Summary
Background
Understanding health trends and estimating the burden of disease at the national and subnational levels helps policy makers track progress and identify disparities in overall health performance. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 provides comprehensive estimates for Pakistan. Comparison of health indicators since 1990 provides valuable insights about Pakistan's ability to strengthen its health-care system, reduce inequalities, improve female and child health outcomes, achieve universal health coverage, and meet the UN Sustainable Development Goals. We present estimates of the burden of disease, injuries, and risk factors for Pakistan provinces and territories from 1990 to 2019 based on GBD 2019 to improve health and health outcomes in the country.
Methods
We used methods and data inputs from GBD 2019 to estimate socio-demographic index, total fertility rate, cause-specific deaths, years of life lost, years lived with disability, disability-adjusted life-years, healthy life expectancy, and risk factors for 286 causes of death and 369 causes of non-fatal health loss in Pakistan and its four provinces and three territories from 1990 to 2019. To generate estimates for Pakistan at the national and subnational levels, we used 68 location-years of data to estimate Pakistan-specific demographic indicators, 316 location-years of data for Pakistan-specific causes of death, 579 location-years of data for Pakistan-specific non-fatal outcomes, 296 location-years of data for Pakistan-specific risk factors, and 3089 location-years of data for Pakistan-specific covariates.
Findings
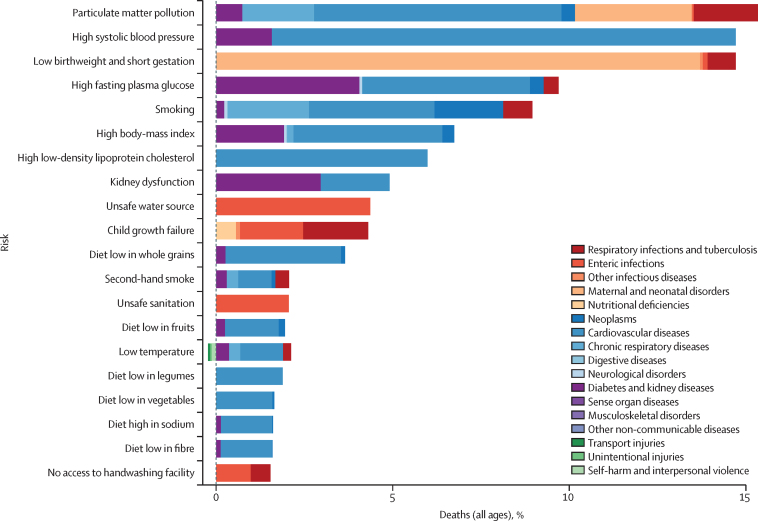
Life expectancy for both sexes in Pakistan increased nationally from 61·1 (95% uncertainty interval [UI] 60·0–62·1) years in 1990 to 65·9 (63·8–67·8) years in 2019; however, these gains were not uniform across the provinces and federal territories. Pakistan saw a narrowing of the difference in healthy life expectancy between the sexes from 1990 to 2019, as health gains for women occurred at faster rates than for men. For women, life expectancy increased by 8·2% (95% UI 6·3–13·8) between 1990 and 2019, whereas the male life expectancy increased by 7·6% (3·5–11·8). Neonatal disorders, followed by ischaemic heart disease, stroke, diarrhoeal diseases, and lower respiratory infections were the leading causes of all-age premature mortality in 2019. Child and maternal malnutrition, air pollution, high systolic blood pressure, dietary risks, and tobacco consumption were the leading all-age risk factors for death and disability-adjusted life-years at the national level in 2019. Five non-communicable diseases—ischaemic heart disease, stroke, congenital defects, cirrhosis, and chronic kidney disease—were among the ten leading causes of years of life lost in Pakistan. Burden varied by socio-demographic index. Notably, Balochistan and Khyber Pakhtunkhwa had the lowest observed gains in life expectancy. Dietary iron deficiency was the leading cause of years lived with disability for both men and women in 1990 and 2019. Low birthweight and short gestation and particulate matter pollution were the leading contributors to overall disease burden in both 1990 and 2019 despite moderate improvements, with a 23·5% (95% UI 3·8–39·2) and 27·6% (14·3–38·6) reduction in age-standardised attributable DALY rates during the study period.
Interpretation
Our study shows that progress has been made on reducing Pakistan's disease burden since 1990, but geographical, age, and sex disparities persist. Equitable investment in the health system, as well as the prioritisation of high-impact policy interventions and programmes, are needed to save lives and improve health outcomes. Pakistan is facing several domestic and foreign challenges—the Taliban's return to power in Afghanistan, political turmoil, catastrophic flooding, the COVID-19 pandemic—that will shape the trajectory of the country's health and development. Pakistan must address the burden of infectious disease and curb rising rates of non-communicable diseases. Prioritising these three areas will enhance Pakistan's ability to achieve universal health coverage, meet its Sustainable Development Goals, and improve the overall health outcomes.
Funding
Bill & Melinda Gates Foundation.
Translation
For the Urdu translation of the abstract see Supplementary Materials section.
Research in context.
Evidence before this study
The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 provided national-level policy-relevant findings on life expectancy, incidence, prevalence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years due to 369 diseases and injuries and 87 risk factors for 204 countries and territories. GBD estimates are produced for 17 countries, including Pakistan, at both the national and subnational levels. The analysis contains estimates of deaths, years of life lost, years lived with disability, and disability-adjusted life-years attributable to metabolic, environmental, occupational, and behavioural risk factors. To identify previously published estimates of the burden of disease in Pakistan, we completed a systematic literature review of scientific research about health in Pakistan by searching the terms “Pakistan” OR “Burden of Disease” OR “Public Health” OR “Epidemiology” OR “universal health care” OR “sustainable development goals” from inception to Sept 15, 2022, using PubMed and Google Scholar. We limited our search to English-only publications. A 2013 series Health Transitions in Pakistan in The Lancet, for instance, presented commentaries and research that analysed the country's health-care challenges, governance, and performance. The controversy surrounding Pakistan's polio vaccination efforts has also received attention from health and policy researchers. Another area of research has focused on multi-drug-resistant typhoid, tuberculosis, and anti-microbial resistance more generally. Researchers have also examined the effects of a loosely regulated retail pharmacy sector in Pakistan, where the availability of medicines without prescriptions, self-diagnoses, and self-medication are common. Although national GBD estimates for Pakistan have been in the public domain since the release of GBD 2010, the subnational estimates have not been previously released or analysed in a scientific publication. We present GBD 2019 for Pakistan and its provinces and territories to improve health policy and inform resource allocation to help the country meet its health and development goals.
Added value of this study
The GBD estimation cycle makes methodological improvements each year and continually adds to the evidence base that informs estimates, and national and subnational analyses of health and health loss for some countries provide additional insights and findings. Previous GBD publications have not focused on Pakistan and its subnational administrative units. To our knowledge, this is the first study to report on the overall burden of disease in Pakistan and provides pre-COVID-19 pandemic baseline estimates for diseases, injuries, and risk factors. As the COVID-19 pandemic continues, benchmarking with GBD estimates provides pre-pandemic historical context of health for the country at both the national and subnational levels. These results include 1571 national and subnational source counts specific to Pakistan and its seven subnational administrative units. Our analysis illuminates on health challenges at both national and subnational levels, while also revealing diseases, injuries, and risk factors that will require policy makers to focus their efforts on economic investments, community outreach, and policy reforms to improve population health in Pakistan. By including an analysis of Pakistan's four provinces and three territories, this study underscores subnational variations of life expectancy gains and other important metrics and highlights opportunities to reduce burden due to morbidity and premature mortality.
Implications of all the available evidence
Pakistan is facing several challenges as it undergoes an epidemiological transition. Although progress has been made, Pakistan's health status is falling behind that of its neighbours and similarly ranked socio-demographic index comparator countries. This study calls for major investments in health spending and supporting infrastructure to address the burden of disease to improve the country's overall health status, while reducing geographical, age, and sex disparities. GBD estimates can directly inform long-term planning for health in Pakistan. As the population of Pakistan grows and ages, health investments and policies guided by the best available evidence are needed both to solve immediate problems such as the COVID-19 pandemic and to ensure long-term prosperity and economic growth. There is a need to address the social determinants of health in Pakistan in the form of increased education opportunities and other socioeconomic development programmes. Reducing the double burden of communicable and non-communicable diseases in the context of the COVID-19 pandemic and demographically transitioning populations is also crucial, especially in rural and remote areas that are historically underserved and lack resources. Estimates of health and health loss in Pakistan and its provinces and territories will be improved with the collection and uptake of high-quality data, especially with systematic efforts by provincial and territorial governments to improve routine health information systems through programmes such as the District Health Information System Punjab.
