Abstract
Background
Attention-deficit/hyperactivity disorder (ADHD) in adulthood, with an estimated prevalence of 2–3 %, is associated with several challenges in daily life functioning. Still, the availability of evidence-based psychological interventions for adults with ADHD is limited. Interventions delivered over the Internet on smartphones or personal computers may help to increase the availability of and access to effective psychological interventions.
Objective
This study reports on the efficacy of a self-guided psychological Internet-delivered intervention on severity levels of ADHD symptomatology and quality of life in adults with ADHD.
Methods
Adults with a self-reported ADHD diagnosis (N = 120) were included in a randomized controlled trial with two arms: 1) self-guided Internet-delivered intervention for managing symptoms and impairments related to ADHD (n = 61); 2) online psychoeducation module (control group, n = 59). The primary clinical outcome was severity levels of ADHD as measured with the Adult ADHD Self-Report Scale. Secondary outcomes were quality of life as measured with the Adult ADHD Quality of Life scale and stress as measured with the Perceived Stress Scale. Measures were obtained at three time points: before (baseline), immediately after (8 weeks) and 3 months after the intervention. The secondary objective of the study was to explore user satisfaction with and adherence to the intervention.
Results
Linear Mixed Model analysis revealed moderate to large between group effect-size improvements on self-report measures of ADHD symptomatology (d = 0.70) and quality of life (d = 0.53). Importantly, effects were maintained at 3-month follow-up (d = 0.76 and d = 0.52). In terms of adherence, 29 % completed all modules, while 59 % completed at least five modules (out of 7). Treatment satisfaction was adequate, with n = 34 (79 %) indicating that they were very satisfied or satisfied with the intervention, and n = 37 (88 %) indicating that they would recommend the intervention to a friend.
Discussion
The study demonstrated the efficacy of a self-guided Internet-delivered intervention by showing reliable and statistically significant improvements in self-reported ADHD symptomatology and quality of life. The intervention may be suitable for better managing ADHD symptoms in primary care and as a low intensity intervention population wide.
Trial registration
ClinicalTrials.gov, Identifier NCT04726813, January 27, 2021.
Keywords: Internet, Self-help, Attention deficit hyperactivity disorder, ADHD, Randomized controlled trial, Inattention, Hyperactivity, Quality of life
Highlights
-
•
The intervention significantly reduced ADHD symptoms and increased quality of life.
-
•
Between group effect sizes were moderate to large on the primary outcome.
-
•
Within group effect sizes were large for the intervention group.
-
•
Fifty-eight percent of intervention group participants demonstrated reliable change.
-
•
The majority of the participants were satisfied with the intervention.
1. Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by pervasive symptoms of inattention and/or hyperactivity/impulsivity that persist across different situations (Edition, 2013). Longitudinal studies have shown that at least 60 % of children diagnosed with ADHD will continue to show core symptoms of ADHD into adulthood (Faraone et al., 2006; Franke et al., 2018; Kessler et al., 2005a). They also show that symptoms of hyperactivity/impulsivity decline with increasing age, but that inattentiveness and symptoms related to mood regulation, sleep problems, emotion regulation, procrastination, and frustration tolerance tend to persist or to worsen with increasing age (Yadav et al., 2021). The prevalence of ADHD in adulthood is estimated to be 2–3 %, which makes it a common disorder (Kessler et al., 2005a).
ADHD is defined as a neurodevelopmental disorder, but may not be diagnosed until adulthood (Turgay et al., 2012). Although research suggests that ADHD is more prevalent in boys than girls, in childhood, studies in adulthood have revealed an equal distribution of ADHD among both genders (Kooij et al., 2005), suggesting that women are more likely to receive a diagnosis of ADHD later in life. When diagnosed with ADHD in adulthood, psychological treatments are commonly not available, even though the disorder is associated with a wide range of challenges affecting daily life functioning (Franke et al., 2018). Executive functions, comprising functions like working memory, the ability to plan, initiate and control emotions, are commonly impaired, affecting academic and work performance as well as social function (Franke et al., 2018). Treatment options for adults with ADHD that consider these impairments should therefore be developed and made available for this group of adults.
1.1. Treatment for adults with ADHD
Pharmacological treatment is a first choice of treatment for adults with ADHD. Although effective on a group basis, it is acknowledged that many adults with ADHD experience significant ongoing impairment, even when taking ADHD medication (Advokat et al., 2011; Safren et al., 2010). Some show intolerance to medication, while others experience side-effects such as reduced sleep and appetite (Spencer et al., 1996). Due to this, non-pharmacological treatment options are increasingly demanded by adults with ADHD (Solberg et al., 2019; Vidal et al., 2013). Increased availability and use of non-pharmacological treatment options are also part of official policy (Nutt et al., 2007; Gibbins and Weiss, 2009), but so far, psychological treatments for ADHD are still not broadly available in routine clinical practice. Relatively few adults with ADHD are therefore offered psychological treatment following completion of neuropsychiatric assessment and diagnosis, even though long-term studies have underscored its importance (Kooij et al., 2019).
A small but growing number of studies provide data on the use of psychological interventions to effectively manage ADHD in adult college students (He and Antshel, 2017). In addition to encouraging results in college student samples, there is strong evidence for the use of cognitive behavioral treatment (CBT) to address symptoms and impairments associated with ADHD in the general adult population (Knouse and Safren, 2010; Knouse et al., 2017; Weiss et al., 2012). Others have examined effects of dialectical behaviour therapy (DBT) for adults with ADHD (Hesslinger et al., 2002; Hirvikoski et al., 2011). These studies have shown promising results, both when it comes to reducing ADHD related symptoms and improving life quality. The focus in these treatment approaches is to enhance executive and organizational skills, improve consequence thinking and impulse control as well as emotion regulation skills. Other interventions, like goal management training (GMT), have also been investigated as treatment options for adults with ADHD (In de Braek et al., 2017; Braek et al., 2009). As executive functions are often impaired in adults with ADHD, GMT teaches strategies for stopping unwanted behaviours, improving planning of activities and structuring intentions (In de Braek et al., 2017).
Taken together, the psychological interventions described above, provide compensatory strategies and skills for problems related to attention, executive functioning, impulse control and emotion regulation, but are often not available to adults with ADHD due to barriers such as: limited resources, lack of knowledge and qualified therapists, and other factors such as geographical distance and stigma (Solberg et al., 2019; Weiss et al., 2008).
1.2. Internet-delivered interventions for adults with ADHD
Psychological interventions delivered via the Internet on personal computers and mobile phones may help to overcome these barriers, as this mode of delivery has the potential to offer treatment outside of the traditional treatment centres, reach individuals in regions where psychological treatment is not available and offer more flexibility for the individual (Andersson, 2016). Self-guided Internet-delivered interventions, might be even more easily available to those in need, as this is a relatively easy scalable intervention, with no therapist involvement. Internet-delivered interventions might be appropriate for adults with ADHD who have insufficient response to medication, who are in need for an add-on treatment option, and/or prefer non-pharmacological treatment options. However, there is a lack of controlled studies investigating whether self-guided Internet-delivered interventions contribute to improve symptoms and impairments related to ADHD in adults, although some recent feasibility studies show promising results (Nordby et al., 2021; Nasri, 2017).
1.3. Objectives
The primary objective of this study was to evaluate the effects of a self-guided Internet-delivered psychological intervention (MyADHD) on severity levels of ADHD, quality of life and symptoms of stress. The secondary objective of the study was to explore user satisfaction with and adherence to the intervention.
