Abstract
The SARS-CoV-2 (COVID-19) pandemic has increased healthcare worker (HCW) susceptibility to mental illness. We conducted a meta-analysis to investigate the prevalence and possible factors associated with post-traumatic stress disorder (PTSD) symptoms among HCW during the COVID-19 pandemic. We searched PubMed, SCOPUS and EMBASE databases up to May 4th, 2022. We performed random effects meta-analysis and moderator analyses for the prevalence of PTSD-relevant symptoms and severe PTSD symptoms. We identified 1276 studies, reviewed 209 full-text articles, and included 119 studies (117,143 participants) with a total of 121 data points in our final analysis. 34 studies (24,541 participants) reported prevalence of severe PTSD symptoms. Approximately 25.2% of participants were physicians, 42.8% nurses, 12.4% allied health professionals, 8.9% auxiliary health professionals, and 10.8% “other”. The pooled prevalence of PTSD symptoms among HCWs was 34% (95% CI, 0.30–0.39, I2 >90%), and 14% for severe PTSD (95% CI, 0.11 - 0.17, I2 >90%). The introduction of COVID vaccines was associated with a sharp decline in the prevalence of PTSD, and new virus variants were associated with small increases in PTSD rates. It is important that policies work towards allocating adequate resources towards protecting the well-being of healthcare workers to minimize adverse consequences of PTSD.
Keywords: SARS-CoV-2, COVID-19, Pandemic, Healthcare workers, Post-stress distress, Mental health
1. Introduction
On March 11, 2020, the World Health Organization (WHO) declared COVID-19 as a pandemic (Cucinotta and Vanelli, 2020). As of September 2nd, 2022, there have been over 601 million reported cases and 6.4 million deaths due to the SARS-CoV2 coronavirus (“WHO Coronavirus Disease (COVID-19) Dashboard,” 2020). This unprecedented high exposure and risk of illness and death pose a long-term mental health burden for the public (Dutheil et al., 2021), and increase the demand for healthcare workers (HCW).
HCWs are facing a variety of unusual challenges. Frontline healthcare workers are dealing with infected patients, putting themselves at an increased risk of being infected, and in turn, putting their loved ones at risk too. Other challenges include shortages of personal protective equipment (PPE), changes in work hours, changing hospital practices, increased workload, uncertainty in managing a novel disease, and public un-cooperation to public health safety guidelines (Lai et al., 2020; Mehta et al., 2021). The culmination of these factors increases HCW susceptibility to psychological and mental illnesses including, but not limited to, burnout (Antonio A. Lasalvia et al., 2021), anxiety (Sahebi et al., 2021), depression (Sahebi et al., 2021), insomnia (Pappa et al., 2020), and post-traumatic stress disorder (PTSD) (d'Ettorre et al., 2021).
PTSD is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM–5-TR) as exposure to a traumatic event, accompanied by symptoms in four categories: intrusion, avoidance, negative changes in cognitions and mood, and changes in arousal and reactivity (American Psychiatric Association, 2022). Previous research demonstrates that prior infectious outbreaks such as the severe acute respiratory syndrome (SARS), 2009 novel influenza A (H1N1), and Middle East respiratory syndrome (MERS) increase the prevalence of PTSD in the HCW population (Preti et al., 2020). Recent systematic reviews also highlight increased rates of HCW PTSD during the COVID-19 pandemic (Benfante et al., 2020; d'Ettorre et al., 2021; Marvaldi et al., 2021; Preti et al., 2020; Sanghera et al., 2020). However, these studies only include studies from earlier stages of the pandemic, limiting the generalizability of the findings.
In this study, we performed a systematic review and meta-analysis of studies to assess current COVID-19 literature using validated survey tools to report the prevalence of PTSD symptoms and severe PTSD symptoms among healthcare workers. We selected studies using validated survey tools because validated survey tools have been used to report rates of PTSD symptoms among various populations. They also provide a specific list of symptoms with certain sensitivity and specificity for PTSD so that participants can easily follow. Furthermore, validated tools provide standardized scores, such as cut-off values for mild, moderate, and severe symptoms, allowing for comparison between studies using the same tools. We planned to include a larger pool of studies so that we would be able to perform several subgroup analyses to better understand which populations are more vulnerable and the global effects of this disease on healthcare workers. Including a larger pool of studies also allows us to report a more up-to-date prevalence due to more published research in later stages of the pandemic.
2. Methods
2.1. Search strategy and selection criteria
We conducted the study in accordance with the 2020 Preferred Reporting Items for Systematic Review and Meta-Analyses statement (PRISMA) (Page et al., 2021). We first performed a literature search of the PubMed, SCOPUS and EMBASE databases for COVID-19 related studies that assessed PTSD symptoms from January 1st, 2020 until May 4th, 2022.
We included prospective (randomized trials, quasi-randomized trials) and observational studies. We included all full-text English language studies focused on assessing PTSD symptoms in HCW using the Impact of Events - Revised Scale (IES-R) or the PTSD Checklist for the 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders (PCL-5) scales during the COVID-19 pandemic. We focused on these two scales because they are the most commonly used during cross-sectional studies and allow for consistency when comparing studies. Healthcare workers included physicians, nurses, allied health professions (non-physician and non-nurse healthcare providers such as physician assistants, pharmacists, laboratory and imaging personnel, rehabilitation professions, medical technologists, occupational and respiratory therapists, and emergency medical technicians), and hospital auxiliary staff (non-healthcare provider staff such as medical students, hospital administrative staff, custodial staff, security, and cafeteria staff). We excluded studies not reporting the prevalence of PTSD symptoms. We excluded all review studies, meta-analyses, case reports, non-English language studies, pediatric studies, letters to editors, unpublished studies, and abstract-only studies. We also excluded studies that used non-validated survey tools such as self-reported qualitative measures, and also excluded studies that did not use the IES-R or PCL-5 to assess PTSD symptoms. We screened the references of included studies for eligible studies, but we did not contact authors for additional details or data. We also scanned the website Retraction Watch website (retractionwatch.com) for potential retracted COVID-related studies that may have been included in our study and we did not find any.
We used Covidence (www.covidence.org; Melbourne, Australia) to manage our search, duplicates, and meta-analysis. Titles and abstracts were screened by two independent investigators. A third investigator adjudicated disagreements among investigators. Two agreements allowed an abstract to move to full text screening. Similarly, full texts required agreement between at least two investigators to move to the data extraction stage. Our protocol was approved by Prospero with the registration ID CRD42022330405 (“Post-traumatic stress in healthcare workers during the SARS-CoV-2 (COVID-19) pandemic: A systematic review and meta-analysis,” n.d.). The senior investigators (Dr. Pourmand) and the Corresponding authors (Dr. Quincy K Tran) have authored over two dozen systematic reviews and meta-analyses.
2.2. Search terms
The search terms used for our search were: (SARS-COV-2 OR COVID-19) AND (IES-R OR PCL).
2.3. Outcome measures
The primary outcome of interest was the prevalence of clinically relevant PTSD symptoms, which are defined as having mild, moderate or severe symptoms among healthcare workers during the COVID-19 Pandemic. Definitions of having symptoms in each of these categories are based on the validated tools’ cut-off points, and by definition of the authors of the studies. The secondary outcome was the prevalence of severe PTSD symptoms among HCW during the pandemic.
2.4. Quality assessment / heterogeneity
We evaluated study quality with the modified Newcastle Ottawa Scale (modified NOS) (Murad et al., 2018) due to the cross-sectional nature of all included studies. The NOS (Wells et al., 2014) has a maximum of 9 points based on 1) selection of the cohort, 2) comparability of the groups, and 3) quality of outcome. High quality is defined by a score of ≥7, moderate quality a score of 4–6, and low quality ≤ 3. The modified NOS has a maximum of 5 points for the same 3 domains, and thus studies are only able to achieve moderate quality due to inherent limitations of observational studies. Two independent researchers completed the modified NOS for each eligible study. Discrepancies were adjudicated as a group. Therefore, inter-raters’ agreement, and Kappa score, was not used to assess interrater agreement. We assessed heterogeneity with the I2 statistic, which measures the total variance of effect size between studies, not due to chance, from the true effect size. We also measured heterogeneity with the Cochrane's Q-statistic, which examines the null hypothesis that all studies would have similar effect with the true effect size.
2.5. Data extraction
We extracted the following data from each eligible study: study size, study duration, study setting, study month, percentages of participants (female, physicians, nurses, allied health professionals, auxiliary staff, HCW with COVID-19 patient contact), survey instrument and cut-offs used to assess clinically relevant PTSD symptoms and severity, total prevalence of PTSD symptoms, and prevalence of PTSD by severity of symptoms. We recorded data in a standardized Excel spreadsheet (Microsoft Corp, Redmond, Washington, USA). Two investigators extracted the data independently. We did not calculate interrater agreement and the Kappa score as any disagreements between 2 investigators were adjudicated and the results were reported per the group's consensus.
2.6. Statistical analysis
We performed random-effects meta-analysis to assess the prevalence of PTSD symptoms among health care workers, as reported by the study authors. We also performed sensitivity analysis, using one-study-removed random-effect meta-analysis of prevalence of PTSD symptoms. The one-study-removed meta-analysis performs a random-effect meta-analysis after systematically removing individual studies one-by-one. This one-study-removed meta-analysis shows if any individual study would heavily affect the overall effect size of the pooled population.
Since we anticipated heterogeneity, we performed subgroup analyses, using moderator analyses of categorical variables to identify potential sources of heterogeneity, and to compare the prevalence of PTSD symptoms among subgroups. For these subgroup analyses, we used study characteristics such as: regions of the World Health Organization (WHO) of study origin, month of study completion, participant survey setting (inpatient, outpatient, online or mixed settings), and types of survey tool (IES-R or PCL-5). Previous meta-analyses were not able to compare the prevalence of mental health problems due to COVID-19 between different countries due to limited literature, and cited this as a future direction for research once more literature is available because countries are affected differently (Dragioti et al., 2022; Sun et al., 2021). Given our up-to-date search, we anticipated sufficient literature to compare the prevalence between WHO regions to identify potential similarities or differences. We compared prevalence from studies with different months of study completion to contribute to our time-series analysis, which allowed us to draw correlations between changes in prevalence of PTSD symptoms and key events in the pandemic such as the availability of vaccines (Hidaka et al., 2021; Koltai et al., 2022). We compared survey tools because previous studies on the topic found differences between the results from IES-R and PCL-5 (Chen et al., 2022; Qi et al., 2022). Study setting was an important factor to look at because different departments are at varying risks of COVID-19, and hence might be more or less susceptible to PTSD symptoms (Prasad et al., 2021; Qi et al., 2022). We were interested in survey setting because different clinical settings are involved with treating COVID in different ways, and the type of survey tool was important because the IES-R and PCL-5 assess PTSD symptoms differently. Prior to categorizing subgroups, we performed histogram analysis of continuous variables and divided them into subgroups according to their frequency of distributions. A significant difference in prevalence between subgroups was determined with a p-value cutoff of 0.05.
To identify potential patients’ characteristics that may have been associated with the prevalence of PTSD symptoms, we performed exploratory multivariable meta-regression, using continuous variables. The continuous variables, as reported by study authors, were percentages of participants as: female, physicians, nurses, allied health professionals, auxiliary staff, and participants who had contacts with COVID-19 patients. To ensure adequate power for the multivariable regressions, we presented the regressions with the highest possible number of independent variables and the highest possible number of studies. We also conducted a time series analysis to compare the number of global COVID cases with the prevalence of PTSD symptoms for each month. We used the dataset titled “Number of cumulative cases of coronavirus (COVID-19) worldwide from January 22, 2020 to August 28, 2022, by day” from statista.com to obtain data on global COVID cases (“COVID-19 cumulative cases by day worldwide 2022,” n.d.). Monthly PTSD prevalence was obtained from our data extraction.
We did not perform publication bias assessment which estimates whether the missing studies would change an intervention's overall effect size. Our random-effect meta-analysis only measured the prevalence of PTSD symptoms, but not intervention, so publication bias assessment was not applicable (Borenstein, 2019).
We performed our random-effects meta-analysis, one-study-removed meta-analysis, multivariable meta-regression using Comprehensive Meta-Analysis (www.meta-analysis.com; Englewood, New Jersey, USA). Any variable with 2-sided p-value < 0.05 was considered statistically significant.
3. Results
3.1. Study description
We identified 1276 studies eligible for the title and abstract screening that matched our search criteria (Fig. 1 ). 209 articles continued to the full text screening stage, of which 119 studies were selected for inclusion in our meta-analysis with a total of 117,143 participants (Table 1A ). All 119 studies were cross-sectional observational studies (Agberotimi et al., 2020; Alah et al., 2021; Ali et al., 2020, 2022, 2021; Alonso et al., 2021; Alshehri and Alghamdi, 2021; Asnakew et al., 2021; Ayalew et al., 2022; Azoulay et al., 2021; Bassi et al., 2021; Benzakour et al., 2022; Bizri et al., 2022; Bonzini et al., 2022; Bulut et al., 2021; Caillet et al., 2020; Caliandro et al., 2022; Carmassi et al., 2022, 2021a, 2021b; Chang et al., 2022; Chan et al., 2021; Chatzittofis et al., 2021; Chaudhary et al., 2021; B. Chen et al., 2022; Cheng et al., 2020; Chen et al., 2021; Chew et al., 2020; Chowdhury et al., 2021; Civantos et al., 2020a, 2020b; Cortés-Álvarez and Vuelvas-Olmos, 2020; Costantini et al., 2022; Crowe et al., 2022; Demartini et al., 2020; Dobson et al., 2021; Dykes et al., 2022; Ergai et al., 2022; Essadek et al., 2022; Fattori et al., 2021; Geng et al., 2021; Gilleen et al., 2021; Gorini et al., 2020; Guo et al., 2021; Hajure et al., 2021; Hasanvandi et al., 2022; Honarmand et al., 2022; Hong et al., 2021; Huarcaya-Victoria et al., 2022; J. 2021; Ide et al., 2021; Ifthikar et al., 2021; Ilias et al., 2021; Jang et al., 2021; Jemal et al., 2021; Ji et al., 2021; Johnson et al., 2020; Jo et al., 2020; Juan et al., 2020; Kiefer et al., 2021; Kumar et al., 2021; Lamiani et al., 2021; Lange et al., 2022; Lasalvia et al., 2021; Lasalvia et al., 2022; Laurent et al., 2022; León Rojas et al., 2022; Li et al., 2021, 2020; Liu et al., 2021; Luceño-Moreno et al., 2020; Lum et al., 2021; Luo et al., 2021; Magalhaes et al., 2021; Manh Than et al., 2020; Marco et al., 2020; Marcomini et al., 2021; Martín et al., 2021; Meena et al., 2022; Mehta et al., 2022; Mirzaei et al., 2022; Moderato et al., 2021; Mulatu et al., 2021; Naheed et al., 2021; Nguyen et al., 2021; Nguyen et al., 2021; Ouyang et al., 2022; Pan et al., n.d.; Pappa et al., 2021; Prasad et al., 2020; Qiu et al., 2021; Ranieri et al., 2021; Riello et al., 2020; Robles et al., 2021; Rosenthal et al., 2021; Rouse and Regan, 2021; Sachdeva et al., 2021; Sahin et al., 2022; Sarapultseva et al., 2021; Shah et al., 2021; Sobregrau Sangrà et al., 2022; Styra et al., 2021; Tebbeb et al., 2022; Topal et al., 2021; Udgiri et al., 2021; Van Wert et al., 2022; Vlah Tomičević and Lang, 2021; Wadasadawala et al., 2021; Wang et al., 2020; Wanigasooriya et al., 2021; Xia et al., 2021; Yang et al., 2021; Yin et al., 2020; Yitayih et al., 2020; Zakeri et al., 2021; Zara et al., 2021; Zhang et al., 2021; Zhu et al., 2020). Two studies assessed PTSD at two separate times (Ouyang et al., 2022; Qiu et al., 2021), resulting in a total of 121 data points. All studies included the primary outcome of PTSD-relevant symptoms, with 34 studies also including the secondary outcome involving severe symptoms of PTSD. These 34 studies included a total of 24,541 participants who were eligible for our secondary outcome analysis. 83 studies assessed levels of PTSD symptoms in physicians (Table 1B ), with 85 studies investigating nurses, 51 studies including allied health workers, 24 studies investigating auxiliary staff, and 8 studies included participants that were not specified into a category of healthcare workers. 29 studies also did not specify any of their participants into a specific category of healthcare workers (i.e. physicians, nurses, auxiliary staff, allied health staff).
Fig. 1.
PRISMA flow diagram for study selection.
Table 1A.
