Abstract
Oropouche virus (OROV) historically caused a self-limiting disease, yet recent strains are associated with congenital infection and neurodevelopmental disruption. These cases highlight a need to study OROV as a congenital pathogen and determine the impact of infection on neurodevelopment. Here, we show that OROV is vertically transmitted and induces a microcephaly-like phenotype in human forebrain organoids. We found OROV robustly infects human neural progenitor cells in organoids. In contrast to ZIKV, OROV had a heightened capacity for infection and organoid pathology. We show this increased pathogenesis is partially attributable to OROV antagonism of innate immune signaling. We further demonstrate that OROV is vertically transmitted and infects the fetal tissues in a murine model of congenital infection. Our results demonstrate that OROV can be vertically transmitted and has heightened capacity for neurodevelopmental disruption. These findings underscore need for monitoring OROV as a re-emerging virus capable of inducing microcephaly in infected fetuses.
INTRODUCTION
Oropouche virus (OROV) is an understudied, re-emerging virus that historically causes a self-limiting febrile illness in healthy individuals1. Typically transmitted by the Culicoides biting midge, OROV has a tri-segmented RNA genome, and as such, is capable of genetic reassortment2. In fact, novel OROV reassortants have been increasingly associated with recently reported adverse perinatal outcomes3 and disease4,5. As of August 2025, multiple cases of OROV vertical transmission have been confirmed and associated with fetal death and congenital anomalies3,6,7. Observed birth defects involve the fetal central nervous system and include severe microcephaly, cerebellar hypoplasia, ventriculomegaly, and lytic neural necrosis8. Despite detection of OROV RNA and antigen in fetal tissue3, there is no causal link between OROV infection and these pathologies, highlighting a critical need to study OROV as a congenital pathogen and to determine the impact of infection on neurodevelopment.
TORCH pathogens are infectious agents that can be transmitted in utero. Viruses, such as Zika virus (ZIKV), have the capacity to cross the placental barrier and infect the fetal central nervous system9. ZIKV has a tropism for neural progenitor cells in the fetal brain10,11, which are critical for proper neuronal development. As multipotent stem cells, neural progenitor cells give rise to various neuronal and glial lineages in the central nervous system. Virus infection and subsequent virus-induced dysregulation of neural progenitor cells can trigger structural brain defects, and in severe cases cause microcephaly12. To model microcephaly in a relevant human model, multiple groups have used iPSC-derived brain organoids to assess the impact of TORCH pathogens on human neurons11,13–17. Importantly, forebrain organoids mimic the first-trimester fetal brain and contain neurons of varying differentiation states, such as neural progenitor cells. Despite growing concern about OROV-induced fetal microcephaly, the impact of OROV infection on developmental neuronal dysregulation has not been characterized.
To probe the mechanism of OROV-induced microcephaly, we used forebrain organoids as a complex in vitro human model system. We demonstrate that both the historical TR 9760 OROV strain and more recent 240023 OROV strain robustly infect neurons of varying differentiation states in forebrain organoids, including neural progenitor cells. Notably, we demonstrate that OROV infection of early-stage forebrain organoids restricted organoid growth to induce a microcephaly-like phenotype, similar to ZIKV. Yet, distinct from ZIKV, OROV had a heightened capacity for neuroinfection and developmental disruption. We found that neurons were particularly permissive to OROV neuroinfection since OROV replication was not sensitive to IFN signaling in neurons. Lastly, using in vivo murine modeling, we demonstrate the capacity of OROV to cross the maternal-fetal barrier and establish infection in fetal tissues. Cumulatively, these results suggest that OROV is a vertically transmitted pathogen that can induce microcephaly-like phenotype in forebrain organoids. These data align with the rising clinical associations between OROV infection and fetal microcephaly.
RESULTS
OROV infects SOX2+ neural progenitor cells in human forebrain organoids
We first assessed whether OROV could productively infect human forebrain organoids at day-in-vitro 35 (35-DIV), when forebrain organoids are comprised of a mix of neural progenitor cells and more differentiated neurons (Fig. S1A). We used two strains of OROV: a historic strain, TR 9760, isolated in 1955 (OROV-Prototypical, or OROV-P), and a more recent strain, 240023, isolated in 2024 from the serum of an infected Cuban traveler (OROV-Traveler, or OROV-T)18. Both OROV-P and OROV-T strains exhibited robust replication in forebrain organoids and reached peak virus titers by 2-days post-infection (dpi) (Fig. 1A). In contrast, ZIKV exhibited slower viral production and reached peak titers at 4-dpi. Since we did not see an increase in OROV titers past 2-dpi, we sought to clarify if OROV can establish productive infection in forebrain organoids. Thus, we reduced virus inoculum to 50 PFU (Fig. 1D) and observed that OROV-P and OROV-T reached peak virus titers as early as 3-dpi.
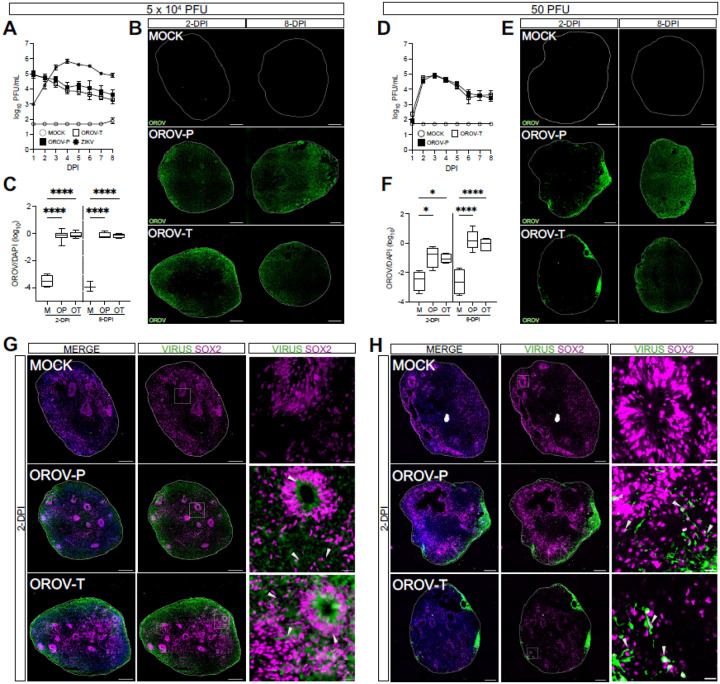
Figure 1. OROV infects SOX2+ neural progenitor cells in human forebrain organoids.
