Abstract
Background
Proximal tibiofibular joint instability (PTJI) is a rare condition, particularly in total knee arthroplasty (TKA) revision, with only one prior case reported. This case highlights the importance of considering PTJI in patients with chronic lateral knee pain and instability following TKA and demonstrates a novel stabilization approach for managing this challenging condition.
Case Description
A 73-year-old female with a history of multiple knee surgeries presented to our clinic due to increasing lateral knee pain radiating along the syndesmosis, aggravated by activities like squatting. Clinical examination revealed anteroposterior subluxation of the fibular head, suggesting PTJI. Radiological findings confirmed tibial component loosening, and the diagnosis of aseptic loosening with PTJI was made. Given her complex surgical history, a two-stage revision was planned. The first stage involved prosthesis removal, bacteriological sampling, and spacer placement. The second stage included revision TKA and proximal tibiofibular joint (PTFJ) stabilization using a Twin Tail Tight-Rope™ system and Arthrex endobutton, preserving joint mobility and restoring functional stability. A hinged revision knee prosthesis was then implanted. The patient had an uneventful recovery. At 1-year follow-up, the pain score was 1/10 and she achieved good mobility. Radiographs showed satisfactory implant positioning. The Western Ontario and McMaster Universities Arthritis Index (WOMAC) score of 15/96 indicated a successful outcome.
Conclusions
PTJI is rare and is not typically associated with TKA. This case report highlights a unique presentation of PTJI in a multi-revised TKA, raising concerns about the potential role of repeated proximal tibial resections in ligamentous instability of the PTFJ. The specific localization of pain and its resolution following PTFJ fixation support this hypothesis. Therefore, careful assessment of the PTFJ should be considered in TKA revisions, particularly in cases involving extensive lateral tibial resections.
Keywords: Proximal tibiofibular joint instability (PTJI), revision knee surgery, case report, ligamentous injury, complications in total knee arthroplasty (complications in TKA)
Highlight box.
Key findings
• Proximal tibiofibular joint instability (PTJI) is an exceptionally rare condition in the context of total knee arthroplasty revisions, with only one previously reported case.
• This case describes a 73-year-old patient with chronic lateral knee pain due to PTJI following multiple total knee arthroplasty revisions.
• Surgical stabilization using a Twin Tail Tight-Rope™ system and an Arthrex endobutton resulted in pain resolution and satisfactory functional outcomes.
What is known and what is new?
• PTJI is most commonly associated with trauma but is not typically linked to total knee arthroplasty.
• This case raises the possibility that repeated proximal tibial resections during total knee arthroplasty revisions may contribute to ligamentous insufficiency, leading to instability. It also demonstrates a successful surgical stabilization technique that preserves some joint mobility.
What is the implication, and what should change now?
• Surgeons performing total knee arthroplasty revisions should consider PTJI as a potential cause of persistent lateral knee pain.
• In cases where instability is confirmed intraoperatively, appropriate stabilization should be performed to improve patient outcomes.
• Further research is needed to determine the prevalence of this complication and whether prophylactic measures should be considered in revision total knee arthroplasty procedures.
Introduction
The proximal tibiofibular joint (PTFJ) is a frequently overlooked articulation that plays a crucial role in the biomechanics and stability of the knee. Instability of PTFJ although rare, constitutes a significant traumatic knee injury that often goes undiagnosed due to its subtle clinical presentation and low incidence. This condition accounts for less than 1% of all knee injuries, making it an uncommon diagnosis in clinical practice (1). PTFJ instability (PTJI) has been documented in both idiopathic cases—where no obvious trauma is evident—and in individuals who have sustained high-energy trauma, such as knee dislocations or long bone fractures (2). Notably, the incidence of PTJI is higher among athletes participating in pivoting contact sports, due to the increased mechanical stress on the joint (3).
