Abstract
Physician burnout is recognized as a global crisis and an epidemic. However, burnout in rheumatology is an understudied phenomenon. We explored the prevalence of physician burnout among rheumatologists from South Asia in the peri-pandemic period (2021–2022). Rheumatologists from Asian countries were invited to participate in an anonymized, validated, and pilot-tested e-survey via social media platforms from December 2021 to April 2022. Demographic information, social aspects (marital status, income, vacation time, daily exercise), substance abuse, EHR (electronic health record) use, and years in practice were obtained. In addition, burnout was estimated using Maslach Burnout Inventory-Human Services Survey for Medical Personnel (MBI-HSS) in three domains: emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA), and intergroup comparisons were made using independent t test and one-way ANOVA using SPSS v27. Of 146 respondents who participated in the survey, 134 belonged to Asian nations. The highest number of respondents was from Pakistan (56/134, 38.36%), followed by India (49/134, 33.56%). Slightly more respondents were male, 75 (51.4%), than females, 71 (48.6%). Over two-thirds of our respondents (99/134, 67.8%) reported burnout in at least one domain. Notably, we found statistically significant increased depersonalization scores in males. (P < 0.05). Females scored significantly higher on the following items: #5 (I feel I treat some patients as if they were impersonal objects), item# 10 (I've become more insensitive toward people since I took this job and item#22 (I feel patients blame me for some of their problems) (P < 0.05). We found differences in monthly salaries among South Asian (1484 ± 2717 USD) and non-South Asian respondents (5672 ± 8874 USD) (P < 0.01). A substantial proportion of rheumatologists in our survey report burnout, suggesting a felt need to introduce organizational measures to prevent and mitigate burnout and preserve the rheumatology workforce.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00296-023-05304-7.
Keywords: Professional burnout, Occupational burnout, Mental health, Rheumatologists, Asia, South Asia, Surveys and questionnaires, COVID-19, Pandemic
Introduction
Burnout is classified by the World Health Organization as an occupational syndrome resulting from poorly managed workplace stress, characterized by exhaustion, feelings of cynicism, and reduced professional efficacy [1]. Physician burnout is associated with job dissatisfaction [2] and a decline in practitioners' mental and physical well-being [3, 4]. In addition, burnout can result in poor quality of healthcare [5, 6] and reduces the efficacy of healthcare systems due to prescription errors [7].
Recently, physician burnout has been increasingly recognized as a global crisis and an epidemic [8]. It is estimated that the prevalence of physician burnout ranges from 0 to 80.5% [9]. However, burnout in rheumatology is an understudied phenomenon. Although rheumatology is considered a low-risk specialty, it is estimated that half of all rheumatologists in the Western world suffer from burnout [10–12]. Younger age, extended working hours, low income, low self-esteem, and dissatisfaction with electronic health records (EHR) are some risk factors for burnout identified in various studies [10, 12]. Given that sociodemographic construct and health economics are expected to have an outsized impact on mental health, we hypothesize that burnout prevalence and extent may differ in Asia, particularly in the South Asian region, a conglomerate of Asian countries in the lower and middle-income countries (LMIC) bracket, and due to unique healthcare pressures in the peri-pandemic period [13].
Existent literature acknowledges the scarcity of data on physician burnout from LMIC [8]. Besides one study from Latin America [12], most of the data on burnout in rheumatology emerges from developed countries such as the USA [10, 14, 15] and Canada [11]. Unlike the developed countries, the healthcare workforce in Asia is a heterogenous population faced with unique challenges [16, 17]. Even though Asia is home to some of the most densely populated countries, it faces multiple challenges such as a rheumatology workforce shortage [18] and widespread gender disparities [19]. Consequently, the prevalence of burnout among rheumatologists in Asia could differ from those in developed countries. Currently, there are no studies on rheumatologist burnout from Asia in general and South Asia in specific. To explore the prevalence of burnout, we invited Asian rheumatologists to participate in an online survey.
Methods
We designed a self-reported electronic survey based on a demographic questionnaire and a standardized tool, Maslach Burnout Inventory-Human Services Survey for Medical Personnel (MBI-HSS). Demographic information included age, sex, marital status, tobacco use, EHR (Electronic health record) use, income, exercise, vacation time, and years in practice. We adapted some items on the demographic questionnaire from Tiwari et al. [10]. All items from the MBI-HSS were included. All questions were in English.
