Abstract
Background:
Accidents are common in the agricultural industry, particularly among dairy farmers. How said farmers get hurt is well established, but far less is known about how distal, socio-environmental factors influence injuries. This study examined associations between medically-attended agricultural injuries and: (1) personal sociodemographic characteristics, and (2) farm environment features and general safety practices.
Methods:
A cross-sectional survey was implemented with linked data from electronic health records on prior agricultural injuries that occurred between 01/01/2002–12/31/2015. The sample included adult dairy producers who resided in north-central Wisconsin (USA) and were medically-homed to the Marshfield Clinic Health System. Multiple logistic regression was used to analyze associations between socio-environmental characteristics and agricultural injuries.
Results:
There were 620 dairy farmers in the analytical sample, with 50 medically-attended agricultural injuries observed during the 14-year study time period (5.7 injuries per 1000 dairy farmers per year). In the multivariable model, the odds of agricultural injury were significantly greater among farmers who have private individually-purchased health insurance (OR = 4.25; 95% CI: 1.31, 13.84), do not live at their dairy operation (OR = 2.91; CI: 1.27, 6.67), and do not provide safety training to their workers (OR = 4.27; CI: 1.00, 18.21).
Conclusions:
Dairy farmers in this analysis who did not live at their dairy operation, did not provide safety training to all their workers, or had individually-purchased health insurance were more apt to get injured, but more research is needed to confirm these findings in prospectively designed studies. How these factors can be directly addressed or otherwise used to better focus farm injury prevention initiatives should also be explored.
Keywords: Farmers, Injuries, Epidemiology
Introduction
With an annual fatality rate of 27 per 100,000 workers, farming is the sixth deadliest occupation in the U.S., second only to sales/delivery transportation in the absolute number of occupational deaths [1]. Rates of non-fatal agricultural injuries are much higher than severe injuries, but all injuries combined can generally be expected to impact about 10% of farm workers each year [2,3]. Precise injury estimates are complicated by how injury data is collected, as farmers are known to delay medical care, save for the most acute health events [4,5]. Health hazards are unequally distributed across farming types/operations. For example, Pratt et al. [6] found that, after controlling for age and numbers of work hours, dairy farm owners appeared to be at particularly high risk with about 17 injuries per 100 dairy farm owners per year. Other studies have indicated farmers in dairy production are at somewhat lower risk compared to those in other agricultural areas, such as beef production [7].
How dairy farmers get injured has been examined in several prior studies. Use of heavy equipment remains the most common cause of fatal or disabling injury (e.g., tractor rollover, rotating shaft entanglement) [8]. Less severe dairy farm injuries are usually the result of falls and interactions with animals [9,10]. Other causes of injuries include chemical exposures, confined space (e.g., manure lagoons), and use of motorized equipment (e.g., all-terrain vehicles [ATV]) and power tools without personal protective equipment. Ways in which distal factors, including characteristics of the farm environment and farmers’ sociodemographic profile, might also influence dairy injuries are not well known. A recent meta-analysis of 32 studies, focused on all agricultural operations from around the world, found that males, full-time farmers, farm owners, those with a history of prior injury, hearing loss, regular medication use, and stress/depression were associated with ~1.5–2.0 higher odds of agricultural injury (usually self-reported) [11].
While nearly all agricultural injuries are theoretically preventable, identifying the modifiable factors that can reduce injury risk in dairy operations is a challenge. Developing a better understanding of injury determinants may be particularly important for dairy farmers due to the unique, technologically dynamic environment in which they work. Minimal research has been conducted on dairy injury antecedents beyond the most proximal causes (e.g., tractor rollover, animal assault). Methods that combine primary and passive data collection, via linking survey data on general dairy farm exposures to injury documentation in electronic health records (EHR), may offer advantages in terms of minimizing respondent burden and negating injury recall biases. There are burgeoning models of the secondary use of EHR data to capture various disease events and certain types of injuries [12,13], but such methods have only recently been tested to augment farm injury surveillance [14]. The purpose of this study was to examine associations between medically-attended agricultural injuries and: (1) personal sociodemographic characteristics, and (2) farm environment features and general safety practices. This was an exploratory study designed to inform future agricultural injury prevention research and safety initiatives, thus analyses were conducted without a priori hypotheses.
Materials and methods
Design and setting
This was a cross-sectional survey with linked participant EHR data on agricultural injuries that occurred over a prior 14-year period (01/01/2002–12/31/2015). The target population included adult dairy producers from north-central Wisconsin, and for whom there was a reasonable expectation of complete capture of their medical care by Marshfield Clinic Health System’s (MCHS) electronic data repository. MCHS is a large integrated care system serving a predominantly rural area of north-central Wisconsin.