Characteristics of studies included in the meta-analysis.
| Author, Country | Month & year of study completion | Length of study, days | Survey tools | Cut-off scores | Survey Settings | Study Quality (NOS) |
|---|---|---|---|---|---|---|
| Abed Alah, Qatar | December 2020 | 37 | IES-R | Clinical concern for PTSD: > 24 Best diagnostic accuracy for PTSD: >33 |
online | Medium (5) |
| Agberotimi, Nigeria | April 2020 | 30 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
online | Medium (4) |
| Ali, Ireland | June 2020 | 14 | IES-R | Clinical concern for PTSD: > 24 | online | Medium (5) |
| Ali, Kenya | November 2022 | 90 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
online | Medium (5) |
| Ali, Kenya | November 2020 | 90 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
online | Medium (5) |
| Alonso, Spain | September 2020 | 124 | PCL-5 | Current PTSD: ≥ 7 | online | Medium (5) |
| Alshehri, Saudi Arabia | NR | NR | PCL-5 | Diagnosis of PTSD: >31 | online | Medium (4) |
| Asnakew, Ethiopia | May 2020 | 60 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
NR | Medium (5) |
| Ayalew, Ethiopia | October 2020 | 30 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
Mixed | Medium (5) |
| Azoulay, France | December 2020 | 33 | IES-R | PTSD Symptoms: ≥ 26 | online | Medium (5) |
| Bassi, Italy | May 2020 | 18 | PCL-5 | Provisional PTSD Diagnosis: ≥ 33 | Online | Medium (5) |
| Benzakour, Switzerland | June 2020 | 83 | PCL-5 | Diagnosis of PTSD: >33 | online | Medium (4) |
| Bizri, Lebanon | May 2020 | 60 | IES-R | Clinical concern for PTSD: >24 Probable diagnosis of PTSD: >33 |
online | Medium (5) |
| Bonzini, Italy | July 2021 | 60 | IES-R | Probable diagnosis of PTSD: >33 | online | Medium (5) |
| Bulut, Turkey | NR | NR | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
Online | Medium (5) |
| Bulut, Turkey | NR | NR | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
Online | Medium (5) |
| Caillet, France | April 2020 | 13 | IES-R | Moderate and severe symptoms: > 33 | Inpatient | Medium (5) |
| Caliandro, Italy | May 2021 | 60 | IES-R | Significant PTSD symptoms: > 33 | NR | Medium (4) |
| Carmassi, Italy | June 2020 | 90 | IES-R | Severe PTSD symptoms: > 33 | mixed | Medium (5) |
| Carmassi, Italy | May 2020 | 60 | IES-R | PTSD: > 32 | NR | Medium (5) |
| Carmassi, Italy | May 2020 | 60 | IES-R | PTSD Diagnosis: > 32 | NR | Medium (5) |
| Chang, United States | January 2020 | 210 | PCL-5 | PTSD Diagnosis: >31 | online | Low (3) |
| Chan, Singapore | August 2020 | 60 | IES-R | Moderate to Severe PTSD Symptoms: >25 | online | Medium (5) |
| Chatzittofis, Cyprus | May 2020 | 25 | IES-R | Clinically relevant PTSD symptoms: > 33 |
online | Medium (5) |
| Chaudhary, Pakistan | July 2020 | 120 | IES-R | PTSD: >20 | outpatient | Medium (5) |
| Chen, China | March 2020 | 57 | IES-R | High Risk for PTSD: 20 | online | Medium (4) |
| Cheng, China | February 2020 | 24 | PCL-5 | Provisional Diagnosis for PTSD: > 33 | Online | Medium (5) |
| Chen, China | May 2020 | 63 | IES-R | PTSD Symptoms: ≥20 | NR | Medium (4) |
| Chew, Singapore & India | April 2020 | 58 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 Clinical concern for PTSD: > 24 |
NR | Medium (4) |
| Chowdhary, Bangladesh | December 2020 | 14 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 Clinical concern for PTSD: > 24 |
online | Medium (5) |
| Civantos, United States | April 2020 | 12 | IES-R | Mild: 9‐25 Moderate: 26‐43 Severe distress: 44‐75 Risk for PTSD: ≥ 27 |
Online | Medium (5) |
| Civantos, Brazil | May 2020 | 18 | IES-R | Clinical concern: 24–32 Probable PTSD: 33–36 Probable PTSD with immune suppression: 37–88 |
Online | Medium (5) |
| Cortés-Álvarez, Mexico | June 2020 | 11 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 Clinical concern for PTSD: > 24 |
online | Medium (4) |
| Constantini, Italy | June 2022 | 7 | IES-R | Probable PTSD: > 50 | online | Medium (5) |
| Crowe, Canada | June 2021 | 61 | IES-R | Some PTSD symptoms: 24 - 32 Probable Diagnosis of PTSD: 33 - 36 Significant PTSD symptoms: < 37 |
online | Medium (5) |
| Demartini, Italy | March 2020 | 7 | IES-R | Some PTSD symptoms: 24 - 32 Probable Diagnosis of PTSD: 33 - 36 Significant PTSD symptoms: < 37 At risk for PTSD: >33 |
online | Medium (4) |
| Dobson, Australia | May 2020 | 28 | IES-R | NR | Mixed | Medium (5) |
| Dykes, United Kingdom | July 2020 | 21 | IES-R | Suggestive of PTSD: 12–32 Diagnosis of PTSD (IES-R ≥ 33) |
NR | Medium (4) |
| Ergai, United States | October 2020 | 136 | IES-R | Extreme Distress: ≥33 | online | Medium (5) |
| Essadek, France | April 2020 | 4 | IES-R | PTSD: ≥ 26 | online | Medium (5) |
| Fattori, Italy | December 2020 | 152 | IES-R | PTSD: ≥ 33 | NR | Medium (5) |
| Geng, China | June 2020 | 14 | PCL-5 | PTSD: > 33 | online | Medium (5) |
| Gilleen, United Kingdom | May 2020 | 19 | IES-R | High PTSD symptoms: ≥ 26 | Online | Medium (5) |
| Gorini, Italy | May 2020 | 30 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: > 37 |
Online | Medium (5) |
| Guo, China | February 2020 | 9 | IES-R | Significant Mental Stress: > 34 | online | Medium (4) |
| Hajure, Ethiopia | May 2020 | 15 | IES-R | Subclinical PTSD: 0–8 Mild PTSD: 9–25 Moderate PTSD: 26–43 Severe PTSD: 44–88 PTSD cut-off score: > 33 |
mixed | Medium (5) |
| Hassanvandi, Iran | July 2020 | 61 | PCL-5 | PTSD: ≥33 | online | Medium (5) |
| Honarmand, Canada | September 2020 | 92 | IES-R | PTSD is a clinical concern: 24 - 32 Probable diagnosis of PTSD: ≥33 Scores high enough to suppress immune functioning: ≥37 |
online | Medium (4) |
| Hong, China | March 2020 | 66 | IES-R | PTSD Symptoms ≥ 20 | outpatient | Medium (5) |
| Huarcaya-Victoria, Peru | May 2020 | 16 | IES-R | Mild: (9–25) Moderate: 26–43 Severe: 44–88 |
online | Medium (4) |
| Huarcaya-Victoria, Peru | April 2020 | 13 | IES-R | Mild: 9–25 Moderate: 26–43 Severe (44–88) |
online | Medium (4) |
| Ide, Japan | April 2020 | 14 | IES-R | PTSD Symptoms: > 24 | Mixed | Medium (4) |
| Ifthikar, Saudi Arabia | August 2020 | 63 | IES-R | Clinical Concern for PTSD: 24–32 Probable PTSD: 33–36 Severe PTSD: > 37 |
online | Medium (4) |
| Ilias, Greece | June 2020 | 6 | IES-R | PTSD: > 33 | Mixed | Medium (5) |
| Jang, Korea | March 2020 | 14 | IES-R | PTSD ≥ 25 | NR | Medium (5) |
| Jemal, Ethiopia | July 2020 | 31 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: ≥ 44 |
Mixed | Medium (5) |
| Ji, China | March 2020 | 15 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
online | Medium (5) |
| Jo, South Korea | May 2020 | 14 | IES-R | High-risk for PTSD: > 25 | Inpatient | Medium (5) |
| Johnson, Norway | April 2020 | 7 | PCL-5 | Subclinical PTSD: > 22 PTSD Diagnosis: > 31 |
online | Medium (5) |
| Juan, China | February 2020 | 14 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
Inpatient | Medium (5) |
| Kiefer, United States | October 2020 | 13 | IES-R | PTSD Symptoms: ≥ 24 | online | Medium (5) |
| Kumar, Pakistan | December 2020 | 150 | IES-R | Clinical concern for PTSD: > 24 Probable Diagnosis of PTSD: 33 - 36 Diagnosis of PTSD: ≥37 |
online | Medium (4) |
| Lamiani, Italy | October 2020 | 91 | PCL-5 | Mild PTSD: 12 - 30 Probable PTSD: ≥31 |
online | Medium (4) |
| Lange, France | April 2020 | NR | IES-R | PTSD Symptoms ≥ 33 | online | Medium (4) |
| Lasalvia, Italy | May 2020 | 16 | IES-R | PTSD Symptoms ≥ 24 | online | Medium (5) |
| Lasalvia, Italy | May 2020 | 15 | IES-R | PTSD symptoms ≥ 24 | online | Medium (5) |
| Laurent, Italy | July 2020 | 34 | IES-R | PTSD Symptoms ≥ 33 | online | Medium (5) |
| LeónRojas, Mexico | July 2020 | 60 | PCL-5 | PTSD Symptoms ≥ 33 | online | Medium (5) |
| Li, China | NR | NR | IES-R | Subclinical PTSD: 0–8 Mild PTSD: 9–25 Moderate PTSD: 26–43 Severe PTSD: 44–88 |
online | Medium (5) |
| Liu, China | February 2020 | 6 | IES-R | PTSD Symptoms: >20 | online | Medium (5) |
| Li, China | April 2020 | 3 | IES-R | Clinical Concern for PTSD: >24 | online | Medium (4) |
| Luceno-Moreno, Spain | April 2020 | 30 | IES-R | Diagnosis of PTSD: > 20 | Mixed | Medium (5) |
| Lum, Singapore | September 2020 | 180 | IES-R | At Risk for PTSD: >24 | mixed | Medium (5) |
| Luo, China | February 2020 | 14 | IES-R | Mild: 9–25 Moderate: 26–44 Moderately Severe: > 44 |
online | Medium (5) |
| Magalhaes, United States | August 2020 | 90 | IES-R | NR | online | Medium (5) |
| ManhThan, Vietnam | April 2020 | NR | IES-R | Clinical Concern for PTSD: >24 | NR | Medium (4) |
| Marco, United States | June 2020 | 32 | PCL-5 | PTSD: >33 | online | Medium (5) |
| Marcomini, Italy | September 2020 | 90 | IES-R | Probable PTSD Diagnosis: >33 | mixed | Medium (5) |
| Martin, Spain | NR | 180 | IES-R | Mild: 9‐25 Moderate: 26‐43 Severe: 44‐88 |
online | Medium (4) |
| Meena, India | June 2021 | 120 | IES-R | Clinical Relevance for PTSD: >24 | mixed | Medium (5) |
| Mehta, Canada | August 2020 | 90 | IES-R | Clinical Concern for PTSD: 24–32 Probable PTSD: ≥ 33 |
online | Medium (5) |
| Mirzaei, Iran | August 2020 | 90 | IES-R | Moderate PTSD: 18–24 Full PTSD: >24 |
online | Medium (5) |
| Moderato, Italy | April 2020 | 14 | IES-R | PTSD: >33 | online | Medium (4) |
| Mulatu, Ethiopia | August 2020 | 30 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 Diagnosis of distress: ≥33 |
mixed | Medium (5) |
| Naheed, Pakistan | July 2020 | 180 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
mixed | Medium (5) |
| Nguyen, Vietnam (a) | May 2020 | 20 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: >37 |
online | Medium (5) |
| Nguyen, Vietnam (b) | April 2020 | 22 | IES-R | Clinical Concern for PTSD: 24–32 PTSD: 33–36 Severe PTSD: ≥ 37 |
online | Medium (5) |
| Ouyang, China | June 2020 | 60 | PCL-5 | Significant PTSD: > 33 | mixed | Medium (5) |
| Ouyang, China | June 2021 | 365 | PCL-5 | Significant PTSD: > 33 | mixed | Medium (5) |
| Pan, China | December 2020 | 60 | PCL-5 | Probable PTSD: ≥ 33 | online | Medium (5) |
| Pappa, Greece | June 2020 | NR | IES-R | Mild (24–32) Moderate (33–36) Severe (>37) PTSD of clinical conern: > 24 |
Online | Medium (5) |
| Prasad, United States | April 2020 | 12 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–75 |
Mixed | Medium (5) |
| Qiu, China | February 2020 | 7 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
mixed | Medium (5) |
| Qiu, China | June 2020 | 11 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
mixed | Medium (5) |
| Ranieri, Italy | September 2020 | 210 | IES-R | Concern for PTSD: >33 | mixed | Medium (5) |
| Riello, Italy | July 2020 | 11 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 |
Outpatient | Medium (5) |
| Robles, Mexico | May 2020 | 21 | PCL-5 | NR | Online | Medium (5) |
| Rosenthal, United States | NR | NR | IES-R | Clinical concern for PTSD: > 24 Probable Diagnosis of PTSD: > 33 Severe PTSD: >37 |
online | Medium (5) |
| Rouse, Ireland | June 2020 | NR | IES-R | Mild: 24–32 Moderate: 33–36 Severe: 37–88 |
online | Medium (5) |
| Sachdeva, India | NR | NR | IES-R | Concern for PTSD: >24 | mixed | Medium (5) |
| Sahin, Turkey | May 2020 | 31 | IES-R | Mild: 9–25 Moderate: 26–43 Severe: 44–88 PTSD: > 24 |
online | Medium (5) |
| Sarapultseva, Russia | September 2020 | 20 | IES-R | Mild: 24–32 Moderate: 33–36 Severe: 37–88 |
outpatient | Medium (5) |
| Shah, Kenya | Nov 2020 | 30 | IES-R | Mild: 9–23 Moderate: 24–32 Severe: >33 |
Mixed | Medium (5) |
| SobregrauSangrà, Spain | October 2020 | 120 | PCL-5 | Severe, suspected PTSD: >30 | Mixed | Medium (5) |
| Styra, Canada | July 2020 | 15 | IES-R | Mild: 9–23 Moderate: 24–32 Severe Distress: >33 |
online | Medium (5) |
| Tebbeb, France | May 2021 | 66 | PCL-5 | PTSD: > 38 | outpatient | Medium (5) |
| Topal, Turkey | October 2020 | 300 | PCL-5 | NR | inpatient | Medium (5) |
| Udgiri, India | NR | NR | IES-R | Clinical Concern for PTSD: >24 Probable PTSD: > 33 Severe PTSD: > 37 |
online | Medium (5) |
| VanWert, United States | Nov 2020 | 90 | IES-R | Clinical Concern for PTSD: ≥ 22 | online | Medium (5) |
| VlahTomičević, Croatia | May 2020 | 15 | IES-R | Clinical Concern for PTSD: 24–32 Probable PTSD: 33–36 Diagnosis of PTSD: 37–88 |
online | Medium (5) |
| Wadasadawala, Bangladesh, India, Indonesia and Nepal | July 2020 | 90 | IES-R | Clinical concern for PTSD: >24 PTSD | Mixed | Medium (5) |
| Wang, China | Feb 2020 | 10 | IES-R | Distress: >44 | online | Medium (5) |
| Wanigasooriya, United Kingdom | July 2020 | 56 | IES-R | Probable PTSD: > 33 | Mixed | Medium (5) |
| Xia, China | Feb 2020 | 13 | PCL-5 | Probable PTSD: > 33 | online | Medium (5) |
| Yang, China | April 2020 | 30 | PCL-5 | PTSD: ≥ 31 | online | Medium (5) |
| Yin, China | Feb 2022 | 5 | PCL-5 | PTSD: > 33 | online | Medium (5) |
| Yitayih, Ethiopia | March 2020 | 7 | IES-R | Mild: 9–25 Moderate: 26–44 Severe: >46 |
Mixed | Medium (5) |
| Zakeri, Iran | April 2020 | 30 | IES-R | PTSD: > 33 points | inpatient | Medium (5) |
| Zara, Italy | June 2020 | 38 | IES-R | NR | online | Medium (5) |
| Zhang, China | March 2021 | 33 | IES-R | PTSD: > 33 | online | Medium (5) |
| Zhu, China | Feburary 2020 | 3 | IES-R | PTSD: > 33 | online | Medium (5) |
Abbreviations: IES-R= Impact of Event Scale-Revised, PCL=Posttraumatic Stress Disorder Checklist, NOS = The Newcastle-Ottawa Scale, NR = Not Reported.
Table 1B.
