Abstract
Background
Endometriosis is a prevalent gynaecological condition, significantly affecting women's lives. Clinical presentations may vary from absence of symptoms to complaints of chronic pelvic pain, most notably dysmenorrhoea. The management of pain in endometriosis is currently inadequate. Acupuncture has been studied in gynaecological disorders but its effectiveness for pain in endometriosis is uncertain.
Objectives
To determine the effectiveness and safety of acupuncture for pain in endometriosis.
Search methods
We searched the Cochrane Menstrual Disorders and Subfertility Group (MSDG) Specialised Register of controlled trials, Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library), MEDLINE, EMBASE, CINAHL, AMED, PsycINFO, CNKI and TCMDS (from inception to 2010) and reference lists of retrieved articles.
Selection criteria
Randomised single or double‐blind controlled trials enrolling women of reproductive age with a laparoscopically confirmed diagnosis of endometriosis and comparing acupuncture (body, scalp or auricular) to either placebo or sham, no treatment, conventional therapies or Chinese herbal medicine.
Data collection and analysis
Three authors independently assessed risk of bias and extracted data; we contacted study authors for additional information. Meta‐analyses were not performed as only one study was included. The primary outcome measure was decrease in pain from endometriosis. Secondary outcome measures included improvement in quality of life scores, pregnancy rate, adverse effects and rate of endometriosis recurrence.
Main results
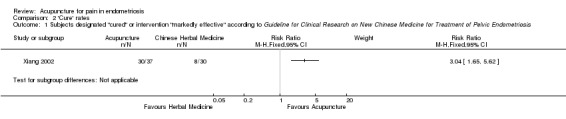
Twenty‐four studies were identified that involved acupuncture for endometriosis; however only one trial, enrolling 67 participants, met all the inclusion criteria. The single included trial defined pain scores and cure rates according to the Guideline for Clinical Research on New Chinese Medicine. Dysmenorrhoea scores were lower in the acupuncture group (mean difference ‐4.81 points, 95% confidence interval ‐6.25 to ‐3.37, P < 0.00001) using the 15‐point Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis scale. The total effective rate ('cured', 'significantly effective' or 'effective') for auricular acupuncture and Chinese herbal medicine was 91.9% and 60%, respectively (risk ratio 3.04, 95% confidence interval 1.65 to 5.62, P = 0.0004). The improvement rate did not differ significantly between auricular acupuncture and Chinese herbal medicine for cases of mild to moderate dysmenorrhoea, whereas auricular acupuncture did significantly reduce pain in cases of severe dysmenorrhoea.
Data were not available for secondary outcomes measures.
Authors' conclusions
The evidence to support the effectiveness of acupuncture for pain in endometriosis is limited, based on the results of only a single study that was included in this review. This review highlights the necessity for developing future studies that are well‐designed, double‐blinded, randomised controlled trials that assess various types of acupuncture in comparison to conventional therapies.
Keywords: Female; Humans; Acupuncture, Ear; Acupuncture, Ear/methods; Drugs, Chinese Herbal; Drugs, Chinese Herbal/therapeutic use; Dysmenorrhea; Dysmenorrhea/therapy; Endometriosis; Endometriosis/complications; Pelvic Pain; Pelvic Pain/etiology; Pelvic Pain/therapy; Randomized Controlled Trials as Topic
Plain language summary
Acupuncture for pain in endometriosis
Endometriosis is a gynaecological disease that causes chronic pelvic pain, most notably painful menstruation, as the most common complaint. Acupuncture is frequently used to treat both pain and various gynaecological conditions. This review examined the effectiveness of acupuncture for reducing pain in endometriosis; however only one study met our inclusion criteria. The data from the included study, involving 67 women, indicated that ear acupuncture is more effective compared to Chinese herbal medicine for reducing menstrual pain. The study did not report whether participants suffered any side effects from their treatments. Larger, well‐designed studies comparing acupuncture with conventional therapies are necessary to confirm these results.
Background
Description of the condition
Endometriosis is a chronic, estrogen‐dependent disorder (Frankiewicz 2000) that occurs when endometrial tissue grows abnormally and adheres outside the uterus, most often it is found in the abdominal or pelvic cavity (Bajaj 2003). The most common symptom is chronic pelvic pain, notably dysmenorrhoea (painful menstruation) (Xiang 2002), though symptoms may also include dyspareunia (painful intercourse), dyschezia (pain on defecation) and subfertility (Farquhar 2007).
Endometriosis is the primary cause of infertility and affects approximately 20% to 50% of infertile women (Frankiewicz 2000; Wu 2007). Normal hormonal fluctuations induce the shedding of the endometrial lining at the end of each menstrual cycle. In endometriosis this hormonal change also triggers the abnormal growth of endometrial tissue to break down and bleed, at sites such as the ovaries, fallopian tubes, uterine ligaments, bladder, and less commonly the thoracic cavity. Although the pain mechanism perpetuating endometriosis has not been fully elucidated, it is thought that the pain arises because endometrial tissue adhesions outside of the uterus cannot be eliminated as menstrual discharge and the surrounding sites become inflamed (Frankiewicz 2000).
Endometriosis is difficult to diagnose because the pain symptoms that are experienced are not unique to endometriosis (Gao 2006) and physicians may discredit women's reports of pain (Denny 2004). A woman's pain experience may also not correlate with the extent of damage to the pelvic cavity (Farquhar 2000; Prentice 2001). There are a lack of truly reliable, non‐invasive procedures for diagnosis of this disease and currently the gold standard is diagnosis by laparoscopic visual inspection (Farquhar 2007; Frankiewicz 2000). However, a negative histology does not rule out endometriosis (Kennedy 2005; Stratton 2006). The true prevalence of endometriosis is unknown, though it is estimated to occur in 10% of women of reproductive age (Jackson 2006). Endometriosis is present in 40% to 60% of women who present with dysmenorrhoea as their primary pain complaint (Farquhar 2000).
Conventional treatments do not provide long‐term pain relief and their adverse effects may be intolerable for some women. These therapies range from analgesics, hormonal therapies that decrease menses, inhibit ovarian function and cause atrophy of ectopic endometrial cells (Farquhar 2007) to more invasive surgical interventions. All pharmacotherapeutic interventions have side effects that may reduce women's compliance (Gao 2006; Prentice 2001). Although non‐steroidal anti‐inflammatory drug (NSAID) therapy is first‐line therapy, evidence supporting its effectiveness is inconclusive (Allen 2005) and its long‐term safety profile is poor (Prentice 2001). Oral contraceptive pills (OCPs) may be more tolerable for long‐term use (Davis 2007) however side effects range from mild nausea, bloating and altered mood to rarer, more severe events such as cardiac complications or stroke (Proctor 2002). Gonadotropin‐releasing hormone (GnRH) induces menopausal symptoms and increases bone loss (Farmer 2003; Olive 2008). The five‐year disease recurrence rate is 70% for NSAIDs or OCPs and 33% to 50% for GnRH (Gao 2006). While danazol is highly effective (Jackson 2006), it causes unpleasant androgenic side effects (Selak 2007) such as acne, weight gain and hirsutism (Hughes 2007). Surgical removal of endometriosis, which may include hysterectomy, is not always curative and drug therapy may still be required following surgery (Shakiba 2008). The five‐year disease recurrence rate is 40% to 50% following laparoscopy and 5% to 10% after partial or complete hysterectomy (Gao 2006).
In conclusion, although drug therapies and surgical interventions may manage the pain symptoms of endometriosis, women must weigh therapeutic benefit against unpleasant side effects and recognise that all treatments have a risk of disease recurrence.
Description of the intervention
Acupuncture is one of the main forms of traditional Chinese medicine (TCM) and has been practised within the Chinese healthcare system for thousands of years (Qiu 1993). Since the late 20th century, the demand for acupuncture has been growing steadily in many Western nations (Hamilton 2008; Harkin 2007; Hope‐Allan 2004; Schmineke 2008). In China, acupuncture is currently used in public hospitals for the treatment of endometriosis (Xiang 2002).
There are several different forms of acupuncture, including body acupuncture, electroacupuncture, auricular acupuncture and scalp acupuncture (Zhang 2008).
Body acupuncture is defined as the needling of acupuncture points on the human body along the traditional meridians, excluding cranial and ear points (Lan 1997).
Electroacupuncture (EA) is the stimulation of acupuncture points using an electrical current (Qiu 1993).
Scalp acupuncture is the parallel insertion of needles along the scalp, for treating neurological conditions (Qiu 1993).
Auricular acupuncture is a microsystem within TCM and involves stimulation of acupuncture points in the ear (Qiu 1993).
According to TCM theory there is a natural pattern of vital energy (Qi) throughout the body; a disruption in this flow of energy indicates disease and pain (Maciocia 1998). Although endometriosis was not recorded in the classical text as a defined entity, the symptoms are treated under the categories of dysmenorrhoea, irregular menstruation, abdominal mass, and infertility (Xia 2000; Yu 1998). The key pathology of endometriosis is impeded flow of Qi and blood, resulting in obstruction of the Chong and Ren channels (Li 2001). It is also believed that a constitutional deficiency is the underlying pathology (Liao 2008). The principle behind the application of acupuncture is to rectify imbalance and unblock the obstruction in the related channels.