Sampling frame
Survey inclusion criteria were, as of December 2015: (1) listed on the register of licensed dairy producers from Wisconsin’s Department of Agriculture, Trade and Consumer Protection, (2) dairy production operation address listed within the targeted 20-county region (as outlined in Fig. 1), and (3) complete capture of medical care within MCHS data systems, as evidenced by at least one of the following:
Member of MCHS’s Virtual Data Warehouse population – The Virtual Data Warehouse is a defined medical research population used as part of the broader Health Care Systems Research Network [15]. It includes individuals who are members of an MCHS-affiliated health insurance plan (Security Health Plan of Wisconsin) and/or residents of the Marshfield Epidemiologic Study Area (MESA). Individuals in MESA receive the vast majority of their medical care from MCHS and reside in one of 24 postal codes that surround primary service areas in central and northern Wisconsin [16].
Medically-homed to MCHS – This includes individuals with an MCHS primary care provider assigned to them, or with a preponderance of primary medical care visits having occurred at an MCHS Center over the past three years, per standard definitions used by the MCHS Institute for Quality, Innovation and Patient Safety.
Fig. 1.
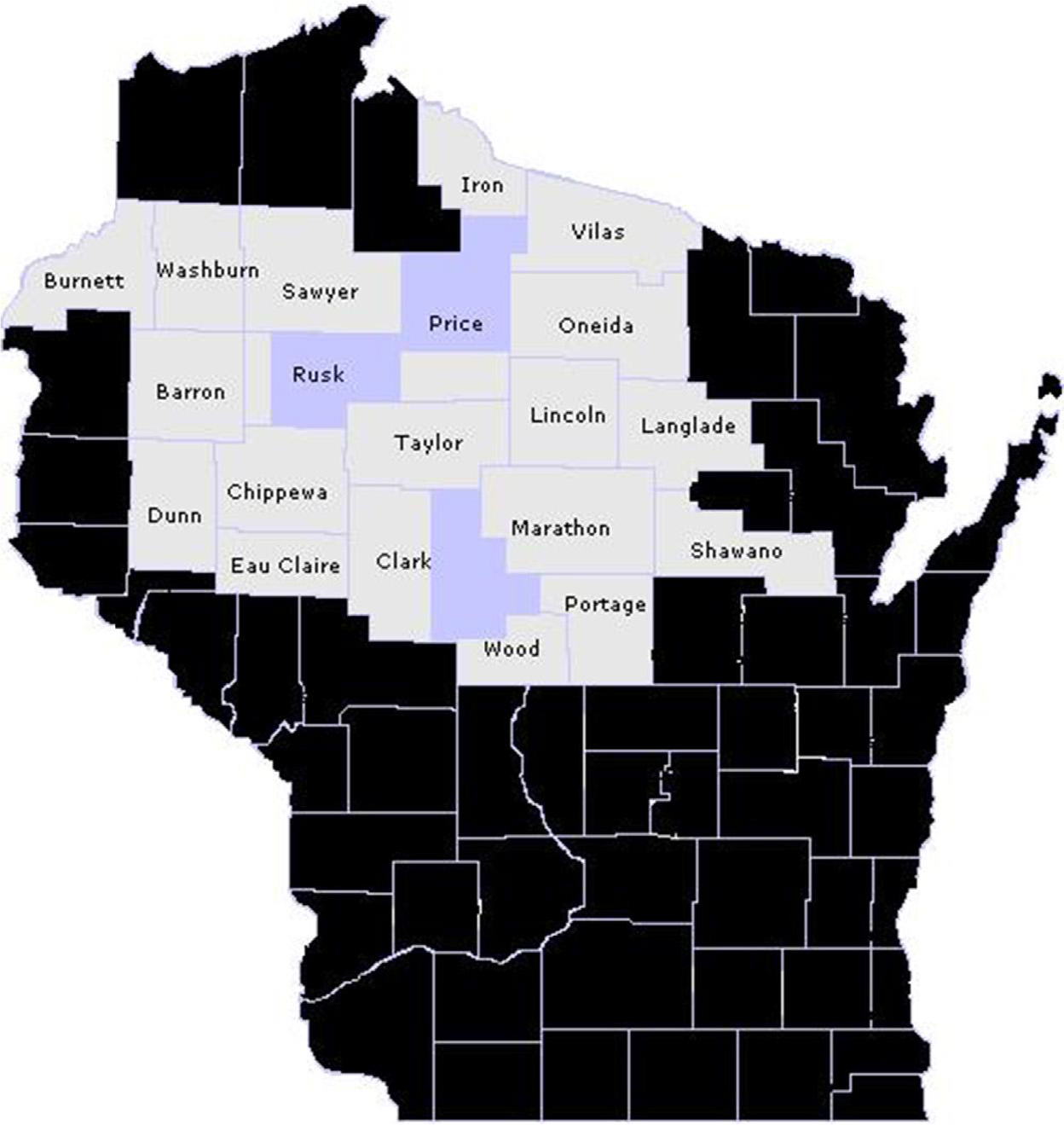
Source population, including individuals with a dairy production address in the outlined 20-county region of Wisconsin (lighter shaded 20 counties) and who were: (1) members of Marshfield Clinic Health System’s Virtual Data Warehouse population (i.e., members of Security Health Plan of Wisconsin and/or residents of the Marshfield Epidemiologic Study Area [24 darker shaded postal code areas]), or (2) medically-homed to the Marshfield Clinic Health System (i.e., primary care provider assigned to them, or with a preponderance of primary care visits having occurred at a Marshfield Clinic Health System center over the past three years).
