Abstract
Objectives
Poor sleep is common among older adults with chronic health conditions and their spousal caregivers. However, dyadic sleep patterns among spouses are underexplored within the literature. This study examines dyadic sleep characteristics and associated contextual factors among spousal care dyads.
Methods
Participants included 462 older adult spousal care dyads from the 2015 National Health and Aging Trends Study and National Study of Caregiving (mean ages of care recipients/caregivers = 79 and 76 years, respectively; 22% of dyads were living with dementia). Self-reported sleep included frequency of (a) trouble falling back asleep among dyads, (b) care-related sleep disturbances among caregivers, and (c) trouble initiating sleep among care recipients. Predictors included between-dyad characteristics such as whether respondents had dementia, care burden and support, relationship quality, neighborhood cohesion, and within-dyad characteristics such as demographics, depression, and positive affect. We conducted multilevel dyadic analysis and actor–partner interdependence modeling.
Results
Sleep was correlated more among dyads living with dementia than those with other chronic conditions. Care dyads had poorer sleep if caregivers reported higher care burden; however, better relationship quality marginally ameliorated the association. Depressive symptoms had a partner effect on poorer sleep among care dyads, whereas positive emotions and older age only had an actor effect on better sleep for care recipients and spousal caregivers. Neighborhood cohesion, care support, and other demographic characteristics were not associated with dyadic sleep outcomes.
Discussion
Addressing both care recipient- and caregiver-related factors may improve sleep health for both members of the care dyad living with chronic conditions.
Keywords: Alzheimer’s disease, Caregiving, Depression, Health outcomes, Marriage
Poor sleep, characterized by difficulty falling asleep, multiple awakenings during sleep, and early morning awakenings, is common among older adults with chronic health conditions (Bonanni et al., 2005; Moran et al., 2005; Tractenberg et al., 2006). Unsurprisingly, poor sleep is also a common health issue among family caregivers—particularly spouses providing dementia care who also bedshare (Liu et al., 2021; Peng et al., 2019). Spousal caregivers may awaken during the night due to caregiving tasks or dementia-related behaviors (Creese et al., 2008; Gibson et al., 2014; Song et al., 2018), which may make it difficult to return to sleep and/or lead to early morning awakenings—core symptoms of clinical insomnia disorder. Insomnia in spousal caregivers may result in higher care burden and acceleration of age-related normative changes in overall physical functioning and sleep health (Pinquart & Sörensen, 2011; Robinson et al., 2005). Ultimately, poor sleep among family caregivers can negatively affect ability to provide care, which may lead to early institutionalization for care recipients (Gaugler et al., 2009; Yaffe et al., 2002). Spousal dyad sleep health is an important target symptom requiring attention.
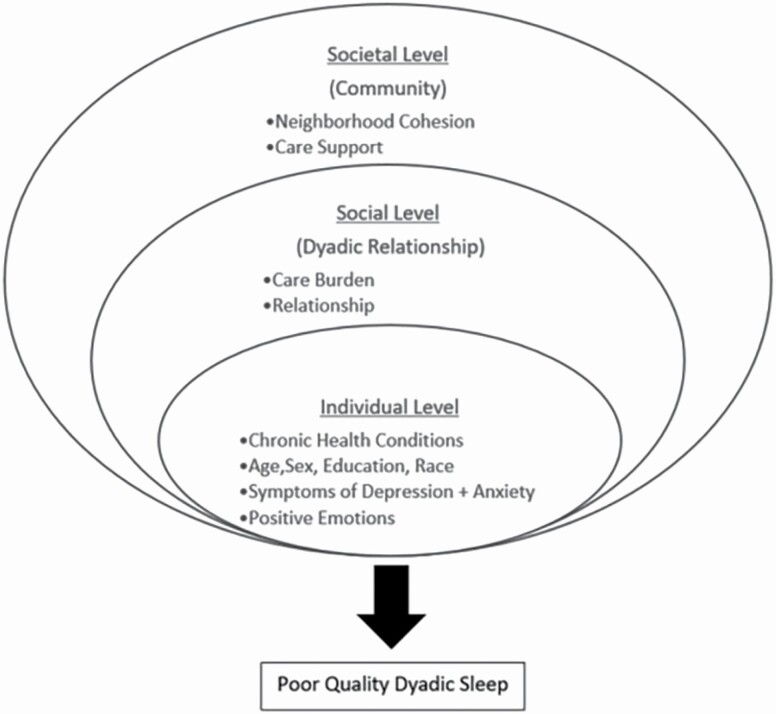
Various factors contribute to poor sleep within care dyads. However, the literature has primarily emphasized factors and outcomes at the individual level. The social–ecological model of sleep describes factors affecting poor sleep at three levels: individual, social, and societal (Grandner, 2020). The individual level is embedded within the social level and includes dyadic relationships (see Figure 1). In addition to known individual-level factors such as health conditions (e.g., dementia), older age, being female, minoritized race/ethnicity, and lower socioeconomic status (Grandner et al., 2016), dyadic-level characteristics, such as relationship quality and care burden, can affect sleep for care recipients and caregivers (Troxel et al., 2007). Care burden and relationship quality both have strong theoretical and empirical historical basis in family caregiving research.
Figure 1.
Conceptual model of dyadic sleep and contextual factors.
For instance, the stress process model posits that care burden is associated with compromised well-being in caregivers (Pearlin et al., 1990); however, some coping strategies caregivers use to manage care burden can negatively affect care recipients’ health and well-being—including dementia progression (Tschanz et al., 2013). Interestingly, cognitive and functional decline among care recipients with dementia has also been associated with dyadic closeness (Norton et al., 2009), and caregivers who report poorer relationship quality are at greatest risk of care burden (Lea Steadman et al., 2007). Although relationship quality and care burden are important for dyadic well-being, few studies have examined these relationships dyadically—particularly how they may affect sleep.
Additionally, these individual-, social-, and dyadic-level factors are further embedded within the societal level, which includes neighborhood characteristics and the care support environment. Neighborhood cohesion influences sleep by creating support networks, trust, and community spirit, increasing perceived safety, and reinforcement of local social norms (e.g., not staying up late at night; Alhasan et al., 2020; Billings et al., 2020). Care support and social engagement (i.e., service use, emotional support) are also associated with better sleep among caregivers (Lee et al., 2007; Liang et al., 2020).