How the intervention might work
The mechanism of action of acupuncture in the treatment of endometriosis remains largely unclear. However, emerging literature demonstrates acupuncture‐mediated analgesia and alteration of specific hormone levels.
The influence of acupuncture on the body's naturally occurring pain mediators (endogenous opioids such as ß‐endorphin) has been established since the 1970s (Lin 2008 a). Cabýoglu et al (Cabýoglu 2006) summarised the findings from several studies which propose that increases of endogenous opioids and the neurotransmitters serotonin and dopamine cause analgesia, sedation and recovery of motor function. It is also reported that acupuncture may induce visceral and somatic signals that are transmitted to the central nervous system to induce an anti‐inflammatory signal through both humoral and neural mechanisms (Cho 2006). Lin et al (Lin 2008 b) found that the therapeutic effect of acupuncture for dysmenorrhoea may be through its influence on prostaglandin F2α (PGF2α) levels in menstrual fluid. Some researchers hypothesise that acupuncture may have a role in ovulation induction and fertility treatment through normalizing the hypothalamic‐pituitary ovarian axis (Cai 1997; Chen 2007). Studies of auricular acupuncture suggest that its main therapeutic actions may be through elevation of plasma ß‐endorphin levels and coordination of uterine activity (Xiang 2005). Finally, it is postulated that acupuncture may have immunomodulating effects and lipolithic effects on metabolism (Cabýoglu 2006).
Acupuncture appears to have a favourable safety profile (MacPherson 2007). It may be a treatment option for women who do not satisfactorily respond to conventional interventions or who seek an alternative for managing pain from endometriosis.
Why it is important to do this review
It is reported that endometriosis is the third leading reason for gynaecological hospitalisations and hysterectomy in the United States (Frankiewicz 2000). Endometriosis adversely affects women's ability to work, family relationships and sense of self worth. The management of pain in women with endometriosis is currently inadequate. Surgical intervention may be curative; however it may not always be a desirable treatment option due to its invasive nature and associated risks. Acupuncture may have a role in managing pain and other symptoms associated with endometriosis without the adverse event profile associated with conventional treatments.
This review aims to analyse randomised controlled trials (RCTs) of acupuncture to establish its efficacy and safety in the treatment of women suffering from pain in association with endometriosis. In addition, it provides evidence‐based information for all healthcare practitioners recommending acupuncture treatment for women whose endometriosis condition is not effectively managed by current clinical management methods.
Objectives
To assess the effectiveness and safety of acupuncture in the treatment of women with pain from endometriosis.
Methods
Criteria for considering studies for this review
Types of studies
Studies were included if they were single or double‐blind RCTs that compared treatment using acupuncture with placebo (sham acupuncture) or biomedical therapy for the reduction of pain from endometriosis.
Studies containing data on one or more of the secondary outcome variables were also included in this review. Quasi‐randomised trials were excluded.
Types of participants
Women of reproductive age with a diagnosis of endometriosis confirmed laparoscopically. Participant exclusion criteria included primary dysmenorrhoea (the absence of an identifiable pathological condition) or asymptomatic endometriosis.
Types of interventions
The acupuncture treatment technique for needle location and stimulation varies greatly and for this reason we felt it was appropriate, and more true to the practice of acupuncture, to assess interventions separately. Therefore, types of interventions included body acupuncture with needle insertion at traditional acupuncture points or insertion at non‐traditional points, also called 'Ashi' or tender areas; scalp or auricular acupuncture; and electroacupuncture. The source of stimulation could be the hand, moxibustion as a warming needle, or electrical stimulation. We excluded acupuncture studies that involved non‐insertive techniques, laser acupuncture, acupressure, point injection, blood letting tap pricking, or cupping on pricked superficial blood vessels. We excluded trials only comparing different acupuncture treatments.
We excluded Japanese style acupuncture since the needle technique and diagnostic evaluation are quite distinct in Japanese and Chinese styles of acupuncture.
The control intervention could be placebo, also called sham acupuncture (with the use of a non‐penetrating needle) (Streitberger 1998), or non‐traditional acupoints that were not tender to touch and were located in the vicinity of traditional acupoints (Zhang 2008), conventional biomedical treatment, or no treatment at all.
Specific interventions considered were as follows.
Acupuncture (body, scalp, auricular) versus placebo or sham acupuncture.
Acupuncture (body, scalp, auricular) versus no treatment.
Acupuncture (body, scalp, auricular) plus conventional therapies (e.g. OCPs, surgical intervention) versus conventional therapies (e.g. OCPs, surgical intervention).
Acupuncture (body, scalp, auricular) with stimulation (hand, electronic recurrence, moxa) versus placebo or sham acupuncture with stimulation (hand, electronic recurrence, moxa).
Acupuncture (body, scalp, auricular) with stimulation (hand, electronic recurrence, moxa) versus no treatment.
Acupuncture (body, scalp, auricular) with stimulation (hand, electronic recurrence, moxa) plus conventional therapies (e.g. OCPs, surgical intervention) versus conventional therapies (e.g. OCPs, surgical intervention).
Types of outcome measures
Primary outcomes
Decrease in pain caused by endometriosis
The following validated pain scales were considered acceptable for assessing either pain intensity or pain relief:
visual analogue scale (VAS);
four‐point categorical scale with wording comparable to no relief, some relief, much relief, complete relief; or none, mild, moderate, severe;
other validated numeric rating scales;
other validated dichotomous measures.
During the development of the review, we found that the Guideline for Clinical Research on New Chinese Medicine for the Treatment of Pelvic Endometriosis (Ministry of Public Health 1993) was adapted by many Chinese studies. The Guideline provides not only diagnostic criteria but also outcome measurements such as dysmenorrhoea scores and cure rate. See the Included studies section for details.
Secondary outcomes
Improvement in quality of life scores using validated quality of life instruments including the Short Form (SF36) General Health Questionnaire (Medical Outcomes Trust 1994), the Sickness Impact Profile (Deyo 1983), and the Nottingham Health Profile (Hunt 1986)
Pregnancy rate
Adverse events (incidence, severity, and type of side effects)
Rate of endometriosis recurrence
Search methods for identification of studies
Electronic searches
The Cochrane Menstrual Disorders and Subfertility Group (MDSG) search strategy was adopted. Reports which described (or might describe) randomised controlled trials of acupuncture in the treatment of endometriosis were obtained using the following strategy.
(1) The MDSG Specialised Register of controlled trials was searched for any trials with endometriosis in the title, abstract, or keyword sections.
(2) The following electronic databases were searched (from inception to 2010): Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library), MEDLINE, EMBASE, CINAHL, AMED, and PsycINFO.
(3) Two electronic Chinese databases were examined (1990 to 2010): China Knowledge Infrastructure (CNKI), and Traditional Chinese Medicine Database System (TCMDS).
For a detailed search string see (Appendix 1).
Searching other resources
We searched bibliographies from retrieved studies, narrative reviews, and meta‐analyses to identify further relevant articles. Additional searches included conference abstracts on the ISI Web of Knowledge.
Data collection and analysis
Selection of studies
XZ implemented the search strategy using the Chinese language databases. Translation of Chinese papers was undertaken by an additional researcher and trial selection was performed by three authors (XZ, KH, EM). Two review authors (KH, EM) independently assessed potential studies and selected eligible studies identified by the English language databases. Any disagreements were settled by discussion.
Data extraction and management
XZ, EM and KH independently participated in data extraction using a pre‐developed Microsoft Excel data extraction form (Appendix 2) to assess study characteristics including methods, participants, interventions, and outcomes. XZ, EM and KH independently evaluated the methodological quality of the selected study to assess the extent to which trial design, data collection, and statistical analysis reduced or avoided bias. Data were independently entered into RevMan 5 by the individual authors to prevent transcription errors.
Assessment of risk of bias in included studies
XZ, EM and KH independently critically assessed the risk of bias of the included study in this review using a domain‐based evaluation that includes the following domains: sequence generation (randomisation), quality of allocation concealment (in accordance with the guidelines established by the Menstrual Disorders and Subfertility Group), blinding, incomplete outcome data, and selective outcome reporting. The review authors' assessments for each domain were entered into a 'Risk of bias' table in which: 'Yes' indicates a low risk of bias, 'No' indicates a high risk of bias, and 'Unclear' indicates either a lack of information or uncertainty regarding the potential for bias (Higgins 2008).
We contacted all study contact authors by mail or e‐mail to confirm that trials were randomised and met our inclusion criteria. If we were unable to contact the authors, the study was excluded unless randomisation could otherwise be confirmed.
Measures of treatment effect
Dichotomous data
We intended to use discrete events such as preference, numbers of participants reporting 50% pain relief or better, or the number of participants reporting adverse events to calculate the absolute risk reduction (ARR, also known as risk difference) using RevMan 5 software (Cook 1995; McQuay 1998). If a statistically significant ARR existed between interventions, numbers needed to treat to benefit (NNT) or harm (NNH) were to be derived. Dichotomous outcomes were also presented in terms of both raw numbers and percentages of participants in each study arm who benefited from therapy or suffered adverse events. However, only one study was included, rendering meta‐analysis irrelevant.
Continuous data
Meta‐analysis was not undertaken since there was only one study included.
Unit of analysis issues
This was not applicable.
