A genomic investigation of 3,600 small cell lung cancer (SCLC) tumors reveals novel rare cohorts with potential therapeutic importance, biopsy site–specific heterogeneity, and new insights into SCLC histologic transformation.
Abstract
Small cell lung cancer (SCLC) is a recalcitrant neuroendocrine carcinoma with dismal survival outcomes. A major barrier in the field has been the relative paucity of human tumors studied. Here we provide an integrated analysis of 3,600 “real-world” SCLC cases. This large cohort allowed us to identify new recurrent alterations and genetic subtypes, including STK11-mutant tumors (1.7%) and TP53/RB1 wild-type tumors (5.5%), as well as rare cases that were human papillomavirus–positive. In our cohort, gene amplifications on 4q12 are associated with increased overall survival, whereas CCNE1 amplification is associated with decreased overall survival. We also identify more frequent alterations in the PTEN pathway in brain metastases. Finally, profiling cases of SCLC containing oncogenic drivers typically associated with NSCLC demonstrates that SCLC transformation may occur across multiple distinct molecular cohorts of NSCLC. These novel and unsuspected genetic features of SCLC may help personalize treatment approaches for this fatal form of cancer.
Significance:
Minimal changes in therapy and survival outcomes have occurred in SCLC for the past four decades. The identification of new genetic subtypes and novel recurrent mutations as well as an improved understanding of the mechanisms of transformation to SCLC from NSCLC may guide the development of personalized therapies for subsets of patients with SCLC.
This article is highlighted in the In This Issue feature, p. 1501
INTRODUCTION
Small cell lung cancer (SCLC) is the most fatal type of lung cancer, with a 5-year overall survival (OS) of ∼6%. It is estimated that SCLC kills 200,000 to 250,000 patients every year worldwide. Tobacco exposure has been linked to SCLC pathogenesis. SCLC tumors are characterized by fast growth and rapid metastatic spread to multiple sites, as well as a striking resistance to a variety of therapies (1). Patients with SCLC have not yet benefited from advances in targeted therapies, and improvements from addition of immune-checkpoint inhibitor (ICI) therapy have been modest (2, 3). This is in stark contrast with non–small cell lung cancer (NSCLC), in which ICI therapy and targeted therapies have revolutionized the treatment of molecularly defined tumor subtypes, resulting in striking increases in patient survival (4).
A major barrier toward advancing treatment paradigms for patients with SCLC has been the limited availability of tumor samples for detailed molecular characterization. In part, this is because surgical resection is uncommon, thereby limiting access to samples for analysis (5, 6). Available tumor biopsies are often small and necrotic, and rebiopsy at the time of disease progression is not standard of care. The largest published study thus far included genome sequencing of 110 SCLC genomes from resected tumors (7). Combining this study and other smaller studies with more limited genomic analyses (e.g., whole-exome sequencing and targeted sequencing, such as in refs. 8–14), it may be possible to get an estimate of genetic alterations in a few hundred patients at best. In addition, the disparate platforms used in these different studies make it difficult to analyze the data as a group. Moreover, there is a bias toward early-stage tumors in many of these studies. This limits our understanding of the genetic underpinning of tumor progression and metastatic spread, even though the vast majority of patients die with metastatic disease (15). One exciting new opportunity arose in the past few years with the realization that patients with SCLC often have a high number of circulating tumor cells (CTC; ref. 16). It is likely that longitudinal genomic analyses of SCLC CTCs will be informative regarding the mechanisms of SCLC progression, metastasis, and resistance to treatment (17–19). However, these studies have so far been limited to a small number of patients at large medical centers capable of serially collecting and purifying CTCs. Furthermore, there is still the possibility that CTCs do not exactly reflect the biology and the genetics of primary tumors and metastases. Overall, our understanding of recurrent genetic alterations, their co-occurrence and mutual exclusivity, and how the genetic landscape of SCLC changes with tumor progression and resistance to treatment remains limited.
Performing repeat biopsies to study molecular mechanisms of acquired resistance to tyrosine kinase inhibitors (TKI) in EGFR-mutant NSCLC has been a cornerstone for the development of next-generation treatment strategies. Analysis of repeat biopsies has elucidated that histologic transformation to SCLC is detected in ∼3% to 14% of patients with acquired resistance to EGFR TKI therapy (20–24). These cases likely represent subclonal evolution from the original EGFR-mutant clonal population and not second primary cancers, as they typically maintain the original EGFR mutation (24, 25). Histologic transformation to SCLC has been repeatedly observed across multiple cohorts after the emergence of resistance to first-, second-, and third-generation EGFR TKIs. These lung adenocarcinomas show loss of RB1 as they transition to the SCLC phenotype (23, 26), and evidence from a few cases suggests that mutation signatures and copy-number variations may also change during this transition (27). Other data suggest that SCLC transformation from lung adenocarcinoma is driven mainly by transcriptional reprogramming rather than by genetic events (28). Still, despite the clinical importance of SCLC transformation from NSCLC, our understanding of this transformation process and its genetic basis remains incomplete.
To address some of the limitations of previous studies, we evaluated a large cohort of real-world SCLC cases. This cohort of 3,600 cases is more than 30 times larger than the largest published study (7) and allowed us to identify new genetic subgroups in SCLC, site-specific mutational patterns, and insights into histologic transformation from NSCLC. The new insights gained from this integrated analysis open new avenues of research in the field and readily suggest new therapeutic opportunities for subsets of patients with SCLC.
RESULTS
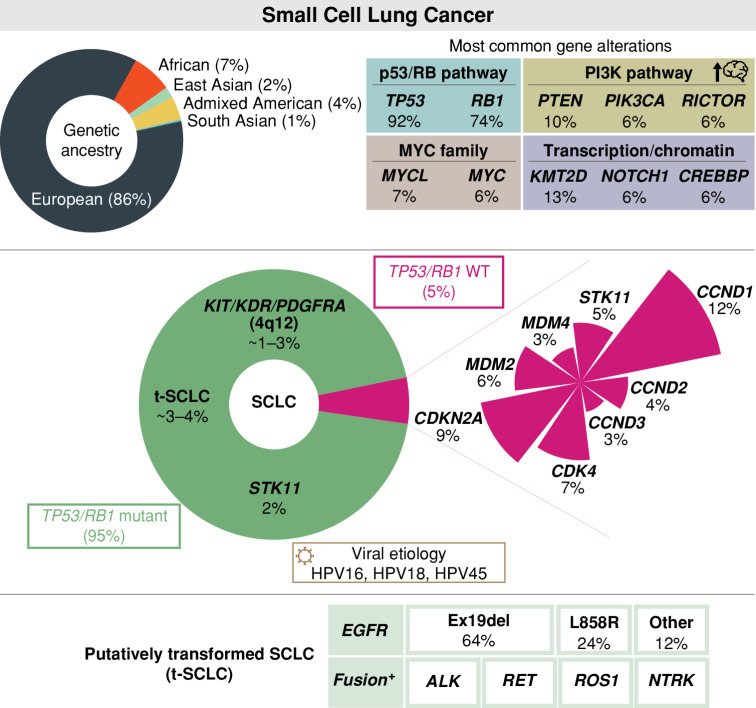
Clinical Characteristics of a Large Cohort of Real-World Patients with SCLC
The cohort consisted of 3,600 patients with tumor tissue biopsies submitted to Foundation Medicine, Inc. with a diagnosis of SCLC for genomic profiling (Fig. 1A and Table 1A). Of these patients, 52.1% were female and 47.9% were male, with a median age of 65 years (range, 21–89 years). A total of 3,114 patients (86.5%) were predicted to have a European ancestry (EUR), with the remaining patients classified into the following ancestry groups: African (AFR; n = 256, 7.1%), Admixed American (AMR; n = 150, 4.2%), East Asian (EAS; n = 69, 1.9%), and South Asian (SAS; n = 11, 0.3%). Tumor samples were most frequently profiled from the lung (37.8%) but also comprised other sites such as regional/distant lymph nodes (n = 901, 25.0%), liver (n = 747, 20.8%), brain (n = 116, 3.2%), and soft tissue (n = 114, 3.2%). As expected from previous analyses (7), most cases (99.5%) were microsatellite stable. Tumor mutational burden (TMB) varied across cases [range, 0–276.3 mutations/megabase (mut/Mb)], with a median of 7.8 mut/Mb and a mean of 9.5 mut/Mb; 38.9% of cases had a TMB-high status (TMB ≥10 mut/Mb). TMB was similar across patients from diverse genetic ancestries (Supplementary Fig. S1).
Figure 1.
The genomic landscape of SCLC tumors in a real-world cohort of patients with SCLC. A, Schematic representation of the overall study design in the SCLC cohort comprising 3,600 patients, including 678 cases for which clinical data are available. B, Patterns of the 20 most frequent gene alterations identified in SCLC tumors. Genes are indicated on the left and their alteration frequency on the right. Predicted genomic ancestry, TMB, and microsatellite instability (MSI) status for each patient are overlaid on top. Each sample is color coded based on the type of gene alteration detected. Short variants, such as nonsense, frameshift, and splice alterations, as well as specific rearrangements that result in truncation of the gene product are grouped together as “truncation.” indel, insertions or deletions; MSI-H, high microsatellite instability; MSS, microsatellite stable. C, Prevalence of chromosomal copy-number loss (blue) and gain (red) in SCLC tumors. Notable genes are indicated for some chromosome arms. D, Association between OS and genetic alterations (for genes altered in ≥5 cases) in the clinical cohort of evaluable stage III/IV SCLC (N = 511). Genes identified to be associated with increased survival are shown in green and those identified to be associated with decreased survival are shown in orange (P ≤ 0.05). KDR, PDGFRA, and KIT are all located on 4q12. After FDR-based adjustment, only WHSC1L1 was statistically significant (adjusted P = 0.001). HR, hazard ratio.
Table 1.
Clinicopathologic characteristics of the real-world SCLC cohort. Clinicopathologic characteristics of 3,600 patients (overall cohort; A) as well as 678 patients with clinical information (clinical cohort; B). The clinical cohort had a large, but not complete, overlap with the overall cohort
| A Overall cohort (N = 3,600) | ||
|---|---|---|
| Age range (median), years | 21–89 (65) | |
| Sex | Male | 1,712 (47.9) |
| Female | 1,864 (52.1) | |
| Unknown | 24 | |
| Predicted genomic ancestry | EUR | 3,114 (86.5) |
| AFR | 256 (7.1) | |
| AMR | 150 (4.2) | |
| EAS | 69 (1.9) | |
| SAS | 11 (0.3) | |
| Site | Lung | 1,362 (37.8) |
| Lymph node | 901 (25.0) | |
| Liver | 747 (20.8) | |
| Brain | 116 (3.2) | |
| Soft tissue | 114 (3.2) | |
| Abdomen/pelvis | 84 (2.3) | |
| Adrenal gland | 74 (2.1) | |
| Bone | 73 (2.0) | |
| Upper airways | 51 (1.4) | |
| Skin and chest wall | 36 (1.0) | |
| Breast | 21 (0.6) | |
| Other/unknown | 21 (0.6) | |
| Microsatellite instability | MSS | 3,448 (99.5) |
| MSI-H | 12 (0.3) | |
| Intermediate | 7 (0.2) | |
| Unknown | 133 | |
| TMB range (median), mut/Mb | 0–276.3 (7.8) | |
| TMB status | TMB-high (≥ 10) | 1,399 (38.9) |
| TMB-low (< 10) | 2,201 (61.1) | |
| B Clinical cohort (N = 678) | ||
| Age at diagnosis range (median), years | 20–85 (66) | |
| Sex | Male | 329 (48.5) |
| Female | 349 (51.5) | |
| Predicted genomic ancestry | EUR | 605 (89.2) |
| AFR | 40 (5.9) | |
| AMR | 19 (2.8) | |
| EAS/SASa | 14 (2.1) | |
| TMB range (median), mut/Mb | 0–84 (8) | |
| Smoking status | Ever-smoker | 654 (96.5) |
| Never-smoker | 24 (3.5) | |
| Stage at initial diagnosis | I | 12 (1.8) |
| II | 8 (1.2) | |
| III | 106 (15.6) | |
| IV | 454 (67.0) | |
| Unknown | 98 (14.4) | |
| Median OS (available for N = 607) | 8.0 months (95% CI, 7.3–9.0 months) | |
| Practice type | Community | 619 (91.3) |
| Academic | 59 (8.7) | |
| Lines of therapy range (median) (available for N = 605) | 1–8 (2) | |
NOTE: Data are presented as N (%) unless stated otherwise.