Exclusion criteria were: (1) under age 18 years, or (2) inability to read the English language survey. The sampling frame included all study-eligible individuals. All study procedures were approved in advance by the Marshfield Clinic Research Foundation Institutional Review Board, with a request to waive documentation of informed consent and HIPAA authorization procedures.
Recruitment
Contact information for study-eligible individuals was extracted from administrative records in the MCHS research data warehouse. An adaptation of survey recruitment methods outlined by Dillman et al. [17] was used, including: (1) Mailed Invitation Packet sent to all enumerated individuals, which included a cover letter, study information sheet, survey instrument, return mailer, and $5 cash incentive, (2) Mailed Reminder/Thanks Postcard sent to all enumerated individuals, (3) Mailed Follow-up Packet, which included the same elements as the Mailed Invitation Packet, sent to all non-respondents, and (4) Follow-up Telephone Calls of up to four attempts for remaining non-respondents (plus a verbal survey response option). Recruitment efforts and survey completion occurred between May and July 2016.
Exposures
Participants completed a 32-item self-report survey that queried dairy operational procedures, safety practices, select farm characteristics, and basic respondent sociodemographics. Other exposures were extracted from linked EHR data (collected as part of routine medical care), including age, gender, and race/ethnicity. Specific exposure variables tested in this analysis included:
Personal sociodemographic characteristics – age, gender, race/ethnicity, household income, health insurance, farm ownership, farm residence, off-farm employment
Farm environment features and general safety practices – acres in agricultural production, number of cows, number of workers, feed storage facilities, number of tractors, use of other farm equipment, milking methods, manure handling methods, safety management role, safety training provided to workers, tractor rollover protection, and other available safety equipment.
Agricultural injuries
Based on a surveillance model recently developed by Landsteiner et al. [18], the outcome in our study was medically-attended agricultural injuries. These included injuries (experienced during the course of farm work) that were treated in outpatient, urgent care, emergency room, or inpatient medical settings. Such injuries were screened for between 01/01/2002 and 12/31/2015, which corresponds to the timeframe between when external cause of injury codes (E codes) were required for medical facility discharges in Wisconsin and sample enumeration. The specific E-codes screened for included E849.1–farm accidents, and E919.0-accidents caused by agricultural machines. These particular E codes have been shown to capture agricultural injuries with very good specificity among known farmers [19,20]. As of October 2015, however, E-codes were replaced by more specific billing codes as part of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) system. Thus we also screened for the parallel of E-codes E849.1 and E919.0 from ICD-10 coded injuries, which included Y92.7X and W30.XXX, respectively. Any participant with ≥1 of these diagnostic codes observed during the study timeframe was considered to be a medically-attended agricultural injury case. All other participants were considered non-cases.
Analyses
Analytical procedures were conducted with SAS Version 9.4 (Cary, NC). Summary injury data were reported on all cases. Given the exploratory nature of the study, participants were not excluded if they had missing exposure variables. This was treated as informative by creating an ‘unknown’ response category for missing exposures. Multivariable logistic regression was used to examine the association between agricultural injury and all exposures. The outcome was modeled dichotomously as injured vs. not injured. Two modeling approaches were conducted. First, univariate models were fit to examine the crude association between each exposure and agricultural injury. Any univariate exposure-outcome association with p-value less than 0.10 was considered for inclusion in the multivariable modeling. A full multivariable model was fit that included all exposures simultaneously, and was then reduced by manually removing exposures until only significant (p < 0.05) independent predictors of injury remained.