Introduction
With a population approaching 225 million, Pakistan is the fifth most populous country in the world.1 An ethnically and linguistically diverse country, Pakistan is a Muslim majority nation and home to the second largest Muslim population in the world after Indonesia.2 Pakistan was established in 1947 as part of the partition of British India. In 1971, east Pakistan broke away from Pakistan to become the independent country of Bangladesh. The capital of Pakistan is Islamabad, a federally administered territory. Metropolises such as Karachi and Lahore are the economic and cultural centres of Pakistan, with populations of approximately 16 million and 11 million, respectively, but the country remains overwhelmingly rural with roughly 63·6% of its population living outside urban areas.3 Punjab is the largest province by population. Pakistan is prone to the calamitous effects of climate change and natural disasters, including the 2005 Kashmir earthquake and catastrophic floods in 2010 and 2022, all of which have impacted major health policies and reforms.4 Historically, Pakistan's agrarian sector has been a large contributor to the country's gross domestic product (GDP), but the economy has diversified with robust service, engineering, and information technology sectors.3 English and Urdu are the official state languages of Pakistan, and there are sizable populations of speakers of regional languages, such as Punjabi, Pashto, Sindhi, and Balochi, among others.3
Pakistan has a federal governance structure with four provinces (Balochistan, Punjab, Sindh, and Khyber Pakhtunkhwa) and three federal territories (Islamabad Capital Territory, Gilgit-Baltistan, and Azad Jammu and Kashmir). Subnational administrative units serve important roles in the country's health policy and planning. In 2010, the government amended Pakistan's constitution to curtail federal power and invested provincial governments with greater authority.5 The 18th Constitutional Amendment transformed Pakistan's governing structures and has had a profound effect on the country's health policy and system.5 The amendment abolished the Federal Ministry of Health and shifted health policy and management to the provinces. In 2013, a federal health ministry was revived as the Ministry of National Health Services, Regulations, and Coordination. This ministry coordinates health policy, standards, and targets, and provides an overarching framework, whereas the provincial and territorial agencies set their own health policies and priorities and maintain responsibility for implementation. These reforms remade the powers of federal and provincial agencies and brought new administrative challenges.5
In recent years, the Pakistani Government launched several national programmes to reduce poverty and financial hardship as it relates to health-care costs. Total health expenditure per GDP was 3·0% (95% uncertainty interval [UI] 2·8–3·3) in 2019,6 whereas health-care spending per person in 2019 was US$43 (95% UI 40–46).6 In 2016, out-of-pocket spending was 62·7% (95% UI 49·5–74·3).7 Despite investments in medical education, research, and training capacities, the “actual state of affairs is neither exciting nor remarkable” and health-care resources remain concentrated in the private sector.8 The Benazir Income Support Program, a scheme initiated in July, 2008, provides monthly direct cash transfers to female heads of poor households.9, 10 This programme was replaced by the poverty alleviation programme Ehsaas in March, 2019.11 The National Health Programme, known as Sehat Sahulat, was created to provide cashless health care to families living below the poverty line for medical services.12 Despite administrative and financial challenges, these programmes are increasing health insurance coverage and strengthening the social safety net. Pakistan is also pursuing universal health coverage (UHC),13 although in 2019 it ranked globally in the bottom tenth of countries in terms of effective UHC coverage.14 Nevertheless, National Health Vision 2016–25 recognises UHC as the top national priority.15 Even with these public investments in Pakistan's health system, the private sector remains the largest provider of health-care services to most of the population.8
Our analysis sets pre-COVID-19 pandemic baselines for health and health loss in Pakistan. The health challenges that Pakistan currently faces are compounded by the ongoing COVID-19 pandemic and extreme flooding. Pakistan has not yet eradicated wild polio,16, 17, 18 underscoring the health and immunisation disparities in remote and underserved areas. This manuscript, which was produced as part of the Global Burden of Disease, Injuries and Risk Factors Study (GBD) 2019 and the GBD Collaborator Network in accordance with the GBD protocol,19 presents estimates of the burden of disease and calls for improving the collection of high-quality data to help address sources of health loss in Pakistan. The GBD 2019 estimates for Pakistan at the national and subnational levels are informed by data from federal offices, provincial health authorities, and Pakistan-based public health research enterprises, as well as international agencies such as WHO. This analysis also uses troves of nationally and provincially representative household surveys. If data collection enterprises continue to yield results, and partnerships and collaborations with academic research and public agencies in Pakistan deepen, the groundwork will be laid for future studies of disease burden in Pakistan at the district and municipal levels. Fine-grained analyses of health and health loss will equip professionals and policy makers with useful information about urgent health problems, while also informing long-term planning and preparations for future health scenarios.
This analysis presents the burden of disease, injuries, and risk factors for Pakistan and its provinces and territories from 1990 to 2019 to equip policy makers, practitioners, government agencies, and non-governmental organisations with high-quality estimates of health and health loss at a population level.
Methods
Overview
We estimated cause-specific deaths, years of life lost (YLLs), years lived with disability (YLDs), disability-adjusted life-years (DALYs), life expectancy (LE), healthy life expectancy (HALE), and 87 risk factors for 286 causes of death and 369 causes of non-fatal health loss for Pakistan and its four provinces and three federal territories from 1990 to 2019. Each point estimate includes 95% UIs. In addition to the GBD 2019 data sources, we used 550 Pakistan-specific sources, including several Demographic and Health Surveys, Pakistan Social and Living Standards Measurement Surveys, epidemiological surveillance, reports, and articles. The Pakistan Demographic and Health Survey and provincial Multiple Indicator Cluster Survey offer large shares of data used in this study. We incorporated 550 local data inputs and 213 430 total source metadata rows (appendix 2 pp 3–36). A summary of the data sources used in the GBD 2019 Pakistan analysis is provided in appendix 2 (pp 3–36). For GBD 2019, 87 risk factors for 286 causes of death and 369 causes of non-fatal health loss were classified into cause and risk hierarchies. GBD 2019 cause and risk hierarchies are each structured into four levels. A list of these data sources is available on the Global Health Data Exchange. We followed the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER).20 A complete GATHER table is available in appendix 2 (pp 44–45).
No separate ethical approval was required for this specific analysis. The entire GBD protocol is publicly available.
Analyses were done with Python version 3.6.2, Stata version 13, and R versions 3.5.0–4.0.3. The statistical code used to generate GBD estimates is available in the GitHub public domain. Additional results from this study and the larger GBD 2019 analysis can be explored using our data visualisation tools and downloaded using a query tool.
Pakistan geographical units
We applied the standard GBD subnational estimation process to estimate all metrics by province and federal territory of Pakistan from 1990 to 2019. Subnational estimates for Pakistan are not produced before 1990. To make accurate comparisons, data are adjusted to fit provincial and national boundaries for 2019 for the entire period of study. We modified the estimation process to account for major changes to the national political map that occurred between 1990 and 2019. Estimates for Khyber Pakhtunkhwa, formerly the North-West Frontier Province, are inclusive of observed results in the federally administered tribal areas.
Mortality and causes of death
We estimated all-cause mortality for each age-sex-location-year across Pakistan and its subnational administrative units using the GBD model life table system. The GBD model life table system identifies a reference life table for each specific location and was used to produce a complete set of abridged life tables (age-specific mortality rates), based on the nearest matches found in our empirical life table database.21 Cause-specific mortality rates were estimated for 282 causes of death using the GBD cause of death database and a Bayesian meta-regression and Cause of Death Ensemble modelling for each combination of location, year, age, and sex. Adjustments were made for incomplete or missing data, general heterogeneity in data completeness and quality, and the redistribution of “garbage codes”,22 which are deaths that have been incorrectly assigned in vital registration systems.
YLLs
YLLs are a measure of premature death. We used these estimates to produce YLL rates and age-standardised mortality rates by multiplying each cause-specific death by the standard LE at each age.23 Details of these calculations are available elsewhere.23
YLDs
YLDs are computed as the product of prevalence and disability weight, preserving the severity distributions for each prevalence estimate and applying the corresponding disability weight or combined disability weight using DisMod-MR (version 2.1), a Bayesian meta-regression tool.23 Details of GBD 2019 calculations have been previously described elsewhere.23
DALYs and HALE
DALYs were calculated by summing YLLs and YLDs for each location, year, age group, and cause, by sex. To compute HALE at birth and specific age groups, we used the method originally developed by Sullivan to estimate HALE.24 Detailed methods of DALYs and HALE are available elsewhere.1
Risk factors
We estimated relative risk of mortality and morbidity, exposure to, and attributable deaths or DALYs for each risk-outcome pair for 87 behavioural, environmental, occupational, and metabolic risk factors or clusters of risks in GBD 2019.25 We completed this analysis for Pakistan and its seven subnational units from 1990 to 2019 using 550 data sources (appendix 2 pp 3–36). To calculate attributable burden for each risk-outcome pair, total deaths or DALYs were multiplied by the population attributable fraction. For each risk, the summary exposure value was calculated as a risk-weighted prevalence of exposure. Summary exposure value ranged between 0% and 100%, where 0% reflects no excess risk in the given population and 100% indicates the entire population is exposed to the highest possible level for the given risk.25
Decomposition of change
To decompose change in numbers of deaths by cause from 1990 to 2019, we used methods originally adapted in GBD 2019 and in demographic research from Das Gupta.26 These methods are described elsewhere.1, 23
Uncertainty analysis
Uncertainty in our estimates was propagated at multiple stages in the GBD modelling process using 1000 draws.1, 23, 25 Distributions were determined from sampling error of data inputs; cause-specific model specifications; varied data availability by age, sex, location, or year; uncertainty of the model coefficients; variability of sample size within data sources; and uncertainty of the severity of disability weights used in non-fatal modelling.1, 23, 25 Final estimates were derived using the mean estimate across all 1000 draws, whereas 95% UIs were determined based on the 25th and 975th ranked values across all draws. Changes over time were considered significant when the posterior probability of the change was at least 95%.
