Abstract
Behaviors related to water, sanitation, and hygiene (WASH) are key drivers of infectious disease transmission, and experiences of WASH are potential influencers of mental well-being. Important knowledge gaps exist related to the content and delivery of effective WASH programs and their associated health impacts, particularly within the contexts of government programs implemented at scale. We developed and tested a demand-side intervention called Andilaye, which aimed to change behaviors related to sanitation, personal hygiene, and household environmental sanitation. This theory-informed intervention was delivered through the existing Ethiopian Health Extension Programme (HEP). It was a multilevel intervention with a catalyzing event at the community level and behavior change activities at group and household levels. We randomly selected and assigned 50 kebeles (sub-districts) from three woredas (districts), half to receive the Andilaye intervention, and half the standard of care sanitation and hygiene programming (i.e., community-led total sanitation and hygiene [CLTSH]). We collected data on WASH access, behavioral outcomes, and mental well-being. A total of 1,589 households were enrolled into the study at baseline; 1,472 households (94%) participated in an endline assessment two years after baseline, and approximately 14 months after the initiation of a multi-level intervention. The intervention did not improve construction of latrines (prevalence ratio [PR]: 0.99; 95% CI: 0.82, 1.21) or handwashing stations with water (PR: 0.96; 95% CI: 0.72, 1.26), or the removal of animal feces from the compound (PR: 1.10; 95% CI: 0.95, 1.28). Nor did it impact anxiety (PR: 0.90; 95% CI: 0.72, 1.11), depression (PR: 0.83; 95% CI: 0.64, 1.07), emotional distress (PR: 0.86; 95% CI: 0.67, 1.09) or well-being (PR: 0.90; 95% CI: 0.74, 1.10) scores. We report limited impact of the intervention, as delivered, on changes in behavior and mental well-being. The effectiveness of the intervention was limited by poor intervention fidelity. While sanitation and hygiene improvements have been documented in Ethiopia, behavioral slippage, or regression to unimproved practices, in communities previously declared open defecation free is widespread. Evidence from this trial may help address knowledge gaps related to challenges associated with scalable alternatives to CLTSH and inform sanitation and hygiene programming and policy in Ethiopia and beyond.
Trial registration: This trial was registered with clinicaltrials.gov (NCT03075436) on March 9, 2017.
Introduction
Inadequate water, sanitation, and hygiene (WASH) are key drivers of infectious disease transmission [1, 2]. Diarrhea accounts for an estimated 1.65 million deaths annually [3] and nearly 10% of all under-5 deaths in low-income settings [4]. Deficiencies in WASH are also a major contributor of neglected tropical diseases (NTDs) [5, 6]. Over one billion people are at risk of soil-transmitted helminthiasis, which leads to nearly five million disability adjusted life years (DALYs), and schistosomiasis leads to two million DALYs [7, 8]. Trachoma, the leading infectious cause of blindness [9], is precipitated by repeat infections with Chlamydia trachomatis bacteria, which are often perpetuated by poor hygiene [10]. These infections are environmentally mediated [11], and are largely attributed to inadequate WASH [12, 13].
While WASH studies have primarily focused on infectious diseases or anthropometric measures of growth amongst young children, this narrow focus does not fully encapsulate the World Health Organization (WHO)’s definition of health as “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity” [14]. A growing body of research has identified linkages between water and sanitation and mental health outcomes [14–17]. For example, extensive qualitative and quantitative research has demonstrated how water insecurity can influence mental health, particularly among women [18–21]. Research on sanitation and mental health is emergent, and predominantly qualitative [22–24]. A cross-sectional study in Odisha, India, found women’s sanitation insecurity—their negative sanitation experiences and concerns—to be associated with stress, depression, distress, and impaired general well-being, even among those with access to a sanitation facility [25]. Further, a systematic review of sanitation and well-being found open defecation and use of sanitation facilities can negatively influence mental and social well-being for women and girls, especially when they experience or perceive a lack of privacy and safety [14]. As such, improvements in women’s mental health likely requires more than physical access to sanitation facilities, but also gender-sensitive modifications to facilities and shifts in gender norms to improve women’s experiences of sanitation [23, 25]. To date, limited research has assessed the impact of water interventions on mental health outcomes [26], and few studies have assessed the impact of sanitation interventions on mental health outcomes [14].
Despite the urgent need to improve sanitation and hygiene—including the target of universal basic access to sanitation as part of Sustainable Development Goal target 6.2—many large-scale sanitation interventions have shown poor uptake and sustainability [27], as well as mixed impacts on health [1]. Without sustained sanitation and hygiene behavior change, health gains are unlikely.
Community-led total sanitation (CLTS) has been heralded as a low-cost approach to improve community coverage of sanitation [28]. CLTS uses a demand-side approach—promoting the demand to execute improved sanitation behaviors, rather than supply-side provision of infrastructure—that involves engaging the community, typically via an initial “triggering” event, to become open defecation free (ODF) through community-activities and local champions. Rigorous evaluations of CLTS, like those of other sanitation interventions, have yielded mixed health effects [29–31]. To date, there is mixed evidence on the potential of CLTS to achieve and sustain changes to WASH coverage and access [32–35]. Engaging local champions in CLTS delivery may yield beneficial results. Program delivery through Health Extension Workers (HEW) and the engagement of teachers both led to substantial improvements in sanitation coverage and use [34], although less than when delivered by trained natural leaders in Ghana [32]; yet these gains were not well sustained [36].
There are several documented limitations of community-led total sanitation and hygiene (CLTSH), a variation of CLTS that incorporates hygiene-related interventions. HEWs charged with implementing CLTSH have many responsibilities, limited incentives and motivations, few tools, and little capacity to continually reinforce messages [37]. The use of negative affective motivators employed by CLTS(H) may not be culturally appropriate or the most effective drivers of sanitation and hygiene behavior change [38], and may erode mental well-being. Together, the focus on negative affective motivators, poor facilitation of initial triggering, and a lack of follow-up, has left many communities with negative impressions of CLTSH initiatives [39].
In Ethiopia, CLTSH, which has been implemented widely through the Ethiopian Health Extension Programme (HEP), relies chiefly on negative affective motives (e.g., shame, disgust) to drive open defecation cessation. However, like prior evaluations of CLTS, evidence suggests that CLTSH is largely ineffective, with one out of six Ethiopian households continuing to practice open defecation after their respective villages were certified as ODF [40].
We designed a study to generate evidence to address knowledge gaps related to demand-side sanitation and hygiene programming and examine less studied, yet critical, inter-personal factors related to sustained behavioral adoption and downstream health impacts [41]. Specifically, we conducted a cluster-randomized trial (CRT) to test whether an intervention delivered at scale within the existing Ethiopian HEP would lead to sustained WASH behavior change and improved mental health. Leveraging feedback received from community members and key stakeholders, we designed a theoretically-informed [42–44] and evidence-based demand-side sanitation and hygiene intervention called Andilaye—Amharic for “togetherness/integration.” The intervention takes a positive, encouragement approach to behavior change by promoting incremental improvements in behavior and incorporating behavioral maintenance strategies to foster sustained behavior change.
Methods
The study’s primary aim was to determine whether a demand-side sanitation and hygiene intervention (Andilaye) impacted WASH behavior change and mental health, specifically general well-being and symptoms of anxiety, depression, and non-specific emotional distress. A protocol detailing the methods, intervention, and baseline results are published elsewhere [41].
Ethics and trial registration
Ethical approval for the Andilaye Trial was provided by Emory University (IRB00076141), the London School of Hygiene & Tropical Medicine (9595), and locally by the Amhara Regional Health Bureau (HRTT0135909). The trial was registered with clinicaltrials.gov (NCT03075436) on March 9, 2017. Approval was obtained at district and sub-district government offices. Informed consent was obtained orally at each household due to low literacy rates of the population and concerns about historically coercive practices which including obtaining signatures. Oral consent was approved by all ethics boards.
Study design
This parallel CRT was conducted in West Gojjam and South Gondar Zones of the Amhara National Regional State, a region of Ethiopia in which WASH conditions are inadequate [45], slippage in sanitation coverage and improved sanitation behaviors has been documented, and several NTDs (e.g., soil-transmitted helminths, trachoma) are hyperendemic [46]. Three districts (woredas)—Bahir Dar Zuria Woreda in West Gojjam Zone and Fogera and Farta Woredas in South Gondar Zone—were targeted for this study and represent a range of the topographical conditions present in Amhara, and Ethiopia in general. We targeted specific behaviors, including sanitation (constructing, maintaining, and using a latrine), personal hygiene (handwashing at key times and face washing), and household environmental sanitation (keeping animals separate from living quarters and keeping the compound free of feces). We sought to investigate whether any changes in WASH behaviors targeted by the Andilaye intervention were sustained, and we tracked intervention fidelity through a process evaluation.
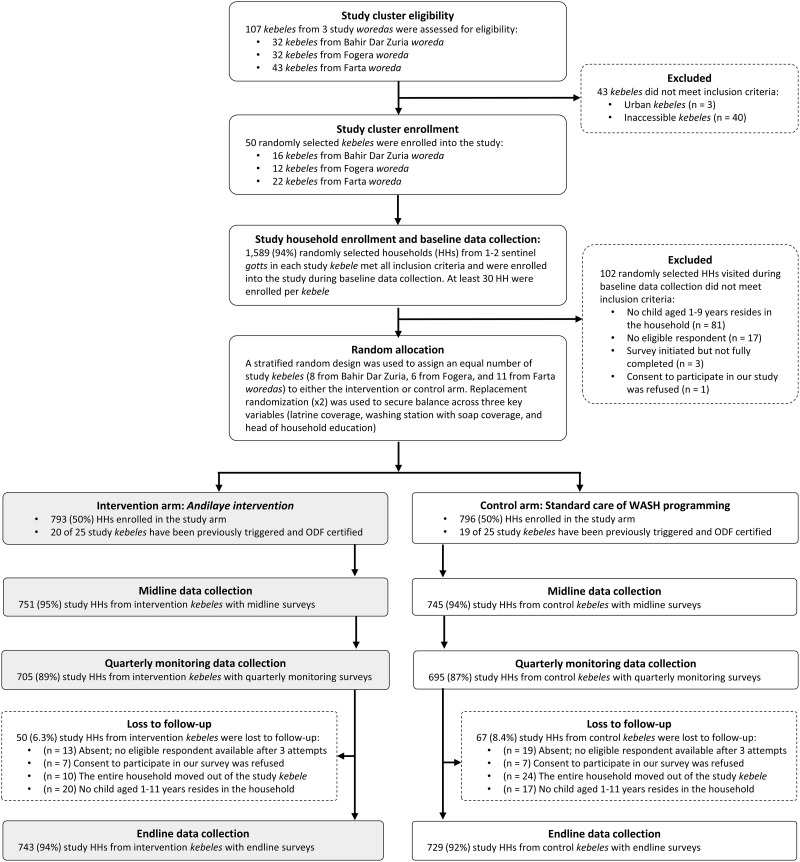
We employed a structured sampling strategy to randomly select 50 eligible clusters within our sampling frame. Fig 1 provides further details in the CONSORT flow diagram. Clusters were defined as rural or peri-urban sub-districts (kebeles)—the smallest government administrative unit in Ethiopia—that were accessible throughout the course of the year. Of the 50 kebeles enrolled into the study, 22 were selected from Farta, 12 from Fogera, and 16 from Bahir Dar Zuria. The secondary sampling unit for this study was the household; specifically, any household residing in a targeted, sentinel village (gott) within a randomly selected study kebele. We utilized a ‘fried egg’ [47] approach to purposively select one to two gotts that were either situated in or near the center of the kebele (if there were centric gotts) or were not adjacent to any other study kebele (in the event there are no centric gotts). This approach minimized spill-over of intervention effects and other externalities associated with the research between intervention and control clusters, especially those adjacent to each other. The number of targeted gotts depended only on the number of eligible households identified in gott census books.