Participant demographics from studies included in meta-analysis.
| Author, Country | Study Sample Size, (n) | Symptoms of PTSD, n (%) | Symptoms of PTSD by Severity, n (%) | Female, n (%) | Categories of Participants, n (%) | Contact with COVID-19 Patients n (%) |
|---|---|---|---|---|---|---|
| Abed Alah, Qatar | 394 | 73 (18.5) | Clinical Concern for PTSD: 35 (8.9) Diagnosis of PTSD: 38 (9.6) |
0 (0) | Physician: 101 (25.6) Nurse: 181 (45.9) Allied Health: 112 (28.4) |
280 (71.1) |
| Agberotimi, Nigeria | 382 | 201 (52.6) | NR | 169 (44.2) | NR | NR |
| Ali, Ireland | 472 | 213 (45.13) | NR | 326 (69) | Physician: 19.28 (91) Nurse: 29.03 (137) Allied Health: 194 (41.1) Auxillary: 82 (17.4) |
57.63 (272) |
| Ali, Kenya | 100 | 34 (34) | Mild: 13 (13.5%) Moderate: 3 (3.1%) Severe: 18 (18.8%) |
53 (53) | Physicians: 100 (100) | 66 (66) |
| Ali, Kenya | 171 | 48 (27.1) | Mild: 19 (11.4%) Moderate: 9 (5.4%) Severe: 20 (12.0%) |
120 (70.2) | Nurses 171 (100) | 111 (64.9) |
| Alonso, Spain | 9138 | 1946 (22.2) | NR | 7372 (80.7) | Physician: 2953 (26.4) Nurse: 2746 (30.6) Allied Health: 1841 (22.8) Auxiliary: 1598 (20.3) |
4180 (43.6) |
| Alshehri, Saudi Arabia | 404 | 60 (14.9) | NR | 218 (54) | Physician: 86 (21.3) Nurse: 119 (29.5) Allied health: 111 (27.5) Others: 89 (22) |
192 (47.5) |
| Asnakew, Ethiopia | 396 | 219 (55.1) | Severe: 108 (23.5) | 122 (30.8) | Physician: 77 (19.4) Nurse: 230 (58.1) Allied Health: 89 (22.5) |
NR |
| Ayalew, Ethiopia | 387 | 220 (56.8) | Mild: 50 (12.9) Moderate: 28 (7.8) Severe: 142 (36.7) |
160 (41.3) | Physician: 88 (22.7) Nurses: 197 (50.9) Others: 102 (26.4) |
NR |
| Azoulay, France | 845 | 240 (28.4) | NR | 571 (67.5%) | Physician: 272 (32.2) Nurse: 412 (48.7) Allied Health: 161 (19.1) |
845 (100) |
| Bassi, Italy | 653 | 260 (39.8) | NR | 482 (73.8) | Physician: 189 (28.9) Nurse: 318 (48.7) Allied Health: 146 (22.4) |
261 (40) |
| Benzakour, Switzerland | 25 | 7 (38.9) | NR | 14 (77.8) | Physician: 2 (11.1) Nurse: 9 (50) Allied Health: 4 (22.2) Auxillary: 6 (24) |
13 (72.2) |
| Bizri, Lebanon | 150 | 45 (30.0) | NR | 84 (56) | Post-graduate trainee/clinical fellow/senior attending physician 94 (62.7) Registered nurse 56 (37.3) |
42 (28) |
| Bonzini, Italy | 990 | 192 (19.4) | NR | 693 (70) | Physician: 233 (23.5) Nurse: 416 (42) Allied Health: 63 (6.5) Auxillary: 119 (12) Others: 159 (16) |
446 (45) |
| Bulut, Turkey | 348 | 134 (38.5) | Mild: 109 (31.3) Moderate: 54 (15.5) Severe: 80 (23) |
176 (50.6) | Physician: 190 (54.6) Nurse: 158 (45.4) |
348 (100) |
| Bulut, Turkey | 159 | 87 (45.3%) | NR | 0 (0) | Physician: 102 (64.2) Nurse: 57 (35.8) |
159 (100) |
| Caillet, France | 208 | 52 (25) | NR | 156 (75) | Physician: 17 (8) Nurse: 99 (47.6) Allied Health: 62 (30.3) Auxillary: 25 (12) |
150 (73) |
| Caliandro, Italy | 26 | 9 (33) | NR | 19 (73) | Physician: 9 (34.6) Nurse: 3 (11.5) Allied Health: 9 (36) Auxillary: 5 (19.2) |
NR |
| Carmassi, Italy | 514 | 121 (24.5) | NR | 292 (56.8) | Physician: 183, (35.6) Nurse: 251 (48.8) Other: 80 (15.6) |
514 (100) |
| Carmassi, Italy | 265 | 47 (17.7) | NR | 181 (68.3) | Physician: 85 (32.1) Nurse: 133 (50.2) Allied Health: 47 (17.7) |
NR |
| Carmassi, Italy | 74 | 23 (31) | NR | 47 (63.5) | Physician: 18 (24.3) Other: 56 (75.7) |
46 (62.2) |
| Chang, United States | 31 | 11 (35) | At risk for PTSD: 2 (6.5) Diagnosis of PTSD: 11 (35) |
NR | Physician: 31 (100) | NR |
| Chan, Singapore | 789 | 199 (25.2) | NR | 589 (74.7) | Physician: 305 (8.4) Nurse: 1870 (51.7) Allied health: 677 (18.7) Administrative: 739 (20.4) |
404 (11.2) |
| Chatzittofis, Cyprus | 424 | 62 (15) | Severe: 8 (1.9) | 248 (58) | Physician: 178 (42) Nurse: 103 (24) Allied Health: 75 (18) Other: 68 (16) |
8 (1.9) |
| Chaudhary, Pakistan | 392 | 55 (14) | NR | 176 (45) | Dentist: 254 (64.8) Allied Health: 138 (35.2) |
NR |
| Chen, China | 422 | 302 (71.6) | NR | NR | NR | NR |
| Cheng, China | 212 | 125 (59) | NR | 103 (48.6) | Physician: 190 (89.6) Allied Health: 22 (10.4) |
212 (100) |
| Chen, China | 597 | 270 (45.2) | NR | 525 (87.94) | Doctor: 41 (6.87) Nurse: 549 (91.96) Other: 7 (1.17) |
322 (54) |
| Chew, Singapore & India | 906 | 67 (7.4) | Moderate to Severe PTSD: 34 (3.8) | 583 (64.3) | Physician: 268 (29.6) Nurse: 355 (39.2) Allied Health: 136 (15) Auxillary: 147 (16.2) |
NR |
| Chowdhary, Bangladesh | 547 | 338 (61.9) | Normal 209 (38.2) Mild 113 (20.7) Moderate 49 (9) Severe 176 (32.2) |
361 (66) | Nurse: 547 (100) | 226 (41.3) |
| Civantos, United States | 349 | 96 (28) | Mild: 14, (32.7) Moderate: 73 (20.9) Severe: 23 (6.6) |
137 (39.3) | Physicians: 349 (100) | NR |
| Civantos, Brazil | 163 | 32 (20) | Clinical concern: 11, (6.7) Probable PTSD: 8 (4.9) Probable PTSD with immune suppression: 24 (14.7) |
42 (25.8) | Physicians: 163 (100) | NR |
| Cortés-Álvarez, Mexico | 462 | 365 (79) | Mild: 149 (32.3) Moderate to Severe: 216 (46.7) |
356 (77.1) | Nurse: 462 (100) | 348 (75.3) |
| Constantini, Italy | 237 | 8 (8.4) | NR | 206 (86.9) | Physician: 237 (100) | 46 (21.9) |
| Crowe, Canada | 425 | 316 (74.4) | NR | 384 (92.5) | Nurse: 425 (100) | NR |
| Demartini, Italy | 123 | 23 (18.7) | NR | 97 (78.9) | NR | 49 (39.9) |
| Dobson, Australia | 320 | 246 (77) | Severe: 5 (1.6) | 248 (78.5) | Physicians: 99 (31) Nurse: 84 (26) Allied Health: 105 (33) Auxiliary: 28 (9) |
121 (38.7) |
| Dykes, United Kingdom | 131 | 37 (28.2) | Suggestive of PTSD: 57 (43.5) PTSD Diagnosis: 37 (28.2) |
97 (74) | Physician: 43 (32.8) Nurse: 69 (52.7) Allied Health: 14 (10.7) Auxillary: 5 (3.8) |
NR |
| Ergai, United States | 388 | 153 (39.4) | NR | 348 (89.7) | Admin 49 (12.6) Ethicists 25 (6.4) Radiology 33 (8.5) RN 212 (54.6) Others (Physician, PA, tech, lab, pharmacy, dietician, PT) 68 (17.5) |
NR |
| Essadek, France | 668 | 246 (36.8) | NR | 500 (74.9) | Auxillary: 668 (100) | 237 (35.5) |
| Fattori, Italy | 550 | 121 (22) | NR | 353 (46) | Physician: 164 (29) Nurse: 222 (40) Allied Health: 89 (16.2) Auxillary: 75 (13.6) |
NR |
| Geng, China | 317 | 34 (10.7) | NR | 221 (69.7) | Physician: 140 (44.2) Nurse: 144 (45.4) Others: 33 (10.4) |
NR |
| Gilleen, United Kingdom | 2773 | 404 (14.6) | Severe: 426 (15.36) | 2365 (85.29) | Physician: 386 (13.9) Nurse: 852 (30.7) Allied Health: 772 (27.8) Auxiliary: 245 (8.8) Other: 499 (18) NR: 19 (0.7) |
1224 (44.1) |
| Gorini, Italy | 650 | 290 (44.6) | Mild:104 (16.1) Moderate: 36 (5.6) Severe: 150 (23.2) |
439 (67.5) | Physicians: 177 (27.2) Nurses: 214 (32.9) Allied Health: 217 (33.4) Auxiliary: 42 (6.5) |
395 (60.8) |
| Guo, China | 610 | 481 (78.9) | NR | 464 (76.1) | Physician: 164 (26.9) Nurse: 446 (73.1) |
610 (100) |
| Hajure, Ethiopia | 127 | 51 (40.2) | Subclinical: 14 (11) Mild: 47 (37) Moderate: 37 (29) Severe: 28 (22) |
41 (32.3) | NR | NR |
| Hassanvandi, Iran | 180 | 93 (51.7) | NR | 129 (71.7) | NR | 122 (67.8) |
| Honarmand, Canada | 849 | 423 (49.8) | Clinical concern: 424 (50) Probable PTSD: 83 (9.8) ≥37: 204 (24) |
NR | NR | NR |
| Hong, China | 102 | 6 (5.9) | NR | 77 (75.5) | Physician: 40 (39.2) Nurse: 54 (52.9) Allied Health: 8 (7.8) |
93 (91.2) |
| Huarcaya-Victoria, Peru | 1238 | NR | Mild: 454 (37) Moderate: 216 (17) Severe: 133 (11) |
848 (68.5) | Auxillary: 1238 (100) | NR |
| Huarcaya-Victoria, Peru | 310 | NR | Mild: 83 (26.8) Moderate: 21 (6.8) Severe: 9 (2.9) |
149 (48.1) | Physician: 310 (100) | 196 (63.2) |
| Ide, Japan | 2697 | 189 (7) | NR | 1995 (74.0) | Physician: 555 (20.6) Nurse: 1045 (38.7) Allied Health: 359 (13.3) Auxillary: 738 (27.4) |
328 (12.2) |
| Ifthikar, Saudi Arabia | 309 | 173 (56) | Clinical Concern for PTSD: 57 (18.4) Probable PTSD: 27 (8.6) Severe PTSD: 89 (29) |
225 (72.6) | Auxillary: 309 (100) | NR |
| Ilias, Greece | 162 | 162 (35) | NR | 125 (77) | Physician: 43 (27) Nurse: 102 (63) Allied Health: 17 (10) |
NR |
| Jang, Korea | 99 | 27 (27.6) | NR | 52 (52.5) | Physician: 5 (5.05) Nurse: 71 (71.7) Allied Health: 23 (23.2) |
22 (22.2) |
| Jemal, Ethiopia | 417 | NR | Mild: 55 (13.2) Moderate: 48 (11.5) Severe: 20 (4.8) |
138 (33.1) | Doctor: 55.5 (13.3) Nurse: 103.8 (24.9) Allied Health: 123.4 (29.6) |
97 (23.3) |
| Ji, China | 723 | NR | Mild: 283 (39.1) Moderate: 66 (9.13) Severe: 34 (4.70) |
449 (62.1) | Physician: 409 (56.6) Nurse: 314 (43.4) |
723 (100) |
| Jo, South Korea | 253 | 54 (21) | NR | 210 (83.0) | Physicians: 27 (10.7) Nurse: 149 (58.9) Allied Health: 35 (13.8) Auxiliary: 35 (13.8) |
NR |
| Johnson, Norway | 1270 | 207 (11.7) | Subclinical PTSD: 305 (17.2) PTSD: 207 (11.7) |
1502 (84.7) | Physician: 178 (10.0) Nurse: 770 (43.4) Allied Health: 402 (31.2) Other: 433 (34.1) |
298 (16.8) |
| Juan, China | 456 | 197 (43.2) | Mild: 148 (32.5) Moderate – severe: 49 (10.7) |
322 (70.6) | Physicians: 195 (42.8) Nurse: 261 (57.2) |
20 (21.2) |
| Kiefer, United States | 558 | 209 (37.5) | NR | 463 (82.9) | Physician: 486 (87.1) Nurse: 15 (2.7%) |
194 (35.5) |
| Kumar, Pakistan | 420 | 236 (56.2) | Clinical concern of PTSD: 75 (17.9) Probable diagnosis of PTSD: 28 (6.7) High enough to PTSD: 133 (31.7) |
184 (43.8) | Auxillary: 420 (100) | NR |
| Lamiani, Italy | 308 | 152 (40) | Mild PTSD: 71 (30) Severe PTSD: 23 (10) |
246 (80) | Administrative 48 (16%) Physician: 48 (16) Nurse: 111 (36) Allied Health: 71 (23.1) Auxillary: 65 (21.1) Other 13 (4%) |
160 (52) |
| Lange, France | 135 | 23 (17) | NR | 78 (59.1) | Allied Health: 135 (100) | NR |
| Lasalvia, Italy | 215 | 77 (35.9) | NR | 109 (50.5) | Physician: 215 (100) | 198 (92.1) |
| Lasalvia, Italy | 2195 | 1181 (53.8) | NR | 1647 (75.3) | Physician: 667 (30.4) Nurse: 783 (35.7) Allied Health: 533 (24.3) Auxillary: 212 (9.7) |
540 (24.6) |
| Laurent, Italy | 2153 | 443 (20.6) | NR | 1614 (75) | Physicians 358 (16.6) Nurse: 1210 (56.2) Allied Health: 424 (19.7) Auxillary: 161 (7.5) |
1365 (63.4) |
| LeónRojas, Mexico | 303 | 59 (19.4) | NR | 303 (100) | Physician: 303 (100) | 120 (39.6) |
| Li, China | 890 | 226 (25.4) | Subclinical PTSD: 93 (10.45) Mild PTSD: 275 (30.9) Moderate PTSD: 296 (33.3) Severe PTSD: 226 (25.4) |
815 (91.6) | Nurse: 890 (100) | 438 (49.2) |
| Liu, China | 1563 | 821 (52.5) | NR | 1293 (82.7) | Physician: 454 (29.0) Nurse: 984 (63.0) Others: 125 (8.0) |
689 (44.1) |
| Li, China | 225 | 71 (31.6) | NR | 162 (72) | Physician: 13 (18.3) Nurse: 53 (74.6) Other: 5 (7.0) |
NR |
| Luceno-Moreno, Spain | 1422 | 805 (56.6) | NR | 1228 (86.4) | Physicians: 143 (10) Nurse: 486 (34.2) Allied Health: 560 (39.4) Other: 233 (16.4) |
1367 (96.1) |
| Lum, Singapore | 257 | 23 (8.9) | NR | 112 (43.6) | NR | NR |
| Luo, China | 2574 | 1772 (68.8) | Mild: 940 (36.5) Moderate: 593 (23) Moderately Severe: 239 (9.29) |
2036 (79.1) | Physician: 783 (30.4) Nurse: 1587 (61.7) Other: 204 (7.93) |
915 (35.5) |
| Magalhaes, United States | 456 | 316 (69.3) | Minimal PTSD Symptoms: 141 (37.7) Moderate PTSD Symptoms: 287 (33.2) Severe PTSD Symptoms: 29 (24.6) |
NR | Physician: 121 (26.5) Nurse: 117 (25.7) Other: 218 (47.8) |
NR |
| ManhThan, Vietnam | 173 | 21 (12.1) | NR | 64 (60.4) | NR | 106 (61) |
| Marco, United States | 1300 | 290 (22.3) | NR | 780 (60) | Physician: 1300 (100) | NR |
| Marcomini, Italy | 173 | 69 (39.9) | NR | 132 (76.3) | Nurse: 173 (100) | NR |