We expected that participants receiving MyADHD would show significantly greater improvements in ADHD symptom levels and quality of life than participants in a psychoeducation control group. Using reliable change indices to address clinical significance of the findings, we also expected that a higher percentage of intervention group participants would show positive reliable change post-intervention in ADHD symptomatology relative to the psychoeducation control group participants.
2. Methods
2.1. Trial design
More details on the study design can be read in the published study protocol (Kenter et al., 2021). In short, this study has a randomized controlled trial (RCT) design with two arms: 1) an immediate intervention condition, where participants received direct access to the 7-week psychological Internet-delivered intervention and 2) a psychoeducation control condition. Participants in the control condition were given access to the Internet-delivered intervention after 3 months. The intervention group was followed up 3 months after they ended the intervention to evaluate the maintenance of potential intervention effects.
Power calculations were informed by the feasibility study of MyADHD (Nordby et al., 2021), providing an effect corresponding to Cohens d = 0.70 on the primary outcome measure ASRS. The sample size of the RCT was calculated by using the statistical analysis software G*power 3.1 (Faul et al., 2009, Faul et al., 2007). The minimum sample size for each group (alpha set at 0.05, power at 0.80) was identified to be 45, but at least 30 % more were recruited to hedge against expected attrition (n = 59). The minimum total sample size was set to be N = 118.
2.2. Eligibility criteria
Adults (≥18) with a self-reported ADHD diagnosis were eligible to participate in the study. Participants were screened for inclusion and exclusion criteria before randomization with open-ended questions and the Mini International Neuropsychiatric Interview (MINI), by trained psychiatric nurses and/or psychologists who were under the supervision of a specialist in clinical psychology.
Inclusion criteria were:
-
a)
Age ≥ 18
-
b)
Self-reported ADHD diagnosis with details of date, venue, and diagnosing physician/mental healthcare setting
-
c)
Ability to access and use a computer, smartphone, and the Internet
-
d)
Current self-reported problems with organizing daily activities
-
e)
Ability to comply with the intervention protocol and participate in assessment measures, as determined by investigators
-
f)
Fluency in Norwegian language, including speaking, writing, and reading
-
g)
Stability in prescribed ADHD medication for at least four weeks prior to and during the study with no changes in medication type or dosage
Exclusion criteria were:
-
h)
Current diagnosis of severe psychiatric illness such as severe depression, borderline or antisocial personality disorder, bipolar disorder
-
i)
Ongoing substance abuse
-
j)
Ongoing suicidal ideation
-
k)
Ongoing engagement in another psychological treatment
2.3. Participant recruitment and randomization
Recruitment of participants took place in March 2021 through the social media pages from the national ADHD association. Prospective participants were directed to the study website to learn more about the study and, if interested, were asked to complete a pre-screener via a secure online portal. Eligible participants were then invited to participate in a further eligibility assessment through a telephone call by a psychiatric nurse or psychologist.
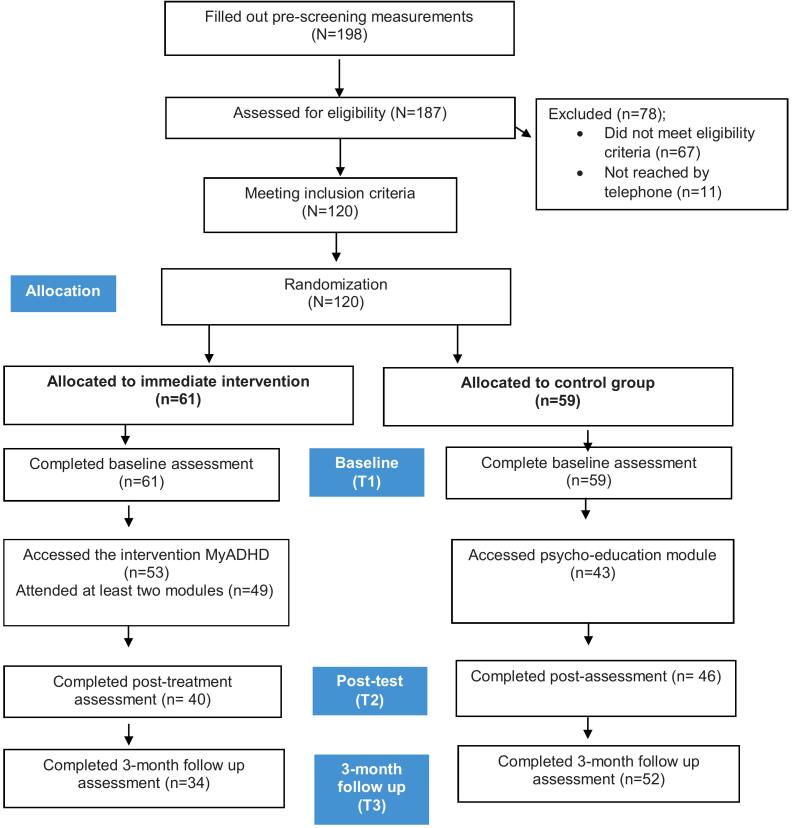
A total of 187 individuals were assessed by telephone of eligibility. Of these, 120 participants fulfilled all eligibility criteria and were randomized with sealed envelopes to one of the two study arms. Randomization was performed by the clinician who performed the telephone interview. A detailed description of the participant flow is shown in Fig. 1.
Fig. 1.
CONSORT flow diagram showing flow of participants though the trial.
Sixty-seven participants were excluded after the telephone interview due to comorbidities, unstable medication doses or ongoing involvement in other psychological treatment. By accident, one extra participant was assigned to the intervention group. This, however, was discovered during the analysis phase when inclusion for the study was ended. Therefore, we had an unequal number of participants in the two groups.
Participants allocated to the MyADHD intervention received immediate access to the intervention and could log in to the platform with BankID (level 4 protection). If they did not log on to the platform within two days after allocation, they received a reminder SMS. Twenty weeks after pre-assessments, control group participants received access to the intervention.
2.4. Measures
All outcome measures were based on self-report questionnaires that the participants filled out via an online secure platform.
2.4.1. Primary outcome measure
2.4.1.1. The Adult ADHD Self-Rating Scale (ASRS)
The 18-item Adult ADHD Self-Rating Scale (ASRS) is the official screening instrument for key ADHD symptoms in adults with ADHD of the World Health Organization (WHO) (Kessler et al., 2005b). One part of the scale assesses symptoms of inattention (9 questions), the other part assesses symptoms of hyperactivity/impulsivity (9 questions). The response type consists of a 5-point Likert scale with options “Never” (0), “Rarely” (1), “Sometimes” (2), “Often” (3) or “Very Often” (4) giving the scale a total score of 72 and 36 for each of the two subscales. Test–retest reliability of the Norwegian translation of ASRS is reported to be 0.88 (Kornør and Hysing, 2011). In our sample, Cronbach's alpha was 0.85.
2.4.2. Secondary outcome measures
2.4.2.1. Adult ADHD Quality of Life Measure (AAQol)
The AAQoL has 29 items designed to assess health related quality of life during the past two weeks among adults with ADHD (Gjervan et al., 2019). Each item is rated by participants on a five-point Likert scale from ‘Not at all/Never’ (1) to ‘Extremely/Very Often’ (Gjervan and Nordahl, 2010). The AAQoL yields a total score and four subscale scores: Life Productivity, Psychological Health, Life Outlook, and Relationships. Total and subscale scores are derived by reversing item scores for negatively worded items, then transforming all item scores to a 0–100 point scale. Item scores are then summed and divided by item count to generate subscale and total scores. A higher score indicates higher quality of life. The internal consistency of the scale in our sample was adequate (0.81 for overall, 0.75–0.91 for subscales).