The pathophysiology of PTJI involves disruption or weakening of the stabilizing ligamentous structures of the joint, including the anterior and posterior ligamentous bundles. Among these, the posterior bundle is recognized as the weaker structure, predisposing the joint to anterolateral subluxation of the fibular head, particularly during activities such as deep knee flexion or walking (4). Clinically, this instability manifests as chronic lateral knee pain, neurologic symptoms from irritation of the common peroneal nerve, and functional limitations (5). PTFJ disorders such as osteoarthritis (OA) can also be sources of pain and instability in the knee (6).
Management of PTJI depends on symptom severity and underlying etiology. Conservative treatment, including temporary immobilization, is typically the initial approach. However, in severe or refractory cases, surgical interventions such as internal fixation, arthrodesis, fibular head resection, direct ligament repair, or ligament reconstruction with a free graft may be necessary (7,8).
In the context of total knee arthroplasty (TKA), PTJI is exceedingly rare, with an even lower incidence following revision TKA. To date, only one case of PTJI after TKA has been documented in the literature (9).
We present the case of a 73-year-old patient with anterolateral PTJI that developed after multiple revision TKAs. This case highlights the importance of considering PTJI in the differential diagnosis of patients presenting with chronic lateral knee pain and instability after TKA. Additionally, it underscores a potentially effective approach to diagnosing and managing this rare, yet challenging condition. We present this case in accordance with the CARE reporting checklist (available at https://acr.amegroups.com/article/view/10.21037/acr-25-46/rc).
Case presentation
Anamnesis and clinical presentation
The patient, a 73-year-old female with a history of multiple surgeries on her right knee, initially managed at another clinic, presented to our center, Hôpital Cantonal de Fribourg, seeking a second opinion. She reported increasing knee pain radiating into the leg, following the syndesmosis, particularly exacerbated by activities such as squatting. Clinical examination revealed an anterior subluxation type of PTJI. Additionally, she experienced sharp, electric-like pain during mobilization of the fibular head, further supporting the diagnosis of PTJI.
Her history dates back to 2008, at the age of 60 years, when she presented with persistent medial knee pain following two skiing accidents in 2005 and 2007. Both incidents required arthroscopic intervention for a medial meniscal tear and further evaluation, though no ligamentous injuries were identified. Despite treatment, her symptoms persisted, prompting more investigations.
In 2008, a magnetic resonance imaging (MRI) revealed aseptic necrosis of the medial femoral condyle, with an intact anterior cruciate ligament (ACL). This finding led to the implantation of a unicompartmental knee arthroplasty (UKA) in 2009, initially with good outcomes. However, by 2013, the patient reported worsening knee pain. Radiographs demonstrated loosening of the tibial component of the UKA, leading to the decision to remove the implant and replace it with a TKA. A NexGen TKA with a tibial stem for enhanced stability was implanted in February 2013. Intraoperative cultures were sterile.
In May 2019, the patient returned with recurrent knee pain. A joint aspiration ruled out infection, but radiographs revealed a radiolucent line around the tibial component. Revision surgery was performed, during which a conflict between the tibial implant and the fibular head was noted. To address this, a smaller tibial component was selected, necessitating the replacement of the femoral component to match the tibial implant. A Legacy Constrained Condylar Knee (LCCK) polyethylene insert was used to enhance stability. All microbiological examinations were sterile.
Despite these revisions, the patient continued to report significant knee pain in December 2019. Aspiration was again sterile, leading to the decision to revise the prosthesis. During surgery, the tibial implant was found to be loose and easily removable, with the cement adhering only to the implant and not to the bone. Additionally, a blockage was identified in the tibial medullary canal, which may have interfered with proper seating of the tibial implant. The canal was reamed, the obstruction removed, and a new tibial implant was securely placed. This series of events highlights a complex surgical history with recurrent pain and instability necessitating multiple revisions, summarized in Table 1 and illustrated in Figures 1,2.
