Abstract
Because the application of intracavitary electrocardiogram (IC‐ECG)‐guided peripherally inserted central catheter (PICC) in the treatment of neonates is controversial in terms of phlebitis reduction compared with traditional X‐ray positioning technique, a systematical evaluation is needed on the impact of IC‐ECG on this common complication following PICC. Literature retrieval was conducted on large databases including PubMed, Google Scholar, Cochrane library, and CNKI. Randomised controlled trials (RTCs) of intracavitary electrocardiogram‐guided peripherally inserted central catheter tip placement in the treatment of neonates up to July 7, 2022, were collected. Then indicators of included studies were compared and analysed by two researchers. Meta‐analysis was performed on the STATA 17.0 software. After excluding invalid trials, 11 out of 316 randomised controlled trials were included for further analysis. Meta‐analysis results showed that compared with the control group, IC‐ECG‐guided PICC could decrease the incidence of phlebitis (I 2 = 0.00%, P = 0.76, OR = 0.33, 95% CI 0.19–0.56) and that no significant difference was observed between preterm neonates and term neonates (P = 0.74). Meanwhile, total complications were decreased in neonates (I 2 = 0.00%, P = 0.00 OR = 0.23, 95% CI 0.16–0.33). IC‐ECG‐guided PICC could also improve the accuracy of optimal tip location (I 2 = 0.00%, P = 0.53, OR = 5.37, 95% CI 3.80–7.59). IC‐ECG‐guided PICC could achieve reduced phlebitis incidence and total complications in the treatment of neonates, as well as increased accuracy of optimal tip location, no matter if those neonates were preterm or not. This study was registered in inplasy.com with No. INPLASY202280012 (DOI: 10.37766/inplasy2022.8.0012).
Keywords: intracavitary electrocardiogram, meta‐analysis, neonate, phlebitis, PICC
1. BACKGROUND
Phlebitis as a common complication associated with PICC lines and the inflammation of the tunica intima of the vein may lead to further consequences, such as discomfort, damage of affected veins, missed medication doses, significant morbidity or mortality, and a subsequent longer hospital stay with increased treatment costs. 1 PICC is a highly recommended venous infusion technique which provides long‐term intravenous medication and nutrition to critically ill newborns in neonatal intensive care units (NICU). 2 , 3 Proper placement of the catheter tip plays a crucial role in ensuring the effectiveness of PICC. The optimal location of a central venous catheter tip is the cavoatrial junction (CAJ) and other acceptable locations include lower third of superior vena cava (SVC) and upper part of the right atrium (RA). 4 Although chest radiography has long been a standard approach to verifying the correct tip location after catheterization, 5 IC‐ECG has been developed for real‐time monitoring and verification of PICC tip placement. 6 , 7 Nevertheless, it's noteworthy that it is more difficult to place the tip in a correct location in neonates because of the uncertainty in estimating the depth from the puncture site to the CAJ. 4 Furthermore, repeated peripheral venipuncture may cause pain and hinder the neurodevelopment in neonates. Therefore, reposition more complications may occur with neonatal PICC replacement and repositions are needed. In clinical studies, incorrect tip placement is accompanied by the risk of phlebitis. 8 , 9 , 10 As phlebitis is irreversible, early diagnosis and treatment are particularly important for neonates with PICC. 11 , 12 , 13
The traditional evaluation standard of the positioning accuracy of PICC catheter tip is X‐ray chest examination, 14 which then was replaced by the “IC‐ECG.” Recently, the IC‐ECG‐guided PICC insertion to support accurate tip placement is available in NICU settings. The IC‐ECG monitor is connected to the neonate via 3 ECG pads and the ECG waveform is observed when the PICC is correctly placed. When the catheter reaches the superior vena cava, the P wave is elevated or amplified. As the catheter continues to reach the junction of the superior vena cava and the right atrium, the P‐wave amplitude increases to a peak. 15 Variations in P‐wave amplitude are used to adjust the real‐time PICC tip position. 16 This IC‐ECG‐guided PICC tip positioning technique helps nurses and physicians identify the PICC tip position in real time. 17 , 18 This improved approach is expected to help reduce the incidence of phlebitis and is recommended by domestic and foreign guidelines for the treatment of PICC. 19 , 20 , 21 However, several studies have reported the incidence of phlebitis. Huang et al 22 indicated that incidence rate of phlebitis within a week post‐PICC guided by IC‐ECG was not lower than that positioned by traditional measurement of body surface. Jiang et al and Yang et al also reported that nearly 3% patients received the treatment of IC‐ECG‐guided PICC had phlebitis. 23 , 24 The current limited clinical application report data of IC‐ECG‐guided PICC in neonate and the inconsistent results of related studies for technical limitations of randomised controlled trials might limit the application of that in clinical practice. Therefore, our current study conducted a meta‐analysis of phlebitis prevalence by pooling estimations from individual studies, which hopefully provides evidence for the PICC treatment.
