Abstract
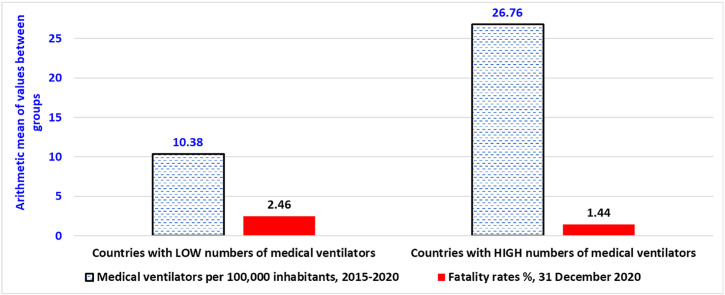
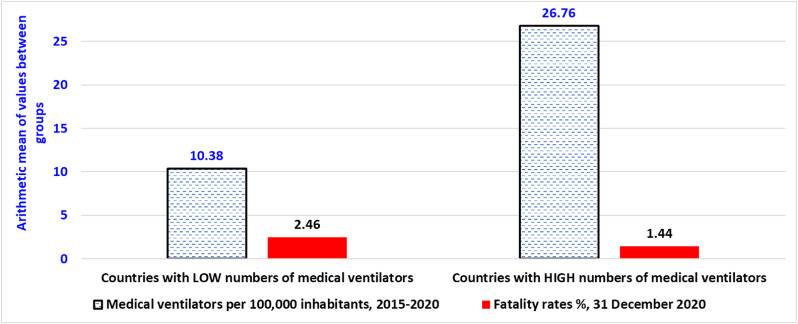
Some countries in the presence of unforeseen Coronavirus Disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), have experienced lower total deaths, though higher numbers of COVID-19 related infections. Results here suggest that one of the explanations is the critical role of ventilator technology in clinical health environment to cope with the initial stage of COVID-19 pandemic crisis. Statistical evidence shows that a large number of ventilators or breathing devices in countries (26.76 units per 100,000 inhabitants) is associated with a fatality rate of 1.44% (December 2020), whereas a higher fatality rate given by 2.46% is in nations with lower numbers of ventilator devices (10.38 average units per 100,000 people). These findings suggest that a large number of medical ventilators in clinical setting has a high potential for more efficient healthcare and improves the effective preparedness of crisis management to cope with new respiratory pandemic diseases in society. Hence, a forward-thinking and technology-oriented strategy in healthcare sector, based on investments in high-tech ventilator devices and other new medical technologies, can help clinicians deliver effective care and reduce negative effects of present and future respiratory infectious diseases, in particular when new drugs and appropriate treatments are missing in clinical environment to face unknown respiratory viral agents .
Keywords: COVID-19 pandemic, Pandemic preparedness, Public health preparedness/response, Innovation policy, Fatality rate, Breathing devices, Effective healthcare, Medical ventilators, Ventilation machines, Mechanical ventilation, Respiratory therapies, Ventilator technology innovation, Coronavirus Disease 2019, Artificial ventilation
Graphical abstract
1. Introduction
In the presence of Coronavirus Disease 2019 (COVID-19) pandemic crisis, countries have applied health policies to stop and/or reduce the transmission of the novel infection and consequently high numbers of deaths [[1], [2], [3], [4]]. However, many countries have experienced in the initial stage of the COVID-19 pandemic, although containment and/or mitigation policies, high numbers of deaths, such as Italy, Central and South American countries, etc. [2,3,[5], [6], [7], [8]]. Manifold factors affect the negative impact of COVID-19 pandemic in society, such as high air pollution and density of people in cities [9], intensive commercial trade between countries [10,11], low investments in healthcare sector, etc. [12,13], etc. COVID-19 with initial variants Alfa and Delta generated critically respiratory failure in ill patients, heterogeneous pulmonary parenchymal involvement, profound hypoxemia, pulmonary vascular injury and other negative health effects [14]. One of the treatments in the initial stage of the COVID-19 pandemic is the application, to patients with respiratory disorders, of mechanical ventilator that is based on an internal compressor and mixer to moderate and control the gas mixture delivered to ill patients. Nevertheless, a major problem was the shortage of these breathing devices [[15], [16], [17]]. Jones [18] argues that in India only 50% of intensive care units (ICUs) has a mechanical ventilator. Innovative projects were launched, during the initial phase of COVID-19 pandemic crisis in 2020, to solve this problem of the shortage of ventilators in order to improve manufacturing and flexibility in supply chain, also with strategic partnership and collaborative networks in this industry to boost R&D performance, production, storage and maintenance of ventilator devices [14,[19], [20], [21], [22], [23], [24], [25]]. A main example is product development of the PocketVent ventilator in less than six months with efficient technical characteristics of pressure and volume controlled to help patients in breathing [17]. Other scholars suggested that the use of medical gasses and flow interruption strategy can support high performance and low cost in ventilator technology [14]. This technological approach reduces many physical components present in traditional ventilators, shortens the time from storage to clinical deployment and improves reliability in terms of life-saving ventilatory support, satisfying emergency guidelines of the U.S. FDA. Planners and policymakers also realized that during COVID-19 pandemic crisis, the technical personnel to operate mechanical ventilation was another resource of shortage [15]. Jimenez-Maturano and Licona [26] maintain that the demand increase for the production of ventilation devices can create risks concerning the correct equipment's operation and effective safety to care for COVID-19 patients.
In the presence of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) and similar viral agents that cause severe respiratory illness responsible of outbreaks, a vital research question is to analyze the relation between numbers of mechanical ventilators (breathing devices) and COVID-19 fatality rates across countries because it can support effective health policy responses of crisis management to face future pandemic threats of deadly infections. In particular, the purpose of the present study is to verify whether the statistical evidence supports the hypothesis that, in the initial stage of COVID-19 pandemic crisis, lower rates of fatality in some countries can be explained by large numbers of mechanical ventilators in healthcare. Findings here can clarify the critical role of this medical technology as one of the main resources in effective health strategies of crisis management that improves preparedness and responsiveness of countries to face pandemic threats, reducing negative impact in society.
2. Theoretical framework
Mechanical ventilator is an artificial breathing device used for patients that are not able to breathe naturally because of a critical illness and/or severe acute respiratory disorders, such as respiratory failure generated by Coronavirus Disease 2019 (COVID-19) and similar infectious diseases, Chronic Obstructive Pulmonary Disease (COPD), lung cancer, etc. [27]. In particular, mechanical ventilator is applied to patients with acute or acute-on-chronic respiratory failure that do not respond to standard therapeutic interventions, such as antibiotics, bronchodilators, etc. [28,29].
Mechanical ventilators can be:
-
•
stationary devices for Intensive Care Units (ICUs)
-
•
mobile devices used to transfer patients within and between hospitals, for in-home use, etc.
-
•
Invasive devices based on endotracheal intubation
-
•
Non-Invasive Ventilation (NIV) devices with various types of face masks
Invasive devices for mechanical ventilation are based on endotracheal tube to deliver to patient's lungs the appropriate levels of oxygen and initiate lung healing from respiratory disorders [30]. However, invasive ventilation technology generates some health problems such as, ventilator-associated lung injury, alveolar overdistension that leads to inflammatory processes and fluid accumulation in lungs, ventilator-associated pneumonia (VAP), etc. [[31], [32], [33]]. Garnier et al. [34] confirm that COVID-19 patients treated with invasive mechanical ventilation are at high risk of developing VAP. In fact, VAP affected about 50% of COVID-19 patients with mechanical ventilation and had a negative impact on 90-day mortality.