Table 1. Surgical history of the patient.
| Date | Event |
|---|---|
| 2009 | Unicompartmental knee arthroplasty |
| 2013 | Total knee arthroplasty |
| 2019 | Revision total knee arthroplasty |
| 2020 | Revision total knee arthroplasty |
| 2023 January | Prosthesis removal and insertion of a spacer |
| 2023 March | Implantation of a hinged total knee arthroplasty + stabilization of the proximal tibiofibular joint using a Twin Tail Tight-Rope™ system |
Figure 1.
X-ray follow-up. (A) Native knee. (B) Unicompartmental knee arthroplasty. (C) Unicompartmental knee arthroplasty with a loose tibia. (D) Conversion to a total knee arthroplasty with a stem.
Figure 2.
X-ray follow-up. (A) Total knee arthroplasty with a loose tibial component. (B) Conversion to a revision prosthesis. (C) Change of the tibial component. (D) Change of the prosthesis with stabilisation of the proximal tibiofibular joint.
The combination of persistent pain, mechanical failure, and the eventual discovery of a clinical PTJI underscores the need for comprehensive evaluation in cases with such extensive revision histories. Radiological investigations, including X-ray imaging and computed tomography (CT) scan, revealed tibial component loosening but no signs of OA in the knee or PTFJ. Additionally, scintigraphy showed hypercaptation in both the tibial component and the PTFJ (Figure 3). With a negative knee puncture, the authors concluded that the patient had aseptic loosening of the prosthesis associated with PTJI. Surgery was then proposed.
Figure 3.
Scintigraphy. (A) Axial, (B) coronal, (C,D) sagittal views of the scintigraphy showing tibia component loosening, and activity around the proximal fibula.
Surgical technique
The authors proceeded with a two-stage revision to exclude a low-grade infection. During the first stage, the prosthesis was removed, and multiple bacteriological biopsies were performed, along with prosthesis sonication, all of which returned negative results. A cemented spacer was implanted, and the patient received co-amoxicillin 1.2 g four times per day until bacteriological results were confirmed as negative 15 days post-surgery. Following confirmation, a revision TKA with PTJI fixation was securely performed.
The patient was placed in a supine position on the operating table. Under general anesthesia, PTJI was confirmed, as the fibular head demonstrated significantly increased anteroposterior mobility compared to the contralateral side. Intravenous cefuroxime 1.5 g was administered for antibiotic prophylaxis. A standard anterior knee approach with a medial parapatellar arthrotomy was performed, utilizing the previous skin incision to minimize additional tissue trauma. The spacer was removed, and samples were taken for microbiological analysis.
Intraoperatively, PTJI was reassessed. Using surgical forceps, we confirmed increased mobility of the fibular head, which was located in the posterolateral aspect of the operative field. It appeared that the level of resection of the proximal tibia was below the stabilizing ligaments, leading to PTJI. A 2-mm tibial cut was performed using an intramedullary guide before stabilization was achieved with a Twin Tail TightRope™ (Arthrex, Inc., Naples, FL, USA) (Figure 4).
Figure 4.