| Martin, Spain | 2089 | 1260 (60.4) | Mild: 477 (22.9) Moderate: 512 (24.5) Severe: 713 (34.2) |
1683 (80.6) | Physician: 812 (39.13) Nurse: 1041 (50.17) Other: 222 (10.7) |
1663 (80.4) |
| Meena, India | 100 | 2 (2) | NR | 92 (92) | Physician: 39 (39) Nurse: 45 (45) Other: 16 |
64 (64) |
| Mehta, Canada | 455 | 140 (30.8) | Clinical Concern for PTSD: 46 (12.2) Probable PTSD: 94 (24.9) |
365/455 (80.2) | Physician: 69 (15.2) Nurse: 279 (61.3) Allied Health: 61 (13.4) Auxillary: 34 (7.47) Other: 8 (1.8) |
346 (76) |
| Mirzaei, Iran | 395 | 342 (86.6) | Moderate PTSD: 28 (7.1) Full PTSD: 314 (79.5) |
288 (72.9) | Nurse: 395 (100) | NR |
| Moderato, Italy | 858 | 450 (52.5) | NR | 724 (84.4) | Physician: 658 (76.7) Nurse: 149 (17.4) Other: 49 (5.7) |
858 (100) |
| Mulatu, Ethiopia | 420 | 243 (57.9) | Mild: 142 (33.8) Moderate: 71 (16.9) Severe: 30 (7.1) |
174 (41.4) | Physician: 115 (27.4) Nurse: 237 (56.4) Allied Health: 68 (16.2) |
296 (70.5) |
| Naheed, Pakistan | 398 | 204 (51.3) | Mild: 62 (15.6) Moderate: 30 (7.5) Severe: 112 (28.1) |
224 (56.3) | Physician: 398 (100) | 186 (46.7) |
| Nguyen, Vietnam (a) | 761 | 261 (34.3) | Mild: 113 (14.8) Moderate: 51 (6.7) Severe: 97 12.7) |
443 (58.2) | NR | 211 (27.7) |
| Nguyen, Vietnam (b) | 349 | 79 (22.6) | Clinical Concern for PTSD: 36 (10.3) PTSD: 16 (4.6) Severe PTSD: 27 (7.7) |
213 (61) | Physician: 199 (57.0) Nurse: 82 (23.5) Other: 68 (19.5) |
227 (65) |
| Ouyang, China | 317 | 31 (10.7) | NR | 221 (69.7) | Physician: 140 (44.2) Nurse: 144 (45.4) Allied Health: 22 (10.4) |
NR |
| Ouyang, China | 403 | 84 (20.8) | NR | 269 (66.7) | Physician: 146 (36.2) Nurse: 243 (60.3) Allied Health: 14 (3.5) |
NR |
| Pan, China | 659 | 90 (13.7) | NR | 597 (90.6) | Physcian: 55 (8.3) Nurse: 573 (86.9) Auxillary: 31 (4.7) |
659 (100) |
| Pappa, Greece | 464 | 199 (42.9) | Mild: 52 (12) Moderate: 22 (5.1) Severe: 125 (28.8) |
319 (68.8) | Physicians: 179 (38.6) Nurses: 200 (43.1) Other: 85 (18.3) |
407 (87.7) |
| Prasad, United States | 347 | 292 (84.1) | Mild: 84 (24.2) Moderate; 128 (36.9) Severe: 80 (23.1) |
315 (90.8) | Nurse: 248 (71.5) Allied Health: 36 (10.4) Auxiliary: 63 (18.2) |
NR |
| Qiu, China | 1717 | 1417 (82.5) | NR | 1436 (83.6) | Physician: 325 (18.9) Nurse: 1226 (71.4) Allied Health: 166 (9.7) |
1717 (100) |
| Qiu, China | 2214 | 590 (26.6) | NR | 1918 (86.6) | Physician: 420 (19) Nurse: 1751 (79.1) Allied Health: 43 (1.9) |
2414 (100) |
| Ranieri, Italy | 69 | 36 (52.6) | NR | 69 (100) | Nurse: 69 (100) | 38 (55) |
| Riello, Italy | 1071 | 902 (84.2) | Mild: 169 (15.8) Moderate: 303 (28.3) Severe: 130 (12.1) |
916 (85.5) | Healthcare Staff: 810 (75.6) Technical Staff: 146 (13.6) Administrative Staff: 115 (10.8)⁎⁎ |
343 (32) |
| Robles, Mexico | 5938 | 1745 (29.4) | NR | 4420 (74.4) | Physicians: 1994 (33.6) Nurses: 1184 (19.9) Allied Health: 1979 (33.3) Auxiliary: 781 (13.2) |
1389 (23.4) |
| Rosenthal, United States | 222 | 88 (39.6) | NR | 204 (92) | Auxillary: 222 (100) | NR |
| Rouse, Ireland | 92 | 24 (26) | NR | 89 (97) | Allied Health: 94 (100) | NR |
| Sachdeva, India | 150 | 95 (63.6) | NR | 54 (36) | Physician: 72 (48) Nurse: 40 (26) Allied Health: 22 (14.6) Other: 16 (10.6) |
90 (60) |
| Sahin, Turkey | 939 | 717 (76.3) | Mild: 416 (44.3) Moderate: 171 (18.2) Severe: 130 (13.8) |
620 (66) | Physicians: 580 (61.8) Nurse: 254 (27.1) Other: 105 (11.2) |
569 (60.6) |
| Sarapultseva, Russia | 128 | 7 (5.5) | Normal: 119 (93) Mild: 5 (3.9) Moderate: 2 (1.6) Severe: 2 (1.6) |
101 (78.9) | Dentist: 43 (33.6) Allied Health: 37 (28.9) Dental auxillary 48 (37.5) |
80 (62.5) |
| Shah, Kenya | 433 | 127 (29.3) | Normal: 283 (69) Mild: 44 (10.7) Moderate: 24 (5.9) Severe: 59 (14.4) |
253 (58.4) | Physician: 243 (56.1) Nurse: 190 (43.9) |
298 (68.8) |
| SobregrauSangrà, Spain | 184 | 43 (23.3) | NR | 156 (84.8) | Physician: 43 (23.4) Nurse: 104 (56.5) Allied Health: 37 (20.1) |
NR |
| Styra, Canada | 3852 | 2698 (70) | Normal: 659 (19.6) Mild: 1013 (30.2) Moderate: 530 (15.8) Severe: 1155 (34.4) |
3245 (84.2) | Physician: 345 (9.4) Nurse: 1256 (34.1) Allied Health: 1034 (28.1) Auxillary: 1243 (28.3) |
2375 (64.6) |
| Tebbeb, France | 373 | 26 (7) | NR | 306 (82) | NR | NR |
| Topal, Turkey | 210 | 80 (38) | NR | 152 (72) | Physician: 86 (41) Nurse: 124 (59) |
NR |
| Udgiri, India | 80 | 80 (100) | NR | 43 (54) | Auxillary: 80 (100) | 45 (56) |
| VanWert, United States | 605 | 135 (22.3) | NR | 475 (78.5) | Social work/MHC/case manager 166 (27.4) Physician/resident/PA/NP 139 (23) Nurse/PCT/RT 283 (46.8) NR 17 (2.6) |
361 (60) |
| VlahTomičević, Croatia | 534 | 176 (33) | Clinical Concern for PTSD: 71 (13.3) Probable PTSD: 32 (5.9) Diagnosis of PTSD: 74 (13.8) |
451 (84.5) | NR | NR |
| Wadasadawala, Bangladesh, India, Indonesia and Nepal | 758 | 138 (18.2) | NR | 394 (52) | Physician: 294 (38.8) Nurse: 92 (12.1) Allied Health: 279 (36.8) Auxillary: 63 (8.3) Other: 30 (4.0) |
NR |
| Wang, China | 1897 | 186 (9.8) | NR | 565 (82.5) | Physician: 563 (29.7) Nurse: 1334 (70.3) |
NR |
| Wanigasooriya, United Kingdom | 2638 | 646 (24.5) | NR | 2097 (79.5) | Physician: 460 (17.4) Nurse: 775 (29.4) Other: 1403 (53.2) |
720 (27.3) |
| Xia, China | 1728 | 676 (39.1) | NR | 1632 (94.4) | Nurse: 1728 (100) | NR |
| Yang, China | 19,379 | 1008 (5.2) | NR | 15,509 (80) | Physician: 4492 (23.2) Nurse: 8863 (45.7) Other: 6024 (31.1) |
7799 (40.2) |
| Yin, China | 371 | 14 (3.8) | NR | 228 (61.5) | Physician: 67 (18.1) Nurse: 264 (71.2) Other: 40 (10.2) |
371 (100) |
| Yitayih, Ethiopia | 249 | 195 (78.3) | Mild: 22 (8.8) Moderate: 101 (40.6) Severe: 72 (28.9) |
131 (52.6) | Physician: 86 (34.5) Nurse: 130 (52.2) Allied Health: 33 (13.3) |
NR |
| Zakeri, Iran | 185 | 64 (34.6) | NR | 143 (77.3) | Nurse: 185 (100) | 109 (60.2) |
| Zara, Italy | 4550 | 1674 (36.8) | NR | 3540 (78) | Physican: 969 (21.3) Nurse: 1492 (32.8) Allied Health: 1553 (34.1) Auxillary: 536 (11.8) |
NR |
| Zhang, China | 401 | 53 (13.2) | NR | 277 (69.1) | NR | NR |
| Zhu, China | 5062 | 1509 (29.8) | NR | 4304 (85) | Physician: 243 (16.1) Nurse: 1130 (74.9) Allied Health: 136 (9.1) |
2000 (39.5) |
Medical/healthcare staff included: physicians, nurses, healthcare auxiliary staff, physiotherapists, experts in psychiatric rehabilitation, speech therapists and psychologists. Technical staff included: educators, entertainers, mediators, caseworkers, trainers, sociologists, specialized auxiliaries, technicians for the maintenance of the building and cleaning staff. Professional staff included: lawyers and religious assistants.
Ninety-nine (99) studies used the IES-R scale, while only 22 studies used the PCL-5 scale. All studies reported the country in which the study was conducted, study sample size, and the survey tools. All included studies but 8 reported the date of study compilation, and only 1 study did not report the survey setting. 11 studies did not report the length of the data collection period. Study days ranged from one day of data collection to 365 days of data collection. Survey settings included surveys conducted online, inpatient, outpatient, or a mix of all three. Tables 1A and 1B show this data.
3.2. Study quality
The majority of the cross-sectional observational studies were found to be of medium quality, scoring on the modified Newcastle Ottawa Scale either 4 or 5 points. One study scored a 3 on the modified NOS indicating low quality, while 23 studies scored a 4, indicating medium quality. All other studies scored a 5 on the modified NOS (Table 1A).
3.3. Patient characteristics
A total of 117,143 healthcare workers across 119 studies were included in our meta-analysis. Of the studies that reported the following data, 87,280 (74.5%) of participants included in our meta-analysis were female. 45,538 (38.9%) participants were in direct occupational contact with COVID-19 patients. Studies focused on the prevalence of PTSD among different types of healthcare professionals including physicians, nurses, allied health professionals, and auxiliary health professionals. Twelve (12) studies did not report the makeup of their study population. Of the included studies that reported study population in more detail, 28,365 (25.2%) were physicians, 48,171 (42.8%) were nurses, 13,903 (12.4%) were allied health professionals, 10,029 (8.9%) were auxiliary health professionals, and 12,103 (10.8%) participants were specified as “other”. Four (4) studies specified the breakdown of their study population by profession, but used different categories that did not allow us to fully separate the data for our analysis (Collantoni et al., 2021; Ergai et al., 2022; Riello et al., 2020; Van Wert et al., 2022). Table 1 summarizes this data.
3.4. Primary outcome
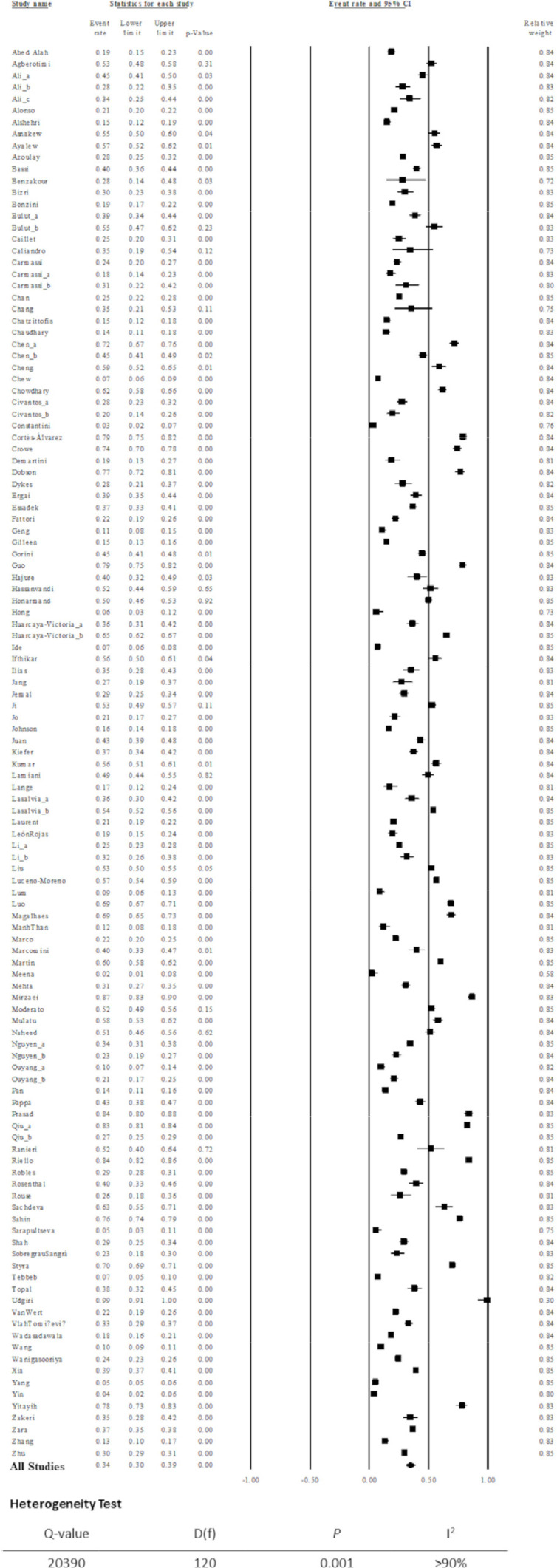
Our primary outcome of interest was defined as the prevalence of PTSD symptoms among healthcare workers and was reported by all 119 studies included in our meta-analysis (Fig. 2 A). Approximately 34% of the 117,143 healthcare workers reported by 119 studies displayed PTSD-relevant (Event rate 0.34, 95% CI, 0.30–0.39, I2 = >90%). The percentage of participants with PTSD-relevant symptoms ranged from 2% to 100%. The Cochrane Q value of 20,390, with 120 degrees of freedom [D(f)], which resulted in a P-value < 0.001. This information caused us to reject the null hypothesis, which stated that the effect size of our studies was similar to the true effect size. Additionally, the I2 value was greater than 90%, which indicated that 90% of variance between our studies’ effect size and the true effect size was due to sampling errors.
Fig. 2.
A: Forest Plot from random effects meta-analysis of studies reporting any PTSD among health care workers during the Coronavirus Disease 2019 (COVID-19) pandemic.
B. Sensitivity analysis of random effects meta-analysis of studies reporting any PTSD among health care workers during the Coronavirus 2019 pandemic. The sensitivity analysis used a one-study-removed method.
The one-study-removed sensitivity analysis results and forest plot are shown in Fig. 2B. The pooled prevalence of PTSD-relevant symptoms persisted between 34%−35% when the random-effects meta-analysis removed each individual study from the pooled population one by one. These results from the sensitivity analysis suggested that our pooled effect size was not affected by any individual study.
3.5. Secondary outcome
Thirty-four (34) studies with 24,541 patients reported our secondary outcome, which was the prevalence of severe PTSD symptoms amongst HCW as defined by the study authors. These studies showed a range of 1.6% to 36.7% of participants reporting severe PTSD symptoms. Our random-effects meta-analysis showed a prevalence of severe PTSD among healthcare workers during the COVID-19 pandemic as 14% (Event rate 0.14, 95% CI, 0.11 - 0.17, I2 = >90% (Fig. 3 ). The P-value for the Q statistic was <0.001, which rejected the null hypothesis that our studies’ effect size was similar to the true effect size. Similarly, the I2 was greater than 90%, indicating that more than 90% of variance between our studies and the true effect size was not due to chance and that there was high heterogeneity present.
Fig. 3.
