Abstract
Background:
Delirium is a common complication of hospitalization and is associated with poor outcomes. Multicomponent delirium prevention strategies such as the Hospital Elder Life Program (HELP) have proven effective, but rely on face-to-face intervention protocols and volunteer staff, which was not possible due to restrictions during the COVID-19 pandemic. We developed the Modified and Extended Hospital Elder Life Program (HELP-ME), an innovative adaptation of HELP for remote and/or physically distanced application.
Methods:
HELP-ME protocols were adapted from well-established multicomponent delirium prevention strategies and was implemented at 4 expert HELP sites. Each site contributed to the protocol modifications and compilation of a HELP-ME Operations Manual with standardized protocols and training instructions during 3 expert panel working groups. Implementation was overseen and monitored during 7 learning sessions plus 4 coaching sessions from January 8, 2021 through September 24, 2021. Feasibility of implementing HELP-ME was measured by protocol adherence rates. Focus groups were conducted to evaluate acceptability, provide feedback, and identify facilitators and barriers to implementation.
Results:
A total of 106 patients were enrolled across 4 sites, and data were collected for 214 patient-days. Overall adherence was 82% (1473 completed protocols/1798 patient-days) achieving our feasibility target of >75% overall adherence. Individual adherence rates ranged from 55% to 96% across sites for the individual protocols. Protocols with high adherence rates include the nursing delirium protocol (96%), nursing medication review (96%), vision (89%), hearing (87%), and orientation (88%), whereas the lower adherence occurred with fluid repletion (64%) and range-of-motion exercises (55%). Focus group feedback was generally positive for acceptability, with recommendations that an optimal approach would be hybrid, balancing in-person and remote interventions for potency and long-term sustainability.
Conclusions:
HELP-ME was fully implemented at 4 HELP sites, demonstrating feasibility and acceptability. Testing hybrid approaches and evaluating effectiveness is recommended for future work.
Keywords: delirium, delirium prevention, multicomponent, COVID-19
Overview
Delirium is a common complication of hospitalization for older adults, characterized by an acute change in attention and cognition, and associated with serious complications, including increased rates of morbidity, institutionalization, and mortality.1 More than 2.6 million adults 65 years and older develop delirium each year, with associated healthcare costs attributable to delirium estimated at more than $164 billion per year in the United States.2 However, numerous studies have shown at least 40% of cases may be preventable using multicomponent delirium prevention strategies.3–5
The Hospital Elder Life Program (HELP) is the original delirium prevention model, published in 1999 with primary goals of: (1) maintaining physical and cognitive functioning throughout hospitalization; (2) maximizing independence at discharge; (3) promoting the transition from hospital to home; and (4) preventing unplanned readmission.6 These goals are accomplished by an interdisciplinary team of hospital staff and trained volunteers who administer targeted intervention protocols: a Daily Visitor Program, Therapeutic Activities, Early Mobilization, Sleep Enhancement, and Feeding Assistance. Providing assistance and activities to older patients helps keep them physically and mentally active, and maximizes independence at discharge. HELP is currently implemented in more than 250 hospitals worldwide. The efficacy of HELP for delirium prevention has been well-demonstrated in over 20 trials to date.4, 7 HELP has also demonstrated efficacy for decreasing hospital falls,4 cognitive and functional decline,7, 8 length of stay,9, 10 use of sitters,11 institutionalization,11 and readmissions.12, 13 Meta-analyses have demonstrated significant reductions in delirium incidence across 14 clinical trials (odds ratio [OR], 0.47; 95% CI, 0.37–0.59), while the rate of falls was reduced by 42% among intervention patients in three clinical trials. Cost-savings attributable to HELP are estimated at $1600–3800 (2018 US dollars) per patient for hospital costs, and over $16,000 (2018 US dollars) per person-year for long-term care costs in the year following an episode of delirium across 9 studies.7
Adaptations to the original HELP program have proved successful. For example, the Tailored, Family-Involved Hospital Elder Life Program (t-HELP) includes modifications to involve family members in place of volunteers in accordance with cultural norms. Implementing t-HELP resulted in a reduction in the incidence of post-operative delirium, with a relative risk (RR) of 0.14 (95% CI, 0.05–0.38), maintenance or improvement in physical and cognitive function, and a reduction of hospital length of stay by 4 days.14 Modified HELP (mHELP), which implemented a bundle of 3 HELP interventions by bedside surgical nurses, reduced the odds of delirium by 56% and length of stay by 2 days.15 Multiple other delirium prevention models have incorporated HELP interventions and demonstrated effectiveness across other settings, including home health care (Bundled HELP and HELP in Home Care),16 long-term care (HELP-LTC),17, 18 acute rehabilitation,19 and low-resource settings.20 In 2019, HELP transitioned to the American Geriatrics Society as AGS CoCare®: HELP.