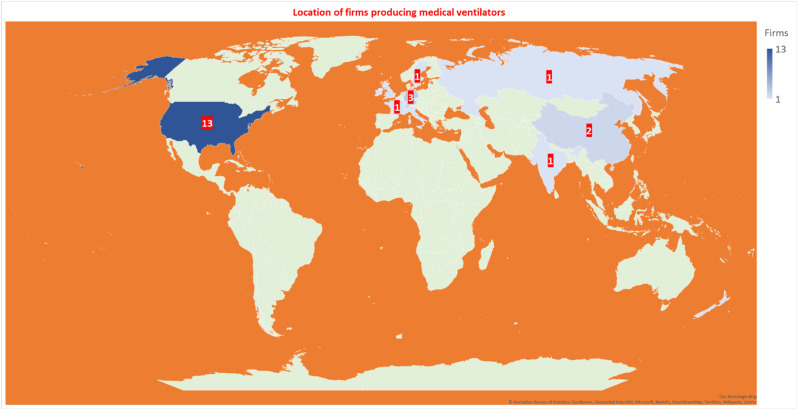
A different technology is the Non-Invasive Ventilation (NIV) that can reduce ventilator-associated lung injuries, VAP and other health problems [35,36]. The application of NIV devices (with helmet, facemask, etc.) is increasing and now this new technology care better patients having acute and/or chronic respiratory failure, in ICUs or at home [[37], [38], [39]]. Technological advances of NIV are based on respiratory abdominal sensors and transducers, and other innovations that measure with accuracy patient's airway pressure, monitor and improve breath rate, etc. [40]. In addition, new technology in NIV provides more natural breathing with an adequate humidification to maintain airway clearance and enhance patient comfort (similarly to normal functions of the nose and air passages in the human respiratory tract that are to warm, moisten and filter the inhaled gases before they reach the lungs without damaging the alveoli: tiny air sacs where the lungs and the blood exchange oxygen and carbon dioxide during the process of breathing in and breathing out) [41,42]. Weerakkody et al. [43] argue that the NIV can be superior to high-flow nasal oxygen because reduces the respiratory complications. Zhang et al. [44] find that the early adoption of NIV can improve the health of patients with severe acute respiratory syndrome (e.g., COVID-19), COPD and other respiratory disorders. Chandrasekaran and Monikandan [31] analyze the therapeutic advantages of oxygen helmet with negative pressure ventilator in patients exposed to various ventilator-induced lung injuries, such as barotrauma, VAP, etc. New technology in this industry is also directed to ventilators with flexible application for adults, children and newborns [45]. NIV and other high-tech devises for mobile mechanical ventilation, in ill patients of COVID-19 and other diseases causing respiratory disorders and/or failures, are safe, cost-effective and associated with better technical performance and comfort [43,46,47]. Table 1 and Fig. 1 show that global market of ventilator technology in medicine has leading companies mainly in the USA and Germany. The firms with the highest market share in this high-tech industry, over 2019, are: Hamilton Medical (22%), Getinge (22%), Draeger (16%), Minday (10%), Medtronic (5%), Philips (3%), Vyaire Medical (3%), Becton Dickinson, Fisher & Paykel Healthcare, GE Healthcare, and Smiths Group (cf., [48,50]; see, Table 1).
Table 1.
Top firms producing mechanical ventilators and their headquarters (city and country).
| Company | Headquarters Location | Country |
|---|---|---|
| Airon Corporation | Melbourne, Florida | USA |
| Becton Dickinson and Company | Franklin Lakes, NJ | USA |
| Bio-Med Devices, Inc. | Guilford, CT | USA |
| Bunnell Incorporated | Salt Lake City, UT | USA |
| Cardinal Health | Dublin, OH | USA |
| GE Healthcare | Chicago, IL | USA |
| Hartwell Medical Corp. | Carlsbad, CA | USA |
| Hillrom | Chicago, IL | USA |
| Vyaire Medical Inc. | Chicago, IL | USA |
| Oceanic Medical Products, Inc. | Atchison, KS | USA |
| ResMed Corp. | San Diego, CA | USA |
| United Hayek Industries, Inc. | San Diego, CA | USA |
| Ventec Life Systems | Bothell, WA | USA |
| Hamilton Medical | Bonaduz | USA/Switzerland |
| ACUTRONIC Medical Systems AG | Hirzel | Switzerland |
| Smiths Group | London | UK |
| Medtronic | Dublin | Ireland |
| Air Liquide Healthcare | Paris | France |
| Getinge AB | Göteborg | Sweden |
| aXcent medical | Koblenz | Germany |
| Drägerwerk AG | Lübeck | Germany |
| Löwenstein Medical Innovation | Kronberg | Germany |
| Dima Italia | Bologna | Italy |
| Philips | Amsterdam | The Netherlands |
| Avasarala Technologies Limited | Bengaluru | India |
| Aeonmed co., ltd. | Beijing | China |
| Mindray Medical International | Shenzen | China |
| Triton Electronics Systems, Ltd. | Yekaterinburg | Russia |
| Fisher & Paykel | Auckland | New Zealand |
Fig. 1.
Geographical distribution in countries of main firms producing mechanical ventilators.
Note: The USA has 13 firms, Germany 3, Switzerland 2, China 2, the UK 1 firm, Ireland 1, France 1, Sweden 1, Italy 1, the Netherlands 1, India 1, Russia 1 and finally New Zealand 1 firm.
Overall, then, mechanical ventilators can play a critical role to treat respiratory illnesses and to cope with negative effects of emerging viral agents that cause severe acute respiratory syndrome responsible of unforeseen pandemics, such as COVID-19, when appropriate drugs are missing. Next section presents the methodology to investigate this critical problem and verify the hypothesis stated in introduction that, in the initial stage of COVID-19 pandemic crisis, lower rates of fatality in some countries can be due to large numbers of mechanical ventilators in healthcare, suggesting that these high-tech devices can improve preparedness in crisis management to face unexpected health emergencies (e.g. pandemics of new respiratory viruses),
3. Methods
3.1. Sample
This study analyzes data of mechanical ventilators and of other variables in nine countries: Canada, France, Germany, New Zealand, Norway, South Korea, Switzerland, United Kingdom and United States [51]. This sample has all data of variables under study.
3.2. Measures for statistical analyses
-
−
Mechanical ventilators. Total number of ventilators over 2015–2020. Source: Our World in Data [51].
-
−
Wealth of nations. Gross Domestic Product (GDP) per capita in 2020, constant 2010US$. Source: The World Bank [52].
-
−
Population total. All resident people in 2020. Source: The World Bank [53].
-
−
Health expenditure as % of GDP. It includes healthcare goods and services consumed during a certain year. Average values over 2008–2018 (2018 is the last year available in dataset). The Word Bank [54].
-
−
COVID-19 Mortality. Normalized deaths per country are based on Case Fatality Ratio (CFR) % of COVID-19 [12,[55], [56], [57]]:
CFR of COVID-19 is a critical indicator to support appropriate health policies of governments to cope with pandemic crisis and similar health emergencies [58]. CFR of COVID-19 is measured as of December 31st, 2020, before the plans of vaccination between countries, to assess the effective role of mechanical ventilators to mitigate the number of deaths, when these technological devices were the only therapeutic treatment for COVID-19 patients because effective drugs to face new coronavirus were missing. CFR of COVID-19 is also considered as of February 21st, 2022, after the vaccination campaign, for a comparative analysis of long period. Source of data: Johns Hopkins Center for System Science and Engineering [59].
3.3. Data analysis procedure
-
a).Total number of mechanical ventilators is divided by total population of countries and multiplied by 100,000 to have a normalized value between countries. Average value of mechanical ventilators per 100,000 people in sample under study is fifteen units. Hence, countries are categorized simply in:
-
−Group 1: Countries with a large number of mechanical ventilators: more than 15 ventilators per 100,000 people
-
−Group 2: Countries with a small number of mechanical ventilators: lower than 15 ventilators per 100,000 people
-
−
-
b).
Arithmetic mean (M) of COVID-19 fatality rates between countries in groups 1 and 2 can suggest the effectiveness of ventilation technology to cope with deadly infections of COVID-19 in society [60].
-
c).