Forest Plot from random effects meta-analysis of studies reporting prevalence of severe PTSD among health care workers during the Coronavirus Disease 2019 (COVID-19) pandemic.
Additionally, we performed a moderator analysis for both the primary outcome (Table 2A ) and the secondary outcome Table 2A) by dividing the studies into subgroups, including WHO region (African Region AFR; Region of the Americas, AMR; Eastern Mediterranean Region, EMR; European Region, EUR; South East Asian Region, SEAR; Western Pacific Region, WPR;), month of study completion (February 2020, March 2020, April 2020, May 2020, June 2020, July 2020, August 2020, September 2020, October 2020, November 2020, December 2020, 2021, 2022), study setting (inpatient, outpatient, mixed, online), and survey tools (IES-R, PCL, other). The I2 was > 90% for all of the subgroups in moderator analysis, indicating that >90% of the variability between the true effect size and our studies’ effect size was by sampling errors, and not by chance.
Table 2A.
Moderator analysis of subgroups using categorical variables for the rates of any PTSD.
| Meta-analysis | Heterogeneity | Between group comparison | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Moderator Variables | Number of studies | Any PTSD,% | 95% CI | P-value | Q-value | D(f) | P | I2 | P | |
| Date of Survey Completion | 2020 February | 9 | 0.51 | 0.34–0.67 | 0.92 | 2748 | 8 | 0.001 | >90% | 0.01 |
| 2020 March | 6 | 0.40 | 0.22–0.61 | 0.33 | 223 | 5 | 0.001 | >90% | ||
| 2020 April | 17 | 0.27 | 0.18–0.38 | 0.001 | 4800 | 16 | 0.001 | >90% | ||
| 2020 May | 20 | 0.38 | 0.28–0.49 | 0.03 | 2216 | 19 | 0.001 | >90% | ||
| 2020 June | 12 | 0.30 | 0.19–0.44 | 0.01 | 649 | 11 | 0.001 | >90% | ||
| 2020 July | 11 | 0.36 | 0.23–0.51 | 0.07 | 2720 | 10 | 0.001 | >90% | ||
| 2020 August | 6 | 0.55 | 0.35–0.74 | 0.61 | 477 | 5 | 0.001 | >90% | ||
| 2020 September | 6 | 0.25 | 0.12–0.44 | 0.01 | 412 | 5 | 0.001 | >90% | ||
| 2020 October | 6 | 0.40 | 0.23–0.61 | 0.36 | 72 | 5 | 0.001 | >90% | ||
| 2020 November | 3 | 0.26 | 0.10–0.54 | 0.09 | 7 | 2 | 0.03 | 72% | ||
| 2020 December | 6 | 0.31 | 0.16–0.51 | 0.06 | 449 | 5 | 0.001 | >90% | ||
| 2021 | 9 | 0.22 | 0.12–0.37 | 0.001 | 498 | 8 | 0.001 | >90% | ||
| 2022 | 2 | 0.04 | 0.01–0.14 | 0.001 | 0.1 | 1 | 0.8 | 0% | ||
| NR | 8 | 0.47 | 0.30–0.66 | 0.79 | 482 | 7 | 0.001 | >90% | ||
| Regions of the World Health Organization | ||||||||||
| AFR | 10 | 0.46 | 0.31–0.62 | 0.64 | 266 | 9 | 0.001 | >90% | 0.10 | |
| AMR | 19 | 0.45 | 0.33–0.56 | 0.37 | 2795 | 18 | 0.001 | >90% | ||
| EMR | 10 | 0.41 | 0.26–0.56 | 0.23 | 598 | 9 | 0.001 | >90% | ||
| EUR | 44 | 0.31 | 0.25–0.38 | 0.001 | 4874 | 43 | 0.001 | >90% | ||
| SEAR | 6 | 0.32 | 0.16–0.54 | 0.1 | 550 | 5 | 0.001 | >90% | ||
| WPR | 32 | 0.28 | 0.21–0.36 | 0.001 | 10,005 | 31 | 0.001 | >90% | ||
| Survey tools | ||||||||||
| IES-R | 99 | 0.37 | 0.33–0.42 | 0.001 | 122,227 | 98 | 0.001 | >90% | 0.001 | |
| PCL-5 | 22 | 0.22 | 0.16–0.29 | 0.001 | 3638 | 21 | 0.001 | >99% | ||
| Survey settings | ||||||||||
| Inpatient | 5 | 0.32 | 0.16–0.54 | 0.11 | 43 | 4 | 0.001 | >90% | 0.19 | |
| Outpatient | 5 | 0.17 | 0.07–0.34 | 0.001 | 800 | 4 | 0.001 | >90% | ||
| Mixed settings | 25 | 0.37 | 0.28–0.47 | 0.013 | 3452 | 24 | 0.001 | >90% | ||
| Online | 76 | 0.36 | 0.31–0.42 | 0.001 | 15,460 | 65 | 0.001 | >90% | ||
| NR | 10 | 0.26 | 0.15–0.40 | 0.002 | 408 | 9 | 0.001 | >90% | ||
Abbreviations: CI, confidence interval; WHO, World Health Organization; AFR, African Region; AMR, Region of the Americas; EMR, Eastern Mediterranean Region; EUR, European Region; SEAR, South East Asian Region; WPR, Western Pacific Region; NR, not reported by the authors; IES- R, Impact of Event Scale - Revised; PCL, Posttraumatic Stress Disorder Checklist;.
From subgroup comparisons, there was a significant difference in the effect size of PTSD-relevant symptoms from the study belonging to the EUR, SEAR, and WPR of the WHO regions, compared with other WHO regions (Table 2A). Similarly, studies that used PCL-5 as the primary survey tool reported a lower prevalence of PTSD symptoms (22%, P < 0.005) than studies that used IES-R (37%, P <0.001).
We performed a multivariable meta-regression using patients’ characteristics as reported by studies’ authors (Table 2B ). We used seven variables that were consistently reported by the studies’ authors for our meta-regression, but none of these variables were significantly associated with the prevalence of PTSD-relevant symptoms. In a multivariable meta-regression using the most possible number of studies (23 studies) and number of independent variables (7) (Table 2B), the percentage of physician participants was negatively correlated with the rates of severe PTSD symptoms (correlation coefficient −3.2, 95% CI −5.3 to −1.1, ``-value = 0.001). The percentage of auxiliary workers was also negatively correlated with the rates of severe PTSD (correlation coefficient −5.5, 95% CI −8.5 to −2.4, p-value = 0.001). Three other variables were not significantly associated with the rate of severe PTSD. (Table 2c )
Table 2B.
Multivariable meta-regression to measure participants’ characteristics and association with prevalence with any PTSD from Health care workers during the COVID-19 pandemic. All listed continuous variables were included in the meta-regression.
| Variables | Number of studies | Corr. Coeff. (95% CI) | P | I2 |
|---|---|---|---|---|
| Percentage of female participants | 70 | −1.3 (−3.2 to 0.61) | 0.18 | >90% |
| Percentage of physician participants | −0.89 (−3.8 to 2.1) | 0.55 | ||
| Percentage of nurse participants | −0.33 (−3.1 to 2.5) | 0.82 | ||
| Percentage of Allied Health Professional | −2.0 (−5.1 to 1.1) | 0.21 | ||
| Percentage of Auxiliary Healthcare Worker | 0.86 (−2.1 to 3.8) | 0.57 | ||
| Percentage of Other types of healthcare worker | −2.3 (−5.3 to 0.65) | 0.13 | ||
| Percentage of workers having contacts with COVID-19 patients | 0.63 (−0.32 to 1.6) | 0.20 |
Abbreviations: CI, confidence interval; COVID-19, Coronavirus Disease 2019; HCW, healthcare worker; PTSD, post-traumatic stress disorder.
Table 2C.
Multivariable meta-regression to measure participants’ characteristics and association with prevalence with Severe PTSD from Health care workers during the COVID-19 pandemic. All listed continuous variables were included in the meta-regression.
| Variables | Number of studies | Corr. Coeff. (95% CI) | P | I2 |
|---|---|---|---|---|
| Percentage of female participants | 23 | 0.63 (−2.4 to 3.7) | 0.69 | >90% |
| Percentage of physician participants | −3.2 (−5.3 to −1.1) | 0.001 | ||
| Percentage of nurse participants | −2.1 (−4.6 to 0.35) | 0.09 | ||
| Percentage of Allied Health Professional | −5.5 (−8.5 to −2.4) | 0.001 | ||
| Percentage of Auxiliary Healthcare Worker | −2.4 (−5.6 to 0.72) | 0.13 | ||
| Percentage of Other types of healthcare worker | −2.3 (−8.6 to 3.89) | 0.46 | ||
| Percentage of workers having contacts with COVID-19 patients | 0.77 (−0.99 to 2.54) | 0.39 |
Abbreviations: CI, confidence interval; COVID-19, Coronavirus Disease 2019; HCW, healthcare worker; PTSD, post-traumatic stress disorder.
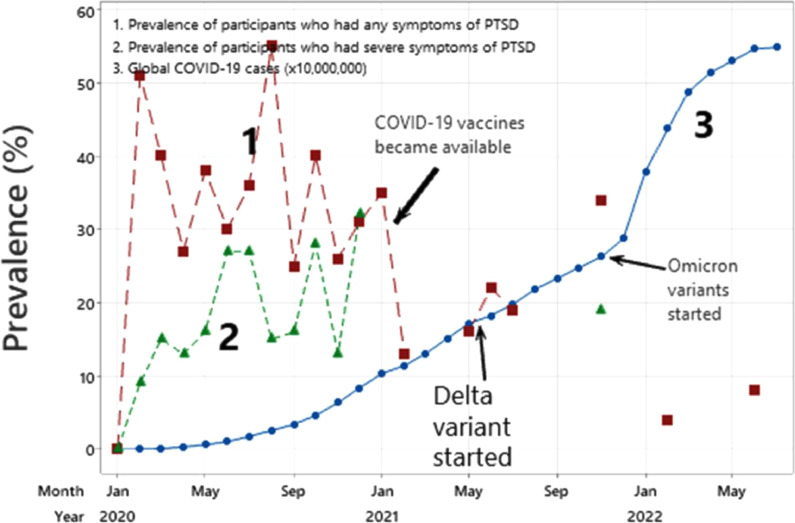
3.6. Time series analysis
Fig. 4A and 4B depict the percentages of participants who reported any PTSD symptoms and severe PTSD symptoms with both the total monthly global cases of COVID-19 and new monthly global cases of COVID-19, respectively. The percentages of participants reporting PTSD-relevant symptoms appeared to parallel the rise of global cases until January 2021. After January 2021, which marks the beginning of COVID-19 vaccines being available, the prevalence of PTSD symptoms sharply declined. The prevalence of PTSD rose again with the introduction of the Delta and Omicron variants, but did not return to the peak rates in August 2020.
Fig. 4.
A. Time series analysis depicting the prevalence of participants who reported any or severe PTSD symptoms and the monthly global cases of COVID-19.
Legend: The Dashed Red Line with Squares (Line 1) indicates the prevalence of participants who had any symptoms of PTSD over the course of the pandemic. The Dashed Green Line with Triangles (Line 2) indicates the prevalence of participants who had severe symptoms of PTSD. The Solid Blue Line with Dots (Line 3) indicates the global number of COVID-19 cases as a factor of 10 million. We mark key events during the pandemic with a solid arrow. Key events include the availability of COVID-19 vaccines, the start of the Delta variant, and the start of the Omicron variant.
B. Time series analysis depicting the percentages of participants who reported any or severe PTSD symptoms and the monthly global NEW cases of COVID-19.
Legend: The Solid Blue Line with Dots (Line 1) indicates the prevalence of participants who had any symptoms of PTSD over the course of the pandemic. The Dashed Red Line with Triangles (Line 2) indicates the prevalence of participants who had severe symptoms of PTSD. The Dashed Green Line with Diamonds indicates (Line 3) the global number of new COVID-19 cases as a factor of 1 million. We mark key events during the pandemic with a solid arrow. Key events include the availability of COVID-19 vaccines, the start of the Delta variant, and the start of the Omicron variant.
4. Discussion
Our meta-analysis indicates that the pooled incidence of PTSD symptoms in the healthcare worker population during COVID-19 is 34% (121 data points), and 14% for severe PTSD symptoms (34 studies). Additionally, we included enough studies to perform moderator analyses for different subgroups including WHO region of study setting and month of study completion.
Trauma, as defined by the DSM-5 criteria, is “actual or threatened death, serious injury, or sexual violence” (Weathers, 2018). Under this criteria, stress-inducing events that do not involve an immediate threat to life or physical injury are not considered trauma (Nemeroff and Marmar, 2018). However, several previous studies have shown how stressful events that fall outside of this narrow definition of trauma can still induce symptoms of PTSD (Cordova et al., 2017; Galea et al., 2008; Gold et al., 2005). The COVID-19 pandemic also falls out of this definition, but has been suggested to be considered a traumatic stressor for several reasons including the uncertainty of the pandemic's timeline, fear of future sickness and death events whether it be for themselves or loved ones, media coverage, and more (Bridgland et al., 2021). Although healthcare workers are regularly exposed to death and injury during their typical jobs, the pandemic introduces additional elements of uncertainty, risk to personal safety, seeking co-workers to fall ill, and higher patient volume. Literature has also shown a strong correlation between risk perception and PTSD, including during the pandemic (Geng et al., 2021; Wu et al., 2009; Yin et al., 2021). Nevertheless, it is important to note that broadening the definition of PTSD may have unintended consequences. For example, it has been suggested that broadening the definition of trauma can result in increased vulnerability because it can affect how a person interprets a stressful event (Jones and McNally, n.d.).
The prevalence we reported was higher than those reported in previous meta-analyses assessing the prevalence of PTSD symptoms in healthcare workers during COVID-19 (Civantos et al., 2020b; Falasi et al., 2021; Marvaldi et al., 2021; Salehi et al., 2021; Sanghera et al., 2020; Yuan et al., 2021). Prior reported prevalence typically ranged from 20% to 26.9%. This may be because we included a larger pool of studies, or our meta-analysis included studies over a span of more than two years from the beginning of the pandemic. Prior to our analysis, the most comprehensive meta-analysis on the subject only included 20 studies and concluded their search by August 2020 (Yuan et al., 2021). Symptoms of PTSD can typically surface months after the traumatic experience. Therefore, our findings are clinically important because even after COVID-19, healthcare workers will experience high rates of psychological distress. PTSD among healthcare workers is associated with increased medical errors, reduced productivity, compassion fatigue, all of which contributes to lower quality of care (Gates et al., 2011; Karanikola et al., 2015). Prior meta-analyses on the topic also either did not focus exclusively on the COVID-19 pandemic or exclusively on healthcare workers, limiting their subgroup analysis specific to PTSD symptoms in healthcare workers during COVID-19. The prevalence we reported was also higher than those reported in meta-analyses of PTSD among healthcare workers during past outbreaks and public health emergencies (Cheng et al., 2020; Fan et al., 2021; Zhou et al., 2021). This may be due to the higher incidence rate of SARS-2-CoV which contributed to insufficient PPE and high patient volume, increased media coverage and misinformation, and fear due to increased risk and uncertainty of infecting others (Billings et al., 2021; Greene et al., 2021; Norful et al., 2021).
A meta-analysis performed by Salehi et al. examined the prevalence of PTSD-relevant symptoms among the general population from all previous coronavirus outbreaks (SARS-CoV, MERS, SARS-CoV-2) between November 01, 2012 until May 18, 2020 (Salehi et al., 2021). This study included 36 studies and reported an overall rate of PTSD for all studies (general population, healthcare workers, patients/survivors, etc.) at 18% (95% CI 0.15–0.20). The prevalence of PTSD symptoms among healthcare workers was 18% (95% CI 13%−24%, I2 = 97%), whereas the prevalence of PTSD among patients was 29% (95% CI 18%−39%, I2 = 96%). On the other hand, the rate of the general population was the lowest at 12% (95% CI 8%−16%, I2 = 98%) during these outbreaks. The rate of PTSD symptoms among healthcare workers from Salehi was lower than ours because the authors only included COVID-19 studies up to May 2020, when the full effect of the COVID-19 pandemic was still unfolding and not totally reported in the literature. Although our studies are not comparable, these results from Salehi et al. provided interesting insights. Healthcare workers are more susceptible to higher rates of PTSD than the general population during previous coronavirus outbreaks. Therefore, a similar trend would be observed during the COVID-19 pandemic.
We noticed a significant difference in the outcome observed between studies that used the IES-R scale and studies that used the PCL-5 scale, with studies using the PCL-5 scale reporting a lower prevalence of PTSD. This suggests that future studies should be standardized to one tool. While both tools are validated, the IES-R is not used to diagnose PTSD under the revised DSM-5 criteria and may not accurately reflect rates of PTSD, while the PCL-5 can provide a provisional diagnosis and is recommended for use by the National Center for PTSD (National Center for PTSD, n.d.; Umberger, 2019). For these reasons, we suggest that future studies only use PCL-5 to assess the prevalence of PTSD among healthcare workers in a more standardized manner. However, a majority of studies used the IES-R. Additionally, despite the use of validated tools, there was some variability in the cut-offs used by authors. This strongly suggests the need for establishing universal cut-offs to standardize data collection and comparisons for prevalence studies.
