Abstract
Introduction
Although exploded hand syndrome is well described in the literature, only a few cases have been reported. A sudden compressive force to the hand leads to extrusion of the intrinsic muscles through burst lacerations in the skin. This case report has been reported in line with the SCARE checklist.
Case report
A 45-year-old male industrial worker sustained a crush injury to his right hand when a compressor plate hit the hand at the factory. Besides extrusion of the intrinsic muscles and multiple metacarpal fractures, two unique features were seen: fractures of the phalangeal necks and hand ischemia. The extruded muscles were excised, and all wounds were closed. Closed reduction (without fixation) was done to all fractures. Immediate mobilization of the fingers was done. A good outcome was obtained with this simple approach.
Discussion
Our case of exploded hand syndrome was unique in both presentation and management.
Conclusion
We demonstrate that a good outcome with closed reduction (without fixation) of fractures is recommended in cases of exploded hand syndrome with concurrent hand ischemia. The rationale behind this approach is the fear of further compromising the blood supply of the hand with open reduction and fixation of the multiple fractures.
Keywords: Hand injury, Fracture, Management
Highlights
-
•
A unique case of exploded hand syndrome is reported.
-
•
There was extrusion of the intrinsic muscles and hand ischemia.
-
•
The multiple fractures were treated conservatively.
-
•
A good outcome was obtained.
1. Introduction
Exploded hand syndrome is well described in the literature [[1], [2], [3]]. A high compressive force excessively flattens the arches of the hand, leading to sudden hydraulic-induced bursting of the skin with extrusion of the intrinsic muscles. Since the thumb is normally at a higher plane than the fingers, extrusion of the thenar muscles and thumb ray fractures are the most common manifestations of the syndrome. Other features of this injury include longitudinal fractures of metacarpals, carpometacarpal fractures of the fingers, and fractures of the carpal bones. Concurrent compartment syndrome and vascular compromise of the hand are not normally seen with this pattern of injury. In this communication, the author reports a unique case of exploded hand syndrome. Besides the classic features of the syndrome, there was concurrent hand ischemia and phalangeal neck fractures of all fingers. Furthermore, management included the reduction of displaced fractures without fixation. The case has been reported in line with SCARE criteria [4].
2. Case report
A 45-year-old male industrial worker sustained a crush injury to his right hand when a compressor plate hit his hand at the factory. Upon arrival to the emergency department, the hand had extrusion of the adductor pollicis muscle through a burst laceration at the first web space and extrusion of the thenar muscles through a burst laceration on the radial border of the hand (Fig. 1). The patient was able to do a flicker of flexion of the fingers. No fine touch sensation was present in any of the digits. Pulse oximetry of the digits showed a value between 85 % and 89 %. Radiological examination showed fractures of the bases of the metacarpals of all fingers, comminuted fractures of the shaft and head of the first metacarpal, and undisplaced fractures of the necks of the proximal phalanges of all fingers (Fig.2-A and B). The patient was given prophylactic Cephalosporin antibiotic, which was continuously for one day after surgery.
Fig. 1.

Appearance at presentation – note the extruded intrinsic muscle.
Fig. 2.

A. X-ray at the time of presentation showing the fractures (see text for details).
B. Close-up x-ray showing the undisplaced phalangeal neck fractures of the fingers.
The patient was taken to the operating room by two consultants (1 Consultant Plastic Surgeon and 1 Consultant Orthopedic Surgeon). After general anesthesia, the hand was examined again, and a decision was made not to do any plastic surgery reconstruction of the crushed blood vessel. Simple skin closure after debridement of extruded muscles and fracture reduction under intraoperative x-ray was done.
A thumb spica splint was applied to immobilize the thumb in the abducted position and the wrist in extension. All finger joints were left free to allow immediate post-operative mobilization. No wire fixation was done to any of the fractures. The blood supply to the digits gradually improved (pulse oximetry was 92–96 % in all digits by one week post injury). However, there was blistering of the skin at the wrist, which healed spontaneously. The splint was removed at three weeks, and physiotherapy was initiated for the wrist and thumb ray after removal of the splint. The patient continued physiotherapy as an outpatient.
At final follow-up eight months after injury, assessment of the hand showed the following: Normal pulse oximetry to all digits (95–99 %), excellent recovery of sensation to all digits (static 2-point discrimination of 3 mm), and recovery of 70 % of the range of motion of the fingers. In the thumb, there were thirty degrees of flexion at the interphalangeal joint of the thumb and a completely stiff metacarpophalangeal joint (Fig. 3A and B).
Fig. 3.