Fig 1. CONSORT flow diagram.
Following baseline data collection, a stratified random design at the woreda-level was used to assign an equal number of study kebeles to either the Andilaye intervention or the control group receiving no intervention using a computer-based random number generator. To secure balance across three key potential confounders (i.e., latrine coverage, washing station with soap coverage, and head of household education), we established a priori that the intervention and control mean values for these three variables, using baseline data, should be within two standard deviations of the overall mean [41]. The randomization process was repeated twice using replacement rerandomization [48] to achieve balance according to that a priori criterion.
The Health Extension Services Package, and its accompanying CLTSH module delivered via the HEP, were being scaled throughout Ethiopia [49] and reflected the existing government-supported demand-side sanitation and hygiene approach. No attempt was made to modify the roll out of this standard of care of WASH programming in any of our study kebeles. There were no meaningful differences in the number of previously CLTSH-triggered and ODF certified kebeles, between study arms (Fig 1). Baseline WASH and demographic statistics [41], along with the fact that 39 of 50 kebele study clusters randomly selected for inclusion in the Andilaye Trial had been triggered with CLTSH, and certified ODF, provided strong evidence that behavioral slippage was, indeed, an issue that needed to be addressed in Amhara and perhaps elsewhere in Ethiopia.
“Andilaye” intervention
The Andilaye intervention motto was “Together we can be a strong, caring, healthy community”. Intervention activities offered aspirational messages that emphasized the need for collective action to make positive change in the community and used verbal persuasion to enhance collective efficacy perceptions [50]. The Andilaye intervention focused on three WASH-related behavioral themes, informed by formative research: (1) sanitation, (2) personal hygiene, and (3) household environmental sanitation. Within these themes were 11 constituent practices targeted by the intervention (Table 1); these practices were identified through formative research as ones that could be targeted using demand-side approaches, and were seen as achievable, per stakeholder feedback [41].
Table 1. Key outcome indicators for WASH behavioral themes and constituent practices of interest of the Andilaye intervention at endline.
| Indicators | Intervention | Control | ||||
|---|---|---|---|---|---|---|
| Sanitation (S) | Total N | % | Total N | % | PR (95% CI) a | PD (95% CI) b |
| S1: Construct a long-lasting latrine that is comfortable and hygienic | ||||||
| • Households with access to at least one household latrine | 743 | 61.2 | 729 | 62.0 | 0.99 (0.82, 1.21) | 0.00 (-0.13, 0.12) |
| • Households with access to an improved household latrine c | 741 | 34.6 | 726 | 30.6 | 1.13 (0.81, 1.59) | 0.41 (-0.07, 0.15) |
| • Households with access to a fully constructed household latrine | 742 | 33.0 | 729 | 28.7 | 1.15 (0.86, 1.54) | 0.04 (-0.46, 0.13) |
| S2: Repair your latrine whenever it is damaged | ||||||
| • Facility observed to require obvious repair | 455 | 70.1 | 451 | 80.5 | 0.88 (0.78, 0.99) | -0.10 (-0.19, -0.01) |
| S3: Upgrade your latrine so it becomes more long-lasting, comfortable, and hygienic | ||||||
| • Household has added or improved anything on the latrine since its original construction | 453 | 17.2 | 446 | 15.7 | 1.08 (0.71, 1.65) | 0.01 (-0.06, 0.08) |
| • Households with latrine with smooth and cleanable slab/floor | 743 | 16.3 | 728 | 13.3 | 1.19 (0.70, 2.03) | 0.03 (-0.05, 0.11) |
| • Presence of drop hole cover in the latrine | 455 | 18.2 | 451 | 10.0 | 1.77 (1.19, 2.63) | 0.08 (0.02, 0.14) |
| S4: Close your pit when it becomes full and reconstruct a new latrine | ||||||
| • Is the pit that is in use full or close to being full | 454 | 11.7 | 451 | 12.6 | 0.92 (0.57, 1.49) | -0.01 (-0.68, 0.05) |
| S5: All household members use a latrine every time they defecate | ||||||
| • Respondent always exclusively used a latrine for defecation during last 7 days | 743 | 53.2 | 729 | 54.1 | 0.99 (0.79, 1.24) | 0.00 (-0.12, 0.12) |
| • Head of household always exclusively used a latrine for defecation during last 7 days | 529 | 36.5 | 473 | 33.0 | 1.07 (0.79, 1.47) | 0.03 (-0.09, 0.15) |
| • Ages 4–17 always exclusively used a latrine for defecation during last 7 days | 1447 | 42.6 | 1385 | 35.0 | 1.15 (0.89, 1.50) | 0.06 (-0.05, 0.16) |
| S6: Immediately dispose of children’s feces into the latrine | ||||||
| • Child feces were safely disposed of during the last 2 days | 401 | 36.7 | 376 | 41.2 | 0.96 (0.69, 1.32) | -0.02 (-0.15, 0.11) |
| Personal hygiene (PH) | ||||||
| PH1: All household members wash their hands with water and soap or soap substitute AFTER handling animal and human feces, even children’s feces | ||||||
| • Household hand or facewashing station(s) | 743 | 98.3 | 729 | 97.7 | 1.01 (0.99, 1.02) | 0.01 (-0.01, 0.02) |
| • The last time the respondent defecated, s/he cleaned hands with water and soap, substitute | 738 | 51.9 | 725 | 46.1 | 1.13 (0.94, 1.35) | 0.06 (-0.03, 0.15) |
| • The last time the index child defecated, s/he cleaned hands with water and soap, substitute | 713 | 43.9 | 697 | 39.6 | 1.12 (0.92, 1.35) | 0.05 (-0.04, 0.13) |
| PH2: All household members wash their hands with water and soap or soap substitute BEFORE handling food | ||||||
| • The last time the respondent prepared food, s/he cleaned hands with water and soap, substitute before beginning food preparations | 700 | 53.6 | 703 | 48.5 | 1.11 (0.95, 1.29) | 0.05 (-0.03, 0.13) |
| PH3: All household members wash their faces with water whenever they are dirty and use soap when it is available | ||||||
| • Ocular discharge present among children aged 1–9 years | 822 | 26.9 | 874 | 30.4 | 0.88 (0.68, 1.15) | -0.04 (-0.11, 0.04) |
| • Wet nasal discharge present among children aged 1–9 years | 822 | 37.0 | 874 | 39.4 | 0.94 (0.78, 1.13) | -0.02 (-0.09, 0.05) |
| • Dry nasal discharge present among children aged 1–9 years | 822 | 42.7 | 874 | 45.2 | 0.97 (0.81, 1.16) | -0.02 (-0.10, 0.06) |
| • Dirt/dust/other debris present among children aged 1–9 years | 822 | 50.5 | 874 | 49.5 | 1.03 (0.89, 1.20) | 0.02 (-0.06, 0.09) |
| Household Environmental Sanitation (HES) | ||||||
| HES1: Keep all animals separated from the house | ||||||
| • Observed animal feces present in the compound | 743 | 82.2 | 729 | 82.4 | 1.01 (0.92, 1.11) | 0.01 (-0.07, 0.08) |
| HES2: Keep the household compound clean by disposing of all animal feces and other waste on a DAILY basis | ||||||
| • Animal feces/waste not left out in open in compound | 743 | 56.4 | 729 | 51.2 | 1.10 (0.95, 1.28) | 0.05 (-0.03, 0.13) |
| • Solid waste was not observed to have been left out in the open | 743 | 34.6 | 729 | 27.6 | 1.26 (0.93, 1.69) | 0.07 (-0.02, 0.17) |
Notes.
a We used log-linear binomial regression models to compare the prevalence of the outcomes between the intervention and control arms. Models accounted the stratified design by including woreda indicator variables [58], and accounted for clustering within kebeles by using generalized estimating equations with robust standard errors.
b Prevalence differences (PD) were calculated using post-estimation commands to estimate the average marginal effects.
c “Improved” was defined based on the WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation definition.
Intervention activities and behavior change tools were informed by our formative research and specifically designed to incorporate techniques that addressed behavioral factors such as action knowledge, perceived personal and household barriers to behavioral adoption, identification and planning, and behavioral control perceptions amongst others [41]. Activities occurred at four levels—district, community, group, and household (S1 Fig and S1 Table). Key activities included community mobilization and commitment events, community conversations with influential community members through facilitated group dialog, and household counseling visits with caregivers—all of which were guided by behavior change tools (e.g., community commitment banner, community conversations flipbook, and household counseling flipbook and goal cards) with illustrations produced by an artist based in Ethiopia.