There were significant differences in prevalence rates between WHO regions. While further research is needed to explain this finding, we hypothesize that this might be due to differences in staff-case ratio, access to resources and PPE, politicization of the pandemic, the public's health behavior, and other factors. Few studies reported the specialties of study participants, whether or not the participants had any prior psychiatric conditions, or the outcome stratified by exposure to COVID-19. This barred us from conducting moderator analyses for these subgroups. These data would have contributed to a better understanding of risk factors for PTSD, and hence another suggestion for future studies. It is also important that studies are conducted even after the end of the pandemic to understand how PTSD may persist and to better guide interventions and allocation of resources to healthcare worker wellness.
Our findings demonstrate the need for interventions and policies that lower the risk of PTSD among healthcare workers. It is important that health policy focuses on ensuring the availability and accessibility of PPE (Carmassi et al., 2020; Kisely et al., 2020). Hospitals should also ensure that counseling and peer support are widely available with low barriers of access, and that interventions take a trauma-informed approach to ensure that unwanted triggers are not activated (d'Ettorre et al., 2021). Regular screening for PTSD among healthcare workers can identify those at-risk and affected, ensuring timely and targeted interventions. Our time-series analysis showed that the introduction of COVID−19 vaccines was correlated with a decrease in the prevalence of PTSD, hence a protective factor. The mental health effects of the COVID-19 pandemic among HCWs will remain long-after the pandemic ends in the forms of PTSD. Researchers should continue assessing the prevalence of PTSD as the pandemic evolves and well beyond the pandemic as well to better understand vaccine rollout and other factors affect the prevalence.
4.1. Limitations
Our study has several limitations which present future directions for studies. Although we utilized very broad search terms that returned a large eligible number of studies, due to the explosive number of publications during the COVID-19 pandemic and because we did not search other databases such as Google Scholar, our search might have missed other articles. All included studies had a moderate or high risk of bias due to their cross-sectional survey format. Additionally, we excluded all studies that used non-validated surveys to measure PTSD symptoms. This may affect the pooled prevalence we found in our analysis. Despite several subgroup analyses to identify potential sources of heterogeneity, there was high heterogeneity among the studies we included in our meta-analysis, which may affect the generalizability of the finding. Despite the use of validated tools, there was still variability in author's definitions of cut-offs. We also included different categories of healthcare workers from a variety of clinical settings, different time periods of the pandemic, different practice settings, and different levels of experience. This was expected because COVID-19 was a global pandemic that affected several countries at various degrees.
We cannot know with certainty that the PTSD symptoms were or were not driven by other mood disorders because we did not control for other mood disorders. Approximately half of people with PTSD are also affected by major depressive disorder (MDD), and it has been suggested that this is a reflection of overlapping symptoms. It is also important to note that studies conducted on the topic prior to the pandemic also found the presence of PTSD symptoms among healthcare workers (DeLucia et al., 2019; Joseph, 2021). Future research should seek to determine what proportion of the prevalence of PTSD symptoms during COVID-19 pandemic is due to the pandemic, and how much is pre-existing, perhaps by using methods such as difference-in-difference analysis.
Conclusion
Our systematic review and meta-analysis suggested a high prevalence of PTSD symptoms among healthcare workers during the COVID-19 pandemic among studies using validated survey tools. It is important that policies work towards allocating adequate attention and resources towards protecting the well-being of healthcare workers to minimize the adverse consequences of PTSD, and in turn, ensure higher quality of care for patients.
Author statements
No ethical approval was needed because only data from previous published studies in which informed consent was obtained by primary investigators was retrieved and analyzed.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Sanketh Andhavarapu: Conceptualization, Methodology, Validation, Project administration, Investigation, Writing – original draft, Writing – review & editing. Isha Yardi: Investigation, Writing – original draft, Writing – review & editing. Vera Bzhilyanskaya: Investigation, Writing – original draft, Writing – review & editing. Tucker Lurie: Investigation, Writing – original draft, Writing – review & editing. Mujtaba Bhinder: Investigation, Writing – review & editing. Priya Patel: Investigation, Writing – review & editing. Ali Pourmand: Writing – review & editing. Quincy K Tran: Conceptualization, Methodology, Validation, Project administration, Formal analysis, Resources, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare no competing interests.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2022.114890.
Appendix. Supplementary materials
References
- Agberotimi S.F., Akinsola O.S., Oguntayo R., Olaseni A.O. Interactions between socioeconomic status and mental health outcomes in the Nigerian context amid COVID-19 pandemic: a comparative study. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.559819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alah M.A., Ali K., Abdeen S., Al-Jayyousi G., Kasem H., Poolakundan F., Al-Mahbshii S., Bougmiza I. The psychological impact of COVID-19 on health care workers working in a unique environment under the umbrella of Qatar Red Crescent Society. Heliyon. 2021 doi: 10.1016/j.heliyon.2021.e07236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S.K., Shah J., Du K., Leekha N., Talib Z. Mental health disorders among post graduate residents in Kenya during the COVID-19 pandemic. PLoS ONE. 2022;17 doi: 10.1371/journal.pone.0266570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S.K., Shah J., Talib Z. COVID-19 and mental well-being of nurses in a tertiary facility in Kenya. PLoS ONE. 2021 doi: 10.1371/journal.pone.0254074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S., Maguire S., Marks E., Doyle M., Sheehy C. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicentre study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alonso J., Vilagut G., Mortier P., Ferrer M., Alayo I., Aragón-Peña A., Aragonès E., Campos M., Cura-González I.D., Emparanza J.I., Espuga M., Forjaz M.J., González-Pinto A., Haro J.M., López-Fresneña N., Salázar A.D.M.de, Molina J.D., Ortí-Lucas R.M., Parellada M., Pelayo-Terán J.M., Pérez-Zapata A., Pijoan J.I., Plana N., Puig M.T., Rius C., Rodríguez-Blázquez C., Sanz F., Serra C., Kessler R.C., Bruffaerts R., Vieta E., Pérez-Solà V., MINDCOVID Working group Mental health impact of the first wave of COVID-19 pandemic on Spanish healthcare workers: a large cross-sectional survey. Rev. Psiquiatr. Salud Ment. 2021;14:90–105. doi: 10.1016/j.rpsm.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshehri A.S., Alghamdi A.H. Post-traumatic stress disorder among healthcare workers diagnosed with COVID-19 in Jeddah, Kingdom of Saudi Arabia, 2020 to 2021. Cureus. 2021;13:e17371. doi: 10.7759/cureus.17371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association, 2022. Diagnostic and statistical manual of mental disorders: DSM-5-TR.
- Asnakew S., Legas G., Muche Liyeh T., Belete A., Haile K., Yitbarek G.Y., Bayih W.A., Feleke D.G., Birhane B.M., Amha H., Shumet S., Chanie E.S. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia, 2020: a multi-centered cross-sectional study. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0255340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayalew M., Deribe B., Abraham Y., Reta Y., Tadesse F., Defar S. Post-traumatic stress disorder symptoms and its predictors among healthcare workers following COVID-19 pandemic in Southern Ethiopia: a cross-sectional study. Front Psychiatry. 2022 doi: 10.3389/fpsyt.2021.818910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay E., Pochard F., Reignier J., Argaud L., Bruneel F., Courbon P., Cariou A., Klouche K., Labbé V., Barbier F., Guitton C., Demoule A., Kouatchet A., Guisset O., Jourdain M., Papazian L., Van Der Meersch G., Reuter D., Souppart V., Resche-Rigon M., Darmon M., Kentish-Barnes N., FAMIREA Study Group Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest. 2021;160:944–955. doi: 10.1016/j.chest.2021.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassi M., Negri L., Delle Fave A., Accardi R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy. Italy. J. Affect. Disord. 2021;280:1–6. doi: 10.1016/j.jad.2020.11.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benfante A., Di Tella M., Romeo A., Castelli L. Traumatic stress in healthcare workers during COVID-19 pandemic: a review of the immediate impact. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.569935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benzakour L., Langlois G., Marini V., Groz A., Chiabotto C., Apetrei D., Corneau B., Bondolfi G. Implementation of a psychiatric consultation for healthcare workers during first wave of COVID-19 outbreak. Int. J. Environ. Res. Public Health. 2022;19 doi: 10.3390/ijerph19084780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings J., Ching B.C.F., Gkofa V., Greene T., Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv. Res. 2021;21:923. doi: 10.1186/s12913-021-06917-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bizri M., Kassir G., Tamim H., Kobeissy F., El Hayek S. Psychological distress experienced by physicians and nurses at a tertiary care center in Lebanon during the COVID-19 outbreak. J Health Psychol. 2022 doi: 10.1177/1359105321991630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonzini M., Comotti A., Fattori A., Cantù F., Colombo E., Tombola V., Myslymi E., Gatti M., Stucchi G., Nava C., Bordini L., Riboldi L., Brambilla P. One year facing COVID. Systematic evaluation of risk factors associated with mental distress among hospital workers in Italy. Front Psychiatry. 2022 doi: 10.3389/fpsyt.2022.834753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein, M., 2019. Common mistakes in meta-analysis: and how to avoid them.
- Bridgland V.M.E., Moeck E.K., Green D.M., Swain T.L., Nayda D.M., Matson L.A., Hutchison N.P., Takarangi M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0240146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulut D., Sefa Sayar M., Koparal B., Cem Bulut E., Çelik S. Which of us were more affected by the pandemic? The psychiatric impacts of the COVID-19 pandemic on healthcare professionals in the province where the first quarantine units were established in Turkey. Int. J. Clin. Pract. 2021;75:e14235. doi: 10.1111/ijcp.14235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caillet A., Coste C., Sanchez R., Allaouchiche B. Psychological impact of COVID-19 on ICU caregivers. Anaesth Crit Care Pain Med. 2020;39:717–722. doi: 10.1016/j.accpm.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caliandro M., Fabiana G., Surgo A., Carbonara R., Ciliberti M.P., Bonaparte I., Caputo S., Fiorentino A. Impact on mental health of the COVID-19 pandemic in a radiation oncology department. Radiol Med. 2022 doi: 10.1007/s11547-021-01440-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Dell'Oste V., Bui E., Foghi C., Bertelloni C.A., Atti A.R., Buselli R., Di Paolo M., Goracci A., Malacarne P., Nanni M.G., Gesi C., Cerveri G., Dell'Osso L. The interplay between acute post-traumatic stress, depressive and anxiety symptoms on healthcare workers functioning during the COVID-19 emergency: a multicenter study comparing regions with increasing pandemic incidence. J. Affect. Disord. 2022;298:209–216. doi: 10.1016/j.jad.2021.10.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Foghi C., Dell'Oste V., Cordone A., Bertelloni C.A., Bui E., Dell'Osso L. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Pedrinelli V., Dell'Oste V., Bertelloni C.A., Cordone A., Bouanani S., Corsi M., Baldanzi S., Malacarne P., Dell'Osso L., Buselli R. Work and social functioning in frontline healthcare workers during the covid-19 pandemic in Italy: role of acute post-traumatic stress, depressive and anxiety symptoms. Riv. Psichiatr. 2021;56:189–197. doi: 10.1708/3654.36346. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Pedrinelli V., Dell'Oste V., Bertelloni C.A., Grossi C., Gesi C., Cerveri G., Dell'Osso L. PTSD and depression in healthcare workers in the Italian epicenter of the COVID-19 outbreak. Clin. Pract. Epidemiol. Ment. Health. 2021;17:242–252. doi: 10.2174/1745017902117010242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J., Ray J.M., Joseph D., Evans L.V., Joseph M. Burnout and post-traumatic stress disorder symptoms among emergency medicine resident physicians during the COVID-19 pandemic. West. J. Emerg. Med. 2022;23:251–257. doi: 10.5811/westjem.2021.11.53186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan L.G., Tan P.L.L., Sim K., Tan M.Y., Goh K.H., Su P.Q., Tan A.K.H., Lee E.S., Tan S.Y., Lim W.P., Aw C.H., Goh Y.Z., Sadarangani S., Chow A. Psychological impact of repeated epidemic exposure on healthcare workers: findings from an online survey of a healthcare workforce exposed to both SARS (severe acute respiratory syndrome) and COVID-19. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-051895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatzittofis A., Karanikola M., Michailidou K., Constantinidou A. Impact of the COVID-19 pandemic on the mental health of healthcare workers. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18041435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhary F.A., Ahmad B., Gul M., Rafiq A., Butt D.Q., Rehman M., Ahmad P. The psychological impact of the COVID-19 pandemic on oral health care workers and its impact on their willingness to work during this pandemic. Archives of Psychiatry Research. 2021 doi: 10.20471/dec.2021.57.02.06. [DOI] [Google Scholar]
- Chen B., Li Q.-.X., Zhang H., Zhu J.-.Y., Yang X., Wu Y.-.H., Xiong J., Li F., Wang H., Chen Z.-.T. The psychological impact of COVID-19 outbreak on medical staff and the general public. Curr. Psychol. 2022;41:5631–5639. doi: 10.1007/s12144-020-01109-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng P., Xu L.-.Z., Zheng W.-.H., Ng R.M.K., Zhang L., Li L.-.J., Li W.-.H. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J. Affect. Disord. 2020;277:368–374. doi: 10.1016/j.jad.2020.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Zhang S.X., Yin A., Yáñez J.A. Mental health symptoms during the COVID-19 pandemic in developing countries: a systematic review and meta-analysis. J. Glob. Health. 2022;12:05011. doi: 10.7189/jogh.12.05011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Lin D., Feng H. An investigation of mental health status among medical staff following COVID-19 outbreaks: a cross-sectional study. Med. Sci. Monit. 2021;27 doi: 10.12659/MSM.929454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury S.R., Sunna T.C., Das D.C., Kabir H., Hossain A., Mahmud S., Ahmed S. Mental health symptoms among the nurses of Bangladesh during the COVID-19 pandemic. Middle East Curr. Psychiatry. 2021 doi: 10.1186/s43045-021-00103-x. [DOI] [Google Scholar]
- Civantos A.M., Bertelli A., Gonçalves A., Getzen E., Chang C., Long Q., Rajasekaran K. Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: a national study. Am. J. Otolaryngol. 2020;41 doi: 10.1016/j.amjoto.2020.102694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civantos A.M., Byrnes Y., Chang C., Prasad A., Chorath K., Poonia S.K., Jenks C.M., Bur A.M., Thakkar P., Graboyes E.M., Seth R., Trosman S., Wong A., Laitman B.M., Harris B.N., Shah J., Stubbs V., Choby G., Long Q., Rassekh C.H., Thaler E., Rajasekaran K. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck. 2020;42:1597–1609. doi: 10.1002/hed.26292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collantoni E., Saieva A.M., Meregalli V., Girotto C., Carretta G., Boemo D.G., Bordignon G., Capizzi A., Contessa C., Nesoti M.V., Donato D., Flesia L., Favaro A. Psychological distress, fear of COVID-19, and resilient coping abilities among healthcare workers in a tertiary first-line hospital during the coronavirus pandemic. J. Clin. Med. 2021 doi: 10.3390/jcm10071465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cordova M.J., Riba M.B., Spiegel D. Post-traumatic stress disorder and cancer. Lancet Psychiatry. 2017;4:330–338. doi: 10.1016/S2215-0366(17)30014-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortés-Álvarez N.Y., Vuelvas-Olmos C.R. COVID 19: psychological effects and associated factors in Mexican nurses. Disaster Med. Public Health Prep. 2020:1–7. doi: 10.1017/dmp.2020.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini A., Mazzotti E., Serpentini S., Piattelli A., Scarponi D., De Benedetta G., Bellani M. COVID-19 pandemic distress among a sample of Italian psycho-oncologists: risk of isolation and loneliness. Tumori. 2022;108:77–85. doi: 10.1177/0300891621992129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 cumulative cases by day worldwide 2022 [WWW Document], n.d. . Statista. URL https://www.statista.com/statistics/1103040/cumulative-coronavirus-covid19-cases-number-worldwide-by-day/(accessed 9.1.22).