Dealing with missing data
We contacted the study authors by email and mail to obtain any missing participant data, and we recorded the date of contact. If we were unable to obtain missing data, analyses were based on participant populations in which outcomes were reported. Discrepancies between the number of participants enrolled and the number in whom outcomes were reported were to be noted in the 'Characteristics of included studies' table. Where studies reported statistics based on intention to treat (ITT) or modified ITT populations, available case analyses were to be performed (Higgins 2008). However, the single included study reported data on all enrolled participants.
Assessment of heterogeneity
Assessment of heterogeneity was not performed since there was only one included study.
Assessment of reporting biases
We made no attempt to assess reporting bias (other than selective outcome reporting).
Data synthesis
No data synthesis was performed, since there was only one included study.
Subgroup analysis and investigation of heterogeneity
We did not perform subgroup analysis since there was only one included study; however the authors of the included study performed subanalysis, which is described in the 'Results' section. It was not possible to ascertain from the manuscript whether the investigators’ subanalysis was part of their protocol.
Sensitivity analysis
No sensitivity analysis was performed since there was only one included study.
Results
Description of studies
See: 'Characteristics of included studies' table and 'Characteristics of excluded studies' table.
Results of the search
Our search produced two results from the MDSG Specialised Register, 16 from CENTRAL, 17 from MEDLINE, 33 from EMBASE, 9 from CINAHL, 18 from AMED, 5 from PsycINFO, 11 from CNKI and 3 from TCMDS. After individually reviewing all retrieved abstracts we identified 24 potentially relevant studies.
Included studies
One RCT with parallel groups (Xiang 2002) met all inclusion criteria for this review. The trial was conducted in China and enrolled 67 participants, of which 37 were randomly assigned to an auricular acupuncture group and 30 were assigned to receive Chinese herbal medicine. Treatments were administered once every other day, four times for each menstrual point, with three menstrual cycles constituting a therapeutic course.
Participants
The included study clearly stated inclusion criteria. Xiang et al (Xiang 2002) enrolled participants (ranging from 22 to 47 years of age) from Guangdong Provincial Hospital of Traditional Chinese Medicine, China, who met diagnostic criteria for endometriosis as defined in the Guideline for Clinical Research on New Chinese Medicine for the Treatment of Pelvic Endometriosis (Ministry of Public Health 1993). Diagnostic criteria were as follows: (1) progressive dysmenorrhoea; (2) progressive lower abdominal or back pain during menstruation; (3) progressive cyclic rectal irritation symptoms; (4) nodules with tenderness in the posterior fornix, uterosacral ligament or uterine isthmus; (5) adnexal masses adhered with nodular feeling under the envelope, Fallopian tubes unobstructed or partly obstructed; (6) the size of the adnexal mass changes significantly before and after menstruation.
Clinical diagnosis is made for women who satisfy one criterion in (1) to (3) and one in (4) to (6), that is one of (1), (2) or (3) plus one of (4), (5) or (6).
Endometriosis was confirmed by laparoscopic surgery and surgical pathology in all 67 participants. The number of participants in both groups was comparable for each of the three grades of dysmenorrhoea (mild, moderate or severe pain). Of the 37 women in the auricular acupuncture group, 16, 12 and 9 suffered mild, moderate and severe dysmenorrhoea, respectively. Of the 30 women treated with Chinese herbal medicine, 12, 10 and 8 were classified with mild, moderate and severe dysmenorrhoea, respectively. It was reported that ages and pain grades were not statistically different between groups. Eight additional healthy women were recruited as a control group for an outcome measuring ß‐endorphin levels (results not presented in this review). The study did not present details of exclusion criteria.
Interventions
Auricular acupuncture was performed in the study (Xiang 2002). The study assessed the use of five auricular acupuncture points: Ting Zhong (centre of cymba auriculae), Pi Zhi Xia (hypo‐cortex), Nei Fen Mi (endocrine), Jiao Gan (sympathetic) and Nei Sheng Zhi Qi (internal genitals). These points are traditionally used for alleviating pain and targeting the reproductive system.
Comparison and control groups
The comparison group received a Chinese herbal medicine prescription for increasing blood circulation and alleviating stasis according to the framework of TCM. The following Chinese medicinals were used: Dan Shen Radix Salviae Miltiorrhizae, ChiShao Radix Paeoniae Rubra, San Leng Rhizoma Sparganii, E Zhu Rhizoma Curcumae, Zhi Qiao Fructus Aurantii and Xiang Fu Rhizoma Cyperi. An additional acupuncture control group, for assessing ß‐endorphin levels, was comprised of eight healthy women. No placebo or sham acupuncture group was included.
Outcome measures
The measurements of outcome from the one included study were made based on the Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis (Ministry of Public Health 1993). Dysmenorrhoea scores, as defined in the guideline, were assessed pre‐ and post‐intervention. Severity was calculated as follows: severe case, scores ranged from 13 to15; moderate case, scores ranged from 8 to12; mild case, scores ranged from 5 to 7 (for detail, see Table 1).
1. Dysmenorrhea scores.
| Dysmenorhea symptoms | Score |
| Pain in the lower abdomen prior to and during menstruation | 5 |
| Unbearable abdominal pain | 1 |
| Pronounced abdominal pain | 0.5 |
| Restless | 1 |
| Pass out (loss of consciousness) | 2 |
| Pale complexion | 0.5 |
| Perspiration | 1 |
| Cool extremities | 1 |
| Required bed resting | 1 |
| Interfering with daily activity | 1 |
| No relief from common used analgesic | 1 |
| Relief from common used analgesic | 0.5 |
| Lower back pain | 0.5 |
| Nausea, vomiting | 0.5 |
| Distension and sore in the anus | 1 |
| Pain within a day | 1 |
| Pain occurs on each additional day | 0.5 |
Pain was also considered with other relevant symptoms as a combined outcome measure, with patients assessed as 'cured', 'substantial improvement', 'effective' or 'no improvement' as follows.
Cured clinically: all symptoms disappeared; abdominal masses or nodules disappeared. Pregnancy occurred within three years of clinical intervention.
Substantial improvement: symptoms almost disappeared, abdominal masses or nodules reduced (comparison made during the same period of menstrual cycle via internal (vaginal) examination and ultrasound). Pregnancy occurred, although symptoms persisted.
Effective: symptoms reduced; no enlarged abdominal masses or nodules, or slightly reduced (comparison made during the same period of menstrual cycle via internal (vaginal) examination and ultrasound). No relapse after cessation of the clinical intervention.
No improvement: no change of abdominal pain or other symptoms.
Other outcomes included in the study were changes in blood ß‐endorphin levels (not reported in this review).
Excluded studies
Twenty‐three studies failed to meet the inclusion criteria for our review based on the following results.
One RCT evaluated acupuncture versus drug therapy (danazol); however the pain conditions were not solely related to endometriosis (Yan 2008).
One study did not assess a pain outcome (Qu 2007).
One study did not include endometriosis among pain conditions (Lim 2009).
One study included surgical intervention and not acupuncture (Vercellini 2009).
One study evaluated the effectiveness of moxibustion alone and point injection rather than moxibustion as an adjunctive therapy with acupuncture (Liu 2003).
One study was not properly randomised. It employed the sequence of hospital admission for assignment of interventions (Sun 2006).
Two studies involved evaluating the effectiveness of a combination of acupuncture plus Chinese herbal medicine versus drug therapy (Fu 2005; Xia 2006).
Four studies assessed Japanese‐style acupuncture (Ahn 2009; Conboy 2008; Schnyer 2008; Wayne 2008).
Four studies compared different methods of acupuncture and lacked a placebo or biomedical group (Jin 2009; Liu 2009; Sun 2007; Zhen 2009).
Seven studies were non‐randomised (Danielsson 2001; Fugh‐Berman 2003; Green 2010; Highfield 2006; Lundeberg 2008; Sanfilippo 2008; Van Steirteghem 2009).
For more information pertaining to these studies refer to 'Characteristics of excluded studies'.
Risk of bias in included studies
For summary, see Figure 1.
1.
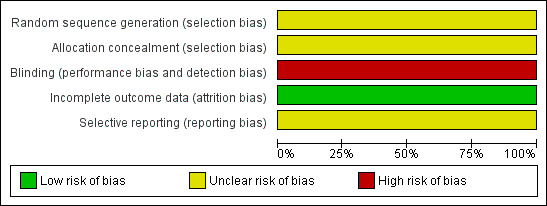
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
The included trial (Xiang 2002) was described as randomised but no details were given. Attempts at allocation concealment were not described.
Blinding
In the single included trial, no mention of blinding was made and it appears that patients and investigators were aware of assigned treatments.
Incomplete outcome data
In the single included study it appears that data were presented for all participants in both groups, for all outcomes.
Selective reporting
It appears that data were presented for every outcome assessed. However, the outcomes assessed were not introduced until the results section, so it was not possible to ascertain whether other outcomes had initially been considered or measured.