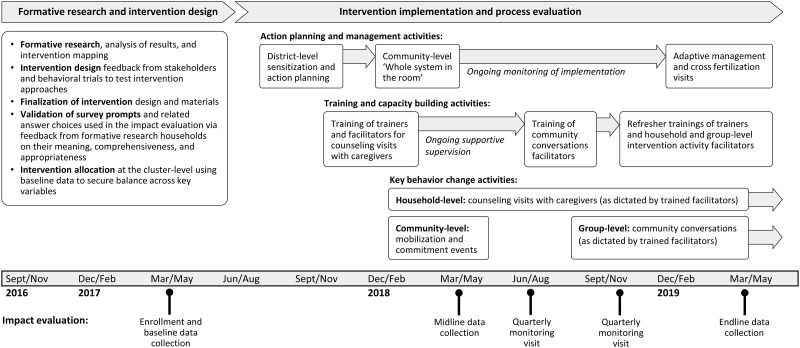
The Andilaye intervention was delivered through Ethiopia’s HEP, via trained government-salaried Woreda Health Office officials, HEWs, and volunteer Women’s Development Army Leaders (WDALs) (Fig 2; see S2 Table for an alignment of relevant roles and responsibilities of the HEP and Andilaye Trial). Implementation of the Andilaye intervention was overseen by an Ethiopia-based study team. The Andilaye intervention commenced with district-level capacity building activities, such as action planning to orient key government stakeholders and training of trainers who would facilitate intervention activities in kebeles allocated to receive the Andilaye intervention. Further, district-level refresher trainings and adaptive management activities were conducted to reinforce previously acquired knowledge and skills, address trainer/facilitator turnover, and review successes and address challenges faced in implementing group and household level activities. Community-level activities included the ‘Whole System in the Room’ [51], community mobilization and commitment events, and cross-fertilization visits. These activities intended to engage community stakeholders in action planning, create an enabling environment in which change may occur, and address inter-personal factors related to public commitment, social norms, and social support related to improved practices, among others. WDALs from each intervention kebele were trained on how to conduct Andilaye household counseling visits with caregivers from each household in her catchment area. WDALs are unpaid community health workers as part of the government-organized Women’s Development Army (WDA) strategy, which uses networks of neighboring women to increase the efficiency of HEWs in reaching every household, with one WDAL for every 30 households. During household-level counselling visits, trained WDALs provided personalized counselling to caregivers to equip them with the knowledge, skills, and motivation necessary to adopt and maintain improved WASH practices. Structured community conversations, implemented by trained community facilitators, provided further opportunity for group-level counselling and support.
Fig 2. The Andilaye Trial consists of three major phases: (1) formative research and intervention design, (2) intervention implementation and process evaluation, and (3) impact evaluation.
Kebele and household enrollment took place during baseline data collection (March to April 2017). Implementation of Andilaye intervention activities began in September 2017 and continued through midline data collection (March to April 2018), quarterly monitoring (June to July and November to December 2018), and endline evaluation (March to May 2019). See S1 Table for specific dates of the delivery of intervention activities. Midline data reflected at least 2 months since the start of household-level behavior change activities and 3 weeks since the completion of a catalyzing community-level mobilization and commitment event. Our endline data reflected the implementation of 14–15 months of household-level behavior change activities and 6–7 months of group-level behavior change activities (as dictated by trained activity facilitators) and 13–14 months since the community mobilization and commitment events.
Outcomes of interest
Survey instruments administered for our impact evaluation collected data on key outcomes through self-reports from respondents and other household members. Primary outcomes of interest included mental health and three targeted WASH behavioral themes (1) sanitation, (2) personal hygiene, and (3) household environmental sanitation behaviors, consisting of 11 constituent practices (Table 1). To measures WASH outcomes, we pulled from standard WASH indicators and leveraged formative research data to contextually adapt survey prompts and answer choices (shown in S4 Table of Delea et al., 2019). Sustainability of WASH-related behaviors was measured through the proportion of individuals and households consistently practicing target behaviors at midline and endline.
For mental health, we assessed subjective well-being using the validated WHO’s Well-Being Index (WHO-5) [52] and symptoms of anxiety, depression, and non-specific emotional distress using the Hopkins Symptom Checklist (HSCL) [53]. WHO-5 asks the respondent to indicate how frequently they relate to each of five statements in the previous two weeks using a five-point Likert scale. Higher scores are better (range: 0–25) with scores below 13 indicating poor well-being. The HSCL is a non-diagnostic tool that includes 25 items to assess symptoms of anxiety (items 1–10), depression (items 11–25) and overall emotional distress (all 25 items). We omitted two items from the depression set: an item on sexual desire, which was deemed inappropriate for unmarried women, and an item on suicide ideation, because we were unable to provide clinical recourse if needed. Participants indicated how much symptoms bothered them in the previous week (‘not at all’ [1] to ‘Extremely’ [4]). The final score for each state is a mean of responses for each of the relevant items (range from 1 to 4). Scores of 1.75 or higher indicate that the condition could be present while lower scores are an indication of lower anxiety, depression, or distress.
Secondary outcomes included 7-day and 2-day diarrhea period prevalence, measured through caregiver report of the index child (i.e., youngest child in the household aged one to nine years at baseline), sanitation insecurity, and water insecurity. For sanitation insecurity, we asked respondents to indicate how often (never, sometimes, often, always) they felt one of seven different forms of sanitation insecurity (i.e., 7 factors). Scores were means of all items in the factor. A higher score represents higher sanitation insecurity. The factors were predesignated, and based on a validation that was done in another study [23]. Water insecurity was measured through the Household Water Insecurity Experiences (HWISE) scale [54]. HWISE includes 12 items with four response categories (never, rarely, sometimes, often/always). The score is the sum of responses, ranging from 0–36. A higher score indicates greater household water insecurity, and we considered households to be water insecure with a score of 12 or more, as described elsewhere [54]. Measures of collective efficacy [50] and intermediate behavioral antecedents were also collected, but are not reported here.
Process evaluation
We conducted a process evaluation alongside our impact evaluation to describe and analyze key aspects of the Andilaye’s implementation and provide insights and understanding of program impacts. We defined fidelity as the degree to which the intervention or program was delivered as intended [55]. Quantitative process data on dose delivered, participation, and dose received were collected through the direct observation of all district and community-level activities—these activities being facilitated or co-facilitated by the Ethiopia-based study team. Questions were incorporated into our survey instruments administered during quarterly monitoring and endline data collection to capture exposure to key Andilaye behavior change activities by respondents from study-enrolled households in intervention kebeles. This included self-reported awareness of and attendance at the community mobilization and commitment event and community conversations, and the number of household counseling visits received from WDALs. Per protocol, all community members were targeted to attend the community mobilization and commitment event; routine (1–2 per month) community conversations primarily focused on influential community members (e.g., male heads of households, religious leaders, mother-in-laws) targeted in the ‘Whole System in the Room’; and caregivers were to receive monthly household counseling visits (each visit lasting approximately 30 minutes) following the typical structure for the WDAL and in accordance the HEP.
Sample size and power
A detailed description of sample size considerations is published in the study protocol [41]. Briefly, we powered this study on mental well-being outcomes, as measure by the HSCL [53], utilizing data from Ethiopia and East Africa suggesting that approximately 20–35% of rural women experience elevated symptoms of anxiety and depression [56, 57]. Our sample size determination indicated we should recruit and enroll 25 households from each of our 50 study kebeles, with 25 kebeles per study arm, targeting one index child per household. We increased our final sample size to accommodate for 20% of households being lost to follow-up. Our target sample, therefore, included 30 households in each kebele, or 1,500 households in total (i.e., 750 per study arm).
Data collection
Data were collected via structured household interviews and observations by trained enumerators during rounds of data collection. Surveys were collected using mobile phones equipped with the freely available Open Data Kit (http://opendatakit.org/). Households with at least one child aged one to nine years were randomly selected from the gott census book residing in the target gott(s) of the 50 study kebeles at baseline, and were followed for each round of data collection. Fig 2 and S1 Table provide a summary of the timeline of intervention implementation in relation to points of data collection for our impact evaluation. At the time of endline data collection, household-level activities had taken place for the past 14–15 months, group-level activities for the past 6–7 months, and community-level mobilization and commitment events were completed 13–14 months prior. Elements of the intervention were still ongoing during the time of our endline data collection, and we did not collect further data after the endline visit. Given the nature of the intervention, neither participants nor field teams were blinded to intervention status.
Analytical methods
We followed a pre-analysis plan developed following baseline data collection [41]. The primary analysis method was an “intention-to-treat” analysis, which compares the intervention arm to the control arm without regard to intervention fidelity or compliance. The majority of our primary and secondary outcomes were binary variables, and for these we used log-linear binomial regression models and report the prevalence ratio (PR). For these binary outcomes we also present prevalence differences (PD), which were calculated using the post-estimation margins command to estimate the average marginal effects. For continuous outcomes, such as WHO-5 and HSCL scores, we used linear regression models. All models included an intervention variable as a fixed effect, accounted for the stratified design through the inclusion of the woreda indicator variable [58], and incorporated generalized estimating equations with robust standard errors to account for the clustering of observations within kebeles. For each of our primary outcomes of interest, we assessed if there was interaction across various sub-groups, including exposure to previous CLTSH triggering and sex of the index child. We also assessed if water insecurity modified the effectiveness on hygiene behaviors. For all of these analyses, we included interaction terms to test if effect modification was present (i.e., the interaction term had a p-value <0.05).
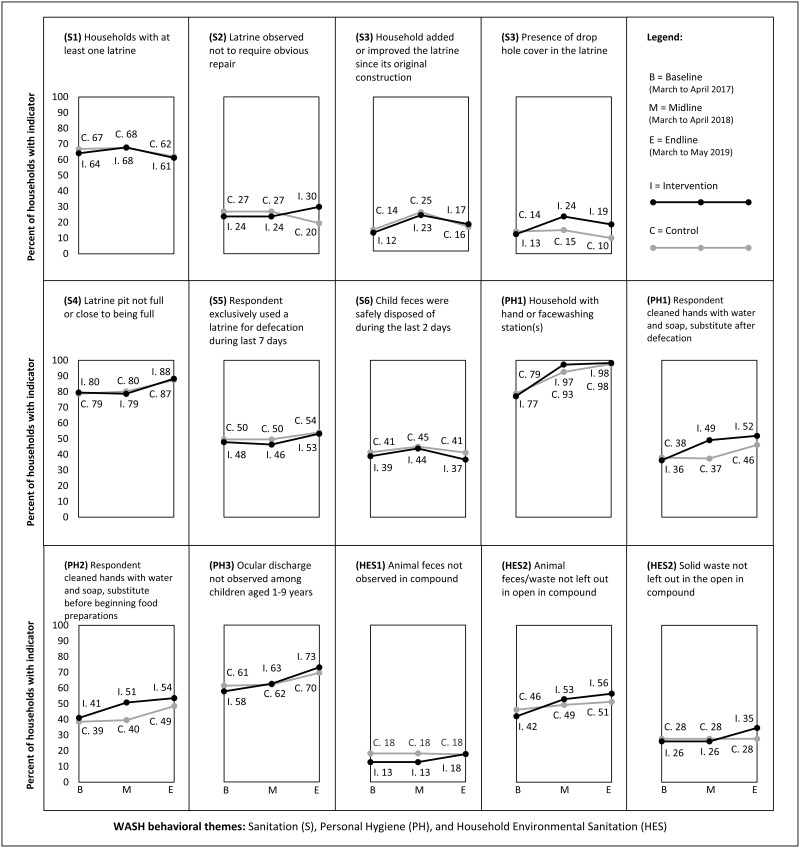
To assess whether any improvements in WASH behaviors were sustained between follow-up periods, we compared the prevalence of key targeted sanitation, hygiene, household environmental sanitation indicators between the demand-side intervention arm and the control arm group using the baseline, midline, and endline data (Fig 2).