It is unclear how these individual, dyadic, social, and societal factors may influence dyadic sleep patterns. The few studies that have explored spousal sleep patterns dyadically have had small sample sizes or targeted couples in clinical settings (Chen, 2017; Elsey et al., 2019; Gunn et al., 2015, 2021; Hasler & Troxel, 2010). By using a national sample to examine the dyadic sleep patterns between older adults with chronic health conditions and their family caregivers, a better understanding of the factors related to poor sleep in both members of spousal care dyads may be developed along with targeted interventions designed to improve family sleep health.
The Current Study
This study aimed to examine the dyadic sleep patterns of older adults with chronic health conditions and their spousal caregivers, and to explore the contextual factors that may influence dyadic sleep outcomes. Based on the known differences in the caregiving demands and caregiver distress between general caregiving versus dementia caregiving populations (Pinquart & Sörensen, 2007), we hypothesized that sleep would be more correlated among care dyads living with dementia than those with other chronic conditions (H1). Based on prior findings about how care burden can affect care dyads’ well-being, we hypothesized that care dyads would have poorer sleep if the caregiver reported higher care burden (H2.1). As sleep disturbance is more prevalent in dementia, we also hypothesized that care dyads living with dementia would have poorer sleep than those with other chronic conditions (H2.2). In addition, based on the social–ecological model of sleep, we hypothesized that care dyads living in a less cohesive neighborhood, having caregivers reporting lower care support and poorer relationship quality, would have poorer sleep (H2.3). Further, based on prior findings about how relationship quality relates to varying levels of well-being among care dyads, we hypothesized that better relationship quality would moderate the effect of high care burden on poor sleep among care dyads regardless of chronic conditions (H3). Finally, we examined how within-dyad and individual characteristics may affect dyadic sleep outcomes based on the actor–partner interdependence models (APIM).
Method
Data and Study Population
This cross-sectional study used data from the 2015 National Health and Aging Trends Study (NHATS) and National Study of Caregiving (NSOC), national surveys of older adults and their caregivers in the United States (Freedman et al., 2019; Kasper & Freedman, 2020). The NHATS aims to collect data to reduce disability, maximize functioning and other health outcomes, and enhance the quality of life among older adults (Freedman & Kasper, 2019). Participants were eligible for NHATS if they were Medicare beneficiaries aged 65 and older and lived in the contiguous United States. Participants were asked to answer questions regarding their physical and cognitive capacity, health, and well-being. A proxy respondent (generally a family caregiver) was interviewed when participants were unable to do so because of dementia or other serious illness.
The NSOC is a supplement of NHATS that surveys caregivers of NHATS participants who received assistance with self-care, mobility, household activities, transportation, or medical care from at least one unpaid family caregiver. The NSOC collects detailed information regarding activities for which help was provided, duration and intensity of help, support services, effects on caregivers, and health and well-being of caregivers. Of the 8,334 NHATS respondents in 2015, 1,458 had at least one caregiver complete the NSOC, with a total of 2,204 caregivers interviewed. Only NHATS respondents and their spousal caregivers who lived in the same household in the community setting were included in this study. The final analytic sample consisted of 462 spousal care dyads.
Measures
Dyadic sleep outcomes
Both older adults with chronic conditions and their caregivers answered a single-item question related to frequency of trouble falling back asleep (“In the last month, on nights when you woke up before you wanted to get up, how often did you have trouble falling back asleep?”) Responses were provided using a 5-point Likert scale, ranging from 1 (every night) to 5 (never), with higher scores suggesting less frequent trouble and better sleep. In addition, we created a composite variable of insomnia symptoms by combining the above single-item sleep question with two additional sleep items rated by each member of the dyads. They included frequency of trouble initiating sleep among care recipients (“In the last month, how often did it take more than 30 min to fall asleep?”) and frequency of interrupted sleep due to providing care to a spouse (“In the last month, how often did helping the patient cause your sleep to be interrupted?”). Responses to these questions used the same 5-point Likert scale, ranging from 1 (every night) to 5 (never), with higher scores suggesting fewer insomnia symptoms and better sleep. We calculated the average scores based on the two sleep items for care recipients (α = 0.68) and caregivers (α = 0.21). The scores proxied the level of insomnia symptoms, with higher scores suggesting less severe symptoms and better sleep.
Dementia and chronic health conditions
Care recipients were deemed to have probable dementia if they met any of the following criteria: (a) having ≤ 1.5 standard deviations (SDs) below mean in at least two domains of cognitive tests: memory (e.g., immediate and delayed 10-word recall), orientation (e.g., date, month, year, and day of the week, naming the President and Vice President), and executive function (e.g., clock drawing test), (b) having a score of 2 or higher on the AD8 Dementia Screening Interview (Galvin et al., 2005) administered to proxy respondents, or (c) having self- or proxy report of a diagnosis of dementia or Alzheimer’s disease (Kasper et al., 2013). Other chronic conditions were self- or proxy-reported, including physician-diagnosed conditions and/or serious difficulty hearing and seeing.
Predictors of between-dyad characteristics
We examined four contextual factors reported by either care recipients or the caregivers, including caregiving burden, neighborhood cohesion, care support, and relationship quality.
Four items measured care burden (α = 0.67) evaluating if (1) caregivers were exhausted when going to bed at night, (2) caregivers had more things to do than they could handle, (3) caregivers did not have time for themselves, and (4) as soon as a routine gets going, the patient’s needs change. Caregivers responded on a 3-point Likert scale ranging from 1 = very to 3 = not so much. We reverse-coded each item and calculated the scale score as the mean, with higher scores suggesting greater caregiving burden.
Three items measured neighborhood cohesion (α = 0.73), evaluating how community members (1) know each other very well, (2) are willing to help each other, and (3) can be trusted. Care recipient self- or proxy-reported on a 3-point Likert scale ranging from 1 = agree a lot to 3 = do not agree. We reverse-coded each item and calculated the scale score as the mean, with higher scores suggesting better neighborhood cohesion.