Model Description: Modified and Extended Hospital Elder Life Program (HELP-ME)
Within the COVID-19 pandemic, delirium became epidemic, with prevalence rates >25–65% reported in multiple studies21–23, and the need for HELP and multicomponent prevention strategies assumed even greater importance. However, many HELP programs had their staff redeployed, and volunteers, a key component of many programs, were not allowed in many hospitals. Thus, despite the heightened need during a surge in delirium, the effective approaches of HELP became all but impossible. COVID-19 restrictions left patients isolated and essentially precluded contact with HELP staff, volunteers, and family. Many HELP sites had to suspend operations or limit interventions. In this context, we urgently needed to adapt. This approach extends the reach of HELP, creating a broader and more flexible program applicable even after the pandemic, whenever in-person contact may be restricted or staffing limited. The specific aims of this project were: (1) to design and standardize new intervention approaches to accomplish HELP-ME with remote and/or physically distanced application; and (2) to pilot-test the HELP-ME protocols for feasibility (i.e., achieving ≥75% overall adherence across all protocols) and acceptability to patients and staff in 100 hospitalized patients across 4 sites.
METHODS
The HELP-ME study occurred from January 8, 2021 through September 24, 2021 with implementation and data collection across the sites from March 26, 2021 through August 3, 2021. This project was conducted under a waiver of informed consent from the Institutional Review Board of Hebrew SeniorLife, the study coordinating center, and each study site as required, since the project was considered a quality improvement project for an existing program and all data collection involved completely deidentified data.
Developing the HELP-ME program
Expert working group.
Adaptation of key HELP interventions for remote and/or physically distanced approaches resulted from an expert working group which included geriatricians (SKI, WZ, LW), a neurologist (TGF), advanced practice and acute care nurses (MB, SC, AK, NP, SJ), and Elder Life specialists (AM, MA) from the coordinating center at Hebrew SeniorLife, Boston, MA and 4 experienced AGS CoCare®: HELP sites. These sites were selected based on their expertise and included 3 HELP Centers of Excellence and one experienced recognized HELP site: Allegheny Health Network (Pittsburgh, PA), California Pacific Medical Center (San Francisco, CA), Maine Medical Center (Portland, ME), and University of Utah Health (Salt Lake City, UT). Specific details on each site are listed in Supplementary Table S1. The expert working group met three times to select and adapt the HELP protocols and reached consensus using a Delphi approach.24 The criteria for selection of preferred approaches included the anticipated potency of the intervention, acceptability to patients, and ease/feasibility of implementation. The expert working group also recommended the frequency (# times/day) and duration (# minutes) for each adapted intervention. Each of the 4 HELP sites were responsible for the initial development of protocol adaptations for 1–2 interventions. Consensus agreement was reached for the final remote and/or physically distanced standardized protocols (Table 1). These standardized protocols were incorporated into a HELP-ME Operations Manual revised and approved by each site prior to training. Next, all 4 sites underwent virtual training sessions to review all adaptations to the interventions, discuss any issues with screening/enrollment for the pilot, and clarify any procedural issues.
Table 1.
Standardized HELP-ME Intervention Protocols
| Intervention | Intervention Assignment Criteria | Description of HELP-ME Intervention (Remote and/or physically distanced) |
|---|---|---|
| Orientation/Daily Visitor |
|
|
| Therapeutic Activities |
|
|
| Early Mobilization |
|
|
| Sleep Enhancement |
|
|
| Feeding Assistance |
|
|
| Fluid Repletion |
|
|
| Vision Protocol |
|
|
| Hearing Protocol |
|
|
SPMSQ = Short Portable Mental Status Questionnaire
Site Preparation and Training
Sites were responsible for setting up touchscreen tablets and remote procedures, training staff including all HELP personnel (i.e. Elder Life Specialists (ELS), Elder Life Nurse Specialist (ELNS), Geriatric physician (GP), and volunteers) and planning educational sessions for floor nurses during their preparation for HELP-ME implementation. Staffing and training with the new HELP-ME standardized protocols were verified by the coordinating center. The specific number of individuals trained varied according to the discretion of the site leaders.
The intention of HELP-ME was to be as remote-based as possible, which is uniquely distinct from standard HELP. Initiating the remote connection with the patient was done by a trained HELP-ME staff member or floor nurse who could enter the patient’s room and set up the tablet. Thereafter, the program was conducted remotely via the tablets by HELP-ME staff or at some sites, by trained volunteers who were located off-site (as all hospitals were closed to volunteers and family visits during the study period).
A HELP Resource Box (“HELP Gift Box”)25 was developed and adapted by each site to provide needed supplies and equipment for intervention protocols and provided to each enrolled patient. These boxes included items such as notecards with patient instructions on the following protocols: hydration, nutrition, mobility, sleep, and orientation, and materials for various activities/exercises (https://help.agscocare.org/table-of-contents/delirium-prevention-toolkit-amidst-covid-19/H00107). For example, an “Orientation Card” was updated daily and provided the date, day of week, daily schedule, times of meals, and names of the physician, nurse, aide, and HELP staff. A notecard on “What Should I Know About Sleep?” provided information on the use of the non-pharmacological sleep protocol instead of sleeping medications. Other notecards provided instructions for relaxation exercises, active range of motion (AROM) exercises, safe walking, and stress ball and/or exercise band use. Other materials in the HELP Gift Box (customizable for the needs of the patient) included word searches and crossword puzzles, adaptive equipment (e.g., magnifying glass, flashlight, amplifier), exercise bands, stress ball for squeezing, pencil/pen, notepad, ear plugs, eye mask, and herbal tea.