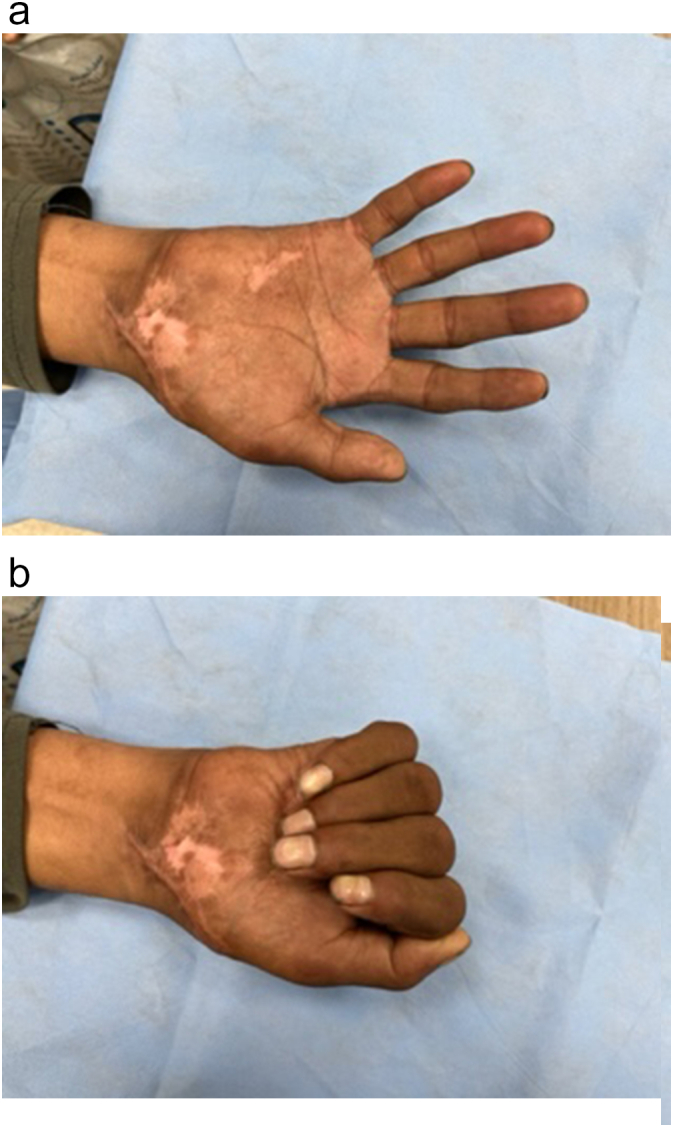
Range of motion at final follow-up.
A. digital extension.
B. digital flexion.
Although there was no clawing of the fingers, intrinsic muscle testing showed limited finger abduction/adduction. The thumb opposition only reached the tip of the middle finger. Hand grip power was 55 % of the contralateral hand.
Radiologically, all fractures healed except for the nonunion of the fracture of the head/neck of the metacarpal of the thumb (Fig.4). However, there was no instability or pain. The patient was able to return to work nine months post-injury. Table 1 is a timeline of the sequence of intervention and follow-up.
Fig. 4.

X-ray at final follow-up.
Table 1.
Timeline of management.
| Day/month after injury | Management |
|---|---|
| Day 1 | Initial Assessment, Antibiotics, Surgery (Debridement of extruded muscles, swim closure, closed reduction of fractures, splint to wrist and thumb ray (finger joints were left free) |
| Day 1–21 | Daily assessment showed gradual improvement in vascularity, antibiotics continued for one day after surgery, and gentle physiotherapy to the finger joints |
| Day 21 | Removal of the splint and physiotherapy to the wrist and the thumb ray was initiated |
| 3 weeks – 8 months | Continuation of Physiotherapy and strengthening exercises |
3. Discussion
Our case of exploded hand syndrome was unique in both presentation and management. Digital ischemia and fractures of the phalangeal necks of the proximal phalanges were unique features, and both were treated conservatively with a good outcome. Fractures of the phalangeal necks were undisplaced, and conservative management of such undisplaced fractures with splints has been recommended [5,6]. No splints were used in the fingers in our case, and gentle range of motion was allowed immediately post-injury.
The vascular compromise of the hand in our case was unique compared to other cases in the literature [[1], [2], [3]]. We believed that this vascular compromise was related to several factors, including the high degree of pressure from the compressive force, and the patient's attempt to simultaneously withdraw his hand, leading to a combined stretching force on the neurovascular bundles.
The other unique feature in our case was the avoidance of fracture fixation. Previous cases in the literature with no vascular compromise underwent fixation, and we fully agree with this approach. The rationale behind avoiding open reduction and internal fixation in our cases was the fear of further compromising the blood supply of the hand.
