Abstract
The worldwide prevalence of anxiety disorders among college students is high, which negatively affects countries, schools, families, and individual students to varying degrees. This paper reviews the relevant literature regarding risk factors and digital interventions for anxiety disorders among college students from the perspectives of different stakeholders. Risk factors at the national and societal levels include class differences and the coronavirus disease 2019 pandemic. College-level risk factors include the indoor environment design of the college environment, peer relationships, student satisfaction with college culture, and school functional levels. Family-level risk factors include parenting style, family relationship, and parental level of education. Individual-level risk factors include biological factors, lifestyle, and personality. Among the intervention options for college students' anxiety disorders, in addition to traditional cognitive behavioral therapy, mindfulness-based interventions, psychological counseling, and group counseling, digital mental health interventions are increasingly popular due to their low cost, positive effect, and convenient diagnostics and treatment. To better apply digital intervention to the prevention and treatment of college students' anxiety, this paper suggests that the different stakeholders form a synergy among themselves. The nation and society should provide necessary policy guarantees, financial support, and moral and ethical supervision for the prevention and treatment of college students' anxiety disorders. Colleges should actively participate in the screening and intervention of college students' anxiety disorders. Families should increase their awareness of college students' anxiety disorders and take the initiative to study and understand various digital intervention methods. College students with anxiety disorders should actively seek psychological assistance and actively accept and participate in digital intervention projects and services. We believe that in the future, the application of methods such as big data and artificial intelligence to improve digital interventions and provide individualized treatment plans will become the primary means of preventing and treating anxiety disorders among college students.
Keywords: College students, Anxiety disorders, Stakeholders, Digital intervention, Big data, Artificial intelligence
Core Tip: This paper reviews the literature on risk factors and digital interventions for college students' anxiety disorders from the perspectives of different stakeholders. The risk factors include class differences, the coronavirus disease 2019 pandemic, peer relationships, student satisfaction with college culture, school functioning levels, parenting style, family relationships, parental education, personal lifestyle, and personality. Different stakeholders should play a corresponding role in the prevention and treatment of anxiety disorders. Methods such as big data and artificial intelligence applied to improve digital interventions and individualized treatment plans will become the primary means of prevention and treatment of anxiety disorders among college students.
INTRODUCTION
The mental health of college students has become an increasingly prominent public health problem on college campuses, and an increasing number of studies have been carried out on the mental health of college students[1]. The World Health Organization conducted an epidemiological survey of 1527 college students and 4178 noncollege students of the same age from 21 different countries. According to survey data, anxiety disorder is the most common disorder among all groups (11.7%-14.7%)[2]. The high prevalence of anxiety disorders among college students has become a global problem[3,4]. In Asia, a cross-sectional study of 617 college students in India showed that the prevalence of anxiety disorders was 30% higher than that of depression, which was 18%[5]. In Europe, a study on depression, anxiety, and stress symptoms in 1074 Spanish college students found that the prevalence of anxiety disorders in this group was 23.6%, which was also higher than that of depression (18.4%), showing a tendency of mild prevalence[6]. Among the 15859 students in the six Association of Southeast Asian Nations countries (Cambodia, Laos, Malaysia, Myanmar, Thailand, and Vietnam), the prevalence of mental health problems was high, with depression and anxiety disorders being the most prominent, and the median prevalence of anxiety disorders was 42.4%[7]. From a meta-analysis conducted to assess the prevalence and potential correlates of depressive and anxiety disorders among college students worldwide, it was discovered that the prevalence of anxiety disorders among college students was 39.0%, and the highest prevalence of anxiety disorders was in North America and in low- and middle-income countries[1].
In early 2020, coronavirus disease 2019 (COVID-19) continued its global spread, rapidly escalating into a global health crisis[8]. Numerous studies have shown higher rates of anxiety disorders among college students following this public health emergency. For example, a study evaluating the psychological status of Chinese college students during the COVID-19 outbreak found that approximately two-fifths of the 89588 college students sampled experienced anxiety disorders during this period[9], and acute stress, anxiety, and depression symptoms were common among college students, displaying a significantly increasing trend in the early stage of the epidemic[10]. In the United States, the COVID-19 pandemic had a direct impact on the mental health of students, and the pandemic was associated with higher levels of anxiety disorders, with one study showing a 52.1% risk among the 610 college students sampled of having a possible generalized anxiety disorder[11,12]. More than one-third of a sample of 496 college students in Nigeria experienced symptoms of anxiety and depression during the COVID-19 pandemic-induced lockdown[13]. The mental health of Israeli college students was significantly affected by the epidemic. One year after the outbreak, the average anxiety level of 366 college students sampled in a study was 8.89, and 39% of the students showed moderate to severe anxiety[14].
College students are a special group. They are in a critical transition period from adolescence to adulthood, working on the formation of values, adaptability, global outlook, and outlook on life[5,15]. At the same time, they are also faced with various pressures arising from role changes, learning tasks, interpersonal relationships, and employment[15,16]. In this case, the depression, anxiety, and other symptoms experienced by college students and the resulting psychological distress exert a negative impact on their academic performance and social interaction[9,17,18]. The outbreak of COVID-19 has brought higher levels of pressure and presented additional challenges to the prevention and treatment of college students' anxiety. Evidence suggests that during the COVID-19 period, college students have suicidal thoughts due to experiencing higher levels of psychological stress[19], and mental health disorders, such as anxiety and depression, are strong triggers for suicide[20]. Therefore, it is urgent to pay close attention to mental health problems such as anxiety in college students and take effective measures to prevent and treat these problems.
In recent years, with the rapid development of artificial intelligence, machine learning, and deep learning, digital technology has gradually been applied to the field of mental health, changing the way that people experience health care. Digital mental health, also known as digital diagnosis and treatment, refers to services for the prevention or treatment of psychological disorders delivered through digital platforms. This takes many forms, including online therapy, Apps to guide therapy, virtual assistants and chatbots, gamified therapy, etc.[21]. Research shows that while the COVID-19 pandemic has put enormous pressure on mental health care systems, it has also brought about new opportunities for the development of digital mental health interventions[22].
Overall, anxiety disorder among college students has become a global public health problem that cannot be ignored. For nations, the importance of college students to human capital potential cannot be overemphasized, and untreated mental illness can have a significant impact on productivity, substance use, and social relationships, thereby hindering a nation’s human capital[2,16]. For colleges, anxiety has become an increasingly common and prominent problem, posing a challenge to public health on campuses[1]. Additionally, the family plays an important role in helping to guide children from childhood into adults ready to enter society, and the influence of parents may affect children's anxiety in different ways[23,24]. For students, anxiety affects their motivation to study and to engage in social interaction, which then affects the successful development of students[18].
Therefore, college student anxiety is not caused by a single factor, and it cannot be effectively intervened by a single force. It needs to be studied from the perspective of different stakeholders. However, there are few literature reviews on this topic, and most studies analyze individual risk factors and intervention methods, failing to grasp the trend of digital mental health intervention development. The purpose of this literature review is to review and discuss the main literature on college student anxiety and analyze the risk factors and new digital intervention methods for college student anxiety from the perspective of four different stakeholders: The state, the school, the family, and the individual. The aim is to provide a reference for effective intervention and reduction of anxiety in this group.
LITERATURE SEARCH STRATEGY
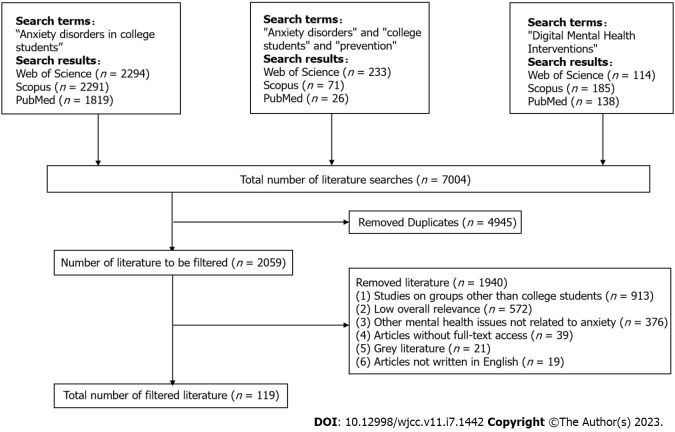
The literature search was conducted in November 2022. PubMed, Web of Science Core Collection, and Scopus databases were searched using the keywords "anxiety disorders in college (university) students", "anxiety disorders" and "college (university) students" and "prevention", and "digital mental health interventions". After eliminating duplicates, the literature was screened based on the title, abstract, and keywords, with the exclusion criteria being: (1) Studies on groups other than college students; (2) titles that did not appear in the search terms but were only briefly mentioned in the abstract, with low overall relevance; (3) other mental health issues unrelated to anxiety; (4) articles without full-text access; (5) gray literature; and (6) articles not written in English. The detailed process of literature screening is shown in Figure 1.