Implementation and Feasibility Testing
Study population.
For the HELP-ME implementation and pilot testing, a target enrollment of 25 participants per site (100 total for the study) was selected from among patients who met eligibility criteria for enrollment into standard HELP. Eligibility criteria were previously developed to target patients at moderate to high risk for delirium, and able to participate in interventions.8 Inclusion criteria are: age 70 and older; able to communicate verbally or in writing; at least one of the following risk factors for delirium: cognitive impairment; any impairment in activities of daily living; vision or hearing impairment; or BUN/Cr ratio>18. Patients were excluded for conditions that precluded interventions, including: coma; mechanical ventilation; aphasia; imminently terminal condition; severe psychotic disorder or severe dementia. The Confusion Assessment Method (CAM),26 and the Ultra-Brief CAM (UB-CAM)27, 28 was used to screen for delirium.
Feasibility testing.
Sites were expected to apply protocols and procedures in standardized fashion with enrolled patients, remotely using touchscreen tablets and/or physically distanced. The tablets were also used by patients to communicate with family members, by staff to communicate with floor nurses to assess the patient (e.g., mental status changes, mobility/walking at baseline, nutrition and fluid needs, sleep) for assigning protocols, and for recording adherence with interventions. Implementation was overseen and monitored during 7 learning sessions and 4 coaching calls, described further below. The 4 HELP sites were encouraged to utilize data collection to identify effective strategies and barriers to address for protocol implementation, and from this to further refine the protocol for feasibility at their site (Figure 1).
Figure 1.
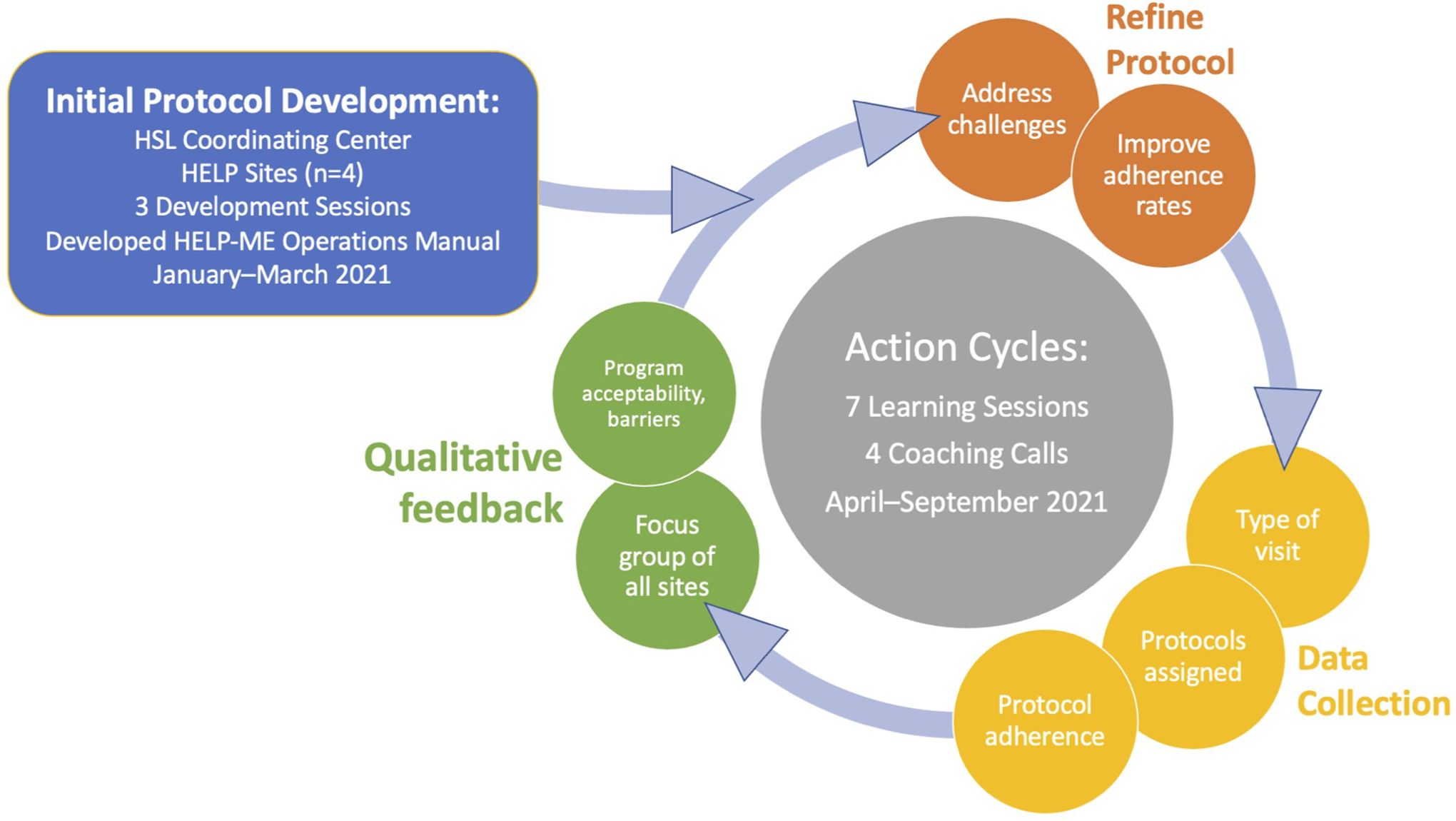
Overview of HELP-ME Process. The Initial Protocol Development Group was created with 4 AGS CoCare®: HELP sites and the coordinating center (blue rectangle). The action cycles (gray circle) were centered around 11 webinars, which included 7 learning sessions and 4 coaching calls. Sites were assigned to modify 1–2 HELP protocols during the first action cycle and further refine the protocols in subsequent cycles based on data collected and feedback received from patients and family.