Effects of interventions
Decrease in pain caused by endometriosis
Pain scores ‐ auricular acupuncture versus Chinese herbal medicine
The included study (Xiang 2002) found that dysmenorrhoea scores were significantly lower in the acupuncture group (mean difference ‐4.81 points, 95% confidence interval (CI) ‐6.25 to ‐3.37, P < 0.00001, n = 67) (Figure 2) using the 15‐point Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis scale (as defined in Table 1, maximum score = 15). Additionally, comparison of pre‐ and post‐treatment scores within groups demonstrated significantly lower scores in the acupuncture group (12.19 ± 2.42 pre‐treatment versus 5.53 ± 2.17 post‐treatment, P < 0.05), whereas Chinese herbal medicine did not have a statistically significant effect (11.22 ± 3.11 pre‐treatment versus 10.34 ± 3.51 post‐treatment, P > 0.05).
2.
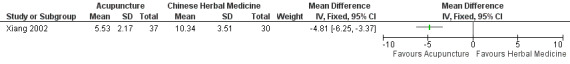
Forest plot of comparison: 1 Dysmenorrhoea scores, outcome: 1.1 Scores post‐therapy.
Pain and other associated overall symptoms ‐ auricular acupuncture versus Chinese herbal medicine
When assessing overall improvement, as defined by the Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis (Ministry of Public Health 1993) (see Included studies), auricular acupuncture showed a statistically significant increase in the rate of those cured and with significant improvement (81.1% versus 26.7%, risk ratio 3.04 (95% CI 1.65 to 5.62), P = 0.0004) (Figure 3) in comparison to the standardized preparation of Chinese herbal medicine. Among individuals who received auricular acupuncture 11 of the 37 participants were cured, whereas 3 of the 30 participants treated with Chinese herbal medicine were cured. The total effective rate (cured, significantly effective or effective) for auricular acupuncture and Chinese herbal medicine was 91.9% and 60%, respectively (Xiang 2002).
3.
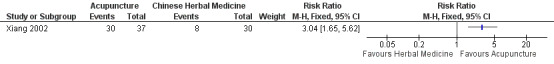
Forest plot of comparison: 1 "Cure" rates, outcome: 1.1 Subjects designated "cured" or intervention "significantly effective" according to Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis.
Improvements were also evaluated by the investigators with respect to subgroups within each group, based on initial pain grades of dysmenorrhoea. Results showed a lack of significant difference in therapeutic effectiveness between auricular acupuncture and Chinese herbal medicine for cases of mild to moderate dysmenorrhoea (acupuncture group: n = 27 effective, n = 1 ineffective; Chinese medicine group: n = 18 effective, n = 4 ineffective). However, auricular acupuncture compared to Chinese herbal medicine statistically reduced pain in cases of severe dysmenorrhoea (acupuncture group: n = 7 effective, n = 2 ineffective; Chinese medicine group: n = 11 effective, n = 1 ineffective). It was not possible to ascertain from the manuscript whether the subanalysis was included in the study protocol or was performed post hoc.
Improved quality of life ‐ auricular acupuncture versus Chinese herbal medicine
Data were not available for this outcome.
Pregnancy rate ‐ auricular acupuncture versus Chinese herbal medicine
Although pregnancy was measured as part of the composite outcome 'cure rate', it was not clear whether the women classified under 'effective' or 'no improvement' did or did not become pregnant; therefore it was not possible to establish the pregnancy rate in each group.
Adverse effects ‐ auricular acupuncture versus Chinese herbal medicine
Data were not reported for this outcome.
Rate of endometriosis recurrence ‐ auricular acupuncture versus Chinese Herbal medicine
Based on study of the Guidelines (Ministry of Public Health 1993), we assumed that the number of patients who had no improvement might suffer from recurrence (acupuncture group: 3 cases versus Chinese herbal medicine:12 cases).
Data were not available on other comparisons or groups.
Discussion
Summary of main results
Pain reduction
One trial (Xiang 2002) evaluated the therapeutic effect of auricular acupuncture compared to standard Chinese herbal medicine and demonstrated a reduction in pain post‐intervention in those receiving acupuncture but not in those receiving Chinese herbal medicine.
Pain and other associated overall improvement
As defined by the Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis (Ministry of Public Health 1993), significantly more patients in the acupuncture group showed improvement versus those receiving Chinese herbal medicine. Subanalysis (probably post hoc) demonstrated that statistical significance only occurred when comparing patients with severe dysmenorrhoea pre‐intervention and not in patients with mild or moderate pain. It is not clear from this small sample whether acupuncture is genuinely more effective in those with more severe symptoms or whether the difference is simply due to inadequate numbers of women for each comparison.
Overall completeness and applicability of evidence
The purpose of this review was to evaluate the effectiveness and safety of acupuncture for the treatment of pain from endometriosis. While acupuncture has been used for thousands of years to ameliorate various pain conditions, there has been a lack of rigorous trials to support the use of acupuncture for pain from endometriosis.
This review found one RCT to support the therapeutic effectiveness of auricular acupuncture compared to Chinese herbal medicine (Xiang 2002). The study's findings suggest that acupuncture may be an effective analgesic intervention in women with endometriosis. However, the study did not include a placebo control so it is not possible to rule out therapeutic effectiveness due to a placebo response, or to ascertain whether placebo effects may have varied by intervention, that is, women may have had different expectations of efficacy depending on the intervention they received. We are not aware of evidence regarding placebo rates for acupuncture or Chinese herbal medicine in endometriosis studies, but indirect evidence from the study of dysmenorrhoea indicates that the placebo response can be as high as 35% to 44% (Dawood 1991; Dawood 2006) and it has been suggested that placebo response may be greater in individuals receiving sham acupuncture versus those receiving an 'inert' oral pill for pain (Kaptchuk 2006; Linde 2010). It is recommended that studies assessing whether acupuncture needles have any specific effect should include a control arm where participants receive either 'penetrating sham' or 'non‐penetrating sham' procedures (White 2001).
In conclusion, larger studies including comparisons with either placebo or other conventional therapies are necessary before definitive conclusions may be extrapolated to the general public.
Quality of the evidence
Methodological risk of bias
The trial included in this review (Xiang 2002) was methodologically weak. Participants were randomised based on their diagnosis of endometriosis over a two‐year period; however it appears that neither participants nor researchers were blind to the therapeutic intervention.
The small sample size of only 67 participants was an additional weakness in this trial. It is estimated that 40 patients per arm are required to demonstrate statistical superiority of an effective intervention over placebo. However, to reach a clinically credible estimate of efficacy, several hundred patients are required (Moore 1998). Sample size is important since large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects (Moore 1998). While the study enrolled a sufficient number of participants to demonstrate a significant difference within groups for the primary outcome (dysmenorrhoea scores), it was inadequately powered to demonstrate a difference in cure rates between groups when rates were subanalyzed with respect to initial severity of dysmenorrhoea.
While measurement outcomes were defined according to the Guideline for Clinical Research on New Chinese Drugs for Treatment of Pelvic Endometriosis (Ministry of Public Health 1993), the study lacked a detailed explanation for the manner in which they were determined. Under these guidelines 'cured clinically' indicated the disappearance of symptoms, masses and nodules and pregnancy occurring within three years following clinical intervention. However, researchers (Xiang 2002) did not indicate whether cases cured of endometriosis were re‐evaluated by laparoscopic visual inspection, which is currently the gold standard (Frankiewicz 2000; Stratton 2006). Endometriosis may present asymptomatically and therefore the absence of dysmenorrhoea does not imply a cured case (Jackson 2006).
Authors' conclusions
Implications for practice.
There is not enough evidence to support the effectiveness of acupuncture for pain in endometriosis based on the results of the single RCT included in this review. While the results of this trial (Xiang 2002) did show that auricular acupuncture decreased pain from endometriosis in comparison to Chinese herbal medicine, the overall low‐quality of methodology makes broad implications for practice difficult to determine.
Auricular acupuncture is but one facet of acupuncture therapy and the effectiveness of body acupuncture, most commonly used in practice, has not been evaluated. There is currently a lack of high quality trials to determine the effectiveness of acupuncture versus conventional therapies or placebo.
Implications for research.
The trial included in this review indicated the effectiveness of acupuncture in treating pain from endometriosis in comparison to Chinese herbal medicine (Xiang 2002); however no conclusive recommendation can be drawn from one small study. There is a need for more high quality trials, enrolling large numbers of women, before a definitive conclusion can be made. This review highlights the necessity of developing future studies that are well‐designed, double‐blinded, randomised controlled trials that assess various types of acupuncture in comparison to conventional treatments and placebo.
History
Protocol first published: Issue 3, 2009 Review first published: Issue 9, 2011
| Date | Event | Description |
|---|---|---|
| 14 April 2008 | Amended | Converted to new review format. |
| 20 December 2005 | New citation required and major changes | Substantive amendment |
Acknowledgements
Menstrual Disorders and Subfertility Group for its editorial guidance and assistance.
Guining Jiang from University of Western Sydney for providing the English translation of Chinese papers.