The conservative management of the metacarpal base and thumb ray fractures (These were treated with closed reduction and cast immobilization for three weeks) resulted in bone union with good alignment.
There was non-union of the head of the metacarpal of the thumb. The non-union of the metacarpal head was not associated with any pain or instability. Hence, no further management was thought to be indicated.
As mentioned in the case report, there were several residual deficits in the hand at final follow-up, such as limited thumb motion and reduced grip strength. These deficits were expected after such a severe injury. The functional implications for the patient's daily activities at work will also be expected. We advise that the patient should go back to work with lighter duties. However, we do not believe that further intervention will be considered in the future.
Further discussion regarding limitations, treatment alternatives, and rehabilitation is mandatory. It should be noted that the most important limitation of our case is that it is a single case report. In our case, other treatment alternatives were exploring the crushed blood vessels and the reconstruction using vein grafts with simultaneous internal fixation of fractures. However, this would mean further incisions in the ischemic and the degloved skin, with the risk of injury to the collateral blood vessels. Our case is a severe crushed injury, and post-traumatic hand edema was seen as expected. The literature recommends bandaging to treat this edema [7]. However, bandaging was also avoided in our case because of the concurrent ischemia. It should also be noted that conservative non-surgical management of isolated hand fractures has become popular in recent literature [8]. Hence, the conservative management of fractures in our case also goes with these reasons and directions. We started gentle mobilization of the metacarpophalangeal joint of the fingers immediately post-operative. Physiotherapy at the wrist and thumb ray at three weeks after surgery.
As mentioned in the introduction, the flattening force in the hand affects the thumb ray more than the fingers because the thumb lies at a higher plane compared to the fingers. This explains that the extruded muscles were the adductor pollicis and the thenar muscles. Furthermore, the most severe fractures were seen in the thumb ray. Finally, the outcome in the thumb ray was worse than the fingers.
4. Conclusion
A unique case of exploded hand syndrome is presented to demonstrate that closed reduction (without fixation) of fractures is recommended in the presence of concurrent hand ischemia and to demonstrate a good outcome with early physiotherapy despite the severe nature of the injury. Both the patient and surgeon were happy with the final outcome.
Consent
Written informed consent was obtained from the patient for publication of data and images.
Ethical approval
The study was approved by the Research Committee of Medical Consultants Clinics approved on April 1, 2025; approval number 16-25.
Funding
None.
Author contribution
The author collected the data and wrote the management.
Guarantor
Dr. Saad Al Mohrij.
Research registration number
Not relevant here.
Conflict of interest statement
None.
References
- 1.Graham T.J. The exploded hand syndrome: logical evaluation and comprehensive treatment of the severely crushed hands. J. Hand Surg. Arm. 2006;31:1012–1023. doi: 10.1016/j.jhsa.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Del Pinal F., Pisan D., Garcia-Bernal F.J., Rguldo J., Pino del F.J., Ayala H. Massive hand crush: the role of a free muscle flap to obliterate the dead space and clear deep infection. J. Hand Surg. Br. 2006;31:588–592. doi: 10.1016/j.jhsb.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Al-Qattan M.M. The exploded hand syndrome: a report of fire industrial injury cases. J. Hand Surg. Eur. 2013;38:880–887. doi: 10.1177/1753193412468577. [DOI] [PubMed] [Google Scholar]
- 4.Kerwan A., Al-Jabir A., Mathew G., Sohrabi C., Rashid R., Franchi T., Nicola M., Agha M., Agha R.A. Revised surgical CAse REport (SCARE) guideline: an update for the age of artificial intelligence. Prem. J. Sci. 2025;10 [Google Scholar]
- 5.Al-Qattan M.M., ALQattan A.M. A review of phalangeal neck fractures in children. Injury. 2015;46:935–944. doi: 10.1016/j.injury.2015.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Al-Qattan M.M. Phalangeal neck fractures in adults. J. Hand Surg. Eur. 2006;31(5):484–488. doi: 10.1016/j.jhsb.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Santandrea S, Benassi M, Tedeschi, R. "Comparison of short-stretch bandage and long-stretch bandage for post-traumatic hand edema" - 10.1016/j.ijscr.2023.108854. [DOI] [PMC free article] [PubMed]
- 8.Boccolari P, Pantaleoni F, Donati D, Tedeschi R. "Non-surgical treatment of oblique diaphyseal fractures of the fourth and fifth metacarpals in a professional athlete: A case report" - 10.1016/j.ijscr.2024.109256. [DOI] [PMC free article] [PubMed]