Parametric independent samples T-test assesses whether arithmetic means of variables between groups (1 and 2) are significantly different: i.e., if countries having average large numbers of mechanical ventilators per inhabitants, they have also lower average fatality rates of COVID-19 (cf. hypothesis in the introduction here). Finally, the control analysis is performed with the Kruskal-Wallis H-test (a rank-based nonparametric test).
4. Results and discussions
Table 2 shows that:
-
❑
Countries with large numbers of mechanical ventilators have average ventilator devices per 100,000 people over 2015–2020 (last year available) given by M (arithmetic mean) = 26.76 units (Standard Deviation, SD = 14.94 units)
-
❑
Countries with a small number of mechanical ventilators have average ventilators per 100,000 people over 2015–2020 (last year available) equal to M = 10.38 units (SD = 2.57 units)
Table 2.
Descriptive statistics.
| Description of variables | Countries with HIGH numbers of ventilators, N = 5 |
Countries with LOW numbers of ventilators, N = 4 |
||
|---|---|---|---|---|
| M | SD | M | SD | |
| Mechanical ventilators per 100,000 inhabitants, 2015–2020 | 26.76 | 14.94 | 10.38 | 2.57 |
| GDP per capita in 2020, U$ | 51,196.42 | 24,067.16 | 52,093.27 | 19,156.84 |
| Health expenditure as % of GDP, 2008–2018 | 10.950 | 3.680 | 10.960 | 0.800 |
| COVID-19 Fatality rates %, December 31st, 2020 (§) | 1.436 | 0.412 | 2.460 | 0.561 |
| COVID-19 Fatality rates %, February 21st, 2022 | 0.550 | 0.470 | 0.770 | 0.280 |
Note: M = arithmetic mean; SD=Standard Deviation; (§) this value assesses the real effect of mechanical ventilators on the health of people because it refers to a previous period the vaccination campaign between countries, when effective drugs to treat the novel coronavirus SARS-CoV-2 are missing.
Table 2 reveals a main finding: countries having high average numbers of mechanical ventilators per 100,000 people (M = 26.76 units), they have a low average fatality rate of COVID-19 (M = 1.43%) as of December 31st, 2020 compared to countries with low average numbers of mechanical ventilators (M = 10.38 units) that have a higher average fatality rate related to COVID-19 (M = 2.46%) in the same period. These results are in a homogenous socioeconomic framework because GDP per capita and average health expenditure as % of GDP in two groups of countries under study are comparable values.
Table 3 shows a significant difference of the arithmetic means of COVID-19 fatality rate % as of December 31st, 2020 between groups of countries with high and low average number of mechanical ventilators (p-value=0.05). Moreover, as of February 21st, 2022, although average COVID-19 fatality rate is lower in countries with large numbers of mechanical ventilators, the difference between groups is not significant. This result can be explained with the widespread and pervasive diffusion of vaccinations to treat COVID-19 in these countries that has generated a substitution effect with mechanical ventilators in therapeutic treatments of COVID-19 [3,61].
Table 3.
Independent Samples T-Test in countries with high vs. low numbers of mechanical ventilators per 100,000 people.
| Levene's Test for equality of variances |
T-test for equality of Means |
|||||||
|---|---|---|---|---|---|---|---|---|
| F | Sig. | t | df | Sig. 2-tailed |
Mean Difference | Std. Error Difference | ||
| Log Mechanical ventilators per 100,000 inhabitants, 2015–2020 (#) |
|
6.499 | 0.038 | −2.904 | 7 | 0.023 | −0.852 | 0.293 |
|
−3.144 | 5.959 | 0.020 | −0.852 | 0.271 | |||
| COVID-19 Fatality rates %, December 31st, 2020 (§) |
|
0.161 | 0.701 | 3.164 | 7 | 0.016 | 1.024 | 0.324 |
|
3.046 | 5.395 | 0.026 | 1.024 | 0.336 | |||
| COVID-19 Fatality rates %, February 21st, 2022 |
|
3.319 | 0.111 | 0.822 | 7 | 0.438 | 0.220 | 0.267 |
|
0.874 | 6.563 | 0.413 | 0.220 | 0.251 | |||
Note:# Log transformation is applied to have a normal distribution of this variable within two groups (§). This value assesses the real effect of mechanical ventilator devices on COVID-19 patients with acute respiratory disorders because it refers to a previous period the roll-out of vaccination campaign between countries, when alternative and effective therapeutic treatments are missing.
Kruskal-Wallis H test in Table 4 confirms a statistically significant difference of COVID-19 fatality rates as of December 31st, 2020 between groups. In particular:
-
•
there was a statistically significant difference in mechanical ventilators between groups χ2(1) = 6.00, p-value = 0.01, with a mean rank score of 2.5 for countries having LOW numbers of mechanical ventilators per 100,000 people and a mean rank score of 7 for countries having HIGH numbers of mechanical ventilators per 100,000 people.
-
•
there was a statistically significant difference in COVID-19 fatality rates as of December 31st, 2020 between groups having a high/low level of mechanical ventilators χ2(1) = 3.85, p-value = 0.05, with a mean rank score of 7 for countries with LOW numbers of mechanical ventilators per 100,000 people and a mean rank score of 3.4 for countries having HIGH numbers of mechanical ventilators per 100,000 people.
Table 4.
Kruskal-Wallis Test between countries with high vs. low numbers of mechanical ventilators per 100,000 inhabitants.
| Ranks, a) | N | Mean Rank | |
|---|---|---|---|
| Mechanical ventilators per 100,000 inhabitants, 2015–2020 | LOW number of mechanical ventilators per 100,000 people | 4 | 2.5 |
| HIGH number of mechanical ventilators per 100,000 people | 5 | 7.0 | |
| Total | 9 | ||
| COVID-19 Fatality rates %, December 31st, 2020 | LOW number of mechanical ventilators per 100,000 people | 4 | 7.0 |
| HIGH number of mechanical ventilators per 100,000 people | 5 | 3.4 | |
| Total | 9 | ||
| COVID-19 Fatality rates %, February 21st, 2022 |
LOW number of mechanical ventilators per 100,000 people | 4 | 5.75 |
| HIGH number of mechanical ventilators per 100,000 people | 5 | 4.4 | |
| Total |
9 |
||
| Mechanical ventilators per 100,000 inhabitants, 2015–2020 |
COVID-19 Fatality rates %, December 31st, 2020 |
COVID-19 Fatality rates %, February 21st, 2022 |
|
| Kruskal-Wallis Test Statistics, b) | |||
| Chi-Square χ2 | 6 | 3.84 | 0.54 |
| df | 1 | 1 | 1 |
| Asymp. Sig. | 0.014 | 0.05 | 0.462 |
Note: a) Grouping Variable; b) Kruskal Wallis Test.
As explained for Independent sample T-test, the differences of COVID-19 fatality rate between groups as of February 21st, 2022 are statistically insignificant because of vaccination plans that have provided with new vaccines an alternative therapeutic treatment to mechanical ventilator devices, because countries with low numbers of mechanical ventilators have, in general, high levels of vaccination in population that reduced fatality rate [3,[62], [63], [64]].
Fig. 2 synthetizes main findings: countries with a high average number of mechanical ventilators of about 27 units per 100,000 people, compared to countries with low numbers of mechanical ventilators of about 10 units per 100,000 people [65], have a lower average fatality rate of COVID- 19 given by 1.44% vs. 2.46%.
Fig. 2.
Comparative analysis of COVID-19 fatality rates between countries with high and low numbers of mechanical ventilators.
The ever-looming threat of the emergence of a new viral agent or the evolution of a new variant of SARS-CoV-2 that can evade new vaccines and antivirals is very real [66]. These facts suggest that mutant SARS-CoV-2 and similar respiratory viruses will continue to play a major role in society for the foreseeable future [67].
This uncertain scenario compels countries to face in future more complex social, economic, political, and clinical environments and to absorb the lessons learned from the COVID-19 responses to be prepared for minimizing negative effects of next health emergencies.