Abbreviations: CI, confidence interval; MSI-H, high microsatellite instability; MSS, microsatellite stable.
aReported together to maintain confidentiality due to the low number of samples.
Of the 3,600 patients, 678 patients had additional clinical data derived from electronic health records (EHR) as part of the Clinico-Genomic Database (CGDB; Table 1B). Characteristics of the CGDB cohort were analogous to the overall dataset, with a median age of 66 years (range, 20–85 years), a similar distribution based on sex (51.5% female, 48.5% male), predominantly EUR ancestry (89.2%), and similar TMB distributions (median: 8 mut/Mb, range, 0–84 mut/Mb). This subcohort also contained additional clinicopathologic and treatment data. Most patients had a smoking history (96.5%) and exhibited advanced-stage disease at the time of initial diagnosis. As expected, 91.3% of patients in CGDB were treated in a community setting compared with 8.7% treated in an academic setting. Median OS (mOS) for the cohort was 8.0 months [95% confidence interval (CI), 7.3–9.0 months]. Patients received a median of two lines of therapy (range, 1–8) prior to tumor genomic profiling. Only 60 patients received a tumor genomic profiling test result from Foundation Medicine, Inc. before they started first line of treatment, whereas 545 patients received their tumor testing after they started first-line treatment. This is not unexpected because tumor genomic profiling is not currently part of the standard of care for patients with SCLC and is not required to make treatment decisions. In the first line, 86.2% of patients received platinum-based doublet chemotherapy and 23.3% of patients received a PD-L1 inhibitor (Supplementary Table S1). In the second line and beyond, patients were treated with multiple different chemotherapies and ICIs, with no one therapy representing a majority, reflecting the clinical uncertainty of how to treat relapsed SCLC.
Utilizing this large dataset, we sought to perform an integrative analysis of SCLC tumors to gain a better understanding of the genetic underpinning of SCLC progression and metastasis.
Overview of Recurrent Genomic Alterations in 3,600 Cases of SCLC
Deep sequencing of exons from up to 324 cancer-related genes and select introns from up to 34 genes frequently rearranged in cancer (Supplementary Table S2) revealed a number of recurrent alterations. As expected, alterations resulting in the inactivation of the TP53 and RB1 genes were the most frequent and observed in 91.6% and 73.5% cases, respectively (Fig. 1B; Supplementary Table S3). The frequency of TP53 mutations is similar to that observed in other SCLC datasets, whereas previous studies reported a slightly higher prevalence of biallelic RB1 loss (see below; refs. 7, 13, 29). In TP53-mutant samples, inactivation was observed mostly through short variants, comprising base substitutions and insertions or deletions (indel; 98%) whereas RB1-mutant cases included high rates of short variants (85%) and focal copy-number loss (14%; Supplementary Table S3). The base substitutions were similar to what has been observed in NSCLC, in which carcinogens from cigarette smoke are also frequent drivers of cancer initiation (Supplementary Fig. S2A and S2B; ref. 30).
Our analysis also confirmed the previously described recurrent loss-of-function alterations in KMT2D (MLL2; 12.9%), CREBBP (6.1%), and NOTCH1 (5.9%), as well as gain-of-function events and copy-number amplifications in MYC (6.0%), MYCL (7.2%), and SOX2 (3.4%; refs. 7–9; Fig. 1B and C; Supplementary Table S3). Compared with previous smaller-scale studies, we noted an increased representation of alterations in PI3K pathway genes (e.g., PTEN 9.9%, PIK3CA 5.6%, and RICTOR 5.6%) and the RAS/MAPK pathway genes (e.g., EGFR 3.4%, KRAS 3.3.%, and NF1 3.3%; see below; Fig. 1B and C; Supplementary Table S3). We observed similar trends through analysis of cell-free DNA obtained from peripheral blood liquid biopsies from 81 patients with SCLC (Supplementary Fig. S3A and Supplementary Table S4), which is abundant in SCLC compared with NSCLC and other tumor types (Supplementary Fig. S3B; ref. 31).
At the chromosomal level, loss of chromosome arms 3p and 17p was the most common (77.6% and 64.5%, respectively) in SCLC tumors, whereas chromosome arm–level gains were frequently observed in 5p and 3q (64.0% and 55.0%, respectively), among other regions (Fig. 1C; Supplementary Table S5). Overall, chromosome arm losses were more frequent than gains in SCLC tumors, and these losses were significantly enriched in regions with a high tumor suppressor gene score (ref. 32; Fig. 1C; Supplementary Fig. S4A and S4B; Supplementary Table S5), providing additional evidence that SCLC is in large part driven by the loss of tumor suppressors.
Novel Recurrent Gene Mutations in SCLC
Through our analysis of such a large dataset, we were able to identify genes for which mutations have not been previously associated with SCLC (Supplementary Table S3). For example, whereas alterations in KEAP1 have mostly been associated with NSCLC (30, 33, 34), ∼3% of SCLC samples had mutations in this gene, suggesting that inactivation of KEAP1 may contribute to SCLC pathogenesis. Mutations in TET2, which contribute to the development of hematologic malignancies (35), are also found in ∼2% of SCLC cases, indicating again a possible tumor suppressor role in SCLC. Of note, loss-of-function alterations in TET2 detected in this cohort were predominantly nonsense and frameshift alterations (84.0%; Supplementary Table S6), suggesting likely pathogenic potential (36); albeit rare, TET2 alterations were detected in prior SCLC studies as well (7, 37). Histologic evaluation confirmed a diagnosis of SCLC (Supplementary Fig. S5 and Supplementary Table S7). Recently, pathogenic mutations in SMARCA4 have been correlated with the expression of YAP1 in SCLC tumors (bioRxiv 2022.10.09.511505). In our cohort, SMARCA4-inactivating alterations were detected in 54 cases (1.5%). Although these cases were predominantly TP53/RB1 altered (Supplementary Fig. S6A), they exhibited a higher prevalence of CDKN2A alterations compared with samples lacking SMARCA4 alterations (Supplementary Fig. S6B; Supplementary Table S8). As a final example, recurrent amplification events for ZNF703 (2.9%) support that the transcriptional regulator coded by the gene has oncogenic potential in SCLC, possibly because ZNF703 can control the expression of SOX2 (38), a known oncogene in SCLC (ref. 9; Fig. 1B; Supplementary Table S3).
Recurrent Gene Rearrangements in SCLC
We identified frequent gene rearrangements in 338 tumors, including in RB1 (n = 31), NOTCH1 (n = 11), CREBBP (n = 10), KMT2D (n = 9), and TP53 (n = 8), suggesting that these events contributed to inactivation of these tumor suppressors (Supplementary Fig. S7A). This analysis also identified several rearrangements not previously described in SCLC, including events involving ETV6 (n = 15). Based on the oncogenic role of rearrangements involving the transcription factor coded by this gene in leukemia and solid tumors (39, 40), these observations suggest that ETV6 rearrangements could also contribute to SCLC development. Intriguingly, tumors with gene rearrangements showed enrichment for other specific genetic alterations, including mutations in MCL1, which codes for an antiapoptotic factor, as well as in SMARCA4 and DNMT3A, which code for epigenetic modulators (Supplementary Fig. S7B and Supplementary Table S9). A recent study by Ciampricotti and colleagues showed the oncogenic potential of RLF–MYCL fusions in SCLC (41). Although the assay utilized for the current study does not target RLF, we identified 15 instances of MYCL rearrangements with breakpoints predominantly in exon 2 or intron 1, as shown in the Ciampricotti study. Given this limited information, MYCL rearrangements are currently annotated as variants of unknown significance in the Foundation Medicine, Inc. database; however, they may represent potentially oncogenic events that warrant further investigation.
Gene Amplifications on 4q12 Are Associated with Increased OS in Patients with SCLC
The availability of a large group of patients with both genetic characterization and clinical data provided us with a unique ability to determine if any of the recurrently detected genomic alterations were associated with mOS. For the entire clinical cohort with survival information (n = 607), the mOS from the date of initial diagnosis was 8.0 months (95% CI, 7.2–9.0 months) across patients of different genetic ancestry (Supplementary Fig. S8A) and varied by stage of initial diagnosis (Supplementary Fig. S8B).
We focused our analysis on patients with advanced disease (stage III/IV SCLC, N = 511). We identified recurrent gene amplification events at 4q12 associated with increased survival (Fig. 1D and Supplementary Table S10). This region contains three genes coding for receptor tyrosine kinases (RTK): KDR (coding for VEGFR2), PDGFRA, and KIT. Alterations in these genes were associated with improved OS, with a mOS of 67.9 months (KDR and PDGFRA) and 24.0 months (KIT; Supplementary Table S10). c-KIT has been investigated unsuccessfully as a possible drug target in SCLC (42) based in part on evidence that high levels of c-KIT can be associated with worse OS (43, 44). However, other studies suggest that low protein expression of c-KIT can be correlated with worse survival (45). No study has examined coexpression of the three RTKs, and it is possible that too much RTK signaling upon genomic amplification might slow the expansion of SCLC tumors. Of note, amplifications on 4q12 were observed in 1.1% of the overall SCLC cohort. We also identified genes whose recurrent inactivation is associated with worse survival, including mutations in APC, which codes for a Wnt pathway regulator and whose loss has been associated with relapsed SCLC (12), as well as a new association between amplification of the CCNE1 gene, which codes for the cell-cycle regulator Cyclin E1, and worse survival in patients with SCLC (Fig. 1D; Supplementary Table S10). Together, these analyses identify new candidate factors that may play a role in the development and progression of SCLC.
Mutation Spectrum by Different Sites of Metastasis
Clinical prognostic factors for patients with SCLC include the stage and extent of the disease (Table 1). Overall, the number of organ sites involved is inversely related to prognosis, with certain metastatic sites—such as the central nervous system, liver, and bone marrow—conferring poorer prognosis (14, 46, 47). However, the genetic underpinning of SCLC metastasis is largely unknown (15). We examined if tumors at different sites had distinct patterns of genetic alterations, focusing on major sites of metastasis and grouping rarer sites by general area in the body (Table 1).
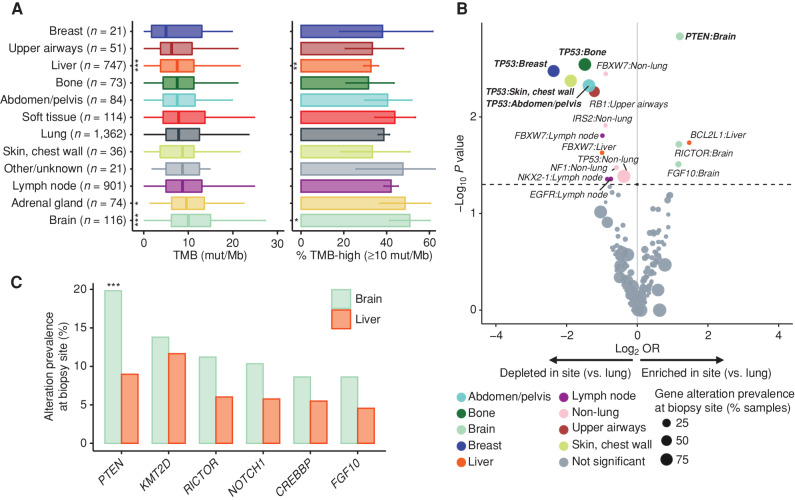
When we first examined the tumor site and TMB, we made the unexpected observation that brain metastases had the highest TMB (median TMB 10.0 mut/Mb), with adrenal gland metastases (median TMB 9.6 mut/Mb) also having a significantly higher TMB compared with lung tumors (median TMB 7.8 mut/Mb; Fig. 2A). Of note, brain metastases also had a higher prevalence of TMB-high samples, defined at a threshold of 10 mut/Mb (50.9% vs. 38.7%, P = 0.01; Supplementary Table S11). Although the underlying tumor purity may contribute to some of the observed differences, we generally observed a high median tumor purity across all the sites (Supplementary Fig. S9A, Supplementary Table S12) and did not observe any strong associations with tumor purity that may explain these TMB differences (Supplementary Fig. S9B, Supplementary Table S12). Brain and liver metastases also showed a significant increase in chromosomal arm–level gains compared with lung-biopsied tumors (Supplementary Fig. S10A and Supplementary Table S13), further suggesting unique genetic mechanisms. We and others have identified Nfib amplification in metastatic mouse SCLC tumors (48–50). Although NFIB expression is high in a large fraction of SCLC metastasis (49, 51), the NFIB gene is rarely amplified in human SCLC tumors (7), even though this amplification may be selected in human SCLC cell lines (52). The NFIB gene itself is not analyzed in our panel, but we did not find a significant gain of 9p where NFIB is located (Supplementary Table S13). The identity of potential drivers of SCLC metastasis on chromosome 16p, the top gain (Supplementary Fig. S10B), remains unknown, but the genomic gain of 16p13.3 has been associated with poor outcomes in prostate cancer (53), and this region contains the PDPK1 gene, coding for a component of the PI3K/AKT pathway.