Figure 1.
Literature search strategy.
RISK FACTORS
Most of the current studies analyze one or several risk factors. Considering that anxiety disorder among college students is a social problem that affects multiple stakeholders, we conduct an analysis from the perspectives of different stakeholders and roughly divide the stakeholders into four groups: The nation and society, colleges, families, and college students (Table 1).
Table 1.
Risk factors for college students' anxiety disorder from the perspective of different stakeholders
|
Stakeholders
|
Risk factors
|
Specific performance
|
| Country and society | Socioeconomic conditions | Low socioeconomic status and large class differences[25,26] |
| Economic difficulties[27] | ||
| Low material standard of living[31] | ||
| COVID-19 pandemic | Highly sudden and quick spreading[36] | |
| Misleading, negative information[37] | ||
| Lack of coping experience[18] | ||
| Learning[1,6], Graduation[9], Employment[41] | ||
| Lack of interpersonal communication[18,40] | ||
| Close friend or acquaintance diagnosed[18] | ||
| Residence[18,41] | ||
| Colleges | Campus environment | Indoor environment design of colleges[43] |
| Peer relationship | Drinking[47], School Bullying[49,50] | |
| Satisfaction with the college | Satisfaction with college culture[52] | |
| Low level of school functionality[53] | ||
| Families | Parenting style | Authoritarian parenting style[57] |
| Hostility from the father[59] | ||
| Mother's overprotection[59] | ||
| Excessive parental expectations[22] | ||
| Family relationship | Domestic violence[57] | |
| Verbal assault by parents[60] | ||
| Family conflict[61], parents quarrel, separation[1] | ||
| Educational level of parents | Father's low education level[22] | |
| Family function | Low level of family functioning[66] | |
| College students | Biological factors | Gender issues[69] |
| Older age[6,71] | ||
| Lifestyle | Poor sleep quality, irregular diet, low frequency of transportation, obesity, smoking, alcohol consumption[52,72] | |
| Personality | Introverted personality[73] | |
| Low level of self-esteem and weak self-efficacy[1,74] |
COVID-19: Coronavirus disease 2019.
Country and society
Most studies suggest that socioeconomic status is associated with higher rates of anxiety[25,26]. Studies have shown that students with lower socioeconomic status have a significantly higher risk of developing anxiety disorders. Students with lower socioeconomic status were 109.1% more likely to suffer from anxiety disorders than those with high economic status[27]. The study found an inverse relationship between socioeconomic status and mental health in the general population[28-30]. There is a higher prevalence of panic, various phobias, and generalized anxiety disorder in people of lower socioeconomic status[26]. In addition, a meta-analysis of certain European countries found that experiencing financial difficulties increases the incidence of depression and anxiety disorders[27]. A survey from the United Kingdom found that the risk of depression and anxiety disorders is related to low living standards[31,32]. Currently, there are two theories that explain the specific direction of the association between socioeconomic status and mental health. Social causality theory suggests that living in poor neighborhoods contributes to mental illness through stress[33]. Social choice theory argues that mental illness leads to poor choices that result in poor neighborhoods[32].
Anxiety among college students has also been impacted by the COVID-19 pandemic. Numerous studies have confirmed that the COVID-19 outbreak has had a significant negative impact on the economy, social activities, and public health. Since the outbreak of the epidemic, people have been prone to severe panic and anxiety, and the prevalence of anxiety disorders, depression, and suicidal thoughts has increased[12,34-36]. A review of the literature finds that the impact of the COVID-19 pandemic on college students' anxiety can be analyzed from two aspects: The characteristics of the epidemic (including the new coronavirus pneumonia epidemic) and the particularity of college students. For the former, on the one hand, the epidemic has the characteristics of strong suddenness, strong contagion, rapid spread, and wide range. In the absence of specific drugs for its treatment, the mortality rate of high-risk groups is high[36]. On the other hand, a lack of information from official channels causes the media, and thus society, to be presented with misleading and negative information, which affects the accuracy of people's understanding of the epidemic. The overload of information in the media and the lack of psychological assistance measures to address these types of public events undoubtedly aggravate the negative psychological emotions or symptoms of the public[36,37].
Regarding the latter, the impact of the COVID-19 pandemic on college students' anxiety is reflected in the following aspects. First, the epidemic has caused different degrees of pressure and fear[11]. Compared with the general population, college students lack experience in dealing with emergencies, making it difficult for them to conduct rational analyses and perform good decision-making[18]. In addition, the lives of college students have been uniquely affected by their inability to return to school12]. Exposed to the multiple stresses that are unique to this developmental stage, college students become a group particularly vulnerable to psychological problems[38]. Second, the COVID-19 pandemic has had a negative impact on college students' learning[39]. The academic performance of students was affected by being unable to attend school normally[36], an increased number of courses[1], and the challenges posed by online learning[18] and other factors, all of which affected the academic progress and performance of students. Third, measures such as lockdowns, quarantine measures, and strict outbreak monitoring have resulted in less face-to-face communication and increased the distance between people. Lack of interpersonal communication can easily exacerbate the anxiety disorders of college students[18,40]. Fourth, research shows that college students' anxiety about the epidemic is related to their place of residence. However, no agreement has been reached on the specific impact mechanism. Some studies suggest that college students living in rural areas show a lower prevalence of anxiety[18], while other studies suggest that students living in rural areas have higher levels of anxiety[41].
Colleges
College is a critical time for individuals to experience such transformation and stress[42]. While providing development opportunities for students, colleges also have many risk factors that affect students' mental health. Research shows that the college indoor environment, peer relationships, and satisfaction with college all affect college students' anxiety levels. First, psychology posits that an individual's psychology is affected by their environment[43]. Research shows that the general classroom environment is not conducive to students' mental health. Designing the indoor environment of colleges based on design psychology and providing cognitive stimulation to students through art visual therapy can effectively alleviate the anxiety of college students[43]. Second, the growing importance of peer influence is one of the hallmarks of adolescent psychosocial functioning[44]. In adolescence, students are more strongly influenced by their peers than they are in adulthood[45]. Research confirms that college students with high levels of social anxiety are more likely to be influenced by their peers[46] and that heavy drinking with their close peers can increase the risk of anxiety[47]. Compared with relationships with teachers, peer relationships have a stronger predictive effect regarding college students' anxiety[22,48]. Additionally, school bullying is more notable. A number of studies have shown that school bullying not only causes certain physical and psychological harm to students but also significantly increases the level of anxiety and depression in students[49,50]. Compared with college students who did not experience school bullying, students who experienced school bullying showed higher levels of anxiety and depression[51]. As a strong predictor of anxiety, school bullying has a strong predictive effect on college students' anxiety, and its mechanism comprises two aspects: A relatively negative self-perception and a poor ability to deal with negative comments. This causes an individual to be more prone to anxiety when dealing with interpersonal problems or other difficulties[51]. Finally, the study found that dissatisfaction with college culture[52] and low levels of school functioning[52,53] are closely related to mood and anxiety disorders in college students and are risk factors for college students' anxiety.
Families
The family represents the immediate environment in which an individual lives and grows. According to ecosystem theory, the family as a microsystem has a profound impact on a person's development[54]. Family upbringing is the starting point of individual psychological adaptation[55], and the family is the root of all psychological symptoms[56]. Parenting styles (including corresponding behavioral patterns and tendencies), family relationships and atmosphere, parents' educational level, and family functions are all closely related to children's mental health. Specifically, parenting style has a significant correlation with the mental health level of college students[55]. Compared with children raised under positive, democratic parenting styles, children raised in negative, authoritarian[57] families are more likely to have negative emotions in life, which endangers their mental health[58]. A study analyzed 545 students at a Chinese college and found that college students who were hostile toward their fathers were more likely to suffer from anxiety. This study also revealed that maternal overprotection had a significant impact on college students' anxiety[59]. Second, compared with college students from harmonious families, college students from settings involving domestic violence are more likely to exhibit anxiety disorders, depressive symptoms, and comorbidities[57]. Domestic violence can cause negative emotions such as fear, anger, and worry in children, making children more emotionally sensitive[57]. Research shows that parental verbal aggression[60] and family conflict[61] can lead to psychological problems such as anxiety, depression, and stress in children. Family cohesion is also closely related to students' depression, anxiety, insomnia, etc.[62-64]. Third, the educational level of parents also has a certain impact on the mental health of college students[65]. Some studies have noted that college students whose fathers have a low level of education are more likely to show psychological symptoms such as anxiety[55]. This may be because parents with higher education levels are relatively more capable of promoting their children's all-around development and tend to pay more attention to their children's mental health education[65]. Fourth, healthy family functioning contributes to the development and maintenance of students’ mental health[66]. The relationship between family functioning and college students' anxiety has been highlighted during the COVID-19 epidemic. The results of the study show that healthy family function can effectively alleviate the anxiety of college students during the coronavirus pneumonia epidemic, and anxiety is reduced when staying with their parents[66].