- Crowe S., Fuchsia Howard A., Vanderspank B. The mental health impact of the COVID-19 pandemic on Canadian critical care nurses. Intensive Crit. Care Nurs. 2022;71 doi: 10.1016/j.iccn.2022.103241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91 doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLucia J.A., Bitter C., Fitzgerald J., Greenberg M., Dalwari P., Buchanan P. Prevalence of post-traumatic stress disorder in emergency physicians in the United States. West. J. Emerg. Med. 2019;20:740–746. doi: 10.5811/westjem.2019.7.42671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demartini B., Nisticò V., D'Agostino A., Priori A., Gambini O. Early psychiatric impact of COVID-19 pandemic on the general population and healthcare workers in Italy: a preliminary study. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.561345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d'Ettorre G., Ceccarelli G., Santinelli L., Vassalini P., Innocenti G.P., Alessandri F., Koukopoulos A.E., Russo A., d'Ettorre G., Tarsitani L. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobson H., Malpas C.B., Burrell A.J., Gurvich C., Chen L., Kulkarni J., Winton-Brown T. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas. Psychiatry. 2021;29:26–30. doi: 10.1177/1039856220965045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dragioti E., Li H., Tsitsas G., Lee K.H., Choi J., Kim J., Choi Y.J., Tsamakis K., Estradé A., Agorastos A., Vancampfort D., Tsiptsios D., Thompson T., Mosina A., Vakadaris G., Fusar-Poli P., Carvalho A.F., Correll C.U., Han Y.J., Park S., Il Shin J., Solmi M. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022;94:1935–1949. doi: 10.1002/jmv.27549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med. 2021 doi: 10.1017/s0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dykes N., Johnson O., Bamford P. Assessing the psychological impact of COVID-19 on intensive care workers: a single-centre cross-sectional UK-based study. Pediatr. Crit. Care Med. 2022;23:132–138. doi: 10.1177/1751143720983182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ergai A., Spiva L., Li L., Breshears R., Zhan G. Perceptions of risk, work, and lifestyle changes on mental health of healthcare workers amidst the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2022;19 doi: 10.3390/ijerph19095420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essadek A., Gressier F., Robin M., Shadili G., Bastien L., Peronnet J.-.C., Falissard B., Rabeyron T. Mental health of medical students during the COVID19: impact of studies years. J Affect Disord Rep. 2022;8 doi: 10.1016/j.jadr.2022.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falasi B.al, al Falasi B., al Mazrouei M., al Ali M., al Dhamani M., al Ali A., al Kindi M., Dalkilinc M., al Qubaisi M., Campos L.A., al Tunaiji H., Baltatu O.C. Prevalence and determinants of immediate and long-term PTSD consequences of coronavirus-related (CoV-1 and CoV-2) pandemics among healthcare professionals: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health. 2021 doi: 10.3390/ijerph18042182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan F.C., Zhang S.Y., Cheng Y. Incidence of psychological illness after coronavirus outbreak: a meta-analysis study. J. Epidemiol. Community Health. 2021;75:836–842. doi: 10.1136/jech-2020-215927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattori A., Cantù F., Comotti A., Tombola V., Colombo E., Nava C., Bordini L., Riboldi L., Bonzini M., Brambilla P. Hospital workers mental health during the COVID-19 pandemic: methods of data collection and characteristics of study sample in a university hospital in Milan (Italy) BMC Med. Res. Methodol. 2021 doi: 10.1186/s12874-021-01355-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Tracy M., Norris F., Coffey S.F. Financial and social circumstances and the incidence and course of PTSD in Mississippi during the first two years after Hurricane Katrina. J. Trauma. Stress. 2008;21:357–368. doi: 10.1002/jts.20355. [DOI] [PubMed] [Google Scholar]
- Gates D.M., Gillespie G.L., Succop P. Violence against nurses and its impact on stress and productivity. Nurs. Econ. 2011;29:59–66. quiz 67. [PubMed] [Google Scholar]
- Geng S., Zhou Y., Zhang W., Lou A., Cai Y., Xie J., Sun J., Zhou W., Liu W., Li X. The influence of risk perception for COVID-19 pandemic on posttraumatic stress disorder in healthcare workers: a survey from four designated hospitals. Clin. Psychol. Psychother. 2021;28:1146–1159. doi: 10.1002/cpp.2564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilleen J., Santaolalla A., Valdearenas L., Salice C., Fusté M. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open. 2021 doi: 10.1192/bjo.2021.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold S.D., Marx B.P., Soler-Baillo J.M., Sloan D.M. Is life stress more traumatic than traumatic stress? J. Anxiety Disord. 2005 doi: 10.1016/j.janxdis.2004.06.002. [DOI] [PubMed] [Google Scholar]
- Gorini A., Fiabane E., Sommaruga M., Barbieri S., Sottotetti F., La Rovere M.T., Tremoli E., Gabanelli P. Mental health and risk perception among Italian healthcare workers during the second month of the Covid-19 pandemic. Arch. Psychiatr. Nurs. 2020;34:537–544. doi: 10.1016/j.apnu.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene T., Harju-Seppänen J., Adeniji M., Steel C., Grey N., Brewin C.R., Bloomfield M.A., Billings J. Predictors and rates of PTSD, depression and anxiety in UK frontline health and social care workers during COVID-19. 2021. [DOI] [PMC free article] [PubMed]
- Guo X., McCutcheon R., Pillinger T., Arumuham A., Chen J., Ma S., Yang J., Wang Y., Hu S., Wang G., Liu Z.-.C. Acute psychological impact of coronavirus disease 2019 outbreak among psychiatric professionals in China: a multicentre, cross-sectional, web-based study. BMJ Open. 2021 doi: 10.1136/bmjopen-2020-047828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajure M., Dibaba B., Shemsu S., Desalegn D., Reshad M., Mohammedhussein M. Psychological distress among health care workers in health facilities of Mettu town during COVID-19 outbreak, South West Ethiopia, 2020. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.574671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasanvandi S., Saadat S.H., Shahyad S. Predicting the possibility of post-traumatic stress disorder based on demographic variables, levels of exposure to Covid-19, Covid-19 anxiety and sleep quality dimensions in health care workers. Trauma Mon. 2022;27:8–17. [Google Scholar]
- Hidaka Y., Sasaki N., Imamura K., Tsuno K., Kuroda R., Kawakami N. Changes in fears and worries related to COVID-19 during the pandemic among current employees in Japan: a 5-month longitudinal study. Public Health. 2021;198:69–74. doi: 10.1016/j.puhe.2021.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honarmand K., Yarnell C.J., Young-Ritchie C., Maunder R., Priestap F., Abdalla M., Ball I.M., Basmaji J., Bell C.M., Jeffs L., Shah S., Chen J., LeBlanc D., Kayitesi J., Eta-Ndu C., Mehta S. Personal, professional, and psychological impact of the COVID-19 pandemic on hospital workers: a cross-sectional survey. PLoS ONE. 2022;17 doi: 10.1371/journal.pone.0263438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong X., Cao J., Wei J., Duan Y., Zhao X., Jiang J., Jiang Y., Geng W., Zhu H. Stress and psychological impact of the COVID-19 outbreak on the healthcare staff at the fever clinic of a tertiary general hospital in Beijing: a cross-sectional study. BJPsych Open. 2021;7:e76. doi: 10.1192/bjo.2021.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huarcaya-Victoria J., Elera-Fitzcarrald C., Crisol-Deza D., Villanueva-Zúñiga L., Pacherres A., Torres A., Huertas G., Calderón D., Noriega-Baella C., Astonitas E., Salvador-Carrillo J. Factors associated with mental health in Peruvian medical students during the COVID-19 pandemic: a multicentre quantitative study. Rev. Colomb. Psiquiatr. 2021 doi: 10.1016/j.rcp.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huarcaya-Victoria J., Podestá A., Rojas W. Factors associated with distress among medical staff during the initial phase of the COVID-19 pandemic in Peru. Int. J. Ment. Health Addict. 2022:1–10. doi: 10.1007/s11469-022-00804-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ide K., Asami T., Suda A., Yoshimi A., Fujita J., Nomoto M., Roppongi T., Hino K., Takahashi Y., Watanabe K., Shimada T., Hamasaki T., Endo E., Kaneko T., Suzuki M., Kubota K., Saigusa Y., Kato H., Odawara T., Nakajima H., Takeuchi I., Goto T., Aihara M., Hishimoto A. The psychological effects of COVID-19 on hospital workers at the beginning of the outbreak with a large disease cluster on the Diamond Princess cruise ship. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0245294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ifthikar Z., Fakih S.S., Johnson S., Alex J. Post-traumatic stress disorder following COVID-19 pandemic among medical students in Riyadh: a cross-sectional study. Middle East Curr. Psychiatry. 2021 doi: 10.1186/s43045-021-00127-3. [DOI] [Google Scholar]
- Ilias I., Mantziou V., Vamvakas E., Kampisiouli E., Theodorakopoulou M., Vrettou C., Douka E., Vassiliou A.G., Orfanos S., Kotanidou A., Dimopoulou I. Post-traumatic stress disorder and burnout in healthcare professionals during the SARS-CoV-2 pandemic: a cross-sectional study. J Crit Care Med (Targu Mures) 2021;7:14–20. doi: 10.2478/jccm-2020-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang O.-.J., Chung Y.-.I., Lee J.-.W., Kim H.-.C., Seo J.S. Emotional distress of the COVID-19 cluster infection on health care workers working at a National Hospital in Korea. J. Korean Med. Sci. 2021 doi: 10.3346/jkms.2021.36.e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal K., Deriba B.S., Geleta T.A. Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa Zone. Oromiya Region. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.628898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji Z., Han W., Deng Z., Lu K. Distress, appraisal, and coping among the frontline healthcare provider redeployed to the epicenter in China during COVID-19 pandemic. Front. Psychol. 2021 doi: 10.3389/fpsyg.2021.678369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson S.U., Ebrahimi O.V., Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones, P.J., McNally, R.J., 2022. Does broadening one's concept of trauma undermine resilience? https://doi.org/10.31234/osf.io/5ureb. [DOI] [PubMed]
- Joseph, K., 2021. COVID-19: pandemic increases PTSD, suicidal ideation in health care workers [WWW Document]. Psychiatry Advisor. URL https://www.psychiatryadvisor.com/home/conference-highlights/apa-2021/health-care-workers-reported-increased-rates-of-depression-anxiety-and-stress-during-the-covid-19-pandemic/(accessed 10.1.22).
- Jo S.-.H., Koo B.-.H., Seo W.-.S., Yun S.-.H., Kim H.-.G. The psychological impact of the coronavirus disease pandemic on hospital workers in Daegu, South Korea. Compr. Psychiatry. 2020;103 doi: 10.1016/j.comppsych.2020.152213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan Y., Yuanyuan C., Qiuxiang Y., Cong L., Xiaofeng L., Yundong Z., Jing C., Peifeng Q., Yan L., Xiaojiao X., Yujie L. Psychological distress surveillance and related impact analysis of hospital staff during the COVID-19 epidemic in Chongqing. China. Compr. Psychiatry. 2020;103 doi: 10.1016/j.comppsych.2020.152198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karanikola M., Giannakopoulou M., Mpouzika M., Kaite C.P., Tsiaousis G.Z., Papathanassoglou E.D.E. Dysfunctional psychological responses among intensive care unit nurses: a systematic review of the literature. Rev. Esc. Enferm. USP. 2015;49:847–857. doi: 10.1590/S0080-623420150000500020. [DOI] [PubMed] [Google Scholar]
- Kiefer M.K., Mehl R.R., Venkatesh K.K., Costantine M.M., Rood K.M. High frequency of posttraumatic stress symptoms among US obstetrical and gynecologic providers during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. 2021;224:410–413. doi: 10.1016/j.ajog.2020.12.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koltai J., Raifman J., Bor J., McKee M., Stuckler D. COVID-19 vaccination and mental health: a difference-in-difference analysis of the understanding America study. Am. J. Prev. Med. 2022;62:679–687. doi: 10.1016/j.amepre.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar R., Kumar H., Kumari R., Dars J., Qureshi S., Ameer Hamza M., Khoso A.B., Mubeen S.M. The impact of Covid-19 on medical students: a cross sectional survey. Pak. J. Med. Health Sci. 2021 doi: 10.53350/pjmhs2115112905. [DOI] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamiani G., Borghi L., Poli S., Razzini K., Colosio C., Vegni E. Hospital employees’ well-being six months after the COVID-19 outbreak: results from a psychological screening program in Italy. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18115649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange M., Licaj I., Boulouard M., Garon D., Richard E., Le Bas J., Salmon R., Stroiazzo R., Le Bas F., Humbert X. Psychological impact of the COVID-19 outbreak in community pharmacists: a longitudinal study. J. Am. Pharm. Assoc. 2022;62:1359–1363. doi: 10.1016/j.japh.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Amaddeo F., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Bonetto C. Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open. 2021 doi: 10.1136/bmjopen-2020-045127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Bonetto C., Porru S., Carta A., Tardivo S., Bovo C., Ruggeri M., Amaddeo F. Psychological impact of COVID-19 pandemic on healthcare workers in a highly burdened area of north-east Italy. Epidemiol. Psychiatr. Sci. 2021 doi: 10.1017/s2045796020001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasalvia A., Rigon G., Rugiu C., Negri C., Del Zotti F., Amaddeo F., Bonetto C. The psychological impact of COVID-19 among primary care physicians in the province of Verona, Italy: a cross-sectional study during the first pandemic wave. Fam. Pract. 2022;39:65–73. doi: 10.1093/fampra/cmab106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent A., Fournier A., Lheureux F., Poujol A.-.L., Deltour V., Ecarnot F., Meunier-Beillard N., Loiseau M., Binquet C., Quenot J.-.P. Risk and protective factors for the possible development of post-traumatic stress disorder among intensive care professionals in France during the first peak of the COVID-19 epidemic. Eur. J. Psychotraumatol. 2022;13 doi: 10.1080/20008198.2021.2011603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- León Rojas D., Castorena Torres F., Garza Ornelas B., Rodríguez-de-Ita J. Mental health outcomes and risk factors among female physicians during the COVID-19 pandemic. Heliyon. 2022;8:e09325. doi: 10.1016/j.heliyon.2022.e09325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Su Q., Li X., Peng Y., Liu Y. COVID-19 negatively impacts on psychological and somatic status in frontline nurses. J. Affect. Disord. 2021;294:279–285. doi: 10.1016/j.jad.2021.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xu Y., Cai L., Ma S., Wang Y., Cai Z., Du H., Li R., Kang L., Zheng H., Liu Z., Zhang B. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J. Psychiatr. Res. 2021;137:393–400. doi: 10.1016/j.jpsychires.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Li S., Xiang M., Fang Y., Qian K., Xu J., Li J., Zhang Z., Wang B. The prevalence and risk factors of PTSD symptoms among medical assistance workers during the COVID-19 pandemic. J. Psychosom. Res. 2020;139 doi: 10.1016/j.jpsychores.2020.110270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luceño-Moreno L., Talavera-Velasco B., García-Albuerne Y., Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17155514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum A., Goh Y.-.L., Wong K.S., Seah J., Teo G., Ng J.Q., Abdin E., Hendricks M.M., Tham J., Nan W., Fung D. Impact of COVID-19 on the mental health of Singaporean GPs: a cross-sectional study. BJGP Open. 2021;5 doi: 10.3399/BJGPO.2021.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo D., Liu Q., Chen Q., Huang R., Chen P., Yang B.X., Liu Z. Mental health status of the general public, frontline, and non-frontline healthcare providers in the early stage of COVID-19. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.553021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magalhaes E., Stoner A., Palmer J., Schranze R., Grandy S., Amin S., Cheng N. An assessment of mental health outcomes during the COVID-19 pandemic. Community Ment. Health J. 2021;57:1267. doi: 10.1007/s10597-021-00876-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manh Than H., Minh Nong V., Trung Nguyen C., Phu Dong K., Ngo H.T., Thu Doan T., Thu Do N., Huyen Thi Nguyen T., Van Do T., Xuan Dao C., Quang Nguyen T., Ngoc Pham T., Duy Do C. Mental health and health-related quality-of-life outcomes among frontline health workers during the peak of COVID-19 outbreak in Vietnam: a cross-sectional study. Risk Manag. Healthc. Policy. 2020;13:2927–2936. doi: 10.2147/RMHP.S280749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcomini I., Agus C., Milani L., Sfogliarini R., Bona A., Castagna M. COVID-19 and post-traumatic stress disorder among nurses: a descriptive cross-sectional study in a COVID hospital. Med. Lav. 2021;112:241. doi: 10.23749/mdl.v112i3.11129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín J., Padierna Á., Villanueva A., Quintana J.M. Evaluation of the mental health of health professionals in the COVID-19 era. What mental health conditions are our health care workers facing in the new wave of coronavirus? Int. J. Clin. Pract. 2021;75:e14607. doi: 10.1111/ijcp.14607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marvaldi M., Mallet J., Dubertret C., Moro M.R., Guessoum S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021;126:252–264. doi: 10.1016/j.neubiorev.2021.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meena J., Dhiman S., Sharma R., Kumari K., Singhal S., Kulshrestha V., Vatsa R., Perumal V. The impact of the COVID-19 pandemic on the psychological well-being of healthcare workers in obstetrics and gynaecology: an observational study at an Apex Institute. Cureus. 2022;14:e24040. doi: 10.7759/cureus.24040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S., Machado F., Kwizera A., Papazian L., Moss M., Azoulay É., Herridge M. COVID-19: a heavy toll on health-care workers. Lancet Respir. Med. 2021;9:226–228. doi: 10.1016/S2213-2600(21)00068-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta S., Yarnell C., Shah S., Dodek P., Parsons-Leigh J., Maunder R., Kayitesi J., Eta-Ndu C., Priestap F., LeBlanc D., Chen J., Honarmand K., Canadian Critical Care Trials Group The impact of the COVID-19 pandemic on intensive care unit workers: a nationwide survey. Can. J. Anaesth. 2022;69:472–484. doi: 10.1007/s12630-021-02175-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirzaei A., Molaei B., Habibi-Soola A. Post-traumatic stress disorder and its related factors in nurses caring for COVID-19 patients. Iran. J. Nurs. Midwifery Res. 2022;27:106–111. doi: 10.4103/ijnmr.ijnmr_456_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moderato L., Lazzeroni D., Oppo A., Dell'Orco F., Moderato P., Presti G. Acute stress response profiles in health workers facing SARS-CoV-2. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.660156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulatu H.A., Tesfaye M., Woldeyes E., Bayisa T., Fisseha H., Kassu R.A. The prevalence of common mental disorders among healthcare professionals during the COVID-19 pandemic at a tertiary Hospital in Addis Ababa. Ethiopia. J. Affect. Disord. Reports. 2021 doi: 10.1016/j.jadr.2021.100246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murad M.H., Sultan S., Haffar S., Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid.-Based Med. 2018 doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naheed A., Ahmed A., Choudhary Z.I., Fatima S., Naseem S., Ghias M. COVID-19 pandemic: psychological stress and coping strategies among doctors. Pak. J. Med. Health Sci. 2021 doi: 10.53350/pjmhs211592504. [DOI] [Google Scholar]
- National Center for PTSD, n.d. PTSD: National Center for PTSD [WWW Document]. URL https://www.ptsd.va.gov/(accessed 9.3.22).