2.4.2.2. The perceived stress scale (PSS)
The Perceived Stress Scale (PSS) is a widely used psychological instrument for measuring stress (Cohen et al., 1994). Items were designed to measure stress and how the respondents find their lives during the last week. The PSS version used in this study has 10 items with response alternatives 0 (never) to 4 (very often). Cronbach's alpha in our sample was 0.81.
2.4.3. User satisfaction and adherence
User satisfaction was measured by two open-end questions and three multiple choice questions derived from the Client Satisfaction Questionnaire (CSQ-8):
-
1.
Were there parts of the modules that you experienced as helpful and/or supportive?
-
2.
Were there parts of the modules that you experienced as complicated and/or unhelpful?
-
3.
Would you recommend this intervention to a friend or a family member with similar difficulties as yourself? On a scale from 1 to 5
-
4.
To what extent has the intervention met your needs? On a scale from 1 to 5
-
5.
How satisfied are you with the intervention? On a scale from 1 to 5
2.4.4. Adherence
Module completion was the main outcome for measuring adherence. A module was considered as completed if the participant had clicked through all pages of the module, and spent a minimum of 10 min on a module to ensure exposure to the material.
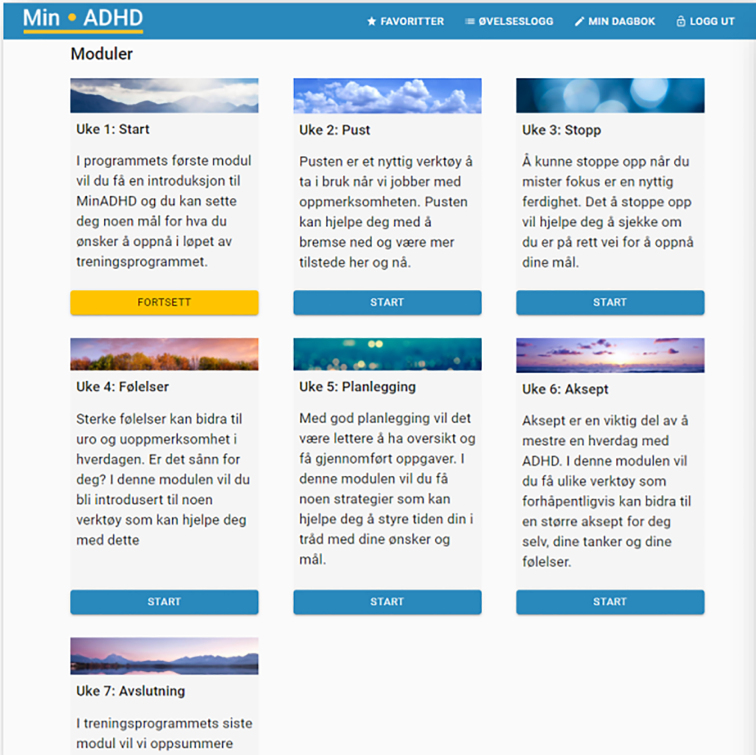
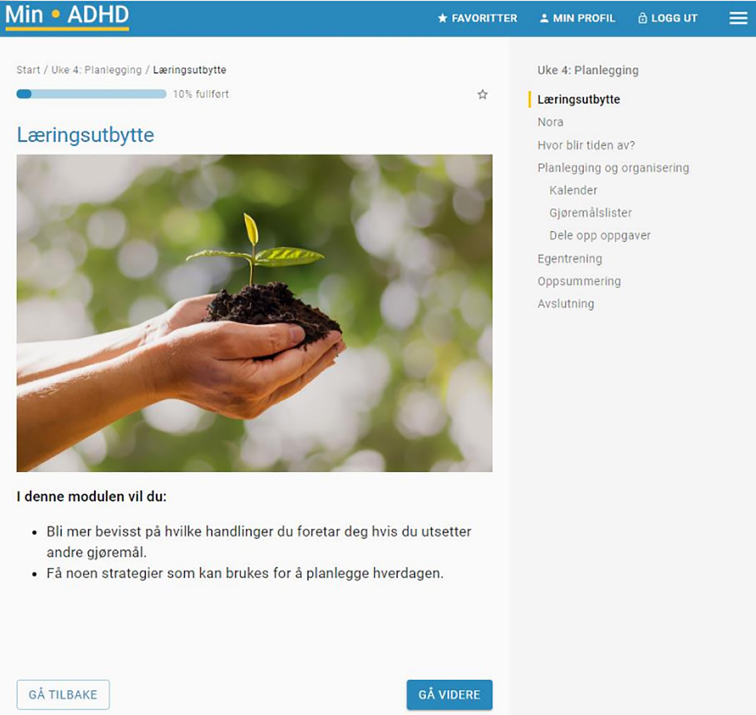
2.5. MyADHD intervention
The intervention was delivered via an online secure portal, which was accessible on smartphones, tablets, laptops and personal computers. The intervention was a short-term, structured self-guided intervention with modified elements from CBT, DBT and GMT to target specific challenges experienced by adults with ADHD. For more information on the development of MyADHD we refer to the research protocol by Kenter et al. (2021) and subsequent studies by Flobak et al. (2021), and Nordby et al. (2021). In short, the intervention consists of seven online modules (goalsetting; awareness training; inhibition training; emotional regulation; planning and organizing daily life; self-acceptance; and making a plan for the future) that were released weekly for the intervention group participants. The main goals of the intervention were to help participants to obtain improved functioning in daily life activities; offer strategies associated with stress reduction, reduce inattention, and improve quality of life. Each module included psychoeducation alongside text, audio and video material instructing participants in the use of specific techniques. Additionally, modules included case vignettes and lived-experience videos serving to clarify important treatment principles and help participants make connections between the material and their own experiences (see supplementary material). Automatic reminders were sent when a participant did not log on within one day after release of a new module, or the participant did not finish a module within 4 days. Homework was given after modules 2–6, where the participants were asked to continue training in everyday situations on the newly learned skills and to log situations in which the participants succeeded or failed. Homework was intended to provide a structured opportunity to implement the learned strategies in daily life. Table 1 gives an overview of the modules of intervention, their rationale and content.
Table 1.