Results
Survey results
Our baseline assessment showed balance in terms of our primary outcomes of interest and demographic variables [41]. Our endline results reflect complete data from 1,472 (93%) of 1,589 households enrolled in the study at baseline, and exceeded our sample size requirement of 1,250 households. Of the 793 enrolled intervention households and 796 enrolled control households, retention was similar in both arms, at 94% and 92%, respectively (Fig 1). A large majority (90%) of the respondents were female, who were typically the primary caretakers. Of these 1,472 respondents, 85% were the mother of the index child.
Process evaluation
Reports from Woreda Health Offices collected at endline indicated that none of the 50 study kebeles (intervention or control) received additional CLTSH triggering or re-triggering during the course of the Andilaye Trial. For the Andilaye intervention, the fidelity of action planning workshops and trainings at the district and community levels were high (See S3 Table for a summary of process data on dose delivered, participation, and dose received for all intervention activities). All three study woredas and their intervention kebeles (n = 25) had action planning and management (S3a Table) and training and capacity building (S3b Table) intervention activities completed as planned, at the district and community levels, respectively. Participation was high among targeted government and community stakeholders during catalyzing and maintenance action planning and management activities (S3a Table). Nearly all of our targeted Woreda Health Office officials, HEWs, and WDALs were trained on Andilaye counseling visits with caregivers and all intervention kebeles had a pair of facilitators trained on Andilaye community conversations—including rounds of review meetings and refresher trainings (S3b Table). All intervention kebeles had a community mobilization and commitment event completed as planned, with an estimated average of around 300 adult community members in attendance per event (S3c Table).
Our household process evaluation survey results reflect complete data from 703 (89%) and 707 (89%) of 793 study-enrolled households in intervention kebeles from quarterly monitoring and endline data collection, respectively. Reported frequency of household-level counseling visits reflected a total of 665 study-enrolled households as these questions were not relevant for 42 households that were residents of WDALs who were trained to conduct Andilaye counselling visits.
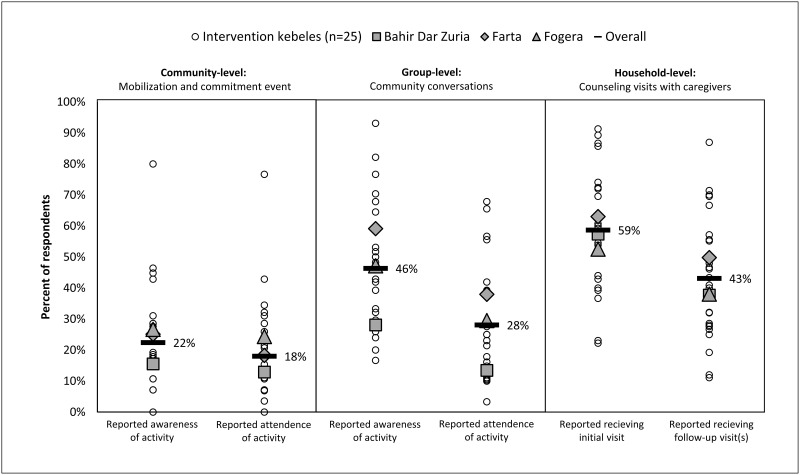
Household respondent-reported exposure of key behavior change activities varied, but was generally suboptimal (Fig 3). Overall, only 18% of respondents reported attending the community mobilization and commitment event, and 22% reported being aware of the activity in the months following the event (i.e., during quarterly monitoring). At endline, 28% of respondents reported attending at least one community conversation, and 46% reported being aware of the activity. WDALs and their supervisors (i.e., HEWs) were trained to facilitate monthly counseling visits with households in their catchment area. However, at endline, only 59% of respondents reported receiving a counseling visit and 43% reported receiving at least one follow-up visit during the 14-15-month implementation period. No intervention kebele had WDALs conducting counseling visits monthly. The average number of visits was 2–3 among respondents reporting at least one counseling visit (n = 391) (S3c Table). For households receiving a visit, 72% of respondents reported that they set household goals or incremental improvements, and two-thirds reported that they identified barriers and their WDAL provided counseling on how to plan for, cope with, and overcome barriers in accordance to the Andilaye behavior change tools (i.e., household counseling flipbook and goal cards) (S3c Table).
Fig 3. Respondent-reported exposure of key behavior change activities of the Andilaye intervention.
Respondents from study-enrolled households in intervention kebeles (n = 793) were surveyed on their awareness and attendance in the community-level mobilization and commitment event during quarterly monitoring visits and awareness and attendance of group-level community conversations and frequency household-level counseling visits received by endline visits. A total of 703 (89%) and 707 (89%) surveys with responses to process evaluation prompts were completed from quarterly monitoring and endline, respectively. Reported frequency of counseling visits reflected a total of 665 survey responses as these questions were not relevant for study-enrolled households that were residents of caregivers who were trained as Women’s Development Army Leaders (WDALs) responsible for conducting the Andilaye counselling visits (n = 42).
Impacts on sanitation, personal hygiene, and household environmental sanitation
The intervention did not increase latrine access. At endline, 62% of both intervention and control households had at least one latrine (prevalence ratio [PR] 0.99; 95% CI: 0.82, 1.21) (Table 1). There was no difference in the prevalence of improved latrines (PR 1.13; 95% CI: 0.81, 1.59) or in fully constructed latrines (PR 1.15; 95% CI: 0.86, 1.54). Although there were improvements in many latrine characteristics in the intervention arm compared to the control arm (e.g., presence of water available or cleansing agent near or inside the latrine for handwashing, and water available for flushing or self-cleansing), the conditions (e.g., presence of feces on floor) of latrines in the intervention arm were often poor (S4 Table).
The intervention did not impact defecation practices. Overall, 40% of respondents reported practicing open defecation during the previous two days; only 46% of respondents had defecated in any latrine during the previous two days (S4 Table). All measures of latrine utilization and non-utilization were similar across intervention and control arms. This includes indicators of respondent open defecation (PR: 1.05; 95% CI: 0.76, 1.45), safe disposal of child feces (PR: 0.96; 95% CI: 0.69, 1.32), and number of people from another household who used a latrine during last seven days (difference: -0.40; 95% CI: -0.85, 0.05).
The intervention did not impact personal hygiene behaviors. The prevalence of washing stations with water (PR: 0.96; 95% CI: 0.72, 1.26) was similar between the intervention and control arms. Presence of hand or face washing stations were observed in 98% of households (Table 1), although water and soap were observed in only 20% of handwashing stations and 2% of facewashing stations (S4 Table). The prevalence of stations with soap was higher in the intervention arm, although only 3% of households in this arm had a washing station with soap present. Among all children aged one to nine years at endline, observations of facial cleanliness indicated 29% had ocular discharge, 38% had wet nasal discharge, 44% had dry nasal discharge, and 50% had dust, dirt, or debris on their faces (Table 1). There were no meaningful differences between the study arms for any of these facial cleanliness measures.
We found no evidence that the Andilaye intervention impacted household environmental sanitation. Across both arms, the majority of respondents and heads of household had animal herding responsibilities (88% overall), and animal feces were present in the compound in 82% household compounds (S4 Table). A similar proportion of households in intervention and control kept animals separate from the house (PR = 1.01, 95% CI 0.91, 1.11). About half of households did not leave animal feces/waste in the open (Table 1); this was similar between the intervention and control arms (PR = 1.10; 95% CI: 0.95, 1.28).
Sustained changes of key indicators
There was little difference in the sustainability of key targeted indicators—assessed by changes between midline and endline—on sanitation access and practices, personal hygiene access and practices, and household environmental sanitation over the course of follow up (Fig 4). At midline, most variables continued to show little difference between the intervention and control arms, although the prevalence of drop hole covers in latrines and the prevalence of appropriate hygiene behaviors were more common in the intervention arm. At the endline visit, the prevalence of drop hole cover was largely sustained in the intervention arm, while the prevalence of drop hole covers decreased in the control arm (PR = 1.77’ 95% CI: 1.19, 2.63). All other variables at endline had similar prevalence levels when comparing the two arms. While the prevalence of hand hygiene behaviors was maintained at levels similar to the midline visit, increases in hand hygiene behaviors in the control arm narrowed the difference between the intervention and control arms at endline. Over the two follow-up surveys, there was an increase in the prevalence of household hand or facewashing stations that appeared among study arms.
Fig 4. The prevalence of key sanitation, personal hygiene, and household environmental sanitation indicators over time.
Impacts on mental health
There was no difference between study arms in the scores for anxiety, depression, emotional distress or general well-being (Table 2). There was also no difference between the intervention and control arms in the prevalence of each mental health condition: anxiety (PR = 0.90; 95% CI: 0.72, 1.11), depression (PR: 0.83; 95% CI: 0.64, 1.07), emotional distress (PR: 0.86; 95% CI: 0.67, 1.09) and poor well-being (PR: 0.90; 95% CI: 0.74, 1.10) (Table 2). All measures of mental health trended in the protective direction for both mean scores and prevalence (2–3% reduction), but were not statistically different between study arms.