Figure 2.
Biopsy-site-specific patterns of TMB and gene alterations in SCLC. A, Patterns of TMB in SCLC tumors by anatomic location. Shown are box plots of the TMB distribution (left) and the percentage of TMB-high samples (right) at each site. The sites are ordered by their median TMB from lowest (top) to highest (bottom). B, Volcano plot showing patterns of enrichment or depletion of recurrent gene alterations in different tumor sites compared with lung-biopsied SCLC tumors. Gene alterations identified to be statistically different in prevalence between a metastatic site and lung are indicated, with those statistically significant after correcting for multiple hypothesis testing in bold. OR, odds ratio. C, Prevalence and comparison of the most frequently identified gene alterations in brain vs. liver SCLC metastases. (P value thresholds: *, 0.05; **, 0.01; ***, 0.001)
Importantly, when we investigated alterations in specific genes, we found that brain metastases were significantly enriched for PTEN alterations compared with lung tumors (19.8% vs. 9.7%, P = 0.012; Fig. 2B; Supplementary Table S14). This was also true for brain versus liver metastases (19.8% vs. 9.0%, P = 0.007; Fig. 2C; Supplementary Table S15). Notably, PTEN loss-of-function mutations were predominantly clonal across biopsy sites (Supplementary Table S16). Similar observations of elevated prevalence in brain biopsies were made for amplification of RICTOR, a gene that codes for a regulator of mTOR activity (54), although this did not reach statistical significance after correcting for multiple testing (11.2% brain metastases vs. 5.3% lung biopsies). These data suggest that the PI3K/AKT/MTOR pathway may play a unique role in SCLC brain metastasis.
Defining Genetic Subtypes in SCLC
A previous study of 110 SCLC tumors failed to identify clear genetic subtypes (7). In contrast, a growing consensus in the field is that SCLC subtypes may be defined by transcriptional signatures driven by specific transcription factors (55–57). Importantly, some of the subtypes may have unique vulnerabilities, including, for example, sensitivity to Aurora kinase inhibitors in the MYC-high NEUROD1-high SCLC subtype (58). The large number of tumors analyzed enabled us to investigate genetic interactions in SCLC defined by co-occurrence and mutual exclusivity that may help conclusively determine whether such genetic subtypes exist in SCLC (Supplementary Fig. S11 and Supplementary Table S17). Not surprisingly, mutations in TP53 and RB1 were highly significantly co-occurring [odds ratio (OR) = 7.4, P < 10−5]. Some observations were more unexpected: For example, alterations in the PIK3CA gene that activate the catalytic subunit of the PI3K kinase are significantly co-occurring with amplification of the gene coding for SOX2, suggesting cooperative effects between these two oncogenes in SCLC (59). Our analysis of recurrent mutations and alterations further suggested three possible subtypes. First, some tumors had no alterations in TP53 and/or RB1. Second, we noticed a subgroup of tumors with STK11 mutations (STK11 codes for the LKB1 kinase). Third, our analysis found SCLC tumors with oncogenic driver mutations characteristic of NSCLC, which is suggestive of transformation from NSCLC to SCLC. These genetic groups are further discussed below.
SCLC Tumors without Genomic Inactivation of TP53 and/or RB1
Although SCLC is viewed as a cancer type in which cells are functionally mutant for RB and p53, not all SCLC cells show inactivation of the RB1 and TP53 genes. For example, chromothripsis, a catastrophic event characterized by massive genomic rearrangements, has been suggested to lead to the amplification of the CCND1 gene coding for Cyclin D1, which may result in the functional inactivation of RB by increased phosphorylation (7). Importantly, SCLC cells expressing wild-type RB may be sensitive to CDK4/6 inhibitors (60) and more sensitive to ICIs activating T cells than RB-mutant tumors (61). Similarly, strategies are being developed to treat p53 wild-type tumors (62). Thus, a better understanding of SCLC tumors that have functional RB and/or p53 molecules may help develop distinct targeted therapies for these patients.
We analyzed SCLC tumors in our cohort that may be RB1 and/or TP53 wild-type. For this analysis, we defined RB1- and TP53-mutant tumors as tumors for which we could detect pathogenic alterations in these genes; wild-type tumors had no pathogenic variants and no variants of unknown significance (VUS). We also assumed that tumors with one detected mutant allele of RB1 or TP53 may have lost the other allele via gene silencing or other less readily detectable events (and in some cases, we are able to document this loss of heterozygosity). This analysis of 3,590 tumors (excluding 10 tumors with VUS in RB1 or TP53) identified 96 TP53 wild-type tumors (2.7%), 747 RB1 wild-type tumors (20.8%), and 197 tumors wild-type for both TP53 and RB1 (5.5%). Recent studies using immunostaining to detect RB on tumor sections found 6% to 14% of RB wild-type tumors (13, 29), indicating that our genetic analyses overestimate wild-type tumors, possibly with some genetic and/or epigenetic alterations inactivating RB1 or TP53 not being detected in our platform. The presence of wild-type TP53 or wild-type RB1 was significantly associated with a lower TMB, and tumors with both TP53 and RB1 wild-type genes had the lowest TMB (Fig. 3A and B; Supplementary Fig. S12A–S12D).
Figure 3.
TP53 and RB1 wild-type tumors represent a distinct genetic subtype of SCLC associated with human papilloma virus (HPV) infection. A, Distribution of TMB (mut/Mb) in SCLC tumors wild-type and/or mutant for TP53 and RB1. The TMB in each mutation group was compared against cases identified to be TP53 + RB1 double mutants (P value thresholds: **, 0.01; ***, 0.001). B, Prevalence of TMB-high status (≥10 mut/Mb) in SCLC tumors wild-type and/or mutant for TP53 and RB1. C, Prevalence of gene alterations in SCLC tumors wild-type for TP53 and RB1 compared with TP53- or RB1-mutant SCLC tumors. D, Analysis of the number of mutations representing the tobacco-associated signature (SBS4) in TP53/RB1 wild-type and TP53/RB1-mutant SCLC tumors. E, Comparative prevalence of TP53 and RB1 alterations in patients of EUR and AFR ancestry. F–I, Additional validation of an index case of HPV-positive SCLC detected based on sequencing. The genomic profiling of a liver biopsy showed a TP53 alteration, and a CCNE1 amplification was identified to be wild-type for RB1. Of note, the patient had a prior history of lung adenocarcinoma and prior negative cervical Pap smears. F, Hematoxylin and eosin staining showing the SCLC tumor (200× magnification). G, Immunohistochemistry (IHC) indicating high positivity for p16 (200× magnification). H, IHC indicating retained RB1 (200× magnification). I, PCR-based HPV genotyping from formalin-fixed, paraffin-embedded tumor tissue (two replicates) and a positive control. WT, wild-type.
We also used the large size of our cohort to examine co-occurrences and mutual exclusivity events in TP53 and/or RB1 wild-type tumors compared with mutant tumors (Supplementary Table S18). As expected, inactivating alterations in CDKN2A—which codes for p16, a positive regulator of RB—and activation alterations in CCND1—which codes for Cyclin D1, a negative regulator of RB—were significantly mutually exclusive with alterations in RB1. Similarly, amplification of MDM2, a negative regulator of p53, was significantly mutually exclusive with inactivation of TP53 (Fig. 3C; Supplementary Fig. S13A and S13B). Although CCNE1 amplification events are frequent in SCLC tumors, and whereas Cyclin E/CDK2 kinase complexes inhibit RB function, CCNE1 amplification was not enriched in RB1 wild-type tumors (Supplementary Fig. S13B). Because CCNE1 amplification was enriched in TP53-mutant tumors (Supplementary Fig. S13A), it is possible that p53 loss is important to prevent cell death or cell-cycle arrest upon increased Cyclin E/CDK2 activity. Enrichment in TP53 and/or RB1 wild-type tumors in alterations in genes such as FGFR1, KRAS, KEAP1, or BRAF (Fig. 3C; Supplementary Fig. S13A and S13B), which are frequently mutated in NSCLC, suggests that a number of these tumors may have arisen from NSCLC (see below). In support of this possibility, TP53 and RB1 wild-type tumors had a lower signature associated with smoking (Fig. 3D; Supplementary Fig. S14A and S14B), and TP53 and RB1 alterations were less frequent among the 24 never-smokers available in the clinical cohort (TP53 96.5% ever-smokers vs. 45% never-smokers, RB1 77.0% vs. 45%; Supplementary Fig. S15).
There was no significant difference in mOS between TP53/RB1-mutant and wild-type tumors (Supplementary Fig. S16A), supporting the notion that the wild-type tumors were indeed SCLC. When assessed separately, RB1 wild-type and RB1-mutant tumors also showed no differences in mOS (Supplementary Fig. S16B). TP53-mutant tumors showed a slightly lower mOS compared with TP53 wild-type tumors [8.0 vs. 8.8 months, hazard ratio (HR) = 1.6 (1.1–2.5), P = 0.03; Supplementary Fig. S16C), although this analysis is limited by the small cohort size of TP53 wild-type tumors.
Notably, AFR genetic ancestry was associated with decreased presence of TP53 or RB1 alterations (Fig. 3E). Further, when examining alterations in young patients of all genetic ancestries (<50 years; N = 239) compared with older patients (≥50 years; N = 3,361), TP53 and RB1 alterations were less frequent in younger patients: 77.0% vs. 92.6% TP53 (P < 10−4) and 60.7% vs. 74.4% RB1 (P < 10−4), respectively (Supplementary Fig. S17 and Supplementary Table S19).
Identification of Human Papillomavirus in SCLC
The presence of tumors with no genetic alterations in TP53 and RB1 led us to investigate if the p53 and RB proteins may be inactivated by other means in these tumors. Oncoproteins for several human viruses can functionally inactivate p53 and RB [e.g., E6/E7 from human papillomavirus (HPV); refs. 63, 64]. Sequencing reads left unmapped to the human reference genome were compared against strains of oncoviruses as described previously (65). In our initial analysis, we identified 87 tumors with HPV sequences (Supplementary Fig. S18A). Although the most frequent alterations within these HPV-positive (HPV+) cases included TP53 and RB1, the rates were lower than in HPV-negative tumors (Supplementary Fig. S18B; Supplementary Table S20). Interestingly, 12.7% (25/197) RB1/TP53 wild-type tumors were HPV+, whereas only 1.8% (62/3,393) of RB1/TP53-mutant tumors were HPV+ (Supplementary Fig. S19A). In HPV+RB1/TP53-mutant tumors, the E7 oncoprotein from HPV may inactivate the RB family members p107 and p130 (66), which may further promote tumor growth. Most of the HPV+RB1/TP53 wild-type cases were HPV16/18/45, which are among the most oncogenic subtypes. Although basal cells in the lung epithelium may be infected by some HPV strains (67), the lungs are not a frequent site of HPV infection. A thorough analysis of 15 recent cases of HPV+ SCLC tumors in our cohort (10 RB1/TP53 wild-type and five RB1/TP53 mutant) showed that some of these cases are very likely to represent metastases from small cell neuroendocrine (NE) tumors at other body sites as reported before (68). However, our analysis also identified two cases with likely lung origin (Supplementary Fig. S19B and Supplementary Table S21). In particular, we were able to perform additional validation in one case with sufficient tissue for analysis. The patient was an 82-year-old female former smoker who was diagnosed with multifocal well-differentiated adenocarcinoma of the lung, EGFR wild-type. She was initially treated with radiotherapy to the right upper lobe. Approximately 1 year later, interval imaging showed further progression of the disease, and a liver biopsy at that time was positive for metastatic SCLC (Fig. 3F). Genomic profiling revealed a TMB of 23 mut/Mb, with RB1 wild-type and a TP53-mutant status, as well as CCNE1 amplification and evidence for HPV16 based on sequencing. The patient also had prior negative cervical Pap smears. Additionally, immunohistochemistry (IHC) analysis revealed strong expression of p16 (Fig. 3G) and expression of RB (Fig. 3H). HPV genotyping indicated HPV16/18/33 positive and HPV31/35 negative (Fig. 3I).