The MBI-HSS is the most widely used tool to assess physician burnout [20]. It is based on 22 items scored from 0 to 6 on a Likert scale. There are three domains of the MBI-HSS—emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA). EE scores of ≥ 27, DP scores of ≥ 10, and PA scores of ≤ 33 are considered positive for burnout. Two rheumatologists reviewed the questions for face validity. In addition, pilot testing was done using dummy completions with 25 people to identify errors and critically evaluate face validity.
Inclusion criteria were rheumatologist physicians and trainees of any age and gender practicing in Asian countries, from all settings (public, private hospital/clinic, or university) and experience level. Non-rheumatologist physicians and other rheumatology healthcare professionals (e.g., nurses, physiotherapists, occupational therapists or physician assistants) were excluded. We used convenience sampling to enroll participants. The survey was disseminated through various means, including emails to rheumatologists, personal contacts, and word of mouth. In addition, we used social media platforms, including Twitter, Facebook, and WhatsApp groups to spread the survey.
The survey was hosted online using google forms and was initiated in December 2021. Due to lower response rate, we decided to extend the survey to April 2022 and also allowed responses from rheumatologists from other parts of the globe. To improve response rates, we repeated reminders through emails and social media posts; however, no incentives were offered for survey completion.
Before conducting the survey, ethical approval was obtained from the ethical review board of the Pakistan Institute of Medical Sciences, Islamabad, Pakistan. Explanations were provided in the cover letter of the survey, including its purpose, content, and informed consent for publication of results. The survey was fully anonymized to protect participant information. We adhered to the "Checklist for Reporting Results of Internet E-Surveys" protocols in data reporting [21].
Statistical analyses were performed using SPSS V27. Categorical variables were presented as frequencies and percentages, while continuous variables were presented as means and medians with standard deviation. We used the Pearson Chi-square test to compare differences in the proportions of categorical variables. The normality of distribution was tested using the Shapiro–Wilk test. We compared the mean burnout scores between gender, regions, marital status, smoking status, EHR use, and practice type using the independent t-test and Mann–Whitney U test. We also compared burnout scores between countries, age groups, number of days exercised in a week, number of vacations taken in a year, and years in practice in rheumatology using One-Way ANOVA and the Kruskal–Wallis test. Medians were compared using K sample median test. The statistical significance was set at a value of < 0.05. Incomes were obtained in local currencies and were converted into USD using an online exchange platform (https://www.exchangerates.org.uk/).
Results
Among 146 respondents, a substantial proportion (136, 93.2%) belonged to Asian-Pacific nations, while 10 (6.8%) were from other countries. There was an over-representation of South Asians among our survey respondents (113, 77.4%). The highest number of respondents was from Pakistan (56, 38.4%), followed by India (49, 33.6%). The complete list of respondent countries and their proportions are in the supplementary table 1. There were slightly more male respondents (75, 51.4%) than females (71, 48.6%). Most respondents were married (87.7%) and non-smokers (95.2). The median monthly salary of our respondents was 1,768 USD, with 267 USD reported as the minimum and 40,871 USD reported as the maximum. The demographic and baseline characteristics of the respondents are summarized in Table 1.
Table 1.
