Abstract
Experiences of child abuse and neglect are risk factors for youth suicidal thoughts and behaviors. Accordingly, suicide risk may emerge as a developmental process that is heavily influenced by the rearing environment. We argue that a developmental, theoretical framework is needed to guide future research on child maltreatment and youth (i.e., adolescent and emerging adult) suicide, and to subsequently inform suicide prevention efforts. We propose a developmental model that integrates principles of developmental psychopathology and current theories of suicide to explain the association between child maltreatment and youth suicide risk. This model bears significant implications for future research on child maltreatment and youth suicide risk, and for suicide prevention efforts that target youth with child maltreatment experiences.
Keywords: adverse childhood experiences, child maltreatment, suicide prevention, trauma, youth suicide
Preventing youth suicide is an urgent public health need. Suicide is the second cause of death for young people aged 15–24, and reports of suicidal thoughts and behaviors (STBs) have risen in the past 10 years (Curtin & Heron, 2019; Kann et al., 2018). Data from both self-reported and clinical assessments suggest that maltreated youth are more likely to consider and attempt suicide (Angelakis et al., 2020; Norman et al., 2012). A recent meta-analysis showed young people who experienced any type of child abuse or neglect were 2.91 times more likely to attempt suicide and 2.36 times more likely to have suicidal ideation compared to their non-maltreated counterparts, respectively (Angelakis et al., 2020). The prevalence of child maltreatment in the United States is substantial, making its impact on youth suicide alarming. There were over 3.4 million children involved in a child maltreatment investigation in the United States in 2019 (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, 2021). Further, estimates show 37.4% of US youth are involved in a child maltreatment investigation by the time they reach age 18 (Kim et al., 2017). Globally, the World Health Organization (2020) estimates approximately one billion children aged 2–17 experience violence such as child maltreatment each year. Thus, suicide prevention for maltreated youth globally is an urgent public health problem.
A large body of research exists on the associations between child maltreatment and suicide risk (for a review, see Miller et al., 2013), but scientists have yet to consolidate this body of knowledge into a conceptual model to guide research and prevention in this area. In the present paper, we argue that suicide prevention for maltreated youth will benefit from integrating theories of suicide with developmental perspectives, which give attention to age-specific mechanisms and antecedents of STBs in this vulnerable youth population. While current theoretical models of suicide (e.g., the interpersonal theory of suicide) specify the causal mechanisms that underlie STBs among adult samples, they have largely not integrated developmental perspectives on youth suicide.
A developmental lens is essential for understanding the etiology between child maltreatment and STBs during adolescence, specifically. Adolescence is a developmental period wherein young people undergo multiple changes at the biological, psychological, and interpersonal levels (e.g., puberty, the development of romantic relationships, and transitioning to spending more time with peers than family members). There is evidence that adolescence is a sensitive period in development with heightened brain plasticity (Fuhrmann et al., 2015). This makes adolescence both a time of vulnerability and opportunity. While adolescents are often at risk for the onset of mental health disorders (Kessler et al., 2005), heightened plasticity during this time confers a “window of opportunity” for preventive programs that build upon youth strengths to prevent suicide (Wyman, 2014).
Overall, a developmental model of the link between child maltreatment and youth suicide will contribute to this research area by offering (a) hypothesized mechanisms underlying the link between child maltreatment and youth suicide; (b) hypothesized risk and protective factors for youth STBs; and (c) implications for preventative efforts. Specifying the role of child maltreatment in the developmental processes leading to youth STBs, as opposed to the role of other childhood adversities (e.g., poverty, parental incarceration, divorce), is an important endeavor due to the unique nature of child maltreatment as a toxic interpersonal stressor and the salience of interpersonal stressors in the etiology of STBs (Van Orden et al., 2010). Children exposed to maltreatment not only experience extreme and often chronic stress, but often do so at the hands of their primary or secondary attachment figures. Ultimately, an integrative developmental conceptual model of the link between child maltreatment and youth suicide will inform targeted prevention efforts to reduce the rates of STBs among youth with child maltreatment experiences.
Consequently, in this paper we will outline the current knowledge on child maltreatment and youth suicide and review the theoretical frameworks that guide our conceptual model, which are primarily the developmental psychopathology perspective and ideation-to-action theories of suicide. Next, based on the literature and our existing theoretical frameworks, we will propose a developmentally informed conceptual model for the association between child maltreatment and suicide risk. The purpose of this conceptual model is to propose developmental pathways from child maltreatment to youth suicide that are based on the existing literature and relevant theoretical models (McGregor, 2018). Note that we do not intend for this model to be exhaustive nor to present a formal causal theory, but instead to offer insight and future directions for research in this specific area. Last, we will discuss implications of this model for advancing efficacious suicide prevention efforts, with a focus on upstream prevention.
Youth suicidal thoughts and behaviors: definitions and overview
We define STBs as including cognitions or actions (non-fatal or fatal) that involve intent to die. Specifically, suicidal ideation is defined as “thinking about, considering, or planning for suicide” (Crosby et al., 2011, p. 21), suicide attempts are defined as “a non-fatal self-directed potentially injurious behavior with any intent to die as a result of the behavior” (Crosby et al., 2011, p. 21), and suicide as “death caused by self-directed injurious behavior with any intent to die as a result of the behavior” (Crosby et al., 2011, p. 21). Although suicidal ideation, attempts, and suicide are correlated, they differ significantly in etiology and prevalence, and therefore should be investigated separately. Suicidal ideation increases the likelihood of a suicide attempt, but most individuals who think about suicide do not ultimately attempt or die by suicide (Klonsky et al., 2016). For instance, an estimated 12.0 million adults in the United States exhibited suicidal ideation and 1.4 million attempted suicide in the year 2019 (U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, 2020). Thus, informed by recommendations in the suicide literature, we will be referring to suicidal thoughts and suicidal behaviors as separate but related phenomena.
Child maltreatment and suicide risk
Current state of the literature
Direct associations
There is consensus in the literature that child maltreatment experiences heighten the risk for future STBs (for a review, see Miller et al., 2013). Investigators have found significant associations between childhood maltreatment and adolescent suicidal ideation (Fergusson et al., 2000) and attempts (Fergusson et al., 2000; Rhodes et al., 2012) using both cross-sectional (Hoertel et al., 2015) and prospective designs (Fergusson et al., 2000). These results extend to studies with young adults (Dunn et al., 2013; Johnson et al., 2002; Puzia et al., 2014) and adult samples (Dube et al., 2001). In a nationally representative sample of maltreated youth, researchers found that 23% of adolescents reported suicidal ideation (Coohey et al., 2014). Additionally, a study using a population-based Canadian sample found adolescents permanently removed from their homes due to maltreatment were five times more likely to present to the emergency department for STBs, compared to non-maltreated youth (Rhodes et al., 2012).
Mediators
Although the association between child maltreatment and youth STBs is well established, there is less research and subsequently less consensus on the mechanisms of this association. In other words, although we know that child maltreatment confers risk for STBs during adolescence and young adulthood, we have much to learn regarding the developmental processes that underlie this association. Thus, to inform our proposed conceptual model, we conducted a literature review on the mechanisms between child maltreatment and youth STBs (see Table 1 for a summary). This review highlights that the processes in the association between child maltreatment and youth suicide are multi-level in nature, spanning from interpersonal factors (e.g., mother-daughter relationship problems; Handley, Adams, et al., 2019) to psychological factors such as internalizing symptomology (Kwok & Gu, 2019; Paul & Ortin, 2019). In Table 1, we categorized the literature by type of mediator (i.e., biological, psychological, or interpersonal) and type of outcome (i.e., suicidal ideation, suicidal behavior, or a combination). It is clear from our findings that there are notable gaps in the literature. Most studies have focused on individual-level psychopathology or symptomology as mediators. Additionally, most studies use suicidal ideation as a primary outcome, and thus there is a need for more research on mediators linking child maltreatment to suicidal behavior. Additionally, there is a lack of research on biological mechanisms in the association between child maltreatment and youth suicide (as an exception, see Russell et al., 2019).
Table 1.
Identified mediators in the association between child maltreatment and adolescent and young adult STBs
| Suicidal ideation | Suicide attempts or behavior | Combined | |
|---|---|---|---|
| Biological | n/a | n/a | n/a |
| Psychological |
General maltreatment: • Depression and/or depressive symptoms (Cromer et al., 2019*b; Handley, Adams, et al., 2019; Miller et al., 2014*) • Negative emotions (Cho & Glassner, 2020*) Sexual abuse: • Guilt and depressive symptoms (Sekowski et al., 2020) • Depressed mood (Sigfusdottir et al., 2013) • Comorbid internalizing and externalizing symptom trajectory (Duprey et al., 2019b*) Physical abuse: • Psychological distress (Thompson et al., 2012*) • Internalizing problems (Salzinger et al., 2007*; Wan & Leung, 2010) • Externalizing problems (Wan & Leung, 2010) • Guilt and depressive symptoms (Sekowski et al., 2020) • Guilt and shame (Sekowski et al., 2020) Emotional abuse: • Psychological distress (Thompson et al., 2012*) • Self-compassion (Zhang et al., 2020) • Psychache (Li et al., 2019*) • Self-esteem (Duprey et al., 2019a) • Gratitude (Kwok et al., 2019*) Neglect: • Depression and/or depressive symptoms (Kwok & Gu, 2019*; Sekowski et al., 2020) • Depressive/anxious symptoms (Paul & Ortin, 2019*) • Comorbid aggressive and internalizing symptoms (Paul & Ortin, 2019*) • Guilt and depressive symptoms (Sekowski et al., 2020) • Self-compassion (Zhang et al., 2020) |
General maltreatment: • Mental healthcare service utilization (Ammerman et al., 2018*b) • General fatigue and sleep problems (Ammerman et al., 2018*b) • Self-esteem (Ammerman et al., 2018*b) • Poor appetite (Ammerman et al., 2018*b) • Having run away from home (Ammerman et al., 2018*b) Sexual abuse: • Depressed mood or depression (Sigfusdottir et al., 2013) • Bipolar disorder (Barbot et al., 2020*) • Anger (Sigfusdottir et al., 2013) • Comorbid internalizing and externalizing symptom trajectory (Duprey et al., 2019b*) Physical abuse: • Self-esteem (Cero & Sifers, 2013) Emotional abuse: • Mood disorders (Barbot et al., 2020*a) • Psychotic symptoms (Barbot et al., 2020*b) |
General maltreatment: • Emotion dysregulation (Marques-Feixa et al., 2021) Emotional abuse: • PTSD (Tang et al., 2018) • Depression (Tang et al., 2018) • Self-criticism (Falgares et al., 2018) Neglect: • Depression (Tang et al., 2018) • Self-criticism (Falgares et al., 2018) |
| Interpersonal |
General maltreatment: • Mother-daughter relationship quality (Handley, Adams, et al., 2019) • Mother-daughter conflict (Handley, Adams, et al., 2019) Physical abuse: • Poor family relationships (Wan & Leung, 2010) Emotional abuse: • Perceived burdensomeness (Puzia et al., 2014*) |
General maltreatment: • Interpersonal difficulties (Johnson et al., 2002) • Exposure to peer suicidal behaviors (Ammerman et al., 2018*b) • Relationship closeness and satisfaction with father (Ammerman et al., 2018*b) • Relationship satisfaction with mother (Ammerman et al., 2018*b) |
Note. Emotional abuse includes verbal abuse. Neglect includes physical and emotional neglect. Studies using ACE measures (broadly defined) not included in table.
Studies using longitudinal or prospective designs.
Finding was significant for boys only.
Finding was significant for girls only.
Moderators
Similar to the literature on mediators of child maltreatment and youth suicide, moderators (e.g., risk or protective factors1) in the association between maltreatment and youth STBs range from biological to contextual factors (see Table 2). For example, individual traits such as empathy, problem-solving, and emotional competence have all been found to be protective factors in the association between child maltreatment and youth suicidal ideation in US-based and international samples (Esposito & Clum, 2002; Kwok et al., 2015; Low et al., 2017), while substance use problems were found to amplify this association (Miller & Esposito-Smythers, 2013). At the interpersonal level, there is evidence for protective factors including social support (Esposito & Clum, 2002; Logan-Greene et al., 2017), school belonging (Zhang et al., 2020), and participation in youth activities (Cero & Sifers, 2013). Researchers also note evidence for biological modifying factors, such as the oxytocin genotype (CD38), in the association between child maltreatment and youth STBs (Handley, Warmingham, et al., 2019). However, more research is needed to identify and replicate protective and moderating risk factors that modify the association between child maltreatment and youth STBs. Additionally, there are very few studies investigating protective factors between child maltreatment and suicidal behavior specifically.
Table 2.
Identified moderators in the association between child maltreatment and adolescent and young adult STBs
| Suicidal ideation | Suicide attempts or behavior | |
|---|---|---|
| Biological |
General maltreatment: • 5-HTT polymorphism (l/l genotype of 5-HTTLPR) (Cicchetti, Rogosch, Sturge-Apple, et al., 2010*) • Oxytocin (CD38) polymorphism (Handley, Warmingham, et al., 2019*) Emotional abuse: • Sex (Seff & Stark, 2019a) • Heart rate variability (Duprey et al., 2019a) |
n/a |
| Psychological |
General maltreatment: • Alcohol- and drug-related problems (Miller & Esposito-Smythers, 2013) Sexual abuse: • Problem-solving confidence (Esposito & Clum, 2002) Physical abuse: • Empathy (Kwok et al., 2015) • Social problem-solving (Kwok et al., 2015) • Emotional competence (Low et al., 2017) • Resilience factors (Low et al., 2017) • Problem-solving confidence (Esposito & Clum, 2002) |
General maltreatment: • Attention (Zelazny et al., 2019*b) |
| Interpersonal |
General maltreatment: • Adolescent dating violence (Adams et al., 2021) • Social support (Logan-Greene et al., 2017) Sexual abuse: • Social support satisfaction (Esposito & Clum, 2002) Physical abuse: • Low perceived family functioning (Kwok et al., 2015) Emotional abuse: • School belonging (Zhang et al., 2020) |
Physical abuse: • Participation in youth activities (Cero & Sifers, 2013) Sexual abuse: • Social support satisfaction (Esposito & Clum, 2002c) |
| Other |
General maltreatment: • Access to firearms (Kim, 2020*) |
Sexual abuse: • Degree of relatedness between child and abuser (Brezo et al., 2008*) • Gender (Ammerman et al., 2018*d) |
Note. Emotional abuse includes verbal abuse. Neglect includes physical and emotional neglect. Studies using ACE measures (broadly defined) not included in table.
Studies using longitudinal or prospective designs.
This result was found among adolescents in Kenya but not in the other countries investigated (Haiti, Tanzania).
Outcome measure was suicidal behavior, consisting of actual, attempted, and ambiguous suicide attempts and visits to the emergency room for severe suicidal ideation.
Outcome measure was a composite of suicidal behavior, consisting of behavioral preparation for suicide attempts, efforts to avoid communication about suicide ideation, and lethality of attempt.
The association between child maltreatment and suicide attempts was significant for females but not for males.
The literature suggests the link between child maltreatment and STBs have different etiological mechanisms for boys and girls (e.g., moderation by gender). For example, Ammerman et al. (2018) observed a significant association between child maltreatment and suicide attempts for girls but not boys. Similarly, Cromer et al. (2019) found that depressive symptoms mediated the association between cumulative child maltreatment exposure and suicidal ideation among girls only. Last, Barbot et al. (2020) found that psychosis mediated the association between emotional abuse and suicide attempts for girls only, while mood disorder symptoms mediated this association for boys only.
Current theoretical models of suicide
Research on child maltreatment and youth STBs must be guided by relevant theories in the field of suicidology. Our conceptual model of child maltreatment and youth STBs is specifically guided by the interpersonal theory of suicide (Van Orden et al., 2010), due to the salience of interpersonal stressors for maltreated youth, as well as other ideation-to-action frameworks of suicide (Klonsky & May, 2015). The interpersonal theory of suicide proposes that individuals develop a desire for suicide through two interpersonal processes, thwarted belongingness (i.e., social isolation or lack of social connectedness) and perceived burdensomeness (i.e., the belief that one is a burden to close others, which includes aspects of self-hatred and the belief that one’s life is a liability; Van Orden et al., 2010). Further, an acquired capability for suicide (i.e., learned fearlessness of death and tolerance for pain) is required for suicidal behaviors and suicide to occur. Other ideation-to-action frameworks of suicide similarly propose that the pathways leading to risk for suicidal ideation differ from those leading to suicidal behavior and suicide. For example, according to the three-step theory of suicide, psychological pain and hopelessness are critical explanatory factors for the development of suicidal ideation, while the progression from suicidal ideation to suicidal behavior is explained by one’s capacity to inflict self-injury (Klonsky & May, 2015). We draw from these current theories of suicide in our conceptual model by differentiating the processes leading to suicidal ideation and suicidal behaviors.
In the field of suicidology, the preponderance of theoretical models are based on adult samples and lack a developmental perspective specific to youth suicide risk. Current theories in suicidology such as the ones above suggest the same set of risk and protective factors for suicide for all individuals despite their age and/or developmental stage. Some mechanisms towards suicide (e.g., depression) indeed are most likely the same for all individuals across development. However, other mechanisms and risk and protective factors are likely more salient for adolescents and young adults due to normative developmental changes and the stage-salient developmental tasks during this period. For instance, adolescent risk factors such as a lack of future orientation (i.e., having low or no expectations or goals for one’s future; Oshri, Duprey, et al., 2018) and bullying may not be as relevant for older individuals. Adolescents are also particularly sensitive to acute stress due to normative developmental changes in biological stress response systems, and “failure” of these stress response systems have been proposed as a key risk factor for adolescent suicide (Miller & Prinstein, 2019). These risk factors may be particularly salient for maltreated youth, and may moderate (i.e., exacerbate) the association between maltreatment and youth STBs. Additionally, theories in suicidology tend to be broad and do not specify the hypothesized developmental chain stemming from a triggering event, such as child maltreatment, towards youth STBs.
