Abstract
Introduction and importance:
Fahr’s syndrome is a rare neurodegenerative disorder characterized by bilateral intracranial calcifications, primarily affecting the basal ganglia, thalamus, and cerebellum. It presents with a wide range of neurological and psychiatric symptoms, often mimicking more common conditions.
Case presentation:
We report the case of a 45-year-old South Asian male with no known comorbidities who presented with acute fever, altered consciousness, and generalized tonic-clonic seizures. Initial management targeted a suspected central nervous system infection, but neuroimaging revealed bilateral basal ganglia calcifications.
Clinical discussion:
Extensive metabolic and infectious workups were unremarkable, leading to a diagnosis of Fahr’s syndrome through multidisciplinary evaluation. Genetic testing was not performed due to financial constraints. The patient showed significant improvement with empirical anticonvulsant therapy and supportive care and was advised outpatient follow-up.
Conclusion:
This case emphasizes the importance of considering Fahr’s syndrome in patients presenting with unexplained neurological symptoms, particularly in resource-limited settings where access to genetic testing is restricted. Early recognition through neuroimaging is crucial to avoid misdiagnosis and ensure appropriate management. Increased awareness among clinicians is necessary for timely intervention and improved patient outcomes.
Keywords: calcification, case report, Fahr syndrome, neurodegenerative disease, seizures
HIGHLIGHTS
This case report presents a unique and intriguing case of a 45-year-old man who presented with seizures, altered mental status, and disorientation.
The diagnosis was made after a comprehensive evaluation, including magnetic resonance imaging, magnetic resonance angiography, lumbar puncture, and laboratory investigations, which ruled out other potential causes of his symptoms.
The case report considering rare and unusual diagnoses in patients presenting with seizures and altered mental status, and demonstrates the value of a multidisciplinary approach to diagnosis and management. The patient’s response to treatment and improvement in symptoms are also noteworthy.
Introduction
Fahr’s syndrome, a rare neurodegenerative disorder, is a form of secondary bilateral, symmetrical intracranial calcification. Fahr’s syndrome is thought to be caused by a variety of factors. The most common association of Fahr’s syndrome is endocrine abnormalities[1]. Fahr syndrome differs from Fahr’s disease which is an inherited, mostly as an autosomal dominant trait[2]. It is a male-dominant disease with a ratio of 2:1 and an overall prevalence of less than 1 in 1 000 000[3]. Abnormal deposits of calcium carbonate and phosphate are not confined to the basal ganglia and can also accumulate in other regions such as the thalamus, hippocampus, dentate nucleus, cerebral cortex, and subcortical white matter of the cerebellum[4] therefore contribute to an array of symptoms ranging from movement disorders like chorea, parkinsonism, athetosis, cerebellar symptoms, and speech disorders[5] to neuropsychiatric symptoms like hallucinations, delusions, anxiety and mania[6].
We describe a case of a 45-year-old male who presented with acute fever, altered level of consciousness (ALOC), and seizures, initially diagnosed and treated as a central nervous system (CNS) infection. However, further investigations revealed bilateral calcifications in the caudate and lentiform nuclei on magnetic resonance imaging (MRI) and hyperdensities on bilateral basal ganglia.
The work has been reported in line with the SCARE 2023 criteria[7].
Case presentation
A 45-year-old South Asian man with a 20-pack-year smoking history and no known comorbidities presented to the emergency department with 2–3 episodes of generalized tonic-clonic seizures, ALOC, disorientation, irrelevant speech, and drowsiness.
The patient was vitally stable, and on neurological examination, his Glasgow Coma Scale (GCS) score was 8/15 (E1, M5, V2). The plantar reflexes were down-going bilaterally, and both pupils were reactive to light.
According to his family, the patient had experienced a low-grade fever 4 days prior, which was treated at a local clinic as a viral illness, possibly Chikungunya. The fever resolved completely after treatment. However, after 4 days, he developed multiple seizure episodes for the first time in his life, accompanied by frothing at the mouth, upward eye rolling, and urinary incontinence.