Demographics and baseline characteristics of respondents
| Parameter | Frequency (n = 146) |
|---|---|
| Median age (years) | 39 ± 7.7 |
| Gender | |
| Female | 75 (51.4%) |
| Male | 71 (48.6%) |
| Marital Status | |
| Married | 128 (87.7%) |
| Single | 15 (10.3%) |
| Divorced | 3 (2.1%) |
| Respondents by regions | |
| Asia–Pacific | 136 (93.2%) |
| Africa | 5 (3.4%) |
| Others | 5 (3.4%) |
| Respondents by countries | |
| Pakistan | 56 (38.4%) |
| India | 49 (33.6%) |
| Others | 41 (28.0%) |
| Training status | |
| Specialist | 109 (74.7%) |
| Fellow | 37 (25.3%) |
| Practice type | |
| Public hospital | 75 (51.4%) |
| Private hospital | 59 (40.4%) |
| Academic university | 47 (32.2%) |
| Private clinic | 41 (28.1%) |
| Years in rheumatology practice | |
| 0–5 years | 69 (47.3%) |
| 6–10 years | 44 (30.1%) |
| 11–15 years | 14 (9.6%) |
| 16–20 years | 9 (6.2%) |
| 21–25 years | 5 (3.4%) |
| > 25 years | 5 (3.4%) |
| EHR use | |
| Yes | 77 (52.7%) |
| No | 69 (47.3%) |
| Monthly income (USD) | |
| Median | 1,768 ± 5,051.314 |
| Range | 267 ± 40,871 |
| 200–499 USD | 13 (9.4%) |
| 500–999 USD | 35 (25.4%) |
| 1000–2499 USD | 37 (26.8%) |
| 2500–4999 USD | 27 (19.6%) |
| 5000–9999 USD | 14(10.1%) |
| > 10,000 USD | 12 (8.7%) |
| Exercise (days/week) | |
| 0–1 days | 49 (37.1%) |
| 2–4 days | 65 (49.2%) |
| > 5 days | 18(13.6%) |
| Vacation (week/year) | |
| ≤ 1 week | 48 (32.9%) |
| 2 weeks | 43 (29.5%) |
| 3 weeks | 17 (11.6%) |
| 4 weeks | 18 (12.3%) |
| 5 weeks | 8 (5.5%) |
| > 5 weeks | 12 (8.2%) |
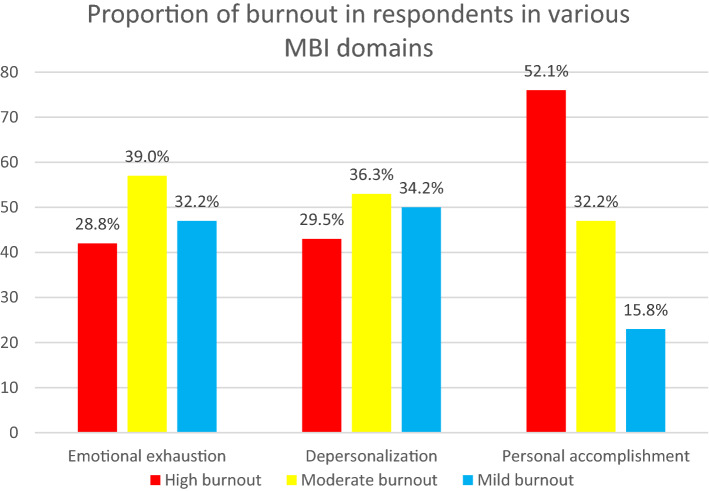
Nearly two-thirds of respondents (99, 67.8%) reported burnout in at least one domain, and about one-third (52, 34.9%) reported burnout in two domains. The most frequent type of burnout experienced by the respondents was in the PA domain (76, 52.1%), followed by DP (43, 29.5%) and EE (42, 28.8%) (Fig. 1).
Fig. 1.
Proportion of burnout in respondents in various MBI domains
A significant difference was found between the proportion of respondents suffering from DP and EE (P < 0.05) and DP and PA (P < 0.05) but not between the proportion of respondents suffering from EE and PA (supplementary table 1). In addition, we found differences in the mean depersonalization scores between males and females (P < 0.05) (Table 2).
Table 2.