Lesson learned of crisis management to face next pandemic threat that this study adds is that statistical evidence here seems in general to support the hypothesis that a lower COVID-19 fatality rate (during the initial phase of pandemic crisis when vaccines and antivirals to treat new viral respiratory disease of COVID-19 are missing) can be explained with a large number of mechanical ventilators that has helped clinicians deliver quality and effective care to mitigate mortality in society [68]. Since the impact of next pandemic will be determined by how well-prepared countries are when health emergency occurs at any time with little warning, and how countries timely respond, these findings here suggest that a technology-oriented strategy based on high levels of R&D investments in health sector and in particular in medical technology of ventilators can support more efficient healthcare and improve the preparedness of countries to cope with pandemic crises and as a consequence to reduce negative effects of high numbers of COVID-19 related deaths in society [2]. Hence, nations have to invest in new mechanical ventilators to prepare healthcare sector to face next health emergencies, probably caused by emerging viral respiratory diseases, as well as in the presence of increasing chronic obstructive pulmonary diseases in society (associated with high air pollution in cities), of many people affected by hypertension and cardiovascular diseases, of growing geriatric population, and finally of increasing tobacco consumption worldwide leading to lung cancer [[69], [70], [71], [72], [73]].1 The mechanical ventilator market shows that the segment of non-invasive ventilators is growing at a rapid pace because this new technology has fewer side effects in ill patients (e.g., low incidence of ventilator-associated pneumonia, lung injuries, barotrauma, etc.), accelerates recovery of patients and leads to flexible applications to different age group of patients (i.e., pediatric, adult, geriatric people). In this context, Germany is an interesting case study to support empirical results here, because although high numbers of COVID-19 confirmed cases relative to population equal to 45.49% (as of February 28th, 2023), the COVID-19 fatality rate is low (0.44%) compared to other countries, such as Italy having a COVID-19 fatality rate of 0.73% at the same date [59]. One of the reasons is that Germany in 2020, when COVID-19 starts the diffusion in Europe, had about 30,000 mechanical ventilators [51] with a total population of more than 83 million [52], having so the highest number of mechanical ventilators per 100,000 people (Table 1). Leading companies of medical ventilators, headquartered in Germany, have supported a widespread diffusion of high-tech breathing devices in healthcare system that, during the initial phases of COVID-19 pandemic crisis, has minimized the pandemic impact (i.e., mortality) in society [45,74]. In fact, large numbers of mechanical ventilators can support an efficient healthcare that minimizes negative effects of pandemic disease in society, in particular when alternative treatments are missing and drug discovery process to treat unknown viral agents needs years to generate effective innovations. Hence, these findings bring us to suggest that an appropriate strategy of crisis management for respiratory deadly infections should be technology-oriented and focused on high levels of R&D investments in health sector, in skilled human resources and in a pervasive diffusion of high-tech mechanical ventilators that improve the preparedness in countries to cope with unforeseen pandemic crisis [67].
5. Conclusions and technology policy implications for next pandemic crisis
The dynamics and effects of COVID-19 pandemic in society are due to a variety of factors associated with environmental pollution, climate, public governance, institutions, healthcare system, national system of innovation, etc. [9,12,13,[75], [76], [77], [78], [79], [80], [81], [82], [83], [84]]. In the presence of pandemic crises, one of the goals of nations is to mitigate mortality and support the socioeconomic system [13]. Studies analyze different non-pharmaceutical interventions to cope with the spread of COVID-19 but these control measures generate uncertain results to mitigate negative effects given by high numbers of infections and deaths of new viral respiratory disease in society [3,64,[85], [86], [87], [88]]. The findings here suggest a technology-oriented strategy of crisis management for future pandemic threats: high levels of investments in healthcare sector, high levels of R&D investments in drug discovery process and in new technology of mechanical ventilators, etc. that support the preparedness and resilience of countries to face unknown infectious respiratory diseases and also other diseases, such as COPD, asthma, bronchitis, lung cancer, etc. [[89], [90], [91], [92]]. To put it differently, the preparedness of countries for next pandemic crises should be oriented to strengthen new technologies in health system to cope with future health emergencies, especially when effective drugs to treat patients with acute respiratory illness are missing [12,63,78,79,86,89,[93], [94], [95], [96], [97], [98], [99]]. Koonin et al. [16] observe that according to the extent of the outbreak, there may be insufficient institutional capacity to provide ventilator support to all of those in need. Meltzer and Patel [100] argued that any influenza pandemic can put hospital capacities under organizational stress for insufficient supplies when the burden of ill patients is very high. As a consequence, all capable public health services should develop and carry out plans to stockpile critical resources, such as mechanical ventilators, needed to support patients that are severely ill of severe acute respiratory syndrome when alternative and effective treatments lack. One of the major challenges, based on results here, is to plan the amount of ventilators to stockpile and how to manage them to be effectively and timely used for potential pandemic responses. Appropriate strategies can assist national policymakers and local planners to allocate stockpiled ventilators to healthcare facilities during a pandemic emergence, accounting for facilities' ability to make use of additional ventilators. These strategies include actions for increasing numbers of ventilators both in the pre-pandemic and intra-pandemic stages to minimize fatality rates as the study here reveals. In this context, facilities must have sufficient staff, space, equipment, and supplies to utilize allocated ventilators adequately. Moreover, scarce life-saving resources during a pandemic crisis should also consider ethical principles to allocate with equity ventilator devices across different healthcare structures. In addition to ethical principles, decisions of policymakers should assess needs, determinate facilities' ability to use additional ventilators, and also facilities' capacity to ensure access to ventilators for vulnerable populations (e.g., rural, inner city, and uninsured and underinsured individuals) or high-risk populations that may be more susceptible to respiratory illness [16]. Meltzer and Patel [100] also argued that an accurate planning to determine how many ventilators to stockpile and where to stockpile them, it should consider the timing of a pandemic's peak locally (in fact, not all regions will experience simultaneous peak demands for ventilators); wastage (ventilators not sent to where they are needed); and expected unmet demand for mechanical ventilators (i.e., when a hospital has more ill patients that need mechanical ventilation than available breathing devices). Studies suggest that during moderate or severe pandemics, a higher level of unmet demand might need to be expected. Huang et al. [101] argue that hospitals must manage the costs and human resources needed to maintain an excess of ventilators that are likely to be unused in the absence of pandemic-related surges in demand. However, one of the advantages of stockpiling ventilators at hospitals is to facilitate staff training to have skilled human resources prepared when health emergencies occur. Hence, considering results of the study here, a basic strategy to cope with next pandemics is a systematic planning, which should consider the number to be stockpiled of ventilators, how and where stockpiles should be held, maintenance of stockpiles, conditions for release, considerations for use, and what to do when stockpiles are insufficient to adapt meet surges in demand of healthcare structures ([100,101] and [[109], [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [128], [129], [127]]).
Overall, then, results of this analysis here seem to suggest that in the first pandemic wave of COVID-19, countries with a high number of mechanical ventilators experienced a lower fatality rate of COVID-19. The findings here propose a general strategy of crisis management for future pandemic threats based on high levels of investments in healthcare sector for a widespread implementation of new medical ventilators, a transparent and consistent communication of rules, and also strategic collaborative networks between firms and institutions for improving R&D performance in the presence of health emergencies [24]. These strategic implications can support the overall preparedness of countries to cope with negative effects of next deadly infections on health of people and pandemic impact on socioeconomic system. These conclusions are of course tentative. There is need for much more research in these topics because not all the confounding factors that affect the interaction between COVID-19 fatality rates and diffusion of mechanical ventilators in health systems are discussed. Therefore, results here have to be reinforced with a follow-up investigation based on a large sample of countries for additional analyses of the relation between diffusion of mechanical ventilators and negative effects of pandemic respiratory diseases in society.
Credit author statement
Mario Coccia, in the role of main author, has totally developed the following intellectual content of the paper: Conceptualization, Data curation, Formal analysis, Scientific investigation, Designed research, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing - original draft, Writing – review and editing.