Overview of the intervention in Arm I.
| Modulea | Rationale, content and coping techniques |
|---|---|
| 1. Start module | This module gives an introduction to the program. Introduction to key elements such as goal setting and homework exercises. |
| 2. Mindful awareness | Inattention is a core symptom of ADHD. In this module, participants are given information about different aspect of attention and concentration and how to cope with impairments. In this module the participants start training on mindful awareness (“being here and now”) by focusing on their breathing. Coping techniques in the module are focused breathing, thoughtful breathing and attentive walking. The module incorporates elements from DBT, utilizing therapeutic techniques, concepts and approaches. |
| 3. Inhibition training | Impulsivity and loss of impulse control are common among adults with ADHD. This module consists of exercises focussing on impulse control and goal oriented-directed behaviour (stop, observe, proceed, check) which the goal to increase attentive awareness in routine activities. The module employed the principles and methods of GMT. |
| 4. Emotional regulation | Emotional instability and brief recurrent states of feelings are common in ADHD. In this module, participants are first informed about modern theories of emotion (primary emotions, relationship cognition-emotion and emotion-behaviour) and then presented exercises to improve emotional analysis (emotions record, emotion diary) and emotional regulation. Based on DBT. |
| 5. Planning and organizing daily life | Problems with planning an organizing sequential behaviour often result in situations where adults with ADHD do several different things at the same time, feel pressurized, and end up finishing none of their planned tasks. Adults with ADHD often feel that this behaviour is a result of emotional stress and experience this deficit as stressful in itself. This module presents stress management techniques, how to handle a tendency towards procrastination, breaking down large tasks. Based on CBT. |
| 6. Self-acceptance | In this module the focus is on accepting what one cannot change and to be kind to oneself. Psychoeducation about understanding how actions are separate from ones qualities, identifying and acknowledging strengths, practice forgiveness. The goal is to enhance self-compassion. Based on DBT. |
| 7. Summary and road ahead | Summary of all the modules and planning for the future |
Features common across all modules: automatic reminders, (homework) exercises, downloadable hand-outs, weekly questionnaires, progress graphs, lived-experience videos, audio files.
2.6. Psychoeducation control
Participants in the control group were assigned to a psychoeducation module, which was accessible through the secure platform. Psychoeducation is generally recommended in the treatment of adult ADHD, therefore this was chosen as a control condition.
The module consisted of text-based information that aimed to educate individuals about ADHD, including risk factors, symptoms, and management strategies. Although the same coping strategies as in the intervention group were covered, the control module lacked exercises, videos, and audio files. The topics covered in the psychoeducation included: Understanding ADHD; Behaviour Management; Problem Solving; Emotion Regulation; and Self-Acceptance. The module also addressed common misunderstandings and negative stereotypes surrounding ADHD and aimed to help individuals to develop a deeper understanding of their own experiences with the condition.
2.7. Statistical methods
Descriptive statistics (Chi-square and t-tests) were used to analyse sociodemographic and clinical variables of the two groups at baseline. Linear Mixed Models (LMM) were used to analyse change in clinical outcomes from pre-assessment to post- and follow-up assessment, with IBM SPSS 26 statistical software (SPSS I, 2018). Caused by the two intervals, time was declared as a factor with two levels. The model was a random intercept fixed slope model. Treatment differences over time were represented as a group x time interaction. All participants' data were included, irrespective of treatment compliance under the assumption of missing at random (Enders, 2010). The effect of the Internet-delivered intervention on the clinical outcome measures was examined separately for each measure. The magnitude of the treatment effect within and between the two groups was calculated using the Cohen d statistic (Cohen, 2013). Cohen describes an effect size of 0.2 as small, 0.5 as medium, and 0.8 as large. Additionally, reliable change was assessed using the Jacobson and Truax (Jacobson and Truax, 1992) reliable change criteria. Positive reliable change was defined when having a reliable change index (RCI) > 1.96 on the ASRS, while deterioration was defined as RCI < −1.96. Logistic regression was used to examine study dropout.
3. Results
3.1. Baseline evaluation
Table 2 presents the baseline characteristics of the participants and between-group comparisons. The mean age of all participants was 40.9 (SD = 10.6, range = 20–77 years). The majority were females (n = 96, 80.0 %), had a university or college degree (n = 65, 54.2 %) and were engaged in full-time paid work or were students (n = 75, 62.5 %). In total, 100 participants (83.3 %) were taking medication for their ADHD, of which 87 (72.5 %) on a daily basis. None of the participants engaged in another treatment and all were on stable dosages of ADHD medication. The average baseline score on the ASRS was 48.7 (SD = 9.5). There were no significant between-group differences in demographic variables, nor were there significant between-group differences on any of the outcome measures (p's > 0.27). A large part of the sample (95 %) was diagnosed with ADHD in adulthood, with a mean age of diagnosis of 34.9 years (SD = 11.1; range: 3–66), 50.4 % were diagnosed in the past three years and only 6 (5 %) were diagnosed in childhood.
Table 2.
Sample characteristics at baseline.
| Total |
Intervention |
Control |
Statistics |
|
|---|---|---|---|---|
| N = 120 | n = 61 | n = 59 | (t-test or χ2) | |
| Demographic characteristics | ||||
| Mean age (SD) | 40.9 (10.6) | 40.1 (10.0) | 41.2 (11.2) | t(118) = −0.31; p = .76 |
| Gender (%) | ||||
| Male | 24 (20.0) | 15 (25 %) | 9 (15 %) | χ2 (1) = 2.73; p = .26 |
| Female | 96 (80.0) | 45 (75 %) | 50 (85 %) | |
| Highest education (%) | ||||
| Elementary school | 7 (5.8) | 6 (10 %) | 1 (2 %) | χ2 (2) = 4.63; p = .10 |
| High school | 48 (40.0) | 26 (43 %) | 22 (37 %) | |
| College/university | 65 (54.2) | 29 (47 %) | 36 (61 %) | |
| Employment | ||||
| Working/employed/studying | 75 (62.5) | 34 (56 %) | 41 (70 %) | χ2 (3) = 3.31; p = .35 |
| Sick leave | 22 (18.3) | 13 (21 %) | 9 (15 %) | |
| Disability pension | 18 (15.0) | 12 (20 %) | 7 (12 %) | |
| Unemployed | 4 (3.3) | 2 (3 %) | 2 (3 %) | |
| Diagnosis and treatment variables | ||||
| ADHD medication | ||||
| Daily | 87 (72.5) | 43 (71 %) | 44 (75 %) | χ2 (4) = 4.11; p = .39 |
| Weekly | 8 (6.7) | 2 (3 %) | 6 (10 %) | |
| Monthly | 2 (1.7) | 1 (2 %) | 1 (2 %) | |
| Few times a year | 3 (2.5) | 2 (3 %) | 1 (2 %) | |
| No medication | 20 (16.7) | 13 (21 %) | 7 (11 %) | |
| Age of diagnosis (SD) | 34.9 (11.1) | 34.5 (11.7) | 35.4 (10.6) | t(118) = −0.41; p = .68 |
| Baseline scores | ||||
| ASRS total score (SD) | 48.7 (9.5) | 49.2 (10.0) | 48.1 (9.1) | t(118) = 0.65; p = .52 |
| ASRS Inattention (SD) | 26.0 (5.1) | 26.0 (5.1) | 26.3 (5.1) | t(118) = −0.07; p = .94 |
| ASRS Hyperactivity (SD) | 22.7 (5.9) | 23.3 (6.3) | 22.1 (5.6) | t(118) = 0.37; p = .27 |
| AAQoL total score (SD) | 47.3 (12.7) | 47.8 (13.1) | 46.8 (12.3) | t(118) = 0.45; p = .66 |
| PSS-14 total score (SD) | 31.4 (3.6) | 31.3 (3.7) | 31.5 (3.5) | t(118) = −0.27; p = .79 |
Note. SD = standard deviation; ASRS = Adult ADHD Self-report Scale; AAQoL = Adult ADHD Qualitity of Life scale: PSS-14 = Perceived stress scale.