Comparison of burnout scores between different correspondent characteristics
| Characteristics | P value | ||
|---|---|---|---|
| Gender | Female | Male | |
| EE | 23.51 | 23.95 | 0.818 |
| DP | 7.30 | 9.72 | < 0.05 |
| PA | 33.20 | 32.59 | 0.620 |
| Region | Asian-Pacific | Non-Asian-Pacific | |
| EE | 23.22 | 29.50 | 0.070 |
| DP | 8.60 | 7.92 | 0.683 |
| PA | 32.99 | 31.67 | 0.554 |
| Marital status | Single | Married | |
| EE | 22.87 | 23.96 | 0.731 |
| DP | 11.27 | 8.29 | 0.089 |
| PA | 30.00 | 33.04 | 0.131 |
| EHR use | No | Yes | |
| EE | 24.28 | 23.25 | 0.591 |
| DP | 8.52 | 8.56 | 0.968 |
| PA | 32.49 | 33.23 | 0.548 |
| Smoking status | Non-smoker | Smoker | |
| EE | 23.77 | 20.40 | 0.521 |
| DP | 8.59 | 6.20 | 0.344 |
| PA | 33.01 | 34.20 | 0.719 |
| Type of practice | Public hospital | All others | |
| EE | 23.76 | 23.70 | 0.977 |
| DP | 8.51 | 8.58 | 0.938 |
| PA | 32.57 | 33.21 | 0.638 |
| Type of practice | Private hospital | All others | |
| EE | 23.69 | 23.76 | 0.974 |
| DP | 8.10 | 8.84 | 0.429 |
| PA | 33.29 | 32.61 | 0.588 |
| Type of practice | Private clinic | ||
| EE | 23.83 | 23.70 | 0.950 |
| DP | 7.46 | 8.96 | 0.140 |
| PA | 33.05 | 32.82 | 0.867 |
| Type of practice | Academic/university | All others | |
| EE | 24.02 | 23.13 | 0.663 |
| DP | 8.82 | 7.96 | 0.379 |
| PA | 32.82 | 33.02 | 0.877 |
| Qualification status | Specialist | Trainee | |
| EE | 24.34 | 21.95 | 0.276 |
| DP | 8.63 | 8.27 | 0.730 |
| PA | 32.80 | 33.14 | 0.812 |
EE emotional exhaustion, DP depersonalization, PA personal accomplishment
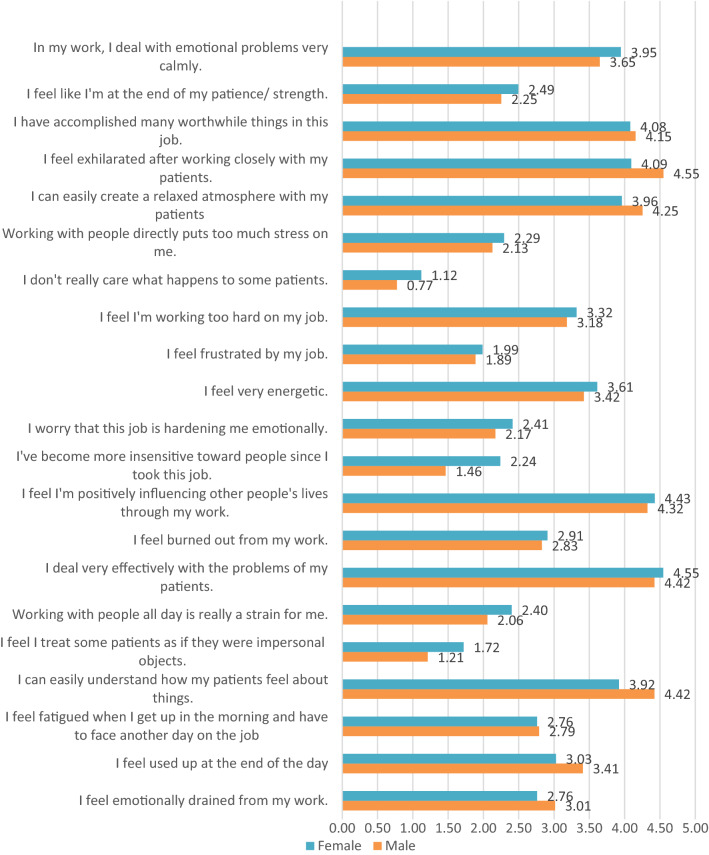
We compared the characteristics of male and female respondents in our survey (supplementary table 2) and the response to each component of the MBI-HSS (Fig. 2). More females (10/71, 14.1%) were single compared to males (5/75, 6.7%). Among the responses to the MBI-HSS questions, females scored significantly higher on the following items: #5 (I feel I treat some patients as if they were impersonal objects), item# 10 (I've become more insensitive toward people since I took this job and item#22 (I feel patients blame me for some of their problems) (P < 0.05). Males scored significantly higher on item #4 (I can easily understand how my patients feel about things) (P < 0.05) (supplementary table 5).