College students
Every student is unique. Anxiety is a psychological and physiological state comprising cognitive, somatic, emotional, and behavioral components[67]. Therefore, in addition to the above external factors, the influence of the individual heterogeneity of college students on their anxiety cannot be ignored. After reviewing and summarizing the literature, individual heterogeneity can be roughly divided into three parts: Biological factors, lifestyle, and personality. First, in terms of biological factors, multiple studies have shown that compared with males, female college students experience a higher prevalence of anxiety disorders[1,6,68,69]. This may be due to biological differences between males and females (such as genetic vulnerability, hormone and cortisol levels, etc.). Such physiological differences and perceptions of vulnerability can manifest through emotion and behavior[70]. However, some studies have also found that there is no significant difference between sexes in the prevalence of anxiety disorders in college students[9]. In addition, age was also significantly associated with higher anxiety levels[6,71]. Second, the lifestyle of college students, as embodied by poor sleep quality, irregular diet, low exercise frequency, obesity, smoking, and drinking[52,72], affects their anxiety disorders and levels to a large degree. Third, students' personalities determine their attitudes toward difficulties and their willingness to express negative emotions. Extroverts are more confident and tend to experience higher levels of positive emotions. In contrast, introverts are more likely to experience more psychological problems and have a higher risk of developing anxiety disorders[73,74]. It should be noted that self-esteem and self-efficacy are negatively correlated with symptoms such as anxiety and depression in college students[1].
DIGITAL INTERVENTIONS
Psychological disturbances such as anxiety and depression have a negative impact on students’ studies, lives, physical health, and future employment to varying degrees and can even lead to suicidal behaviors[75-77]. Early intervention and management of anxiety and depression in college students can effectively alleviate symptoms and promote the development of students' mental health[78]. At present, a variety of measures have been developed to intervene in the mental health of college students, such as antidepressants, cognitive behavioral therapy, mindfulness-based interventions, yoga interventions, physical exercise, and art therapy. These measures can alleviate the anxiety disorders of college students to varying degrees[75,79]. Among them, the more common interventions include cognitive behavioral therapy, mindfulness-based interventions, psychological counseling, and group counseling. Cognitive behavioral therapy, which aims to change personal thoughts and behaviors and has long-term effects on the treatment of anxiety disorders[80,81], is one of the most widely used psychotherapies. Cognitive behavioral therapy under multimodal delivery provides a variety of choices for mental health interventions aimed at different groups[82,83]. The mechanism behind the effect of mindfulness intervention on anxiety disorders is as follows. On the one hand, it can reduce the self-identification of success and failure in social and stressful situations, and on the other hand, it can stop patients from evaluating situations that are prone to cause anxiety[84]. Psychological counseling is conducted through purposeful communication with patients aimed at helping them perceive the impact of past experiences to better understand their emotions and behaviors. Group counseling effectively integrates time, space, human resources, and other resources, can treat a large number of patients, and is widely used in clinical practice[85].
It is worth noting that the drawbacks of traditional interventions and the barriers that students face in accessing mental health services need to be considered. First, traditional interventions require the participation of mental health professionals, while the prevalence of anxiety disorders among college students is high, and the number of mental health professionals and the availability of mental health services are limited[86,87]. Second, because of the risk of stigmatization, college students have a low willingness to seek help. Multiple studies have shown that stigma is a major barrier to seeking psychological assistance. Patients worry about the opinions of others and may internalize the stigma, thereby exacerbating their anxiety disorders[88-90]. Third, for college students, another barrier to psychological assistance is the lack of continuity in access to therapy[76]. College students are busy with schoolwork, exams, and various activities, and their time is relatively divided[6]. In addition, psychological counseling institutions in colleges are more inclined to provide short-term counseling services, which is not conducive to long-term follow-up treatment, thereby moderating the effectiveness of treatment[91].
In recent years, digital medical care has received increasing attention[22]. In the field of mental health, digital medical applications have shown unique advantages and are considered to be an alternative solution to the obstacles reviewed[92]. Its advantages are mainly as follows. First, digital mental health interventions do not rely on professional psychologists, which can effectively alleviate the imbalance between the supply and demand for mental health professionals[93]. Second, unlike traditional face-to-face interventions, digital interventions rely on the internet, big data, and artificial intelligence, which provide high anonymity and accessibility and can effectively protect patients’ privacy, reducing the risk of stigma[78,94]. Third, digital interventions afford students more flexibility in time and space[94]. Fourth, because students are considered ‘digital natives’, digital interventions are particularly attractive to college students. Survey data show that in the United States, young people aged 18-29 have the highest usage rates for the internet and smartphones[93]. More importantly, different stakeholders can also benefit from digital interventions. At a national level, college students are more likely to drop out of school due to anxiety disorders, which not only seriously affects human capital[94] but also burdens society with both direct and indirect costs[78]. In addition, stress and mental disorders during work and study also directly contribute to lost productivity[95]. Digital intervention can effectively treat college students' anxiety, depression, and other symptoms, is cost-effective, and has development potential[76]. At the school level, digital intervention is highly acceptable, feasible, and effective and can reduce the difficulties caused by insufficient human resources[96,97]. From the level of families and students, there is no doubt that alleviating students’ anxiety disorders through digital intervention is conducive to promoting family harmony and the physical and mental health of students[78].
Current digital interventions mainly include web-based or computer-based programs or mobile applications, chatbots powered by artificial intelligence, and virtual reality tools[98]: (1) There are network-based support systems, such as MePlusMe and the Mana Maali Digital Anxiety Program. MePlusMe is an online support system specifically developed to provide support throughout the day to college students experiencing mild to moderate psychological distress. Studies have shown that the use of MePlusMe can significantly relieve students' anxiety and depression symptoms[77]. The Mana Maali Digital Anxiety Program is an online support system specifically developed to provide support throughout the day to college students experiencing mild to moderate psychological distress; (2) There are mobile applications such as DeStressfy that are mindfulness-based applications designed to provide practice questions in the form of audio, video, or text files. The practice questions include four parts: Basic visualization, gratitude, imagining the life you want, and finding meaning. Research shows that students who use this therapy experience significantly fewer anxiety disorders[91] than those who do not; (3) There are chatbots powered by artificial intelligence. A chatbot is a computer program that simulates human conversation, creating the illusion of intelligent conversation[99,100], primarily for the delivery of cognitive behavioral therapy[101]. Through interaction, chatbots can provide college students with personalized mental health counseling, which can effectively prevent anxiety and improve their sense of well-being[102]; and (4) There are virtual reality tools. Counseling systems that combine psychological knowledge and virtual reality technology use virtual agents in the form of chatbots to interact with students in a virtual environment. At this time, the chatbot acts as a psychological counselor, leading the group in counseling to relieve pressure on students and improve their quality of life[85].
Research shows that digital mental health intervention is a potential solution for the effective treatment of college students' anxiety, but its implementation depends on stakeholder acceptance. Digital interventions are more likely to benefit college students’ mental health development when all stakeholders that are affected by digital interventions form a synergy[103]. In conclusion, digital mental health interventions need to be analyzed from the perspectives of different stakeholders, both in terms of importance and necessity (Table 2).
Table 2.
Digital interventions for college students' anxiety disorder from the perspective of different stakeholders
|
Stakeholders
|
Interventions
|
| Country and society | Provide an enabling policy environment[22] |
| Propose subsidies or grants[106] | |
| Establish clear and targeted regulatory standards and processes[109] | |
| Colleges | Accept and actively introduce technology-based mental health resources[104] |
| Conduct regular mental health screenings[104] | |
| Conduct preventive education[22] | |
| Form digital intervention teams[22] | |
| Families | Create a good family atmosphere[113] |
| Show concern about children's learning and living conditions[116] | |
| Active learning and understanding of digital interventions[117] | |
| Active participation in digital intervention research and practice[116] | |
| College students | Proactively seeking psychological assistance[103] |
| Active participation and cooperation with digital intervention exercises[103] |
Country and society
Digital interventions, with their unique advantages, provide patients with more effective treatment options and reduce the likelihood of developing barriers to mental health services[104]. The use of digital interventions to address unmet mental health care needs has become even more critical during the COVID-19 pandemic[105]. Notably, however, while digital interventions have shown great promise in the field of mental health, they have inevitably raised concerns. For example, does the entire intervention process comply with ethical norms? How can we avoid risks to student privacy? Who owns the data that is generated during treatment[104]?