3.2. Drop-out analysis and adherence to the intervention
Of the 120 randomized participants, 86 (71.7 %) completed post-assessment and 86 (71.7 %) completed follow-up assessments (see Fig. 1.). The analyses assessing study drop-out for the post and 3-month follow up questionnaires showed that there were significant differences in terms of gender (males > females, p = .01) and higher ASRS score at pre-treatment (p = .01) in the participants who did compared to those who did not fill out post-assessments. In addition, participants who did not fill out the post-assessment completed a significantly lower number of modules (p = .03). Moreover, participants who did not fill out the post-assessment were more often in the intervention group (p = .01).
On average, intervention group participants completed 4.52 modules (SD = 2.3) out of 7. Among the intervention drop-outs, 8 participants never started the program, and 12 completed only the first module. Completion rates were based on log-data.
3.3. Clinical outcomes
Table 3 presents the observed and estimated means, the standard deviations and confidence intervals and between group effect sizes, while Table 4 presents the LMM results. The predominant patterns that emerged from the results were statistically significant group x time effects on the ASRS scores from pre to post and pre to follow up (p < .001). This was also true for both the inattention and hyperactivity subscales (p < .001). There were moderate to large reductions in ASRS scores from pre-treatment to post on the ASRS (within group d = 0.80) and from pre to follow up (within group d = 0.67).
Table 3.
Estimated marginal means across time-points and by group.
| Outcome | Time-point | Estimated |
Within group ES, 95 % CI |
Between group ES, 95 % CI |
|||
|---|---|---|---|---|---|---|---|
| Intervention |
Control |
Pre-Post Pre-Fu |
|||||
| M | CI | M | CI | ||||
| ASRS | Pre-treatment | 49.2 | 46.8, 51.7 | 48.1 | 46.8, 51.7 | ||
| Post-treatment | 42.4 | 39.7, 45.0 | 48.1 | 45.5, 50.7 | 0.80 (0.34–1.20) | 0.70 (0.43–0.96) | |
| Follow-up | 42.6 | 39.9, 45.3 | 48.8 | 46.3, 51.4 | 0.77 (0.24–1.10) | 0.76 (0.48–1.02) | |
| AAQoL | Pre-treatment | 47.8 | 44.6, 51.1 | 46.8 | 43.5, 50.1 | ||
| Post-treatment | 55.1 | 51.0, 59.1 | 45.8 | 42.3, 49.4 | 0.60 (0.17–1.02) | 0.53 (0.34–0.83) | |
| Follow-up | 50.7 | 46.0, 55.5 | 44.7 | 41.3, 48.2 | 0.23 (−0.29–0.74) | 0.52 (0.32–0.84) | |
| PSS-14 | Pre-treatment | 31.3 | 30.5, 32,4 | 31.5 | 30.5, 32.4 | ||
| Post-treatment | 28.3 | 27.0, 29.6 | 29.4 | 28.32, 30.5 | 0.2 (−0.24–0.65) | ||
Note. SD = standard deviation; ES = effect size; Fu = follow-up. ASRS = Adult ADHD Self-Report Scale; AAQOL = Adult ADHD Quality of Life; PSS-14 = Perceived Stress Scale. Estimated marginal means in the intervention-arm at 8 and 20 weeks are based on linear mixed models.
Table 4.
Results from linear mixed models.
| Baseline Level |
Pre-Post |
Pre-FU |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| b | p | CI | b | p | CI | b | p | CI | |
| ASRS | |||||||||
| Controls | 48.10 | <.001 | 45.63, 50.57 | −0.01 | .992 | −1.67, 1.65 | 0.74 | .360 | −0.85, 2.32 |
| Intervention (×time)a | 1.13 | .520 | −2.33, 4.59 | −6.85 | <.001 | −9.29, -4.42 | −7.33 | <.001 | −9.80, -4.86 |
| Inattention | |||||||||
| Controls | 26.03 | <.001 | 24.73, 27.34 | −0.58 | .270 | −1.61, 0.45 | 0.064 | .898 | −0.92, 1.05 |
| Intervention (×time)a | −0.07 | .943 | −1.90, 1.77 | −3.56 | <.001 | −5.07, -2.05 | −3.80 | <.001 | −5.32, -2.26 |
| Hyperactivity | |||||||||
| Controls | 22.07 | <.001 | 20.53, 23.60 | 0.58 | .220 | −0.35, 1.526 | 0.69 | .129 | −0.20, 1.59 |
| Intervention (×time)a | 1.19 | .275 | −0.96, 3.35 | −3.24 | <.001 | −4.61, -1.85 | −3.58 | <.001 | −4.98, -2.18 |
| AAQoL | |||||||||
| Controls | 46.79 | <.001 | 43.49, 50.09 | −0.94 | .538 | −3.98, 2.08 | −2.03 | 1.67 | −4.92, 0.85 |
| Intervention (×time)a | 1.04 | .658 | −3.59, 5.66 | 8.19 | .001 | 3.48, 12.9 | 4.94 | .066 | −0.33, 10.2 |
| PSS-14 | |||||||||
| Controls | 31.48 | <.001 | 30.52, 32.43 | −2.08 | .001 | −3.28, -0.87 | |||
| Intervention (×time)a | −0.14 | .836 | −1.48, 1.20 | −1.00 | .290 | −2.85, 0.86 | |||
Note. Fu = follow-up. ASRS = Adult ADHD Self-Report Scale; AAQOL = Adult ADHD Quality of Life; PSS-14 = Perceived Stress Scale.
Baseline level: Intervention group differences; Pre-Post/Pre-FU changes: Intervention group × time effects.
For the quality of life measure, the analysis showed statistically significant time effects from pre to post (p = .001 overall, 0.004–0.025 for subscales), but not from post to follow up (p = .07 overall). Only on the relation subscale of the AAQoL we found a significant effect at follow up (p = .03). Within group effect sizes on the AAQoL scale ranged from moderate (d = 0.60) at post to small (d = 0.23) at follow up.
No statically significant effects were found for the PSS-14 scale (p = .86).
3.4. Reliable change
A total of 45 % (n = 18) of the participants who completed post-test assessments in the intervention group showed Positive reliable change (RCI > 1.96) on the total ASRS, whereas 7.5 % (n = 3) showed a deterioration (RCI < −1.96). For the control group participants, 10.8 % (n = 5) showed a positive reliable change (RCI > 1.96) on the total ASRS at post-test, whereas 15.2 % (n = 7) showed a deterioration (RCI < −1.96). Results showed significant between group differences in terms of clinically significant change on the ASRS (χ2 = 12.72, p = .001). The remaining participants showed no clinically significant change (RCI between −1.96 and 1.96).
At 3-month follow up, a total of n = 20 (58.8 %) showed positive reliable change in the intervention group, whilst a total of n = 7 (15.2 %) in the control group showed positive reliable change (χ2 = 19.64, p = .00). None showed reliable deterioration in the intervention group at follow-up (total n = 34), while 10 (19.2 %) showed deterioration from pre to 3-month follow up in the control group (χ2 = 7.40, p = .007) (Table 5).
Table 5.
Number of participants reporting reliable change and reliable deterioration.
| Group | Post-treatment |
3-month follow up |
||
|---|---|---|---|---|
| Positive reliable change n (%) |
Reliable deterioration n (%) |
Positive reliable change n % |
Reliable deterioration n % |
|
| MyADHD | 18 (45.0) | 3 (7.5) | 20 (58.8) | 0 (0) |
| Control | 5 (10.8) | 7 (15.2) | 7 (15.2) | 10 (19.2) |
Note. Outcomes are based on observed data only.