2. METHODS
The meta‐analysis is conducted in accordance with the Preferred Reporting Items for Systematic Evaluation and Meta‐Analysis (PRISMA). 25 As personal data of the participants were not included in this analysis, ethical approval was not required.
2.1. Search strategy
Two researchers (Gan and Hu) searched relevant papers about RCTs of IC‐ECG‐guided PICC tip placement in neonates that were published before 7 July 2022 in PubMed, Google Scholar, Cochrane library and CNKI by using the key words of (“PICC” OR “peripherally inserted central venous catheter” AND “IC‐ECG” OR “intracavitary electrocardiogram” OR “tip placement” AND “phlebitis” AND “neonate” AND “RCT” OR “randomized controlled trial” [MeSH]). No limitation of language was conducted in included study.
2.2. Literature inclusion and exclusion criteria
The following inclusion criteria were implemented: (1) RCTs of intracavitary electrocardiogram‐guided PICC tip placement in the treatment of neonates less than a month of birth; (2) all patients were diagnosed with PICC. The experimental group received treatment with intracavitary electrocardiogram while the control group received the conventional X‐ray chest examination. Other clinical treatments were the same on the two groups. (3) The indicators for phlebitis estimation were reported. The exclusion criteria included (1) duplicate publications; (2) studies whose data were unusable or missing; and (3) reviews, letters, meta‐analysis, and cases.
2.3. Data extraction
Two researchers independently screened and cross‐checked the literature we retrieved against the inclusion and exclusion criteria. In case of disagreement, they discussed or consulted a third party to assist in the verdict. Information including authors, year of publication, basic information about the study population, sample size, treatment regimen, outcome indicators, and other important data were extracted by the two researchers according to the designed data extraction form. If there was not enough relevant outcome data, we would contact the authors whenever possible.
2.4. Quality evaluation
The second version of the Cochrane risk of bias toll (RoB 2.0) 26 was used to evaluate the methodological quality and risk of bias of included RCTs, and any disagreement concerning the quality evaluation was resolved by discussion and consensus. The Cochrane risk of bias tool includes five specific domains: randomization process, deviations from the intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. 27 The tool provides an overall rating of a study, and the measured results can be classified into low‐risk bias, high‐risk bias, or unclear risk of bias according to specific judging criteria.
2.5. Statistical analysis
The STATA 17.0 software (Stata Corp LLC, Texas) was adopted in this study to perform a meta‐analysis of the included literature. Odds ratio (OR) was used to describe dichotomous variables, mean difference (MD) was used to describe continuity variables, and all effect sizes were expressed as 95% confidence interval (CI). P < 0.05 suggests that the difference between groups was statistically significant. Concerning the clinical and methodological heterogeneity of the included studies, the DerSimonian & Laird method, a random‐effect model, was selected for meta‐analysis in this study. 28 I 2 value from 0 to 25% was considered as mild heterogeneity, between 50% and 75% was corresponded to moderate heterogeneity, and between 75% and 100% was an indicator of high heterogeneity. Funnel plot and Egger's test were conducted to determine whether there was a publication bias reflected by the results of meta‐analysis. 29 If a publication bias was identified, the shear and complement method would be used to further evaluate the stability and reliability of the meta‐analysis results. In addition, sensitivity analysis was performed to assess the robustness of the meta‐analysis results.