In addition, as a new treatment concept, digital intervention is still in its early stages, and its further application and development still face many challenges. There is an urgent need to increase social awareness of digital interventions. In this case, policy guarantees, funding, and supervision from the national level are particularly important. First, the government needs to provide a favorable policy environment. The government should consider adjusting existing health care policies to incorporate more complex socioeconomic factors into the scope of policy guarantees. This would be conducive to the development of effective digital interventions across platforms while maintaining the consistency of basic treatment principles[22]. Second, the government should actively reach cooperation agreements with insurance companies and developers to jointly study optimal ways to subsidize or finance digital health management[106]. Governments can also provide funding for resources, such as the creation of region-specific digital health toolkits, to enrich the content and form of digital interventions[107,108]. Finally, considering the ethical and privacy issues that may exist in digital interventions, the government needs to establish clear and targeted regulatory standards and regulatory processes to ensure the safety and further commercialization of digital interventions[109-111].
Colleges
Colleges are important venues for implementing digital mental health interventions. On college campuses, counseling centers are the primary source of psychological assistance for students[112]. To address the psychological problems of students and promote the healthy development of students' physical and mental health, schools need to provide active support, preventive and timely intervention, and reasonable staff deployments. First, schools should accept and introduce mental health resources based on technology support according to their own conditions and the needs of their students[104], including but not limited to some mindfulness-based internet interventions[91], mobile apps[96], and the Digital Health Toolkit[108]. Second, it is necessary for schools to conduct regular mental health screenings to detect possible abnormalities in students in a timely manner to intervene as quickly as possible. For example, schools could introduce technology-enabled standardized mental health screening programs on campus websites. When students complete screenings for common mental health and behavioral problems, schools can obtain feedback on the assessment results, which can further the identification of the possible risks of mental disorders[104]. Schools should also strengthen preventive education on psychological problems such as anxiety and depression among students. Finally, schools need to set up a digital intervention team of managers, psychologists, and professional instructors for their counseling centers. Research shows that in the absence of physician guidance, digital interventions are significantly less likely to be successful[22]. Therefore, team members should coordinate and guide students in the correct use of technology-enabled projects, thus maximizing the advantages of digital intervention projects.
Families
Family members play an important role in the prevention and treatment of mental disorders such as anxiety and depression in college students[113,114]. Studies have found that when family members participate in treatment, the risk of disease recurrence is significantly reduced[115]. Therefore, it is important to involve family members in the process of digital mental health intervention for college students. However, research in this field is very limited. Therefore, we present the following prospects on the basis of the influence that family exerts on the anxiety disorders of college students and the effectiveness of digital intervention. First, parents should be aware of the impact of family relationships and parenting styles on their children's mental health, make their best attempt to create a good family atmosphere for their children, care about their children's academic and living conditions, and give their children warmth. Second, parents can actively learn the design concept of digital psychological intervention and understand the role and usage of current digital intervention methods to better guide children in the correct use of these intervention methods. Finally, parents and other family members can actively participate in the research and practice of supporting college students' mental health through technology. Parents may have different concerns about digital interventions than children[116,117]. For example, do some Apps cause children to become addicted to smartphones and waste time? Do digital interventions negatively impact treatment adherence and recovery? These concerns are of high value for the application and development of digital interventions and should be carefully considered.
College students
Students have more mental health needs and are the primary stakeholders in digital interventions. The prevalence of anxiety disorders among college students is high, but their willingness to seek help is low. This phenomenon adds a certain degree of difficulty to the timely detection of and intervention in anxiety disorders in college students. A study conducted an online cross-sectional survey of 570 college students across 23 schools in the United States and found that most students did not use digital interventions to address mental health problems, and many students were unaware of this possibility[103]. Therefore, students need to increase their awareness and actively seek psychological assistance and pay better attention to channeling information such as Apps, mental health questionnaires, and crisis hotline text messages. Under the premise of protecting their own privacy, students can expand their understanding of digital mental health interventions and accept measures such as monitoring information systems and mental health services. In addition, the degree of acceptance and cooperation displayed by students directly affects the implementation effect of digital interventions. Students should actively participate in and cooperate with the relevant exercises in the process of receiving the intervention and report any problems encountered to an instructor or doctor in a timely manner.
FUTURE DIRECTIONS
This review found that current research on the influencing factors of college student anxiety is relatively limited and lacks a comprehensive analysis. For example, most studies have separately explored the impact of the COVID-19 pandemic, family functioning, sleep, diet, drinking, and other factors on college student anxiety[36,37,52,66]. Therefore, this study takes the perspective of different stakeholders and reasonably divides various influencing factors, which facilitates clearer and more in-depth discussion. After reviewing and summarizing the literature, it can be found that heterogeneity at the individual level is a more important factor that triggers college student anxiety, mainly manifested in biological factors, lifestyles, and personalities. Previous research has comprehensively and sufficiently demonstrated the influence and mechanisms of physiological and behavioral factors on college student anxiety. It is worth noting that individual psychological characteristics may be the potential motivation for manifest behavior, which can also have a direct or indirect impact on college student anxiety. Future research should include individual psychological characteristics in the scope of study. Individuals inevitably show heterogeneity under the influence of the external environment, and family and school are key external factors that influence college student anxiety. Currently, research on families mainly focuses on parenting styles, family relationships, and family functioning. In fact, the impact of families on college student anxiety largely depends on the quality of the family environment and relationships. This impact is also more far-reaching. Previous research has also confirmed this point. Considering the special influence of families, future research can consider using qualitative research methods based on diverse samples to explore the deeper mechanisms behind this influence. Colleges are the direct environment for college students' learning and living. Previous research has paid more attention to the influence of peer relationships in colleges on college student anxiety, especially malignant peer relationships[49,50]. However, other interpersonal relationships, campus environment, and support provided by colleges should not be ignored. Future research should pay attention to other risk factors within colleges to enrich and deepen research in this field. As background factors, the national and social environment has an impact on college student anxiety. Previous research has thoroughly demonstrated the state of college student anxiety and its causes during the COVID-19 pandemic, providing an important reference for seeking coping strategies[18,37]. The overall economic development and employment environment may be included in future research as supplementary background factors.
In terms of interventions for college student anxiety, in addition to traditional cognitive behavioral therapy and mindfulness interventions, digital mental health has become a new trend in recent years. Its characteristics of scalability and unique advantages of high cost-effectiveness and sustainability have attracted much attention. Currently, research combines traditional intervention methods with digital interventions to analyze their effectiveness in relieving college student anxiety and introduces mobile applications, chatbots, and virtual reality tools in interventions to demonstrate the implementation process and effectiveness. However, these intervention methods are often developed by individuals or teams, which limits their scope and effectiveness. Therefore, the complete digital intervention process, including development, implementation, supervision, evaluation and feedback, and assistance, requires the participation of different stakeholders. At the national and social levels, only a few studies currently focus on policy protection, funding, and regulation, but there are differences in the attitudes of different countries toward digital interventions, as well as the policy measures and regulatory standards adopted[110,111]. There is a need for further research and exploration on how to ensure the security, effectiveness, and sustainability of digital interventions at the national level. At the school level, there is currently a lack of research on the application of digital intervention projects in college campuses and the efforts that schools, as stakeholders, should make. Schools, as important entities for addressing students' mental health issues and promoting the physical and mental health development of students, need to take appropriate measures to make full use of digital interventions, such as establishing digital intervention service policies and seeking appropriate intervention models. At the family level, existing research ignores the importance of families in digital mental health interventions for college students. In fact, parents may be more likely to notice abnormal mental states in college students. Therefore, it is possible to consider integrating the role of families into specific digital intervention projects, plans, or applications in the future. At the individual level of college students, as the direct subjects of digital intervention, future research should focus on the specific demands and feedback of college students and enhance their proactive seeking of mental health assistance and participation in digital interventions. In summary, how various stakeholders can play a full role in digital interventions and form multifaceted interactive interventions is the main direction of future research.
LIMITATIONS
The limitations of this study include the following. On the one hand, this article analyzes the relevant literature written in English while excluding studies written in other languages. On the other hand, this article is a narrative review of risk factors and digital interventions for anxiety among college students and does not involve systematic and retrospective reviews. The study only introduces research in related fields by summarizing its main conclusions. The purpose of this study is to provide a macro overview of the research on anxiety disorders in college students, and the content of this study cannot be directly applied to clinical treatment.