Taken together, these data indicate that tumors with wild-type RB1 and/or TP53 define a distinct subgroup of SCLC tumors that may be amenable to unique treatment modalities.
Cohort of SCLC Tumors Defined by STK11 Mutations
Genetic alterations in STK11 are frequent in NSCLC. Functional inactivation of LKB1 has been shown to promote tumor development and metastasis (69, 70) and modify response to ICI therapy (71–73). Recurrent STK11 mutations are also found in a subset of NSCLC-like large cell NE cancers (34). In contrast, STK11 mutations have not been identified as recurrent events in SCLC, and little is known about LKB1 in SCLC (74). We identified 62 STK11-mutant tumors in our cohort, representing 1.7% of the entire cohort (Fig. 4A). Histologic evaluation confirmed a diagnosis of SCLC (Supplementary Fig. S5 and Supplementary Table S7). These tumors were enriched for mutations in genes associated with the development of NSCLC, including KRAS and KEAP1, suggesting the possibility of SCLC transformation (see below), and harbored fewer mutations in RB1 compared with the STK11 wild-type cohort (Fig. 4A and B; Supplementary Table S22). These tumors also showed a significant trend for higher TMB (Fig. 4C). Patients with STK11-mutant SCLC tended to be enriched for AFR origin (Fig. 4D). Although the number of patients with STK11-mutant tumors was limited in the clinical cohort (n = 7), we observed a reduction in survival in these patients (Fig. 4E). These findings define a rare subtype of SCLC tumors (1%–2%) with mutant STK11. Patients with STK11-mutant SCLC tumors may benefit from efforts in other cancer types with the same mutations to develop new therapeutic approaches (75).
Figure 4.
STK11 alterations define a new genetic subtype of SCLC with decreased OS. A, Most frequently detected gene alterations in STK11-mutant SCLC tumors. Gene alterations identified more frequently in STK11-mutant SCLC tumors compared with STK11 wild-type tumors are displayed in mint green, and those identified less frequently in STK11-mutant SCLC tumors compared with STK11 wild-type tumors are in orange. Genes that were similarly prevalent are shown in gray. B, Oncoplot of the most frequent gene alterations identified in STK11-mutant SCLC tumors. Genes are indicated on the left and their alteration frequency on the right. Ancestry and TMB for each case are indicated on top. C, Distribution of TMB (right) and the prevalence of TMB-high status, defined as ≥10 mut/Mb (left), in STK11-mutant and wild-type SCLC tumors. D, Comparative prevalence of STK11 alterations in patients of AFR ancestry compared with other ancestry groups (NA: not available due to low sample counts). E, OS of patients with STK11-mutant and wild-type SCLC tumors. Samples with unknown/ambiguous functional status or reduced quality were excluded from the STK11 wild-type cohort. NA, not available due to low sample counts; WT, wild-type.
NSCLC Driver Mutations Are Recurrently Detected in SCLC, Suggesting that SCLC Transformation Is More Frequent than Suspected
Histologic transformation from NSCLC to SCLC has been observed in ∼3% to 14% of patients with EGFR-mutant NSCLC that develop acquired resistance to EGFR TKI therapy (23, 24, 76). These SCLC tumors are thought to represent subclonal evolution from the original EGFR-mutant clonal population and not a new primary tumor, as they maintain the original EGFR mutation (24, 26). Previous studies have suggested that EGFR-mutant transformed SCLC (t-SCLC) may adopt similar genomic and phenotypic characteristics of de novo SCLC but have been limited by very small sample sizes.
In our cohort, we identified 107 SCLC samples harboring activating mutations within the EGFR kinase domain. The genetic ancestry of this subgroup of patients was composed of 71.0% EUR (n = 76), 8.4% AFR (n = 9), 3.7% AMR (n = 4), 15.0% EAS (n = 16), and 1.9% SAS (n = 2), suggesting that lineage transformation can occur across all ancestries. Overall, the EGFR-mutant t-SCLC cohort mirrored the genomic landscape of de novo SCLC, with RB1 and TP53 mutations in the majority of the sample (95.3% and 83.2%, respectively; Fig. 5A; Supplementary Table S23). Notably, PIK3CA mutations were enriched in the EGFR-mutant t-SCLC cohort compared with SCLC samples lacking an EGFR alteration (25.2% vs. 5.0%, OR = 6.4, P < 10−5). Other genetic events enriched in EGFR-mutant t-SCLC included amplification and gain-of-function alterations in NFKBIA (10.3% vs. 1.6%), NKX2-1 (13.1% vs. 2.5%), and CCNE1 (10.3% vs. 4.1%); RBM10 loss-of-function mutations (7.5% vs. 1.1%); and IRS2 (8.4% vs. 1.8%) and GNAS mutations (6.5% vs. 1.0%). As expected, because EGFR-mutant tumors are most often found in never/former light smokers, TMB was significantly lower in the EGFR-mutant t-SCLC cohort versus the EGFR wild-type SCLC cohort (Fig. 5B). Similarly, as expected, EGFR-mutant t-SCLC tumors were enriched in patients with EAS ancestry (Fig. 5C). EGFR-mutant t-SCLC cases were also enriched for APOBEC mutational signatures (SBS2 and SBS13; Fig. 5D; Supplementary Fig. S20A and S20B), indicating that these t-SCLC tumors may present with specific APOBEC-associated mutagenesis, corroborating and expanding on similar analyses in smaller numbers of tumor samples (77). There was no significant difference in mOS between EGFR-mutant and wild-type tumors (Supplementary Fig. S21).
Figure 5.
Distinct genetic features of SCLC tumors harboring driver oncogenes traditionally associated with NSCLC. A, Oncoplot of the most frequent gene alterations identified in SCLC tumors with kinase-domain mutations in the EGFR gene (n = 107). Genes are indicated on the left, and their alteration frequency is on the right. Ancestry and TMB for each case are indicated on top. B, Distribution of TMB in EGFR-mutant and wild-type SCLC tumors. C, Comparative prevalence of EGFR alterations in patients of EAS ancestry compared with other ancestry groups. D, Analysis of the number of mutations representing APOBEC-associated single-base substitution signatures (SBS2 and SBS13) in EGFR wild-type and mutant SCLC tumors. E, Breakdown of the different EGFR kinase-domain mutations identified in SCLC tumors. F, Oncoplot for SCLC tumors with alterations in known oncogenic drivers of NSCLC, excluding EGFR. Genes identified to be altered in these cases are shown on the left, and their alteration frequency is on the right. TMB and ancestry for each case are overlaid on top. WT, wild-type. G, Genomic and clinicopathologic characteristics of 41 patients with paired NSCLC/SCLC samples. Patients were grouped into four categories based on the patterns of alterations detected: shared alterations with driver (+) in NSCLC and SCLC (orange bar); shared alterations with driver (−) in NSCLC and SCLC (pink bar); shared alterations with driver (+) in NSCLC only and lost/undetected in the matched SCLC (gray bar); and no shared alterations between NSCLC and SCLC (blue bar). Each patient is annotated with the histology, the time between the collection of the NSCLC and SCLC biopsies, the driver alteration (if detected), and TMB. Only genes identified to be altered in ≥2 patients are shown. Bar plots showing the total number of patients with each gene alteration are shown on the right for NSCLC and SCLC samples. LCNEC, large cell neuroendocrine cancer; LUAD, lung adenocarcinoma; nos, not otherwise specified; SCC, squamous cell carcinoma.
We also observed that our EGFR-mutant t-SCLC cohort was enriched for patients with exon 19 deletion (Ex19del; n = 68) versus L858R (n = 26; Fig. 5E; Supplementary Table S24). Notably, these two “canonical” EGFR mutations occur at approximately equal frequency in NSCLC based on numerous previous reports. Indeed, in our dataset as well, Ex19del is detected in 45% of all EGFR-mutant NSCLC versus 64% of all EGFR-mutant t-SCLC tumors (Supplementary Fig. S22), which can also be seen in a smaller cohort (76), suggesting that tumors with Ex19del may have an enhanced proclivity for lineage transformation.
Interestingly, we also detected other recurrent NSCLC-associated oncogenic driver mutations, including ALK (n = 5), RET (n = 5), ROS1 (n = 3), and NTRK1 (n = 1) fusions, in SCLC tumor samples, suggesting that transformation to SCLC is not exclusive to EGFR-mutant NSCLC (Fig. 5F). Co-occurring mutations and TMB were similar to the EGFR-mutant t-SCLC cohort.
Longitudinal Analysis of NSCLC to SCLC Samples Reveals Potential Mechanisms of Transformation
Forty-one of the 121 (34%) patients described above had both an NSCLC and an SCLC tumor biopsy genotyped within our dataset. Patterns of shared as well as unique gene alterations were assessed between single-nucleotide polymorphism (SNP)–matched paired NSCLC and SCLC samples from the same patient across different time intervals, and patients were grouped into potential categories based on these patterns (Fig. 5G). First, there were 7 of 41 (17%) patients in whom there were no shared alterations between the NSCLC and SCLC samples. The most likely explanation is that these tumors developed independently within the patients (Fig. 5G, light blue box). Second, there were 7 of 41 patients (17%) in which the NSCLC and SCLC samples shared alterations, but no previously described NSCLC driver gene alteration was detected in either biopsy (Fig. 5G, pink box). These patients would not have been treated with oncogene-targeted therapies, suggesting that other treatment modalities, such as chemotherapy and immunotherapy, can also drive SCLC transformation. Third, in 25 of 41 patients (61%), the NSCLC and SCLC tumor samples both contained a driver mutation previously associated with NSCLC (Fig. 5G, orange box). This was the largest cohort within the matched, paired patient NSCLC–SCLC samples, and our results are concordant with previous data showing that cases of t-SCLC typically retain the original NSCLC driver mutation (26, 76, 77). Finally, there were two patients for whom a driver mutation was detected in the NSCLC sample but not in the SCLC sample (Fig. 5G, gray box). In both cases, the NSCLC and SCLC samples shared other alterations, suggesting that the driver mutation was lost during the transformation process, for example, by recombination with the wild-type allele.
Taken together, our analysis of >100 putative t-SCLC reveals that lineage plasticity may arise from multiple different molecular cohorts of NSCLC, including EGFR-mutant and fusion kinase–positive NSCLC. Furthermore, analysis of paired samples demonstrates that putative SCLC transformation may occur at variable lengths of time from the original NSCLC diagnosis and suggests that time on therapy may not be a factor for stratifying which patients may have t-SCLC at the time of disease progression. With increased use of inhibitors targeting these oncogenic drivers in the clinic, it is likely that more cases of t-SCLC coming from these other types of NSCLC will be identified in the future, and a broader implementation of rebiopsy at the time of acquired therapeutic resistance may prove important.
DISCUSSION
Herein, we present a genomic analysis of the largest cohort of SCLC tumors evaluated to date, encompassing 3,600 tumor specimens. This study is unique in many ways. First, the SCLC samples in our cohort have been predominantly obtained from community sites throughout the United States, representing a more typical “real-world” cohort of SCLC. Second, genomic data are tied to clinical data (including survival) and predicted ancestry data, parameters that have been limited in most previous SCLC studies. This allowed us for the first time to investigate genetic differences in SCLC tumors based on ancestry. Third, to the best of our knowledge, our study contains the analysis of the largest number of SCLC tumors from AFR ancestry to date (n = 256, 7.1% of the entire cohort). Fourth, as a result of the large sample size, we were able to evaluate mutational status by anatomic location of the tumor and show site-specific enrichment of certain genomic alterations. Fifth, this study contains the largest cohort studied of putative t-SCLC (n = 121, including 107 EGFR-mutant cases).