3. RESULTS
3.1. Study inclusion
As shown in Figure 1, a total of 316 literature entries were obtained from PubMed, Google Scholar, Cochrane library, Embase and CNKI, among which 11 RCTs were selected for further analysis and quantitative synthesis. 3 , 19 , 22 , 23 , 24 , 30 , 31 , 32 , 33 , 34 , 35 Table 1 shows the characteristics of the included studies.
FIGURE 1.

PRISMA flow diagram
TABLE 1.
Characteristics of included studies
| Study ID | Total Patients | Phlebitis events(n) | PICC tip verified? | Approach | Catheters | Preterm neonates reported? | |||
|---|---|---|---|---|---|---|---|---|---|
| IC⁃ECG group | Comparison group | ||||||||
| Yes | No | Yes | No | ||||||
| Xiao et al, 2019 | 161 | 2 | 76 | 7 | 76 | Yes | superior vena cava | 1.9Fr Medcomp | Yes |
| Ling et al, 2019 | 160 | 1 | 79 | 7 | 73 | Yes | superior vena cava | 1.9Fr Medcomp | Yes |
| Huang Y et al, 2020 | 144 | 2 | 70 | 5 | 67 | Yes | lower limb veins | 1.9Fr | Yes |
| Huang T et al, 2020 | 62 | 0 | 31 | 2 | 29 | NR | superior vena cava | NR | No |
| Tang et al, 2021 | 210 | 2 | 103 | 9 | 96 | Yes | superior vena cava | 1.9Fr PRODIMED | Yes |
| Yu et al, 2021 | 130 | 1 | 54 | 10 | 65 | Yes | superior vena cava | 1.9Fr | No |
| Yang L et al, 2021 | 400 | 6 | 194 | 7 | 193 | Yes | superior vena cava | 1.9Fr, Medcomp | No |
| Jiang et al, 2021 | 172 | 3 | 83 | 6 | 80 | Yes | superior vena cava | 1.9Fr UNI | Yes |
| Yang C et al, 2021 | 180 | 0 | 90 | 4 | 86 | Yes | lower limb veins | NR | No |
| Zhang, 2021 | 142 | 0 | 71 | 5 | 66 | NR | superior vena cava | 1.9Fr UNI | No |
| Zhang et al, 2022 | 200 | 1 | 99 | 3 | 97 | Yes | superior vena cava | NR | No |
3.2. Quality of included studies
The bias risk assessment tool was adopted for quality evaluation. 36 As can be seen in Figure S1 and Figure 2, nine RCTs were confirmed with a low risk of bias, while the remaining two RCTs were classified with some concerns. The domain which was highly rated with some‐concerns was randomization process, in which two RCTs with unknown randomization scheme had clear randomization schemes, and the patients were randomised using a random number table or the computer randomization method.
FIGURE 2.

Risk of bias summary
3.3. Synthesised outcomes
3.3.1. Phlebitis
The eleven studies reported the probability of phlebitis caused by IC‐ECG‐guided PICC tip placement in neonates. Compared with the control group, IC‐ECG‐guided PICC placement in the treatment of neonates significantly reduced the risk of phlebitis. (OR = 0.33, 95% CI 0.19–0.56, P < 0.001, in Figure 3). Moreover, five studies reported the probability of phlebitis caused by IC‐ECG‐guided PICC tip placement in preterm neonates and six studies in term neonates. Subgroup analysis suggested that there was no significant difference of results between the preterm and term group (P = 0.74) (Figure 4).
FIGURE 3.

Forest plots of phlebitis with neonates
FIGURE 4.