Footnotes
Data availability
Data will be made available on request.
References
- 1.Anttiroiko Ari-Veikko. Successful government responses to the pandemic: contextualizing national and urban responses to the COVID-19 outbreak in east and west. International Journal of E-Planning Research (IJEPR), IGI Global. 2021;10(2):1–17. [Google Scholar]
- 2.Coccia M. Pandemic prevention: lessons from COVID-19. Encyclopedia 2021. 2021;1:433–444. doi: 10.3390/encyclopedia1020036. MDPI, Basel, Switzerland, Encyclopedia of COVID-19, open access journal. [DOI] [Google Scholar]
- 3.Coccia M. Optimal levels of vaccination to reduce COVID-19 infected individuals and deaths: a global analysis. Environ. Res. 2022;204 doi: 10.1016/j.envres.2021.112314. Part C, March 2022, Article number 112314, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vinceti M., Filippini T., Rothman K.J., Di Federico S., Orsini N. SARS-CoV-2 infection incidence during the first and second COVID-19 waves in Italy. Environ. Res. 2021;197 doi: 10.1016/j.envres.2021.111097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akan A.P., Coccia M. Changes of air pollution between countries because of lockdowns to face COVID-19 pandemic. Appl. Sci. 2022;12(24) doi: 10.3390/app122412806. [DOI] [Google Scholar]
- 6.Chowdhury T., Chowdhury H., Bontempi E., Coccia M., Masrur H., Sait S.M., Senjyu T. Are mega-events super spreaders of infectious diseases similar to COVID-19? A look into Tokyo 2020 Olympics and Paralympics to improve preparedness of next international events. Environ. Sci. Pollut. Control Ser. 2023;30(4):10099–10109. doi: 10.1007/s11356-022-22660-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benati I., Coccia M. Effective contact tracing system minimizes COVID-19 related infections and deaths: policy lessons to reduce the impact of future pandemic diseases. J. Publ. Adm. Govern. 2022;12(3):19–33. doi: 10.5296/jpag.v12i3.19834. [DOI] [Google Scholar]
- 8.Coccia M. Effects of strict containment policies on COVID-19 pandemic crisis: lessons to cope with next pandemic impacts. Environ. Sci. Pollut. Res. Int. 2023;30(1):2020–2028. doi: 10.1007/s11356-022-22024-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bontempi E., Coccia M., Vergalli S., Zanoletti A. vol. 201. Environmental Research; 2021. (Can Commercial Trade Represent the Main Indicator of the COVID-19 Diffusion Due to Human-To-Human Interactions? A Comparative Analysis between Italy, France, and Spain). Article number 111529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bontempi E., Coccia M. International trade as critical parameter of COVID-19 spread that outclasses demographic, economic, environmental, and pollution factors. Environ. Res. 2021;201 doi: 10.1016/j.envres.2021.111514. Article number 111514, PII S0013-9351(21)00808-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coccia M. High health expenditures and low exposure of population to air pollution as critical factors that can reduce fatality rate in COVID-19 pandemic crisis: a global analysis. Environ. Res. 2021;199 doi: 10.1016/j.envres.2021.111339. Article number 111339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coccia M. The relation between length of lockdown, numbers of infected people and deaths of COVID-19, and economic growth of countries: lessons learned to cope with future pandemics similar to COVID-19. Sci. Total Environ. 2021;775 doi: 10.1016/j.scitotenv.2021.145801. number 145801. [DOI] [Google Scholar]
- 14.Raymond S.J., Baker S., Liu Y., Bustamante M.J., Ley B., Horzewski M.J., et al. A low-cost, highly functional, emergency use ventilator for the COVID-19 crisis. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0266173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Branson R.D., Rodriquez D., Jr. COVID-19 lessons learned: response to the anticipated ventilator shortage. Respir. Care. 2023;68(1):129–150. doi: 10.4187/respcare.10676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koonin L.M., Pillai S., Kahn E.B., Moulia D., Patel A. Strategies to inform allocation of stockpiled ventilators to healthcare facilities during a pandemic. Health security. 2020;18(2):69–74. doi: 10.1089/hs.2020.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morris J., Schofield J., Bull C.…Proctor P., Shore P. Dynamic collaboration in a crisis: creating a low-cost ventilator and test facility. Meas. Sci. Technol. 2023;(3) [Google Scholar]
- 18.Jones R.P. A pragmatic method to compare international critical care beds: implications to pandemic preparedness and non-pandemic planning. Int. J. Health Plann. Manag. 2022;37(4):2167–2182. doi: 10.1002/hpm.3458. [DOI] [PubMed] [Google Scholar]
- 19.Coccia M. Driving forces of technological change in medicine: radical innovations induced by side effects and their impact on society and healthcare. Technol. Soc. 2012;34(4):271–283. doi: 10.1016/j.techsoc.2012.06.002. [DOI] [Google Scholar]
- 20.Coccia M. Socio-cultural origins of the patterns of technological innovation: what is the likely interaction among religious culture, religious plurality and innovation? Towards a theory of socio-cultural drivers of the patterns of technological innovation. Technol. Soc. 2014;36(1):13–25. doi: 10.1016/j.techsoc.2013.11.002. [DOI] [Google Scholar]
- 21.Geurts A., Geerdink T., Sprenkeling M. Accelerated innovation in crises: the role of collaboration in the development of alternative ventilators during the COVID-19 pandemic. Technol. Soc. 2022;68 doi: 10.1016/j.techsoc.2022.101923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Furstenau, Bertolin Leonardo, Zani, Carolina, Terra, Xavier Stela, Sott, Kremer Michele, Choo, Raymond Kim-Kwang, Saurin, Abreu Tarcisio. Resilience capabilities of healthcare supply chain and supportive digital technologies. Technol. Soc. 2022;71(C) doi: 10.1016/j.techsoc.2022.102095. n. 102095. [DOI] [Google Scholar]
- 23.Rezapour Niari, Koroush Eshghi M., Valilai Omid Fatahi. Using cloud manufacturing to establish an ecosystem network for COVID-19 ventilator production. Int. J. Comput. Integrated Manuf. 2023 doi: 10.1080/0951192X.2022.2162586. [DOI] [Google Scholar]
- 24.Ippoliti R., Ramello Giovanni B., Scherer Frederic M. Partnership and innovation in the pharmaceutical industry: the case of clinical research. Econ. Innovat. N. Technol. 2021;30(3):317–334. doi: 10.1080/10438599.2019.1701782. [DOI] [Google Scholar]
- 25.Zimmerling A., Chen X. Innovation and possible long-term impact driven by COVID-19: manufacturing, personal protective equipment and digital technologies. Technol. Soc. 2021;65 doi: 10.1016/j.techsoc.2021.101541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jimenez-Maturano R.J., Martinez-Licona F. IFMBE Proceedings86; 2023. Obsolescence Assessment Approach: Case of Mechanical Ventilators under the Covid-19 Environment; pp. 816–825. [Google Scholar]
- 27.Gong X., Kang S., Guo X.…Gao H., Yuan Y. Associated risk factors with disease severity and antiviral drug therapy in patients with COVID-19. BMC Infect. Dis. 2021;21(1):549. doi: 10.1186/s12879-021-06282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cabrini L., Landoni G., Pintaudi M., Bocchino S., Zangrillo A. The many pros and the few cons of noninvasive ventilation in ordinary wards. Rev. Mal. Respir. 2015;32(9):887–891. doi: 10.1016/j.rmr.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Hu X., Xie F., Wang K.…Zhao Z., Xie L. Scoring system to evaluate the performance of ICU ventilators in the pandemic of COVID-19: a lung model study. Front. Med. 2021;8 doi: 10.3389/fmed.2021.663608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.IMARC . 2022. Mechanical Ventilators Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2021-2026.https://www.imarcgroup.com/mechanical-ventilators-market accessed 2022. [Google Scholar]