HELP-ME Learning Sessions and Coaching Calls
Over the course of the implementation, from April through September 2021, 7 monthly meetings (learning sessions) were held by videoconference to enhance peer learning and support, obtain feedback on the process, discuss need for further adaptation of protocols or procedures, monitor enrollment status by site, address implementation challenges encountered, and share successes. For example, the AROM intervention was particularly challenging to implement, with low adherence rates initially. After feedback from the sites and following a coaching call with an expert, the sites were able to achieve substantially improved adherence. In addition to the learning sessions, 4 coaching calls were held to provide specialized didactic training and support. These were attended by all sites and featured expert guest speakers on topics including family involvement in remote interventions, communicating with hearing impaired patients, enhancing mobility, and implementing active range of motion exercises. All learning sessions and coaching calls were attended on average by 2–4 persons from each the sites plus the coordinating center.
Data Collection
During the enrollment and data collection phase, each of the HELP-ME sites entered deidentified data daily directly into a secure REDCap database for each enrolled patient. Data entered included the type of visit (initial or follow-up), the specific protocols assigned on that date, and whether the protocol was completed in full, partially, or not at all (see full definitions below). The dedicated HELP staff were allowed to conduct interventions interchangeably in many cases. This allowed for customization and adaptation at the individual site according to the needs of the patient. Each of the 11 protocols could be assigned to a patient 1, 2 or 3+ times per day, or not at all, depending on the clinical situation. For example, the orientation protocol would be assigned 3 times per day for patients with cognitive impairment, whereas patients ordered to be on bed rest would not be assigned the walking protocol. If a protocol was assigned but not completed, all reasons were selected from a checklist and annotated with free text details. All sites were encouraged to provide as much detail as possible. Adherence was achieved if the patient completed all parts of the assigned protocol for the total number of times it was to be given that day. Non-adherence occurred if the protocol was partially completed or not completed at all. Partial completion occurred if the patient received some but not all parts of the protocol on at least one occasion, or if they did not receive the protocol for the required number of times that day. If the assigned protocol was not executed that day at any time, the protocol was marked as not completed. An adherence rate was then calculated for each protocol by patient-day by taking the total number of complete adherence occurrences divided by the total number of days during which the protocol was assigned to be administered.
Upon completion of enrollment, all HELP-ME team members at each site completed an overall evaluation of HELP-ME via REDCap with free-text descriptions of barriers and challenges encountered, potential solutions, and recommendations for improving protocol adherence. Focus group sessions were held to provide feedback and assessment of HELP-ME efficacy, and to assess barriers to future implementation.
RESULTS
Enrollment
Enrollment was 106 patients across all sites, with a total of 214 patient-days. An average of 7.6 (±2.6) unique protocols were assigned per day across all sites (Table 2).
Table 2.
Enrollment
| Enrollment by Site | Allegheny Health Network (Pittsburgh, PA) |
California Pacific Medical Center (San Francisco, CA) |
Maine Medical Center (Portland, ME) |
University of Utah Health (Salt Lake City, UT) |
TOTAL |
|---|---|---|---|---|---|
| Patients | 25 | 26 | 30 | 25 | 106 |
| Patient-Days | 49 | 52 | 53 | 60 | 214 |
| Average # of protocols assigned/day | 7.6 ± 2.4 | 7.2 ± 1.1 | 8.1 ± 4.3 | 7.6 ± 1.7 | 7.6 ± 2.6 |
“Protocols assigned/day” was calculated by counting the number of unique protocols administered at least one time/day, reported as mean ± standard deviation. Note that protocols could be assigned multiple times in one day, but the protocol was only counted once.
Evaluation of feasibility of implementation
For this evaluation, our outcomes to be measured were program implementation and intervention adherence rates. Implementation was defined as successful execution of the full HELP-ME procedures and protocols as outlined in the HELP-ME Operations Manual across each of the sites. Overall, this was achieved with full uptake across all 4 sites (100% uptake). We had set an a priori target of ≥75% overall adherence across all protocols to demonstrate feasibility. An overall adherence rate of 82% (1,473 completed protocols/1,798 patient-days) was successfully achieved. Individual adherence rates for each of the 11 intervention protocols ranged from 55% to 96% across sites. Protocols with high adherence rates include the nursing delirium protocol (96%), nursing medication review (96%), vision (89%), hearing (87%), and orientation (88%), whereas the lowest adherence was seen for fluid repletion (64%) and AROM exercises (55%) (Table 3).