Table 2. Mental well-being outcomes at endline.
| Indicator | Cronbach Alpha | Intervention | Control | ||||
|---|---|---|---|---|---|---|---|
| Scores | N | Mean (SD) | N | Mean (SD) | - | difference (95% CI) a e | |
| Anxiety score b | 0.89 | 742 | 1.46 (0.61) | 729 | 1.52 (0.64) | - | ‒0.06 (‒0.14, 0.02) |
| Depression score b | 0.87 | 742 | 1.35 (0.48) | 728 | 1.39 (0.52) | - | ‒0.04 (‒0.08, 0.01) |
| Emotional distress score b | 0.93 | 741 | 1.29 (0.46) | 728 | 1.33 (0.49) | - | ‒0.04 (‒0.09, 0.01) |
| Well-being score c | 0.97 | 749 | 17.6 (6.8) | 728 | 17.0 (6.7) | - | 0.50 (‒0.19, 1.28) |
| Prevalence | N | % | N | % | PR (95% CI) d | PD (95% CI) e | |
| High Anxiety f | - | 742 | 22.2 | 729 | 24.8 | 0.90 (0.72, 1.11) | ‒0.03 (‒0.08, 0.03) |
| High Depression f | - | 742 | 14.0 | 728 | 16.9 | 0.83 (0.64, 1.07) | ‒0.03 (‒0.07, 0.01) |
| High Emotional distress f | - | 741 | 14.0 | 728 | 16.4 | 0.86 (0.67, 1.09) | ‒0.02 (‒0.06, 0.01) |
| Poor well-being g | - | 749 | 25.2 | 728 | 27.8 | 0.90 (0.74, 1.10) | ‒0.03 (‒0.08, 0.02) |
Notes.
a We used linear regression models to estimate the difference in the outcomes comparing the intervention and control arms. Models accounted the stratified design by including woreda indicator variables [58], and accounted for clustering within kebeles by using generalized estimating equations with robust standard errors.
b We asked respondents to indicate how much the symptoms bothered them in the previous week with four potential response options (not at all (1) to extremely (4)). The first ten symptoms assess anxiety (i.e., ‘suddenly scared for no reason’, ‘nervousness or shakiness inside’), the next 13 assess depression (i.e. ‘feeling low in energy’, ‘feeling hopeless about the future’), and the 23 collectively assess non-specific emotional distress. For each outcome, the score is the sum of the responses divided by the number of items.
c We asked respondents about well-being, and responses ranged from ‘(0) At no time’ to (5) All of the time’. Scores were summed, and range from 0–25; the higher the score, the better the well-being.
d We used similar log-linear binomial regression models to compare the prevalence of the outcomes between the intervention and control arms.
e Prevalence differences (PD) were calculated using post-estimation commands to estimate the average marginal effects.
f Each of the above scores was dichotomized, with scores greater than 1.75 indicating a positive status for any of the three outcomes.
g The above score was dichotomized with scores below 13 indicating poor well-being.
Secondary health outcomes
Reported diarrhea
Diarrhea prevalence during the last seven days among index children was similar in the intervention (7%) and control (6%) arms (PR: 1.20; 95% CI: 0.74, 1.93; Table 3). Among index children, there were also similarities comparing study arms in diarrhea prevalence when assessing episodes over the last two days (PR: 1.25; 95% CI: 0.71, 2.22).
Table 3. Secondary health outcomes at endline.
| Indicator | Cronbach Alpha | Intervention | Control | ||||
|---|---|---|---|---|---|---|---|
| Diarrhea | N | % | N | % | PR (95% CI) a | PD (95% CI) b | |
| During the last 2 days, index child had three or more loose stools per day | - | 730 | 5.9 | 720 | 4.7 | 1.62 (0.71, 2.22) | 0.01 (‒0.018, 0.042) |
| During the last 7 days, index child had three or more loose stools per day | - | 731 | 7.1 | 721 | 6.0 | 1.20 (0.74, 1.93) | 0.01 (‒0.019, 0.043) |
| Water and sanitation insecurity scores | N | mean (SE) | N | mean (SE) | - | difference (95% CI) c | |
| Water-HWISE Scale d | 0.96 | 565 | 1.71 (0.37) | 388 | 2.71 (0.89) | - | ‒1.29 (‒3.19, 0.61) |
| Sanitation-Potential harmsd | 0.85 | 365 | 0.46 (0.026) | 327 | 0.50 (0.033) | - | ‒0.05 (‒0.13, 0.03) |
| Sanitation-Social expectations resultant repercussions d | 0.79 | 366 | 0.28 (0.025) | 327 | 0.30 (0.022) | - | ‒0.03 (‒0.09, 0.03) |
| Sanitation-Physical exertion or strain d | 0.57 | 366 | 0.42 (0.046) | 328 | 0.40 (0.043) | - | 0.01 (‒0.11, 0.13) |
| Sanitation-Night concerns d | 0.56 | 366 | 0.32 (0.022) | 328 | 0.37 (0.027) | - | ‒0.05 (‒0.12, 0.02) |
| Sanitation-Social support d | 0.88 | 366 | 0.10 (0.021) | 328 | 0.20 (0.023) | - | ‒0.10 (‒0.16, ‒0.43) |
| Sanitation-Physical agility d | 0.56 | 366 | 0.14 (0.017) | 328 | 0.14 (0.020) | - | 0.00 (‒0.05, 0.05) |
| Sanitation-Defecation place d | 0.81 | 366 | 0.35 (0.038) | 327 | 0.32 (0.028) | - | 0.02 (‒0.06, 0.11) |
| Water insecurity prevalence | N | % | N | % | PR (95% CI) a | PD (95% CI) b | |
| Water insecure (HWISE score 12 or more) d | - | 565 | 5.7 | 388 | 8.8 | 0.50 (0.21, 1.23) | -0.05 (-0.12, 0.03) |
Notes.
a We used log-linear binomial regression models to compare the prevalence of the outcomes between the intervention and control arms. Models accounted the stratified design by including woreda indicator variables [58], and accounted for clustering within kebeles by using generalized estimating equations with robust standard errors.
b Prevalence differences (PD) were calculated using post-estimation commands to estimate the average marginal effects.
c We used similar linear regression models to estimate the difference in the outcomes comparing the intervention and control arms.
d We asked respondents to indicate how often they felt some form of sanitation insecurity (never, sometimes, often, always). These items were then summed with all other items in that factor and divided by the numbers of items to create a score. The factors were predesignated, and based on a validation that was done in another study [23]. A higher score represents higher sanitation insecurity. d We used similar linear regression models to estimate difference comparing the outcomes between the intervention and control arms. This used a 12-item scale with four response categories (never, rarely, sometimes, often/always), and a total summed score of those response categories ranging from 0–36. A higher score indicates greater household water insecurity. We considered water insecure as a score of 12 or more, as described elsewhere [54].
Water and sanitation insecurity
The intervention did not statistically reduce water insecurity prevalence between intervention (5.7%) and control (8.8%) arms (PR: 0.50 (95% CI: .21, 1.2); Table 3). At endline, sanitation insecurity scores related to social support were statistically lower (i.e., better) in the intervention arm than in the control arm (score difference: -0.10, 95% CI: -0.16, -0.43), indicating a reduced frequency of experiencing the circumstances in the social support domain (e.g., trouble finding support to watch dependents during urination, worry about dependents when going to defecate, had to leave dependents alone to urinate, etc.). Other sanitation insecurity measures were similar between arms.
Interaction and effect modification
There was no interaction of the intervention by previous CLTSH triggering for any of the primary outcome variables of interest. We did not detect effect measure modification by sex for any of the four mental health outcomes. Similarly, we did not detect interaction by child’s sex for any of these outcomes. We also did not detect interaction between the intervention and water insecurity on any of the primary handwashing or face washing variables.
Discussion
The Andilaye intervention generally did not improve WASH conditions or outcomes. Without sustained changes to these WASH conditions and behaviors, changes in well-being were not likely, and indeed, were not detected. Improving sanitation and hygiene behaviors in rural communities remains a considerable challenge, especially in regions with poor water access and high levels of WASH-related NTD endemicity. Most studies designed to change sanitation and hygiene behavior are efficacy studies [27]—meant to assess changes under controlled conditions; ours was an effectiveness study, designed to measure changes in a real-world context. We believe that poor fidelity of intervention delivery played a considerable role in uptake of the intervention, pointing to challenges in delivering demand-side sanitation and hygiene interventions at scale and through existing community-based models.
We did not find statistical differences between study arms at endline and few promising trends in intervention communities for some of the targeted behaviors. Changes were much lower than with approaches found by Crocker et al. elsewhere in Ethiopia [33, 36]. Similarly, Apanga et al. found that implementation of the Rural Sustainable Sanitation and Hygiene for All (SSH4A) approach that employs a multidimensional intervention led to a large increase of 77 percentage points in sanitation coverage in Ethiopia and also coverage gains in many other countries under study [59], although slippage did occur after conclusion of program activities, whereas many other countries sustained their previous sanitation coverage gains [60].
Our Andilaye intervention did not statistically impact validated mental health measures. Few studies have measured the impact of a sanitation intervention on mental health outcomes despite calls for broader investigations of sanitation-related health impacts [14, 61, 62]. In rural India, women’s experiences of sanitation, as measured by a validated sanitation insecurity measure, were associated with well-being, anxiety, depression, and distress, even when women had access to a facility [25]. Similarly, in urban Mozambique, latrine location and neighborhood violence were important determinants of safety perceptions and corresponding psychosocial stress [63]. These findings highlight the need for interventions to consider the experience of sanitation beyond access to a facility alone and the intrinsic value of sanitation [64]. We assessed if changes to sanitation access and sanitation insecurity—changes that we anticipated would be generated by this intervention—would lead to improved mental health states, including improved well-being and reduction in symptoms associated with anxiety, depression, distress and general wellbeing. The intention-to-treat analysis did not detect changes to mental well-being scores or to sanitation insecurity scores, which was perhaps limited by our short evaluation period, and sanitation quality (Fig 2). However, we saw some, non-statistically different, preventive trends across all mental health measures which were primarily among women (90% of respondents). Our impact on sanitation social support is indicative of the underlying philosophy of the Andilaye intervention, which was designed contrary to the “shame” drivers of more traditional CLTSH [28, 65]. These findings are encouraging despite the low fidelity of the intervention delivery at household-level, suggesting improved fidelity may result in evidence of impact. We believe further studies are warranted to test the hypothesis that improved sanitation would impact mental well-being, as our intervention did not change sanitation behaviors, quality, or access.