Day-in-vitro (DIV) 35 iPSC-derived human forebrain organoids were mock-infected (MOCK or M) or infected with Zika virus (ZIKV or Z), the historical Oropouche prototypical strain (OROV-P or OP), or a recent traveler isolate of Oropouche (OROV-T or OT) at (A-C) 5×104 or (D-F) 50 plaque forming units (PFU) for 24 hours. (A, D) Plaque assays were performed on culture supernatant through 8-days post infection (dpi) to quantify infectious virus production over time. Data presented as mean ± SEM (n ≥ 4 organoids, N ≥ 3 independent experiments). (B, E) Representative immunofluorescent images of organoids mock-infected or infected with OROV-P or OROV-T at 2- or 8-dpi. Organoid sections were outlined using DAPI (blue) and stained for OROV antigen (green). Scale bars = 200 μm. (C, F) Quantification of OROV+ organoid area relative to DAPI+ area in immunofluorescent images. Data presented as box and whisker plot; whiskers indicate minimum and maximum (n ≥ 3 organoids, N ≥ 2 independent experiments). (G-H) Representative immunofluorescent images of mock-, OROV-P- or OROV-T-infected for 2-dpi at (G) 5×104 PFU or (H) 50 PFU. Sectioned organoids were outlined using DAPI (blue) and stained for OROV or ZIKV antigen (green) and SOX2 (magenta). White box indicates inset. Gray arrows indicate virus-infected SOX2+ cells. Scale bars of whole organoids = 200 μm and inset = 20 μm. (n ≥ 4 organoids, N ≥ 2 independent experiments). Statistical analysis performed with one-way ANOVA followed by Sidak’s multiple comparisons test, * p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Orthogonally, we analyzed OROV-infected forebrain organoids for OROV antigen at 2- and 8-dpi via immunofluorescence. At the higher inoculum concentration, we detected viral antigen at 2-dpi that persisted at 8-dpi (Fig. 1B). At the lower inoculum concentration, we detected viral antigen at the periphery of the organoid as early as 2-dpi that spread by 8-dpi (Fig. 1E, 1F), indicating the virus can efficiently disseminate and infect human forebrain organoids. However, both OROV strains shared similar infection kinetics indicating no significant differences in neuroinfection between the two strains. Collectively, these data demonstrate that OROV, regardless of strain, robustly infects and replicates in complex human forebrain organoids, underscoring its putative role in neuropathogenesis.
Forebrain organoids are comprised of multiple neurons in various stages of differentiation (Fig. S1A-D)19. Thus, we next sought to identify the neuronal subtypes targeted by OROV-P and OROV-T. 35-DIV forebrain organoids were infected with 5 × 104 PFU (Fig. 1G) or 50 PFU (Fig. 1H) of OROV-P or OROV-T and analyzed via immunofluorescence at 2-dpi. Both OROV-P and OROV-T infected SOX2+ and SOX2− neurons, revealing capacity to infect both neural progenitor cells and differentiated neurons. Together, these data establish that OROV can productively infect human forebrain organoids with more robust replication kinetics than Zika virus. Additionally, OROV exhibits a tropism for neural progenitor cells in addition to more differentiated neuronal subtypes.
OROV disrupts forebrain organoid development
As human forebrain organoids develop in vitro, the proportion of neural progenitor cells decrease as differentiated neurons are generated (Fig. 2A). As such, early-stage organoids are comprised of a greater proportion of SOX2+ neural progenitor cells in organized structures called neural rosettes19. Previous studies show ZIKV infection of early-stage organoids markedly impacts organoid structure11,15,16. Thus, to further assess impact of OROV on forebrain organoid structure and growth, we examined how infection influences organoid growth and development at 15-DIV.
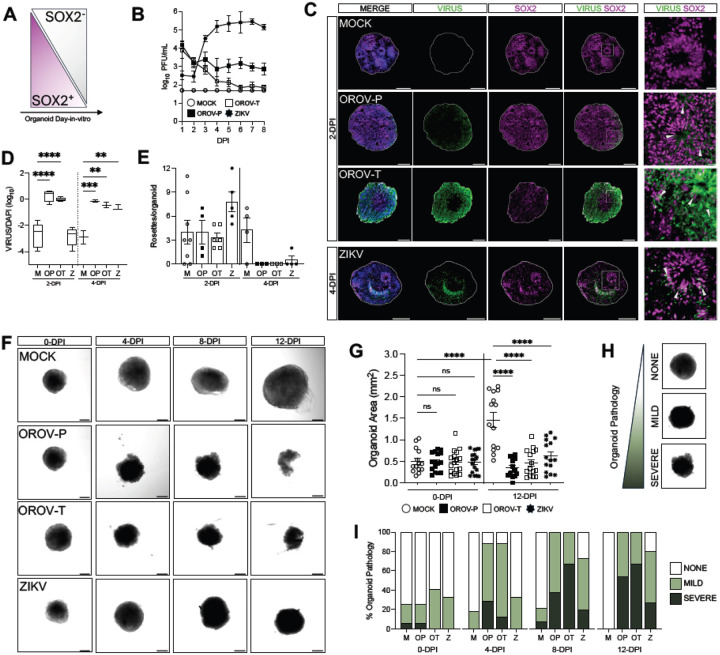
Figure 2. OROV disrupts forebrain organoid development.