Table 3.
Adherence rates for HELP-ME protocols
| Protocol | Assigned | Completion | Adherence | ||
|---|---|---|---|---|---|
| Completed | Partially Completed | Not Completed | |||
| Orientation | 212 | 186 | 11 | 15 | 88% |
| Therapeutic | 211 | 163 | 34 | 14 | 77% |
| Sleep | 162 | 132 | 3 | 27 | 81% |
| Walking | 129 | 101 | 11 | 17 | 78% |
| AROM | 160 | 88 | 53 | 19 | 55% |
| Vision | 177 | 158 | 1 | 18 | 89% |
| Hearing | 112 | 97 | 0 | 15 | 87% |
| Feeding | 91 | 64 | 11 | 16 | 70% |
| Fluid | 123 | 79 | 28 | 16 | 64% |
| Nursing Delirium | 212 | 204 | 2 | 6 | 96% |
| Nursing Med Review | 209 | 201 | 2 | 6 | 96% |
| OVERALL | 1,798 | 1,473 | 156 | 169 | 82% |
Adherence was calculated for each protocol by taking the number of times the protocol was completed and dividing by the total number of times which the protocol was assigned to be administered. Partially completed and not completed are counted as non-adherence.
Reasons for Non-Adherence
Common reasons for overall non-adherence across all protocols included patient refusal (23%), severe medical symptoms or illness precluding participation (14%), patient unavailability due to a medical-related procedure or treatment (11%), lack of HELP staff (9%), lack of available volunteers (8%), patient discharge (6%), or inability to reach patient virtually (5%). However, the individual protocols varied in their leading reasons for non-adherence, for example, patient unavailability due to a medical-related procedure or treatment was the most common documented reason for non-adherence with therapeutic activities, whereas patient refusal was the most common reason for non-adherence with AROM exercises (Table 4).
Table 4.
Reasons for protocol non-adherence (N=325 protocols per patient-day)*
| Reasons for Non-Adherence | Protocol N (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Orientation | Therapeutic | Sleep | Walking | AROM | Vision | Hearing | Feeding | Fluid | Nursing Delirium | Nursing Med Review | OVERALL | |
| Pt refusal | 5 (1.2) | 9 (2.1) | 11 (2.6) | 10 (2.4) | 32 (7.5) | 5 (1.2) | 5 (1.2) | 8 (1.9) | 7 (1.7) | 2 (0.5) | 2 (0.5) | 96 (22.6) |
| Medical symptoms or illness | 3 (0.7) | 5 (1.2) | 4 (0.9) | 8 (1.9) | 17 (4.0) | 3 (0.7) | 3 (0.7) | 6 (1.4) | 7 (1.7) | 1 (0.2) | 1 (0.2) | 58 (13.7) |
| Medical procedure | 4 (0.9) | 10 (2.4) | 4 (0.9) | 7 (1.7) | 9 (2.1) | 1 (0.2) | 1 (0.2) | 4 (0.9) | 5 (1.2) | 1 (0.2) | 1 (0.2) | 47 (11.1) |
| Lack of HELP staff | 4 (0.9) | 6 (1.4) | 3 (0.7) | 1 (0.2) | 6 (1.4) | 2 (0.5) | 2 (0.5) | 4 (0.9) | 3 (0.7) | 3 (0.7) | 3 (0.7) | 37 (8.7) |
| Lack of volunteers | 4 (0.9) | 5 (1.2) | 3 (0.7) | 1 (0.2) | 7 (1.7) | 1 (0.2) | 1 (0.2) | 3 (0.7) | 9 (2.1) | 1 (0.2) | 1 (0.2) | 36 (8.5) |
| Pt discharge | 2 (0.5) | 3 (0.7) | 2 (0.5) | 3 (0.7) | 4 (0.9) | 2 (0.5) | 2 (0.5) | 2 (0.5) | 3 (0.7) | 1 (0.2) | 1 (0.2) | 25 (5.9) |
| Unable to contact Pt virtually† | 3 (0.7) | 6 (1.4) | 4 (0.9) | 0 (0.0) | 5 (1.2) | 0 (0.0) | 0 (0.0) | 1 (0.2) | 2 (0.5) | 0 (0.0) | 0 (0.0) | 21 (5.0) |
| Technology unavailable | 0 (0.0) | 1 (0.2) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 1 (0.2) | 0 (0.0) | 0 (0.0) | 4 (0.9) |
| Other** | 7 (1.7) | 15 (3.5) | 12 (2.8) | 3 (0.7) | 21 (5.0) | 7 (1.7) | 4 (0.9) | 9 (2.1) | 20 (4.7) | 1 (0.2) | 1 (0.2) | 100 (23.6) |
| OVERALL | 32 (7.5) | 60 (14.2) | 44 (10.4) | 33 (7.8) | 101 (23.8) | 22 (5.2) | 18 (4.2) | 37 (8.7) | 57 (13.4) | 10 (2.4) | 10 (2.4) | 424 (100) |
Pt = patient; AROM = active range of motion exercises
Multiple reasons for non-adherence were counted for each protocol per patient-day. Adherence was achieved if the patient completed all parts of the assigned protocol for the total number of times the protocol was assigned. Non-adherence occurred if the patient did not complete all parts of the protocol (partially completed), or if the protocol was assigned but not completed at all. Sites reported one or more reasons for each occurrence of non-adherence. For the 325 protocols per patient-day that did not meet adherence, a total of 424 reasons for non-adherence were documented by the sites.