Care support was measured by the sum of seven items reported by caregivers (α = 0.54). These dichotomous items asked caregivers whether caregivers had friends or family to talk about important things in life and helped with their daily activities; helped care for a spouse; and in the last year, had gone to a support group for people who gave care; used any service, received any training or found financial help to help take care of the patient. We calculated the scale score as the sum, with higher scores suggesting better care support.
Four items measured relationship quality (α = 0.63), asking caregivers (1) how much they enjoyed being with the care recipient, how much the care recipient (2) argued with them, (3) appreciated what they did for them, and (4) got on their nerves. Caregivers responded on a 4-point Likert scale, ranging from 1 = a lot to 4 = not at all, coded with higher scores suggesting better relationship quality.
Predictors of within-dyad characteristics
We examined demographic characteristics, depressive symptoms, and positive emotions assessed for each member of the care dyads.
Demographic characteristics included care recipient and caregiver biological age, sex, education, and whether one was non-Hispanic White or non-Hispanic Black.
Symptoms of depression and anxiety were measured by the Patient Health Questionnaire-4 (Kroenke et al., 2009; α = 0.74 for care recipients and 0.70 for caregivers). It asked the frequency of four symptoms that occurred over the past month (1) had little interest or pleasure in doing things, (2) felt down, depressed, or hopeless, (3) felt nervous, anxious, or on edge, and (4) been unable to stop or control worrying. Responses ranged from not at all (= 1) to nearly every day (= 4), with higher scores suggesting more severe symptoms.
Positive emotions were measured by four items (α = 0.68 for care recipients and 0.64 for caregivers) asking both care recipients and their spousal caregivers how often they felt cheerful, bored, full of life, and upset over the last month (Freedman et al., 2014). Responses were scored on a 5-point Likert scale, ranging from 1 = every day to 5 = never. We reverse-coded the positive items and calculated the scale score as the mean, with higher scores suggesting higher positive emotions.
Analytical Strategy
Preliminary descriptive analyses were conducted for demographic characteristics and all study variables for care dyads. To examine H1, we fit empty multilevel models (i.e., without any predictors) with dyadic sleep outcomes measured for both care recipients and spousal caregivers living with dementia versus other chronic health conditions to examine intraclass correlations in dyadic sleep (Model 0). Then, we added predictors of between-dyad characteristics to the empty model to examine the second hypothesis. Specifically, to examine H2.1, we fit models with care burden as a predictor (Model 1); to examine H2.2, we added dementia in Model 1 as an additional predictor (Model 2); to examine H2.3, we added in Model 2 the following variables as other predictors: neighborhood cohesion, care support, and relationship quality (Model 3). To examine H3, we added in Model 3 the interaction term relationship quality × care burden (Model 4).
Further, we explored the actor and partner effects of within-dyad demographic characteristics (i.e., individual age, sex, education, race) and emotional well-being (i.e., individual symptoms of depression and anxiety, and positive emotions) on dyadic sleep outcomes. We implemented the APIM using a multilevel modeling framework in SAS (version 9.4), and Supplementary Figure 1 illustrates the general form of the model. These models allow testing simultaneously the effects of the care recipients’ characteristics on their own sleep outcomes and the effect of their characteristics on the caregiver sleep outcomes and vice versa. These models also account for the intercorrelation among care dyads for predictors and outcomes. All models were estimated using maximum likelihood estimation, allowing care recipients to be included even when caregiver information was missing. These individuals contributed information to the analysis of actor effects in the models. Separate models fit each combination of the six predictors and two outcomes resulting in 12 models. For these statistical tests, p < .05 was considered statistically significant.
Results
Participant Characteristics
Care recipient and caregiver characteristics are presented in Table 1. Care recipient and caregiver mean ages were 78.59 years (SD = 7.22, ranging from 65 to 99) and 75.77 years (SD = 8.82, ranging from 43 to 97), respectively. More than half of the care recipients were men. Both care recipients (77%) and caregivers (73%) were predominantly non-Hispanic White. Most dyads (72%) were non-Hispanic White, whereas 17% had both spouses being non-Hispanic Black. Most care recipients and spousal caregivers graduated from high school (19% vs 31%, respectively), followed by those who graduated from college and beyond (12% vs 29%, respectively). Among 462 spousal care dyads, 22% (n = 103) lived with dementia. Nine percent of the participants (n = 43) had proxy reports on behalf of them; among these proxy reports, 74% (n = 32) was because of dementia, and the rest were due to other illnesses or limitations such as cardiovascular problems, diabetes, cancer, speech or hearing impairment, or language barriers. About 93% (n = 429) of the care recipients lived in the community, and 7% (n = 33) in assisted living or other facilities. About half of the care recipients had trouble falling back asleep (51%), among whom 53% had spouses who were also having trouble falling back asleep. Slightly more than half of the care recipients also had difficulty initiating sleep (57%), among whom 28% had spouses who were also having disrupted sleep because of providing care.
Table 1.