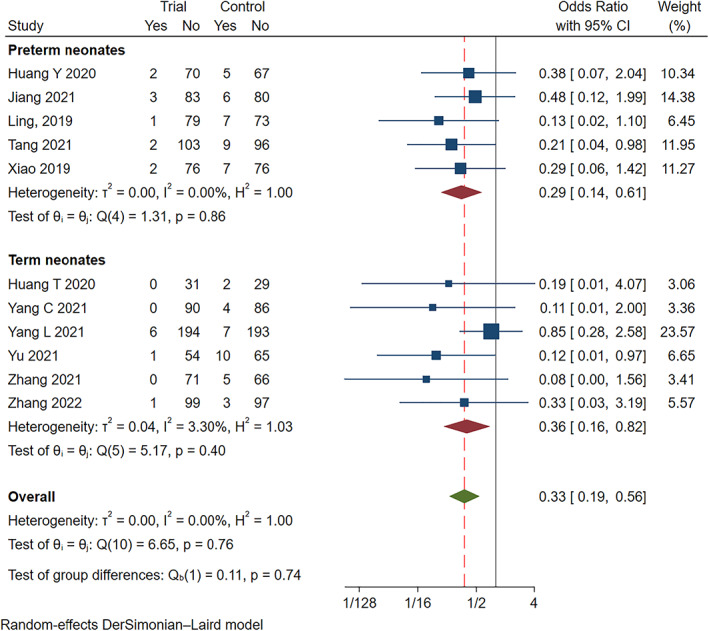
Forest plots of phlebitis with preterm neonates and term neonates
3.3.2. Optimal tip location
Ten studies reported the optimal tip location of IC‐ECG‐guided PICC tip placement in neonates. Meta‐analysis results indicated that there was no heterogeneity between studies (I 2 = 0.00%, P = 0.53), and a fixed‐effects model was selected. Compared with the control group, IC‐ECG increased the accuracy of optimal tip location in the treatment of neonates (OR = 5.37, 95% CI 3.80–7.59, P < 0.001, in Figure. 5).
FIGURE 5.

Forest plots of optimal tip location
3.3.3. Total complications
Eleven RCTs reported implications associated with IC‐ECG‐guided PICC tip placement in neonates. The results of meta‐analysis identified no heterogeneity among the eleven studies (I 2 = 0.00%, P = 0.00), and a fixed‐effects model was selected. Compared with the control group, IC‐ECG‐guided PICC tip placement significantly reduces the occurrence of total complications (OR = 0.23, 95% CI 0.16–0.33, P < 0.001, in Figure S2) in neonates.
3.3.4. Catheter dwell time
Two studies reported reduced catheter dwell time of IC‐ECG‐guided PICC tip placement in neonates (MD = −5.86, 95% CI −16.36 to 4.65, P = 0.00). The results of meta‐analysis identified considerable heterogeneity between studies (I 2 = 99.64%) (Figure S3).
3.4. Sensitivity analysis
Sensitivity analysis presented that the studies led to none of significant change in the primary data, suggesting the stability and reliance.
3.5. Publications of bias
Publication bias was assessed by funnel plot and egger's test. As shown by the results in Figure 6, Figures S4 and S5, the shear and complement method present stable result although there is publication bias (P = 0.0019).
FIGURE 6.

Funnel plot of included studies
4. DISCUSSION
Our study set out to systematically compare the incidence of phlebitis in PICC‐treated neonates between IC‐ECG and traditional X‐ray method through a meta‐analysis. Our synthesised data suggested that the incidence of phlebitis was lower in neonates treated with IC‐ECG‐guided PICC tip placement compared with that of X‐ray control. The main strength of this meta‐analysis is that all trials were conducted prospectively to be similar with each other in design. As a result, related heterogeneity across the trials was low.
Phlebitis is known as inflammation and a common complication of PICC, which can bring mechanical risk factors, such as catheter material, size, site and duration, to vein. 37 , 38 This means that different methods of catheter placement led to varying catheter tip positioning accuracy, which may increase the risk of complications, especially in neonates because of significant individual differences in the vascular conditions of them. Among these determinants, accuracy of location was in our study proved to be increased if IC‐ECG could be used as the positioning technique rather than conventional method in PICC. This was in line with previous systematic review reported by Liu et al that the success rate of IC‐ECG‐guided PICC tip position was greater than conventional x‐ray methods in adult patients. 39 Also, Chen et al conducted a meta‐analysis suggested that ECG applied in PICC tip positioning helps improve the accuracy of catheter tip positioning while reducing the incidence of related complications, including phlebitis, which further supported our conclusions despite of a limited sample size. 40
Apart from these, characteristics of the X‐ray technique, including weakness of real‐time monitoring, increasing operating time, and radiological damage, may cause the minimised efficiency and accuracy during PICC procedure. 16 , 41 In contrast, advantages of IC‐ECG‐guided PICC catheter tip positioning such as early detection of ectopic PICC tip location, simple operation at the bedside which was time‐consuming and reduced physical radiation might also be underlying mechanisms of our conclusion. 42 , 43
However, this meta‐analysis also has some limitations. First, participants included in our study were relatively small, partly because of low patient compliance and follow‐up losses. Second, up‐to‐date academic conference literature or unpublished data were not included in our analysis. A larger sample size and more reliable data should be incorporated in future studies to further examine the role of IC‐ECG‐guided PICC placement in phlebitis incidence reduction and placement success improvement.
