), underlying how critical that time interval is. In addition, the present study considered an evaluation range until 72 h, that represented the interval time in which post‐endodontic pain is mainly represented (Shamszadeh et al. 2020). Pain is inherently multifactorial, and its subjective nature varies across individuals (Spohr et al. 2019). In addition, other variables might contribute to pain incidence and intensity, as correct use of irrigants, obturation technique, number of visits/interventions, and operator's skills (Ng et al. 2004; Valizadeh et al. 2024; Tirupathi et al. 2019; Priyadarshini 2021). Regarding disinfection protocols, some variations were reported by the included studies. 1% NaOCl was the most widely used concentration, followed by 2.5% and 3%. Moreover, EDTA or CHX were used in a few other studies, without precisely describing the volume or the irrigation regimen followed. These inconsistencies might be considered as confounding factors in postoperative pain incidence and should be taken into account in the interpretation of outcomes, although current data from high‐quality evidence revealed no significant differences between 1% NaOCl and higher concentrations in pulpectomy procedures (Gurunathan et al. 2024). Moreover, the effect on peri‐apical tissue of apical extrusion of irrigants or infected debris caused by irrigation procedures should be considered as additional cofounding variables in pain incidence (Valizadeh et al. 2024). Regarding obturation material, the iodoform‐calcium hydroxide combination was mostly used in the included studies, not representing a potential unfavorable factor in the interpretation of the results. Although extrusion of obturation material is an uncommon event in the treatment of primary teeth, the success of tridimensional sealing of the root canal system strictly depends on the proper technique of instrumentation (Priyadarshini 2021). All included studies, except for Moudgalya et al. (2024), performed pulpectomies in a single visit, without intracanal medication. This aspect might be relevant in the outcomes' interpretation and is in line with current scientific literature that emphasized the importance of completing the pulpectomy in a single visit whenever feasible (Tirupathi et al. 2019).
Quality analysis of included studies demonstrated an overall low risk of bias. All studies were randomized clinical trials, except for Bohidar et al. (2024) which was a clinical study with some concerns. Moreover, all included papers clearly reported their sample sizes, mainly employed 80% power for their calculations, and did not experience loss to follow‐up, reducing potential bias.
The results obtained by the present systematic review and meta‐analysis might provide a significant clinical implication, since in pediatric patients, treatment time is a crucial factor in reducing anxiety (Manchanda et al. 2020), which, in turn, improves operator efficiency and enhances therapeutic outcomes. Children often lack the communication skills or the ability to properly express discomfort, and together with the difficulty of the treatment procedure, as well as the need for rapid interventions, are of paramount importance in their management. In this regard, mechanical instrumentation is not only advantageous in decreasing overall treatment time, but also in reducing pain incidence after therapy. However, further clinical trials should be prospectively planned to support the obtained outcomes and precisely individualize all factors that would contribute to the clinical success over time, reducing side effects.
5. Limitations
Regarding the limitations of the current systematic review and meta‐analysis, it should be noted that the current review pooled together all types of instrumentation designs and kinematics, including rotary and reciprocating systems. Therefore, the extrapolation of results cannot be confined to a single system or design. Future systematic reviews are warranted to evaluate success rates and clinical outcomes, precisely assessing single instrumentation systems and making comparisons between systematics. In addition, the present study included papers dealing with non‐vital primary teeth or vital primary teeth with signs and symptoms of irreversible pulpitis, that were candidate to root canal therapy; however, the pulp status and degree of inflammation were impossible to be evaluated, and these aspects may have an impact in pain perception, healing and postoperative pain incidence. Moreover, the presence of preoperative pain was clearly assessed in only 4 papers (Thakur et al. 2023; Jeevanandan et al. 2020; Tyagi et al. 2021; Bohidar et al. 2024), and its impact on post‐endodontic pain remained difficult to figure out. Finally, it should be stressed that pain assessment was based on a subjective evaluation carried out by patients and/or their caregivers, expressed through different scales that assessed only pain presence/absence or its level as mild/moderate/severe. These aspects limited the clear description of pain without providing specific signs and symptoms.