Characteristics of Spousal Care Dyads (N = 462)
| Care recipient | Caregiver | |||||
|---|---|---|---|---|---|---|
| Mean or (Freq) | SD or (%) | Range | Mean or (Freq) | SD or (%) | Range | |
| Age (years) | 78.59 | 7.22 | 65–99 | 75.77 | 8.82 | 43–97 |
| Female | (196) | (42.42) | (269) | (58.23) | ||
| Race and Hispanic ethnicity | ||||||
| White, non-Hispanic | (355) | (76.84) | (335) | (72.51) | ||
| Black, non-Hispanic | (85) | (18.40) | (84) | (18.18) | ||
| Other (American Indian, Asian, Native Hawaiian, Pacific Islander, Other), non-Hispanic | (12) | (2.60) | (15) | (3.25) | ||
| Hispanic | (9) | (1.95) | (15) | (3.25) | ||
| More than one | (9) | (1.95) | ||||
| Don’t know and refused | (1) | (0.22) | (4) | (0.87) | ||
| Education levels (recoded) | 1.75 | 1.06 | 1–4 | 2.63 | 1.08 | 1–4 |
| Grade school (no diploma) | (275) | (59.52) | (82) | (17.75) | ||
| High school graduate (HS diploma or equivalent) | (86) | (18.61) | (141) | (30.52) | ||
| Vocational and some college | (44) | (9.52) | (106) | (22.94) | ||
| College graduate and professional degree | (57) | (12.34) | (133) | (28.79) | ||
| Chronic health conditions | ||||||
| Probable dementia | (103) | (22.34) | NA | |||
| Possible dementia | (55) | (11.93) | NA | |||
| Other chronic conditions | NA | NA | 0–1 | NA | NA | 0–1 |
| Heart attack | (57) | (12.36) | (81) | (17.69) | ||
| Heart disease | (130) | (28.20) | (62) | (13.57) | ||
| Hypertension | (363) | (78.57) | (288) | (62.75) | ||
| Arthritis | (329) | (71.21) | (248) | (54.03) | ||
| Osteoporosis | (110) | (23.86) | (97) | (21.23) | ||
| Diabetes | (177) | (38.31) | (116) | (25.33) | ||
| Lung disease | (106) | (22.94) | (82) | (17.86) | ||
| Cancer | (77) | (16.67) | (107) | (23.41) | ||
| Hearing impairment (used hearing aid) | (90) | (19.48) | (98) | (21.35) | ||
| Sight impairment (trouble seeing across the street) | (400) | (89.69) | (45) | (9.80) | ||
| Sleep last month | ||||||
| Trouble falling back asleep | 3.51 | 1.17 | 1–5 | 3.40 | 1.05 | 1–5 |
| Insomnia symptomsa | 3.46 | 1.08 | 1–5 | 3.75 | 0.77 | 1–5 |
| Care burdenb | NA | NA | NA | 1.59 | 0.53 | 1–3 |
| Care supportc (sum of seven binary indicators) | NA | NA | NA | 1.95 | 1.33 | 0–6 |
| Neighborhood cohesiond | 2.38 | 0.58 | 1–3 | NA | NA | |
| Relationship qualitye | NA | NA | NA | 3.29 | 0.51 | 1–4 |
| Symptoms of depression/anxiety last monthf | 1.63 | 0.67 | 1–4 | 1.56 | 0.59 | 1–4 |
| Positive emotions last monthg | 3.77 | 0.67 | 1–5 | 3.79 | 0.66 | 1–5 |
Notes: SD = standard deviation.
aInsomnia symptoms were measured by the mean of two items. For care recipients, these items took more than 30 min to fall asleep and the frequency of trouble falling back asleep; for caregivers, these items were interrupted sleep because of caregiving and frequency of trouble falling back asleep.
bCare burden was self-reported by caregivers only; response range was 1 = very much, 2 = somewhat, 3 = not so much; the scale score was the mean coded so that higher scores suggested greater burden.
cCare support was the sum of seven items (1 = yes, 0 = no), including whether caregivers have friends or family to talk about important things in your life; help with your daily activities, such as running errands, or helping you with things around the house; help care for care recipient; and in the last year, have gone to a support group for people who give care; used any service that took care of the care recipient so that you could take some time away from helping; received any training to help you take care of the care recipient; found financial help for the care recipient, including helping him/her apply for Medicaid.
dNeighborhood cohesion was self-reported by the care recipient only; response range was 1 = agree a lot, 2 = agree a little, 3 = do not agree; each item was reverse-coded and the scale score was the mean coded so that higher scores suggested better cohesion.
eRelationship quality item response range was 1 = a lot, 2 = some, 3 = a little, 4 = not at all; positive items were reverse-coded and the scale score was the mean coded so that higher scores suggested better quality.
fSymptoms of depression and anxiety response range was 1 = not at all, 2 = several days, 3 = more than half the days, 4 = nearly every day; the scale score was the mean coded so that higher scores suggested more depressive symptoms.
gPositive emotion items response range was 1 = every day, 2 = most days, 3 = some days, 4 = rarely, or 5 = never; positive items were reverse-coded and the scale score was the mean coded so that higher scores suggested better positive affect/mood.
Hypothesis Testing on Dyadic Sleep and Associated Between-Dyad Factors
For H1, the extent of raw intraclass correlations of trouble falling back asleep and insomnia symptoms was larger among care dyads living with dementia (i.e., 0.062 and 0.123, respectively) than those living with other chronic health conditions (i.e., 0.025 and 0.043, respectively). The findings (presented in Table 2) supported H1 and suggested that care recipient and caregiver sleep was more similar and correlated among dementia care dyads than those living with other chronic conditions.
Table 2.
Intraclass Correlation in Dyadic Sleep Outcomes (Model 0 for H1)
| Frequency in trouble falling back asleep | Insomnia symptoms | |
|---|---|---|
| Dementia care dyads | 0.062 | 0.123 |
| Nondementia care dyads | 0.025 | 0.043 |
| All care dyads | 0.034 | 0.062 |
Notes: Frequency in trouble falling back asleep was measured by the single item “In the last month, on nights when you woke up before you wanted to get up, how often did you have trouble falling back asleep?” for care recipients and their spousal caregivers. Insomnia symptoms were measured by two items in addition to the aforementioned single item; for care recipients, they were “In the last month, how often did it take more than 30 min to fall asleep?” and “In the last month, on nights when you woke up before you wanted to get up, how often did you have trouble falling back asleep?”; for spousal caregivers, they were “In the last month, how often did it take more than 30 min to fall asleep?” and “In the last month, on nights when you woke up before you wanted to get up, how often did you have trouble falling back asleep?”
Main-Effect Associations With Dyadic Sleep
For H2, findings from Models 1–3 in Table 3 suggested that higher care burden was associated with poorer dyadic sleep, in terms of more frequent trouble falling back asleep (β = −0.292, standard error [SE] = 0.069, p < .001) and more insomnia symptoms (β = −0.334, SE = 0.058, p < .001) for both care recipients and caregivers within care dyads. However, dementia status and other between-dyad characteristics (i.e., neighborhood cohesion, care support, and relationship quality) did not have any main-effect associations with dyadic sleep outcomes (Models 2 and 3).
Table 3.