A major limitation of our study is the number of genes for which alterations are queried, with deep sequencing of exons from up to 324 cancer-related genes and select introns from up to 34 genes frequently rearranged in cancer. Because SCLC is a cancer type with unique biology, it is possible that some frequently altered genes are not included in the list of genes analyzed. For example, whole-genome sequencing identified recurrent loss-of-function alterations in genes coding for the RB family members p107 and p130 (7), but these two genes (RBL1 and RBL2) are not included in our panel. Another limitation of our data is the lack of RNA/protein expression profiles for the tumors analyzed. It is possible that some gene alterations identified at the DNA level do not result in changes in gene/protein expression in SCLC cells, including some of the new rearrangements identified. Finally, our genetic analysis of new or rare alterations has not been validated in cell or animal models. One exception is TSC1, which shows alterations in ∼1% of cases in our cohort, and that we recently validated in mouse models and human cells as a potent tumor suppressor in SCLC (78). Despite these limitations, we have made several key observations related to SCLC pathobiology that were not possible from previous studies due to sample size, including new genetic subgroups, site-specific mutational patterns, and insights into histologic transformation (summarized in Fig. 6).
Figure 6.
Overview and summary of the main findings from this analysis of 3,600 cases of SCLC. Schematic representation highlighting the main findings from our integrative analysis of 3,600 patients with SCLC with diverse genetic ancestry. WT, wild-type.
Our work underscores the existence of genetic subtypes in SCLC and key genetic determinants of patient outcomes. Some of these subtypes may be rare or very rare, but patients with these tumors may greatly benefit from personalized treatments. For example, HPV+TP53/RB1 wild-type tumors may represent <0.1% of cases, but these tumors may be uniquely responsive to strategies targeting the virus or reactivating p53 function to induce cell death. As another example, STK11 mutations were detected in 1.7% of our entire cohort, were enriched in patients of AFR ancestry, and were associated with a decreased OS compared with the STK11 wild-type cohort. Numerous studies have now shown that STK11 mutations are associated with decreased response to ICI therapy in NSCLC (71–73), and it is possible that the same is true in SCLC.
Therapeutic selection based on tumor mutational status has revolutionized the care of patients with NSCLC, leading to the development of numerous new drugs and implementation of personalized treatment approaches that have become the accepted standard of care for patients with NSCLC around the world. However, the implementation of personalized therapies for patients with SCLC has remained elusive. Classification of SCLC into subtypes defined by transcriptional programs has been postulated, with two main subtypes emerging—NE and non-NE (55). However, the prognostic, predictive, and clinical significance of these subtypes is not well defined. Furthermore, how specific mutations influence the subtype landscape remains unclear. NE tumors are enriched for alterations in RB1, NOTCH1, MYCL1, and chromatin modifier genes, and these NE tumors may have improved responses to replication stress inhibitors and poorer responses to ICI therapy compared with non-NE tumors (14). However, in this same study, there were no differences in OS between patients with NE and non-NE tumors, suggesting that the transcriptomic type alone may be insufficient for stratification.
Our data identified more frequent PTEN alterations in brain metastases versus other tumor sites. In genetically engineered mouse models of SCLC, loss of PTEN has been shown to promote tumor development (79, 80), but this was not accompanied by the development of brain metastases. In part, this is likely due to the rapid death of the mutant mice from their primary tumors in the lungs and from liver metastases, although it is also possible that mice do not provide an accurate model for the development of brain metastases. The development of such models will help ascertain the role of the PTEN pathway in SCLC brain metastasis.
Importantly, our large “real-world” cohort, while composed of a majority of patients from EUR ancestry, is also the most diverse cohort of SCLC tumors analyzed to date, which allowed us for the first time to investigate genetic differences in SCLC tumors based on ancestry. For instance, we previously discussed the need to better investigate genetic, environmental, and socioeconomic factors associated with SCLC development in various populations, including in Black patients with SCLC (81). SCLC tumor samples harboring activating mutations within the EGFR kinase domain were found in all ancestry groups but enriched in patients of EAS ancestry, as expected (82, 83). More surprisingly, when we analyzed 256 SCLC tumors in patients of AFR ancestry, we found that these tumors were more likely to be wild-type for RB1 and TP53, and mutant for STK11, suggesting that populations of different ancestry may be enriched for different genetic subtypes of SCLC. These observations may help guide genetic testing and clinical decisions. The challenges associated with capturing and analyzing self-reported race in the clinical trial setting have been well described in the literature (84). The use of genomic ancestry in this real-world population offers a model for describing genomic differences across ancestral populations and contributes to a growing number of similar studies in other cancer types (85–87).
Our cohort of patients with matched NSCLC and SCLC samples also extends on previous observations related to lineage plasticity in several ways. Notably, these data show that SCLC transformation can occur across multiple different NSCLC driver mutations, not just EGFR-mutant NSCLC. This is important because tumor rebiopsy at the time of disease progression is not currently mandated for all molecular cohorts of NSCLC. Yet, at present, tumor biopsy is the only way to definitively diagnose SCLC transformation, and a finding of SCLC in a patient previously diagnosed with NSCLC would change clinical management in terms of therapeutic selection. Current clinical trials attempting to prevent SCLC transformation by combining targeted therapy with platinum–etoposide chemotherapy (traditionally used for SCLC) necessitate that the NSCLC tumor harbors both TP53 and RB1 mutations (NCT03567642). This is important based on our data that putative transformation from NSCLC to SCLC does not strictly require both mutation in TP53 and mutation in RB1.
Overall, these data are expected to serve as a catalyst for additional laboratory-based and clinical research studies that will further our knowledge of SCLC biology and the biology of other types of NE tumors as well as provide much-needed advances in treatment paradigms for patients with SCLC.
METHODS
Targeted Next-Generation Sequencing of SCLC Tumors
Formalin-fixed, paraffin-embedded (FFPE) tissue sections of SCLC from 3,600 patients were profiled using FoundationOne (N = 1,515) or FoundationOneCDx (N = 2,085) comprehensive genomic profiling (CGP) assays in a Clinical Laboratory Improvement Amendments–certified, College of American Pathologists–accredited laboratory (Foundation Medicine, Inc.). Briefly, a minimum of 50 ng of DNA was extracted from FFPE sections and CGP was performed on hybridization-captured, adapter ligation–based libraries to a median exon coverage depth of >500× for exons of up to 324 cancer-related genes and select introns from 34 genes frequently rearranged in cancer (Supplementary Table S2).
A multistage pathology review was performed prior to and after sequencing. Prior to sequencing, board-certified pathologists on staff at Foundation Medicine, Inc. reviewed the submitted pathologic diagnosis of each case and examined hematoxylin and eosin (H&E)–stained slides. The H&E slide used for pathology review is the same as the FFPE tissue section dissected for sequencing. Tumor type assignment for each case was performed based on the submitting diagnosis and rereview of the H&E. If necessary, pathologist-directed macrodissection to achieve >20% estimated percent tumor nuclei (%TN) in each case was performed, where %TN is defined as 100 times the number of tumor cells divided by the total number of nucleated cells. Approval for this study, including a waiver of informed consent and the Health Insurance Portability and Accountability Act (HIPAA) waiver of authorization, was obtained from the Western Institutional Review Board (Protocol No. 20152817).
Identification of Genomic Alterations
Different classes of genomic alterations, comprising short variants (base substitutions and small insertions/deletions), copy-number alterations (focal amplifications and homozygous deletions), and rearrangements, were identified using the approach described previously (88). TMB was determined on 0.8 to 1.2 Mb of the sequenced region, and samples with a TMB of at least 10 mut/Mb were classified as TMB-high (89). For PTEN short variants, the clonality was estimated using results from the somatic-germline-zygosity algorithm (90). For each somatic mutation detected in a sample, a variant-based tumor fraction (vTF) was calculated using the following formula: 2AF/(mc – AF(wc + mc −2)), where variant allele fraction (AF), mutant copies (mc), and wild-type copies (wc) were used (91). The maximum vTF among all the somatic mutations in a sample was used as an estimate for the tumor fraction of the sample (sTF). Clonal fraction was then calculated as the ratio of vTF to the sTF, with ≥50% considered clonal.
Detection of Chromosomal Arm–Level Aneuploidy
A copy-number modeling algorithm was used to identify chromosome arm–level aneuploidy. Briefly, for each sample, the algorithm utilizes the coverage profile for regions of the genome targeted in the assay, normalized to a process-matched normal control, to model the copy number of each segment. The minor allele frequencies of up to 59,622 SNPs distributed across each segment were used, along with the normalized intensities to identify regions under aneuploidy (gain, loss). If over 50% of a chromosome arm exhibited a gain or a loss, it was classified as a chromosomal arm–level aneuploidy event. Additionally, the chromosome arm score (Charm) for tumor suppressors (CharmTSG) and oncogenes (CharmOG) described by Davoli and colleagues (32) was used to perform correlation analyses against the identified chromosomal arm–level aneuploidy events identified in our cohort.
Prediction of Patient Genomic Ancestry
Ancestry for each patient was predicted using SNPs from the targeted next-generation sequencing assay that overlapped with those captured in the phase 3 1000 Genomes (92). This SNP-based approach was projected down to five principal components that were used to train a random forest classifier to identify the ancestry groups EUR, AFR, EAS, SAS, and AMR, as described previously (93).
Analysis of Genomic and Clinical Patterns in Specific Subpopulations
Differences in the prevalence of gene alterations and biomarkers were assessed using a Fisher exact test with FDR-based correction for multiple testing. Only genes that were targeted on both assay platforms were assessed (Supplementary Table S2). Additionally, for continuous variable biomarkers (e.g., TMB), the Wilcoxon rank sum test was used to assess the differences between different subgroups.
Identification of Mutational Signatures
We utilized a pooled approach to assess mutational signatures in different SCLC alteration subgroups from the targeted panel assay. Comparisons were performed between EGFR-mutant and EGFR wild-type as well as TP53/RB1-mutant and TP53/RB1 wild-type samples. Mutagenic signatures are typically considered to be additive, and therefore the difference between the two groups was used to understand the additional effect of mutations. All variants that were predicted nongermline and VUS were pooled for this analysis. The contributions of the known COSMIC v3.2 signatures were obtained as described previously (94). The number and percentage of mutations attributed to each mutational signature were calculated relative to the total number of pooled mutations. The stability of this pooled approach was evaluated by resampling the cohorts to a jackknife sample size, defined as the mutations from 30 samples. Both cohorts were resampled without replacement 1,000 times, and signature attribution was assessed on each of the resampled pools of mutations. This provides both the median and 95% CI for the contribution of all known COSMIC v3.2 mutation signatures in each cohort. Samples with a very high TMB (≥50 mut/Mb) were excluded from this pooled mutation signature analysis.
Analysis of Clinical Outcomes
This study used the nationwide (U.S.-based) deidentified Flatiron Health (FH)–Foundation Medicine, Inc. (FMI) SCLC CGDB. The deidentified data originated from approximately 280 U.S. cancer clinics (∼800 sites of care). Retrospective longitudinal clinical data, derived from EHRs comprising patient-level structured and unstructured data, were curated via technology-enabled abstraction, and linked to the genomic data obtained from the CGP test at FMI using deidentified, deterministic matching (95). This study included 678 patients with an SCLC diagnosis who received care in the FH network between January 2011 and September 2021 and underwent tissue biopsy–based CGP (FoundationOne or FoundationOneCDx) between October 2012 and September 2021. Institutional Review Board approval of the study was obtained prior to study conduct and included a waiver of informed consent based on the observational, noninterventional nature of the study (WCG IRB, Protocol No. 420180044).
OS was calculated from the date of SCLC diagnosis to either date of death or date of last clinic visit. Patients were treated as at risk of death only after the later of their first sequencing report date and their second visit to the FH network on or after January 1, 2011, as both are requirements for inclusion in the database. Treatment start dates were determined by oncologist-defined, rule-based lines of therapy. Time to next treatment was calculated from the first-line treatment start date to either the second-line treatment start date or date of death if death occurred prior to the start of second-line treatment. Patients without an event were censored at the date of their last clinic visit. All time-to-event outcomes were assessed by log-rank test and univariate Cox proportional hazards models. Analyses were performed on R software version 4.0.3.