The socio-demographic index (SDI)
The SDI is a value between 0 and 1·0 calculated from the geometric mean of three rescaled components: total fertility rate under 25, lag-distributed income per capita, and educational attainment in the population aged older than 15 years.1
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
LE, HALE, and SDI
Between 1990 and 2019, national LE in Pakistan increased from 61·1 (95% UI 60·0–62·1) years to 65·9 (63·8–67·8) years for both sexes combined, an increase of 7·86%; HALE similarly increased from 53·2 (50·8–55·3) years to 57·2 (54·3–60·1) years, an increase of 7·56%. Pakistan saw a narrowing of the difference in HALE between the sexes from 1990 to 2019 as health gains for women occurred at faster rates than men. HALE increased from 53·6 (51·4–55·6) years in 1990 to 57·4 (54·3–60·5) years in 2019 for men and from 52·8 (50·0–55·3) years to 57·1 (53·7–60·4) years for women. For women, life expectancy increased by 8·22% between 1990 and 2019; during that same period, life expectancy for men increased by only 7·44%. The table displays LE and HALE for Pakistan and its seven subnational units disaggregated by sex. The largest increases in life expectancy were seen in the two northern territories, Gilgit-Baltistan and Azad Jammu and Kashmir, increasing from 58·2 (55·5–60·8) years in 1990 to 64·6 (61·5–67·9) years in 2019, and 62·6 (60·0–65·2) years in 1990 to 68·6 (65·8–71·4) years in 2019, respectively. However, the lowest gains in life expectancy were observed in two of Pakistan's western provinces: Balochistan and Khyber Pakhtunkhwa. Our study finds that the disease burden is due to violence caused by war and conflict in these provinces, and although this is greater than in other areas of the country, it does not represent a share of health and health loss at the magnitude of communicable and non-communicable diseases (NCDs).
Table.
Life expectancy, healthy life expectancy, and socio-demographic index for Pakistan and subnational locations for both sexes combined, men, and women, 1990 to 2019
|
Life expectancy at birth |
Life expectancy % change |
Healthy life expectancy |
Healthy life expectancy % change |
Socio-demographic index |
Socio-demographic index % change |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2010 | 2019 | 1990 to 2010 | 2010 to 2019 | 1990 to 2019 | 1990 | 2010 | 2019 | 1990 to 2010 | 2010 to 2019 | 1990 to 2019 | 1990 | 2010 | 2019 | 1990 to 2010 | 2010 to 2019 | 1990 to 2019 | |
| Both sexes combined | ||||||||||||||||||
| Pakistan | 61·1 (60·0–62·1) | 63·3 (61·7–65·0) | 65·9 (63·8–67·8) | 3·63% | 4·09% | 7·87% | 53·2 (50·8–55·3) | 55·1 (52·7–57·6) | 57·2 (54·3–60·1) | 3·69% | 3·74% | 7·56% | 0·26 | 0·42 | 0·48 | 60·50% | 14·10% | 83·13% |
| Azad Jammu and Kashmir | 62·6 (60·0–65·2) | 66·5 (63·6–69·2) | 68·6 (65·8–71·4) | 6·16% | 3·18% | 9·53% | 54·6 (51·6–57·5) | 57·4 (54·2–60·4) | 59·3 (56·0–62·3) | 5·27% | 3·23% | 8·67% | 0·27 | 0·46 | 0·52 | 73·81% | 13·21% | 96·77% |
| Balochistan | 61·4 (58·9–63·9) | 61·3 (58·2–64·4) | 63·4 (60·2–66·6) | −0·14% | 3·36% | 3·22% | 53·5 (50·6–56·4) | 53·5 (50·4–56·6) | 55·2 (52·0–58·4) | 0·04% | 3·04% | 3·08% | 0·22 | 0·39 | 0·44 | 78·82% | 13·30% | 102·60% |
| Gilgit-Baltistan | 58·2 (55·5–60·8) | 62·1 (59·1–65·2) | 64·6 (61·5–67·9) | 6·61% | 4·09% | 10·97% | 50·7 (47·7–53·8) | 54·1 (51·0–57·4) | 56·2 (52·8–59·8) | 6·81% | 3·82% | 10·89% | 0·18 | 0·36 | 0·41 | 102·54% | 14·93% | 132·77% |
| Islamabad Capital Territory | 67·7 (65·2–70·2) | 70·9 (68·7–73·4) | 72·7 (70·2–75·0) | 4·68% | 2·53% | 7·33% | 59·0 (55·9–62·0) | 61·8 (58·7–64·7) | 63·1 (59·9–66·2) | 4·66% | 2·17% | 6·93% | 0·46 | 0·67 | 0·73 | 43·90% | 8·79% | 56·54% |
| Khyber Pakhtunkhwa | 65·3 (63·0–67·6) | 64·7 (62·1–67·5) | 67·1 (64·2–69·9) | −0·83% | 3·67% | 2·81% | 56·7 (53·8–59·6) | 56·4 (53·3–59·5) | 58·3 (55·2–61·6) | −0·65% | 3·34% | 2·67% | 0·16 | 0·29 | 0·34 | 84·01% | 16·72% | 114·78% |
| Punjab | 59·5 (58·0–60·9) | 62·5 (60·6–64·7) | 65·1 (62·7–67·4) | 5·11% | 4·07% | 9·38% | 52·1 (49·6–54·4) | 54·7 (52·2–57·3) | 56·7 (53·6–59·8) | 5·11% | 3·72% | 9·02% | 0·27 | 0·41 | 0·48 | 53·22% | 15·26% | 76·60% |
| Sindh | 61·9 (59·7–64·2) | 63·9 (61·2–66·6) | 66·6 (63·8–69·3) | 3·24% | 4·27% | 7·65% | 53·4 (50·2–56·2) | 55·2 (52·2–58·4) | 57·4 (54·2–60·6) | 3·48% | 3·92% | 7·54% | 0·26 | 0·46 | 0·52 | 73·51% | 12·58% | 95·34% |
| Women | ||||||||||||||||||
| Pakistan | 61·8 (60·5–63·1) | 64·4 (62·4–66·5) | 66·8 (63·9–69·5) | 4·25% | 3·80% | 8·22% | 52·8 (50·0–55·3) | 55·1 (52·3–58·2) | 57·1 (53·7–60·4) | 4·39% | 3·58% | 8·13% | 0·26 | 0·42 | 0·48 | 60·50% | 14·10% | 83·13% |
| Azad Jammu and Kashmir | 63·5 (60·1–66·9) | 67·5 (63·4–71·1) | 69·4 (65·1–73·3) | 6·24% | 2·95% | 9·37% | 54·5 (51·1–58·0) | 57·7 (53·5–61·6) | 59·4 (55·2–63·3) | 5·86% | 2·97% | 8·99% | 0·27 | 0·46 | 0·52 | 73·81% | 13·21% | 96·77% |
| Balochistan | 62·5 (59·3–66·1) | 62·5 (58·4–66·7) | 64·3 (60·0–68·5) | −0·06% | 2·95% | 2·88% | 53·5 (50·0–57·0) | 53·6 (49·6–57·5) | 55·1 (50·8–59·2) | 0·24% | 2·78% | 3·03% | 0·22 | 0·39 | 0·44 | 78·82% | 13·30% | 102·60% |
| Gilgit-Baltistan | 59·3 (56·0–62·5) | 63·0 (58·7–67·5) | 65·4 (61·0–69·7) | 6·27% | 3·77% | 10·28% | 50·7 (47·1–54·2) | 54·1 (49·9–58·1) | 56·0 (51·9–60·2) | 6·67% | 3·60% | 10·51% | 0·18 | 0·36 | 0·41 | 102·54% | 14·93% | 132·77% |
| Islamabad Capital Territory | 68·4 (65·3–71·4) | 72·2 (68·7–75·8) | 74·2 (70·5–77·6) | 5·60% | 2·77% | 8·53% | 58·6 (54·9–62·0) | 61·9 (58·1–65·8) | 63·4 (59·7–67·5) | 5·78% | 2·40% | 8·32% | 0·46 | 0·67 | 0·73 | 43·90% | 8·79% | 56·54% |