A developmentally informed model of child maltreatment and youth suicide will contribute to the literature by considering the unique aspects of the developmental period across multiple levels of analysis with the aim of identifying salient risk and protective factors and mechanisms. This will inform research in several ways, including but not limited to measurement (e.g., using appropriate measures for the specific developmental stage being tested), conceptualization (e.g., how concepts are operationalized and tested for adolescents compared to older adults), and study design (e.g., sampling and recruitment). Further, a developmentally informed model of suicide will contribute to applied research by providing developmentally appropriate mechanisms to target in interventions (e.g., targeting attachment processes for children or peer skills among high school students), and by emphasizing that mechanistic targets will be different and must be tuned to participants’ developmental stage. Importantly, the model we present in this paper focuses on child maltreatment as a specific precursor to suicide risk. Thus, our model is specific to maltreated youth and is intended to inform suicide prevention approaches among youth exposed to child abuse and neglect.
A developmental perspective on youth STBs
We utilize a developmental psychopathology perspective to understand and integrate the disparate literature on mechanisms and moderators in the link between child maltreatment and youth STBs, and to inform our conceptual model of the pathways from child maltreatment to youth STBs. Developmental psychopathology is an overarching framework for studying typical and atypical behavior (Cicchetti, 1984). Several core principles of this framework shape our proposed conceptual model, including the principles of equifinality and multifinality. According to the concept of equifinality, the same outcome can be reached through multiple different developmental pathways (Cicchetti & Rogosch, 2002). For example, two adolescents who each exhibit suicidal ideation may have reached that outcome through various developmental risk processes: one may have experienced extreme early childhood neglect, resulting in an insecure attachment relationship that cascaded into mistrust of others, social isolation, and depression; the other may have experienced physical abuse that resulted in externalizing behaviors and impulsivity. These illustrative developmental pathways, although different, each may predict the emergence of STBs during adolescence. Alternatively, according to the concept of multifinality, the same or a similar set of risk factors may result in different processes and outcomes (Cicchetti & Rogosch, 2002). For example, two children who were sexually abused may show distinct outcomes by exhibiting either psychopathology or resilience in adolescence. Different risk factors (e.g., disordered neighborhoods, peer victimization) and protective factors (e.g., peer social support, emotion regulation) contribute to the process of multifinality by modifying (i.e., moderating) the outcomes stemming from child maltreatment, including the developmental processes that are implicated in the pathway from child maltreatment towards youth STBs. Additionally, risk and protective factors at different levels of the youths’ ecology may interact with one another to produce cascading transactional effects that lead to diverse outcomes.
The developmental systems perspective, which has over time been integrated into the developmental psychopathology approach, informs the concepts of multifinality and equifinality (Lerner & Castellino, 2002). According to this perspective, developmental processes emerge from integrating multiple systems, both internal and external to the individual (Lerner & Castellino, 2002). Here, systems are defined as “ . . . a complex of interacting components together with the relationships among them that permit the identification of a boundary-maintaining entity or process” (Laszlo & Krippner, 1998, p. 47). A growing child, in this perspective, is thought of as a developmental system that consists of the elements or subsystems within it (e.g., biological systems) that change over time due to the interactions among internal subsystems and with other outside systems (e.g., the family system). In our conceptual model, we draw from the transactional model of the developmental systems perspective, which posits that human development is the product of interdependent and bidirectional influences between the person and their environment (Sameroff, 2009). Transactions can also occur between different subsystems within the individual. For example, the development and functioning of the stress response system and the immune system may both influence one another bidirectionally over time (Oshri, Duprey, Liu & Ehrlich, 2020; Sameroff, 2009).
The proposed theoretical model was also informed by the organizational theory of development, a core tenet of the developmental psychopathology approach. According to the organizational theory, children must successfully master stage-salient developmental tasks, such as attaining secure attachment with a primary caregiver or gaining a positive self-concept and sense of mastery in early childhood (Cicchetti & Banny, 2014). At each stage of development, the attainment of new developmental tasks requires reorganizing multiple systems within the individual (e.g., physiological, cognitive, and socioemotional). Successful reorganization is necessary to master subsequent tasks in the same developmental domain. Harsh, chaotic, or impoverished rearing environments can lead to failure in mastering critical developmental tasks (Cicchetti & Banny, 2014). Accordingly, children who experience child maltreatment are at risk for STBs due in part to disruption in the attainment of stage-salient tasks.
The aforementioned tenets of the developmental psychopathology and developmental systems frameworks have been integrated into several existing models of youth STBs, including models on the development of borderline personality disorder and self-injurious behaviors (Crowell et al., 2008; Derbridge & Beauchaine, 2014), the developmental-transactional model of youth suicidal behavior (Bridge et al., 2006), and the recent theory of adolescent suicide as a failure of physiological stress response systems (Miller & Prinstein, 2019). Our model adds to this knowledge base by considering the developmental processes involved in the emergence of youth STBs specifically for maltreated youth. Additionally, our conceptual model integrates the developmental psychopathology and developmental systems frameworks with modern theories of suicide, including the interpersonal theory of suicide and other ideation-to-action frameworks of suicide, as detailed prior (Klonsky & May, 2015; Van Orden et al., 2010).
A conceptual model of child maltreatment and youth suicide risk
Based on the literature reviewed above, the developmental psychopathology framework, and ideation-to-action theories in suicidology, we propose a developmental model of the progression from child maltreatment to adolescent STBs (see Figure 1). There are three overarching propositions to this model. First, we suggest three primary, dynamic mechanisms at different levels of analysis (i.e., biological, psychological, and interpersonal) that link child maltreatment to the emergence of STBs in adolescence. These mechanisms are not separate processes, but instead interact with and influence one another over time. Together, in line with the three-step theory of suicide, these biological, psychological, and interpersonal processes may culminate in extreme psychological pain that can prompt youth to desire ending their lives (Klonsky & May, 2015).
Figure 1.
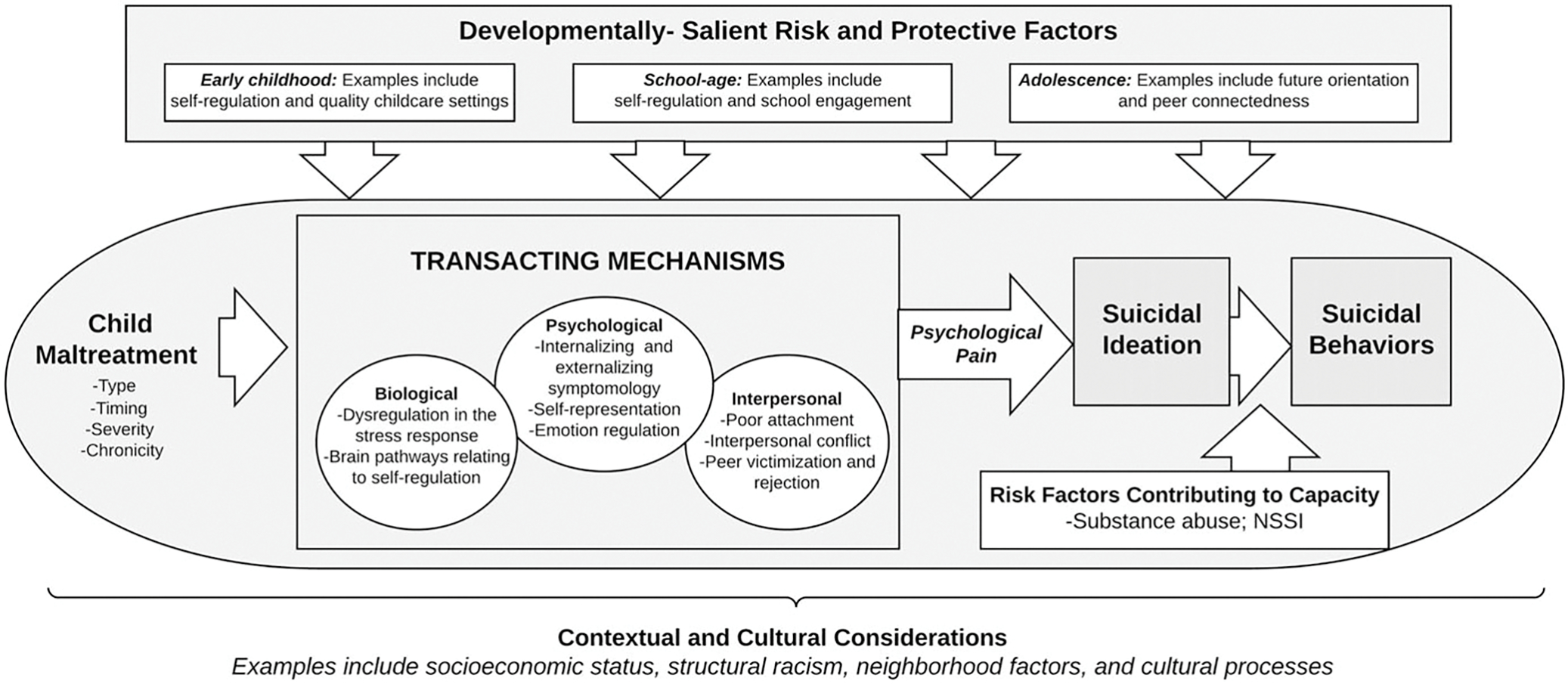
Developmental conceptual model of child maltreatment and youth suicidal thoughts and behaviors.
Second, we propose developmentally salient risk factors for adolescent STBs, such as pubertal development, stressful life events, and peer problems, and protective factors such as school belonging and future orientation. Last, in line with ideation-to-action frameworks of suicide, we propose that for youth with maltreatment experiences, the progression from suicidal ideation to suicidal behaviors is exacerbated by individual vulnerabilities that may increase youths’ propensity for participating in suicidal behaviors. Such vulnerabilities include consequences of child maltreatment, such as dysregulation of the physiological stress response, substance use behaviors, and non-suicidal self-injury (NSSI). External factors associated with child maltreatment, such as recent stressful life events, may also exacerbate the pathway from suicidal ideation to suicidal behaviors. This third aspect of our model, which explains the transition from suicidal ideation to behaviors, differentiates our model from other etiological theories for related psychopathology outcomes.
Together, our model proposes a set of risk factors and a set of hypothesized relations between these risk factors. Consistent with the concept of multifinality, many of our proposed risk factors (e.g., child maltreatment exposure, interpersonal risk factors, and psychopathology) are general-risk factors that are associated not only with STBs but other adverse outcomes such as substance use disorders or NSSI. However, several aspects of our model are specific to STBs. For instance, psychological pain (i.e., psychache or mental pain) is a suicide-specific risk factor that we propose results from several multi-level transacting developmental mechanisms. A recent systematic review revealed that mental pain is a predictor of suicide risk both within clinical samples of adolescents and adults and within non-clinical samples (Verrocchio et al., 2016). Additionally, we propose several suicide-specific risk factors that are involved in the progression from suicidal ideation to suicide attempts. Thus, the following model of child maltreatment and youth STBs is specific to the goal of understanding the development of youth STBs, and can be used to guide suicide-specific prevention interventions.
Considering the dimensionality of child maltreatment
Our model considers the complex and multidimensional nature of child maltreatment experiences and how this influences developmental trajectories towards suicide risk. Child maltreatment can be measured along several dimensions including type, severity, developmental timing (i.e., the age or developmental stage at which maltreatment occurs), relationship with the perpetrator (i.e., familial versus non-familial), and chronicity (i.e., whether maltreatment occurs once or is a recurring event throughout childhood; English et al., 2005; Manly et al., 2001). Accounting for the dimensionality of child maltreatment is important not only for ecologically valid measurement, but also per the developmental psychopathology theoretical framework. Different dimensions of child maltreatment represent distinct experiences children may have in their rearing environment. Consequently, the complexity in child maltreatment experiences contributes to the multifinality in youth developmental outcomes. This complexity is particularly important to consider in our model of child maltreatment and youth STBs, as different dimensions of child maltreatment experiences can differentially impact the developmental mechanisms that are most salient in the pathway to youth STBs. Additionally, the dimensionality of child maltreatment has implications for the way maltreatment is operationalized and modeled. For instance, within samples of maltreated youth, dimensions of maltreatment such as severity or perpetrator type may moderate the association between maltreatment exposure and youth STBs.
Developmental timing and chronicity of maltreatment are critical to consider in the context of youth STBs. According to the organizational theory of development, maltreatment will impact the stage-salient developmental tasks that correspond to the developmental stage of the child when maltreatment occurs. Consequently, which developmental tasks are disrupted will impact children’s and adolescents’ developmental trajectories and the possible emergence of psychopathology. For instance, maltreatment during infancy may reasonably disrupt the attainment of a secure attachment relationship with a primary caregiver (Stronach et al., 2011). In contrast, maltreatment that occurs during adolescence may disrupt salient milestones such as identity development. Likewise, maltreatment is often chronic throughout childhood and adolescence (Warmingham et al., 2019), and this chronicity can influence the developmental pathways to youth suicidal thoughts and behaviors. Chronic childhood maltreatment that occurs in several developmental stages may upend the attainment of multiple stage-salient developmental tasks, compounding the risk for subsequent psychopathology outcomes, including STBs. Several studies have indeed investigated maltreatment timing and chronicity in relation to subsequent suicidal thoughts and behaviors during adolescence. In the National Longitudinal Study of Adolescent Health, adolescents who were first exposed to physical abuse in preschool (i.e., ages 3–5) or in adolescence (i.e., ages 11–17), and adolescents who were first exposed to sexual abuse in preschool, had a heightened risk for suicidal ideation (Dunn et al., 2013). Further, emerging adults who first experienced maltreatment during infancy were more likely to exhibit suicidal ideation compared to those who first experienced maltreatment in later childhood (Handley, Warmingham, et al., 2019).
The developmental timing and chronicity of child maltreatment are also pertinent to the onset and timing of youth STBs. In a cross-national study, a history of childhood physical or sexual abuse increased the odds of a suicide attempt in childhood (i.e., ages 4–12) by 6–10-fold, respectively (Bruffaerts et al., 2010). The same study showed that childhood abuse had a smaller but still significant impact on the onset of suicidal behavior in young adulthood and adulthood (OR range: 2.5–3.1). However, child maltreatment was assessed retrospectively, and thus it is unclear whether timing of childhood sexual and physical abuse played a role in the onset and timing of suicidal behavior. Theoretically, the timing of child maltreatment may be related to both the onset of youth STBs and the mechanisms relevant to this onset. Childhood maltreatment that is chronic throughout both childhood and adolescence may reasonably be related to an earlier onset of STBs that occurs concurrently with the abuse. However, more research is needed to assess how timing and chronicity of child maltreatment is related with timing (e.g., onset and persistence) of youth STBs.
Different subtypes of maltreatment may also impact unique developmental processes that serve as mechanisms linking maltreatment to subsequent STBs. There is indeed evidence for the impact of maltreatment type on eventual STB outcomes. For example, a recent meta-analysis showed differential associations between child maltreatment type and risk for suicidal behavior among young people. Findings showed that sexual abuse contributed to a 3.41-fold increase in odds of suicidal behavior, while physical neglect contributed to a 1.79-fold increase in odds of suicidal behavior (Angelakis et al., 2020). Relatedly, recent perspectives on childhood adversity posit that threat (e.g., physical abuse) and deprivation (e.g., neglect) are unique aspects of adversity with specific mechanisms towards adverse outcomes (McLaughlin & Sheridan, 2016). For instance, disruptions to emotional processing are hypothesized to be a primary mechanism linking experiences of threat to adverse psychopathology outcomes (McLaughlin & Sheridan, 2016). Further research is needed that incorporates dimensional models of childhood maltreatment with respect to the development of STBs.
Recent studies have also demonstrated the complexity in child maltreatment experiences, and the common co-occurrence of types, by using person-centered approaches. For example, among a sample of child protective services (CPS) involved children, latent classes of child maltreatment experiences (e.g., type, chronicity) predicted different child functioning outcomes. The majority of children in this study were characterized as having chronic and multi-subtype maltreatment, and subsequently had the highest risk for emotional and behavioral problems (Warmingham et al., 2019). Future research is needed to uncover how the complexity in child maltreatment experiences relates to risk for youth STBs, and to better understand the developmental pathways in these associations.
Biological, psychological, and interpersonal mediating processes
Following a developmental psychopathology approach, our model of youth STBs proposes three critical developmental processes at three levels of analysis (biological, psychological, and interpersonal). These processes include physiological dysregulation, disruptions in emotion regulation, and risky interpersonal and family processes (see Figure 1). Importantly, informed by the developmental systems perspective, these three mediating processes are not discrete, but instead transact with one another over time to influence the emergence of STBs. For example, physiological dysregulation can underlie or exacerbate psychopathology while also contributing to stressful family contexts. There is also evidence that youth psychopathology and family stress transact with and exacerbate one another (Chan et al., 2014). A child’s disruptive or internalizing behavior can cause conflict within the family system, which may prolong or exacerbate the internalizing or externalizing behaviors of the child. Together, these risky processes may result in the psychological pain that theoretically precedes suicidal behavior (Klonsky & May, 2015). Below, we outline the specific developmental mechanisms we propose in the pathway from child maltreatment experiences to youth STBs.
Biological processes
Experiences of early life stress, including childhood maltreatment, are known to negatively impact the development of various bioregulatory systems within the individual (Lovallo, 2013; Obradović, 2012; Wismer Fries et al., 2008). Thus, at the biological level, we propose that child maltreatment impacts neurobiological and physiological systems of self-regulation, which in turn can transact with other proposed mechanisms (e.g., internalizing psychopathology and interpersonal problems), leading to the psychological pain that is the theoretical root cause for STBs (Klonsky & May, 2015). Specifically, we propose that child maltreatment impacts risk for youth STBs via (a) dysregulation of psychophysiological stress response systems, and relatedly, (b) neurobiological mechanisms associated with self-regulation.
Stress response systems.
There is a consensus through psychophysiological, genetic, and neuropsychological (e.g., functional magnetic resonance imaging (fMRI)) studies that childhood adversity such as child maltreatment can impact multiple biological systems involved in the stress response. This includes the two primary stress response systems, the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis (Gunnar & Quevedo, 2007). The autonomic system consists of the sympathetic nervous system, which responds to external demands with immediate fight or flight reactions, and the parasympathetic nervous system, which works to regulate the individual and maintain homeostasis (Gunnar & Quevedo, 2007). The autonomic nervous system transacts with the HPA axis, which mediates the individual response to stressors by facilitating the secretion and action of glucocorticoids (i.e., cortisol) throughout the body (Tarullo & Gunnar, 2006). Glucocorticoids have a variety of actions in the body, including suppressing the immune and inflammatory response (Irwin & Cole, 2011), regulating energy via glucose metabolism, and inhibiting the short-term fight or flight response (Gunnar & Quevedo, 2007).