In summary, IC‐ECG as a technique with high accuracy and feasibility, could guide the PICC tip placement in neonates, and reduce phlebitis rates and total complications with great safety and effectiveness, as well as increase accuracy of optimal tip location, no matter if those neonates were preterm or not. As such, the IC‐ECG‐guided PICC placement could be recommended for the clinical treatment of neonatal diseases.
Supporting information
Figure S1. Risk of bias graph
Figure S2. Forest plots of complications
Figure S3. Forest plots of catheter dwell time
Figure S4. Egger's test of included studies
Figure S5. Shear and complement results
Gan W, Hu L, Luo Y, Tang M. Impact of peripherally inserted central venous catheter‐associated phlebitis in neonate guided by intracavitary electrocardiogram: A systematic review and meta‐analysis of randomised controlled trials. Int Wound J. 2023;20(4):1130‐1138. doi: 10.1111/iwj.13971
Funding information West China Hospital Clinical Research Incubation Project, Grant/Award Number: 2018HXFH042
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. González López JL, Arribi Vilela A, Fernández del Palacio E, Olivares Corral J, Benedicto Martí C, Herrera PP. Indwell times, complications and costs of open vs closed safety peripheral intravenous catheters: a randomized study. J Hosp Infect. 2014;86(2):117‐126. [DOI] [PubMed] [Google Scholar]
- 2. Ozkiraz S, Gokmen Z, Anuk Ince D, et al. Peripherally inserted central venous catheters in critically ill premature neonates. J Vasc Access. 2013;14(4):320‐324. [DOI] [PubMed] [Google Scholar]
- 3. Xiao AQ, Sun J, Zhu LH, et al. Effectiveness of intracavitary electrocardiogram‐guided peripherally inserted central catheter tip placement in premature infants: a multicentre pre‐post intervention study. Eur J Pediatr. 2020;179(3):439‐446. [DOI] [PubMed] [Google Scholar]
- 4. Rossetti F, Pittiruti M, Lamperti M, Graziano U, Celentano D, Capozzoli G. The intracavitary ECG method for positioning the tip of central venous access devices in pediatric patients: results of an Italian multicenter study. J Vasc Access. 2015;16(2):137‐143. [DOI] [PubMed] [Google Scholar]
- 5. Pittiruti M, La Greca A, Scoppettuolo G. The electrocardiographic method for positioning the tip of central venous catheters. J Vasc Access. 2011;12(4):280‐291. [DOI] [PubMed] [Google Scholar]
- 6. Oliver G, Jones M. ECG or X‐ray as the 'gold standard' for establishing PICC‐tip location? Br J Nurs. 2014;23(Suppl 19):S10‐S16. [DOI] [PubMed] [Google Scholar]
- 7. Baldinelli F, Capozzoli G, Pedrazzoli R, Marzano N. Evaluation of the correct position of peripherally inserted central catheters: anatomical landmark vs. electrocardiographic technique. J Vasc Access. 2015;16(5):394‐398. [DOI] [PubMed] [Google Scholar]
- 8. da Silva PS, Waisberg J. Induction of life‐threatening supraventricular tachycardia during central venous catheter placement: an unusual complication. J Pediatr Surg. 2010;45(8):E13‐E16. [DOI] [PubMed] [Google Scholar]
- 9. Fallouh N, McGuirk HM, Flanders SA, Chopra V. Peripherally inserted central catheter‐associated deep vein thrombosis: a narrative review. Am J Med. 2015;128(7):722‐738. [DOI] [PubMed] [Google Scholar]
- 10. Morano SG, Latagliata R, Girmenia C, et al. Catheter‐associated bloodstream infections and thrombotic risk in hematologic patients with peripherally inserted central catheters (PICC). Support Care Cancer. 2015;23(11):3289‐3295. [DOI] [PubMed] [Google Scholar]