| Khyber Pakhtunkhwa | 66·0 (63·0–69·2) | 65·9 (62·3–69·5) | 67·9 (63·9–71·6) | −0·26% | 3·05% | 2·78% | 56·6 (53·4–60·1) | 56·6 (52·8–60·3) | 58·2 (54·6–62·0) | 0·02% | 2·84% | 2·86% | 0·16 | 0·29 | 0·34 | 84·01% | 16·72% | 114·78% |
| Punjab | 60·6 (58·7–62·4) | 63·9 (61·3–66·5) | 66·3 (63·0–69·7) | 5·49% | 3·78% | 9·48% | 52·0 (49·3–54·7) | 54·8 (51·7–58·1) | 56·8 (53·2–60·4) | 5·52% | 3·56% | 9·27% | 0·27 | 0·41 | 0·48 | 53·22% | 15·26% | 76·60% |
| Sindh | 62·9 (59·9–66·0) | 65·1 (61·6–68·7) | 67·7 (63·8–71·3) | 3·53% | 3·97% | 7·65% | 53·0 (49·4–56·5) | 55·1 (51·5–58·8) | 57·2 (53·2–61·3) | 3·95% | 3·76% | 7·85% | 0·26 | 0·46 | 0·52 | 73·51% | 12·58% | 95·34% |
| Men | ||||||||||||||||||
| Pakistan | 60·5 (59·3–61·7) | 62·3 (60·1–64·8) | 65·0 (61·9–68·0) | 3·02% | 4·29% | 7·44% | 53·6 (51·4–55·6) | 55·2 (52·7–58·0) | 57·4 (54·3–60·5) | 3·13% | 3·90% | 7·15% | 0·26 | 0·42 | 0·48 | 60·50% | 14·10% | 83·13% |
| Azad Jammu and Kashmir | 61·9 (58·5–65·8) | 65·6 (61·4–69·6) | 67·8 (63·5–72·3) | 5·94% | 3·33% | 9·47% | 54·7 (51·5–58·2) | 57·4 (53·5–60·9) | 59·3 (55·2–63·3) | 4·77% | 3·46% | 8·40% | 0·27 | 0·46 | 0·52 | 73·81% | 13·21% | 96·77% |
| Balochistan | 60·5 (57·2–64·3) | 60·4 (56·6–64·8) | 62·6 (58·0–67·4) | −0·15% | 3·59% | 3·44% | 53·6 (50·3–57·1) | 53·7 (49·9–57·5) | 55·4 (51·3–59·6) | 0·10% | 3·25% | 3·35% | 0·22 | 0·39 | 0·44 | 78·82% | 13·30% | 102·60% |
| Gilgit-Baltistan | 57·2 (53·9–60·9) | 61·2 (57·0–65·7) | 63·9 (59·4–68·8) | 6·95% | 4·36% | 11·61% | 50·8 (47·5–54·3) | 54·3 (50·4–58·1) | 56·5 (52·3–60·9) | 7·02% | 4·01% | 11·31% | 0·18 | 0·36 | 0·41 | 102·54% | 14·93% | 132·77% |
| Islamabad Capital Territory | 67·2 (63·7–71·0) | 69·8 (66·3–73·6) | 71·4 (67·4–75·5) | 3·96% | 2·31% | 6·36% | 59·4 (55·9–63·0) | 61·8 (58·4–65·2) | 63·0 (59·0–66·9) | 3·95% | 2·04% | 6·07% | 0·46 | 0·67 | 0·73 | 43·90% | 8·79% | 56·54% |
| Khyber Pakhtunkhwa | 64·6 (61·3–67·8) | 63·6 (59·7–67·5) | 66·4 (62·0–71·1) | −1·47% | 4·28% | 2·75% | 56·9 (53·7–60·2) | 56·2 (52·6–59·7) | 58·4 (54·5–62·4) | −1·26% | 3·93% | 2·62% | 0·16 | 0·29 | 0·34 | 84·01% | 16·72% | 114·78% |
| Punjab | 58·6 (56·6–60·6) | 61·3 (58·6–64·3) | 64·0 (60·5–67·2) | 4·70% | 4·25% | 9·15% | 52·2 (49·8–54·4) | 54·7 (52·0–57·5) | 56·8 (53·2–60·0) | 4·82% | 3·86% | 8·87% | 0·27 | 0·41 | 0·48 | 53·22% | 15·26% | 76·60% |
| Sindh | 61·0 (58·2–64·4) | 62·9 (59·4–66·7) | 65·7 (61·7–69·9) | 2·98% | 4·48% | 7·60% | 53·7 (50·5–56·8) | 55·4 (51·9–58·9) | 57·7 (54·0–61·5) | 3·21% | 4·08% | 7·43% | 0·26 | 0·46 | 0·52 | 73·51% | 12·58% | 95·34% |
Data are years (95% uncertainty interval), unless otherwise specified.
The overall SDI of Pakistan increased from 0·26 in 1990 to 0·48 in 2019. The 2019 SDI of Pakistan's four provinces and three territories ranged from 0·34 in Khyber Pakhtunkhwa to 0·73 in Islamabad. Inequality between the highest and lowest SDI units increased by 54% since 1990. The lowest SDI among Pakistan's subnational geographical units (0·34) was higher than that of Afghanistan (0·33) and lower than that of Nepal (0·43). The highest SDI for a province or territory in Pakistan (0·73) was higher than those of both Iran (0·70) and China (0·69). The SDI of Pakistan's GBD region—South Asia—is 0·54, which is higher than Pakistan's national SDI of 0·48. Appendix 2 (p 38) shows the LE, HALE, and SDI of Pakistan compared with regional comparator countries, as well as countries with similar demographic, economic, and health profiles, between 1990 and 2019.
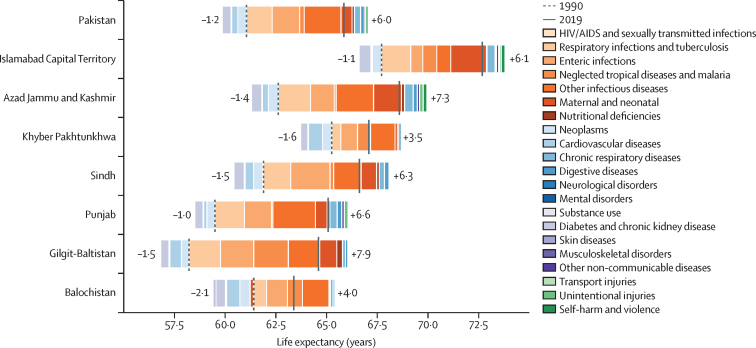
Decomposition of LE
Between 1990 and 2019, all provinces and federal territories saw increases in LE due to the reduction in communicable, maternal, neonatal, and nutritional diseases. Figure 1 shows the decomposition of change in life expectancy for both sexes combined (for male and female sex disaggregation, see appendix 2 p 38). Balochistan saw both the smallest reduction across these conditions and the largest increase in burden due to NCDs and injuries. Islamabad maintained the highest life expectancy in the country throughout the study period. Only one subnational unit, Azad Jammu and Kashmir, achieved the 1990 level of life expectancy of Islamabad (67·7 [95% UI 65·2–70·2] years); in 2019, Azad Jammu and Kashmir had the second highest life expectancy in the country at 68·6 (65·8–71·4) years.
Figure 1.
Decomposition of change in life expectancy for Pakistan and subnational locations for both sexes combined, 1990–2019
Causes of death and YLLs
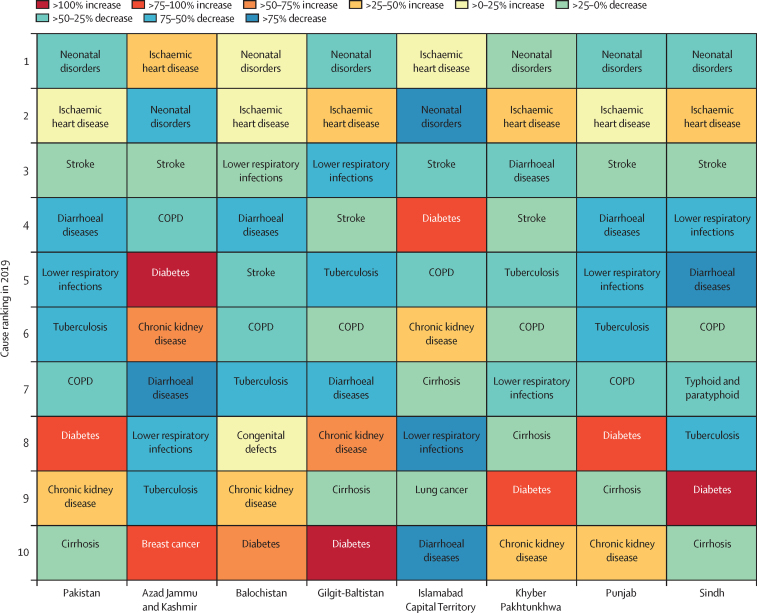
In 2019, the five leading causes of premature mortality were neonatal disorders, ischaemic heart disease, stroke, diarrhoeal diseases, and lower respiratory infections. Appendix 2 (p 41) and the online visualisation tool show the 20 leading causes of all-age deaths from 1990 to 2019 for both sexes combined. Figure 2 shows a heat map of the leading causes of all-age deaths in 2019 across Pakistan and the subnational units; the top two contributors to mortality burden are the same in all locations, with neonatal disorders and ischaemic heart disease the first and second ranked causes nationally and in all subnational locations, except that in Azad Jammu and Kashmir and Islamabad their order is reversed. In the two highest SDI subnational locations—Islamabad and Azad Jammu and Kashmir—stroke, chronic obstructive pulmonary disease, and diabetes are the next leading causes of all-ages deaths.
Figure 2.
Heat map of leading causes of all-age deaths in Pakistan and subnational locations, 2019
Percentage increase and decrease are relative to 2019. COPD=chronic obstructive pulmonary disease.