In some cases, this was because staff were not available to assist the patient to use virtual technology. However, with training and support, most older adults were able to utilize the touchscreen tablets provided.
e.g., patient unavailable for nonmedical reason; provider entered room to speak with patient; patient had visitors; other reason; or undocumented reason for non-adherence.
Acceptability
Overall, we achieved full implementation and high adherence across all 4 sites. Qualitative feedback from sites during the focus group was largely positive, and supported the overall acceptability of the HELP-ME strategy. For example, all sites reported that participating in HELP-ME revitalized their overall HELP program, because it helped them recognize that it was still possible to implement intervention protocols even during COVID-19. HELP-ME also contributed to the education of hospital nursing staff regarding the importance of delirium prevention especially during COVID-19 more broadly, and helped to support nursing staff throughout a difficult time. Importantly, HELP-ME allowed for additional interaction that would not have otherwise been possible during the pandemic. Patients enrolled in HELP-ME had contact with HELP staff, volunteers, and family members remotely and/or physically distanced. Those who were able to use a HELP-ME touchscreen tablet were able to interact with family in a variety of ways, such as participating in HELP-ME therapeutic activities, listening to music, watch streaming videos, and other activities. With visitor restrictions in place, many of the HELP staff found that patients enjoyed talking on the phone or video-calling, and that connecting with patients with families can be meaningful in all forms. HELP staff also noted that from an efficiency standpoint, when a staff member or volunteer was available to do either virtual or phone interventions, they were able to conduct interventions with more patients per day than with in-person visits, because of time saved by not needing to walk from room to room or unit to unit. HELP-ME was reported to be particularly beneficial to provide HELP interventions when the program did not have available volunteers and/or staff had been deployed to other positions.
Dissemination to other sites
As part of this initiative, we developed the HELP COVID-19 Resource Toolkit which is available free of charge from the American Geriatrics CoCare HELP website at https://help.agscocare.org/productAbstract/H00107.25 This resource has already been disseminated broadly, with >300 unique users who accessed the toolkit from May 2020 to June 2022.
Discussion
HELP-ME is an innovative approach modifying a well-established and highly successful delirium prevention program for use during the COVID-19 pandemic when in-person and face-to-face interaction was limited or restricted. HELP-ME was fully implemented (100% uptake of protocols and procedures) at 4 sites, with enrollment of 106 patients with 214 patient-days of intervention. Overall adherence rate across all sites on 11 protocols was 82% (1473/1798 patient-days), which exceeded our target of 75% overall adherence indicating success of this feasibility pilot. Out of 11 individual protocols, 8 achieved adherence rates above 75%. The 3 protocols that did not achieve 75% were AROM exercises, feeding assistance, and fluid repletion. All sites agreed that a physically distanced and/or remote model is feasible and generally acceptable to staff and patients.
A major strength of HELP-ME was that it could be readily implemented during the pandemic. Some hospitals already had equipment on hand (e.g., touchscreen tablets) and others were provided by the pilot study. Many of the adaptations were straightforward to implement. Finding a way to continue HELP during the pandemic maintained accessibility to HELP interventions, further allowing for new connections to be made and strengthening existing relationships with nursing, physical and occupational therapy in delirium prevention.
Several caveats about HELP-ME are important to mention. Concerns were raised by the teams that remote interventions may not be potent enough for effective delirium prevention, that is, the “dose” of a remote intervention may not be as effective as an in-person intervention. Secondly, while open discussion at learning and coaching sessions along with careful recording of nonadherence with detailed reasons lends confidence to the results, we acknowledge the fact that the interventionists recorded adherence results may have introduced bias towards higher adherence rates. Third, while many aspects of HELP could be adapted to be physically distanced and/or remote, it was not possible to fully substitute for face-to-face human contact across all HELP protocols, such as feeding, where the intervention includes physically assisting patients, or walking, in a patient with safety concerns. Fourth, while we were often able to implement remote interventions with adequate training, support, and encouragement, we acknowledge that patients with cognitive and sensory impairments may not be able to participate in a fully remote program. Next, another significant challenge is that HELP-ME is a “high-tech, low-touch” approach, in contrast to the “low-tech, high-touch” spirit of HELP. Many older adults strongly prefer in-person or face-to-face interventions, and we found some will refuse physically distanced and/or remote interventions. Some older adults had difficulty utilizing remote equipment, such as touchscreen tablets, for multiple reasons, including sensory, cognitive, or motor impairments, or simply a lack of familiarity, although we could often address this with training, support, and encouragement. Lastly, as a feasibility study, we did not measure delirium rates or other clinical outcomes, but this is planned for future effectiveness studies.