- 11. Santacruz E, Mateo‐Lobo R, Vega‐Piñero B, et al. Colocación de catéteres centrales de inserción periférica (PICC) mediante control electrocardiográfico intracavitario (ECG‐IC) de la punta del catéter [Intracavitary electrocardiogram (IC‐ECG) guidance for peripherally inserted central catheter (PICC) placement]. Nutr Hosp. 2018;35(5):1005‐1008. [DOI] [PubMed] [Google Scholar]
- 12. Dong H, Zhu Y, Zhang X, Yin X, Liu F. Chest CT tomography vs. intracavitary electrocardiogram guidance in predicting the length of PICC placement. BMC Surg. 2022;22(1):197 Published May 19, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou LJ, Xua HZ, Xu MF, Hu Y, Lou XF. An accuracy study of the Intracavitary electrocardiogram (IC‐ECG) guided peripherally inserted central catheter tip placement among neonates. Open Med (Wars). 2017;12:125‐130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gao Y, Liu Y, Zhang H, Fang F, Song L. The safety and accuracy of ECG‐guided PICC tip position verification applied in patients with atrial fibrillation. Ther Clin Risk Manag. 2018;14:1075‐1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jeon Y, Ryu HG, Yoon SZ, Kim JH, Bahk JH. Transesophageal echocardiographic evaluation of ECG‐guided central venous catheter placement. Can J Anaesth. 2006;53(10):978‐983. [DOI] [PubMed] [Google Scholar]
- 16. Wang G, Guo L, Jiang B, Huang M, Zhang J, Qin Y. Factors influencing Intracavitary electrocardiographic P‐wave changes during central venous catheter placement. PLoS One. 2015;10(4):e0124846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu YJ, Dong L, Lou XP, et al. Evaluating ECG‐aided tip localization of peripherally inserted central catheter in patients with cancer. Int J Clin Exp Med. 2015;8(8):14127‐14129. [PMC free article] [PubMed] [Google Scholar]
- 18. Yu T, Wu L, Yuan L, et al. The diagnostic value of intracavitary electrocardiogram for verifying tip position of peripherally inserted central catheters in cancer patients: a retrospective multicenter study. J Vasc Access. 2019;20(6):636‐645. [DOI] [PubMed] [Google Scholar]
- 19. Tang BZ, Chen CH, Chen H, Ling QY. RCT of reduction in catheter‐related complications by using Intracavitary electrocardiogram‐assisted guidance in neonatal peripherally inserted central catheters placement. Sichuan Da Xue Xue Bao Yi Xue Ban. 2021;52(3):497‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhou L, Xu H, Liang J, Xu M, Yu J. Effectiveness of Intracavitary electrocardiogram guidance in peripherally inserted central catheter tip placement in neonates. J Perinat Neonatal Nurs. 2017;31(4):326‐331. [DOI] [PubMed] [Google Scholar]
- 21. Yang L, Bing X, Song L, Na C, Minghong D, Annuo L. Intracavitary electrocardiogram guidance for placement of peripherally inserted central catheters in premature infants. Medicine (Baltimore). 2019;98(50):e18368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Huang YS, Xiong XY, Sun PP, et al. Application of intracavitary electromyography in the localization of peripherally inserted central catheter tip of lower limb in premature infants. J Clin Care. 2020;19(5):29‐31. [Google Scholar]
- 23. Jiang M, Pan JZ, Lan J, Li J. The application of different P wave amplitudes in the positioning of the tip of central venous catheter in premature infants guided by intracavitary electrocardiogram through peripheral vein puncture. Chin Drug Clin Med. 2021;21(10):2. [Google Scholar]
- 24. Yang LJ, Ren Y. Analysis of clinical application of atrial electrocardiogram guided peripherally inserted central catheters tip localization in neonates. J Xinjiang Med Univ. 2021;44(12):1417‐1421. [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924‐926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. George BJ, Aban IB. An application of meta‐analysis based on DerSimonian and Laird method. J Nucl Cardiol. 2016;23(4):690‐692. [DOI] [PubMed] [Google Scholar]
