Abstract
Patients experience interindividual variation in response to analgesics, which may be partially explained by genetics. This commentary discusses a recently published trial on COMT genotype and opioid dose requirements and describes the potential role for COMT and other genes (eg, CYP2D6) on opioid therapy and the current evidence for germline pharmacogenetics and resources for opioid pharmacogenetics.
Keywords: pharmacogenetics, pharmacogenomics, pain, opioids, cancer pain
Highlighting a recently published trial on COMT genotype and opioid dose requirements, this commentary describes the potential role for COMT and other genes (e.g., CYP2D6) on opioid therapy and current evidence for germline pharmacogenetics and resources for opioid pharmacogenetics.
Patients are more likely to be prescribed opioids if they have cancer or have survived cancer, compared to those without a history of cancer.1 Opioid therapy is complicated by interindividual variation in response. Pharmacogenetics, the use of genetics to guide medication therapy, is a tool that clinicians may be able to use to combat this variability.2,3 A recent randomized trial by Matsuoka et al. investigated whether catechol-O-methyltransferase (COMT) genotype was associated with high-dose requirements of oxycodone or morphine.4,5 This commentary will discuss this trial, describe the potential role for COMT and other genes in opioid therapy and the current evidence for germline pharmacogenetics. Panel 1 shows the national guidelines for pharmacogenetics in opioid management.
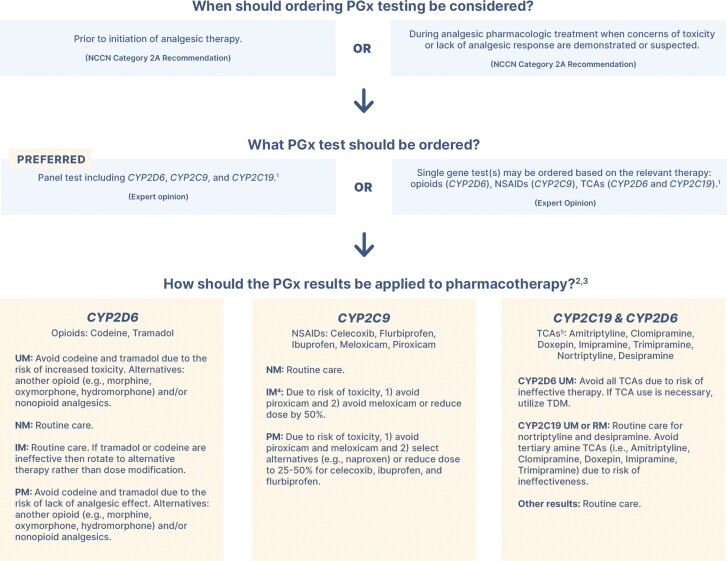
Panel 1: Guidelines Describing the Clinical Evidence and Relevance of Pharmacogenetics.
The National Comprehensive Cancer Network (NCCN) guidelines for adult cancer pain management include recommendations for ordering and interpretation of pharmacogenetic tests.6 NCCN guidelines include recommendations for select opioids (eg, tramadol, codeine), non-steroidal anti-inflammatory drugs (NSAIDs; eg, ibuprofen, meloxicam), and tricyclic antidepressants (TCAs; eg, amitriptyline, nortriptyline) largely based on evidence and recommendations described by the U.S Food and Drug Administration (FDA) or the Clinical Pharmacogenetics Implementation Consortium (CPIC). The FDA recently published Tables of Pharmacogenetic Associations that list drug-gene pairs where there is sufficient scientific pharmacogenetic evidence to support therapeutic management recommendations and potential impact on safety or response.7 The tables state that tramadol and codeine have (1) increased risk of toxicity in CYP2D6 ultrarapid metabolizers due to elevated concentrations of active metabolites and (2) increased risk of reduced efficacy in CYP2D6 poor metabolizers due to lower systemic active metabolite concentrations. These statements align with recommendations from the CPIC (www.CPICpgx.org).8
The CPIC is a National Institutes of Health (NIH)-funded consortium of international experts in pharmacogenetics that utilize systematic reviews to develop clinical practice guidelines.9 The CPIC opioid guidelines, updated in 2021, reviewed evidence for CYP2D6, OPRM1, and COMT.8 All 3 genes have biologically plausible mechanisms for affecting opioid response (CYP2D6—drug metabolism, OPRM1—drug target, COMT—pain perception). There are additional drug-gene associations that are likely undiscovered or have preliminary evidence and lack guidance from the FDA or CPIC at this time (eg, ABCB1-morphine, CYP3A4-fentanyl, CYP2B6-methadone).10,11 The guidelines identified insufficient or mixed evidence for OPRM1 and COMT but found evidence that supported interindividual response based CYP2D6 for select opioids. The CYP2D6 enzyme bioactivates tramadol and codeine to their active metabolites O-desmethyl-tramadol and morphine, respectively. For tramadol and codeine, the CPIC guidelines recommend alternative therapy for CYP2D6 poor and ultrarapid metabolizers due to the risk of ineffectiveness and toxicity, respectively. CYP2D6 also metabolizes oxycodone and hydrocodone to more active metabolites (oxymorphone and hydromorphone, respectively) although it is unclear how important this conversion is for clinical response for these medications. The CPIC does not recommend alternative therapy based on genotype for oxycodone or hydrocodone. The NCCN guidelines align with these CPIC recommendations.6Figure 1 displays a clinical algorithm that incorporates recommendations from the NCCN and CPIC guidelines on the use of pharmacogenetic testing in the treatment of pain.