In 1990, the five leading causes of premature mortality were all communicable, maternal, neonatal, and nutritional diseases (neonatal disorders, diarrhoeal diseases, lower respiratory infections, measles, and tuberculosis). Only three NCDs—congenital defects, ischaemic heart disease, and stroke—were among the top ten leading causes of death. In 2019, neonatal disorders, ischaemic heart disease, lower respiratory infection, diarrhoeal diseases, and tuberculosis were the five leading causes of all-age years of life lost. The leading 20 causes of YLLs for all ages and both sexes between 1990 and 2019 are represented in appendix 2 (p 41) and the online visualisation tool. Five NCDs—ischaemic heart disease, stroke, congenital defects, cirrhosis, and chronic kidney disease—were in the top ten of leading causes of YLL. Age-standardised YLL rates increased from 1990 to 2019 for ischaemic heart disease, diabetes, chronic kidney disease, breast cancer, road injuries, other malignant neoplasms, and self-harm. Diabetes had the highest percentage change during the same period (109·2% [95% UI 53·1 to 186]), followed by breast cancer and chronic kidney disease. Neonatal disorders remained the leading all-age cause, but the age-standardised rate of neonatal disorders declined by 13·5% (8·1 to 32·6). Ischaemic heart disease rose in all-age rank from eighth to second. Road injuries rank increased from 23rd to 15th, and the age-standardised rate of road injuries increased by 20·4% (–13·8 to 42·0).
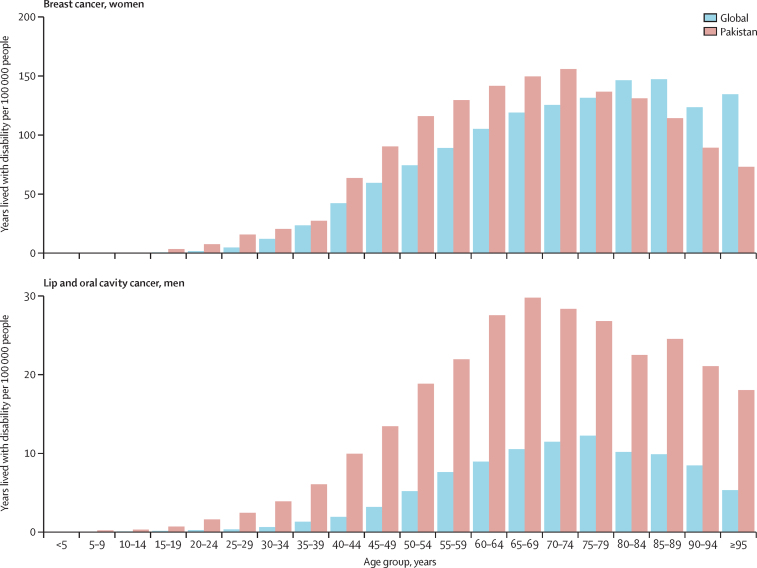
YLDs
Dietary iron deficiency, depressive disorders, and headache disorders were the three leading causes of all-age YLDs. The highest age-standardised increases were observed for diabetes, road injuries, other musculoskeletal disorders, and neonatal disorders, whereas the greatest decreases were for dietary iron deficiency, diarrhoeal diseases, haemoglobinopathies, blindness and vision impairment, tuberculosis, and intestinal nematodes. Dietary iron deficiency remained the leading all-age cause of YLDs in both years, although its age-standardised rate declined by 8·8% (95% UI 4·0–19·9). Appendix 2 (p 42) and the online visualisation tool illustrate the changes in national-level YLDs for Pakistan between 1990 and 2019 for all ages and both sexes. Figure 3 shows YLDs by age and by sex due to select cancers. YLDs due to breast cancer in girls and women aged 10–24 years in Pakistan are the highest in the world (3·3 YLDs per 100 000 people [95% UI 1·9–5·3]), with the burden increasing across female age groups. For boys and men, Pakistan's disability burden due to lip and oral cavity cancer is one of the highest globally in those aged 10–24 years and increases across male age groups.
Figure 3.
Rates per 100 000 people for years lived with disability by age for breast cancer in women and lip and oral cavity cancer for men for Pakistan compared with global rates, 2019
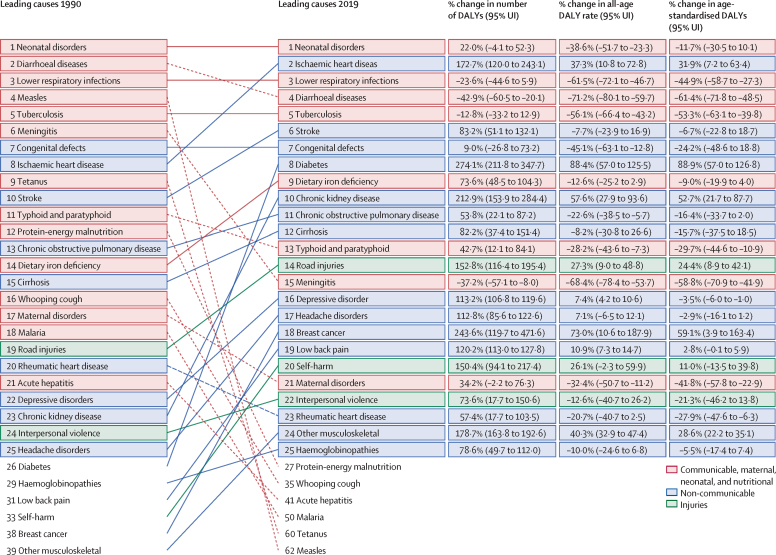
DALYs
Figure 4 shows the 25 leading causes of DALYs in 1990 and 2019 with their percentage change during the period.
Figure 4.
Leading 25 causes of DALYs in Pakistan with percentage changes, both sexes, all ages, 1990–2019
Dashed lines represent a decrease between 1990 and 2019 and solid lines represent an increase between 1990 and 2019. DALYs=disability-adjusted life-years. UI=uncertainty interval.
NCD DALYs increased from 25·3% (95% UI 23·1– 27·5) of total DALYs in 1990 to 43·7% (39·9–47·6) in 2019. Neonatal disorders were the leading cause for all-ages DALYs in 2019, but their age-standardised rate declined by 11·7% (10·1–30·5). Ischaemic heart disease increased in all-ages rank from eighth to second, and the age-standardised rate increased by 31·9% (7·2–63·4). The age-standardised rate of DALYs for lower respiratory infections and diarrhoeal diseases decreased by 44·9% (27·3–58·7) and 61·4% (48·5–71·8), respectively. The age-standardised rate of DALYs for both diabetes and chronic kidney disease increased from 1990 to 2019, rising by 88·9% (57·0–126·8) and 52·7% (21·7–87·7), respectively, whereas the rate of DALYs due to maternal disorders decreased by 41·8% (22·9–57·8).
Risk factors
Low birthweight and short gestation and particulate matter pollution were the leading contributors to overall disease burden in both 1990 and 2019 despite moderate improvements, with a 23·5% (95% UI 3·8–39·2) and 27·6% (14·3–38·6) reduction in age-standardised attributable DALY rates during the study period. Appendix 2 (p 43) and the online visualisation tool provide the number of deaths and the percentage of DALYs attributable to the 25 leading risk factors in 2019. Figure 5 provides a breakdown of the percentage of cause-specific risk-attributable all-age deaths in Pakistan in 2019 at level 3 (the GBD provides four levels of details for its diseases, injuries, and risk factors with the first level as infectious diseases, NCDs, and injuries. Each subsequent level breaks down the previous level to provide users with more detailed information). The two leading risk factors at level 3 for all-cause mortality were particulate matter pollution and high systolic blood pressure, contributing primarily to mortality due to cardiovascular disease. The third leading risk factor for all-cause mortality was low birthweight and short gestation, contributing primarily to the mortality burden due to maternal and neonatal disorders.
Figure 5.
Percentage contribution of top 20 risk factors to all-age deaths in Pakistan for both sexes combined, 2019
Discussion
Despite periods of political and economic turbulence since 1990, Pakistan has made positive strides in improving overall health outcomes at the population level and continues to seek innovative solutions to challenging health and health policy problems. To draw attention to Pakistan's health challenges, as well as highlight areas of improvement and new directions, we present the first comprehensive study of the burden of disease, injuries, and risk factors in Pakistan and its subnational administrative units. The results of our study contain estimates of disease burden by age, sex, and year between 1990 and 2019. In support of Pakistan's UHC programme, the Ministry of National Health Services Regulations and Coordination has used national-level GBD estimates to inform the essential packages of care under the Disease Control Priorities, Third Edition methodology; however, given the disparate health profiles of the subnational locations presented in this study, more targeted packages of essential care will aid in UHC planning. These estimates can also be used to inform Pakistan's UHC programme and assist the country's plan to meet the Sustainable Development Goal (SDG) targets.
The Pakistan health ministry has joined its UHC programme to Sehat Sahulat, the federal health insurance initiative for resource-lacking citizens. In a programme launched by the Pakistan Government in early 2022 following a successful pilot programme in Khyber Pakhtunkhwa, residents of Punjab will be awarded a health card to cover most medical expenses. Such programmes, however, face an uphill climb given our analyses of Pakistan's health-care system performance. For instance, our analysis of 195 countries and territories in 2016 found that Pakistan's Healthcare Access and Quality Index was 37·6 (95% UI 33·7–41·9), ranking 154th of the 195 countries.27 In 2019, we reported on the health components of the UN SDGs for 188 countries and the chance of achieving them by 2030;28 Pakistan ranked 164th. We published a report on the Human Capital Index, a combined score of expected years of life from age 20 to 64 years adjusted for educational attainment, learning or education quality, and functional health status for 195 countries and territories;29 Pakistan ranked 116th. Our analysis could be used to address these problems and help build capacities, design disease-prevention activities, and set health priorities at both national and subnational levels in Pakistan.