(A) Schematic showing the proportion of SOX2+/SOX2-cells in iPSC-derived human forebrain organoid development. (B-I) DIV15 forebrain organoids were mock-infected or infected with 5×104 PFU of OROV-P, OROV-T, or ZIKV for 24 hours. (B) Viral plaque assay was performed on culture supernatant through 8-days post infection (dpi). Data presented as mean ± SEM. (n ≥ 2 organoids, N ≥ 2 independent experiments). (C) Representative immunofluorescent images of organoids mock-infected or infected with OROV-P, OROV-T at 2-dpi, or ZIKV at 4-dpi. Organoid sections were outlined using DAPI (blue) and stained for OROV or ZIKV antigen (green) and SOX2 neural progenitor cell marker (magenta). White box indicates inset. Gray arrows indicate virus-infected SOX2+ neural progenitor cells. Scale bars of whole organoids = 200 μm and inset = 20 μm. (D) Quantification of OROV+ organoid area relative to DAPI+ area in immunofluorescent images of organoids infected for 2- and 4-dpi. Data presented as box and whisker plot; whiskers indicate minimum and maximum (n ≥ 2 organoids, N ≥ 2 independent experiments). (E) Number of neural rosettes per mock- or virus-infected human forebrain organoid were quantified at 2- and 4-dpi. Data presented as means ± SEM (n ≥ 2 organoids, N ≥ 2 independent experiments). (F) Representative confocal images of mock or virus-infected organoids at 0-, 4-, 8-, and 12-dpi (n ≥ 13 organoids, N = 3 independent experiments). (G) Quantification of mock- or virus-infected organoid area at 0- and 12-dpi. (H) Organoid pathology was assessed via confocal microscopy and categorized as no, mild, or severe pathology. (I) Organoid pathology assessment was quantified and percentages plotted as contingency plots. Differences in categorical distribution of organoid pathology were analyzed using the Cochran-Armitage test and P values were adjusted for multiple comparisons using the Bonferroni correction (n ≥ 13 organoids, N = 3 independent experiments). All other statistical analysis were performed with one-way ANOVA followed by Sidak’s multiple comparisons test, ns p ≥ 0.05, * p < 0.05, ***p < 0.001, ****p < 0.0001.
15-DIV organoids were either mock-infected or infected with 5 × 104 PFU of OROV-P, OROV-T or ZIKV and infectious virus production was assessed over time. Similar to 35-DIV organoids, both strain of OROV and ZIKV infect and replicate in 15-DIV forebrain organoids (Fig, 2B). OROV antigen was detected as early as 2-dpi while ZIKV antigen was detected at 4-dpi (Fig. 2C, 2D). We then assessed if virus infection impacted neural rosette formation in organoids. At 2-dpi, virus infections did not impact neural rosette counts in the organoids. However, by 4-dpi, all virus infections significantly reduced the number of neural rosettes (Fig. 2E).
To determine if neural rosette disruption impacted organoid growth, we next evaluated organoid morphology and size over 12 days of infection (Fig. 2F). While mock-infected organoids significantly grew over time (Fig. 2F, 2G), OROV- and ZIKV-infected organoids did not increase in size, with significant growth inhibition at 12-dpi (Fig. 2G). To understand whether OROV caused overt pathology in forebrain organoids, we systematically evaluated organoid pathology over time using three observable categories: ‘none, ‘mild’ and ‘severe’ (Fig. 2H) as determined by organoid integrity, circular structure, and density. At 0-dpi, all organoids displayed similar proportions of pathology, consistent with the mechanical stress of removing forebrain organoids from Matrigel. Both OROV-P and OROV-T significantly induced severe pathology in a greater number of organoids exhibiting as early as 4-dpi compared to mock- and ZIKV-infected organoids (Fig. 2I). This observation held until 12-dpi; a greater proportion of OROV and ZIKV– infected organoids exhibited severe pathology compared to mock-infected organoids. Further, more than half of OROV-infected organoids, regardless of virus strain, exhibited severe pathology, while ZIKV infection induced severe pathology in only 27% of organoids (Fig. 2I). These data indicate both strains of OROV induce neurodevelopmental disruption, organoid growth restriction, and neuropathology more rapidly and severely than ZIKV.
We hypothesized that organoid disruption may be driven by virus-induced cell death. Therefore, we next assessed if virus infection induced cell death in 15- and 35-DIV forebrain organoids by deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) immunofluorescence, (Fig. S2A, S2C). We show that at 4-dpi, both OROV-P and OROV-T infection induces an increase in TUNEL staining. In contrast, TUNEL+ cells remain unchanged with ZIKV infection at 4-dpi (Fig. S2C). In 35-DIV organoids, all viruses induced cell death by 8-dpi (Fig. S2B, S2D). Collectively, these data suggest that virus-induced neuronal death likely contributes to the severity of organoid pathology observed in Fig. 2I.
OROV antagonizes type I interferon signaling
We next sought to explore why forebrain organoids were particularly permissive to OROV-P and OROV-T neuroinfection. We have previously identified neural progenitor cells as important bystander cells that prevent viral replication and spread20. Given the intrinsic antiviral capacity and pronounced OROV tropism for neural progenitors, we investigated whether exogenous induction of type I IFN signaling could suppress OROV infection. Specifically, we pretreated organoids with a representative type I IFN, IFNβ, 6-hours prior to mock-infection or infection with 5×104 PFU of ZIKV, OROV-P or OROV-T. We then stimulated with IFNβ every other day while harvesting organoid supernatant daily until 8-dpi. We found that IFNβ treatment significantly inhibited ZIKV virus production at multiple timepoints, indicating that ISGs induced by IFNβ restrict ZIKV replication in forebrain organoids (Fig. 3A). However, IFNβ treatment did not impact OROV-P or OROV-T virus production at any of the timepoints studied (Fig. 3B). This finding was consistent when organoids were infected with 50 PFU of OROV (Fig. 3C). Collectively, our findings reveal that OROV infection is not limited by type I IFN signaling in organoids.
Figure 3. OROV antagonizes type I interferon signaling.