- 31.Chandrasekaran K., Monikandan Shaji A. The role of a negative pressure ventilator coupled with oxygen helmet against COVID-19: a review. Research on Biomedical Engineering. 2022;38(1):267–278. doi: 10.1007/s42600-021-00149-0. [DOI] [Google Scholar]
- 32.Gosangi B., Rubinowitz A.N., Irugu D.…Bader A., Cortopassi I. COVID-19 ards: a review of imaging features and overview of mechanical ventilation and its complications. Emerg. Radiol. 2022;29(1):23–34. doi: 10.1007/s10140-021-01976-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma X., Dong Z., Wang Y.…Fang J., Gao S. Risk factors analysis of thoracic trauma complicated with acute respiratory distress syndrome and observation of curative effect of lung-protective ventilation. Frontiers in Surgery. 2022;8 doi: 10.3389/fsurg.2021.826682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garnier M., Constantin J.M., Heming N., Camous L., Ferré A., Razazi K., Lapidus N., COVID-ICU Investigators Epidemiology, risk factors and prognosis of ventilator-associated pneumonia during severe COVID-19: multicenter observational study across 149 European Intensive Care Units. Anaesthesia, critical care & pain medicine. 2023;42(1) doi: 10.1016/j.accpm.2022.101184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lobato D., Mayoralas Alises S. Modern non-invasive mechanical ventilation turns 25. Arch. Bronconeumol. 2013;49(11):475–479. doi: 10.1016/j.arbres.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 36.Pierson D.J. History and epidemiology of noninvasive ventilation in the acute-care setting. Respir. Care. 2009;54(1):40–52. [PubMed] [Google Scholar]
- 37.Saxena A., Nazir N., Pandey R., Gupta S. Comparison of effect of non-invasive ventilation delivered by helmet vs face mask in patients with COVID-19 infection: a randomized control study. Indian J. Crit. Care Med. 2022;26(3):282–287. doi: 10.5005/jp-journals-10071-24155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Soo Hoo G.W. Medscape; 2020. Noninvasive Ventilation.https://emedicine.medscape.com/article/304235-overview Accessed January 2021. [Google Scholar]
- 39.Soo Hoo G.W. Noninvasive ventilation in adults with acute respiratory distress: a primer for the clinician. Hosp. Pract. 2010;38(1):16–25. doi: 10.3810/hp.2010.02.275. 1995. [DOI] [PubMed] [Google Scholar]
- 40.Medtronic . 2022. Mechanical Ventilation, Puritan Bennett™ 980 Ventilator Series.https://www.medtronic.com/covidien/en-us/products/mechanical-ventilation/puritan-bennett-980-ventilator.html accessed March 2022. [Google Scholar]
- 41.Wilamed . 2022. WILAflow Elite.https://live.wilamed.de/Products/wilaflow-elite/?lang=en accessed March 2022. [Google Scholar]
- 42.Maheshwarappa H.M., Mishra S., Sreedharan J.K. 2021. Technology of Non-invasive Ventilators. Intensive Care and Non-intensive Care Devices. Bi-level Ventilators. Software-Algorithm. Leak Compensation. Performance. Airway Pressure Transducers, Flow Sensors (Book Chapter), Principles and Practice of Non-invasive Mechanical Ventilation Monitoring: from Intensive Care to Home Care; pp. 100–109. [Google Scholar]
- 43.Weerakkody S., Arina P., Glenister J.…Singer M., Montgomery H.E. Non-invasive respiratory support in the management of acute COVID-19 pneumonia: considerations for clinical practice and priorities for research. Lancet Respir. Med. 2022;10(2):199–213. doi: 10.1016/S2213-2600(21)00414-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang J., Wang Y., Shen J., Zou D., Huang J., Han X., Zhang R., Fei Z., Zheng Y., Zhao J., Xu T., Yu X., Huang J. Application of non-invasive ventilator in treatment of severe COVID-19 patients. Clin. Lab. 2022;68(1) doi: 10.7754/Clin.Lab.2021.210416. 10.7754/Clin.Lab.2021.210416. [DOI] [PubMed] [Google Scholar]
- 45.Dräger . 2022. Evita Infinity V500 (2022)https://www.draeger.com/en-us_us/Products/Evita-Infinity-V500-ventilator (accessed March 2022) [Google Scholar]
- 46.Auld S.C., Caridi-Scheible M., Blum J.M., Robichaux C., Kraft C., Jacob J.T., Jabaley C.S.…Murphy D.J., ICU and Ventilator Mortality among Critically Ill Adults with Coronavirus Disease 2019 . 2020. Critical Care Medicine; pp. E799–E804. Cited 186 times. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee J.Y., Kim H.A., Huh K., Hyun M., Rhee J.-Y., Jang S., Kim J.-Y.…Chang H.-H. Risk factors for mortality and respiratory support in elderly patients hospitalized with COVID-19 in Korea(Open Access) (2020) J. Kor. Med. Sci. 2020;35(23):E223. doi: 10.3346/JKMS.2020.35.E223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Müller G.V. Neue Zürcher Zeitung; 2020. Hersteller von Beatmungsgeräten produzieren massiv mehr, aber können die Nachfrage trotzdem nicht decken. (in German). Retrieved 2020-03-30. With reference to: IPG Research. [Google Scholar]
- 49.Edwards Ed Thomas. 2022. Medical Ventilator Manufacturers and Companies.https://www.thomasnet.com/articles/top-suppliers/medical-ventilators-manufacturers-companies/ Accessed March 2022. [Google Scholar]
- 50.Smiths Medical . 2022. Ventilation Products.https://www.smiths-medical.com/products/ventilation accessed March 2022. [Google Scholar]
- 51.Our World in Data . 2022. Ventilators (Total Number), Variable Time Span: 2015 – 2020.https://ourworldindata.org/grapher/number-of-medical-ventilators [Google Scholar]
- 52.The World Bank . 2022. GDP Per Capita (Constant 2010 US$)https://data.worldbank.org/indicator/NY.GDP.PCAP.KD accessed March 2022. [Google Scholar]
- 53.The World Bank . 2022. Data, Population, Total.https://data.worldbank.org/indicator/SP.POP.TOTL Accessed January 2022. [Google Scholar]
- 54.The World Bank . 2022. Current Health Expenditure (% of GDP)https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS Accessed February 2022. [Google Scholar]
- 55.Lau H., Khosrawipour T., Kocbach P., Ichii H., Bania J., Khosrawipour V. Evaluating the massive underreporting and undertesting of COVID-19 cases in multiple global epicenters. Pulmonology. 2021;27(2):110–115. doi: 10.1016/j.pulmoe.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Who . 2020. Estimating Mortality from COVID-19, Scientific Brief.https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19,4 August Accessed. [Google Scholar]
- 57.Wilson N., Kvalsvig A., Barnard L., et al. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg. Infect. Dis. 2020;26(6):1339–1441. doi: 10.3201/eid2606.200320. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Angelopoulos A.N., Pathak R., Varma R., Jordan M.I. On identifying and mitigating bias in the estimation of the COVID-19 case fatality rate. Harvard Data Science Review. 2020 doi: 10.1162/99608f92.f01ee285. [DOI] [Google Scholar]
- 59.Johns Hopkins Center for System Science and Engineering . 2023. Coronavirus COVID-19 Global Cases.https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 accessed in. [Google Scholar]
- 60.Coccia M. An introduction to the methods of inquiry in social sciences. Journal of Social and Administrative Sciences. 2018;5(2):116–126. doi: 10.1453/jsas.v5i2.1651. [DOI] [Google Scholar]
- 61.Magazzino C., Mele M., Coccia M. Epidemiology and infection; 2022. A Machine Learning Algorithm to Analyze the Effects of Vaccination on COVID-19 Mortality; pp. 1–24. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Benati I., Coccia M. Global analysis of timely COVID-19 vaccinations: improving governance to reinforce response policies for pandemic crises. International Journal of Health Governance. 2022;27(3):240–253. doi: 10.1108/IJHG-07-2021-0072. [DOI] [Google Scholar]