CONCLUSION
This paper reviews the primary literature related to college students' anxiety disorders and presents a review of the related risk factors and digital interventions for college students' anxiety disorders from different stakeholder perspectives. From the perspective of the country and society, class differences and the new coronavirus pneumonia epidemic are the main risk factors for college students' anxiety. To better apply digital intervention to the prevention and treatment of anxiety among college students, the state and society should provide necessary policy guarantees and funding and ensure supervision. At the school level, the indoor design of the environment, peer relationships, student satisfaction with college culture, and school function levels may cause or even aggravate students' anxiety disorders. Among these, the psychological trauma caused by school bullying requires schools to pay special attention. Schools should take effective measures to prevent this phenomenon. Accordingly, schools can give full play to the role of digital intervention by actively introducing digital intervention resources and services, improving mental health screening systems, conducting preventive education, and establishing professional teams. At the family level, parenting style, family relationship, and parental education level all have different effects on the anxiety disorders of college students. Parents should establish a good family relationship, actively understand the concepts and methods of digital intervention, actively participate in relevant research and practice, and have the courage to express their concerns. At the individual level, college students are heterogeneous in terms of biological factors (sex, age, etc.), lifestyle, and personality. Among them, aspects of lifestyle, such as diet, exercise, sleep, etc., are more likely to have a direct impact on anxiety. Therefore, college students should actively seek psychological assistance and accept and participate in digital intervention services to promote their physical and mental health.
Numerous studies have been conducted on the status, influencing factors, prevention, and intervention methods for anxiety disorders among college students worldwide, with significant findings. This literature review refines and summarizes the influencing factors and digital interventions for anxiety disorders among college students from the perspective of stakeholders, emphasizing the important roles played by different stakeholder groups, and provides valuable references for improving the mental health of college students. We believe that digital intervention, as an effective solution for mental health issues, has strong appeal and potential for development. Future research should focus on the development and application of digital mental health interventions. First, artificial intelligence and big data-based intervention methods for anxiety disorders should be implemented and enriched, with large-scale data collected and precise diagnosis achieved. Using algorithms that predict college students' anxiety levels based on various factors can enable diagnosis in natural states and reduce college students' fear of doctors. Second, because the causes, symptom expressions, and severity of anxiety disorders vary among college students, future research should consider the personalized mental health needs of students. As some researchers have pointed out, the goal of digital representation of college students is not only to understand the reasons for students' mental health problems but also to provide personalized care[118]. Based on the evaluation data regularly collected from patients and healthcare providers, stakeholders can develop decision trees and machine algorithms to formulate personalized treatment plans and improve the flexibility of treatment[22]. Third, future adjustments can be made from the development end of the application, slightly weakening college students' awareness that they are "receiving psychological treatment," protecting their privacy, and reducing the risk of stigmatization.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: November 24, 2022
First decision: December 26, 2022
Article in press: February 10, 2023
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Liu Q, China; Tang F, China S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR
Contributor Information
Xin-Qiao Liu, School of Education, Tianjin University, Tianjin 300350, China. xinqiaoliu@pku.edu.cn.
Yu-Xin Guo, School of Education, Tianjin University, Tianjin 300350, China.
Yi Xu, School of Education, Tianjin University, Tianjin 300350, China.
References
- 1.Li W, Zhao Z, Chen D, Peng Y, Lu Z. Prevalence and associated factors of depression and anxiety symptoms among college students: a systematic review and meta-analysis. J Child Psychol Psychiatry. 2022;63:1222–1230. doi: 10.1111/jcpp.13606. [DOI] [PubMed] [Google Scholar]
- 2.Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, Hwang I, Kessler RC, Liu H, Mortier P, Nock MK, Pinder-Amaker S, Sampson NA, Aguilar-Gaxiola S, Al-Hamzawi A, Andrade LH, Benjet C, Caldas-de-Almeida JM, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, Haro JM, Karam EG, Kiejna A, Kovess-Masfety V, Lee S, McGrath JJ, O'Neill S, Pennell BE, Scott K, Ten Have M, Torres Y, Zaslavsky AM, Zarkov Z, Bruffaerts R. Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychol Med. 2016;46:2955–2970. doi: 10.1017/S0033291716001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandal RK, Goel NK, Sharma MK, Bakshi RK, Singh N, Kumar D. Prevalence of Depression, Anxiety and Stress among school going adolescent in Chandigarh. J Family Med Prim Care. 2017;6:405–410. doi: 10.4103/2249-4863.219988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bahhawi TA, Albasheer OB, Makeen AM, Arishi AM, Hakami OM, Maashi SM, Al-Khairat HK, Alganmy OM, Sahal YA, Sharif AA, Mahfouz MS. Depression, anxiety, and stress and their association with khat use: a cross-sectional study among Jazan University students, Saudi Arabia. Neuropsychiatr Dis Treat. 2018;14:2755–2761. doi: 10.2147/NDT.S182744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghrouz AK, Noohu MM, Dilshad Manzar M, Warren Spence D, BaHammam AS, Pandi-Perumal SR. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019;23:627–634. doi: 10.1007/s11325-019-01780-z. [DOI] [PubMed] [Google Scholar]
- 6.Ramón-Arbués E, Gea-Caballero V, Granada-López JM, Juárez-Vela R, Pellicer-García B, Antón-Solanas I. The Prevalence of Depression, Anxiety and Stress and Their Associated Factors in College Students. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17197001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dessauvagie AS, Dang HM, Nguyen TAT, Groen G. Mental Health of University Students in Southeastern Asia: A Systematic Review. Asia Pac J Public Health. 2022;34:172–181. doi: 10.1177/10105395211055545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun J, He WT, Wang L, Lai A, Ji X, Zhai X, Li G, Suchard MA, Tian J, Zhou J, Veit M, Su S. COVID-19: Epidemiology, Evolution, and Cross-Disciplinary Perspectives. Trends Mol Med. 2020;26:483–495. doi: 10.1016/j.molmed.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu W, Yan S, Zong Q, Anderson-Luxford D, Song X, Lv Z, Lv C. Mental health of college students during the COVID-19 epidemic in China. J Affect Disord. 2021;280:7–10. doi: 10.1016/j.jad.2020.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gonzalez Mendez MJ, Xu HF, Li M, Xu KP, Guo LW, Chen Q, Zheng LY, Chen PP, Salah DS, Ning Y, Zhang SK, Qiao YL. Mental Health and Associated Factors Among College Students During the COVID-19 Pandemic in China. Asia Pac J Public Health. 2022;34:427–429. doi: 10.1177/10105395221074535. [DOI] [PubMed] [Google Scholar]