(A-C) DIV35 forebrain organoids were pretreated with IFNβ or vehicle prior to infection with (A) 5×104 PFU of ZIKV (B) 5×104 PFU or (C) 50 PFU of either OROV-P or OROV-T for 24 hours. Plaque assays were performed on culture supernatant through 8-dpi. Additional IFNβ or vehicle treatments were given at 2-, 4-, and 6-dpi. Data presented as mean ± SEM. (n ≥ 2 organoids, N ≥ 2 independent experiments). (D-E) DIV35 organoids were mock-infected (M) or infected with 5×104 PFU of OROV-P (OP), OROV-T (OT), or ZIKV (Z). Organoid RNA was harvested at 2- and 8-dpi and RT-qPCR was performed for (D) IFNβ and (E) IFIT1. (F) Representative immunofluorescent images of DIV35 forebrain organoids mock-infected, or infected with 5×104 PFU of OROV-P, OROV-T or ZIKV for 24-hours prior to stimulation with IFNβ or vehicle for 24-hours. Organoid sections were outlined using DAPI (blue) and stained for IFIT1 protein (gray), SOX2 neural progenitor cell marker (magenta), and OROV or ZIKV antigen (green). White box indicates inset. Orange arrows indicate virus-infected IFIT1+ cells. Yellow arrows indicate virus-infected IFIT- cells. Gray arrows indicate IFIT+ uninfected cells. Scale bars of whole organoids = 200 μm and inset = 20 μm. (G) Quantification of IFIT1+ area relative to DAPI+ area in immunofluorescent images of organoids in (F). Data presented as box and whisker plot; whiskers indicate minimum and maximum. (n ≥ 7 organoids, N = 2 independent experiments). (H) Quantification of IFIT1+ area that was either OROV negative or OROV positive of organoids in (F). Statistical analysis for (A-C) were performed with ordinary two-way ANOVA followed by Sidak’s multiple comparisons test. All other analyses were performed with one-way ANOVA followed by Sidak’s multiple comparisons test, ns p > 0.05, * p < 0.05, **p < 0.01, ****p < 0.0001.
Similar to other bunyaviruses, OROV has a nonstructural protein that antagonizes type I IFN signaling in host cells21. We therefore next sought to understand if OROV infection antagonizes ISG production in forebrain organoids. We mock-infected or infected 35-DIV forebrain organoids with 5×104 PFU of OROV-P, OROV-T or ZIKV for 2- or 8-days. We found that infection with either OROV-P or OROV-T did not impact IFNβ transcripts at 2-dpi, but significantly increased IFNβ transcripts at 8-dpi (Fig. 3D). This was in contrast with ZIKV-infected organoids, which did not increase IFNβ transcripts at either time point. We next analyzed the impact of OROV infection on the downstream ISG, IFN-induced protein with tetratricopeptide repeats 1 (IFIT1) to determine if upregulation of IFNβ impact downstream ISG induction. Notably, we show that only OROV-P infection downregulates IFIT1 expression at 8-dpi (Fig. 3E).
To directly investigate OROV-induced type I IFN antagonism in neurons, we next assessed the ability of OROV infected neurons to induce IFN signaling. To do this, we mock-infected or infected forebrain organoids with OROV-P, OROV-T or ZIKV at 5×104 PFU for 24-hours followed by stimulation with exogenous IFNβ for 24-hours. We then determined the expression of IFIT1 protein in actively infected neurons versus bystander non-infected neurons via immunofluorescence. If OROV actively antagonizes IFN signaling, we would expect restricted IFIT1 protein expression in infected cells, while uninfected bystander cells would retain IFIT1 expression. Exogenous IFNβ induced IFIT1 protein expression in SOX2+ neural progenitor cells of mock-infected and infected organoids (Fig. 3F, 3G). But importantly, OROV-infected neural progenitor cells largely did not express IFIT1 24-hours after IFNβ-stimulation (Fig. 3F, 3G). In fact, approximately 82% of the IFIT1+ regions of infected organoids were OROV- (Fig. 3H).
However, bystander non-infected neural progenitor cells expressed the IFIT1 protein, suggesting active OROV infection limits IFIT1 protein induction. Given the short period of infection, ZIKV antigen was mostly undetected, limiting the comparison of infected versus bystander cells. Altogether, these data suggest OROV neuroinfection is particularly permissible as OROV replication is not sensitive to the repertoire of ISGs induced by neurons and actively antagonizes type I IFN signaling in infected neurons.
OROV is vertically transmitted to the developing fetus
The clinical manifestations of OROV infection in fetuses from infected pregnant women, coupled with our work establishing the ability of OROV to induce neurodevelopment disruption in forebrain organoids led us to explore the potential of OROV vertical transmission and fetal infection in vivo. We, and others, did not detect robust OROV dissemination in pregnant C57BL/6 (WT) dams22. Therefore, to promote viral dissemination in a pregnant dam, we transiently depleted type I IFN signaling using an IFNAR1-blocking antibody (αIFNAR1) one day prior to infection to acutely permit productive OROV replication and viral dissemination. Specifically, we treated 9–12-week-old pregnant females with 0.5 mg αIFNAR1 or isotype-control antibody 24-hours prior to a footpad infection of 104 PFU/mouse of OROV-P at embryonic day 6.5 (E6.5). We then monitored mice for 7 days (Fig. 4A) and harvested maternal peripheral tissue (spleen, liver, heart, serum), maternal reproductive tissue (vagina, uterus), and fetal tissue (placenta, fetal heads) on E13.5. Notably, we detected increased OROV RNA in all maternal peripheral and reproductive tissues (Fig. 4B) of αIFNAR1-treated compared to isotype-treated C57BL/6 dams. Interestingly, we noted a difference in fetal pathology in αIFNAR1-treated compared to isotype-treated dams (Fig. 4C), where we observed a slight increase in fetal resorption rate (Fig. 4D) and a significant reduction in fetal body area (Fig. 4E). We detected OROV RNA in the placenta and fetal heads of αIFNAR1-treated dams, this is in stark contrast with isotype control (Fig. 4F). Notably, we found resorbed fetuses (demarked by open diamonds) to have higher viral loads than all intact fetal heads (Fig. 4F). Lastly, we detected infectious virus by plaque assay in a subset of placental samples from αIFNAR1-treated dams, whereas no placentas from control dams contained infectious OROV (Fig. 4G). Notably, the placentas with infectious OROV detectable by plaque assay contained the greatest amount of OROV RNA by RT-qPCR (Figure S3A), suggesting that the amount of OROV RNA found in fetal tissues at this infection timepoint may not have yet reached a threshold for infectious virus to be detected via plaque assay. Altogether, our data indicate that transient blockade of type I IFN signaling permits vertical transmission of OROV resulting in fetal tissue infection and fetal growth restriction.
Figure 4. OROV is vertically transmitted to the developing fetus.