Viral Detection
A de novo assembly of off-target sequencing reads left unmapped to the human reference genome (hg19) was performed as described previously (65). These assembled contigs were competitively aligned by BLASTn to the NCBI database of viral nucleotide sequences to detect oncoviruses, including the HPV types. Contigs ≥80 nucleotides in length and with ≥97% identity to the BLAST sequence were determined to be positive for viral status.
For HPV genotyping, DNA was extracted from FFPE tissue sections; concentration and quality were assessed using a NanoDrop spectrophotometer (Thermo Fisher Scientific). PCR using cycling conditions of 94°C for 30 seconds followed by 55°C for 1 minute at a ramp rate of 2°C/second for 35 cycles (C1000 Touch Thermal Cycler; Bio-Rad) was performed with probes designed to specifically target HPV16E6, HPV18E6, HPV31E6, HPV33E6, and HPV35E6. Amplified PCR products were visualized using 1% agarose/GelRed gel. Two separate samples from the same patient were run. In addition, IHC was performed on FFPE specimens of this case to evaluate RB and p16INK4A expression as previously described (96).
Investigation of Liquid Biopsies
A total of 81 SCLC cases profiled on the FoundationOneLiquid CDx assay were examined for their mutational patterns (97). Quantification of the circulating tumor DNA (ctDNA) fraction was performed using two complementary methods: a tumor fraction estimator (TFE) and the maximum somatic allele frequency (MSAF) method (98). TFE is based on a measure of tumor aneuploidy and MSAF uses allele fraction from somatic coding alterations to estimate ctDNA fraction. Patterns of ctDNA fraction in this SCLC cohort were contrasted to 4,573 NSCLCs profiled on the same assay.
Data Availability
The sequencing data generated in this study are derived from clinical samples. All consented data supporting the findings of this study that can be released are provided within the article and its supplementary files. Due to HIPAA requirements, we are not authorized to share underlying sequence data or individualized patient genomic data, which contain potentially identifying or sensitive patient information. Foundation Medicine, Inc. is committed to collaborative data analysis, and it has well-established and widely utilized mechanisms by which investigators can query its core genomic database of >600,000 deidentified sequenced cancers to obtain aggregated datasets. For more information and mechanisms of access to the Foundation Medicine, Inc. data in this study, please contact the corresponding authors or the Foundation Medicine, Inc. Data Governance Council at data.governance.council@foundationmedicine.com. You and your institution will be required to sign a data transfer agreement.
Supplementary Material
Supplementary Table S1: First-, second-, and third-line systemic therapy in the SCLC clinical cohort. Supplementary Table S2: Genes analyzed as part of this study. Supplementary Table S3: Prevalence of alterations in the genes analyzed. Supplementary Table S4: Prevalence of gene alterations in 81 cases with liquid biopsies. Supplementary Table S5: Chromosomal losses and gains in SCLC. Supplementary Table S6: TET2 loss of function alterations detected in SCLCs. Supplementary Table S7: Manual review of specific mutation subgroups in SCLCs. Supplementary Table S8: Patterns of gene alterations in SMARCA4 altered and wild-type tumors. Supplementary Table S9: Prevalence of gene alterations in rearrangement-positive SCLCs. Supplementary Table S10: Univariate analysis of association between gene alterations and overall surival in the clinical cohort of stage III/IV SCLC tumors. Supplementary Table S11: Patterns of tumor mutational burden based on site of biopsy. Supplementary Table 12: Summary of tumor purity and tumor mutational burden by biopsy site. Supplementary Table S13: Aneuploidy patterns based on site of biopsy. Supplementary Table S14: Comparison of gene alterations in each biopsy site against lung biopsies. Supplementary Table S15: Comparison of gene alterations in liver and brain metastases. Supplementary Table S16: Summary of PTEN alterations in brain and other biopsy sites. Supplementary Table S17: Patterns of co-occurrence and mutual exclusivity between gene alterations in the overall SCLC cohort. Supplementary Table S18: Patterns of gene alterations in TP53 and/or RB1 mutant and wild-type cohorts. Supplementary Table S19: Patterns of gene alterations in young and older patients with SCLC. Supplementary Table S20: Patterns of gene alterations in HPV positive and HPV negative tumors. Supplementary Table S21: Manual review of specific HPV+ SCLCs. Supplementary Table S22: Patterns of gene alterations in STK11 mutant and wild-type cohorts. Supplementary Table S23: Patterns of gene alterations in EGFR mutant and wild-type cohorts. Supplementary Table S24: EGFR kinase domain alterations identified in the overall SCLC cohort.
Figure S1: Patterns of tumor mutational burden across different ancestry groups. Figure S2: Spectrum of TP53 and RB1 mutations in SCLC. Figure S3: Gene alteration landscape detected from targeted sequencing of liquid biopsies. Figure S4: Chromosomal loss events are frequent in SCLC and are preferentially enriched for tumor suppressor genes. Figure S5: Hematoxylin & Eosin (H&E) staining for some representative SCLC tumors with rare genomic alterations. Figure S6: Gene alterations detected in SMARCA4-altered SCLC. Figure S7: SCLC tumors exhibit recurrent gene rearrangements with therapeutic potential. Figure S8: Trends of overall survival across different ancestry groups and stage in the clinical cohort. Figure S9: Examination of tumor purity and tumor mutational burden (TMB). Figure S10: Liver and Brain SCLC metastases are enriched for chromosomal arm-level gains compared to lung-biopsied SCLC tumors. Figure S11: SCLC tumors present with unique co-occurring and mutual exclusive patterns of gene alterations. Figure S12: SCLC tumors with wild-type TP53 and/or RB1 have a low tumor mutational burden. Figure S13: SCLC tumors with wild-type TP53 and/or RB1 present with specific gene alterations. Figure S14: A smoking-associated mutational signature is rare in TP53/RB1 WT SCLC tumors. Figure S15: TP53 and RB1 alterations are less frequent in never smokers. Figure S16: Patterns of overall survival based on TP53 and RB1 alteration status. Figure S17: TP53 and RB1 mutations are more frequent in older patients with SCLC. Figure S18: Gene alterations detected in HPV-positive SCLC. Figure S19: Examination of HPV subtypes and prevalence in TP53/RB1 mutant and wild-type SCLC tumors. Figure S20: EGFR-mutant SCLC tumors exhibit unique mutational signature profiles. Figure S21: No overall survival differences based on EGFR mutation status in SCLC. Figure S22: Putative transformed SCLC tumors from EGFR-mutant NSCLC are enriched for EGFR exon 19 deletions.
Acknowledgments
The authors thank members of the Lovly and Sage labs, the Foundation Medicine, Inc. scientific review team, and members of the U54 SCLC Consortia for critical comments on the manuscript. This work was supported by the NIH (grant numbers CA231851, CA217450, and CA231997 to J. Sage and CA217450, CA224276, CA233259, CA086485, and CA129243 to C.M. Lovly). C.M. Lovly was also partially supported by a LUNGevity Foundation award with funds raised by EGFR Resisters for the 2021 EGFR Resisters/LUNGevity Foundation Lung Cancer Research Award Program, as well as the Phran Galante Research Fund.
The publication costs of this article were defrayed in part by the payment of publication fees. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Footnotes
Note: Supplementary data for this article are available at Cancer Discovery Online (http://cancerdiscovery.aacrjournals.org/).
Authors’ Disclosures
S. Sivakumar reports personal fees from Foundation Medicine, Inc. and other support from Roche during the conduct of the study. M. Montesion reports personal fees from Foundation Medicine, Inc. and other support from Roche during the conduct of the study. R. Sharaf reports other support from Foundation Medicine, Inc. and Roche during the conduct of the study. D.I. Lin is a full-time employee of Foundation Medicine, Inc., which is a wholly owned subsidiary of Roche, and reports Roche stock ownership outside the submitted work. Z. Fleischmann reports personal fees from Foundation Medicine, Inc. and other support from Roche during the conduct of the study. E.M. Ebot is an employee of Foundation Medicine, Inc. and a stockholder in Roche. J.Y. Newberg reports other support from Roche outside the submitted work. J.M. Mills reports other support from Foundation Medicine, Inc. and Roche during the conduct of the study; other support from Foundation Medicine, Inc., Roche, Merck, Abbott, and AbbVie outside the submitted work; and is an employee of Foundation Medicine, Inc. and a stockholder in Roche, Merck, Abbott, and AbbVie. P.S. Hegde reports other support from Foundation Medicine, Inc. outside the submitted work. A. Dowlati reports other support from Tempus, Amgen, AstraZeneca, Ipsen, Prelude, and Genomic Health outside the submitted work. J. Sage reports personal fees from Disco Pharmaceuticals outside the submitted work. C.M. Lovly reports other support from Amgen, AnHeart, AstraZeneca, Blueprint Medicines, Boehringer Ingelheim, Cepheid, D2G Oncology, Daiichi Sankyo, Eli Lilly, EMD Serono, Genentech, Indupro, Janssen, Medscape, Novartis, Pfizer, Puma, and Takeda outside the submitted work, and is on the Data and Safety Monitoring Board for Janssen (uncompensated). No disclosures were reported by the other authors.
Authors’ Contributions
S. Sivakumar: Conceptualization, formal analysis, investigation, visualization, writing–original draft, writing–review and editing. J.A. Moore: Formal analysis, writing–review and editing. M. Montesion: Formal analysis, visualization, writing–review and editing. R. Sharaf: Formal analysis, writing–review and editing. D.I. Lin: Formal analysis, writing–review and editing. C.I. Colon: Validation, writing–review and editing. Z. Fleischmann: Formal analysis, writing–review and editing. E.M. Ebot: Formal analysis, writing–review and editing. J.Y. Newberg: Formal analysis, writing–review and editing. J.M. Mills: Supervision, writing–review and editing. P.S. Hegde: Supervision, writing–review and editing. Q. Pan: Validation, writing–review and editing. A. Dowlati: Validation, writing–review and editing. G.M. Frampton: Supervision, writing–review and editing. J. Sage: Conceptualization, supervision, investigation, writing–original draft, writing–review and editing. C.M. Lovly: Conceptualization, supervision, investigation, writing–original draft, writing–review and editing.