- 11.Barbosa-Camacho FJ, Romero-Limón OM, Ibarrola-Peña JC, Almanza-Mena YL, Pintor-Belmontes KJ, Sánchez-López VA, Chejfec-Ciociano JM, Guzmán-Ramírez BG, Sapién-Fernández JH, Guzmán-Ruvalcaba MJ, Nájar-Hinojosa R, Ochoa-Rodriguez I, Cueto-Valadez TA, Cueto-Valadez AE, Fuentes-Orozco C, Cortés-Flores AO, Miranda-Ackerman RC, Cervantes-Cardona GA, Cervantes-Guevara G, González-Ojeda A. Depression, anxiety, and academic performance in COVID-19: a cross-sectional study. BMC Psychiatry. 2022;22:443. doi: 10.1186/s12888-022-04062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bountress KE, Cusack SE, Conley AH, Aggen SH The Spit For Science Working Group. Vassileva J, Dick DM, Amstadter AB. The COVID-19 pandemic impacts psychiatric outcomes and alcohol use among college students. Eur J Psychotraumatol. 2022;13:2022279. doi: 10.1080/20008198.2021.2022279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chinawa A, Aronu A, Ossai E, Chinawa J. Promotive factors associated with internalising symptoms amongst college students during the COVID-19 lockdown in Enugu metropolis, Nigeria. S Afr J Psychiatr. 2022;28:1672. doi: 10.4102/sajpsychiatry.v28i0.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bashkin O, Shapovalov N, Faingersch E, Abramov L. Mental health among college students a year after COVID-19 outbreak in Israel: The association between wellbeing and anxiety. J Am Coll Health. 2022:1–7. doi: 10.1080/07448481.2022.2082844. [DOI] [PubMed] [Google Scholar]
- 15.Ramsay JE, Yang F, Pang JS, Lai CM, Ho RC, Mak KK. Divergent pathways to influence: Cognition and behavior differentially mediate the effects of optimism on physical and mental quality of life in Chinese university students. J Health Psychol. 2015;20:963–973. doi: 10.1177/1359105313504441. [DOI] [PubMed] [Google Scholar]
- 16.Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. 2010;46:3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. Am J Psychiatry. 1995;152:1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 18.Guan J, Wu C, Wei D, Xu Q, Wang J, Lin H, Wang C, Mao Z. Prevalence and Factors for Anxiety during the COVID-19 Pandemic among College Students in China. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18094974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tasnim R, Islam MS, Sujan MSH, Sikder MT, Potenza MN. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: Prevalence estimates and correlates. Child Youth Serv Rev. 2020;119:105703. doi: 10.1016/j.childyouth.2020.105703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garlow SJ, Rosenberg J, Moore JD, Haas AP, Koestner B, Hendin H, Nemeroff CB. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress Anxiety. 2008;25:482–488. doi: 10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- 21.Park S, Garcia-Palacios J, Cohen A, Varga Z. From treatment to prevention: The evolution of digital healthcare. Nature. 2019:573. [Google Scholar]
- 22.Philippe TJ, Sikder N, Jackson A, Koblanski ME, Liow E, Pilarinos A, Vasarhelyi K. Digital Health Interventions for Delivery of Mental Health Care: Systematic and Comprehensive Meta-Review. JMIR Ment Health. 2022;9:e35159. doi: 10.2196/35159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malatras JW, Israel AC. The influence of family stability on self-control and adjustment. J Clin Psychol. 2013;69:661–670. doi: 10.1002/jclp.21935. [DOI] [PubMed] [Google Scholar]
- 24.Bögels SM, van Dongen L, Muris P. Family influences on dysfunctional thinking in anxious children: Family Influences on Dysfunctional Thinking. Inf Child Develop. 2003;12:243–52. [Google Scholar]
- 25.Salami TK, Walker RL. Socioeconomic Status and Symptoms of Depression and Anxiety in African American College Students: The Mediating Role of Hopelessness. J Black Psy. 2014;40:275–290. [Google Scholar]
- 26.Muntaner C, Eaton WW, Miech R, O'Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- 27.Simić-Vukomanović I, Mihajlović G, Kocić S, Djonović N, Banković D, Vukomanović V, Djukić-Dejanović S. The prevalence and socioeconomic correlates of depressive and anxiety symptoms in a group of 1,940 Serbian university students. Vojnosanit Pregl. 2016;73:169–177. doi: 10.2298/vsp141106143s. [DOI] [PubMed] [Google Scholar]
- 28.Chen L, Wang L, Qiu XH, Yang XX, Qiao ZX, Yang YJ, Liang Y. Depression among Chinese university students: prevalence and socio-demographic correlates. PLoS One. 2013;8:e58379. doi: 10.1371/journal.pone.0058379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: variation across student subgroups and across campuses. J Nerv Ment Dis. 2013;201:60–67. doi: 10.1097/NMD.0b013e31827ab077. [DOI] [PubMed] [Google Scholar]
- 30.Mancevska S, Bozinovska L, Tecce J, Pluncevik-Gligoroska J, Sivevska-Smilevska E. Depression, anxiety and substance use in medical students in the Republic of Macedonia. Bratisl Lek Listy. 2008;109:568–572. [PubMed] [Google Scholar]
- 31.Weich S, Lewis G. Material standard of living, social class, and the prevalence of the common mental disorders in Great Britain. J Epidemiol Community Health. 1998;52:8–14. doi: 10.1136/jech.52.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wender PH, Rosenthal D, Kety SS, Schulsinger F, Welner J. Social class and psychopathology in adoptees. A natural experimental method for separating the roles of genetic and experimential factors. Arch Gen Psychiatry. 1973;28:318–325. doi: 10.1001/archpsyc.1973.01750330020003. [DOI] [PubMed] [Google Scholar]
- 33.Hollingshead AB, Redlich FC. Social class and mental illness: a community study. 1958. Am J Public Health. 2007;97:1756–1757. doi: 10.2105/ajph.97.10.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. N Engl J Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 36.Gao D, Xiang Q, Lu G, Tong J, Jiang W, Yu X, Wang R, Lv Z, Li D. Evaluation and analysis of anxiety and depression symptoms for college students during COVID-19 pandemic. BMC Psychol. 2022;10:227. doi: 10.1186/s40359-022-00934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torales J, O'Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- 38.Christensen H, Jorm AF, Mackinnon AJ, Korten AE, Jacomb PA, Henderson AS, Rodgers B. Age differences in depression and anxiety symptoms: a structural equation modelling analysis of data from a general population sample. Psychol Med. 1999;29:325–339. doi: 10.1017/s0033291798008150. [DOI] [PubMed] [Google Scholar]
- 39.Cornine A. Reducing Nursing Student Anxiety in the Clinical Setting: An Integrative Review. Nurs Educ Perspect. 2020;41:229–234. doi: 10.1097/01.NEP.0000000000000633. [DOI] [PubMed] [Google Scholar]
- 40.Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu H, Liu X, Xu W. Prevalence and influencing factors of anxiety in medical students during the COVID-19 pandemic. Heliyon. 2022;8:e10487. doi: 10.1016/j.heliyon.2022.e10487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Elizabeth H, Eustis , Sarah , Krill , Williston , Lucas PK, Morgan , Jessica , R , Graham , Sarah A, Hayes-Skelton , Lizabeth , Roemer Development, Acceptability, and Effectiveness of an Acceptance-Based Behavioral Stress/Anxiety Management Workshop for University Students. Cog Behav Practice . 2017:174–186. [Google Scholar]
- 43.Ding L, Gao X, Zheng HW. Analysis on Influence of Interior Environment of Certain Missile Chassis on Driving Reliability. Bingqi Zhuangbei Gongcheng Xuebao. 2015;3:28–30. [Google Scholar]
- 44.Brown B. Adolescents’ relationships with peers. In R. Lerner & L. Steinberg (Eds.), Handbook of adolescent psychology. New York: Wiley, 2004: 363–394. [Google Scholar]
- 45.Steinberg L, Monahan KC. Age differences in resistance to peer influence. Dev Psychol. 2007;43:1531–1543. doi: 10.1037/0012-1649.43.6.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Margo C, Villarosa , Saarah , Danielle , Kison , Michael B, Madson , Virgil , Zeigler-Hill Everyone else is doing it: examining the role of peer influence on the relationship between social anxiety and alcohol use behaviours. Addic Rese Theory. 2016;24:124–134. [Google Scholar]
- 47.Kenney SR, DiGuiseppi GT, Meisel MK, Balestrieri SG, Barnett NP. Poor mental health, peer drinking norms, and alcohol risk in a social network of first-year college students. Addict Behav. 2018;84:151–159. doi: 10.1016/j.addbeh.2018.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gilbert W, Bureau JS, Poellhuber B, Guay F. Predicting college students' psychological distress through basic psychological need-relevant practices by teachers, peers, and the academic program. Motiv Emot . 2021;45:436–55. [Google Scholar]
- 49.Karanikola MNK, Lyberg A, Holm AL, Severinsson E. The Association between Deliberate Self-Harm and School Bullying Victimization and the Mediating Effect of Depressive Symptoms and Self-Stigma: A Systematic Review. Biomed Res Int. 2018;2018:4745791. doi: 10.1155/2018/4745791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bond L, Carlin JB, Thomas L, Rubin K, Patton G. Does bullying cause emotional problems? BMJ. 2001;323:480–484. doi: 10.1136/bmj.323.7311.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yu Q, Wu S, Twayigira M, Luo X, Gao X, Shen Y, Long Y, Huang C. Prevalence and associated factors of school bullying among Chinese college students in Changsha, China. J Affect Disord. 2022;297:62–67. doi: 10.1016/j.jad.2021.10.010. [DOI] [PubMed] [Google Scholar]