According to the adaptive calibration model, an evolutionary-developmental theory, early life experiences shape the development of stress response systems (del Giudice et al., 2011). Specifically, inputs from the physical environment modify physiological systems, including the autonomic nervous system and HPA axis, to facilitate adaptation to the current environment (Frankenhuis et al., 2020). For example, it is possible that young children exposed to physical abuse will become hyper-responsive to stress to facilitate their survival in this type of threatening environment. However, adaptive strategies that include hyper- or hypo-stress-responsiveness can lead to maladaptation later in life when the individual is no longer in the threatening or adverse environment.
There is a robust research literature linking early life stress, and specifically child maltreatment, to physiological dysregulation in stress response systems (Obradović, 2012). For example, several research groups have investigated the impact of early life stress by utilizing samples of chronically deprived children from orphanages in Romania (Gunnar et al., 2001; Humphreys et al., 2020). Children who spent most of their childhood in these institutions were found to have heightened salivary cortisol levels (a marker of dysregulated HPA axis function), as compared to children who were not raised in institutions and children who were adopted early in life (Gunnar et al., 2001). In US-based samples, experiences of childhood maltreatment have also been found to impact diurnal patterns of cortisol (Bernard et al., 2010), as well as cortisol reactivity (Harkness et al., 2011), although this literature is mixed. There is also literature documenting the associations between child maltreatment and activity in the autonomic nervous system (Huffman et al., 2020). For example, adolescents who reported experiences of childhood maltreatment were more likely to have a heightened sympathetic nervous system response to a common psychosocial stress task, as compared to non-maltreated adolescents (McLaughlin et al., 2014). Early life adversities such as child maltreatment confer risk for methylation and other epigenetic changes in genes relating to HPA function (Cicchetti et al., 2016), suggesting that epigenetic modifications in genes relating to the stress response may serve as an underlying mechanism between child maltreatment and suicide. However, most epigenetic studies have used clinical adult samples, and thus additional research is needed on how child maltreatment influences youth STBs via epigenetic mechanisms, and how this relates to stress response reactivity.
Dysregulation in physiological stress response systems may serve as a critical and developmentally salient risk factor for suicide among adolescents (Miller & Prinstein, 2019). Moreover, an abnormal response to stress in the HPA axis has been posited as a risk factor for suicidal behavior in part due to associated behaviors such as impaired decision making and aggression (Steinberg & Mann, 2020). There is some empirical evidence to support these suggestions. For example, heightened reactivity in the HPA axis in response to a laboratory-administered psychosocial stress task was related to suicidal ideation three months later in a sample of adolescent girls at risk for suicidal behaviors (Giletta et al., 2015). Alterations in the autonomic nervous system have also been observed in relation to STBs. Women with a history of suicide attempts had lower basal high-frequency heart rate variability, a measure of parasympathetic nervous system capacity, as compared to women without a history of suicide attempt (Wilson et al., 2016). This finding indicates that a lesser capacity of the parasympathetic nervous system, or a dampened ability to regulate oneself, may be linked with suicide-related behaviors.
It is important to note that early life stress such as child maltreatment can produce both dampened responsiveness (hypo-responsivity; Liu et al., 2020; Lovallo, 2013) as well as heightened responsiveness (hyper-responsivity; e.g., Harkness et al., 2011) in stress response systems. It is possible that the type and timing of stressor experienced, genetic and temperamental differences, and the developmental stage of the child impacts whether youth exhibit hypo- or hyper-reactivity to stress (Bosch et al., 2012; Cicchetti et al., 2010; Obradović, 2012). Indeed, the stress response system exhibits marked plasticity and adapts dynamically to changing environmental circumstances such as stressful rearing contexts. For example, there is some evidence that the stress response system is initially hyper-active after a child experiences toxic stressors such as child maltreatment, and then eventually becomes suppressed due to habituation of the stress response (Trickett et al., 2010). Additionally, some research suggests that child psychopathology might moderate the association between child maltreatment and cortisol regulation (Cicchetti et al., 2010). However, more research is needed to investigate the complex relationships between early life stress experiences and dysregulation of physiological stress response systems. Thus, our proposed model suggests that dysregulation in stress response systems, including both dampened and heightened responsiveness, can serve as a mechanism between child maltreatment and youth STBs.
Neurobiological pathways relating to self-regulation.
We also propose that neurobiological changes to brain pathways relating to self-regulation may underlie the association between child maltreatment experiences and youth STBs. Although we discuss these mechanisms here separately, these neurobiological mechanisms are related to the aforementioned psychophysiological stress response mechanisms. Below we discuss several findings relevant to a neurobiological pathway related to self-regulation; however, an exhaustive review of the brain mechanisms related to child maltreatment and youth suicide are outside the scope of the present article.
Experiences of early life stress, including child maltreatment, may impede normative and healthy brain development (Berens et al., 2017; Twardosz & Lutzker, 2010). The developing brain shows marked plasticity throughout childhood and adolescence, and consequently, traumatic environmental experiences such as maltreatment can influence both the structure and function of certain brain areas and networks (Twardosz & Lutzker, 2010). Child maltreatment is known to impact brain areas that are implicated in heightened emotional reactivity and increased salience of threatening stimuli, both of which are common for individuals exposed to childhood trauma, and which have been suggested as behavioral mechanisms linking child maltreatment to future psychopathology (McLaughlin & Lambert, 2017). Indeed, structural and functional differences have been found among maltreated children and adults in areas relating to emotion processing and emotion regulation (e.g., limbic and frontal brain regions; Hallowell et al., 2019; Oshri et al., 2019). For example, children and adults who have prior experiences of child maltreatment are more likely to exhibit increased activation in the amygdala in response to an fMRI task with emotional stimuli (Hein & Monk, 2017; Tottenham et al., 2011). Functional changes in relevant frontal cortex areas may also underlie emotion regulation difficulties among maltreated children and adolescents (McLaughlin et al., 2015; Pechtel & Pizzagalli, 2011).
Neurobiological deficits in emotion regulation and reactivity have also been implicated in suicidal ideation and behaviors (Li et al., 2020; Pan et al., 2013). For instance, a meta-analysis comparing findings from task-based fMRI studies found that adult patients with major depressive disorder and history of a suicide attempt, compared to major depressive disorder patients without a history of attempt, showed functional changes in brain areas relevant to emotion regulation and processing, including the insula and fusiform gyrus (Li et al., 2020). In another study, adolescents with a history of suicide attempts evinced significantly different activation patterns of several brain areas in response to an emotion-processing paradigm, in comparison to a group of adolescents with depression but no history of suicide attempts and to a healthy control group (Pan et al., 2013). Specifically, adolescent suicide attempters presented a heightened response to angry faces in sensory cortical areas and areas associated with attention processing. Thus, although no studies to our knowledge have used formal mediation analysis to examine brain pathways as mechanisms between child maltreatment and youth STBs, it is evident that neurobiological pathways implicated in emotion regulation can influence the risk for STBs among youth with exposure to child maltreatment. Specifically, these neurobiological findings may reflect an individuals’ inability to adaptively cope with stressful or emotional experiences, which in turn can lead to excessive or prolonged negative mood states (i.e., psychological pain) and subsequent suicidal ideation (Van Heeringen & Mann, 2014).
Psychological processes
The second proposed mechanism linking early life stress with adolescent suicide-related behaviors is through psychological processes, including emotion regulation, self-representation, and internalizing and externalizing symptomology. In accordance with the organizational perspective on development, a key tenet of the developmental psychopathology perspective, adverse rearing environments can disrupt stage-salient tasks relating to children’s socioemotional development, such as self-concept development and emotion regulation (Cicchetti & Banny, 2014). For example, opinions and actions of caregivers toward the child contribute to the child’s own perceived worth (Harter, 2016). Consequently, a child in an insecure or abusive rearing environment may grow to make negative attributions about oneself which are associated with concurrent or subsequent internalizing symptoms such as anxiety and depression (Harter, 2016). Further, child maltreatment can disrupt the attainment of self-regulation abilities, including emotion regulation and self-system processes, cascading into externalizing behaviors such as disruptiveness and impulsiveness (Kim & Cicchetti, 2009). These disruptions in stage-salient developmental tasks prompted by maltreatment can subsequently lead to increased risk for STBs during adolescence and emerging adulthood.
Emotion regulation.
Children and adolescents who have been exposed to child maltreatment are more likely than non-abused peers to have problems with emotion regulation, including having less access to emotion regulation strategies and greater emotion reactivity (Kim-Spoon et al., 2013). For instance, children aged 6–12 who were exposed to child maltreatment, measured prospectively, were more likely to exhibit emotion regulation problems such as low emotional awareness and inappropriate emotional displays (Kim & Cicchetti, 2009). In a recent meta-analysis, child maltreatment was significantly associated with emotion dysregulation (Lavi et al., 2019). The biological underpinnings of emotion regulation, including the neurological processes involved in emotion processing and the physiological processes relating to the acute stress response, have also been associated with child maltreatment (Koss & Gunnar, 2018; Twardosz & Lutzker, 2010).
Adolescents and young adults who have problems regulating and coping with difficult emotions may think about suicide and act upon self-injurious thoughts to escape from their psychological pain. Indeed, in a sample of adolescent inpatients, youth who had impulse control difficulties and who lacked sufficient access to emotion regulation strategies were more likely to have past-year suicidal ideation, even when controlling for mood, anxiety, and behavioral disorders (Hatkevich et al., 2019). In another study using a sample of high school students in rural, low-income communities, teens who reported having limited access to emotion regulation strategies were more likely to also report a suicide attempt (Pisani et al., 2013). Relatedly, a recent cross-sectional study found evidence for emotion dysregulation as a mediator between child maltreatment and adolescent self-harm (Peh et al., 2017). Thus, sufficient evidence exists to encourage further investigations of emotion regulation (including emotion regulation strategies and emotion reactivity) as a mediator between child maltreatment and youth STBs.
Self-representation.
The availability of sensitive and stable caregivers is crucial to the normative development of self-representation throughout childhood (Harter, 2006). Theoretically, having a secure attachment relationship gives children a solid foundation for healthy development, including the development of a positive self-concept. Experiences of abuse may trigger youth to incorporate negative feedback from caregivers (e.g., connotations of being “bad”) into their own self-concept. Studies show that youth who have been abused or neglected by their caregivers have lower self-esteem compared to their non-maltreated peers (Kim & Cicchetti, 2006; Shen, 2009). In a story-telling task, the narratives of maltreated preschoolers were more likely to contain negative self-representations compared to the narratives of their non-maltreated counterparts (Toth et al., 2000).
Several studies provide support for the role of self-representation in the developmental pathway from child maltreatment to youth STBs. In a sample of adolescents living in rural China, those who had experienced neglect and emotional abuse were more likely to report suicidal ideation, and this was mediated by a lack of self-compassion (Zhang et al., 2020). There is also evidence for the role of self-representation, including self-esteem and self-criticism, in the association between child maltreatment and suicidal behaviors (Cero & Sifers, 2013; Falgares et al., 2018). For instance, in a sample of undergraduate students in Italy, self-criticism partially mediated the association between retrospectively reported experiences of child maltreatment and an index measuring the propensity for suicide (Falgares et al., 2018). It is possible that these self-processes are underlying behavioral symptomology, including internalizing and externalizing symptoms, in the psychological developmental pathways from child maltreatment to youth STBs.
Internalizing and externalizing psychopathology.
There is much empirical research that has linked child maltreatment with mental illness and symptoms of psychopathology during adolescence. Abuse or neglect during childhood predicts heightened internalizing symptoms in longitudinal studies (Bolger & Patterson, 2001; Duprey et al., 2017; Lewis et al., 2011). For example, findings from the longitudinal Isle of Wight study indicated that youth who were maltreated were 15.5 times more likely to experience minor depression and 8.11 times more likely to experience an anxiety disorder, compared to non-abused youth (Collishaw et al., 2007). Internalizing symptomology, in turn, is a strong predictor of suicide-related behaviors during adolescence and emerging adulthood (Bridge et al., 2006).
It is also likely that, for some youth, externalizing psychopathology (e.g., disruptiveness and impulsivity) plays a role in the connection between child maltreatment and youth STBs. Child maltreatment is a robust predictor of externalizing disorders throughout childhood, adolescence, and young adulthood (Oshri et al., 2011; Thompson et al., 2016). In turn, recent studies have shown that externalizing disorders are a direct risk factor for suicide-related behaviors. For example, in a clinical sample of psychiatrically hospitalized adolescents, 67.9% of those who had attempted suicide multiple times were diagnosed with an externalizing disorder (e.g., disruptive behavior disorders, substance use disorders; D’Eramo et al., 2004). In fact, scholars have recently posited that impulsivity may serve as a primary mechanism linking childhood maltreatment with suicide (Braquehais et al., 2010).
Most investigations on mechanisms between child maltreatment and youth STBs have focused on individual symptomology, including internalizing and externalizing-related symptoms. Not surprisingly, internalizing problems (including depression and depressive symptoms) were found as a mediator between child maltreatment and suicidal ideation in numerous studies (Cromer et al., 2019; Handley, Adams, et al., 2019; Sekowski et al., 2020; Wan & Leung, 2010). There is also evidence for other related mediators, including psychache (i.e., psychological pain; Li et al., 2019), negative emotionality (Cho & Glassner, 2020), and recent psychological distress (Thompson et al., 2012). Similar mediating mechanisms have been found in the association between child maltreatment and suicide attempts. For instance, depressed mood was found as a mediator between both sexual abuse and family conflict and adolescent suicide attempts (Sigfusdottir et al., 2013). There are considerably fewer studies investigating externalizing behaviors in the pathway from child maltreatment to youth STBs, but some evidence exists. For instance, externalizing problems mediated the association between childhood physical abuse and youth suicidal ideation in a large sample of Chinese high school students (Wan & Leung, 2010).
Taken together, there is strong evidence that various forms and symptoms of psychopathology play a role in the developmental pathway between child maltreatment and adolescent STBs. It is possible that more generalized forms of psychopathology, as opposed to specific diagnoses, are mechanisms in this link. Recent models suggest that a higher-order, p factor, of general psychopathology underlies traditional psychiatric diagnoses such as in the DSM and includes diagnoses on both the internalizing and externalizing spectrum (Caspi et al., 2014). This model on the structure of psychopathology can also explain the high rates of comorbidity that exist between internalizing and externalizing disorders (Caspi et al., 2014). To our knowledge, just one study has specifically investigated comorbidity between externalizing and internalizing symptomology as a mechanism between childhood maltreatment and adolescent STBs (Duprey et al., 2019b). Theoretically, the combination of internally focused symptoms like depression and anxiety with externally focused symptoms like substance use, impulsivity, and deviance might exacerbate vulnerability for risk behaviors such as suicidal thoughts and behaviors during adolescence. Thus, given the high rates of comorbidity between symptoms and disorders on the internalizing and externalizing psychopathology spectrums, and newer models on the structure of psychopathology, future research should investigate psychopathology comorbidity as a mediator in the link between child maltreatment and youth STBs.
Interpersonal and family processes
The third broad transactional mechanism that we propose is risky family and interpersonal processes (Repetti et al., 2002), and more specifically, attachment processes, family conflict, and peer problems. As with other aspects of our model, these proposed mechanisms are informed by prior literature and developmental psychopathology theory. Additionally, the interpersonal theory of suicide (Van Orden et al., 2010) guides the proposed interpersonal mechanisms linking child maltreatment to youth STBs. The interpersonal theory of suicide posits that interpersonal risk factors (particularly, thwarted belongingness and perceived burdensomeness) lead to the emergence of STBs (Van Orden et al., 2010). Thwarted belongingness and perceived burdensomeness may result from youth’s interpersonal interactions with their families and peers. In the family context, youth who grow up in abusive households may develop feelings of both thwarted belongingness and perceived burdensomeness due to a lack of connectedness to their family unit, and/or a self-hatred that might stem from emotional abuse or other forms of maltreatment. Indeed, experiences of childhood emotional abuse predicted both thwarted belongingness and perceive burdensomeness (Smith et al., 2018), and perceived burdensomeness was found to mediate the association between childhood experiences of emotional abuse and young adult suicidal ideation (Puzia et al., 2014).
Attachment.
In accordance with a developmental psychopathology framework, children who are maltreated may develop insecure attachment relationships with their caregivers (Stronach et al., 2011), and these poor attachment relationships can cascade into future adverse outcomes, including psychopathology (Hankin, 2005). As noted prior, theories of attachment and developmental psychopathology suggest that a secure attachment relationship with one’s caregiver is a foundation on which subsequent healthy development can build upon (Sroufe et al., 1999). Insecure attachment may initiate a cascade of developmental maladaptation, and together these early experiences and developmental perturbations may probabilistically result in future psychopathology including suicide risk. Accordingly, attachment processes are deeply interconnected with the other developmental mechanisms named in our model such as emotion regulation, self-representation, and behavioral problems. For instance, a maltreated child with an insecure attachment relationship with their caregiver may develop negative self-representations and poor self-esteem, which paired with a consistent negative home environment, can trigger depressive symptomology and suicide risk during adolescence.
Family conflict.
Youth who lack secure attachment to a primary caregiver may also later develop relationships with that caregiver characterized by conflict and insecurity (Aikins et al., 2009). Family conflict is a major source of stress and psychological pain for adolescents and may precede suicidal thoughts and behaviors (Pelkonen et al., 2011). Thus, we propose that conflict with family members is a key mechanism linking child maltreatment to future STBs. Theoretically, conflict with family members can predispose youth to feeling burdensome and lacking belonging to a central family unit, and this burdensomeness and thwarted belonging may cause STBs to emerge. Indeed, there is empirical support for the role of family conflict as a mediator between child maltreatment and youth suicidal ideation. Within a sample of depressed low-socioeconomic status adolescent girls, Handley, Adams, et al. (2019) tested three competing mediators (i.e., mother-adolescent conflict, mother-adolescent relationship quality, and depressive symptoms) and found evidence for mother-daughter relationship quality and depressive symptoms as mediators in the association between child maltreatment and suicidal ideation. Similarly, poor family relationships (operationalized as lower levels of cohesion and expressiveness, and higher levels of conflict) mediated the association between physical abuse and suicidal ideation in a large sample of Chinese high school students (Wan & Leung, 2010).