Multiplanar and multi-sequential MRI revealed bilateral symmetrical patchy areas of high T1 signals involving the caudate and lentiform nuclei. A small, inhomogeneous area with predominantly low signal intensity was observed in the right frontal region. These areas demonstrated blooming artifacts on gradient-recalled echo (GRE), indicative of calcification, as shown in Figure 1.
Figure 1.
Axial T1-weighted images (A, B) show symmetrical signal changes in the basal ganglia, particularly in the putamen and caudate nuclei. Coronal T1-weighted images (C, D) further highlight the involvement of the globus pallidus and thalamus. Axial T2-weighted images (E, F) demonstrate hyperintense signals in the putamen, caudate nuclei, and thalamus.
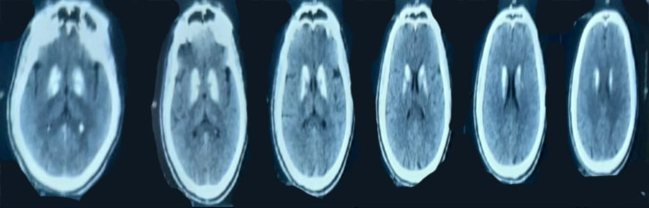
Non-contrast axial computed tomography (CT) brain imaging was also performed, demonstrating bilateral symmetrical hyperdense foci in the region of the basal ganglia. The ventricular system appeared normal in size and configuration, with no evidence of midline shift or hydrocephalus. No acute intracranial hemorrhage, mass effect, or significant parenchymal hypodensity was noted. The cortical sulci and basal cisterns were preserved, as shown in Figure 2.
Figure 2.
Axial non-contrast CT brain showing bilateral basal ganglia hyperdensities.
Magnetic resonance angiography showed moderate segmental narrowing in the anterior circulation and mild segmental narrowing in the posterior circulation, with reduced peripheral cortical branches.
The patient was hospitalized for etiological clarification. MRI ruled out ischemic stroke, lumbar puncture excluded any viral or bacterial infection, and laboratory investigations showed no biochemical abnormality regarding phosphocalcium metabolism, as summarized in Table 1. EEG findings were also normal.
Table 1.
Showing laboratory investigations
| Laboratory investigations | |
| Calcium (8.4–10.2 mg/dL) | 9.11 |
| Phosphate (3.0–4.5 mg/dL) | 3.51 |
| PTH (10–60 pg/mL) | 68 |
| Chloride (95–105 mEq/L) | 100 |
| Sodium (136–146 mEq/L) | 142 |
| Bicarbonate (22–28 mEq/L) | 26 |
| Potassium (3.5–5.0 mEq/L) | 4.4 |
| Magnesium (1.5–2.0 mEq/L) | 2.4 |
| TSH (0.4–4.0 μU/mL) | 0.25 |
| T4 (5.0–12 μg/dL) | 7.35 |
| T3 | 0.65 |
| Urea (7.0–18 mg/dL) | 24 |
| CSF D/R | |
| Sugar (40–70 mg/dL) | 92 |
| Protein (<40 mg/dL) | 37 |
| RBC | 60 |
| WBC (0–5/mm3) | NIL |
Following a multidisciplinary discussion involving the radiology and neurology teams, a diagnosis of Fahr’s disease was confirmed. However, further genetic evaluation was not performed due to financial constraints and the unavailability of gene testing for Fahr syndrome.
Given the preceding febrile illness, the patient was empirically managed with Ceftriaxone 2 g IV BID, Vancomycin 750 mg IV every 6 hours, Levetiracetam 500 mg IV BID, Dexamethasone 4 mg IV TDS, Paracetamol 1 g IV TDS, Omeprazole 40 mg IV OD, and Acyclovir 750 mg IV TDS, along with chest physiotherapy. This regimen improved symptoms, and by the fifth day, the patient became clinically stable with a GCS of 15/15.