Results
Surveys were mailed to all 1293 study-eligible dairy farmers in the target region, with 935 (72%) of them responding. There were 315 survey respondents excluded from the main analysis because they did not consent to having their survey responses linked to their EHR data, yielding a final analytical sample of 620 dairy farmers for the injury analyses. As outlined in Table 1, the sample was predominantly middle-age (4%were younger than age 30; 25% were age 60 or older) male dairy owners who live and work on their farm. Dairy farms in this target region tend to be mid-size with about 2–3 total workers per farm, and few large industrial operations as are commonplace in other parts of the U.S. [21]. In addition, dairy farms were generally not specialized, as there were considerable land and equipment resources dedicated to agricultural production (see Table 2). Comparisons between survey respondents and non-respondents on available personal characteristics in the EHR found that both groups had similar gender proportions, average age, and racial/ethnic background (data not shown).
Table 1.
Sociodemographic Characteristics of North-Central Wisconsin Dairy Farmers, along with Univariate Associations with Medically-attended Agricultural Injuries.
| Characteristics | Respondents n = 620 | Univariate Association with Agricultural Injury (Yes vs. No) |
|---|---|---|
|
| ||
| Age (years) | 51.9 ±12.0 | 1.01 (0.99,1.04), p = 0.389 |
| Gender | ||
| Male | 590 (95%) | – |
| Female | 30 (5%) | |
| Race/Ethnicity | ||
| White, non-Hispanic | 468 (75%) | – |
| Non-White, non-Hispanic | 7 (1%) | |
| Unknown | 145 (23%) | |
| Annual Household Income | ||
| <$40,000 | 160 (26%) | – ref. – |
| $40,000–$79,999 | 137 (22%) | 0.69 (031,1.51), p = 0.353 |
| ≥$80,000 | 166 (27%) | 0.40 (0.17, 0.95), p=0.037 |
| Unknown | 157 (25%) | 0.71 (034,1.51), p = 0375 |
| Health Insurance | ||
| Private – Employer/Union | 115 (19%) | – ref. – |
| Private – Individually-purchased | 89 (14%) | 432 (134,13.90), p=0.014 |
| Public assisted | 270 (44%) | 2.83 (0.96, 833), p=0.059 |
| Other | 28 (5%) | 2.13 (037,12.28), p = 0396 |
| None | 79 (13%) | 1.48 (036, 6.10), p = 0.588 |
| Unknown | 39 (6%) | 231 (0.49,10.82), p = 0.287 |
| Ownership | ||
| Non-owner | 44(7%) | – ref. – |
| Owner | 576 (93%) | 1.21 (0.36,4.07), p = 0.753 |
| Resides | ||
| On Farm | 545 (88%) | – ref. – |
| Off Farm | 47 (8%) | 3.07 (139, 6.81), p=0.006 |
| Unknown | 28 (5%) | 1.00 (0.23,4.36), p = 0.998 |
| Occupation | ||
| Dairy only | 506 (82%) | – ref. – |
| Dairy plus another job | 114 (18%) | 0.71 (031,1.61), p = 0.406 |
Values in second column are reported as mean ± SD or frequency (% of respondents).
Values in last column are reported as odds ratio (95% confidence interval) of injured vs. not injured. Values less than 1 indicate that, relative to the reference category, the odds of injury decreased.
– indicates the exposure variable was not estimable due to very low numbers in one of the injured categories.
Bolded variables were considered for entry into the final multivariable analysis because their univariate association was p < 0.10.
Table 2.
Environmental and Safety Features of North-Central Wisconsin Dairy Farms, along with Univariate Associations with Medically-attended Agricultural Injuries among Dairy Farmers.