The results of our study reveal that Pakistan is showing signs of undergoing an epidemiological transition as the burden shifts to NCDs; nevertheless, communicable diseases remain a source of health loss. NCD DALYs increased from 25·3% (95% UI 23·1–27·5) of total DALYs in 1990 to 43·7% (39·9–47·6) in 2019. For a country such as Pakistan with a large percentage of the population aged under 40 years, efforts to reduce the burden of NCDs must focus on informing the youth and young adults about lifestyle choices, behaviours, and medical interventions that will reduce the risk of NCDs. Although there is an ageing population that is increasingly affected by NCDs, investments in health systems and preventive medicine can reach younger generations.
At the same time, the country continues to face a large burden of infectious diseases that are not impacting the population equally across sexes, ages, and locations. The burden of tuberculosis and hepatitis is higher than expected given the country's SDI, and containing their spread remains a challenge. Reducing the prevalence of tuberculosis and hepatitis is further complicated by the fact that in most parts of the country, antibiotics prescriptions and injections are not regulated adequately by health professionals.30, 31 Indeed, the use of low-quality medicines is an issue in Pakistan and other low-income and middle-income countries.32 Pakistan should redouble its commitment to national tuberculosis and hepatitis control programmes. Additionally, Pakistan remains one of the last countries (including its neighbour Afghanistan) with endemic wild polio virus.16 Since 1994, Pakistan has undertaken a public health campaign to eradicate polio. The burden of polio is quite low. There were only 147 confirmed cases of polio in 2019,33 which were concentrated in the mountainous tribal regions near the Pakistan–Afghanistan border. The presence of wild polio in Pakistan has been viewed by the international global health community as a governmental failure and driven partly by regional conflicts and terrorism. As a result, resources have been directed to address this problem through childhood vaccinations.18 Despite these efforts, there must be continued public health campaigns aimed at eradicating the disease. Deaths caused by vaccine-preventable diseases such as whooping cough and tetanus have decreased in Pakistan, but the goals for reducing the prevalence of measles and eradicating polio have not been met. There are also concerns over the emergence of drug-resistant typhoid,34, 35, 36 and the overall burdens of typhoid and paratyphoid in Pakistan are some of the highest levels in the world.
NCD burden is increasing in Pakistan, as our study and previous research indicate.37 Cardiovascular disease, cancers, and diabetes were major causes of death and disability in 2019. The rise of NCDs in Pakistan where the population is young deserves special attention. Although the country still faces infectious diseases challenges, equal attention to NCD prevention is needed to reduce the current and future burden. These NCD patterns are observed in other countries with similar demographics and characteristics, such as India and Saudi Arabia. Focusing on the leading risk factors of NCDs through development and implementations of policies and programmes will yield great health benefits. The forecasted burden for Pakistan for 2040 shows a rapid increase in cardiovascular disease, cancers, and diabetes, and we estimate that by 2040 these will be the three leading causes of death.38
The increase in mental health burden in Pakistan is relevant for policy makers and practitioners. The reported results on mental health disorders do not include the effect of the COVID-19 pandemic; however, based on other GBD studies, we can probably expect that Pakistan—like other global locations39—will see a rise in mental health burden due to the COVID-19 pandemic. Addressing mental health needs in Pakistan is crucial to improving health outcomes. Indeed, developing a national plan for improving mental health is needed to ensure that mental-health-care resources are adequate for Pakistan.
Our study revealed slow reductions in maternal and child mortality, high fertility rates, and persistent issues of gender disparities, and these areas of women's and children's health warrant a renewed focus and investment. For instance, a primary health-care programme coordinated by Aga Khan University (Karachi, Pakistan), Aga Khan Health Services (multiple locations, Pakistan), and local governments in the northern areas resulted in a reduction of infant and maternal mortalities between 1980 and 2004.40 The federal government also has a task force addressing children's health and submitted several recommendations to reduce malnutrition.41, 42 Pakistan has high rates of maternal and adolescent girl malnutrition, micronutrient deficiencies, fetal malnutrition, and low birthweight.41, 42 Although the country has nutrition initiatives underway, including large-scale food fortification and vitamin A supplementation programmes, there is no single national nutrition policy. This is urgently needed, especially as climate change and the increased severity of drought, flood, and pestilence threaten food security.43 Investing in raising living standards by increasing access to clean water and sanitation will advance gender-equity goals. There has been progress in reducing deaths by vaccine-preventable diseases such as measles, whooping cough, typhus, and tetanus in Pakistan, especially in low-ranked SDI areas. This is evidence that Pakistan's childhood vaccination campaigns are making some progress; however, many children globally who have never received a routine vaccination live in Pakistan,44 and the COVID-19 pandemic has disrupted such efforts.45, 46
Burden of disease estimates serve as baselines for future trends and allow health professionals to identify areas of intervention. National-level estimates can obscure differential health outcomes and disparities that occur at the subnational level. Pakistan is a populous country, but with only seven subnational units, the value of subnational estimates is limited by data sources and geographical scope. Variations within Punjab, especially between rural and urban areas and the northern and southern regions of the province, are missed as a result. Performing estimates at the district level will be a necessary next step. Improving vital registration systems in Pakistan to ensure accurate coding of deaths would improve the ability of policy makers, officials, and researchers to address sources of health loss. Increasing the engagement of local and national health officials is crucial to ensure that GBD estimates are used to improve health in Pakistan.
Our study has limitations. First, the availability of data affects the accuracy of our estimates. Data collection efforts must be prioritised by provincial and federal governments, especially vital registries, and other essential health records. Transparency around data collection and analytical practices must also be prioritised to improve the overall accuracy, usefulness, and confidence of health estimates. Increased data sharing and collaboration between academic researchers and government representatives would be a positive step in this direction. For instance, we have more data sources for certain outcomes such as maternal and child health due to the focus of researchers, but less data on outcomes such as adult dietary intake as a result of priorities and resources. Second, data sources from Pakistan's private health sector could not be included in this study as the providers neither reported data to the government nor published data in publicly accessible reports. Similar limitations apply to practitioners of Indigenous and traditional techniques. We are constrained by the sociological categories used in surveys and other data collection techniques and are not able to provide estimates based on language, ethnicity, and religion. Third, it can be difficult to differentiate between changes in disease and risk factors occurrence and measurement errors. GBD methodology accounts for bias, but sometimes sparse data and variable survey quality in remote and conflict areas impact these corrections. Fourth, GBD includes risk-outcome pairs according to World Cancer Research Fund criteria of causality and may exclude some that do not meet the criteria.
Our analysis of diseases, injuries, and risk factors in Pakistan and across its seven subnational administrative units should lay the foundation for future studies that use the GBD framework to help build and strengthen the capacity of domestic health systems. GBD 2019 provides a baseline of evidence immediately before the COVID-19 pandemic, and future projects could examine the impact the pandemic has had on gender, age, and mental health; childhood vaccinations; several NCDs associated with lifestyle and diet; and overall health-care spending. Future research on the burden of disease in Pakistan will depend on the collection, availability, and quality of data. Additionally, the next step in the GBD for Pakistan could be analyses at the district and municipal level, which would provide local estimates of health and health loss for policy makers working in Pakistan's decentralised health system.
Data sharing
This study follows the Guidelines for Accurate and Transparent Health Estimates Reporting. To download the data used in these analyses, please visit the Global Health Data Exchange GBD 2019 Data Resources page.
Declaration of interests
S Afzal reports support for the present manuscript from the Department of Community Medicine and Epidemiology, King Edward Medical University for performing duties as Faculty Member and Dean. S Afzal reports participation on a Data Safety Monitoring Board or Advisory Board with Corona Expert Advisory Group and Dengue Expert Advisory Group; unpaid leadership or fiduciary roles in board, society, committee, or advocacy groups with Pakistan Society of Community Medicine & Public Health, Pakistan Association of Medical Editors, and Pakistan Society of Medical Infectious Diseases; all outside the submitted work. Z Samad reports grants or contracts from Bill & Melinda Gates Foundation (INV-021944 and INV-050389); Fogarty International Center of the National Institutes of Health (D43TW011625); National Institute for Health and Care Research; Yale University, Duke University; Certara; and PHRI; and payment from Cytokinetics as an advisor for participation in the Heart Failure Publication Committee meeting, outside the submitted work
Acknowledgments
Acknowledgments
This work was supported by the Bill & Melinda Gates Foundation. S Afzal acknowledges institutional support from the Department of Community Medicine and Epidemiology, King Edward Medical University. U Saeed and Z Z Piracha acknowledge support from the International Center of Medical Sciences Research, Islamabad (44000), Pakistan.
Editorial note: The Lancet Group takes a neutral position with respect to territorial claims in published tables, text, appendices, and institutional affiliations.