Figure 1.
Guideline recommendations for pharmacogenetic testing to guide pain management. 1Genetic tests should include all AMP Tier 1 alleles. A panel test is preferred since it is more efficient and often the same cost to the patient as a single gene pharmacogenetic test.12-142 Determine phenotypes (eg, metabolizer statuses) per CPIC guidelines, which can be further refined by assessment of drug-drug interactions (eg, CYP2D6 inhibitors).8,15-173Recommendations are adapted from the NCCN and CPIC guidelines.6,8,16,174TCAs are typically used at lower doses when treating pain. If using higher doses (eg, depression doses), utilize CPIC guidelines for additional recommendations.16 Abbreviations: IM, intermediate metabolizer; NM, normal metabolizer; NSAID, nonsteroidal anti-inflammatory drug; PM, poor metabolizer; RM, rapid metabolizer; TCA, tricyclic antidepressant; TDM, therapeutic drug monitoring; UM, ultrarapid metabolizer.
Compared with oxycodone and morphine, tramadol is less commonly prescribed to treat cancer pain, often because it is perceived to be less effective. However, this experience may be secondary to genetic variation as approximately 40% of patients with chronic pain have reduced CYP2D6 activity (ie, poor or intermediate CYP2D6 metabolism).15 A prospective cluster-designed trial compared usual care to a CYP2D6-guided approach that delivered recommendations to providers.15 The CYP2D6-guided recommendations were for opioids metabolized by CYP2D6 (ie, tramadol, codeine, hydrocodone, oxycodone) and recommendations for alternative therapy were provided for CYP2D6 poor, intermediate, and ultrarapid. The primary outcome was focused on the group hypothesized to experience the largest improvement in pain control from CYP2D6-guided therapy (ie, poor and intermediate metabolizers prescribed tramadol or codeine). CYP2D6-guided therapy was associated with improvement in pain intensity compared to usual care among patients with poor or intermediate CYP2D6 metabolism who were prescribed tramadol or codeine.15 Secondary analyses of this study found CYP2D6-guided therapy was not helpful for oxycodone. A post hoc analysis of poor or intermediate metabolizers prescribed hydrocodone, tramadol, or codeine suggested improved pain intensity was associated with the CYP2D6-guided group versus usual care. However, the findings for hydrocodone and intermediate metabolizers require further validation.
There are 2 ongoing randomized controlled trials evaluating pharmacogenetics-guided care vs. usual care in chronic and acute pain populations (NCT04445792; NCT04685304). The larger trial, A Depression and Opioid Pragmatic Trial in Pharmacogenetics (ADOPT-PGx), includes a set of 3 randomizations that will enroll 4509 participants across a chronic pain trial, an acute pain trial, and a depression trial. The second trial, Pharmacogenomics Applied to Chronic Pain Treatment in Primary Care (PGx-ACT), is a smaller study that seeks to utilize panel-based testing to apply pharmacogenetics beyond opioid therapy by utilizing CPIC guidelines for NSAIDs and other medications that treat patient comorbidities (eg, antidepressants). One limitation is that none of these trials are focused specifically on cancer pain; however, the pharmacological mechanism behind the intervention is expected to translate to indications where these opioids are prescribed.