6. Conclusion
The present systematic review and meta‐analysis demonstrated a statistically significant reduction in pain incidence 6 and 12 h after pulpectomy of primary teeth with mechanical instrumentation when compared to manual files. The obtained results might be useful not only in decreasing overall intervention time, but also in improving the therapeutic outcomes and ease pulpectomy that nowadays represents an important and widely used procedure to preserve primary teeth.
Author Contributions
Kavalipurapu Venkata Teja: study design and data extraction. Kaligotla Apoorva Vasundhara: data extraction and meta‐analysis. Gianrico Spagnuolo: critical revision and results interpretation. Niccolò Giuseppe Armogida: artworks and literature search. Flavia Iaculli: writing and editing of the original manuscript. Carlo Rengo: supervision.
Ethics Statement
The authors have nothing to report.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgments
Open access publishing facilitated by Universita degli Studi di Napoli Federico II, as part of the Wiley ‐ CRUI‐CARE agreement.
Flavia Iaculli and Carlo Rengo equally contributed equally to this study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Ahmed, H. M. A. , Musale P. K., El Shahawy O. I., and Dummer P. M. H.. 2020. “Application of a New System for Classifying Tooth, Root and Canal Morphology in the Primary Dentition.” International Endodontic Journal 53: 27–35. [DOI] [PubMed] [Google Scholar]
- Alhayki, M. M. 2025. “Evaluation of Apically Extruded Debris During Root Canal Preparation Using ProTaper Ultimate and ProTaper Gold: An Ex Vivo Study.” European Endodontic Journal 10: 41–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias, A. , de la Macorra J. C., Hidalgo J. J., and Azabal M.. 2013. “Predictive Models of Pain Following Root Canal Treatment: A Prospective Clinical Study.” International Endodontic Journal 46: 784–793. [DOI] [PubMed] [Google Scholar]
- Asokan, S. , Natchiyar N., Priya P. R. G., and Kumar T. D. Y.. 2021. “Comparison of Clinical and Radiographic Success of Rotary With Manual Instrumentation Techniques in Primary Teeth: A Systematic Review.” International Journal of Clinical Pediatric Dentistry 14: 8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azizi, A. , and Azizi A.. 2021. “In‐Depth Metallurgical and Microstructural Analysis of Oneshape and Heat Treated Onecurve Instruments.” European Endodontic Journal 6, no. 1: 90–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barasuol, J. C. , Massignan C., Bortoluzzi E. A., Cardoso M., and Bolan M.. 2021. “Influence of Hand and Rotary Files for Endodontic Treatment of Primary Teeth on Immediate Outcomes: Secondary Analysis of a Randomized Controlled Trial.” International Journal of Paediatric Dentistry 31: 143–151. [DOI] [PubMed] [Google Scholar]
- Bohidar, S. , Goswami P., Arya A., Singh S., Samir P. V., and Bhargava T.. 2024. “An In Vivo Evaluation of Postoperative Pain After Root Canal Instrumentation Using Manual K‐Files and Kedo‐S Rotary Files in Primary Molars.” Journal of Pharmacy and BioAllied Sciences 16: S136–S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chugh, V. K. , Patnana A. K., Chugh A., Kumar P., Wadhwa P., and Singh S.. 2021. “Clinical Differences of Hand and Rotary Instrumentations During Biomechanical Preparation in Primary Teeth – A Systematic Review and Meta‐Analysis.” International Journal of Paediatric Dentistry 31: 131–142. [DOI] [PubMed] [Google Scholar]
- Cleghorn, B. M. , Boorberg N. B., and Christie W. H.. 2010. “Primary Human Teeth and Their Root Canal Systems.” Endodontic Topics 23: 6–33. [Google Scholar]
- Divya, S. , Jeevanandan G., Sujatha S., Subramanian E. G., and Ravindran V.. 2019. “Comparison of Quality of Obturation and Post‐Operative Pain Using Manual vs Rotary Files in Primary Teeth – A Randomised Clinical Trial.” Indian Journal of Dental Research 30: 904–908. [DOI] [PubMed] [Google Scholar]