(A) Schematic of experimental design. 9–12-week-old female pregnant C57BL/6 mice (dams) were treated with either 0.5mg/mouse of αIFNAR1 (MAR1–5A3) or isotype control (mouse IgG1) intraperitoneally on embryonic day 5.5 (E5.5). On E6.5, dams were infected with 104 PFU of OROV-P (strain TR9760) subcutaneously via footpad injection. (B-G) All maternal and fetal tissues were analyzed at 7dpi (E13.5). (B) Peripheral maternal tissue (spleen, liver, heart, serum) along with female reproductive tissue (vagina, uterus) were harvested and OROV RNA in peripheral and reproductive maternal tissues quantified via RT-qPCR (n=3 dams per condition, N=3 independent experiments). (C) Representative images of matched fetuses and placentas from isotype-and αIFNAR1-treated dams. (D) Quantification of resorbed and intact fetal tissue (E) Quantification of fetal body area. (F) OROV RNA in placenta and fetal heads were quantified via RT-qPCR. Open symbols denote fetal resorptions. (G) Viral titers in placenta and fetal heads were quantified via plaque assay. Dashed line indicates limit of detection for each assay (n>14 samples per condition, N=3 independent experiments). Statistical analysis for (F) was performed with an unpaired t-test. All other analyses were performed with two-way ANOVA adjusted for multiple comparisons, ns p > 0.05, * p < 0.05, ***p < 0.001, ****p < 0.0001.
DISCUSSION
Historically, human OROV infection has led to self-limiting febrile illness1. However, the 2022–2024 OROV outbreak has been increasingly associated with adverse neurotropic complications in adults4,5, vertical transmission, and fetal abnormalities8. These growing clinical associations signal the possible emergence of a new TORCH pathogen. We designed this study to investigate OROV infection-induced neurodevelopmental disruption and putative congenital infection capacity. We demonstrate that OROV robustly infects neural progenitor cells and more differentiated neurons in iPSC-derived forebrain organoids, a human model of early fetal brain development. We find that OROV infection in early-stage forebrain organoids induces severe pathology and microcephaly-like phenotype, as defined by reduced organoid size and ablation of neural rosette formation. Notably, OROV had a heightened capacity for neuroinfection, and developmental disruption as compared to the neurotropic, TORCH pathogen, ZIKV. OROV infection also antagonized type I IFN signaling early in neuroinfection which may contribute to this increased pathogenesis. Lastly, by establishing a new in vivo model of robust congenital infection, we show that OROV can cross the maternal-fetal barrier to establish infection in both the placenta and fetus. Further, our in vivo model associates murine OROV congenital infection with fetal growth restriction.
The recent OROV outbreak is speculated to be caused by a novel viral reassortment event leading to increased clinical cases7. Previous work using an Ifnar1−/− mouse model22 found novel strains of OROV to be more permissive and virulent. Yet, our data suggest the historic OROV-P and novel OROV-T infection of forebrain organoids do not exhibit strong differences in virus replication and virus-induced pathology. These conflicting data could be due to differences of OROV replication dynamics in mouse versus human model systems, or distinctions in the host immune capacity of infection model. Further work is needed to assess how strain differences are linked to increased incidence of OROV fetal neuroinfection. Interestingly, OROV-T was found to better replicate in midges, the primary OROV vector, as compared to a historic OROV strain23. It is also therefore plausible that novel OROV strains may cause increased human disease indirectly through increased vector infectivity.
Regardless of strain, we observed that OROV infection is heightened compared to ZIKV infection in forebrain organoids. We show both OROV strains efficiently infect neural progenitor cells and other neurons in the forebrain organoid. In contrast, ZIKV infection was largely restricted to neural progenitor cells and exhibited slower viral replication kinetics. We also show that type I IFN signaling limits ZIKV infection, but not OROV infection in the forebrain organoid model. Enhanced antagonism of type I IFN signaling by OROV may explain its widespread neurotropism compared to ZIKV. Additionally, OROV entry into neurons exploits the entry factor Lrp124, a mechanism absent in ZIKV infection. This may explain the expanded tropism of OROV for both SOX2+ and SOX2− cells in the organoid model. This difference in neurotropism, early infection immune antagonism, and differences in viral entry may explain why OROV infection leads to increased neuron death and organoid pathology.
Additionally, we developed a congenital murine model of OROV infection. In immunocompetent mice, we show that type I IFN signaling is important in controlling viral dissemination, since transient depletion of type I IFN signaling in pregnant dams allowed for vertical transmission and fetal infection. These data indicate that in mice, IFNAR signaling is important for virus dissemination to fetal tissues. Of note, OROV neuroinfection in our organoid model was not impacted by active type I IFN signaling. This suggests that type I IFN signaling is important for neuroinvasion, but not infection. This is likely due to the differential antiviral capacities, or repertoire of ISGs induced by different cell types (i.e. monocytes versus neurons). Alternatively, this could be due to species differences in antiviral dynamics between mouse and human, which is known to occur with ZIKV infection25,26. However, further experiments are needed to explore this difference.
Cumulatively, our work is the first to define OROV as a TORCH pathogen capable of neurodevelopmental disruption by targeting neural progenitor cells and suppressing innate antiviral responses. We further show that a novel strain reassortment did not impact direct neuroinfection. These data align with the rising clinical associations between OROV infection and fetal microcephaly. The work presented here underscores the significance of monitoring OROV as a re-emerging virus capable of in utero transmission.
METHODS
Viruses and cells
OROV-P, TR-9760, was purchased from ATCC (VR-266), while OROV-T, strain 240023, was obtained from BEI resources, NIAID, NIH, (NR-59930). OROV stocks were propagated in Vero cells. African green monkey kidney (Vero) (ATCC, Cat#CCL-81) cells were grown and maintained in Dulbecco’s modification of eagle’s medium (Corning, Cat#10–013-CV) supplemented with 10% fetal bovine serum (Sigma-Aldrich, Cat#F2442) and 1% penicillin–streptomycin (ThermoFisher Scientific, Cat#15140122). ZIKV Cambodian FSS13025 strain (ZIKV-CAM) was obtained from the World Reference Center for Emerging Viruses and Arboviruses at University of Texas Medical Branch, Galveston. ZIKV-CAM stocks were propagated in C6/36 mosquito (Aedes albopictus) cells. C6/36 cells (ATCC, CRL-1660) were maintained in Dulbecco’s Modified Eagle’s Medium (ThermoFisher, 11965092) supplemented with 10% heat-inactivated fetal bovine serum (FBS) (ThermoFisher, A5670701), 1% penicillin/streptomycin (ThermoFisher, 15140122) and 1% tryptose phosphate broth (Sigma-Aldrich, T8159) at 30°C. For high-titer doses, ZIKV and OROV were concentrated by ultrafiltration (Centricon Plus-70; MWCO: 30,000). Human-induced pluripotent stem cell line C1–227 was maintained in mTSeR media (StemCell Technologies, Cat#100–1130) prior to forebrain organoid generation. Cell lines were authenticated by morphology and were routinely tested for mycoplasma contamination.