Peer problems.
Child maltreatment experiences increase the risk for bullying victimization and peer rejection in childhood and adolescence (Hong et al., 2012). Similar to family conflict, youth who experience peer victimization or rejection may lack feelings of belonging, which can predispose them to engage in suicidal thinking. Indeed, there is a large body of evidence showing that adolescents who are bullied by their peers (in person or via cyberbullying) are more likely to engage in suicidal thinking and suicide attempts (Hinduja & Patchin, 2010). A recent meta-analysis found that bullying victimization and perpetration were both significantly associated with a greater odds of suicidal ideation and behaviors, with odds ratios ranging from 2.12 to 4.02 (Holt et al., 2015). Certain groups of youth, particularly those who identify as lesbian, gay, bisexual, transgender, and questioning (LGBTQ), are subject to increased levels of bullying and discrimination from peers that can put them at an increased risk of suicide (Ybarra et al., 2015).
Taken together, there is convincing theoretical and empirical support that interpersonal processes play a unique role in the developmental pathway from child maltreatment experiences to the emergence of STBs in adolescence and young adulthood. However, more research is needed to replicate prior findings and investigate specific interpersonal processes in the pathway from child maltreatment to youth STBs. For example, disruption in attachment processes is a candidate mechanism that is associated with child maltreatment and poor mental health outcomes (Hankin, 2005; Stronach et al., 2011), but has not been investigated specifically in relation to youth STBs. Additionally, most studies investigating interpersonal processes in the association between child maltreatment and youth STBs examined suicidal ideation as an outcome variable. It will be important for future research to examine the role of interpersonal processes, both within and outside of the family, as precursors to youth suicidal behaviors and suicide.
Developmentally salient risk and protective factors
In our model, we specify the role of developmentally salient risk and protective factors that can buffer youth from the harm posed by exposure to child maltreatment. According to the developmental psychopathology approach and the concept of multifinality, the emergence of youth STBs is one of many possible outcomes stemming from exposure to child maltreatment. Importantly, many youth who experience child maltreatment along with its various adverse outcomes (e.g., internalizing psychopathology or family-child conflict) do not end up exhibiting suicidal thoughts and behaviors in adolescence nor later in life. Protective factors are moderators that can buffer, or lessen, the impact of child maltreatment exposure on the likelihood of developing suicidal thinking or behaviors (Rutter, 1985), while moderating risk factors can exacerbate the impact of child maltreatment on youth STBs.
In line with a developmental perspective on youth STBs, it is important to consider that both protective and risk (i.e., exacerbating) factors can affect suicidal ideation and behaviors differently depending on the time in a child’s development. In Figure 1, we give examples of empirically supported risk and protective factors for maltreated children and adolescents at different stages of development (i.e., early childhood, school age, and adolescence). For example, school belonging and participation in youth activities were found to be protective in the association between physical abuse and suicidal ideation and attempts among adolescents (Cero & Sifers, 2013; Zhang et al., 2020). These protective factors are salient to the developmental stage of adolescence, which is characterized by rapid social development and the growing importance of peer groups.
Our conceptual model also posits that there are developmentally salient moderating risk factors that can exacerbate the pathway from child maltreatment to youth STBs. Adolescence marks an extended transition between childhood and young adulthood, and includes biological shifts such as puberty, as well as personality and social shifts including identity development and the increased salience of peers. During this time, certain developmental transitions and risk factors (both direct and moderating) may exacerbate the pathway towards suicidal ideation, and between suicidal ideation and suicidal behaviors. Therefore, in this model, the transactions between vulnerability factors that may have been continuous throughout childhood (i.e., physiological dysregulation, psychopathology, and interpersonal problems), coupled with the challenges of adolescence, can result in the emergence of STBs. For example, stressful life events exacerbated the association between child maltreatment and suicidal ideation in a sample of adolescent girls (Duprey et al., 2021). Other possible developmentally salient risk factors to consider by future research include, but are not limited to, pubertal development, risky sexual behaviors, and peer victimization.
Progression from suicidal ideation to suicidal behaviors
Our conceptual model is informed by ideation to action theories of suicide, such as the interpersonal theory of suicide (Van Orden et al., 2010) and the three-step theory (Klonsky & May, 2015), which posit that different risk factors and processes characterize the development of suicidal thoughts versus those that characterize the progression from suicidal thoughts towards suicidal behaviors. We integrate these theories of suicidology (which are based on adult models) with a developmental psychopathology lens to apply them to the emergence of STBs in adolescence and emerging adulthood. According to these frameworks, the progression from suicidal ideation to suicide behaviors (i.e., attempts) is driven by capability (defined as an individual’s capacity to engage in self-harming behaviors). For most people, including those who may have suicidal ideation, there is a biologically and evolutionary-driven fear of engaging in suicidal behaviors. However, for some individuals with increased capability, this fear is reduced, and they are subsequently more likely to engage in suicidal behaviors. Consequently, our model suggests that there are capability-building risk factors that contribute to the progression from suicidal ideation towards suicidal behaviors, which stem from experiences of child maltreatment.
In the interpersonal theory of suicide, capability includes two components, both of which are not innate but acquired or learned throughout the lifetime: reduced fear of death, and an increase in pain tolerance (Van Orden et al., 2010). In contrast, the three-step theory posits that capability can also be trait-like, or dispositional, in addition to acquired. This theory also considers the role of practical sources of capability, such as access to lethal means (Klonsky & May, 2015). In our model of child maltreatment and youth STBs, we focus specifically on the role of acquired capability. The developmental consequences of child maltreatment are multifaceted, and include several outcomes related to an increased capability for suicide. These outcomes include but are not limited to dysregulated responses to stress, substance use behaviors, and engagement in NSSI. Below, we detail how these three specific risk factors might contribute to the ideation-to-action pathway. Note that these risk factors might work by exacerbating the association between suicidal ideation and behaviors (i.e., acting as a statistical moderator), or by contributing directly to the likelihood of suicidal behaviors (i.e., having a direct statistical association with suicide attempts).
As detailed above, child maltreatment and other adverse, chronic stressful experiences in childhood can predict future dysregulation in physiological stress response systems (Gunnar et al., 2001; Lovallo, 2013). Specifically, a blunted physiological response to acute stressors is characteristic for youth and adults who have undergone traumatic childhood experiences like child maltreatment (Lovallo, 2013). There is some empirical evidence for the role of blunted stress reactivity in the capacity for suicidal and self-harming behaviors. For example, a recent study with adolescent girls found that psychosocial stressors predicted suicidal ideation, while the combination of psychosocial stressors with blunted HPA function predicted suicidal behaviors (Eisenlohr-Moul et al., 2018). Additionally, in the same study, adolescents with a history of suicidal behavior had a significantly more blunted cortisol response to a psychosocial stressor compared to those with only suicidal ideation and to controls with no lifetime suicidal ideation or behaviors. A separate study also found that adolescent girls with a history of self-harm had a blunted HPA reaction to a laboratory social stress task compared to girls with no history of self-harm (Plener et al., 2017).
Similarly, youth who suffer from child abuse and neglect are more likely to engage in substance use behaviors, including alcohol, marijuana, and other drug use (Cicchetti & Handley, 2019). Substance use is a major proximal risk factor for engagement in suicidal behaviors among youth (Esposito-Smythers & Spirito, 2004). For instance, in a case-control study, substance use disorders were significant risk factors for adolescent suicide attempts (Kelly et al., 2002). Substance use was also associated with suicide attempts, after controlling for sociodemographic factors and psychiatric disorders including suicidal ideation, in a cross-sectional study using a community sample of adolescents (Wu et al., 2004). Additionally, a recent study found that cannabis and other illicit drug use predicted the transition from suicidal ideation to attempts in a high-risk sample of adolescents (Mars et al., 2019).
The frequency and severity of substance use behaviors increase dramatically during adolescence and emerging adulthood, and risky substance use is even more common for youth with histories of child maltreatment (Cicchetti & Handley, 2019). While under the influence of substances that cause disinhibition, such as alcohol or opiates, youth have reduced impulse control and may also have reduced fear of risk behaviors and self-injury (Dawes et al., 2008). Indeed, in a community sample of adolescents, alcohol abuse and dependence, drug use, and cigarette use were all significant predictors for suicide attempts even after controlling for depressive symptoms and suicidal ideation (Wu et al., 2004). Thus, we recommend that future research investigate alcohol and drug use as predictors of suicidal behaviors in samples of youth with histories of maltreatment.
A third possible capacity-enhancing factor stemming from experiences of child maltreatment is NSSI. A recent meta-analysis showed that child maltreatment significantly predicted engagement in NSSI, with an average effect size of OR = 3.42 (Liu et al., 2018). Through the process of habituation (Van Orden et al., 2010), youth who frequently engage in NSSI may have an increased tolerance for pain, thus enhancing their capacity for engaging in suicidal behavior. Indeed, evidence shows that a lifetime history of NSSI predicts future suicide attempts in adolescent clinical (Horwitz et al., 2015) and non-clinical samples (Scott et al., 2015). It is also possible that engagement in NSSI reduces youths’ fear of death, thereby increasing the risk for suicidal behaviors. Several researchers have tested this hypothesis, with mixed findings that both support (George et al., 2016) and refute (Harris & Ribeiro, 2021) the role of reduced fear of death in the association between NSSI and suicidal behaviors. Further research is needed that explores the role of NSSI in perpetuating suicidal behavior, specifically in samples of maltreated youth.
Contextual and cultural considerations
One of the hallmarks of the developmental psychopathology framework is the incorporation of multiple levels of analysis, ranging from biological influences outwards towards macro-system and cultural influences. Accordingly, our model considers the role of youths’ context, and particularly the role of the institutions and cultures in which they belong, in the etiological processes linking child maltreatment and STBs. Child maltreatment and suicide are both phenomena that are heavily influenced by the institutions and contextual systems that individuals are a part of. It is particularly important to account for the inequities perpetuated by these institutions and systems when investigating associations between child maltreatment and youth suicide. Racism, poverty, and other sources of disparities must be considered as part of our model of child maltreatment and youth STBs. Below, we outline several ways that culture and context play a role in our proposed conceptual model.
First, context plays a role in the prevalence and reporting of child maltreatment. Environmental characteristics such as family poverty and neighborhood disadvantage can be considered enduring vulnerability factors that contribute to the etiology of child maltreatment (Cicchetti & Toth, 2016). Importantly, Black families in the United States are disproportionally reported to CPS, and Black children are disproportionally more likely to be removed from their homes as a result of CPS investigations (Palusci & Botash, 2021). More than half (53.0%) of Black children in the United States are involved in a child welfare investigation by the time they reach age 18, which is substantially higher than the prevalence of child welfare involvement in the general population of US youth (37.4%; Kim et al., 2017). Experts have often attributed disparities in CPS reporting to increased surveillance in neighborhoods with large percentages of racial-ethnic minority families, and racial bias in the reporting and investigation of child maltreatment (Palusci & Botash, 2021). Beyond the effects of child maltreatment, involvement with the child welfare system, including separation from caregivers, can lead to disruptions in stage-salient tasks and cascading mental health problems including suicidality.
Contextual factors relevant to the etiology of child maltreatment, such as poverty and parental psychopathology, are also implicated in the developmental mechanisms we hypothesize in the pathway between child maltreatment and youth STBs. For instance, although family poverty may increase the likelihood of child maltreatment, it is also associated with developmental mechanisms in our model such as problems with self-regulation (Cicchetti & Toth, 2016; Palacios-Barrios & Hanson, 2019). It is also particularly important to consider the role of racism in the mechanistic pathways from child maltreatment towards youth suicidal ideation and behaviors. Racism is an acute and chronic stressor that can the health and development of children and adolescents (Trent et al., 2019). Racism can impact children directly through the effects of interpersonal racism including bias and discrimination, and indirectly through the effects of structural racism. Structural and historical racism permeates the culture of the United States, impacting children of color in a multitude of ways including by diminishing families’ economic opportunities, interfering with the ability to secure safe and stable housing, and sustaining educational disparities (Trent et al., 2019).
The aforementioned contextual factors must also be considered when studying the acute (i.e., immediate) direct and exacerbating risk factors for suicide. According to the Cultural Model of Suicide (Chu et al., 2010), culture-specific risk factors for suicide may be related to cultural norms (e.g., acceptability of self-harm in some communities) and culture-specific stressors (e.g., discrimination and acculturation stress). Relatedly, some scholars assert that youth suicide should be framed as a sociopolitical issue, and that power and oppression play an integral role in rates of youth suicide in the United States (White & Kral, 2014). For instance, negative attitudes towards the LGBTQ community and the heteronormative sociopolitical context in the United States can lead to emotional distress, bullying, and other immediate risk factors for suicide among LGBTQ youth (Aranmolate et al., 2017). Furthermore, there are racial disparities in recent suicide trends among youth in the United States. Specifically, rates of suicide among Black children and adolescents are increasing, and among all children, young Black boys are the demographic group most likely to die by suicide (Bridge et al., 2015; Emergency Taskforce on Black Youth Suicide and Mental Health, 2019; Shain, 2019). There are also disparities in rates of STBs by geography, with rural youth more likely to die by suicide (Fontanella et al., 2015). Youth who live in rural or otherwise under-resourced communities that lack access to healthcare, or who do not have access to behavioral healthcare due to their socioeconomic status, may be particularly at risk (Campo, 2009; Graves et al., 2020).
Culture not only plays a role in the risk factors for youth STBs, but also when considering protective factors that can prevent suicide and promote positive mental health outcomes. Parallel to the culture-specific risk factors listed prior, culture-specific protective factors may also be related to cultural norms, such as the unacceptability of suicide. For instance, religiosity (e.g., belonging to a church community and attending religious events) is a protective factor that reduces the risk for suicidal thoughts and behaviors among Black teens (Fitzpatrick et al., 2008). Another relevant culture-specific protective factor for teens is familism, a cultural value for many Latino individuals and communities which places value on interconnectedness and commitment to one’s family. Research shows that Latina teens with higher levels of familism were less likely to attempt suicide compared to teens who reported lower levels of familism (Peña et al., 2011). Thus, future research on the developmental processes leading to STBs among youth exposed to child maltreatment should consider both contextual and culture-specific risk and protective factors.
Discussion
In sum, we propose that child maltreatment may lead to suicidal thoughts in adolescence via several mechanisms at the biological, psychological, and interpersonal levels. It is not the individual action of a single mechanism, but the transactional and joint nature of these mechanisms that can cause the psychological pain necessary for a youth to think about ending their own life. Furthermore, experiences of child maltreatment may increase the risk for several capacity-building factors (e.g., substance abuse) that can further propel the adolescent or young adult to move from thinking about suicide towards engaging in suicidal behavior. Notably, there are different risk and protective factors at every stage of development that can either exacerbate this developmental pathway and further propel the youth towards STBs, or buffer this pathway and reduce the probability of STBs.
Implications for suicide prevention: future directions for research
Our proposed model of child maltreatment and youth STBs has implications for future research in basic and applied areas. It is apparent from our review that there are several major gaps in the literature on mechanisms and moderators between childhood maltreatment and youth STBs that should be considered for future research. First, most studies looking at mechanisms and moderators in the association between child maltreatment and youth STBs have examined psychological mediators, such as depressive symptoms, self-esteem, and psychache. Very few studies have investigated biological mechanisms or moderators, despite empirical and theoretical evidence that supports these investigations (Cicchetti et al., 2010; Miller & Prinstein, 2019). There is also a lack of research examining contextual processes (e.g., involvement with child welfare services and neighborhood factors) in the association between child maltreatment and youth STBs. Additionally, few studies have investigated concurrent or interacting multi-level mechanisms (i.e., interpersonal, psychological, and biological) in the link between child maltreatment and youth suicide (notable exceptions include Ammerman et al., 2018; Salzinger et al., 2007; Wan & Leung, 2010). Alternatively, in line with a developmental psychopathology approach and our proposed conceptual model, we posit that there are multi-level transactional factors that mediate the link between child maltreatment and youth suicide. Thus, based on gaps in prior literature and our proposed conceptual model, future research should examine mediators of child maltreatment and youth STBs at multiple levels of analysis, and should consider how these mechanisms interact or transact with one another over time.
There is also a dearth of literature investigating mediators and moderators of child maltreatment and suicidal behaviors (specifically, suicide attempts). The majority of articles that we reviewed used suicidal ideation as an outcome instead of suicide attempts or suicide. Our model suggests that the mechanisms, risk factors (both direct and moderating), and protective factors in the developmental pathway to suicidal ideation are different from those in the pathway from ideation to suicidal behaviors. It will be important for future research to differentiate these outcomes, and to specifically investigate predictors and risk factors for suicidal behaviors in high-risk samples. We proposed three possible capacity-building factors that may play a role in the pathway from suicidal ideation towards suicidal behavior among maltreated youth: (1) stress response reactivity, (2) substance use behaviors, and (3) NSSI. These and other possible factors need to be further examined both in clinical and non-clinical samples of youth.
We also found that many studies have used cross-sectional data to investigate the link between child abuse and neglect and STBs among adolescents and emerging adults (see Table 1). Large prospective studies are needed to test the hypothesized mechanisms and risk and protective factors suggested by the present conceptual model. Thus, future research should strive to use prospective data to investigate mechanisms and moderators of the link between child maltreatment and youth suicide at multiple levels of analysis, while also considering developmentally salient risk and protective factors. Our model of child maltreatment and youth STBs provides a conceptual framework that researchers can use to inform studies in this area.
Additionally, child maltreatment is a complex and multidimensional construct. More work is needed to specifically assess the role of maltreatment type, timing, severity, and chronicity in the etiology of adolescent and young adult suicidal thoughts and behaviors. Person-centered approaches to modeling child maltreatment, such as latent class analysis, may help to better understand the complexity of child maltreatment in relation to subsequent suicide risk (e.g., Warmingham et al., 2019). Additionally, dimensional approaches to studying childhood adversity and maltreatment (McLaughlin & Sheridan, 2016) should be extended to investigations of youth STBs.