- 29. Palmer TM, Sutton AJ, Peters JL, Moreno SG. Contour‐enhanced funnel plots for meta‐analysis. STATA J. 2008;8(2):242‐254. [Google Scholar]
- 30. Ling Q, Chen H, Tang M, Qu Y, Tang B. Accuracy and safety study of Intracavitary electrocardiographic guidance for peripherally inserted central catheter placement in neonates. J Perinat Neonatal Nurs. 2019;33(1):89‐95. [DOI] [PubMed] [Google Scholar]
- 31. Huang TT, Wang Y, Zhang MP, Zhuang TT. Application and effect of intracavity electrocardiography in locating the tip of peripherally inserted central catheter catheter in neonates. Electron J Pract Clin Nurs Sci. 2020;5:2096‐2479. [Google Scholar]
- 32. Yu YP, Yang XJ, Li LF, Li YQ. Application of modified intracavitary electrocardiographic guidance for peripherally inserted central catheter placement in neonates. Chin Gen Pract Nurs. 2022;19(21):2396‐2398. [Google Scholar]
- 33. Yang C, Tang ML, Luo YL, Hu L, Song JP. Accuracy and safety of intracavitary electrocardiogram jointing in vitro measurement in locating peripherally inserted central catheter tip of lower extremity vein in children: a randomized controlled trial. Chin Nurs Res. 2021;35(24):4358. [Google Scholar]
- 34. Zhang QY. Effectiveness of intracavitary electrocardiogram in the localization of the tip of peripherally inserted central catheter catheter in neonates. Med Diet Health. 2021;19(8):2096. [Google Scholar]
- 35. Zhang QY, Lin Y, Zhang QY, Chen WM. The role of intracavity electrocardiogram localization technique in neonatal peripherally inserted central catheter catheterization to improve the success rate of one‐time catheterization. Heilongjiang Trad Chin Med. 2022;2:172. [Google Scholar]
- 36. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 37. Zhang Q, Peng H, Hu L, Ren R, Peng X, Song J. Association between ABO blood group and venous thromboembolism risk in patients with peripherally inserted central catheters: a meta‐analysis and systematic review. Front Oncol. 2022;12:906427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nassaji‐Zavareh M, Ghorbani R. Peripheral intravenous catheter‐related phlebitis and related risk factors. Singapore Med J. 2007;48(8):733‐736. [PubMed] [Google Scholar]
- 39. Liu G, Hou W, Zhou C, et al. Meta‐analysis of intracavitary electrocardiogram guidance for peripherally inserted central catheter placement. J Vasc Access. 2019;20(6):577‐582. [DOI] [PubMed] [Google Scholar]
- 40. Yuan L, Li R, Meng A, et al. Superior success rate of intracavitary electrocardiogram guidance for peripherally inserted central catheter placement in patients with cancer: a randomized open‐label controlled multicenter study. PLoS One. 2017;12(3):e0171630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lee JH, Bahk JH, Ryu HG, Jung CW, Jeon Y. Comparison of the bedside central venous catheter placement techniques: landmark vs electrocardiogram guidance. Br J Anaesth. 2009;102(5):662‐666. [DOI] [PubMed] [Google Scholar]
- 42. Neubauer AP. Percutaneous central i.v. access in the neonate: experience with 535 silastic catheters. Acta Paediatr. 1995;84(7):756‐760. [DOI] [PubMed] [Google Scholar]
- 43. Oliver G, Jones M. Evaluation of an electrocardiograph‐based PICC tip verification system. Br J Nurs. 2013;22(14):S24‐S28. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Risk of bias graph
Figure S2. Forest plots of complications
Figure S3. Forest plots of catheter dwell time
Figure S4. Egger's test of included studies
Figure S5. Shear and complement results
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