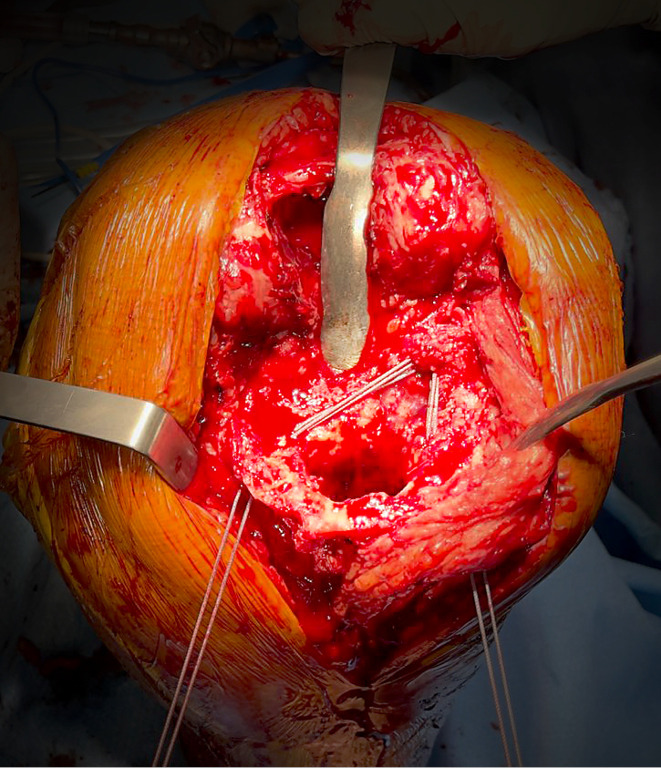
Intra operative image. The tibial cut is too low, resulting in the absence of the proximal tibiofibular ligament. The Twin Tail Tight-Rope™ is passing through the fibula head, with two strands across the tibia, avoiding the medullary canal.
An Arthrex endobutton was used because it preserves joint mobility, facilitates precise reduction, avoids interference with prosthesis stem positioning, and aims to restore functional stability by approximating the orientation of the stabilizing ligaments. A first portal was drilled through the fibular head using a 4-mm bit, taking care to avoid damage to the common peroneal nerve. The trajectory was aimed laterally at the level of the fibular head, ensuring the common peroneal nerve, which moves anteriorly at the level of the fibular neck, was not compromised. Subsequently, two holes were drilled through the tibia, staying peripheral to the medullary canal to avoid obstructing stem placement. The button was passed through the fibular head, with the other two positioned through the tibia, and was then fixed in place (Figure 5). At this stage, the PTFJ was stable, as the fibular head no longer exhibited anteroposterior instability.
Figure 5.

Illustration of the stabilisation system.
We then proceeded with the implantation of a hinged revision knee prosthesis, the Balansys Revision Knee Prosthesis (Mathys Ltd., Bettlach, Switzerland). Femoral cuts were completed, and a tibial component with an offset stem and 8 mm wedges medially and laterally was implanted. The femoral component included a stem and 8 mm distal and posterior external augmentations. After assessing stability, a 12-mm inlay was inserted and fixed with a screw.
Finally, thorough wound irrigation (washout), hemostasis control, and final closure were performed.
Follow-up
Postoperative radiographs were satisfactory (Figure 6). All bacteriological samples, including implant sonication and granuloma biopsy, remained negative after 10 days. The patient experienced an uneventful recovery, with no wound complications and good progression in physiotherapy. She followed a rehabilitation protocol with partial weight-bearing for 6 weeks, after which she was allowed full weight-bearing without restrictions.
Figure 6.
Post-operative X-ray. (A) Anteroposterior at 6 weeks. (B) Lateral at 6 weeks. (C) Anteroposterior at 1 year. (D) Lateral at 1 year.
Follow-up assessments were conducted at 6 weeks, 3 months, and 1 year. At 6 weeks, the patient no longer reported the previous lateral knee pain. Range of motion (ROM) was 100°/5°/0°. The Oxford Knee Score was 30, and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score was 17/96 (17.7%). At the 1-year follow-up, the pain score was 1/10, with a WOMAC score of 15/96 and a ROM of 110°/5°/0°.
Ethical statement
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
PTFJ has been referred to as the fourth compartment of the knee due to its communication with the femorotibial synovial envelope. This communication was observed in at least 10% of adults in a study using magnetic resonance (MR) arthrography, reporting a prevalence of up to 64% (10).
The PTFJ connects the lateral tibial condyle with the fibular head and is encapsulated by a dense fibrous capsule, which is reinforced by two accessory ligaments; the anterior proximal tibiofibular ligament, and the posterior proximal tibiofibular ligament, a single thick band extending from the fibular head to the tibial plateau, covered by the popliteus tendon (4). Specific innervation of the PTFJ is provided by the recurrent fibular branch of the common peroneal nerve and the nerve to the popliteus, which is derived from the tibial nerve (11).