GBD 2019 Pakistan Collaborators
Assad Hafeez, William James Dangel, Samuel M Ostroff, Ayyaz Gul Kiani, Scott D Glenn, Jaffar Abbas, Muhammad Sohail Afzal, Saira Afzal, Sajjad Ahmad, Ali Ahmed, Haroon Ahmed, Liaqat Ali, Muhammad Ali, Zahid Ali, Muhammad Arshad, Tahira Ashraf, Zulfiqar A Bhutta, Sadia Bibi, Zahid A Butt, Jai K Das, Zehra Fadoo, Asif Hanif, Khezar Hayat, Ayesha Humayun, Khalid Iqbal, Usman Iqbal, Nauman Khalid, Ejaz Ahmad Khan, Muhammad Shahzeb Khan, Ahmad Azam Malik, Muhammad Naveed, Shumaila Naz, Robina Khan Niazi, Zahra Zahid Piracha, Umar Saeed, Muhammad Salman, Zainab Samad, Muhammad Arif Nadeem Saqib, Syed Mahboob Shah, Izza Shahid, Masood Ali Shaikh, Hina Shamshad, Kanwar Hamza Shuja, Muhammad Suleman, Anayat Ullah, Irfan Ullah, Saif Ullah, Sana Ullah, Yasir Waheed, Abdul Waris, Simon I Hay, Christopher J L Murray, and Ali H Mokdad.
Affiliations
Department of Public Health (A Hafeez PhD) and Department of Epidemiology and Biostatistics (E A Khan MPH), Health Services Academy, Islamabad, Pakistan; Institute for Health Metrics and Evaluation (W J Dangel MEd, S M Ostroff PhD, A G Kiani MPH, S D Glenn MSc, Prof S I Hay FMedSci, Prof C J L Murray DPhil, A H Mokdad PhD), Henry M Jackson School of International Studies (S M Ostroff), Department of Health Metrics Sciences, School of Medicine (Prof S I Hay, Prof C J L Murray, A H Mokdad), University of Washington, Seattle, WA, USA; Antai College of Economics (J Abbas PhD), Shanghai Jiao Tong University, Shanghai, China; Department of Life Sciences (M S Afzal PhD, I Ullah PhD), School of Food and Agricultural Sciences (N Khalid PhD), School of Sciences (M A N Saqib PhD), University of Management and Technology, Lahore, Pakistan; Department of Community Medicine (Prof S Afzal PhD), King Edward Memorial Hospital, Lahore, Pakistan; Department of Public Health (Prof S Afzal), Public Health Institute, Lahore, Pakistan; Department of Health and Biological Sciences (S Ahmad PhD), Abasyn University, Peshawar, Pakistan; School of Pharmacy (A Ahmed Mphil), Monash University, Bandar Sunway, Malaysia; Department of Pharmacy (A Ahmed), Quaid I Azam University Islamabad, Islamabad, Pakistan; Department of Biosciences (H Ahmed PhD), COMSATS Institute of Information Technology, Islamabad, Pakistan; Department of Biological Sciences (L Ali PhD, S Naz PhD), Multidisciplinary Department (A Ullah MS), National University of Medical Sciences, Rawalpindi, Pakistan; Department of Biotechnology (M Ali PhD), National Institute of Psychology (K H Shuja MS), Quaid-i-Azam University, Islamabad, Pakistan; Pakistan Academy of Sciences, Islamabad, Pakistan (M Ali); Department of Pharmacy (Z Ali PharmD), Center of Biotechnology and Microbiology (M Arshad PhD), University of Peshawar, Peshawar, Pakistan; University Institute of Radiological Sciences and Medical Imaging Technology (T Ashraf MS), University Institute of Public Health (A Hanif PhD, A A Malik PhD), Department of Pharmacy Practice (M Salman PhD), The University of Lahore, Lahore, Pakistan; Centre for Global Child Health (Prof Z A Bhutta PhD), University of Toronto, Toronto, ON, Canada; Centre of Excellence in Women & Child Health (Prof Z A Bhutta), Division of Women and Child Health (J K Das MD), Department of Oncology (Prof Z Fadoo MD), Department of Medicine (Prof Z Samad MD), Department of Family Medicine (Prof S M Shah PhD), Aga Khan University, Karachi, Pakistan; Institute of Soil and Environmental Sciences (S Bibi PhD, Saif Ullah PhD), University of Agriculture, Faisalabad, Pakistan; School of Public Health and Health Systems (Z A Butt PhD), University of Waterloo, Waterloo, ON, Canada; Al Shifa School of Public Health (Z A Butt), Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan; Institute of Pharmaceutical Sciences (K Hayat MS), University of Veterinary and Animal Sciences, Lahore, Pakistan; Department of Pharmacy Administration and Clinical Pharmacy (K Hayat), Xian Jiaotong University, Xian, China; Department of Public Health and Community Medicine (Prof A Humayun PhD), Shaikh Khalifa Bin Zayed Al-Nahyan Medical College, Lahore, Pakistan; Department of Human Nutrition (K Iqbal DrPH), Khyber Medical University, Peshawar, Pakistan; College of Public Health (U Iqbal PhD), Taipei Medical University, Taipei, Taiwan; Department of Internal Medicine (M S Khan MD), John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, USA; Department of Internal Medicine (M S Khan), Dow University of Health Sciences, Karachi, Pakistan; Rabigh Faculty of Medicine (A A Malik), King Abdulaziz University, Jeddah, Saudi Arabia; Department of Biotechnology (M Naveed PhD), University of Central Punjab, Lahore, Pakistan; International Islamic University Islamabad, Islamabad, Pakistan (R K Niazi PhD); International Center of Medical Sciences Research, Islamabad, Pakistan (Z Z Piracha PhD, Prof U Saeed PhD); Department of Pathology and Microbiology (Prof U Saeed), Jinnah Medical College, Peshawar, Pakistan; Department of Medicine (Prof Z Samad), Duke University, Durham, NC, USA; Research Development Coordination Section (M A N Saqib), Pakistan Health Research Council, Islamabad, Pakistan; Institute of Public Health (Prof S M Shah), United Arab Emirates University, Al Ain, United Arab Emirates; Department of Internal Medicine (I Shahid MBBS), Ziauddin University, Karachi, Pakistan; Independent Consultant, Karachi, Pakistan (M A Shaikh MD); Research Institute of Pharmaceutical Sciences (H Shamshad PhD), University of Karachi, Karachi, Pakistan; Center for Biotechnology and Microbiology (M Suleman PhD), University of Swat, Mingora, Pakistan; School of Life Sciences (M Suleman), Xiamen University, Xiamen, China; Department of Zoology (Sana Ullah PhD), Division of Science and Technology (Sana Ullah), University of Education, Lahore, Pakistan; Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan (Prof Y Waheed PhD); Department of Biomedical Sciences (A Waris MS), City University of Hong Kong, Hong Kong Special Administrative Region, China.
Contributors
WJD, SIH, AHM, CJLM, and SMO managed the overall research enterprise. WJD, AGK, AHM, and SMO wrote the first draft of the manuscript. AHM had the primary responsibility for applying analytical methods to produce estimates. SDG had the primary responsibility for seeking, cataloguing, extracting, or cleaning data and designing or coding figures and tables. SAf, SAh, HA, LA, MAl, TA, ZABh, SB, AHaf, SIH, KH, KI, UI, NK, EAK, MSK, AHM, SN, RKN, ZZP, US, ZS, SMS, MAS, HS, KHS, MSu, AU, IU, SaiU, SanU, YW, and AW provided data or critical feedback on data sources. SAf, AA, LA, SIH, AHM, US, ZS, and MSu developed methods or computational machinery. JA, MSA, SAf, SAh, AA, HA, LA, ZA, MAr, TA, ZABh, SB, ZABu, JKD, ZF, AHaf, AHan, SIH, KH, AHum, KI, UI, NK, EAK, MSK, AAM, AHM, MN, SN, RKN, ZZP, US, MSa, ZS, MANS, SMS, IS, MAS, KHS, MSu, AU, IU, SaiU, SanU, YW, and AW provided critical feedback on methods or results. JA, MSA, SAf, AA, LA, MAl, ZA, MAr, ZABh, SB, WJD, ZF, AHaf, SIH, UI, EAK, MSK, AAM, AHM, SN, RKN, SMO, ZZP, US, ZS, SMS, IS, MSu, AU, IU, and SaiU revised the manuscript critically for important intellectual content. SAf, WJD, SIH, AHM, CJLM, SMO, and ZS managed the estimation or publications process. All authors had full access to the data in this study and had final responsibility for the decision to submit for publication. AHM and AHaf accessed and verified the underlying data reported in this study.