Appendices
Appendix 1. Electronic Searches
AMED (Allied and Complementary Medicine)
1 exp Endometriosis/ (22)
2 adenomyosis.tw. (5)
3 Endometriosis.tw. (57)
4 pelvic pain.tw. (84)
5 dyspareunia.tw. (18)
6 dyschezia.tw. (0)
7 (pain$ adj1 defecat$).tw. (1)
8 (pain$ adj1 intercourse).tw. (1)
9 or/1‐8 (155)
10 exp Acupuncture/ (3110)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (5488)
12 acupressure$.tw. (298)
13 Acupuncture.tw. (7508)
14 (electroacupuncture or electro‐acupuncture).tw. (769)
15 meridian$.tw. (480)
16 mox$.tw. (456)
17 (shiatsu or tui na).tw. (241)
18 needling.tw. (623)
19 shu.tw. (68)
20 acup$ point$.tw. (406)
21 or/10‐20 (8508)
22 21 and 9 (15)
23 from 22 keep 1‐15 (15)
Cochrane Central Register of Controlled Trials
1 exp Endometriosis/ (361)
2 adenomyosis.tw. (21)
3 Endometriosis.tw. (611)
4 pelvic pain.tw. (301)
5 dyspareunia.tw. (140)
6 dyschezia.tw. (5)
7 (pain$ adj1 defecat$).tw. (39)
8 (pain$ adj1 intercourse).tw. (8)
9 or/1‐8 (1004)
10 exp Acupuncture/ (77)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (1315)
12 acupressure$.tw. (173)
13 Acupuncture.tw. (2869)
14 (electroacupuncture or electro‐acupuncture).tw. (383)
15 meridian$.tw. (206)
16 mox$.tw. (713)
17 (shiatsu or tui na).tw. (3)
18 needling.tw. (340)
19 shu.tw. (38)
20 acup$ point$.tw. (314)
21 or/10‐20 (4173)
22 21 and 9 (11)
23 from 22 keep 1‐11 (11)
CINAHL ‐ Cumulative Index to Nursing & Allied Health Literature
1 exp Endometriosis/ (643)
2 adenomyosis.tw. (35)
3 Endometriosis.tw. (526)
4 pelvic pain.tw. (530)
5 dyspareunia.tw. (164)
6 dyschezia.tw. (2)
7 (pain$ adj1 defecat$).tw. (10)
8 (pain$ adj1 intercourse).tw. (14)
9 or/1‐8 (1317)
10 exp Acupuncture/ (4698)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (5058)
12 acupressure$.tw. (242)
13 Acupuncture.tw. (3350)
14 (electroacupuncture or electro‐acupuncture).tw. (190)
15 meridian$.tw. (173)
16 mox$.tw. (253)
17 (shiatsu or tui na).tw. (82)
18 needling.tw. (215)
19 shu.tw. (26)
20 acup$ point$.tw. (225)
21 or/10‐20 (5808)
22 21 and 9 (26)
23 exp clinical trials/ (67221)
24 Clinical trial.pt. (35632)
25 (clinic$ adj trial$1).tw. (15341)
26 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$3 or mask$3)).tw. (9013)
27 Randomi?ed control$ trial$.tw. (13067)
28 Random assignment/ (19726)
29 Random$ allocat$.tw. (1376)
30 Placebo$.tw. (12433)
31 Placebos/ (4799)
32 Quantitative studies/ (4384)
33 Allocat$ random$.tw. (78)
34 or/23‐33 (92479)
35 22 and 34 (9)
36 from 35 keep 1‐9 (9)
EMBASE
1 exp Endometriosis/ (10676)
2 adenomyosis.tw. (997)
3 Endometriosis.tw. (9227)
4 pelvic pain.tw. (3513)
5 dyspareunia.tw. (1473)
6 dyschezia.tw. (81)
7 (pain$ adj1 defecat$).tw. (81)
8 (pain$ adj1 intercourse).tw. (52)
9 or/1‐8 (16057)
10 exp Acupuncture/ (12529)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (12558)
12 acupressure$.tw. (263)
13 Acupuncture.tw. (7795)
14 (electroacupuncture or electro‐acupuncture).tw. (1354)
15 meridian$.tw. (2166)
16 mox$.tw. (4993)
17 (shiatsu or tui na).tw. (40)
18 needling.tw. (692)
19 shu.tw. (729)
20 acup$ point$.tw. (852)
21 or/10‐20 (20380)
22 21 and 9 (100)
23 Clinical Trial/ (520486)
24 Randomized Controlled Trial/ (162855)
25 exp randomisation/ (26302)
26 Single Blind Procedure/ (7803)
27 Double Blind Procedure/ (70488)
28 Crossover Procedure/ (20698)
29 Placebo/ (119870)
30 Randomi?ed controlled trial$.tw. (31151)
31 Rct.tw. (2543)
32 random allocation.tw. (631)
33 randomly allocated.tw. (9977)
34 allocated randomly.tw. (1336)
35 (allocated adj2 random).tw. (558)
36 Single blind$.tw. (7314)
37 Double blind$.tw. (83363)
38 ((treble or triple) adj blind$).tw. (137)
39 placebo$.tw. (107847)
40 prospective study/ (78123)
41 or/23‐40 (684779)
42 case study/ (5785)
43 case report.tw. (116332)
44 abstract report/ or letter/ (483164)
45 or/42‐44 (603087)
46 41 not 45 (660891)
47 22 and 46 (40)
48 limit 47 to yr="2007 ‐ 2008" (18)
49 from 48 keep 1‐18 (18)
Ovid MEDLINE
1 exp Endometriosis/ (13078)
2 adenomyosis.tw. (1165)
3 Endometriosis.tw. (11216)
4 pelvic pain.tw. (3613)
5 dyspareunia.tw. (1500)
6 dyschezia.tw. (107)
7 (pain$ adj1 defecat$).tw. (88)
8 (pain$ adj1 intercourse).tw. (60)
9 or/1‐8 (19094)
10 exp Acupuncture/ (758)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (11341)
12 acupressure$.tw. (321)
13 Acupuncture.tw. (8965)
14 (electroacupuncture or electro‐acupuncture).tw. (1730)
15 meridian$.tw. (2643)
16 mox$.tw. (4513)
17 (shiatsu or tui na).tw. (51)
18 needling.tw. (777)
19 shu.tw. (317)
20 acup$ point$.tw. (752)
21 or/10‐20 (19860)
22 21 and 9 (42)
23 randomised controlled trial.pt. (268396)
24 controlled clinical trial.pt. (80624)
25 (randomised or randomised).ab. (210408)
26 placebo.ab. (110956)
27 drug therapy.fs. (1313713)
28 randomly.ab. (127995)
29 trial.ab. (183698)
30 groups.ab. (885980)
31 or/23‐30 (2380643)
32 (animals not (humans and animals)).sh. (3285079)
33 31 not 32 (2019976)
34 33 and 22 (18)
35 from 34 keep 1‐18 (18)
PsycINFO
1 exp Endometriosis/ (0)
2 adenomyosis.tw. (4)
3 Endometriosis.tw. (93)
4 pelvic pain.tw. (248)
5 dyspareunia.tw. (264)
6 dyschezia.tw. (3)
7 (pain$ adj1 defecat$).tw. (6)
8 (pain$ adj1 intercourse).tw. (34)
9 or/1‐8 (595)
10 exp Acupuncture/ (669)
11 exp acupuncture therapy/ or exp acupressure/ or exp acupuncture analgesia/ or exp acupuncture, ear/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/ (0)
12 acupressure$.tw. (59)
13 Acupuncture.tw. (921)
14 (electroacupuncture or electro‐acupuncture).tw. (135)
15 meridian$.tw. (549)
16 mox$.tw. (80)
17 (shiatsu or tui na).tw. (11)
18 needling.tw. (62)
19 shu.tw. (91)
20 acup$ point$.tw. (73)
21 or/10‐20 (1728)
22 21 and 9 (4)
23 from 22 keep 1‐4
China Knowledge Infrastructure (CNKI) and Traditional Chinese Medicine Database System (TCMDS). The following terms in Pingyin were used:
1. Zi Gong Nei Mu Yi Wei Zheng (endometriosis)
2. Tong Jing (period pain)
3. Ji Fa Xing Tong Jing (secondary dysmenorrhoea)
4. 1 or 2 or 3
5. Zheng Jiu (acupuncture and moxibustion)
6. Ti Zheng (body acupuncture)
7. Er Zheng (auricular acupuncture)
8. Tou Zheng (scalp acupuncture)
9. Dian Zheng (electro‐acupuncture)
10. Lin Chuang (clinical)
11. Lin Chuang Yun Yong (clinical application)
12. Lin Chuang Zhi Liao (clinical treatment)
13. Lin Chuang Yan Jiu (clinical research)
14. Lin Chuang Guan Cha (clinical observation)
15. Lin Chuang Dui Zhao (clinical comparison)
16. 5 or 6 or 7 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16.
17. 4 and 16.
Appendix 2. Data extraction form
General study data
First author
Publication year
Study unique ID number
Title
Journal
Criteria for including in study
Was the study a RCT?
Was the study double or single blinded?
Is pain outcome assessed?
Final decision: if all replies are 'yes' ‐ include; any 'no' ‐ exclude and STOP here
Characteristics of included studies
Risk of bias assessment
Was the allocation sequence adequately generated (randomisation)? No ‐ N, Yes ‐ Y, and Unclear ‐ U
Was the allocation adequately concealed? No‐ N, Yes‐ Y and Unclear‐ U
Was the knowledge of the allocated intervention adequately prevented during the study (blinding)? No ‐ N, Yes ‐ Y, and Unclear ‐ U
Were incomplete outcome data adequately addressed? No ‐ N, Yes ‐ Y, and Unclear ‐ U
Are reports of the study free of suggestion of selective outcome reporting? No ‐ N, Yes ‐ Y, and Unclear ‐ U
Methodology
Study duration
Inclusion criteria
Exclusion criteria
Control groups (placebo/sham acupuncture or active): list type of acupuncture intervention and nature of placebo
Total N randomised (entire study)
Number completing study: acupuncture, control groups
Total number analyzed (ITT): acupuncture, control groups
Participants
Age of acupuncture group: mean ± SD
Age placebo group: mean ± SD
Duration of endometriosis (number of years since first diagnosed)
Stage of endometriosis (Stage 1, 2, 3, or 4).