- 52.Hossain S, Anjum A, Uddin ME, Rahman MA, Hossain MF. Impacts of socio-cultural environment and lifestyle factors on the psychological health of university students in Bangladesh: A longitudinal study. J Affect Disord. 2019;256:393–403. doi: 10.1016/j.jad.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 53.Hajduk M, Heretik A Jr, Vaseckova B, Forgacova L, Pecenak J. Prevalence and correlations of depression and anxiety among Slovak college students. Bratisl Lek Listy. 2019;120:695–698. doi: 10.4149/BLL_2019_117. [DOI] [PubMed] [Google Scholar]
- 54.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Dev Psychol. 1986;22:723–742. [Google Scholar]
- 55.Ge M, Sun X, Huang Z. Correlation between Parenting Style by Personality Traits and Mental Health of College Students. Occup Ther Int. 2022;2022:6990151. doi: 10.1155/2022/6990151. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 56.Ladge JJ, Little LM. When Expectations Become Reality: Work-Family Image Management and Identity Adaptation. AMR. 2019;44:126–49. [Google Scholar]
- 57.Cheng S, Jia C, Wang Y. Only Children Were Associated with Anxiety and Depressive Symptoms among College Students in China. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17114035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Feng L, Zhang L, Zhong H. Perceived Parenting Styles and Mental Health: The Multiple Mediation Effect of Perfectionism and Altruistic Behavior. Psychol Res Behav Manag. 2021;14:1157–1170. doi: 10.2147/PRBM.S318446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cui M. Understanding Parenting Influence on Chinese University Students’ Well-Being. Asian J Soc Sci . 2017;45:465–482. [Google Scholar]
- 60.Aloia LS. The influence of family relationship schemas, parental support, and parental verbal aggression on mental well-being. J Family Stud. 2022;28:294–307. [Google Scholar]
- 61.Song HT, Ge CH, Chang LX, Zhao TT, Wu W, Ge DX, Zhai CP, Zhang XL. Investigation on the psychological status of college students during the coronavirus disease-2019 epidemic. J Gen Psychol. 2022;149:456–467. doi: 10.1080/00221309.2021.1893637. [DOI] [PubMed] [Google Scholar]
- 62.Zeng Y, Ye B, Zhang Y, Yang Q. Family Cohesion and Stress Consequences Among Chinese College Students During COVID-19 Pandemic: A Moderated Mediation Model. Front Public Health. 2021;9:703899. doi: 10.3389/fpubh.2021.703899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Guassi Moreira JF, Telzer EH. Changes in family cohesion and links to depression during the college transition. J Adolesc. 2015;43:72–82. doi: 10.1016/j.adolescence.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 64.Sheidow AJ, Henry DB, Tolan PH, Strachan MK. The Role of Stress Exposure and Family Functioning in Internalizing Outcomes of Urban Families. J Child Fam Stud. 2014;23:1351–1365. doi: 10.1007/s10826-013-9793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yang F, Meng H, Chen H, Xu XH, Liu Z, Luo A, Feng ZC. Influencing factors of mental health of medical students in China. J Huazhong Univ Sci Technolog Med Sci. 2014;34:443–449. doi: 10.1007/s11596-014-1298-9. [DOI] [PubMed] [Google Scholar]
- 66.Chu Y, Zhang Y, Yang D, Wang S, Liang C, Wang X, Dai H. Influence of family function on social anxiety among Chinese nursing students: The mediating role of alexithymia. Nurs Open. 2022 doi: 10.1002/nop2.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cohen S, Kessler R, Gordon LG. Strategies for measuring stress in studies of psychiatric and physical disorder. 1995. Available from: https://www.researchgate.net/publication/247654118_Strategies_for_measuring_stress_in_studies_of_psychiatric_and_physical_disorder .
- 68.Kessler RC, Sampson NA, Berglund P, Gruber MJ, Al-Hamzawi A, Andrade L, Bunting B, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, He Y, Hu C, Huang Y, Karam E, Kovess-Masfety V, Lee S, Levinson D, Medina Mora ME, Moskalewicz J, Nakamura Y, Navarro-Mateu F, Browne MA, Piazza M, Posada-Villa J, Slade T, Ten Have M, Torres Y, Vilagut G, Xavier M, Zarkov Z, Shahly V, Wilcox MA. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol Psychiatr Sci. 2015;24:210–226. doi: 10.1017/S2045796015000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gao WJ, Luo YF, Cao XJ, Liu XQ. Gender differences in the relationship between self-esteem and depression among college students: A cross-lagged study from China. J Res Pers. 2022;97:104202. [Google Scholar]
- 70.Hankin BL, Abramson LY. Development of gender differences in depression: description and possible explanations. Ann Med. 1999;31:372–379. doi: 10.3109/07853899908998794. [DOI] [PubMed] [Google Scholar]
- 71.Abdel Wahed WY, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria J Med. 2017;53:77–84. [Google Scholar]
- 72.Baroni A, Bruzzese JM, Di Bartolo CA, Ciarleglio A, Shatkin JP. Impact of a sleep course on sleep, mood and anxiety symptoms in college students: A pilot study. J Am Coll Health. 2018;66:41–50. doi: 10.1080/07448481.2017.1369091. [DOI] [PubMed] [Google Scholar]
- 73.Shokrkon A, Nicoladis E. How personality traits of neuroticism and extroversion predict the effects of the COVID-19 on the mental health of Canadians. PLoS One. 2021;16:e0251097. doi: 10.1371/journal.pone.0251097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu X, Cao X, Gao W. Does Low Self-Esteem Predict Anxiety Among Chinese College Students? Psychol Res Behav Manag. 2022;15:1481–1487. doi: 10.2147/PRBM.S361807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huang J, Nigatu YT, Smail-Crevier R, Zhang X, Wang J. Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. J Psychiatr Res. 2018;107:1–10. doi: 10.1016/j.jpsychires.2018.09.018. [DOI] [PubMed] [Google Scholar]
- 76.Fitzsimmons-Craft EE, Taylor CB, Newman MG, Zainal NH, Rojas-Ashe EE, Lipson SK, Firebaugh ML, Ceglarek P, Topooco N, Jacobson NC, Graham AK, Kim HM, Eisenberg D, Wilfley DE. Harnessing mobile technology to reduce mental health disorders in college populations: A randomized controlled trial study protocol. Contemp Clin Trials. 2021;103:106320. doi: 10.1016/j.cct.2021.106320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Goozee R, Barrable A, Lubenko J, Papadatou-Pastou M, Haddad M, McKeown E, Hirani SP, Martin M, Tzotzoli P. Investigating the feasibility of MePlusMe, an online intervention to support mental health, well-being, and study skills in higher education students. J Ment Health. 2022:1–11. doi: 10.1080/09638237.2022.2069699. [DOI] [PubMed] [Google Scholar]
- 78.Karyotaki E, Klein AM, Riper H, Wit L, Krijnen L, Bol E, Bolinski F, Burger S, Ebert DD, Auerbach RP, Kessler RC, Bruffaerts R, Batelaan N, van der Heijde CM, Vonk P, Kleiboer A, Wiers RW, Cuijpers P. Examining the effectiveness of a web-based intervention for symptoms of depression and anxiety in college students: study protocol of a randomised controlled trial. BMJ Open. 2019;9:e028739. doi: 10.1136/bmjopen-2018-028739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Falsafi N. A Randomized Controlled Trial of Mindfulness Versus Yoga: Effects on Depression and/or Anxiety in College Students. J Am Psychiatr Nurses Assoc. 2016;22:483–497. doi: 10.1177/1078390316663307. [DOI] [PubMed] [Google Scholar]
- 80.Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 81.Liu XQ, Guo YX, Zhang WJ, Gao WJ. Influencing factors, prediction and prevention of depression in college students: A literature review. World J Psychiatry. 2022;12:860–873. doi: 10.5498/wjp.v12.i7.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Twomey C, O'Reilly G, Byrne M. Effectiveness of cognitive behavioural therapy for anxiety and depression in primary care: a meta-analysis. Fam Pract. 2015;32:3–15. doi: 10.1093/fampra/cmu060. [DOI] [PubMed] [Google Scholar]
- 83.Sigurvinsdóttir AL, Jensínudóttir KB, Baldvinsdóttir KD, Smárason O, Skarphedinsson G. Effectiveness of cognitive behavioral therapy (CBT) for child and adolescent anxiety disorders across different CBT modalities and comparisons: a systematic review and meta-analysis. Nord J Psychiatry. 2020;74:168–180. doi: 10.1080/08039488.2019.1686653. [DOI] [PubMed] [Google Scholar]
- 84.Ștefan CA, Căpraru C, Szilágyi M. Investigating Effects and Mechanisms of a Mindfulness-Based Stress Reduction Intervention in a Sample of College Students at Risk for Social Anxiety. Mindfulness . 2018;9:1509–1521. [Google Scholar]