Dyadic-Level Characteristics and Associations With Dyadic Sleep Outcomes (Models 1–4 for H2–3)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Est (SE) | Est (SE) | Est (SE) | Est (SE) | |
| Frequency of trouble falling back asleep | ||||
| Fixed effect | ||||
| Intercept | 3.918 (0.115)*** | 3.927 (0.115)*** | 3.264 (0.335)*** | 2.026 (0.787)** |
| Caregiving burden | −0.292 (0.069)*** | −0.310 (0.070)*** | −0.283 (0.073)*** | 0.457 (0.432) |
| Dementia | 0.100 (0.090) | 0.107 (0.091) | 0.093 (0.091) | |
| Neighborhood cohesion | 0.085 (0.064) | 0.088 (0.064) | ||
| Care support | 0.021 (0.028) | 0.025 (0.028) | ||
| Relationship quality | 0.114 (0.077) | 0.492 (0.231)* | ||
| Care burden × relationship quality | −0.232 (0.133)† | |||
| Random effect | ||||
| Compound symmetry | 0.018 (0.057) | 0.017 (0.057) | 0.017 (0.057) | 0.014 (0.057) |
| Residual | 1.203 (0.080)*** | 1.205 (0.080)*** | 1.200 (0.080)*** | 1.200 (0.080)*** |
| −2 log likelihood | 2,785.4 | 2,782.4 | 2,775.4 | 2,774.6 |
| AIC; BIC | 2,789.4; 2,797.6 | 2,786.4; 2,794.7 | 2,779.4; 2,787.6 | 2,778.6; 2,786.8 |
| Insomnia symptoms | ||||
| Fixed effect | ||||
| Intercept | 4.132 (0.098)*** | 4.140 (0.098)*** | 3.693 (0.285)*** | 3.075 (0.670)*** |
| Caregiving burden | −0.334 (0.058)*** | −0.356 (0.060)*** | −0.328 (0.062)*** | 0.042 (0.368) |
| Dementia | 0.122 (0.077) | 0.129 (0.077) | 0.122 (0.077) | |
| Neighborhood cohesion | 0.086 (0.054) | 0.087 (0.054) | ||
| Care support | −0.006 (0.024) | −0.005 (0.024) | ||
| Relationship quality | 0.064 (0.065) | 0.253 (0.196) | ||
| Care burden × relationship quality | −0.116 (0.113) | |||
| Random effect | ||||
| Compound symmetry | 0.025 (0.041) | 0.023 (0.041) | 0.021 (0.041) | 0.021 (0.041) |
| Residual | 0.844 (0.056)*** | 0.846 (0.056)*** | 0.848 (0.056)*** | 0.849 (0.056)*** |
| −2 log likelihood | 2,477.5 | 2,470.8 | 2,474.6 | 2,476.1 |
| AIC; BIC | 2,481.5; 2,489.7 | 2,478.0; 2,486.3 | 2,478.6; 2,486.9 | 2,480.1; 2,488.4 |
Notes: All predictors in Models 1–4 were measured at the dyadic level, reported by either care recipients or spousal caregivers. Caregivers reported caregiving burden, care support, and relationship quality. Dementia diagnosis was based on the care recipients only; care recipients reported neighborhood cohesion. AIC = Akaike information criterion; BIC = Bayesian information criterion; EST = estimate; SE = standard error.
*p < .05. **p < .01. ***p < .001. †p < .08.
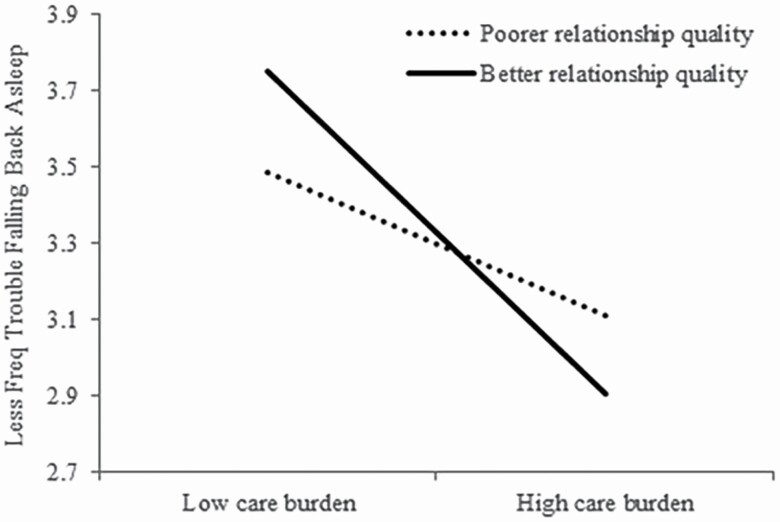
For H3, the interaction term between relationship quality and care burden in Model 4 was marginally significant. Specifically, relationship quality marginally moderated the association between caregiving burden and dyadic frequency of trouble falling back asleep (β = −0.232, SE = 0.133, p = .083). As illustrated in Figure 2, better relationship quality was protective against less frequent trouble falling back asleep among care dyads but only when the care burden was low; when the care burden was high, better relationship quality was associated with more frequent trouble falling back asleep dyadically.
Figure 2.
Better relationship quality marginally moderated the care burden–trouble falling back asleep association among care dyads.
The Actor and Partner Effects of the Within-Dyad Characteristics on Dyadic Sleep
We built multilevel APIM to explore how within-dyad and individual demographic characteristics, symptoms of depression and anxiety, and positive emotions were associated with dyadic sleep outcomes. Models were created sequentially by adding one of the following predictors (measured for both care recipients and the spousal caregivers) into Model 4: biological age, sex, education, race, depressive symptoms, and finally, positive affect (Supplementary Figure 1).