It will also be important for future research to address the role of culture (e.g., race, ethnicity, immigrant status, and nationality), discrimination, and systemic disparities in the development of STBs for youth with histories of child maltreatment. Thus far, there is a lack of research that has examined child maltreatment and youth suicide using underrepresented samples of youth, including Black youth and LGBTQ youth. These two subpopulations are critical: rates of suicide among Black youth, particularly males, are rising rapidly compared to rates in other demographic groups (Emergency Taskforce on Black Youth Suicide and Mental Health, 2019). Relatedly, youth who identify as LGBTQ are at an increased risk for experiencing suicidal ideation and partaking in suicidal behaviors (Ivey-Stephenson et al., 2020). Relatedly, and in line with our prior recommendation of investigating contextual processes in the pathway from child maltreatment to youth STBs, social determinants of health are imperative to consider when studying youth suicide. This is particularly important given the increasing rates of STBs among youth in the last decade (Ivey-Stephenson et al., 2020). It is possible that child maltreatment and other social determinants of health are related to these epidemiological shifts in rates of youth STBs. The suicide prevention community, including researchers, clinicians, and survivors, will need to focus critically on social determinants of health to understand and prevent suicide among youth with maltreatment histories.
Importantly, to advance the science on child maltreatment and youth STBs, a cohesive conceptual model is necessary. The proposed developmental model of child maltreatment and youth STBs provides a basis for asking questions and forming hypotheses about the developmental processes involved in the pathway between child abuse and neglect and youths’ suicidal ideation and attempts. Our conceptual model involves various transactions at multiple ecological levels and, due to this complexity, it likely is not possible to test all components of our model at once.
We propose several proximal next steps to test and refine our model. First, research with longitudinal designs and statistical models (e.g., cross-lagged models; latent growth models) can be used to test the role of multiple mediators at the different levels we propose in our model (biological, psychological, and interpersonal) in the pathway between childhood maltreatment and youth STBs. With sufficient power, designs such as moderated mediation will also help elucidate relations between different mechanisms and risk and protective factors in our model. Second, we propose that an important next step for refining our model is to test the role of moderating risk factors that contribute to capacity for suicide (e.g., NSSI, substance abuse) among youth exposed to child maltreatment. This research can inform interventions that respond to acute suicide risk in populations of maltreated adolescents and young adults. Third, applied research that tests suicide prevention and intervention programs can inform the mechanisms proposed in our model. Relatedly, experimental therapeutics is a research approach originally used in medicine that has recently been applied to behavioral interventions, including suicide prevention, to elucidate theoretical mechanisms of action (Insel & Gogtay, 2014). Research using the experimental therapeutics approach not only can help develop and refine suicide prevention interventions for maltreated youth, but can also iteratively inform and refine the present developmental model of child maltreatment and youth STBs.
Implications for suicide prevention
Our model focuses on the short and long-term developmental antecedents of youth suicidal ideation and behavior. As such, the implications of our model for suicide prevention center around upstream prevention. Upstream prevention programs seek to modify salient risk and protective factors and mechanisms for suicide (e.g., those established by the present model such as child maltreatment, internalizing and externalizing psychopathology, emotion regulation, and interpersonal processes) before the emergence of suicidal thoughts and behaviors (Caine et al., 2018). Accordingly, these interventions have the potential to make population-level impacts on reducing youth suicidal thoughts and behaviors. Our recommendations for suicide prevention are also grounded in the Institute of Medicine continuum of care model (Gordon, 1987), which differentiates three types of prevention: universal (i.e., programs that target the general population), selective (i.e., programs that target a subpopulation who have a specific vulnerability factor for an eventual adverse outcome, such as youth with maltreatment histories) and indicated (i.e., programs that target a subpopulation who have elevated vulnerability and are showing some signs or symptoms, such as maltreated youth with elevated depressive symptoms).
The model presented in this paper has implications for the mechanistic targets of suicide prevention and intervention programs for youth with maltreatment histories. For instance, we consider the etiology of adolescent suicide-related behavior to consist of transactions between multiple levels of influence (i.e., physiological, behavioral, and contextual). Accordingly, efforts to intervene and interrupt processes leading to adolescent STBs may be most effective through modifications in the relations, or transactions, between multiple levels, as opposed to altering a single level of analysis (Lerner & Castellino, 2002). For example, the Good Behavior Game (GBG) intervention focuses on improving young children’s behavioral self-regulation in the classroom and aims to alter the social environment to promote social integration (Kellam et al., 2008). An intervention that only targeted self-regulation skills or school social environment may not have had as efficient an impact in reducing risk for suicidal behaviors. In such interventions, mechanisms and outcomes of investigation should be considered at multiple levels of analysis. As an example, Cicchetti and colleagues found that an interpersonal intervention for maltreated youth and families was related to a biological outcome. Specifically, this intervention produced changes in infants’ HPA functioning (Cicchetti et al., 2011). Last, it should be noted that various mechanisms presented in our model (e.g., emotion regulation) are also relevant etiological pathways for other disorders, including depression and substance use disorders. Thus, suicide prevention approaches that are implied from our model may also serve to prevent other adverse outcomes.
Interventionists and researchers must always consider developmental timing and the developmental salience of risk and protective factors when selecting intervention targets for youth. For example, while interpersonal processes are hypothesized in our model as a primary mechanism linking child maltreatment to youth STBs, and consequently would be an appropriate target for suicide prevention interventions, it is important to specify which interpersonal processes are being targeted and if these are appropriate for participants’ developmental stage. For young children who have been exposed to child abuse and neglect, attachment processes are an appropriate intervention target to prevent downstream suicide risk, and several intervention approaches (e.g., parent-child psychotherapy) have been shown to effectively improve attachment security (Toth et al., 2006). Below, we give specific recommendations for suicide prevention along with examples across different developmental stages of participants, settings, and target mechanisms.
Prevention of child maltreatment
First, the model presented in this paper focuses on the detrimental impact of child maltreatment on future suicidal behavior. This highlights the importance of universal prevention of childhood maltreatment. Child maltreatment places an extreme burden on children, families, communities, and our society – including an economic burden estimated to range from $428 billion to $2 trillion per year in the United States (Peterson et al., 2018). Globally, violence against children has been estimated to cost up to $7 trillion (Pereznieto et al., 2014). The primary prevention of child maltreatment must be a public health priority both in the United States and globally, given these programs’ potential for numerous downstream effects, including the prevention of psychopathology and suicidal behaviors during adolescence. Several programs have shown promise for the primary prevention of maltreatment in the United States, including the Nurse-Family Partnership (Olds, 2008) and the Building Healthy Children program (Demeusy et al., 2021). The prevention of child maltreatment can, and should be, considered a form of universal suicide prevention.
Prevention in normative social settings
Our conceptual model of child maltreatment and youth suicide also has several implications for developmentally focused upstream suicide prevention interventions for children and adolescents with histories of maltreatment. In Wyman’s developmental model of upstream suicide prevention for adolescents (2014), the author proposes that upstream prevention can have the most impact when implemented via normative and reparative social systems throughout childhood and adolescence. Normative social systems are those that reach the broadest youth populations, such as schools and families and, with increasing age, more complex and influential peer networks. Reparative social systems are settings or systems designed for youth with particular vulnerabilities, such as juvenile justice or foster care systems (Wyman, 2014). Strengthening the natural social systems that youth are a part of can have positive cascading effects on reducing psychopathology and promoting positive youth outcomes.
In normative social systems, there is evidence for the effectiveness of suicide prevention programs that reduce children’s and adolescent’s risk for STBs by modifying selective risk and protective factors, and the transaction among those factors. For example, the early grade school-based GBG, a classroom-based universal program that aims to reduce externalizing (i.e., aggressive and disruptive) behaviors in childhood (Kellam et al., 2008), has shown promise in long-term follow-up of participants. Emerging adults who had participated in the GBG intervention as children were significantly less likely to report prior suicidal ideation or behaviors, as compared to emerging adults who had been in a non-GBG comparison condition (Wilcox et al., 2008). Increased peer group social integration in later grade school partially mediated the effect of the GBG program on reduced STBs (Newcomer et al., 2016).
School-based universal prevention programs may also have potential in reducing suicide risk by modifying interpersonal risk processes that are implicated in our model of child maltreatment and youth STBs. Peer-based interventions may be particularly salient for adolescents with maltreatment experiences, due to the increased likelihood of involvement in peer victimization and lack of peer support (Hong et al., 2012; Pepin & Banyard, 2006). For example, the school-based Sources of Strength program prepares diverse adolescent opinion leaders to disseminate healthy coping norms and practices through their natural social networks and fosters youth connections to supportive and trustworthy adults (Wyman et al., 2010). Results from a group-randomized control trial showed that Sources of Strength increased school-wide positive norms relating to suicide, including the acceptability of seeking help from trusted adults, and trained peer leaders were four times more likely to refer suicidal peers to adults for support (Wyman et al., 2010).
There is also evidence for various school-based indicated suicide prevention programs, which have been shown to be effective for youth with risk factors for suicide. For example, the C-CARE (Counselors CARE) and CAST (Coping and Support Training) programs are school-based interventions that have been tested and found to be efficacious with high school youth who are at an indicated risk due to their academic problems and presence of suicidal ideation (Thompson et al., 2001). Findings from an efficacy study showed that youth in either the C-CARE or CAST programs exhibited reductions in suicidal ideation, hopelessness, and depression, while youth in the CAST program (an intervention supplemented with small-group skill training) also showed improvements in protective factors such as coping (Thompson et al., 2001). Additional work is needed, however, to determine whether and/or how programs such as CAST, CARE, and Sources of Strength are effective in reducing STBs in populations of youth with histories of child maltreatment. Other peer-based programs, including those that incorporate peer mentoring or youth advocacy, might be impactful for improving mental health outcomes and reducing suicide risk factors (e.g., substance use) among maltreated adolescents, but this has not yet been tested.
Upstream suicide prevention programs that occur in the family context are also important for this population. We recommend family-based suicide prevention programs that target interpersonal skills and processes that have been posited as mechanisms in our conceptual model. Many of the existing family-based suicide prevention interventions are indicated programs, and consequently have primarily been developed and implemented with youth who are showing proximal signs of suicide risk such as suicidal ideation and/or deliberate self-harm. For instance, Parents CARE (P-CARE) is an adaptation of the CARE suicide prevention program that incorporates parent training in socioemotional skills (e.g., conflict reduction, supportive listening) and psychoeducation (e.g., learning suicide warning signs; Hooven et al., 2012). An efficacy study found that P-CARE reduced direct risk factors for suicide, such as suicidal ideation and hopelessness, compared to an active control group (Hooven et al., 2012). Another prevention program that could have potential among maltreated youth is the Resourceful Adolescent Parent Program (RAP-P), which was developed for use with youth after they present to the emergency department for suicidal behavior (Pineda & Dadds, 2013). Like P-CARE, RAP-P provides psychosocial skills and psychoeducation to parents to enhance family-based protective factors and reduce family risk factors for suicidal youth. In an randomized controlled trial, youth whose families enrolled in RAP-P reported less suicide risk at follow-up compared to youth in a treatment-as-usual condition, and this was fully mediated by the effects of RAP-P on parent-reported family functioning (Pineda & Dadds, 2013). Thus, there is evidence of efficacy for family-based indicated suicide prevention programs for youth. However, due to their special family context and circumstances (e.g., placement in foster care; history of abuse in the family context), we recommend that these interventions be tested and adapted specifically for youth with maltreatment histories.
Prevention in reparative social settings
There is potential for suicide prevention strategies for maltreated youth to be implemented in reparative systems, including foster care and juvenile justice settings. Among teenage girls in the juvenile justice system, Multidimensional Treatment Foster Care (a family-based preventative intervention for youth in the foster care system) reduced trajectories of depression symptoms and suicidal ideation at the two-year follow-up (Kerr et al., 2014). Thus, reparative social systems may be an ideal setting for selective suicide prevention interventions that target all youth in that setting, many with maltreatment histories.
More work is needed to integrate universal suicide prevention programs into reparative social systems that are relevant to maltreated youth. Specific future directions in this area include: (a) examining exposure to childhood maltreatment as a moderator of treatment effect in existing upstream prevention interventions; (b) collecting qualitative data on the acceptability and feasibility of existing upstream prevention interventions among children and adolescents with involvement in child welfare services; (c) calibrating new or existing prevention interventions to align with the specific suicide risk factors for maltreated youth, which may be different from risk factors in the general population of adolescents; and (d) developing and/or adapting suicide prevention programs to be implemented in reparative social system settings such as foster care and juvenile justice settings.
Screening
Finally, screening is an essential part of suicide prevention. We have several recommendations for suicide risk screening based on our model. First, given their overall increased risk of suicide, we recommend that child welfare-involved youth be screened regularly for suicide risk factors. Youth who are exposed to child maltreatment are often involved in multiple systems (e.g., healthcare, behavioral health, and child welfare; Cerulli et al., 2021). Accordingly, we recommend a multi-pronged approach to suicide risk screening that involves multiple systems including but not limited to healthcare (e.g., screening at pediatrics well-child visits), child welfare services (e.g., screening by case workers), and court-based settings where many of these children find themselves for issues related to family disruption, custody, visitation and child welfare adjudications. Second, practitioners should screen for suicide risk factors (such as substance use and/or NSSI) among child maltreatment-exposed youth who are already having suicidal thoughts. Identifying such proximal risk factors that predict the transition from suicidal ideation to attempts in samples of child maltreatment-exposed youth will be necessary to inform future screening approaches. Screening tools that may show utility in at-risk populations of youth include the widely used Ask Suicide-Screening Questions (Horowitz et al., 2012), which has been validated for use in multiple clinical settings including hospitals and primary care offices (Aguinaldo et al., 2021; DeVylder et al., 2020), and the newly developed Computerized Adaptive Screen for Suicidal Youth (King et al., 2021).
Implications for clinical interventions
Our conceptual model and current findings on child maltreatment and youth suicide also have implications for clinical practice. We briefly review these implications here, although a full discussion of these implications are beyond the scope of the present paper. First, our model has implications for treatment interventions that aim to prevent suicide among those with indicated risk factors (e.g., current suicidal ideation or a recent suicide attempt). The development, testing, and implementation of indicated suicide prevention interventions is sorely needed. A recent meta-analysis showed that, among all studies in the past 50 years that tested clinical interventions to reduce self-injurious thoughts and behaviors, cumulative effect sizes were small and did not show improvement over time (Fox et al., 2020). Notably, these effect sizes were smallest in studies testing interventions with children and adolescents. This underscores the need for more efficacious interventions to reduce suicidal thoughts and behaviors among young people. However, as noted by Kleiman and colleagues in their recent editorial (2021), these meta-analytic findings do not necessarily indicate the need for novel interventions but instead indicate the need to further refine and improve the efficacy of existing interventions.
Interventions that are individualized for specific subpopulations and risk factors (e.g., youth with maltreatment experiences) may be more effective in reducing suicide risk. Consequently, current interventions to reduce STBs should be modified to treat adolescents and emerging adults with maltreatment exposure. Clinical interventions that focus on the role of family support and repairing familial relationships may be particularly effective for use with adolescents who have experienced maltreatment. Indeed, family-based interventions and interventions that target other sources of social support are effective in reducing adolescent STBs (Brent et al., 2013). Studies that extend these family-based interventions to youth who have histories of maltreatment may be particularly beneficial. For instance, attachment-based family therapy has been shown to be efficacious in reducing suicidal ideation and depressive symptoms among adolescents (Diamond et al., 2010), but to our knowledge has not been tested among youth with maltreatment histories.
Additionally, multiple studies have provided evidence for Dialectical Behavior Therapy for Adolescents as an effective tool for mitigating risk for suicide and self-harm among high-risk youth. For instance, in two randomized trials by McCauley et al. (2018) and Mehlum et al. (2014), results supported Dialectical Behavior Therapy as an efficacious intervention to reduce self-harm, suicidal ideation, and depression among adolescents with repetitive self-harming behavior. Results indicated that improvements in emotion regulation mediated the association between Dialectical Behavior Therapy for Adolescents and reductions in harm behaviors (Asarnow et al., 2021). Additionally, work by Berk et al. (2014) supports the Dialectical Behavior Therapy approach in targeting suicidal and self-harm behaviors and posttraumatic stress disorder symptoms among adolescents exposed to early trauma. Thus, Dialectical Behavior Therapy for Adolescents is a treatment modality with potential to reduce STBs specifically among youth with exposure to child maltreatment, and is consistent with the mechanisms we propose in our conceptual model.
Another possible direction for future research is to modify current interventions that are effective in reducing symptomatology among maltreated youth, into adapted interventions that specifically target the reduction of STBs in this population. Interpersonal Therapy for Depressed Adolescents and Dialectical Behavior Therapy for Adolescents are two modalities of note that target mechanisms included in our model (respectively, interpersonal processes and emotion regulation; Berk et al., 2014; Lipsitz & Markowitz, 2013; Toth et al., 2020). These treatment modalities may have potential application to the treatment of STBs among youth exposed to maltreatment. For example, Interpersonal Therapy for Depressed Adolescents was found to be efficacious in treating depressive symptoms among adolescent girls with a history of maltreatment (Toth et al., 2020). It is possible that an enhanced version of Interpersonal Therapy for Depressed Adolescents of could also effectively treat and reduce suicidal ideation in this population, but this remains to be tested.
Implications for policy
Our model likewise has relevance for suicide prevention policy. First and foremost, upstream suicide prevention involves reducing risk factors that contribute to STBs, including exposure to child maltreatment. Thus, policies to prevent child maltreatment are an important step to reducing suicide among young people. Funding is needed for research on evidence-based or informed child maltreatment prevention services to reduce child maltreatment risk (e.g., Nurse-Family Partnership and other home visiting programs; Olds, 2008). Additionally, policies are needed to support accessible and affordable mental health care, including suicide prevention services, for underserved populations (including families and youth with involvement with CPS). Youth who are in transition from foster care are an especially vulnerable population (Kaspar, 2014) and policies are needed to fund and support services for these youth. Enhancing community-based and culturally informed services are important, as well as including laws that support parity for behavioral healthcare. Schools play an important role in suicide prevention, and resources should be provided to implement suicide prevention strategies in school settings, including trauma-informed training. However, youth impacted by abuse and neglect are at higher risk for dropping out of school, and thus support is also needed for community-based interventions. Ultimately, cross-sector collaborations are needed to support and integrate preventative mental health services for youth with maltreatment histories, including youth involved with CPS and the foster care system. Both public and private sector organizations can play a role in strengthening the services and resources available to youth and families with maltreatment histories to prevent STBs.