| Features | Respondents n = 620 | Univariate Association with Agricultural Injury (Yes vs. No) |
|---|---|---|
|
| ||
| Acres in Agricultural Production | ||
| <100 | 47 (8%) | 0.47 (0.11,1.99), p = 0.303 |
| 100–499 | 459 (74%) | – ref. – |
| ≥500 | 73 (12%) | 0.61 (0.21,1.75), p = 0.356 |
| Unknown | 41 (7%) | 1.13 (0.38, 3.34), p = 0.822 |
| Milking Cows | ||
| <30 | 48 (8%) | 1.48(0.55,4.01), p = 0.438 |
| 30–99 | 426 (69%) | – ref. – |
| ≥100 | 113 (18%) | 1.37 (0.67, 2.83), p = 0.388 |
| Unknown | 33 (5%) | 1.27 (0.37,4.41), p = 0.702 |
| Number of Workers | ||
| 1 | 102 (16%) | – ref. – |
| 2–3 | 238 (38%) | 1.47 (0.57,3.77), p = 0.425 |
| ≥4 | 224 (36%) | 1.57(0.61, 4.03), p = 0350 |
| Unknown | 56 (9%) | 1.23 (033,4.56), p = 0.756 |
| Number of Tractors | ||
| 0–3 | 129 (21%) | 0.41 (0.15,1.08), p = 0.070 |
| 4–6 | 322 (52%) | – ref. – |
| ≥7 | 136 (22%) | 0.98 (0.48,1.98), p = 0.950 |
| Unknown | 33 (5%) | 1.39 (0.46, 4.24), p = 0.559 |
| Rollover Protections Used On | ||
| No Tractors | 82 (13%) | – ref. – |
| Some Tractors | 402 (65%) | 1.06 (0.43, 2.63), p = 0.903 |
| All Tractors | 95 (15%) | 1.33 (0.45, 3.90), p = 0.608 |
| Unknown | 41 (7%) | 1.37 (036, 5.15), p = 0.642 |
| Machinery and Equipment | ||
| All-Terrain Vehicle | 410 (66%) | 1.69 (0.86, 330), p = 0.128 |
| Dump/Grain Truck | 87 (14%) | 0.51 (0.18,1.46), p = 0.208 |
| Hay Baler | 458 (74%) | 1.46 (0.71, 2.98), p = 0306 |
| Skid Steer | 430 (69%) | 1.28 (0.67, 2.47), p = 0.459 |
| End Loader | 278 (45%) | 1.25 (0.70, 2.23), p = 0.445 |
| Combine | 224 (36%) | 0.90 (0.49,1.66), p = 0.744 |
| Corn Picker | 93 (15%) | 0.92 (0.40, 2.10), p = 0.836 |
| Sprayer | 199 (32%) | 1.00 (0.54,1.85), p = 0.988 |
| Chisel Plow | 375 (60%) | 0.98 (0.54,1.77), p = 0.942 |
| Mower | 510 (82%) | 1.64(0.68, 3.94), p = 0.272 |
| Seed Drill | 504 (81%) | 2.18 (0.84, 5.61), p = 0.108 |
| Feed Mixer | 268 (43%) | 1.13 (0.63, 2.02), p = 0.680 |
| Feed Storage Facilities | ||
| Upright Silo | 484 (78%) | 1.52 (0.70, 3.32), p = 0.293 |
| Bunker Silo | 65 (10%) | 1.71 (0.77,3.83), p = 0.189 |
| Corn Crib | 63 (10%) | 0.54(0.16,1.80), p = 0317 |
| Open Building | 40 (6%) | 1.29 (0.44, 3.78), p = 0.643 |
| Closed Building | 109 (18%) | 0.75 (033,1.77), p = 0.490 |
| Silo Bags | 312 (50%) | 0.90 (0.51,1.61), p = 0.732 |
| Bin/tank | 246 (40%) | 0.77 (0.42,1.41), p = 0393 |
| Other | 69 (11%) | 1.87 (0.86, 4.03), p = 0.112 |
| Milking Method | ||
| Step-up/walkthrough/tie stall/stanchion | 478 (77%) | 0.96 (0.53,1.73), p = 0.884 |
| Parlor | 88 (14%) | 1.22 (0.69, 2.19), p = 0.494 |
| Other | 58 (9%) | 0.83 (0.29, 2.40), p = 0.732 |
| Manure Handling/Storage | ||
| Gutter | 378 (61%) | 0.96 (0.53,1.73), p = 0.884 |
| Pit | 306 (49%) | 1.22 (0.69, 2.19), p = 0.494 |
| Lot | 61 (10%) | 0.56 (0.17,1.87), p = 0348 |
| Pasture | 61 (10%) | 0.78 (0.27, 2.25), p = 0.650 |
| Manual | 45 (7%) | 0.51 (0.12, 2.17), p = 0.363 |
| Other | 52 (8%) | 1.24(0.47,3.27), p = 0.668 |
| Farm Safety Managed By | ||
| Shared (Self plus Staff) | 237 (38%) | – ref. – |
| Self Only | 277 (45%) | 0.93 (0.51,1.70), p = 0.807 |
| Nobody | 35 (6%) | 0.29 (0.04, 2.20), p = 0.230 |
| Unknown | 71 (11%) | 0.43 (0.13,1.49), p = 0.182 |
| Safety Training | ||
| Features | Respondents n = 620 | Univariate Association with Agricultural Injury (Yes vs. No) |
| Provided to All Workers | 85 (14%) | – ref. – |
| Not Provided to All Workers | 445 (72%) | 4.21 (1.00.17.76), p=0.050 |
| Unknown | 90 (15%) | 3.50 (0.71,1735), p = 0.125 |
| Protective Equipment Supplied to Workers | ||
| Gloves | 453 (73%) | 0.85 (0.45,1.60), p = 0.611 |
| Masks | 325(52%) | 0.98 (0.55,1.75), p = 0.951 |
| Eye Protection | 281 (45%) | 134(0.75, 2.39), p = 0324 |
| Hearing Protection | 273 (44%) | 0.84(0.46,1.51), p = 0.550 |
| Helmets | 62 (10%) | 035 (0.08,1.50), p = 0.158 |
| Respirators | 51 (8%) | 0.44(0.11,1.88), p = 0.269 |
| Coveralls | 85 (14%) | 0.53 (0.18,1.50), p = 0.228 |
| Rubber Boots | 292 (47%) | 0.61 (033,1.11), p = 0.104 |
Values in second column are reported as frequency (% of respondents). Some values do not sum to 100% because multiple responses could be selected.