Fig. 2.
Mean gender differences in responses to the question “describe how frequently you feel that way on a scale of 0 to 6, where zero describes you never had this feeling and 6 describes you had this feeling every day”
We also compared median monthly salaries among correspondent categories (supplementary table 3). We found differences in monthly salaries among South Asian (1484 ± 2717 USD) and non-South Asian respondents (5672 ± 8874 USD) (P < 0.01). We also noted differences in median monthly wages of rheumatologists from Pakistan (673 ± 1570 USD, India (2720 ± 3119 USD), and other countries (3869 ± 8313 USD) (P < 0.01).
Discussion
In this study, we report the prevalence of physician burnout among South Asian rheumatologists. To our knowledge, this is the first insight into rheumatologist burnout in Asia. Our study reveals a higher prevalence of burnout than previously reported (67.8%). A significant proportion of our survey respondents were young and early carrier rheumatologists. These contribute to burnout, as appreciated in other studies [12, 14, 22]. However, we could not find statistically significant differences in burnout scores among age groups and years in rheumatology practice among our respondents.
Burnout affects physicians around the globe. Its presence has consequences pertaining to patient care, physician health, the physician workforce, and the healthcare systems. Work-related stressors such as record keeping, long working hours and administrative tasks, and individual factors such as age, sex, and years in clinical practice may contribute to burnout [22]. In concurrent times, the COVID-19 pandemic has contributed significantly to the rise of burnout among frontline specialties [23].
Physician burnout is on the rise. Physician Burnout and Depression Report 2022, published by Medscape, suggests an increase in burnout from 42% in 2021 to 47% in 2022 [24]. Emergency medicine, critical care, obstetrics, and gynecology have been reported as the most burned-out specialties in 2022. While traditionally, rheumatology is considered a low-burnout specialty; it was among the top burned-out specialties in 2021, with 50% reporting burnout [25]. The prevalence of rheumatologist burnout was 54% in a survey from the USA [10]. Similar results were reported from Canada (51%) [11] and Latin America (56.5%) [12].
We observed higher depersonalization scores in male respondents in our survey. Such observations were also made in other studies of physician burnout [26, 27]. Increased burnout among singles compared to married has been reported in studies of burnout from Asian countries [26, 28]. Low income is another factor potentially associated with burnout [12, 28]. We identified that 35% of our respondents make less than 1000 USD a month, which is way lower than the average salary reported in Latin America and the USA [12, 29].
Besides increased depersonalization scores in males, we also observed that males scored higher on one item on the MBI-HSS, while females scored higher on three items. These findings suggest that there may be gender differences in how practitioners experience burnout. They may also indicate different challenges and stressors faced by both sexes, calling for further investigation and targeted interventions. Differences in salaries among rheumatologists may have implications for workforce retention and recruitment.
The global rheumatology workforce is facing several challenges. The shortage of rheumatologists in developed countries like the USA and Canada is a potential contributor to the prevalence of burnout. This workforce shortage is anticipated to worsen in the coming years [11, 30, 31]. While we do not have recent data from Asia, a report published in 2015 revealed only a 100 recognized rheumatologists working around that time in India and about 20 in Pakistan [18]. The situation in China seems to be no different [32]. Several solutions have been proposed to meet the workforce shortage, such as training nurse practitioners and physician assistants and enhancing interest in rheumatology training [30].
The high prevalence of burnout in our study suggests the need to explore the causes of burnout in Asian rheumatologists and address them. These results may reflect widespread disparities and broader challenges faced by Asian rheumatologists. We also identified individuals with severe burnout (reported in more than one domain) who needed urgent intervention. Strategies to prevent and mitigate burnout are essential to curb this challenge. On the individual level, stress management, resilience training, positive coping strategies, and mindfulness are some proposed solutions. Other self-care practices, such as regular exercise [33], healthy eating [34], and adequate rest [35], can also be helpful.
The presence of differences in burnout between male and female rheumatologists suggests that gender-specific interventions may be necessary to address burnout effectively. Targeted support groups or workshops that address gender-related stressors in the workplace can be helpful. Our results also suggest income disparities between respondent subgroups. To promote equity and burnout, organizations should ensure that rheumatologists are adequately compensated for their work, and that disparities in salaries are addressed.