- 85.Lin APC, Trappey CV, Luan C-C, Trappey AJC, Tu KLK. A Test Platform for Managing School Stress Using a Virtual Reality Group Chatbot Counseling System. Applied Sci. 2021;11:9071. [Google Scholar]
- 86.Renton T, Tang H, Ennis N, Cusimano MD, Bhalerao S, Schweizer TA, Topolovec-Vranic J. Web-based intervention programs for depression: a scoping review and evaluation. J Med Internet Res. 2014;16:e209. doi: 10.2196/jmir.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Johnson KF, Kalkbrenner MT. The Utilization of Technological Innovations to Support College Student Mental Health: Mobile Health Communication. J Technol Hum Serv . 2017;35:314–339. [Google Scholar]
- 88.Sasaki M. Barriers to use of mental health services by Japanese university students. Psychol Rep. 2007;100:400–406. doi: 10.2466/pr0.100.2.400-406. [DOI] [PubMed] [Google Scholar]
- 89.Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jorm AF, Wright A, Morgan AJ. Where to seek help for a mental disorder? Med J Aust. 2007;187:556–560. doi: 10.5694/j.1326-5377.2007.tb01415.x. [DOI] [PubMed] [Google Scholar]
- 91.Lee RA, Jung ME. Evaluation of an mHealth App (DeStressify) on University Students' Mental Health: Pilot Trial. JMIR Ment Health. 2018;5:e2. doi: 10.2196/mental.8324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Herrero R, Mira A, Cormo G, Etchemendy E, Baños R, García-Palacios A, Ebert DD, Franke M, Berger T, Schaub MP, Görlich D, Jacobi C, Botella C. An Internet based intervention for improving resilience and coping strategies in university students: Study protocol for a randomized controlled trial. Internet Interv. 2019;16:43–51. doi: 10.1016/j.invent.2018.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sugarman DE, Meyer LE, Reilly ME, Rauch SL, Greenfield SF. Exploring Technology-Based Enhancements to Inpatient and Residential Treatment for Young Adult Women with Co-Occurring Substance Use. J Dual Diagn. 2021;17:236–247. doi: 10.1080/15504263.2021.1940412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bolinski F, Kleiboer A, Karyotaki E, Bosmans JE, Zarski AC, Weisel KK, Ebert DD, Jacobi C, Cuijpers P, Riper H. Effectiveness of a transdiagnostic individually tailored Internet-based and mobile-supported intervention for the indicated prevention of depression and anxiety (ICare Prevent) in Dutch college students: study protocol for a randomised controlled trial. Trials. 2018;19:118. doi: 10.1186/s13063-018-2477-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lim KL, Jacobs P, Ohinmaa A, Schopflocher D, Dewa CS. A new population-based measure of the economic burden of mental illness in Canada. Chronic Dis Can. 2008;28:92–98. [PubMed] [Google Scholar]
- 96.Oliveira C, Pereira A, Vagos P, Nóbrega C, Gonçalves J, Afonso B. Effectiveness of Mobile App-Based Psychological Interventions for College Students: A Systematic Review of the Literature. Front Psychol. 2021;12:647606. doi: 10.3389/fpsyg.2021.647606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kanuri N, Arora P, Talluru S, Colaco B, Dutta R, Rawat A, Taylor BC, Manjula M, Newman MG. Examining the initial usability, acceptability and feasibility of a digital mental health intervention for college students in India. Int J Psychol. 2020;55:657–673. doi: 10.1002/ijop.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jardine J, Bowman R, Doherty G. Digital Interventions to Enhance Readiness for Psychological Therapy: Scoping Review. J Med Internet Res. 2022;24:e37851. doi: 10.2196/37851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Warwick K, Shah H. Good machine performance in turing’s imitation game. IEEE Trans. 2014;6:289–299. [Google Scholar]
- 100.Abdul-Kader SA, Woods J. Survey on Chatbot Design Techniques in Speech Conversation Systems. ijacsa . 2015:6. [Google Scholar]
- 101.Fulmer R. Artificial intelligence and counseling: Four levels of implementation. Theory & Psy. 2019;29:807–819. [Google Scholar]
- 102.Dekker I, De Jong EM, Schippers MC, De Bruijn-Smolders M, Alexiou A, Giesbers B. Optimizing Students' Mental Health and Academic Performance: AI-Enhanced Life Crafting. Front Psychol. 2020;11:1063. doi: 10.3389/fpsyg.2020.01063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Topooco N, Fowler LA, Fitzsimmons-Craft EE, DePietro B, Vázquez MM, Firebaugh ML, Ceglarek P, Monterubio G, Newman MG, Eisenberg D, Wilfley DE, Taylor CB. Digital interventions to address mental health needs in colleges: Perspectives of student stakeholders. Internet Interv. 2022;28:100528. doi: 10.1016/j.invent.2022.100528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lattie EG, Lipson SK, Eisenberg D. Technology and College Student Mental Health: Challenges and Opportunities. Front Psychiatry. 2019;10:246. doi: 10.3389/fpsyt.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Akbarialiabad H, Bastani B, Taghrir MH, Paydar S, Ghahramani N, Kumar M. Threats to Global Mental Health From Unregulated Digital Phenotyping and Neuromarketing: Recommendations for COVID-19 Era and Beyond. Front Psychiatry. 2021;12:713987. doi: 10.3389/fpsyt.2021.713987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Inkster B, O'Brien R, Selby E, Joshi S, Subramanian V, Kadaba M, Schroeder K, Godson S, Comley K, Vollmer SJ, Mateen BA. Digital Health Management During and Beyond the COVID-19 Pandemic: Opportunities, Barriers, and Recommendations. JMIR Ment Health. 2020;7:e19246. doi: 10.2196/19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hoffman L, Wisniewski H, Hays R, Henson P, Vaidyam A, Hendel V Autonomy , Relatedness , and Alliance for Those With Serious Mental Illness. et al Digital Opportunities for Outcomes in Recovery Services (DOORS): A Pragmatic Hands-On Group Approach Toward Increasing Digital Health and Smartphone Competencies. J Psychiatr Pract 2020; 26: 80-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ganapathy K. Telemedicine and Neurological Practice in the COVID-19 Era. Neurol India. 2020;68:555–559. doi: 10.4103/0028-3886.288994. [DOI] [PubMed] [Google Scholar]
- 109.Gooding P. Mapping the rise of digital mental health technologies: Emerging issues for law and society. Int J Law Psychiatry. 2019;67:101498. doi: 10.1016/j.ijlp.2019.101498. [DOI] [PubMed] [Google Scholar]
- 110.Carl JR, Jones DJ, Lindhiem OJ, Doss BD, Weingardt KR, Timmons AC, Comer JS. Regulating digital therapeutics for mental health: Opportunities, challenges, and the essential role of psychologists. Br J Clin Psychol. 2022;61 Suppl 1:130–135. doi: 10.1111/bjc.12286. [DOI] [PubMed] [Google Scholar]
- 111.Topooco N, Riper H, Araya R, Berking M, Brunn M, Chevreul K, Cieslak R, Ebert DD, Etchmendy E, Herrero R, Kleiboer A, Krieger T, García-Palacios A, Cerga-Pashoja A, Smoktunowicz E, Urech A, Vis C, Andersson G E-COMPARED consortium. Attitudes towards digital treatment for depression: A European stakeholder survey. Internet Interv. 2017;8:1–9. doi: 10.1016/j.invent.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Meng J, Hussain SA, Mohr DC, Czerwinski M, Zhang M. Exploring User Needs for a Mobile Behavioral-Sensing Technology for Depression Management: Qualitative Study. J Med Internet Res. 2018;20:e10139. doi: 10.2196/10139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Addington J, Collins A, McCleery A, Addington D. The role of family work in early psychosis. Schizophr Res. 2005;79:77–83. doi: 10.1016/j.schres.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 114.Glick ID, Stekoll AH, Hays S. The role of the family and improvement in treatment maintenance, adherence, and outcome for schizophrenia. J Clin Psychopharmacol. 2011;31:82–85. doi: 10.1097/JCP.0b013e31820597fa. [DOI] [PubMed] [Google Scholar]
- 115.Pharoah F, Mari J, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database Syst Rev. 2010:CD000088. doi: 10.1002/14651858.CD000088.pub2. [DOI] [PubMed] [Google Scholar]
- 116.Porche MV, Folk JB, Tolou-Shams M, Fortuna LR. Researchers' Perspectives on Digital Mental Health Intervention Co-Design With Marginalized Community Stakeholder Youth and Families. Front Psychiatry. 2022;13:867460. doi: 10.3389/fpsyt.2022.867460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cao XJ, Liu XQ. Artificial intelligence-assisted psychosis risk screening in adolescents: Practices and challenges. World J Psychiatry. 2022;12:1287–1297. doi: 10.5498/wjp.v12.i10.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Melcher J, Hays R, Torous J. Digital phenotyping for mental health of college students: a clinical review. Evid Based Ment Health. 2020;23:161–166. doi: 10.1136/ebmental-2020-300180. [DOI] [PMC free article] [PubMed] [Google Scholar]