From a biomechanical perspective, the PTFJ plays a critical role in distributing axial and longitudinal loads. The fibula transmits approximately one-sixth of the static load from the ankle to the PTFJ (12). Additionally, the joint functions to relieve torsional stresses at the ankle, control lateral bending moments of the tibia, and sustain tensile rather than compressive forces. Moreover, robotic cadaveric models have shown that TKA balancing alters tibiofibular kinematics, further suggesting its involvement in post-surgical knee stability (13).
Despite its importance, PTJI is often misdiagnosed due to its heterogeneous and nonspecific clinical presentation. Symptoms can include lateral or anterolateral knee pain, neuropathic pain radiating along the peroneal nerve distribution, antalgic gait, difficulty climbing stairs, hamstring discomfort, knee weakness, and a sensation of instability (11). During physical examination, PTJI may be suspected based on when patients present lateral pain on palpation of the fibular head, increased PTFJ mobility—assessed by applying pressure to the fibular head in anterolateral and posteromedial directions with the knee relaxed at 45° flexion—or during ankle dorsiflexion-plantar flexion with the knee flexed (14).
Up to 57% of late or recurrent cases require surgical stabilisation due to chronic instability and ongoing pain (15). Various surgical approaches have been described, including internal fixation, arthrodesis, fibular head resection, direct ligamentous repair, and ligament reconstruction using a free graft (7). However, there is no consensus regarding the optimal treatment approach, as each method presents distinct advantages and potential complications.
PTJI associated with TKA is exceptionally rare, with only one case described in the literature (9). In this case, the patient had undergone TKA following knee OA secondary to a Schatzker type 2 tibial plateau fracture. The authors implanted a tibial component with a stem and a lateral augment, but the patient subsequently developed lateral knee pain and PTJI, leading to surgical arthrodesis, which resulted in a favorable outcome at 43-month follow-up. Additionally, two cases involving concurrent knee and proximal tibiofibular OA have been reported (16,17). Aebischer et al. treated the patient with TKA and PTFJ arthrodesis, while Herndon et al. performed TKA with proximal fibular head resection and peroneal nerve decompression. In these cases, joint stabilization was not recommended due to the presence of OA.
Fibular head resection can reduce instability but may also compromise knee stability by removing key ligamentous attachments, including the lateral collateral ligament (LCL) and the biceps femoris tendon. Conversely, PTFJ arthrodesis provides joint stability but can alter ankle biomechanics, restrict fibular mobility, and introduce hardware-related complications. A systematic review by Kruckeberg et al. (7) reported moderate complication rates for both techniques, with arthrodesis (28%) and fibular head resection (20%) demonstrating similar outcomes. Importantly, given the role of the PTFJ in tibiofibular rotation, excessively rigid stabilization techniques may be less desirable.
The use of Twin Tail Tight-Rope™ or suspension button constructs—commonly utilized for distal tibiofibular syndesmosis injuries—has recently been explored for PTJI stabilization. Multiple case reports and small case series have reported promising results (18-21). A biomechanical study demonstrated that optimal device placement, which should enter from the posterior and superior section of the fibular head and aim transversely and superiorly, significantly improves anterolateral stability and restores fibular internal rotation (22). Another cadaveric study highlighted that while a single device is sufficient for restoring anterolateral stability, two devices are needed to address posteromedial instability (23).
To our knowledge, this is the first report describing PTFJ stabilization in the context of revision TKA. A unique feature of this case was the recurrent tibial component instability, necessitating multiple revisions and the use of a lateral augment. The extensive lateral tibial plateau resection likely resulted in loss of the posterior band of the proximal tibiofibular ligament, contributing to PTJI.