Organizations should also not lag in producing physician-friendly policies by providing resources for stress management, offering training and education on coping strategies, promoting work–life balance, and communicating and collaborating among colleagues. They should also take steps to define duty hour limits, appropriate distribution of job roles, encourage physician leadership and shared decision making [22].
It is reassuring to see many global and national initiatives to curb the epidemic of physician burnout. Ending Clinician Burnout Global community is one initiative working toward preventing and reversing physician burnout [36]. In the USA, the Health Resources and Services Administration is awarding over 100 million USD in grants to combat physician burnout and promote mental well-being among physicians [37]. Given the deep-rooted consequences of burnout and the alarmingly high prevalence of burnout in our study, we call upon all stakeholders to take measures to prevent and cease burnout. Regional rheumatology leagues and organizations should come forward and form task forces to look into the causes of burnout and formulate potential interventions to confront it. Stratified risk assessment for individualized approaches may identify rheumatologists at particular risk of burnout and implement appropriate preventative strategies to preserve the thinning workforce.
There are several limitations to this study. We had only received limited responses at the beginning of the survey. Therefore, we had to increase the study duration and allow for non-Asian rheumatologists' responses. The relatively small sample size was another limitation of this study. We used social media platforms to disseminate our survey and could only include those respondents who were willing to participate.
Our survey was only available in English, another factor limiting its outreach. In addition, this was a self-reported survey, and we did not screen respondents for a history of mental illness. Although most of our respondents were Asians, there was an over-representation from South Asia, making it difficult to generalize the results to other Asian regions. Finally, as this was an observational study, we did not investigate interventions for preventing or mitigating burnout. However, further large-scale research in other countries, including controlled trials and interventional study designs, can explore the prevalence of burnout and the usefulness of potential interventions.
Conclusion
A substantial proportion of rheumatologists in our survey report burnout, with the most frequent type of burnout being in the personal accomplishment domain. Our findings suggest that males may be at increased risk of depersonalization burnout. We also observed that females scored significantly higher on three items of the MBI-HSS, and males scored higher on one item. These findings shed light on potential risk factors of burnout among rheumatologists and may help develop targeted interventions.
A shortage of rheumatology manpower is a potential cause of burnout among rheumatologists. Some proposed solutions include training nurses and physician assistants and enhancing interest in rheumatology training. In addition, strategies to prevent and mitigate burnout on a personal level include stress management, resilience training, and other self-care strategies.
The introduction of organizational measures to prevent and mitigate burnout is crucial, particularly in personal accomplishment and depersonalization. Organizations should ensure the well-being of physicians by providing compensation, physician-friendly policies, promoting work–life balance, and encouraging shared decision making. Further large-scale research, including controlled and interventional studies, will usefully ascertain the efficacy of such interventions in reducing burnout.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank all respondents for taking the survey.
Author contributions
TK: conceptualization, data curation, investigation, formal analysis, investigation, methodology, writing – original draft, writing – review and editing. MS: data curation, investigation, writing – review and editing. MSK: data curation, writing – review and editing. AM: data curation, writing – review and editing. WA: supervision, methodology, writing – review and editing. SS: data curation, writing – review and editing. LG: supervision, methodology, writing – review and editing. MAM: data curation, formal analysis, writing – review and editing. All authors: reviewed and approved the final version of the manuscript for submission and take full responsibility for the integrity and accuracy of all aspects of this manuscript.
Funding
No specific funding was received from any bodies in the public, commercial, or not-for-profit sectors to carry out the work described in this article.
Declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Name of ethics committee: FMTI Ethics Research Review Board, Pakistan Institute of Medical Sciences, Islamabad Pakistan. Date of ethics approval: 25th November 2021. Protocol number: FMT ERRB/02/10.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WHO (2019) Burnout an "occupational phenomenon": international classification of diseases. World Health Organization. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases. Accessed 26 February 2023
- 2.Ledikwe JH, Kleinman NJ, Mpho M, Mothibedi H, Mawandia S, Semo BW, O'Malley G. Associations between healthcare worker participation in workplace wellness activities and job satisfaction, occupational stress and burnout: a cross-sectional study in Botswana. BMJ Open. 2018;8(3):e018492. doi: 10.1136/bmjopen-2017-018492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, Durning S, Moutier C, Szydlo DW, Novotny PJ, Sloan JA, Shanafelt TD. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Balch CM, Bechamps GJ, Russell T, Dyrbye L, Satele D, Collicott P, Novotny PJ, Sloan J, Freischlag JA. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250(3):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 5.Dewa CS, Loong D, Bonato S, Trojanowski L, Rea M. The relationship between resident burnout and safety-related and acceptability-related quality of healthcare: a systematic literature review. BMC Med Educ. 2017;17(1):195. doi: 10.1186/s12909-017-1040-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Low ZX, Yeo KA, Sharma VK, Leung GK, McIntyre RS, Guerrero A, Lu B, Sin Fai Lam CC, Tran BX, Nguyen LH, Ho CS, Tam WW, Ho RC. Prevalence of burnout in medical and surgical residents: a meta-analysis. Int J Environ Res Public Health. 2019 doi: 10.3390/ijerph16091479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kang EK, Lihm HS, Kong EH. Association of intern and resident burnout with self-reported medical errors. Korean J Fam Med. 2013;34(1):36–42. doi: 10.4082/kjfm.2013.34.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The L. Physician burnout: a global crisis. Lancet (London, England) 2019;394(10193):93. doi: 10.1016/s0140-6736(19)31573-9. [DOI] [PubMed] [Google Scholar]
- 9.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiwari V, Kavanaugh A, Martin G, Bergman M. High burden of burnout on rheumatology practitioners. J Rheumatol. 2020;47(12):1831–1834. doi: 10.3899/jrheum.191110. [DOI] [PubMed] [Google Scholar]
- 11.Kulhawy-Wibe SC, Widdifield J, Lee JJY, Thorne JC, Yacyshyn EA, Batthish M, Jerome D, Shupak R, Jilkine K, Purvis J, Shamis J, Roberts J, Kur J, Burt JE, Johnson NA, Barnabe C, Hartfeld NMS, Harrison M, Pope JE, Barber CEH. Results from the 2020 Canadian rheumatology association's workforce and wellness survey. J Rheumatol. 2022;49(6):635–643. doi: 10.3899/jrheum.210990. [DOI] [PubMed] [Google Scholar]
- 12.Intriago M, Maldonado G, Soriano E, Toro C, Moreno L, Ríos C. Burnout in rheumatologists in Latin America. J Clin Rheumatol: Pract Rep Rheum Musculoskelet Dis. 2022;28(1):1–6. doi: 10.1097/rhu.0000000000001795. [DOI] [PubMed] [Google Scholar]
- 13.Manzano García G, Montañés Muro MP, López Megías J. Does the economic crisis contribute to the burnout and engagement of Spanish nurses? Curr Psychol (New Brunswick, NJ) 2021 doi: 10.1007/s12144-021-01527-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar B, Swee ML, Suneja M, Iyer P. Well-being burnout, and resiliency among early-career rheumatologists: a qualitative study. JCR: J Clin Rheumatol. 2021;27(8):e404–e411. doi: 10.1097/rhu.0000000000001485. [DOI] [PubMed] [Google Scholar]
- 15.McNearney TA, Hunnicutt SE, Maganti R, Rice J. What factors relate to job satisfaction among rheumatologists? J Clin Rheumatol: Pract Rep Rheum Musculoskelet Dis. 2008;14(3):133–137. doi: 10.1097/RHU.0b013e318177274d. [DOI] [PubMed] [Google Scholar]
- 16.Pham CT, Lee CB, Nguyen TLH, Lin J-D, Ali S, Chu C. Integrative settings approach to workplace health promotion to address contemporary challenges for worker health in the Asia-Pacific. Global Health Promot. 2020;27(2):82–90. doi: 10.1177/1757975918816691. [DOI] [PubMed] [Google Scholar]
- 17.Aggarwal A, Haq SA. Rheumatology workforce issues in South Asia: challenges and solutions. Int J Rheum Dis. 2020;23(3):443–447. doi: 10.1111/1756-185X.13793. [DOI] [PubMed] [Google Scholar]
- 18.Gibson T. Rheumatology in India and Pakistan today. Rheumatology. 2014;54(5):753–754. doi: 10.1093/rheumatology/keu306%JRheumatology. [DOI] [PubMed] [Google Scholar]
- 19.Khursheed T, Ovseiko PV, Harifi G, Badsha H, Cheng YK, Hill CL, Haq SA, Danda D, Gupta L. Gender equity in rheumatology leadership in the Asia-Pacific. Rheumatol Adv Pract. 2022;6(3):rkac087. doi: 10.1093/rap/rkac087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory. Scarecrow Education; 1997. [Google Scholar]
- 21.Gaur PS, Zimba O, Agarwal V, Gupta L. Reporting survey based studies - a primer for authors. J Korean Med Sci. 2020;35(45):e398–e398. doi: 10.3346/jkms.2020.35.e398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 23.Melnikow J, Padovani A, Miller M. Frontline physician burnout during the COVID-19 pandemic: national survey findings. BMC Health Serv Res. 2022;22(1):365. doi: 10.1186/s12913-022-07728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kane LJMP (2022) Physician burnout and depression report 2022: stress, anxiety, and anger.