Additional study has been performed on the COMT gene, which encodes catechol-O-methyltransferase, which metabolizes catecholamines (eg, norepinephrine, dopamine), catcholestrogens, and select medications (eg, levodopa). It has been studied in relation to psychiatric disorders, breast cancer, and opioid receptor-mediated pain perception.18 The variant most widely studied, including by Matsouka et al, is rs4680G > A, which results in a change in the amino acid sequence (p.Val158Met).4 The exact mechanism of this variant on opioid receptor-mediated pain perception is uncertain. It is hypothesized that the change to methionine (met) reduces the levels of the COMT enzyme and therefore influences pain perception through catecholamine transmission via α or β adrenergic receptors.19–21 It has also been hypothesized that lower COMT activity is associated with lower levels of enkephalins and therefore decreased endogenous opioid analgesia and increased pain. Previous studies have found associations between G/G (Val/Val) genotype and higher morphine dose requirements, which was thought to be related to elevated COMT activity.10,21 However, the results of other studies have been mixed.22–24
The recent explanatory trial by Matsuoka et al used a randomized open-label design to investigate the hypothesis that, among participants with the COMT rs4680 GG genotype, a larger proportion would be prescribed high-dose opioids in the morphine group compared to the oxycodone group.4,5 The authors concluded that COMT rs4680 genotype was not associated with morphine or oxycodone dose requirements. A similar number of participants were prescribed high-dose opioids among those assigned oxycodone (~20%) and morphine (~45%) regardless of genotype. The proportion of participants on high-dose vs. low-dose opioids may have been related to how providers modified doses for each drug rather than genotype or that the definition of high-dose opioids required 2 dose increases for oxycodone and one dose increase for morphine.5
There are additional design considerations that affected this study and may affect future pharmacogenetic studies on opioids. Clinicians dose opioids per clinical response in an effort to balance the risks of toxicity and ineffectiveness. Identification of patients likely to require high-dose opioids could inform these risks; however, it is a surrogate outcome with unclear clinical implications. The primary endpoint would have been more informative if it were a direct measurement of adverse effects or effectiveness (eg, pain intensity, physical function), which would better align with core outcome measures in pain trials.25 An estimated high-dose opioid requirement may be difficult to translate to specific therapeutic actions. Additionally, for any pharmacodynamic gene implicated in drug response, it is vital to identify whether it is a class effect or limited to specific opioids so clinicians can better understand how to apply this information. The issue of class-specific vs. drug-specific effects is relevant for other genes under investigation for associations with drug response (eg, SLC6A4 for selective serotonin reuptake inhibitors).26 This study was specific to a single COMT variant when comparing morphine and oxycodone dosing and did not investigate other variants within COMT or other genes that may influence dosing (eg, CYP2D6 for oxycodone; CYP2B6 for morphine, OPRM1 for multiple opioids). Additionally, it does not further elucidate the mechanism for COMT in opioid response. Importantly, this study does not reflect a lack of evidence for pharmacogenetics as a field, rather it serves as inspiration to discuss resources available for pharmacogenetics and implications for patients with cancer and those who require pain management.
Pharmacogenetics likely has implications for patients with cancer beyond pain management. A recent analysis of patients with cancer found 60% were prescribed at least one medication with CPIC guidelines.27 These include anticancer medications (eg, fluorouracil, mercaptopurine) and medications used in supportive care (eg, antidepressants, analgesics, antiemetics). A single panel test with a handful of genes could impact a patient’s care across their longitudinal battle against cancer and related maladies.28 The clinical use of pharmacogenetics is becoming more accessible due to the erosion of historical barriers to PGx testing, including: cost of PGx testing (eg, now decreased to ~$100-300), insurance reimbursement (eg, since 2020 Medicare added coverage across 40 states for 101 medications with CPIC guidelines or those listed on the FDA Table of Pharmacogenetic Associations), access to testing (eg, many commercial laboratories now offer provider-ordered testing, FDA recently cleared a direct-to-consumer test from 23andMe ), NCCN recommendations supporting testing, and availability of high-quality clinical evidence and guidance.6,29-38 Clinicians can find laboratories that perform testing by searching NIH’s Genetic Testing Registry (https://www.ncbi.nlm.nih.gov/gtr/). Our patients have a need for improved pain management, and pharmacogenetic testing is an NCCN-recommended approach that is widely covered by Medicare. It is time for pharmacogenetic testing to advance from an obscure unused test to a viable decision aid.
Contributor Information
D Max Smith, MedStar Genetic Medicine, MedStar Health, Columbia, MD, USA; Department of Oncology, Georgetown University Medical Center, Washington, DC, USA.