Mice
C57BL/6 (wild-type; WT) mice were purchased from The Jackson Laboratory (strain #000664) and maintained at the University of Pennsylvania under specific pathogen-free conditions. Timed matings were performed by mating >8-week old female WT mice to male WT mice overnight. Subsequently male and female mice were separated the following morning after checking for the presence or absence of a copulation plug, with plug observation date designated E0.5. Female mice with a copulation plug were used for congenital OROV infection experiments. All experiments were performed following IACUC guidelines.
In vivo OROV Infections
9–12-week old pregnant female C57BL/6 WT mice were treated intraperitoneally with 0.5mg/mouse of either an αIFNAR1-blocking antibody (clone MAR1–5A3; BioXCell Cat#BE0241) or an IgG1 isotype-control antibody (BioXCell Cat#BE0083) on E5.5. αIFNAR1-pregnant female WT mice were then infected subcutaneously via footpad with 104 PFU of OROV-P (strain TR9760) on E6.5. Mice were monitored daily for weight changes and sacrificed 7 dpi, on E13.5. Tissues were isolated, placenta and fetuses were photographed on measurement paper using an iPhone camera, and all tissues were collected into tubes containing 1mL of DMEM 2%FBS, 1% penicillin/streptomycin, 1% HEPES + silica beads, homogenized, and analyzed for subsequently for viral loads.
Generation of forebrain organoids
Forebrain organoids were generated using a previously described protocol19,20. In short, iPSCs were maintained and incubated at 5% CO2, 37 °C. iPSCs exhibiting signs of differentiation were excluded from organoid generation. At 0-DIV, iPSCs were seeded in low-attachment 96-well plates (Corning, Cat#3474) at a density of 100,000 cells/well in mTeSR1 supplemented with 10 μM of ROCK inhibitor (StemCell Technologies, Cat#72304). At 2-DIV, embryoid bodies (EB) were transferred using cut 200uL pipette tips into 6-well plates in DMEM:F12 media (Gibco, Cat#11320033), supplemented with 20% Knockout Serum Replacement (Gibco, Cat#10828028), 1X GlutaMAX, 1X MEM Non-essential Amino Acids (Gibco, Cat#11140–050), 1X EmbryoMax 2-Mercaptoethanol (Sigma-Aldrich, Cat#ES-007-E), 1X Penicillin/Streptomycin, 1uM LDN193189 (StemCell Technologies, Cat#72147), 1 mM SB-431542 (StemCell Technologies, Cat#72234) and 2 μg/mL 0.2% heparin solution (StemCell Technologies, Cat#7980). Media changes were performed daily. At 6-DIV, EB media was replaced with induction media consisting of DMEM:F12, 1X N-2 Supplement (ThermoFisher Scientific, Cat#17502048), 1X Penicillin/Streptomycin, 1X NEAA, 1X GlutaMAX, 1 μM CHIR99021 (StemCell Technologies, Cat#72054), and 1 μM SB-431542. Round EBs with bright edges were selected at 7-DIV, coated with Matrigel, and plated on ultra-low-attachment 6-well plates (Corning, Cat#3471). Media was changed every other day until 14-DIV when EB-Matrigel complexes were disassociated. EBs, now organoids, were maintained until either 15-DIV or 35-DIV with daily media changes consisting of 1:1 Neurobasal media and DMEM/F12 supplemented with 1X N-2, 1X B-27, 1X GlutaMAX, 1X MEM Non-essential Amino Acids, 1X EmbryoMax 2-Mercaptoethanol, 1X Penicillin/Streptomycin and 2.5 μg/mL of insulin (Sigma-Aldrich, Cat#I9278). All EBs and organoids were maintained at 5% CO2, 37 °C and incubated on a shaking platform at 120 revolutions per minute, except when EBs were complexed with Matrigel.
In vitro forebrain organoid virus infections
Forebrain organoids (15-DIV or 35-DIV) were placed in 24-well tissue culture treated plates with two organoids per well. Culture media was completely removed and replaced with fresh culture media containing 5×104 or 50 plaque forming units (PFU) of virus as indicated. Organoids were infected for 24-hours at 37°C with complete media changes daily until samples were harvested. For cumulative virus quantification, organoid media remained unchanged.
Interferon treatments
35-DIV forebrain organoids were pretreated 100 IU/mL of recombinant human IFNβ (PeproTech, Cat#300–02BC) for 6-hours prior to virus infection. After 24h of infection, virus containing media was removed and replaced with fresh media. Media was then supplemented with 100 IU/mL recombinant IFNβ at 2-, 4-, and 6-days post-infection.
RNA extraction, cDNA generation and quantitative RT-PCR
Forebrain organoids were homogenized in TRIzol ((Invitrogen, Cat#15,596,018) and RNA was subsequently extracted using Clean and Concentrator kit (Zymo, Cat#R1017) as per the manufacturer’s instructions. RNA concentration was quantified using the ThermoFisher Scientific Nanodrop One spectrophotometer. cDNA was generated using 200 ng of RNA in iScript cDNA synthesis kit (Bio-Rad, Cat#1708890) following manufacturer’s instructions. Quantitative RT-PCR was performed with Power SYBR Green Master Mix (ThermoFisher Scientific, Cat#4367659). Reactions were run via QuantStudio3 (50 °C: 2’; 95 °C: 10’; 40 × 95 °C: 15 s, 60 °C: 1’) with the addition of a final melt curve (95 °C: 15 s; 60 °C: 1’; 95 °C: 1’). All samples were loaded in technical duplicates. Average threshold cycle (Ct) value was calculated per sample for IFNβ ((F: 5′-CTTTGCTATTTTCAGACAAGATTCA-3′, R: 5′-GCCAGGAGGTTCTCAACAAT-3′) or IFIT1 (F: 5′-TACAGCAACCATGAGTACAA-3′, R: 5′- TCAGGTGTTTCACATAGGC-3′), which was normalized against expression of housekeeping gene, HPRT (F: 5′-CATTATGCTGAGGATTTGGAAAGG-3′, R: 5′-CTTGAGCACACAGAGGGCTACA-3′), and presented as fold change.