The patient was discharged with instructions for outpatient follow-up and was prescribed Brivaracetam 50 mg, Pyridoxine 50 mg, Haloperidol 1.5 mg, and Domperidone 10 mg. He demonstrated a positive response to treatment.
Discussion
Fahr’s syndrome, also known as primary familial brain calcification, is a rare neurodegenerative disorder characterized by bilateral basal ganglia and cortical calcifications. It is typically associated with metabolic disturbances, including parathyroid disorders, but may also present idiopathically[4]. This case highlights an unusual presentation of Fahr’s syndrome in a previously healthy middle-aged man who developed acute neurological symptoms, including altered mental status and seizures, in the absence of known metabolic or genetic predispositions.
Neurologically, Fahr’s syndrome can present with a wide range of symptoms, including movement disorders such as Parkinsonism, chorea, dystonia, myoclonus and cognitive impairment, psychiatric disturbances, and seizures[1]. Our patient’s initial GCS score of 8/15, coupled with seizures and focal neurological deficits, aligns with the known heterogeneity of clinical presentations in Fahr’s syndrome. The acute onset of symptoms in the setting of a recent febrile illness may suggest a possible inflammatory or post-infectious trigger exacerbating an underlying predisposition to basal ganglia dysfunction.
The diagnostic criteria for Fahr’s syndrome include the presence of bilateral basal ganglia calcifications, progressive neurological dysfunction, the exclusion of metabolic causes such as hypoparathyroidism, and the absence of infectious, toxic, or traumatic etiologies[8]. MRI and CT scans are the primary imaging modalities used for diagnosis, with CT being more sensitive in localizing and assessing the extent of cerebral calcification. Laboratory tests, including calcium, phosphate, parathyroid hormone, and genetic testing, are often performed to rule out secondary causes[1].
Our patient’s clinical presentation with disorientation, irrelevant speech, seizures, and asymmetric motor impairment initially raised concerns for multiple differential diagnoses, including CNS infections, autoimmune encephalitis, ischemic stroke, and metabolic encephalopathies. Given his history of a recent febrile illness initially diagnosed as chikungunya, infectious causes were of particular concern. However, extensive workup, including cerebrospinal fluid analysis and MRI, ruled out ischemic or infectious etiologies. MRI findings of bilateral basal ganglia calcifications, vascular narrowing, and normal phosphocalcium metabolism led to the diagnosis of Fahr’s syndrome after a multidisciplinary discussion.
The treatment of Fahr’s syndrome is majorly symptomatic and primarily focuses on symptom relief through pharmacological intervention[9]. Seizures and parkinsonian features are managed with appropriate antiepileptic and antiparkinsonian medications. In patients exhibiting psychiatric symptoms such as psychosis, irritability, or behavioural disturbances, antipsychotic medications may be used cautiously, considering their potential to exacerbate extrapyramidal symptoms[10,11].
The therapeutic approach in this case was primarily initially empirical, including broad-spectrum antibiotics, antiviral therapy, corticosteroids, and antiepileptic medications. The rapid improvement in neurological status following treatment, with the patient regaining full consciousness and functional stability by day five, underscores the importance of early supportive management in such cases. Long-term outpatient therapy was initiated with Brivaracetam, Haloperidol, Pyridoxine, and Domperidone to manage ongoing neurological and psychiatric symptoms.
Several previously published case reports have described similar presentations of Fahr’s syndrome. A case was documented of a 50-year-old patient presenting with new-onset seizures and cognitive decline, who was ultimately diagnosed with Fahr’s syndrome following extensive metabolic and genetic evaluation[12]. Another report highlighted a patient with movement disorders and psychiatric symptoms, underscoring the varied phenotypic spectrum of this condition[13]. These cases, like ours, emphasize the critical role of neuroimaging in diagnosing Fahr’s syndrome, mainly when metabolic abnormalities are absent.