William D Figg, Molecular Pharmacology Section, Genitourinary Malignancies Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, MD, USA.
Conflict of Interest
D. Max Smith reported grants (to institution) from Kailos Genetics. William D. Figg indicated no financial relationships.
References
- 1. Jairam V, Yang DX, Verma V, Yu JB, Park HS.. National patterns in prescription opioid use and misuse among cancer survivors in the United States. JAMA Netw Open. 2020;3(8):e2013605. https://doi.org/ 10.1001/jamanetworkopen.2020.13605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Roden DM, McLeod HL, Relling MV, et al. Pharmacogenomics. Lancet. 2019;394(10197):521-532. https://doi.org/ 10.1016/s0140-6736(19)31276-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Smith DM, Stevenson JM, Ho TT, et al. Pharmacogenetics: a precision medicine approach to combatting the opioid epidemic. J Am Coll Clin Pharm. 2021;5(2):239-250. https://doi.org/ 10.1002/jac5.1582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Matsuoka H, Tsurutani J, Chiba Y, et al. Morphine versus oxycodone for cancer pain using a catechol-O-methyltransferase genotype biomarker: a multicenter, randomized, open-label, phase III clinical trial (RELIEF Study). Oncologist. 2023;28(3):278–279. 10.1093/oncolo/oyac233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Matsuoka H, Tsurutani J, Chiba Y, et al. Selection of opioids for cancer-related pain using a biomarker: a randomized, multi-institutional, open-label trial (RELIEF study). BMC Cancer. 2017;17(1):674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Swarm RA, Youngwerth JM, Anghelescu DL, et al. Adult cancer pain, version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022. [Google Scholar]
- 7. U.S. Food and Drug Administration. Table of Pharmacogenomic Associations. Date accessed May 10, 2022. https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations.
- 8. Crews KR, Monte AA, Huddart R, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6, OPRM1, and COMT genotype and select opioid therapy. Clin Pharmacol Ther. 2021;37(1):1105-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Relling MV, Klein TE, Gammal RS, et al. The clinical pharmacogenetics implementation consortium: 10 years later. Clin Pharmacol Ther. 2020;107(1):171-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Owusu Obeng A, Hamadeh I, Smith M.. Review of opioid pharmacogenetics and considerations for pain management. Pharmacotherapy. 2017;110(4):888- 896. [DOI] [PubMed] [Google Scholar]
- 11. Smith DM, Weitzel KW, Cavallari LH, Elsey AR, Schmidt SO.. Clinical application of pharmacogenetics in pain management. Per Med. 2018;15(2):117-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pratt VM, Cavallari LH, Del Tredici AL, et al. Recommendations for clinical CYP2D6 genotyping allele selection: a joint consensus recommendation of the Association for Molecular Pathology, College of American Pathologists, Dutch Pharmacogenetics Working Group of the Royal Dutch Pharmacists Association, and European Society for Pharmacogenomics and Personalized Therapy. J Mol Diagn. 2021;23(9):1047-1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pratt VM, Cavallari LH, Del Tredici AL, et al. Recommendations for clinical CYP2C9 genotyping allele selection: a joint recommendation of the Association for Molecular Pathology and College of American Pathologists. J Mol Diagn. 2019;21(5):746-755. https://doi.org/ 10.1016/j.jmoldx.2019.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pratt VM, Del Tredici AL, Hachad H, et al. Recommendations for clinical CYP2C19 genotyping allele selection: a report of the association for molecular pathology. J Mol Diagn. 2018;20(3):269-276. https://doi.org/ 10.1016/j.jmoldx.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 15. Smith DM, Weitzel KW, Elsey AR, et al. CYP2D6-guided opioid therapy improves pain control in CYP2D6 intermediate and poor metabolizers: a pragmatic clinical trial. Genet Med. 2019;21(8):1842-1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hicks JK, Sangkuhl K, Swen JJ, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37-44. https://doi.org/ 10.1002/cpt.597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Theken KN, Lee CR, Gong L, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2C9 and nonsteroidal anti-inflammatory drugs. Clin Pharmacol Ther. 2020;108(2):191-200. https://doi.org/ 10.1002/cpt.1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hodge A.https://www.pharmgkb.org/vip/PA166165409 PharmGKB summary: very important pharmacogene information for COMT 2006.