- George, S. , Anandaraj S., Issac J. S., John S. A., and Harris A.. 2016. “Rotary Endodontics in Primary Teeth – A Review.” Saudi Dental Journal 28: 12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girish Babu, K. L. , Gururaj Hebbar K., and Doddamani G. M.. 2024. “Correlation Between Quality of Obturation and Outcome of Pulpectomized Primary Molars Following Root Canal Instrumentation With Pediatric Rotary File Systems.” Pediatric Dental Journal 34: 27–34. [Google Scholar]
- Gurunathan, D. , Thangavelu L., and Mukundan D.. 2024. “Comparative Evaluation of 1% Sodium Hypochlorite vs Other Intracanal Irrigants During Pulpectomy of Primary Teeth: A Systematic Review.” World Journal of Dentistry 15: 451–456. [Google Scholar]
- Hadwa, S. M. , Ghouraba R. F., Kabbash I. A., and El‐Desouky S. S.. 2023. “Assessment of Clinical and Radiographic Efficiency of Manual and Pediatric Rotary File Systems in Primary Root Canal Preparation: A Randomized Controlled Clinical Trial.” BMC Oral Health 23: 687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeevanandan, G. , Ravindran V., Subramanian E. M., and Kumar A. S.. 2020. “Postoperative Pain With Hand, Reciprocating, and Rotary Instrumentation Techniques After Root Canal Preparation in Primary Molars: A Randomized Clinical Trial.” International Journal of Clinical Pediatric Dentistry 13: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalaskar, R. , Vinay V., Gala U. P., Joshi S., and Doiphode A. R.. 2024. “Comparative Evaluation of Effectiveness of Rotary and Hand File Systems in Terms of Quality of Obturation and Instrumentation Time Among Primary Teeth: A Systematic Review and Meta‐Analysis of Randomized Controlled Trials.” International Journal of Clinical Pediatric Dentistry 17: 962–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamatchi, M. , Gawthaman M., Vinodh S., Manoharan M., Kowsalya S., and Mathian V. M.. 2024. “Comparative Evaluation of Apical Debris Extrusion in Primary Molars Using Three Different Pediatric Rotary Systems: An In Vitro Study.” International Journal of Clinical Pediatric Dentistry 17: 1224–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadmi, I. , Hamrouni A., and Chouchene F.. 2025. “Different Outcomes of Rotary and Manual Instrumentation in Primary Teeth Pulpectomy: A Systematic Review and Meta‐Analysis.” European Archives of Paediatric Dentistry 26: 423–450. 10.1007/s40368-025-01020-x. [DOI] [PubMed] [Google Scholar]
- Kumaran, P. , Xavier A. M., Venugopal M., et al. 2024. “Volumetric Analysis of Hand and Rotary Instrumentation, Root Canal Filling Techniques, and Obturation Materials in Primary Teeth Using Spiral CT.” Journal of Contemporary Dental Practice 25: 250–259. [DOI] [PubMed] [Google Scholar]
- Lakshmanan, L. , Somasundaram S., Jeevanandan G., and Subramanian E.. 2021. “Evaluation of Postoperative Pain After Pulpectomy Using Different File Systems in Primary Teeth: A Systematic Review.” Contemporary Clinical Dentistry 12: 3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, L. , Yang X., Ju W., Li J., and Yang X.. 2023. “Impact of Primary Molars With Periapical Disease on Permanent Successors: A Retrospective Radiographic Study.” Heliyon 9: e15854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchanda, S. , Sardana D., and Yiu C. K. Y.. 2020. “A Systematic Review and Meta‐Analysis of Randomized Clinical Trials Comparing Rotary Canal Instrumentation Techniques With Manual Instrumentation Techniques in Primary Teeth.” International Endodontic Journal 53: 333–353. [DOI] [PubMed] [Google Scholar]
- Marques, R. P. S. , Oliveira N. M., Barbosa V. R. P., et al. 2023. “Reciprocating Instrumentation for Endodontic Treatment of Primary Molars: 24‐month Randomized Clinical Trial.” International Journal of Paediatric Dentistry 33: 325–334. [DOI] [PubMed] [Google Scholar]