Values in last column are reported as odds ratio (95% confidence interval) of injured vs. not injured. Values less than 1 indicate that, relative to the reference category, the odds of injury decreased.
Bolded variables were considered for entry into the final multivariable analysis because their univariate association was p < 0.10.
Fifty medically-attended agricultural injuries were observed, which translates into an estimated 5.7 injuries per 1000 dairy farmers per year, a rate somewhat higher than that observed among all Minnesota farmers (dairy and non-dairy) [18]. About three-fourths of all injury cases were coded as farm accidents (E849.1). Univariate models found that household income, health insurance, farm residence, number of tractors, and worker safety training were significantly associated with agricultural injuries, and were thus tested for potential inclusion in the multivariable model (see Tables 1 and 2). In the final reduced multivariable model, the odds of agricultural injury were significantly greater among farmers who have private individually-purchased health insurance (odds ratio [OR]=4.25; 95%confidence interval [CI]: 1.31, 13.84), do not live at their dairy operation (OR=2.91; CI: 1.27, 6.67), and do not provide safety training to their workers (OR=4.27; CI: 1.00, 18.21) (see Table 3).
Table 3.
Reduced Multivariable Model of the Association between Socio-environmental Factors and Medically-attended Agricultural Injuries among North-Central Wisconsin Dairy Farmers (n = 620).
| Exposures | Agricultural Injury (Yes vs. No) |
|---|---|
|
| |
| Health Insurance | |
| Private – Employer/Union | – ref. – |
| Private – Individually-purchased | 4.25 (131.13.84), p=0.016 |
| Public assisted | 2.73 (0.92, 8.08), p = 0.071 |
| Other | 237(0.41,13.90), p = 0.338 |
| None | 1.58 (0.38, 6.62), p = 0.528 |
| Unknown | 2.15 (035,13.23), p = 0.408 |
| Resides | |
| On Farm | – ref. – |
| Off Farm | 2.91 (137, 6.67), p=0.012 |
| Unknown | 1.05 (0.15, 7.18), p = 0.959 |
| Safety Training | |
| Provided to All Workers | – ref. – |
| Not Provided to All Workers | 437 (1.00,1831), p=0.049 |
| Unknown | 3.99(0.76, 20.81), p = 0.101 |
Values are reported as odds ratio (95% confidence interval) of injured vs. not injured. Values greater than 1 indicate that, relative to the reference category, the odds of injury increased.
Bolded variables were significantly (p < 0.05) associated with agricultural injury, as compared to the reference category.
Discussion
Dairy farming in north-central Wisconsin remains a risky occupation, with 8% of respondents having experienced a medically-attended agricultural injury over the previous 14 years. Prior research finds that such injuries are typically the result of machinery contact, animal assaults, or falls [8–10], but our findings also indicate that agricultural injuries are more common in dairy farmers who do not live at their dairy operation, do not provide safety training to their workers, and have a private individually-purchased health insurance policy.
These socio-environmental determinants of agricultural injury may have implications for farm safety programs and initiatives. As previously studied and advocated for [22,23]. safety is an important core component of training/education for farm owners and workers. Though we did not assess if respondents received safety training directly, nearly three of every four farmers in our study failed to provide safety training to all of their workers, thus highlighting the potential population-level value of targeting this modifiable risk factor. Why farm residence and health insurance type predicts agricultural injuries is less clear, but these factors perhaps suggest that some subgroups of dairy farmers are more apt to benefit from farm-level safety training or other injury prevention programs. Living on the farm was protective against injury risk. This may reflect more compact operations where there is less need for travel or use of various (dangerous) production implements. Having private/commercial health insurance coverage, presumably via a spouse’s employer or union plan, was also a protective factor as compared to an individually-purchased health insurance policy. Reasons for this are obviously quite speculative, particularly in light of the rapidly changing healthcare coverage environment in the U.S., but private insurance could perhaps be a general marker of economic vitality within farm families where there is dual income; one householder typically managing the farm and another householder working at a job where commercial health insurance is available for the family. This may free up resources to use, or otherwise more readily prioritize, injury prevention activities such as equipment protections.