The availability of HELP-ME remote interventions carries important implications, with wider applicability and adaptability across settings, such as for patients on droplet precautions or other isolation (e.g., COVID-19, tuberculosis, etc.), rural or underserved hospitals, or areas without availability of geriatric-trained staff. Moreover, such strategies may work well to provide delirium prevention and care in settings outside the hospital (e.g., home or extended care facilities), during staffing shortages, or in future emergency situations (e.g., natural disasters, climate crises, or other pandemics) where physical access or contact may be limited.
Maintaining HELP accessibility in circumstances where traditional HELP is not feasible is crucial to preventing complications of delirium. Considering the limitations of HELP-ME, the expert sites therefore recommended a hybrid approach, including both HELP-ME physically distanced and/or remote protocols along with in-person protocols, customized and individualized to the patients, was likely to be most effective long-term with highest rates of adherence. This would allow for both in-person interventions wherever possible, with remote interventions for patients on isolation or where staffing may be inadequate. Incorporating brief delirium screening tools, such as the Ultra-Brief CAM,29, 30 that can be done remotely to measure delirium rates might be another feasible approach for future studies evaluating the effectiveness of HELP-ME.
In summary, HELP-ME is feasible to implement and generally acceptable to staff and patients. However, not all protocols can be fully adapted and the potency will need to be evaluated in future studies. A future randomized trial will be needed to test effectiveness. If proven effective, these strategies will create a more broadly applicable program, allowing flexible incorporation of both in-person and physically distanced and/or remote strategies.
Supplementary Material
Supplementary Table S1. HELP-ME Sites
Overview of HELP-ME Sites. These sites were selected based on their expertise with HELP and include 3 HELP Centers of Excellence and 1 experienced recognized HELP site.
KEY POINTS.
Delirium is a common complication of hospitalization for older adults and is associated with poor outcomes such as increased mortality, institutionalization, and cognitive decline.
Multicomponent delirium prevention strategies have proven effective, but many rely on an interdisciplinary team of hospital staff and trained volunteers to administer face-to-face intervention protocols.
Motivated by the COVID-19 pandemic, we adapted the original Hospital Elder Life Program (HELP) multicomponent delirium prevention protocols by adding innovative modifications for remote and/or physically distanced application, resulting in the Modified and Extended Hospital Elder Life Program (HELP-ME), which was fully implemented at 4 HELP sites, demonstrating feasibility and acceptability.
WHY DOES THIS MATTER?
HELP-ME has the potential to broaden the reach of already established multicomponent delirium prevention models to aid in improving the care of older adults.
Acknowledgments:
This study is dedicated to the memory of Joshua Bryan Inouye Helfand. The authors wish to thank other HELP-ME contributors: Swarna Arora MA, Rhonda L. Babine MS, APRN, Miriam G. Beattie DNP, Elisha M. Boatman BSN, Emily L. Carter MD, Autumn Moss-Corcoran MA, MaryBeth Duffy BSN, Alijana Kahriman MS, Anu Kirupananthan NP, Kaitlyn R. Lorey BSW, Morgan Mihok MD, Natalie Peraza MSN, APRN, Christin J. Scott MPH. Finally, we wish to thank the patients, families, and physicians who participated in the HELP-ME study across all study sites.
Grant Funding:
This study was funded in part by a pilot grant from the Interventional Studies in Aging Center at Hebrew SeniorLife, and by Grant No. R33AG071744 from the National Institute on Aging. Dr. Inouye holds the Milton and Shirley F. Levy Family Chair at Hebrew SeniorLife/Harvard Medical School.
Funding:
Interventional Studies in Aging Center pilot program (internal Marcus Institute for Aging Research grant), and Grant no. R33AG071744 (SKI) from the National Institute on Aging.
Sponsor’s Role:
The funding sources had no role in the design, conduct, or reporting of this study. This article represents the views of the authors.
Footnotes
Conflict of Interest: PV is supported in part by BlueCross BlueShield of Michigan. There are no other conflicts to disclose.