Conclusion
To better understand the processes connecting child maltreatment and adolescent suicide, there is a need for a developmentally informed theoretical model that explains and offers hypotheses regarding the risk for suicide in adolescence associated with adverse rearing contexts. In this paper, we reviewed and provided a brief synopsis of the relevant literature on mechanisms and moderators of the link between child maltreatment and youth suicide. Based on this review, the developmental psychopathology framework, and current theories in suicidology, we presented a conceptual model on child maltreatment and the development of suicide risk during adolescence and emerging adulthood.
We acknowledge that there are several limitations of our model, including the potential absence of other variables of interest (e.g., family history of suicidality) that are pertinent to the study of child maltreatment and youth STBs. Additionally, although we propose an integrative conceptual model for youth STBs, several components of our model (e.g., biological and interpersonal mechanisms) overlap with other etiological models of psychopathology. This is understandable given the multifinality of outcomes stemming from child maltreatment and related developmental sequelae, and the recent understanding that there are shared transdiagnostic mechanisms towards multiple forms of psychopathology. Despite these limitations, it is our hope that this conceptual model will provide a starting point for theoretically grounded and developmentally driven research on child maltreatment and youth suicide, and that this future research will iteratively inform modifications to our model’s precepts.
Importantly, given that an estimated 3.5 million youth in the United States are involved in a child maltreatment investigation each year, suicide prevention for youth who suffer these adverse childhood experiences should be an utmost priority in the field (U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, & Children’s Bureau, 2020). Primary prevention of child maltreatment and upstream prevention programs that focus on mending consequences of child maltreatment are necessary to prevent STBs and suicide in this at-risk youth population.
Funding statement.
We are grateful to the National Institute of Child Health and Human Development (P50-HD096698 to Sheree L. Toth and Dante Cicchetti) for their support of this work. Training support was provided to the lead author via the National Institute of Mental Health (T32 MH20061).
Footnotes
Conflicts of interest. None.
In the present manuscript, consistent with literature on resilience and developmental psychopathology (Oshri, Duprey, Liu & Gonzalez, 2020; Zimmerman et al., 2013), we define protective factors as assets or resources that buffer the association between a known risk factor (e.g., child maltreatment) and an unwanted outcome (e.g., STBs). Protective factors are tested statistically with moderation. Similarly, we conceptualize risk factors as those which exacerbate or worsen the likelihood of an adverse outcome. Risk factors can be tested with moderation, such as those risk factors we present in Table 2. Risk factors may often also have a direct association with an adverse outcome.
References
- Adams TR, Handley ED, Warmingham JM, Manly JT, Cicchetti D, & Toth SL (2021). Patterns of dating violence moderate the effect of child maltreatment on suicide risk among disadvantaged minority female adolescents with depressive symptoms. Journal of Family Violence, 36(1), 5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguinaldo LD, Sullivant S, Lanzillo EC, Ross A, He J-P, Bradley-Ewing A, Bridge JA, Horowitz LM, & Wharff EA (2021). Validation of the ask suicide-screening questions (ASQ) with youth in outpatient specialty and primary care clinics. General Hospital Psychiatry, 68(6), 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aikins JW, Howes C, & Hamilton C (2009). Attachment stability and the emergence of unresolved representations during adolescence. Attachment and Human Development, 11(5), 491–512. 10.1080/14616730903017019 [DOI] [PubMed] [Google Scholar]
- Ammerman BA, Serang S, Jacobucci R, Burke TA, Alloy LB, & McCloskey MS (2018). Exploratory analysis of mediators of the relationship between childhood maltreatment and suicidal behavior. Journal of Adolescence, 69, 103–112. 10.1016/j.adolescence.2018.09.004 [DOI] [PubMed] [Google Scholar]
- Angelakis I, Austin JL, & Gooding P (2020). Association of childhood maltreatment with suicide behaviors among young people. JAMA Network Open, 3(8), e2012563. 10.1001/jamanetworkopen.2020.12563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aranmolate R, Bogan DR, Hoard T, & Mawson AR (2017). Suicide risk factors among LGBTQ youth: Review. JSM Schizophr, 2(2), 1011, https://www.researchgate.net/publication/317582401 [Google Scholar]
- Asarnow JR, Berk MS, Bedics J, Adrian M, Gallop R, Cohen J,Korslund K, Hughes J, Avina C, Linehan MM, McCauley E (2021). Dialectical behavior therapy for suicidal self-harming youth: Emotion regulation, mechanisms, and mediators. Journal of the American Academy of Child & Adolescent Psychiatry, 60(9), 1105–1115.e4. 10.1016/j.jaac.2021.01.016 [DOI] [PubMed] [Google Scholar]
- Barbot B, Eff H, Weiss SR, & McCarthy JB (2020). The role of psychopathology in the relationship between history of maltreatment and suicide attempts among children and adolescent inpatients. Child and Adolescent Mental Health, 10.1111/camh.12393 [DOI] [PubMed] [Google Scholar]
- Berens AE, Jensen SKG, & Nelson CA (2017). Biological embedding of childhood adversity: From physiological mechanisms to clinical implications. BMC Medicine, 15(1), 1–12. 10.1186/s12916-017-0895-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berk MS, Shelby J, Avina C, & Tangeman KR (2014). Dialectical behavior therapy for suicidal and self-harming adolescents with trauma symptoms. In Timmer S, & Urquiza A (Eds.), Evidence-based approaches for the treatment of maltreated children: Considering core components and treatment effectiveness (pp. 215–236). Springer. 10.1007/978-94-007-7404-9_12 [DOI] [Google Scholar]
- Bernard K, Butzin-Dozier Z, Rittenhouse J, & Dozier M (2010). Cortisol production patterns in young children living with birth parents vs children placed in foster care following involvement of Child Protective Services. Archives of Pediatrics & Adolescent Medicine, 164(5), 438–443. 10.1001/archpediatrics.2010.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolger KE, & Patterson CJ (2001). Pathways from child maltreatment to internalizing problems: Perceptions of control as mediators and moderators. Development and Psychopathology, 13(4), 913–940. 10.1017/S0954579401004096 [DOI] [PubMed] [Google Scholar]
- Bosch NM, Riese H, Reijneveld SA, Bakker MP, Verhulst FC,Ormel J, & Oldehinkel AJ (2012). Timing matters: Long term effects of adversities from prenatal period up to adolescence on adolescents’ cortisol stress response. The TRAILS study. Psychoneuroendocrinology, 37(9), 1439–1447. 10.1016/j.psyneuen.2012.01.013 [DOI] [PubMed] [Google Scholar]
- Braquehais MD, Oquendo MA, Baca-García E, & Sher L (2010). Is impulsivity a link between childhood abuse and suicide? Comprehensive Psychiatry, 51(2), 121–129. 10.1016/j.comppsych.2009.05.003 [DOI] [PubMed] [Google Scholar]
- Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, & Douaihy AB (2013). Protecting adolescents from self-harm: A critical review of intervention studies. Journal of the American Academy of Child and Adolescent Psychiatry, 52(12), 1260–1271. 10.1016/j.jaac.2013.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezo J, Paris J, Vitaro F, Hebert M, Tremblay RE, & Turecki G (2008). Predicting suicide attempts in young adults with histories of childhood abuse. The British Journal of Psychiatry, 193(2), 134–139. [DOI] [PubMed] [Google Scholar]
- Bridge JA, Asti L, Horowitz LM, Greenhouse JB, Fontanella CA, Sheftall AH, Kelleher KJ, & Campo J.v (2015). Suicide trends among elementary school-aged children in the United States from 1993 to 2012. JAMA Pediatrics, 169(7), 673–677. 10.1001/jamapediatrics.2015.0465 [DOI] [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, & Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47(3–4), 372–394. 10.1111/j.1469-7610.2006.01615.x [DOI] [PubMed] [Google Scholar]
- Bruffaerts R, Demyttenaere K, Borges G, Haro JM, Chiu WT, Hwang I, Karam EG, Kessler RC, Sampson N, Alonso J, Andrade LH, Angermeyer M, Benjet C, Bromet E, de Girolamo G, de Graaf R, Florescu S, Gureje O, Horiguchi I, Nock MK, & et al. (2010). Childhood adversities as risk factors for onset and persistence of suicidal behaviour. British Journal of Psychiatry, 197(1), 20–27. 10.1192/bjp.bp.109.074716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caine ED, Reed J, Hindman J, & Quinlan K (2018). Comprehensive, integrated approaches to suicide prevention: Practical guidance. Injury Prevention, 24(Suppl 1), i38–i45. 10.1136/injuryprev-2017-042366 [DOI] [PubMed] [Google Scholar]
- Campo J.v (2009). Youth suicide prevention: Does access to care matter? Current Opinion in Pediatrics, 21(5), 628–634. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cero I, & Sifers S (2013). Moderating factors in the path from physical abuse to attempted suicide in adolescents: Application of the interpersonal-psychological theory of suicide. Suicide and Life-Threatening Behavior, 43(3), 296–304. 10.1111/sltb.12016 [DOI] [PubMed] [Google Scholar]
- Cerulli C, Cicchetti D, Handley ED, Manly JT, Rogosch FA, & Toth SL (2021). Transforming the paradigm of child welfare. Development and Psychopathology, 33(2), 377–393. 10.1017/S0954579420002138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan PT, Doan SN, & Tompson MC (2014). Stress generation in a developmental context: The role of youth depressive symptoms, maternal depression, the parent-child relationship, and family stress. Journal of Family Psychology, 28(1), 32–41. 10.1037/a0035277 [DOI] [PubMed] [Google Scholar]
- Cho S, & Glassner S (2020). Examining the mediating effects of negative emotions on the link between multiple strains and suicidal ideation: A longitudinal analysis. Archives of Suicide Research, 24(sup1), 380–399. 10.1080/13811118.2019.1586604 [DOI] [PubMed] [Google Scholar]
- Chu JP, Goldblum P, Floyd R, & Bongar B (2010). The cultural theory and model of suicide. Applied and Preventive Psychology, 14(1–4), 25–40. 10.1016/j.appsy.2011.11.001 [DOI] [Google Scholar]
- Cicchetti D (1984). The emergence of developmental psychopathology. Child Development, 55(1), 1–7. [PubMed] [Google Scholar]
- Cicchetti D, & Banny A (2014). A developmental psychopathology perspective on child maltreatment. In Lewis M, & Rudolph KD (Eds.), Handbook of developmental psychopathology (pp. 723–741). Springer. 10.1007/978-1-4614-9608-3_37 [DOI] [Google Scholar]
- Cicchetti D, & Handley ED (2019). Child maltreatment and the development of substance use and disorder. Neurobiology of Stress, 10, 100144. 10.1016/j.ynstr.2018.100144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Hetzel S, Rogosch FA, Handley ED, & Toth SL (2016). An investigation of child maltreatment and epigenetic mechanisms of mental and physical health risk. Development and Psychopathology, 28(4pt2), 1305–1317. 10.1017/S0954579416000869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Rogosch FA (2002). A developmental psychopathology perspective on adolescence. Journal of Consulting and Clinical Psychology, 70(1), 6–20. 10.1037/0022-006X.70.1.6 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Gunnar MR, & Toth SL (2010). The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school-aged children. Child Development, 81(1), 252–269. 10.1111/j.1467-8624.2009.01393.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Sturge-Apple M, & Toth SL (2010). Interaction of child maltreatment and 5-HTT polymorphisms: Suicidal ideation among children from low-SES backgrounds. Journal of Pediatric Psychology, 35(5), 536–546. 10.1093/jpepsy/jsp078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL, & Sturge-Apple ML (2011). Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology, 23(3), 789–800. 10.1017/S0954579411000307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, & Toth SL (2016). Child maltreatment and developmental psychopathology: A multilevel perspective. In Developmental psychopathology (pp. 1–56). John Wiley & Sons, Inc. 10.1002/9781119125556.devpsy311 [DOI] [Google Scholar]
- Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, & Maughan B (2007). Resilience to adult psychopathology following childhood maltreatment: Evidence from a community sample. Child Abuse & Neglect, 31(3), 211–229. [DOI] [PubMed] [Google Scholar]
- Coohey C, Dirks-Bihun A, Renner LM, & Baller R (2014). Strain, depressed mood and suicidal thoughts among maltreated adolescents in the United States. Child Abuse & Neglect, 38(7), 1171–1179. 10.1016/j.chiabu.2014.04.008 [DOI] [PubMed] [Google Scholar]
- Cromer KD, Villodas MT, & Chou T (2019). Gender differences in psychological distress as a mediational pathway to suicidal ideation among adolescents at high risk for victimization by violence. Psychology of Violence, 9(6), 587–595. 10.1037/vio0000200 [DOI] [Google Scholar]
- Crosby AE, Ortega L, & Melanson C (2011). Self-directed violence surveillance: Uniform definitions and recommended data elements, Version 1.0. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Google Scholar]
- Crowell SE, Beauchaine TP, & Lenzenweger MF (2008). The development of borderline personality disorder and self-injurious behavior. In Beauchaine TP, & Hinshaw SP (Eds.), Child and adolescent psychopathology (pp. 510–539). John Wiley & Sons. [Google Scholar]
- Curtin SC, & Heron M (2019). Death rates due to suicide and homicide among persons aged 10–24: United States, 2000 – 2017. NCHS Data Brief, no 352. [PubMed] [Google Scholar]
- D’Eramo KS, Prinstein MJ, Freeman J, Grapentine WL, & Spirito A (2004). Psychiatric diagnoses and comorbidity in relation to suicidal behavior among psychiatrically hospitalized adolescents. Child Psychiatry and Human Development, 35(1), 21–35. 10.1023/B:CHUD.0000039318.72868 [DOI] [PubMed] [Google Scholar]
- Dawes MA, Mathias CW, Richard DM, Hill-Kapturczak N, & Dougherty DM (2008). Adolescent suicidal behavior and substance use: Developmental mechanisms. Substance Abuse: Research and Treatment, 2(210), SART.S1044. 10.4137/SART.S1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- del Giudice M, Ellis BJ, & Shirtcliff E.a (2011). The Adaptive Calibration Model of stress responsivity. Neuroscience & Biobehavioral Reviews, 35(7), 1562–1592. 10.1016/j.neubiorev.2010.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demeusy EM, Handley ED, Manly JT, Sturm R, & Toth SL (2021). Building Healthy Children: A preventive intervention for high-risk young families. Development and Psychopathology, 33(2), 598–613. 10.1017/S0954579420001625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derbridge CM, & Beauchaine TP (2014). A developmental model of self-inflicted injury, borderline personality, and suicide risk. In Lewis M, & Rudolph K (Eds.), Handbook of developmental psychopathology (pp. 521–542). Springer. 10.1007/978-1-4615-4163-9 [DOI] [Google Scholar]
- DeVylder JE, Ryan TC, Cwik M, Jay SY, Wilson ME, Goldstein M, & Wilcox HC (2020). Screening for suicide risk among youths with a psychotic disorder in a pediatric emergency department. Psychiatric Services, 71(2), 205–208. [DOI] [PubMed] [Google Scholar]
- Diamond GS, Wintersteen MB, Brown GK, Diamond GM, Gallop R, Shelef K, & Levy S (2010). Attachment-based family therapy for adolescents with suicidal ideation: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 49(2), 122–131. 10.1016/j.jaac.2009.11.002 [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA, 286(24), 3089. 10.1001/jama.286.24.3089 [DOI] [PubMed] [Google Scholar]
- Dunn EC, McLaughlin KA, Slopen N, Rosand J, & Smoller JW (2013). Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: Results from the national longitudinal study of adolescent health. Depression and Anxiety, 30(10), 955–964. 10.1002/da.22102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duprey EB, Handley ED, Manly JT, Cicchetti D, & Toth SL (2021). Child maltreatment, recent stressful life events, and suicide ideation: A test of the stress sensitivity hypothesis. Child Abuse and Neglect, 113, 104926. 10.1016/j.chiabu.2020.104926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Caughy MO (2017). Childhood neglect, internalizing symptoms and adolescent substance use: Does the neighborhood context matter? Journal of Youth and Adolescence, 46(7), 1582–1597. 10.1007/s10964-017-0672-x [DOI] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Liu S (2019a). Childhood maltreatment, self-esteem, and suicidal ideation in a low-SES emerging adult sample: The moderating role of heart rate variability. Archives of Suicide Research, 23(2), 333–352. [DOI] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Liu S (2019b). Developmental pathways from child maltreatment to adolescent suicide-related behaviors: The internalizing and externalizing comorbidity hypothesis. Development and Psychopathology, 32(3), 945–959. 10.1017/S0954579419000919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenlohr-Moul TA, Miller AB, Giletta M, Hastings PD, Rudolph KD, Nock MK, & Prinstein MJ (2018). HPA axis response and psychosocial stress as interactive predictors of suicidal ideation and behavior in adolescent females: A multilevel diathesis-stress framework. Neuropsychopharmacology, 43(13), 2564–2571. 10.1038/s41386-018-0206-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emergency Taskforce on Black Youth Suicide and Mental Health (2019). Ring the alarm: The crisis of Black youth suicide in America. 10.1017/s1742058x20000132 [DOI]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, & Dubowitz H (2005). Maltreatment’s wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect, 29(5), 597–619. 10.1016/j.chiabu.2004.12.008 [DOI] [PubMed] [Google Scholar]
- Esposito CL, & Clum GA (2002). Social support and problem-solving as moderators of the relationship between childhood abuse and suicidality: Applications to a delinquent population. Journal of Traumatic Stress, 15(2), 137–146. 10.1023/A:1014860024980 [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, & Spirito A (2004). Adolescent substance use and suicidal behavior: A review with implications for treatment research. Alcoholism: Clinical and Experimental Research, 28(5 Suppl), 77–88. 10.1097/01.alc.0000127417.99752.87 [DOI] [PubMed] [Google Scholar]