Findings from these APIM suggested that biological age had an actor effect (but no partner effect), so that older age was associated with more frequent trouble falling back asleep (β = −0.019, SE = 0.006, p = .001) as well as having more insomnia symptoms (β = −0.010, SE = 0.005, p = .036) for individual care recipients and caregivers themselves. Sex, education, or race were not significantly associated with any dyadic sleep outcomes. Further, symptoms of depression and anxiety had both actor and partner effects on the two dyadic sleep outcomes. Specifically, worse symptoms of depression and anxiety were associated with more frequent trouble falling back asleep and more insomnia symptoms for oneself (β = −0.465, SE = 0.060, p < .001 and β = −0.460, SE = 0.050, p = .001, respectively) as well as for their spousal caregivers (β = −0.127, SE = 0.060, p < .001 and β = −0.105, SE = 0.050, p = .038, respectively). Finally, higher positive emotions had an actor effect (but no partner effect), such that more positive emotion was associated with less frequent trouble falling back asleep (β = 0.211, SE = 0.072, p = .003) as well as having fewer insomnia symptoms (β = 0.277, SE = 0.059, p < .001) for care recipients and caregivers themselves.
Discussion
Utilizing a national sample, we examined the critical sleep characteristics of older adults with chronic health conditions and their spousal caregivers. Specifically, we examined the contextual factors of dyadic sleep outcomes at the individual, dyadic, social, and societal levels to inform future evidence-based interventions designed to promote sleep health among care dyads living with chronic health conditions. Our findings suggested that sleep health was more correlated among dementia care dyads than those living with other chronic health conditions. Further, higher care burden was associated with poorer dyadic sleep for all care partners in general. Better relationship quality seemed to benefit dyadic sleep, especially when the care burden was low. Additionally, while older age and higher levels of positive emotions were associated with poorer sleep for oneself, more symptoms of depression and anxiety were associated with poorer sleep for oneself, and one’s care partner.
Dyadic Sleep, and Associated Between- and Within-Dyad Factors
Our findings confirm that the extent of correlation of sleep outcomes within the caregiving dyad was an essential characteristic of dyadic sleep, but may not necessarily be associated with individual sleep outcomes (e.g., dementia status was not significantly associated with average dyadic sleep). However, higher care burden was associated with poorer dyadic sleep outcomes. Higher caregiver-reported burden suggests increased perceived subjective stress and perhaps more care needs of the care recipient. Future study is necessary to better understand how dyadic spousal interactions affect sleep health.
For example, it is not yet clear why and how symptoms of depression and anxiety had a greater influence on dyadic sleep outcomes than positive emotions and affected spouses’ sleep in addition to one’s own. Although it is beyond the scope of the current study to examine whether poor sleep also affected worse symptoms of depression and anxiety for dyads, the findings suggest that addressing depression and anxiety symptoms of both the care recipient and their caregiver may improve sleep health among care dyads.
We did not find any main-effect associations, and relationship quality only marginally moderated the care burden–sleep association so that a better relationship seemed to be protective against more frequent trouble falling back asleep, especially when the care burden was low; when the care burden was high, however, better relationship quality was associated with poorer dyadic sleep. Better relationship quality may protect caregivers against daily distress in response to the care recipient behavior problems (Chunga et al., 2020) and lower role captivity and overload across time (Bangerter et al., 2019). Though we used standard items to assess relationship quality, this information was only available from caregivers. Future studies evaluating relationship quality from both members of the dyad will help clarify whether perspective-taking and empathy are relevant constructs to consider.
Lastly, we did not find significant relationships between neighborhood cohesion or care support and dyadic sleep. It is known that spousal caregivers tend to be the sole caregivers but are reluctant to seek and accept help and support even when they need it (Fee et al., 2020; Ornstein et al., 2019). It is possible that the measures in the current study emphasized the available social support in the community, whereas prior studies emphasized the neighborhood quality and disadvantage as a stressor (Hale et al., 2013).
Limitations and Conclusion
This study has several limitations. Relying on cross-sectional data, we cannot address the causal relationship between dyadic sleep and the contextual factors examined in the study. Sleep data were collected based on subjective reports and did not capture all aspects of clinical insomnia disorder. Further, the retrospective reporting used for key study questions may have resulted in some recall bias. In addition, while our study only examined spousal care dyads, those in different relationships, such as adult–child caregivers, may have different sleep health behaviors. These interesting patterns of preliminary findings add to the sleep literature and raise important questions about how individual characteristics may affect care partners’ sleep health. Although the study utilized a national sample, several measures had relatively low Cronbach’s alpha, and the measure on insomnia symptoms did not fully capture clinical insomnia in this population. Further, we did not apply survey weights in our models. These unweighted findings can inform dyadic sleep characteristics for older adults living with chronic conditions and their caregivers but are not fully representative of the population. Finally, due to health limitations, a small percentage (less than 10%) of care recipients had proxy- rather than self-reports; given that most of the proxy data (74%) was within dyads with dementia, interclass correlation coefficients may be inflated. Due to these limitations, caution should be used in generalizing the findings.
To our knowledge, this is the first study exploring dyadic sleep health among spousal care dyads living with chronic conditions using national survey data from the United States. Sleep is a shared health behavior among older care partners and our findings suggest that care burden and poor relationship quality are relevant contextual factors. Additionally, while positive emotion was only related to one’s own better sleep, depressive symptoms were associated with poorer sleep for both oneself and the care partner. Effective caregiver support should address the mental health needs of both members of the care dyad and ultimately the family relationship. An increased focus on families may improve the sustainability of aging in place with a chronic health condition.
Supplementary Material
Acknowledgments
A part of this work was accepted for presentation at the Gerontological Society of America Annual Meeting, November 2021.
Contributor Information
Yin Liu, Department of Human Development and Family Studies, Utah State University, Logan, Utah, USA.
Yeonsu Song, School of Nursing, University of California Los Angeles, California, Los Angeles, USA.
Florence U Johnson, Department of Systems, Populations, and Leadership, School of Nursing, University of Michigan, Ann Arbor, Michigan, USA.
Lianlian Lei, Department of Psychiatry, Michigan Medicine, University of Michigan, Ann Arbor, Michigan, USA.
Seung-won Emily Choi, Department of Sociology, Anthropology, and Social Work, Texas Tech University, Lubbock, Texas, USA.
Toni C Antonucci, Department of Psychology, University of Michigan, Ann Arbor, Michigan, USA.
Sheria G Robinson-Lane, Department of Systems, Populations, and Leadership, School of Nursing, University of Michigan, Ann Arbor, Michigan, USA.