We hypothesize that PTJI may have played a role in tibial component loosening, as its biomechanical alterations could have contributed to recurrent implant failure. The patient had already undergone two previous revisions for tibial component loosening, despite the use of a stemmed implant, and infection had been ruled out through negative bacterial cultures.
A significant aspect of this case was the successful stabilization of the PTFJ using a Twin Tail Tight-Rope™ system. Despite the presence of a tibial stem in the revision prosthesis, we were able to secure the joint while staying peripheral to the stem’s trajectory, thereby avoiding interference with implant fixation. This technique not only addressed joint instability but also enabled anatomical reconstruction of the proximal tibiofibular ligamentous structures, restoring both anterior and posterior ligamentous integrity.
Given the findings of this case, we suggest that PTJI should be routinely assessed in patients undergoing TKA or revision TKA with a lateral tibial augment. If instability is detected, appropriate stabilization should be performed to prevent postoperative complications, including tibial component loosening and persistent lateral knee pain.
Conclusions
PTJI is rare and not typically associated with TKA. This case highlights a unique presentation of PTJI in a multi-revised TKA, suggesting that repeated proximal tibial resections may contribute to ligamentous instability. The specific localization of pain and its resolution following stabilization support this hypothesis. To address this instability, we used an innovative anatomical fixation technique with the Twin Tail Tight Rope™ system, which preserves joint mobility while restoring ligamentous integrity. This approach proved effective in relieving symptoms and ensuring joint stability, highlighting the importance of considering PTFJ involvement in complex TKA revisions.
Supplementary
The article’s supplementary files as
Acknowledgments
A portion of this work was presented as a poster at the Swiss Society of Orthopaedics and Traumatology (Swiss Orthopaedics) annual meeting in June 2023. We would like to express our gratitude to Ms. Julie Matos-Strasser for her valuable assistance in formatting, design, and photo editing, which enhanced the presentation of the figures and the overall graphical quality of the manuscript.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Footnotes
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://acr.amegroups.com/article/view/10.21037/acr-25-46/rc
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://acr.amegroups.com/article/view/10.21037/acr-25-46/coif). The authors have no conflicts of interest to declare.
References
- 1.Nunes J, Direito-Santos B, Costa A, et al. Acute proximal tibiofibular joint dislocation: a sports related injury?—two different cases. Ann Joint 2019;4:11. [Google Scholar]
- 2.Ogden JA. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg Am 1974;56:145-54. [PubMed] [Google Scholar]
- 3.Turco VJ, Spinella AJ. Anterolateral dislocation of the head of the fibula in sports. Am J Sports Med 1985;13:209-15. 10.1177/036354658501300401 [DOI] [PubMed] [Google Scholar]
- 4.Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;(101):186-91. [PubMed] [Google Scholar]
- 5.Dennis JB, Rutledge BA. Bilateral recurrent dislocations of the superior tibiofibular joint with peroneal-nerve palsy. J Bone Joint Surg Am 1958;40-A:1146-8. [PubMed] [Google Scholar]
- 6.Forster BB, Lee JS, Kelly S, et al. Proximal tibiofibular joint: an often-forgotten cause of lateral knee pain. AJR Am J Roentgenol 2007;188:W359-66. 10.2214/AJR.06.0627 [DOI] [PubMed] [Google Scholar]