It was somewhat surprising that other farm/farmer factors did not predict injuries. For example, full-time farmers and farm ownership were strong risk factors in a previous meta-analysis of studies not specific to dairy [11], but these factors did not predict injury risk in this sample of Wisconsin dairy farmers. Given their prominence in current farm injury prevention initiatives [24,25], use of tractor rollover protections was also not significantly associated with injuries in our study. The rather weak correlation between these factors and injury risk may have been partially a function of a major methodological limitation in our study; the temporality of exposure and outcome assessments. Exposures were essentially measured at study end and injuries were assessed looking back 14 years from that time point. This general approach, though common in agricultural injury research [11], assumes that exposures were reasonably representative throughout the whole study timeframe. But reverse causation is a possibility for some observations. For example, those who experienced a tractor rollover injury in the past may have been more apt to retrofit rollover protections on their current tractors, thereby obscuring the association between tractor rollover protection use (as measured today) and prior injuries.
The main study strengths were the objective capture of agricultural injuries and the defined source population. But ascertainment of agricultural injuries using E-codes alone, while practical and specific, may lack sensitivity. A recent surveillance model developed by Scott et al. estimated that E-codes alone only captured about 63% of all medically-attended agricultural injuries that occurred in Maine [26], a state where external cause of injury coding is not mandated. E-codes are mandated in Wisconsin and would presumably capture a higher fraction of all medically-attended injuries, but it is possible that some agricultural injuries can be missed without also using complementary methods such as reviews of ambulance records. Other methodological limitations were the homogeneity of the source population and the reliance on self-reports to assess most exposure variables, which may be subject to recall or self-presentation biases. Also, farm workers (who are not owners) and field fatalities that did not receive medical attention were generally not captured. Future research should attempt to confirm the associations observed in this study using prospective methods that include more non-owner farm workers and field fatalities, as well as direct observation of exposures wherever possible.
Conclusion
Though study findings were correlational, they reinforce prior observations that injuries to dairy farmers remain common and suggest that said farmers who do not live at their dairy operation, do not provide safety training to their workers, or have individually-purchased health insurance are more likely to be injured compared to those who live at their dairy operation, provide safety training, or have private/commercial health insurance, respectively. More research is needed to confirm these findings in prospective studies and to promote the general health and safety of dairy farmers.
Acknowledgements
This work was supported by the Upper Midwest Agricultural Safety and Health Center, as part of cooperative agreement U540H010170 from the National Institute for Occupational Safety and Health, U.S. Centers for Disease Control and Prevention.
Footnotes
Conflict of interest statement
The authors have no conflicting financial interests to disclose.
References
- [1].Johnson D The most dangerous jobs in America, http://time.com/4326676/dangerous-jobs-america/ [Accessed 24 October 2016]. [Google Scholar]
- [2].Cooper SP, Burau KE, Frankowski R, Shipp EM, Del Junco DJ, Whitworth RE. A cohort study of injuries in migrant farm worker families in South Texas. Ann Epidemiol 2006;16:313–20. [DOI] [PubMed] [Google Scholar]
- [3].Rautiainen RH, Reynolds SJ. Mortality and morbidity in agriculture in the United States. J Agric Saf Health 2002;8:259–76. [DOI] [PubMed] [Google Scholar]
- [4].Brower MA, Earle-Richardson GB, May JJ, Jenkins PL Occupational injury and treatment patterns of migrant and seasonal farmworkers. J Agromed 2009;14:172–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Reed DB, Rayens MK, Winter K, Zhang M. Health care delay of farmers 50 years and older in Kentucky and South Carolina. J Agromed 2008;13:71–9. [DOI] [PubMed] [Google Scholar]
- [6].Pratt DS, Marvel LH, Darrow D, Stallones L May JJ, Jenkins P. The dangers of dairy farming: the injury experience of 600 workers followed for two years. Am J Ind Med 1992;21:637–50. [DOI] [PubMed] [Google Scholar]
- [7].Brison RJ, Pickett CW. Non-fatal farm injuries on 117 eastern Ontario beef and dairy farms: a one-year study. Am J Ind Med 1992;21:623–36. [DOI] [PubMed] [Google Scholar]
- [8].Douphrate DI, Stallones L, Lunner Kolstrup C, Nonnenmann MW, Pinzke S, Hagevoort GR. Work-related injuries and fatalities on dairy farm operations–a global perspective. J Agromed 2013;18:256–64. [DOI] [PubMed] [Google Scholar]
- [9].Boyle D, Gerberich SG, Gibson RW, Maldonado G, Robinson RA, Martin F. Injury from dairy cattle activities. Epidemiology 1997;8:37–41. [DOI] [PubMed] [Google Scholar]
- [10].University of Wisconsin River Falls Center for Dairy Farm Safety. Injury trends – trainer (Module 2). www.osha.gov/dte/grant_materials/fy11/sh-22318-11/Mod_2_InjuryTrendsInstructorNotes.pdf [Accessed 24 October 2016].