3.5. Treatment satisfaction
Of the participants providing feedback about the intervention (n = 43), 34 (79.1 %) indicated that they were very satisfied or satisfied with the intervention, 37 (88.1 %) indicated that they would recommend the intervention to a friend.
4. Discussion
4.1. Principal findings and comparisons to prior work
The results demonstrated the efficacy of a self-guided Internet-delivered intervention (MyADHD). The intervention group showed significantly reduced ADHD related symptoms and increased quality of life at post treatment, with moderate to large effect sizes. Effects on ADHD symptoms were maintained at 3-month follow-up. Furthermore, 45 % of the participants in the invention group demonstrated reliable change at post treatment and 58 % at follow-up, indicating that the statistical significance represents a clinically relevant change in ADHD symptomatology. Most participants were satisfied with the intervention and adherence to the intervention was satisfactory, considering that this was an entirely self-guided intervention.
The results in our study are consistent to the findings from our previous uncontrolled study, with a similar reduction in ADHD symptomatology and increase in quality of life, and similar engagement and satisfaction with the intervention (Nordby et al., 2022). The reduction in severity level of ADHD symptoms are also comparable with results in other self-guided Internet-delivered interventions for adults with ADHD (Moëll et al., 2015; Pettersson et al., 2017). As for clinically significant improvement, 45 %- 58 % who completed post- and follow-up assessments showed positive reliable change. Considering that the diagnostic criteria are defined by the persistence of ADHD symptomatology, a larger improvement in ADHD symptoms was not to be expected. Notably, reliable deterioration occurred in five participants. However, on the self-report scale none had reported unwanted negative effects of the intervention (Rozental et al., 2018). Although we expected a decrease in stress levels for the participants in our intervention group, this was not observed in the results.
On average, participants in our intervention group completed 5 out of 7 modules. These completion rates are favourable compared to results in other studies on self-guided, Internet-delivered interventions, although it may be related to the fairly broad definition of completion used in the present study. A meta-analysis on self-guided Internet-delivered interventions for depression have found that 74 % of the participants do not adhere to the treatment (Richards and Richardson, 2012), and that 70 % of the participants drop out before completing 75 % of the modules (Karyotaki et al., 2015). A study that examined a self-guided Internet-delivered intervention for adults with ADHD found that 77 % of the participants did not complete the intervention (Pettersson et al., 2017). Thus, adherence rates were better in our intervention compared to previous studies on ADHD, and studies on self-guided interventions for other mental health disorders. This may be explained by the fact that participants in the previous mentioned studies (Moëll et al., 2015; Pettersson et al., 2017) were recruited from psychiatric outpatient clinics, while our participants were not enrolled in any form of treatment in outpatients' clinics. Our participants also self-assigned to the study and may potentially be high(er) functioning and more motivated, even though clinical scores at baseline were at a similar level as the scores reported in other studies. Our sample's mean baseline scores are also similar to a Norwegian study including a clinically validated patient sample (Brevik et al., 2020).
Although self-guided Internet-delivered interventions have advantages over regular interventions for this group, e.g., by providing the possibility to work with the program in their home environment, at their own convenience, taking short breaks to better fit for their attentional style, repeat and retain content of the text/videos, we acknowledge that such interventions might not suite all adults with ADHD. This is reflected in the module completion rates in our sample, were participants completed 5 of 7 modules of the intervention on average, suggesting that strategies designed to increase adherence (e.g., adding guidance) could be an important improvement of the intervention. Adherence rates also underscore the importance of having a wider selection of (online and offline) psychological interventions available for adults with ADHD.
4.2. Strengths and limitations
Our results showed that adults with ADHD can benefit from a self-guided Internet-delivered psychological intervention. This has not previously been shown in an RCT for this group of adults, although the relevance of conducting a controlled study on Internet-delivered psychological intervention for adults with ADHD is high for several reasons. Firstly, as demonstrated previously, core symptoms of ADHD affect many aspects of daily life, but the availability of psychological support is limited. Any intervention contributing to more people receiving better care for managing their symptoms against relatively low costs should be helpful. A final strength is the delivery over the Internet, which has the potential to reach people in need of psychological help across a larger geographical area.
It is important to note the limitations of the current study. One major limitation is the reliance on solely self-reported outcome measures, which can be affected by biases such as recall and short-term confounders like mood fluctuations (Brevik et al., 2020; Collett et al., 2003) and sleep difficulties (Lundervold et al., 2011). Additionally, the validity of the self-reported ADHD diagnosis was not formally confirmed through diagnostic interviews or tests, although the date, venue, and mental health institution where the diagnosis was made were reported and checked. The purpose of the study was to make the intervention accessible to a large group of individuals with ADHD, so a full clinical assessment for each participant was not conducted and self-reported diagnoses were used instead. Despite the limitations associated with self-reported measures, the results are encouraging as all participants met the cut-off score of 17 points on the ASRS rating scale and reported common difficulties associated with ADHD symptoms in daily life.
Second, this study excluded those with personality disorders, current substance use, suicidal ideation, and other severe psychiatric problems although these adults represent a significant proportion of the population of adults with ADHD. The exclusion of individuals with additional psychiatric disorders thus affects the generalizability of the findings. Nevertheless, the choice was made to exclude those with severe psychiatric illnesses due to the lack of support from clinicians in the present study.
Third, a large proportion of the participants in both groups had ongoing medication for their ADHD symptoms, all with stable medication doses and dosage regiments. It could nevertheless have affected the findings of the study. The use of medication could interact with the intervention, potentially altering its effectiveness. This makes it difficult to determine the specific impact of this psychological intervention. Heterogeneity of medication use could also represent a limitation as individuals in the study population may be taking different medications or doses during the intervention program. In the study, we attempted to account for medication use by requiring participants to maintain a stable medication regimen throughout the entire duration of the study.
A fourth limitation of this study is inclusion of a sample of convenience, which may inadequately represent the full population of adults with ADHD. There is also an unequal gender balance in our study. Epidemiological studies indicate an equal gender distribution for ADHD in adulthood (Kessler et al., 2005a; Kooij et al., 2005), but not in childhood. Females tend to be diagnosed with ADHD later in life. In our sample most participants have been diagnosed with ADHD in the past few years, which means that the majority received their diagnosis as adults. As psychological support for ADHD is scarce for adults, these females might have reached out to participate in our study. Additionally, the gender imbalance in our study may be due to recruitment bias, with women being more likely to participate in research studies for social, cultural, and other reasons. Women may also be more likely to seek help for their ADHD symptoms compared to men (Rucklidge, 2010). Overall, the gender distribution in studies on adults with ADHD may be influenced by a combination of these factors, and more research is needed to better understand the reasons for gender imbalance in participation rates.
Fifth, the drop-out rate was relatively high over time, with 29 % dropout at post-test and follow-up. Although missing values were accounted for in the estimated models under the Missing At Random assumption, we cannot be sure if missing over time was at random. This difference is not empirical testable and can only be analysed with sensitivity analyses with missingness included into the statistical model, for example the Diggle-Kenward and pattern-mixture models (Enders, 2010). These models relate missingness to the level and change in the process in focus, either to the observed variables or to the intercept and slope factors. However, these models assume very strict statistical assumptions and we decided not to explore these models.
In light of these limitations, the study results should be interpreted with caution and more studies are needed to verify the generalisability of the results, e.g., to individuals with comorbid psychiatric and somatic disorders.