To quantify OROV RNA in infected mouse tissues, 200μL of tissue homogenate or serum was added to 600μL of TRIzol, frozen at −80, and RNA was subsequently extracted using Phasemaker (Invitrogen; #A33251) tubes according to manufacturer’s protocol. Total RNA was then quantified as above, and cDNA was generated as above using 1μg total RNA per reaction. OROV cDNA was quantified by as above by RT-qPCR using previously published primers targeting the S segment of OROV (F: 5′- GCGTCACCATCATTCCAAGTA-3′, R: 5′-CCCAGATGCGATCACCAATTA-3′)28. Ct values were fitted to a standard curve generated from a known concentration (PFU/mL) of stock OROV-P to determine the PFU equivalents/mL of a given sample. Samples were then normalized to respective starting mass (g) or volume (mL) and reported as PFU equivalents/g or mL.
Plaque assay
Vero cells were seeded at a density of 5×105 cells/well in a 6-well plate overnight. After 24-hours, supernatants were harvested from infected forebrain organoids and serially diluted in DMEM (Corning, Cat#10–013-CV) supplemented with 10% heat-inactivated Fetal Bovine Serum (Sigma-Aldrich, Cat#F2442) and 1% Penicillin/Streptomycin (ThermoFisher Scientific, Cat#15140122). Seeded Vero cells were treated with 200μL of diluted supernatants and incubated for 1-hour, with rotations every 15 minutes. Following incubation, inoculum was aspirated and replaced with MEM (Sigma-Aldrich, Cat#11430030) supplemented with 5% FBS, 1% GlutaMAX, 1% Non-essential amino acids, and 0.65% agarose (Lonza, Cat#50111). OROV- and ZIKV-infected cells were fixed at 4- and 7-DPI respectively with 2 mL 10% NBF (ThermoFisher Scientific, Cat#22050105) and visualized using 0.1% crystal violet (ThermoFisher Scientific, Cat#C581–25). Plaques were manually counted, and virus titer was calculated.
Immunofluorescence
Human forebrain organoids were incubated in 4% Paraformaldehyde solution (Thermofisher, Cat# J19943.K2) for 30 min at room temperature, while rocking, followed by overnight incubation in 30% sucrose. Fixed organoids were embedded in OCT (Sakura, Cat#4583) and cryosectioned (10 μm) using a Leica Cryostat. Slides were washed three times with PBS prior to membrane disruption with PBST (PBS supplemented with 0.4% Triton X (Sigma-Aldrich, Cat#T8787)). Sample was blocked with PBS supplemented with 1% bovine serum albumin (Sigma-Aldrich, Cat#B2518) and 2% normal donkey serum (Jackson, Cat#017-000-121) for 1-hour prior to overnight incubation with a combination of 1:200 mouse anti-OROV immune ascitic fluid (ATCC, Cat#VR-1228AF) 1:100 mouse Anti-Flavivirus Group Antigen Antibody (Millipore, Cat#MAB10216-I-25UG), or 1:100 rabbit anti-IFIT1 (CST, Cat#14769) diluted in blocking buffer. Samples were washed three times for 10 min with PBST. After washing, samples were incubated for 2-hours in a combination of 1:1000 goat anti-mouse Cy7 (Thermofisher, Cat#A-21037), 1:1000 goat anti-rabbit Cy7 (Thermofisher, Cat#A21039), 1:1000 rabbit monoclonal anti-SOX2 (CST, Cat#5067) and 1xDAPI (ThermoFisher Scientific, Cat#AC202710100) diluted in PBST. Following incubation, sections were washed with PBST and ultrapure water. Sections covered with mounting media and a coverslip was applied and sealed. Images of organoids were acquired using a Nikon Ti2E scope. Image processing was conducted using ImageJ software.
Organoid Size Quantification, Pathology Scoring, and Rosette Counting
Organoids were imaged using a 10X or 4X brightfield microscope depending on organoid size. All organoids were outlined and organoid area measured using ImageJ. Using a single-blinded process, healthy organoids with no pathology were characterized by clearly defined edges with no blebbing or hypodensities. Organoids with mild pathology were classified by the presence of blebbing, a lack of hypodense areas, and generally rounded organoid structure. Organoids with severe pathology were categorized by the presence of blebbing, marked hypodense areas, disruption of round structure and organoid disintegration. Lastly, organoid neural rosettes as demarcated by well-organized SOX2+ neural progenitor cells were quantified in a separate single-blinded study.
Fetal size quantification
Fetus size from αIFNAR1-treated and isotype-control-treated WT dams were quantified using photos of respective litters and converting pixels to millimeters (mm). Fetal crown-rump length, the direct length from the edge of the fetal head to the start of the tail, was multiplied by occipital diameter, the direct length from the front to the back of the fetal head, to quantify overall fetal size. All analysis was performed using ImageJ software.
Data analysis
All graphs were plotted, and statistical analyses were performed using GraphPad Prism. Data are expressed as Mean ± error of the mean (SEM) or as box and whisker plot; whiskers indicate minimum and maximum. Number of biological samples used per experiment (n), number of individual experiments (N), and statistical tests used for each experiment are included in figure legends. Statistical significance was determined by Unpaired Student’s t tests for group means, One-Way or Two-Way ANOVA followed by post-hoc multiple comparisons test as indicated. Differences in categorical distribution of organoid pathology were analyzed using the Cochran-Armitage test and P values were adjusted for multiple comparisons using the Bonferroni correction. p < 0.05 was considered as significant. ns = non-significant, *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001.
Supplementary Files
This is a list of supplementary files associated with this preprint. Click to download.
ACKNOWLEDGMENTS
We thank Dr. Christine Vazquez and Dr. Seble Negatu for assistance in editing this manuscript. This work was in part supported by the National Institutes of Health (1R01AI180138-01 to KAJ), the University of Pennsylvania Office of the President (KAJ) and Breyer Virology Fund.