Contributor Information
GBD 2019 Pakistan Collaborators:
Assad Hafeez, William James Dangel, Samuel M Ostroff, Ayyaz Gul Kiani, Scott D Glenn, Jaffar Abbas, Muhammad Sohail Afzal, Saira Afzal, Sajjad Ahmad, Ali Ahmed, Haroon Ahmed, Liaqat Ali, Muhammad Ali, Zahid Ali, Muhammad Arshad, Tahira Ashraf, Zulfiqar A Bhutta, Sadia Bibi, Zahid A Butt, Jai K Das, Zehra Fadoo, Asif Hanif, Khezar Hayat, Ayesha Humayun, Khalid Iqbal, Usman Iqbal, Nauman Khalid, Ejaz Ahmad Khan, Muhammad Shahzeb Khan, Ahmad Azam Malik, Muhammad Naveed, Shumaila Naz, Robina Khan Niazi, Zahra Zahid Piracha, Umar Saeed, Muhammad Salman, Zainab Samad, Muhammad Arif Nadeem Saqib, Syed Mahboob Shah, Izza Shahid, Masood Ali Shaikh, Hina Shamshad, Kanwar Hamza Shuja, Muhammad Suleman, Anayat Ullah, Irfan Ullah, Saif Ullah, Sana Ullah, Yasir Waheed, Abdul Waris, Simon I Hay, Christopher J L Murray, and Ali H Mokdad
Supplementary Materials
References
- 1.Wang H, Abbas KM, Abbasifard M, et al. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mboi N, Murty Surbakti I, Trihandini I, et al. On the road to universal health care in Indonesia, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:581–591. doi: 10.1016/S0140-6736(18)30595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pakistan Bureau of Statistics Final results (census 2017) https://www.pbs.gov.pk/content/final-results-census-2017
- 4.Rasmussen B, Allen S, Rasmussen ZA, Bajwa R. Learning from disasters to save lives every day in Pakistan. Lancet. 2013;381:2232–2234. doi: 10.1016/S0140-6736(13)60652-2. [DOI] [PubMed] [Google Scholar]
- 5.Nishtar S, Boerma T, Amjad S, et al. Pakistan's health system: performance and prospects after the 18th Constitutional Amendment. Lancet. 2013;381:2193–2206. doi: 10.1016/S0140-6736(13)60019-7. [DOI] [PubMed] [Google Scholar]
- 6.GBD 2020 Health Financing Collaborator Network Tracking development assistance for health and for COVID-19: a review of development assistance, government, out-of-pocket, and other private spending on health for 204 countries and territories, 1990–2050. Lancet. 2021;398:1317–1343. doi: 10.1016/S0140-6736(21)01258-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang AY, Cowling K, Micah AE, et al. Past, present, and future of global health financing: a review of development assistance, government, out-of-pocket, and other private spending on health for 195 countries, 1995–2050. Lancet. 2019;393:2233–2260. doi: 10.1016/S0140-6736(19)30841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghaffar A, Zaidi S, Qureshi H, Hafeez A. Medical education and research in Pakistan. Lancet. 2013;381:2234–2236. doi: 10.1016/S0140-6736(13)60146-4. [DOI] [PubMed] [Google Scholar]
- 9.Benazir Income Support Programme Overview. https://www.bisp.gov.pk/Overview
- 10.Cheema I, Hunt S, Javeed S, Lone T, O'Leary S. Oxford Policy Management; Oxford: 2016. Benazir income support programme: final impact evaluation report. [Google Scholar]
- 11.Ministry of Poverty Alleviation and Social Safety. Government of Pakistan About us. https://www.pass.gov.pk/default.aspx
- 12.Hussain S, Hussain R, Hafeez A, Khan A. Prime Minister's national health programme (PMNHP): a cost comparison analysis. Pak J Health. 2018;8:37–42. [Google Scholar]
- 13.Khalid F, Petro Brunal M, Sattar A, et al. Assessing the efficiency of sub-national units in making progress towards universal health coverage: evidence from Pakistan. Health Syst Reform. 2020;6:1–14. doi: 10.1080/23288604.2019.1617026. [DOI] [PubMed] [Google Scholar]
- 14.Lozano R, Fullman N, Mumford JE, et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1250–1284. doi: 10.1016/S0140-6736(20)30750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute of Health Islamic Republic of Pakistan Institute of Nutrition and Health. https://www.nih.org.pk/institute-of-nutirition-and-health
- 16.Yusufzai A. Efforts to eradicate polio virus in Pakistan and Afghanistan. Lancet Child Adolesc Health. 2020;4:17. [Google Scholar]
- 17.Kanwal S, Hussain A, Mannan S, Perveen S. Regression in polio eradication in Pakistan: a national tragedy. J Pak Med Assoc. 2016;66:328–333. [PubMed] [Google Scholar]
- 18.Khan MT, Zaheer S, Shafique K. Maternal education, empowerment, economic status and child polio vaccination uptake in Pakistan: a population based cross sectional study. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-013853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute for Health Metrics and Evaluation . IHME; Seattle, WA: 2020. Protocol for the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) [Google Scholar]
- 20.Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Abajobir AA, Abate KH, et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1084–1150. doi: 10.1016/S0140-6736(17)31833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naghavi M, Richards N, Chowdhury H, et al. Improving the quality of cause of death data for public health policy: are all ‘garbage’ codes equally problematic? BMC Med. 2020;18:55. doi: 10.1186/s12916-020-01525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sullivan DF. A single index of mortality and morbidity. HSMHA Health Rep. 1971;86:347–354. [PMC free article] [PubMed] [Google Scholar]
- 25.Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Das Gupta P. US Government Printing Office; Washington, DC: 1993. Standardization and decomposition of rates: a user's manual. [Google Scholar]
- 27.Fullman N, Yearwood J, Abay SM, et al. Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2018;391:2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lozano R, Fullman N, Abate D, et al. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related Sustainable Development Goals for 195 countries and territories: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:2091–2138. doi: 10.1016/S0140-6736(18)32281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim SS, Updike RL, Kaldjian AS, et al. Measuring human capital: a systematic analysis of 195 countries and territories, 1990–2016. Lancet. 2018;392:1217–1234. doi: 10.1016/S0140-6736(18)31941-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saleem Z, Saeed H, Ahmad M, et al. Antibiotic self-prescribing trends, experiences and attitudes in upper respiratory tract infection among pharmacy and non-pharmacy students: a study from Lahore. PLoS One. 2016;11 doi: 10.1371/journal.pone.0149929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saleem Z, Hassali MA, Hashmi FK. Pakistan's national action plan for antimicrobial resistance: translating ideas into reality. Lancet Infect Dis. 2018;18:1066–1067. doi: 10.1016/S1473-3099(18)30516-4. [DOI] [PubMed] [Google Scholar]
- 32.Zaman MH. Oxford University Press; Oxford, New York: 2018. Bitter pills: the global war on counterfeit drugs. [Google Scholar]
- 33.Pakistan Polio Eradication Programme Polio cases in provinces. 2020. https://www.endpolio.com.pk/polioin-pakistan/polio-cases-in-provinces
- 34.Antillón M, Warren JL, Crawford FW, et al. The burden of typhoid fever in low- and middle-income countries: a meta-regression approach. PLoS Negl Trop Dis. 2017;11 doi: 10.1371/journal.pntd.0005376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saleem Z, Hassali MA. Travellers take heed: outbreak of extensively drug resistant (XDR) typhoid fever in Pakistan and a warning from the US CDC. Travel Med Infect Dis. 2019;27:127. doi: 10.1016/j.tmaid.2018.10.013. [DOI] [PubMed] [Google Scholar]
- 36.Yousafzai MT, Karim S, Qureshi S, et al. Effectiveness of typhoid conjugate vaccine against culture-confirmed Salmonella enterica serotype Typhi in an extensively drug-resistant outbreak setting of Hyderabad, Pakistan: a cohort study. Lancet Glob Health. 2021;9:e1154–e1162. doi: 10.1016/S2214-109X(21)00255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jafar TH, Haaland BA, Rahman A, et al. Non-communicable diseases and injuries in Pakistan: strategic priorities. Lancet. 2013;381:2281–2290. doi: 10.1016/S0140-6736(13)60646-7. [DOI] [PubMed] [Google Scholar]
- 38.Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016–40 for 195 countries and territories. Lancet. 2018;392:2052–2090. doi: 10.1016/S0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Santomauro DF, Herrera AMM, Shadid J, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Walraven G, Manaseki-Holland S, Hussain A, Tomaro JB. Improving maternal and child health in difficult environments: the case for “cross-border” health care. PLoS Med. 2009;6:e5. doi: 10.1371/journal.pmed.1000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhutta ZA, Hafeez A, Rizvi A, et al. Reproductive, maternal, newborn, and child health in Pakistan: challenges and opportunities. Lancet. 2013;381:2207–2218. doi: 10.1016/S0140-6736(12)61999-0. [DOI] [PubMed] [Google Scholar]
- 42.Malik SM, Bhutta ZA. Reform of primary health care in Pakistan. Lancet. 2018;392:1375–1377. doi: 10.1016/S0140-6736(18)32275-X. [DOI] [PubMed] [Google Scholar]
- 43.National Disaster Management Authority. Prime Minister's Office. Government of Pakistan NDMA Annual Report 2017. http://cms.ndma.gov.pk/storage/app/public/publications/October2020/Q0zYourItlTWdj03sSZk.pdf
- 44.Galles N, Liu P, Updike R, et al. Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: a systematic analysis for the Global Burden of Disease 2019 Study. Lancet. 2021;398:503–521. doi: 10.1016/S0140-6736(21)00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Causey K, Fullman N, Sorensen RJD, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398:522–534. doi: 10.1016/S0140-6736(21)01337-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chandir S, Siddiqi DA, Setayesh H, Khan AJ. Impact of COVID-19 lockdown on routine immunisation in Karachi, Pakistan. Lancet Glob Health. 2020;8:e1118–e1120. doi: 10.1016/S2214-109X(20)30290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This study follows the Guidelines for Accurate and Transparent Health Estimates Reporting. To download the data used in these analyses, please visit the Global Health Data Exchange GBD 2019 Data Resources page.