The purpose of this study was to develop and test an intervention that could be scaled within the existing Ethiopian HEP. The intervention was designed to be incorporated into prevailing programs (e.g., HEP) to demonstrate potential for scale-up, and did not succeed in this regard. For example, despite high attendance at trainings and action planning workshops, and the provision of supportive supervision and on-the-job-training tools, many households did not receive Andilaye counseling visits (Fig 3). WDALs and HEWs reported that they did not receive supportive supervision from relevant government officials in accordance with their action plans (S3b Table). While supportive supervision considerations were acknowledged and incorporated into the design of the Andilaye intervention, these requirements did not go above and beyond what is expected of the HEP (S2 Table) [66]. These delivery challenges are consistent with those associated with CLTSH programming and HEP more broadly [37, 67]. Additionally, a majority of intervention kebeles had non-active WDALs at the start of implementation, as identified by our Ethiopian-based study team during initial recruitment of activity facilitators. At endline, only 66% of respondents from our process evaluation surveys were able to identify the WDAL responsible for conducting their Andilaye counseling visits (S3c Table). A cross-sectional study in four regions of Ethiopia found similar trends in varying levels of WDAL strategy implementation strength among 423 kebeles [68]. Importantly, findings from Damtew et al. suggest HEP outreach activities were higher in kebeles where active WDAL density was higher (i.e., fewer households per active WDAL). Although HEWs were paid health workers, WDALs were not. This has brought questions of ethics and sustainability as WDALs are increasingly asked to provide more and more services. Recent qualitative and quantitative studies suggest that unpaid WDALs are actually worse off than their peers and makes women, especially unmarried women, vulnerable to negative gossip and psychological distress [69, 70]. Although this point goes much deeper into the political economy, it is an important gap to bring up in the context of empowering women volunteers to enact positive change in their communities [71]. Further, when community health workers are paid to deliver the intervention, there is evidence of successful delivery [72]. Together, these findings raise questions about the possibility of bringing new programs and approaches to the HEP without adequate support.
Evidence suggests that it is important to move away from information-based interventions to address the array of behavioral factors and determinants that operate at various levels of influence [73–78]. Few sanitation and hygiene interventions employ behavioral theory to locally adapt messages [36, 79]. Exceptions include the SuperAmma intervention, which was developed and implemented in India, and found substantial gains in handwashing with soap [80] and studies that examined the effectiveness of the risk, attitudes, norms, abilities and self-regulation (RANAS) behavioral model to intervention design and showed positive impacts on a variety of WASH behaviors including safe water consumption, solar water disinfection, handwashing, and cleaning of shared sanitation [81–87]. Our intervention aimed to focus on a variety of contextually appropriate behavioral factors rather than knowledge alone. Given the low fidelity of the intervention delivery, further capacity building of federal, regional, and local-level government officials as well as community-level change agents may be necessary for the successful implementation of approaches that move beyond dissemination of information and messages [88–90].
The WASH sector has traditionally relied on unpaid female labor (in this case HEWs, WDALs), which are gender exploitative approaches that reinforce women as the household duty bearers for WASH [91]. While our assessment of mental health highlights the potential impact on women beyond their roles as mothers and caregivers, our intervention strategy provided little exception to the longstanding program strategy of adding to the already burdensome roles as child caregiver. Interventions that fail to assess burdens on women, and mothers in particular, may impose harms or burdens that can exacerbate inequalities [92]. Gender-disaggregated data on the workload of women and girls in household responsibilities [93], as well as better sex-disaggregated data on program outcomes could support WASH strategies that lead to gender transformative, and ultimately more sustainable programming [61].
Study strengths
Our intervention was theory-informed and included an extensive intervention design process during which we emphasized the solicitation and incorporation of feedback from key stakeholders at regional, zonal, woreda, and community-levels. It was designed to be delivered at scale within the Ethiopian HEP. We utilized a randomized study design, in which intervention and control communities were allocated to treatment arms randomly. While CRTs tend to emphasize internal validity, we made considerable effort to enhance external validity. Our study was spread over three woredas in two zones, yielding a heterogeneous mix of contexts and topographical conditions—which serve as a proxy for factors such as soil type, access to markets, and flooding risk—and support external validity of the findings. To improve interval validity, we used a ‘fried egg’ [47] approach—while allocation occurred at the kebele level, intervention activities and data collection occur in one to two sentinel gotts per kebele, purposively selected to minimize spillover. We targeted both rural and peri-urban communities and collected behavioral outcome data on a variety of household members (e.g., primary female caregiver of index child, head of household, all children aged 0–17 years).
Study limitations
The study faced significant delays in gaining local ethical approval to start the project which led to truncated implementation and follow-up periods. Key government actors were less involved than planned, which may have led to sub-optimal fidelity. The integration of Andilaye intervention activities into non-Ethiopian HEP delivery structures (e.g., hired independent community implementers) may yield further investigations into the effectiveness of the intervention on sustained behavior change and mental well-being. Several of our behavioral outcomes were reported (vs. observed), and these types of outcomes may be prone to reporting biases, indicated by differences in our reported and observed measures.
Conclusions
We did not find that the Andilaye intervention yielded changes in behaviors and conditions related to sanitation, personal hygiene, or household environmental sanitation; nor did it impact mental health outcomes. Limited integration of Andilaye activities into the HEP likely explains the minimal impact observed and points to considerable challenges related to implementing demand-side interventions at scale in Ethiopia. There is a crucial need to identify and scale effective service delivery models in order to meet the ambitious Sustainable Development Goal targets for sanitation and hygiene [94]. Evidence from this trial may help address knowledge gaps related to scalable alternatives to CLTSH and inform sanitation and hygiene programming and policy in Ethiopia and beyond. A greater emphasis on implementation research in WASH delivery would support tools and approaches for developing, testing, and adapting scalable best-practice interventions [95].
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The authors would like to thank our Andilaye study participants, who generously gave their time to participate in our formative work, behavioral trials, and summative assessment surveys. We are grateful for the support we receive from numerous partners at the Democratic Republic of Ethiopia’s Federal Ministry of Health; the Amhara Regional Health Bureau; South Gondar and West Gojjam Zonal Health Departments; and the Bahir Dar Zuria, Farta, and Fogera Woreda Health Offices. We would also like to acknowledge support provided by the Health Extension Workers, Women’s Development Army Leaders, and Health Development Army members from our study kebeles. We thank the cadre of field supervisors and enumerators who captured these data (Yeworkwuha Abay, Mantegbosh Abebe, Selamawit Abebe, Tigist Abebe, Rosa Abesha, Mahider Adamu, Balemlaye Addisu, Adanech Admasu, Tirusew Alayu, Adisalem Arega, Yalemwork Asaye, Destaw Asnakew, Yalemwork Ayanew, Ayalnesh Belay, Asayech Bimrew, Tigist Bitew, Tiruzer Engidaw, Yeserash Gashaw, Natsenat Gebretsadkan, Woyneshet Genetu, Tewodaj Gizachew, Tibeltalech Mihiret, Yehizbalem Minale, Senait Mulualem, Eleni Nebiyu, Elsabet Seyoum, Mulubirhan Shitu, Sewunet Tadesse, Beza Tesfaye, Rahel Tsegaye, Sintayehu Wasihun, and Maritu Yibrie).
Data Availability
Data from the trial is available via 10.17605/OSF.IO/VH7YS. Additional information is available via OSF site https://osf.io/vh7ys/.
Funding Statement
This research was funded by grants to Emory University from the World Bank Group (7175829 / PI:MCF), Children’s Investment Fund Foundation (1606-01334 / PI:MCF), and the International Initiative for Impact Evaluation (TW11.1016 / PI:MCF). The funders have otherwise played no role in the design of the study; collection, analysis, or interpretation of the data; or writing of the manuscript.
References
- 1.Freeman MC, Garn JV, Sclar GD, Boisson S, Medlicott K, Alexander KT, et al. The impact of sanitation on infectious disease and nutritional status: A systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220: 928–949. doi: 10.1016/j.ijheh.2017.05.007 [DOI] [PubMed] [Google Scholar]
- 2.Wolf J, Hunter PR, Freeman MC, Cumming O, Clasen T, Bartram J, et al. Impact of drinking water, sanitation and handwashing with soap on childhood diarrhoeal disease: updated meta-analysis and meta-regression. Trop Med Int Health. 2018;23: 508–525. doi: 10.1111/tmi.13051 [DOI] [PubMed] [Google Scholar]
- 3.Troeger C, Blacker BF, Khalil IA, Rao PC, Cao S, Zimsen SR, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18: 1211–1228. doi: 10.1016/S1473-3099(18)30362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392: 1736–1788. doi: 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman MC, Ogden S, Jacobson J, Abbott D, Addiss DG, Amnie AG, et al. Integration of water, sanitation, and hygiene for the prevention and control of neglected tropical diseases: a rationale for inter-sectoral collaboration. PLoS Negl Trop Dis. 2013;7: e2439. doi: 10.1371/journal.pntd.0002439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. WASH and health working together: A “how to” guide for neglected tripical disease programmes. Geneva: World Health Organization & the Neglected Tropical Disease NGO Network; 2019.
- 7.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380: 2197–2223. [DOI] [PubMed] [Google Scholar]
- 8.Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasit Vectors. 2014;7: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82: 844–51. [PMC free article] [PubMed] [Google Scholar]
- 10.Stocks ME, Ogden S, Haddad D, Addiss DG, McGuire C, Freeman MC. Effect of water, sanitation, and hygiene on the prevention of trachoma: a systematic review and meta-analysis. PLoS Med. 2014;11: e1001605. doi: 10.1371/journal.pmed.1001605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prüss-Ustün A, Wolf J, Corvalán C, Bos R, Neira M. Preventing disease through healthy environments: A global assessment of the burden of disease through environmental risks. Geneva: WHO; 2016.