A comparison with these cases suggests that while the majority of Fahr’s syndrome patients exhibit chronic neuropsychiatric symptoms, acute neurological presentations, as observed in our case, may be under-recognized. Additionally, though rarely documented, infectious or inflammatory triggers warrant further investigation. Our case thus contributes to the growing body of literature by reinforcing the need for a high index of suspicion in patients with unexplained basal ganglia calcifications and acute neurological decline.
This case adds to the existing literature on Fahr’s syndrome by demonstrating an acute-onset presentation with seizures and altered mental status in the absence of known metabolic abnormalities. It also highlights the role of advanced neuroimaging in distinguishing Fahr’s syndrome from other neurological disorders with similar presentations. Further research is needed to elucidate potential infectious or inflammatory triggers in the pathogenesis of Fahr’s syndrome and optimize long-term management strategies for affected patients.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Muhammad Nawaz Khan, Email: nawaz.khan67khan@gmail.com.
Iman Muhammad Tahir, Email: iman.tahir40@gmail.com.
Manal Arshad Malik, Email: Manalarshadmalik.99@gmail.com.
Ahsan Ali Jafri, Email: ahsanjaffri222@gmail.com.
Syed Muhammad Sinaan Ali, Email: sinaan.salman@gmail.com.
Md Ariful Haque, Email: arifulhaque58@gmail.com.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from a legally authorized representative(s) for anonymized patient information to be published in this article.
Sources of funding
Authors have not received any funds.
Author contributions
All authors have equally contributed to the manuscript and have approved the final manuscript to be published.
Conflicts of interest disclosure
Not applicable.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Muhammad Nawaz Khan.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data availability statement
Not applicable.
References
- [1].Saleem S, Aslam HM, Anwar M, et al. Fahr’s syndrome: literature review of current evidence. Orphanet J Rare Dis 2013;8:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Perugula ML, Lippmann S. Fahr’s disease or Fahr’s syndrome? ICNS 2016;13:45–46. [PMC free article] [PubMed] [Google Scholar]
- [3].Manyam PB, Bilateral striopallidodentate calcinosis Orphanet: Orphanet; 2010. https://www.orpha.net/en/disease/detail/1980%20[Internet].%20Bilateral%20striopallidodentate%20calcinosis#menu%20
- [4].Amisha F, Munakomi SFS. StatPearls. Treasure Island (FL) Ineligible Companies. StatPearls Publishing; 2023. [Google Scholar]
- [5].Manyam BV, Walters AS, Narla KR. Bilateral striopallidodentate calcinosis: clinical characteristics of patients seen in a registry. J Mov Disord Soc 2001;16:258–64. [DOI] [PubMed] [Google Scholar]
- [6].Trautner RJ, Cummings JL, Read SL, et al. Idiopathic basal ganglia calcification and organic mood disorder. Am J Psychiatry 1988;145:350–53. [DOI] [PubMed] [Google Scholar]
- [7].Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Manyam BV. What is and what is not ‘Fahr’s disease’. Parkinsonism Relat Disord 2005;11:73–80. [DOI] [PubMed] [Google Scholar]
- [9].Ooi HW, Er C, Hussain I, et al. Bilateral Basal Ganglia Calcification: Fahr’s Disease. Cureus 2019;11:e4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Agarwal R, Lahiri D, Biswas A, et al. A rare cause of seizures, parkinsonian, and cerebellar signs: brain calcinosis secondary to thyroidectomy. N Am J Med Sci 2014;6:540–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wazir MH, Ali Y, Mufti AZ, et al. Fahr’s syndrome: a rare case presentation. Cureus 2023;15:e47812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lamessa A, Tesfaye K, Woyimo TG, et al. First-time seizure revealing late-onset Fahr’s disease: a case report and brief literature review. Front Hum Neurosci 2024;18:1456610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Carbone MG, Della Rocca F. Neuropsychiatric manifestations of Fahr’s disease, diagnostic and therapeutic challenge: a case report and a literature review. Clin Neuropsychiatry 2022;19:121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.