4.3. Conclusion and implications
Self-guided Internet-delivered psychological interventions are a feasible way to support adults with ADHD. Results from the study show that a self-guided psychological intervention significantly reduced ADHD symptoms and increased ADHD related quality of life with moderate to large between group effect sizes in comparison with psychoeducation alone. The intervention can be a promising low intensity treatment for adults with ADHD in primary care settings or as a low intensity intervention population wide, where self-guided interventions can serve as a first low threshold step in a stepped care model, with easy access to the intervention and the possibility to step up to more intensive care if needed However, the core symptoms of ADHD can interfere with self-guided treatment formats and these formats might not be suitable for all. Adding therapist guidance to those not benefitting from or not adhering to the self-guided format and examining the effects of Internet-delivered interventions in outpatient samples should be important research topics for future research. Future research should also focus on examining the effects of Internet-delivered psychological interventions in a more diverse sample of adults with ADHD in order to make the results generalizable to a wider part of the population of adults with ADHD.
CRediT authorship contribution statement
RK is the chief investigator in this study, led the study design and study execution, ethics application and drafted the manuscript. RG contributed to the statistical analyses and interpretation of outcomes. AJL contributed as the domain expert in the ADHD case, to the intervention and the psychoeducation control and to the drafting of the manuscript. TN contributed as the head of INTROMAT, to the study design, and drafting of the manuscript. All authors critically reviewed and approved the final manuscript.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: RK and AJL have designed and created the Internet-delivered intervention, but derive no economic profit from it.
Acknowledgments
Acknowledgements
The authors would like to acknowledge the experts with ADHD focus group and lived-experience group participants who contributed to the development of the intervention and videos. We also want to acknowledge Eivind Flobak, Frode Guribye and Yavuz Inal for contributing with IT-functionalities and design of the platform for the intervention and videos, and Emilie Sektnan Nordby, Anne Synnøve Samdal Thomassen and Adrian Schønning for their contribution to the project.
Financing and insurance
This RCT is financed by NRC through INTROMAT (NFR project number 259293). Haukeland University Hospital is project owner and UiB is partner in the project. IT development in the project is done by the INTROMAT consortium by business and research partners.
Ethics approval and consent to participate
This study was reviewed and approved by Norwegian Regional Committee for Medical and Health Research Ethics, REC South East #203804. The participants provided their written informed consent to participate in this study.
Consent for publication
Consent for publication was signed by all participants.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2023.100614.
Appendix A. Supplementary data
Still from the video in the intervention.
Interventions dashboard.
Screenshot of the intervention.
References
- Advokat C., Lane S.M., Luo C. College students with and without ADHD: comparison of self-report of medication usage, study habits, and academic achievement. J. Atten. Disord. 2011;15(8):656–666. doi: 10.1177/1087054710371168. [DOI] [PubMed] [Google Scholar]
- Andersson G. Internet-delivered psychological treatments. Annu. Rev. Clin. Psychol. 2016;12:157–179. doi: 10.1146/annurev-clinpsy-021815-093006. [DOI] [PubMed] [Google Scholar]
- Braek D., Dijkstra J., Ponds R., Jolles J. Attention dysfunction and ADHD in adults: determinants and interventions Maastricht. Neuropsych Publishers; 2009. Goal management training in adults with Attention-Deficit/Hyperactivity Disorder (ADHD): an intervention study; pp. 115–130. [Google Scholar]
- Brevik E.J., Lundervold A.J., Haavik J., Posserud M.B. Validity and accuracy of the adult attention-Deficit/Hyperactivity disorder (ADHD) self-report scale (ASRS) and the wender Utah rating scale (WURS) symptom checklists in discriminating between adults with and without ADHD. Brain Behav. 2020;10(6) doi: 10.1002/brb3.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Routledge; 2013. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. Measuring Stress: A Guide for Health and Social Scientists. 10(2) 1994. Perceived stress scale; pp. 1–2. [Google Scholar]
- Collett B.R., Ohan J.L., Myers K.M. Ten-year review of rating scales. V: scales assessing attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2003;42(9):1015–1037. doi: 10.1097/01.CHI.0000070245.24125.B6. [DOI] [PubMed] [Google Scholar]
- Edition F. Diagnostic and statistical manual of mental disorders. Am. Psychiatric. Assoc. 2013;21(21):591–643. [Google Scholar]
- Enders C. Guilford Press; New York: 2010. Applied Missing Data Analysis (Methodology in the Social Sciences) [Google Scholar]
- Faraone S.V., Biederman J., Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol. Med. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.-G., Buchner A. G* power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Buchner A., Lang A.-G. Statistical power analyses using G* power 3.1: tests for correlation and regression analyses. Behav. Res. Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Flobak E., Nordby E.S., Guribye F., Kenter R., Nordgreen T., Lundervold A.J. Designing videos with and for adults with ADHD for an online intervention: participatory design study and thematic analysis of evaluation. JMIR Ment. Health. 2021;8(9) doi: 10.2196/30292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke B., Michelini G., Asherson P., Banaschewski T., Bilbow A., Buitelaar J.K., et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur. Neuropsychopharmacol. 2018;28(10):1059–1088. doi: 10.1016/j.euroneuro.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbins C., Weiss M. Clinical recommendations in current practice guidelines for diagnosis and treatment of ADHD in adults. Curr. Atten. Disord. Rep. 2009;1(3):116–122. doi: 10.1007/s11920-007-0055-1. [DOI] [PubMed] [Google Scholar]
- Gjervan B., Nordahl H.M. The adult ADHD quality of life questionnaire (AAQoL): a new disease specific measure for assessment of ADHD. Nord. Psychol. 2010;62(1):24. [Google Scholar]
- Gjervan B., Torgersen T., Hjemdal O. The norwegian translation of the adult attention-deficit/hyperactivity disorder quality of life scale: validation and assessment of QoL in 313 adults with ADHD. J. Atten. Disord. 2019;23(9):931–939. doi: 10.1177/1087054716640087. [DOI] [PubMed] [Google Scholar]
- He J.A., Antshel K.M. Cognitive behavioral therapy for attention-deficit/hyperactivity disorder in college students: a review of the literature. Cogn. Behav. Pract. 2017;24(2):152–173. [Google Scholar]
- Hesslinger B., Tebartz van Elst L., Nyberg E., Dykierek P., Richter H., Berner M., et al. Psychotherapy of attention deficit hyperactivity disorder in adults. Eur. Arch. Psychiatry Clin. Neurosci. 2002;252(4):177–184. doi: 10.1007/s00406-002-0379-0. [DOI] [PubMed] [Google Scholar]
- Hirvikoski T., Waaler E., Alfredsson J., Pihlgren C., Holmström A., Johnson A., et al. Reduced ADHD symptoms in adults with ADHD after structured skills training group: results from a randomized controlled trial. Behav. Res. Ther. 2011;49(3):175–185. doi: 10.1016/j.brat.2011.01.001. [DOI] [PubMed] [Google Scholar]