Footnotes
COMPETING INTEREST DECLARATION
The authors declare no competing interests.
All data generated during this study are included in this published article and its Supplemental Information files. Microscopy data reported in this paper will be shared by the lead contact upon request. Further correspondence and requests for resources and reagents should be directed to and will be fulfilled by the lead contact, Kellie A. Jurado (kellie.jurado@pennmedicine.upenn.edu).
Contributor Information
Kellie Jurado, University of Pennsylvania.
Carl Bannerman, University of Pennsylvania.
Drake Philip, University of Pennsylvania.
Taylor Miller-Ensminger, University of Pennsylvania.
Elizabeth Kennedy, University of Pennsylvania.
Stephanie Liu, University of Pennsylvania.
Kristen Walsh, University of Pennsylvania.
Guo-li Ming, University of Pennsylvania.
References
- 1.Sakkas H., Bozidis P., Franks A. & Papadopoulou C. Oropouche Fever: A Review. Viruses 10, 175 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elliott R. M. Orthobunyaviruses: recent genetic and structural insights. Nat. Rev. Microbiol. 12, 673–685 (2014). [DOI] [PubMed] [Google Scholar]
- 3.Medeiros de D. B.A. et al. Case Series of Adverse Pregnancy Outcomes Associated with Oropouche Virus Infection. Viruses 17, 816 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gatti F. D. et al. Neuroinvasive Oropouche virus in a patient with HIV from extra-Amazonian Brazil. Lancet Infect. Dis. (2025) doi: 10.1016/s1473-3099(25)00352-4. [DOI] [Google Scholar]
- 5.Ewing C. B., Siraj D. & Lepak A. First Case of Neuroinvasive Oropouche Virus in Wisconsin: A Case Report. Open Forum Infect. Dis. ofaf402 (2025) doi: 10.1093/ofid/ofaf402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martins das F. E. N. et al. Newborns with microcephaly in Brazil and potential vertical transmission of Oropouche virus: a case series. Lancet Infect. Dis. 25, 155–165 (2025). [DOI] [PubMed] [Google Scholar]
- 7.Schwartz D. A. Novel Reassortants of Oropouche Virus (OROV) Are Causing Maternal–Fetal Infection During Pregnancy, Stillbirth, Congenital Microcephaly and Malformation Syndromes. Genes 16, 87 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ribeiro de B. F. R. et al. Congenital Oropouche in Humans: Clinical Characterization of a Possible New Teratogenic Syndrome. Viruses 17, 397 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coyne C. B. & Lazear H. M. Zika virus — reigniting the TORCH. Nat. Rev. Microbiol. 14, 707–715 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Tang H. et al. Zika Virus Infects Human Cortical Neural Progenitors and Attenuates Their Growth. Cell Stem Cell 18, 587–590 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dang J. et al. Zika Virus Depletes Neural Progenitors in Human Cerebral Organoids through Activation of the Innate Immune Receptor TLR3. Cell Stem Cell 19, 258–265 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li C. et al. Zika Virus Disrupts Neural Progenitor Development and Leads to Microcephaly in Mice. Cell Stem Cell 19, 120–126 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Harding A. T. et al. Oxidative Stress and Interferon Signaling Drive Differential Pathogenesis of Ancestral and Contemporary Zika Viruses in Human Cerebral Organoids. bioRxiv 2025.08.12.669648 (2025) doi: 10.1101/2025.08.12.669648. [DOI] [Google Scholar]
- 14.Cugola F. R. et al. The Brazilian Zika virus strain causes birth defects in experimental models. Nature 534, 267–271 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcez P. P. et al. Zika virus impairs growth in human neurospheres and brain organoids. Science 352, 816–818 (2016). [DOI] [PubMed] [Google Scholar]
- 16.Krenn V. et al. Organoid modeling of Zika and herpes simplex virus 1 infections reveals virusspecific responses leading to microcephaly. Cell Stem Cell 28, 1362–1379.e7 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xu Y.-P. et al. Zika virus infection induces RNAi-mediated antiviral immunity in human neural progenitors and brain organoids. Cell Res. 29, 265–273 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mancon A. et al. Oropouche fever diagnosed in Milan, Italy in returning travellers from Rio de Janeiro, March 2024, and Cuba, July 2024. J. Travel Med. 31, taae115 (2024). [DOI] [PubMed] [Google Scholar]
- 19.Vazquez C. et al. Antiviral immunity within neural stem cells distinguishes Enterovirus-D68 strain differences in forebrain organoids. J. Neuroinflammation 21, 288 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Negatu S. G. et al. Bystander neuronal progenitors in forebrain organoids promote protective antiviral responses. J. neuroinflammation 22, 65 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tilston-Lunel N. L., Acrani G. O., Randall R. E. & Elliott R. M. Generation of Recombinant Oropouche Viruses Lacking the Nonstructural Protein NSm or NSs. J. Virol. 90, 2616–2627 (2016). [Google Scholar]
- 22.Gunter K. B. et al. From prototype to outbreak: conserved pathogenesis of Oropouche virus in a novel murine pregnancy model highlights its public health implications. bioRxiv 2025.08.02.668287 (2025) doi: 10.1101/2025.08.02.668287. [DOI] [Google Scholar]
- 23.Scroggs S. L. P. et al. Enhanced infection and transmission of the 2022–2024 Oropouche virus strain in the North American biting midge Culicoides sonorensis. Sci. Rep. 15, 27368 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwarz M. M. et al. Oropouche orthobunyavirus infection is mediated by the cellular host factor Lrp1. Proc. Natl. Acad. Sci. United States Am. 119, e2204706119 (2022). [Google Scholar]
- 25.Gorman M. J. et al. An Immunocompetent Mouse Model of Zika Virus Infection. Cell Host Microbe 23, 672–685.e6 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant A. et al. Zika Virus Targets Human STAT2 to Inhibit Type I Interferon Signaling. Cell Host Microbe 19, 882–890 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiang C.-H. et al. Integration-free induced pluripotent stem cells derived from schizophrenia patients with a DISC1 mutation. Mol. Psychiatry 16, 358–360 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gunter K. et al. A reporter Oropouche virus expressing ZsGreen from the M segment enables pathogenesis studies in mice. J. Virol. 98, e00893–24 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]