- 19. Andersen S, Skorpen F.. Variation in the COMT gene: implications for pain perception and pain treatment. Pharmacogenomics. 2009;10(4):669-684. https://doi.org/ 10.2217/pgs.09.13 [DOI] [PubMed] [Google Scholar]
- 20. Segall SK, Maixner W, Belfer I, et al. Janus molecule I: dichotomous effects of COMT in neuropathic vs nociceptive pain modalities. CNS Neurol Disord Drug Targets. 2012;11(3):222-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rakvag TT, Klepstad P, Baar C, et al. The Val158Met polymorphism of the human catechol-O-methyltransferase (COMT) gene may influence morphine requirements in cancer pain patients. Pain. 2005;116(1-2):73-78. [DOI] [PubMed] [Google Scholar]
- 22. Lee MG, Kim HJ, Lee KH, Choi YS.. The influence of genotype polymorphism on morphine analgesic effect for postoperative pain in children. Korean J Pain. 2016;29(1):34-39. https://doi.org/ 10.3344/kjp.2016.29.1.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ross JR, Riley J, Taegetmeyer AB, et al. Genetic variation and response to morphine in cancer patients: catechol-O-methyltransferase and multidrug resistance-1 gene polymorphisms are associated with central side effects. Cancer. 2008;112(6):1390-1403. https://doi.org/ 10.1002/cncr.23292 [DOI] [PubMed] [Google Scholar]
- 24. Tammimaki A, Mannisto PT.. Catechol-O-methyltransferase gene polymorphism and chronic human pain: a systematic review and meta-analysis. Pharmacogenet Genom. 2012;22(9):673-691. [DOI] [PubMed] [Google Scholar]
- 25. Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1-2):9-19. [DOI] [PubMed] [Google Scholar]
- 26. Zhu J, Klein-Fedyshin M, Stevenson JM.. Serotonin transporter gene polymorphisms and selective serotonin reuptake inhibitor tolerability: review of pharmacogenetic evidence. Pharmacotherapy. 2017;37(9):1089-1104. https://doi.org/ 10.1002/phar.1978 [DOI] [PubMed] [Google Scholar]
- 27. Shugg T, Ly RC, Rowe EJ, et al. Clinical opportunities for germline pharmacogenetics and management of drug-drug interactions in patients with advanced solid cancers. JCO Precis Oncol. 2022;6(1):e2100312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Patel JN, Wiebe LA, Dunnenberger HM, McLeod HL.. Value of supportive care pharmacogenomics in oncology practice. Oncologist. 2018;23(8):956-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bonner L. 23andMe expands direct-to-consumer pharmacogenetics reports. Pharm Today. 2020;26(11):3131. https://doi.org/ 10.1016/j.ptdy.2020.10.049 [DOI] [Google Scholar]
- 30. Clinical Pharmacogenetics Implementation Consortium (CPIC). Guidelines . Date accessed December 2, 2021. https://cpicpgx.org/guidelines/
- 31. National Center for Biotechnology Information, U.S. National Library of Medicine. Genetic Testing Registry. Date accessed August 2, 2021. https://www.ncbi.nlm.nih.gov/gtr/all/tests/?term=pharmacogenetics
- 32. Palmetto GBA. Local Coverage Determination (LCD): MolDX: Pharmacogenomics Testing (L38294) ; 2020. https://www.cms.gov/medicare-coverage-database/details/lcddetails.aspx?LCDId=38294&ver=16
- 33. Wisconsin Physicians Service Insurance Corporation. Local Coverage Determination (LCD): MolDX: Pharmacogenomics Testing (L38435); 2020. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=38435&ver=8&bc=0
- 34. Noridian Healthcare Solutions, LLC. Local Coverage Determination (LCD): MolDX: Pharmacogenomics Testing (L38337); 2020. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=38337&ver=8&bc=0
- 35. Noridian Healthcare Solutions, LLC. Local Coverage Determination (LCD): MolDX: pharmacogenomics Testing (L38335); 2020. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=38335&ver=7&bc=0
- 36. CGS Administrators, LLC. Local Coverage Determination (LCD): MolDX: pharmacogenomics Testing (L38394); 2020. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=38394&ver=6&bc=0
- 37. Novitas Solutions, Inc. Local Coverage Determination (LCD): pharmacogenomics Testing (L39063); 2021. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=39063&ver=11&bc=0
- 38. First Coast Options, Inc. Local Coverage Determination (LCD): pharmacogenomics Testing (L39073); 2021. https://www.cms.gov/medicare-coverage-database/view/lcd.aspx?lcdid=39073&ver=4&bc=0