Comorbid pathophysiology: secondary pains due to endometriosis; psychological condition
Interventions
Number of acupuncture treatments
Type of acupuncture: body, scalp, auricular or electroacupuncture
Control intervention: sham at acupoints, true acupuncture at non‐traditional acupoints, biomedical therapy, or no acupuncture
Outcome measures evaluated
Pain INTENSITY scale used: categorical, numerical rating scale or VAS?
Categorical scale: specify categories
Numerical scale: details (0 to 5, 0 to 10, 0 to 100) and anchors
VAS scale: details (0 to 5, 0 to 10, 0 to 100) and anchors
Pain RELIEF scale: number of categories used and details.
Baseline CATEGORICAL pain intensity score ACUPUNCTURE: mean ± SD (or specify if other measure of average and spread)
Baseline NUMERICAL pain intensity score ACUPUNCTURE: mean ± SD (or specify if other measure of average and spread)
Baseline VAS pain intensity score ACUPUNCTURE: mean ± SD (or specify if other measure of average and spread).
Baseline CATEGORICAL pain intensity score CONTROL groups: mean ± SD (or specify if other measure of average and spread)
Baseline NUMERICAL pain intensity score CONTROL groups: mean ± SD (or specify if other measure of average and spread)
Baseline VAS pain intensity score CONTROL groups: mean ± SD (or specify if other measure of average and spread).
# of patients > 50% pain relief (n/N): acupuncture
# of patients > 50% pain relief (n/N): control groups
Other pain outcome (e.g. global evaluation, time to onset of analgesia). Specify and detail for all groups
Adverse events
Number of patients reporting ANY adverse event: acupuncture group (n/N)
Number of patients reporting SPECIFIC adverse events (list each): acupuncture group (n/N)
If scale used for intensity of specific side effect(s), specify: acupuncture group
Number of patients reporting ANY adverse event: control group (n/N)
Number of patients reporting SPECIFIC adverse events (list each): control group (n/N)
If scale used for intensity of specific side effect(s), specify: control group (n/N)
Reason for dropouts: acupuncture group
Reason for dropouts: control group
Comments
Data and analyses
Comparison 1. Dysmenorrhoea scores.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Scores post‐therapy | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only |
1.1. Analysis.
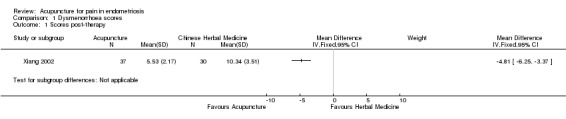
Comparison 1 Dysmenorrhoea scores, Outcome 1 Scores post‐therapy.
Comparison 2. 'Cure' rates.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjects designated "cured" or intervention "markedly effective" according to Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
2.1. Analysis.
Comparison 2 'Cure' rates, Outcome 1 Subjects designated "cured" or intervention "markedly effective" according to Guideline for Clinical Research on New Chinese Medicine for Treatment of Pelvic Endometriosis.
Characteristics of studies
Characteristics of included studies [ordered by year of study]
Xiang 2002.
| Methods | Randomised, active‐controlled study comparing auricular acupuncture with Chinese herbal medicine over the course of 3 menstrual periods. Method of blinding (if any) not reported. | |
| Participants | Chinese study. 67 women ages 22‐47 years. Diagnostic criteria met for endometriosis (Guideline for Clinical Research on New Chinese Drugs for Treatment of Pelvic Endometriosis, 1993). Participants were diagnosed by peritoneoscopy and operative pathology. Baseline severity of pain: Acupuncture group (n): mild 6, moderate 12, severe 9; Herbal medicine group: mild 12, moderate 10, severe 8. |
|
| Interventions | Ear acupuncture therapy (EAT): Ting Zong (centre of cymba auriculae), Pi Zhi Xia (hypo‐cortex), Nei Fen Mi (endocrine), Jiao Gan (sympathetic) and Nei Sheng Zhi Qi (internal genitals). Acupuncture treatment began 5 days before menstruation and was given four times every other day. A therapeutic course constituted 3 menstrual cycles. Chinese herbal medicine: a decoction of Dan Shen Radix Salviae Miltiorrhizae, ChiShao Radix Paeoniae Rubra, San Leng Rhizoma Sparganii, E Zhu Rhizoma Curcumae, Zhi Qiao Fructus Aurantii and Xiang Fu Rhizoma Cyperi was administered 5 days before menstruation; one dose for 7 days. A therapeutic course constituted 3 menstrual cycles. |
|
| Outcomes | Pain: dysmenorrhoea score (see Table 1 for details) Therapeutic effect: categorical (cured to ineffective) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised, but no details |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were presented for all participants in both groups for all outcomes |
| Selective reporting (reporting bias) | Unclear risk | The outcomes assessed were not introduced until the Results section, so it was not possible to ascertain whether other outcomes had initially been considered or measured. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahn 2009 | Intervention included Japanese style acupuncture. |
| Conboy 2008 | Intervention included Japanese style acupuncture. |
| Danielsson 2001 | Not randomised. |
| Fu 2005 | Intervention included acupuncture and Chinese herbal medicine versus drug therapy. |
| Fugh‐Berman 2003 | Not randomised. |
| Green 2010 | Not randomised. |
| Highfield 2006 | Not randomised. |
| Jin 2009 | Intervention included electro‐acupuncture using body acupoints versus electro‐acupuncture using auricular acupoints. |
| Lim 2009 | No mention of endometriosis. |
| Liu 2003 | Intervention was moxibustion only. |
| Liu 2009 | Interventions included: acupuncture versus acupuncture plus ear tapping versus acupuncture plus moxibustion. |
| Lundeberg 2008 | Not randomised. |
| Qu 2007 | No assessment of pain outcome. |
| Sanfilippo 2008 | Not randomised. |
| Schnyer 2008 | Intervention included Japanese style acupuncture. |
| Sun 2006 | Allocation was made based on sequence of hospital admission. |
| Sun 2007 | Interventions were auricular acupuncture versus body acupuncture. |
| Van Steirteghem 2009 | Not randomised. |
| Vercellini 2009 | Intervention was surgery, not acupuncture. |
| Wayne 2008 | Intervention included Japanese style acupuncture. |
| Xia 2006 | Intervention included acupuncture plus Chinese herbal medicine versus drug therapy. |
| Yan 2008 | Participants were not specifically diagnosed with endometriosis. Cases included: anaemia, pelvic inflammatory disease, uterine adenomyosis, uterine leiomyoma and ovarian cysts. |
| Zhen 2009 | Trial compared different methods of acupuncture: warming‐needle versus general acupuncture. |
Differences between protocol and review
Searches for trials identified a trial comparing auricular acupuncture with Chinese herbal medicine (Xiang 2002). The original protocol for this review did not include this control intervention. However, this trial was included in the review to ensure that a full comparison of treatments could be made.
Additionally, the original protocol for this review stated that we would examine three Chinese language databases. However, there was little need to search the Chinese Biomedicine Database since only one Chinese database is required according to the Group policy.
Since cure rate was reported in the included study as one of combined outcome measures, we have included the original data to reflect clinical practice.
Contributions of authors
XZ coordinated the project and co‐drafted the first version of the protocol and participated in the review preparation. KH proposed the original title and developed the first version of the protocol and review. EM co‐designed and co‐drafted the first version of the protocol and participated in the review preparation. XZ and EM reviewed and commented upon the initial draft of the protocol and review. XZ, KH and EM conducted the initial process of data extraction and trial selection, which were reviewed and commented on by EM.
Sources of support
Internal sources
Menstrual Disorders and Subfertility Group, New Zealand.
External sources
-
Richard Saltonstall Charitable Foundation, USA.
Financial
University of Western Sydney, Australia.