- Falgares G, Marchetti D, Manna G, Musso P, Oasi O, Kopala-Sibley DC, de Santis S, & Verrocchio MC (2018). Childhood maltreatment, pathological personality dimensions, and suicide risk in young adults. Frontiers in Psychology, 9, 1–12. 10.3389/fpsyg.2018.00806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Woodward LJ, & Horwood LJ (2000). Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychological Medicine, 30(1), 23–39. 10.1017/S003329179900135X [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KM, Piko BF, & Miller E (2008). Suicide ideation and attempts among low-income African American adolescents. Suicide and Life-Threatening Behavior, 38(5), 552–563. [DOI] [PubMed] [Google Scholar]
- Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, & Campo J.v (2015). Widening rural-urban disparities in youth suicides, United States, 1996–2010. JAMA Pediatrics, 169(5), 466. 10.1001/jamapediatrics.2014.3561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox KR, Huang X, Guzmán EM, Funsch KM, Cha CB, Ribeiro JD, & Franklin JC (2020). Interventions for suicide and self-injury: A meta-analysis of randomized controlled trials across nearly 50 years of research. Psychological Bulletin, 146(12), 1117–1145. 10.1037/bul0000305 [DOI] [PubMed] [Google Scholar]
- Frankenhuis WE, Young ES, & Ellis BJ (2020). The hidden talents approach: Theoretical and methodological challenges. Trends in Cognitive Sciences, 24(7), 569–581. 10.1016/j.tics.2020.03.007 [DOI] [PubMed] [Google Scholar]
- Fuhrmann D, Knoll LJ, & Blakemore SJ (2015). Adolescence as a sensitive period of brain development. Trends in Cognitive Sciences, 19(10), 558–566. 10.1016/j.tics.2015.07.008 [DOI] [PubMed] [Google Scholar]
- George SE, Page AC, Hooke GR, & Stritzke WGK (2016). Multifacet assessment of capability for suicide: Development and prospective validation of the acquired capability with rehearsal for suicide scale. Psychological Assessment, 28(11), 1452–1464. 10.1037/pas0000276 [DOI] [PubMed] [Google Scholar]
- Giletta M, Calhoun CD, Hastings PD, Rudolph KD, Nock MK, & Prinstein MJ (2015). Multi-level risk factors for suicidal ideation among at-risk adolescent females: The role of hypothalamic-pituitary-adrenal axis responses to stress. Journal of Abnormal Child Psychology, 43(5), 807–820. 10.1007/s10802-014-9897-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon R (1987). An operational classification of disease prevention. In Preventing mental disorders: A research perspective (pp. 20–26). National Institute of Mental Health. [Google Scholar]
- Graves JM, Abshire DA, Mackelprang JL, Amiri S, & Beck A (2020). Association of rurality with availability of youth mental health facilities with suicide prevention services in the US. JAMA Network Open, 3(10), e2021471. 10.1001/jamanetworkopen.2020.21471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M, & Quevedo K (2007). The neurobiology of stress and development. Annual Review of Psychology, 58(1), 145–173. 10.1146/annurev.psych.58.110405.085605 [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Morison SJ, Chisholm K, & Schuder M (2001). Salivary cortisol levels in children adopted from Romanian orphanages. Development and Psychopathology, 13(3), 611–628. 10.1017/S095457940100311X [DOI] [PubMed] [Google Scholar]
- Hallowell ES, Oshri A, Liebel SW, Liu S, Duda B, Clark US, &Sweet LH (2019). The mediating role of neural activity on the relationship between childhood maltreatment and impulsivity. Child Maltreatment, 24(4), 389–399. 10.1177/1077559519835975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Adams TR, Manly JT, Cicchetti D, & Toth SL (2019). Mother-daughter interpersonal processes underlying the association between child maltreatment and adolescent suicide ideation. Suicide and Life-Threatening Behavior, 49(5), 1232–1240. 10.1111/sltb.12522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handley ED, Warmingham JM, Rogosch FA, & Cicchetti D (2019). Infancy onset maltreatment and the development of suicide ideation: An investigation of moderation by oxytocin-related gene polymorphisms. Journal of Affective Disorders, 257(June), 421–427. 10.1016/j.jad.2019.06.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL (2005). Childhood maltreatment and psychopathology: Prospective tests of attachment, cognitive vulnerability, and stress as mediating processes. Cognitive Therapy and Research, 29(6), 645–671. 10.1007/s10608-005-9631-z [DOI] [Google Scholar]
- Harkness KL, Stewart JG, & Wynne-Edwards KE (2011). Cortisol reactivity to social stress in adolescents: Role of depression severity and child maltreatment. Psychoneuroendocrinology, 36(2), 173–181. 10.1016/j.psyneuen.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Harris LM, & Ribeiro JD (2021). Does fearlessness about death mediate the association between NSSI and suicide attempts? A longitudinal study of over 1,000 high-risk individuals. Journal of Consulting and Clinical Psychology, 89(3), 176–187. 10.1037/ccp0000626 [DOI] [PubMed] [Google Scholar]
- Harter S (2006). The self. In Damon W, & Lerner RM (Eds.), Handbook of child psychology (6th ed., pp. 505–570). John Wiley & Sons. [Google Scholar]
- Harter S (2016). I-self and me-self processes affecting developmental psychopathology and mental health. In Cicchetti D (Eds.), Developmental psychopathology, theory and method (3rd ed., pp. 470–526). John Wiley & Sons. [Google Scholar]
- Hatkevich C, Penner F, & Sharp C (2019). Difficulties in emotion regulation and suicide ideation and attempt in adolescent inpatients. Psychiatry Research, 271, 230–238. 10.1016/j.psychres.2018.11.038 [DOI] [PubMed] [Google Scholar]
- Hein TC, & Monk CS (2017). Research review: Neural response to threat in children, adolescents, and adults after child maltreatment – a quantitative meta-analysis. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58(3), 222–230. 10.1111/jcpp.12651 [DOI] [PubMed] [Google Scholar]
- Hinduja S, & Patchin JW (2010). Bullying, cyberbullying, and suicide. Archives of Suicide Research, 14(3), 206–221. 10.1080/13811118.2010.494133 [DOI] [PubMed] [Google Scholar]
- Hoertel N, Franco S, Wall MM, Oquendo MA, Wang S, Limosin F, & Blanco C (2015). Childhood maltreatment and risk of suicide attempt: A nationally representative study. Journal of Clinical Psychiatry, 76(7), 916–923. 10.4088/JCP.14m09420 [DOI] [PubMed] [Google Scholar]
- Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, Wolfe M, & Reid G (2015). Bullying and suicidal ideation and behaviors: A meta-analysis. Pediatrics, 135(2), e496–e509. 10.1542/peds.2014-1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong JS, Espelage DL, Grogan-Kaylor A, & Allen-Meares P (2012). Identifying potential mediators and moderators of the association between child maltreatment and bullying perpetration and victimization in school. Educational Psychology Review, 24(2), 167–186. 10.1007/s10648-011-9185-4 [DOI] [Google Scholar]
- Hooven C, Walsh E, Pike KC, & Herting JR (2012). Promoting CARE: Including parents in youth suicide prevention. Family and Community Health, 35(3), 225–235. 10.1097/FCH.0b013e318250bcf9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, Wharff EA, Ginnis K, Cannon E, Joshi P, Pao M (2012). Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Archives of Pediatrics & Adolescent Medicine, 166(12), 1170–1176. 10.1001/archpediatrics.2012.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AG, Czyz EK, & King CA (2015). Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. Journal of Clinical Child & Adolescent Psychology, 44(5), 751–761. 10.1080/15374416.2014.910789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman LG, Oshri A, & Caughy M (2020). An autonomic nervous system context of harsh parenting and youth aggression versus delinquency. Biological Psychology, 156, 107966. 10.1016/j.biopsycho.2020.107966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Guyon-Harris KL, Tibu F, Wade M, Nelson CA, Fox NA, & Zeanah CH (2020). Psychiatric outcomes following severe deprivation in early childhood: Follow-up of a randomized controlled trial at age 16. Journal of Consulting and Clinical Psychology, 88(12), 1079–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel TR, & Gogtay N (2014). National Institute of Mental Health Clinical Trials. JAMA Psychiatry, 71(7), 745. 10.1001/jamapsychiatry.2014.426 [DOI] [PubMed] [Google Scholar]
- Irwin MR, & Cole SW (2011). Reciprocal regulation of the neural and innate immune systems. Nature Reviews. Immunology, 11(9), 625–632. 10.1038/nri3042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivey-Stephenson AZ, Demissie Z, Crosby AE, Stone DM, Gaylor E, Wilkins N, Lowry R, & Brown M (2020). Suicidal ideation and behaviors among high school students - Youth Risk Behavior Survey, United States. 2019 MMWR Supplements, 69(1), 47–55. 10.15585/mmwr.su6901a6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, & Brook JS (2002). Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Archives of General Psychiatry, 59(8), 741–749. 10.1001/archpsyc.59.8.741 [DOI] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, Lowry R, Chyen D, Whittle L, Thornton J, Lim C, Bradford D, Yamakawa Y, Leon M, Brener N, Ethier K (2018). Youth Risk Behavior Surveillance-United States 2017. MMWR Surveillance Summaries 2018, 67(8). 10.1144/jmpaleo2015-007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaspar V (2014). Long-term depression and suicidal ideation outcomes subsequent to emancipation from foster care: Pathways to psychiatric risk in the Métis population. Psychiatry Research, 215(2), 347–354. 10.1016/j.psychres.2013.09.003 [DOI] [PubMed] [Google Scholar]
- Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, Toyinbo P, Petras H, Ford C, Windham A, Wilcox HC (2008). Effects of a universal classroom behavior management program in first and second grades on young adult behavioral, psychiatric, and social outcomes. Drug and Alcohol Dependence, 95(Suppl 1). 10.1016/j.drugalcdep.2008.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly TM, Cornelius JR, & Lynch KG (2002). Psychiatric and substance use disorders as risk factors for attempted suicide among adolescents: A case control study. Suicide and Life-Threatening Behavior, 32(3), 301–312. 10.1521/suli.32.3.301.22168 [DOI] [PubMed] [Google Scholar]
- Kerr DCR, DeGarmo DS, Leve LD, & Chamberlain P (2014). Juvenile justice girls’ depressive symptoms and suicidal ideation 9 years after multidimensional treatment foster care. Journal of Consulting and Clinical Psychology, 82(4), 684–693. 10.1037/a0036521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kim J (2020). Suicidal ideation in adolescence: The role of in-home firearm access and childhood maltreatment. Child and Youth Care Forum, 49(1), 121–149. 10.1007/s10566-019-09522-8 [DOI] [Google Scholar]
- Kim H, Wildeman C, Jonson-Reid M, & Drake B (2017). Lifetime prevalence of investigating child maltreatment among US children. American Journal of Public Health, 107(2), 274–280. 10.2105/AJPH.2016.303545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2006). Longitudinal trajectories of self-system processes and depressive symptoms among maltreated and nonmaltreated children. Child Development, 77(3), 624–639. 10.1111/j.1467-8624.2006.00894.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2009). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Spoon J, Cicchetti D, & Rogosch FA (2013). A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development, 84(2), 512–527. 10.1111/j.1467-8624.2012.01857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Brent D, Grupp-Phelan J, Casper TC, Dean JM,Chernick LS, Fein JA, Mahabee-Gittens EM, Patel SJ, Mistry RD (2021). Prospective development and validation of the computerized adaptive screen for suicidal youth. JAMA Psychiatry, 78(5), 540–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Bentley KH, Glenn CR, Liu RT, & Rizvi SL (2021). Building on the past 50 years, not starting over: A balanced interpretation of meta-analyses, reviews, and commentaries on treatments for suicide and self-injury. General Hospital Psychiatry, 74(6), 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky E, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the, ideation-to-action. framework International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/ijct.2015.8.2.114 [DOI] [Google Scholar]
- Klonsky ED, May AM, & Saffer BY (2016). Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology, 12(1), 307–330. 10.1146/annurev-clinpsy-021815-093204 [DOI] [PubMed] [Google Scholar]
- Koss KJ, & Gunnar MR (2018). Annual Research Review: Early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. Journal of Child Psychology and Psychiatry, 59(4), 327–346. 10.1111/jcpp.12784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok SY, Gu M, & Cheung A (2019). A longitudinal study on the relationship among childhood emotional abuse, gratitude, and suicidal ideation of Chinese adolescents. Child Abuse & Neglect, 94, 104031. [DOI] [PubMed] [Google Scholar]
- Kwok SYCL, & Gu M (2019). Childhood neglect and adolescent suicidal ideation: A moderated mediation model of hope and depression. Prevention Science, 20(5), 632–642. 10.1007/s11121-018-0962-x [DOI] [PubMed] [Google Scholar]
- Kwok SYCL, Yeung JWK, Low AYT, Lo HHM, & Tam CHL (2015). The roles of emotional competence and social problem-solving in the relationship between physical abuse and adolescent suicidal ideation in China. Child Abuse & Neglect, 44, 117–129. 10.1016/j.chiabu.2015.03.020 [DOI] [PubMed] [Google Scholar]
- Laszlo A, & Krippner S (1998). Systems theories: Their origins, foundations, and development. In Jordan JS (Eds.), Systems theories and a priori aspects of perception (pp. 47–74). Elsevier. 10.1016/S0166-4115(98)80017-4 [DOI] [Google Scholar]
- Lavi I, Katz LF, Ozer EJ, & Gross JJ (2019). Emotion reactivity and regulation in maltreated children: A meta-analysis. Child Development, 90(5), 1503–1524. 10.1111/cdev.13272 [DOI] [PubMed] [Google Scholar]
- Lerner RM, & Castellino DR (2002). Contemporary developmental theory and adolescence: Developmental systems and applied developmental science. Journal of Adolescent Health, 31(6 Suppl), 122–135, 10.1016/S1054-139X(02)00495-0, [DOI] [PubMed] [Google Scholar]
- Lewis TL, Kotch J, Wiley TRA, Litrownik AJ, English DJ, Thompson R, Zolotor AJ, Block SD, & Dubowitz H (2011). Internalizing problems: A potential pathway from childhood maltreatment to adolescent smoking. Journal of Adolescent Health, 48(3), 247–252. 10.1016/j.jadohealth.2010.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Chen Z, Gong Q, & Jia Z (2020). Voxel-wise meta-analysis of task-related brain activation abnormalities in major depressive disorder with suicide behavior. Brain Imaging and Behavior, 14(4), 1298–1308. 10.1007/s11682-019-00045-3 [DOI] [PubMed] [Google Scholar]
- Li X, You J, Ren Y, Zhou J, Sun R, Liu X, & Leung F (2019). A longitudinal study testing the role of psychache in the association between emotional abuse and suicidal ideation. Journal of Clinical Psychology, 75(12), 2284–2292. 10.1002/jclp.22847 [DOI] [PubMed] [Google Scholar]
- Lipsitz JD, & Markowitz JC (2013). Mechanisms of change in interpersonal therapy (IPT). Clinical Psychology Review, 33(8), 1134–1147. 10.1016/j.cpr.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Scopelliti KM, Pittman SK, & Zamora AS (2018). Childhood maltreatment and non-suicidal self-injury: A systematic review and meta-analysis. The Lancet Psychiatry, 5(1), 51–64. 10.1016/S2215-0366(17)30469-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Cui Z, Duprey EB, Kogan SM, & Oshri A (2020). Adverse parenting is indirectly linked to delayed reward discounting via blunted RSA reactivity: The protective role of a shift-and-persist coping strategy. Adversity and Resilience Science, 1(3), 149–163. 10.1007/s42844-020-00012-8 [DOI] [Google Scholar]
- Logan-Greene P, Tennyson RL, Nurius PS, & Borja S (2017). Adverse childhood experiences, coping resources, and mental health problems among court-involved youth. Child and Youth Care Forum, 46(6), 923–946. 10.1007/s10566-017-9413-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR (2013). Early life adversity reduces stress reactivity and enhances impulsive behavior: Implications for health behaviors. International Journal of Psychophysiology, 90(1), 8–16. 10.1016/j.ijpsycho.2012.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low YTA, Kwok SYCL, Tam HLC, Yeung WKJ, & Lo HHM (2017). The relationship between childhood physical abuse and suicidal ideation among Chinese university students: Possible moderators. Children and Youth Services Review, 81, 94–100. 10.1016/j.childyouth.2017.07.026 [DOI] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology, 13(4), 759–782. [PubMed] [Google Scholar]
- Marques-Feixa L, Moya-Higueras J, Romero S, Santamarina-Pérez P, Rapado-Castro M, Zorrilla I, Martín M, Anglada E, Lobato MJ, Ramírez M, Moreno N, Mayoral M, Marín-Vila M, Arias B, Fañanás L, & Epi-Young Stress Group (2021). Risk of suicidal behavior in children and adolescents exposed to maltreatment: The mediating role of borderline personality traits and recent stressful life events. Journal of Clinical Medicine, 10(22), 5293. 10.3390/jcm10225293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B, Heron J, Klonsky ED, Moran P, O’Connor RC, Tilling K, Wilkinson P, & Gunnell D (2019). Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: A population-based birth cohort study. The Lancet Psychiatry, 6(4), 327–337. 10.1016/S2215-0366(19)30030-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, Avina C, Hughes J, Harned M, Gallop R (2018). Efficacy of dialectical behavior therapy for adolescents at high risk for suicide: A randomized clinical trial. JAMA Psychiatry, 75(8), 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor SLT (2018). Understanding and evaluating research: A critical guide. In Understanding and evaluating research: A critical guide. SAGE Publications, Inc. 10.4135/9781071802656 [DOI] [Google Scholar]
- McLaughlin KA, & Lambert HK (2017). Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Current Opinion in Psychology, 14, 29–34. 10.1016/j.copsyc.2016.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Peverill M, Gold AL, Alves S, & Sheridan MA (2015). Child maltreatment and neural systems underlying emotion regulation. Journal of the American Academy of Child & Adolescent Psychiatry, 54(9), 753–762. 10.1016/j.jaac.2015.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Alves S, & Mendes WB (2014). Child maltreatment and autonomic nervous system reactivity: Identifying dysregulated stress reactivity patterns using the biopsychosocial model of challenge and threat. Psychosomatic Medicine, 76(7), 538–546. 10.1097/PSY.0000000000000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehlum L, Tørmoen AJ, Ramberg M, Haga E, Diep LM, Laberg S,Larsson BS, Stanley BH, Miller AL, Sund AM (2014). Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(10), 1082–1091. [DOI] [PubMed] [Google Scholar]