References
- 1. Rudin CM, Brambilla E, Faivre-Finn C, Sage J. Small-cell lung cancer. Nat Rev Dis Primers 2021;7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Horn L, Mansfield AS, Szczesna A, Havel L, Krzakowski M, Hochmair MJ, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med 2018;379:2220–9. [DOI] [PubMed] [Google Scholar]
- 3. Paz-Ares L, Dvorkin M, Chen Y, Reinmuth N, Hotta K, Trukhin D, et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet 2019;394:1929–39. [DOI] [PubMed] [Google Scholar]
- 4. Howlader N, Forjaz G, Mooradian MJ, Meza R, Kong CY, Cronin KA, et al. The effect of advances in lung-cancer treatment on population mortality. N Engl J Med 2020;383:640–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhao X, Kallakury B, Chahine JJ, Hartmann D, Zhang Y, Chen Y, et al. Surgical resection of SCLC: prognostic factors and the tumor microenvironment. J Thorac Oncol 2019;14:914–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Martucci N, Morabito A, La Rocca A, De Luca G, De Cecio R, Botti G, et al. Surgery in small-cell lung cancer. Cancers (Basel) 2021;13:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. George J, Lim JS, Jang SJ, Cun Y, Ozretic L, Kong G, et al. Comprehensive genomic profiles of small cell lung cancer. Nature 2015;524:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Peifer M, Fernandez-Cuesta L, Sos ML, George J, Seidel D, Kasper LH, et al. Integrative genome analyses identify key somatic driver mutations of small-cell lung cancer. Nat Genet 2012;44:1104–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rudin CM, Durinck S, Stawiski EW, Poirier JT, Modrusan Z, Shames DS, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet 2012;44:1111–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhou H, Hu Y, Luo R, Zhao Y, Pan H, Ji L, et al. Multi-region exome sequencing reveals the intratumoral heterogeneity of surgically resected small cell lung cancer. Nat Commun 2021;12:5431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Roper N, Velez MJ, Chiappori A, Kim YS, Wei JS, Sindiri S, et al. Notch signaling and efficacy of PD-1/PD-L1 blockade in relapsed small cell lung cancer. Nat Commun 2021;12:3880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wagner AH, Devarakonda S, Skidmore ZL, Krysiak K, Ramu A, Trani L, et al. Recurrent WNT pathway alterations are frequent in relapsed small cell lung cancer. Nat Commun 2018;9:3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Febres-Aldana CA, Chang JC, Ptashkin R, Wang Y, Gedvilaite E, Baine MK, et al. Rb tumor suppressor in small cell lung cancer: combined genomic and IHC analysis with a description of a distinct Rb-proficient subset. Clin Cancer Res 2022;28:4702–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lissa D, Takahashi N, Desai P, Manukyan I, Schultz CW, Rajapakse V, et al. Heterogeneity of neuroendocrine transcriptional states in metastatic small cell lung cancers and patient-derived models. Nat Commun 2022;13:2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ko J, Winslow MM, Sage J. Mechanisms of small cell lung cancer metastasis. EMBO Mol Med 2021;13:e13122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hodgkinson CL, Morrow CJ, Li Y, Metcalf RL, Rothwell DG, Trapani F, et al. Tumorigenicity and genetic profiling of circulating tumor cells in small-cell lung cancer. Nat Med 2014;20:897–903. [DOI] [PubMed] [Google Scholar]
- 17. Carter L, Rothwell DG, Mesquita B, Smowton C, Leong HS, Fernandez-Gutierrez F, et al. Molecular analysis of circulating tumor cells identifies distinct copy-number profiles in patients with chemosensitive and chemorefractory small-cell lung cancer. Nat Med 2017;23:114–9. [DOI] [PubMed] [Google Scholar]
- 18. Savarese-Brenner B, Heugl M, Rath B, Schweizer C, Obermayr E, Stickler S, et al. MUC1 and CD147 are promising markers for the detection of circulating tumor cells in small cell lung cancer. Anticancer Res 2022;42:429–39. [DOI] [PubMed] [Google Scholar]
- 19. Zhang B, Stewart CA, Wang Q, Cardnell RJ, Rocha P, Fujimoto J, et al. Dynamic expression of schlafen 11 (SLFN11) in circulating tumour cells as a liquid biomarker in small cell lung cancer. Br J Cancer 2022;127:569–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yu HA, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res 2013;19:2240–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oxnard GR, Hu Y, Mileham KF, Husain H, Costa DB, Tracy P, et al. Assessment of resistance mechanisms and clinical implications in patients with EGFR T790M-positive lung cancer and acquired resistance to osimertinib. JAMA Oncol 2018;4:1527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Piotrowska Z, Isozaki H, Lennerz JK, Gainor JF, Lennes IT, Zhu VW, et al. Landscape of acquired resistance to osimertinib in EGFR-mutant NSCLC and clinical validation of combined EGFR and RET inhibition with osimertinib and BLU-667 for acquired RET fusion. Cancer Discov 2018;8:1529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schoenfeld AJ, Chan JM, Kubota D, Sato H, Rizvi H, Daneshbod Y, et al. Tumor analyses reveal squamous transformation and off-target alterations as early resistance mechanisms to first-line osimertinib in. Clin Cancer Res 2020;26:2654–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sequist LV, Waltman BA, Dias-Santagata D, Digumarthy S, Turke AB, Fidias P, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med 2011;3:75ra26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shaurova T, Zhang L, Goodrich DW, Hershberger PA. Understanding lineage plasticity as a path to targeted therapy failure in. Front Genet 2020;11:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Niederst MJ, Sequist LV, Poirier JT, Mermel CH, Lockerman EL, Garcia AR, et al. RB loss in resistant EGFR mutant lung adenocarcinomas that transform to small-cell lung cancer. Nat Commun 2015;6:6377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Xie T, Li Y, Ying J, Cai W, Li J, Lee KY, et al. Whole exome sequencing (WES) analysis of transformed small cell lung cancer (SCLC) from lung adenocarcinoma (LUAD). Transl Lung Cancer Res 2020;9:2428–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Quintanal-Villalonga A, Taniguchi H, Zhan YA, Hasan MM, Chavan SS, Meng F, et al. Multiomic analysis of lung tumors defines pathways activated in neuroendocrine transformation. Cancer Discov 2021;11:3028–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wildey G, Shay AM, McColl KS, Yoon S, Shatat MA, Perwez A, et al. Retinoblastoma expression and targeting by CDK4/6 inhibitors in small cell lung cancer. Mol Cancer Ther 2023;22:264–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 2014;511:543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Almodovar K, Iams WT, Meador CB, Zhao Z, York S, Horn L, et al. Longitudinal cell-free DNA analysis in patients with small cell lung cancer reveals dynamic insights into treatment efficacy and disease relapse. J Thorac Oncol 2018;13:112–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Davoli T, Xu AW, Mengwasser KE, Sack LM, Yoon JC, Park PJ, et al. Cumulative haploinsufficiency and triplosensitivity drive aneuploidy patterns and shape the cancer genome. Cell 2013;155:948–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cancer Genome Atlas Research Network. Comprehensive genomic characterization of squamous cell lung cancers. Nature 2012;489:519–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. George J, Walter V, Peifer M, Alexandrov LB, Seidel D, Leenders F, et al. Integrative genomic profiling of large-cell neuroendocrine carcinomas reveals distinct subtypes of high-grade neuroendocrine lung tumors. Nat Commun 2018;9:1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bowman RL, Levine RL. TET2 in normal and malignant hematopoiesis. Cold Spring Harb Perspect Med 2017;7:a026518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chakravarty D, Gao J, Phillips SM, Kundra R, Zhang H, Wang J, et al. OncoKB: a precision oncology knowledge base. JCO Precis Oncol 2017;2017:PO.17.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Pugh TJ, Bell JL, Bruce JP, Doherty GJ, Galvin M, Green MF, et al. AACR Project GENIE: 100,000 cases and beyond. Cancer Discov 2022;12:2044–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Janesick A, Tang W, Ampig K, Blumberg B. Znf703 is a novel RA target in the neural plate border. Sci Rep 2019;9:8275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Biswas A, Rajesh Y, Mitra P, Mandal M. ETV6 gene aberrations in non-haematological malignancies: a review highlighting ETV6 associated fusion genes in solid tumors. Biochim Biophys Acta Rev Cancer 2020;1874:188389. [DOI] [PubMed] [Google Scholar]
- 40. Hock H, Shimamura A. ETV6 in hematopoiesis and leukemia predisposition. Semin Hematol 2017;54:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ciampricotti M, Karakousi T, Richards AL, Quintanal-Villalonga À, Karatza A, Caeser R, et al. Rlf-Mycl gene fusion drives tumorigenesis and metastasis in a mouse model of small cell lung cancer. Cancer Discov 2021;11:3214–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dy GK, Miller AA, Mandrekar SJ, Aubry MC, Langdon RM, Morton RF, et al. A phase II trial of imatinib (ST1571) in patients with c-kit expressing relapsed small-cell lung cancer: a CALGB and NCCTG study. Ann Oncol 2005;16:1811–6. [DOI] [PubMed] [Google Scholar]
- 43. Lu HY, Zhang G, Cheng QY, Chen B, Cai JF, Wang XJ, et al. Expression and mutation of the c-kit gene and correlation with prognosis of small cell lung cancer. Oncol Lett 2012;4:89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Micke P, Basrai M, Faldum A, Bittinger F, Ronnstrand L, Blaukat A, et al. Characterization of c-kit expression in small cell lung cancer: prognostic and therapeutic implications. Clin Cancer Res 2003;9:188–94. [PubMed] [Google Scholar]
- 45. Rohr UP, Rehfeld N, Pflugfelder L, Geddert H, Müller W, Steidl U, et al. Expression of the tyrosine kinase c-kit is an independent prognostic factor in patients with small cell lung cancer. Int J Cancer 2004;111:259–63. [DOI] [PubMed] [Google Scholar]
- 46. Albain KS, Crowley JJ, Livingston RB. Long-term survival and toxicity in small cell lung cancer. Expanded Southwest Oncology Group experience. Chest 1991;99:1425–32. [DOI] [PubMed] [Google Scholar]
- 47. Nakazawa K, Kurishima K, Tamura T, Kagohashi K, Ishikawa H, Satoh H, et al. Specific organ metastases and survival in small cell lung cancer. Oncol Lett 2012;4:617–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Denny SK, Yang D, Chuang CH, Brady JJ, Lim JS, Gruner BM, et al. Nfib Promotes metastasis through a widespread increase in chromatin accessibility. Cell 2016;166:328–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Semenova EA, Kwon MC, Monkhorst K, Song JY, Bhaskaran R, Krijgsman O, et al. Transcription factor NFIB is a driver of small cell lung cancer progression in mice and marks metastatic disease in patients. Cell Rep 2016;16:631–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wu N, Jia D, Ibrahim AH, Bachurski CJ, Gronostajski RM, MacPherson D. NFIB overexpression cooperates with Rb/p53 deletion to promote small cell lung cancer. Oncotarget 2016;7:57514–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yang D, Denny SK, Greenside PG, Chaikovsky AC, Brady JJ, Ouadah Y, et al. Intertumoral heterogeneity in SCLC is influenced by the cell type of origin. Cancer Discov 2018;8:1316–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Dooley AL, Winslow MM, Chiang DY, Banerji S, Stransky N, Dayton TL, et al. Nuclear factor I/B is an oncogene in small cell lung cancer. Genes Dev 2011;25:1470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bramhecha YM, Guérard KP, Rouzbeh S, Scarlata E, Brimo F, Chevalier S, et al. Genomic gain of 16p13.3 in prostate cancer predicts poor clinical outcome after surgical intervention. Mol Cancer Res 2018;16:115–23. [DOI] [PubMed] [Google Scholar]
- 54. Sarbassov DD, Ali SM, Kim DH, Guertin DA, Latek RR, Erdjument-Bromage H, et al. Rictor, a novel binding partner of mTOR, defines a rapamycin-insensitive and raptor-independent pathway that regulates the cytoskeleton. Curr Biol 2004;14:1296–302. [DOI] [PubMed] [Google Scholar]
- 55. Rudin CM, Poirier JT, Byers LA, Dive C, Dowlati A, George J, et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat Rev Cancer 2019;19:289–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Baine MK, Hsieh MS, Lai WV, Egger JV, Jungbluth AA, Daneshbod Y, et al. SCLC subtypes defined by ASCL1, NEUROD1, POU2F3, and YAP1: a comprehensive immunohistochemical and histopathologic characterization. J Thorac Oncol 2020;15:1823–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Qu S, Fetsch P, Thomas A, Pommier Y, Schrump DS, Miettinen MM, et al. Molecular subtypes of primary SCLC tumors and their associations with neuroendocrine and therapeutic markers. J Thorac Oncol 2022;17:141–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mollaoglu G, Guthrie MR, Bohm S, Bragelmann J, Can I, Ballieu PM, et al. MYC drives progression of small cell lung cancer to a variant neuroendocrine subtype with vulnerability to aurora kinase inhibition. Cancer Cell 2017;31:270–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Schaefer T, Lengerke C. SOX2 protein biochemistry in stemness, reprogramming, and cancer: the PI3K/AKT/SOX2 axis and beyond. Oncogene 2020;39:278–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. McColl K, Wildey G, Sakre N, Lipka MB, Behtaj M, Kresak A, et al. Reciprocal expression of INSM1 and YAP1 defines subgroups in small cell lung cancer. Oncotarget 2017;8:73745–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dowlati A, Abbas A, Chan T, Henick B, Wang X, Doshi P, et al. Immune checkpoint blockade outcome in small-cell lung cancer and its relationship with retinoblastoma mutation status and function. JCO Precis Oncol 2022;6:e2200257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Duffy MJ, Synnott NC, O'Grady S, Crown J. Targeting p53 for the treatment of cancer. Semin Cancer Biol 2022;79:58–67. [DOI] [PubMed] [Google Scholar]