- 12.Grimes JE, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The relationship between water, sanitation and schistosomiasis: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2014;8: e3296. doi: 10.1371/journal.pntd.0003296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC. Water, sanitation, hygiene, and soil-transmitted helminth infection: a systematic review and meta-analysis. PLoS Med. 2014;11: e1001620. doi: 10.1371/journal.pmed.1001620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sclar GD, Penakalapati G, Caruso BA, Rehfuess EA, Garn JV, Alexander KT, et al. Exploring the relationship between sanitation and mental and social well-being: A systematic review and qualitative synthesis. Soc Sci Med. 2018;217: 121–134. doi: 10.1016/j.socscimed.2018.09.016 [DOI] [PubMed] [Google Scholar]
- 15.Bisung E, Elliott SJ. Psychosocial impacts of the lack of access to water and sanitation in low-and middle-income countries: a scoping review. J Water Health. 2017;15: 17–30. doi: 10.2166/wh.2016.158 [DOI] [PubMed] [Google Scholar]
- 16.Kangmennaang J, Elliott SJ. Linking water (in)security and wellbeing in low-and middle-income countries. Water Secur. 2021;13: 100089. doi: 10.1016/j.wasec.2021.100089 [DOI] [Google Scholar]
- 17.Wutich A, Brewis A, Tsai A. Water and mental health. WIREs Water. 2020;7. doi: 10.1002/wat2.1461 [DOI] [Google Scholar]
- 18.Brewis A, Choudhary N, Wutich A. Household water insecurity may influence common mental disorders directly and indirectly through multiple pathways: Evidence from Haiti. Soc Sci Med. 2019;238: 112520. doi: 10.1016/j.socscimed.2019.112520 [DOI] [PubMed] [Google Scholar]
- 19.Collins SM, Mbullo Owuor P, Miller JD, Boateng GO, Wekesa P, Onono M, et al. ‘I know how stressful it is to lack water!’ Exploring the lived experiences of household water insecurity among pregnant and postpartum women in western Kenya. Glob Public Health. 2019;14: 649–662. doi: 10.1080/17441692.2018.1521861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mushavi RC, Burns BFO, Kakuhikire B, Owembabazi M, Vořechovská D, McDonough AQ, et al. “When you have no water, it means you have no peace”: A mixed-methods, whole-population study of water insecurity and depression in rural Uganda. Soc Sci Med. 2020;245: 112561. doi: 10.1016/j.socscimed.2019.112561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stevenson EG, Greene LE, Maes KC, Ambelu A, Tesfaye YA, Rheingans R, et al. Water insecurity in 3 dimensions: An anthropological perspective on water and women’s psychological distress in Ethiopia. Soc Sci Med. 2012;75: 392–400. doi: 10.1016/j.socscimed.2012.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biswas D, Joshi S. Sanitation and gendered psychosocial stress in peri-urban Bangalore. Dev Pract. 2021;31: 548–557. doi: 10.1080/09614524.2020.1862762 [DOI] [Google Scholar]
- 23.Caruso BA, Clasen TF, Hadley C, Yount KM, Haardörfer R, Rout M, et al. Understanding and defining sanitation insecurity: Women’s gendered experiences of urination, defecation and menstruation in rural Odisha, India. BMJ Glob Health. 2017;2: e000414. doi: 10.1136/bmjgh-2017-000414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sahoo KC, Hulland KRS, Caruso BA, Swain R, Freeman MC, Panigrahi P, et al. Sanitation-related psychosocial stress: A grounded theory study of women across the life-course in Odisha, India. Soc Sci Med. 2015;139: 80–89. doi: 10.1016/j.socscimed.2015.06.031 [DOI] [PubMed] [Google Scholar]
- 25.Caruso BA, Cooper HL, Haardörfer R, Yount KM, Routray P, Torondel B, et al. The association between women’s sanitation experiences and mental health: A cross-sectional study in Rural, Odisha India. SSM-Popul Health. 2018;5: 257–266. doi: 10.1016/j.ssmph.2018.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stevenson E, Ambelu A, Caruso B, Tesfaye Y, Freeman M. Community water improvement, household water insecurity, and women’s psychological distress: An intervention and control study in Ethiopia. PloS One. 2016;11: e0153432. doi: 10.1371/journal.pone.0153432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garn JV, Sclar GD, Freeman MC, Penakalapati G, Alexander KT, Brooks P, et al. The impact of sanitation interventions on latrine coverage and latrine use: A systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220: 329–340. doi: 10.1016/j.ijheh.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kar K, Chambers R. Handbook on community-led total sanitation. 2008.
- 29.Patil SR, Arnold BF, Salvatore AL, Briceno B, Ganguly S, Colford JM Jr, et al. The Effect of India’s Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial. PLOS Med. 2014;11: e1001709. doi: 10.1371/journal.pmed.1001709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pattanayak SK, Yang J-C, Dickinson KL, Poulos C, Patil SR, Mallick RK, et al. Shame or subsidy revisited: social mobilization for sanitation in Orissa, India. Bull World Health Organ. 2009;87: 580–587. doi: 10.2471/blt.08.057422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pickering AJ, Djebbari H, Lopez C, Coulibaly M, Alzua ML. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Glob Health. 2015;3: e701–e711. doi: 10.1016/S2214-109X(15)00144-8 [DOI] [PubMed] [Google Scholar]
- 32.Crocker J, Abodoo E, Asamani D, Domapielle W, Gyapong B, Bartram J. Impact evaluation of training natural leaders during a community-led total sanitation intervention: a cluster-randomized field trial in Ghana. Environ Sci Technol. 2016;50: 8867–8875. doi: 10.1021/acs.est.6b01557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crocker J, Geremew A, Atalie F, Yetie M, Bartram J. Teachers and sanitation promotion: an assessment of community-led total sanitation in Ethiopia. Environ Sci Technol. 2016;50: 6517–6525. doi: 10.1021/acs.est.6b01021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guiteras R, Levinsohn J, Mobarak AM. Encouraging sanitation investment in the developing world: a cluster-randomized trial. Science. 2015;348: 903–906. doi: 10.1126/science.aaa0491 [DOI] [PubMed] [Google Scholar]
- 35.Hammer J, Spears D. Village sanitation and child health: effects and external validity in a randomized field experiment in rural India. J Health Econ. 2016;48: 135–148. doi: 10.1016/j.jhealeco.2016.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crocker J, Saywell D, Bartram J. Sustainability of community-led total sanitation outcomes: Evidence from Ethiopia and Ghana. Int J Hyg Environ Health. 2017;220: 551–557. doi: 10.1016/j.ijheh.2017.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Snel M, Jacimovic R. Turning CLTS Challenges into Opportunities for Success. PanAfrican CLTS Programme: Empowering Self-Help Sanitation of Rural and Peri-Urban Communities and Schools in Africa. The Hague, The Netherlands: IRC; 2014.
- 38.Alemu F, Kumie A, Medhin G, Gebre T, Godfrey P. A socio-ecological analysis of barriers to the adoption, sustainablity and consistent use of sanitation facilities in rural Ethiopia. BMC Public Health. 2017;17: 706. doi: 10.1186/s12889-017-4717-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berhe R, Delea M, Sclar G, Woreta M, Zewudie K, Muhammed S, et al. Maintaining behaviour change: innovations in demand-side sanitation and hygiene interventions. Shaw RJ Ed Transform Sustain Resilient WASH Serv Proc 41st WEDC Int Conf Nakuru Kenya 9–13 July 2018. 2018; 6.
- 40.Abebe TA, Tucho GT. Open defecation-free slippage and its associated factors in Ethiopia: a systematic review. Syst Rev. 2020;9: 252. doi: 10.1186/s13643-020-01511-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Delea MG, Snyder JS, Belew M, Caruso BA, Garn JV, Sclar GD, et al. Design of a parallel cluster-randomized trial assessing the impact of a demand-side sanitation and hygiene intervention on sustained behavior change and mental well-being in rural and peri-urban Amhara, Ethiopia: Andilaye study protocol. BMC Public Health. 2019;19: 801. doi: 10.1186/s12889-019-7040-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Flay BR, Petraitis J. The Theory of Triadic Influence: A New Theory of Health Behavior With Implications for Preventive Interventions. Adv Med Sociol. 1994;4: 19–44. [Google Scholar]
- 43.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med Publ Soc Behav Med. 2013;46: 81–95. doi: 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- 44.Mosler HJ. A systematic approach to behavior change interventions for the water and sanitation sector in developing countries: a conceptual model, a review, and a guideline. Int J Env Health Res. 2012;22: 431–49. doi: 10.1080/09603123.2011.650156 [DOI] [PubMed] [Google Scholar]
- 45.CSA-Ethiopia ICF. International: Ethiopia Demographic and Health Survey 2016. Cent Stat Agency Ethiop ICF Int Addis Ababa Ethiop Calverton Md USA. 2017.
- 46.Initiative International Trachoma. Global Trachoma Atlas. Trach Atlas Available. 2019.
- 47.Hayes RJ, Moulton LH. Cluster Randomised Trials. Taylor & Francis; 2009. https://books.google.co.uk/books?id=p-rPAAAACAAJ. [Google Scholar]
- 48.Lachin JM. Statistical properties of randomization in clinical trials. Control Clin Trials. 1988;9: 289–311. doi: 10.1016/0197-2456(88)90045-1 [DOI] [PubMed] [Google Scholar]
- 49.Wang H, Tesfaye R, Ramana G, Chekagn C. Ethiopia Health Extension Program: An Institutionalized Community Approach for Universal Health Coverage. Washington, D.C.: World Bank; 2016. [Google Scholar]
- 50.Delea M, Sclar G, Woreta M, Haardörfer R, Nagel C, Caruso B, et al. Collective efficacy: Development and validation of a measurement scale for use in public health and development programmes. Int J Environ Res Public Health. 2018;15: 2139. doi: 10.3390/ijerph15102139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Federal Democratic Republic of Ethiopia Ministry of Health. Implementation Guideline for CLTSH Programming. Addis Ababa. 2012.
- 52.Bech P. Measuring the dimension of psychological general well-being by the WHO-5. Qual Life Newsl. 2004; 15–16.
- 53.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav Sci. 1974;19: 1–15. doi: 10.1002/bs.3830190102 [DOI] [PubMed] [Google Scholar]
- 54.Young SL, Boateng GO, Jamaluddine Z, Miller JD, Frongillo EA, Neilands TB, et al. The Household Water InSecurity Experiences (HWISE) Scale: development and validation of a household water insecurity measure for low-income and middle-income countries. BMJ Glob Health. 2019;4. doi: 10.1136/bmjgh-2019-001750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci. 2007;2: 40. doi: 10.1186/1748-5908-2-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hadley C, Tegegn A, Tessema F, Cowan JA, Asefa M, Galea S. Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: evidence from the Gilgel Gibe growth and development study. J Epidemiol Community Health. 2008;62: 980–986. doi: 10.1136/jech.2007.068460 [DOI] [PubMed] [Google Scholar]
- 57.Hadley C, Patil CL. Food insecurity in rural Tanzania is associated with maternal anxiety and depression. Am J Hum Biol. 2006;18: 359–368. doi: 10.1002/ajhb.20505 [DOI] [PubMed] [Google Scholar]
- 58.Kahan BC, Morris TP. Reporting and analysis of trials using stratified randomisation in leading medical journals: review and reanalysis. BMJ. 2012;345: e5840. doi: 10.1136/bmj.e5840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Apanga PA, Garn JV, Sakas Z, Freeman MC. Assessing the Impact and Equity of an Integrated Rural Sanitation Approach: A Longitudinal Evaluation in 11 Sub-Saharan Africa and Asian Countries. Int J Environ Res Public Health. 2020;17: 1808. doi: 10.3390/ijerph17051808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sakas Z, Apanga PA, Freeman M, Snyder JS, Garn JV. Assessing the sustainability of an integrated rural sanitation approach in 10 countries in Africa and Asia. Colorado WASH Symposium; 2021 Mar 11; University of Colorado, Boulder.