References
- [1].Wilson JE, Mart MF, Cunningham C, et al. Delirium. Nat Rev Dis Primers. 2020;6: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168: 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hshieh TT, Inouye SK, Oh ES. Delirium in the Elderly. Clin Geriatr Med. 2020;36: 183–199. [DOI] [PubMed] [Google Scholar]
- [4].Hshieh TT, Yue J, Oh E, et al. Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med. 2015;175: 512–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Khan A, Boukrina O, Oh-Park M, Flanagan NA, Singh M, Oldham M. Preventing Delirium Takes a Village: Systematic Review and Meta-Analysis of Delirium Preventive Models of Care. J Hosp Med. 2019;14: E1–e7. [DOI] [PubMed] [Google Scholar]
- [6].Inouye SK, Bogardus ST Jr., Charpentier PA, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999;340: 669–676. [DOI] [PubMed] [Google Scholar]
- [7].Hshieh TT, Yang T, Gartaganis SL, Yue J, Inouye SK. Hospital Elder Life Program: Systematic Review and Meta-analysis of Effectiveness. Am J Geriatr Psychiatry. 2018;26: 1015–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Inouye SK, Bogardus ST Jr., Baker DI, Leo-Summers L, Cooney LM Jr. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. J Am Geriatr Soc. 2000;48: 1697–1706. [DOI] [PubMed] [Google Scholar]
- [9].Rubin FH, Neal K, Fenlon K, Hassan S, Inouye SK. Sustainability and scalability of the hospital elder life program at a community hospital. J Am Geriatr Soc. 2011;59: 359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Rubin FH, Williams JT, Lescisin DA, Mook WJ, Hassan S, Inouye SK. Replicating the Hospital Elder Life Program in a community hospital and demonstrating effectiveness using quality improvement methodology. J Am Geriatr Soc. 2006;54: 969–974. [DOI] [PubMed] [Google Scholar]
- [11].Caplan GA, Harper EL. Recruitment of volunteers to improve vitality in the elderly: the REVIVE study. Intern Med J. 2007;37: 95–100. [DOI] [PubMed] [Google Scholar]
- [12].Rubin FH, Bellon J, Bilderback A, Urda K, Inouye SK. Effect of the Hospital Elder Life Program on Risk of 30-Day Readmission. J Am Geriatr Soc. 2018;66: 145–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zachary W, Kirupananthan A, Cotter S, Barbara GH, Cooke RC 3rd, Sipho M. The impact of Hospital Elder Life Program interventions, on 30-day readmission Rates of older hospitalized patients. Arch Gerontol Geriatr. 2020;86: 103963. [DOI] [PubMed] [Google Scholar]
- [14].Wang YY, Yue JR, Xie DM, et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on Postoperative Delirium and Function in Older Adults: A Randomized Clinical Trial. JAMA Intern Med. 2020;180: 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chen CC, Li HC, Liang JT, et al. Effect of a Modified Hospital Elder Life Program on Delirium and Length of Hospital Stay in Patients Undergoing Abdominal Surgery: A Cluster Randomized Clinical Trial. JAMA Surg. 2017;152: 827–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Simpson M, Macias Tejada J, Driscoll A, Singh M, Klein M, Malone M. The Bundled Hospital Elder Life Program-HELP and HELP in Home Care-and Its Association With Clinical Outcomes Among Older Adults Discharged to Home Healthcare. J Am Geriatr Soc. 2019;67: 1730–1736. [DOI] [PubMed] [Google Scholar]
- [17].Boockvar KS, Judon KM, Eimicke JP, Teresi JA, Inouye SK. Hospital Elder Life Program in Long-Term Care (HELP-LTC): A Cluster Randomized Controlled Trial. J Am Geriatr Soc. 2020;68: 2329–2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Boockvar KS, Teresi JA, Inouye SK. Preliminary Data: An Adapted Hospital Elder Life Program to Prevent Delirium and Reduce Complications of Acute Illness in Long-Term Care Delivered by Certified Nursing Assistants. J Am Geriatr Soc. 2016;64: 1108–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Huson K, Stolee P, Pearce N, Bradfield C, Heckman GA. Examining the Hospital Elder Life Program in a rehabilitation setting: a pilot feasibility study. BMC Geriatr. 2016;16: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Kojaie-Bidgoli A, Sharifi F, Maghsoud F, Alizadeh-Khoei M, Jafari F, Sadeghi F. The Modified Hospital Elder Life Program (HELP) in geriatric hospitalized patients in internal wards: A double-blind randomized control trial. BMC Geriatr. 2021;21: 599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gan JM, Kho J, Akhunbay-Fudge M, et al. Atypical presentation of COVID-19 in hospitalised older adults. Ir J Med Sci. 2021;190: 469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].O’Hanlon S, Inouye SK. Delirium: a missing piece in the COVID-19 pandemic puzzle. Age Ageing. 2020;49: 497–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Ward CF, Figiel GS, McDonald WM. Altered Mental Status as a Novel Initial Clinical Presentation for COVID-19 Infection in the Elderly. Am J Geriatr Psychiatry. 2020;28: 808–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Dalkey N, Helmer O. An Experimental Application of the DELPHI Method to the Use of Experts. Management Science. 1963;9: 458–467. [Google Scholar]
- [25].Inouye SK. The Importance of Delirium and Delirium Prevention in Older Adults During Lockdowns. Jama. 2021;325: 1779–1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113: 941–948. [DOI] [PubMed] [Google Scholar]
- [27].Fick DM, Inouye SK, Guess J, et al. Preliminary development of an ultrabrief two-item bedside test for delirium. J Hosp Med. 2015;10: 645–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Fick DM, Inouye SK, McDermott C, et al. Pilot Study of a Two-Step Delirium Detection Protocol Administered By Certified Nursing Assistants, Physicians, and Registered Nurses. J Gerontol Nurs. 2018;44: 18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Husser EK, Fick DM, Boltz M, et al. Implementing a Rapid, Two-Step Delirium Screening Protocol in Acute Care: Barriers and Facilitators. J Am Geriatr Soc. 2021;69: 1349–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Motyl CM, Ngo L, Zhou W, et al. Comparative Accuracy and Efficiency of Four Delirium Screening Protocols. J Am Geriatr Soc. 2020;68: 2572–2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. HELP-ME Sites
Overview of HELP-ME Sites. These sites were selected based on their expertise with HELP and include 3 HELP Centers of Excellence and 1 experienced recognized HELP site.