Funding
This work was supported by the Michigan Center for Contextual Factors in Alzheimer’s Disease (MCCFAD) [P30 AG059300], funded by the National Institute on Aging of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The National Health and Aging Trends Study was sponsored by the National Institute on Aging (NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. The National Study of Caregiving was funded by the NIA (R01AG054004). Additional National Institute on Aging grants supported this work (K01AG065420 to S. G. Robinson-Lane; K23AG055668 to Y. Song).
Conflict of Interest
None declared.
Author Contributions
All authors (Y. Liu, Y. Song, F. U. Johnson, L. Lei, S. E. Choi, T. C. Antonucci, and S. G. Robinson-Lane) contributed equally to the study design, data interpretation, and preparation of the manuscript. Y. Liu performed the statistical analysis.
References
- Alhasan, D. M., Gaston, S. A., Jackson, W. B., 2nd, Williams, P. C., Kawachi, I., & Jackson, C. L. (2020). Neighborhood social cohesion and sleep health by age, sex/gender, and race/ethnicity in the United States. Internaltional Journal of Environmental Research and Public Health, 17(24), 1–19. doi: 10.3390/ijerph17249475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bangerter, L. R., Liu, Y., & Zarit, S. H. (2019). Longitudinal trajectories of subjective care stressors: The role of personal, dyadic, and family resources. Aging & Mental Health, 23(2), 255–262. doi: 10.1080/13607863.2017.1402292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings, M. E., Hale, L., & Johnson, D. A. (2020). Physical and social environment relationship with sleep health and disorders. Chest, 157(5), 1304–1312. doi: 10.1016/j.chest.2019.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanni, E., Maestri, M., Tognoni, G., Fabbrini, M., Nucciarone, B., Manca, M. L., Gori, S., Iudice, A., & Murri, L. (2005). Daytime sleepiness in mild and moderate Alzheimer’s disease and its relationship with cognitive impairment. Journal of Sleep Research, 14(3), 311–317. doi: 10.1111/j.1365-2869.2005.00462.x [DOI] [PubMed] [Google Scholar]
- Chen, J. H. (2017). Couples’ sleep and psychological distress: A dyadic perspective. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(1), 30–39. doi: 10.1093/geronb/gbx001 [DOI] [PubMed] [Google Scholar]
- Chunga, R. E., Kim, K., Liu, Y., & Zarit, S. H. (2020). Family caregivers’ distress responses to daily behavioral and psychological symptoms of dementia: The moderating role of relationship quality. International Journal of Geriatric Psychiatry. Advance online publication. doi: 10.1002/gps.5482 [DOI] [PubMed] [Google Scholar]
- Creese, J., Bédard, M., Brazil, K., & Chambers, L. (2008). Sleep disturbances in spousal caregivers of individuals with Alzheimer’s disease. International Psychogeriatrics, 20(1), 149–161. doi: 10.1017/S1041610207005339 [DOI] [PubMed] [Google Scholar]
- Elsey, T., Keller, P. S., & El-Sheikh, M. (2019). The role of couple sleep concordance in sleep quality: Attachment as a moderator of associations. Journal of Sleep Research, 28(5), e12825. doi: 10.1111/jsr.12825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fee, A., McIlfatrick, S., & Ryan, A. (2020). Examining the support needs of older male spousal caregivers of people with a long-term condition: A systematic review of the literature. International Journal of Older People Nursing, 15(3), e12318. doi: 10.1111/opn.12318 [DOI] [PubMed] [Google Scholar]
- Freedman, V. A., & Kasper, J. D. (2019). Cohort profile: The National Health and Aging Trends Study (NHATS). International Journal of Epidemiology, 48(4), 1044–1045g. doi: 10.1093/ije/dyz109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Kasper, J. D., Spillman, B. C., Agree, E. M., Mor, V., Wallace, R. B., & Wolf, D. A. (2014). Behavioral adaptation and late-life disability: A new spectrum for assessing public health impacts. American Journal of Public Health, 104(2), e88–e94. doi: 10.2105/ajph.2013.301687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Skehan, M. E., Hu, M., Wolff, J., & Kasper, J. D.(2019). National Study of Caregiving I–III user guide. https://www.nhats.org/sites/default/files/2021-01/NSOC%20I-III%20USER%20GUIDE%20Version%205_Final_2_0.pdf [Google Scholar]
- Galvin, J. E., Roe, C. M., Powlishta, K. K., Coats, M. A., Muich, S. J., Grant, E., Miller, J. P., Storandt, M., & Morris, J. C. (2005). The AD8: A brief informant interview to detect dementia. Neurology, 65(4), 559–564. doi: 10.1212/01.wnl.0000172958.95282.2a [DOI] [PubMed] [Google Scholar]
- Gaugler, J. E., Yu, F., Krichbaum, K., & Wyman, J. F. (2009). Predictors of nursing home admission for persons with dementia. Medical Care, 47(2), 191–198. doi: 10.1097/MLR.0b013e31818457ce [DOI] [PubMed] [Google Scholar]
- Gibson, R. H., Gander, P. H., & Jones, L. M. (2014). Understanding the sleep problems of people with dementia and their family caregivers. Dementia (London), 13(3), 350–365. doi: 10.1177/1471301212473884 [DOI] [PubMed] [Google Scholar]
- Grandner, M. A. (2020). Sleep, health, and society. Sleep Medicine Clinics, 15(2), 319–340. doi: 10.1016/j.jsmc.2020.02.017 [DOI] [PubMed] [Google Scholar]