- 25.Kane LJNY, NY: Medscape (2021) Death by 1000 cuts': Medscape national physician burnout and suicide report 2021.
- 26.Ozyurt A, Hayran O, Sur H. Predictors of burnout and job satisfaction among Turkish physicians. QJM: Int J Med. 2006;99(3):161–169. doi: 10.1093/qjmed/hcl019. [DOI] [PubMed] [Google Scholar]
- 27.Lebares CC, Braun HJ, Guvva EV, Epel ES, Hecht FM. Burnout and gender in surgical training: a call to re-evaluate coping and dysfunction. Am J Surg. 2018;216(4):800–804. doi: 10.1016/j.amjsurg.2018.07.058. [DOI] [PubMed] [Google Scholar]
- 28.Lo D, Wu F, Chan M, Chu R, Li D. A systematic review of burnout among doctors in China: a cultural perspective. Asia Pac Fam Med. 2018;17:3. doi: 10.1186/s12930-018-0040-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kane LJMA (2021) Medscape physician compensation report 2021: the recovery begins. 16
- 30.Miloslavsky EM, Bolster MB. Addressing the rheumatology workforce shortage: a multifaceted approach. Semin Arthritis Rheum. 2020;50(4):791–796. doi: 10.1016/j.semarthrit.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Lancet R Battling burnout. Lancet Rheumatol. 2022;4(3):e153. doi: 10.1016/S2665-9913(22)00043-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li Z, Yang Y. Rheumatology in China: challenges and development. Rheumatology. 2012;51(10):1733–1734. doi: 10.1093/rheumatology/kes166%JRheumatology. [DOI] [PubMed] [Google Scholar]
- 33.Kouvonen A, Vahtera J, Oksanen T, Pentti J, Väänänen AK, Heponiemi T, Salo P, Virtanen M, Kivimäki M. Chronic workplace stress and insufficient physical activity: a cohort study. Occup Environ Med. 2013;70(1):3–8. doi: 10.1136/oemed-2012-100808. [DOI] [PubMed] [Google Scholar]
- 34.Esquivel MK. Nutrition strategies for reducing risk of burnout among physicians and health care professionals. Am J Lifestyle Med. 2021;15(2):126–129. doi: 10.1177/1559827620976538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakata A. Work hours, sleep sufficiency, and prevalence of depression among full-time employees: a community-based cross-sectional study. J Clin Psychiatry. 2011;72(5):605–614. doi: 10.4088/JCP.10m06397gry. [DOI] [PubMed] [Google Scholar]
- 36.Sandoval LR, Buckey JC, Ainslie R, Tombari M, Stone W, Hegel MT. Randomized controlled trial of a computerized interactive media-based problem solving treatment for depression. Behav Ther. 2017;48(3):413–425. doi: 10.1016/j.beth.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Workforce HH (2022) Health workforce resiliency awards. https://bhw.hrsa.gov/funding/health-workforce-resiliency-awards. Accessed 26 Feb 2023
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.