- Nemeroff C.B., Marmar C. Oxford University Press; 2018. Post-Traumatic Stress Disorder. [Google Scholar]
- Nguyen P.T.L., Nguyen T.B.L., Pham A.G., Duong K.N.C., Gloria M.A.J., Van Vo T., Van Vo B., Phung T.L. Psychological stress risk factors, concerns and mental health support among health care workers in Vietnam during the coronavirus disease 2019 (COVID-19) outbreak. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.628341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T.T., Le X.T.T., Nguyen N.T.T., Nguyen Q.N., Le H.T., Pham Q.T., Ta N.K.T., Nguyen Q.T., Nguyen A.N., Hoang M.T., Pham H.Q., Vu L.G., Luong A.M., Koh D., Nguyen T.H., Tran B.X., Latkin C.A., Ho C.S.H., Ho R.C.M. Psychosocial impacts of COVID-19 on healthcare workers during the nationwide partial lockdown in Vietnam in april 2020. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.562337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norful A.A., Rosenfeld A., Schroeder K., Travers J.L., Aliyu S. Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. Gen. Hosp. Psychiatry. 2021;69:20–26. doi: 10.1016/j.genhosppsych.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouyang H., Geng S., Zhou Y., Wang J., Zhan J., Shang Z., Jia Y., Yan W., Zhang Y., Li X., Liu W. The increase of PTSD in front-line health care workers during the COVID-19 pandemic and the mediating role of risk perception: a one-year follow-up study. Transl. Psychiatry. 2022;12:180. doi: 10.1038/s41398-022-01953-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. 2021;74:790–799. doi: 10.1016/j.rec.2021.07.010. [DOI] [PubMed] [Google Scholar]
- Pan, L., Xu, Q., Kuang, X., Zhang, X., Fang, F., Gui, L., Li, M., Tefsen, B., Zha, L., Liu, H., 2021. Prevalence and factors associated with post-traumatic stress disorder in healthcare workers exposed to COVID-19 in Wuhan, China: a cross-sectional survey. https://doi.org/10.21203/rs.3.rs-593920/v1. [DOI] [PMC free article] [PubMed]
- Pappa S., Athanasiou N., Sakkas N., Patrinos S., Sakka E., Barmparessou Z., Tsikrika S., Adraktas A., Pataka A., Migdalis I., Gida S., Katsaounou P. From recession to depression? Prevalence and correlates of depression, anxiety, traumatic stress and burnout in healthcare workers during the COVID-19 pandemic in Greece: a multi-center, cross-sectional study. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18052390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V.G., Papoutsi, E., Katsaounou, P., 2020 Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. SSRN electronic journal. 10.2139/ssrn.3594632. [DOI] [PMC free article] [PubMed]
- Prasad A., Civantos A.M., Byrnes Y., Chorath K., Poonia S., Chang C., Graboyes E.M., Bur A.M., Thakkar P., Deng J., Seth R., Trosman S., Wong A., Laitman B.M., Shah J., Stubbs V., Long Q., Choby G., Rassekh C.H., Thaler E.R., Rajasekaran K. Snapshot impact of COVID-19 on mental wellness in nonphysician otolaryngology health care workers: a national study. OTO Open. 2020;4 doi: 10.1177/2473974X20948835. 2473974X20948835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasad K., McLoughlin C., Stillman M., Poplau S., Goelz E., Taylor S., Nankivil N., Brown R., Linzer M., Cappelucci K., Barbouche M., Sinsky C.A. Prevalence and correlates of stress and burnout among U.S. healthcare workers during the COVID-19 pandemic: a national cross-sectional survey study. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., Di Pierro R., Madeddu F., Calati R. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr. Psychiatry Rep. 2020 doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi G., Yuan P., Qi M., Hu X., Shi S., Shi X. Influencing factors of high PTSD among medical staff during COVID-19: evidences from both meta-analysis and subgroup analysis. Saf. Health Work. 2022;13:269–278. doi: 10.1016/j.shaw.2022.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X., Lan Y., Miao J., Wang H., Wang H., Wu J., Li G., Zhao X., Cao Z., Mei J., Sun W., Zhu Z., Zhu S., Wang W. A comparative study on the psychological health of frontline health workers in Wuhan under and after the lockdown. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.701032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranieri J., Guerra F., Perilli E., Passafiume D., Maccarone D., Ferri C., Di Giacomo D. Prolonged COVID 19 outbreak and psychological response of nurses in Italian healthcare system: cross-sectional study. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.608413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riello M., Purgato M., Bove C., MacTaggart D., Rusconi E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. R. Soc. Open Sci. 2020;7 doi: 10.1098/rsos.200880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles R., Rodríguez E., Vega-Ramírez H., Álvarez-Icaza D., Madrigal E., Durand S., Morales-Chainé S., Astudillo C., Real-Ramírez J., Medina-Mora M.-.E., Becerra C., Escamilla R., Alcocer-Castillejos N., Ascencio L., Díaz D., González H., Barrón-Velázquez E., Fresán A., Rodríguez-Bores L., Quijada-Gaytán J.-.M., Zabicky G., Tejadilla-Orozco D., González-Olvera J.-.J., Reyes-Terán G. Mental health problems among healthcare workers involved with the COVID-19 outbreak. Braz. J. Psychiatry. 2021;43:494–503. doi: 10.1590/1516-4446-2020-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L., Lee S., Jenkins P., Arbet J., Carrington S., Hoon S., Purcell S.K., Nodine P. A survey of mental health in graduate nursing students during the COVID-19 pandemic. Nurse Educ. 2021;46:215–220. doi: 10.1097/NNE.0000000000001013. [DOI] [PubMed] [Google Scholar]
- Rouse R., Regan J. Psychological impact of COVID-19 on speech and language therapists working with adult dysphagia: a national survey. Int. J. Lang. Commun. Disord. 2021;56:1037–1052. doi: 10.1111/1460-6984.12654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachdeva A., Nandini H., Kumar V., Chawla R.K., Chopra K. From stress to stigma – Mental health considerations of health care workers involved in COVID19 management. Indian J. Tubercul. 2021 doi: 10.1016/j.ijtb.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin S.K., Arslan E., Atalay Ü.M., Demir B., Elboga G., Altındağ A. Psychological impact of COVID-19 outbreak on health workers in a university hospital in Turkey. Psychol. Health Med. 2022 doi: 10.1080/13548506.2021.1900578. [DOI] [PubMed] [Google Scholar]
- Salehi M., Amanat M., Mohammadi M., Salmanian M., Rezaei N., Saghazadeh A., Garakani A. The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: a systematic-review and meta-analysis. J. Affect. Disord. 2021;282:527–538. doi: 10.1016/j.jad.2020.12.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanghera J., Pattani N., Hashmi Y., Varley K.F., Cheruvu M.S., Bradley A., Burke J.R. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—a systematic review. J. Occup. Health. 2020 doi: 10.1002/1348-9585.12175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarapultseva M., Zolotareva A., Kritsky I., Nasretdinova N.’ya, Sarapultsev A. Psychological distress and post-traumatic symptomatology among dental healthcare workers in russia: results of a pilot study. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18020708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah J., Monroe-Wise A., Talib Z., Nabiswa A., Said M., Abeid A., Ali Mohamed M., Mohamed S., Ali S.K. Mental health disorders among healthcare workers during the COVID-19 pandemic: a cross-sectional survey from three major hospitals in Kenya. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobregrau Sangrà P., Aguiló Mir S., Castro Ribeiro T., Esteban-Sepúlveda S., García Pagès E., López Barbeito B., Pomar Moya-Prats J.L., Pintor Pérez L., Aguiló Llobet J. Mental health assessment of Spanish healthcare workers during the SARS-CoV-2 pandemic. A cross-sectional study. Compr. Psychiatry. 2022;112 doi: 10.1016/j.comppsych.2021.152278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Styra R., Hawryluck L., Mc Geer A., Dimas M., Sheen J., Giacobbe P., Dattani N., Lorello G., Rac V.E., Francis T., Wu P.E., Luk W.-.S., Ng E., Nadarajah J., Wingrove K., Gold W.L. Surviving SARS and living through COVID-19: healthcare worker mental health outcomes and insights for coping. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0258893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun P., Wang M., Song T., Wu Y., Luo J., Chen L., Yan L. The psychological impact of COVID-19 pandemic on health care workers: a systematic review and meta-analysis. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.626547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tebbeb N., Villemagne F., Prieur T., Dorier S., Fort E., Célarier T., Fontana L., Barth N., Pélissier C. COVID-19 health crisis workloads and screening for psychological impact in nursing home staff: a qualitative and quantitative survey. Int. J. Environ. Res. Public Health. 2022 doi: 10.3390/ijerph19074061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topal S., Yilmaz O., Ceylan G., Sandal O.S., Karaarslan U., Atakul G., Colak M., Soydan E., Seven P., Caliskan Polat A., Agin H. The effect of COVID-19 outbreak on the mental status of health care professionals in the pediatric intensive care unit. Psychiatr. Danub. 2021;33:364–371. [PubMed] [Google Scholar]
- Udgiri R.S., Biradar S.G., Shannawaz M. Assessing impact event scale of post-traumatic stress disorder of covid-19 pandemic among postgraduates working at tertiary care hospital — a cross-sectional study. J. Indian Med. Assoc. 2021:19–23. [Google Scholar]
- Umberger R. What is the best core measure after critical illness when the IES-R is no longer accessible for new researchers? Crit. Care. 2019 doi: 10.1186/s13054-019-2595-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Wert M.J., Gandhi S., Gupta I., Singh A., Eid S.M., Haroon Burhanullah M., Michtalik H., Malik M. Healthcare worker mental health after the initial peak of the COVID-19 pandemic: a US medical center cross-sectional survey. J. Gen. Intern. Med. 2022;37:1169–1176. doi: 10.1007/s11606-021-07251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlah Tomičević S., Lang V.B. Psychological outcomes amongst family medicine healthcare professionals during COVID-19 outbreak: a cross-sectional study in Croatia. Eur. J. Gen. Pract. 2021;27:184–190. doi: 10.1080/13814788.2021.1954154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadasadawala T., Kumar A., Laskar S.G., Gondhowiardjo S., Mokal S., Goswami S., Giselvania A., Kapoor R., Das A., Pradhan S., Pujari L., Acharya B., Chapagain S., Mahantshetty U., Vadgaonkar R., Hussain Q.M., Akbarov K., Agarwal J.P. Multinational study to assess stress levels among the health care workers of radiation oncology community at the outset of the COVID-19 pandemic. JCO Glob Oncol. 2021;7:464–473. doi: 10.1200/GO.20.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Ma S., Yang C., Cai Z., Hu S., Zhang B., Tang S., Bai H., Guo X., Wu J., Du H., Kang L., Tan H., Li R., Yao L., Wang G., Liu Z. Acute psychological effects of coronavirus disease 2019 outbreak among healthcare workers in China: a cross-sectional study. Transl. Psychiatry. 2020 doi: 10.1038/s41398-020-01031-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanigasooriya K., Palimar P., Naumann D.N., Ismail K., Fellows J.L., Logan P., Thompson C.V., Bermingham H., Beggs A.D., Ismail T. Mental health symptoms in a cohort of hospital healthcare workers following the first peak of the COVID-19 pandemic in the UK. BJPsych Open. 2021 doi: 10.1192/bjo.2020.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W. DSM-5 diagnostic criteria for PTSD. Oxford Med. Online. 2018 doi: 10.1093/med/9780190259440.003.0002. [DOI] [Google Scholar]
- Wells, G., Shea, B., O'Connell, D., Peterson, J., Welch, Losos, M., Tugwell, P., Ga, S.W., Zello, G., Petersen, J., 2014. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- WHO Coronavirus Disease (COVID-19) Dashboard, 2020. Bangladesh physiotherapy journal. https://doi.org/10.46945/bpj.10.1.03.01.
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia L., Yan Y., Wu D. Protective predictors associated with posttraumatic stress and psychological distress in Chinese nurses during the outbreak of COVID-19. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.684222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X., Chen D., Chen Y., Wang N., Lyv C., Li Y., Jie J., Zhou T., Li Y., Zhou P. Geographical distribution and prevalence of mental disorders among healthcare workers in China: a cross-sectional country-wide survey. Int. J. Health Plann. Manage. 2021 doi: 10.1002/hpm.3186. [DOI] [PubMed] [Google Scholar]
- Yin Q., Chen A., Song X., Deng G., Dong W. Risk perception and PTSD symptoms of medical staff combating against COVID-19: a PLS structural equation model. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.607612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin Q., Sun Z., Liu T., Ni X., Deng X., Jia Y., Shang Z., Zhou Y., Liu W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin. Psychol. Psychother. 2020;27:384–395. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yitayih Y., Mekonen S., Zeynudin A., Mengistie E., Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. 2020;7:e1. doi: 10.1192/bjo.2020.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K., Gong Y.-.M., Liu L., Sun Y.-.K., Tian S.-.S., Wang Y.-.J., Zhong Y., Zhang A.-.Y., Su S.-.Z., Liu X.-.X., Zhang Y.-.X., Lin X., Shi L., Yan W., Fazel S., Vitiello M.V., Bryant R.A., Zhou X.-.Y., Ran M.-.S., Bao Y.-.P., Shi J., Lu L. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Mol. Psychiatry. 2021;26:4982–4998. doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zakeri M.A., Hossini Rafsanjanipoor S.M., Zakeri M., Dehghan M. The relationship between frontline nurses’ psychosocial status, satisfaction with life and resilience during the prevalence of COVID-19 disease. Nurs Open. 2021;8:1829–1839. doi: 10.1002/nop2.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zara G., Settanni M., Zuffranieri M., Veggi S., Castelli L. The long psychological shadow of COVID-19 upon healthcare workers: a global concern for action. J. Affect. Disord. 2021 doi: 10.1016/j.jad.2021.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Hou T., Kong X., Wang G., Wang H., Xu S., Xu J., He J., Xiao L., Wang Y., Du J., Huang Y., Su T., Tang Y. PTSD among healthcare workers during the COVID-19 outbreak: a study raises concern for non-medical staff in low-risk areas. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.696200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Sun Z., Wang Y., Xing C., Sun L., Shang Z., Liu W. The prevalence of PTSS under the influence of public health emergencies in last two decades: a systematic review and meta-analysis. Clin. Psychol. Rev. 2021;83 doi: 10.1016/j.cpr.2020.101938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Z., Xu S., Wang H., Liu Z., Wu J., Li G., Miao J., Zhang C., Yang Y., Sun W., Zhu S., Fan Y., Chen Y., Hu J., Liu J., Wang W. COVID-19 in Wuhan: sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24 doi: 10.1016/j.eclinm.2020.100443. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.