- 63.Coccia M. COVID-19 pandemic over 2020 (with lockdowns) and 2021 (with vaccinations): similar effects for seasonality and environmental factors. Environ. Res. 2022;208 doi: 10.1016/j.envres.2022.112711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Coccia M. Improving preparedness for next pandemics: max level of COVID-19 vaccinations without social impositions to design effective health policy and avoid flawed democracies. Environ. Res. 2022;213 doi: 10.1016/j.envres.2022.113566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Atkeson A.G. Brookings Papers on Economic Activity; Spring: 2021. Behavior and the Dynamic of Epidemics. [Google Scholar]
- 66.El-Sadr W.M., Vasan A., El-Mohandes A. Facing the new covid-19 reality. N. Engl. J. Med. 2023;388(5):385–387. doi: 10.1056/NEJMp2213920. [DOI] [PubMed] [Google Scholar]
- 67.Coccia M. Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency[J] AIMS Public Health. 2023;10(1):145–168. doi: 10.3934/publichealth.2023012. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Birch J. Science and policy in extremis: the UK's initial response to COVID-19. Eur. J. Phil. Sci. 2021;11:90. doi: 10.1007/s13194-021-00407-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Coccia M. Deep learning technology for improving cancer care in society: new directions in cancer imaging driven by artificial intelligence. Technol. Soc. 2020;60(February):1–11. doi: 10.1016/j.techsoc.2019.101198. art. n. 101198. [DOI] [Google Scholar]
- 70.Coccia M. Springer; Cham: 2020. Destructive Technologies for Industrial and Corporate Change. A. Farazmand A., Global Encyclopedia of Public Administration, Public Policy, and Governance. [DOI] [Google Scholar]
- 71.Coccia M. Fishbone diagram for technological analysis and foresight. Int. J. Foresight Innovation Policy. 2020;14:225–247. doi: 10.1504/IJFIP.2020.111221. Nos. 2/3/4. [DOI] [Google Scholar]
- 72.Coccia M. Evolution of technology in replacement of heart valves: transcatheter aortic valves, a revolution for management of valvular heart diseases. Health Policy and Technology. 2021;10(2) doi: 10.1016/j.hlpt.2021.100512. [DOI] [Google Scholar]
- 73.Coccia M. Evolution and structure of research fields driven by crises and environmental threats: the COVID-19 research. Scientometrics. 2021;126(12):9405–9429. doi: 10.1007/s11192-021-04172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Löwenstein Medical Innovation . 2022. Ventilators.https://hospital.loewensteinmedical.com/en/ventilation/ Accessed March 2022. [Google Scholar]
- 75.Allen Douglas W. Covid-19 lockdown cost/benefits: a critical assessment of the literature. Int. J. Econ. Bus. 2022;29(1):1–32. doi: 10.1080/13571516.2021.1976051. [DOI] [Google Scholar]
- 76.Ball P. Interface Focus; 2021. What the COVID-19 Pandemic Reveals about Science, Policy and Society. 112021002220210022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barro R.J. NBER Working Paper; 2020. Non-Pharmaceutical Interventions and Mortality in U.S. Cities during the Great Influenza Pandemic, 1918-1919. No. 27049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Coccia M. In: Global Encyclopedia of Public Administration, Public Policy, and Governance. Farazmand A., editor. Springer; 2019. Comparative institutional changes. [DOI] [Google Scholar]
- 79.Coccia M. Why do nations produce science advances and new technology? Technol. Soc. 2019;59(November):1–9. doi: 10.1016/j.techsoc.2019.03.007. 101124. [DOI] [Google Scholar]
- 80.Coccia M. Intrinsic and extrinsic incentives to support motivation and performance of public organizations. Journal of Economics Bibliography. 2019;6(1):20–29. doi: 10.1453/jeb.v6i1.1795. [DOI] [Google Scholar]
- 81.Goolsbee A., Syverson C. Fear, lockdown, and diversion: comparing drivers of pandemic economic decline 2020. J. Publ. Econ. 2021;193 doi: 10.1016/j.jpubeco.2020.104311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Homburg S. Effectiveness of corona lockdowns: evidence for a number of countries. Econ. Voice. 2020;17(1) [Google Scholar]
- 83.Pagliaro M., Coccia M. How self-determination of scholars outclasses shrinking public research lab budgets, supporting scientific production: a case study and R&D management implications. Heliyon. 2021;7(1) doi: 10.1016/j.heliyon.2021.e05998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wieland T. A phenomenological approach to assessing the effectiveness of COVID-19 related nonpharmaceutical interventions in Germany. Saf. Sci. 2020;131 doi: 10.1016/j.ssci.2020.104924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Askitas N., Tatsiramos K., Verheyden B. Estimating worldwide effects of non-pharmaceutical interventions on COVID-19 incidence and population mobility patterns using a multiple-event study. Sci. Rep. 2021;11(1) doi: 10.1038/s41598-021-81442-x. art. no. 1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Coccia M. Preparedness of countries to face covid-19 pandemic crisis: strategic positioning and underlying structural factors to support strategies of prevention of pandemic threats. Environ. Res. 2022;203 doi: 10.1016/j.envres.2021.111678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., Whittaker C.…Bhatt S. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 88.Shattock A.J., Le Rutte E.A., Dünner R.P.…Chitnis N., Penny M.A. Impact of vaccination and non-pharmaceutical interventions on SARS-CoV-2 dynamics in Switzerland. Epidemics. 2022;38 doi: 10.1016/j.epidem.2021.100535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Coccia M. Probability of discoveries between research fields to explain scientific and technological change. Technol. Soc. 2022;68 doi: 10.1016/j.techsoc.2022.101874. February, n. [DOI] [Google Scholar]
- 90.Mosleh M., Roshani S., Coccia M. Scientific laws of research funding to support citations and diffusion of knowledge in life science. Scientometrics. 2022;127:1931–1951. doi: 10.1007/s11192-022-04300-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Roshani S., Bagheri R., Mosleh M., Coccia M. What is the relationship between research funding and citation-based performance? A comparative analysis between critical disciplines. Scientometrics. 2021;126:7859–7874. doi: 10.1007/s11192-021-04077-9. [DOI] [Google Scholar]
- 92.Roshani S., Coccia M., Mosleh M. Sensor technology for opening new pathways in diagnosis and therapeutics of breast, lung, colorectal and prostate cancer. HighTech and Innovation Journal. 2022;3(3):356–375. doi: 10.28991/HIJ-2022-03-03-010. September. [DOI] [Google Scholar]
- 93.Ardito L., Coccia M., Messeni Petruzzelli A. Technological exaptation and crisis management: evidence from COVID-19 outbreaks. R&D Management. 2021;51(4):381–392. doi: 10.1111/radm.12455. [DOI] [Google Scholar]
- 94.Kluge H.H.P., Nitzan D., Azzopardi-Muscat N. COVID-19: reflecting on experience and anticipating the next steps. A perspective from the WHO Regional Office for Europe. Eurohealth. 2020;26(2) 2020. [Google Scholar]
- 95.Coccia M. General sources of general purpose technologies in complex societies: theory of global leadership-driven innovation, warfare and human development. Technol. Soc. 2015;42(August):199–226. doi: 10.1016/j.techsoc.2015.05.008. [DOI] [Google Scholar]
- 96.Coccia M. The Nexus between technological performances of countries and incidence of cancers in society. Technol. Soc. 2015;42(August):61–70. doi: 10.1016/j.techsoc.2015.02.003. [DOI] [Google Scholar]