- Grandner, M. A., Williams, N. J., Knutson, K. L., Roberts, D., & Jean-Louis, G. (2016). Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Medicine, 18, 7–18. doi: 10.1016/j.sleep.2015.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn, H. E., Buysse, D. J., Hasler, B. P., Begley, A., & Troxel, W. M. (2015). Sleep concordance in couples is associated with relationship characteristics. Sleep, 38(6), 933–939. doi: 10.5665/sleep.4744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn, H. E., Lee, S., Eberhardt, K. R., Buxton, O. M., & Troxel, W. M. (2021). Nightly sleep–wake concordance and daily marital interactions. Sleep Health, 7(2), 266–272. doi: 10.1016/j.sleh.2020.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale, L., Hill, T. D., Friedman, E., Javier Nieto, F., Galvao, L. W., Engelman, C. D., Malecki, K. M. C., & Peppard, P. E. (2013). Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Social Science & Medicine, 79, 16–22. doi: 10.1016/j.socscimed.2012.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasler, B. P., & Troxel, W. M. (2010). Couples’ nighttime sleep efficiency and concordance: Evidence for bidirectional associations with daytime relationship functioning. Psychosomatic Medicine, 72(8), 794–801. doi: 10.1097/PSY.0b013e3181ecd08a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper, J. D., & Freedman, V. A. (2020). National Health and Aging Trends Study user guide: Rounds 1–9 final release. https://nhats.org/sites/default/files/2021-04/NHATS_User_Guide_R9_Final_Release_0.pdf [Google Scholar]
- Kasper, J. D., Freedman, V. A., & Spillman, B. (2013). Classification of persons by dementia status in the National Health and Aging Trends Study. https://nhatspubdemo.westat.com/scripts/documents/NHATS_Dementia_Technical_Paper_5_Jul2013.pdf [Google Scholar]
- Kroenke, K., Spitzer, R. L., Williams, J. B., & Löwe, B. (2009). An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics, 50(6), 613–621. doi: 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- Lea Steadman, P., Tremont, G., & Duncan Davis, J. (2007). Premorbid relationship satisfaction and caregiver burden in dementia caregivers. Journal of Geriatric Psychiatry and Neurology, 20(2), 115–119. doi: 10.1177/0891988706298624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, D., Morgan, K., & Lindesay, J. (2007). Effect of institutional respite care on the sleep of people with dementia and their primary caregivers. Journal of the American Geriatrics Society, 55(2), 252–258. doi: 10.1111/j.1532-5415.2007.01036.x [DOI] [PubMed] [Google Scholar]
- Liang, J., Aranda, M. P., & Lloyd, D. A. (2020). Association between role overload and sleep disturbance among dementia caregivers: The impact of social support and social engagement. Journal of Aging and Health, 32(10), 1345–1354. doi: 10.1177/0898264320926062 [DOI] [PubMed] [Google Scholar]
- Liu, Y., Leggett, A. N., Kim, K., Polenick, C. A., McCurry, S. M., & Zarit, S. H. (2021). Daily sleep, well-being, and adult day services use among dementia care dyads. Aging & Mental Health. Advance online publication. doi: 10.1080/13607863.2021.1998354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran, M., Lynch, C. A., Walsh, C., Coen, R., Coakley, D., & Lawlor, B. A. (2005). Sleep disturbance in mild to moderate Alzheimer’s disease. Sleep Medicine, 6(4), 347–352. doi: 10.1016/j.sleep.2004.12.005 [DOI] [PubMed] [Google Scholar]
- Norton, M. C., Piercy, K. W., Rabins, P. V., Green, R. C., Breitner, J. C. S., Østbye, T., Corcoran, C., Welsh-Bohmer, K. A., Lyketsos, C. G., & Tschanz, J. T. (2009). Caregiver–recipient closeness and symptom progression in Alzheimer disease. The Cache County Dementia Progression Study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(5), 560–568. doi: 10.1093/geronb/gbp052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornstein, K. A., Wolff, J. L., Bollens-Lund, E., Rahman, O.-K., & Kelley, A. S. (2019). Spousal caregivers are caregiving alone in the last years of life. Health Affairs, 38(6), 964–972. doi: 10.1377/hlthaff.2019.00087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. doi: 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Peng, H. L., Lorenz, R. A., & Chang, Y. P. (2019). Factors associated with sleep in family caregivers of individuals with dementia. Perspectives in Psychiatric Care, 55(1), 95–102. doi: 10.1111/ppc.12307 [DOI] [PubMed] [Google Scholar]
- Pinquart, M., & Sörensen, S. (2007). Correlates of physical health of informal caregivers: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62(2), 126–137. doi: 10.1093/geronb/62.2.p126 [DOI] [PubMed] [Google Scholar]
- Pinquart, M., & Sörensen, S. (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26(1), 1–14. doi: 10.1037/a0021863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, K. M., Buckwalter, K. C., & Reed, D. (2005). Predictors of use of services among dementia caregivers. Western Journal of Nursing Research, 27(2), 126–140. doi: 10.1177/0193945904272453 [DOI] [PubMed] [Google Scholar]
- Song, Y., McCurry, S. M., Fung, C. H., Josephson, K. R., Teng, E., Irwin, M. R., Alessi, C. A., & Martin, J. L. (2018). Sleep and caregiving experiences among caregivers of veterans in an adult day health care program: A pilot study. Clinical Gerontologist, 41(2), 167–171. doi: 10.1080/07317115.2017.1365795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tractenberg, R. E., Singer, C. M., & Kaye, J. A. (2006). Characterizing sleep problems in persons with Alzheimer’s disease and normal elderly. Journal of Sleep Research, 15(1), 97–103. doi: 10.1111/j.1365-2869.2006.00499.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troxel, W. M., Robles, T. F., Hall, M., & Buysse, D. J. (2007). Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Med Reviews, 11(5), 389–404. doi: 10.1016/j.smrv.2007.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschanz, J. T., Piercy, K., Corcoran, C. D., Fauth, E., Norton, M. C., Rabins, P. V., Tschanz, B., Deberard, M. S., Snyder, C., Smith, C., Lee, L., & Lyketsos, C. G. (2013). Caregiver coping strategies predict cognitive and functional decline in dementia: The Cache County Dementia Progression Study. The American Journal of Geriatric Psychiatry, 21(1), 57–66. doi: 10.1016/j.jagp.2012.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe, K., Fox, P., Newcomer, R., Sands, L., Lindquist, K., Dane, K., & Covinsky, K. E. (2002). Patient and caregiver characteristics and nursing home placement in patients with dementia. Journal of American Medical Association, 287(16), 2090–2097. doi: 10.1001/jama.287.16.2090 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.