- 7.Kruckeberg BM, Cinque ME, Moatshe G, et al. Proximal Tibiofibular Joint Instability and Treatment Approaches: A Systematic Review of the Literature. Arthroscopy 2017;33:1743-51. 10.1016/j.arthro.2017.03.027 [DOI] [PubMed] [Google Scholar]
- 8.Thangamani SK, Muthu S, Reddy SP. Biological Stabilization of Proximal Tibiofibular Joint Recurrent Instability with Semitendinosus Graft - Surgical Technique and Case Report. J Orthop Case Rep 2025;15:134-9. 10.13107/jocr.2025.v15.i03.5362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bédard M, Corriveau-Durand S. Instability of the proximal tibiofibular joint associated with total knee arthroplasty. Arthroplast Today 2016;2:93-6. 10.1016/j.artd.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bozkurt M, Yilmaz E, Atlihan D, et al. The proximal tibiofibular joint: an anatomic study. Clin Orthop Relat Res 2003;(406):136-40. 10.1097/01.blo.0000030167.56585.2f [DOI] [PubMed] [Google Scholar]
- 11.Ogden JA. Subluxation of the proximal tibiofibular joint. Clin Orthop Relat Res 1974;(101):192-7. [PubMed] [Google Scholar]
- 12.Lambert KL. The Weight-Bearing Function of the Fibula: a strain gauge study. JBJS 1971;53:507. [PubMed] [Google Scholar]
- 13.Barsoum WK, Lee HH, Murray TG, et al. Robotic testing of proximal tibio-fibular joint kinematics for measuring instability following total knee arthroplasty. J Orthop Res 2011;29:47-52. 10.1002/jor.21207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ozcan O, Boya H, Oztekin HH. Clinical evaluation of the proximal tibiofibular joint in knees with severe tibiofemoral primary osteoarthritis. Knee 2009;16:248-50. 10.1016/j.knee.2008.12.013 [DOI] [PubMed] [Google Scholar]
- 15.Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg 2003;11:120-8. 10.5435/00124635-200303000-00006 [DOI] [PubMed] [Google Scholar]
- 16.Herndon CL, Alonge T, McDermott Nance E, et al. Concurrent Surgical Management of Advanced Osteoarthritis of the Knee and Proximal Tibiofibular Joint With Compressive Peroneal Neuropathy: 3-Year Follow-Up On a Complex Case. Arthroplast Today 2020;6:993-7. 10.1016/j.artd.2020.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aebischer AS, Wing N, Wall CJ. Simultaneous Total Knee Arthroplasty and Proximal Tibiofibular Joint Arthrodesis: A Case Report. JBJS Case Connect 2021;11(2). Available online: https://doi.org/ 10.2106/JBJS.CC.20.00555 [DOI] [PubMed]
- 18.Miettinen H, Kettunen J, Väätäinen U. Dislocation of the proximal tibiofibular joint. Arch Orth Traum Surg 1999;119:358-9. 10.1007/s004020050428 [DOI] [PubMed] [Google Scholar]
- 19.Okoroha KR, Mahan MC, Matar R, et al. Proximal Tibiofibular Dislocation Repaired with Syndesmotic Suture Buttons: A Case Report. J Orthop Case Rep 2018;8:82-5. 10.13107/jocr.2250-0685.1224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srimongkolpitak S, Manop P, Chernchujit B. Suture Repair and Suspensory Button Fixation of Avulsion Fracture of the Fibular Styloid (Arcuate Fracture). Arthrosc Tech 2025;14:103182. 10.1016/j.eats.2024.103182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanakamedala AC, Hinz M, Wang Y, et al. Proximal Tibiofibular Joint Stabilization Using an Adjustable-Length Suspensory Fixation Device. Video J Sports Med 2024;4:26350254241272113. 10.1177/26350254241272113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang S, Habet N, Rice OM, et al. Superiorly and transversely orienting the bicortical suspension device provides optimal anterolateral stability to the proximal tibiofibular joint: a finite-element study. Knee Surg Sports Traumatol Arthrosc 2022;30:3767-75. 10.1007/s00167-022-06991-8 [DOI] [PubMed] [Google Scholar]
- 23.Wang S, Rice OM, Habet NA, et al. Biomechanical Assessment of Bicortical Suspension Device Fixation for Proximal Tibiofibular Joint Instability: Single Versus Double Device. Am J Sports Med 2023;51:3742-8. 10.1177/03635465231203213 [DOI] [PubMed] [Google Scholar]