- 97.Coccia M. In: Socioeconomic Dynamics of the COVID-19 Crisis, Global, Regional, and Local Perspectives. Faghih N., Forouharfar A., editors. Springer International Publishing; 2022. The spread of the novel Coronavirus disease 2019 in polluted cities: lessons learned from environmental and demographic factors for prevention of pandemic diseases. [DOI] [Google Scholar]
- 98.Coccia M. COVID-19 vaccination is not a sufficient public policy to face crisis management of next pandemic threats. Publ. Organ. Rev. 2022 doi: 10.1007/s11115-022-00661-6. [DOI] [Google Scholar]
- 99.Kapitsinis N. The underlying factors of the COVID-19 spatially uneven spread. Initial evidence from regions in nine EU countries. Regional Science Policy and Practice. 2020;12(6):1027–1045. [Google Scholar]
- 100.Meltzer M.I., Patel A. Stockpiling ventilators for influenza pandemics. Emerg. Infect. Dis. 2017;23(6):1021–1022. doi: 10.3201/eid2306.170434. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Huang H.C., Araz O.M., Morton D.P., Johnson G.P., Damien P., Clements B., Meyers L.A. Stockpiling ventilators for influenza pandemics. Emerg. Infect. Dis. 2017;23(6):914–921. doi: 10.3201/eid2306.161417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Coccia M. Sources of technological innovation: radical and incremental innovation problem-driven to support competitive advantage of firms. Technol. Anal. Strat. Manag. 2017;29(9):1048–1061. doi: 10.1080/09537325.2016.1268682. [DOI] [Google Scholar]
- 103.Coccia M. The Fishbone diagram to identify, systematize and analyze the sources of general purpose technologies. Journal of Social and Administrative Sciences. 2017;4(4):291–303. doi: 10.1453/jsas.v4i4.1518. [DOI] [Google Scholar]
- 104.Coccia M. Classification of innovation considering technological interaction. Journal of Economics Bibliography. 2018;5(2):76–93. doi: 10.1453/jeb.v5i2.1650. [DOI] [Google Scholar]
- 105.Coccia M. General properties of the evolution of research fields: a scientometric study of human microbiome, evolutionary robotics and astrobiology. Scientometrics. 2018;117(2):1265–1283. doi: 10.1007/s11192-018-2902-8. [DOI] [Google Scholar]
- 106.Coccia M. Asymmetry of the technological cycle of disruptive innovations. Technol. Anal. Strat. Manag. 2020;32(12):1462–1477. doi: 10.1080/09537325.2020.1785415. [DOI] [Google Scholar]
- 107.Coccia M. The evolution of scientific disciplines in applied sciences: dynamics and empirical properties of experimental physics. Scientometrics. 2020;124:451–487. doi: 10.1007/s11192-020-03464-y. [DOI] [Google Scholar]
- 108.Coccia M. Technology Analysis & Strategic Management; 2022. Technological Trajectories in Quantum Computing to Design a Quantum Ecosystem for Industrial Change. 10.1080/09537325.2022.2110056. [DOI] [Google Scholar]
- 109.Coccia M. Competition between basic and applied research in the organizational behaviour of public research labs. J. Econ. Lib. 2018;5(2):118–133. doi: 10.1453/jel.v5i2.1652. [DOI] [Google Scholar]
- 110.Coccia M. In: Global Encyclopedia of Public Administration, Public Policy, and Governance, Springer Nature Switzerland. Farazmand A., editor. 2019. The Role of Superpowers in Conflict Development and Resolutions. [DOI] [Google Scholar]
- 111.Coccia M. Types of government and innovative performance of countries. J. Adm. Soc. Sci. 2018;5(1):15–33. doi: 10.1453/jsas.v5i1.1573. [DOI] [Google Scholar]
- 112.Coccia M., Bellitto M. A critique of human progress: a new definition and inconsistencies in society. Quaderni IRCrES-CNR. 2018;4(3):51–67. doi: 10.23760/2499-6661.2018.017. [DOI] [Google Scholar]
- 113.Coccia M. In: Strategic Entrepreneurship. Contributions to Management Science. Faghih N., Forouharfar A., editors. Springer; Cham: 2022. Innovation Strategies for Strategic Entrepreneurship in Ever-Increasing Turbulent Markets. [DOI] [Google Scholar]
- 114.Coccia M. In: Global Encyclopedia of Public Administration, Public Policy, and Governance. Farazmand A., editor. Springer; 2019. Metabolism of Public Organizations. [DOI] [Google Scholar]
- 115.Coccia M. Recurring waves of Covid-19 pandemic with different effects in public health. J. Econ. Bib. 2021;8(1):28–45. doi: 10.1453/jeb.v8i1.2184. [DOI] [Google Scholar]
- 116.Coccia M., Wang L. Evolution and convergence of the patterns of international scientific collaboration. Proc. Natl. Acad. Sci. U.S.A. 2016;113(8):2057–2061. doi: 10.1073/pnas.1510820113. www.pnas.org/cgi/doi/10.1073/pnas.1510820113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Coccia M., Watts J. A theory of the evolution of technology: technological parasitism and the implications for innovation management. J. Eng. Technol. Manag. 2020;55 doi: 10.1016/j.jengtecman.2019.11.003. [DOI] [Google Scholar]
- 118.Coccia M. A Theory of classification and evolution of technologies within a Generalized Darwinism. Technol. Anal. Strat. Manag. 2019;31(5):517–531. doi: 10.1080/09537325.2018.1523385. [DOI] [Google Scholar]
- 119.Coccia M. Technological Innovation. The Blackwell Encyclopedia of Sociology. Edited by George Ritzer and Chris Rojek. John Wiley & Sons, Ltd.; 2021. [DOI] [Google Scholar]
- 120.Coccia M.Coccia, Benati I. What is the relation between public manager compensation and government effectiveness? An explorative analysis with public management implications. Quaderni Ircres-CNR. 2017;2(2):1–36. doi: 10.23760/2499-6661.2017.001. [DOI] [Google Scholar]
- 121.Coccia M. Effects of air pollution on COVID-19 and public health, COVID-19 preprint in Research Square. [DOI]
- 122.Coccia M., Benati I. In: Global Encyclopedia of Public Administration, Public Policy, and Governance. Farazmand A., editor. Springer International Publishing AG, part of Springer Nature; 2018. Comparative Evaluation Systems. [DOI] [Google Scholar]
- 123.Coccia M. Measuring the impact of sustainable technological innovation. Int. J. Technol. Intell. Plann. 2009;5(3):276–288. doi: 10.1504/IJTIP.2009.026749. [DOI] [Google Scholar]
- 124.Coccia M. 2008. Spatial mobility of knowledge transfer and absorptive capacity: analysis and measurement of the impact within the geoeconomic space, J. Technol. Trans., vol. 33, n. 1, pp. 105-122. 10.1007/s10961-007-9032-4. [DOI]
- 125.Coccia M. The source and nature of general purpose technologies for supporting next K-waves: Global leadership and the case study of the U.S. Navy’s Mobile User Objective System. Technol. Forecast. Soc. Change. 2017;116:331–339. doi: 10.1016/j.techfore.2016.05.019. [DOI] [Google Scholar]
- 126.Coccia M. Measuring scientific performance of public research units for strategic change. J. Informetr. 2008;2(3):183–194. doi: 10.1016/j.joi.2008.04.001. [DOI] [Google Scholar]
- 127.Coccia M. Converging scientific fields and new technological paradigms as main drivers of the division of scientific labour in drug discovery process: the effects on strategic management of the R&D corporate change. Technol. Anal. Strat. Manag. 2014;26(7):733–749. doi: 10.1080/09537325.2014.882501. [DOI] [Google Scholar]
- 128.Coccia M. Spatial metrics of the technological transfer: analysis and strategic management. Technol. Anal. Strat. Manag. 2004;16(1):31–52. doi: 10.1080/0953732032000175490. [DOI] [Google Scholar]
- 129.Coccia M. Optimization in R&D intensity and tax on corporate profits for supporting labor productivity of nations. J. Technol. Trans. 2018;43(3):792–814. doi: 10.1007/s10961-017-9572-1. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.