- 63. Levine AJ. The common mechanisms of transformation by the small DNA tumor viruses: the inactivation of tumor suppressor gene products: p53. Virology 2009;384:285–93. [DOI] [PubMed] [Google Scholar]
- 64. Moody CA, Laimins LA. Human papillomavirus oncoproteins: pathways to transformation. Nat Rev Cancer 2010;10:550–60. [DOI] [PubMed] [Google Scholar]
- 65. Knepper TC, Montesion M, Russell JS, Sokol ES, Frampton GM, Miller VA, et al. The genomic landscape of merkel cell carcinoma and clinicogenomic biomarkers of response to immune checkpoint inhibitor therapy. Clin Cancer Res 2019;25:5961–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gonzalez SL, Stremlau M, He X, Basile JR, Munger K. Degradation of the retinoblastoma tumor suppressor by the human papillomavirus type 16 E7 oncoprotein is important for functional inactivation and is separable from proteasomal degradation of E7. J Virol 2001;75:7583–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Fortes HR, von Ranke FM, Escuissato DL, Araujo Neto CA, Zanetti G, Hochhegger B, et al. Recurrent respiratory papillomatosis: a state-of-the-art review. Respir Med 2017;126:116–21. [DOI] [PubMed] [Google Scholar]
- 68. Bishop JA, Ogawa T, Chang X, Illei PB, Gabrielson E, Pai SI, et al. HPV analysis in distinguishing second primary tumors from lung metastases in patients with head and neck squamous cell carcinoma. Am J Surg Pathol 2012;36:142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Sanchez-Cespedes M, Parrella P, Esteller M, Nomoto S, Trink B, Engles JM, et al. Inactivation of LKB1/STK11 is a common event in adenocarcinomas of the lung. Cancer Res 2002;62:3659–62. [PubMed] [Google Scholar]
- 70. Ji H, Ramsey MR, Hayes DN, Fan C, McNamara K, Kozlowski P, et al. LKB1 modulates lung cancer differentiation and metastasis. Nature 2007;448:807–10. [DOI] [PubMed] [Google Scholar]
- 71. Skoulidis F, Goldberg ME, Greenawalt DM, Hellmann MD, Awad MM, Gainor JF, et al. STK11/LKB1 mutations and PD-1 inhibitor resistance in KRAS-mutant lung adenocarcinoma. Cancer Discov 2018;8:822–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Kim HS, Mendiratta S, Kim J, Pecot CV, Larsen JE, Zubovych I, et al. Systematic identification of molecular subtype-selective vulnerabilities in non–small-cell lung cancer. Cell 2013;155:552–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Chen Z, Cheng K, Walton Z, Wang Y, Ebi H, Shimamura T, et al. A murine lung cancer co-clinical trial identifies genetic modifiers of therapeutic response. Nature 2012;483:613–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Cardnell RJ, Feng Y, Mukherjee S, Diao L, Tong P, Stewart CA, et al. Activation of the PI3K/mTOR pathway following PARP inhibition in small cell lung cancer. PLoS One 2016;11:e0152584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Momcilovic M, Shackelford DB. Targeting LKB1 in cancer - exposing and exploiting vulnerabilities. Br J Cancer 2015;113:574–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Marcoux N, Gettinger SN, O'Kane G, Arbour KC, Neal JW, Husain H, et al. EGFR-mutant adenocarcinomas that transform to Small-cell lung cancer and other neuroendocrine carcinomas: clinical outcomes. J Clin Oncol 2019;37:278–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Offin M, Chan JM, Tenet M, Rizvi HA, Shen R, Riely GJ, et al. Concurrent RB1 and TP53 alterations define a subset of EGFR-mutant lung cancers at risk for histologic transformation and inferior clinical outcomes. J Thorac Oncol 2019;14:1784–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lee MC, Cai H, Murray CW, Li C, Shue YT, Andrejka L, et al. A multiplexed in vivo approach to identify driver genes in small cell lung cancer. Cell Rep 2023;42:111990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. McFadden DG, Papagiannakopoulos T, Taylor-Weiner A, Stewart C, Carter SL, Cibulskis K, et al. Genetic and clonal dissection of murine small cell lung carcinoma progression by genome sequencing. Cell 2014;156:1298–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Cui M, Augert A, Rongione M, Conkrite K, Parazzoli S, Nikitin AY, et al. PTEN is a potent suppressor of small cell lung cancer. Mol Cancer Res 2014;12:654–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Thomas PL, Madubata CJ, Aldrich MC, Lee MM, Owonikoko TK, Minna JD, et al. A call to action: dismantling racial injustices in preclinical research and clinical care of black patients living with small cell lung cancer. Cancer Discov 2021;11:240–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst 2005;97:339–46. [DOI] [PubMed] [Google Scholar]
- 83. Chen J, Yang H, Teo ASM, Amer LB, Sherbaf FG, Tan CQ, et al. Genomic landscape of lung adenocarcinoma in East Asians. Nat Genet 2020;52:177–86. [DOI] [PubMed] [Google Scholar]
- 84. Loree JM, Anand S, Dasari A, Unger JM, Gothwal A, Ellis LM, et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol 2019;5:e191870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Myer PA, Lee JK, Madison RW, Pradhan K, Newberg JY, Isasi CR, et al. The genomics of colorectal cancer in populations with African and European ancestry. Cancer Discov 2022;12:1282–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lord BD, Martini RN, Davis MB. Understanding how genetic ancestry may influence cancer development. Trends Cancer 2022;8:276–9. [DOI] [PubMed] [Google Scholar]
- 87. Adib E, Nassar AH, Abou Alaiwi S, Groha S, Akl EW, Sholl LM, et al. Variation in targetable genomic alterations in non-small cell lung cancer by genetic ancestry, sex, smoking history, and histology. Genome Med 2022;14:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Frampton GM, Fichtenholtz A, Otto GA, Wang K, Downing SR, He J, et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat Biotechnol 2013;31:1023–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med 2017;9:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sun JX, He Y, Sanford E, Montesion M, Frampton GM, Vignot S, et al. A computational approach to distinguish somatic vs. germline origin of genomic alterations from deep sequencing of cancer specimens without a matched normal. PLoS Comput Biol 2018;14:e1005965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sivakumar S, Jin DX, Rathod R, Ross J, Cantley LC, Scaltriti M, et al. Genetic heterogeneity and tissue-specific patterns of tumors with multiple PIK3CA mutations. Clin Cancer Res 2023;29:1125–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al. A global reference for human genetic variation. Nature 2015;526:68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Connelly CF, Carrot-Zhang J, Stephens PJ, Frampton GM. Abstract 1227: somatic genome alterations in cancer as compared to inferred patient ancestry. Cancer Res 2018;78:1227. [Google Scholar]
- 94. Alexandrov LB, Kim J, Haradhvala NJ, Huang MN, Tian Ng AW, Wu Y, et al. The repertoire of mutational signatures in human cancer. Nature 2020;578:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Singal G, Miller PG, Agarwala V, Li G, Kaushik G, Backenroth D, et al. Association of patient characteristics and tumor genomics with clinical outcomes among patients with non-small cell lung cancer using a clinicogenomic database. JAMA 2019;321:1391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Bhateja P, Chiu M, Wildey G, Lipka MB, Fu P, Yang MCL, et al. Retinoblastoma mutation predicts poor outcomes in advanced non small cell lung cancer. Cancer Med 2019;8:1459–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Woodhouse R, Li M, Hughes J, Delfosse D, Skoletsky J, Ma P, et al. Clinical and analytical validation of FoundationOne liquid CDx, a novel 324-gene cfDNA-based comprehensive genomic profiling assay for cancers of solid tumor origin. PLoS One 2020;15:e0237802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Husain H, Pavlick DC, Fendler BJ, Madison RW, Decker B, Gjoerup O, et al. Tumor fraction correlates with detection of actionable variants across >23,000 circulating tumor DNA samples. JCO Precis Oncol 2022;6:e2200261. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: First-, second-, and third-line systemic therapy in the SCLC clinical cohort. Supplementary Table S2: Genes analyzed as part of this study. Supplementary Table S3: Prevalence of alterations in the genes analyzed. Supplementary Table S4: Prevalence of gene alterations in 81 cases with liquid biopsies. Supplementary Table S5: Chromosomal losses and gains in SCLC. Supplementary Table S6: TET2 loss of function alterations detected in SCLCs. Supplementary Table S7: Manual review of specific mutation subgroups in SCLCs. Supplementary Table S8: Patterns of gene alterations in SMARCA4 altered and wild-type tumors. Supplementary Table S9: Prevalence of gene alterations in rearrangement-positive SCLCs. Supplementary Table S10: Univariate analysis of association between gene alterations and overall surival in the clinical cohort of stage III/IV SCLC tumors. Supplementary Table S11: Patterns of tumor mutational burden based on site of biopsy. Supplementary Table 12: Summary of tumor purity and tumor mutational burden by biopsy site. Supplementary Table S13: Aneuploidy patterns based on site of biopsy. Supplementary Table S14: Comparison of gene alterations in each biopsy site against lung biopsies. Supplementary Table S15: Comparison of gene alterations in liver and brain metastases. Supplementary Table S16: Summary of PTEN alterations in brain and other biopsy sites. Supplementary Table S17: Patterns of co-occurrence and mutual exclusivity between gene alterations in the overall SCLC cohort. Supplementary Table S18: Patterns of gene alterations in TP53 and/or RB1 mutant and wild-type cohorts. Supplementary Table S19: Patterns of gene alterations in young and older patients with SCLC. Supplementary Table S20: Patterns of gene alterations in HPV positive and HPV negative tumors. Supplementary Table S21: Manual review of specific HPV+ SCLCs. Supplementary Table S22: Patterns of gene alterations in STK11 mutant and wild-type cohorts. Supplementary Table S23: Patterns of gene alterations in EGFR mutant and wild-type cohorts. Supplementary Table S24: EGFR kinase domain alterations identified in the overall SCLC cohort.
Figure S1: Patterns of tumor mutational burden across different ancestry groups. Figure S2: Spectrum of TP53 and RB1 mutations in SCLC. Figure S3: Gene alteration landscape detected from targeted sequencing of liquid biopsies. Figure S4: Chromosomal loss events are frequent in SCLC and are preferentially enriched for tumor suppressor genes. Figure S5: Hematoxylin & Eosin (H&E) staining for some representative SCLC tumors with rare genomic alterations. Figure S6: Gene alterations detected in SMARCA4-altered SCLC. Figure S7: SCLC tumors exhibit recurrent gene rearrangements with therapeutic potential. Figure S8: Trends of overall survival across different ancestry groups and stage in the clinical cohort. Figure S9: Examination of tumor purity and tumor mutational burden (TMB). Figure S10: Liver and Brain SCLC metastases are enriched for chromosomal arm-level gains compared to lung-biopsied SCLC tumors. Figure S11: SCLC tumors present with unique co-occurring and mutual exclusive patterns of gene alterations. Figure S12: SCLC tumors with wild-type TP53 and/or RB1 have a low tumor mutational burden. Figure S13: SCLC tumors with wild-type TP53 and/or RB1 present with specific gene alterations. Figure S14: A smoking-associated mutational signature is rare in TP53/RB1 WT SCLC tumors. Figure S15: TP53 and RB1 alterations are less frequent in never smokers. Figure S16: Patterns of overall survival based on TP53 and RB1 alteration status. Figure S17: TP53 and RB1 mutations are more frequent in older patients with SCLC. Figure S18: Gene alterations detected in HPV-positive SCLC. Figure S19: Examination of HPV subtypes and prevalence in TP53/RB1 mutant and wild-type SCLC tumors. Figure S20: EGFR-mutant SCLC tumors exhibit unique mutational signature profiles. Figure S21: No overall survival differences based on EGFR mutation status in SCLC. Figure S22: Putative transformed SCLC tumors from EGFR-mutant NSCLC are enriched for EGFR exon 19 deletions.
Data Availability Statement
The sequencing data generated in this study are derived from clinical samples. All consented data supporting the findings of this study that can be released are provided within the article and its supplementary files. Due to HIPAA requirements, we are not authorized to share underlying sequence data or individualized patient genomic data, which contain potentially identifying or sensitive patient information. Foundation Medicine, Inc. is committed to collaborative data analysis, and it has well-established and widely utilized mechanisms by which investigators can query its core genomic database of >600,000 deidentified sequenced cancers to obtain aggregated datasets. For more information and mechanisms of access to the Foundation Medicine, Inc. data in this study, please contact the corresponding authors or the Foundation Medicine, Inc. Data Governance Council at data.governance.council@foundationmedicine.com. You and your institution will be required to sign a data transfer agreement.