- 61.Caruso BA, Sevilimedu V, Fung IC-H, Patkar A, Baker KK. Gender disparities in water, sanitation, and global health. Lancet Lond Engl. 2015;386: 650–651. doi: 10.1016/S0140-6736(15)61497-0 [DOI] [PubMed] [Google Scholar]
- 62.Pradyumna A, Im P, Ck G. Moving beyond sanitation’s diarrhoea fixation. Lancet Glob Health. 2015;3: e16. doi: 10.1016/S2214-109X(14)70288-8 [DOI] [PubMed] [Google Scholar]
- 63.Shiras T, Cumming O, Brown J, Muneme B, Nala R, Dreibelbis R. Shared latrines in Maputo, Mozambique: exploring emotional well-being and psychosocial stress. BMC Int Health Hum Rights. 2018;18: 30. doi: 10.1186/s12914-018-0169-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jain A, Subramanian SV. Intrinsic and instrumental perspectives to sanitation. SSM—Popul Health. 2018;5: 267–269. doi: 10.1016/j.ssmph.2018.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bateman M, Engel S. To shame or not to shame—that is the sanitation question. Dev Policy Rev. 2018;36: 155–173. doi: 10.1111/dpr.12317 [DOI] [Google Scholar]
- 66.Workie NW and R Gandham NV. Ethiopia—The health extension program in Ethiopia. Washington, DC: World Bank; 2013. http://documents.worldbank.org/curated/en/356621468032070256/Ethiopia-The-health-extension-program-in-Ethiopia.
- 67.Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15: 24. doi: 10.1186/s12992-019-0470-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Damtew ZA, Karim AM, Chekagn CT, Fesseha Zemichael N, Yihun B, Willey BA, et al. Correlates of the Women’s Development Army strategy implementation strength with household reproductive, maternal, newborn and child healthcare practices: a cross-sectional study in four regions of Ethiopia. BMC Pregnancy Childbirth. 2018;18: 373. doi: 10.1186/s12884-018-1975-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maes K, Closser S, Tesfaye Y, Abesha R. Psychosocial distress among unpaid community health workers in rural Ethiopia: Comparing leaders in Ethiopia’s Women’s Development Army to their peers. Soc Sci Med. 2019;230: 138–146. doi: 10.1016/j.socscimed.2019.04.005 [DOI] [PubMed] [Google Scholar]
- 70.Maes K, Closser S, Tesfaye Y, Gilbert Y, Abesha R. Volunteers in Ethiopia’s women’s development army are more deprived and distressed than their neighbors: cross-sectional survey data from rural Ethiopia. BMC Public Health. 2018;18: 258. doi: 10.1186/s12889-018-5159-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Closser S, Napier H, Maes K, Abesha R, Gebremariam H, Backe G, et al. Does volunteer community health work empower women? Evidence from Ethiopia’s Women’s Development Army. Health Policy Plan. 2019. doi: 10.1093/heapol/czz025 [DOI] [PubMed] [Google Scholar]
- 72.Fankhauser K, Nagel CL, Barstow CK, Kirby M, Thomas EA. Geospatial-temporal, demographic, and programmatic adoption characteristics of a large-scale water filter and improved cookstove intervention in Western Province, Rwanda. Cogent Environ Sci. 2019;5: 1625481. [Google Scholar]
- 73.Briscoe C, Aboud F. Behaviour change communication targeting four health behaviours in developing countries: a review of change techniques. Soc Sci Med 1982. 2012;75: 612–621. doi: 10.1016/j.socscimed.2012.03.016 [DOI] [PubMed] [Google Scholar]
- 74.Hulland K, Martin N, Dreibelbis R, DeBruicker Valliant J, Winch P. What factors affect sustained adoption of safe water, hygiene and sanitation technologies? A systematic review of literature Hulland K, Martin N, Dreibelbis R, DeBruicker Valliant J, Winch P (2015) What factors affect sustained adoption of safe water, hygiene and sanitation technologies? A systematic review of literature. London: EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London. UCL Institute of Education, University College London: London: EPPI-Centre, Social Science Research Unit; 2015 p. 169.
- 75.Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: the importance of targeting automatic processes. Science. 2012;337: 1492–1495. doi: 10.1126/science.1226918 [DOI] [PubMed] [Google Scholar]
- 76.Rabbi SE, Dey NC. Exploring the gap between hand washing knowledge and practices in Bangladesh: a cross-sectional comparative study. BMC Public Health. 2013;13: 89. doi: 10.1186/1471-2458-13-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wood W, Neal DT. Healthy through habit: Interventions for initiating & maintaining health behavior change. Behav Sci Policy. 2016;2: 71–83. doi: 10.1353/bsp.2016.0008 [DOI] [Google Scholar]
- 78.Delea MG, Solomon H, Solomon AW, Freeman MC. Interventions to maximize facial cleanliness and achieve environmental improvement for trachoma elimination: A review of the grey literature. PLoS Negl Trop Dis. 2018;12: e0006178. doi: 10.1371/journal.pntd.0006178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Whittington D, Radin M, Jeuland M. Evidence-based policy analysis? The strange case of the randomized controlled trials of community-led total sanitation. Oxf Rev Econ Policy. 2020;36: 191–221. [Google Scholar]
- 80.Biran A, Schmidt WP, Varadharajan KS, Rajaraman D, Kumar R, Greenland K, et al. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): a cluster-randomised trial. Lancet Glob Health. 2014;2: e145–54. doi: 10.1016/S2214-109X(13)70160-8 [DOI] [PubMed] [Google Scholar]
- 81.Contzen N, Meili IH, Mosler H-J. Changing handwashing behaviour in southern Ethiopia: A longitudinal study on infrastructural and commitment interventions. Soc Sci Med. 2015;124: 103–114. doi: 10.1016/j.socscimed.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 82.Friedrich MND, Kappler A, Mosler H-J. Enhancing handwashing frequency and technique of primary caregivers in Harare, Zimbabwe: A cluster-randomized controlled trial using behavioral and microbial outcomes. Soc Sci Med. 2018;196: 66–76. doi: 10.1016/j.socscimed.2017.10.025 [DOI] [PubMed] [Google Scholar]
- 83.Huber AC, Tobias R, Mosler H-J. Evidence-Based Tailoring of Behavior-Change Campaigns: Increasing Fluoride-Free Water Consumption in Rural Ethiopia with Persuasion: Tailoring of Behavior-Change Campaigns. Appl Psychol Health Well-Being. 2014;6: 96–118. doi: 10.1111/aphw.12018 [DOI] [PubMed] [Google Scholar]
- 84.Inauen J, Mosler H-J. Developing and testing theory-based and evidence-based interventions to promote switching to arsenic-safe wells in Bangladesh. J Health Psychol. 2014;19: 1483–1498. doi: 10.1177/1359105313493811 [DOI] [PubMed] [Google Scholar]
- 85.Kraemer SM, Mosler H-J. Effectiveness and Effects of Promotion Strategies for Behaviour Change: Solar Water Disinfection in Zimbabwe: PROMOTION OF BEHAVIOUR CHANGE. Appl Psychol. 2012;61: 392–414. doi: 10.1111/j.1464-0597.2011.00475.x [DOI] [Google Scholar]
- 86.Lilje J, Mosler H-J. Effects of a behavior change campaign on household drinking water disinfection in the Lake Chad basin using the RANAS approach. Sci Total Environ. 2018;619–620: 1599–1607. doi: 10.1016/j.scitotenv.2017.10.142 [DOI] [PubMed] [Google Scholar]
- 87.Tumwebaze IK, Mosler H-J. Effectiveness of group discussions and commitment in improving cleaning behaviour of shared sanitation users in Kampala, Uganda slums. Soc Sci Med. 2015;147: 72–79. doi: 10.1016/j.socscimed.2015.10.059 [DOI] [PubMed] [Google Scholar]
- 88.Abbink J. Dam controversies: contested governance and developmental discourse on the Ethiopian Omo River dam: DAM CONTROVERSIES, ETHIOPIA. Soc Anthropol. 2012;20: 125–144. doi: 10.1111/j.1469-8676.2012.00196.x [DOI] [Google Scholar]
- 89.Adem TA. The Local Politics of Ethiopia’s Green Revolution in South Wollo. Afr Stud Rev. 2012;55: 81–102. doi: 10.1017/S0002020600007216 [DOI] [Google Scholar]
- 90.Maes K, Closser S, Vorel E, Tesfaye Y. A Women’s Development Army: Narratives of Community Health Worker Investment and Empowerment in Rural Ethiopia. Stud Comp Int Dev. 2015;50: 455–478. doi: 10.1007/s12116-015-9197-z [DOI] [Google Scholar]
- 91.Pederson A, Greaves L, Poole N. Gender-transformative health promotion for women: a framework for action. Health Promot Int. 2015;30: 140–150. doi: 10.1093/heapro/dau083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Evans DK, Jakiela P, Knauer HA. The impact of early childhood interventions on mothers. Science. 2021;372: 794–796. doi: 10.1126/science.abg0132 [DOI] [PubMed] [Google Scholar]
- 93.Caruso BA, Sinharoy SS. Gender data gaps represent missed opportunities in WASH. Lancet Glob Health. 2019;7: e1617. doi: 10.1016/S2214-109X(19)30449-8 [DOI] [PubMed] [Google Scholar]
- 94.Amebelu A, Ban R, Bhagwan J, Brown J, Chilengi R, Chandler C, et al. The Lancet Commission on water, sanitation and hygiene, and health. The Lancet. 2021;0. doi: 10.1016/S0140-6736(21)02005-5 [DOI] [PubMed] [Google Scholar]
- 95.Haque SS, Freeman MC. The Applications of Implementation Science in Water, Sanitation, and Hygiene (WASH) Research and Practice. Environ Health Perspect. 2021;129: 065002. doi: 10.1289/EHP7762 [DOI] [PMC free article] [PubMed] [Google Scholar]