- In de Braek D.M., Dijkstra J.B., Ponds R.W., Jolles J. Goal management training in adults with ADHD: an intervention study. J. Atten. Disord. 2017;21(13):1130–1137. doi: 10.1177/1087054712468052. [DOI] [PubMed] [Google Scholar]
- Jacobson N.S., Truax P. 1992. Clinical Significance: A Statistical Approach to Defining Meaningful Change in Psychotherapy Research. [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Kleiboer A., Smit F., Turner D.T., Pastor A.M., Andersson G., et al. Predictors of treatment dropout in self-guided web-based interventions for depression: an ‘individual patient data’meta-analysis. Psychol. Med. 2015;45(13):2717–2726. doi: 10.1017/S0033291715000665. [DOI] [PubMed] [Google Scholar]
- Kenter R.M.F., Lundervold A.J., Nordgreen T. A self-guided internet-delivered intervention for adults with ADHD: a protocol for a randomized controlled trial. Internet Interv. 2021;26 doi: 10.1016/j.invent.2021.100485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Adler L.A., Barkley R., Biederman J., Conners C.K., Faraone S.V., et al. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the national comorbidity survey replication. Biol. Psychiatry. 2005;57(11):1442–1451. doi: 10.1016/j.biopsych.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Adler L., Ames M., Demler O., Faraone S., Hiripi E., et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol. Med. 2005;35(2):245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Knouse L.E., Safren S.A. Current status of cognitive behavioral therapy for adult attention-deficit hyperactivity disorder. Psychiatr. Clin. 2010;33(3):497–509. doi: 10.1016/j.psc.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knouse L.E., Teller J., Brooks M.A. Meta-analysis of cognitive–behavioral treatments for adult ADHD. J. Consult. Clin. Psychol. 2017;85(7):737. doi: 10.1037/ccp0000216. [DOI] [PubMed] [Google Scholar]
- Kooij J.S., Buitelaar J.K., Furer J.W., Rijnders C.A.T., Hodiamont P.P. Internal and external validity of attention-deficit hyperactivity disorder in a population-based sample of adults. Psychol. Med. 2005;35(6):817–827. doi: 10.1017/s003329170400337x. [DOI] [PubMed] [Google Scholar]
- Kooij J., Bijlenga D., Salerno L., Jaeschke R., Bitter I., Balazs J., et al. Updated European consensus statement on diagnosis and treatment of adult ADHD. Eur. Psychiatry. 2019;56(1):14–34. doi: 10.1016/j.eurpsy.2018.11.001. [DOI] [PubMed] [Google Scholar]
- Kornør H., Hysing M. 2011. Måleegenskaper ved den norske versjonen av Adult ADHD Self Report Scale, 1.1 (ASRS) [Google Scholar]
- Lundervold A.J., Adolfsdottir S., Halleland H., Halmøy A., Plessen K., Haavik J. Attention network test in adults with ADHD-the impact of affective fluctuations. Behav. Brain Funct. 2011;7(1):1–8. doi: 10.1186/1744-9081-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moëll B., Kollberg L., Nasri B., Lindefors N., Kaldo V. Living SMART—A randomized controlled trial of a guided online course teaching adults with ADHD or sub-clinical ADHD to use smartphones to structure their everyday life. Internet Interv. 2015;2(1):24–31. [Google Scholar]
- Nasri B. Karolinska Institutet; Sweden: 2017. New Approach to the Treatment of Adhd Through Internet and Smartphones: from Impairment to Improvement. [Google Scholar]
- Nordby E.S., Kenter R.M., Lundervold A.J., Nordgreen T. A self-guided internet-delivered intervention for adults with ADHD: a feasibility study. Internet Interv. 2021;25 doi: 10.1016/j.invent.2021.100416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordby E.S., Gjestad R., Kenter R.M., Guribye F., Mukhiya S.K., Lundervold A.J. The effect of SMS reminders on adherence in a self-guided internet-delivered intervention for adults with ADHD. Front. Digit. Health. 2022:67. doi: 10.3389/fdgth.2022.821031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt D., Fone K., Asherson P., Bramble D., Hill P., Matthews K., et al. Evidence-based guidelines for management of attention-deficit/hyperactivity disorder in adolescents in transition to adult services and in adults: recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 2007;21(1):10–41. doi: 10.1177/0269881106073219. [DOI] [PubMed] [Google Scholar]
- Pettersson R., Söderström S., Edlund-Söderström K., Nilsson K.W. Internet-based cognitive behavioral therapy for adults with ADHD in outpatient psychiatric care: a randomized trial. J. Atten. Disord. 2017;21(6):508–521. doi: 10.1177/1087054714539998. [DOI] [PubMed] [Google Scholar]
- Richards D., Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin. Psychol. Rev. 2012;32(4):329–342. doi: 10.1016/j.cpr.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Rozental A., Castonguay L., Dimidjian S., Lambert M., Shafran R., Andersson G., Carlbring P. Negative effects in psychotherapy: commentary and recommendations for future research and clinical practice. BJPsych Open. 2018;4(4):307–312. doi: 10.1192/bjo.2018.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucklidge J.J. Gender differences in attention-deficit/hyperactivity disorder. Psychiatr. Clin. 2010;33(2) doi: 10.1016/j.psc.2010.01.006. 357-73.51. [DOI] [PubMed] [Google Scholar]
- Safren S.A., Sprich S.E., Cooper-Vince C., Knouse L.E., Lerner J.A. Life impairments in adults with medication-treated ADHD. J. Atten. Disord. 2010;13(5):524–531. doi: 10.1177/1087054709332460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg B.S., Haavik J., Halmøy A. Health care services for adults with ADHD: patient satisfaction and the role of psycho-education. J. Atten. Disord. 2019;23(1):99–108. doi: 10.1177/1087054715587941. [DOI] [PubMed] [Google Scholar]
- Spencer T., Biederman J., Wilens T., Harding M., O'Donnell D., Griffin S. Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J. Am. Acad. Child Adolesc. Psychiatry. 1996;35(4):409–432. doi: 10.1097/00004583-199604000-00008. [DOI] [PubMed] [Google Scholar]
- SPSS I . IBM Corp; Armonk, NY: 2018. Corp Ibm SPSS Statistics for Windows, Version 26.0. Released. [Google Scholar]
- Turgay A., Goodman D.W., Asherson P., Lasser R.A., Babcock T.F., Pucci M.L., et al. Lifespan persistence of ADHD: the life transition model and its application. J. Clin. Psychiatry. 2012;73(2):10337. doi: 10.4088/JCP.10m06628. [DOI] [PubMed] [Google Scholar]
- Vidal R., Bosch R., Nogueira M., Gómez-Barros N., Valero S., Palomar G., et al. Psychoeducation for adults with attention deficit hyperactivity disorder vs. Cognitive behavioral group therapy: a randomized controlled pilot study. J. Nerv. Ment. Dis. 2013;201(10):894–900. doi: 10.1097/NMD.0b013e3182a5c2c5. [DOI] [PubMed] [Google Scholar]
- Weiss M., Safren S.A., Solanto M.V., Hechtman L., Rostain A.L., Ramsay J.R., et al. Research forum on psychological treatment of adults with ADHD. J. Atten. Disord. 2008;11(6):642–651. doi: 10.1177/1087054708315063. [DOI] [PubMed] [Google Scholar]
- Weiss M., Murray C., Wasdell M., Greenfield B., Giles L., Hechtman L. A randomized controlled trial of CBT therapy for adults with ADHD with and without medication. BMC Psychiatry. 2012;12(1):1–8. doi: 10.1186/1471-244X-12-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav S.K., Bhat A.A., Hashem S., Nisar S., Kamal M., Syed N., et al. Genetic variations influence brain changes in patients with attention-deficit hyperactivity disorder. Transl. Psychiatry. 2021;11(1):349. doi: 10.1038/s41398-021-01473-w. [DOI] [PMC free article] [PubMed] [Google Scholar]