- [11].Jadhav R, Achutan C, Haynatzki G, Rajaram S, Rautiainen R. Risk factors for agricultural injury: a systematic review and meta-analysis. J Agromed 2015;20:434–49. [DOI] [PubMed] [Google Scholar]
- [12].VanWormer JJ, Holsman RH, Petchenik JB, Dhuey BJ, Keifer MC. Epidemiologic trends in medically-attended tree stand fall injuries among Wisconsin deer hunters. Injury 2016;47:220–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Acharya A, VanWormer JJ, Waring SC, Miller AW, Fuehrer JT, Nycz GR. Regional epidemiologic assessment of prevalent periodontitis using an electronic health record system. Am J Epidemiol 2013;177:700–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Earle-Richardson GB, Jenkins PL Scott EE, May JJ. Improving agricultural injury surveillance: a comparison of incidence and type of injury event among three data sources. Am J Ind Med 2011;54:586–96. [DOI] [PubMed] [Google Scholar]
- [15].Hombrook MC, Hart G, Ellis JL Bachman DJ, Ansell G, Greene SM. Building a virtual cancer research organization. J Natl Cancer Inst Monogr 2005;35:12–25. [DOI] [PubMed] [Google Scholar]
- [16].DeStefano F, Eaker ED, Broste SK, Nordstrom DL, Peissig PL, Vierkant RA. Epidemiologic research in an integrated regional medical care system: the Marshfield Epidemiologic Study Area. J Clin Epidemiol 1996;49:643–52. [DOI] [PubMed] [Google Scholar]
- [17].Dillman DA, Smyth JD, Christian LM. Internet, phone, mail, and mixed-mode surveys: the tailored design method. New Jersey: John Wiley & Sons; 2014. [Google Scholar]
- [18].Landsteiner AM, McGovern PM, Alexander BH, Lindgren PG, Williams AN. Incidence rates and trend of serious farm-related injury in Minnesota, 2000–2011. J Agromed 2015;20:419–26. [DOI] [PubMed] [Google Scholar]
- [19].Pickett W, Hartling L Dimich-Ward H, Guernsey JR, Hagel L Voaklander DC. Surveillance of hospitalized farm injuries in Canada. Inj Prev 2001;7:123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Meyer RE, Hayes AM. Inpatient hospitalizations related to agricultural machine injuries in North Carolina, 2006–2010. NC MedJ 2011;72:488–91. [PubMed] [Google Scholar]
- [21].De Witte A, Nowak J, Schierholz F, Lassen BJ. Dairy farming in Wisconsin and California: different challenges–different future? www.agribenchmark.org/fileadmin/Dateiablage/B-Dairy/Misc/10_Snapshot_USA.pdf [Accessed 24 October 2016].
- [22].Nilsson K Interventions to reduce injuries among older workers in agriculture: a review of evaluated intervention projects. Work 2016;55:471–80. [DOI] [PubMed] [Google Scholar]
- [23].Hagevoort GR, Douphrate DI, Reynolds SJ. A review of health and safety leadership and managerial practices on modern dairy farms. J Agromed 2013;18:265–73. [DOI] [PubMed] [Google Scholar]
- [24].Tine PJ, Ayers P, May JJ, Purschwitz MA, Park S, Bayes B. Implementing a national tractor safety program: using Whole System in a Room to mobilize partners and implement solutions. J Agromed 2016;21:127–31. [DOI] [PubMed] [Google Scholar]
- [25].Liu B, Koc AB. Field tests of a tractor rollover detection and emergency notification system. J Agric Saf Health 2015;21:113–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Scott EE, Krupa NL, Horsman M, Jenkins PL Estimation of agricultural and logging injury incidence in Maine using electronic administrative data sets. J Agromed 2015;20:195–204. [DOI] [PubMed] [Google Scholar]