Declarations of interest
None known
New
References
References to studies included in this review
Xiang 2002 {published data only}
- Xiang D, Situ Y, Liang X, Cheng L, Zhang G. Ear acupuncture therapy for 37 cases of dysmenorrhoea due to endometriosis. Zhong Yi Za Zhi [Journal of Traditional Chinese Medicine] 2002;22:282‐5. [PubMed] [Google Scholar]
References to studies excluded from this review
Ahn 2009 {published data only}
- Anh AC, Schnyer R, Conboy L, Laufer M, Wayne, PM. Electrodermal measures of Jing‐well points and their clinical relevance in endometriosis‐related chronic pelvic pain. The Journal of Alternative and Complementary Medicine 2009;15:1293‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conboy 2008 {published data only}
- Conboy L, Quilty MT, Kerr C, Shaw J, Wayne P. A qualitative analysis of adolescents’ experiences of active and sham Japanese‐style acupuncture protocols administered in a clinical trial. The Journal of Alternative and Complementary Medicine 2008;14(6):699‐705. [DOI] [PubMed] [Google Scholar]
Danielsson 2001 {published data only}
- Danielsson I. Dyspareunia in women with special reference to vulvar vestibulitis. Scandinavian Journal of Sexology 2001;4:235‐7. [Google Scholar]
Fu 2005 {published data only}
- Fu Y, Xia T. Clinical observation on the use of acupuncture and Chinese herbal medicine in combination for endometriosis. Shang Hai Zheng Jiu Za Zhi [Shang Hai Journal of Acupuncture and Moxibustion] 2005;24(3):3‐5. [Google Scholar]
Fugh‐Berman 2003 {published data only}
- Fugh‐Berman A, Kronenberg F. Complementary and alternative medicine (CAM) in reproductive‐age women: a review of randomised controlled trials. Reproductive Toxicology 2003;17:137‐52. [DOI] [PubMed] [Google Scholar]
Green 2010 {published data only}
- Green I, Cohen SL, Finkenzeller D, Christo PJ. Interventional therapies for controlling pelvic pain: What is the evidence?. Current Pain Headache Report 2010;14:22‐32. [DOI] [PubMed] [Google Scholar]
Highfield 2006 {published data only}
- Highfield ES, Laufer MR, Schnyer RN, Kerr C, Thomas P, Wayne PM. Adolescent endometriosis‐related pelvic pain treated with acupuncture: Two case reports. The Journal of Alternative and Complementary Medicine 2006;12(3):317‐22. [DOI] [PubMed] [Google Scholar]
Jin 2009 {published data only}
- Jin YB, Sun ZL, Jin HF. Randomised controlled study on ear‐electroacupuncture treatment of endometriosis induced dysmenorrhoea. Acupuncture Research 2009;26(3):188‐92. [PubMed] [Google Scholar]
Lim 2009 {published data only}
- Lim B, Manheimer E, Lao L, Ziea E, Wisniewski J, Liu J, Berman BM. Acupuncture for the treatment of irritable bowel syndrome (review). Cochrane Database of Systematic Reivews 2006;18(4):CD005111. Review. [DOI] [PubMed] [Google Scholar]
Liu 2003 {published data only}
- Liu YX, Cao YX, Wang RY, MA XW, Fei L. Clinical observation on the use of herbal moxibustion with properties of warming and soothing functions for 76 cases of endometriosis. Xin Zhong Yi [New Chinese Medicine] 2003;35(5):55. [Google Scholar]
Liu 2009 {published data only}
- Liu YY, Ai Z, Xi YF, Lin F. Clinical observation on different acupuncture methods for endometriosis. Hu Bei Zhong Yi Za Zhi [Hu Bei Journal of Traditional Chinese Medicine] 2003;31(7):53. [Google Scholar]
Lundeberg 2008 {published data only}
- Lundeberg T, Lund I. Is there a role for acupuncture in endometriosis pain or 'endometrialgia'?. Acupuncture Medicine 2008;26(2):94‐110. [DOI] [PubMed] [Google Scholar]
Qu 2007 {published data only}
- Qu F, Zhou J. Acupuncture enhances the curative effect of Chinese medicinal herbs in treating infertility due to endometriosis. The Journal of Alternative and Complementary Medicine 2007;13:856. [Google Scholar]
Sanfilippo 2008 {published data only}
- Sanfiliippo J, Erb T. Evaluation and management of dysmenorrhoea in adolescents. Clinical Obstetrics and Gynecology 2008;51(2):257‐67. [DOI] [PubMed] [Google Scholar]
Schnyer 2008 {published data only}
- Schnyer, RN, Iuliano D, Kay J, Shields M, Wayne P. Development of protocols for randomised sham‐controlled trials of complex treatment interventions: Japanese acupuncture for endometriosis‐related pelvic pain. The Journal of Alternative and Complementary Medicine 2008;14(5):515‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sun 2006 {published data only}
- Sun, YZ, Chen, HL. A control study on the use of acupuncture Shu and Mu points in combination for endometriosis. Zhong Guo Zhen Jiu [Chinese Acupuncture and Moxibustion] 2006;26:863‐5. [PubMed] [Google Scholar]
Sun 2007 {published data only}
- Sun ZL, Jin YP. Clinical observation on the use of auricular acupuncture for 32 cases of endometriosis. Zhe Jiang Zhong Xi Yi Jie Za Zhi [Zhe Jiang Journal of Integration of Traditional Chinese and Western Medicine] 2007;17(12):738‐9. [Google Scholar]
Van Steirteghem 2009 {published data only}
- Steirteghem A. Editor's Choice. Human Reproduction 2009;24(5):1007. [Google Scholar]
Vercellini 2009 {published data only}
- Vercellini P, Crosignani PG, Abbiati A, Somiglinana E, Vigano P, Fedele L. The effect of surgery for symptomatic endometriosis: the other side of the story. Human Reproduction Update 2009;15(2):177‐88. [DOI] [PubMed] [Google Scholar]
Wayne 2008 {published data only}
- Wayne PM, Kerr CE, Schnyer RN, Legedza AT, Savetsky‐German J, Shields MH, et al. Japanese‐style acupuncture for endometriosis‐related pelvic pain in adolescents and young women: results of a randomised sham‐controlled trial. Journal of Pediatric & Adolescent Gynecology. 2008;21(5):247‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xia 2006 {published data only}
- Xia T. Effect of acupuncture and Chinese medicine in treating endometriosis. Guo Ji Lin Chuang Zhen Ji [International Journal of Clinical Acupuncture] 2006;15(3):145‐50. [Google Scholar]
Yan 2008 {published data only}
- Yan H, Huang X, Deng, G. Observation on therapeutic effect of acupuncture and moxibustion on disorders of myometrial gland. Zhong Guo Zhen Jiu [Chinese Acupuncture and Moxibustion] 2008;28(8):579‐81. [PubMed] [Google Scholar]
Zhen 2009 {published data only}
- Zeng R, Hong W. Clinical observation of the use of acupuncture with warming needle method for 38 cases of endometriosis. Yi Xue Li Lun Yu Shi Jian [Journal of Medical Theory & Practice] 2009;22(5):571‐2. [Google Scholar]
Additional references
Allen 2005
- Allen C. Non‐steroid anti‐inflammatory drugs for pain in women with endometriosis. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD004753.pub2] [DOI] [PubMed] [Google Scholar]
Bajaj 2003
- Bajaj P, Bajaj P, Madsen H, Arendt‐Nielsen L. Endometriosis is associated with central sensitization: a psychophysical controlled study. The Journal of Pain 2003;4(7):372‐80. [DOI] [PubMed] [Google Scholar]
Cabýoglu 2006
- Cabýoglu MT, Ergene N, Tan U. The mechanism of acupuncture and clinical applications. International Journal of Neurosciences 2006;116(2):115‐25. [DOI] [PubMed] [Google Scholar]
Cai 1997
- Chai X. Substitution of acupuncture for human chorionic gonadotropin in ovulation induction. Zhong Yi Za Zhi [Journal of Traditional Chinese Medicine] 1997;17:19‐21. [Google Scholar]
Chen 2007
- Chen D, Chen SR, Shi XL, Guo FL, Zhu YK, Li S, et al. Clinical study on needle‐pricking therapy for treatment of polycystic ovary syndrome. Zhong Guo Zhen Jiu [Chinese Acupuncture and Moxibustion] 2007;27(2):99‐102. [PubMed] [Google Scholar]
Cho 2006
- Cho ZH, Hwang SC, Wong EK, Son YD, Kang CK, Park TS, et al. Neural substrates, experimental evidences and functional hypothesis of acupuncture mechanisms. Acta Neurologica Scandinavica 2006;113:370‐7. [DOI] [PubMed] [Google Scholar]
Cook 1995
- Cook RJ, Sackett DL. The number needed to treat: a clinically useful measure of treatment effect. BMJ 1995;310:452‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davis 2007
- Davis L, Kennedy SS, Moore J, Prentice A. Modern combined oral contraceptives for pain associated with endometriosis. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD001019.pub2] [DOI] [PubMed] [Google Scholar]
Dawood 1991
- Dawood MY. Dysmenorrhoea. In: Max M, Portenoy R, Laska E editor(s). The design of analgesic clinical trials. New York: Raven Press, 1991. [Google Scholar]
Dawood 2006
- Dawood MY. Primary dysmenorrhoea: Advances in pathogenesis and management. Obstetrics and Gynaecology 2006;108(2):428‐41. [DOI] [PubMed] [Google Scholar]
Denny 2004
- Denny E. Women's experience of endometriosis. Journal of Advanced Nursing 2004;46(6):641‐8. [DOI] [PubMed] [Google Scholar]
Deyo 1983
- Deyo R A, Inui TS, Leininger JD. Measuring functional outcomes in chronic disease: a comparison of traditional scales and a self administered health status questionnaire in patients with rheumatoid arthritis. Medical Care 1983;21:180‐92. [DOI] [PubMed] [Google Scholar]
Farmer 2003
- Farmer JE, Prentice A, Breeze A, Ahmad G, Duffy JMN, Watson A, Pick A. Gonadotrophin‐releasing hormone analogues for endometriosis: bone mineral density. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD001297] [DOI] [PMC free article] [PubMed] [Google Scholar]
Farquhar 2000
- Farquhar C. Extracts from the "clinical evidence". Endometriosis. BMJ 2000;320(7247):1449‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Farquhar 2007
- Farquhar C. Endometriosis. BMJ 2007;334:249‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frankiewicz 2000
- Frackiewicz E. Endometriosis: an overview of the disease and its treatment. Journal of the American Pharmacists Association 2000;40(5):645‐57. [DOI] [PubMed] [Google Scholar]
Gao 2006
- Gao X, Outley J, Botteman M, Spaulding J, Simon J, Pashos C. Economic burden of endometriosis. Fertility and Sterility 2006;86(6):1561‐72. [DOI] [PubMed] [Google Scholar]
Hamilton 2008
- Hamilton JL, Roemheld‐Hamm B, Young DM, Jalba M, DiCicco‐Bloom Y. Complementary and alternative medicine in US family medicine practices: a pilot qualitative study. Alternative Therapies in Health & Medicine 2008;14(3):22‐7. [PubMed] [Google Scholar]
Harkin 2007
- Harkin C, Parker R. A prospective, randomised control trial of acupuncture for select common conditions within the emergency department. Journal of Chinese Medicine 2007;85:41‐8. [Google Scholar]
Higgins 2008
- Higgins JPT, Altman DG (editors) on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors, Cochrane Handbook of Systematic Reviews of Intervention. Version 5.0.0 (updated February 2008). The Cochrane Collaboration, 2008. Available from www.cochrane‐handbook.org.