- Miller AB, Adams LM, Esposito-Smythers C, Thompson R, &Proctor LJ (2014). Parents and friendships: A longitudinal examination of interpersonal mediators of the relationship between child maltreatment and suicidal ideation. Psychiatry Research, 220(3), 998–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, & Esposito-Smythers C (2013). How do cognitive distortions and substance-related problems affect the relationship between child maltreatment and adolescent suicidal ideation? Psychology of Violence, 3(4), 340–353. 10.1037/a0031355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Esposito-Smythers C, Weismoore JT, & Renshaw KD (2013). The relation between child maltreatment and adolescent suicidal behavior: A systematic review and critical examination of the literature. Clinical Child and Family Psychology Review, 16(2), 146–172. 10.1007/s10567-013-0131-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, & Prinstein MJ (2019). Adolescent suicide as a failure of acute stress-response systems. Annual Review of Clinical Psychology, 15(1), 425–450. 10.1146/annurev-clinpsy-050718-095625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomer AR, Roth KB, Kellam SG, Wang W, Ialongo NS, Hart SR, Wagner BM, & Wilcox HC (2016). Higher childhood peer reports of social preference mediates the impact of the good behavior game on suicide attempt. Prevention Science, 17(2), 145–156. 10.1007/s11121-015-0593-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9(11), e1001349. 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obradović J (2012). How can the study of physiological reactivity contribute to our understanding of adversity and resilience processes in development? Development and Psychopathology, 24(2), 371–387. 10.1017/S0954579412000053 [DOI] [PubMed] [Google Scholar]
- Olds DL (2008). Preventing child maltreatment and crime with prenatal and infancy support of parents: The Nurse-Family Partnership. Journal of Scandinavian Studies in Criminology and Crime Prevention, 9(sup1), 2–24. 10.1080/14043850802450096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Duprey E, Liu S, & Gonzalez A (2020). ACEs and resilience: Methodological and conceptual issues. In Asmundson GJG, & Afifi TO (Eds.), Adverse childhood experiences (pp. 287–306). Academic Press. 10.1016/B978-0-12-816065-7.00014-8 [DOI] [Google Scholar]
- Oshri A, Duprey EB, Kogan SM, Carlson MW, & Liu S (2018). Growth patterns of future orientation among maltreated youth: A prospective examination of the emergence of resilience. Developmental Psychology, 54, 1456–1471. 10.1037/dev0000528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Duprey EB, Liu S, & Ehrlich KB (2020). Harsh parenting and youth systemic inflammation: Modulation by the autonomic nervous system. Health Psychology, 39(6), 482–496. 10.1037/hea0000852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Gray JC, Owens MM, Liu S, Duprey EB, Sweet LH, &MacKillop J (2019). Adverse childhood experiences and amygdalar reduction: High-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreatment, 24(4), 400–410. 10.1177/1077559519839491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Liu S, Duprey EB, & MacKillop J (2018). Child maltreatment, delayed reward discounting, and alcohol and other drug use problems: The moderating role of heart rate variability. Alcoholism: Clinical and Experimental Research, 42(10), 2033–2046. 10.1111/acer.13858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A, Rogosch FA, Burnette ML, & Cicchetti D (2011). Developmental pathways to adolescent cannabis abuse and dependence: Child maltreatment, emerging personality, and internalizing versus externalizing psychopathology. Psychology of Addictive Behaviors, 25(4), 634–644. 10.1037/a0023151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacios-Barrios EE, & Hanson JL (2019). Poverty and self-regulation: Connecting psychosocial processes, neurobiology, and the risk for psychopathology. Comprehensive Psychiatry, 90, 52–64. 10.1016/j.comppsych.2018.12.012 [DOI] [PubMed] [Google Scholar]
- Palusci VJ,& Botash AS (2021). Race and bias in child maltreatment diagnosis and reporting. Pediatrics, 148(1). 10.1542/peds.2020-049625 [DOI] [PubMed] [Google Scholar]
- Pan LA, Hassel S, Segreti AM, Nau SA, Brent DA, & Phillips ML (2013). Differential patterns of activity and functional connectivity in emotion processing neural circuitry to angry and happy faces in adolescents with and without suicide attempt. Psychological Medicine, 43(10), 2129–2142. 10.1017/S0033291712002966 [DOI] [PubMed] [Google Scholar]
- Paul E, & Ortin A (2019). Psychopathological mechanisms of early neglect and abuse on suicidal ideation and self-harm in middle childhood. European Child and Adolescent Psychiatry, 28(10), 1311–1319. 10.1007/s00787-019-01287-8 [DOI] [PubMed] [Google Scholar]
- Pechtel P,& Pizzagalli DA (2011). Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology, 214(1), 55–70. 10.1007/s00213-010-2009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peh CX, Shahwan S, Fauziana R, Mahesh M.v, Sambasivam R, Zhang YJ, Ong SH, Chong SA, & Subramaniam M (2017). Emotion dysregulation as a mechanism linking child maltreatment exposure and self-harm behaviors in adolescents. Child Abuse and Neglect, 67, 383–390. 10.1016/j.chiabu.2017.03.013 [DOI] [PubMed] [Google Scholar]
- Pelkonen M, Karlsson L, & Marttunen M (2011). Child and adolescent suicide: Epidemiology, risk factors, and approaches to prevention. Current Pediatric Reviews, 7(1), 52–67. 10.2174/157339611795429080 [DOI] [Google Scholar]
- Peña JB, Kuhlberg JA, Zayas LH, Baumann AA, Gulbas L, Hausmann-Stabile C, & Nolle AP (2011). Familism, family environment, and suicide attempts among Latina youth. Suicide and Life-Threatening Behavior, 41(3), 330–341. 10.1111/j.1943-278X.2011.00032.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepin EN, & Banyard VL (2006). Social support: A mediator between child maltreatment and developmental outcomes. Journal of Youth and Adolescence, 35(4), 617–630. 10.1007/s10964-006-9063-4 [DOI] [Google Scholar]
- Pereznieto P, Montes A, Routier S, & Langston L (2014). The costs and economic impact of violence against children. Childfund. [Google Scholar]
- Peterson C, Florence C, & Klevens J (2018). The economic burden of child maltreatment in the United States. 2015 Child Abuse & Neglect, 86(1), 178–183. 10.1016/j.chiabu.2018.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineda J, & Dadds MR (2013). Family intervention for adolescents with suicidal behavior: A randomized controlled trial and mediation analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 52(8), 851–862. 10.1016/j.jaac.2013.05.015 [DOI] [PubMed] [Google Scholar]
- Pisani AR, Wyman PA, Petrova M, Schmeelk-Cone K, Goldston DB, Xia Y, & Gould MS (2013). Emotion regulation difficulties, youth-adult relationships, and suicide attempts among high school students in underserved communities. Journal of Youth and Adolescence, 42(6), 807–820. 10.1007/s10964-012-9884-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plener PL, Zohsel K, Hohm E, Buchmann AF, Banaschewski T, Zimmermann US, & Laucht M (2017). Lower cortisol level in response to a psychosocial stressor in young females with self-harm. Psychoneuroendocrinology, 76, 84–87. 10.1016/j.psyneuen.2016.11.009 [DOI] [PubMed] [Google Scholar]
- Puzia ME, Kraines MA, Liu RT, & Kleiman EM (2014). Early life stressors and suicidal ideation: Mediation by interpersonal risk factors. Personality and Individual Differences, 56(1), 68–72. 10.1016/j.paid.2013.08.027 [DOI] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. 10.1037//0033-2909.128.2.330 [DOI] [PubMed] [Google Scholar]
- Rhodes AE, Boyle MH, Bethell J, Wekerle C, Goodman D, Tonmyr L, Leslie B, Lam K, & Manion I (2012). Child maltreatment and onset of emergency department presentations for suicide-related behaviors. Child Abuse and Neglect, 36(6), 542–551. 10.1016/j.chiabu.2012.04.006 [DOI] [PubMed] [Google Scholar]
- Russell AE, Heron J, Gunnell D, Ford T, Hemani G, Joinson C, Moran P, Relton C, Suderman M, Mars B (2019). Pathways between early-life adversity and adolescent self-harm: The mediating role of inflammation in the Avon Longitudinal Study of Parents and Children. Journal of Child Psychology and Psychiatry and Allied Disciplines, 60(10), 1094–1103. 10.1111/jcpp.13100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M (1985). Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. The British Journal of Psychiatry, 147(6), 598–611. [DOI] [PubMed] [Google Scholar]
- Salzinger S, Rosario M, Feldman RS, & Ng-Mak DS (2007). Adolescent suicidal behavior: Associations with preadolescent physical abuse and selected risk and protective factors. Journal of the American Academy of Child and Adolescent Psychiatry, 46(7), 859–866. 10.1097/chi.0b013e318054e702 [DOI] [PubMed] [Google Scholar]
- Sameroff AJ (2009). The transactional model. In The transactional model of development: How children and contexts shape each other (pp. 3–21). American Psychological Association. [Google Scholar]
- Scott LN, Pilkonis PA, Hipwell AE, Keenan K, & Stepp SD (2015). Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: A multi-wave prospective study. Comprehensive Psychiatry, 58, 1–10. 10.1016/j.comppsych.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seff I, & Stark L (2019). A sex-disaggregated analysis of how emotional violence relates to suicide ideation in low-and middle-income countries. Child Abuse & Neglect, 93, 222–227. [DOI] [PubMed] [Google Scholar]
- Sekowski M, Gambin M, Cudo A, Wozniak-Prus M, Penner F, Fonagy P, & Sharp C (2020). The relations between childhood maltreatment, shame, guilt, depression and suicidal ideation in inpatient adolescents. Journal of Affective Disorders, 276(May), 667–677. 10.1016/j.jad.2020.07.056 [DOI] [PubMed] [Google Scholar]
- Shain BN (2019). Increases in rates of suicide and suicide attempts among black adolescents. Pediatrics, 144(5), 2019–2022. 10.1542/peds.2019-1912 [DOI] [PubMed] [Google Scholar]
- Shen AC-T (2009). Self-esteem of young adults experiencing interparental violence and child physical maltreatment. Journal of Interpersonal Violence, 24(5), 770–794. 10.1177/0886260508317188 [DOI] [PubMed] [Google Scholar]
- Sigfusdottir ID, Asgeirsdottir BB, Gudjonsson GH, & Sigurdsson JF (2013). Suicidal ideations and attempts among adolescents subjected to childhood sexual abuse and family conflict/violence:The mediating role of anger and depressed mood. Journal of Adolescence, 36(6), 1227–1236. 10.1016/j.adolescence.2013.10.001 [DOI] [PubMed] [Google Scholar]
- Smith NB, Monteith LL, Rozek DC, & Meuret AE (2018). Childhood abuse, the interpersonal-psychological theory of suicide, and the mediating role of depression. Suicide and Life-Threatening Behavior, 48(5), 559–569. 10.1111/sltb.12380 [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Carlson EA, Levy AK, & Egeland B (1999). Implications of attachment theory for developmental psychopathology. Development and Psychopathology, 11, 1–13, https://www.cambridge.org/core [DOI] [PubMed] [Google Scholar]
- Steinberg LJ, & Mann JJ (2020). Abnormal stress responsiveness and suicidal behavior: A risk phenotype. Biomarkers in Neuropsychiatry, 2(January), 100011. 10.1016/j.bionps.2020.100011 [DOI] [Google Scholar]
- Stronach EP, Toth SL, Rogosch F, Oshri A, Manly JT, & Cicchetti D (2011). Child maltreatment, attachment security, and internal representations of mother and mother-child relationships. Child Maltreatment, 16(2), 137–145. 10.1177/1077559511398294 [DOI] [PubMed] [Google Scholar]
- Tang W, Zhao J, Lu Y, Zha Y, Liu H, Sun Y, ... & Xu J (2018). Suicidality, posttraumatic stress, and depressive reactions after earthquake and maltreatment: A cross-sectional survey of a random sample of 6132 Chinese children and adolescents. Journal of Affective Disorders, 232, 363–369. [DOI] [PubMed] [Google Scholar]
- Tarullo AR, & Gunnar MR (2006). Child maltreatment and the developing HPA axis. Hormones and Behavior, 50(4), 632–639. 10.1016/j.yhbeh.2006.06.010 [DOI] [PubMed] [Google Scholar]
- Thompson EA, Eggert LL, Randell BP, & Pike KC (2001). Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. American Journal of Public Health, 91(5), 742–752. 10.2105/AJPH.91.5.742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, English DJ, & White CR (2016). Maltreatment history as persistent risk: An extension of Li and Godinet (2014). Children and Youth Services Review, 64, 117–121. 10.1016/j.childyouth.2016.03.003 [DOI] [Google Scholar]
- Thompson R, Proctor LJ, English DJ, Dubowitz H, Narasimhan S, & Everson MD (2012). Suicidal ideation in adolescence: Examining the role of recent adverse experiences. Journal of Adolescence, 35(1), 175–186. 10.1016/j.adolescence.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth SL, Cicchetti D, MacFie J, Maughan A, & Vanmeenen K (2000). Narrative representations of caregivers and self in maltreated pre-schoolers. Attachment & Human Development, 2(3), 271–305. 10.1080/14616730010000849 [DOI] [PubMed] [Google Scholar]
- Toth SL, Handley ED, Manly JT, Sturm R, Adams TR, Demeusy EM, & Cicchetti D (2020). The moderating role of child maltreatment in treatment efficacy for adolescent depression. Journal of Abnormal Child Psychology, 48(10), 1351–1365. 10.1007/s10802-020-00682-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, & Cicchetti D (2006). The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: A randomized preventive trial. Journal of Consulting and Clinical Psychology, 74(6), 1006–1016. 10.1037/0022-006X.74.6.1006 [DOI] [PubMed] [Google Scholar]
- Tottenham N, Hare TA, Millner A, Gilhooly T, Zevin JD, & Casey BJ (2011). Elevated amygdala response to faces following early deprivation. Developmental Science, 14(2), 190–204. 10.1111/j.1467-7687.2010.00971.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trent M, Dooley DG, Dougé J, Trent ME, Cavanaugh RM, Lacroix AE, Fanburg J, Rahmandar MH, Hornberger LL, Schneider MB, Yen S, Chilton LA, Green AE, Dilley KJ, Gutierrez JR, Duffee JH, Keane VA, Krugman SD, McKelvey CD, Wallace SB,& et al. (2019). The impact of racism on child and adolescent health. Pediatrics, 144(2). 10.1542/peds.2019-1765 [DOI] [PubMed] [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, & Putnam FW (2010). Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology, 22(1), 165–175. 10.1017/S0954579409990332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twardosz S, & Lutzker JR (2010). Child maltreatment and the developing brain: A review of neuroscience perspectives. Aggression and Violent Behavior, 15(1), 59–68. 10.1016/j.avb.2009.08.003 [DOI] [Google Scholar]
- U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, & Children’s Bureau (2021). Child maltreatment 2019.
- U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality (2020). National Survey on Drug Use and Health 2019 (NSDUH–2019). Retrieved from https://datafiles.samhsa.gov/
- Van Heeringen K,& Mann JJ (2014). The neurobiology of suicide. The Lancet Psychiatry, 1(1), 63–72. 10.1016/S2215-0366(14)70220-2 [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby E.a, & Joiner TE (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verrocchio MC, Carrozzino D, Marchetti D, Andreasson K, Fulcheri M, & Bech P (2016). Mental pain and suicide: A systematic review of the literature. Frontiers in Psychiatry, 7, 108. 10.3389/fpsyt.2016.00108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan GWY, & Leung PWL (2010). Factors accounting for youth suicide attempt in Hong Kong: A model building. Journal of Adolescence, 33(5), 575–582. 10.1016/j.adolescence.2009.12.007 [DOI] [PubMed] [Google Scholar]
- Warmingham JM, Handley ED, Rogosch FA, Manly JT, & Cicchetti D (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse and Neglect, 87(May 2017), 28–39. 10.1016/j.chiabu.2018.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J, & Kral MJ (2014). Re-thinking youth suicide: Language, culture, and power. Journal for Social Action in Counseling & Psychology, 6(1), 122–142. 10.33043/jsacp.6.1.122-142 [DOI] [Google Scholar]
- Wilcox HC, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, & Anthony JC (2008). The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence, 95(Suppl 1), 60–73. 10.1016/j.drugalcdep.2008.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson ST, Chesin M, Fertuck E, Keilp J, Brodsky B, Mann JJ, Ceren C, Benjamin-phillips C, & Stanley B (2016). Heart rate variability and suicidal behavior. Psychiatry Research, 240, 241–247. 10.1016/j.psychres.2016.04.033 [DOI] [PubMed] [Google Scholar]
- Wismer Fries AB, Shirtcliff EA, & Pollak SD (2008). Neuroendocrine dysregulation following early social deprivation in children. Developmental Psychobiology, 50(6), 588–599. 10.1002/dev.20319.Neuroendocrine [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). Global status report on preventing violence against children 2020. World Health Organization. [Google Scholar]
- Wu P, Hoven CW, Liu X, Cohen P, Fuller CJ, & Shaffer D (2004). Substance use, suicidal ideation and attempts in children and adolescents. Suicide and Life-Threatening Behavior, 34(4), 408–420. 10.1521/suli.34.4.408.53733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA (2014). Developmental approach to prevent adolescent suicides: Research pathways to effective upstream preventive interventions. American Journal of Preventive Medicine, 47(3), S251–S256. 10.1016/j.amepre.2014.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA, Brown CH, LoMurray M, Schmeelk-Cone K, Petrova M, Yu Q, Walsh E, Tu X, & Wang W (2010). An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. American Journal of Public Health, 100(9), 1653–1661. 10.2105/AJPH.2009.190025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ybarra ML, Mitchell KJ, Kosciw JG, & Korchmaros JD (2015). Understanding linkages between bullying and suicidal ideation in a national sample of LGB and heterosexual youth in the United States. Prevention Science, 16(3), 451–462. 10.1007/s11121-014-0510-2 [DOI] [PubMed] [Google Scholar]
- Zelazny J, Melhem N, Porta G, Biernesser C, Keilp JG, Mann JJ, ... & Brent DA (2019). Childhood maltreatment, neuropsychological function and suicidal behavior. Journal of Child Psychology and Psychiatry, 60(10), 1085–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Liu M, & Long H (2020). Child maltreatment and suicide ideation in rural China: The roles of self-compassion and school belonging. Child and Adolescent Social Work Journal, 38. 10.1007/s10560-020-00679-z [DOI] [Google Scholar]
- Zimmerman MA, Stoddard SA, Eisman AB, Caldwell CH, Aiyer SM, & Miller A (2013). Adolescent resilience: Promotive factors that inform prevention. Child Development Perspectives, 7(4), 215–220. 10.1111/cdep.12042 [DOI] [PMC free article] [PubMed] [Google Scholar]