- Martins, C. , De Souza Batista V., Andolfatto Souza A., Andrada A., Mori G., and Gomes Filho J.. 2019. “Reciprocating Kinematics Leads to Lower Incidences of Postoperative Pain Than Rotary Kinematics After Endodontic Treatment: A Systematic Review and Meta‐Analysis of Randomized Controlled Trial.” Journal of Conservative Dentistry 22: 320–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morankar, R. , Goyal A., Gauba K., Kapur A., and Bhatia S. K.. 2018. “Manual Versus Rotary Instrumentation for Primary Molar Pulpectomies – A 24 Months Randomized Clinical Trial.” Pediatric Dental Journal 28: 96–102. [Google Scholar]
- Moudgalya, M. S. , Tyagi P., Tiwari S., Tiwari T., Umarekar P., and Shrivastava S.. 2024. “To Compare and Evaluate Rotary and Manual Techniques in Biomechanical Preparation of Primary Molars to Know Their Effects in Terms of Cleaning and Shaping Efficacy.” International Journal of Clinical Pediatric Dentistry 17: 864–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng, Y. L. , Glennon J. P., Setchell D. J., and Gulabivala K.. 2004. “Prevalence of and Factors Affecting Post‐Obturation Pain in Patients Undergoing Root Canal Treatment.” International Endodontic Journal 37: 381–391. [DOI] [PubMed] [Google Scholar]
- Nisar, P. , Katge F., Chimata V. K., Pradhan D., Patil D., and Agrawal I.. 2024. “Comparative Evaluation of Hand and Rotary File Systems on Dentinal Microcrack Formation During Pulpectomy Procedure in Primary Teeth: An In Vitro Study.” European Archives of Paediatric Dentistry 25: 181–189. [DOI] [PubMed] [Google Scholar]
- Padmawar, N. , Pawar N., Tripathi V., Banerjee S., Tyagi G., and Joshi S. R.. 2025. “Comparative Analysis of Rotary Versus Manual Instrumentation in Paediatric Pulpectomy Procedures: A Systematic Review and Meta‐Analysis.” Australian Endodontic Journal 51: 181–196. 10.1111/aej.12899. [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie J. E., Bossuyt P. M., et al. 2021. “The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews.” BMJ 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal, V. , Jeevanandan G., and Erulappan S. M.. 2019. “Comparison Between the Effectiveness of Rotary and Manual Instrumentation in Primary Teeth: A Systematic Review.” International Journal of Clinical Pediatric Dentistry 12: 340–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal, V. , Jeevanandan G., and Subramanian E. M. G.. 2019. “Comparison of Post‐Operative Pain After Root Canal Instrumentation With Hand K‐Files, H‐Files and Rotary Kedo‐S Files in Primary Teeth: A Randomised Clinical Trial.” European Archives of Paediatric Dentistry 20: 467–472. [DOI] [PubMed] [Google Scholar]
- Pelliccioni, G. A. , Schiavon R., Zamparini F., et al. 2023. “Physico‐Mechanical Properties of Two Different Heat Treated Nickel‐Titanium Instruments: In Vitro Study.” Giornale Italiano Di Endodonzia 38, no. 1: 28–36. [Google Scholar]
- Priyadarshini, P. 2021. “Comparative Evaluation of Quality of Obturation and Its Effect on Postoperative Pain Between Pediatric Hand and Rotary Files: A Double‐Blinded Randomized Controlled Trial.” International Journal of Clinical Pediatric Dentistry 14: 88–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahbani Nobar, B. , Dianat O., Rahbani Nobar B., et al. 2021. “Effect of Rotary and Reciprocating Instrumentation Motions on Postoperative Pain Incidence in Non‐Surgical Endodontic Treatments: A Systematic Review and Meta‐Analysis.” European Endodontic Journal 6: 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha, S. , and Singh P.. 2022. “Cone‐Beam Computed Tomographic Analysis of Deciduous Root Canals After Instrumentation With Different Filing Systems: An In Vitro Study.” International Journal of Clinical Pediatric Dentistry 15: S22–S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter, D. , Blumer S., Sarsur S., et al. 2023. “Exploring a Paradigm Shift in Primary Teeth Root Canal Preparation: An Ex Vivo Micro‐CT Study.” Children 10: 792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamszadeh, S. , Shirvani A., and Asgary S.. 2020. “Does Occlusal Reduction Reduce Post‐Endodontic Pain? A Systematic Review and Meta‐Analysis.” Journal of Oral Rehabilitation 47: 528–535. [DOI] [PubMed] [Google Scholar]