Hope‐Allan 2004
- Hope‐Allan N, Adams J, Sibbritt D, Tracy S. The use of acupuncture in maternity care: a pilot study evaluating the acupuncture service in an Australian hospital antenatal clinic. Complementary Therapies in Nursing & Midwifery 2004;10(4):229‐32. [DOI] [PubMed] [Google Scholar]
Hughes 2007
- Hughes E, Brown J, Collins JJ, Farquhar C, Fedorkow DM, Vandekerckhove P. Ovulation suppression for endometriosis. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD000155.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunt 1986
- Hunt SM, McEwan J, McKenna SP. Measuring Health Status. Beckenham: Croom Helm, 1986. [Google Scholar]
Jackson 2006
- Jackson B, Telner DE. Managing the misplaced. Canadian Family Physician 2006;52:1420‐4. [PMC free article] [PubMed] [Google Scholar]
Kaptchuk 2006
- Kaptchuk TJ, Stason WB, Davis RB, Legedza ATR, Schnyer RN, Kerr CE, et al. Sham device vs inert pill: randomised controlled trial of two placebo treatments. BMJ 2006;332:391‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2005
- Kennedy S, Bergqvist A, Chapron C, D'Hooghe T, Dunselman G, Greb R, et al. ESHRE Special Interest Group for Endometriosis and Endometrium Guideline Development Group. ESHRE guideline for the diagnosis and treatment of endometriosis. Human Reproduction 2005;20(10):2698‐704. [DOI] [PubMed] [Google Scholar]
Lan 1997
- Lan FL, Li D. The development of study on acupuncture for uterine fibroids. Zhong Guo Zhen Jiu [Journal of Clinical Acupuncture and Moxibustion] 1997;13(10):51‐3. [Google Scholar]
Li 2001
- Li X. Exploration of the use of TCM for the diagnosis and treatment of endometriosis. Shang Hai Zhong Yi Yao Da Xue Xue Bao [ACTA Universitatis of Traditions Medicalis Sinensis Pharmacologiaeque Shanghai] 2001;15(3):33‐4. [Google Scholar]
Liao 2008
- Liao XH, Zhang GM, Qi QY, Zhang YY. Overview of TCM research on endometriosis. Zhong Yi Yao Xin Xi [Information on Traditional Chinese Medicine] 2008;25(1):24‐5. [Google Scholar]
Lin 2008 a
- Lin J, Chen W. Acupuncture analgesia: a review of its mechanisms of actions. American Journal of Chinese Medicine 2008;36(4):635‐45. [DOI] [PubMed] [Google Scholar]
Lin 2008 b
- Lin LL, Liu C, ZHuang BY. Clinical observation on treatment of primary dysmenorrhoea with acupuncture and massage. Zhong Guo Zhong Xi Yi Jie He Za Zhi [China Journal of Integrated Traditional and Western Medicine] 2008;28(5):418‐20. [PubMed] [Google Scholar]
Linde 2010
- Linde K, Niemanna K, Meissner K. Are sham acupuncture interventions more effective than (other) placebos? A re‐analysis of data from the Cochrane Review on Placebo Effects. Fortschritte der Komplementmedizin 2010;17:259‐64. [DOI] [PubMed] [Google Scholar]
Maciocia 1998
- Maciocia G. The foundations of Chinese medicine: a comprehensive text for acupuncturists and herbalists. Edinburgh: Churchill Livingstone, 1998. [Google Scholar]
MacPherson 2007
- MacPherson H, White A, Bensoussan A. Chapter 5: The Safety of Acupuncture. In: MacPherson H, Hummerschlag, R, Lewith G, Schyer R editor(s). Acupuncture Research: Strategies for Establishing an Evidence Base. Churchill Livingstone, 2007:57‐76. [Google Scholar]
McQuay 1998
- McQuay H, Moore R. Summary measures. In: McQuay H, Moore R editor(s). An evidence‐based resource for pain relief. 1st Edition. Oxford: Oxford University Press, 1998:14‐8. [Google Scholar]
Medical Outcomes Trust 1994
- Medical Outcomes Trust. SF‐36 Health Survey scoring manual language adaptations: Australia/New Zealand, Canada, United Kingdom. Boston: Medical Outcomes Trust, 1994. [Google Scholar]
Ministry of Public Health 1993
- Ministry of Public Health, P.R. China. Guideline for clinical research on new Chinese medicine for the treatment of pelvic endometriosis. Guideline for Clinical Research on New Chinese Medicine 1993;1:267. [Google Scholar]
Moore 1998
- Moore RA, Gavaghan D, Tramer MR, Collins SL, McQuay HJ. Size is everything – large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects. Pain 1998;78:209‐16. [DOI] [PubMed] [Google Scholar]
Olive 2008
- Olive DL. Gonadotropin‐releasing hormone agonists for endometriosis. New England Journal of Medicine 2008;359:1136‐42. [DOI] [PubMed] [Google Scholar]
Prentice 2001
- Prentice A. Endometriosis. BMJ 2001;323(14):93‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Proctor 2002
- Proctor ML, Smith CA, Farquhar CM, Stones RW. Transcutaneous electrical nerve stimulation and acupuncture for primary dysmenorrhoea. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD002123] [DOI] [PMC free article] [PubMed] [Google Scholar]
Qiu 1993
- Qiu ML, Li LY. Chinese Acupuncture and Moxibustion. Singapore: Churchill Livingstone, 1993. [Google Scholar]
Schmineke 2008
- Schmincke C, Torres‐Londoño P, Seiling M, Gaus W. Evaluating traditional Chinese medicine as applied in the Clinic at Steigerwald. Part 1: Methods of assessment. Fortschritte der Komplementmedizin 2008;Apr;15(2):89‐95. [DOI] [PubMed] [Google Scholar]
Selak 2007
- Selak V, Farquhar C, Prentice A, Singla A. Danazol for pelvic pain associated with endometriosis. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD000068.pub2] [DOI] [PubMed] [Google Scholar]
Shakiba 2008
- Shakiba K, Bena JF, McGill KM, Minger J, Falcone T. Treatment of endometriosis: a 7‐year follow‐up on the requirement for further surgery. Obstetrics and Gynecology 2008;111(6):1285‐92. [DOI] [PubMed] [Google Scholar]
Stratton 2006
- Stratton P. The tangled web of reasons for the delay in diagnosis of endometriosis in women with chronic pelvic pain: will the suffering end?. Fertility and Sterility 2006;86(5):1302‐4. [DOI] [PubMed] [Google Scholar]
Streitberger 1998
- Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352(9125):364‐5. [DOI] [PubMed] [Google Scholar]
White 2001
- White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complementary Therapies in Medicine 2001;9:237‐45. [DOI] [PubMed] [Google Scholar]
Wu 2007
- Wu M, Shoji Y, Chuang P, Tsai S. Endometriosis: disease pathophysiology and the role of prostaglandins. Expert Reviews in Molecular Medicine 2007;9(2):1‐20. [DOI] [PubMed] [Google Scholar]
Xia 2000
- Xia GC. Chinese medicine diagnosis and treatment in the management of menstrual disorders. Beijing: People's Press, 2000. [Google Scholar]
Xiang 2005
- Xiang DF, Si DY. Laboratory study on influence of auricular acupuncture in regulating β‐endorphin and uterine activity on animal model of endometriosis. Guo Yi Lun Tan [Forum on Traditional Chinese Medicine] 2005;20(4):46‐7. [Google Scholar]
Yu 1998
- Yu J. Handbook of Obstetrics and Gynaecology in Chinese Medicine: an integrated approach. Seattle: Eastland Press, 1998. [Google Scholar]
Zhang 2008
- Zhang Y, Clarke J, Feng H, Liu Z, Weina P. Acupuncture for uterine fibroids. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD007221] [DOI] [PMC free article] [PubMed] [Google Scholar]