- Shetty, B. , Singh R., Patil V., Tirupathi S. P., Nene K., and Rathi N.. 2023. “Comparative Evaluation of Single Rotary File System and Sequential Multi‐File Rotary Systems on Time for Biomechanical Preparation and Obturation Quality in Single‐Visit Pulpectomy Protocol: A Double‐Blind Randomized Clinical Trial.” International Journal of Clinical Pediatric Dentistry 16: 247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, E. A. , Marshall J. G., Selph S. S., Barker D. R., and Sedgley C. M.. 2017. “Nonsteroidal Anti‐Inflammatory Drugs for Managing Postoperative Endodontic Pain in Patients Who Present With Preoperative Pain: A Systematic Review and Meta‐Analysis.” Journal of Endodontics 43: 7–15. [DOI] [PubMed] [Google Scholar]
- Spohr, A. R. , Sarkis‐Onofre R., Pereira‐Cenci T., Pappen F. G., and Dornelles Morgental R.. 2019. “A Systematic Review: Effect of Hand, Rotary and Reciprocating Instrumentation on Endodontic Postoperative Pain.” Giornale Italiano Di Endodonzia 33: 24–34. [Google Scholar]
- Sterne, J. A. C. , Savović J., Page M. J., et al. 2019. “RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials.” BMJ 366: l4898. [DOI] [PubMed] [Google Scholar]
- Sun, C. , Sun J., Tan M., Hu B., Gao X., and Song J.. 2018. “Pain After Root Canal Treatment With Different Instruments: A Systematic Review and Meta‐Analysis.” Oral Diseases 24: 908–919. [DOI] [PubMed] [Google Scholar]
- Suresh, B. , Jeevanandan G., Ravindran V., et al. 2023. “Comparative Evaluation of Extrusion of Apical Debris in Primary Maxillary Anterior Teeth Using Two Different Rotary Systems and Hand Files: An In Vitro Study.” Children 10: 898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabassum, S. , Zafar K., and Umer F.. 2019. “Nickel‐Titanium Rotary File Systems: What's New?” European Endodontic Journal 4: 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur, B. , Bhardwaj A., Wahjuningrum D. A., et al. 2023. “Incidence of Post‐Operative Pain Following a Single‐Visit Pulpectomy in Primary Molars Employing Adaptive, Rotary, and Manual Instrumentation: A Randomized Clinical Trial.” Medicina 59: 355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirupathi, S. P. , Krishna N., Rajasekhar S., and Nuvvula S.. 2019. “Clinical Efficacy of Single‐Visit Pulpectomy Over Multiple‐Visit Pulpectomy in Primary Teeth: A Systematic Review.” International Journal of Clinical Pediatric Dentistry 12: 453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topçuoğlu, G. , Topçuoğlu H. S., Delikan E., Aydınbelge M., and Dogan S.. 2017. “Postoperative Pain After Root Canal Preparation With Hand and Rotary Files in Primary Molar Teeth.” Pediatric Dentistry 39: 192–196. [PubMed] [Google Scholar]
- Tyagi, R. , Khatri A., Kalra N., and Sabherwal P.. 2021. “Comparative Evaluation of Hand K‐Flex Files, Pediatric Rotary Files, and Reciprocating Files on Instrumentation Time, Postoperative Pain, and Child's Behavior in 4–8‐Year‐Old Children.” International Journal of Clinical Pediatric Dentistry 14: 201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valizadeh, M. , Gheidari A., Daghestani N., Mohammadzadeh Z., and Khorakian F.. 2024. “Evaluation of Various Root Canal Irrigation Methods in Primary Teeth: A Systematic Review.” BMC Oral Health 24: 1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villani, F. A. , Zamparini F., Spinelli A., Aiuto R., and Prati C.. 2024. “Apical Debris Extrusion and Potential Risk of Endodontic Flare‐Up: Correlation With Rotating and Reciprocating Instruments Used in Daily Clinical Practice.” Giornale Italiano Di Endodonzia 38, no. 1: 79–23. [Google Scholar]
- Western, J. , and Dicksit D.. 2017. “Apical Extrusion of Debris in Four Different Endodontic Instrumentation Systems: A Meta‐Analysis.” Journal of Conservative Dentistry 20: 30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zupanc, J. , Vahdat‐Pajouh N., and Schäfer E.. 2018. “New Thermomechanically Treated NiTi Alloys – A Review.” International Endodontic Journal 51: 1088–1103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


